Abstract
Obesity has been increasing worldwide. Data on obesity status among men of reproductive age are scarce. This study aimed to assess the national prevalence and trend of overweight and obesity among reproductive-age men in rural China. In the nationwide population-based study, data were obtained from the National Free Preconception Health Examination Project in rural China from 2010 to 2014. Weight and height were measured in 16 161 982 men aged 15–49 years and their female partners (15 997 739 participants aged 15–49 years) before conception, and body mass index (BMI) was calculated. We found that the prevalence of combined overweight and obesity among men was 33.8% (33.7–33.9%) according to Chinese criteria (BMI ≥ 24.0 kg/m2), the corresponding rates of obesity were 6.3% (6.2–6.4%; BMI ≥ 28.0 kg/m2), respectively. The prevalence varied in different ethnic groups, geographic regions, age, education and GDP levels, and increasing trend was observed over the 5-year study period. In addition, 45.8% of couples had at least one of them as overweight or obesity. About one third of men aged 15–49 years before conception in rural China are overweight or obese. Overweight/obesity clusters in families, which highlights the importance of family involvement of early prevention of obesity in China.
Introduction
Obesity prevalence has increased dramatically over the past several decades, and the global estimate suggests that more than one-third of adults are overweight or obese1. Overweight and obesity are well-established risk factors for diabetes, cardiovascular disease (CVD), certain cancers and premature death, as well as adverse reproductive consequences2–5. Studies have documented that maternal obesity is associated with an increased risk of infertility, pregnancy complications, and chronic diseases in the offspring6. However, whether paternal obesity has an effect on the pregnancy outcomes and long-term health of their children remains to be explored. Several studies have shown that male obesity is related to higher risk of infertility, and accumulating evidence also indicates the importance of paternal obesity in programming offspring obesity/metabolic phenotype through epigenetic modifications at the very early stage, even before conception7–9.
Substantial variability exists across the globe in the prevalence of overweight and obesity in men of reproductive age1. In the US, about two thirds of men aged 20–39 years were overweight or obese in 2012, although the prevalence remained stable in recent years10. A previous small-scale study reported that the prevalence of overweight and obesity in China tripled from 8.2% to 26.5% among men aged 18–39 years between 1993 and 200911. For better assessing the paternal risks and improving pregnancy outcomes, it is critical to examine weight status of reproductive-age men before conception; however, relevant data are scarce. The purpose of this study is to provide the most recent national estimates of overweight and obesity among reproductive-age men before conception in rural China and to analyze the trends between 2010 and 2014. Data are based on measured values of weight and height from the National Free Preconception Health Examination Project (NFPHEP) database, a mega cohort of more than 15 million couples.
Results
The detailed demographic characteristic of reproductive-age men across study years are shown in Table 1. Based on data for 16 161 982 men aged 15–49 years in rural China, the numbers of participants were almost equally distributed in the three age groups (15–29, 30–39, and 40–49 years), and majority of them (61.9%) had an education level of junior high school, while only 13.4% had college or higher degrees. Among their female partner (See Supplementary Table S1), the majority of women (77.8%) were younger than 30 years old, and other characteristics of women were similar to that of men.
Table 1.
Sample sizes and weighted proportion of demographic characteristics of reproductive-age men in rural China between 2010 and 2014a.
| 2010 | 2011 | 2012 | 2013 | 2014 | Total | |
|---|---|---|---|---|---|---|
| Total | 308 383 | 928 606 | 3 656 639 | 5 848 388 | 5 419 966 | 16 161 982 |
| Age groups | ||||||
| 15–29 | 37.9 | 40.1 | 33.4 | 34.7 | 31.7 | 33.9 |
| 30–39 | 34.0 | 32.2 | 31.1 | 31.8 | 32.7 | 32.0 |
| 40–49 | 28.1 | 27.7 | 35.5 | 33.5 | 35.6 | 34.1 |
| Ethnic origin | ||||||
| Han | 96.6 | 91.6 | 89.7 | 90.8 | 91.1 | 90.8 |
| Uyghur | — | 3.5 | 2.6 | 2.4 | 2.0 | 2.3 |
| Zhuang | 1.7 | 1.2 | 1.9 | 1.8 | 1.8 | 1.8 |
| Miao | 0.2 | 0.8 | 1.2 | 0.9 | 1.1 | 1.0 |
| Manchu | 0.1 | 1.0 | 0.6 | 0.7 | 0.6 | 0.6 |
| Mongol | — | 0.6 | 0.7 | 0.6 | 0.5 | .06 |
| Yi | 1.1 | 0.7 | 0.4 | 0.5 | 0.6 | 0.5 |
| Hui | 0.2 | 0.3 | 1.3 | 1.2 | 1.2 | 1.1 |
| Tujia | — | 0.3 | 1.2 | 0.8 | 0.8 | 0.8 |
| Tibetan | 0.2 | 0.1 | 0.4 | 0.5 | 0.4 | 0.4 |
| Region | ||||||
| North | 12.1 | 22.1 | 10.3 | 11.5 | 11.9 | 12.1 |
| Northeast | 4.1 | 7.3 | 11.0 | 12.6 | 13.7 | 12.0 |
| East | 19.7 | 25.5 | 20.1 | 23.7 | 24.3 | 23.1 |
| Central | 13.0 | 13.0 | 18.7 | 16.7 | 15.5 | 16.4 |
| South | 17.0 | 7.0 | 9.5 | 11.7 | 10.0 | 10.4 |
| Northwest | 20.6 | 13.9 | 10.4 | 9.2 | 8.5 | 9.9 |
| Southwest | 19.7 | 11.2 | 19.9 | 14.6 | 16.1 | 16.2 |
| Education | ||||||
| Primary school or below | 7.7 | 7.3 | 10.3 | 8.9 | 8.2 | 8.9 |
| Junior high school | 64.6 | 64.5 | 63.4 | 61.8 | 60.0 | 61.9 |
| High school | 18.7 | 17.2 | 15.8 | 15.4 | 15.7 | 15.8 |
| College or higher | 9.0 | 10.9 | 10.4 | 14.0 | 16.1 | 13.4 |
| GDP level | ||||||
| Tertitle 1 | 46.6 | 48.9 | 45.0 | 40.2 | 42.2 | 42.9 |
| Tertitle 2 | 19.6 | 21.5 | 28.8 | 30.7 | 30.7 | 29.2 |
| Tertitle 3 | 33.8 | 29.6 | 26.2 | 29.1 | 27.1 | 27.9 |
aThe data are shown as percentage of participants in each year, and all proportion estimates were weighted using the China Population Census in 2010.
The overall prevalence (95% CI) of combined overweight and obesity was 33.6% (33.5–33.7%) among reproductive-age men, and the prevalence of obesity alone was 6.3% (6.2–6.4%) according to the Chinese criteria (Table 2). The prevalence of overweight and obesity was higher among men in the 30–39 and 40–49 years age group compared to those aged 15–29 years. Among our participants, the minority ethnic groups of Mongolian (43.7%) and Manchu (43.0%) had substantially higher rates of overweight and obesity than do Han ethnic group (34.0%). The prevalence varied dramatically across regions, and it was highest in the north region (43.5%), and lowest in the south (24.8%) or northwest (25.9%) regions. The prevalence increased monotonically with higher education and GDP levels. The prevalence (95% CI) according to the WHO criteria was 22.4% (22.3–22.5%) for combined overweight and obesity, and 2.5% (2.4–2.6%) for obesity (See Supplementary Table S2). The overall and the sociodemographic profiles were similar to that based on the Chinese criteria.
