Abstract
Asthma is a chronic inflammatory disease of the lungs which has been thought to arise as a result of inappropriately directed T helper type-2 (Th2) immune responses of the lungs to otherwise innocuous inhaled antigens. Current asthma therapeutics are directed towards the amelioration of downstream consequences of type-2 immune responses (i.e. β-agonists) or broad-spectrum immunosuppression (i.e. corticosteroids). However, few approaches to date have been focused on the primary prevention of immune deviation. Advances in molecular phenotyping reveal heterogeneity within the asthmatic population with multiple endotypes whose varying expression depends on the interplay between numerous environmental factors and the inheritance of a broad range of susceptibility genes. The most common endotype is one described as “type-2-high” (i.e. high levels of interleukin [IL]-13, eosinophilia, and periostin). The identification of multiple endotypes has provided a potential explanation for the observations that therapies directed at typical Th2 cytokines (IL-4, IL-5, and IL-13) and their receptors have often fallen short when they were tested in a diverse group of asthmatic patients without first stratifying based on disease endotype or severity. However, despite the incorporation of endotype-dependent stratification schemes into clinical trial designs, variation in drug responses are still apparent, suggesting that additional genetic/environmental factors may be contributing to the diversity in drug efficacy. Herein, we will review recent advances in our understanding of the complex pathways involved in the initiation and regulation of type-2-mediated immune responses and their modulation by host factors (genetics, metabolic status, and the microbiome). Particular consideration will be given to how this knowledge could pave the way for further refinement of disease endotypes and/or the development of novel therapeutic strategies for the treatment of asthma .
Keywords: asthma, Th2 inflammation, cytokines, alarmins, cellular metabolism, signalling, allergic inflammation
Introduction
Asthma is a phenotypically heterogeneous inflammatory disease of the lungs generally characterized by airflow obstruction and airway inflammation. Advances in molecular phenotyping reveal heterogeneity within the asthmatic population with multiple endotypes 1– 3 whose varying expression depends on the interplay between numerous environmental factors and the inheritance of a broad range of susceptibility genes. Patients with a type-2-high profile are found in half of the mild asthmatic patients and are reported to be responsive to steroids 3, 4. The type-2-high asthma endotype is one of the most consistent endotypes to emerge 3– 9. This common subtype of asthma is characterized by the release of signature cytokines interleukin (IL)-4, IL-5, and IL-13 from cells of both the innate and the adaptive immune systems. These type-2 cytokines are targets for pharmaceutical intervention, and a number of therapeutic options are under clinical investigation for asthma. These will be discussed in detail below. The identification of multiple endotypes has provided an explanation for the observations that therapies directed at these typical T helper type-2 (Th2) cytokines and their receptors have often fallen short when they were tested in a diverse group of asthmatic patients without first stratifying based on disease endotype or severity. The stratification of patients in clinical trials based on specific endotypes has lent support for continued efforts to modify IL-4 and IL-13 pathways in type-2-high asthma, yet additional variation in treatment response is still apparent. These results suggest that regulation of type-2 cytokine production and responsiveness is more complex than was previously appreciated and that other genetic/environmental factors may be contributing to the diversity in drug response. As many ongoing efforts are designed to target the type-2 immune response, it is critical to fully understand the intricacies of regulation of this arm of the immune response. In this review, we will discuss new insights into the mechanisms by which IL-4- and IL-13-mediated inflammation is initiated, enhanced, perpetuated, or inhibited, with a focus on new players that modulate IL-4 and IL-13 responses. Although we will touch briefly on IL-5 as an additional important Th2 cytokine in promoting the allergic inflammatory response, we will focus our comments here on IL-4 and IL-13. We will highlight how some of the new pathways that influence IL-4 and IL-13 responses might potentially be harnessed for therapeutic benefit to downregulate type-2 immune responses in type-2-high asthmatics.
Role of canonical Th2 pathways in allergic inflammation
The Th2 immune response is characterized by the expansion of CD4 + T cells producing the prototypical Th2 cytokines IL-4, IL-13, and IL-5. Although IL-9 was originally thought to be produced by Th2 cells, more recent studies suggest that it is primarily produced by a unique CD4 + T cell subset referred to as Th9 10, 11. More recent studies show that other cell types such as type-2 innate lymphoid cells (ILC2s), mast cells, and eosinophils also produce these type-2-associated cytokines. These cytokines act on multiple cell types and trigger the hallmark features of a type-2 immune response, including the synthesis of immunoglobulin (Ig)E, eosinophilia, mast cell activation, mucus cell hyperplasia, and macrophage polarization. Although a type-2 immune response is critical in host defense against helminth infections, inappropriate activation of type-2 responses against otherwise innocuous antigens leads to allergic responses in different barrier organs, such as the skin, gut, and lungs.
Aberrant production of the prototypical type-2 cytokines IL-4 and IL-13 has long been associated with the pathogenesis of allergic disorders 12, 13. The overproduction of mucus resulting in airway obstruction in asthma is an effect of IL-4/IL-13 action on goblet cells, inducing mucin gene expression, hyperplasia, and hypertrophy 14. IL-4 and IL-13 also have direct effects on airway smooth muscle cells that may explain the hypercontractility of these cells in the airways of asthmatics 15. IL-4 and IL-13 also induce chemokine release from airway smooth muscle cells 16. The activity of IL-4 and IL-13 on the structural cells of the lung such as vascular endothelial cells and airway epithelial cells elicits the expression of adhesion molecules, chemokines, and transforming growth factor (TGF)-β production. These molecules direct the influx of circulating inflammatory cells, such as eosinophils, basophils, and others, to the lung tissue and airway lumen and induce lung tissue remodeling. Neutrophils also migrate into the lungs during allergic inflammation, but they are particularly elevated in patients with severe asthma. These patients are different from the type-2-high endotype and their disease is believed to be driven by Th17-mediated inflammation. As such, they are also typically unresponsive to the IL-4-/IL-13-directed therapies discussed in the previous section and to treatment with corticosteroids. IL-4 enhances the capacity of dendritic cells (DCs) to stimulate T cell secretion of Th2 cytokines, whereas IL-13 enhances the capacity of DCs to suppress T cell secretion of interferon (IFN)-γ in mice 17. Both IL-4 and IL-13 increase DC antigen uptake 18, 19 and cell migration into the lymph nodes where they prime naive T cells to differentiate into Th2 cells 20. B cell class switching to production of IgE is driven by IL-4 21, 22 and by IL-13 in human but not in mouse B cells, which lack IL-13 receptor α1 (IL-13Rα1) 23. Fibroblast responses to IL-4 and IL-13 contribute indirectly to the lung remodeling that occurs in chronic asthma by eliciting the production of adhesion molecules and chemokines as well as cytokines that then stimulate epithelial cells to secrete TGF-β1 24.
The eosinophilia observed in asthma and allergic diseases is partially controlled by the Th2 cytokine IL-5. IL-5 is critical for the genesis (in the bone marrow) 23, growth 24, 25, and survival of eosinophils. Eosinophils are a key target of therapeutic strategies in the treatment of allergic disease because of their ability to cause tissue damage and inflammation following the activation and release of a toxic mixture of their different granule proteins in inflamed tissue. IL-5 acts on eosinophils by binding to its receptor (IL-5R), which is a heterodimer composed of two chains: one α subunit (which binds IL-5) and one β subunit (which is implicated in signal transduction) 25. Accordingly, blocking IL-5 with antibodies has been useful at lowering peripheral and sputum eosinophil counts in asthmatics. While several studies indicate that anti-IL-5 treatment had no effect on improvement in quality of life measures in asthmatics compared to placebo controls 26, others have demonstrated that patients have fewer exacerbations concomitant with reduction in blood eosinophil counts 27. Beyond blocking IL-5, blocking the IL-5 receptor has also been an important therapeutic target against asthma. Currently, two anti-IL-5 antibodies are FDA approved for use in asthmatics older than 12 years of age 27, and a third antibody, which binds the IL-5Rα, is now in phase III clinical trials 28. However, as mentioned above, blocking IL-5 alone is not sufficient to decrease asthma severity. Future trials combining the blockade of IL-5/IL-5R together with other therapies will provide more robust strategies to improve quality of life in asthmatic patients.
Lung macrophages (alveolar and interstitial macrophages) are critical regulators of lung homeostasis and the inflammatory response to inhaled allergens 29. Similar to T cells, lung macrophages that encounter IL-4 and IL-13 polarize into a distinct phenotype, formerly known as “alternatively activated” or M2 macrophages. M2 macrophages express arginase I (ARG1) and other hallmark M2 gene products, such as YM1 and Found in Inflammatory Zone (FIZZ)1 in mice 30. This is in contrast to Th1 cytokines, viruses, and microbes that induce skewing to M1 macrophages and that express inducible nitric oxide synthase (iNOS), IL-1β, tumor necrosis factor (TNF)-α, and other pro-inflammatory mediators 31. Although both M1 and M2 macrophages are found in the lung during the course of allergic inflammation, M2 macrophages are increased in the lungs of asthmatics compared to healthy controls, and their abundance correlates with declines in lung function 32– 38. Mouse models of allergic inflammation recapitulate the observations in humans 39– 42. Adoptive transfer experiments revealed that the transfer of IL-4Rα-sufficient macrophages, but not IL-4Rα-deficient macrophages, into RAG2 –/– mice was sufficient for the development of allergen-driven lung eosinophilia 40.
M2 macrophages are thought to promote allergic lung inflammation through the secretion of angiogenic and pro-fibrotic factors, including vascular endothelial growth factor, insulin-like growth factor (IGF)-I, TGF-β1, matrix metalloproteinases (MMPs), acidic mammalian chitinase (AMCase), BRP-39/YKL-40 43, and FIZZ1 44– 46, that have the potential to promote lung remodeling. M2 macrophages also produce many inflammatory cell-recruiting chemokines (CCL11, 24, and 26, YM1, and others) that recruit eosinophils, basophils, T cells, and other immune cell types to the inflamed lung. Lastly, M2 macrophages have immunomodulatory properties also through direct and indirect effects on T cells, airway epithelium, and DCs 47– 49. Since alveolar macrophages are one of the “first responders” to inhaled allergens and owing to their key role in immunomodulation and maintaining homeostasis, modifying their phenotype and function is an attractive concept for intervention.
In the section below, we will describe how IL-4 and IL-13 regulate most of the features of allergic inflammation through their interaction with the IL-4/IL-13 receptor complexes and downstream signaling in multiple cell types. We will also highlight how new insights into these processes could provide opportunities for the development of therapeutic intervention in asthmatics.
IL-4 and IL-13 cytokine receptor regulation
IL-4 and IL-13 are functionally and structurally related cytokines that have both overlapping and unique biological responses owing, in part, to the utilization of a combination of shared and unique receptors 12, 50, 51. IL-4 is recognized by two types of membrane receptors, type I (IL-4Rα and the common gamma-chain [γc]) and type II (IL-4Rα and IL-13Rα1), while IL-13 is recognized only by the type II IL-4 receptor. IL-13 is also bound with incredibly high affinity by IL-13Rα2, which exists in membrane-bound and soluble forms. IL-4 promotes and maintains the polarization of Th2 cells through ligating the type I IL-4R 52, whereas IL-13 has no effect on T cells because of their lack of IL-13Rα1 expression. On the other hand, IL-13 is thought to be more important in the induction of the physiological aspects of allergic asthma, including airway hyper-responsiveness (AHR), mucus hypersecretion, airway smooth muscle alterations, and subepithelial fibrosis, than IL-4 52, 53. The exact molecular mechanism(s) by which these two cytokines regulate distinct features of the allergic response and how their contributions, either individually or in concert, induce the pathophysiological manifestations of disease remain to be fully uncovered. Recent discoveries of differences in utilization/assembly and affinity of IL-4 and IL-13 for the type-2 receptor and the regulation of the receptors along with the discovery of unique ILC2s which preferentially produce IL-13, and not IL-4, are beginning to shed light on these mysteries 12. Moreover, the identification of new cellular and molecular pathways affecting the regulation of IL-4/IL-13 receptor chains is painting a very complex picture in which a series of intricate feedback loops serve to keep the expression of type-2 inflammation in check. Understanding this delicate balance and how it is disturbed in asthma may inform the development of novel therapeutic approaches for the treatment of asthma.
IL-4Rα
Given the importance of IL-4Rα in triggering Th2 inflammation 54, 55 and the strong association between polymorphisms in this gene and asthma risk 56– 58, understanding the mechanisms by which IL-4Rα expression is controlled is critical. In this regard, recent studies suggest a role for STUB1 (STIPI homology and U-box-containing protein 1), a chaperone-dependent E3 ubiquitin ligase 59 which interacts with IL-4Rα and targets it for proteasomal degradation to regulate signaling. STUB1-deficient mice show spontaneous airway inflammation, alternative M2 activation, and increased serum IgE levels, which was correlated with increased IL-4Rα expression. Interestingly, STUB1 mRNA levels are up-regulated in the airways of subjects with asthmatic and chronic obstructive pulmonary disease (COPD), suggesting that elevation of STUB1 expression may serve as a possible feedback mechanism in an effort to dampen IL-4Rα signaling 60. The development of strategies to modulate STUB1 activity may represent a promising approach for targeting IL-4-/IL-13-dependent allergic inflammation.
Several therapeutic strategies aimed at blocking IL-4Rα-initiated signaling have been attempted. These approaches include treatment with a variant IL-4R protein and with several individual monoclonal antibodies directed against IL-4Rα. First, a variant of the IL-4 protein, pitrakinra, that contains two amino acid changes that allow it to bind the IL-4Rα-chain, without allowing it to complex with either the γC or the IL-13Rα1 chains, has shown some promise. In an allergen challenge study, treatment with nebulized pitrakinra resulted in a decrease in the late-phase allergic response measured by FEV1 61. A larger follow-up study of symptomatic moderate-to-severe adult asthmatics using corticosteroids revealed that although there was no therapeutic benefit for the entire population treated with pitrakinra compared to placebo, there was a significant reduction in asthma exacerbations in a pre-specified subset of subjects with high blood eosinophil counts 62. A later study revealed a pharmacologic interaction between therapy and variation (IL4RA Q576R) within the gene encoding the IL-4Rα chain ( IL-4RA), identifying an asthma subgroup that was more responsive to pitrakinra 63. Another strategy to block IL-4Rα signaling has been to treat with humanized high-affinity monoclonal antibodies directed against IL-4Rα (AMG-317, dupilumab). A randomized controlled phase IIA trial showed that treatment with dupilumab (SAR231893/REGN668, NCT01312961) prevented asthma exacerbations when long-acting β-agonists and inhaled corticosteroid were withheld in patients with moderate-to-severe asthma as compared to placebo 5. Phase III studies are underway which should provide more definitive information regarding the efficacy of blocking the IL-4Rα in asthma.
