Abstract
Background
Binge eating is a marker of weight gain and obesity, and a hallmark feature of eating disorders. Yet, its component constructs—overeating and loss of control (LOC) while eating—are poorly understood and difficult to measure.
Objective
To critically review the human literature concerning the validity of LOC and overeating across the age and weight spectrum.
Data sources
English-language articles addressing the face, convergent, discriminant, and predictive validity of LOC and overeating were included.
Results
LOC and overeating appear to have adequate face validity. Emerging evidence supports the convergent and predictive validity of the LOC construct, given its unique cross-sectional and prospective associations with numerous anthropometric, psychosocial, and eating behavior-related factors. Overeating may be best conceptualized as a marker of excess weight status.
Limitations
Binge eating constructs, particularly in the context of subjectively large episodes, are challenging to measure reliably. Few studies addressed overeating in the absence of LOC, thereby limiting conclusions about the validity of the overeating construct independent of LOC. Additional studies addressing the discriminant validity of both constructs are warranted.
Discussion
Suggestions for future weight-related research and for appropriately defining binge eating in the eating disorders diagnostic scheme are presented.
Keywords: Binge eating, loss of control, overeating, validity
Binge eating and overeating are two prevalent obesity-related phenotypes that contribute to excess energy intake and weight gain.1 Binge eating is characterized by the subjective experience of loss of control (LOC) while eating, irrespective of the actual amount of food consumed. Overeating is characterized by eating a large amount of food, irrespective of LOC. Therefore, LOC and overeating are two independent but inter-related constructs.
In addition to being associated with weight-related characteristics, binge eating is a hallmark feature of eating disorders, which affect up to 5% of the population.2 An additional 10–15% of individuals in the community report LOC and overeating behaviors that fail to meet the size and/or frequency thresholds for these diagnoses.3,4 Because LOC and overeating lie at the intersection of obesity and eating disorders, researchers have studied these constructs more closely over the past several decades.
Research suggests that LOC is uniquely related to weight-related and psychosocial outcomes, while overeating may best be conceptualized as a marker of risk for excess weight gain and obesity.5 However, both constructs have been difficult to operationalize and measure reliably because of their complexity and variability in phenotypic presentation. The current paper critically reviews the human literature supporting and challenging the validity of binge eating constructs. Studies related to face, convergent, discriminant, and predictive validity of LOC and overeating are described and synthesized with the goal of highlighting major gaps in the literature and emphasizing priorities for future research.
Methods
Searches of PUBMED and PSYCINFO were conducted between November, 2015 and July, 2016 to identify peer-reviewed articles published in English-language journals. No start date was enforced in the search. Search terms included, “loss of control,” “overeating,” “binge eating,” “objective,” “subjective,” and “large.” Reference lists of identified articles were also searched to locate additional studies.
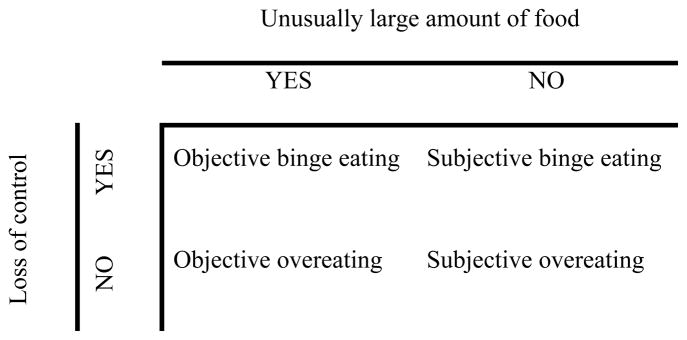
To address whether LOC and overeating are uniquely valid constructs, special efforts were made to identify studies that investigated LOC irrespective of episode size, and overeating irrespective of LOC. Thus, four types of binge eating and overeating episodes were assessed:6 objective binge eating (OBE) involving consumption of an unambiguously large amount of food accompanied by LOC; subjective binge eating (SBE) involving LOC while eating an amount of food that is deemed excessive by the respondent, but is not unusually large according to clinical rating standards; objective overeating (OO) involving consumption of an unambiguously large amount of food in the absence of LOC; and subjective overeating (SO), involving consumption an amount of food that is considered excessive by the respondent, but is not unusually large by clinical rating standards, in the absence of LOC (see Figure 1).
Figure 1.
Matrix of binge eating constructs
Data addressing face validity (the degree to which the measurement of a construct reflects what it is purported to measure) were included if they pertained to individuals’ appraisals of their own or others’ LOC and/or overeating behaviors. Data concerning convergent validity (the extent to which a construct is related to other constructs to which it should theoretically be related) and discriminant validity (the extent to which a construct empirically differs from theoretically unrelated constructs) were included if they pertained to cross-sectional associations among binge eating constructs and other anthropometric, psychosocial, or behavioral constructs. Data addressing predictive validity (the degree to which a construct predicts meaningful outcomes) were included if they referred to longitudinal outcomes of binge eating constructs, that is, if assessment of binge eating constructs preceded assessment of relevant outcomes. EMA data were included with studies of convergent validity, rather than studies of predictive validity, because although analysis of EMA data is often prospective in that it assesses momentary antecedents and consequences of binge eating constructs, extant EMA studies of binge eating constructs are focused on capturing a cross-section of experiences as opposed to investigating how these constructs longitudinally predict experiential outcomes. Across validity domains, studies that did not attempt to parse the unique effects of LOC and overeating (e.g., comparisons of individuals with BED and healthy controls, which are confounded by size, frequency, and duration criteria for the disorder) were not included.
This review focuses primarily on studies of children and adults with overweight and obesity. However, given the relevance of binge eating constructs to eating disorders classification, studies conducted in eating disordered samples are also included. Although analogue studies have been developed to approximate binge eating in animals,7 these studies were beyond the scope of this review and thus were not included.
Assessment
In order to facilitate an understanding of the ways in which the validity of LOC and overeating have been explored, a detailed description of current methods for measuring binge eating constructs is provided in Table 1. In short, binge eating constructs are most commonly assessed via semi-structured interviews and self-report measures, the latter of which includes pencil-and-paper questionnaires, self-monitoring records, and ecological momentary assessment (EMA). Directly observing binge eating constructs via feeding laboratory paradigms is an alternate methodology that avoids many of the biases inherent in assessments based upon self-report. Emerging research suggests that psychophysiological assessment may also be useful in directly observing objective, in vivo markers of binge eating constructs.
Table 1.
Description of tools for measuring binge eating constructs
| Domain | Description | Strengths | Limitations | Measures | ||
|---|---|---|---|---|---|---|
|
Respondent-based measures
| ||||||
| Title | Age | Sample items | ||||
| Semi-structured interviews | Trained assessors rate behavioral, cognitive, and affective experiences based on information provided by respondents |
|
|
Eating Disorder Examination6 | 14+* |
|
| Eating Disorders Assessment for DSM-5104 | 18+ |
|
||||
| Structured Clinical Interview for DSM-IV-TR Axis I Disorders: Patient Edition105 | 18+ |
|
||||
| Structured Interview for Anorexic and Bulimic Syndromes106 | 18+ |
|
||||
|
| ||||||
| Self-report questionnaires | Respondents read and independently respond to written questions |
|
|
Binge Eating Scale107 | 18+ |
|
| Eating Attitudes Test108 | 11–18* |
|
||||
| Eating Disorder Diagnostic Scale109 | 13–65 |
|
||||
| Eating Disorder Examination-Questionnaire110 | 16+* |
|
||||
| Questionnaire on Eating and Weight Patterns111 | 18+* |
|
||||
| Loss of Control Over Eating scale112 |
|
|||||
| Eating Loss of Control scale113 | 18+ |
|
||||
|
| ||||||
| Self-monitoring | Respondents record the occurrence of target behaviors and their correlates in the natural environment |
|
|
|
||
|
| ||||||
|
Laboratory-based measures
| ||||||
| Feeding laboratory paradigms | Standardized test meals designed to model LOC and/or overeating episodes administered under controlled conditions |
|
|
|
||
|
| ||||||
| Physiological assessment | Physiological responses tracked during exposure to real or imagined food-related cues |
|
|
Neuroimaging |
|
|
| Eye-tracking |
|
|||||
| Other |
|
|||||
Abbreviations: LOC=loss of control
Also available in formats adapted for youth.
Results
Face Validity
A total of 8 adult and 2 pediatric studies addressing the face validity of LOC and overeating were identified; results of these studies are summarized in Table 2. 75–90% of adults identified LOC as critical in their personal appraisals of binge eating, and 43–90% identified overeating.8–10 LOC was identified less frequently than overeating in personal definitions of binge eating among college students and adolescents.11–13 Factors that influenced binge ratings included BED status, gender of raters and models, and sample composition (e.g., lay persons, clinicians).11,14–16
Table 2.
Summary of studies assessing the face validity of binge eating constructs
| Reference | Sample | n | % female | Age | BMI | Procedure | Summary of main findings |
|---|---|---|---|---|---|---|---|
|
Adults
| |||||||
| 10 | TS: family practice patients | 243 | 100 | 26.6±5.5 | NR | Participants completed EDE and a subset defined binge eating in their own words | 83% of EDE-defined OBE labeled as binges 42% of EDE-defined SBE labeled as binges 19% of EDE-defined OO labeled as binges 13% of EDE-defined SO labeled as binges 93% of participants required large amount of food to classify binge episodes 90% of participants required LOC to classify binge episodes |
|
| |||||||
| 9 | TS: bariatric surgery | 197 | 100 | 39.8±11.2 | 43.0±6.7 | Eating and Exercise Examination interview for quantity/quality of eating episodes | LOC predicted self-reported binge eating (B=.16, t=5.19***) Of women who self-reported binge eating: 75% reported associated LOC; 25% did not report associated LOC; 61% reported consuming ≥6 or more servings of food; 19% reported consuming 1–4 servings of food Of women who self-reported overeating, 22% reported associated LOC but did not define episodes as binge eating |
|
| |||||||
| 114 | NTS: college students | 99 | 76.8 | 25.5 | NR | Vignettes of a model eating varied according to quantity, duration, and LOC, and rated on binge scales | Larger size [t(95)=340.05***] and LOC [t(98)=119.10***] predicted judgements of episodes as binges |
|
| |||||||
| 14 | NTS: community-based | 48 | 100 | 38.9±11.4 | 34.6 | Participants recorded type/amount of food and duration of eating episodes for 3 weeks; peer and dietitian judges rated randomly selected eating episodes as binges or non-binges | Peer judges more likely than dietitians to label eating episodes as binges for participants with full- (z=4.61***) and subthreshold BED (z=3.09**) Peer κ=.39 Dietitian κ=.44 Peer vs. dietitian κ=.40–.48 Participants vs. peer and dietitian κ=.07–.19 |
|
| |||||||
| 15 | NTS: community-based with BED | 23 | 95.7 | 44.7±10.9 | NR | Vignettes of a model eating varied according to quantity, duration, and LOC, and rated on binge scales | Episodes involving a large quantity of food [F(1,80)=374.93**] or LOC [F(1,80)=109.90***] rated as more binge-like Episodes rated as more binge-like if a large amount of food consumed when LOC was present [F(1,80)=3.95*] Participants with BED rated vignettes involving large amounts of food higher on binge scale compared to undergraduates [F(2,80)=4.92**] |
| NTS: mental health professionals | 34 | 50.0 | 30.2±2.2 | ||||
| NTS: college students | 25 | 88.0 | 40.2±8.1 | ||||
|
| |||||||
| 16 | NTS: college students sample 1 | 238 | 70.0 | 20.2±3.0 | 22.3±3.7 | Videotaped eating episodes varied according to model’s gender and quantity of food, and rated as binges/non-binges | Larger size predicted judgements of episodes as binges [Wald χ2(1)=21.22***] |
| NTS: college students sample 2 | 139 | 66.0 | 19.8±2.8 | 22.4±3.0 | |||
| NTS: college students sample 3 | 83 | 59.0 | 20.6±3.7 | 23.0±3.4 | |||
|
| |||||||
| 11 | NTS: college students | 969 | 64.0 | Range=18–40+ | NR | Participants asked to define binge eating in their own words | ~10–25% of participants endorsed LOC as necessary to define a binge; ~65–75% identified quantity of food consumed as necessary to define a binge Individuals with BED identified LOC in defining a binge more frequently than those without BED [χ2(1)=6.57*] Males and females with and without BED were similarly likely to identify quantity in defining a binge |
|
| |||||||
| 8 | NTS: community-based with BED | 60 | 100 | 42.7±9.9 | 36.2±8.4 | Participants asked to define binge eating in their own words and independent raters coded responses for presence/absence of binge features | 82% of participants included LOC in binge eating definition 43% of participants included eating a large amount of food binge eating definition |
|
| |||||||
|
Youth
| |||||||
| 12 | NTS: school-based | 259 | 41.7 | 14.7 | NR | Participants asked to define binge eating in their own words | 72.2% of participants defined binge eating exclusively in terms of quantity of food eaten 12.9% of participants defined binge eating in terms of quantity, duration, and LOC |
|
| |||||||
| 13 | NTS: community-based adolescent/mother dyads | 19 | 100 | 14.5±1.2 | NR | Focus groups with adolescents who reported LOC eating via phone screen | Few participants directly endorsed LOC or binge eating Binge eaters described as “lacking self control” LOC associated with eating sneakily, negative affective antecedents, short-term relief |
Abbreviations: BMI=body mass index (kg/m2); TS=treatment-seeking; NR=not reported; EDE=Eating Disorders Examination; OBE=objective binge eating; SBE=subjective binge eating; OO=objective overeating; SO=subjective overeating; LOC=loss of control; NTS=non-treatment seeking; BED=binge eating disorder
p≤.05
p<.01
p<.001
Convergent Validity
A total of 39 adult and 26 pediatric studies addressed the convergent validity of LOC and overeating; results are summarized in Table 3.
Table 3.