Table 2.
Prevalence of overweight and obesity for reproductive-age men aged 15–49 years in rural China, 2010–2014a.
| Overweight and obesity | Obesity | |||||
|---|---|---|---|---|---|---|
| Prevalence | Crude OR (95%CI) | Adjusted OR (95%CI)b | Prevalence | Crude OR (95%CI) | Adjusted OR (95%CI)b | |
| Total | 33.6 (33.5–33.7) | 6.3 (6.2–6.4) | ||||
| Age groups | ||||||
| 15–29 | 26.9 (26.8–27.0) | 1.00 | 1.00 | 5.4 (5.3–5.5) | 1.00 | 1.00 |
| 30–39 | 37.2 (37.1–37.2) | 1.61 (1.60–1.62) | 1.63 (1.62–1.64) | 7.4 (7.3–7.5) | 1.42 (1.41–1.43) | 1.42 (1.41–1.44) |
| 40–49 | 37.0 (36.6–37.0) | 1.58 (1.57–1.60) | 1.69 (1.67–1.71) | 6.1 (6.0–6.2) | 1.14 (1.12–1.16) | 1.21 (1.18–1.23) |
| Ethnic origin | ||||||
| Han | 34.0 (33.9–34.1) | 1.00 | 1.00 | 6.4 (6.3–6.5) | 1.00 | 1.00 |
| Uyghur | 33.0 (32.7–33.4) | 0.96 (0.94–0.97) | 1.52 (1.50–1.55) | 5.2 (5.0–5.4) | 0.80 (0.78–0.83) | 1.51 (1.46–1.57) |
| Zhuang | 21.5 (21.1–21.8) | 0.53 (0.52–0.54) | 0.65 (0.63–0.66) | 2.8 (2.6–2.9) | 0.42 (0.40–0.44) | 0.60 (0.57–0.63) |
| Miao | 25.0 (24.4–25.5) | 0.65 (0.63–0.66) | 0.93 (0.91–0.96) | 3.1 (2.9–3.3) | 0.47 (0.43–0.50) | 0.77 (0.72–0.83) |
| Manchu | 43.0 (42.1–43.8) | 1.46 (1.41–1.51) | 1.05 (1.01–1.09) | 8.8 (8.3–9.2) | 1.40 (1.33–1.49) | 1.06 (0.99–1.12) |
| Mongol | 43.7 (42.9–44.4) | 1.50 (1.46–1.55) | 1.11 (1.08–1.15) | 9.6 (9.2–10.0) | 1.55 (1.48–1.62) | 1.13 (1.08–1.19) |
| Yi | 23.0 (22.3–23.7) | 0.58 (0.56–0.60) | 1.04 (0.99–1.08) | 3.9 (3.6–4.2) | 0.59 (0.54–0.64) | 1.26 (1.16–1.38) |
| Hui | 28.6 (28.0–29.2) | 0.78 (0.76–0.80) | 1.15 (1.11–1.18) | 5.9 (5.5–6.2) | 0.91 (0.86–0.97) | 1.40 (1.32–1.50) |
| Tujia | 26.3 (25.7–26.9) | 0.69 (0.67–0.71) | 0.81 (0.78–0.84) | 3.3 (3.0–3.5) | 0.49 (0.46–0.53) | 0.66 (0.61–0.71) |
| Tibetan | 23.5 (22.5–24.6) | 0.60 (0.56–0.63) | 1.07 (1.01–1.14) | 3.7 (3.1–4.3) | 0.56 (0.47–0.66) | 1.23 (1.04–1.46) |
| Region | ||||||
| North | 43.5 (43.2–43.8) | 2.34 (2.30–2.37) | 3.03 (2.98–3.08) | 9.8 (9.6–10.0) | 2.71 (2.64–2.78) | 3.56 (3.47–3.66) |
| Northeast | 40.5 (40.2–40.8) | 2.07 (2.04–2.10) | 2.38 (2.34–2.41) | 7.4 (7.3–7.6) | 1.99 (1.94–2.05) | 2.48 (2.41–2.56) |
| East | 38.9 (38.7–39.0) | 1.93 (1.91–1.95) | 2.06 (2.04–2.09) | 8.3 (8.2–8.4) | 2.27 (2.22–2.32) | 2.34 (2.29–2.39) |
| Central | 29.2 (29.1–29.3) | 1.25 (1.24–1.27) | 1.39 (1.37–1.40) | 4.5 (4.4–4.6) | 1.18 (1.16–1.21) | 1.29 (1.26–1.31) |
| South | 24.8 (24.6–24.9) | 1.00 | 1.00 | 3.9 (3.8–4.0) | 1.00 | 1.00 |
| Northwest | 25.9 (25.7–26.0) | 1.06 (1.05–1.07) | 1.54 (1.52–1.57) | 3.8 (3.7–3.9) | 0.98 (0.96–1.01) | 1.49 (1.45–1.54) |
| Southwest | 28.2 (28.1–28.4) | 1.20 (1.18–1.21) | 1.50 (1.48–1.52) | 4.6 (4.5–4.7) | 1.19 (1.16–1.22) | 1.59 (1.55–1.63) |
| Education | ||||||
| Primary school or below | 28.5 (28.2–28.7) | 1.00 | 1.00 | 4.8 (4.7–4.9) | 1.00 | 1.00 |
| Junior high school | 32.2 (32.1–32.3) | 1.19 (1.18–1.21) | 1.10 (1.09–1.12) | 5.7 (5.6–5.8) | 1.19 (1.15–1.23) | 0.97 (0.94–1.01) |
| High school | 34.7 (34.5–34.9) | 1.34 (1.32–1.36) | 1.31 (1.29–1.33) | 7.1 (7.0–7.2) | 1.51 (1.45–1.56) | 1.27 (1.22–1.31) |
| College or higher | 41.9 (41.6–42.1) | 1.81 (1.78–1.84) | 1.67 (1.64–1.70) | 9.1 (8.9–9.2) | 1.98 (1.91–2.06) | 1.56 (1.50–1.62) |
| GDP level | ||||||
| Tertitle 1 | 32.2 (32.1–32.3) | 1.00 | 1.00 | 5.9 (5.8–6.0) | 1.00 | 1.00 |
| Tertitle 2 | 33.4 (33.2–33.5) | 1.05 (1.04–1.06) | 0.94 (0.93–0.95) | 5.8 (5.7–5.9) | 0.99 (0.98–1.01) | 0.89 (0.88–0.91) |
| Tertitle 3 | 35.8 (35.7–35.9) | 1.17 (1.16–1.18) | 1.11 (1.10–1.12) | 7.3 (7.3–7.4) | 1.28 (1.26–1.29) | 1.20 (1.18–1.21) |
OR, odds ratio; CI, confidence interval. aData are shown as prevalence (95% confidence interval), and all estimates were weighted using the China Population Census in 2010. Overweight and obesity were defined according to the Chinese criteria: overweight, 24.0 ≤ BMI ≤ 27.9 kg/m2 and obesity, BMI ≥ 28.0 kg/m2. bAdjusted for all other factors in the table.
