Abstract
Background
Polymorphic premature ventricular complexes (PVCs) are very common, appearing most frequently in patients with hypertension, obesity, sleep apnea, and structural heart disease. Sympathetic hyperactivity plays a critical role in the development, maintenance, and aggravation of ventricular arrhythmias. Endurance exercise training clearly lowers sympathetic activity in sympatho-excitatory disease states and may be tolerated by patients with chronic kidney disease (CKD).
Methods
We assessed 40 CKD patients with hypertension with polymorphic PVCs. Patients underwent a complete medical history and physical examination. We evaluated the effectiveness of β blocker only or β blocker + exercise during 12 months of follow-up regarding the changes of the numbers of PVCs and mean heart rate (HR) by 24-hour-Holter.
Results
We observed in the β blocker group a significant decrease in the number of polymorphic PVCs from baseline 36,515 ± 3,518 to 3, 6, 9 and 12 months of follow-up, 28,314 ± 2,938, 23,709 ± 1,846, 22,564 ± 1,673, and 22,725 ± 1,415, respectively (P < 0.001). In the β blocker + exercise group a significant decrease in the number of polymorphic PVCs also occurred from baseline 36,091 ± 3,327 to 3, 6, 9 and 12 months of follow-up, 29,252 ± 3,211, 20,948 ± 2,386, 14,238 ± 3,338, and 6,225 ± 2,319, respectively (P < 0.001). Comparisons between the two groups at the same time point showed differences from the sixth month onwards: the 6th (Δ = −2,761, P = 0.045), 9th (Δ = −8,325, P < 0.001) and 12th (Δ = −16,500, P < 0.001) months. There was an improvement during the 12 months of follow-up vs. baseline, after the β blocker or β blocker + exercise in mean 24-hour HR Holter monitoring, creatinine values, eGFR, and ACR.
Conclusion
Polymorphic PVCs may be modifiable by physical activity in CKD patients with hypertension without structural heart disease.
Keywords: β blocker, Physical activity, Polymorphic premature ventricular complexes, Sympathetic hyperactivity, Ventricular arrhythmias
Introduction
Premature ventricular complexes (PVCs) are very common, appearing most frequently in patients with hypertension, obesity, sleep apnea, and structural heart disease [1]. In general, PVCs in the structurally normal heart are considered benign [2], though they have been associated with a more than two-fold higher risk of cardiovascular complications, including stroke [3] and death [4]. PVCs have progressively more been recognized as a primary cause for deteriorating left ventricular (LV) systolic function, and heart failure in some subjects, once apparent causes such as cardiac ischemia, valvular disease, toxic metabolic or infiltrative diseases, and persistent tachycardia has been excluded. The pathogenesis of PVC-mediated cardiomyopathy is uncertain [5,6]. The range of benign outflow tract PVCs sorts from single PVCs to repetitive non-sustained ventricular tachycardia to paroxysmal sustained ventricular tachycardia [7]. In rare circumstances, short-coupled right ventricular outflow tract PVCs can initiate polymorphic ventricular tachycardia [8], while even shorter-coupled PVCs frequently originating from the fascicular system or papillary muscles can trigger ventricular fibrillation [9,10]. However, the best progression of action to pursue PVCs that are polymorphic and refractory to medical management is not clear. Possible treatment options embrace mapping and ablating them one by one or attempting a new, alternative therapy.
Sympathetic hyperactivity plays a key title role in the development, maintenance, and aggravation of ventricular arrhythmias [11]. Recently, Professor Esler’s group suggested that endurance training influences many factors which may mediate a reduction in sympathetic activity [12]. Endurance exercise training obviously lowers sympathetic activity in sympatho-excitatory disease states [13,14] and is well-tolerated by patients with chronic kidney disease (CKD) [15,16]. The outcome of endurance training on renal sympathetic nerve activity has been measured in healthy humans [17], but not in humans with CKD. Thus, proofs of principle studies are required.
