Abstract
Objectives
To determine an association between unemployment rates and human immunodeficiency virus (HIV) mortality in the Organisation for Economic Co-operation and Development (OECD).
Design
Multivariate regression analysis.
Participants
OECD member states.
Setting
OECD.
Main outcome measures
World Health Organization HIV mortality.
Results
Between 1981 and 2009, a 1% increase in unemployment was associated with an increase in HIV mortality in the OECD (coefficient for men 0.711, 0.334–1.089, p = 0.0003; coefficient for women 0.166, 0.071–0.260, p = 0.0007). Time lag analysis showed a significant increase in HIV mortality for up to two years after rises in unemployment: p = 0.0008 for men and p = 0.0030 for women in year 1, p = 0.0067 for men and p = 0.0403 for women in year 2.
Conclusions
Rises in unemployment are associated with increased HIV mortality. Economic fiscal policy may impact upon population health. Policy discussions should take into consideration potential health outcomes.
Keywords: HIV, mortality, unemployment, economic recession, austerity
Introduction
The world is facing one of the most severe global recessions in modern history, with rising unemployment levels across a range of countries.1 There are concerns regarding the adverse effect of the prolonged economic recession on population health outcomes. 2
Yet, the prevailing governmental response to this economic downturn, in countries around the world, has been the introduction of austerity measures in an attempt to reduce budget deficits.3 A result of these fiscal policies, in addition to the economic crisis, has been the increased national prevalence of unemployment.4,5 More specifically, the widespread adoption of these austerity policies across the OECD (Organisation for Economic Co-operation and Development) has been associated with an increase in average unemployment rate from 5.6% to 7.6% between 2008 and 2009 (Table 1).1
Table 1.
Unemployment in the OECD, 2006 and 2009.
| Country | Year of OECD membership | 2006 unemployment (% of total labour force) | 2009 unemployment (% of total labour force) | Increase or decrease in unemployment after the economic crisis |
|---|---|---|---|---|
| Australia | 1971 | 4.8 | 5.6 | Increase |
| Austria | 1961 | 4.7 | 4.8 | Increase |
| Belgium | 1961 | 8.2 | 7.9 | Decrease |
| Canada | 1961 | 6.3 | 8.3 | Increase |
| Chilea | 2010 | 7.7 | 9.7 | Increase |
| Czech Republic | 1995 | 7.1 | 6.7 | Decrease |
| Denmark | 1961 | 3.9 | 6.0 | Increase |
| Estoniaa | 2010 | 5.9 | 13.8 | Increase |
| Finland | 1969 | 7.6 | 8.2 | Increase |
| France | 1961 | 8.8 | 9.1 | Increase |
| Germany | 1961 | 10.3 | 7.7 | Decrease |
| Greece | 1961 | 8.9 | 9.5 | Increase |
| Hungary | 1996 | 7.5 | 10.0 | Increase |
| Icelandb | 1961 | 3.0 | 7.2 | Increase |
| Ireland | 1961 | 4.4 | 12.0 | Increase |
| Israela | 2010 | 8.4 | 7.5 | Decrease |
| Italy | 1962 | 6.8 | 7.8 | Increase |
| Japan | 1964 | 4.1 | 5.0 | Increase |
| South Korea | 1996 | 3.4 | 3.6 | Increase |
| Luxembourgb | 1961 | 4.7 | 5.1 | Increase |
| Mexico | 1994 | 3.2 | 5.2 | Increase |
| Netherlands | 1961 | 3.9 | 3.4 | Decrease |
| New Zealand | 1973 | 3.9 | 6.1 | Increase |
| Norway | 1961 | 3.4 | 3.2 | Decrease |
| Poland | 1996 | 13.8 | 8.2 | Decrease |
| Portugal | 1961 | 7.7 | 9.5 | Increase |
| Slovakia | 2000 | 13.3 | 12.1 | Decrease |
| Sloveniaa | 2010 | 6.0 | 5.9 | Decrease |
| Spain | 1961 | 8.5 | 18.0 | Increase |
| Sweden | 1961 | 7.0 | 8.3 | Increase |
| Switzerland | 1961 | 4.0 | 4.1 | Increase |
| Turkeyb | 1961 | 10.2 | 14.0 | Increase |
| United Kingdom | 1961 | 5.4 | 7.7 | Increase |
| United States | 1961 | 4.6 | 9.3 | Increase |
OECD: Organisation for Economic Co-operation and Development.
aChile, Estonia, Israel and Slovenia were excluded from our analysis as they joined the OECD in 2010 (outside the scope of our study).
bIceland, Luxembourg and Turkey were excluded from our analysis due to insufficient HIV mortality data.
