Abstract
Inflammation is one of the major risk factors for cancer. Here, we show that calcium/calmodulin-dependent protein kinase II gamma (CAMK2γ) in intestinal epithelial cells (IECs) modulates inflammatory signals and promotes colitis-associated cancer (CAC) in mice. We have identified CAMK2γ as a downstream target of colitis-induced WNT5a signaling. Furthermore, we have shown that CAMK2γ protects against intestine tissue injury by increasing IEC survival and proliferation. CAMK2γ knockout mice displayed reduced CAC. Furthermore, we used bone marrow transplantation to reveal that CAMK2γ in IECs, but not immune cells, was crucial for its effect on CAC. Consistently, transgenic over-expression of CAMK2γ in IECs accelerated CAC development. Mechanistically, CAMK2γ in IECs enhanced epithelial STAT3 activation to promote survival and proliferation of colonic epithelial cells during CAC development. These results thus identify a new molecular mechanism mediated by CAMK2γ in IECs during CAC development, thereby providing a potential new therapeutic target for CAC.
Keywords: Colitis-associated colorectal cancer, inflammation, CAMK2γ, STAT3, WNT5A
More than 20% of worldwide cancer cases are associated with chronic inflammation1, 2. Chronic inflammation is now well recognized as an important risk factor for gastric cancer, lymphoma3, 4, hepatocellular carcinoma (HCC)5, pancreatic cancer, esophageal cancer, cholangiocarcinoma and colorectal cancer (CRC)6. CRC is the third most common cancer type and the second leading cause of cancer deaths among all cancers in the United States7. Inflammatory bowel disease (IBD), which results from inflammatory disorders of the intestinal tract, shows a strong positive correlation with the occurrence of CRC8. Patients with various types of IBD, including ulcerative colitis (UC), display 3- to 7-fold greater CRC risk than healthy people9–13. Colitis-associated CRC (CAC) is the most severe consequence of IBD14, 15. Patients with CAC are also frequently diagnosed at advanced stages, and have worse prognoses than other CRC patients15–18.
The immune cells in the intestine are key players to maintain tissue homeostasis14, 19. However, defective innate immune responses and dysfunction of the intestinal epithelial cell (IEC) barrier can lead to IBD and enhance the intestinal susceptibility to bacterial invasion. The inflamed environment also promotes mutation accumulation, which can cause tumor development14, 19. Recent studies show that IBD generates an inflammatory environment with extensive tissue regeneration signals, accompanied by activation of pro-oncogenic factors, such as STAT3 and NF-κB, in pre-malignant cells. This inflammatory environment, in turn, suppresses cell death and promotes hyperplasia and malignancy of inflamed tissues14, 19. Despite the recent progress in delineating the molecular mechanisms of CAC, the relative lack of knowledge in its pathogenesis still impedes the development of effective treatments for CAC and other inflammation-related cancers.
CAMK2γ is a serine and threonine kinase that belongs to the calcium/calmodulin-dependent kinase II family20. CAMK2γ was previously reported to promote inflammation21–24. CAMK2γ is critical for T cell maturation, as well as the activation of mature T cells in peripheral lymphoid organs21. It has also been reported that CAMK2γ is the only CAMK2 family member expressed in macrophages23, and that CAMK2γ is required for inflammatory responses induced by a variety of factors22, 24, 25. Recently, we and others found that CAMK2γ is important in both hematopoietic malignancies and solid tumors26–29. Therefore, we ask whether CAMK2γ is involved in CAC.
RESULTS
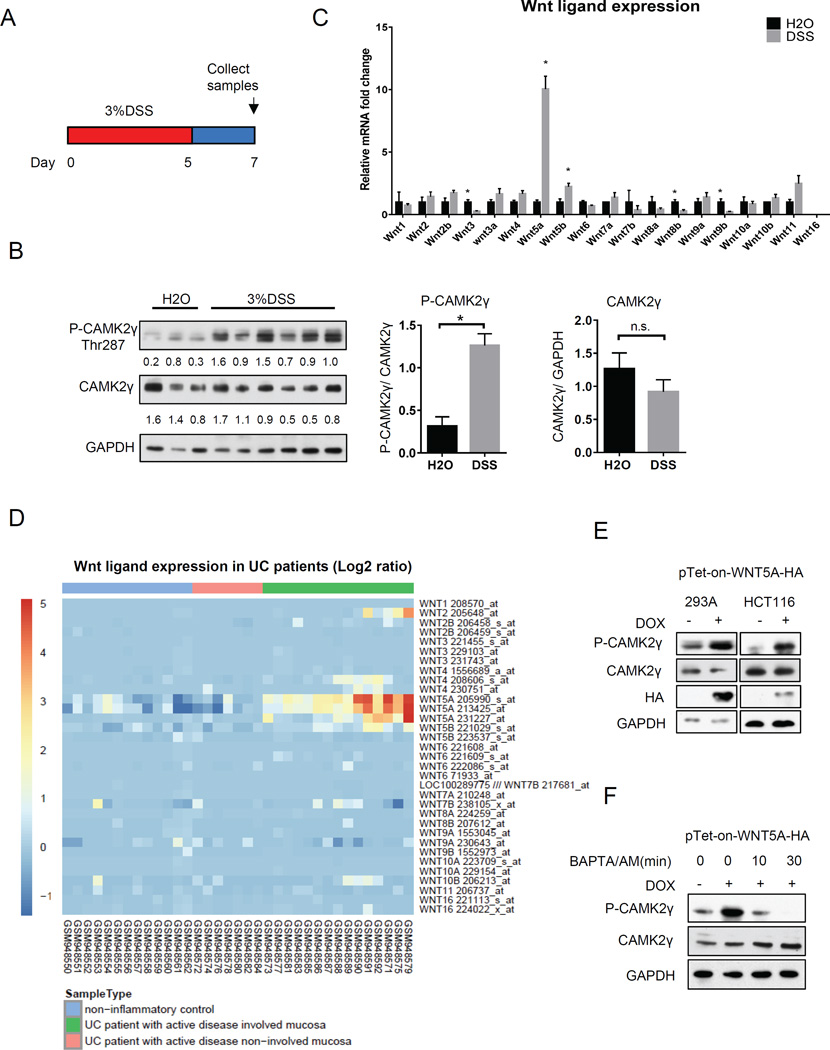
DSS treatment activates colonic CAMK2γ via a non-canonical WNT signal
Dextran sodium sulfate (DSS) challenge in mice causes intestinal inflammation and injury that resembles human colitis30, 31. We first asked whether intestinal CAMK2γ can be activated by DSS challenge. Wild-type (WT) mice received 3% DSS orally for five days to induce acute colitis31, 32, followed by recovery for two days (Fig. 1A). We found that induction of colitis by DSS strongly increased the activity of CAMK2γ in colon tissues, as measured by phosphorylation of CAMK2γ at Thr287, whereas the total colonic CAMK2γ protein level was not changed (Fig. 1B).
Figure 1. DSS induced colitis activates colonic CAMK2γ via non-canonical WNT signaling.
(A) Scheme for colitis induction. Red color indicates the duration of DSS treatment. (B) Protein expression and phosphorylation of CAMK2γ in DSS-induced colitis. The relative expression levels normalized to GAPDH were shown under the blot. They were further quantified and shown as bar plots. (C) The relative mRNA expression profile of WNT ligands in the colonic tissue of H2O- or DSS-treated mice. Expression levels were normalized to H2O-treated mice. (D) Expression of WNT family ligands in a UC patient microarray cohort. (E) Effects of retroviral over-expression of WNT5A in cell lines on CAMK2γ phosphorylation. DOX = doxycycline. (F) Phosphorylation of CAMK2γ by WNT5A in response to intracellular calcium chelator (BAPTA/AM) treatment. Results are presented as mean ± s.e.m. of 3 independent experiments; *P<0.05. See also Supplementary Fig. 1.
We then asked which signals might activate CAMK2γ in colitis. Previous studies have indicated that activation of the non-canonical WNT pathway increases intracellular calcium flux, which could activate CAMK2γ33, 34. Furthermore, colitis and activation of non-canonical WNT signaling can antagonize the canonical WNT signal and suppress the activity of β-catenin35. Consistent with this prior work, we observed a reduction in β-catenin target gene expression in mouse colonic tissues after DSS treatment (Supplementary Fig. 1A). A decrease in WNT/ β-catenin activity may imply a balance shift from the canonical WNT/β-catenin pathway to the non-canonical WNT pathway. Based on the activated CAMK2γ and decreased canonical WNT signal observed in inflamed mouse colonic tissue (Fig. 1B and Supplementary Fig. 1A), we therefore asked whether CAMK2γ was activated by non-canonical WNT ligand-induced signals in the DSS-induced mice. To address this question, we screened the expression of all 14 different WNT ligands in H2O- and DSS-treated mouse colonic tissue samples. As expected, the expression levels of three canonical WNT ligands, Wnt3, Wnt8b and Wnt9b, were significantly decreased after DSS challenge, whereas the expression levels of two non-canonical WNT ligands, Wnt5a and Wnt5b, were robustly increased (Fig. 1C). Specifically, Wnt5a showed a nearly 10-fold induction. To test whether the changes observed in our mouse model are also present in human disease, we retrieved an ulcerative colitis (UC) patient microarray cohort dataset36 from the NCBI Gene Expression Omnibus database. Analysis of the dataset indicated that Wnt5A was the most upregulated WNT ligand in UC patient samples (Fig. 1D).