Methods
In this study, we conducted a prospective, longitudinal study in 40 CKD, controlled hypertensive and sedentary patients with polymorphic PVCs. At baseline, all of them started to use β blocker (bisoprolol 10 mg). However 20 patients remained sedentary, serving as a control group, and the other 20 subjects began to practice physical activity (starting with 150 minutes of moderate activity per week, as recommended by the Brazilian Ministry of Health, and increasing progressively until 300 minutes of moderate to intensive exercise per week). The study was piloted in accordance with the Helsinki Declaration and approved by the Ethics Committee of Hospital e Clínica São Gonçalo (HCSG2013-004). All patients signed the written informed consent before inclusion. In the present study, we aim to evaluate the effects of the exercise in the changes of the numbers of PVCs and heart rate (HR) by 24-hour-Holter, modifications in estimated glomerular filtration rate (eGFR) and the albumin:creatinine ratio (ACR) in all patients.
Definition of polymorphic PVCs
Polymorphic PVCs were defined as 3 or more PVCs of different morphologies in a high incidence each one.
Study subjects
This study was conducted in the state of Rio de Janeiro, Brazil in the Hospital e Clínica São Gonçalo. Patients were recruited from January 2014 to December 2015 and were derived from Arrhythmias and Artificial Cardiac Pacing Service of the same hospital. Patients who had the combination of the following criteria were consecutively enrolled: 1) mean 24-hour systolic ambulatory blood pressure measurements (ABPM) < 130/< 80 mmHg; 2) age between 18 and 70 years; 3) structurally normal heart to myocardial scintigraphy and transthoracic echocar-diography, without ischemia, fibrosis area or any other illness, with a LV ejection fraction of > 50% as measured by echocardiography (Simpson’s method); 4) presenting > 25,000 polymorphic PVCs in 24-hour-Holter monitoring at baseline; 5) experience symptoms such as dyspnea, palpitation, dizziness, pre-syncope or syncope; 6) not having undergone previous treatment; 7) glomerular filtration rate estimated by the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equation, eGFR [18] < 60 mL/min/1.73 m2; and 8) be able to read, understand and sign the informed consent form.
Patients with any of the following criteria were excluded: 1) pregnancy; 2) valvular disease with significant hemodynamic repercussions; 3) myocardial infarction, unstable angina, stroke or transient ischemic attack within the previous 6 months; 4) mobility deficit; 5) psychiatric disease; 6) patients unable to be followed clinically; 7) patient known to have drug addiction or alcohol, can affect the ability to understand or follow medical instructions; 8) patient has a serious disease, which in the opinion of the investigator, may adversely affect the safety and/or efficacy of the participant or the study.
24-hour-Holter monitoring
Patients underwent a 24-hour-Holter monitoring (Galix Biomedical Instrumentation, Miami, FL, USA). A 3-channel recorder was used to record the electrocardiographic traces, calculate the mean HR, the quantity and the morphologies of PVCs at baseline, 3, 6, 9 and 12 months after β blocker only or β blocker + exercise onset.
24-hour ABPM
ABPM was performed for 24 hours at baseline with a clinically validated device (CardioMapa; Cardios, São Paulo, Brazil). The device was set to measure every 15 minutes during the day (06:00 to 22:00) and every 30 minutes during sleep (22:00 to 06:00). Patients were instructed to continue their regular activities during the recording and go to bed no later than 23:00. The waking period typically included 08:00 to 22:00 and the sleep period 24:00 to 06:00 [19]. All individuals were trained to record in a diary their sleeping and waking hours, meals, intake of medications, and any symptoms or events that could influence blood pressure during this period. Measurements were transferred to a computer for analysis. Monitoring was repeated as necessary until ≥ 70% of the measured values obtained during both daytime and nighttime were satisfactory [20].