Summary of studies assessing the convergent validity of binge eating constructs
| Study | Sample | n | %F | Age | BMI | Measurement | Convergence with anthropometric, psychosocial, and behavioral measures | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Domain | Method | |||||||
|
Respondent-based
| ||||||||
|
Adults
| ||||||||
| 70 | NTS: obese with BED | 12 | 100 | 37.9±7.8 | 39.6±6.2 | Energy intake | Interview | OBE>SBE (t=2.71*) |
| % energy from carbohydrate | Interview | OBE>SBE (t=2.79*) | ||||||
| % energy from fat | Interview | OBE=SBE (t=2.20) | ||||||
| % energy from protein | Interview | OBE=SBE (t=0.38) | ||||||
|
| ||||||||
| 24 | TS: college students enrolled in weight gain prevention program | 294 | 100 | 18.2±0.4 | 23.7±2.9 | BMI | Measured | LOC frequency, r=−.03 |
| Total % body fat | Measured | LOC=no-LOC; LOC frequency, r=.04 | ||||||
|
| ||||||||
| 50 | TS: AN | 471 | 97.6 | 25.9±7.7 | NR | Eating-related psychopathology | Self-report | OBE=SBE (F=1.87) |
| TS: BN | 836 | Eating-related QOL | Self-report | OBE=SBE (F=3.42) | ||||
| TS: EDNOS | 845 | Negative affect | Self-report | OBE=SBE (F=0.00) | ||||
| TS: BED | 202 | Global functioning | Self-report | OBE=SBE (F=0.93) | ||||
| Negative self-image | Self-report | OBE=SBE (F=0.21) | ||||||
|
| ||||||||
| 25 | Mixed TS/NTS: BN | 144 | 100 | 25.7±8.8 | 22.9±5.2 | BMI | Self-report | OBE-only=SBE-only |
| Eating-related psychopathology | Self-report | OBE-only=SBE-only [F(1,66)=0.96] | ||||||
| Compensatory behaviors | Self-report | OBE-only=SBE-only [F(4,63)=0.90] | ||||||
| Mixed TS/NTS: subthreshold BN | 60 | Negative affect | Self-report | OBE-only=SBE-only [F(2,64)=2.25] | ||||
| Interpersonal problems | Self-report | OBE-only=SBE-only [F(2,65)=2.11] | ||||||
| Impulsivity | Self-report | SBE-only>OBE-only [F(3,64)=3.42*] | ||||||
|
| ||||||||
| 17 | TS: bariatric surgery | 180 | 78.3 | 44.8±11.2 | 44.5±6.8 | BMI | Self-report | BED>SBE>no-LOC* |
| Body image distress | Self-report | BED>SBE>no-LOC* | ||||||
| Eating-related distress | Self-report | BED>SBE>no-LOC* | ||||||
| Restraint | Self-report | BED=SBE=no-LOC | ||||||
| TS: weight loss support group | 93 | 91.4 | 55.1±12.4 | 32.7±7.3 | Disinhibition | Self-report | BED>SBE>no-LOC* | |
| Hunger | Self-report | BED>SBE>no-LOC* | ||||||
| Depression | Self-report | BED, SBE>no-LOC* | ||||||
| Mental QOL | Self-report | BED>SBE, no-LOC* | ||||||
| NTS: community-based | 158 | 78.5 | 41.3±13.5 | 24.8±5.1 | Physical QOL | Self-report | BED=SBE; SBE=no-LOC; BED>no-LOC* | |
| Energy intake | Self-report | BED>SBE>no-LOC* | ||||||
| Carbohydrates | Self-report | BED>SBE>no-LOC* | ||||||
| Fat | Self-report | BED>SBE, no-LOC* | ||||||
| Protein | Self-report | BED>SBE, no-LOC* | ||||||
|
| ||||||||
| 18 | TS: underweight eating disorders with OBE | 33 | 100 | 27.9±6.9 | 15.4±1.6 | BMI | Measured | OBE>SBE, no-LOC (F=8.14**) |
| Eating-related psychopathology | Interview | OBE, SBE>no-LOC (F=4.60*) | ||||||
| Depression | Self-report | OBE=SBE=no-LOC (F=1.07) | ||||||
| Anxiety | Self-report | OBE=SBE=no-LOC (F=1.14) | ||||||
| TS: underweight eating disorders with SBE | 36 | 25.8±10.5 | 14.0±1.3 | Novelty seeking | Self-report | OBE=SBE=no-LOC (F=2.85) | ||
| Harm avoidance | Self-report | OBE=SBE=no-LOC (F=0.50) | ||||||
| Reward dependence | Self-report | OBE=SBE=no-LOC (F=0.32) | ||||||
| Persistence | Self-report | OBE=SBE=no-LOC (F=1.95) | ||||||
| TS: underweight eating disorders with no LOC | 36 | 24.3±9.0 | 14.4±1.7 | Self-directedness | Self-report | OBE, SBE<no-LOC (F=6.33**) | ||
| Cooperativeness | Self-report | OBE=SBE=no-LOC (F=2.93) | ||||||
| Self-transecendence | Self-report | OBE=SBE=no-LOC (F=0.24) | ||||||
|
| ||||||||
| 32 | TS: diabetes | 274 | 65.0 | 52.5±12.1 | 33.9±6.9 | BMI | Measured | Correlated with binge eating (r=.27*) but not overeating |
|
| ||||||||
| 20 | NTS: community-based with LOC | 16 | 100 | 42.9±10.4 | 31.3±6.7 | BMI | NR | LOC=no-LOC (t=−1.70) |
| NTS: community-based without LOC | 16 | 41.0±14.6 | 28.5±5.6 | Eating-related psychopathology | Interview | LOC>no-LOC (t=−4.63***) | ||
|
| ||||||||
| 53 | Mixed TS/NTS: PD | 101 | 100 | 22.4±5.3 | 22.3±1.9 | Restraint | Self-report | LOC frequency, r=−.22 |
| Disinhibition | Self-report | LOC frequency, r=.35** | ||||||
| Hunger | Self-report | LOC frequency, r=.29** | ||||||
| Body image | Self-report | LOC frequency, r=.21* | ||||||
| Eating-related psychopathology | Interview | LOC frequency, r=.20* | ||||||
| Mood disorder | Interview | LOC frequency, r=.16 | ||||||
| Anxiety disorder | Interview | LOC frequency, r=.23* | ||||||
| Substance use disorder | Interview | LOC frequency, r=.27** | ||||||
| Impulse control disorder | Interview | LOC frequency, r=.32** | ||||||
| Depression | Self-report | LOC frequency, r=.32** | ||||||
| State anxiety | Self-report | LOC frequency, r=.17 | ||||||
| Trait anxiety | Self-report | LOC frequency, r=.15 | ||||||
| Impulsivity | Self-report | LOC frequency, r=.07 | ||||||
| Negative urgency | Self-report | LOC frequency, r=.44*** | ||||||
| Lack of premeditation | Self-report | LOC frequency, r=.25 | ||||||
| Lack of perseverence | Self-report | LOC frequency, r=−.06 | ||||||
| Sensation-seeking | Self-report | LOC frequency, r=.20 | ||||||
| Eating-related QOL | Self-report | LOC frequency, r=.39** | ||||||
| Global functioning | Interview | LOC frequency, r=−.34** | ||||||
|
| ||||||||
| 28 | NTS: community-based with OBE, SBE, and vomiting (1) | 30 | 100 | 24.3±5.4 | 22.7±2.3 | BMI | 1=2=3=4 (F=2.15) | |
| NTS: community-based with OBE (2) | 86 | 24.7±5.4 | 25.7±6.0 | Social functioning | 1, 2>4 (F=8.94***) | |||
| NTS: community-based with SBE (3) | 30 | 25.2±5.4 | 26.7±6.2 | Psychiatric distress | 1>4 (F=6.05***) | |||
| NTS: community-based with heterogeneous symptoms (4) | 102 | 24.6±5.7 | 25.1±5.3 | Self-esteem | 1<4 (F=6.86***) | |||
| Alcohol use | 1=2=3=4 (F=0.15) | |||||||
|
| ||||||||
| 19 | NTS: college students with OBE | 52 | 100 | 19.3±1.5 | 23.5±4.5 | BMI | Self-report | OBE>no pathology; OBE=SBE=OO; SBE=OO=no pathology [F(4,333)=9.2**] |
| NTS: college students with SBE | 40 | 19.1±0.8 | 22.1±3.6 | Eating-related psychopathology | Self-report | OBE, SBE>OO, no pathology [F(4,333)=49.7***] | ||
| NTS: college students with OO | 55 | 19.4±2.0 | 21.9±3.2 | Psychiatric distress | Self-report | OBE, SBE>OO, no pathology [F(4,332)=17.8***] | ||
| NTS: college students with no pathology | 145 | 19.3±2.3 | 21.7±3.2 | Eating-related QOL | Self-report | OBE, SBE>OO, no pathology [F(4,333)=48.3***] | ||
|
| ||||||||
| 51 | NTS: BN | 30 | 100 | 25.4±5.5 | NR | Restraint | Self-report | OBE=SBE [F(1,51)=2.0] |
| Cognitive restraint | Self-report | OBE=SBE [F(1,51)=0.3] | ||||||
| Disinhibition | Self-report | OBE=SBE [F(1,51)=2.5] | ||||||
| Hunger | Self-report | OBE=SBE [F(1,51)=1.7] | ||||||
| Eating-related psychopathology | Self-report | OBE>SBE [F(1,51)=11.1**] | ||||||
| Binge frequency | Self-report | OBE>SBE [F(1,51)=8.0**] | ||||||
| NTS: BN with SBE | 24 | 21.4±3.4 | NR | Purge frequency | Self-report | OBE>SBE [F(1,51)=8.3**] | ||
| Depression | Self-report | OBE=SBE [F(1,51)=0.6] | ||||||
| State anxiety | Self-report | OBE=SBE [F(1,51)=0.0] | ||||||
| Trait anxiety | Self-report | OBE=SBE [F(1,51)=0.0] | ||||||
| Alcohol use | Self-report | OBE=SBE [F(1,51)=3.4] | ||||||
| Drug use | Self-report | OBE=SBE [F(1,51)=1.8] | ||||||
| Impulsivity | Self-report | OBE>SBE [F(1,51)=7.8**] | ||||||
|
| ||||||||
| 54 | NTS: community-based with BED | 18 | 100 | 28.1±10.6 | 27.7±6.5 | Vomiting | Interview | OBE frequency, r=.42**; SBE frequency, r=.40** |
| Laxatives | Interview | OBE frequency, r=.22; SBE frequency, r=.05 | ||||||
| Diuretics | Interview | OBE frequency, r=.21**; SBE frequency, r=.51** | ||||||
| Driven exercise | Interview | OBE frequency, r=.23**; SBE frequency, r=.21** | ||||||
| Restraint | Interview | OBE frequency, r=.47**; SBE frequency, r=.41** | ||||||
| Eating concern | Interview | OBE frequency, r=.51**; SBE frequency, r=.44** | ||||||
| Weight concern | Interview | OBE frequency, r=.50**; SBE frequency, r=.39** | ||||||
| Shape concern | Interview | OBE frequency, r=.53**; SBE frequency, r=.40** | ||||||
| NTS: community-based with BN | 7 | Depression | Self-report | OBE frequency, r=.44**; SBE frequency, r=.33** | ||||
| Anxiety | Self-report | OBE frequency, r=.46**; SBE frequency, r=.36** | ||||||
| Stress | Self-report | OBE frequency, r=.53**; SBE frequency, r=.38** | ||||||
| Drive for thinness | Self-report | OBE frequency, r=.46**; SBE frequency, r=.44** | ||||||
| NTS: community-based with subthreshold BN and BED | 35 | Interospective awareness | Self-report | OBE frequency, r=.49**; SBE frequency, r=.30 | ||||
| Bulimia | Self-report | OBE frequency, r=.69**; SBE frequency, r=.32** | ||||||
| Body dissatisfaction | Self-report | OBE frequency, r=.33**; SBE frequency, r=.27 | ||||||
| Ineffectiveness | Self-report | OBE frequency, r=.46**; SBE frequency, r=.28 | ||||||
| Maturity fears | Self-report | OBE frequency, r=.15; SBE frequency, r=.30** | ||||||
| NTS: community-based with no eating pathology | 21 | Perfectionism | Self-report | OBE frequency, r=.15; SBE frequency, r=.08 | ||||
| Interpersonal distrust | Self-report | OBE frequency, r=.24; SBE frequency, r=.18 | ||||||
| Cognitive restraint | Self-report | OBE frequency, r=.12; SBE frequency, r=.28 | ||||||
| Disinhibition | Self-report | OBE frequency, r=.53**; SBE frequency, r=.26 | ||||||
| Hunger | Self-report | OBE frequency, r=.48**; SBE frequency, r=.23 | ||||||
|
| ||||||||
| 115 | TS: AN | 26 | 100 | 26.3±9.0 | 21.6±7.3 | Physical QOL | Self-report | Variance for OBE=NS; variance for SBE: β=.38* |
| TS: BN | 4 | |||||||
| TS: BED | 1 | Mental QOL | Self-report | Variance for OBE=NS; variance for SBE=NS | ||||
| TS: EDNOS | 10 | |||||||
| TS: undiagnosed | 12 | Depression | Self-report | Variance for OBE=NS; variance for SBE=NS | ||||
|
| ||||||||
| 63 | TS: BN | 21 | 100 | 27.0±9.9 | 21.5±2.9 | Energy intake | Interview | Degree of LOC, r=.57*** |
| Vomiting | Interview | Positively associated with LOC (estimate=.67; SE=.15***) and energy intake (estimate=.00; SE=.00***) | ||||||
| Hunger prior to eating | Interview | Positively associated with LOC (estimate=.14; SE=.05**) but not energy intake | ||||||
| Feeling compelled to start eating | Interview | Positively associated with LOC (estimate=.58; SE=.05***) but not energy intake | ||||||
| Feeling compelled to continue eating | Interview | Positively associated with LOC (estimate=.67; SE=.04***) but not energy intake | ||||||
| Feeling upset after eating | Interview | Positively associated with LOC (estimate=.56; SE=.04***) but not energy intake | ||||||
| Feeling full after eating | Interview | Positively associated with LOC (estimate=.15; SE=.05***) and energy intake (estimate=.00; SE=.00***) | ||||||
|
| ||||||||
| 29 | NTS: community-based with OBE | 37 | 100 | 29.4±6.4 | 29.0±7.8 | BMI | Self-report | OBE>SBE (t=2.25*) |
| Eating-related psychopathology | Self-report | OBE=SBE (t=0.08) | ||||||
| Physical QOL | Self-report | OBE=SBE (t=−1.00) | ||||||
| NTS: community-based with SBE | 52 | 28.6±6.5 | 25.7±5.2 | Mental QOL | Self-report | OBE=SBE (t=0.02) | ||
| Psychological distress | Self-report | OBE=SBE (t=−0.24) | ||||||
| Severe mental health impairment | Self-report | OBE=SBE (χ2=0.04) | ||||||
|
| ||||||||
| 26 | TS: BED | 101 | 100 | 45.7±11.0 | 37.9±7.1 | BMI | NR | OBE=SBE |
| Binge eating severity | Self-report | OBE=SBE | ||||||
| Depression | Self-report | OBE=SBE | ||||||
| Psychiatric distress | Self-report | OBE=SBE | ||||||
| Interpersonal problems | Self-report | OBE=SBE | ||||||
| Restraint | Self-report | OBE=SBE | ||||||
| Hunger | Self-report | OBE=SBE | ||||||
| Disinhibition | Self-report | OBE=SBE | ||||||
|
| ||||||||
| 30 | NTS: community-based with OBE | 154 | 100 | 26.2±7.0 | 27.4±7.2 | BMI | Self-report | OBE>SBE [F(2,311)=6.7***] |
| Driven exercise | Self-report | OBE=SBE=no-LOC (χ2=4.29) | ||||||
| NTS: community-based with SBE | 68 | 25.6±7.8 | 24.1±5.8 | Vomiting | Self-report | OBE=SBE=no-LOC (χ2=0.10) | ||
| Eating-related psychopathology | Self-report | OBE, SBE>no-LOC | ||||||
| NTS: community-based with no LOC | 108 | 25.4±7.6 | 25.4±5.4 | Physical QOL | Self-report | OBE=SBE=no-LOC | ||
| Mental QOL | Self-report | OBE=SBE=no-LOC | ||||||
| Negative affect | Self-report | OBE>no-LOC; OBE=SBE; SBE=no-LOC [F(2,321)=8.0***] | ||||||
|
| ||||||||
| 27 | TS: eating pathology with OBE | 56 | 95.0 | 36.3±10.9 | 37.1±3.7 | BMI | Measured | OBE=SBE |
| Binge eating severity | Self-report | OBE=SBE | ||||||
| TS: eating pathology with SBE | 14 | 93.0 | 39.5±11.7 | 37.8±4.5 | Depression | Self-report | OBE=SBE | |
| Psychiatric comorbidity | Interview | OBE=SBE | ||||||
|
| ||||||||
| 116 | TS: BN | 174 | 100 | 28.4±7.1 | 22.8±4.4 | BMI | NR | OBE+SBE, β=−0.07; OBE-SBE, β=0.08 |
| Weight concern | Interview | OBE+SBE, β=0.07; OBE-SBE, β=0.14 | ||||||
| Shape concern | Interview | OBE+SBE, β=0.18; OBE-SBE, β=0.05 | ||||||
| Restraint | Interview | OBE+SBE, β=−0.03; OBE-SBE, β=0.05 | ||||||
| Depression | Interview | OBE+SBE, β=0.29; OBE-SBE, β=0.02 | ||||||
| Self-esteem | Self-report | OBE+SBE, β=0.12; OBE-SBE, β=0.02 | ||||||
| Psychiatric distress | Self-report | OBE+SBE, β=0.19; OBE-SBE, β=−0.03 | ||||||