To further confirm the activation of CAMK2γ by WNT5A, we stably infected cell lines with retroviruses that permit doxycycline-inducible human WNT5A-HA-expression. Overexpression of WNT5A strongly increased CAMK2γ phosphorylation (Fig. 1E). Over-expression of two known WNT5A receptors, FZD2 and FZD5, as well as the FZD co-receptor ROR2, also activated CAMK2γ (Supplementary Fig. 1B). Moreover, treatment with the intracellular calcium chelator BAPTA/AM blunted the activation of CAMK2γ by WNT5A in 293A cells (Fig. 1F). These results suggested that the colitis-induced WNT5A signal is transduced through a non-canonical WNT pathway to activate CAMK2γ in the colon.
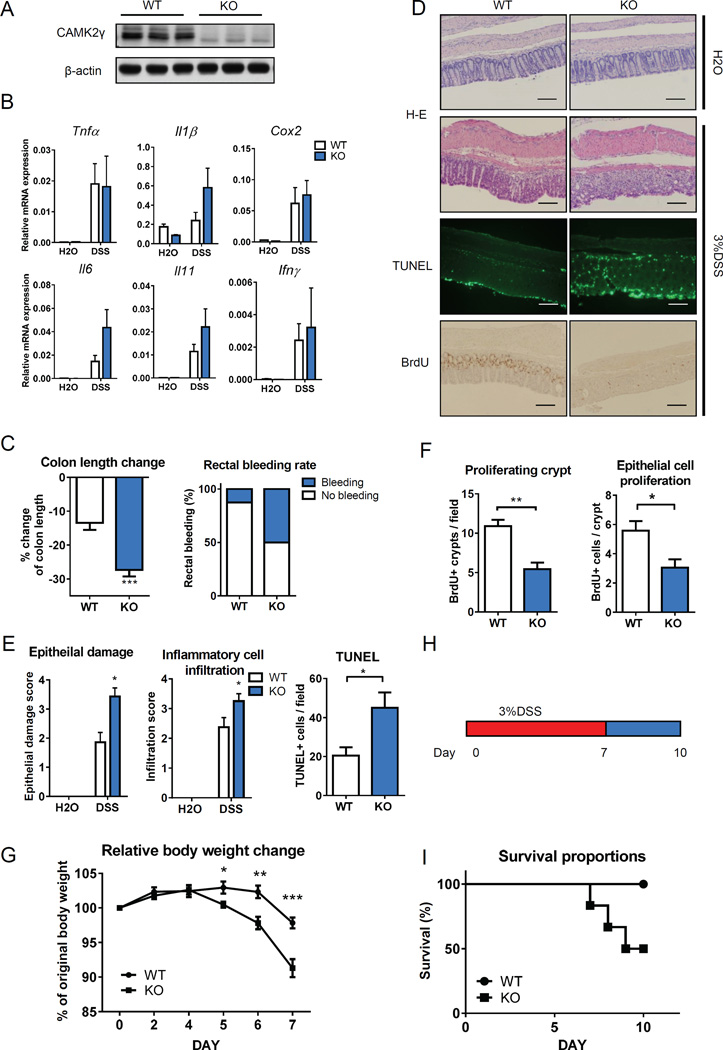
CAMK2γ deficiency increases DSS-induced colonic epithelial cell death and tissue injury
DSS disrupts the colonic epithelia by breaking down the integrity of the epithelial barrier and promoting the invasion of intestinal microbiota37. The invaded microbiota activate innate immune cells and cause excessive inflammation, cell death and tissue damage, which leads to severe clinical symptoms of colitis, including body weight loss, colonic shortening, and rectal bleeding37, 38. Because CAMK2γ is activated in the intestine of DSS-treated mice, we next used CAMK2γ knockout mice (KO) to determine the role of CAMK2γ in DSS-induced colitis (Fig. 2A). We treated the mice as described in Fig. 1a and compared KO mice with their WT littermates. Surprisingly, quantitative real-time PCR (qRT-PCR) revealed that DSS treatment induced similar inflammatory cytokine and enzyme expression, including TNFα, IFN-γ, COX2 and IL-17A in colonic tissues from both WT and CAMK2γ KO mice (Fig. 2A and 2B, Supplementary Fig. 2). Although there were trends toward increased expression of IL-6 and IL-1β in the KO mice, the difference is not statistically significant. (Fig. 2B). The colitis-induced intestinal injury, however, was more severein the CAMK2γ KO mice than the WT controls (Fig. 2C–2G). At day 7 of the treatment regimen, the CAMK2γ KO mice showed shorter colon lengths and higher rectal bleeding rates than the WT mice (Fig. 2C). Hematoxylin and eosin (H&E) staining of the colonic tissue showed that the KO mice had more inflammatory cell infiltration, ulceration and hyperplasia, as indicated by the epithelial damage score and infiltration score (Fig. 2D and 2E). CAMK2γ KO mice also displayed decreased proliferation of colonic epithelial cells during the regeneration stage of colitis (Fig. 2F). CAMK2γ KO mice not only had fewer proliferating crypts in the inflamed colonic tissue but also showed fewer BrdU-positive proliferating cells per crypt (Fig. 2D and 2F). TUNEL staining also indicated that there were more apoptotic epithelial cells after DSS challenge in the CAMK2γ KO mice than the WT mice (Fig. 2D and 2E). Consistently, the CAMK2γ KO mice showed significantly greater weight loss than the WT mice (Fig. 2G). Because enhanced epithelial damage could further lead to increased animal mortality, we then challenged the CAMK2γ KO mice and their WT littermates with a longer DSS treatment (7 days) (Fig. 2H). In this model, 50% of the CAMK2γ KO animals were dead by 10 days after the start of DSS treatment, whereas all of the WT animals survived (Fig. 2I). Taken together, these results indicate that CAMK2γ protects mice from colitis-induced injury by increasing the survival and proliferation of colonic epithelial cells.
Figure 2. CAMK2γ KO increases DSS-induced colonic epithelial cell death and exacerbates tissue injury.
(A) Verification of CAMK2γ deficiency in the colons of CAMK2γ knockout (KO) mice by western blotting. (B) Relative mRNA levels of inflammatory cytokines and enzymes in the colons of WT and KO mice (WT=9, KO=9). (C) The change in colon length and rectal bleeding rate of DSS-treated mice (n=9). (D) Representative images for H&E, TUNEL and BrdU staining of mouse colon sections. Scale bars indicate 200µm length (E) Colonic epithelial damage, inflammatory cell infiltration, and cell death calculated from the staining shown in (d). (F) Average proliferating crypt number per field quantified from BrdU staining of (D). (G) DSS-induced changes in mouse body weight. (H–I) Survival rate of mice (I) in a more severe acute colitis induction model (H) (WT=6, KO=6). Results are presented as mean ± s.e.m. of 3 independent experiments, except where otherwise noted. *P<0.05, **P<0.01, ***P<0.001. See also Supplementary Figure 2.
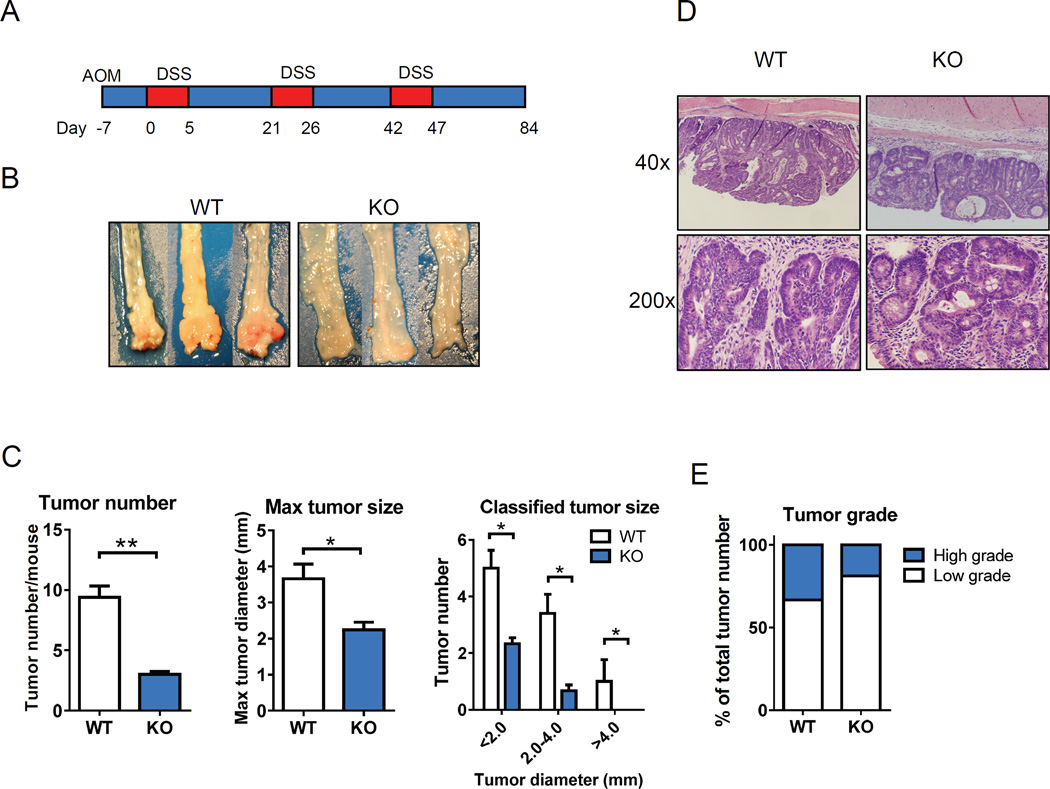
CAC is reduced by CAMK2γ gene deletion in mice
Based on the above results, next we asked whether CAMK2γ might promote colitis-associated tumorigenesis. Because combined delivery of DSS and azoxymethane (AOM) has been widely used as a model for CAC39, we thus used this model to investigate the role of CAMK2γ in inflammation-related tumorigenesis40. WT and CAMK2γ KO mice were injected with AOM once, followed by three rounds of oral administration of 3% DSS in water (Fig. 3A)40.