IL-13Rα1
As discussed above, the role of IL-13Rα1 in mediating Th2 inflammation such as in AHR, mucus production, and fibrosis is well known 64, 65. IL-13Rα1 –/– mice did not develop AHR nor mucus production and had decreased IgE titers in a schistosomal egg antigen-induced model of allergic lung inflammation 66. Similarly, challenging the IL-13Rα1 –/– mice with IL-13, IL-4, or OVA resulted in no mucus production and protection from AHR 64. These studies demonstrate the critical role of IL-13Rα1 in the generation of AHR and mucus production. The development of the fibrotic response is also dependent on IL-13Rα1 in both the schistosomal and the allergic lung inflammation models of Th2 inflammation 64, 66. In response to worm or allergen challenge, IL-13Rα1-deficient animals had decreased expression of characteristic matrix remodeling genes and collagen deposition in their livers 66 and profibrogenic mediators such as TGF-β in their lungs 64. However, recent studies highlight a protective role for IL-13Rα1 in regulating fibrosis in a bleomycin-induced injury murine model. Karo-Atar et al. demonstrated that IL-3Rα1 deficiency resulted in a dysregulation in homeostasis and increased fibrosis due to exaggerated tissue repair 67. Although bleomycin-elicited lung inflammation and injury is not a typical allergic inflammatory response, these results suggest a role for the IL-13Rα1 as a sink for excess cytokine during the wound-healing response. This role could also be important in allergic inflammation, since IL-13Rα1-deficient mice have increased circulating IL-13 and soluble IL-13Rα2 64. Another interesting study demonstrated that the integrin Mac-1 binds to IL-13Rα1 to downregulate macrophage IL-13 signaling, M2 polarization, and foam cell formation 68. Macrophages from the Mac-1-deficient mice had elevated M2 polarization, even in the absence of IL-13. Whether low Mac-1 expression could contribute to the abundance of M2 macrophages in asthmatic lungs is unknown. This work suggests that the interaction between Mac-1 and IL-13Rα1 may be exploited for the regulation of IL-13 signaling and M2 polarization of macrophages in the lung.
Because IL-13R (type II IL-4R) mediates the effects of IL-13 on structural (non-hematopoietic) cells, the clinical efficacy of a number of antibodies directed against IL-13 (IMA-638, IMA-026) has been evaluated in asthma. The results have been mixed. First, Wyeth evaluated the efficacy of two separate humanized anti-IL-13 IgG1 monoclonal antibodies (IMA-638 [NCT00339872]; IMA-026 [NCT00725582]) in asthma clinical trials. Interestingly, after allergen exposure, only treatment with IMA-638, which recognizes the IL-13 epitope that interacts with IL-4Rα, significantly reduced both the early and the late-phase asthmatic response. On the other hand, IMA-026, which binds to the epitope on IL-13 that is critical for binding to both IL-13Rα1 and IL-13Rα2, efficacious 69. Similarly, a more recent clinical trial utilizing another anti-IL-13 IgG1 monoclonal antibody (GSK679586, GlaxoSmithKline), which interferes with binding of IL-13 to both IL-13Rα1 and IL-13Rα2, did not result in any benefit in severe asthmatic patients over placebo controls 70. Thus, it appears that blocking the interaction of IL-13 with IL-4Rα may be more effective than inhibiting binding to either IL-13Rα1 or IL-13Rα2.
Based on the inconsistent results of the previous studies, a study was designed to compare the effects of blocking IL-13 in asthma patients who were pre-identified as exhibiting an IL-13 signature in vivo 70. In this randomized, double-blind trial of asthmatic patients with poorly controlled disease, patients were stratified into either Th2-high or -low subgroups based on their baseline Th2 status (IgE levels, blood eosinophil counts, and periostin) and treated subcutaneously with either placebo or 200 mg of the humanized IgG4 anti-IL-13 monoclonal lebrikizumab (Genentech, NCT00930163). Even in the presence of steroid treatment, lebrikizumab treatment resulted in an improvement in FEV1 in patients with a Th2-high phenotype but had no significant impact on FEV1 in patients with a Th2-low phenotype. These results demonstrate that blocking IL-13 in patients with a documented IL-13 signature may provide significant clinical benefit. As steroid treatment may have complicated the interpretation of the effects of IL-13 inhibition in the original study, a subsequent phase II randomized, double-blind, placebo-controlled study of lebrikizumab (NCT00971035) in asthmatic patients not receiving inhaled corticosteroids was conducted 71. In this study, lebrikizumab treatment did not show significant improvement in disease (pre-bronchodilator FEV1 values), despite effectively inhibiting Th2 biomarkers (IgE levels and exhaled nitric oxide [FeNO]). Surprisingly, these results suggest that IL-13 blockade may be effective in the context of steroid treatment but may not block disease in patients with mild disease (non-steroid dependent). Phase III studies are underway which should provide further clarification of the potential utility of IL-13 blockade in patients with uncontrolled asthma.
IL-13Rα2
IL-13Rα2 was previously described as a decoy receptor that counteracted IL-13-mediated signaling 72, 73 owing to its negligible cytoplasmic domain. Although IL-13Rα2 does not have a signaling domain, recent studies have shown that IL-13Rα2 engages with TMEM219 and that this interaction also contributes to the decoy function of IL-13Rα2 74. However, several lines of evidence suggest that the role of IL-13Rα2 in regulating inflammation may be more complex. For example, Fichtner-Feigl et al. reported that signaling through this receptor was involved in TGF-β1 production 75 and activation of the mitogen-activated protein kinase (MAPK) pathway 76. Consistent with a role for IL-13Rα2 in promoting allergic inflammation, Chen et al. reported that allergen-driven AHR and eosinophilic inflammation were attenuated, rather than enhanced, in IL-13Rα2-deficient mice 77. Normal allergic inflammatory responses were restored by lung epithelial overexpression of membrane IL-13Rα2 in IL-13Rα2-deficient mice, suggesting that membrane-bound and soluble forms of IL-13Rα2 may mediate different functions. Supporting a positive role for IL-13Rα2 in asthma is the recent finding that sputum levels of IL-13Rα2 are associated with poor lung function, Th2 cell gene expression, and airway obstruction in the airways of asthmatics 78. Collectively, these studies suggest that IL-13Rα2 is an important regulator of IL-13-mediated responses: the directionality of its effects are likely dependent upon whether it is found in a soluble or membrane-bound form. Lastly, as will be discussed below, IL-13Rα2 has been shown to have other binding partners besides IL-13, such as chitinase 3-like 1 (Chi3l1) 74. The complex role of IL-13Rα2 in regulating IL-13-mediated signals suggests that approaches to inhibit IL-13 could be a double-edged sword depending on whether or not they impact the ability of IL-13Rα2 to bind IL-13, which might result in the loss of the inhibitory functions of IL-13Rα2.
New twists on IL-4 and IL-13 signaling pathways
Canonical signaling of IL-4 and IL-13 results in signal transducer and activator of transcription (STAT)6 phosphorylation and transcriptional activation of STAT6-dependent genes 79. However, STAT6signaling in response to IL-4 and IL-13 does not always explain all features of Th2-mediated inflammation. A second pathway that is differentially activated by IL-4 and IL-13 could explain some of the subtleties between the two cytokines. Specific activation of both IL-4R complexes by either IL-4 or IL-13 can also trigger insulin receptor substrate (IRS)-2 activation. IRS activation results in the growth-promoting, proliferative effects of IL-4 as well as activating the AKT target of rapamycin (TOR) pathway and gene expression downstream. However, the difference lies in the magnitude of IRS-2 activation by IL-4 compared to IL-13. IL-4 engagement of IL-4R type I triggers IRS-2 activation particularly robustly, significantly enhancing IL-4-induced responses such as M2 macrophage polarization over that elicited by IL-13 79, 80. This was due to the presence of the γc chain in type I IL-4R complexes that is not found in the type II IL-4R. Thus, IRS-2 was concluded to be an amplifier of IL-4-induced M2 macrophage polarization, yet new evidence suggests a more complex role for the IRS-2 molecule. The absence of IRS-2 increased IL-4-induced M2 gene expression in murine bone-marrow-derived macrophages and stronger allergic lung inflammation in vivo. This novel regulatory role for IRS-2 was STAT6 independent 81 and suggests that IRS-2 activation may participate in a negative feedback inhibitory loop through the TOR complex to decrease IL-4 signaling. This will be discussed further in the metabolism section of this review.
In contrast, when IL-4-induced IRS-2 activation was prolonged through knockdown of the negative regulator suppressor of cytokine signaling (SOCS)1 in vitro, enhanced M2 polarization of human monocytes was observed 82. Furthermore, dysregulation of IRS-2 signaling in monocytes from allergic asthmatics was associated with increased M2 macrophage polarization owing to the lack of SOCS1 induction and increased SOCS3 expression 82. SOCS3 was also highly induced in M2 macrophages at the site of contact hypersensitivity (CHS) to control MMP-12 expression and CHS pathology 83. Taken together, differential expression of SOCS1 and SOCS3 in healthy versus inflammatory conditions suggests that an important balance exists between these molecules to maintain homeostasis in macrophages. A similar paradigm exists in T cells. SOCS3 and SOCS5 are mainly expressed in Th2 and Th1 cells, respectively, and reciprocally inhibit Th1 and Th2 differentiation 84. When dysregulation of the balance between different SOCS proteins occurs, pathological Th2 or M2 polarization results. Numerous examples of dysregulation of SOCS expression in eosinophils 85, airway smooth muscle 86, skin 87, and T cells 88 have been documented in allergic inflammation. Single nucleotide polymorphisms (SNPs) in the SOCS1 promoter are associated with adult asthma and total serum IgE in children 89. Hence, restoring SOCS function to ameliorate inflammatory conditions could be considered as a future therapeutic strategy for asthma, as it has been in the setting of autoimmunity 90.
Downstream regulation of allergic inflammation
IL-4 and IL-13 activation of their receptors on a variety of structural and hematopoietic cells leads to the transcription of a wide variety of mediators, which mediate the pathophysiological manifestations of allergic disease, several of which have recently received considerable attention.
Chitinases
Several chitinase (chitin-degrading enzymes) genes are induced by type-2 cytokines in humans and mice including AMCase, YKL-40 (Chi3l1), breast regression protein (BRP)-39, and YM1/2 in mice 91. Chitin is a highly abundant polysaccharide in nature and is an essential component of many organisms that drive type-2 immune responses (fungi, arthropods [house dust mites, crabs, and shrimp], and parasites). The functions of chitin are highly dependent upon its size: chitin has been shown to induce eosinophilic lung infiltration 92 and elicit IL-33 production from epithelial cells 93, 94. The role of AMCase, the only IL-13-induced chitinase with chitinase enzymatic activity, in asthma has been conflicting 95. In contrast, many, but not all, studies suggest that YKL-40 is increased in severe asthma and/or neutrophilic asthma 96. Epithelial cells are thought to be the primary producers of YKL-40, and mechanical stress has been shown to be a trigger of YKL-40 secretion through an epidermal growth factor receptor (EGFR)- and MEK1/2-dependent pathway 97. YKL-40 has been reported to regulate a number of functions in the lung including IL-8 production 98, MUC5AC production 99, and the proliferation of bronchial smooth muscle cells 100. Recent studies demonstrated that the mouse homolog of YKL-40, Chi3l1, binds to and signals via IL-13Rα2. The same group later demonstrated that the membrane protein TMEM219 is a binding partner of IL-13Rα2. Interestingly, blockade of TMEM219 or IL-13Rα2 phenocopied one another in their ability to decrease Chi3l1-stimulated epithelial cell HB-EGF production, macrophage MAPK/ERK and protein kinase B (PKB)/AKT activation, oxidant-induced apoptosis, and lung injury. These studies demonstrate that an important regulatory loop exists among IL-13, Chi3l1, and IL-13Rα2, although the precise role of these interactions in asthma pathogenesis remains to be determined.
FIZZ1
Although FIZZ1 ( Retnla) was identified as a marker of Th2 inflammation 101, 102, recent reports suggest the opposite. The increase in abundance of FIZZ1 in allergic diseases was interpreted as promoting Th2 responses 101, 103, yet Lee et al. demonstrated that overexpression of FIZZ1 did not induce alterations in lung histology and lung function. In contrast, Retnla-overexpressing mice exhibited a reduction in lung inflammation following allergen sensitization and challenge 104. This new evidence suggests a negative regulatory role for FIZZ1, agreeing with studies showing that mice lacking FIZZ1 developed exacerbated lung inflammation after Schistosoma mansoni (Sm) eggs challenge compared with their wild-type counterparts 105. Therefore, the elevated expression of FIZZ1 appears to mediate negative regulation of Th2 inflammation in the lung.
New pathways regulating type-2 cytokine production
Activation of the Th2 pathway is initiated from a complex interaction between the innate and adaptive immune responses. Although the critical role of antigen-presenting cell interactions with CD4 + T cells in the differentiation of naïve T cells into type-2 cytokine-producing cells has long been appreciated,new information is emerging regarding the complex regulation of DC–T cell interactions that result in Th2 immune responses. Moreover, our understanding of the role of epithelial-derived cytokines in the direction of Th2 differentiation and in the regulation of non-T cell sources (ILC2s) of type-2 cytokines is rapidly expanding.