Studies exploring impact of economic downturns on population outcomes have shown that periods of economic hardship are associated with increased mortality and worsening health outcomes.6–8 More recent national studies have confirmed these ‘adverse effects',9–11 demonstrating associations between unemployment and all-cause mortality, suicide rates and road traffic accidents. In contrast, detailed analyses of the relationship between unemployment and specific pathologies have, by and large, been neglected.
A small number of studies have investigated the effect of financial downturns on HIV-infected individuals in single country settings,12,13 concluding that unemployment is an independent risk factor for disease progression and mortality. However, population-wide correlations at the national or multinational level, in addition to long-term trends, have yet to be determined.
We sought to build on earlier studies to determine the effect of changes in unemployment on HIV mortality across the OECD between 1981 and 2009, hypothesising that rising unemployment rates are associated with increased HIV mortality. The substantial increases in unemployment in recent years as well as the availability of high-quality epidemiological and socioeconomic data within the OECD provide a clear opportunity to assess any association.
Methods
Data collection
Data were analysed for 27 of the 34 current OECD member states. Chile, Estonia, Israel and Slovenia were excluded from our analysis as they joined the OECD in 2010, outside the scope of our study. Iceland, Luxembourg and Turkey were excluded from our analysis due to insufficient HIV mortality data (Table 4 in Appendix).
HIV mortality data by sex was obtained from the World Health Organization’s (WHO) mortality database,14 which is updated annually from civil registration systems of member states. Only medically certified deaths attributed to HIV are recorded in this dataset. The quality of this data has been evaluated by the WHO.15 Reported national death statistics were assessed by completeness, coverage and quality. Completeness was defined as the proportion of all deaths that are registered in the population covered by the vital registration system for a country. Of the 27 countries included in our analysis, 26 had achieved 100% completeness. The Republic of Korea had 89% completeness. Coverage is calculated by dividing the total number of deaths reported from vital registration system for a country-year by the total number of deaths estimated by the WHO for that year for the national population. Twenty-one countries included in our analysis had 100% coverage. Greece (88%), Italy (99%), Japan (97%), Republic of Korea (88%), Mexico (96%) and Norway (98%) were assessed to have suboptimal coverage. No adjustments have been made to the raw data to account for under-coverage. Quality was determined by taking into account the revision of the International statistical classification of diseases, and related health problems were used for national vital registration statistics, the completeness of data and minimal use of ill-defined categories of death. Of the 27 national datasets used in our analysis, 11 were considered to be of high quality, 13 of medium quality and 3 of low quality. We used age standardised death rates (ASDR) per 100,000 as the basis of our analysis. The ASDR, as defined by the WHO, is the weighted average of age-specific mortality rate per 100,000, where the weights are proportional to the number of individuals in the corresponding age groups of the WHO standard population.15 We chose to use ASDR as it controls for differences in age distribution within populations by accounting for age-specific mortality rates.16 Socioeconomic data were obtained from the World Bank’s Development Indicators Database 2013.17 Unemployment was taken to be the proportion of the labour force without work but available and seeking employment, as defined by the World Bank.17
Statistical analysis
Multivariate regression analysis was used to assess the relationship between HIV mortality (dependent variable) and unemployment (independent variable). To ensure that results were not driven by extreme observations for certain countries, a fixed-effects approach was used in our regression models, including 26 dummy variables for the 27 countries in the dataset. Doing this meant that the model evaluated mortality changes within individual countries while holding constant time-invariant differences between countries including higher predispositions to HIV, as well as political, cultural and structural differences. This conservative modelling approach made the data more comparable. The demographic structure of the selected countries was also controlled for by incorporating total population size, in addition to the percentage of the population aged over 65 years and less than 15 years into the model. Economic factors were controlled for by incorporating inflation, changes in GDP (gross domestic product) per capita and interest rates into the model. Healthcare resources were controlled for by incorporating the number of hospital beds per 1000 and number of physicians per 100,000. Both out-of-pocket health expenditure and health expenditure per capita (measured in purchasing power parity) were also controlled for. And finally, developmental indicators were controlled for by incorporating the prevalence of urbanisation, the mean calorific intake of the population as well as accessibility to clean water.