Figure 3. CAMK2γ KO mice display reduced CAC development.
(A) Scheme for AOM/DSS-induced CAC in mice. Intestinal tumors are analyzed on day 84. (B) Representative photos of distal colon tissues from WT and CAMK2γ KO mice. (C) Tumor number, maximum tumor size and classified tumor size from the colon tissues of mice. (WT=5, KO=6). (D) Representative H&E staining of colon sections from WT and KO mice. (E) Quantification of tumor grade in WT and KO mice (WT=5, KO=6). Results are presented as mean ± s.e.m.; *P<0.05, **P<0.01. See also Supplementary Figure 3.
At the end of the treatment, all of the mice developed CAC regardless of their genotypes, and tumors were mostly found in the distal colon, as previously described40. Notably, the CAMK2γ KO mice developed much fewer tumors and the tumors were smaller than those in the WT mice (Fig. 3B and 3C). We further classified the tumors into three groups according to the tumor diameters. The CAMK2γ KO mice not only showed lower maximum tumor sizes but also had fewer tumors in each of the tumor size categories (Fig. 3B and 3C). Moreover, histological analysis revealed a decreased high-grade tumor proportion in the CAMK2γ KO mice (Fig. 3D, 3E and Supplementary Fig. 3). These results clearly demonstrated that CAMK2γ KO mice had reduced CAC development in the AOM/DSS model.
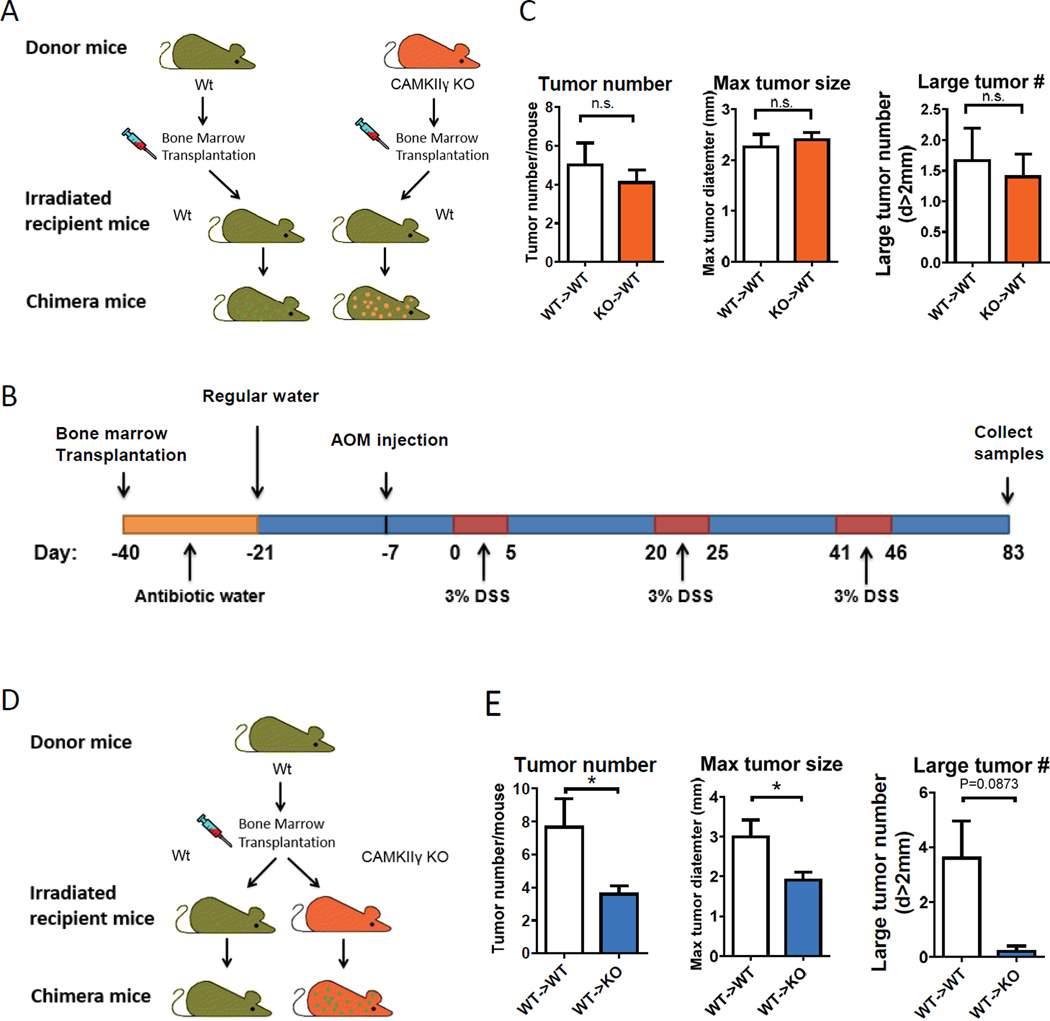
CAMK2γ KO in colonic tissue-resident cells, but not in immune cells, protects mice against CAC
CAMK2γ is ubiquitously expressed in bone marrow-derived immune cells, as well as colonic tissue-resident cells, and both cell types are known to participate in CAC development14, 21, 22, 41, 42. We first asked whether CAMK2γ KO suppressed CAC development through directly regulating the function of inflammatory cells. To answer this question, we isolated bone marrow cells from both WT and CAMK2γ KO CD45.2 donor mice, and then transplanted them into irradiated CD45.1 WT recipient mice (Fig. 4A). The bone marrow reconstitution efficiency was verified by flow cytometry analyses using antibodies targeting the mouse CD45.1 and CD45.2 antigens, as well as by transgenic allele-specific PCR on colonic tissue samples from the chimeric mice (Supplementary Fig. 4A). These two groups of chimeric mice were then subjected to CAC induction, as illustrated in Fig. 4B. Unexpectedly, we observed no difference in either the average tumor number or tumor size between these two groups of chimeric mice (Fig, 4C). Thus, specific deletion of CAMK2γ in inflammatory cells failed to suppress the development of CAC.
Figure 4. CAMK2γ KO in colonic tissue-resident cells, but not in immune cells, results in reduced CAC.
(A) Schematic overview of the generation of bone marrow chimeric mouse groups WT→WT and KO→WT. (B) Scheme for CAC induction in chimeric mice. (C) Tumor number, maximum tumor size, and the number of large tumors (diameter [d] > 2 mm) from WT→WT and KO→WT mice (n=10). (D) Schematic overview of the generation of bone marrow chimeric mouse groups WT→WT and WT→KO. (E) Tumor number, maximum tumor size, and the number of large tumors with diameter over 2 mm from WT→WT and WT→KO mice (n=5). Results are presented as mean ± s.e.m.; *P<0.05, n.s., not significant. See also Supplementary Fig. 4.
We then asked whether CAMK2γ KO in non-immune cells was responsible for the suppression of CAC. We generated two different groups of bone marrow chimeric mice by transplanting bone marrow cells from CD45.1 WT mice into CD45.2 WT and CD45.2 CAMK2γ KO mice (Fig. 4D). The chimeric mice achieved more than 96% immune system reconstitution rates and showed expression of CAMK2γ in peripheral immune cells before the mice were challenged with AOM/DSS, as illustrated in Fig. 4B (Supplementary Fig. 4B). As a result, the WT→KO chimeric mice showed decreases in both the tumor numbers and tumor sizes (Fig. 4E), similar to the phenotype of the whole-body CAMK2γ KO mice. Taken together, these results indicate that deletion of CAMK2γ in tissue-resident cells, but not in bone marrow-derived immune cells, suppresses CAC development.