During the study period, the overall prevalence increased by 8.9% (95% CI 8.6–9.2%) for combined overweight and obesity, and 2.7% (95% CI 2.6–2.9%) for obesity alone defined by the Chinese criteria (all P < 0.0001; Fig. 1 and Table 3). The increase was present in almost all subgroups, although substantial disparities were observed (Table 3). Greater increases in overweight and obesity were observed in men aged 30 years or above, with Han background, with higher education, or in the high GDP region. In addition, the increases were significantly faster in regions of north, northeast, south and northwest. According to the WHO criteria, the prevalence increased by 7.6% (95% CI 7.3–7.8%) for combined overweight and obesity, and 1.1% (95% CI 1.0–1.2%) for obesity alone (See Supplementary Table S2). Information on the prevalence and trend of overweight and obesity in 31 provinces, municipalities and autonomous regions during 2010 and 2014 is shown in Fig. 2A. Again, substantial variations were observed across different regions in China.
Figure 1.
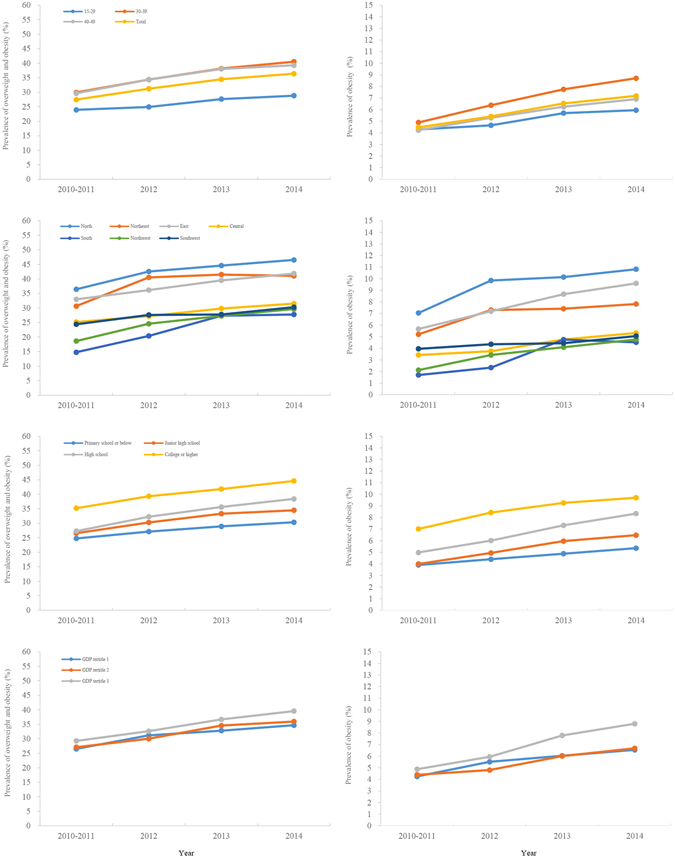
Prevalence and overweight and obesity among men aged 15–49 years by demographic variables, 2010–2014. Overweight and obesity were defined according to the Chinese criteria: overweight, 24.0 ≤ BMI ≤ 27.9 kg/m2 and obesity, BMI ≥ 28.0 kg/m2.
Table 3.
Trends in prevalence of overweight and obesity among reproductive-age men aged 15–49 years in rural China, 2010–2014a.
| Overweight and obesity | Obesity | |||||||
|---|---|---|---|---|---|---|---|---|
| 2010–2011 | 2014 | Change 2010–2011 to 2014, point (95% CI) | p value | 2010–2011 | 2014 | Change 2010–2011 to 2014, point (95% CI) | p value | |
| Total | 27.5 (27.2–27.7) | 36.4 (36.2–36.5) | 8.9 (8.6–9.2) | <0.0001 | 4.5 (4.3–4.6) | 7.2 (7.1–7.3) | 2.7 (2.6–2.9) | <0.0001 |
| Age groups | ||||||||
| 15–29 | 23.9 (23.6–24.2) | 28.8 (28.7–28.9) | 4.9 (4.5–5.2) | <0.0001 | 4.3 (4.1–4.5) | 6.0 (5.9–6.1) | 1.7 (1.5–1.8) | <0.0001 |
| 30–39 | 29.9 (29.6–30.2) | 40.5 (40.4–40.7) | 10.6 (10.3–10.9) | <0.0001 | 4.9 (4.7–5.1) | 8.7 (8.6–8.8) | 3.8 (3.6–4.0) | <0.0001 |
| 40–49 | 29.6 (28.8–30.4) | 39.3 (39.0–39.7) | 9.7 (8.8–10.5) | <0.0001 | 4.2 (3.9–4.6) | 6.9 (6.7–7.1) | 2.7 (2.3–3.1) | <0.0001 |
| Ethnic origin | ||||||||
| Han | 27.4 (27.1–27.7) | 37.1 (37.0–37.3) | 8.3 (8.0–8.5) | <0.0001 | 4.5 (4.4–4.6) | 7.4 (7.3–7.5) | 1.2 (1.1–1.3) | <0.0001 |
| Uyghur | 29.1 (28.0–30.3) | 35.6 (35.0–36.3) | 3.7 (2.6–4.9) | <0.0001 | 4.7 (4.2–5.3) | 6.0 (5.6–6.4) | 0.5 (0.3–0.7) | <0.0001 |
| Zhuang | 15.0 (13.8–16.3) | 22.9 (22.3–23.6) | 7.7 (6.9–8.6) | <0.0001 | 1.1 (0.8–1.3) | 2.8 (2.6–3.1) | 0.5 (0.3–0.7) | <0.0001 |
| Miao | 19.8 (18.1–21.7) | 26.6 (25.7–27.5) | 3.6 (1.9–5.3) | <0.0001 | 3.3 (2.5–4.3) | 3.7 (3.3–4.1) | 0.2 (−0.3–0.7) | 0.376 |
| Manchu | 39.4 (37.0–41.7) | 43.4 (41.9–44.9) | 5.0 (2.6–7.4) | <0.0001 | 5.8 (4.8–7.0) | 9.6 (8.8–10.6) | 1.5 (0.6–2.3) | 0.001 |
| Mongol | 35.9 (33.1–38.8) | 45.1 (43.8–46.4) | 6.4 (3.4–9.4) | <0.0001 | 8.7 (6.8–11.0) | 10.1 (9.4–10.8) | 0.7 (−0.9–2.3) | 0.395 |
| Yi | 19.8 (18.3–21.3) | 25.0 (23.9–26.1) | 3.5 (2.0–5.2) | <0.0001 | 2.5 (2.1–2.9) | 4.7 (4.2–5.3) | 0.4 (0–0.8) | 0.045 |
| Hui | 37.0 (30.2–44.2) | 28.1 (27.2–29.0) | −5.1 (−1.3–2.3) | 0.176 | 6.6 (5.1–8.6) | 6.2 (5.7–6.7) | −0.2 (−1.2–0.8) | 0.671 |