We used the Cook–Weisberg test18 to assess for and to confirm heteroskedasticity (where sub-samples have different distributions) in the data used. Therefore, robust standard errors were included in the regression models; this allowed us to account for heterogeneity in unemployment data due to differences in the way that countries measured unemployment rates, along with factors such as underemployment or social programmes (for example, back-to-work initiatives or programmes that see individuals move from employment to education or training) that may otherwise have hidden or suppressed actual unemployment rates.
This methodology has been widely used in similar health-economic studies and is regarded as a statistically robust approach.8,19–22
The ordinary-least-squares linear regression model was as follows:
where i is country and t is year; H is the health metric (age-standardised HIV mortality); U is the measure of unemployment; G is the measure of annual change in GDP/capita; I is the measure of inflation; R is the interest rate; B is the number of hospital beds; P is the number of physicians; X is the level of private health expenditure; Y is the level of public health expenditure; T is the rate of urbanisation; C is the calorific intake of the population; W is rate of access to clean water; α represents the population structure of the country being analysed; η is a dummy variable for each country included in the regression model; and ɛ is the error term. The coefficient values of these control variables can be found in Table 5 in Appendix.
We conducted one-, two- and three-year time-lag multivariate analyses to quantify the long-term effects of changes in unemployment on HIV mortality. Several robustness checks were also conducted; these are detailed in the Results section.
Stata SE version 12 was used for the analysis (Stata Corporation, Texas, USA). The “regress” command was used for our analysis.
Results
Table 2 displays the results of the regression model based on data collected from 27 OECD countries in the period between 1981 and 2009. The results displayed are adjusted for inter-country differences in demographic structure, financial influences, healthcare infrastructure as well as other developmental indicators, totalling 13 potential confounders and 26 country-specific dummy variables.
Table 2.
Multiple regression and lag analysis.
| Number of years after 1% rise in unemployment | Male HIV mortality per 100,000 |
Female HIV mortality per 100,000 |
||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | p value | Lower confidence interval | Upper confidence interval | Coefficient | p value | Lower confidence interval | Upper confidence interval | |
| Year 0 (year of change in unemployment) | 0.7112 | 0.0003 | 0.3338 | 1.0886 | 0.1657 | 0.0007 | 0.0712 | 0.2601 |
| Year 1 | 0.6271 | 0.0008 | 0.2668 | 0.9873 | 0.1368 | 0.0030 | 0.0475 | 0.2262 |
| Year 2 | 0.4468 | 0.0067 | 0.1263 | 0.7674 | 0.0825 | 0.0403 | 0.0037 | 0.1613 |
| Year 3 | 0.0604 | 0.6545 | -0.2058 | 0.3265 | -0.0072 | 0.8266 | -0.0718 | 0.0574 |
The data show the impact of a hypothetical 1% rise in unemployment on HIV mortality, controlling for proportion of population up to age of 14, proportion of population over age of 65, population size, 30 country controls, inflation, changes in GDP per capita, interest rates, urbanisation, nutrition (mean calorie intake), access to water, number of hospital beds per 1,000, number of physicians per 100,000, out of pocket expenses, health spending per capita (measured in purchasing power parity).
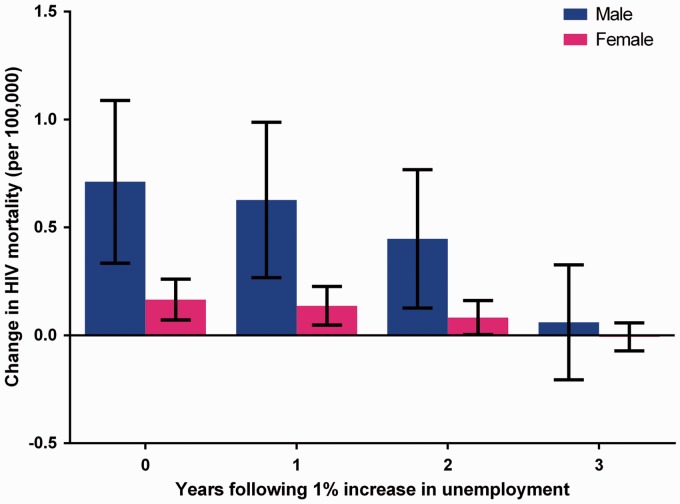
A 1% rise in unemployment was found to be associated with a statistically significant rise in HIV mortality per 100,000 in both men and women (coefficient for men 0.7112, 95% CI: 0.3338–1.0886, p = 0.0003; coefficient for women 0.1657, CI: 0.0712–0.2601, p = 0.0007). According to the most recent UN estimates,23 the combined population of the OECD countries is estimated to exceed 1.24 billion individuals. Based on this, a hypothetical 1% rise in unemployment across the OECD would be associated with 4327 male and 1050 female additional HIV deaths, during the year of the unemployment rise, not taking into consideration any lagged or longer term effects of unemployment. Time lag analysis showed that each given 1% rise in unemployment was associated with increased HIV mortality for up to two years after the initial unemployment change (Table 2, Figure 1). For year 1, coefficient for men is 0.6271, CI: 0.2668–0.9873, p = 0.0008; coefficient for women is 0.1368, CI: 0.0475–0.2262, p = 0.0030. In year 2, coefficient for men is 0.4468, CI: 0.1263–0.7674, p = 0.0067; coefficient for women is 0.0825, CI: 0.0037–0.1613, p = 0.0403. In year 3, changes were non-significant.