| Interpersonal problems | Self-report | OBE+SBE, β=0.16; OBE-SBE, β=0.03 | ||||||
| Social adjustment | Self-report | OBE+SBE, β=0.16; OBE-SBE, β=0.04 | ||||||
| Confidence to resist binge eating | Self-report | OBE+SBE, β=−0.18; OBE-SBE, β=−0.04 | ||||||
| Ability to resist binge eating | Self-report | OBE+SBE, β=−0.24**; OBE-SBE, β=0.20 | ||||||
|
| ||||||||
| 55 | TS: AN-binge/purge subtype | 70 | 97.1 | 29.5±10.6 | 16.3±1.7 | Eating-related psychopathology | Self-report | AN: OBE frequency, r=.21; SBE frequency, r=.12 BN: OBE frequency, r=.39**; SBE frequency, r=.18 |
| TS: BN | 110 | 98.2 | 30.3±8.0 | 23.0±6.7 | Emotional eating | Self-report | AN: OBE frequency, r=.12; SBE frequency, r=.75** BN: OBE frequency, r=.69**; SBE frequency, r=.02 |
|
|
| ||||||||
| 21 | TS: bariatric surgery with LOC | 123 | 79.0 | 43.8±10.9 | 50.5±9.2 | BMI | Measured | LOC=no-LOC (t=−1.50) |
| Eating-related psychopathology | Self-report | LOC>no-LOC (t=−7.26***) | ||||||
| Depression | Self-report | LOC>no-LOC (t=−5.42***) | ||||||
| TS: bariatric surgery without LOC | 103 | 48.9±7.0 | Physical QOL | Self-report | LOC=no-LOC (t=1.53) | |||
| Mental QOL | Self-report | LOC<no-LOC (t=3.63***) | ||||||
| Night eating | Self-report | LOC>no-LOC (t=−5.51***) | ||||||
| Alcohol use | Self-report | LOC=no-LOC (t=−1.10) | ||||||
|
| ||||||||
| 22 | NTS: community-based, obese BED | 53 | 62.3 | F:42.6±11.5 M:42.8±9.7 |
F:39.7±5.9 M:35.2±3.9 |
BMI | Self-report | BED=subBED=OO=no pathology |
| Current shape | Self-report | BED=subBED=OO=no pathology | ||||||
| NTS: community-based, obese subthreshold BED | 119 | 66.4 | F:43.2±11.8 M:47.9±13.2 |
F:38.6±5.9 M:37.2±6.5 |
Desired shape | Self-report | BED=subBED=OO=no pathology | |
| Current/ideal difference | Self-report | BED, subBED>OO, no pathology | ||||||
| Weight dissatisfaction | Self-report | BED, subBED>OO, no pathology | ||||||
| NTS: community-based, obese with OO | 60 | 35.0 | F:47.4±8.1 M:47.8±11.0 |
F:39.3±7.0 M:35.6±4.1 |
Weight importance | Self-report | BED>subBED>OO, no pathology | |
| NTS: community-based, obese with no pathology | 160 | 50.0 | F:44.1±10.4 M:50.8±10.5 |
F:37.9±5.4 M:35.0±4.3 |
Stress | Self-report | BED>OO, no pathology (F=3.18*) | |
| Sadness | Self-report | BED>subBED>OO, no pathology (F=8.68***) | ||||||
| Self-esteem | Self-report | BED<subBED, OO, no pathology; subBED<no pathology (F=7.68***) | ||||||
|
| ||||||||
| 52 | NTS: college students with LOC | 252 | 100 | 20.7±2.0 | NR | Eating-related QOL | Self-report | OBE-only=SBE-only (OR=1.00) |
| NTS: college students without LOC | 297 | Psychiatric comorbidity | Interview | OBE-only=SBE-only (OR=.61) | ||||
|
| ||||||||
| 31 | TS: BN | 112 | 98.0 | 25.0±9.0 | 21.1±2.5 | BMI | Measured | BN>BN with SBE |
| Eating-related psychopathology | Interview | BN=BN with SBE | ||||||
| Compensatory behaviors | Interview | BN=BN with SBE | ||||||
| Psychiatric comorbidity | Interview | BN=BN with SBE | ||||||
| Depression | Self-report | BN=BN with SBE | ||||||
| Anxiety | Self-report | BN=BN with SBE | ||||||
| TS: BN with SBE | 28 | 23.5±3.4 | Stress | Self-report | BN=BN with SBE | |||
| QOL | Self-report | BN=BN with SBE | ||||||
| Self-esteem | Self-report | BN=BN with SBE | ||||||
| Perfectionism | Self-report | BN=BN with SBE | ||||||
| Impulsivity | Self-report | BN=BN with SBE | ||||||
| Interpersonal problems | Self-report | BN=BN with SBE | ||||||
|
| ||||||||
| 23 | TS: bariatric surgery with LOC | 221 | 86.1 | 43.7±10.0 | 51.1±8.3 | BMI | Self-report | LOC=no-LOC(F=2.39) |
| Depression | Self-report | LOC>no-LOC (F=35.82***) | ||||||
| Mental QOL | Self-report | LOC<no-LOC (F=16.19***) | ||||||
| TS: bariatric surgery without LOC | 131 | Physical QOL | Self-report | LOC<no-LOC (F=8.02**) | ||||
| Eating-related psychopathology | Self-report | LOC>no-LOC (F=59.38***) | ||||||
|
| ||||||||
|
Youth
| ||||||||
| 33 | NTS: school-based with BED | 94 | 3.1 | Range=11–17 | F:24.1±4.8 M:27.4±7.9 |
Obesity status | Measured |
F: BED=subBED=OO=no pathology (χ2=4.62) M: BED, sub-BED, OO>no pathology (χ2=17.10***) |
| NTS: school-based with subthreshold BED | 243 | 7.9 | F:24.3±4.9 M:25.8±6.1 |
Body satisfaction | Self-report |
F: BED, subBED<OO<no pathology (F=66.94***) M: BED<OO, no pathology; BED=subBED; subBED=OO (F=17.75***) |
||
| NTS: school-based with OO | 255 | 6.3 | F:24.4±5.5 M:23.4±5.2 | Depression | Self-report |
F: BED, subBED>OO>no pathology (F=40.42***) M: BED, subBED, OO>no pathology (F=10.47***) |
||
| NTS: school-based with no pathology | 4142 | 1950 | F:23.0±4.9 M:23.0±4.7 | Self-esteem | Self-report |
F: BED, subBED>OO>no pathology (F=62.01***) M: BED, subBED, OO>no pathology (F=27.99***) |
||
| Suicidality | Self-report |
F: BED, subBED, OO>no pathology (χ2=111.72***) M: BED, subBED, OO>no pathology (χ2=36.62***) |
||||||
|
| ||||||||
| 34 | NTS: community-based with LOC | 62 | 64.5 | 12.9 ± 2.8 | 1.4±1.0 (z-score) | BMI | Measured | LOC>no-LOC*** |
| Depression | Self-report | LOC>no-LOC (t=−4.91***) | ||||||
| NTS: community-based without LOC | 157 | 43.9 | 13.2 ± 2.8 | 0.8±1.1 (z-score) | Anxiety | Self-report | LOC>no-LOC (t=−6.14***) | |
| Interpersonal problems | Parent-report | LOC>no-LOC (t=−3.73***) | ||||||
|
| ||||||||
| 58 | TS: BN with OBE | 27 | 97.5 | 16.1±1.6 | 22.1±3.0 | Compensatory behaviors | Interview | OBE=SBE [F(4,32)=1.79] |
| Eating pathology | Interview | OBE=SBE [F(1,35)=0.72] | ||||||
| TS: BN with SBE | 10 | Depression | Self-report | OBE<SBE [F(1,35)=6.14*] | ||||
| Self-esteem | Self-report | OBE=SBE [F(1,35)=0.02] | ||||||
|
| ||||||||
| 49 | TS: BN | 128 | 96.1 | 16.4±1.4 | 114.2±25.6 (%EBW) | %EBW | Measured | BN=PD-LOC=PD-noLOC>AN-B/P [F(3,241)=30.72***] |
| Restraint | Interview | BN=PD-LOC=PD-noLOC=AN-B/P [F(3,233)=1.95] | ||||||
| TS: AN-binge/purge | 38 | 97.4 | 15.6±1.8 | 78.2±4.8 (%EBW) | Shape concern | Interview | BN=PD-LOC=PD-noLOC=AN-B/P [F(3,233)=2.19] | |
| Weight concern | Interview | BN=PD-LOC=PD-noLOC=AN-B/P [F(3,233)=1.95] | ||||||
| TS: PD with LOC | 23 | 87.0 | 15.3±1.9 | 105.8±15.0 (%EBW) | Eating concern | Interview | BN>PD-noLOC, AN-B/P; BN=PD-LOC; PD-noLOC=PD-LOC=AN-B/P [F(3,233)=7.53***] | |
| Depression | Self-report | BN=PD-LOC=PD-noLOC=AN-B/P [F(3,233)=0.77; p=.51] | ||||||
| TS: PD without LOC | 56 | 91.1 | 16.2±1.4 | 106.3±13.5 (%EBW) | Self-esteem | Self-report | PD-LOC>BN, PD-noLOC, AN-B/P [F(3,209)=12.45***] | |
|
| ||||||||
| 46 | TS: overweight with BED | 26 | 76.9 | 14.8±0.9 | 1.9±0.4 (z-score) | BMI z-score | Measured | BED=subBED=OO=no pathology |
| TS: overweight with subthreshold BED | 13 | 69.2 | 15.1±0.9 | 1.9±0.6 (z-score) | Weight/shape concerns | Self-report | BED, sub BED>OO, no pathology [F(3,95)=9.17***] | |
| TS: overweight with OO | 18 | 50.0 | 15.4±1.1 | 1.8±0.6 (z-score) | Depression | Self-report | BED>OO, no-pathology; subBED=OO; subBED>no-pathology; OO=no-pathology [F(3,93)=7.39***] | |
| TS: overweight with no pathology | 39 | 76.9 | 15.2±1.1 | 1.8±0.5 (z-score) | ||||
|
| ||||||||
| 3 | NTS: school-based with OBE | 222 | 63.5 | 12–17 | NR | Overweight status | Measured |
F: OBE, OO>no pathology** M: OBE, OO>no pathology** |
| Risky weight control behavior | Self-report |
F: OBE>OO>no pathology* M: OBE, OO>no pathology* |
||||||
| Dieting | Self-report |
F: OBE, OO>no pathology* M: OBE, OO>no pathology* |
||||||
| NTS: school-based with OO | 165 | 61.2 | Body satisfaction | Self-report |
F: OBE, OO<no pathology* M: OBE<OO<no pathology* |
|||
| Cigarette use | Self-report |
F: OBE=OO=no pathology M: OO<OBE, no pathology* |
||||||
| Drug and alcohol use | Self-report |
F: OBE=OO=no pathology M: OBE=OO=no pathology |
||||||
| NTS: school-based with no pathology | 2374 | 51.8 | Self-injury | Self-report |
F: OBE>no pathology; OO>no pathology; OBE=OO* M: OBE, OO>no pathology* |
|||
| Depression | Self-report |
F: OBE>OO>no pathology* M: OBE>OO>no pathology* |
||||||
| Self-esteem | Self-report |
F: OBE<OO<no pathology* M: OBE, OO<no pathology* |
||||||
|
| ||||||||
| 48 | TS: overweight with LOC | 35 | 71.4 | 12.9±1.9 | 179.1±25.4 (adjusted) | Adjusted BMI | NR | LOC=no-LOC [F(1,194)=3.45] |
| Eating-related psychopathology | Interview | OBE>no-LOC; OBE=SBE; SBE=no-LOC [F(8,364)=3.08**] | ||||||
| External eating | Self-report | OBE>no-LOC; OBE=SBE; SBE=no-LOC [F(2,161)=4.36*] | ||||||
| TS: overweight without LOC | 161 | 59.0 | 12.7±1.7 | 169.9±26.8 (adjusted) | Restraint | Self-report | OBE=SBE=no-LOC [F(2,161)=1.23] | |
| Emotional eating | Self-report | OBE>SBE, no-LOC [F(2,161)=14.99***] | ||||||
| Depression | Self-report | OBE>no-LOC; OBE=SBE; SBE=no-LOC [F(2,163)=8.82***] | ||||||
|
| ||||||||
| 35 | NTS: school-based with LOC | 108 | 69.4 | 13.8±0.9 | 19.0±3.2 | BMI | Self-report | LOC>no-LOC (F=2.01) |
| Restraint | Self-report | OBE, SBE>no-LOC (F=19.62***) | ||||||
| Eating concern | Self-report | OBE, SBE>no-LOC (F=30.91***) | ||||||
| Weight concern | Self-report | OBE, SBE>no-LOC (F=17.56***) | ||||||
| Shape concern | Self-report | OBE, SBE>no-LOC (F=19.28***) | ||||||
| NTS: school-based without LOC | 538 | 55.8 | 13.9±0.9 | 18.6±2.5 | Drive for thinness | Self-report | OBE, SBE>no-LOC (F=14.07***) | |
| Bulimia | Self-report | OBE, SBE>no-LOC (F=24.24***) | ||||||
| Body dissatisfaction | Self-report | OBE>no-LOC; OBE=SBE; SBE=no-LOC (F=7.57***) | ||||||
| Depression | Self-report | OBE>SBE>no-LOC (F=4.03***) | ||||||
| Self-esteem | Self-report | OBE>no-LOC; OBE=SBE; SBE=no-LOC (F=6.34**) | ||||||
|
| ||||||||
| 57 | NTS: community-based with LOC | 60 | 56.7 | 10.7±1.5 | 23.0±5.0 | Eating-related psychopathology | Interview | LOC>no-LOC** |
| Empathy | Self-report | LOC=no-LOC [F(1,59)=0.08] | ||||||
| Risk-taking | Self-report | LOC=no-LOC [F(1,59)=1.40] | ||||||
| Impulsivity | Self-report | LOC>no-LOC [F(1,59)=8.72**] | ||||||
| Novelty-seeking | Parent-report | LOC=no-LOC [F(1,59)=3.20] | ||||||
| NTS: community-based without LOC | 60 | Harm avoidance | Parent-report | LOC=no-LOC [F(1,59)=1.74] | ||||
| Reward dependence | Parent-report | LOC=no-LOC [F(1,59)=1.12] | ||||||
| Persistence | Parent-report | LOC=no-LOC [F(1,59)=2.59] | ||||||
| Self-directedness | Parent-report | LOC<no-LOC [F(1,59)=5.92*] | ||||||
| Cooperativeness | Parent-report | LOC<no-LOC [F(1,59)=5.88*] | ||||||
| Self-transcendence | Parent-report | LOC=no-LOC [F(1,59)=0.22] | ||||||
|
| ||||||||
| 56 | TS: overweight with LOC | 4 | 44.0 | 10.1±1.6 | 33.5±4.5 | Restraint | Interview | LOC=no-LOC |
| Eating concern | Interview | LOC>no-LOC*** | ||||||
| TS: overweight without LOC | 23 | Weight concern | Interview | LOC>no-LOC** | ||||
| Shape concern | Interview | LOC=no-LOC | ||||||
|
| ||||||||
| 36 | NTS: community-based, obese with LOC | 37 | 22.0 | 8.3±1.5 | 27.9±4.2 | BMI | Measured | LOC>no-LOC (F=14.5***) |
| Eating-related psychopathology | Self-report | LOC>no-LOC (F=7.8**) | ||||||
| Body dissatisfaction | Self-report | LOC>no-LOC (F=4.0*) | ||||||
| NTS: community-based, obese without LOC | 75 | 38.0 | 8.7±1.4 | 24.6±4.2 | Anxiety | Self-report | LOC>no-LOC (F=9.9**) | |
| Depression | Self-report | LOC>no-LOC (F=10.0**) | ||||||
| Behavioral problems | Parent-report | LOC=no-LOC (F=0.7) | ||||||
|
| ||||||||
| 37 | Mixed TS/NTS: overweight with OBE | 70 | 90.0 | 15.2±1.5 | 27.7±6.5 | BMI | Measured | LOC>no-LOC (t=2.05*); OBE=SBE (t=0.54) |
| Systolic blood pressure | Measured | LOC>no-LOC (F=10.36**); OBE=SBE (F=1.27) | ||||||
| Diastolic blood pressure | Measured | LOC=no-LOC (F=0.75); OBE=SBE (F=1.96) | ||||||
| Mixed TS/NTS: overweight with SBE | 80 | 98.0 | 14.5±1.7 | 28.2±4.2 | Waist circumference | Measured | LOC=no-LOC (F=0.98); OBE=SBE (F=0.17) | |
| Triglycerides | Measured | LOC=no-LOC (F=0.03); OBE=SBE (F=1.60) | ||||||
| HDL-cholesterol | Measured | LOC=no-LOC (F=2.76); OBE>SBE (F=4.03*) | ||||||
| Mixed TS/NTS: overweight with no LOC | 179 | 82.0 | 14.8±1.5 | 26.2±7.9 | LDL-cholesterol | Measured | LOC>no-LOC (F=9.90**); OBE>SBE (F=6.30**) | |
| Plasma glucose | Measured | LOC=no-LOC (F=0.14); OBE=SBE (F=0.83) | ||||||
| Metabolic syndrome | Measured | LOC=no-LOC (χ2=0.00); OBE=SBE (χ2=1.85) | ||||||
|
| ||||||||
| 45 | NTS: community-based with recurrent LOC | 1643 | 84.0 | 14.9±2.7 | 22.1±3.6 | BMI | Measured | Recurrent LOC>non-recurrent LOC>no-LOC [F(2,1587)=34.73***] |
| NTS: community-based with non-recurrent LOC | 156 | 80.1 | 14.8±2.6 | 21.1±3.7 | Eating-related psychopathology | Self-report | Recurrent LOC>non-recurrent LOC>no-LOC [F(2,1640)=240.69***] | |
| NTS: community-based with no LOC | 226 | 56.5 | 15.1±2.8 | 20.0±3.1 | Eating-related QOL | Self-report | Recurrent LOC>non-recurrent LOC>no-LOC [F(2,1640)=264.59***] | |
|
| ||||||||
| 38 | NTS: community-based with OBE | 46 | 60.9 | 12.6±.4 | 1.4±.2 (z-score) | BMI z-score | Measured | OBE, SBE>OO, no pathology (F=5.04**) |
| NTS: community-based with SBE | 42 | 61.9 | 13.4±.4 | 1.4±.2 (z-score) | Eating-related psychopathology | Interview | OBE, SBE>OO, no pathology (F=21.79***) | |
| NTS: community-based with OO | 68 | 50.0 | 13.0±.4 | 1.0±.1 (z-score) | Depression | Self-report | OBE, SBE>OO, no pathology (F=5.83**) | |
| NTS: community-based with no pathology | 211 | 41.7 | 12.5±.2 | .8±.1 (z-score) | Anxiety | Self-report | OBE, SBE>OO, no pathology (F=7.13***) | |
|
| ||||||||
| 39 | Mixed: TS overweight and NTS community-based with OBE | 106 | 60.2 | 13.1±2.6 | Range of means= 1.3±1.2 to 2.4±0.3 (z-score) | BMI z-score | Measured | OBE, SBE>no pathology; OBE>OO SBE=OO [F(3,427)=4.8**] |