| Tujia | 26.3 (23.2–30.0) | 27.9 (26.7–29.0) | 2.1 (−0.7–4.8) | 0.136 | 3.9 (2.6–5.8) | 3.7 (3.3–4.1) | 0.2 (−0.6–1.1) | 0.579 |
| Tibetan | 14.8 (11.8–18.4) | 25.3 (23.5–27.1) | 6.8 (3.7–9.8) | <0.0001 | 1.5 (0.9–2.8) | 4.2 (3.2–5.5) | 0.8 (0–1.5) | 0.054 |
| Region | ||||||||
| North | 36.4 (35.4–37.5) | 46.5 (46.0–47.0) | 10.1 (8.9–11.2) | <0.0001 | 7.0 (6.5–7.6) | 10.8 (10.5–11.1) | 3.8 (3.2–4.4) | <0.0001 |
| Northeast | 30.6 (29.7–31.6) | 41.0 (40.5–41.5) | 10.4 (9.3–11.5) | <0.0001 | 5.2 (4.8–5.7) | 7.8 (7.6–8.1) | 2.6 (2.1–3.1) | <0.0001 |
| East | 33.0 (32.4–33.6) | 41.8 (41.5–42.2) | 8.8 (8.2–9.5) | <0.0001 | 5.7 (5.4–5.9) | 9.6 (9.4–9.8) | 3.9 (3.6–4.3) | <0.0001 |
| Central | 25.2 (24.9–25.5) | 31.5(31.3–31.7) | 6.3 (5.9–6.7) | <0.0001 | 3.4 (3.3–3.6) | 5.3 (5.2–5.4) | 1.9 (1.7–2.1) | <0.0001 |
| South | 14.8 (14.4–15.2) | 27.8 (27.5–28.0) | 13.0 (12.5–13.5) | <0.0001 | 1.7 (1.6–1.9) | 4.5 (4.4–4.6) | 2.8 (2.6–3.0) | <0.0001 |
| Northwest | 18.6 (18.2–19.1) | 29.6 (29.3–30.0) | 11.0 (10.4–11.6) | <0.0001 | 2.1 (2.0–2.3) | 4.8 (4.6–4.9) | 2.6 (2.4–2.9) | <0.0001 |
| Southwest | 24.4 (23.9–24.9) | 30.3 (30.0–30.6) | 5.9 (5.3–6.5) | <0.0001 | 4.0 (3.7–4.2) | 5.1 (4.9–5.2) | 1.1 (0.8–1.4) | <0.0001 |
| Education | ||||||||
| Primary school or below | 24.8 (23.8–25.7) | 30.3 (29.8–30.8) | 5.6 (4.5–6.6) | <0.0001 | 3.9 (3.4–4.4) | 5.4 (5.1–5.6) | 1.4 (0.9–2.0) | <0.0001 |
| Junior high school | 26.6 (26.2–26.9) | 34.5 (34.3–34.6) | 7.9 (7.5–8.3) | <0.0001 | 4.0 (3.8–4.1) | 6.4 (6.3–6.6) | 2.5 (2.3–2.7) | <0.0001 |
| High school | 27.2 (26.6–27.9) | 38.4 (38.0–38.8) | 11.1 (10.4–11.9) | <0.0001 | 5.0 (4.7–5.3) | 8.3 (8.1–8.5) | 3.4 (3.0–3.7) | <0.0001 |
| College or higher | 35.2(34.3–36.1) | 46.1 (45.7–46.5) | 9.4 (8.4–10.4) | <0.0001 | 7.0 (6.5–7.5) | 9.7 (9.4–10.0) | 2.7 (2.1–3.2) | <0.0001 |
| GDP level | ||||||||
| Tertitle 1 | 26.5 (26.1–27.0) | 34.7 (34.4–34.9) | 8.1 (7.6–8.7) | <0.0001 | 4.3 (4.0–4.5) | 6.5 (6.4–6.7) | 2.3 (2.0–2.5) | <0.0001 |
| Tertitle 2 | 27.1 (26.6–27.6) | 35.9 (35.6–36.2) | 8.9 (8.3–9.4) | <0.0001 | 4.4 (4.2–4.6) | 6.7 (6.5–6.9) | 2.3 (2.0–2.5) | <0.0001 |
| Tertitle 3 | 29.2 (28.8–29.7) | 39.5 (39.3–39.8) | 10.3 (9.8–10.8) | <0.0001 | 4.9 (4.7–5.1) | 8.8 (8.7–8.9) | 3.9 (3.7–4.1) | <0.0001 |
aData are shown as prevalence (95% confidence interval), and all estimates were weighted using the China Population Census in 2010. The sample size in 2010 was relatively small, thus data from 2010 and 2011 were combined. Overweight and obesity were defined according to the Chinese criteria: overweight, 24.0 ≤ BMI ≤ 27.9 kg/m2 and obesity, BMI ≥ 28.0 kg/m2.
Figure 2.
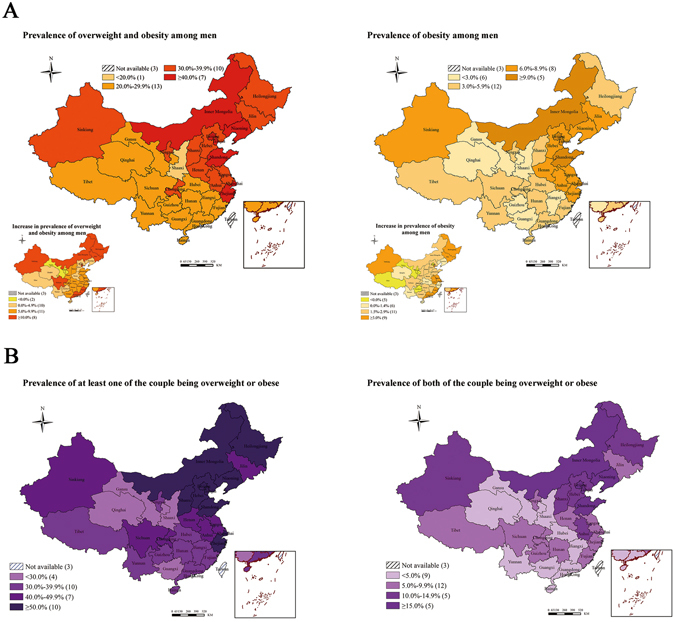
(A) Prevalence and trends in overweight and obesity among reproductive-age men in 31 provinces, municipalities and autonomous regions, 2010–2014; (B) Clustering of overweight and obesity among couples in 31 provinces, municipalities and autonomous regions, 2010–2014. Overweight and obesity were defined according to Chinese criteria: overweight, 24.0 ≤ BMI ≤ 27.9 kg/m2 and obesity, BMI ≥ 28.0 kg/m2; Couples: those with at least one of them being overweight or obese. Figure 2 is created by using the software ArcGIS 10.2 (http://www.esri.com/software/arcgis).