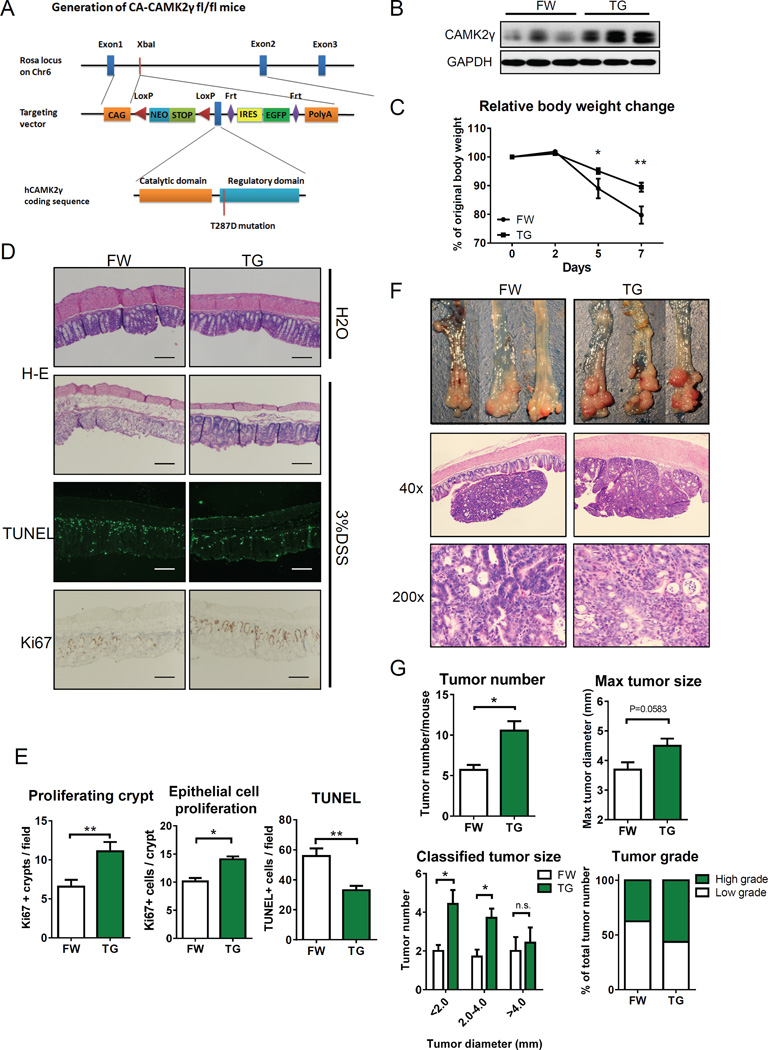
Constitutive CAMK2γ over-expression in intestinal epithelial cells (IECs) protects mice from colitis-induced injury and promotes CAC development
Colonic epithelial cells are the major resident cells in the colonic tissue, and also the source of CRC cells43. To further confirm the role of CAMK2γ in tissue-resident cells during CAC development, we generated a new mouse line that conditionally over-expresses CAMK2γ in the colonic epithelium. We inserted a conditional CAMK2γ over-expression cassette, with a LoxP-flanked STOP cassette, under the control of the CAG promoter in the ROSA26a locus. A T-to-D mutation at Thr287 (T287D) was introduced into the Camk2γ coding sequence (CDS) to allow constitutive activation of CAMK2γ (CA-CAMK2γ fl/fl) (Fig. 5A)21. By crossing Villin-Cre mice with the CA-CAMK2γ fl/fl homozygous mice, we generated Villin-tg (TG) mice with specific CA-CAMK2γ over-expression in colonic epithelial cells (Fig. 5B). The TG mice showed normal gastro-intestinal development compared with CA-CAMK2γ fl/wt (FW) littermates and had no signs of spontaneous colorectal tumor development up to the age of 8 months.
Figure 5. Constitutive CAMK2γ over-expression in intestinal epithelial cells protects mice from tissue injury and promotes CAC.
(A) Scheme for the generation of tissue-specific constitutively active CAMK2γ (CA-CAMK2γ) transgenic mouse lines (TG) and CA-CAMK2γ fl/wt control mice (FW). (B) Representative western blot analysis of CAMK2γ in colon tissues from TG and FW mice. (C) DSS-induced changes in body weight. (D) Representative images for H&E, TUNEL and Ki67 staining of colon sections from FW and TG mice. Scale bar indicate 200µm length. (E) Crypt proliferation, epithelial cell proliferation and apoptotic cell death, calculated from the BrdU and TUNEL staining shown in (D). For C–E, the mice were treated as shown in Fig. 1A. (WT=6, KO=10) (F) Representative images of distal colon tissues and H&E staining of colon sections from FW and TG mice. (G) Tumor number, maximum tumor size, classified tumor size, and tumor grade of colon tumors from FW and TG mice. For F–G, the mice were treated as shown in Fig. 3A. Results are presented as mean ± s.e.m.; *P<0.05, **P<0.01, n.s., not significant. See also Supplementary Fig. 5 and 6.
We first examined the effects of the IEC-specific constitutive CAMK2γ over-expression in protecting mice from colitis-induced injury. This allowed us to analyze the role of CAMK2γ in precancerous colonic disease. The mice were treated as illustrated in Fig. 1A. Over-expression of CA-CAMK2γ in colonic epithelial cells, as expected, suppressed colitis-associated body weight loss (Fig. 5C) and colonic shortening, and decreased the rectal bleeding rate (Supplementary Fig. 5A). Histological analyses also showed that the TG mice maintained better epithelial crypt morphology with a lower epithelial damage score (Supplementary Fig. 5B). In agreement with this observation, the TG mice showed higher proliferation rates and decreased cell deaths in colonic epithelial tissue (Fig. 5D and 5E). To further exclude a possible effect of CAMK2γ in innate immune cells, we crossed CA-CAMK2γ fl/fl mice with Lyz2-Cre mice to over-express CA-CAMK2γ in myeloid cells (Supplementary Fig. 6A). In contrast to the FW control mice, the Lyz2-TG mice showed slightly greater DSS-induced body weight loss but similar colonic shortening and splenic enlargement to the FW control mice (Supplementary Fig. 6B and 6C). Therefore, we conclude that activation of CAMK2γ in colonic epithelial cells, but not that in immune cells, protects mice from colitis-induced tissue damage.
We then subjected TG mice and FW control mice to CAC induction, as illustrated in Fig. 3A. As expected, TG mice showed increased distal CAC compared to the FW control mice (Fig. 5F). The average tumor number per mouse was higher in the TG mice than that in the FW control littermates (Fig. 5G). The TG mice also showed an increased number of small tumors (Fig. 5G) as well as an increased proportion of high-grade tumors (Fig. 5G, supplementary Fig. 5C). Altogether, these results indicate that constitutive activation of CAMK2γ in colonic epithelial cells restores the colonic epithelial morphology change caused by DSS challenge, improves epithelial cell survival and proliferation, protects mice from colitis-induced epithelial damage and promotes CAC development, further demonstrating the role of epithelial CAMK2γ in modulating CAC development.