Transthoracic echocardiography
Transthoracic echocardiography was performed at baseline using a Vivid I ultrasound system (General Electric, Frankfurt, Germany) equipped with a multifre-quency transducer and tissue Doppler imaging software, according to the guidelines of the American Society of Echocardiography [21]. Data were analyzed and interpreted by one experienced echocardiographer who was blinded to treatment status and imaging sequence. The LV mass was calculated from the LV linear dimensions using the Devereux formula [21,22] and normalized to body surface area (BSA) [21,23]. LV hypertrophy was considered to be present when the LV mass exceeded 115 g/ m2 for men and 95 g/m2 for women [21]. The left atrial (LA) volume was measured using a disk sum algorithm similar to that used to measure LV volume [24,25] and normalized to BSA. Although the LA size depends on sex, variation due to sex is generally recognized when it is normalized to the BSA [26]. Furthermore, whereas several methods of normalizing this measurement have been proposed [27,28], normalizing to BSA produces the most reliable data. Normalizing to BSA compensates for sexual dimorphism in LA size, so only the normalized value is reported. The recommended highest value for LA size is 34 mL/m2[28–31] .
Study procedures and assessment
In this study, we assessed 40 CKD patients with hypertension with polymorphic PVCs. Patients underwent a complete medical history and physical examination. We evaluated the effectiveness of β blocker only or β blocker + exercise onset during 12 months of follow-up regarding the changes of the numbers of PVCs and mean HR by 24-hour-Holter. The follow-up was performed quarterly after the interventions. The renal function was also monitored during the follow-up period.
Statistical analysis
The results were expressed as the mean and standard deviation of the mean in the case of normal distribution and as the median with interquartile range otherwise. Statistical tests were all two sided. Comparisons between two-paired values were performed by the paired t-test in case of a Gaussian distribution or, alternatively, by the Wilcoxon test. Comparisons between more than two-paired values were performed by ANOVA for repeated measures or with Kruskal–Wallis ANOVA as appropriate complemented by a post-hoc test. Frequencies were compared with Fisher’s exact test. P-values < 0.05 were considered significant. Correlations between two variables were performed by Pearson in the case of a Gaussian distribution or, alternatively, with the Spearman correlation test. All statistical analysis was performed using the program Graphpad Prism v 7.0 (Graphpad software, La Jolla, CA, USA).
Results
Baseline characteristics of patients and effects on the number of polymorphic PVCs
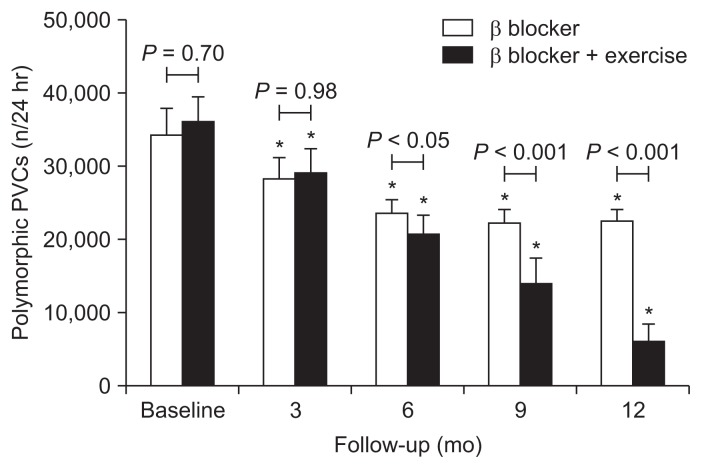
General features of the 40 subjects are listed in Table 1. We observed in the β blocker group a significant decrease in the number of polymorphic PVCs from baseline 36,515 ± 3,518 to 3, 6, 9 and 12 months of follow-up, 28,314 ± 2,938, 23,709 ± 1,846, 22,564 ± 1,673, and 22,725 ± 1,415, respectively (P < 0.001 to all the comparisons between the mean of each time point vs. baseline). In the β blocker + exercise group a significant decrease in the number of polymorphic PVCs also occurred from baseline 36,091 ± 3,327 to 3, 6, 9 and 12 months of follow-up, 29,252 ± 3,211, 20,948 ± 2,386, 14,238 ± 3,338, and 6,225 ± 2,319, respectively (P < 0.001 to all the comparisons between the mean of each time point vs. baseline) as shown in Fig. 1. Comparisons between the two groups at the same time point just showed differences from the sixth month onwards: at the 6th (Δ = −2,761, P = 0.045), 9th (Δ = −8,325, P < 0.001) and 12th (Δ = −16,500, P < 0.001) months.