DC–T cell interactions
Antigen presentation to naïve T cells is an essential step in the development of adaptive immune responses. Recent studies have identified a member of the tumor-associated macrophage (TAM) family receptor tyrosine kinase, TYRO3, as an important negative regulator of DC–T cell interactions and consequently the magnitude of type-2 immune responses 106. Specifically, TYRO3-deficient mice or neutralization of its orthologue in human DCs resulted in the enhancement of type-2 immunity. Interestingly, the TYRO3 agonist protein S1 (PROS1) is specifically induced in CD4 + Th2 cells by IL-4. PROS1, in turn, ligates the rheostat TYRO3 on PDL2 + DCs to limit the intensity of type-2 responses. Importantly, multiple intronic variants in TYRO3 were associated with asthma 106. Modulation of this self-limiting process intrinsic to type-2 immunity provides a novel opportunity to inhibit allergic responses.
Little is known about the signals from DCs that drive Th2 immune responses. New studies show that specific subsets of DCs may contribute to this process. Gao et al. have shown that PDL2 + DCs are able to enhance proliferation and cytokine production by effector and memory CD4 + T cells, but not in naïve cells, compared with PDL2 – DCs 107. Other studies using in vivo depletion approaches have demonstrated an important role for CD301b + but not for CD207 + dermal DCs in driving Th2 differentiation in both OVA-specific transgenic CD4 + T cells and during infection with Nippostrongylus brasiliensis 108. These novel studies suggest that depletion/inhibition of specific DC subsets is a potential therapeutic approach to suppress the initiation of Th2 immune responses.
T cell receptor regulation
T cells play a determinant role in adaptive responses. They are able to recognize an infinite diversity of antigens through the T cell receptor (TCR) with concomitant activation of the T cell 109. As mentioned above, different polarized T helper cell environments participate in the different asthma phenotypes, highlighting the importance of T cell subset differentiation in allergic inflammation. Few T cell intrinsic factors have been identified which govern Th2 differentiation. Newly described mechanisms have been identified that downregulate TCR signaling specifically in Th2 cells. DENND1B, a guanine nucleotide exchange factor 110, downmodulates TCR expression in Th2 cells. Yang et al. demonstrated that in vitro-differentiated Dennd1b –/– Th2 cells have increased TCR-mediated responses when compared to Dennd1b +/+ Th2 cells without changes in Th1 or Th17 responses. This specific effect on Th2 cells may be due to a delayed surface TCR downmodulation upon activation, resulting in increased TCR signaling. This appears to have direct relevance to asthma, as SNPs at the human DENND1B locus have been associated with increased Th2 responses and asthma in young children 111.
E3 ubiquitin ligase regulation of Th2 cells
Recent studies suggest that E3 ubiquitin ligases are critical regulators of T cell activation and cytokine production. For example, overexpression of Grail, an E3 ubiquitin ligase, has been associated with suppressed IL-2 and IL-4 production in T cells 112. Mechanistically, Grail regulates Th2 cytokine production by interacting with STAT6, targeting it for ubiquitination and degradation. Accordingly, Grail-knockout mice are more susceptible to allergen-driven asthma 113. Another E3 ubiquitin ligase, casitas B cell lymphoma (Cbl)-b, which is involved in regulating CD28 signal strength during TCR ligation, has also been shown to be important in the regulation of allergic inflammation 114. Cbl-b-deficient mice have enhanced Th2 cytokine production and delayed resolution of allergen-induced airway inflammation. Interestingly, no changes in IgE levels were noted. Modulation of this class of molecules may provide a unique approach to asthma therapy.
Th17 pathway regulation of Th2-mediated inflammation
In addition to the prototypical Th2 cytokines, other previously unrelated cytokines, such as IL-17, have now been demonstrated to modulate Th2 immune responses. Understanding the molecular mechanism(s) of IL-17’s modulatory role in Th2 responses is of interest, since “mixed” Th2/Th17 T cell populations are present in some asthmatic patients in vivo 115, 116. Co-exposure of mice to IL-13 and IL-17 enhanced all aspects of the allergic phenotype compared to IL-13 treatment alone 115. This was associated with an IL-17-mediated increase in IL-13-induced STAT6 activation in both mouse fibroblasts and primary human nasal epithelial cells (NECs) 117. Conversely, specific suppression of Th2 cytokines in the house dust mite (HDM) model of allergic asthma enhanced Th17 responses, and “Th2-high” and “Th17-high” disease was mutually exclusive in some asthmatic patients 118. These contradictory studies highlight that the exact mechanism(s) dictating the balance between Th2 and Th17 responses remain unclear. Careful immunophenotyping of patients prior to IL-17- or IL-4-/IL-13-based therapies will be essential, as disturbance of the Th2/Th17 balance may worsen the disease in some individuals. Blockade of IL-17RA with brodalumab, a human anti-IL-17RA monoclonal antibody, in subjects with inadequately controlled moderate-to-severe asthma taking regular inhaled corticosteroids did not have a significant impact on asthma. However, there was a positive effect on the asthma control questionnaire score in the high-reversibility subgroup (post-bronchodilator FEV1 improvement >20%) 119. As the significance of this effect is currently not known, further studies are required to unravel the complexities of the contribution of IL-17 to asthma pathogenesis.
IL-31
IL-31 is constitutively expressed by non-hematopoietic cells such as the lung epithelium and is also selectively produced by activated CD4 + T cells skewed towards Th2 cytokine production 120. IL-31RA is a gp130-like type-1 cytokine receptor that pairs with OSMRB to form a functional signaling receptor for IL-31. IL-4 and IL-13 increase the expression of the membrane-bound form of IL-31RA through the type II IL-4R, altering IL-31-mediated signaling in macrophages. IL-31 has been shown to be elevated in Th2-mediated diseases such as atopic dermatitis 121 and is positively associated with asthma severity 122. Consistent with a role for IL-31 in asthma, Yu et al. showed that SNPs in IL-31 were significantly correlated with total serum levels of IgE in patients with asthma 123. Despite the preponderance of evidence suggesting that IL-31 promotes type-2 inflammation, Perrigoue et al. showed that IL-31R activation limited the magnitude of Th2 cytokine-dependent inflammatory responses to intestinal helminth infection 124. Taken together, these studies highlight important interactions between Th2 cytokines and IL-31 signaling pathways; however, further studies are needed to delineate the exact role that IL-31 plays in mediating type-2 immune responses and whether this will be a useful target for therapy in type-2-high asthmatics.
Alarmins as initiators of type-2 inflammation
Although Th2 cytokine production has long been recognized as a pivotal contributor to allergic inflammation, the mechanisms initiating Th2 cell differentiation and cytokine production has long eluded investigators. Recent studies have identified several epithelial-derived molecules such as thymic stromal lymphopoietin (TSLP), IL-25, and IL-33 as early initiators of Th2 inflammation in both mice and humans. These cytokines have been described as "epithelial-derived alarmins" that activate and potentiate the innate and humoral arms of the immune system in response to cellular damage. Each of the three epithelial-derived alarmins has been implicated in the pathophysiology of allergic asthma. A better understanding of the roles that these epithelial-derived alarmins play in disease and how they influence airway immune responses may allow the development of novel therapeutics for asthma treatment.
TSLP. The role of TSLP in allergic lung inflammation has garnered considerable interest. Early studies of mice overexpressing TSLP in airway epithelial cells resulted in spontaneous lung inflammation, enhanced eosinophilia, goblet cell metaplasia, perivascular fibrosis, and AHR 125. Moreover, Han and colleagues found that overexpression of TSLP in the lung induced an alternatively activated phenotype in pulmonary macrophages and increased BAL cell recruitment 126. Support for a role for TSLP was confirmed in studies utilizing Tslpr –/– mice in a model of lung inflammation 127. Interestingly, TSLP effects were not direct but were dependent on IL-13 126. Consistent with the mouse studies, therapeutic antibody blocking of TSLP resulted in a reduction of lung eosinophils in a cynomolgus monkey model of allergic lung inflammation 128. TSLP also synergizes with IL-25 and IL-33 to promote inflammation and lung fibrosis induced by Schistosoma. Only antibody blockade of all three cytokines suppressed Th2-mediated fibrosis, although this approach did not work in a model of chronic HDM-induced allergic lung inflammation 129. These results suggest that fibrosis may be induced in the lung through multiple pathways. TSLP seems to play a more important role in the gut, where it is constitutively expressed in both mice and humans. In the gastrointestinal tract, TSLP is not only an important enhancer of inflammatory Th2 responses 130– 132 but also a key player in the maintenance of homeostasis by controlling inflammatory responses against parasites 133– 137 and Th1 and Th17 responses 138, 139. Therefore, the function of TSLP is complex, both promoting and controlling inflammation in a tissue-dependent manner. Support for a role for TSLP in human disease has recently been provided in a study of a human anti-TSLP monoclonal antibody (AMG 157), which binds TSLP and prevents receptor interaction. In a double-blind, placebo-controlled study, AMG 157 attenuated both early and late allergen-induced bronchoconstriction and indices of airway inflammation in allergic asthmatic subjects 140. Although these results are promising, further studies are required.
IL-25. IL-25, also named IL-17E, is a cytokine able to enhance Th2 immune responses. It was first described as a product of “highly polarized” murine Th2 cells in the presence of IL-4/anti-IL-12 monoclonal antibodies 141. However, more recent studies indicate that IL-25 can be produced by a great variety of cells including eosinophils, basophils, mast cells, macrophages, epithelial cells, and Tuft cells, among others 142, highlighting its importance as an initiator of Th2 responses. For example, during N. brasiliensis infection, hyperplasia of Tuft cells—the only IL-25-releasing cell—occurs in the small intestine. A feed-forward system mediated through IL-25 release by Tuft cells activates ILCs to release IL-13, which in turn regulates the number of Tuft cells 143. Interestingly, Tuft cells express taste receptors such as bitter and umami receptors, which are G-protein-coupled receptors (GPCRs), that participate in the release of acetylcholine when activated 144. This has been associated with changes in nutrient and metabolite levels in the gut lumen, which could help Tuft cells detect danger signals, such as the presence of helminths 145, and initiate a protective Th2 immune response. The signaling and functional responses to helminths at the gut epithelial barrier show remarkable similarity to the lung in that bitter taste receptors and early alarmin signaling may work together to coordinate the immune response to inhaled antigens. Blockade of the IL-25 receptor, IL-17RA, in bronchial rings from donors with asthma significantly reduced acetylcholine-induced contraction compared to that seen in donors without asthma 146. One of the major triggers of asthma exacerbations, rhinovirus infection, was shown to induce significantly greater expression of IL-25 mRNA expression in bronchial epithelial cells from asthmatics compared to those in non-atopic, non-asthmatic healthy individuals 147. Although these studies suggested that blocking IL-17RA in asthma might be promising, studies with the anti-IL-17RA monoclonal antibody brodalumab have failed to show benefit in asthma 119, implying that blocking IL-25 alone is insufficient to modify disease.
IL-33. Another alarmin that has risen to prominence in recent years is IL-33, a novel cytokine discovered almost 10 years ago 148. The importance of IL-33 in allergic disease was initially identified through a genome-wide association study (GWAS). The GABRIEL consortium, the largest GWAS meta-analysis involving more than 26,000 subjects, demonstrated significant association between asthma and a SNP (rs1342326) on chromosome 9 flanking the IL33 gene. Polymorphisms in the IL33 gene were among the top three SNPs to correlate with asthma 149. Similarly, strong associations between variants of the gene encoding the unique IL-33 receptor, suppression of tumorigenicity ( ST2) or IL1RL1, and asthma risk have been observed 150. The identification of IL-33 and its receptor as asthma susceptibility genes has opened up a fruitful new field of study that has exponentially increased our understanding of the mechanisms driving aberrant type-2 immune responses.
IL-33 has been shown to be an important regulator of type-2 cytokine production and the pathogenesis of allergic diseases. In several mouse models of asthma, IL-33 activates lung-resident ILC2s and initiates airway type-2 inflammation 20, 151. Similarly, administration of rIL-33 to mice through a variety of routes resulted in tissue eosinophilia, goblet cell hyperplasia, and elevations in type-2 cytokines 152. The timing of expression of IL-33 in the lung is thought to be critically important to the development of skewed Th2 immune responses. It has been reported that shortly after birth, ILC2s, eosinophils, basophils, and mast cells spontaneously accumulate in the developing lung in an IL-33-dependent fashion 153. Upon encounter with allergens during early lung development, the changes are further boosted, promoting Th2 cell skewing. Thus, enhanced neonatal Th2 cell skewing in response to exposure to inhaled allergens results from postnatal hyper-responsiveness of the IL-33 axis during a period of maximal lung remodeling.
IL-33 is a member of the IL-1 family of cytokines, which is constitutively expressed in the nucleus of a variety of cells in both mice and humans 148. Because of its localization within the nucleus, it is thought to function as a nuclear receptor, although its exact function in the nucleus is unknown. In addition to potential nuclear functions, IL-33 is released primarily from endothelial and epithelial cells and binds its functional receptor on a variety of cells, including mast cells, eosinophils, and ILC2s 154. Unlike other IL-1 family members, IL-33 does not require cleavage by caspase 1 for release from the cell or to initiate signaling via ST2 155; however, it can be inactivated by either caspase-3 or caspase-7. On the other hand, cleavage by extracellular proteases (chymase and tryptase), commonly produced by inflammatory cells such as mast cells present during allergic reactions, results in three major forms of “mature” IL-33. These cleaved versions of IL-33 are up to 30-fold more potent as activators of ILC2s ex vivo compared with full-length human IL-33 156.
Despite the importance of IL-33 to the initiation of an allergic response at mucosal surfaces, the molecular mechanisms responsible for its expression and extracellular release are poorly understood. IL-33 transcription is believed to be initiated from one of two non-coding exons that are associated with constitutive or induced production of IL-33 157. A recent study suggested that the RNA-binding protein Mex-3B regulates IL-33 expression in airway epithelial cells via binding to the IL-33 3' UTR and increasing IL-33 expression by inhibiting miR-487b-3p-mediated repression of IL-33 158. The importance of Mex-3B to the regulation of IL-33 in allergic inflammation is demonstrated in Mex-3B-deficient mice, which are protected against allergen-induced airway inflammation due to the induction of IL-33. Moreover, it was shown that inhalation of an anti-sense oligonucleotide targeting Mex-3B suppressed the development of allergic airway inflammation in mice.