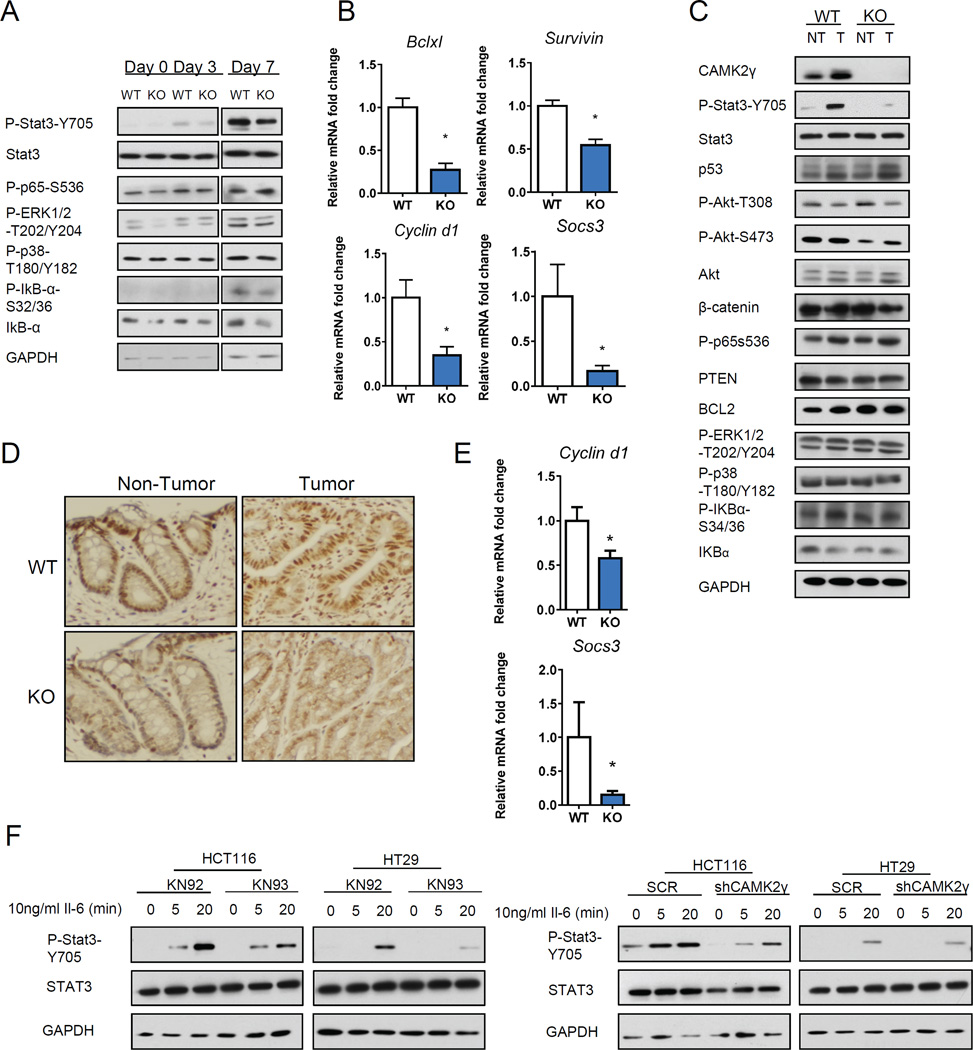
CAMK2γ promotes IEC survival and proliferation via enhancing STAT3 activation
DSS is a non-genotoxic carcinogen, which requires AOM co-injection to induce CAC44. Instead, administration of DSS leads to damage of the epithelial barrier and translocation of the microbiota. Bacterial infiltration-induced inflammation then leads to loss of the epithelial structure and extensive cell death. Next, tissue regeneration is initiated in response to the inflammation-induced damage signals. During this regeneration process, prolonged regeneration signals, including IL-6/IL-11, will activate anti-apoptotic pathways to antagonize cell death and further promote the compensatory proliferation of epithelial cells, which is critical for the development of CAC45. Survival and proliferation modulators, including p38, ERK1/2, NF-κB and STAT3, are reported to play essential roles in this process46–49. Because we observed enhancement of DSS-induced cell death and suppression of DSS-induced colonic epithelial proliferation in CAMK2γ KO mice (Fig. 1 and 2), we hypothesized that CAMK2γ KO might suppress cell survival signaling pathways. To test this hypothesis, we measured the activity of known survival modulators in DSS-challenged WT and CAMK2γ KO colonic tissue samples by western blotting (Fig. 6A). We did not observe any differences in the activities of p38 or ERK1/2, at day 7 after the start of DSS treatment. The protein level of IκBα, the negative regulator of NF-κB, was lower in KO colonic tissue, indicating a slightly higher NF-κB activity in KO colon tissues. In contrast, phosphorylation of STAT3, a key regulator of colonic epithelial cell survival, was significantly reduced in CAMK2γ KO mouse colitis samples (Fig. 6A). QRT-PCR results also indicated that the expression of several STAT3 target genes, which are involved in cell survival and proliferation, was decreased in colon tissues of KO mice (Fig. 6B). Similarly, decreased STAT3 phosphorylation and suppression of STAT3 target gene expression were also observed in CAMK2γ KO tumor tissues from mice treated as described in Fig. 2B (Fig. 6C–E). To further determine whether inhibition of CAMK2γ suppresses STAT3 phosphorylation, we treated human colon cancer cell lines with the CAMK2 inhibitor KN93, or its inactive analog KN92, together with IL-6. Indeed, KN93 suppressed IL-6-induced STAT3 phosphorylation (Fig. 6F). Knockdown of CAMK2γ expression by shRNA in CRC cell lines also inhibited IL-6-induced STAT3 phosphorylation (Fig. 6F, Supplementary Fig. 7). These results indicate that CAMK2γ KO suppresses the survival and proliferation of colonic epithelial cells, possibly through inhibiting IL-6-induced STAT3 activation.
Figure 6. CAMK2γ promotes intestinal epithelial cell survival and proliferation via enhancing STAT3 activation.
(A) Representative western blot analysis of the molecules involved in survival and proliferation signaling pathways in pooled colon tissues from mice with acute colitis. (For Day0 and Day3, n=3; For Day7, n=8) (B) Relative mRNA expression of STAT3 target genes in the colon tissues of DSS-challenged WT and KO mice (n=8). (C) Western blot analysis of molecules involved in survival and proliferation signaling pathways in pooled colonic lysate samples from AOM/DSS treated WT and KO mice. T, tumor tissues in colon; NT, paired adjacent non-tumor colon tissues; (D) Representative IHC staining of P-STAT3 in tumor and non-tumor tissues. (E) Expression of STAT3 target genes in WT and CAMK2γ KO CAC tissues. (F) Suppression of CAMK2γ activity by a specific inhibitor (KN93), but not the inactive analog KN92, decreased IL-6-induced STAT3 activation in human colorectal cancer cell lines. Knockdown of CAMK2γ by shRNAs in human colorectal cancer cell lines also decreased IL-6-induced STAT3 activation in vitro. See also Supplementary Fig. 7.
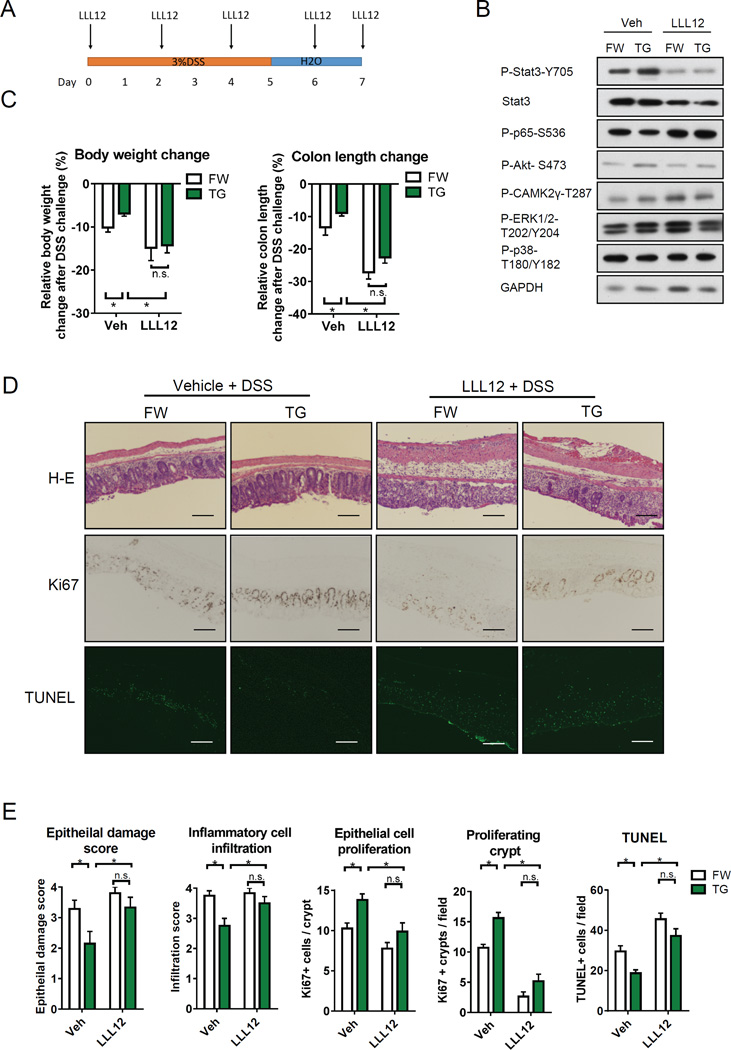
To confirm the requirement for STAT3 in mediating the effects of CAMK2γ in vivo, we injected the STAT3 inhibitor VII (LLL12) into both FW control and TG mice during DSS challenge (Fig. 7A). As expected, LLL12 suppressed STAT3 phosphorylation but did not affect the phosphorylation of CAMK2γ or other signaling pathways (Fig. 7B). Treatment with LLL12 enhanced weight loss, colon length shortening in both FW and TG mice (Fig. 7C). However, although CA-CAMK2γ protected mice treated with DSS and vehicle injection, there was no CA-CAMK2γ-induced protection after LLL12 administration (Fig. 7C). H&E, Ki67 and TUNEL staining also indicated that LLL12-treated TG mice showed similar levels of epithelial damage, immune cell infiltration, epithelial cell death, and proliferation compared to FW mice that received LLL12 injection (Fig. 7D and 7E). These results further demonstrate that CAMK2γ promotes colonic epithelial cell survival and proliferation via enhancing STAT3 activation.
Figure 7. Inhibition of STAT3 blocks the protective effects of CA-CAMK2γ on epithelial cell survival and proliferation in DSS treated mice.
(A) Scheme for LLL12 treatment in DSS-induced colitis on FW and TG mice. The colon tissues were analyzed on day 7. (B) Western blot analysis of molecules involved in survival and proliferation signaling pathways in pooled mouse colonic lysate samples. (C) DSS-induced changes in mouse body weight and colon length. (D) Representative images of H&E, Ki67 and TUNEL staining of mouse colon tissues. Scale bar indicate 200µm length. (E) epithelial damage score and inflammatory cell infiltration were calculated from the H&E staining shown in (D); the number of proliferating epithelial cells and crypts proliferation was calculated from the Ki67 staining shown in (D); Epithelial cell death was calculated from the TUNEL staining shown in (D). n=8. Results are presented as mean ± s.e.m.; *P<0.05, n.s., not significant.