| Meal type of episode | Interview | OBE, SBE>OO, normal episode for snack vs. meal [χ2(N=442)=40.3**] | ||||||
| Overeaten/eaten forbidden food before eating episode | Interview | OBE, SBE>OO, normal episode [χ2(N=444)=27.4**] | ||||||
| Negative emotion before episode | Interview | OBE, SBE>OO, normal episode [χ2(N=445)=38.6**] | ||||||
| Mixed: TS overweight and NTS community-based with SBE | 67 | Restricting before episode | Interview | OBE=SBE=OO=normal episode [χ2(N=445)=2.6] | ||||
| Emotional before episode | Interview | OBE=SBE=OO=normal episode [χ2(N=445)=6.6] | ||||||
| Hungry before episode | Interview | OBE=SBE=OO=normal episode [χ2(N=445)=6.3] | ||||||
| Eating despite lack of hunger before episode | Interview | OBE, SBE>OO, normal episode [χ2(N=440)=70.0**] | ||||||
| Tired before episode | Interview | OBE, SBE, OO>normal episode [χ2(N=445)=8.2*] | ||||||
| Mixed: TS overweight and NTS community-based with OO | 106 | With whom during episode | Interview | OBE, SBE>OO, normal episode for eating alone [χ2(N=441)=20.8**] | ||||
| Time of day during episode | Interview | [χ2(N=443)=15.4] | ||||||
| Celebration during episode | Interview | [χ2(N=443)=4.0] | ||||||
| Secretive during episode | Interview | OBE, SBE>OO, normal episode [χ2(N=444)=38.6**] | ||||||
| Numbing out during episode | Interview | OBE, SBE>OO, normal episode [χ2(N=445)=46.7**] | ||||||
| Mixed: TS overweight and NTS community-based with no pathology | 166 | Hiding food during episode | Interview | OBE>SBE, OO, normal episode [χ2(N=442)=18.4**] | ||||
| Eating quickly during episode | Interview | OBE>SBE, OO, normal episode [χ2(N=444)=43.1**] | ||||||
| Eating more than others during episode | Interview | OBE>SBE, OO, normal episode [χ2(N=441)=57.8**] | ||||||
| Location during episode | Interview | SBE>OBE, OO, normal episode for watching television [χ2(N=439)=32.5**] | ||||||
| Negative emotion after eating | Interview | OBE, SBE>OO, normal episode [χ2(N=445)=53.5**] | ||||||
| Guilt/shame after eating | Interview | OBE, SBE>OO, normal episode [χ2(N=445)=46.2**] | ||||||
| Full after eating | Interview | OBE=SBE=OO=normal episode [χ2(N=445)=5.2] | ||||||
| Sick after eating | Interview | OBE>SBE, OO, normal episode [χ2(N=445)=11.6**] | ||||||
|
| ||||||||
| 41 | NTS: community-based with LOC | 18 | 44.4 | 13.1±2.7 | 1.6±0.9 (z-score) | BMI z-score | Measured | LOC>no-LOC* |
| Eating in response to depression | Self-report | LOC>no-LOC (F=13.2***) | ||||||
| NTS: community-based without LOC | 137 | 54.0 | 14.4±2.3 | 1.0±1.1 (z-score) | Eating in response to anger/anxiety/frustration | Self-report | LOC>no-LOC (F=5.4*) | |
| Eating in response to feeling unsettled | Self-report | LOC>no-LOC (F=12.4**) | ||||||
|
| ||||||||
| 44 | NTS: community-based with LOC | 15 | 86.7 | 10.0±1.8 | 28.2±8.1 | BMI | Measured | OBE+SBE>OO, no pathology [F(2,158)=3.6*] |
| Eating-related psychopathology | Interview | OBE+SBE>OO, no pathology [F(2,158)=7.8**] | ||||||
| NTS: community-based with OO | 33 | 23.8±8.6 | Depression | Self-report | OBE+SBE=OO=no pathology [F(2,150)=0.19] | |||
| Anxiety | Self-report | OBE+SBE=OO=no pathology [F(2,149)=0.24] | ||||||
| NTS: community-based with no pathology | 114 | 21.9±8.0 | Behavioral problems | Parent-report | OBE+SBE=OO=no pathology [F(2,148)=1.2] | |||
|
| ||||||||
| 42 | Mixed TS/NTS: community-based with LOC | 81 | 63.0 | 12.0±2.7 | 2.0±0.8 (z-score) | BMI z-score | Measured | LOC>no-LOC* |
| Energy intake | Interview | LOC=no-LOC | ||||||
| % energy from carbohydrate | Interview | LOC>no-LOC*; OBE=SBE | ||||||
| Mixed TS/NTS: community-based without LOC | 168 | 51.0 | 12.2±2.6 | 1.6±1.1 (z-score) | % energy from protein | Interview | LOC<no-LOC**; OBE, SBE<OO, no pathology | |
| % energy from fat | Interview | LOC=no-LOC; OBE=SBE | ||||||
|
| ||||||||
| 43 | TS: diabetic with BED | 42 | 69.0 | 14.0 | 2.4±0.4 (z-score) | BMI z-score | Measured | BED>OO>no pathology** |
| TS: diabetic with subthreshold BED | 135 | 67.4 | 2.3±0.5 | Eating-related psychopathology | Self-report | BED>OO, no pathology** | ||
| TS: diabetic with OO | 164 | 62.2 | 2.2±0.5 | Depression | Self-report | BED>OO, no pathology** | ||
| TS: diabetic with no pathology | 337 | 65.3 | 2.2±0.5 | QOL | Self-report | BED>OO>no pathology** | ||
|
| ||||||||
|
Ecological momentary assessment
| ||||||||
|
Adults
| ||||||||
| 59,65,117 | NTS: community-based obese with BED | 5 | 84.0 | 43.0±11.9 | 40.3±8.5 | Pre-episode negative affect | Self-report | Increased prior to OBE* but not SBE or OO65 OBE and OO more likely on days characterized by high or increasing negative affect Likelihood of SBE did not differ by affect trajectory117 OBE>SBE, OO, normal episode; SBE>normal episode; SBE=OO; OO=normal episode (Wald χ2=15.67**)59 |
| Post-episode negative affect | Self-report | Decreased after OBE* but not SBE or OO65 OBE>SBE, OO, normal episode; SBE>normal episode; SBE=OO; OO=normal episode (Wald χ2=24.39***)59 |
||||||
| Pre-episode hunger | Self-report | OBE<SBE, normal episode; OBE=OO; SBE=OO, normal episode (Wald χ2=18.14***)59 | ||||||
| Post-episode hunger | Self-report | OBE, OO<SBE, normal episode (Wald χ2=39.75***)59 | ||||||
| NTS: community-based obese without BED | 45 | Pre-episode cravings | Self-report | OBE=SBE=OO=normal episode (Wald χ2=8.14)59 | ||||
| Post-episode cravings | Self-report | OBE<SBE; OBE>OO; OBE=normal episode; SBE>OO; SBE=normal episode; OO<normal episode (Wald χ2=25.87***)59 | ||||||
| Location | Self-report | OBE=SBE=OO=normal episode (Wald χ2=1.22)59 | ||||||
| Eating alone | Self-report | SBE>OBE, OO; SBE=normal eating; normal eating=OBE, OO (Wald χ2=13.2**)59 | ||||||
| Eating while watching television | Self-report | OBE=SBE=OO=normal episode (Wald χ2=0.92)59 | ||||||
| Pre-episode eating because others are eating | Self-report | OBE=SBE=OO=normal episode (Wald χ2=2.07)59 OBE=SBE=OO=normal episode | ||||||
| Post-episode eating because others are eating | Self-report | OBE=SBE=OO=normal episode (Wald χ2=5.37)59 | ||||||
| Pre-episode alcohol ingestion | Self-report | OBE=SBE=OO=normal episode (Wald χ2=10.55)59 | ||||||
| Post-episode stressful event | Self-report | OBE=SBE=OO=normal episode (Wald χ2=2.81)59 | ||||||
|
| ||||||||
| 61,62 | NTS: community-based obese with BED | 9 | 86.4 | 35.7±11.9 | 38.9±8.7 | Pre-episode negative affect | Self-report | Positively associated with LOC [t(1,427)=4.61***]61 Not associated with energy intake [t(1,427)=0.82]61 |
| Post-episode negative affect | Self-report | No main effect for LOC [t(1,427)=1.68]61 No main effect for energy intake [t(1,427)=−1.46]61 Positively associated with energy intake in non-BED [t(1,427)=−2.86**] but not BED61 Positively associated with LOC in BED, irrespective of energy intake, and negatively associated with LOC and energy intake in non-BED [t(1,427)=−2.28*]61 |
||||||
| NTS: community-based without BED | 13 | Post-meal LOC while eating | Self-report | Positively associated with BED status (OR=3.60; SE=0.29***), energy intake (OR=1.00; SE=0.00***), and negative affect (OR=1.16; SE=0.04***) | ||||
|
| ||||||||
| 60 | NTS: AN | 118 | 100 | 25.3±8.4 | 17.2±1.0 | Negative affect | Self-report | OBE,SBE>avoidant eating, restrictive eating>solitary eating (Wald χ2=88.47***) |
| Compensatory behaviors | Self-report | OBE>SBE avoidant eating, restrictive eating; SBE>solitary eating (Wald χ2=87.45***) | ||||||
| Body checking | Self-report | Solitary eating>OBE, avoidant eating>restrictive eating; SBE=binge eating (Wald χ2=29.00***) | ||||||
| Self-weighing | Self-report | OBE=SBE=avoidant eating=restrictive eating=solitary eating (Wald χ2=4.17) | ||||||
| Stress | Self-report | Restrictive eating>OBE, SBE (Wald χ2=65.86***) | ||||||
|
| ||||||||
|
Youth
| ||||||||
| 67 | NTS: community-based with LOC | 59 | 55.9 | 10.8±1.5 | 23.0±5.1 | Energy intake | Interview | LOC>no-LOC across meal types [F(1,106)=4.39*]; binge meal in LOC>normal meal in no-LOC [F(1,157)=4.41*] |
| Carbohydrate | Interview | Binge meal>normal meal in LOC [F(1,366)=6.99**]; binge meal in LOC>normal meal in no-LOC [F(1,150)=9.65**] | ||||||
| Fat | Interview | LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
| Protein | Interview | LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
| Happy | Interview | Binge meals, regular meals<random signal in LOC [F(2,875)=24.98***]; LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
| Sad | Interview | Binge days in LOC>non-binge days in no-LOC [F(1,71)=6.29**]; LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
| NTS: community-based without LOC | 59 | Afraid | Interview | LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||
| Upset | Interview | LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
| Food/eating-related cognitions | Interview | LOC>no-LOC across meal types [F(1,110)=16.62***]; binge meal, normal meal>random signal in LOC [F(2,892)=43.32***]; binge meal in LOC>normal meal in no-LOC [F(1,113)=16.55***] | ||||||
| Body-related cognitions | Interview | LOC>no-LOC across meal types [F(1,116)=10.14**]; binge meal, normal meal>random signal in LOC [F(2,872)=9.22***]; binge meal in LOC>normal meal in no-LOC [F(1,96)=52.73***] | ||||||
| Hunger | Interview | LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
| Satiety | Interview | LOC=no-LOC across meal types; binge meal=normal meal across groups | ||||||
|
| ||||||||
| 68 | NTS: community-based overweight with LOC | 30 | 100 | 14.9±1.5 | 36.1±7.5 | Interpersonal problems | Self-report | Predictive of LOC eating at between (estimate=0.31; SE=0.14*) and within-subjects level (estimate=0.14; SE=0.07*) |
| Negative affect | Self-report | Not predictive of LOC eating at between- (estimate=1.21; SE=0.76) or within-subjects level (estimate=0.33; SE=0.34) | ||||||
|
| ||||||||
| 69 | NTS: community-based overweight with LOC | 17 | 100 | 14.8±1.6 | 2.2±0.5 (z-score) | Heartrate | Measured | Positively associated with LOC at within- (estimate=0.02; SE=0.00***), but not between-subjects level |
| Heartrate variability | Measured | Negatively associated with LOC at within- (estimate=−0.01; SE=0.00***), but not between-subjects level | ||||||
|
| ||||||||
|
Feeding laboratory
| ||||||||
|
Adults
| ||||||||
| 71 | NTS: more obese with BED | 12 | 100 | 31.7±1.3 | 41.5±0.9 | Energy intake | Measured |
BED: Binge meal>normal meal [t(1,37)=2.45*] Non-BED: binge meal=normal mean |
| NTS: more obese without BED | 6 | 35.0±2.8 | 40.4±0.5 | % energy from protein | Measured | Binge meal=normal meal across groups | ||
| NTS: less obese with BED | 9 | 33.7±2.2 | 31.1±0.5 | % energy from carbohydrate | Measured | Binge meal=normal meal across groups | ||
| NTS: less obese without BED | 8 | 32.5±1.8 | 30.4±0.5 | % energy from fat | Measured | Binge meal=normal meal across groups | ||
| NTS: normal-weight with no pathology | 7 | 31.1±3.4 | 21.0±0.7 | Satiety | Self-report |
BED: Binge meal>normal meal [t(1,37)=2.45*] Non-BED: binge meal=normal meal for obese |
||
|
| ||||||||
| 72 | TS: BN | 11 | 100 | 24.2±2.2 | −1.5±12.4 (%deviation from EBW) | Energy intake | Measured | Binge meal>normal meal across groups [F(1,19)=27.20***] |
| NTS: No pathology | 10 | 23.9±4.3 | 0.8±10.3 (%deviation from EBW) | Rate of energy intake | Measured | Binge meal>normal meal across groups [F(1,19)=13.23**] | ||
|
| ||||||||
| 73 | TS: BN | 8 | 100 | 23.0±3.5 | 95.1±12.1 (%EBW) | Energy intake | Measured | Mean binge meal>Mean normal meal for multi-course and single item meals (no statistical tests reported) |
|
| ||||||||
| 74 | TS: BN | 8 | 100 | 24.6±5.0 | 19.5±1.8 | Energy intake | Measured |
BN: binge meal>normal meal [t(14)=4.24***] College students: Binge meal=normal meal |
| Rate of eating | Measured |
BN: binge meal>normal meal for multi-item [t(14)=3.63*] but not single-item meal [t(14)=1.26] College students: binge meal=normal meal |
||||||
| NTS: college students | 8 | 25.3±8.0 | 20.2±1.2 | Pre-episode satiety | Self-report | Binge meal=normal meal across groups [F(1,14)=0.71] | ||
| Post-episode satiety | Self-report | Binge meal=normal meal across groups [F(1,14)=2.82] | ||||||
| Control over eating | Self-report | Binge meal<normal mea across groupsl [F(1,14)=9.38**] | ||||||
|
| ||||||||
| 64 | NTS: community-based with BED | 30 | 100 | 43.8±8.7 | 34.6±6.1 | Energy intake | Measured | Degree of control, r=−.56** |
| NTS: community-based without BED | 30 | 44.7±10.4 | 32.2±6.3 | Depressed mood | Self-report | Self-labeled OBE>self-labeled OO (t=2.51*) Degree of control, r=−.26* |
||
| Anxious mood | Self-report | Self-labeled OBE=self-labeled OO (t=1.95) Degree of control, r=−.21* |
||||||
|
| ||||||||
| 75 | TS: BN | 12 | 100 | 24.1±2.9 | 1.6±11.9 (%deviation from EBW) | Energy intake | Measured |
Multi-item meal: binge meal>multi-item normal meal*; degree of contol, r=.58** for normal meal and r=.61** for binge meal in BN; degree of control, r=NS for normal meal and binge meal in no pathology group Single-item meal: degree of contol, r=.17 for normal meal and r=.63** for binge meal in BN; degree of control, r=.02 for normal meal and r=.00 binge meal in no pathology group |
| NTS: no pathology | 10 | 23.9±4.3 | 0.8±10.3 (%deviation from EBW) | % energy from carbohydrate | Measured | Multi-item binge meal=multi-item normal meal across groups | ||
| % energy from protein | Measured | Multi-item binge meal<multi-item normal meal across groups* | ||||||