Table 1.
General features of patients at baseline
| Parameter | β blocker (n = 20) | β blocker + exercise (n = 20) | P |
|---|---|---|---|
| Age (yr) | 58 ± 12 | 62 ± 10 | 0.24 |
| Body mass index (kg/m2) | 26.4 ± 2.6 | 25.4 ± 2.1 | 0.19 |
| Male gender | 12 (60.0) | 15 (75.0) | 0.50 |
| White ethnicity | 17 (85.0) | 14 (70.0) | 0.45 |
| Polymorphic PVCs | 34,515 ± 3,518 | 36,091 ± 3,327 | 0.70 |
| Type 2 Diabetes mellitus | 10 (50.0) | 8 (40.0) | 0.75 |
| Antihypertensive | |||
| ACE-inhibitors/ARB | 20 (100) | 20 (100) | 1.00 |
| Diuretics | 20 (100) | 20 (100) | 1.00 |
| DHP Ca++ channel blockers | 20 (100) | 20 (100) | 1.00 |
| Clonidine | 12 (60.0) | 10 (50.0) | 0.75 |
| Echocardiographic parameters | |||
| Indexed left atrial volume (mL/m2) | 29.8 ± 3.0 | 31.5 ± 4.2 | 0.15 |
| Interventricular septum tickness (mm) | 10.6 ± 0.7 | 11.0 ± 0.9 | 0.13 |
| LVPWT (mm) | 9.1 ± 1.0 | 9.4 ± 0.7 | 0.28 |
| LVEF, Simpson (%) | 65.4 ± 10.0 | 66.5 ± 12.2 | 0.76 |
| LVEDD (mm) | 45.4 ± 3.5 | 43.8 ± 5.1 | 0.25 |
| LVESD (mm) | 31.7 ± 5.2 | 32.0 ± 6.3 | 0.87 |
| LV mass index (g/m2) | 88.5 ± 13.2 | 97.4 ± 17.5 | 0.08 |
Values are expressed as mean ± standard deviation or number (%).
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; DHP, dihydropyridine; LV, left ventricular; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic diameter; LVPWT, left ventricular posterior wall thickness; PVCs, premature ventricular complexes.
Figure 1. Amount of polymorphic premature ventricular complexes (PVCs).
Decreasing in the number of polymorphic PVCs during the follow-up in β blocker (n = 20) and β blocker + exercise (n = 20) groups. *P < 0.001 to the comparison between baseline and mean of each respective column across the time. Values are presented as mean ± standard deviation.
Effects on renal function and mean heart rate
The changes during the 12 months of follow-up vs. baseline and between groups, after the β blocker or β blocker + exercise onset in mean 24-hour HR Holter monitoring, creatinine values, eGFR, and ACR are displayed in Table 2.
Table 2.