DISCUSSION
In this study, we have identified a novel molecular pathway in a mouse model of inflammation-associated carcinogenesis. In this model, we show that the WNT signal induced by colitis activates CAMK2γ in the IECs to enhance STAT3 activation, thereby promoting CAC. Analyses of the UC patient cohort indicated a positive correlation of the expression levels between WNT5A and a set of STAT3 target genes (Supplementary Fig. 8). Consistently, we showed that CAMK2γ KO suppressed the development of CAC in mice. Interestingly, CAMK2γ in colonic epithelial cells, rather than in inflammatory cells, was critical for the development of CAC, while over-expression of CAMK2γ in IECs, but not in myeloid cells, ameliorated colitis-induced tissue injury and promoted tissue regeneration, resulting in enhanced CAC development. Although previous studies have established a role for CAMK2γ in immune cells to promote inflammation24, 25, we observed no difference in overall inflammation between WT and CAMK2γ KO mice. These results indicate an epithelial-specific role for CAMK2γ in determining the outcome of colitis-induced CAC development by promoting IEC survival and proliferation. However, we could not exclude the possibility that CAMK2γ might directly modulate immune responses in other types of cancers.
These results support the importance of non-canonical WNT signaling in colitis and CAC. In response to colitis, epithelial CAMK2γ was activated by a non-canonical WNT5A signal. This result is consistent with several recent studies showing that WNT5A is one of the WNT ligands with the highest expression level in colonic myofibroblasts from IBD patients and mouse colitis models36, 50, 51. Our results also uncovered an important role of non-canonical WNT/ CAMK2γ signaling in CAC development. Moreover, a recent study of mutation landscape in human CAC tissues shows that mutations in non-canonical WNT associated pathways, such as the Rho and Rac GTPase network components, are observed in about 50% of CAC samples, but rarely observed in sporadic CRC samples52. This further supports a role for non-canonical WNT pathways in CAC development. Activation of WNT5A/CAMK2γ signaling could be one of the essential signal pathways that drives CAC development. This study indicates that in addition to the well-known canonical β-catenin oncogenic pathway, highly activated non-canonical WNT5A/CAMK2γ signaling during colitis could also promote CAC development. Thus, maintenance of “WNT balance” is critical for colon cancer prevention and may also be important for other inflammation associated malignancies. Furthermore, up-regulation of non-canonical WNT signals, particularly WNT5A expression, is also observed in a variety of chronic inflammation diseases, including sarcoidosis and Helicobacter pylori infection, all of which are linked to increased cancer risk53, 54. In this scenario, it is possible that WNT5A/ CAMK2γ signaling also mediate other inflammation-associated malignancies.
Finally, we show that CAMK2γ may promote CAC development via enhancing STAT3 activity in IECs. It has been well established that the survival and expansion of pre-malignant epithelial cells, which rely on inflammation-related tissue repair signaling pathways during colitis, such as STAT3-mediated signaling pathway, is key for the development of CAC14, 16, 47. When such signaling pathways are blocked, the development of CAC will be suppressed. For instance, IEC-specific STAT3 KO mice have more severe tissue injury in colitis than wild type mice, which is due to suppression of cell survival and G2/M phase transitions47. Similar to CAMK2γ KO mice, STAT3 KO mice are highly resistant to CAC development. Furthermore, genetic ablation of cytokines that activate STAT3 also generates phenotypes similar to those of the IEC-specific STAT3 KO mice47, 55, 56. In contrast, mice with constitutively activated STAT3 are resistant to colitis-induced tissue damage, therefore are more susceptible to CAC development47, 55, 56. In this study, we show that CAMK2γ KO mice attenuate the activation of epithelial STAT3, thereby suppressing CAC development. The effect of CAMK2γ on STAT3 could possibly rely on a direct interaction between CAMK2γ and STAT3, as described in leukemia26, or through several other indirect mechanisms as previously reported57, 58. Interestingly, several studies indicate that CAMKII family members could also interact or directly activate other members of IL-6/STAT3 pathway, including JAK259, 60, implying the possibility that CAMK2γ may also function upstream of STAT3. However, further work is still needed to identify the specific molecular link between CAMK2γ and STAT3 activation, particularly in CAC. Although a major role for STAT3 in promoting cancer is now well established, transcription factors such as STAT3 are notoriously difficult to directly target with small-molecule drugs that disrupt protein-protein or protein-DNA interactions61. In addition to our new targeting approaches such as CpG-Stat3 siRNA, developing inhibitors targeting upstream activators of STAT3 pathway is considered as an alternative strategy for STAT3 inhibition62, 63. To this end, CAMK2γ could be a potential target for future drug development to treat CAC and other inflammation-associated malignancies.
METHODS
Animals
CAMK2γ KO mice (C57BL/6J background) were kindly provided by Johannes Backs at the University of Heidelberg64. Mice expressing a conditional (LoxP-flanked STOP cassette) constitutively active CAMK2γ (CA-CAMK2γ fl/fl) (B6/129 mixed background) were generated at the Animal Resources Center of City of Hope National Medical Center, as described in the Results section. CA-CAMK2γ fl/fl mice were crossed with Villin-Cre +/− mice to generate Cre− CA-CAMK2γ fl/wt (FW) mice and Cre+ CA-CAMK2γ fl/wt (TG) littermates. CD45.1, Villin-Cre and Lyz2-Cre mice were purchased from the Jackson Laboratory. All the mice were maintained in a pathogen-free animal facility under standard 12:12 h light:dark cycle, and were fed with standard rodent chow and water ad libitum. All procedures followed the NIH guidelines for the care and use of laboratory animals, and were approved by the City of Hope Institutional Animal Care and Use Committee.
Induction of CAC and acute colitis
For CAC, 7-week-old male mice received intraperitoneal (i.p.) injection of azoxymethane (AOM, 10 mg/kg) on day -7, and received 3% DSS (MPbio, Cat #: 0216011080) in drinking water on days 0–5, 21–26 and 42–47. Then, the mice were euthanized at the indicated time points. For acute colitis, the mice received 3% DSS challenge on days 0–5, and then were allowed to recover for another two days before samples were collected. 5-Bromo-2´-Deoxyuridine (BrdU, Sigma, Cat#: B5002, 10mg/kg body weight) was i.p. injected to the mice two hours before they were euthanized.
Generation of bone marrow chimeric mice
Chimeric mice were generated as described elsewhere65. Briefly, bone marrow cells were isolated from CAMK2γ KO and WT donor mice. Isolated bone marrow cells (1 × 106) were transplanted into irradiated (10Gy) recipient mice through tail vain injection. Recipient mice were allowed access to autoclaved water containing antibiotics (sulfamethoxazole and trimethoprim oral suspension, Hi-Tech) for three weeks. The mice were then returned to antibiotic-free water, to allow repopulation of intestinal microbiota. The bone marrow reconstitution efficiency was tested by measuring the CD45.1/CD45.2 ratios by flow cytometry five weeks after transplantation.
Histology staining and analysis
Colonic specimens were prepared and analyzed by pathologists at the City of Hope Pathology Core Lab. Histology and immunohistochemical staining procedures were described previously29. The antibodies used were as follows: BrdU (DAKO, Cat#: M0744), Ki67 (DAKO, Cat#: M7204), and P-Stat3 Tyr705 (Cell Signaling Technology, Cat#: 9145). TUNEL staining was performed using the Cell Death Detection Kit from Roche (Cat#: 11684795910), according to the manufacturer’s instructions. Standards for tumor grading, epithelial damage score and inflammatory cell infiltration score are described in Tables S1, S2 and S366.
RNA isolation and quantitative real-time PCR
Total RNAs were isolated using the RNeasy kit (QIAGEN, Cat#:74104). Reverse transcription was performed using the Invitrogen RT III system (Cat#: 18080051). The qRT-PCR was performed using the SYBR green and ABI 7500 system (Applied Biosystems). The primers used for qRT-PCR were generated using Invitrogen perfect primer design tool or qPrimerDepot67. Primer sequences were summarized in Table S4. The commercial kits were used according to the manufacturer’s instructions.
Western blotting and quantification
Western blotting was performed as previously described29. The antibodies used were described in Table S5. Quantification of the western blots was performed using the ImageJ software package, as described27.
LLL12 treatment
The STAT inhibitor LLL12 (Calbiochem, Cat#: 573131) was suspended in vehicle (5% DMSO, 0.9% saline) and then i.p. injected into DSS-treated mice with a dosage of 5 mg/kg on days 0, 2, 4, 6 and 7. Control mice only received vehicle injection.
Plasmid and virus infection
HCT116 and HT29 human CRC cell lines were purchased from ATCC, and cultured using the ATCC-recommended methods. Wnt5A-HA over-expression viruses were generated using the tetracycline-inducible virus system from Clontech. Generation of CAMK2γ knockdown cell lines was performed as described previously29.