| % energy from fat | Measured | Multi-item binge meal=multi-item normal meal across groups | ||||||
|
| ||||||||
| 76 | NTS: obese with BED | 10 | 100 | 36.2±2.6 | 40.1±3.4 | Energy intake | Measured | Binge meal>normal meal in BED* but not non-BED |
| % energy from protein | Measured | Binge meal=normal meal across groups | ||||||
| NTS: obese without BED | 9 | 39.0±2.9 | 38.8±1.4 | % energy from carbohydrate | Measured | Binge meal=normal meal across groups | ||
| % energy from fat | Measured | Binge meal=normal meal across groups | ||||||
| LOC while eating | Self-report | Binge meal=normal meal across groups | ||||||
|
| ||||||||
|
Youth
| ||||||||
| 77 | NTS: community-based with LOC | 60 | 56.7 | 10.8±1.5 | 23.0±5.0 | Energy intake | Measured |
Parent-child test meal: LOC=no-LOC Child-only snack: LOC>no-LOC* |
| Total protein | Measured |
Parent-child test meal: LOC=no LOC Child-only snack: LOC>no-LOC* |
||||||
| Total carbohydrate | Measured |
Parent-child test meal: LOC=no LOC Child-only snack: LOC=no LOC |
||||||
| NTS: community-based without LOC | 60 | Total fat | Measured |
Parent-child test meal: LOC=no LOC Child-only snack: LOC>no-LOC* |
||||
| LOC while eating | Self-report |
Parent-child test meal: LOC=no-LOC Child-only snack: LOC>no-LOC* |
||||||
|
| ||||||||
| 47 | NTS: overweight with LOC | 22 | 100 | 10.6±1.8 | 2.3±0.4 (z-score) | BMI z-score | Measured | LOC=no-LOC |
| Energy intake | Measured | LOC=no-LOC | ||||||
| NTS: overweight without LOC | 22 | 10.3±2.0 | 2.1±0.4 (z-score) | LOC while eating | Self-report | Predicted by negative affect prior to mood induction in LOC group [α2 (N=22)=7.08*] | ||
|
| ||||||||
| 66 | NTS:community-based with LOC | 110 | 100 | 14.5±1.7 | 1.5±0.3 (z-score) | Pre-episode negative affect | Measured | Energy intake, β=NS |
| Post-episode negative affect | Measured | Energy intake, β=NS | ||||||
|
| ||||||||
| 40 | NTS: community-based with LOC | 50 | 64.0 | 13.3±2.7 | 27.7±9.9 | BMI | Measured | LOC>no-LOC** |
| Energy intake | Measured | Binge meal>normal meal across groups (estimate=−0.04; SE=0.02**); LOC=no-LOC (estimate=0.00; SE=0.03) | ||||||
| % energy from protein | Measured | LOC<no-LOC across binge and normal meals** | ||||||
| % energy from carbohydrate | Measured | LOC>no-LOC across binge and normal meals* | ||||||
| % energy from fat | Measured | Binge meal=normal meal; LOC=no-LOC | ||||||
| Post-episode anxiety | Self-report | Binge meal=normal meal; positively associated with LOC status* | ||||||
| NTS: community-based without LOC | 127 | 41.7 | 13.6±2.8 | 23.4±7.3 | Post-episode anger | Self-report | Binge meal=normal meal across groups | |
| Post-episode confusion | Self-report | Binge meal=normal meal; positively associated with LOC status* | ||||||
| Post-episode depression | Self-report | Binge meal=normal meal across groups | ||||||
| Post-episode fatigue | Self-report | Binge meal=normal meal across groups | ||||||
| Post-episode tension | Self-report | Binge meal=normal meal across groups | ||||||
| Post-episode vigor | Self-report | Binge meal=normal meal across groups | ||||||
Note: Studies using identical samples are grouped together for ease of reading. Age and BMI reported as means unless otherwise stated. Only comparisons involving binge eating constructs are reported.
Abbreviations: F=female; BMI=body mass index (kg/m2); NTS=non-treatment-seeking; BED=binge eating disorder; OBE=objective binge eating; SBE=subjective binge eating; TS=treatment-seeking; LOC=loss of control; QOL=quality of life; AN=anorexia nervosa; BN=bulimia nervosa; EDNOS=eating disorder not otherwise specified; NR=not reported; PD=purging disorder; OO=objective overeating; NS=not significant; SE=standard error; M=male
p≤.05
p<.01
p<.001
Anthropometric factors
A total of 17 adult and 16 pediatric studies reported on anthropometric characteristics in relation to LOC and/or overeating.
Adults
Of seven adult studies involving controls with no eating pathology, three reported that those with LOC and/or overeating had elevated BMIs relative to those with no LOC or overeating pathology.17–19 However, in two of these studies, BMI differences were found only for those with OBE and not those with SBE.18,19 By contrast, four studies found that BMI did not differ in individuals with LOC and/or overeating compared to those with no LOC or overeating pathology.20–23 One adult study reported elevated %trunk fat, but not total %body fat or %abdominal fat, in those with LOC relative to those without LOC.24 Of 11 adult studies directly comparing those with different forms of LOC and/or overeating, 6 found that OBE, SBE, and/or OO did not differ on BMI,19,22,25–28 while 5 found that BMI was higher in those with OBE relative to those with SBE.17,18,29–31 One adult study reported that BMI was correlated with OBE but not OO frequency,32 while another reported no associations between LOC eating frequency and any anthropometric variables.24
Youth
Of 16 pediatric studies involving controls with no LOC or overeating pathology, 13 found that indices of cardiovascular risk, including BMI and overweight status, were elevated in youth with OBE and/or SBE relative to healthy controls.3,33–45 Of note, in one of these studies, differences in weight status held only for males and not females.33 By contrast, three studies reported no differences in those with OBE, SBE, and/or OO relative to those with no LOC.46–48 Seven pediatric studies reported that individuals with OBE did not differ from those with OO3,33,46 or those with SBE37–39,49 on BMI. Four studies that compared those with OBE and/or SBE to those with OO reported higher BMI in the former than the latter,38,39,43,44 with the exception that Tanofsky-Kraff and colleauges39 reported that youth reporting SBE were similar to those reporting OO on BMI. No pediatric studies reported BMI differences between those with OBE and those with SBE. Finally, 5 pediatric studies reported that youth with OO did not differ from controls on BMI,38,39,44,46 while 3 reported that those with OO had higher BMIs/rates of overweight or obesity than controls (although again, in one study,33 these results pertained only to males).3,33,43
Psychosocial factors
A total of 21 adult and 15 pediatric studies reported on cross-sectional associations between binge eating constructs and psychosocial factors, including eating-related and general psychopathology, quality of life, personality, and interpersonal functioning.
Adults
Of the 21 adult studies, 8 included a control group with no LOC or overeating pathology. All 8 of these studies reported more severe impairment among those with OBE and/or SBE relative to those with no LOC or overeating on at least one index of psychosocial functioning.17–23,30 Of 13 adult studies directly comparing individuals with different forms of LOC and/or overeating, 12 found that those with OBE endorsed similar levels of psychosocial impairment as compared to those with SBE across most measures,18,19,25–31,50–52 while 1 reported greater impairment in those with OBE relative to those with SBE.17 However, the OBE group in this latter study was comprised of individuals with BED; thus, it is unclear whether psychosocial differences were attributable to episode size, frequency, or other diagnostic features of BED. Of only two adult studies reporting on psychosocial functioning in individuals with OO, both found that these individuals endorsed lower impairment than those with LOC, and comparable impairment as compared to those with no eating pathology, on most measures of distress.19,22 Generally, correlations between OBE and SBE frequency and measures of psychosocial impairment were in the moderate to large range.53–55
Youth
Of the 15 pediatric studies, 13 included a control group with no LOC or overeating pathology. Of these, all 13 studies reported more severe impairment among those with OBE and/or SBE relative to those with no LOC or overeating on at least one index of psychosocial functioning.3,33–36,38,43–46,48,56,57 There tended to be fewer differences between youth with LOC and controls with no LOC or overeating pathology on measures of dietary restraint48,56 and personality.57 All six pediatric studies directly comparing individuals with different forms of LOC and/or overeating found that those with OBE endorsed similar levels of psychosocial impairment as compared to those with SBE across most measures;35,38,46,48,49,58 youth with OBE reported greater psychosocial impairment than those with SBE on very few measures.48 Of six pediatric studies reporting on psychosocial functioning in individuals with OO, three found that these individuals endorsed lower impairment than those with LOC, and similar levels of impairment as compared to those with no eating pathology, on most measures of distress.38,43,46 Three studies reported that youth with OO endorsed similar impairment as those with LOC, and/or greater psychosocial impairment than those with no eating pathology on most psychosocial measures.3,33,44
Momentary data
In addition to these distal cross-sectional associations, multiple studies of distress and binge eating constructs have found that LOC frequently occurs in response to negative emotions.
Adults
In adults, one self-report study reported that SBE frequency was correlated with self-reported emotional eating tendencies in individuals with AN-binge/purge subtype, and OBE frequency was correlated with emotional eating tendencies in individuals with BN.55 Data from three independent EMA studies, one dietary recall study, and one laboratory-based study of adults indicated that LOC, particularly in the context of OBE, was associated with elevated pre- and post-episode negative affect pre-episode.59–65 Two adult EMA studies, both of which involved adults with obesity, reported on OO in relation to momentary distress. One of these studies found that that negative affect was not increased prior to OO.65 The other found that pre-episode negative affect was unrelated to energy intake, a potential proxy for OO; post-episode negative affect was related to energy intake in obese individuals without BED, but was unrelated to energy intake in those with BED.61
Youth
Three out of three pediatric self-report studies suggested that LOC eating was associated with eating in response to negative affect,39,41,48 although in one of these studies, associations were only significant for youth with OBE and not SBE.48 Of two laboratory-based studies reporting on negative affect in youth with LOC eating, one found that negative mood ratings predicted the degree to which youth reported LOC during a subsequent test meal,47 while the other found no association between energy intake and negative affect.66 Of two EMA studies of negative affect, both reported that negative affect did not precede LOC eating in adolescents.67,68 In one of these studies, happiness was found to be lower during both binge and normal meals of youth with LOC eating relative to random signal events prompted by the investigators, and sadness was higher on binge days in youth with LOC eating relative to non-binge days of youth without LOC eating.67 Cognitive, stress-related, and interpersonal factors may be more consistently associated with LOC eating episodes in youth.67–69
Eating behavior
Adults
A total of 12 adult studies reported on eating behavior in relation to LOC and/or overeating (as approximated by energy intake), including 5 respondent-based17,59,62,63,70 and 7 laboratory-based studies.64,71–76 The one study17 that specifically investigated binge eating constructs among individuals with eating pathology relative to controls with no eating pathology reported higher overall energy intake in those endorsing LOC and/or overeating relative to controls. Four out of four studies reported that degree of control over eating was highly correlated with energy intake during a self-reported or laboratory-based meal.62–64,75 OBE episodes were associated with greater energy intake than SBE in two out of two studies.17,70 Binge meals were associated with greater energy intake than non-binge meals in six out of six studies,71–76 but, with one exception,72 these findings only applied to individuals with eating disorders and not to healthy controls.
Youth
A total of six pediatric studies reported on eating behavior in relation to LOC and/or overeating, including three respondent-based39,42,67 and three laboratory-based studies.40,47,77 Of five studies generally comparing energy intake in youth with LOC relative to non-LOC controls, three reported no differences between the former and the latter40,42,47 and two reported greater energy intake in youth with LOC relative to controls67,77 (although in Hilbert and colleagues’ 2010 study, differences were reported only during a child-only snack meal). Meals involving LOC were associated with greater energy intake than non-LOC meals in two out of two studies.40,67
Adult and pediatric findings regarding other eating behavior-related variables, such as macronutrient composition, hunger, and satiety, are reported in Table 3.
Discriminant Validity
There were no studies that directly addressed the discriminant validity of binge eating constructs.
Predictive Validity
A total of 9 adult and 8 pediatric studies reported on the predictive validity of binge eating constructs; results of these studies are summarized in Table 4.
Table 4.