Data from 15 997 739 men and their female partners could be matched in this study. Among them, increasing trends in prevalence of overweight and obesity were observed in both men and women (See Supplementary Fig. S1). During the study years, the proportion of couples with at least one of them being overweight or obese was 45.8%, whereas proportion of couples with both of them being overweight or obesity was 9.9% based on the Chinese criteria (Table 4). The clustering of overweight and/or obesity in couples was stronger in older age groups, particularly in women, and in ethnic groups of Uyghur and Mongolian. Higher education was positively associated with higher prevalence of overweight or obesity in couples, whereas it was inversely associated with simultaneous overweight and obesity in men and women. Positive associations between higher GDP level and couples’ overweight and/or obesity were consistent. Similarly, the prevalence of the clustering overweight/obesity was lower in the south region, and higher in the north region (Table 4). In addition, the prevalence of overweight and/or obesity in couples in 31 provinces, municipalities and autonomous regions is also presented in Fig. 2B.
Table 4.
Clustering of overweight and obesity for reproductive-age couples in rural China, 2010–2014a.
| At least one of the couple being overweight or obese | Both of the couple being overweight or obese | |||||
|---|---|---|---|---|---|---|
| Prevalence | Crude OR (95%CI) | Adjusted OR (95%CI) b | Prevalence | Crude OR (95%CI) | Adjusted OR (95%CI)b | |
| Total | 45.8 (45.7–45.9) | 9.9 (9.8–10.0) | ||||
| Male age groups | ||||||
| 15–29 | 34.0 (33.8–34.2) | 1.00 | 1.00 | 4.9 (4.8–5.0) | 1.00 | 1.00 |
| 30–39 | 51.2 (51.1–51.4) | 2.04 (2.02–2.06) | 1.54 (1.52–1.57) | 11.5 (11.4–11.6) | 2.54 (2.48–2.59) | 1.75 (1.70–1.80) |
| 40–49 | 55.6 (55.3–55.8) | 2.43 (2.40–2.47) | 1.50 (1.47–1.54) | 14.9 (14.7–15.2) | 3.42 (3.34–3.51) | 1.74 (1.67–1.82) |
| Female age groups | ||||||
| 15–29 | 34.4 (34.2–34.6) | 1.00 | 1.00 | 4.9 (4.8–5.0) | 1.00 | 1.00 |
| 30–39 | 52.5 (52.4–52.6) | 2.11 (2.09–2.13) | 1.67 (1.65–1.69) | 12.1 (12.0–12.2) | 2.65 (2.60–2.70) | 2.04 (1.99–2.09) |
| 40–49 | 56.1 (55.8–56.3) | 2.43 (2.39–2.47) | 1.79 (1.75–1.84) | 15.3 (15.1–15.5) | 3.49 (3.40–3.57) | 2.36 (2.27–2.46) |
| Male ethnic origin | ||||||
| Han | 46.8 (46.6–46.9) | 1.00 | 1.00 | 10.1 (10.0–10.2) | 1.00 | 1.00 |
| Uyghur | 40.3 (39.6–41.0) | 0.77 (0.75–0.79) | 1.54 (1.50–1.57) | 9.9 (9.5–10.3) | 0.97 (0.92–1.01) | 2.22 (2.13–2.32) |
| Zhuang | 28.3 (27.6–29.1) | 0.45 (0.43–0.47) | 0.58 (0.56–0.60) | 3.8 (3.6–4.1) | 0.35 (0.33–0.37) | 0.50 (0.47–0.54) |
| Miao | 30.0 (28.3–31.6) | 0.49 (0.45–0.52) | 0.93 (0.89–0.97) | 4.5 (4.1–4.8) | 0.41 (0.38–0.45) | 0.93 (0.86–1.02) |
| Manchu | 61.8 (60.7–62.9) | 1.84 (1.76–1.93) | 1.11 (1.05–1.17) | 16.8 (15.9–17.7) | 1.79 (1.68–1.90) | 0.99 (0.93–1.05) |
| Mongol | 61.0 (59.8–62.1) | 1.78 (1.69–1.86) | 1.38 (1.31–1.44) | 17.5 (16.7–18.3) | 1.88 (1.77–1.99) | 1.40 (1.32–1.49) |
| Yi | 33.0 (31.2–34.9) | 0.56 (0.52–0.61) | 1.04 (0.98–1.12) | 4.6 (4.1–5.2) | 0.43 (0.38–0.48) | 0.92 (0.81–1.05) |
| Hui | 29.3 (28.3–30.2) | 0.47 (0.45–0.49) | 1.19 (1.14–1.24) | 4.8 (4.5–5.3) | 0.45 (0.42–0.49) | 1.42 (1.32–1.52) |
| Tujia | 40.6 (39.5–41.6) | 0.78 (0.78–0.81) | 0.83 (0.79–0.87) | 7.0 (6.5–7.6) | 0.67 (0.62–0.73) | 0.73 (0.67–0.80) |
| Tibetan | 32.1 (30.0–34.3) | 0.54 (0.49–0.59) | 0.93 (0.85–1.02) | 7.2 (6.2–8.4) | 0.69 (0.58–0.82) | 1.25 (1.05–1.50) |
| Female ethnic origin | ||||||
| Han | 46.8 (46.6–46.9) | 1.00 | 1.00 | 10.1 (10.0–10.2) | 1.00 | 1.00 |
| Uyghur | 40.4 (39.6–41.1) | 0.77 (0.75–0.79) | 1.50 (1.41–1.59) | 9.9 (9.5–10.3) | 0.97 (0.93–1.02) | 2.21 (2.01–2.42) |
| Zhuang | 28.9 (28.2–29.6) | 0.46 (0.45–0.48) | 0.62 (0.59–0.65) | 3.8 (3.6–4.1) | 0.35 (0.33–0.37) | 0.51 (0.46–0.55) |
| Miao | 30.2 (28.7–31.8) | 0.49 (0.46–0.53) | 0.89 (0.82–0.96) | 4.7 (4.3–5.1) | 0.44 (0.40–0.48) | 0.85 (0.76–0.94) |
| Manchu | 62.3 (61.2–63.4) | 1.88 (1.79–1.97) | 1.17 (1.11–1.24) | 17.4 (16.4–18.3) | 1.86 (1.74–1.99) | 1.07 (1.00–1.16) |
| Mongol | 61.5 (60.4–62.6) | 1.82 (1.74–1.90) | 1.38 (1.31–1.46) | 17.8 (16.9–18.7) | 1.92 (1.81–2.04) | 1.43 (1.33–1.54) |
| Yi | 33.9 (32.2–35.7) | 0.58 (0.54–0.63) | 1.09 (1.00–1.18) | 5.1 (4.5–5.7) | 0.47 (0.42–0.53) | 0.96 (0.85–1.09) |
| Hui | 29.8 (28.8–30.8) | 0.48 (0.46–0.51) | 0.89 (0.85–0.94) | 5.0 (4.6–5.3) | 0.46 (0.43–0.50) | 0.98 (0.90–1.06) |
| Tujia | 41.1 (40.0–42.2) | 0.79 (0.76–0.83) | 0.87 (0.83–0.92) | 7.1 (6.4–8.5) | 0.68 (0.62–0.74) | 0.75 (0.68–0.82) |
| Tibetan | 32.1 (30.1–34.2) | 0.54 (0.49–0.59) | 0.91 (0.83–1.00) | 7.4 (6.4–8.5) | 0.70 (0.60–0.82) | 1.21 (1.03–1.42) |
| Region | ||||||
| North | 58.5 (58.1–58.9) | 3.05 (2.99–3.11) | 3.78 (3.69–3.85) | 15.2 (14.9–15.4) | 3.78 (3.66–3.91) | 4.68 (4.52–4.85) |
| Northeast | 56.9 (56.5–57.3) | 2.86 (2.81–2.92) | 2.78 (2.71–2.83) | 15.0 (14.7–15.3) | 3.73 (3.60–3.87) | 3.31 (3.19–3.44) |
| East | 51.9 (51.6–52.2) | 2.34 (2.31–2.37) | 2.37 (2.34–2.41) | 11.7 (11.5–11.9) | 2.81 (2.72–2.90) | 2.80 (2.72–2.89) |
| Central | 40.6 (40.4–40.8) | 1.48 (1.46–1.50) | 1.52 (1.50–1.54) | 7.2 (7.1–7.3) | 1.65 (1.60–1.70) | 1.64 (1.59–1.69) |
| South | 31.6 (31.3–31.8) | 1.00 | 1.00 | 4.5 (4.4–4.6) | 1.00 | 1.00 |
| Northwest | 32.1 (31.7–32.4) | 1.02 (1.01–1.04) | 1.54 (1.51–1.57) | 5.9 (5.7–6.0) | 1.33 (1.28–1.38) | 2.05 (1.97–2.14) |
| Southwest | 40.8 (40.4–41.1) | 1.49 (1.47–1.52) | 1.78 (1.74–1.81) | 7.8 (7.6–7.9) | 1.78 (1.72–1.85) | 2.01 (1.93–2.09) |
| Male education | ||||||
| Primary school or below | 42.3 (41.9–42.8) | 1.00 | 1.00 | 9.5 (9.3–9.8) | 1.00 | 1.00 |
| Junior high school | 45.9 (45.7–46.0) | 1.16 (1.13–1.18) | 0.99 (0.96–1.01) | 10.4 (10.3–10.5) | 1.10 (1.06–1.13) | 0.96 (0.93–1.00) |