Figure 1.
A 1% rise in unemployment is associated with statistically significant lagged increases in HIV mortality for two years, in both men and women.
Robustness checks
To ensure the robustness of our findings, we conducted a series of further statistical analyses with various additional control variables. The first of these involved controlling for overall tuberculosis mortality, as it has been well documented that tuberculosis co-infection during HIV infection is associated with a worsened prognosis and an increased risk of mortality.24,25 Second, we controlled for changes in public spending on healthcare (measured as a percentage of GDP). Reduced public healthcare expenditure could potentially impact the availability of healthcare resources.26 Third, we controlled for changes in private healthcare expenditure. Fourth, we repeated our core analysis without out of pocket expenditure, since this could be one potential mechanism responsible for an association between unemployment and HIV mortality. Fifth, we controlled for the implicit increased risk of mortality that is associated with unemployment.27 Finally, the phenomenon of autocorrelation is when the national annual data from consecutive years is not truly independent from each other. Assessment of our dataset by the Woolridge test revealed that autocorrelation was present within our dataset. This was corrected for by including the Newey–West variance estimator. Our results (Table 3) showed that, even after accounting for each of these variables, unemployment remained associated with HIV mortality in a statistically significant manner (p < 0.001).
Table 3.
Robustness checks.
| Robustness check | Controls used in multiple regression | Male HIV mortality per 100,000 |
Female HIV mortality per 100,000 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | p value | Lower confidence interval | Upper confidence interval | Coefficient | p value | Lower confidence interval | Upper confidence interval | ||
| Tuberculosis co-infection controls | Original analysis controls and: controlling for overall TB mortality | 0.7526 | 0.0001 | 0.3740 | 1.1311 | 0.1718 | 0.0005 | 0.0765 | 0.2670 |
| Public healthcare spending controls | Original analysis controls and: controlling for changes in public healthcare spending | 0.6664 | 0.0004 | 0.3041 | 1.0286 | 0.1547 | 0.0009 | 0.0643 | 0.2451 |
| Private healthcare spending controls | Original analysis controls and: controlling for changes in private healthcare spending | 0.7149 | 0.0003 | 0.3373 | 1.0924 | 0.1663 | 0.0007 | 0.0719 | 0.2608 |
| Crude death rate controls | Original analysis controls and: controlling for changes in crude death rate during unemployment | 0.6969 | 0.0004 | 0.3140 | 1.0797 | 0.1652 | 0.0010 | 0.0683 | 0.2620 |
| Autocorrelation | Original analysis controls and inclusion of the Newey-West variance estimator. | 0.6789 | 0.0012 | 0.2724 | 1.0854 | 0.1590 | 0.0024 | 0.0573 | 0.2608 |
Multiple regression analyses were re-run using the controls in the original analysis in addition to those mentioned in the table below. The data show the impact of a 1% rise in unemployment, on HIV mortality, using the mentioned controls.
Discussion
Findings
This study has shown that increased unemployment in the OECD countries is associated with an increase in HIV mortality. These effects become apparent in the immediate time frame but also persist in the medium term. The scale of this association is such that a hypothetical 1% rise in unemployment in the OECD would be associated with an excess HIV mortality, in the order of thousands. Importantly, this statistically significant finding persisted even after accounting for a variety of potential confounding factors.