As IL-33 lacks a traditional signal sequence 159, it was originally thought to be released primarily by damaged or necrotic cells 160. However, a more complex picture is emerging in which it can be released from both human and mouse living cells both constitutively and following exposure to a variety of stimuli 161, 162. Under homeostatic conditions, pools of IL-33 become active locally to sustain basal physiology by activating ST2 + cells. In response to a number of perturbations, such as allergen exposure, it can be induced through multiple pathways in the absence of cell death depending on the nature of the stimulus. For example, common allergens such as Alternaria alternata and HDM induce IL-33 secretion through a mechanism dependent on DUOX-1-mediated activation of the epithelial EGFR and the protease calpain-2 through a redox-dependent mechanism involving cysteine oxidation of the EGF and the tyrosine kinase Src 163. Consistent with the importance of this pathway to allergic disease, NECs from allergic asthmatic patients were shown to express more DUOX-1 and IL-33 compared to non-asthmatic individuals. Several studies also suggest that extracellular ATP can induce the secretion of IL-33 164. Alternative splicing resulting in cytoplasmic IL-33 has also been proposed as a potential mechanism of extracellular release 165. Consistent with these findings, splice variants of human IL33 have been recovered from primary cells; however, the physiological relevance of these variants is currently unknown 166. IL-33 is clearly a key player in the initiation of allergic inflammation, suggesting that it would be an excellent target for biologic therapy. However, as it also plays a role in other non-Th2-mediated inflammatory diseases 167, 168, a more detailed understanding of the plethora of IL-33’s actions is required prior to targeting it in allergic individuals.
Impact of cellular metabolism on Th2-mediated inflammation
In recent years, the role of metabolism in regulating the function of immune and non-immune cells that are important in asthma has been uncovered. Balancing nutrient utilization and metabolism is critical for cells to meet energy needs required to survive, proliferate, and perform their specific functions (i.e. cytokine secretion). A variety of metabolic mediators such as arginine, extracellular lactate, and cyclic adenosine monophosphate (cAMP)/ATP have been implicated in various aspects of the asthmatic phenotype. Recent evidence suggests that the integration of these metabolic functions, sensing of the external nutrient milieu, and immune cell polarization occurs through the PI3K/AKT/mammalian TOR (mTOR) pathways 169, 170. While the importance of immune cell metabolic remodeling in different physiological settings is not fully understood, there is a growing realization that inappropriate metabolic function underlies many aberrant immune responses and that reprogramming cellular metabolism may provide a therapeutic avenue to alter immunity 171, 172.
Arginine metabolism
Arginine is a key substrate in the citrulline–NO and tricarboxylic acid cycles. However, little is known about how mitochondrial arginine metabolism modulates inflammation. Elevated expression of the arginine-metabolizing enzymes iNOS and arginase were found in the airway epithelium of asthmatics. Xu et al. described a mechanistic role for arginine metabolism in asthma. Greater arginine flux increased oxidative metabolism in airway epithelium, resulting in lower STAT6 and hypoxia-inducible factor signaling, which are both important drivers of asthma 173. Arginase 1 is also a critical regulator of ILC2 metabolismin the lung. Elevated ARG1 expression was noted specifically in ILC2s from the lung tissue of patients with COPD and idiopathic pulmonary fibrosis. Deletion of Arg1 specifically in ILC2s resulted in the attenuation of type-2-mediated lung inflammation in mice due to diminished ILC2 proliferation and cytokine production. This work has shed new light on how arginine metabolism may influence allergic inflammatory responses 174. Since ILC2s are one of the major producers of the cytokines that initiate Th2 immune responses in allergic inflammation, the modulation of arginine metabolism may provide a promising avenue for the regulation of these low-frequency cells, thereby preventing the initiation of Th2 inflammation.
Lactate
Recent studies have demonstrated that lactic acid produced by tumor cells induces an M2-like polarization with enhanced Arg1 expression in murine TAMs compared with peritoneal macrophages 175. Similarly, a recent study by Selleri et al. demonstrated that the presence of lactate during the differentiation of human monocytes to DCs induced a M2 macrophage phenotype. These M2 macrophages induced Th2 polarization. This effect was due to a decrease in oxidative phosphorylation, lower basal respiration, and more polarized mitochondrial membrane potential as well as higher spare respiratory capacity 176. This lactate-induced M2 phenotype is consistent with the lactic acidosis observed in patients with severe asthma 177, 178 and the observation that asthmatics have more M2 macrophages in their lungs than do non-asthmatics 38, 179. Furthermore, lactic acid has been shown to delay NF-κB activation and suppress LPS-induced TNF-α secretion in monocytes, promoting an M2 macrophage phenotype 180, 181. However, opposite effects have been attributed to lactate, the salt form of lactic acid, in that it enhanced LPS-mediated inflammatory responses in macrophages 182. Recent studies have shown that lactic acid negatively regulates IL-33-mediated cytokine and chemokine production in murine bone-marrow-derived mast cells and primary human mast cells, resulting in the suppression of inflammation 183. Accordingly, lactic acid and lactate might be playing different roles in M2 polarization and asthma depending on the local pH. A better understanding of the conditions that induce either systemic or localized changes in airway pH may inform the development of more effective strategies to control asthma.
mTORC
mTOR complex (mTORC)-activated pathways have emerged as critical regulatory nodes for the polarization of T cells 184, 185 and macrophages 186. The TORC1 pathway is crucial for the development of Th17 polarization in naïve murine T cells, but not the other Th profiles 187, linking the opposing regulation between Th2 and Th17 responses. This points to the mTOR pathway as a possible target for effective therapy to ameliorate Th2/Th17 mixed asthma phenotypes. Exploring the mTOR pathway for type-2-high asthmatics should be approached with caution, however, given the uncertainty surrounding equivocal data on the Th2/Th17 balance discussed above.
Regulation of macrophage polarization following the TORC1/2 dichotomy established for T cells has been an attractive concept. IL-4-dependent M2 macrophage differentiation is associated with mTORC2/STAT6 activation and increased fatty acid oxidation and oxidative phosphorylation 188. In contrast, constitutive activation of mTORC1 due to myeloid-specific deletion of its negative regulator tuberous sclerosis complex 1 leads to decreased M2 macrophage polarization by attenuating IL-4-induced AKT activation and M2 gene expression 189, 190. This correlates with the novel role of TORC1-activated p70S6K1 and GRB10 as key negative regulators of IL-4-induced IRS-2 signaling and M2 macrophage polarization 191. The balance between mTORC1 and mTORC2 in controlling macrophage polarization was also highlighted by studies in mice with a myeloid-specific deletion of rapamycin-insensitive companion of mTOR, a subunit of mTORC2. Lacking functional mTORC2 resulted in exaggerated responses to LPS and other TLR ligands and decreased M2 macrophage markers 192. Taken together, these studies highlight the importance of mTOR complexes in dictating M2 polarization. In addition, they point to possible targets, such as p70S6K or GRB10, that could be used therapeutically to downmodulate IL-4-mediated inflammatory responses and M2 macrophage polarization and to control type-2-high asthma.
cAMP/ATP
cAMP also alters cellular phenotype. Bone-marrow-derived DCs from mice deficient in the production of cAMP triggered Th2 polarization of CD4 + T cells. These mice developed spontaneous elevations in total IgE, resulting in severe Th2-mediated lung inflammation. Exposure to the cell-permeable cAMP analog 8-CPT-cAMP (CPT) decreased their ability to induce Th2 responses 193. However, the role of cAMP in inflammation is more complex and could be cell specific. Mucus production by bronchial epithelial cells depends not only on IL-13 stimulation but also on signaling through the β2-adrenoceptor (β2AR). New research shows that epinephrine activation of β2AR and ERK1/2, JNK, and cAMP signaling is necessary for mucin production. These findings may explain the side effects of chronic β2AR agonist use in asthma 194.
In addition to cAMP, ATP has also been demonstrated to regulate inflammation. Through the utilization of a mouse model of OVA-induced lung inflammation, it was demonstrated that the P2X4 receptor (P2X4R) was upregulated in inflamed mouse lungs. Moreover, through binding to P2X4R, ATP enhanced the expression of α-smooth muscle actin 195 and proliferating cell nuclear antigen 196 in the lungs of allergically challenged mice. Overexpression of these two proteins is an indicator of cell proliferation in asthma. Furthermore, P2X4R antagonists decreased cell recruitment and mucus production in OVA-challenged mice. Taken together with ATP’s role in IL-33 release mentioned above, these studies suggest an important role for ATP in the regulation of airway inflammation and airway remodeling 197.
The microbiome as a modifier of Th2 inflammation
There has been an increased appreciation of the role of the gut and lung microbiota in shaping the Th2 response in asthma. The beneficial effects of exposure to certain bacterial products at key times in immune system development have been demonstrated to reduce the development of asthma in epidemiological studies of infant breastfeeding, vaginal delivery, exposure to certain pets in the home 198– 200, the number of siblings in the home 201, and exposure to farm dust in utero 202. Early life antibiotic use 203, 204, lack of breastfeeding 205, or cesarean birth 206 are associated with an increased risk of developing asthma. While no specific pathogens have been associated with the protective effect of these exposures against disease, recent studies in human asthmatics have suggested that alterations in the diversity of the gut and lung microbiome may be associated with an increased risk of developing asthma 207, 208.
In a recent study in which the effects of the gut microbiome were investigated at the level of genera, the relative abundance of Lachnospiraceae, Veillonella, Faecalibacterium, and Rothia were found to be decreased in the gut in the first 100 days of life in children who later went on to develop atopic asthma 209. Of note, the differences in relative abundance of these genera were no longer present at 1 year of age. The contribution of these species to asthma pathogenesis was further demonstrated in an experimental mouse model. Asthma was induced in germ-free mice that were colonized with the gut microbiome of a child with severe atopic allergy and very low relative abundance of Lachnospiraceae, Veillonella, Faecalibacterium, and Rothia. The effect was reversed with supplementation with the four protective bacterial genera. If replicated, these findings would provide a strong basis for a causal link between these four bacterial genera and the development of atopic asthma. These results are consistent with multiple studies suggesting that there is a critical time period in early life when gut flora imbalances have the most influence on allergic inflammation 209– 211.
Studies in experimental animal models have shed some light on the potential mechanism(s) by which the shifts in phylogenic groups condition the immune system. For example, an intriguing study showed that the susceptibility of newborn mice to the development of HDM-driven BAL eosinophilia and AHR was associated with a lung microbial pattern dominated by Firmicutes and gammaproteobacterial phyla 212. Interestingly, over the first few weeks of life, the balance of lung phyla shifted towards a dominant Bacteroidetes pattern. This shift in the lung microbiota was associated with a reduction in responsiveness to allergen exposure and an increase in the population of PD-L1-dependent T-regulatory cells. Thus, these studies suggest that the establishment of a Bacteroidetes-dominated airway microbial pattern early in life is required to populate the lung with T-regulatory cells which provide sustained protection against the development of aeroallergen-induced airway inflammation.
Further support of the concept that gut colonization with Bacteroidetes is associated with protection against the development of the asthmatic phenotype was provided by a study in mice in which a high-fiber diet protected them from the aeroallergen-induced asthma phenotype, concomitant with a shift towards predominant gut colonization with Bacteroidetes 212. The protection afforded by the high-fiber diet was mediated via short-chain fatty acid-induced alterations in bone marrow hematopoiesis characterized by enhanced generation of macrophage and DC precursors and subsequent recruitment to the lungs of DCs with an impaired ability to promote Th2-cell differentiation. Mechanistically, the authors showed that the effects of one of the short-chain fatty acids (propionate) on the asthma phenotype were mediated via the GPCR 41 (GPR41). These three products of the fermentation of dietary fiber are absorbed by the host, where they circulate and communicate with the immune system by binding to host cell receptors. Indeed, short-chain fatty acids, such as butyrate and acetate, have been shown to regulate mucosal T-regulatory cell differentiation and function 213. In humans, decreased fecal short-chain fatty acids at 3 months of age have been observed in subjects who went on to develop atopy and wheeze at 3 years of age, and germ-free mice inoculated with the microbiome of a child with atopic wheeze had lower levels of the short-chain fatty acid butyrate than did control mice 214.
Taken together, these results suggest that diet and the gut microbiome shape the immunological environment in the lung and that a disrupted microbiota could possibly have detrimental effects. Importantly, these results suggest that microbiota-based interventions could be used to influence the likelihood of developing allergies. However, the timing of administration of such therapies is critical and would likely have to be given in the “window of opportunity” in early life to be effective. Further research is now required to fully dissect the role of the microbiome in disease and ultimately pave the way for the emergence of new therapeutic strategies in combating these conditions.
Conclusion
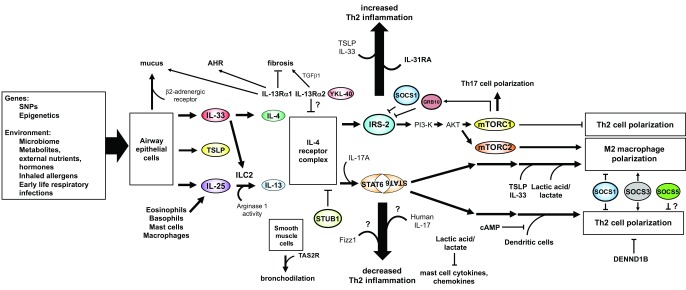
A better understanding of both canonical and newly appreciated pathways of regulation of allergic inflammation will inform the development of strategies to better control asthma and its consequences in Th2-high asthmatics. The new players that we have discussed in this review, such as the role of epithelial-derived cytokines in type-2 cytokine production (TSLP, IL-25, and IL-33), the identification of novel ligands for the IL-13 receptor IL-13Rα2, the role of E3 ubiquitin ligases in T cell differentiation, and the role of cellular metabolism in type-2 immune responses, highlight the tremendous complexity of the pathways and feedback loops that regulate IL-4/IL-13 production, their receptors, their signaling pathways, and their downstream consequences (summarized in Figure 1). Some of these effects are uncovered only in the setting of specific polymorphisms or the presence or absence of other host factors (age as well as gut and lung microbiome). An appreciation of this complexity reinforces the importance of careful phenotyping of asthma endotypes in each patient to direct the appropriate intervention. Our emerging understanding of the intricate web of factors that modify Th2 responses will provide new therapeutic avenues that could lead to the development of better, more effective strategies to treat and/or prevent this increasingly common disease.