| High school | 44.7 (44.3–45.0) | 1.10 (1.07–1.13) | 1.02 (0.99–1.05) | 9.1 (8.9–9.3) | 0.95 (0.92–0.99) | 0.98 (0.94–1.03) |
| College or higher | 50.0 (49.7–50.3) | 1.36 (1.33–1.39) | 1.21 (1.17–1.26) | 8.6 (8.4–8.8) | 0.89 (0.86–0.92) | 0.95 (0.89–1.00) |
| Female education | ||||||
| Primary school or below | 43.8 (43.3–44.3) | 1.00 | 1.00 | 10.0 (9.8–10.3) | 1.00 | 1.00 |
| Junior high school | 45.7 (45.5–45.8) | 1.08 (1.06–1.10) | 0.95 (0.93–0.97) | 10.3 (10.2–10.4) | 1.03 (0.99–1.06) | 0.94 (0.91–0.97) |
| High school | 44.6 (44.3–44.9) | 1.03 (1.01–1.06) | 0.96 (0.93–0.99) | 9.0 (8.8–9.2) | 0.89 (0.86–0.92) | 0.94 (0.90–0.99) |
| College or higher | 50.0 (49.7–50.3) | 1.28 (1.26–1.31) | 1.10 (1.07–1.14) | 8.6 (8.4–8.7) | 0.84 (0.81–0.87) | 0.88 (0.84–0.94) |
| GDP level | ||||||
| Tertitle 1 | 43.5 (43.3–43.7) | 1.00 | 1.00 | 9.4 (9.3–9.5) | 1.00 | 1.00 |
| Tertitle 2 | 47.7 (47.4–47.9) | 1.18 (1.17–1.20) | 0.99 (0.97–1.00) | 10.6 (10.4–10.7) | 1.14 (1.11–1.17) | 0.94 (0.92–0.96) |
| Tertitle 3 | 47.6 (47.4–47.8) | 1.18 (1.17–1.19) | 1.14 (1.12–1.15) | 10.3 (10.1–10.4) | 1.10 (1.08–1.13) | 1.19 (1.17–1.22) |
OR, odds ratio; CI, confidence interval. aData are shown as prevalence (95% confidence interval), and all estimates were weighted using the China Population Census in 2010. Overweight and obesity were defined according to the Chinese criteria: overweight, 24.0 ≤ BMI ≤ 27.9 kg/m2 and obesity, BMI ≥ 28.0 kg/m2. bAdjusted for all other factors in the table.
Discussion
In this largest study to date in rural China, about one third of reproductive-age men aged 15–49 years were overweight/obese and 6.3% of them were obese according to the Chinese criteria. By examining patterns of reginal difference, overweight and obesity prevalence was substantial high in North China, and was low in the south or northwest regions. Of particular relevance is the ethnicity and cultural differences in rural China. The increase trend of overweight and obesity was common in young men, especially among those in higher socioeconomic strata. These findings indicate that the epidemic of overweight and obesity has become a serious public problem among reproductive-age men in rural China.
The weight status in Chinese populations have been examined in general population by a few national surveys. The China National Nutrition and Health Survey (CNNHS) reported that the prevalence of overweight and obesity (BMI ≥ 24.0 kg/m2) in men aged 18–44 years rose rapidly from 14.5% to 30.4% between 1992 and 200212. The annual increasing rate was much higher in younger men aged 18–44 years (1.6% per year) compared with men aged 45–59 years (1.0% per year) and those aged 60 years or above (0.6% per year). A series of China Health and Nutrition Survey (CHNS) studies found that the proportions of men with a BMI ≥ 25 kg/m2 has tripled from 8.2% to 26.5% in the age group of 18–39 years between 1993 and 2009, and the increase was larger than other age groups or in women11. In Western countries, the prevalence of overweight/obesity remained high in young men of reproductive age: 62% in US10, 56.1% in Canada13, and 42% in England14. Comparing with these findings, our results (33.8% according to the Chinese criteria and 22.4% according to the WHO criteria) were lower than that in Western countries, but were generally consistent with results from other smaller studies in Chinese populations.
In the analysis of different geographical regions, the north and northeast were associated with high prevalence of overweight and obesity in rural China. Some provinces even had a high prevalence close to that in the US (two thirds of the total young men)10. Among our participants, several minority ethnic groups (eg. 43.7% for Mongolian and 43.0% for Manchu) have substantially higher rates of overweight and obesity than do Han ethnic group (34.0%). These reginal/ethnic variations could be attributed to the socioeconomic status and the accompanying lifestyle/culture influence, as well as different genetic backgrounds3. People from rural regions are experiencing the nutrition transition towards a high-fat, high-energy diet, and sedentary lifestyles15. Particularly for some minority ethnic groups, such as Mongolian and Manchu, those who mainly live in regions of north and northeast maintain a traditional meat dietary pattern for the reasons of favoring a large body and need against the cold16. Previous evidence also suggests that people living in the north, rural areas consumed more alcohol beverage than their counterparts, and some minority ethnic groups, such as those of Mongolian background, had higher levels of alcohol consumption than other ethnic groups17. Additionally, socioeconomic status (eg. personal educational level, area-level economic status) impacts the prevalence of overweight and obesity that men of higher social strata are more likely to be obese in developing countries18. In our study, the conclusions were consistent that overweight/obesity prevalence was relatively higher among rural men with higher level of education or living in the high GDP areas. Furthermore, there is a clear distinction regarding to genetic predisposition on obesity in different Chinese populations; the characteristics of gut microbiota in Han population are different from minority ethnic groups, which plays an important role in obesity epidemic19, 20. In short, rates of overweight/obesity have increased among rural people of all ages and regions, but some groups are disproportionately affected. Along with the rapid social and economic change with increasing urbanization, the growing burden of overweight and obesity will affect more reproductive-age men across China in the near future.