Statistical Analysis
The data are presented as mean ± SEM. Student's two-tailed t test or one-way analysis of variance (ANOVA) with Dunn’s post-test were used to determine significant differences among groups (p<0.05).
Supplementary Material
Acknowledgments
We thank Dr. Johannes Backs for providing the Camk2γ KO mice. We thank Dr. Richard Ermel and the Animal Resource Center for the technical resources. We thank the pathologists from the City of Hope Pathology Core Lab for sample processing and analysis. We thank Dr. Fong-Fong Chu and Dr. Mei Kong at City of Hope for discussion. We also thank Dr. Nancy Linford for providing editing assistance. This work is supported in part by 2NCI R01-CA139158, the National Natural Science Foundation of China (81270601 and 81328016) and the Open Research Fund of State Key Laboratory of Cellular Stress Biology, Xiamen University (SKLCSB2016KF002). Research reported in this publication was also supported by the National Cancer Institute of the National Institutes of Health under award number P30CA33572. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.
Author Contributions: W.H. supervised the project, designed the experiments and revised the manuscript. X.M. and Z.M. designed the experiments, performed most of the experiments and wrote the manuscript. X.W., Z.X., Y.G., J.Z., L.D., B.K., M.H., and X.G. performed experiments. W.T. assisted with the transgenic mouse line generation. L.J., J.S., H.Y., and R.X. discussed the project, provided suggestions and revised the manuscript.
REFERENCES
- 1.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trinchieri G. Cancer and inflammation: an old intuition with rapidly evolving new concepts. Annual review of immunology. 2012;30:677–706. doi: 10.1146/annurev-immunol-020711-075008. [DOI] [PubMed] [Google Scholar]
- 3.Polk DB, Peek RM., Jr Helicobacter pylori: gastric cancer and beyond. Nature reviews Cancer. 2010;10:403–414. doi: 10.1038/nrc2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wotherspoon AC. A critical review of the effect of Helicobacter pylori eradication on gastric MALT lymphoma. Current gastroenterology reports. 2000;2:494–498. doi: 10.1007/s11894-000-0014-z. [DOI] [PubMed] [Google Scholar]
- 5.Arzumanyan A, Reis HM, Feitelson MA. Pathogenic mechanisms in HBV- and HCV-associated hepatocellular carcinoma. Nature reviews Cancer. 2013;13:123–135. doi: 10.1038/nrc3449. [DOI] [PubMed] [Google Scholar]
- 6.Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nature reviews Cancer. 2013;13:759–771. doi: 10.1038/nrc3611. [DOI] [PubMed] [Google Scholar]
- 7.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 8.Rubin DC, Shaker A, Levin MS. Chronic intestinal inflammation: inflammatory bowel disease and colitis-associated colon cancer. Frontiers in immunology. 2012;3:107. doi: 10.3389/fimmu.2012.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gillen CD, Walmsley RS, Prior P, Andrews HA, Allan RN. Ulcerative colitis and Crohn's disease: a comparison of the colorectal cancer risk in extensive colitis. Gut. 1994;35:1590–1592. doi: 10.1136/gut.35.11.1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jess T, Rungoe C, Peyrin-Biroulet L. Risk of Colorectal Cancer in Patients with Ulcerative Colitis: a Meta-Analysis of Population-Based Cohort Studies. Clin Gastroenterol Hepatol. 2012 doi: 10.1016/j.cgh.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 11.Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–535. doi: 10.1136/gut.48.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Roon AC, Reese G, Teare J, Constantinides V, Darzi AW, Tekkis PP. The risk of cancer in patients with Crohn's disease. Dis Colon Rectum. 2007;50:839–855. doi: 10.1007/s10350-006-0848-z. [DOI] [PubMed] [Google Scholar]
- 13.Ullman TA, Itzkowitz SH. Intestinal inflammation and cancer. Gastroenterology. 2011;140:1807–1816. doi: 10.1053/j.gastro.2011.01.057. [DOI] [PubMed] [Google Scholar]
- 14.Lasry A, Zinger A, Ben-Neriah Y. Inflammatory networks underlying colorectal cancer. Nature immunology. 2016;17:230–240. doi: 10.1038/ni.3384. [DOI] [PubMed] [Google Scholar]
- 15.Van Der Kraak L, Gros P, Beauchemin N. Colitis-associated colon cancer: Is it in your genes? World journal of gastroenterology. 2015;21:11688–11699. doi: 10.3748/wjg.v21.i41.11688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Foersch S, Neurath MF. Colitis-associated neoplasia: molecular basis and clinical translation. Cell Mol Life Sci. 2014;71:3523–3535. doi: 10.1007/s00018-014-1636-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lakatos PL, Lakatos L. Risk for colorectal cancer in ulcerative colitis: changes, causes and management strategies. World journal of gastroenterology. 2008;14:3937–3947. doi: 10.3748/wjg.14.3937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yashiro M. Ulcerative colitis-associated colorectal cancer. World journal of gastroenterology. 2014;20:16389–16397. doi: 10.3748/wjg.v20.i44.16389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 20.Tobimatsu T, Fujisawa H. Tissue-specific expression of four types of rat calmodulin-dependent protein kinase II mRNAs. J Biol Chem. 1989;264:17907–17912. [PubMed] [Google Scholar]
- 21.Bui JD, Calbo S, Hayden-Martinez K, Kane LP, Gardner P, Hedrick SM. A role for CaMKII in T cell memory. Cell. 2000;100:457–467. doi: 10.1016/s0092-8674(00)80681-9. [DOI] [PubMed] [Google Scholar]
- 22.Huang W, Ghisletti S, Saijo K, Gandhi M, Aouadi M, Tesz GJ, et al. Coronin 2A mediates actin-dependent de-repression of inflammatory response genes. Nature. 2011;470:414–418. doi: 10.1038/nature09703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Timmins JM, Ozcan L, Seimon TA, Li G, Malagelada C, Backs J, et al. Calcium/calmodulin-dependent protein kinase II links ER stress with Fas and mitochondrial apoptosis pathways. The Journal of clinical investigation. 2009;119:2925–2941. doi: 10.1172/JCI38857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu X, Yao M, Li N, Wang C, Zheng Y, Cao X. CaMKII promotes TLR-triggered proinflammatory cytokine and type I interferon production by directly binding and activating TAK1 and IRF3 in macrophages. Blood. 2008;112:4961–4970. doi: 10.1182/blood-2008-03-144022. [DOI] [PubMed] [Google Scholar]
- 25.Huang W, Ghisletti S, Perissi V, Rosenfeld MG, Glass CK. Transcriptional integration of TLR2 and TLR4 signaling at the NCoR derepression checkpoint. Molecular cell. 2009;35:48–57. doi: 10.1016/j.molcel.2009.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Si J, Collins SJ. Activated Ca2+/calmodulin-dependent protein kinase IIgamma is a critical regulator of myeloid leukemia cell proliferation. Cancer research. 2008;68:3733–3742. doi: 10.1158/0008-5472.CAN-07-2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gu Y, Chen T, Meng Z, Gan Y, Xu X, Lou G, et al. CaMKII γ, a critical regulator of CML stem/progenitor cells, is a target of the natural product berbamine. Blood. 2012 doi: 10.1182/blood-2012-06-434894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang YY, Zhao R, Zhe H. The emerging role of CaMKII in cancer. Oncotarget. 2015;6:11725–11734. doi: 10.18632/oncotarget.3955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meng Z, Li T, Ma X, Wang X, Van Ness C, Gan Y, et al. Berbamine inhibits the growth of liver cancer cells and cancer-initiating cells by targeting Ca(2)(+)/calmodulin-dependent protein kinase II. Molecular cancer therapeutics. 2013;12:2067–2077. doi: 10.1158/1535-7163.MCT-13-0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wirtz S, Neufert C, Weigmann B, Neurath MF. Chemically induced mouse models of intestinal inflammation. Nature protocols. 2007;2:541–546. doi: 10.1038/nprot.2007.41. [DOI] [PubMed] [Google Scholar]
- 31.Solomon L, Mansor S, Mallon P, Donnelly E, Hoper M, Loughrey M, et al. The dextran sulphate sodium (DSS) model of colitis: an overview. Comparative Clinical Pathology. 2010;19:235–239. [Google Scholar]
- 32.Liang J, Nagahashi M, Kim EY, Harikumar KB, Yamada A, Huang WC, et al. Sphingosine-1-phosphate links persistent STAT3 activation, chronic intestinal inflammation, and development of colitis-associated cancer. Cancer Cell. 2013;23:107–120. doi: 10.1016/j.ccr.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuhl M, Sheldahl LC, Malbon CC, Moon RT. Ca(2+)/calmodulin-dependent protein kinase II is stimulated by Wnt and Frizzled homologs and promotes ventral cell fates in Xenopus. J Biol Chem. 2000;275:12701–12711. doi: 10.1074/jbc.275.17.12701. [DOI] [PubMed] [Google Scholar]
- 34.De A. Wnt/Ca2+ signaling pathway: a brief overview. Acta biochimica et biophysica Sinica. 2011;43:745–756. doi: 10.1093/abbs/gmr079. [DOI] [PubMed] [Google Scholar]