Figure 1. Summary of the canonical Th2 pathway and “new spins” on the pathways that lead to allergic inflammation.
Newly appreciated modifiers of Th2 inflammation, such as alarmins, environmental factors, and G-protein-coupled receptor pathways, are indicated and discussed further in the text. Question marks indicate that the role of these new players is not completely clear or that they have been reported to have an enhancing or reducing effect on the outcome measure depending on the publication. AKT, protein kinase B; cAMP, cyclic adenosine monophosphate; DENND1B, DENN domain-containing 1B; FIZZ1, found in inflammatory zone 1; GRB10, growth factor receptor bound protein 10; IL, interleukin; IL-13Rα1, interleukin-13 receptor α1; ILC2, type-2 innate lymphoid cells; IRS-2, insulin receptor substrate 2; mTORC, mammalian target of rapamycin complex; PI3-K, phosphoinositide 3-kinase; SNP, single nucleotide polymorphism; SOCS, suppressor of cytokine signaling; STAT6, signal transducer and activator of transcription 6; STUB1, STIPI homology and U-box-containing protein 1; TAS2R, taste 2 receptor; TGF-β, transforming growth factor-β; TH2, T helper type-2; TSLP, thymic stromal lymphopoietin; YKL-40, chitinase-3-like protein 1.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Xiaoxia Li, Department of Immunology, Cleveland Clinic Lerner Research Institute, Cleveland, OH, USA
Yeonseok Chung, Laboratory of Immune Regulation, Research Institute for Pharmaceutical Sciences, College of Pharmacy, Seoul National University, Seoul, Korea, South
Funding Statement
This work was funded by NIH R01HL124477 to Nicola M. Heller for Mireya Becerra-Díaz and Nicola M. Heller and NIH RO1AI083315 and NIH U19AI070235 to Marsha Wills-Karp.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; referees: 2 approved]
References
- 1. Lötvall J, Akdis CA, Bacharier LB, et al. : Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J Allergy Clin Immunol. 2011;127(2):355–60. 10.1016/j.jaci.2010.11.037 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 2. Woodruff PG, Boushey HA, Dolganov GM, et al. : Genome-wide profiling identifies epithelial cell genes associated with asthma and with treatment response to corticosteroids. Proc Natl Acad Sci U S A. 2007;104(40):15858–63. 10.1073/pnas.0707413104 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 3. Woodruff PG, Modrek B, Choy DF, et al. : T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med. 2009;180(5):388–95. 10.1164/rccm.200903-0392OC [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 4. Peters MC, Mekonnen ZK, Yuan S, et al. : Measures of gene expression in sputum cells can identify T H2-high and T H2-low subtypes of asthma. J Allergy Clin Immunol. 2014;133(2):388–94. 10.1016/j.jaci.2013.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 5. Wenzel S, Ford L, Pearlman D, et al. : Dupilumab in persistent asthma with elevated eosinophil levels. N Engl J Med. 2013;368(26):2455–66. 10.1056/NEJMoa1304048 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 6. Choy DF, Modrek B, Abbas AR, et al. : Gene expression patterns of Th2 inflammation and intercellular communication in asthmatic airways. J Immunol. 2011;186(3):1861–9. 10.4049/jimmunol.1002568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Corren J, Lemanske RF, Hanania NA, et al. : Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365(12):1088–98. 10.1056/NEJMoa1106469 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 8. Bullens DM, Truyen E, Coteur L, et al. : IL-17 mRNA in sputum of asthmatic patients: linking T cell driven inflammation and granulocytic influx? Respir Res. 2006;7:135. 10.1186/1465-9921-7-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lemière C, Ernst P, Olivenstein R, et al. : Airway inflammation assessed by invasive and noninvasive means in severe asthma: eosinophilic and noneosinophilic phenotypes. J Allergy Clin Immunol. 2006;118(5):1033–9. 10.1016/j.jaci.2006.08.003 [DOI] [PubMed] [Google Scholar]
- 10. Dardalhon V, Awasthi A, Kwon H, et al. : IL-4 inhibits TGF-beta-induced Foxp3 + T cells and, together with TGF-beta, generates IL-9 + IL-10 + Foxp3 - effector T cells. Nat Immunol. 2008;9(12):1347–55. 10.1038/ni.1677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Veldhoen M, Uyttenhove C, van Snick J, et al. : Transforming growth factor-beta 'reprograms' the differentiation of T helper 2 cells and promotes an interleukin 9-producing subset. Nat Immunol. 2008;9(12):1341–6. 10.1038/ni.1659 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 12. Gour N, Wills-Karp M: IL-4 and IL-13 signaling in allergic airway disease. Cytokine. 2015;75(1):68–78. 10.1016/j.cyto.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bao K, Reinhardt RL: The differential expression of IL-4 and IL-13 and its impact on type-2 immunity. Cytokine. 2015;75(1):25–37. 10.1016/j.cyto.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 14. Curran DR, Cohn L: Advances in mucous cell metaplasia: a plug for mucus as a therapeutic focus in chronic airway disease. Am J Respir Cell Mol Biol. 2010;42(3):268–75. 10.1165/rcmb.2009-0151TR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Laporte JC, Moore PE, Baraldo S, et al. : Direct effects of interleukin-13 on signaling pathways for physiological responses in cultured human airway smooth muscle cells. Am J Respir Crit Care Med. 2001;164(1):141–8. 10.1164/ajrccm.164.1.2008060 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 16. Berair R, Hollins F, Brightling C: Airway smooth muscle hypercontractility in asthma. J Allergy (Cairo). 2013;2013: 185971. 10.1155/2013/185971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Webb DC, Cai Y, Matthaei KI, et al. : Comparative roles of IL-4, IL-13, and IL-4Ralpha in dendritic cell maturation and CD4 + Th2 cell function. J Immunol. 2007;178(1):219–27. 10.4049/jimmunol.178.1.219 [DOI] [PubMed] [Google Scholar]
- 18. Ahn JS, Agrawal B: IL-4 is more effective than IL-13 for in vitro differentiation of dendritic cells from peripheral blood mononuclear cells. Int Immunol. 2005;17(10):1337–46. 10.1093/intimm/dxh312 [DOI] [PubMed] [Google Scholar]
- 19. Gaurav R, Agrawal DK: Clinical view on the importance of dendritic cells in asthma. Expert Rev Clin Immunol. 2013;9(10):899–919. 10.1586/1744666X.2013.837260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Halim TY, Steer CA, Mathä L, et al. : Group 2 innate lymphoid cells are critical for the initiation of adaptive T helper 2 cell-mediated allergic lung inflammation. Immunity. 2014;40(3):425–35. 10.1016/j.immuni.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 21. Roper RL, Conrad DH, Brown DM, et al. : Prostaglandin E2 promotes IL-4-induced IgE and IgG1 synthesis. J Immunol. 1990;145(8):2644–51. [PubMed] [Google Scholar]
- 22. Maggi E, Del Prete GF, Tiri A, et al. : Role of interleukin-4 in the induction of human IgE synthesis and its suppression by interferon-gamma. Ric Clin Lab. 1987;17(4):363–7. [DOI] [PubMed] [Google Scholar]
- 23. Graber P, Gretener D, Herren S, et al. : The distribution of IL-13 receptor alpha1 expression on B cells, T cells and monocytes and its regulation by IL-13 and IL-4. Eur J Immunol. 1998;28(12):4286–98. [DOI] [PubMed] [Google Scholar]
- 24. Doucet C, Brouty-Boyé D, Pottin-Clémenceau C, et al. : Interleukin (IL) 4 and IL-13 act on human lung fibroblasts. Implication in asthma. J Clin Invest. 1998;101(10):2129–39. 10.1172/JCI741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ishino T, Robertson N, Chaiken I: Cytokine recognition by human interleukin 5 receptor. Vitam Horm. 2005;71:321–44. 10.1016/S0083-6729(05)71011-6 [DOI] [PubMed] [Google Scholar]
- 26. Flood-Page P, Swenson C, Faiferman I, et al. : A study to evaluate safety and efficacy of mepolizumab in patients with moderate persistent asthma. Am J Respir Crit Care Med. 2007;176(11):1062–71. 10.1164/rccm.200701-085OC [DOI] [PubMed] [Google Scholar]
- 27. Tabatabaian F, Ledford DK, Casale TB: Biologic and New Therapies in Asthma. Immunol Allergy Clin North Am. 2017;37(2):329–43. 10.1016/j.iac.2017.01.007 [DOI] [PubMed] [Google Scholar]
- 28. Castro M, Zangrilli J, Wechsler ME: Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3(5):355–66. 10.1016/S2213-2600(15)00042-9 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 29. Balhara J, Gounni AS: The alveolar macrophages in asthma: a double-edged sword. Mucosal Immunol. 2012;5(6):605–9. 10.1038/mi.2012.74 [DOI] [PubMed] [Google Scholar]
- 30. Rőszer T: Understanding the Mysterious M2 Macrophage through Activation Markers and Effector Mechanisms. Mediators Inflamm. 2015;2015: 816460. 10.1155/2015/816460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arango Duque G, Descoteaux A: Macrophage cytokines: involvement in immunity and infectious diseases. Front Immunol. 2014;5:491. 10.3389/fimmu.2014.00491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Girodet PO, Nguyen D, Mancini JD, et al. : Alternative Macrophage Activation Is Increased in Asthma. Am J Respir Cell Mol Biol. 2016;55(4):467–75. 10.1165/rcmb.2015-0295OC [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 33. Staples KJ, Hinks TS, Ward JA, et al. : Phenotypic characterization of lung macrophages in asthmatic patients: overexpression of CCL17. J Allergy Clin Immunol. 2012;130(6):1404–12.e7. 10.1016/j.jaci.2012.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kim YG, Udayanga KG, Totsuka N, et al. : Gut dysbiosis promotes M2 macrophage polarization and allergic airway inflammation via fungi-induced PGE 2. Cell Host Microbe. 2014;15(1):95–102. 10.1016/j.chom.2013.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Melgert BN, ten Hacken NH, Rutgers B, et al. : More alternative activation of macrophages in lungs of asthmatic patients. J Allergy Clin Immunol. 2011;127(3):831–3. 10.1016/j.jaci.2010.10.045 [DOI] [PubMed] [Google Scholar]
- 36. Agapov E, Battaile JT, Tidwell R, et al. : Macrophage chitinase 1 stratifies chronic obstructive lung disease. Am J Respir Cell Mol Biol. 2009;41(4):379–84. 10.1165/2009-0122R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Winkler C, Witte L, Moraw N, et al. : Impact of endobronchial allergen provocation on macrophage phenotype in asthmatics. BMC Immunol. 2014;15:12. 10.1186/1471-2172-15-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kim EY, Battaile JT, Patel AC, et al. : Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat Med. 2008;14(6):633–40. 10.1038/nm1770 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 39. Müller U, Stenzel W, Köhler G, et al. : IL-13 induces disease-promoting type 2 cytokines, alternatively activated macrophages and allergic inflammation during pulmonary infection of mice with Cryptococcus neoformans. J Immunol. 2007;179(8):5367–77. 10.4049/jimmunol.179.8.5367 [DOI] [PubMed] [Google Scholar]
- 40. Ford AQ, Dasgupta P, Mikhailenko I, et al. : Adoptive transfer of IL-4Rα + macrophages is sufficient to enhance eosinophilic inflammation in a mouse model of allergic lung inflammation. BMC Immunol. 2012;13:6. 10.1186/1471-2172-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dasgupta P, Keegan AD: Contribution of alternatively activated macrophages to allergic lung inflammation: a tale of mice and men. J Innate Immun. 2012;4(5–6):478–88. 10.1159/000336025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Draijer C, Robbe P, Boorsma CE, et al. : Characterization of macrophage phenotypes in three murine models of house-dust-mite-induced asthma. Mediators Inflamm. 2013;2013: 632049. 10.1155/2013/632049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lee CG, Hartl D, Lee GR, et al. : Role of breast regression protein 39 (BRP-39)/chitinase 3-like-1 in Th2 and IL-13-induced tissue responses and apoptosis. J Exp Med. 2009;206(5):1149–66. 10.1084/jem.20081271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gibbons MA, MacKinnon AC, Ramachandran P, et al. : Ly6C hi monocytes direct alternatively activated profibrotic macrophage regulation of lung fibrosis. Am J Respir Crit Care Med. 2011;184(5):569–81. 10.1164/rccm.201010-1719OC [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 45. Zhao A, Urban JF, Jr, Anthony RM, et al. : Th2 cytokine-induced alterations in intestinal smooth muscle function depend on alternatively activated macrophages. Gastroenterology. 2008;135(1):217–225.e1. 10.1053/j.gastro.2008.03.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Migliaccio CT, Buford MC, Jessop F, et al. : The IL-4Ralpha pathway in macrophages and its potential role in silica-induced pulmonary fibrosis. J Leukoc Biol. 2008;83(3):630–9. 10.1189/jlb.0807533 [DOI] [PubMed] [Google Scholar]
- 47. Zhen Y, Zheng J, Zhao Y: Regulatory CD4 +CD25 + T cells and macrophages: communication between two regulators of effector T cells. Inflamm Res. 2008;57(12):564–70. 10.1007/s00011-008-7234-3 [DOI] [PubMed] [Google Scholar]
- 48. Hussell T, Bell TJ: Alveolar macrophages: plasticity in a tissue-specific context. Nat Rev Immunol. 2014;14(2):81–93. 10.1038/nri3600 [DOI] [PubMed] [Google Scholar]
- 49. Lauzon-Joset JF, Marsolais D, Langlois A, et al. : Dysregulation of alveolar macrophages unleashes dendritic cell-mediated mechanisms of allergic airway inflammation. Mucosal Immunol. 2014;7(1):155–64. 10.1038/mi.2013.34 [DOI] [PubMed] [Google Scholar]