Both paternal and maternal obesity are related to the health of the next generation5. Maternal prepregnancy overweight/obesity was associated with adverse pregnancy outcomes21, 22. Male obesity also negatively impacts fertility by changes in the hormones, reduced semen functions, as well as changes in sperm epigenetic marks23. Therefore, it is important to assess the clustering of overweight and obesity couples. In our study, nearly half of rural couples had at least one of them being overweight or obese before conception, and higher prevalence was associated with increasing age, higher socioeconomic strata, specific ethnicity and regions. Meanwhile, about 10% of the couples were overweight or obesity in both of them, and those couples should be prioritized for the interventions. Obesity intervention prior to conception offers unique opportunity for improving pregnancy outcomes, offspring health and also parental health. Overweight/obese couples may share common factors including diet, physical activities and health behaviors, and intervention targeting both couples has been proved more effective than targeting men or women alone24, 25. There is an urgent need for more studies on effective and cost-effective methods of preconception care with an emphasize on weight management, which has been overlooked to a great extent in our society.
Our study has several strengths. First, we included more than 15 million rural men aged 15–49 years in this mega national survey. The study sample covered 80% of the target population in the rural China for couples who intended to get pregnant soon. In addition, we have used a two-stage stratified cluster sampling method and standardized the results to the 2010 China Population Census. Therefore, we considered the results to be representative of actual prevalence of overweight and obesity in reproductive-age men in rural China. Moreover, we utilized the data from couples to examine the distribution of both spouse’s BMI in a general healthy population planning pregnancy. Few studies have analyzed the BMI distribution of a family, while this is certainly important for pregnancy and health of the next generation. We also acknowledge the following limitations of our study. First, our findings are based on a non-random sampling method of 31 provinces, municipalities and autonomous regions, thus the generalization to the entire male population of 15–49 years old in rural China should be cautious. However, due to the very high coverage proportion, we did not think that the results will be materially changed if random sample or total population approaches were used. Second, the majority of men in this study were from rural areas, and the true prevalence of overweight and obesity could be underestimated in the total population because the overweight/obesity prevalence seemed to be slightly higher in urban areas than rural areas in China12, 26, 27. Finally, between-investigator variations in the measurement of body weight and height were possible. However, all study staff (doctors, nurses, and health workers) were adequately trained in standard protocol and the measurement errors could be random, if exist. Given the large sample size, it is unlikely that measure errors could have substantially altered the results.
In conclusion, our study found that about one-third of Chinese young men of reproductive age in rural areas were overweight or obese, and we also observed an increasing trend in the prevalence across the study years. Substantial disparities across geographic regions were observed in the prevalence of overweight and obesity. Further studies are needed to explore the reasons for the disparities, and region-specific health resources and public policies should also be explored to reduce the disease burden of overweight and obesity. In addition, about 45% of couples had at least one of them being overweight or obesity, which will have an enormous impact on the population health of the adults themselves and also the health for the next generation in China. Therefore, effective weight loss strategies are needed for the couples who plan to get pregnant in order to reduce pregnancy complications and improve overall population health.
Methods
Study design and participants
The NFPHEP, launched by National Health and Family Planning Commission and Finance Ministry, is an ongoing preconception care service for rural couples of reproductive age planning pregnancy across China since 2010. The couples who were planning pregnancy within the next 6 months, at least one of whom was defined as a rural resident were eligible for participating in the project. Participants received preconception care including free health checkups, risk assessments and health consultations, as well as two follow-ups for pregnancy outcomes, with the purpose of reducing the potential risk factors for birth defects and improving population health. The NFPHEP began with 100 rural counties in 2010, and extended to 220 rural counties in 2011 and were further extended to 2790 counties of 31 provinces in 2013 afterwards. Before 2013, the numbers of NFPHEP unit were selected in proportion to the local population size and numbers of total counties in each province with a two-stage stratified cluster sampling method. Since NFPHEP is a free healthcare program aiming to improve pregnancy outcomes and reduce birth defects, and women voluntarily came to get the services. Details of the study design, process and data collection are published elsewhere28. In our study, a total of 17 269 054 men who participated in the program between 2010 and 2014 were included in this study. We excluded 289 049 participants aged beyond 20–49 years, 818 023 without physical examination information on weight and height. Finally, data from 16 161 982 of the participants aged between 15 and 49 years were used for statistical analyses. Also we included 15 997 739 female partners, who aged 15–49 years and had complete height and weight information. The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committees of the National Health and Family Planning Commission and National Research Institute for Family Planning. Informed consent in Chinese was obtained from all participants before any data collection.
Data Collection
Data from 31 provinces, municipalities and autonomous regions between 2010 and 2014 were included. During the physical examination, weight and height were measured after participants had removed shoes and heavy clothes. Height (measured to nearest 0.1 cm) and weight (measured to the nearest 0.1 kg) were measured by trained personnel using standardized equipment and protocol provided by the National Research Institute for Family Planning. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and rounded to the nearest tenth. All participants also filled in a standard questionnaire to provide basic demographic information including age, education level and residence address through a face-to-face interview by trained local health staff.
The participants with missing information on height or weight or extreme or implausible BMI values were all excluded in this study. Overweight and obesity were defined according to the Chinese definitions [overweight: BMI 24.0–27.9 kg/m2; obesity: BMI ≥ 28.0 kg/m2] and WHO definitions [overweight: BMI 25.0–29.9 kg/m2; obesity: BMI ≥ 30.0 kg/m2], respectively29, 30. Individuals were grouped by age: 15–29, 30–39 and 40–49 years. The geographical locations were classified as North China (Beijing, Hebei, Inner Mongolia, Shanxi, Tianjin), Northeast China (Heilongjiang, Jilin, Liaoning), East China (Anhui, Fujian, Jiangsu, Jiangxi, Shandong, Shanghai, Zhejiang), Central China (Henan, Hubei, Hunan), South China (Guangdong, Guangxi, Hainan), Northwest China (Gansu, Ningxia, Qianghai, Shaanxi, Sinkiang) and Southwest China (Guizhou, Sichuan, Tibet, Yunnan, Chongqing). Education levels were divided into four groups of primary school or lower, junior high school, high school, and college or above. Economic development was divided into tertiles of gross domestic product (GDP) per head in 2013 with the following ranges: 0.2–3.4, 3.5–4.3, and 4.4–10.0 (CNY10 000), respectively.