Our results show that the increase in HIV mortality, associated with rising unemployment, disproportionately affects males in comparison to females. This difference is reflected in the WHO’s reported HIV mortality figures.14 The underlying explanation for this difference is likely to be a complex interplay between various biological, behavioural and social factors. Furthermore, the increased risk of suicide and all-cause mortality during unemployment tends to be greater in men.27–29 This observed difference may partially be the result of men being more reluctant to seek healthcare services and therefore presenting at later stages of disease progression.30
Potential mechanisms
The mechanism by which unemployment might drive HIV mortality is currently unclear. We hypothesise that a number of mechanisms may potentially link the two variables. First, unemployment might negatively impact upon the socioeconomic status of HIV-infected individuals. The influence of social background on health outcomes has been extensively documented in the published literature.31 Studies have shown that there is a strong association between low socioeconomic status and increased risk of HIV mortality.32–35 Some propose that this is the result of delayed diagnosis and treatment due to reduced healthcare access.32 Others have demonstrated that a statistical association remains even after adjustment for such factors, suggesting that low socioeconomic status may be an independent factor for HIV mortality.34
Similarly, previous regional studies have shown that unemployment itself is also associated with delayed access to treatment.35 It has been shown that even after accounting for this, unemployment remains an independent risk factor for HIV morbidity and mortality.13 Our study shows that this association, at least with regard to HIV mortality, holds true on a much more macroscopic level, across the OECD.
The link between unemployment and an elevated incidence of suicide has also been well established.7,8,10 Underpinning these observations are the detrimental effects that unemployment has on psychological health and wellbeing. It is possible that this psychological effect and its associated behavioural changes may also contribute to increased mortality in HIV patients.
Exclusion of out of pocket expenditure from our analysis reduced the magnitude of association between unemployment and HIV mortality, suggesting that reduced out of pocket expenditure during times of unemployment may not contribute towards increased HIV mortality in year 0 (Table 2).
Strengths and limitations
Our quantitative macroeconomic approach confers several methodological strengths. We considered a much larger range of countries than previous studies, enabling investigation of international trends. Notably, our study used a conservative, fixed-effects regression analysis model. Modelling rates as normally distributed above and below the predicted value, which is essentially done by linear regression, is an unusual approach (rates cannot be negative, for example, yet this method permits and indeed expects negative rates). However, with large datasets, it can be justified if the model fits the data sufficiently: We believe that our analysis meets both of these criteria. This model together with the implemented robustness checks, and inclusion of 13 potential confounders and 26 country-specific dummy variables, account for many of the criticisms levelled at other studies looking at the relationship between health outcomes and unemployment, namely, the omission of potential confounding variables that are likely to be correlated with both unemployment rates and HIV mortality rates. In using a panel data approach to compare unemployment rates at interval of one year, for each year after the increase in unemployment with the mortality rates in each country, we also controlled for time-invariant heterogeneity between countries; something that aggregate, time-series analyses fail to do. The potential influence of bias was also minimised from this study by only using data taken from high-quality, objective, centralised databases. The quality of the mortality data has been evaluated by the WHO.15 However, the dataset makes no attempt to correct suboptimal national civil registration coverage. Despite this, across the whole OECD dataset, a high degree of total coverage is achieved. In addition, mortality in HIV persons where cause of death was not attributed to HIV would have been omitted from our analysis.
However, the broad overview of this study is also a source of weakness. Since we only evaluated annual data compiled at the national level, any variations or discrepancies that might have been present, in smaller geographical regions or across shorter timeframes, would not have been captured. Indeed, it has been shown that substantial variation in unemployment occurs at the subnational and regional levels and this can influence health outcomes.36 Second, the endpoints of our analysis focused solely on measures of mortality. We did not consider the effects of changes in unemployment on other HIV health measures, which could have yielded different results. Third, we were unable to stratify unemployment distribution by socioeconomic class. As discussed above, socioeconomic status is thought to contribute to HIV mortality. As a result, this study fails to dissect the influence of this potential confounding factor. Fourth, while this study does show an association between unemployment and HIV mortality, a causal link cannot be established. It is possible that rises in HIV mortality could result in a rise in unemployment; a phenomenon known as endogeneity. Indeed, there is substantial historical precedent of employment discrimination against HIV-infected individuals. However, the impact of HIV infection status on employability is extremely variable depending on geo-social factors.37 The likelihood of endogeneity confounding our findings is unlikely, since implausibly large increases in HIV prevalence would probably be required in order to affect unemployment rates in such a short timeframe. Additionally, our lag analysis which demonstrates a long-term influence of unemployment on HIV mortality would not be consistent with such a phenomenon. Finally, our study analyses ecological data and so is prone to ecological fallacy – we cannot infer conclusions about individual doctors or patients from country-level data.