Summary of studies assessing the predictive validity of binge eating constructs
| Study | Sample | n | %F | Age | BMI | Predictor | Outcome measure | ||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Length of F/U¥ |
Domain | Method | |||||||
|
Adults
| |||||||||
| 81 | TS: BN | 85 | 96.5 | 29.5±9.1 | 22.8±5.8 | Baseline SBE frequency | 3y | Remission from BN: OR=0.87* | Interview |
| TS: BED | 133 | 88.0 | 43.9±11.9 | 38.0±7.3 | Remission from BED: OR=0.90* | ||||
|
| |||||||||
| 18 | TS: underweight eating disorders with OBE | 33 | 100 | 27.9±6.9 | 15.4±1.6 | Baseline LOC status | 5m | Increase in BMI: OBE, SBE<no-LOC [F(1,2,68)=5.30**] | Measured |
| Decrease in eating-related psychopathology: OBE=SBE=no-LOC [F(1,2,68)=2.24] | Interview | ||||||||
| Decrease in depression: OBE=SBE=no-LOC [F(1,2,68)=2.97] | Self-report | ||||||||
| Decrease in anxiety: OBE=SBE=no-LOC [F(1,2,68)=1.82] | Self-report | ||||||||
| TS: underweight eating disorders with SBE | 36 | 25.8±10.5 | 14.0±1.3 | Decrease in novelty seeking: OBE=SBE=no-LOC [F(1,2,68)=0.80] | Self-report | ||||
| Decrease in harm avoidance: OBE=SBE=no-LOC [F(1,2,68)=0.60] | Self-report | ||||||||
| Decrease in reward dependence: OBE=SBE=no-LOC [F(1,2,68)=0.21] | Self-report | ||||||||
| Decrease in persistence: OBE=SBE=no-LOC [F(1,2,68)=0.70] | Self-report | ||||||||
| TS: underweight eating disorders with no LOC | 36 | 24.3±9.0 | 14.4±1.7 | Decrease in self-directedness: OBE=SBE=no-LOC [F(1,2,68)=0.75] | Self-report | ||||
| Decrease in cooperativeness: OBE=SBE=no-LOC [F(1,2,68)=0.28] | Self-report | ||||||||
| Decrease in self-transecendence: OBE=SBE=no-LOC [F(1,2,68)=0.16] | Self-report | ||||||||
|
| |||||||||
| 78 | TS: bariatric surgery | 129 | 80.0 | 45.2±11.5 | 44.3±6.8 | Pre-surgical LOC status | 12m | % weight loss: LOC=no-LOC | Measured |
|
| |||||||||
| 79 | TS: bariatric surgery | 183 | 83.1 | 46.0 (median) | 45.1 | Pre-surgical monthly OBE | 3y | Weight change: β=−0.7 | Measured |
| Pre-surgical monthly SBE | Weight change: β=1.8 | ||||||||
| Pre-surgical monthly OO | Weight change: β=−1.6 | ||||||||
|
| |||||||||
| 83 | TS: BN | 80 | 90 | 27.3±9.6 | 23.9±5.5 | Baseline to end-of-treatment change in OBE frequency | 4m | Decrease in eating-related psychopathology: B=0.00; SE=0.01 | Interview |
| Decrease in depression: B=0.03; SE=0.07 | Self-report | ||||||||
| Decrease in anxiety: B=0.12; SE=0.08 | Self-report | ||||||||
| Increase in self-esteem: B=−0.00; SE=0.01 | Self-report | ||||||||
| Baseline to end-of-treatment change in SBE frequency | Decrease in eating-related psychopathology: B=0.03; SE=0.01** | Interview | |||||||
| Decrease in depression: B=0.24; SE=0.08** | Self-report | ||||||||
| Decrease in anxiety: B=0.37; SE=0.09*** | Self-report | ||||||||
| Increase in self-esteem: B=−0.02; SE=0.01 | Self-report | ||||||||
|
| |||||||||
| 80 | TS: BED placeb-responders | 147 | 90.3 | 41.8±9.6 | 35.3±5.3 | Baseline OBE days | 4w | Placebo responders<non-responders [t(446)=2.83**] | Interview |
| Baseline SBE days | Placebo responders>non-responders [t(446)=2.70**] | Interview | |||||||
| TS: BED non-placebo-responders | 304 | ||||||||
| Baseline OO days | Placebo responders=non-responders [t(447)=0.05] | Interview | |||||||
|
| |||||||||
| 30 | NTS: community-based with OBE | 154 | 100 | 26.2±7.0 | 27.4±7.2 | Baseline LOC status | 5y | Increase in BMI: OBE=no-LOC (coefficient=−0.90; SE=0.68); OBE>SBE (coefficient=−2.51; SE=0.79*) | Self-report |
| NTS: community-based with SBE | 68 | 25.6±7.8 | 24.1±5.8 | Increase in eating-related psychopathology: OBE>no-LOC (coefficient=−0.42; SE=0.12*); OBE=SBE (coefficient=−0.17; SE=0.13) | Self-report | ||||
| Decrease in physical QOL: OBE=no-LOC (coefficient=0.22; SE=0.84); OBE=SBE (coefficient=0.23; SE=0.98) | Self-report | ||||||||
| NTS: community-based with no LOC | 108 | 25.4±7.6 | 25.4±5.4 | Decrease in mental QOL: OBE<no-LOC (coefficient=2.16; SE=1.08*); OBE=SBE (coefficient=−0.33; SE=1.25) | Self-report | ||||
| Decrease in negative affect: OBE=no-LOC (coefficient=−1.42; SE=0.77); OBE=SBE (coefficient=1.27; SE=0.89) | Self-report | ||||||||
|
| |||||||||
| 82 | TS: BED | 50 | 100 | 42.4±10.1 | 34.2±7.1 | Baseline OBE frequency | 8w | Binge eating remission: B=0.43* | Self-report |
| Baseline SBE frequency | Binge eating remission: NS | ||||||||
|
| |||||||||
| 23 | TS: bariatric surgery | 361 | 86.1 | 43.7±10.0 | 51.1±8.3 | Baseline LOC status | 2y | % weight loss at all available F/U: F(1,381)=0.03 | Self-report |
| 6m LOC status | % weight loss at 12m and 24m: F(1,252)=4.75* | ||||||||
| 12m LOC status | % weight loss at 24m: F(1,130)=8.79** | ||||||||
|
| |||||||||
|
Youth
| |||||||||
| 118 | TS: obesity | 132 | 62.1 | 13.6±2.2 | 2.2±0.3 (z-score) | Baseline OBE status | 10m | Change in BMI: t=1.11 | Measured |
| Attrition: Wald χ2=1.55 | Measured | ||||||||
| Baseline SBE status | Change in BMI: B=0.27 | Measured | |||||||
| Attrition: Wald χ2=3.96* | Measured | ||||||||
|
| |||||||||
| 84 | NTS: community-based with LOC | 60 | 58.3 | 10.8±1.5 | 23.0±5.0 | Baseline LOC status | 5.5y | BMI at F/U: t(59)=−1.06 | Measured |
| Eating-related psychopathology at F/U: t(59)=−1.22 | Self-report | ||||||||
| NTS: community-based without LOC | 60 | 55.0 | Onset of BED: OR=1.39 | Interview | |||||
| Depression at F/U: t(59)=−0.10 | Self-report | ||||||||
|
| |||||||||
| 85 | NTS: community-based with LOC | 55 | 59.8 | 10.7±1.5 | 24.0±5.5 | Baseline LOC status | 2.2y | Change in BMI: LOC=no-LOC | Measured |
| Onset of BED: LOC>no-LOC [t(46)=2.71**] | Interview | ||||||||
| NTS: community-based with LOC | 57 | Change in eating-related psychopathology: LOC=no-LOC [t(46)=1.78] | Interview | ||||||
| Change in depression: LOC=no-LOC [t(46)=0.27] | Self-report | ||||||||
|
| |||||||||
| 56 | TS: overweight with LOC | 4 | 44.0 | 10.1±1.6 | 33.5±4.5 | Baseline LOC status | 4m | Change in BMI: LOC=no-LOC | Measured |
| TS: overweight without LOC | 23 | Attrition: LOC=no-LOC | Measured | ||||||
|
| |||||||||
| 4 | NTS: community-based with OBE | 16882 | 53.5 | 12.0±1.6 | NR | OBE vs. no overeating status | 9y | Onset of overweight: OR=1.73* | Self-report |
| Onset of high depression symptoms: OR=2.19* | |||||||||
| NTS: community-based with OO | Onset of binge drinking: OR=1.14 | Self-report | |||||||
| Onset of marijuana use: OR=1.85* | |||||||||
| Onset of other drug use: OR=1.59* | Self-report | ||||||||
| OO vs. no overeating status | Onset of overweight: OR=1.24 | ||||||||
| NTS: community-based with no pathology | Onset of high depression symptoms: OR=1.58 | Self-report | |||||||
| Onset of binge drinking: OR=1.01 | |||||||||
| Onset of marijuana use: OR=2.67* | Self-report | ||||||||
| Onset of other drug use: OR=1.89* | |||||||||
|
| |||||||||
| 86 | TS: bariatric surgery | 101 | 72.3 | 15.8±1.1 | 47.2±0.9 | Baseline LOC status | 15m | Change in BMI: intercept=0.29; SE=0.14*; slope=0.48; SE=0.08* | Measured |
|
| |||||||||
| 88 | NTS: community-based with LOC | 46 | 73.9 | 10.3±.01 | 25.4±1.1 | Baseline LOC status | 4.7y | Onset of BED: LOC>no-LOC (OR=10.8*) | Interview |
| Increase in eating-related psychopathology: LOC>noLOC* | Interview | ||||||||
| NTS: community-based without LOC | 149 | 52.3 | 10.2±0.0 | 21.8±0.3 | Increase in depression: LOC=no-LOC | Self-report | |||
| Increase in anxiety: LOC>noLOC* | Self-report | ||||||||
|
| |||||||||
| 87 | NTS: community-based aged 6–8y | 29 | 13.3 | 8.3±0.6 | 20.6±5.9 | Baseline LOC status | 4.5y | Change in BMI: LOC>no-LOC (estimate=0.61; SE=0.26**) | Measured |
| NTS: community-based aged 9–10y | 64 | 24.4 | 10.1±0.6 | 23.1±7.6 | |||||
| NTS: community-based aged 11–12y | 50 | 19.6 | 11.9±0.5 | 24.8±6.9 | |||||
Note: Age and BMI reported as means unless otherwise stated. Only comparisons involving binge eating constructs are reported.
Abbreviations: F=female; BMI=body mass index (kg/m2); F/U=follow-up; TS=treatment-seeking; BN=bulimia nervosa; BED=binge eating disorder; SBE=subjective binge eating; OR=odds ratio; LOC=loss of control; OBE=objective binge eating; OO=objective overeating; SE=standard error; NTS=non-treatment-seeking;
y=years; m=months; w=weeks
p≤.05
p<.01
p<.001
Adults
Of the 9 adult studies reporting on the predictive validity of specific binge eating constructs, 8 were conducted in the context of an intervention. Of four studies reporting on weight-related outcomes following psychological or surgical treatment, three found that baseline OBE, SBE, and/or OO were not predictive of weight change,23,78,79 and one found that baseline LOC predicted lower weight re-gain in underweight individuals with eating disorders.18 In one study, LOC eating following bariatric surgery was predictive of lower weight loss at subsequent time-points.23 Of two studies directly comparing binge eating constructs, one found equivalent weight outcomes in those reporting OBE relative to those reporting SBE,18 while the other found OBE to be associated with greater weight gain than SBE.30
In terms of psychosocial outcomes, findings have been mixed. In one study, baseline OBE predicted placebo non-response while baseline SBE predicted placebo response; OO was equivalent among placebo responders and non-responders.80 One study found higher baseline SBE frequency to be predictive of non-remission from an eating disorder,81 while another found OBE, but not SBE, to predict remission status.82 Finally, while two studies reported that individuals with OBE and SBE generally did not differ from one another or from controls with no LOC eating in terms of changes in eating-related and general psychopathology,18,30 another found that changes in SBE, but not OBE, predicted changes in eating-related and general psychopathology during and after psychological treatment.83
Youth
Of eight pediatric studies reporting on the predictive validity of specific binge eating constructs, three were conducted in the context of an intervention. In terms of weight-related outcomes, weight gain was found to be unrelated to LOC eating in four naturalistic or intervention studies,35,56,84,85 while three other studies found that LOC eating predicted poorer weight-related outcomes.4,86,87 OO was not associated with elevated risk for adverse weight outcomes in the single study that reported on this construct.4 LOC eating was associated with poorer psychosocial outcomes, including onset of BED, in most studies,4,85,88 although these associations may not hold up over longer periods of time.84
Discussion
Emerging evidence supports the validity of binge eating constructs, particularly LOC. Overall, the literature suggests that LOC is a psychopathology construct that is uniquely associated with distress and impairment, disturbed eating behavior, and weight-related factors in both cross-sectional and prospective studies, independent of episode size and body weight. Although research on overeating independent of LOC is underrepresented, overeating may best be conceptualized as a marker of risk for excess body weight.
Summary and Interpretations
Studies generally supported the face validity of binge eating constructs by demonstrating the importance of LOC and overeating in individuals’ appraisals of binge eating. However, results were more consistent in adults than in college students and adolescents, who tended to highlight overeating, but not LOC, as central in their appraisals. Thus, it is crucial to consider developmental factors involved in determining the core attributes of binge eating. Such factors may include one’s ability to understand the meaning of LOC and overeating, and eating-related social comparisons specific to one’s peer group.
Support for the convergent validity of LOC in adults was strong for psychosocial and eating-related factors, but mixed for anthropometric characteristics, which may be a function of differing samples. Associations between LOC and body weight were stronger, and less influenced by episode size, among treatment-seeking relative to community-based adults, which may reflect a tendency for individuals with more severe conditions to present in clinical settings;89 therefore, associations between binge eating and increased body weight may be accounted for by the greater severity of binge eating seen in clinical samples, whereas these associations may be less clear in non-clinical samples in which binge eating may be less severe when present. OBE and SBE were indistinguishable on most measures of psychosocial functioning, suggesting that LOC, irrespective of overeating, may be driving associations between binge eating and distress/impairment; however, some recent research indicates that assessing episode size adds incremental value to the convergent validity of LOC.90 The convergent validity of the overeating construct, independent of LOC, was not addressed in most studies.
Pediatric LOC was consistently related to indices of increased body weight and psychosocial impairment, while results for overeating were less consistent in youth. LOC did not consistently track with youth’s energy intake, which may be related to developmental differences in energy intake associated with LOC episodes, perhaps due to varying nutritional needs91 and differing access to energy dense foods92 in children as compared to adults. However, LOC eating was marked by differences in the composition of eating episodes, suggesting that the experience of LOC in youth may manifest in differing food choices rather than overall increased energy intake.
There were limited data addressing the discriminant validity of LOC and overeating, which may partially reflect a bias against publishing null findings.93 However, it is worth noting that LOC appears distinct from other eating- and weight-related problems. Although LOC may overlap to some extent with overeating and other forms of disinhibited eating (e.g., eating in the absence of hunger), research in adults22,59,94 and children38,46,95 suggests that these are distinct constructs with distinct correlates. Indeed, research has shown that the frequency of OBE episodes is unrelated to the frequency of SBE episodes (r range=.08–.22),54,96 suggesting that LOC and overeating are distinct constructs.
Finally, most, but not all, of the studies reviewed supported the predictive validity of LOC in relation to treatment outcome and naturalistic eating- and weight-related outcomes. An additional point to consider is that several studies have shown that persistent LOC eating is associated with adverse health outcomes in youth;84,88 similarly, in the bariatric surgery literature, post-surgical LOC eating has been concurrently associated with poorer weight outcomes in adults.97 While these studies do not fit neatly into the domain of predictive validity as they are not truly prospective in nature, they provide additional support that LOC eating is associated with adverse health-related outcomes across the age spectrum. Finally, as with other validity domains, the predictive validity of OO has been underexplored. Research is also needed to clarify the impact of specific binge eating constructs on treatment outcome in youth.