Mean 24-hour heart rate Holter monitoring, ABPM and renal function at baseline and during follow-up
| Parameter | β blocker (n = 20) | β blocker + exercise (n = 20) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Baseline | 3 mo | 6 mo | 9 mo | 12 mo | Baseline | 3 mo | 6 mo | 9 mo | 12 mo | |
| Mean 24-hour ABPM (mmHg) | ||||||||||
| Systolic | 126 ± 2.4 | 118 ± 2.5** | 119 ± 2.6** | 117 ± 2.3** | 116 ± 2.6** | 125 ± 2.9 | 117 ± 3.2** | 116 ± 3.5**† | 115 ± 3.1**† | 112 ± 2.6**† |
| Diastolic | 76 ± 2.9 | 71 ± 2.0** | 68 ± 1.9** | 66 ± 1.8** | 64 ± 1.8** | 75 ± 2.7 | 65 ± 2.4**†† | 62 ± 1.3**†† | 61 ± 1.0**†† | 61 ± 0.8**†† |
| Mean 24-hour HR Holter monitoring (bpm) | 81.5 ± 5.1 | 70.3 ± 3.9** | 69.5 ± 3.1** | 67.1 ± 3.8** | 64.8 ± 2.6** | 81.2 ± 4.6 | 72.9 ± 3.1** | 67.5 ± 3.2** | 58.3 ± 3.5**†† | 55.7 ± 3.3**†† |
| Creatinine (mg/dL) | 1.88 ± 0.33 | – | 1.95 ± 0.3* | – | 2.06 ± 0.29* | 1.91 ± 0.32 | – | 1.73 ± 0.30** | – | 1.60 ± 0.29**† |
| eGFR (mL/min/1.73 m2) | 36.3 ± 10.3 | – | 34.4 ± 8.2 | – | 31.8 ± 6.8* | 35.9 ± 9.8 | – | 41.0 ± 12.7** | – | 44.8 ± 13.3**† |
| ACR (mg/g) | 80.6 ± 21.7 | – | 85.6 ± 22.8* | – | 94.9 ± 20.8** | 83.1 ± 22.9 | – | 74.3 ± 21.4** | – | 65.1 ± 19.3**† |
Values presented as mean ± standard deviation.
ABPM, ambulatory blood pressure measurements; ACR, albumin:creatinine ratio; eGFR, estimated glomerular filtration rate; HR, heart rate.
P < 0.05 and
P < 0.001 vs. baseline values,
P < 0.05 and
P < 0.001 to the comparison of the means between groups in the same time point.
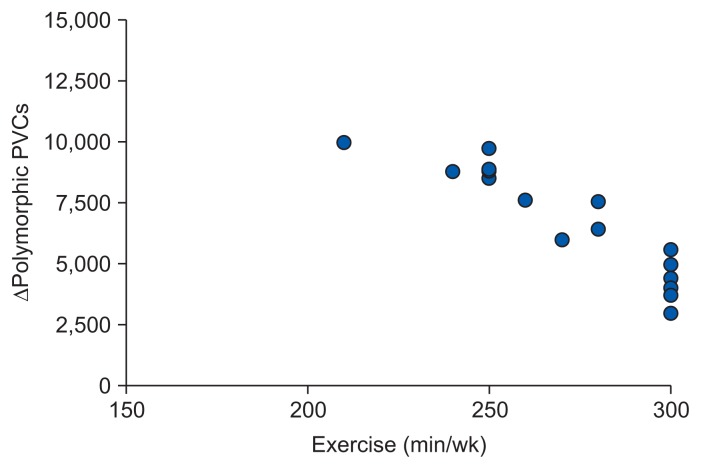
Correlation
A significant correlation was found between the variation (Δ) number of polymorphic PVCs at the 12th month (r = −0.933, 95% confidence interval = −0.974 to −0.836, P < 0.001) after the onset of physical activity and the total time of exercise performed per week, as shown in Fig. 2.
Figure 2. Correlation.
A significant correlation was found between the variation (Δ) number of polymorphic premature ventricular complexes (PVCs) at the 12th month (r = −0.933, 95% confidence interval = −0.974 to −0.836, P < 0.001) after the onset of physical activity and the total time of exercise performed per week.
Discussion
We believe that sympathetic hyperactivity is closely related to the appearance of PVCs. Sympathetic overactivity plays a critical role in the development, maintenance, and aggravation of ventricular arrhythmias [11]. Indeed, there is growing appreciation for the role of the sympathetic system in this setting. The effect of endurance training on renal sympathetic nerve activity has been measured in healthy humans [17], but not in humans with CKD. Thereafter, identifying the ideal patient population should be considered, as most exercise training studies in patients with CKD include only the healthiest of patients, which may limit the generalizability of the findings [32]. Optimization of standard training principles, exercise frequency, intensity, time and type may all influence physiological adaptations and thus need to be studied. The duration of previous studies in clinical populations has typically been 4 months of training at a moderate intensity, 3 days/week while studies in healthy populations have been considerably shorter in duration [13]. Longer duration interventions (≥ 4 months) are more effective in lowering sympathetic activity in other clinical populations, thus Professor Esler’s group recommend adopting a similar approach in patients with CKD [12], because it was previously proved in healthy individuals that intense endurance training has a more pronounced effect on autonomic balance [33], which may be beneficial to patients with high sympathetic tone.