Implications
Our findings could have important implications both for healthcare professionals and to policy makers. Previous studies have shown that unemployment can exacerbate the perceived barriers to healthcare access.38 This is directly reflected by reduced healthcare utilisation by unemployed individuals compared to their employed counterparts.39 Our study provides further support to the importance of clinician awareness of the potentially increased vulnerability of unemployed patients. Steps to facilitate healthcare access and ensure the rapid delivery both of diagnosis and treatments could address such vulnerabilities. What strategies would be most suitable in tackling such an issue is unclear. The evidence supporting the efficacy of different interventions with the aim of addressing health inequalities due to social determinants has been largely inconclusive.40
At the macro level, the influence of economic policy on public health cannot be overlooked. Fiscal policies that increase unemployment rates should only be exercised with due consideration, not only because of their social and economic repercussions but also since they may also act to adversely affect population health, specifically in this case, HIV mortality. Indeed, current austerity measures could contribute towards exacerbating the burden of infectious diseases, including HIV.41 Policies promoting return-to-work such as work-sharing programmes or those that prevent further unemployment could potentially benefit HIV survival.1
Conclusions
The recent global recessions led to a rapid increase in unemployment across almost all OECD member states, and the economies of many countries have yet to recover. This event has raised the question of how unemployment may impact HIV outcomes at the population level. Our study has shown that increases in aggregate unemployment are associated with significantly higher HIV mortality in the OECD. Policy interventions and austerity measures, which may increase unemployment, are a key concern, possibly presenting additional barriers to HIV management.
Acknowledgements
None
Appendix
Table 4.
Basic descriptive statistics of the raw HIV mortality data used in our analysis.
| Country | Number of observations | Mean HIV mortality (per 100,000) | Standard deviation | Min | Max |
|---|---|---|---|---|---|
| Australia | 24 | 2.15 | 1.88 | 0 | 5.9 |
| Austria | 24 | 1.34 | 0.87 | 0.3 | 3.4 |
| Belgium | 18 | 1.23 | 0.94 | 0 | 3.1 |
| Canada | 19 | 4.74 | 2.85 | 1.8 | 9.6 |
| Czech Republic | 24 | 0.04 | 0.05 | 0 | 0.1 |
| Denmark | 13 | 2.30 | 2.55 | 0.6 | 7.8 |
| Finland | 23 | 0.16 | 0.20 | 0 | 0.9 |
| France | 22 | 5.32 | 4.27 | 1.4 | 13.2 |
| Germany | 20 | 1.76 | 1.31 | 0.6 | 4.0 |
| Greece | 23 | 0.32 | 0.32 | 0 | 1.1 |
| Hungary | 23 | 0.21 | 0.16 | 0 | 0.7 |
| Icelanda | 0 | N/A | N/A | N/A | N/A |
| Ireland | 23 | 0.58 | 0.72 | 0 | 2.5 |
| Italy | 22 | 4.75 | 3.99 | 0.1 | 12.8 |
| Japan | 22 | 0.06 | 0.05 | 0 | 0.1 |
| South Korea | 14 | 0.14 | 0.09 | 0 | 0.3 |
| Luxembourga | 0 | N/A | N/A | N/A | N/A |
| Mexico | 11 | 8.14 | 0.14 | 7.9 | 8.4 |
| Netherlands | 27 | 1.66 | 1.46 | 0.1 | 4.6 |
| New Zealand | 23 | 1.47 | 1.12 | 0.2 | 3.4 |
| Norway | 24 | 0.94 | 0.69 | 0.2 | 2.5 |
| Poland | 11 | 0.48 | 0.06 | 0.4 | 0.6 |
| Portugal | 19 | 10.73 | 5.43 | 1.2 | 18.5 |
| Slovakia | 18 | 0.04 | 0.05 | 0 | 0.1 |
| Spain | 26 | 7.76 | 6.65 | 0 | 23.3 |
| Sweden | 23 | 0.83 | 0.67 | 0.2 | 2.3 |
| Switzerland | 13 | 3.17 | 3.19 | 0.9 | 11.6 |
| Turkeya | 0 | N/A | N/A | N/A | N/A |
| United Kingdom | 22 | 0.80 | 0.65 | 0 | 2.0 |
| United States | 26 | 9.91 | 8.17 | 0 | 25.5 |
aIceland, Luxembourg and Turkey were excluded from our analysis due to insufficient HIV mortality data.
Table 5.