Limitations
Measurement issues comprise the major limitation of this review. For example, overeating was approximated corresponding to energy intake for multiple studies. This is an imperfect proxy since the objectively large/not large distinction is determined by the quantity, not quality or density, of food. Thus, an objectively large episode could contain relatively few calories (e.g., 5 apples) while a subjectively large episode could be calorically dense (e.g., typical fast food meal). More generally, the modest reliability of LOC and overeating is an issue that has been raised by other investigators,98 and represents a point of concern for this review since poor reliability can distort interpretations of validity. The modest reliability of the LOC construct may reflect the inherent difficulty of having participants recall momentary constructs that naturally vary over time and are associated with negative affect and current dietary patterns, and of attempting to obtain precise details about features of LOC and overeating episodes that may or may not be important in identifying their presence (e.g., actual/subjective episode quantity, duration, context). Ultimately, the behavioral aspects of LOC and overeating, while potentially easier to identify, appear to be less important than one’s subjective experience during such episodes, the latter of which is fundamentally more difficult to assess. Therefore, future research on binge eating constructs should seek to improve its measurement in the service of enhanced reliability. Finally, as with other literature reviews, the data described herein may be subject to biases in the peer review system (e.g., publication bias, selective reporting). Therefore, results should be interpreted cautiously.
Future Directions
Several areas related to our understanding of LOC and overeating require additional research. First, sociocultural differences, particularly those related to gender and race/ethnicity, in the presentation of LOC and overeating are underexplored, which is problematic since binge eating is more evenly distributed across these domains than other eating disorder behaviors.2–4 Second, the limited data on OO and, to an even greater extent, SO has impeded attempts to tease apart the independent contributions of LOC and perceived/actual overeating to weight- and eating-related outcomes. Previous research has suggested that LOC may be confounded by episode size,62 and as a result, it is unclear whether LOC drives eating behavior, or problematic interpretations of one’s eating behavior (e.g., breaking a dietary rule) drive subjective reports of LOC. It is also unclear why OO or SO may occur in the absence of LOC on some occasions but not others, sometimes within the same individual. This lack of clarity has clinical implications in terms of focusing treatments on enhancing control over eating, versus improving problematic perceptions about eating behavior.
Third, it is unclear whether LOC—especially while consuming a subjectively large amount of food—is related to a general tendency to pathologize one’s behaviors and experiences, which may explain cross-sectional associations between LOC and psychopathology. Relatedly, eating disorders involving LOC and other disorders characterized by self-control impairments frequently co-occur,2 but it is unclear whether the underlying experience of LOC is similar across behavioral phenotypes. Indeed, this issue has been raised in regard to the controversial “food addiction” construct,99 a distinct but potentially overlapping construct relative to binge eating. Therefore, a critical yet unanswered question in the literature is the extent to which LOC is specific to eating behavior, or whether the construct represents generalized pathology extending to multiple reinforcers. Inter-disciplinary cross-talk will be critical in starting to answer this question, as differing labels (e.g., “addiction,” “self-control”) used to describe potentially similar constructs may impede the growth of new knowledge regarding how to study and treat behavioral problems.
A fourth research gap is related to the limited assessment of objective markers of the momentary occurrence of LOC and overeating. A significant impediment to identifying biomarkers of these phenomena is that reliable methods for eliciting LOC in particular are limited. Feeding laboratory studies often involve instructing participants to engage in binge eating episodes, and this methodology is fairly consistently associated with objective changes in eating behavior as compared to instructing participants to engage in eating a normal meal, as reviewed in Table 3. However, systematic collection of other objective data in such studies has been limited, thereby impeding knowledge on the extent to which these objective measures are linked specifically to LOC, overeating, or their confluence, and the unique influence of these constructs on weight regulation. Future directions include developing effective methods for eliciting LOC eating across laboratory-based paradigms, including using proxy designs to simulate LOC eating, and more programmatically assessing biomarkers in other momentary data collection designs.
A final point concerns the classification scheme for eating disorders. DSM-5 requires OBE for diagnoses of BED and BN, while individuals reporting SBE in the absence of OBE are relegated to a residual “otherwise specified” category.100 Given that LOC is a valid construct that is uniquely related to psychopathology independent of overeating, this author would argue that both OBE and SBE should be accounted for in the diagnostic scheme. Several investigators have proposed independent diagnoses which would accommodate individuals who engage in SBE (e.g.,101). A more parsimonious alternative might be to relax the DSM binge eating criterion to include both OBE and SBE, as is likely for ICD-11.102 Alternatively, eliminating size-related distinctions all together may be optimal for future diagnostic schemes, especially given evidence that OBE and SBE episodes are similarly predictive of distress, impairment, and other health-related outcomes. Further diagnostically relevant research will hopefully clarify these taxonomic issues.
Ultimately, developing and implementing efficacious interventions for binge eating-related problems across the size and LOC-severity spectrum should be a priority. Research has shown that SBE may be less responsive than OBE to psychological treatments addressing behavioral and affective antecedents,26,83 suggesting that there may be unique triggers of LOC in the absence of overeating that aren’t adequately addressed in current interventions. Treatments focused on improving distorted cognitions about one’s eating behavior (e.g., subjective perceptions that one has eaten an excessive amount of food, which may be related to the experience of LOC)62 as well as increasing mindfulness/intuitive eating practices to enhance awareness of subjective and objective cues around eating and avoid common LOC triggers103 may be particularly helpful.
In summary, accumulating evidence suggests that LOC is a valid construct despite evidence of its modest reliability, particularly when accompanied by subjectively large amounts of food. Overeating appears to be best considered as a potential marker for excess weight. Future research should focus on clarifying the phenomenology, measurement, and unique outcomes of these constructs to inform prevention/early intervention and classification efforts.
Acknowledgments
Dr. Goldschmidt is supported by NIH grant K23-DK105234. She is grateful to Drs. Andrea E. Kass, Kate Keenan, Stephen A. Wonderlich, Kelly C. Berg, and Carol B. Peterson for their comments and feedback on earlier drafts of this manuscript.
Footnotes
Conflicts of interest: None to report
References
- 1.French SA, Epstein LH, Jeffery RW, Blundell JE, Wardle J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite. 2012;59:541–549. doi: 10.1016/j.appet.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldschmidt AB, Loth KA, MacLehose RF, Pisetsky EM, Berge JM, Neumark-Sztainer D. Overeating with and without loss of control: Associations with weight status, weight-related characteristics, and psychosocial health. Int J Eat Disord. 2015;48:1150–1157. doi: 10.1002/eat.22465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sonneville KR, Horton NJ, Micali N, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatr. 2013;167:149–155. doi: 10.1001/2013.jamapediatrics.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolfe BE, Baker CW, Smith AT, Kelly-Weeder S. Validity and utility of the current definition of binge eating. Int J Eat Disord. 2009;42:674–686. doi: 10.1002/eat.20728. [DOI] [PubMed] [Google Scholar]
- 6.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. Guilford Press; New York, NY: 1993. pp. 317–360. [Google Scholar]
- 7.Rospond B, Szpigiel J, Sadakierska-Chudy A, Filip M. Binge eating in pre-clinical models. Pharmacological Reports. 2015;67:504–512. doi: 10.1016/j.pharep.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Telch CF, Pratt EM, Niego SH. Obese women with binge eating disorder define the term binge. Int J Eat Disord. 1998;24:313–317. doi: 10.1002/(sici)1098-108x(199811)24:3<313::aid-eat9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 9.Coker EL, von Lojewski A, Luscombe GM, Abraham SF. The difficulty in defining binge eating in obese women: How it affects prevalence levels in presurgical bariatric patients. Eat Behav. 2015;17:130–135. doi: 10.1016/j.eatbeh.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 10.Beglin SJ, Fairburn CG. What is meant by the term “binge”? Am J Psychiatry. 1992;149:123–124. doi: 10.1176/ajp.149.1.123. [DOI] [PubMed] [Google Scholar]
- 11.Reslan S, Saules KK. College students’ definitions of an eating “binge” differ as a function of gender and binge eating disorder status. Eat Behav. 2011;12:225–227. doi: 10.1016/j.eatbeh.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Sierra Baigrie S, Lemos Giraldez S. Examining the relationship between binge eating and coping strategies and the definition of binge eating in a sample of Spanish adolescents. Span J Psychol. 2008;11:172–180. doi: 10.1017/s1138741600004212. [DOI] [PubMed] [Google Scholar]
- 13.Palmberg AA, Stern M, Kelly NR, et al. Adolescent girls and their mothers talk about experiences of binge and loss of control eating. J Child Fam Stud. 2014;23:1403–1416. doi: 10.1007/s10826-013-9797-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson WG, Carr-Nangle RE, Nangle DW, Antony MM, Zayfert C. What is binge eating? A comparison of binge eater, peer, and professional judgments of eating episodes. Addict Behav. 1997;22:631–635. doi: 10.1016/s0306-4603(97)00007-5. [DOI] [PubMed] [Google Scholar]
- 15.Johnson WG, Roberson-Nay R, Rohan KJ, Torgrud L. An experimental investigation of DSM-IV binge-eating criteria. Eat Behav. 2003;4:295–303. doi: 10.1016/S1471-0153(03)00028-X. [DOI] [PubMed] [Google Scholar]
- 16.LaPorte DJ. Influences of gender, amount of food, and speed of eating on external raters’ perceptions of binge eating. Appetite. 1996;26:119–127. doi: 10.1006/appe.1996.0010. [DOI] [PubMed] [Google Scholar]
- 17.Colles SL, Dixon JB, O’Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity. 2008;16:608–614. doi: 10.1038/oby.2007.99. [DOI] [PubMed] [Google Scholar]
- 18.Dalle Grave R, Calugi S, Marchesini G. Objective and subjective binge eating in underweight eating disorders: Associated features and treatment outcome. Int J Eat Disord. 2012;45:370–376. doi: 10.1002/eat.20943. [DOI] [PubMed] [Google Scholar]
- 19.Jenkins PE, Conley CS, Rienecke Hoste R, Meyer C, Blissett JM. Perception of control during episodes of eating: Relationships with quality of life and eating psychopathology. Int J Eat Disord. 2012;45:115–119. doi: 10.1002/eat.20913. [DOI] [PubMed] [Google Scholar]
- 20.Elder KA, Paris M, Jr, Anez LM, Grilo CM. Loss of control over eating is associated with eating disorder psychopathology in a community sample of Latinas. Eat Behav. 2008;9:501–503. doi: 10.1016/j.eatbeh.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Royal S, Wnuk S, Warwick K, Hawa R, Sockalingam S. Night eating and loss of control over eating in bariatric surgery candidates. J Clin Psychol Med Settings. 2015;22:14–19. doi: 10.1007/s10880-014-9411-6. [DOI] [PubMed] [Google Scholar]
- 22.Striegel-Moore RH, Wilson GT, Wilfley DE, Elder KA, Brownell KD. Binge eating in an obese community sample. Int J Eat Disord. 1998;23:27–37. doi: 10.1002/(sici)1098-108x(199801)23:1<27::aid-eat4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 23.White MA, Kalarchian MA, Masheb RM, Marcus MD, Grilo CM. Loss of control over eating predicts outcomes in bariatric surgery: A prospective 24-month follow-up study. J Clin Psychiatry. 2010;71:175–184. doi: 10.4088/JCP.08m04328blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berner LA, Arigo D, Mayer LE, Sarwer DB, Lowe MR. Examination of central body fat deposition as a risk factor for loss-of-control eating. Am J Clin Nutr. 2015;102:736–744. doi: 10.3945/ajcn.115.107128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brownstone LM, Bardone-Cone AM, Fitzsimmons-Craft EE, et al. Subjective and objective binge eating in relation to eating disorder symptomatology, negative affect, and personality dimensions. Int J Eat Disord. 2013;46:66–76. doi: 10.1002/eat.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Niego SH, Pratt EM, Agras WS. Subjective or objective binge: Is the distinction valid? Int J Eat Disord. 1997;22:291–298. doi: 10.1002/(sici)1098-108x(199711)22:3<291::aid-eat8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 27.Palavras MA, Morgan CM, Borges FM, Claudino AM, Hay PJ. An investigation of objective and subjective types of binge eating episodes in a clinical sample of people with co-morbid obesity. J Eat Disord. 2013;1:26. doi: 10.1186/2050-2974-1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hay PJ, Fairburn CG, Doll HA. The classification of bulimic eating disorders: A community-based cluster analysis study. Psychol Med. 1996;26:801–812. doi: 10.1017/s003329170003782x. [DOI] [PubMed] [Google Scholar]
- 29.Mond JM, Latner JD, Hay PH, Owen C, Rodgers B. Objective and subjective bulimic episodes in the classification of bulimic-type eating disorders: Another nail in the coffin of a problematic distinction. Behav Res Ther. 2010;48:661–669. doi: 10.1016/j.brat.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 30.Palavras MA, Hay PJ, Lujic S, Claudino AM. Comparing symptomatic and functional outcomes over 5-years in two nonclinical cohorts characterized by binge eating with and without objectively large episodes. Int J Eat Disord. 2015 doi: 10.1002/eat.22466. [DOI] [PubMed] [Google Scholar]
- 31.Watson HJ, Fursland A, Bulik CM, Nathan P. Subjective binge eating with compensatory behaviors: A variant presentation of bulimia nervosa. Int J Eat Disord. 2013;46:119–126. doi: 10.1002/eat.22052. [DOI] [PubMed] [Google Scholar]
- 32.Delahanty LM, Meigs JB, Hayden D, Williamson DA, Nathan DM. Psychological and behavioral correlates of baseline BMI in the diabetes prevention program (DPP) Diabetes Care. 2002;25:1992–1998. doi: 10.2337/diacare.25.11.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ackard DM, Neumark-Sztainer D, Story M, Perry C. Overeating among adolescents: Prevalence and associations with weight-related characteristics and psychological health. Pediatrics. 2003;111:67–74. doi: 10.1542/peds.111.1.67. [DOI] [PubMed] [Google Scholar]
- 34.Elliott CA, Tanofsky-Kraff M, Shomaker LB, et al. An examination of the interpersonal model of loss of control eating in children and adolescents. Behav Res Ther. 2010;48:424–428. doi: 10.1016/j.brat.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goossens L, Soenens B, Braet C. Prevalence and characteristics of binge eating in an adolescent community sample. J Clin Child Adolesc Psychol. 2009;38:342–353. doi: 10.1080/15374410902851697. [DOI] [PubMed] [Google Scholar]