Our findings showed that after the physical activity onset, the number of PVCs and the mean 24-hour HR Holter monitoring decreased during the follow-up period in comparison to baseline and vs. sedentary group. As well, the creatinine values and the ACR reduced. Consequently, the eGFR increased. A significant correlation was found between the Δ number of polymorphic PVCs at the 12th month after the onset of physical activity and the total time of exercise performed per week. In conclusion, our data suggest that the long-term exercise can reduce ventricular arrhythmias and improve the renal function.
This study has some limitations. The non-use of cardiac magnetic resonance occurred because the use of gadolinium, which could lead to nephrogenic systemic fibrosis in chronic kidney disease population [34]. We chose patients with structurally normal heart, to make sure there were no other mechanisms involved in the genesis and maintenance of polymorphic PVCs, beyond the hypothetical mechanisms, aforementioned.
Whilst there was an improvement in the number of polymorphic PVCs, and renal function in the β blocker + exercise group in comparison to β blocker group, these findings should be interpreted with caution given the unblinded non-randomised nature of the study. A randomised trial with appropriate concealment of treatment, more patients and for a long follow-up period is required to address the potential benefits of physical activity in polymorphic PVCs.
In conclusion, polymorphic PVCs may be modifiable by physical activity in CKD patients with hypertension without structural heart disease according to the aforementioned results. Although encouraging, our data are preliminary and need to be validated in a large population and in the long term.
Acknowledgments
The authors thank all the participants in this study, especially, to Pacemed by stimulating the development of research and for the technical support. This study was funded by Pacemed.
Footnotes
Conflicts of interest
All authors have no conflicts of interest to declare.
References
- 1.Noheria A, Deshmukh A, Asirvatham SJ. Ablating premature ventricular complexes: justification, techniques, and outcomes. Methodist Debakey Cardiovasc J. 2015;11:109–120. doi: 10.14797/mdcj-11-2-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kennedy HL, Whitlock JA, Sprague MK, Kennedy LJ, Buckingham TA, Goldberg RJ. Long-term follow-up of asymptomatic healthy subjects with frequent and complex ventricular ectopy. N Engl J Med. 1985;312:193–197. doi: 10.1056/NEJM198501243120401. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal SK, Heiss G, Rautaharju PM, Shahar E, Massing MW, Simpson RJ., Jr Premature ventricular complexes and the risk of incident stroke: the Atherosclerosis Risk In Communities (ARIC) Study. Stroke. 2010;41:588–593. doi: 10.1161/STROKEAHA.109.567800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ataklte F, Erqou S, Laukkanen J, Kaptoge S. Meta-analysis of ventricular premature complexes and their relation to cardiac mortality in general populations. Am J Cardiol. 2013;112:1263–1270. doi: 10.1016/j.amjcard.2013.05.065. [DOI] [PubMed] [Google Scholar]
- 5.Adams JC, Srivathsan K, Shen WK. Advances in management of premature ventricular contractions. J Interv Card Electrophysiol. 2012;35:137–149. doi: 10.1007/s10840-012-9698-x. [DOI] [PubMed] [Google Scholar]
- 6.Lee GK, Klarich KW, Grogan M, Cha YM. Premature ventricular contraction-induced cardiomyopathy: a treatable condition. Circ Arrhythm Electrophysiol. 2012;5:229–236. doi: 10.1161/CIRCEP.111.963348. [DOI] [PubMed] [Google Scholar]