Control variable coefficient values.
| Variable | Male analysis coefficient | Female analysis coefficient |
|---|---|---|
| Population aged >65 | −1.4778 | −0.4714 |
| Population aged <15 | −0.7895 | −0.2218 |
| Population size | −0.0000 | −0.0000 |
| GDP per capita | 0.0363 | 0.0185 |
| Inflation | 0.2212 | 0.0669 |
| Interest rate | 0.0688 | 0.0195 |
| Hospital beds per 1,000 | 0.2695 | 0.0030 |
| Physicians per 100,000 | −0.9478 | −0.2723 |
| Out-of-pocket health expenditure | 1.7849 | 0.4508 |
| Public health expenditure | 0.5691 | 0.0977 |
| Calorific intake | −0.0795 | 0.0005 |
| Prevalence of urbanisation | 0.2687 | 0.1067 |
| Access to clean water | 0.9168 | 0.2787 |
GDP: gross domestic product.
Declarations
Competing Interest
None declared.
Funding
None declared.
Ethical approval
No ethical approval was sought for this paper as it does not involve human participants. All data used in the analysis is freely available and open source.
Guarantor
MM
Contributorship
Study design (MM, CW, RA); data collection (MM, CDZ, CW); data analysis (MM, CW); data interpretation (MM, CDZ, CW, TZ, RA); manuscript development (MM, CDZ, CW, TZ, RA).
Provenance
Not commissioned; peer-reviewed by Simon Howard
References
- 1.Amable B, Mayhew K. Unemployment in the OECD. Oxford Rev Econ Policy 2011; 27: 207–220. [Google Scholar]
- 2.Horton R. The global financial crisis: an acute threat to health. Lancet 2009; 373: 355–356. [DOI] [PubMed] [Google Scholar]
- 3.Ortiz I and Cummins M. The Age of Austerity: A Review of Public Expenditures and Adjustment Measures in 181 Countries. SSRN, 2013.
- 4.Limb M. Austerity measures will lead to rise in unemployment and suicides, says Marmot. BMJ 2012; 344: e2887–e2887. [DOI] [PubMed] [Google Scholar]
- 5.Stuckler D, Basu S. The body economic: why austerity kills, London: Penguin Books Limited, 2013. [Google Scholar]
- 6.Morris JK, Cook DG, Shaper AG. Loss of employment and mortality. BMJ 1994; 308: 1135–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewis G, Sloggett A. Suicide, deprivation, and unemployment: record linkage study. BMJ 1998; 317: 1283–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet 2009; 374: 315–323. [DOI] [PubMed] [Google Scholar]
- 9.Barr B, Taylor-Robinson D, Scott-Samuel A, McKee M, Stuckler D. Suicides associated with the 2008–10 economic recession in England: time trend analysis. BMJ 2012; 345: e5142–e5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karanikolos M, Mladovsky P, Cylus J, Thomson S, Basu S, Stuckler D, et al. Financial crisis, austerity, and health in Europe. Lancet 2013; 381: 1323–1331. [DOI] [PubMed] [Google Scholar]
- 11.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. Effects of the 2008 recession on health: a first look at European data. Lancet 2011; 378: 124–125. [DOI] [PubMed] [Google Scholar]
- 12.Paraskevis D, Nikolopoulos G, Tsiara C, Paraskeva D, Antoniadou A, Lazanas M, et al. HIV-1 outbreak among injecting drug users in Greece, 2011: a preliminary report. Euro Surveill 2011; 16: 19962–19962. [DOI] [PubMed] [Google Scholar]
- 13.Delpierre C, Cuzin L, Lauwers-Cances V, Datta GD, Berkman L, Lang T. Unemployment as a risk factor for AIDS and death for HIV-infected patients in the era of highly active antiretroviral therapy. Sex Transm Infect 2008; 84: 183–186. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Mortality Database, http://apps.who.int/healthinfo/statistics/mortality/whodpms/ (2012, accessed 25 March 2017).
- 15.Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Heal Organ 2005; 83: 171–177. [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Indicator definitions and metadata, http://www.who.int/whosis/whostat2006DefinitionsAndMetadata.pdf?ua=1 (2006, accessed 7 February 2014).
- 17.World Bank. World Development Indicators Database, http://data.worldbank.org/indicator/SL.UEM.TOTL.ZS (2013, accessed 5 February 2014).