Statistical Analysis
All analyses took into account the deviations in the NFPHEP sample compared with the standard population of 2010 China Population Census, using the weight coefficients adjusted for age for every one year and geographical region. Standard errors were estimated with Taylor series linearization method. The adjusted prevalence of overweight and obesity and 95% confidence intervals (CIs) were reported in total and by age, region, education and GDP subgroups. Differences within sociodemographic subgroups were tested by χ² test. Then, we analyzed the trends and absolute changes in prevalence of overweight and obesity from 2010 to 2014 using t statistics and orthogonal contrast matrices, and reported the p value for trends. We further reported the clustering of overweight/obesity among couples, defined as at least one of them was classified as overweight or obesity, or both of them were overweight or obesity. In addition, multivariable logistic regressions were used to explore the association between relevant covariates (age, geographic location, education level and GDP level) and overweight/obesity, and the crude and adjusted odds ratios (ORs) and 95% CIs were reported. Statistical inference was based on 2-sided test and p value < 0.05. All data analyses involved use of STATA software version 13.0.
Electronic supplementary material
Acknowledgements
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors of this manuscript are thankful for the support of all the investigators and participants who contributed to the National Free Preconception Health Examination Project. This work was supported by The National Key Research and Development Program of China (No. 2016YFC1000307, No. 2016YFC1000307-6) and National Natural Science Foundation of China (No. 81602854).
Author Contributions
X.M. and Y.H. conceived and designed the study. Y.H. acquired, analyzed the data, and drafted the manuscript. Y.H. and A.P. interpreted the results. A.P., Y.W., Y.Y., J.X., Y.Z., D.L. and F.H. provided advice and revised the manuscript. Q.W., H.S., Y.Z., D.Y. and Z.P. provided administrative, technical, or material support for this study. Y.H. and A.P. contributed equally.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Yuan He and An Pan contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-04135-4
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yuan He, Email: heyuan8506@126.com.
An Pan, Email: panan@hust.edu.cn.
Xu Ma, Email: xmgenetic@126.com.
References
- 1.Ng M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nature Reviews Endocrinology. 2013;9:13–27. doi: 10.1038/nrendo.2012.199. [DOI] [PubMed] [Google Scholar]
- 3.Hruby A, Hu FB. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics. 2015;33:673–689. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhaskaran K, et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet. 2014;384:755–765. doi: 10.1016/S0140-6736(14)60892-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane M, Zander-Fox DL, Robker RL, McPherson NO. Peri-conception parental obesity, reproductive health, and transgenerational impacts. Trends in endocrinology and metabolism: TEM. 2015;26:84–90. doi: 10.1016/j.tem.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Aviram A, Hod M, Yogev Y. Maternal obesity: implications for pregnancy outcome and long-term risks-a link to maternal nutrition. International Journal of Gynecology & Obstetrics. 2011;115(Suppl 1):S6–10. doi: 10.1016/S0020-7292(11)60004-0. [DOI] [PubMed] [Google Scholar]
- 7.Ng SF, et al. Chronic high-fat diet in fathers programs beta-cell dysfunction in female rat offspring. Nature. 2010;467:963–966. doi: 10.1038/nature09491. [DOI] [PubMed] [Google Scholar]
- 8.Soubry A, et al. Paternal obesity is associated with IGF2 hypomethylation in newborns: results from a Newborn Epigenetics Study (NEST) cohort. BMC medicine. 2013;11:29. doi: 10.1186/1741-7015-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammoud AO, Gibson M, Peterson CM, Meikle AW, Carrell DT. Impact of male obesity on infertility: a critical review of the current literature. Fertility and sterility. 2008;90:897–904. doi: 10.1016/j.fertnstert.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 10.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xi B, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obesity Reviews. 2012;13:287–296. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Mi J, Shan XY, Wang QJ, Ge KY. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes. 2006;31:177–188. doi: 10.1038/sj.ijo.0803354. [DOI] [PubMed] [Google Scholar]
- 13.Twells LK, Gregory DM, Reddigan J, Midodzi WK. Current and predicted prevalence of obesity in Canada: a trend analysis. CMAJ Open. 2014;2:E18–26. doi: 10.9778/cmajo.20130016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shiue I. Associated social factors of body mass index in adults and the very old in the UK. International Journal of Cardiology. 2013;168:543–545. doi: 10.1016/j.ijcard.2013.01.227. [DOI] [PubMed] [Google Scholar]
- 15.S, J. The Tenth Report of the Chinese National Health and Nutrition Examination Survey—Nutrition and Health Status, 1st ed. Beijing: People’s Medical Publishing House (2008).
- 16.Jianbo Liu HY, Zhang L, et al. [Dietary patterns among adult Uyghur residents in Xinjiang] Chin J Public Health. 2016;32:1212–1218. [Google Scholar]
- 17.J C. Alcohol use in China. Alcohol and Alcoholism. 2003;38:537–542. doi: 10.1093/alcalc/agg111. [DOI] [PubMed] [Google Scholar]
- 18.McLaren L. Socioeconomic status and obesity. Epidemiologic reviews. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 19.von Deneen KM, Wei Q, Tian J, Liu Y. Obesity in China: what are the causes? Current pharmaceutical design. 2011;17:1132–1139. doi: 10.2174/138161211795656765. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, et al. A phylo-functional core of gut microbiota in healthy young Chinese cohorts across lifestyles, geography and ethnicities. The ISME journal. 2015;9:1979–1990. doi: 10.1038/ismej.2015.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu Y, Dai W, Dai X, Li Z. Prepregnancy body mass index and gestational weight gain with the outcome of pregnancy: a 13-year study of 292,568 cases in China. Archives of gynecology and obstetrics. 2012;286:905–911. doi: 10.1007/s00404-012-2403-6. [DOI] [PubMed] [Google Scholar]
- 22.Li N, et al. Maternal prepregnancy body mass index and gestational weight gain on pregnancy outcomes. PloS One. 2013;8:e82310. doi: 10.1371/journal.pone.0082310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Du Plessis SS, Cabler S, McAlister DA, Sabanegh E, Agarwal A. The effect of obesity on sperm disorders and male infertility. Nature reviews. Urology. 2010;7:153–161. doi: 10.1038/nrurol.2010.6. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds K, et al. Prevalence and Risk Factors of Overweight and Obesity in China. Obesity. 2007;15:10–18. doi: 10.1038/oby.2007.527. [DOI] [PubMed] [Google Scholar]
- 25.Liang X, et al. Prevalence of cardiovascular disease risk factors in China: Findings from 2010 China Chronic Disease and Risk Factor Surveillance. Heart. 2012;98:E134–E135. [Google Scholar]
- 26.Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20–45 years (1989–2000) International Journal of Obesity. 2007;31:272–278. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]
- 27.National Health and Family Planning Commission. Chronic disease on rise in China: health survey. http://www.chinadaily.com.cn/m/chinahealth/2015-07/08/content_21224293.htm. (Accessed June 25, 2015).
- 28.Zhang S, Wang Q, Shen H. [Design of the national free proception health examination project in China] Zhonghua Yi Xue Za Zhi. 2015;95:162–165. [PubMed] [Google Scholar]
- 29.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. (World Health Organ Tech Rep Ser. 894, i-xii, 1–253 (2000). [PubMed]
- 30.Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