- 50. McCormick SM, Heller NM: Commentary: IL-4 and IL-13 receptors and signaling. Cytokine. 2015;75(1):38–50. 10.1016/j.cyto.2015.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Heller NM, Dasgupta P, Dorsey NJ, et al. : The Type I and Type II Receptor Complexes for IL-4 and IL-13 Differentially Regulate Allergic Lung Inflammation, Allergic Diseases. In: Pereira C, editor. Highlights in the Clinic, Mechanisms and Treatment2012. 10.5772/25650 [DOI] [Google Scholar]
- 52. Barnes PJ: Pathophysiology of allergic inflammation. Immunol Rev. 2011;242(1):31–50. 10.1111/j.1600-065X.2011.01020.x [DOI] [PubMed] [Google Scholar]
- 53. Wills-Karp M, Luyimbazi J, Xu X, et al. : Interleukin-13: central mediator of allergic asthma. Science. 1998;282(5397):2258–61. 10.1126/science.282.5397.2258 [DOI] [PubMed] [Google Scholar]
- 54. Barner M, Mohrs M, Brombacher F, et al. : Differences between IL-4R alpha-deficient and IL-4-deficient mice reveal a role for IL-13 in the regulation of Th2 responses. Curr Biol. 1998;8(11):669–72. 10.1016/S0960-9822(98)70256-8 [DOI] [PubMed] [Google Scholar]
- 55. Müller U, Piehler D, Stenzel W, et al. : Lack of IL-4 receptor expression on T helper cells reduces T helper 2 cell polyfunctionality and confers resistance in allergic bronchopulmonary mycosis. Mucosal Immunol. 2012;5(3):299–310. 10.1038/mi.2012.9 [DOI] [PubMed] [Google Scholar]
- 56. Cortina SD, Drotar D, Ericksen M, et al. : Genetic biomarkers of health-related quality of life in pediatric asthma. J Pediatr. 2011;159(1):21–26.e1. 10.1016/j.jpeds.2010.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Xue H, Sun K, Xie W, et al. : [Meta-analysis on interleukin-4 receptor α chain Q576R gene polymorphisms and bronchial asthma susceptibility]. Zhonghua Jie He He Hu Xi Za Zhi. 2010;33(11):831–6. 10.3760/cma.j.issn.1001-0939.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 58. Knutsen AP, Vijay HM, Kariuki B, et al. : Association of IL-4RA single nucleotide polymorphisms, HLA-DR and HLA-DQ in children with Alternaria-sensitive moderate-severe asthma. Clin Mol Allergy. 2010;8:5. 10.1186/1476-7961-8-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. McDonough H, Patterson C: CHIP: a link between the chaperone and proteasome systems. Cell Stress Chaperones. 2003;8(4):303–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wei Q, Sha Y, Bhattacharya A, et al. : Regulation of IL-4 receptor signaling by STUB1 in lung inflammation. Am J Respir Crit Care Med. 2014;189(1):16–29. 10.1164/rccm.201305-0874OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wenzel S, Wilbraham D, Fuller R, et al. : Effect of an interleukin-4 variant on late phase asthmatic response to allergen challenge in asthmatic patients: results of two phase 2a studies. Lancet. 2007;370(9596):1422–31. 10.1016/S0140-6736(07)61600-6 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 62. Wenzel SE, Ind PW, Otulana BA, et al. : Inhaled pitrakinra, an IL-4/IL-13 antagonist, reduced exacerbations in patients with eosinophilic asthma. Eur Respir J. 2010;2010;36: P3980: 1. Reference Source [Google Scholar]
- 63. Slager RE, Hawkins GA, Ampleford EJ, et al. : IL-4 receptor α polymorphisms are predictors of a pharmacogenetic response to a novel IL-4/IL-13 antagonist. J Allergy Clin Immunol. 2010;126(4):875–8. 10.1016/j.jaci.2010.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Munitz A, Brandt EB, Mingler M, et al. : Distinct roles for IL-13 and IL-4 via IL-13 receptor alpha1 and the type II IL-4 receptor in asthma pathogenesis. Proc Natl Acad Sci U S A. 2008;105(20):7240–5. 10.1073/pnas.0802465105 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 65. Wynn TA: IL-13 effector functions. Annu Rev Immunol. 2003;21:425–56. 10.1146/annurev.immunol.21.120601.141142 [DOI] [PubMed] [Google Scholar]
- 66. Ramalingam TR, Pesce JT, Sheikh F, et al. : Unique functions of the type II interleukin 4 receptor identified in mice lacking the interleukin 13 receptor alpha1 chain. Nat Immunol. 2008;9(1):25–33. 10.1038/ni1544 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 67. Karo-Atar D, Bordowitz A, Wand O, et al. : A protective role for IL-13 receptor α 1 in bleomycin-induced pulmonary injury and repair. Mucosal Immunol. 2016;9(1):240–53. 10.1038/mi.2015.56 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 68. Cao C, Zhao J, Doughty EK, et al. : Mac-1 Regulates IL-13 Activity in Macrophages by Directly Interacting with IL-13Rα1. J Biol Chem. 2015;290(35):21642–51. 10.1074/jbc.M115.645796 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 69. Gauvreau GM, Boulet L, Cockcroft DW, et al. : Effects of interleukin-13 blockade on allergen-induced airway responses in mild atopic asthma. Am J Respir Crit Care Med. 2011;183(8):1007–14. 10.1164/rccm.201008-1210OC [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 70. De Boever EH, Ashman C, Cahn AP, et al. : Efficacy and safety of an anti-IL-13 mAb in patients with severe asthma: a randomized trial. J Allergy Clin Immunol. 2014;133(4):989–96. 10.1016/j.jaci.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 71. Noonan M, Korenblat P, Mosesova S, et al. : Dose-ranging study of lebrikizumab in asthmatic patients not receiving inhaled steroids. J Allergy Clin Immunol. 2013;132(3):567–574.e12. 10.1016/j.jaci.2013.03.051 [DOI] [PubMed] [Google Scholar]
- 72. Feng N, Lugli SM, Schnyder B, et al. : The interleukin-4/interleukin-13 receptor of human synovial fibroblasts: overexpression of the nonsignaling interleukin-13 receptor alpha2. Lab Invest. 1998;78(5):591–602. [PubMed] [Google Scholar]
- 73. Wang W, Shen YX, Li J, et al. : Enhanced expression of the decoy receptor IL-13Ralpha2 in macrophages of Schistosoma japonicum-infected mice. Chin Med J (Engl). 2009;122(14):1650–4. 10.3760/cma.j.issn.0366-6999.2009.14.009 [DOI] [PubMed] [Google Scholar]
- 74. Lee CM, He CH, Nour AM, et al. : IL-13Rα2 uses TMEM219 in chitinase 3-like-1-induced signalling and effector responses. Nat Commun. 2016;7: 12752. 10.1038/ncomms12752 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 75. Fichtner-Feigl S, Strober W, Kawakami K, et al. : IL-13 signaling through the IL-13alpha 2 receptor is involved in induction of TGF-beta 1 production and fibrosis. Nat Med. 2006;12(1):99–106. 10.1038/nm1332 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 76. Mandal D, Levine AD: Elevated IL-13Ralpha2 in intestinal epithelial cells from ulcerative colitis or colorectal cancer initiates MAPK pathway. Inflamm Bowel Dis. 2010;16(5):753–64. 10.1002/ibd.21133 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 77. Chen W, Sivaprasad U, Gibson AM, et al. : IL-13 receptor α2 contributes to development of experimental allergic asthma. J Allergy Clin Immunol. 2013;132(4):951–8.e1–6. 10.1016/j.jaci.2013.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Nezgovorova V, Liu Q, Hu B, et al. : Sputum Gene Expression of IL-13 Receptor α2 Chain Correlates with Airflow Obstruction and Helper T-Cell Type 2 Inflammation in Asthma. Ann Am Thorac Soc. 2016;13(Suppl 1):S96–7. [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 79. Kuperman DA, Schleimer RP: Interleukin-4, interleukin-13, signal transducer and activator of transcription factor 6, and allergic asthma. Curr Mol Med. 2008;8(5):384–92. 10.2174/156652408785161032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Heller NM, Qi X, Junttila IS, et al. : Type I IL-4Rs selectively activate IRS-2 to induce target gene expression in macrophages. Sci Signal. 2008;1(51):ra17. 10.1126/scisignal.1164795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Dasgupta P, Dorsey NJ, Li J, et al. : The adaptor protein insulin receptor substrate 2 inhibits alternative macrophage activation and allergic lung inflammation. Sci Signal. 2016;9(433):ra63. 10.1126/scisignal.aad6724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. McCormick SM, Gowda N, Fang JX, et al. : Suppressor of Cytokine Signaling (SOCS)1 Regulates Interleukin-4 (IL-4)-activated Insulin Receptor Substrate (IRS)-2 Tyrosine Phosphorylation in Monocytes and Macrophages via the Proteasome. J Biol Chem. 2016;291(39):20574–87. 10.1074/jbc.M116.746164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Meguro K, Nakagomi D, Suzuki K, et al. : SOCS3 Expressed in M2 Macrophages Attenuates Contact Hypersensitivity by Suppressing MMP-12 Production. J Invest Dermatol. 2016;136(3):649–57. 10.1016/j.jid.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 84. Kubo M, Inoue H: Suppressor of cytokine signaling 3 (SOCS3) in Th2 cells evokes Th2 cytokines, IgE, and eosinophilia. Curr Allergy Asthma Rep. 2006;6(1):32–9. 10.1007/s11882-006-0007-6 [DOI] [PubMed] [Google Scholar]
- 85. López E, Zafra MP, Sastre B, et al. : Suppressors of cytokine signaling 3 expression in eosinophils: regulation by PGE 2 and Th2 cytokines. Clin Dev Immunol. 2011;2011: 917015. 10.1155/2011/917015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Fukuyama S, Nakano T, Matsumoto T, et al. : Pulmonary suppressor of cytokine signaling-1 induced by IL-13 regulates allergic asthma phenotype. Am J Respir Crit Care Med. 2009;179(11):992–8. 10.1164/rccm.200806-992OC [DOI] [PubMed] [Google Scholar]
- 87. Horiuchi Y, Bae SJ, Katayama I: Overexpression of the suppressor of cytokine signalling 3 (SOCS3) in severe atopic dermatitis. Clin Exp Dermatol. 2006;31(1):100–4. 10.1111/j.1365-2230.2005.01979.x [DOI] [PubMed] [Google Scholar]
- 88. Seki Y, Inoue H, Nagata N, et al. : SOCS-3 regulates onset and maintenance of T (H)2-mediated allergic responses. Nat Med. 2003;9(8):1047–54. 10.1038/nm896 [DOI] [PubMed] [Google Scholar]
- 89. Mostecki J, Cassel SL, Klimecki WT, et al. : A SOCS-1 promoter variant is associated with total serum IgE levels. J Immunol. 2011;187(5):2794–802. 10.4049/jimmunol.0902569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Jager LD, Dabelic R, Waiboci LW, et al. : The kinase inhibitory region of SOCS-1 is sufficient to inhibit T-helper 17 and other immune functions in experimental allergic encephalomyelitis. J Neuroimmunol. 2011;232(1–2):108–18. 10.1016/j.jneuroim.2010.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Mack I, Hector A, Ballbach M, et al. : The role of chitin, chitinases, and chitinase-like proteins in pediatric lung diseases. Mol Cell Pediatr. 2015;2(1):3. 10.1186/s40348-015-0014-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. van Dyken SJ, Garcia D, Porter P, et al. : Fungal chitin from asthma-associated home environments induces eosinophilic lung infiltration. J Immunol. 2011;187(5):2261–7. 10.4049/jimmunol.1100972 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 93. Yasuda K, Muto T, Kawagoe T, et al. : Contribution of IL-33-activated type II innate lymphoid cells to pulmonary eosinophilia in intestinal nematode-infected mice. Proc Natl Acad Sci U S A. 2012;109(9):3451–6. 10.1073/pnas.1201042109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Khosravi AR, Erle DJ: Chitin-Induced Airway Epithelial Cell Innate Immune Responses Are Inhibited by Carvacrol/Thymol. PLoS One. 2016;11(7):e0159459. 10.1371/journal.pone.0159459 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 95. Zhu Z, Zheng T, Homer RJ, et al. : Acidic mammalian chitinase in asthmatic Th2 inflammation and IL-13 pathway activation. Science. 2004;304(5677):1678–82. 10.1126/science.1095336 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 96. Chupp GL, Lee CG, Jarjour N, et al. : A chitinase-like protein in the lung and circulation of patients with severe asthma. N Engl J Med. 2007;357(20):2016–27. 10.1056/NEJMoa073600 [DOI] [PubMed] [Google Scholar]
- 97. Park JA, Drazen JM, Tschumperlin DJ: The chitinase-like protein YKL-40 is secreted by airway epithelial cells at base line and in response to compressive mechanical stress. J Biol Chem. 2010;285(39):29817–25. 10.1074/jbc.M110.103416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Tang H, Shi Z, Xiu Q, et al. : YKL-40-mediated interleukin 8 production may be closely associated with remodeling of bronchial smooth muscle cells. Am J Respir Crit Care Med. 2012;186(4):386; author reply 386–7. 10.1164/ajrccm.186.4.386a [DOI] [PubMed] [Google Scholar]
- 99. Liu C, Li Q, Zhou X, et al. : The chitinase-like protein YKL-40 increases mucin5AC production in human bronchial epithelial cells. Exp Cell Res. 2013;319(18):2866–73. 10.1016/j.yexcr.2013.08.009 [DOI] [PubMed] [Google Scholar]
- 100. Bara I, Ozier A, Girodet PO, et al. : Role of YKL-40 in bronchial smooth muscle remodeling in asthma. Am J Respir Crit Care Med. 2012;185(7):715–22. 10.1164/rccm.201105-0915OC [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 101. Holcomb IN, Kabakoff RC, Chan B, et al. : FIZZ1, a novel cysteine-rich secreted protein associated with pulmonary inflammation, defines a new gene family. EMBO J. 2000;19(15):4046–55. 10.1093/emboj/19.15.4046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Ma WL, Ye H, Tao XN, et al. : [Dynamic changes of found in inflammatory zone 1 protein and mRNA expression in the lung with experimental pulmonary fibrosis of the rat.]. Sheng Li Xue Bao. 2005;57(4):493–7. [PubMed] [Google Scholar]