- 18.Cook RD, Weisberg S. Diagnostics for heteroscedasticity in regression. Biometrika 1983; 70: 1–10. [Google Scholar]
- 19.Davidson R, MacKinnon JG. Estimation and inference in econometrics, New York: Oxford University Press, 1993. [Google Scholar]
- 20.Stuckler D, Basu S, McKee M, King L. Mass incarceration can explain population increases in TB and multidrug-resistant TB in European and central Asian countries. Proc Natl Acad Sci U S A 2008; 105: 13280–13285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stuckler D, King L, McKee M. Mass privatisation and the post-communist mortality crisis: a cross-national analysis. Lancet 2009; 373: 399–407. [DOI] [PubMed] [Google Scholar]
- 22.Saffer H, Chaloupka F. The effect of tobacco advertising bans on tobacco consumption. J Health Econ 2000; 19: 1117–1137. [DOI] [PubMed] [Google Scholar]
- 23.United Nations. World population prospect, the 2012 Revision, http://esa.un.org/unpd/wpp/index.htm (2012, accessed 5 February 2014).
- 24.Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, et al. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med 2003; 163: 1009–1021. [DOI] [PubMed] [Google Scholar]
- 25.Mukadi YD, Maher D, Harries A. Tuberculosis case fatality rates in high HIV prevalence populations in sub-Saharan Africa. AIDS 2001; 15: 143–152. [DOI] [PubMed] [Google Scholar]
- 26.European Observatory on Health Systems and Policies. Health, health systems and economic crisis in Europe – impact and policy implications, Geneva: World Health Organization, 2013. [Google Scholar]
- 27.Martikainen PT, Valkonen T. Excess mortality of unemployed men and women during a period of rapidly increasing unemployment. Lancet 1996; 348: 909–912. [DOI] [PubMed] [Google Scholar]
- 28.Johansson SE, Sundquist J. Unemployment is an important risk factor for suicide in contemporary Sweden: an 11-year follow-up study of a cross-sectional sample of 37,789 people. Publ Health 1997; 111: 41–45. [DOI] [PubMed] [Google Scholar]
- 29.Dorling D. Unemployment and health. BMJ 2009; 338: b829–b829. [DOI] [PubMed] [Google Scholar]
- 30.Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs 2005; 49: 616–623. [DOI] [PubMed] [Google Scholar]
- 31.Feinstein JS. The relationship between socioeconomic status and health: a review of the literature. Milbank Q 1993; 71: 279–322. [PubMed] [Google Scholar]
- 32.Wood E, Montaner JS, Chan K, Tyndall MW, Schechter MT, Bangsberg D, et al. Socioeconomic status, access to triple therapy, and survival from HIV-disease since 1996. AIDS 2002; 16: 2065–2072. [DOI] [PubMed] [Google Scholar]
- 33.Hogg RS, Strathdee SA, Craib KJ, O'Shaughnessy MV, Montaner JS, Schechter MT. Lower socioeconomic status and shorter survival following HIV infection. Lancet 1994; 344: 1120–1124. [DOI] [PubMed] [Google Scholar]
- 34.Cunningham WE, Hays RD, Duan N, Andersen R, Nakazono TT, Bozzette SA, et al. The effect of socioeconomic status on the survival of people receiving care for HIV infection in the United States. J Heal Care Poor Underserved 2005; 16: 655–676. [DOI] [PubMed] [Google Scholar]
- 35.Joy R, Druyts EF, Brandson EK, Lima VD, Rustad CA, Zhang W, et al. Impact of neighborhood-level socioeconomic status on HIV disease progression in a universal health care setting. J Acquir Immune Defic Syndr 2008; 47: 500–505. [DOI] [PubMed] [Google Scholar]
- 36.Lyratzopoulos G, Barbiere JM, Rachet B, Baum M, Thompson MR, Coleman MP. Changes over time in socioeconomic inequalities in breast and rectal cancer survival in England and Wales during a 32-year period (1973–2004): the potential role of health care. Ann Oncol 2011; 22: 1661–1666. [DOI] [PubMed] [Google Scholar]
- 37.McGoldrick C. HIV and employment. Occup Med 2012; 62: 242–253. [DOI] [PubMed] [Google Scholar]
- 38.Ahmed SM, Lemkau JP, Nealeigh N, Mann B. Barriers to healthcare access in a non-elderly urban poor American population. Heal Soc Care Community 2001; 9: 445–453. [DOI] [PubMed] [Google Scholar]
- 39.Tefft N, Kageleiry A. State-level unemployment and the utilization of preventive medical services. Heal Serv Res 2014; 49: 186–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010; 64: 284–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bonovas S, Nikolopoulos G. High-burden epidemics in Greece in the era of economic crisis. Early signs of a public health tragedy. J Prev Med Hyg 2012; 53: 169–171. [PubMed] [Google Scholar]