- 7.Kim RJ, Iwai S, Markowitz SM, Shah BK, Stein KM, Lerman BB. Clinical and electrophysiological spectrum of idiopathic ventricular outflow tract arrhythmias. J Am Coll Cardiol. 2007;49:2035–2043. doi: 10.1016/j.jacc.2007.01.085. [DOI] [PubMed] [Google Scholar]
- 8.Noda T, Shimizu W, Taguchi A, Aiba T, Satomi K, Suyama K, Kurita T, Aihara N, Kamakura S. Malignant entity of idiopathic ventricular fibrillation and polymorphic ventricular tachycardia initiated by premature extrasystoles originating from the right ventricular outflow tract. J Am Coll Cardiol. 2005;46:1288–1294. doi: 10.1016/j.jacc.2005.05.077. [DOI] [PubMed] [Google Scholar]
- 9.Scheinman MM. Role of the His-Purkinje system in the genesis of cardiac arrhythmia. Heart Rhythm. 2009;6:1050–1058. doi: 10.1016/j.hrthm.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Santoro F, Di Biase L, Hranitzky P, Sanchez JE, Santangeli P, Perini AP, Burkhardt JD, Natale A. Ventricular fibrillation triggered by PVCs from papillary muscles: clinical features and ablation. J Cardiovasc Electrophysiol. 2014;25:1158–1164. doi: 10.1111/jce.12478. [DOI] [PubMed] [Google Scholar]
- 11.Leenen FH. Cardiovascular consequences of sympathetic hyperactivity. Can J Cardiol. 1999;15(Suppl A):2A–7A. [PubMed] [Google Scholar]
- 12.Howden EJ, Lawley JS, Esler M, Levine BD. Potential role of endurance training in altering renal sympathetic nerve activity in CKD? Auton Neurosci. 2017;204:74–80. doi: 10.1016/j.autneu.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Carter JR, Ray CA. Sympathetic neural adaptations to exercise training in humans. Auton Neurosci. 2015;188:36–43. doi: 10.1016/j.autneu.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 14.Haack KK, Zucker IH. Central mechanisms for exercise training-induced reduction in sympatho-excitation in chronic heart failure. Auton Neurosci. 2015;188:44–50. doi: 10.1016/j.autneu.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howden EJ, Coombes JS, Strand H, Douglas B, Campbell KL, Isbel NM. Exercise training in CKD: efficacy, adherence, and safety. Am J Kidney Dis. 2015;65:583–591. doi: 10.1053/j.ajkd.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 16.Stray-Gundersen J, Howden EJ, Parsons DB, Thompson JR. Neither hematocrit normalization nor exercise training restores oxygen consumption to normal levels in hemodialysis patients. J Am Soc Nephrol. 2016;27:3769–3779. doi: 10.1681/ASN.2015091034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meredith IT, Friberg P, Jennings GL, Dewar EM, Fazio VA, Lambert GW, Esler MD. Exercise training lowers resting renal but not cardiac sympathetic activity in humans. Hypertension. 1991;18:575–582. doi: 10.1161/01.HYP.18.5.575. [DOI] [PubMed] [Google Scholar]
- 18.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O’Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B Management of Arterial Hypertension of the European Society of Hypertension; European Society of Cardiology. 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2007;25:1105–1187. doi: 10.1097/HJH.0b013e3281fc975a. [DOI] [PubMed] [Google Scholar]
- 20.Stergiou GS, Kollias A, Destounis A, Tzamouranis D. Automated blood pressure measurement in atrial fibrillation: a systematic review and meta-analysis. J Hypertens. 2012;30:2074–2082. doi: 10.1097/HJH.0b013e32835850d7. [DOI] [PubMed] [Google Scholar]