- 103. Reece JJ, Siracusa MC, Scott AL: Innate immune responses to lung-stage helminth infection induce alternatively activated alveolar macrophages. Infect Immun. 2006;74(9):4970–81. 10.1128/IAI.00687-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Lee MR, Shim D, Yoon J, et al. : Retnla overexpression attenuates allergic inflammation of the airway. PLoS One. 2014;9(11):e112666. 10.1371/journal.pone.0112666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Nair MG, Du Y, Perrigoue JG, et al. : Alternatively activated macrophage-derived RELM-{alpha} is a negative regulator of type 2 inflammation in the lung. J Exp Med. 2009;206(4):937–52. 10.1084/jem.20082048 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 106. Chan PY, Carrera Silva EA, De Kouchkovsky D, et al. : The TAM family receptor tyrosine kinase TYRO3 is a negative regulator of type 2 immunity. Science. 2016;352(6281):99–103. 10.1126/science.aaf1358 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 107. Gao Y, Nish SA, Jiang R, et al. : Control of T helper 2 responses by transcription factor IRF4-dependent dendritic cells. Immunity. 2013;39(4):722–32. 10.1016/j.immuni.2013.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 108. Kumamoto Y, Linehan M, Weinstein JS, et al. : CD301b + dermal dendritic cells drive T helper 2 cell-mediated immunity. Immunity. 2013;39(4):733–43. 10.1016/j.immuni.2013.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Griesser H, Mak TW: The T-cell receptor--structure, function, and clinical application. Hematol Pathol. 1994;8(1–2):1–23. [PubMed] [Google Scholar]
- 110. Yoshimura S, Gerondopoulos A, Linford A, et al. : Family-wide characterization of the DENN domain Rab GDP-GTP exchange factors. J Cell Biol. 2010;191(2):367–81. 10.1083/jcb.201008051 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 111. Yang C, Hojer CD, Zhou M, et al. : Regulation of T Cell Receptor Signaling by DENND1B in T H2 Cells and Allergic Disease. Cell. 2016;164(1–2):141–55. 10.1016/j.cell.2015.11.052 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 112. Nurieva RI, Zheng S, Jin W, et al. : The E3 ubiquitin ligase GRAIL regulates T cell tolerance and regulatory T cell function by mediating T cell receptor-CD3 degradation. Immunity. 2010;32(5):670–80. 10.1016/j.immuni.2010.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Sahoo A, Alekseev A, Obertas L, et al. : Grail controls Th2 cell development by targeting STAT6 for degradation. Nat Commun. 2014;5: 4732. 10.1038/ncomms5732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Qiao G, Ying H, Zhao Y, et al. : E3 ubiquitin ligase Cbl-b suppresses proallergic T cell development and allergic airway inflammation. Cell Rep. 2014;6(4):709–23. 10.1016/j.celrep.2014.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Lajoie S, Lewkowich IP, Suzuki Y, et al. : Complement-mediated regulation of the IL-17A axis is a central genetic determinant of the severity of experimental allergic asthma. Nat Immunol. 2010;11(10):928–35. 10.1038/ni.1926 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 116. Wakashin H, Hirose K, Maezawa Y, et al. : IL-23 and Th17 cells enhance Th2-cell-mediated eosinophilic airway inflammation in mice. Am J Respir Crit Care Med. 2008;178(10):1023–32. 10.1164/rccm.200801-086OC [DOI] [PubMed] [Google Scholar]
- 117. Hall SL, Baker T, Lajoie S, et al. : IL-17A enhances IL-13 activity by enhancing IL-13-induced signal transducer and activator of transcription 6 activation. J Allergy Clin Immunol. 2017;139(2):462–471.e14. 10.1016/j.jaci.2016.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 118. Choy DF, Hart KM, Borthwick LA, et al. : T H2 and T H17 inflammatory pathways are reciprocally regulated in asthma. Sci Transl Med. 2015;7(301):301ra129. 10.1126/scitranslmed.aab3142 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 119. Busse WW, Holgate S, Kerwin E, et al. : Randomized, double-blind, placebo-controlled study of brodalumab, a human anti-IL-17 receptor monoclonal antibody, in moderate to severe asthma. Am J Respir Crit Care Med. 2013;188(11):1294–302. 10.1164/rccm.201212-2318OC [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 120. Maier E, Werner D, Duschl A, et al. : Human Th2 but not Th9 cells release IL-31 in a STAT6/NF-κB-dependent way. J Immunol. 2014;193(2):645–54. 10.4049/jimmunol.1301836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Edukulla R, Singh B, Jegga AG, et al. : Th2 Cytokines Augment IL-31/IL-31RA Interactions via STAT6-dependent IL-31RA Expression. J Biol Chem. 2015;290(21):13510–20. 10.1074/jbc.M114.622126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Lai T, Wu D, Li W, et al. : Interleukin-31 expression and relation to disease severity in human asthma. Sci Rep. 2016;6: 22835. 10.1038/srep22835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Yu J, Han WC, Yun K, et al. : Identifying Polymorphisms in IL-31 and Their Association with Susceptibility to Asthma. Korean J Pathol. 2012;46(2):162–8. 10.4132/KoreanJPathol.2012.46.2.162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Perrigoue JG, Zaph C, Guild K, et al. : IL-31-IL-31R interactions limit the magnitude of Th2 cytokine-dependent immunity and inflammation following intestinal helminth infection. J Immunol. 2009;182(10):6088–94. 10.4049/jimmunol.0802459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Zhou B, Comeau MR, De Smedt T, et al. : Thymic stromal lymphopoietin as a key initiator of allergic airway inflammation in mice. Nat Immunol. 2005;6(10):1047–53. 10.1038/ni1247 [DOI] [PubMed] [Google Scholar]
- 126. Han H, Headley MB, Xu W, et al. : Thymic stromal lymphopoietin amplifies the differentiation of alternatively activated macrophages. J Immunol. 2013;190(3):904–12. 10.4049/jimmunol.1201808 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 127. Al-Shami A, Spolski R, Kelly J, et al. : A role for TSLP in the development of inflammation in an asthma model. J Exp Med. 2005;202(6):829–39. 10.1084/jem.20050199 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 128. Cheng DT, Ma C, Niewoehner J, et al. : Thymic stromal lymphopoietin receptor blockade reduces allergic inflammation in a cynomolgus monkey model of asthma. J Allergy Clin Immunol. 2013;132(2):455–62. 10.1016/j.jaci.2013.05.011 [DOI] [PubMed] [Google Scholar]
- 129. Vannella KM, Ramalingam TR, Borthwick LA, et al. : Combinatorial targeting of TSLP, IL-25, and IL-33 in type 2 cytokine-driven inflammation and fibrosis. Sci Transl Med. 2016;8(337):337ra65. 10.1126/scitranslmed.aaf1938 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 130. Kido M, Tanaka J, Aoki N, et al. : Helicobacter pylori promotes the production of thymic stromal lymphopoietin by gastric epithelial cells and induces dendritic cell-mediated inflammatory Th2 responses. Infect Immun. 2010;78(1):108–14. 10.1128/IAI.00762-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Kitajima M, Lee H, Nakayama T, et al. : TSLP enhances the function of helper type 2 cells. Eur J Immunol. 2011;41(7):1862–71. 10.1002/eji.201041195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Li H, Chen ZG, Liu H, et al. : Treatment of allergic rhinitis with CpG oligodeoxynucleotides alleviates the lower airway outcomes of combined allergic rhinitis and asthma syndrome via a mechanism that possibly involves in TSLP. Exp Lung Res. 2016;42(6):322–33. 10.1080/01902148.2016.1215571 [DOI] [PubMed] [Google Scholar]
- 133. Reardon C, Lechmann M, Brüstle A, et al. : Thymic stromal lymphopoetin-induced expression of the endogenous inhibitory enzyme SLPI mediates recovery from colonic inflammation. Immunity. 2011;35(2):223–35. 10.1016/j.immuni.2011.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 134. Noble CL, Abbas AR, Lees CW, et al. : Characterization of intestinal gene expression profiles in Crohn's disease by genome-wide microarray analysis. Inflamm Bowel Dis. 2010;16(10):1717–28. 10.1002/ibd.21263 [DOI] [PubMed] [Google Scholar]
- 135. Eri RD, Adams RJ, Tran TV, et al. : An intestinal epithelial defect conferring ER stress results in inflammation involving both innate and adaptive immunity. Mucosal Immunol. 2011;4(3):354–64. 10.1038/mi.2010.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Zaph C, Troy AE, Taylor BC, et al. : Epithelial-cell-intrinsic IKK-beta expression regulates intestinal immune homeostasis. Nature. 2007;446(7135):552–6. 10.1038/nature05590 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 137. Biton M, Levin A, Slyper M, et al. : Epithelial microRNAs regulate gut mucosal immunity via epithelium-T cell crosstalk. Nat Immunol. 2011;12(3):239–46. 10.1038/ni.1994 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 138. Blázquez AB, Mayer L, Berin MC: Thymic stromal lymphopoietin is required for gastrointestinal allergy but not oral tolerance. Gastroenterology. 2010;139(4):1301–9. 10.1053/j.gastro.2010.06.055 [DOI] [PubMed] [Google Scholar]
- 139. Taylor BC, Zaph C, Troy AE, et al. : TSLP regulates intestinal immunity and inflammation in mouse models of helminth infection and colitis. J Exp Med. 2009;206(3):655–67. 10.1084/jem.20081499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Gauvreau GM, O'Byrne PM, Boulet LP, et al. : Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. N Engl J Med. 2014;370(22):2102–10. 10.1056/NEJMoa1402895 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 141. Fort MM, Cheung J, Yen D, et al. : IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity. 2001;15(6):985–95. 10.1016/S1074-7613(01)00243-6 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 142. Valizadeh A, Khosravi A, Zadeh LJ, et al. : Role of IL-25 in Immunity. J Clin Diagn Res. 2015;9(4):OE01–4. 10.7860/JCDR/2015/12235.5814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. von Moltke J, Ji M, Liang HE, et al. : Tuft-cell-derived IL-25 regulates an intestinal ILC2-epithelial response circuit. Nature. 2016;529(7585):221–5. 10.1038/nature16161 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 144. Gerbe F, Legraverend C, Jay P: The intestinal epithelium tuft cells: specification and function. Cell Mol Life Sci. 2012;69(17):2907–17. 10.1007/s00018-012-0984-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Gronke K, Diefenbach A: Tuft cell-derived IL-25 activates and maintains ILC2. Immunol Cell Biol. 2016;94(3):221–3. 10.1038/icb.2016.10 [DOI] [PubMed] [Google Scholar]
- 146. Willis CR, Siegel L, Leith A, et al. : IL-17RA Signaling in Airway Inflammation and Bronchial Hyperreactivity in Allergic Asthma. Am J Respir Cell Mol Biol. 2015;53(6):810–21. 10.1165/rcmb.2015-0038OC [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 147. Beale J, Jayaraman A, Jackson DJ, et al. : Rhinovirus-induced IL-25 in asthma exacerbation drives type 2 immunity and allergic pulmonary inflammation. Sci Transl Med. 2014;6(256):256ra134. 10.1126/scitranslmed.3009124 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 148. Schmitz J, Owyang A, Oldham E, et al. : IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23(5):479–90. 10.1016/j.immuni.2005.09.015 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 149. Moffatt MF, Gut IG, Demenais F, et al. : A large-scale, consortium-based genomewide association study of asthma. N Engl J Med. 2010;363(13):1211–21. 10.1056/NEJMoa0906312 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 150. Gordon ED, Simpson LJ, Rios CL, et al. : Alternative splicing of interleukin-33 and type 2 inflammation in asthma. Proc Natl Acad Sci U S A. 2016;113(31):8765–70. 10.1073/pnas.1601914113 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 151. Bartemes KR, Iijima K, Kobayashi T, et al. : IL-33-responsive lineage - CD25 + CD44 (hi) lymphoid cells mediate innate type 2 immunity and allergic inflammation in the lungs. J Immunol. 2012;188(3):1503–13. 10.4049/jimmunol.1102832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Humphreys NE, Xu D, Hepworth MR, et al. : IL-33, a potent inducer of adaptive immunity to intestinal nematodes. J Immunol. 2008;180(4):2443–9. 10.4049/jimmunol.180.4.2443 [DOI] [PubMed] [Google Scholar]
- 153. de Kleer IM, Kool M, de Bruijn MJ, et al. : Perinatal Activation of the Interleukin-33 Pathway Promotes Type 2 Immunity in the Developing Lung. Immunity. 2016;45(6):1285–98. 10.1016/j.immuni.2016.10.031 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 154. Xu D, Chan WL, Leung BP, et al. : Selective expression of a stable cell surface molecule on type 2 but not type 1 helper T cells. J Exp Med. 1998;187(5):787–94. 10.1084/jem.187.5.787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Cayrol C, Girard JP: The IL-1-like cytokine IL-33 is inactivated after maturation by caspase-1. Proc Natl Acad Sci U S A. 2009;106(22):9021–6. 10.1073/pnas.0812690106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Lefrançais E, Duval A, Mirey E, et al. : Central domain of IL-33 is cleaved by mast cell proteases for potent activation of group-2 innate lymphoid cells. Proc Natl Acad Sci U S A. 2014;111(43):15502–7. 10.1073/pnas.1410700111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Polumuri SK, Jayakar GG, Shirey KA, et al. : Transcriptional regulation of murine IL-33 by TLR and non-TLR agonists. J Immunol. 2012;189(1):50–60. 10.4049/jimmunol.1003554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Yamazumi Y, Sasaki O, Imamura M, et al. : The RNA Binding Protein Mex-3B Is Required for IL-33 Induction in the Development of Allergic Airway Inflammation. Cell Rep. 2016;16(9):2456–71. 10.1016/j.celrep.2016.07.062 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 159. Garlanda C, Dinarello CA, Mantovani A: The interleukin-1 family: back to the future. Immunity. 2013;39(6):1003–18. 10.1016/j.immuni.2013.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Cayrol C, Girard JP: IL-33: an alarmin cytokine with crucial roles in innate immunity, inflammation and allergy. Curr Opin Immunol. 2014;31:31–7. 10.1016/j.coi.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 161. Moussion C, Ortega N, Girard JP: The IL-1-like cytokine IL-33 is constitutively expressed in the nucleus of endothelial cells and epithelial cells in vivo: a novel 'alarmin'? PLoS One. 2008;3(10):e3331. 10.1371/journal.pone.0003331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Pichery M, Mirey E, Mercier P, et al. : Endogenous IL-33 is highly expressed in mouse epithelial barrier tissues, lymphoid organs, brain, embryos, and inflamed tissues: in situ analysis using a novel Il-33-LacZ gene trap reporter strain. J Immunol. 2012;188(7):3488–95. 10.4049/jimmunol.1101977 [DOI] [PubMed] [Google Scholar]