- 36.Morgan CM, Yanovski SZ, Nguyen TT, et al. Loss of control over eating, adiposity, and psychopathology in overweight children. Int J Eat Disord. 2002;31:430–441. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Radin RM, Tanofsky-Kraff M, Shomaker LB, et al. Metabolic characteristics of youth with loss of control eating. Eat Behav. 2015;19:86–89. doi: 10.1016/j.eatbeh.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shomaker LB, Tanofsky-Kraff M, Elliott C, et al. Salience of loss of control for pediatric binge episodes: Does size really matter? Int J Eat Disord. 2010;43:707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanofsky-Kraff M, Goossens L, Eddy KT, et al. A multisite investigation of binge eating behaviors in children and adolescents. J Consult Clin Psychol. 2007;75:901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, et al. Laboratory assessment of the food intake of children and adolescents with loss of control eating. Am J Clin Nutr. 2009;89:738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tanofsky-Kraff M, Theim KR, Yanovski SZ, et al. Validation of the Emotional Eating Scale Adapted for use in Children and Adolescents (EES-C) Int J Eat Disord. 2007;40:232–240. doi: 10.1002/eat.20362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Theim KR, Tanofsky-Kraff M, Salaita CG, et al. Children’s descriptions of the foods consumed during loss of control eating episodes. Eat Behav. 2007;8:258–265. doi: 10.1016/j.eatbeh.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilfley D, Berkowitz R, Goebel-Fabbri A, et al. Binge eating, mood, and quality of life in youth with type 2 diabetes: baseline data from the today study. Daibetes Care. 2011;34:858–860. doi: 10.2337/dc10-1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. J Consult Clin Psychol. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schluter N, Schmidt R, Kittel R, Tetzlaff A, Hilbert A. Loss of control eating in adolescents from the community. Int J Eat Disord. 2016;49:413–420. doi: 10.1002/eat.22488. [DOI] [PubMed] [Google Scholar]
- 46.Goldschmidt AB, Jones M, Manwaring JL, et al. The clinical significance of loss of control over eating in overweight adolescents. Int J Eat Disord. 2008;41:153–158. doi: 10.1002/eat.20481. [DOI] [PubMed] [Google Scholar]
- 47.Goldschmidt AB, Tanofsky-Kraff M, Wilfley DE. A laboratory-based study of mood and binge eating behavior in overweight children. Eat Behav. 2011;21:37–43. doi: 10.1016/j.eatbeh.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goossens L, Braet C, Decaluwe V. Loss of control over eating in obese youngsters. Behav Res Ther. 2007;45:1–9. doi: 10.1016/j.brat.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 49.Goldschmidt AB, Accurso EC, O’Brien S, Fitzpatrick KK, Lock JD, Le Grange D. The importance of loss of control while eating in adolescents with purging disorder. Int J Eat Disord. 2016;49:801–804. doi: 10.1002/eat.22525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Birgegard A, Clinton D, Norring C. Diagnostic issues of binge eating in eating disorders. Eur Eat Disord Rev. 2013;21:175–183. doi: 10.1002/erv.2227. [DOI] [PubMed] [Google Scholar]
- 51.Keel PK, Mayer SA, Harnden-Fischer JH. Importance of size in defining binge eating episodes in bulimia nervosa. Int J Eat Disord. 2001;29:294–301. doi: 10.1002/eat.1021. [DOI] [PubMed] [Google Scholar]
- 52.Vannucci A, Theim KR, Kass AE, et al. What constitutes clinically significant binge eating? Association between binge features and clinical validators in college-age women. Int J Eat Disord. 2013;46:226–232. doi: 10.1002/eat.22115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Forney KJ, Haedt-Matt AA, Keel PK. The role of loss of control eating in purging disorder. Int J Eat Disord. 2014;47:244–251. doi: 10.1002/eat.22212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Latner JD, Hildebrandt T, Rosewall JK, Chisholm AM, Hayashi K. Loss of control over eating reflects eating disturbances and general psychopathology. Behav Res Ther. 2007;45:2203–2211. doi: 10.1016/j.brat.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 55.Ricca V, Castellini G, Fioravanti G, et al. Emotional eating in anorexia nervosa and bulimia nervosa. Compr Psychiatry. 2012;53:245–251. doi: 10.1016/j.comppsych.2011.04.062. [DOI] [PubMed] [Google Scholar]
- 56.Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Overeating among seriously overweight children seeking treatment: Results of the Children’s Eating Disorder Examination. Int J Eat Disord. 2006;39:135–140. doi: 10.1002/eat.20218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hartmann AS, Czaja J, Rief W, Hilbert A. Personality and psychopathology in children with and without loss of control over eating. Compr Psychiatry. 2010;51:572–578. doi: 10.1016/j.comppsych.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 58.Fitzsimmons-Craft EE, Ciao AC, Accurso EC, et al. Subjective and objective binge eating in relation to eating disorder symptomatology, depressive symptoms, and self-esteem among treatment-seeking adolescents with bulimia nervosa. Eur Eat Disord Rev. 2014;22:230–236. doi: 10.1002/erv.2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goldschmidt AB, Crosby R, Cao L, et al. Ecological momentary assessment of eating episodes in obese adults. Psychosom Med. 2014;76:747–752. doi: 10.1097/PSY.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goldschmidt AB, Wonderlich SA, Crosby RD, et al. Latent profile analysis of eating episodes in anorexia nervosa. J Psychiatr Res. 2014;53:193–199. doi: 10.1016/j.jpsychires.2014.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goldschmidt AB, Engel SG, Wonderlich SA, et al. Momentary affect surrounding loss of control and overeating in obese adults with and without binge eating disorder. Obesity. 2012;20:1206–1211. doi: 10.1038/oby.2011.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pollert GA, Engel SG, Schreiber-Gregory DN, et al. The role of eating and emotion in binge eating disorder and loss of control eating. Int J Eat Disord. 2013;46:233–238. doi: 10.1002/eat.22061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mitchell JE, Karr TM, Peat C, et al. A fine-grained analysis of eating behavior in women with bulimia nervosa. Int J Eat Disord. 2012;45:400–406. doi: 10.1002/eat.20961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Telch CF, Agras WS. Do emotional states influence binge eating in the obese? Int J Eat Disord. 1996;20:271–279. doi: 10.1002/(SICI)1098-108X(199611)20:3<271::AID-EAT6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 65.Berg KC, Crosby RD, Cao L, et al. Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Int J Eat Disord. 2015;48:641–653. doi: 10.1002/eat.22401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ranzenhofer LM, Hannallah L, Field SE, et al. Pre-meal affective state and laboratory test meal intake in adolescent girls with loss of control eating. Appetite. 2013;68:30–37. doi: 10.1016/j.appet.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hilbert A, Rief W, Tuschen-Caffier B, de Zwaan M, Czaja J. Loss of control eating and psychological maintenance in children: An ecological momentary assessment study. Behav Res Ther. 2009;47:26–33. doi: 10.1016/j.brat.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 68.Ranzenhofer LM, Engel SG, Crosby RD, et al. Using ecological momentary assessment to examine interpersonal and affective predictors of loss of control eating in adolescent girls. Int J Eat Disord. 2014 doi: 10.1002/eat.22333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ranzenhofer LM, Engel SG, Crosby RD, et al. Real-time assessment of heart rate variability and loss of control eating in adolescent girls: A pilot study. Int J Eat Disord. 2015 doi: 10.1002/eat.22464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bartholome LT, Raymond NC, Lee SS, Peterson CB, Warren CS. Detailed analysis of binges in obese women with binge eating disorder: Comparisons using multiple methods of data collection. Int J Eat Disord. 2006;39:685–693. doi: 10.1002/eat.20289. [DOI] [PubMed] [Google Scholar]
- 71.Guss JL, Kissileff HR, Devlin MJ, Zimmerli E, Walsh BT. Binge size increases with body mass index in women with binge-eating disorder. Obes Res. 2002;10:1021–1029. doi: 10.1038/oby.2002.139. [DOI] [PubMed] [Google Scholar]
- 72.Hadigan CM, Kissileff HR, Walsh BT. Patterns of food selection during meals in women with bulimia. Am J Clin Nutr. 1989;50:759–766. doi: 10.1093/ajcn/50.4.759. [DOI] [PubMed] [Google Scholar]
- 73.Kissileff HR, Walsh BT, Kral JG, Cassidy SM. Laboratory studies of eating behavior in women with bulimia. Physiol Behav. 1986;38:563–570. doi: 10.1016/0031-9384(86)90426-9. [DOI] [PubMed] [Google Scholar]
- 74.LaChaussee JL, Kissileff HR, Walsh BT, Hadigan CM. The single-item meal as a measure of binge-eating behavior in patients with bulimia nervosa. Physiol Behav. 1992;51:593–600. doi: 10.1016/0031-9384(92)90185-5. [DOI] [PubMed] [Google Scholar]
- 75.Walsh BT, Kissileff HR, Cassidy SM, Dantzic S. Eating behavior of women with bulimia. Arch Gen Psychiatry. 1989;46:54–58. doi: 10.1001/archpsyc.1989.01810010056008. [DOI] [PubMed] [Google Scholar]
- 76.Yanovski SZ, Leet M, Yanovski JA, et al. Food selection and intake of obese women with binge eating disorder. Am J Clin Nutr. 1992;56:975–980. doi: 10.1093/ajcn/56.6.975. [DOI] [PubMed] [Google Scholar]
- 77.Hilbert A, Tuschen-Caffier B, Czaja J. Eating behavior and familial interactions of children with loss of control eating: A laboratory test meal study. Am J Clin Nutr. 2010;91:510–518. doi: 10.3945/ajcn.2009.28843. [DOI] [PubMed] [Google Scholar]
- 78.Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: Two high-risk factors following bariatric surgery. Obesity. 2008;16:615–622. doi: 10.1038/oby.2007.101. [DOI] [PubMed] [Google Scholar]
- 79.Devlin MJ, King WC, Kalarchian MA, et al. Eating pathology and experience and weight loss in a prospective study of bariatric surgery patients: 3-year follow-up. Int J Eat Disord. 2016 doi: 10.1002/eat.22578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jacobs-Pilipski MJ, Wilfley DE, Crow SJ, et al. Placebo response in binge eating disorder. Int J Eat Disord. 2007;40:204–211. doi: 10.1002/eat.20287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Castellini G, Mannucci E, Lo Sauro C, et al. Different moderators of cognitive-behavioral therapy on subjective and objective binge eating in bulimia nervosa and binge eating disorder: A three-year follow-up study. Psychother Psychosom. 2012;81:11–20. doi: 10.1159/000329358. [DOI] [PubMed] [Google Scholar]
- 82.Peterson CB, Crow SJ, Nugent S, Mitchell JE, Engbloom S, Mussell MP. Predictors of treatment outcome for binge eating disorder. Int J Eat Disord. 2000;28:131–138. doi: 10.1002/1098-108x(200009)28:2<131::aid-eat1>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 83.Goldschmidt AB, Accurso EC, Crosby RD, et al. Association between objective and subjective binge eating and psychopathology during a psychological treatment trial for bulimic symptoms. Appetite. 2016;107:471–477. doi: 10.1016/j.appet.2016.08.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hilbert A, Brauhardt A. Childhood loss of control eating over five-year follow-up. Int J Eat Disord. 2014;47:758–761. doi: 10.1002/eat.22312. [DOI] [PubMed] [Google Scholar]
- 85.Hilbert A, Hartmann AS, Czaja J, Schoebi D. Natural course of preadolescent loss of control eating. J Abnorm Psychol. 2013;122:684–693. doi: 10.1037/a0033330. [DOI] [PubMed] [Google Scholar]
- 86.Sysko R, Devlin MJ, Hildebrandt TB, Brewer SK, Zitsman JL, Walsh BT. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychiatry. 2012;73:1351–1357. doi: 10.4088/JCP.12m07690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord. 2009;42:26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tanofsky-Kraff M, Shomaker LB, Olsen C, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120:108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics Bulletin. 1946;2:47–53. [PubMed] [Google Scholar]
- 90.Forney KJ, Bodell LP, Haedt-Matt AA, Keel PK. Incremental validity of the episode size criterion in binge-eating definitions: An examination in women with purging syndromes. Int J Eat Disord. 2016;49:651–662. doi: 10.1002/eat.22508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Torun B. Energy requirements of children and adolescents. Public Health Nutr. 2005;8:968–993. doi: 10.1079/phn2005791. [DOI] [PubMed] [Google Scholar]
- 92.Hill AJ. Developmental issues in attitudes to food and diet. Proc Nutr Soc. 2002;61:259–266. doi: 10.1079/PNS2002152. [DOI] [PubMed] [Google Scholar]
- 93.Franco A, Malhotra N, Simonovits G. Publication bias in the social sciences: Unlocking the file drawer. Science. 2014;345:1502–1505. doi: 10.1126/science.1255484. [DOI] [PubMed] [Google Scholar]
- 94.Gill R, Chen Q, D’Angelo D, Chung WK. Eating in the absence of hunger but not loss of control behaviors are associated with 16p11.2 deletions. Obesity. 2014;22:2625–2631. doi: 10.1002/oby.20892. [DOI] [PubMed] [Google Scholar]
- 95.Vannucci A, Tanofsky-Kraff M, Crosby RD, et al. Latent profile analysis to determine the typology of disinhibited eating behaviors in children and adolescents. J Consult Clin Psychol. 2013;81:494–507. doi: 10.1037/a0031209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kerzhnerman I, Lowe MR. Correlates of subjective and objective binge eating in binge-purge syndromes. Int J Eat Disord. 2002;31:220–228. doi: 10.1002/eat.10026. [DOI] [PubMed] [Google Scholar]
- 97.Meany G, Conceicao E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22:87–91. doi: 10.1002/erv.2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mond JM. Classification of bulimic-type eating disorders: from DSM-IV to DSM-5. J Eat Disord. 2013;1:33. doi: 10.1186/2050-2974-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Davis C. Evolutionary and neuropsychological perspectives on addictive behaviors and addictive substances: relevance to the “food addiction” construct. Substance abuse and rehabilitation. 2014;5:129–137. doi: 10.2147/SAR.S56835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, D.C: 2013. [Google Scholar]
- 101.Tanofsky-Kraff M, Marcus MD, Yanovski SZ, Yanovski JA. Loss of control eating disorder in children age 12 years and younger: Proposed research criteria. Eat Behav. 2008;9:360–365. doi: 10.1016/j.eatbeh.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Uher R, Rutter M. Classification of feeding and eating disorders: Review of evidence and proposals for ICD-11. World psychiatry : official journal of the World Psychiatric Association (WPA) 2012;11:80–92. doi: 10.1016/j.wpsyc.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Leong SL, Gray A, Haszard J, Horwath C. Weight-Control Methods, 3-Year Weight Change, and Eating Behaviors: A Prospective Nationwide Study of Middle-Aged New Zealand Women. J Acad Nutr Diet. 2016;116:1276–1284. doi: 10.1016/j.jand.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 104.Sysko R, Glasofer DR, Hildebrandt T, et al. The eating disorder assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. Int J Eat Disord. 2015;48:452–463. doi: 10.1002/eat.22388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.First M, Spitzer R, Gibbon M, Williams J, editors. Structured clinical interview for DSM-IV Axis I disorders: Patient edition, SCIDI/P. Biometrics; New York, NY: 1995. [Google Scholar]
- 106.Fichter MM, Quadflieg N. The structured interview for anorexic and bulimic disorders for DSM-IV and ICD-10 (SIAB-EX): Reliability and validity. Eur Psychiatry. 2001;16:38–48. doi: 10.1016/s0924-9338(00)00534-4. [DOI] [PubMed] [Google Scholar]
- 107.Gormally J, Black S, Datson S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 108.Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: Psychometric features and clinical correlates. Psychol Med. 1982;12:871–878. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- 109.Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol Assess. 2000;12:123–131. doi: 10.1037//1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- 110.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- 111.Spitzer RL, Devlin M, Walsh BT, et al. Binge eating disorder: A multisite field trial of the diagnostic criteria. Int J Eat Disord. 1992;11:191–203. [Google Scholar]
- 112.Latner JD, Mond JM, Kelly MC, Haynes SN, Hay PJ. The Loss of Control Over Eating Scale: Development and psychometric evaluation. Int J Eat Disord. 2014;47:647–659. doi: 10.1002/eat.22296. [DOI] [PubMed] [Google Scholar]
- 113.Blomquist KK, Roberto CA, Barnes RD, White MA, Masheb RM, Grilo CM. Development and validation of the eating loss of control scale. Psychol Assess. 2014;26:77–89. doi: 10.1037/a0034729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Johnson WG, Boutelle KN, Torgrud L, Davig JP, Turner S. What is a binge? The influence of amount, duration, and loss of control criteria on judgments of binge eating. Int J Eat Disord. 2000;27:471–479. doi: 10.1002/(sici)1098-108x(200005)27:4<471::aid-eat13>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 115.Latner JD, Vallance JK, Buckett G. Health-related quality of life in women with eating disorders: association with subjective and objective binge eating. J Clin Psychol Med Settings. 2008;15:148–153. doi: 10.1007/s10880-008-9111-1. [DOI] [PubMed] [Google Scholar]
- 116.Pratt EM, Niego SH, Agras WS. Does the size of a binge matter? Int J Eat Disord. 1998;24:307–312. doi: 10.1002/(sici)1098-108x(199811)24:3<307::aid-eat8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 117.Berg KC, Peterson CB, Crosby RD, et al. Relationship between daily affect and overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Psychiatry Res. 2014;215:185–191. doi: 10.1016/j.psychres.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Goossens L, Braet C, Van Vlierberghe L, Mels S. Weight parameters and pathological eating as predictors of obesity treatment outcome in children and adolescents. Eat Behav. 2009;10:71–73. doi: 10.1016/j.eatbeh.2008.10.008. [DOI] [PubMed] [Google Scholar]