- 21.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458. doi: 10.1016/0002-9149(86)90771-X. [DOI] [PubMed] [Google Scholar]
- 23.Mosteller RD. Simplified calculation of body-surface area. N Engl J Med. 1987;317(1098) doi: 10.1056/NEJM198710223171717. [DOI] [PubMed] [Google Scholar]
- 24.Thomas L, Levett K, Boyd A, Leung DY, Schiller NB, Ross DL. Compensatory changes in atrial volumes with normal aging: is atrial enlargement inevitable? J Am Coll Cardiol. 2002;40:1630–1635. doi: 10.1016/S0735-1097(02)02371-9. [DOI] [PubMed] [Google Scholar]
- 25.Yamaguchi K, Tanabe K, Tani T, Yagi T, Fujii Y, Konda T, Kawai J, Sumida T, Morioka S, Kihara Y. Left atrial volume in normal Japanese adults. Circ J. 2006;70:285–288. doi: 10.1253/circj.70.285. [DOI] [PubMed] [Google Scholar]
- 26.Kou S, Caballero L, Dulgheru R, Voilliot D, De Sousa C, Kacharava G, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Gomez De Diego JJ, Hagendorff A, Henri C, Hristova K, Lopez T, Magne J, De La Morena G, Popescu BA, Penicka M, Ozyigit T, Rodrigo Carbonero JD, Salustri A, Van De Veire N, Von Bardeleben RS, Vinereanu D, Voigt JU, Zamorano JL, Donal E, Lang RM, Badano LP, Lancellotti P. Echocardiographic reference ranges for normal cardiac chamber size: results from the NORRE study. Eur Heart J Cardiovasc Imaging. 2014;15:680–690. doi: 10.1093/ehjci/jet284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pritchett AM, Jacobsen SJ, Mahoney DW, Rodeheffer RJ, Bailey KR, Redfield MM. Left atrial volume as an index of left atrial size: a population-based study. J Am Coll Cardiol. 2003;41:1036–1043. doi: 10.1016/S0735-1097(02)02981-9. [DOI] [PubMed] [Google Scholar]
- 28.Vasan RS, Levy D, Larson MG, Benjamin EJ. Interpretation of echocardiographic measurements: a call for standardization. Am Heart J. 2000;139:412–422. doi: 10.1016/S0002-8703(00)90084-X. [DOI] [PubMed] [Google Scholar]
- 29.Spencer KT, Mor-Avi V, Gorcsan J, 3rd, DeMaria AN, Kimball TR, Monaghan MJ, Perez JE, Weinert L, Bednarz J, Edelman K, Kwan OL, Glascock B, Hancock J, Baumann C, Lang RM. Effects of aging on left atrial reservoir, conduit, and booster pump function: a multi-institution acoustic quantification study. Heart. 2001;85:272–277. doi: 10.1136/heart.85.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knutsen KM, Stugaard M, Michelsen S, Otterstad JE. M-mode echocardiographic findings in apparently healthy, non-athletic Norwegians aged 20–70 years. Influence of age, sex and body surface area. J Intern Med. 1989;225:111–115. doi: 10.1111/j.1365-2796.1989.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y, Gutman JM, Heilbron D, Wahr D, Schiller NB. Atrial volume in a normal adult population by two-dimensional echocardiography. Chest. 1984;86:595–601. doi: 10.1378/chest.86.4.595. [DOI] [PubMed] [Google Scholar]
- 32.Howden EJ, Fassett RG, Isbel NM, Coombes JS. Exercise training in chronic kidney disease patients. Sports Med. 2012;42:473–488. doi: 10.2165/11630800-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 33.Iwasaki K, Zhang R, Zuckerman JH, Levine BD. Dose-response relationship of the cardiovascular adaptation to endurance training in healthy adults: how much training for what benefit? J Appl Physiol. 1985;2003;95:1575–1583. doi: 10.1152/japplphysiol.00482.2003. [DOI] [PubMed] [Google Scholar]
- 34.Bernstein EJ, Schmidt-Lauber C, Kay J. Nephrogenic systemic fibrosis: a systemic fibrosing disease resulting from gadolinium exposure. Best Pract Res Clin Rheumatol. 2012;26:489–503. doi: 10.1016/j.berh.2012.07.008. [DOI] [PubMed] [Google Scholar]