- 35.Topol L, Jiang X, Choi H, Garrett-Beal L, Carolan PJ, Yang Y. Wnt-5a inhibits the canonical Wnt pathway by promoting GSK-3-independent beta-catenin degradation. The Journal of cell biology. 2003;162:899–908. doi: 10.1083/jcb.200303158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Planell N, Lozano JJ, Mora-Buch R, Masamunt MC, Jimeno M, Ordas I, et al. Transcriptional analysis of the intestinal mucosa of patients with ulcerative colitis in remission reveals lasting epithelial cell alterations. Gut. 2013;62:967–976. doi: 10.1136/gutjnl-2012-303333. [DOI] [PubMed] [Google Scholar]
- 37.Chassaing B, Aitken JD, Malleshappa M, Vijay-Kumar M. Dextran sulfate sodium (DSS)-induced colitis in mice. Current protocols in immunology / edited by John E Coligan [et al] 2014;104(Unit 15):25. doi: 10.1002/0471142735.im1525s104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perse M, Cerar A. Dextran sodium sulphate colitis mouse model: traps and tricks. Journal of biomedicine & biotechnology. 2012;2012:718617. doi: 10.1155/2012/718617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thaker AI, Shaker A, Rao MS, Ciorba MA. Modeling colitis-associated cancer with azoxymethane (AOM) and dextran sulfate sodium (DSS) Journal of visualized experiments : JoVE. 2012 doi: 10.3791/4100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De Robertis M, Massi E, Poeta ML, Carotti S, Morini S, Cecchetelli L, et al. The AOM/DSS murine model for the study of colon carcinogenesis: From pathways to diagnosis and therapy studies. J Carcinog. 2011;10:9. doi: 10.4103/1477-3163.78279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nghiem P, Saati SM, Martens CL, Gardner P, Schulman H. Cloning and analysis of two new isoforms of multifunctional Ca2+/calmodulin-dependent protein kinase. Expression in multiple human tissues. J Biol Chem. 1993;268:5471–5479. [PubMed] [Google Scholar]
- 42.Braun AP, Schulman H. The multifunctional calcium/calmodulin-dependent protein kinase: from form to function. Annual review of physiology. 1995;57:417–445. doi: 10.1146/annurev.ph.57.030195.002221. [DOI] [PubMed] [Google Scholar]
- 43.Blanpain C. Tracing the cellular origin of cancer. Nature cell biology. 2013;15:126–134. doi: 10.1038/ncb2657. [DOI] [PubMed] [Google Scholar]
- 44.Tanaka T, Kohno H, Suzuki R, Yamada Y, Sugie S, Mori H. A novel inflammation-related mouse colon carcinogenesis model induced by azoxymethane and dextran sodium sulfate. Cancer science. 2003;94:965–973. doi: 10.1111/j.1349-7006.2003.tb01386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saleh M, Trinchieri G. Innate immune mechanisms of colitis and colitis-associated colorectal cancer. Nat Rev Immunol. 2011;11:9–20. doi: 10.1038/nri2891. [DOI] [PubMed] [Google Scholar]
- 46.Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ, et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004;118:285–296. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 47.Bollrath J, Phesse TJ, von Burstin VA, Putoczki T, Bennecke M, Bateman T, et al. gp130-mediated Stat3 activation in enterocytes regulates cell survival and cell-cycle progression during colitis-associated tumorigenesis. Cancer Cell. 2009;15:91–102. doi: 10.1016/j.ccr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 48.Del Reino P, Alsina-Beauchamp D, Escos A, Cerezo-Guisado MI, Risco A, Aparicio N, et al. Pro-oncogenic role of alternative p38 mitogen-activated protein kinases p38gamma and p38delta, linking inflammation and cancer in colitis-associated colon cancer. Cancer research. 2014;74:6150–6160. doi: 10.1158/0008-5472.CAN-14-0870. [DOI] [PubMed] [Google Scholar]
- 49.Neufert C, Becker C, Tureci O, Waldner MJ, Backert I, Floh K, et al. Tumor fibroblast-derived epiregulin promotes growth of colitis-associated neoplasms through ERK. J Clin Invest. 2013;123:1428–1443. doi: 10.1172/JCI63748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hughes KR, Sablitzky F, Mahida YR. Expression profiling of Wnt family of genes in normal and inflammatory bowel disease primary human intestinal myofibroblasts and normal human colonic crypt epithelial cells. Inflammatory bowel diseases. 2011;17:213–220. doi: 10.1002/ibd.21353. [DOI] [PubMed] [Google Scholar]
- 51.Sato A, Kayama H, Shojima K, Matsumoto S, Koyama H, Minami Y, et al. The Wnt5a-Ror2 axis promotes the signaling circuit between interleukin-12 and interferon-gamma in colitis. Scientific reports. 2015;5:10536. doi: 10.1038/srep10536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Robles AI, Traverso G, Zhang M, Roberts NJ, Khan MA, Joseph C, et al. Whole-Exome Sequencing Analyses of Inflammatory Bowel Disease-Associated Colorectal Cancers. Gastroenterology. 2016;150:931–943. doi: 10.1053/j.gastro.2015.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Levanen B, Wheelock AM, Eklund A, Grunewald J, Nord M. Increased pulmonary Wnt (wingless/integrated)-signaling in patients with sarcoidosis. Respiratory medicine. 2011;105:282–291. doi: 10.1016/j.rmed.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 54.Zhao C, Ma H, Bu X, Wang W, Zhang N. SFRP5 inhibits gastric epithelial cell migration induced by macrophage-derived Wnt5a. Carcinogenesis. 2013;34:146–152. doi: 10.1093/carcin/bgs309. [DOI] [PubMed] [Google Scholar]
- 55.Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009;15:103–113. doi: 10.1016/j.ccr.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Putoczki TL, Thiem S, Loving A, Busuttil RA, Wilson NJ, Ziegler PK, et al. Interleukin-11 is the dominant IL-6 family cytokine during gastrointestinal tumorigenesis and can be targeted therapeutically. Cancer Cell. 2013;24:257–271. doi: 10.1016/j.ccr.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 57.Lo RK, Cheung H, Wong YH. Constitutively active Galpha16 stimulates STAT3 via a c-Src/JAK- and ERK-dependent mechanism. J Biol Chem. 2003;278:52154–52165. doi: 10.1074/jbc.M307299200. [DOI] [PubMed] [Google Scholar]
- 58.Zhao L, Cheng G, Jin R, Afzal MR, Samanta A, Xuan YT, et al. Deletion of Interleukin-6 Attenuates Pressure Overload-Induced Left Ventricular Hypertrophy and Dysfunction. Circulation research. 2016;118:1918–1929. doi: 10.1161/CIRCRESAHA.116.308688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nguyen A, Chen P, Cai H. Role of CaMKII in hydrogen peroxide activation of ERK1/2, p38 MAPK, HSP27 and actin reorganization in endothelial cells. FEBS letters. 2004;572:307–313. doi: 10.1016/j.febslet.2004.06.061. [DOI] [PubMed] [Google Scholar]
- 60.Gibson RM, Laszlo GS, Nathanson NM. Calmodulin-dependent protein kinases phosphorylate gp130 at the serine-based dileucine internalization motif. Biochimica et biophysica acta. 2005;1714:56–62. doi: 10.1016/j.bbamem.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 61.Yue P, Turkson J. Targeting STAT3 in cancer: how successful are we? Expert opinion on investigational drugs. 2009;18:45–56. doi: 10.1517/13543780802565791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kortylewski M, Swiderski P, Herrmann A, Wang L, Kowolik C, Kujawski M, et al. In vivo delivery of siRNA to immune cells by conjugation to a TLR9 agonist enhances antitumor immune responses. Nature biotechnology. 2009;27:925–932. doi: 10.1038/nbt.1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Furtek SL, Backos DS, Matheson CJ, Reigan P. Strategies and Approaches of Targeting STAT3 for Cancer Treatment. ACS chemical biology. 2016;11:308–318. doi: 10.1021/acschembio.5b00945. [DOI] [PubMed] [Google Scholar]
- 64.Backs J, Stein P, Backs T, Duncan FE, Grueter CE, McAnally J, et al. The gamma isoform of CaM kinase II controls mouse egg activation by regulating cell cycle resumption. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:81–86. doi: 10.1073/pnas.0912658106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brandl K, Sun L, Neppl C, Siggs OM, Le Gall SM, Tomisato W, et al. MyD88 signaling in nonhematopoietic cells protects mice against induced colitis by regulating specific EGF receptor ligands. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:19967–19972. doi: 10.1073/pnas.1014669107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gupta J, del Barco Barrantes I, Igea A, Sakellariou S, Pateras IS, Gorgoulis VG, et al. Dual function of p38alpha MAPK in colon cancer: suppression of colitis-associated tumor initiation but requirement for cancer cell survival. Cancer Cell. 2014;25:484–500. doi: 10.1016/j.ccr.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 67.Cui W, Taub DD, Gardner K. qPrimerDepot: a primer database for quantitative real time PCR. Nucleic acids research. 2007;35:D805–D809. doi: 10.1093/nar/gkl767. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.