- 163. Hristova M, Habibovic A, Veith C, et al. : Airway epithelial dual oxidase 1 mediates allergen-induced IL-33 secretion and activation of type 2 immune responses. J Allergy Clin Immunol. 2016;137(5):1545–1556.e11. 10.1016/j.jaci.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 164. Kouzaki H, Iijima K, Kobayashi T, et al. : The danger signal, extracellular ATP, is a sensor for an airborne allergen and triggers IL-33 release and innate Th2-type responses. J Immunol. 2011;186(7):4375–87. 10.4049/jimmunol.1003020 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 165. Kakkar R, Hei H, Dobner S, et al. : Interleukin 33 as a mechanically responsive cytokine secreted by living cells. J Biol Chem. 2012;287(9):6941–8. 10.1074/jbc.M111.298703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Tsuda H, Komine M, Karakawa M, et al. : Novel splice variants of IL-33: differential expression in normal and transformed cells. J Invest Dermatol. 2012;132(11):2661–4. 10.1038/jid.2012.180 [DOI] [PubMed] [Google Scholar]
- 167. Ragusa R, Cabiati M, Guzzardi MA, et al. : Effects of obesity on IL-33/ST2 system in heart, adipose tissue and liver: study in the experimental model of Zucker rats. Exp Mol Pathol. 2017;102(2):354–9. 10.1016/j.yexmp.2017.03.002 [DOI] [PubMed] [Google Scholar]
- 168. Stav-Noraas TE, Edelmann RJ, La Poulsen LC, et al. : Endothelial IL-33 Expression Is Augmented by Adenoviral Activation of the DNA Damage Machinery. J Immunol. 2017;198(8):3318–25. 10.4049/jimmunol.1600054 [DOI] [PubMed] [Google Scholar]
- 169. Kouidhi S, Elgaaied AB, Chouaib S: Impact of Metabolism on T-Cell Differentiation and Function and Cross Talk with Tumor Microenvironment. Front Immunol. 2017;8:270. 10.3389/fimmu.2017.00270 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 170. Laplante M, Sabatini DM: mTOR signaling in growth control and disease. Cell. 2012;149(2):274–93. 10.1016/j.cell.2012.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Chang CH, Pearce EL: Emerging concepts of T cell metabolism as a target of immunotherapy. Nat Immunol. 2016;17(4):364–8. 10.1038/ni.3415 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 172. Rathmell JC: Metabolism and autophagy in the immune system: immunometabolism comes of age. Immunol Rev. 2012;249(1):5–13. 10.1111/j.1600-065X.2012.01158.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Xu W, Ghosh S, Comhair SA, et al. : Increased mitochondrial arginine metabolism supports bioenergetics in asthma. J Clin Invest. 2016;126(7):2465–81. 10.1172/JCI82925 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 174. Monticelli LA, Buck MD, Flamar AL, et al. : Arginase 1 is an innate lymphoid-cell-intrinsic metabolic checkpoint controlling type 2 inflammation. Nat Immunol. 2016;17(6):656–65. 10.1038/ni.3421 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 175. Colegio OR, Chu NQ, Szabo AL, et al. : Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature. 2014;513(7519):559–63. 10.1038/nature13490 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 176. Selleri S, Bifsha P, Civini S, et al. : Human mesenchymal stromal cell-secreted lactate induces M2-macrophage differentiation by metabolic reprogramming. Oncotarget. 2016;7(21):30193–210. 10.18632/oncotarget.8623 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 177. Roncoroni AJ, Adrougué HJ, De Obrutsky CW, et al. : Metabolic acidosis in status asthmaticus. Respiration. 1976;33(2):85–94. 10.1159/000193721 [DOI] [PubMed] [Google Scholar]
- 178. Mountain RD, Heffner JE, Brackett NC, Jr, et al. : Acid-base disturbances in acute asthma. Chest. 1990;98(3):651–5. 10.1378/chest.98.3.651 [DOI] [PubMed] [Google Scholar]
- 179. Melgert BN, Oriss TB, Qi Z, et al. : Macrophages: regulators of sex differences in asthma? Am J Respir Cell Mol Biol. 2010;42(5):595–603. 10.1165/rcmb.2009-0016OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Peter K, Rehli M, Singer K, et al. : Lactic acid delays the inflammatory response of human monocytes. Biochem Biophys Res Commun. 2015;457(3):412–8. 10.1016/j.bbrc.2015.01.005 [DOI] [PubMed] [Google Scholar]
- 181. Dietl K, Renner K, Dettmer K, et al. : Lactic acid and acidification inhibit TNF secretion and glycolysis of human monocytes. J Immunol. 2010;184(3):1200–9. 10.4049/jimmunol.0902584 [DOI] [PubMed] [Google Scholar]
- 182. Samuvel DJ, Sundararaj KP, Nareika A, et al. : Lactate boosts TLR4 signaling and NF-kappaB pathway-mediated gene transcription in macrophages via monocarboxylate transporters and MD-2 up-regulation. J Immunol. 2009;182(4):2476–84. 10.4049/jimmunol.0802059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Abebayehu D, Spence AJ, Qayum AA, et al. : Lactic Acid Suppresses IL-33-Mediated Mast Cell Inflammatory Responses via Hypoxia-Inducible Factor-1α-Dependent miR-155 Suppression. J Immunol. 2016;197(7):2909–17. 10.4049/jimmunol.1600651 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 184. Ananieva EA, Powell JD, Hutson SM: Leucine Metabolism in T Cell Activation: mTOR Signaling and Beyond. Adv Nutr. 2016;7(4):798S–805S. 10.3945/an.115.011221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Chi H: Regulation and function of mTOR signalling in T cell fate decisions. Nat Rev Immunol. 2012;12(5):325–38. 10.1038/nri3198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Weichhart T, Hengstschläger M, Linke M: Regulation of innate immune cell function by mTOR. Nat Rev Immunol. 2015;15(10):599–614. 10.1038/nri3901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Sasaki CY, Chen G, Munk R, et al. : p( 70S 6K 1) in the TORC1 pathway is essential for the differentiation of Th17 Cells, but not Th1, Th2, or Treg cells in mice. Eur J Immunol. 2016;46(1):212–22. 10.1002/eji.201445422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Huang SC, Smith AM, Everts B, et al. : Metabolic Reprogramming Mediated by the mTORC2-IRF4 Signaling Axis Is Essential for Macrophage Alternative Activation. Immunity. 2016;45(4):817–30. 10.1016/j.immuni.2016.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 189. Byles V, Covarrubias AJ, Ben-Sahra I, et al. : The TSC-mTOR pathway regulates macrophage polarization. Nat Commun. 2013;4: 2834. 10.1038/ncomms3834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Zhu L, Yang T, Li L, et al. : TSC1 controls macrophage polarization to prevent inflammatory disease. Nat Commun. 2014;5: 4696. 10.1038/ncomms5696 [DOI] [PubMed] [Google Scholar]
- 191. Warren KJ, Fang X, Gowda NM, et al. : The TORC1-activated Proteins, p70S6K and GRB10, Regulate IL-4 Signaling and M2 Macrophage Polarization by Modulating Phosphorylation of Insulin Receptor Substrate-2. J Biol Chem. 2016;291(48):24922–30. 10.1074/jbc.M116.756791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Festuccia WT, Pouliot P, Bakan I, et al. : Myeloid-specific Rictor deletion induces M1 macrophage polarization and potentiates in vivo pro-inflammatory response to lipopolysaccharide. PLoS One. 2014;9(4):e95432. 10.1371/journal.pone.0095432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Lee J, Kim TH, Murray F, et al. : Cyclic AMP concentrations in dendritic cells induce and regulate Th2 immunity and allergic asthma. Proc Natl Acad Sci U S A. 2015;112(5):1529–34. 10.1073/pnas.1417972112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Al-Sawalha N, Pokkunuri I, Omoluabi O, et al. : Epinephrine Activation of the β 2-Adrenoceptor Is Required for IL-13-Induced Mucin Production in Human Bronchial Epithelial Cells. PLoS One. 2015;10(7):e0132559. 10.1371/journal.pone.0132559 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 195. Roy SG, Nozaki Y, Phan SH: Regulation of alpha-smooth muscle actin gene expression in myofibroblast differentiation from rat lung fibroblasts. Int J Biochem Cell Biol. 2001;33(7):723–34. 10.1016/S1357-2725(01)00041-3 [DOI] [PubMed] [Google Scholar]
- 196. Kesavan R, Potunuru UR, Nastasijević B, et al. : Inhibition of vascular smooth muscle cell proliferation by Gentiana lutea root extracts. PLoS One. 2013;8(4):e61393. 10.1371/journal.pone.0061393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Chen H, Xia Q, Feng X, et al. : Effect of P2X4R on airway inflammation and airway remodeling in allergic airway challenge in mice. Mol Med Rep. 2016;13(1):697–704. 10.3892/mmr.2015.4622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Kero J, Gissler M, Grönlund MM, et al. : Mode of delivery and asthma -- is there a connection? Pediatr Res. 2002;52(1):6–11. 10.1203/00006450-200207000-00004 [DOI] [PubMed] [Google Scholar]
- 199. Bener A, Ehlayel MS, Alsowaidi S, et al. : Role of breast feeding in primary prevention of asthma and allergic diseases in a traditional society. Eur Ann Allergy Clin Immunol. 2007;39(10):337–43. [PubMed] [Google Scholar]
- 200. Gupta RS, Singh AM, Walkner M, et al. : Hygiene factors associated with childhood food allergy and asthma. Allergy Asthma Proc. 2016;37(6):140–6. 10.2500/aap.2016.37.3988 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 201. Hasegawa K, Linnemann RW, Mansbach JM, et al. : Household siblings and nasal and fecal microbiota in infants. Pediatr Int. 2017;59(4):473–81. 10.1111/ped.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 202. Douwes J, Cheng S, Travier N, et al. : Farm exposure in utero may protect against asthma, hay fever and eczema. Eur Respir J. 2008;32(3):603–11. 10.1183/09031936.00033707 [DOI] [PubMed] [Google Scholar]
- 203. Russell SL, Gold MJ, Willing BP, et al. : Perinatal antibiotic treatment affects murine microbiota, immune responses and allergic asthma. Gut Microbes. 2013;4(2):158–64. 10.4161/gmic.23567 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 204. Murk W, Risnes KR, Bracken MB: Prenatal or early-life exposure to antibiotics and risk of childhood asthma: a systematic review. Pediatrics. 2011;127(6):1125–38. 10.1542/peds.2010-2092 [DOI] [PubMed] [Google Scholar]
- 205. Lodge CJ, Dharmage SC: Breastfeeding and perinatal exposure, and the risk of asthma and allergies. Curr Opin Allergy Clin Immunol. 2016;16(3):231–6. 10.1097/ACI.0000000000000266 [DOI] [PubMed] [Google Scholar]
- 206. Milner JD, Gergen PJ: Transient environmental exposures on the developing immune system: implications for allergy and asthma. Curr Opin Allergy Clin Immunol. 2005;5(3):235–40. 10.1097/01.all.0000168787.59335.8a [DOI] [PubMed] [Google Scholar]
- 207. Hilty M, Burke C, Pedro H, et al. : Disordered microbial communities in asthmatic airways. PLoS One. 2010;5(1):e8578. 10.1371/journal.pone.0008578 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 208. Huang YJ, Nelson CE, Brodie EL, et al. : Airway microbiota and bronchial hyperresponsiveness in patients with suboptimally controlled asthma. J Allergy Clin Immunol. 2011;127(2):372–381.e1-3. 10.1016/j.jaci.2010.10.048 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 209. Arrieta MC, Stiemsma LT, Dimitriu PA, et al. : Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Transl Med. 2015;7(307):307ra152. 10.1126/scitranslmed.aab2271 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 210. Arnold IC, Dehzad N, Reuter S, et al. : Helicobacter pylori infection prevents allergic asthma in mouse models through the induction of regulatory T cells. J Clin Invest. 2011;121(8):3088–93. 10.1172/JCI45041 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 211. Cahenzli J, Köller Y, Wyss M, et al. : Intestinal microbial diversity during early-life colonization shapes long-term IgE levels. Cell Host Microbe. 2013;14(5):559–70. 10.1016/j.chom.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 212. Trompette A, Gollwitzer ES, Yadava K, et al. : Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med. 2014;20(2):159–66. 10.1038/nm.3444 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 213. Kim CH, Park J, Kim M: Gut microbiota-derived short-chain Fatty acids, T cells, and inflammation. Immune Netw. 2014;14(6):277–88. 10.4110/in.2014.14.6.277 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 214. Tamburini S, Shen N, Wu HC, et al. : The microbiome in early life: implications for health outcomes. Nat Med. 2016;22(7):713–22. 10.1038/nm.4142 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation