Abstract
Brain imaging technology has allowed researchers to conduct rigorous studies of the dynamic course of alcoholism through periods of drinking, sobriety, and relapse and to gain insights into the effects of chronic alcoholism on the human brain. Magnetic resonance imaging (MRI) studies have distinguished alcohol-related brain effects that are permanent from those that are reversible with abstinence. In support of postmortem neuropathological studies showing degeneration of white matter, MRI studies have shown a specific vulnerability of white matter to chronic alcohol exposure. Such studies have demonstrated white-matter volume deficits as well as damage to selective gray-matter structures. Diffusion tensor imaging (DTI), by permitting microstructural characterization of white matter, has extended MRI findings in alcoholics. MR spectroscopy (MRS) allows quantification of several metabolites that shed light on brain biochemical alterations caused by alcoholism. This article focuses on MRI, DTI, and MRS findings in neurological disorders that commonly co-occur with alcoholism, including Wernicke’s encephalopathy, Korsakoff’s syndrome, and hepatic encephalopathy. Also reviewed are neuroimaging findings in animal models of alcoholism and related neurological disorders. This report also suggests that the dynamic course of alcoholism presents a unique opportunity to examine brain structural and functional repair and recovery.
Keywords: Magnetic resonance imaging, diffusion tensor imaging, MR spectroscopy, alcohol use disorder, thiamine, liver, cerebellum
Apart from direct effects on the brain, excessive alcohol consumption is associated with increased risk for trauma (i.e., traumatic brain injury) (Alterman and Tarter 1985; Chen et al. 2012), seizures (Eyer et al. 2011; Martindale et al. 2011), and stroke (de los Rios et al. 2012; Suzuki and Izumi 2013), each of which can have effects on brain structure independent of alcohol or each other. Furthermore, alcohol can alter the brain by affecting peripheral organs, including the digestive tract (e.g., Bienia et al. 2002; Duell et al. 2012), liver (e.g., Cederbaum 2012), heart (e.g., Roerecke et al. 2011), pancreas (e.g., Andersen et al. 2008), kidneys (e.g., Schaeffner and Ritz 2012), and lungs (e.g., Yeligar et al. 2012). Mechanisms of these indirect effects of alcohol on the brain are likely mediated via soluble factors, such as ceramides (e.g., de la Monte et al. 2012).
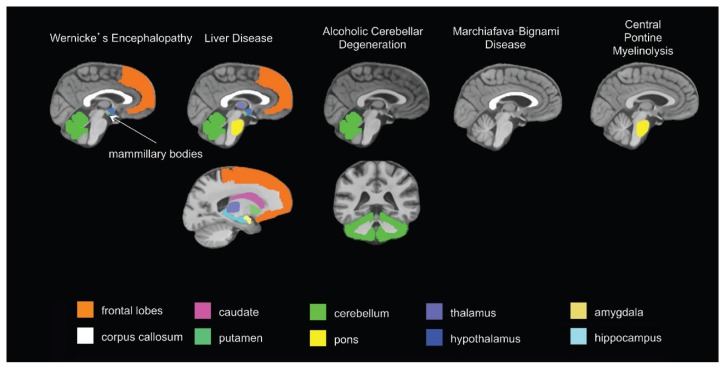
To evaluate alcohol’s central nervous system effects, researchers distinguish “uncomplicated alcoholism” (i.e., alcohol use disorder [AUD]) from the various clinically diagnosable consequences of chronic alcohol consumption, including Wernicke’s encephalopathy (WE), Korsakoff’s syndrome (KS), hepatic encephalopathy (HE), central pontine myelinolysis (CPM), alcoholic cerebellar degeneration (ACD), alcohol-related dementia (ARD), and Marchiafava-Bignami disease (MBD).1 The use of brain-imaging technology to evaluate clinically defined syndromes associated with chronic alcoholism, each with relatively unique radiological signatures (see table 1 and figure 1), provides guideposts for studying brain alterations associated with uncomplicated alcoholism.
Table 1.
Radiological Signatures in Brain Imaging of Patients with Alcoholism-Related Syndromes
| Alcoholism-Related Syndrome | Abbreviation | Primary Targeted Region(s) | Secondary Targeted Regions | Prevalence in Alcoholics (Percentage) |
|---|---|---|---|---|
| Wernicke’s Encephalopathy | WE | Mammillary bodies, periaqueductal gray matter, dorsal medulla, tectal plates, olivary bodies, pons, tissue surrounding 3rd ventricle | 12–18 | |
| Korsakoff’s Syndrome | KS | Mammillary bodies, hippocampus, thalamus, orbitofrontal cortices | Cerebellum, pons | 10–15 |
| Hepatic Encephalopathy | HE | Globus pallidus, substantia nigra | Corticospinal tract, cortex | 3–16 |
| Central Pontine Myelinolysis | CPM | Pons | Basal ganglia, thalamus, cerebral gray–white matter junctions | < 0.5 |
| Alcoholic Cerebellar Degeneration | ACD | Cerebellum | 0.4–42 | |
| Alcohol-Related Dementia | ARD | Frontal cortex | 3–24 | |
| Marchiafava-Bignami Disease | MBD | Corpus callosum | Cortex | < 0.002 |
Figure 1.
Brain regions targeted by alcoholism-related diseases.
Approximately 7 percent of adults age 18 and older have an AUD (Substance Abuse and Mental Health Services Administration 2013). Prevalence estimates of alcoholism-related syndromes are difficult to ascertain. Incidence estimates often are based on postmortem findings. Postmortem evaluation indicates a prevalence of 2 percent of WE in the general population; however, as many as 12 to 18 percent of alcoholics can have postmortem evidence of WE (Harper et al. 1988; Riethdorf et al. 1991; Thomson et al. 2002). Based on observations that 80 to 85 percent of patients with WE can develop KS, the estimated prevalence of KS is 11 to 12 percent of the alcoholic population (Day et al. 2013; Victor et al. 1971). Wernicke-Korsakoff syndrome (WKS) is used to refer to the presence of both WE and KS because of the close relationship between the two disorders.
Estimates of HE are derived from estimates of alcoholic cirrhosis, which can range from 8 percent to 20 percent (Bellentani et al. 1997; Mann et al. 2003; Sorensen et al. 1984). Mild HE occurs in up to 80 percent of cirrhotic patients, and overt HE occurs in up to 45 percent of cirrhotic patients (Bajaj 2008; Poordad 2007). One study estimated the incidence of CPM at 0.5 percent among the general population (Newell and Kleinschmidt-DeMasters 1996). However, prevalence is much higher (30 percent) among patients with liver transplants (Singh et al. 1994). For ACD prevalence, reports based on postmortem evaluation range from as low as 0.4 percent to as high as 42 percent of alcoholics (Riethdorf et al. 1991; Scholz et al. 1986; Stork 1967; Torvik and Torp 1986). Rates of ARD can depend on the setting, with facilities specializing in early identification and treatment of memory disorders reporting rates of 3 percent (McMurtray et al. 2006) and nursing homes reporting rates as high as 24 percent (Carlen et al. 1994; Oslin and Cary 2003; Ritchie and Villebrun 2008). Prevalence can also depend on the age of the population evaluated (i.e., higher prevalence of ARD is found in younger-onset [i.e., ages 45–64] dementia) (Draper et al. 2011b; Harvey et al. 2003). MBD appears to be very rare, with only about 250 cases reported between 1966 and 2001 (Helenius et al. 2001).
Human studies offer a full depiction of the consequences of chronic alcohol exposure but are limited by ethical considerations. That is, rigorous experimentation requires the ability to control for relevant variables such as the premorbid condition of the brain. The wide variation (or heterogeneity) of alcoholic populations examined with respect to genetic predisposition, age of onset, pattern of drinking, frequency of withdrawals, length of sobriety, nutritional, and hepatic status has hampered researcher attempts to isolate specific brain regions and mechanisms affected by alcohol, per se. This heterogeneity, and the complexity that it introduces, makes it difficult to thoroughly characterize the disorder. Animal models, in contrast to the indefinite natural course of alcohol use in humans, allow researchers to determine alcohol toxicity in a way that allows them to control for multiple genetic, environmental, and alcohol consumption factors. Animal models permit the study of underlying mechanisms, enabling researchers to better interpret findings from human studies.
On the other hand, animal models also have limitations. Species differences in brain structure and function—among myriad other differences between humans and other animals—can give inadequate information when animal data are applied to human disease. For example, mice models fail to mimic human inflammatory disease with respect to genomic responses (Seok et al. 2013), and corticosteroids disturb development in animals but not in humans (Needs and Brooks 1985). Furthermore, researchers have hypothesized that the design, conduct, and analysis of a mainstay of animal experiments are questionable (Matthews 2008) and rarely undergo meta-analytical review for consensus (Mignini and Khan 2006; Peters et al. 2006; Pound et al. 2004; Sandercock and Roberts 2002).
This article reports key findings in humans, from macrostructural findings using magnetic resonance imaging (MRI), microstructural findings using diffusion tensor imaging (DTI), and metabolic findings from MR spectroscopy (MRS). Studies of alcohol-related central nervous system disorders are used as a framework for findings in uncomplicated alcoholism. The article also examines studies of abstinence and relapse and current imaging studies of animal models of alcoholism and co-occurring brain disorders. The evidence suggests that human studies are necessary to identify and classify the brain systems modified by concomitants of alcoholism versus alcoholism, per se, and that animal models of alcoholism and its co-occurring brain disorders are essential for a mechanistic understanding of vulnerable brain systems.
Structural MRI
Since the early 1980s, conventional structural MRI has allowed researchers to visualize the living human brain. Detailed images of the brain are possible in part because the different brain tissue types (i.e., gray matter, white matter, and cerebrospinal fluid [CSF]) contain different proportions of water (Rumboldt et al. 2010). With MRI, the brain can be viewed from bottom to top (axial), from front to back (coronal), from left to right (sagittal), or at any oblique angle to these planes. This flexibility also enables greater accuracy in aligning images with internal landmarks, an essential consideration for ensuring consistency of data from replicate images from the same individual (Rohlfing 2006).
Structural MRI Findings in Alcoholism-Related Brain Diseases
Wernicke-Korsakoff Syndrome
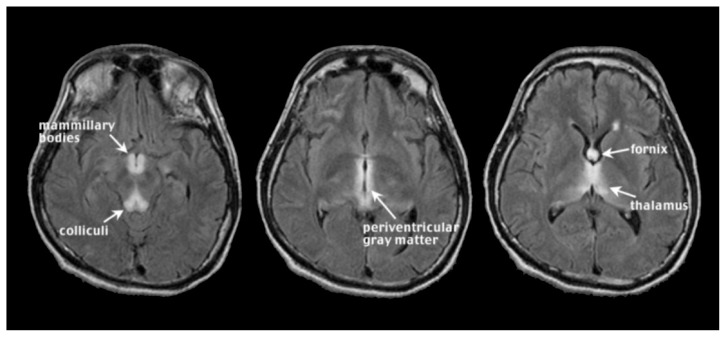
WE occurs with chronic alcoholism and thiamine deficiency. If untreated, WE patients can develop KS, a severe neurological disorder characterized by anterograde amnesia (Harper 2006; Zahr et al. 2011). Malnutrition, vomiting, and diarrhea are common in chronic alcoholism and can contribute to thiamine deficiency (Fields et al. 1994; Gloria et al. 1997; Morgan 1982; Ross et al. 2012). Further, the gastrointestinal tract’s ability to absorb necessary quantities of thiamine is diminished in alcoholics (Hoyumpa 1980; Thomson 2000), and the liver, which houses a large part of the body’s supplies of thiamine, may not be able to store thiamine in the same capacity if it is in a diseased state (Butterworth 2009; Levy et al. 2002). Classical clinical signs of WE included visual, gait, and mental disturbances (Victor et al. 1971), but more recent assessments describe mild, moderate, and severe signs and symptoms including anorexia, loss of memory, and emotional changes (Thomson et al. 2008). An MRI image of acute WE (see figure 2) has symmetrical bright spots, or hyperintensities, clearly visible on T2-weighted images, and those created by fluid attenuation inversion recovery2 (FLAIR). The bright spots appear in the midbrain gray matter surrounding the cerebral aqueduct (i.e., periaqueductal gray matter), mammillary bodies, and tissue surrounding the third ventricle3 (Lenz et al. 2002; Sullivan and Pfefferbaum 2009). These findings agree with postmortem diagnosis of WE, often requiring evidence of lesions in the mammillary bodies and periventricular areas (e.g., Caine et al. 1997). In addition, observed MR hyperintense areas in WE include the thalamus, cerebellar vermis (Murata et al. 2001), dorsal medulla, tectal plates (Ha et al. 2012), olivary bodies, and dorsal pons (Liou et al. 2012). MRI analysis of KS patients compared with unaffected research participants (i.e., nonalcoholic control subjects) revealed substantial volume shrinkage of the mammillary bodies in KS and a lesser but significant volume deficit in uncomplicated alcoholics (Sheedy et al. 1999; Sullivan et al. 1999b; but see Shear et al. 1996; Victor et al. 1989). In contrast with early MR studies suggesting that KS affects the mammillary bodies while sparing the hippocampi (Squire et al. 1990), more recent work demonstrates hippocampal volume deficits in KS (Sullivan and Marsh 2003). Other regions affected by KS are the thalamus, orbitofrontal cortex (Jernigan et al. 1991b), cerebellum, and pons (Zahr et al. 2009).
Figure 2.
Wernick’s encephalopathy (WE). In acute WE, magnetic resonance imaging (MRI) can detect symmetrical, bilateral hyperintense foci, visible on T2-weighted and fluid attenuation inversion recovery (FLAIR) images, in periaqueductal gray matter, mammillary bodies, and tissue surrounding the third ventricle.
Hepatic Encephalopathy (HE)
HE, occurring in acute or chronic liver disease, including acute liver failure and cirrhosis, is believed to arise, at least partially, from high levels of ammonia circulating in the blood. HE patients may appear confused and disoriented and have poor coordination (Prakash and Mullen 2010; Vaquero et al. 2003). T1-weighted images of HE show bilateral, symmetrical, and high-intensity signals in basal ganglia structures, particularly the globus pallidus and substantia nigra (Binesh et al. 2006; Cordoba et al. 2002; Naegele et al. 2000; Pujol et al. 1996; Taylor-Robinson et al. 1995) (see figure 3). T2-weighted FLAIR images show hyperintense signals along the corticospinal tract and diffuse increases in white-matter signal intensities in the cerebral hemispheres (Rovira et al. 2002, 2008). These in vivo MR features correspond with evidence of increased numbers of nonneuronal (i.e., glial) cells called astrocytes in basal ganglia and cerebral cortex of HE brains (Caine et al. 1997). Although discriminating features of WE and HE have been outlined, these diseases can be difficult to differentially diagnose and distinguish, because patients can appear to have similar symptoms and comparable MRI results, especially among alcoholics (Thorarinsson et al. 2011).
Figure 3.
Hepatic encephalopathy (HE). T1-weighted imaging in HE reveals bilateral, symmetrical, high-intensity signals in basal ganglia structures, particularly the globus pallidus and substantia nigra, probably due to manganese deposition and T1 shortening. T2-weighted fluid attenuation inversion recovery (FLAIR) shows hyperintense signals along the corticospinal tract and diffuse hyperintense white matter signal in the cerebral hemispheres.
Central Pontine Myelinolysis (CPM)
A significant proportion of CPM cases (Goebel and Herman-Ben Zur 1976; Messert et al. 1979) include a history of alcoholism. People with CPM, which is associated with electrolyte disturbances and specifically with aggressive correction of low sodium levels in the blood (i.e., hyponatraemia) (Chua et al. 2002), may have symptoms such as the inability to control facial movements, decreased voluntary muscle control (i.e., ataxia), and acute changes in consciousness (Kumar et al. 2006; Pfister et al. 1985). Classically, CPM was characterized by the presence of a symmetric triangular or “bat-wing” lesion in the pons (DeWitt et al. 1984; Gerard et al. 1987), with hypointense T1-weighted (Kleinschmidt-Demasters et al. 2006; Martin and Young 1995) and hyperintense T2-weighted (Buis and Wijdicks 2002; Kleinschmidt-Demasters et al. 2006; Pfister et al. 1985; Martin and Young 1995) images (see figure 4) reflecting damage to the protective covering of nerve cells (i.e., demyelination) as noted postmortem (Goldman and Horoupian 1981). The term osmotic myelinolysis (e.g., Chua et al. 2002; de Souza and Desai 2012) was coined to reflect the fact that other brain regions (e.g., basal ganglia, thalami, and cerebral gray–white matter junctions) are affected in CPM (e.g., Chen et al. 1996; Graff-Radford et al. 2011; Hagiwara et al. 2008; Harlan et al. 1988; Price et al. 1987; Waragai and Satoh 1998), despite suggestions that pathology in these other regions may not strictly represent demyelination (Kleinschmidt-Demasters et al. 2006; Kumar et al. 2006). Because a postmortem study of 112 autopsy cases of CPM patients reported that 28 percent could also be diagnosed with WE (Goebel and Herman-Ben Zur 1976), pontine dysfunction should be regarded as a cardinal clinical sign of CPM.
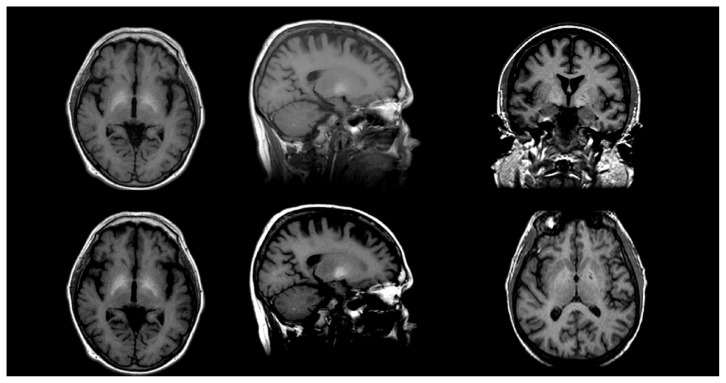
Figure 4.
Central pontine myelinolysis (CPM) is visualized as a hypointense T1 (left, sagittal slice) or hyperintense T2 (middle, right axial slices are early and late echo images) symmetric triangle or “bat-wing” lesion in the pons.
Alcoholic Cerebellar Degeneration (ACD)
ACD patients most frequently display ataxia, although other symptoms can include uncontrollable and repetitive eye movement (i.e., nystagmus) and speech problems resulting from impaired muscle control (i.e., dysarthria) (Fitzpatrick et al. 2012). Neuroimaging in ACD demonstrates damage disproportionately apparent in anterior superior portions of the cerebellar vermis (Sullivan et al. 2000a), with postmortem pathology indicating loss of cerebellar Purkinje cells (Feuerlein 1977).
Alcohol-Related Dementia (ARD)
Alcoholic dementia, or ARD, a currently preferred term, remains a controversial diagnosis because of confounding syndromes such as WE and HE. Nevertheless, certain clinically distinguishing features of ARD exist. It often occurs in socially isolated men at younger ages of onset (i.e., younger than age 65) than other types of dementia (Draper et al. 2011a; Ridley et al. 2013); deficits in visuospatial, executive, and memory functions (Schmidt et al. 2005); slower progression compared with other types of dementia (Gupta and Warner 2008); and partial reversibility (Oslin and Cary 2003). ARD is considered a frontal dementia (Stewart 2006). In support of such categorization, forensic evaluation of a sample of alcoholic brains noted a consistent pattern of synaptic loss in the superior laminae of the frontal cortex (i.e., Brodmann area 10), not related to liver disease (Brun and Andersson 2001).
Marchiafava-Bignami Disease (MBD)
MBD, a disease marked by mildly impaired mental status (e.g., confusion) and sometimes by dysarthria (Lee et al. 2011) or ataxia (Arbelaez et al. 2003), is poorly understood but may be related to nutritional deficiencies in addition to chronic alcohol consumption (Kawamura et al. 1985). Traditionally characterized by demyelination and necrosis of the corpus callosum, a number of reports identify cortical lesions in so-called MBD (Ihn et al. 2007; Johkura et al. 2005; Khaw and Heinrich 2006; Namekawa et al. 2013; Tuntiyatorn and Laothamatas 2008; Yoshizaki et al. 2010). Such data, however, represent single case studies and may reflect inaccurate MBD diagnoses. As observed in the pons in CPM, lesions (Clavier et al. 1986) appear hyperintense on T2-weighted images (Bano et al. 2009; Carrilho et al. 2013; Gambini et al. 2003) and hypointense on T1-weighted images (Bano et al. 2009; Carrilho et al. 2013; Kawamura et al. 1985) and often are located along the entire extent of the corpus callosum (Hillbom et al. 2014).
Given the aforementioned findings in clinically differential and diagnosable alcohol-related syndromes, the following section examines whether similar brain disorders also appear in alcoholics who do not manifest the full spectrum of symptoms present in these conditions. That is, how do the brains of uncomplicated alcoholics compare? Quantitative MRI has shown that relatively mild yet significant structural deficits characteristic of alcoholic syndromes can occur in uncomplicated alcoholics.
Structural MRI Findings in Uncomplicated Alcoholism
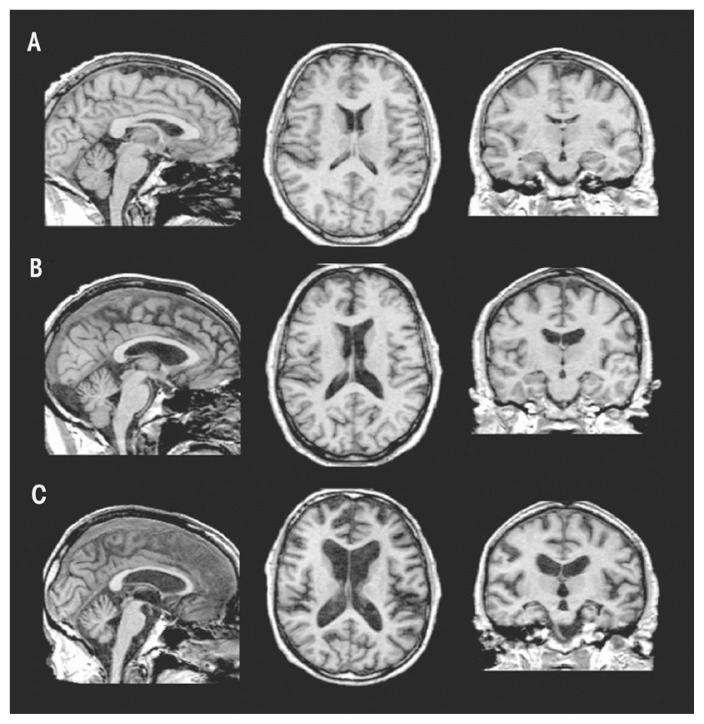
Relative to findings in WKS, research demonstrates mild volume deficits in the mammillary bodies (Shear et al. 1996; Sullivan et al. 1999), hippocampi, and thalami in uncomplicated alcoholics compared with healthy controls (De Bellis et al. 2005; Chanraud et al. 2007; Pitel et al. 2012; Sullivan 2003; van Holst et al. 2012). As shown in figure 5, these structures show a graded effect of volume deficits. That is, volume deficits are greatest in brains of subjects with KS (figure 5C) compared with brains of subjects with uncomplicated alcoholism (figure 5B) and brains unaffected by alcohol (figure 5A). Results suggest that mammillary-body damage is not prerequisite for the development of amnesia in alcoholism (Shear et al. 1996). MR findings also show hippocampal volume deficits in alcoholics compared with healthy controls (Agartz et al. 1999; Beresford et al. 2006; Kurth et al. 2004; Laakso et al. 2000; Sullivan et al. 1995; Wilhelm et al. 2008). Hippocampal volume deficits in alcoholism are influenced by age (Sullivan et al. 1995), even though age-related decline is difficult to detect in cross-sectional studies (Pfefferbaum et al. 2013; Raz et al. 2010; Sullivan et al. 2005b). Although deficits in hippocampal volume are not related to seizure incidence (Bleich et al. 2003; Sullivan et al. 1996), temporal-lobe white matter may be sensitive to alcohol-withdrawal seizures (Sullivan et al. 1996). Hippocampal volume shrinkage in alcoholism is attributed to loss of white matter and decreased axonal diameter (Harding et al. 1997). Glial cell loss (Korbo 1999) or reduced incorporation of newly formed neurons to the dentate gyrus (He et al. 2005; Nixon and Crews 2004), however, could also affect hippocampal volume in alcoholism.
Figure 5.
Brain volume deficits in a healthy control (A) compared with a subject with uncomplicated alcoholism (B) and a subject with Korsakoff’s syndrome (KS) (C). These structural MRIs show a graded effect of volume deficits, notable in the ventricular and sulcal cerebrospinal fluid (CSF)–filled spaces: subjects with KS > subjects with uncomplicated alcoholism > normal controls.
Other regions selectively affected in WE and KS include the orbitofrontal cortices (KS), periaqueductal gray matter, and tissue surrounding the third ventricle (WE). Reports suggest that propensity to relapse following sobriety is related to pronounced atrophy in bilateral orbitofrontal cortices (Beck et al. 2012; Cardenas et al. 2011; Durazzo et al. 2011; also see Rando et al. 2011). The third ventricle (i.e., enlargement) is sensitive to resumption of chronic alcohol consumption (Pfefferbaum et al. 2001; Sullivan et al. 2000b). There currently are no studies regarding periaqueductal gray-matter volume in uncomplicated alcoholics.
Key regions affected in HE include the globus pallidus and substantia nigra. Volume effects on these two structures have not been reported in uncomplicated alcoholics; however, in children with fetal alcohol syndrome, globus pallidus volume is reduced in size compared with unaffected children (Nardelli et al. 2011). In contrast, other basal ganglia nodes of reward circuitry have been described as affected in uncomplicated alcoholism (Durazzo et al. 2011; Makris et al. 2008): MRI studies have revealed smaller volumes of caudate (Boutte et al. 2012), putamen (Jernigan et al. 1991a), amygdala (Fein et al. 2006), and nucleus accumbens, especially in more recently sober alcoholics compared with healthy controls (Sullivan et al. 2005a). Given the role of the amygdala in emotional regulation and behavioral control (for review, see McBride 2002), however, researchers have speculated that premorbid amygdala volume deficits put individuals at heightened risk for developing AUD (Benegal et al. 2007; Clarke et al. 2008; Kamarajan et al. 2006).
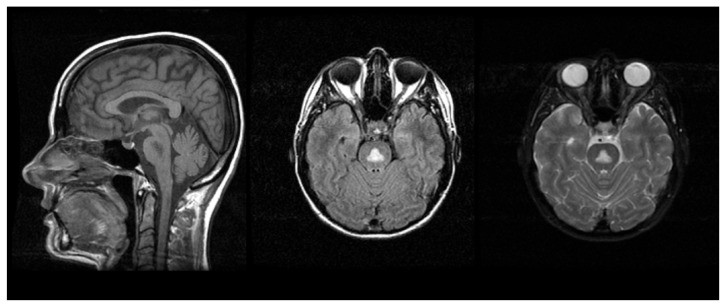
CPM targets the pons and ACD affects the cerebellum. Total infratentorial volume (including pons, cerebellar hemispheres, vermis, fissures, cisterns, and fourth ventricle) is significantly smaller in uncomplicated alcoholics than control subjects. The volume of the pons (Chanraud et al. 2009b; Pfefferbaum et al. 2002b; Sullivan 2003) and cerebellum (i.e., hemispheres) (Boutte et al. 2012; Chanraud et al. 2007, 2009a; De Bellis et al. 2005; Sullivan et al. 2000a,c) is smaller in uncomplicated alcoholics than in normal controls. Alcoholism-related volume deficits are also prevalent in gray and white matter (Shear et al. 1996; Sullivan et al. 2003) of the cerebellar vermis (Antunez et al. 1998; Piguet et al. 2006; Sullivan et al. 2006b, 2010), predominately in anterior superior but not posterior inferior regions (Sullivan et al. 2000a) (see figure 6).
Figure 6.
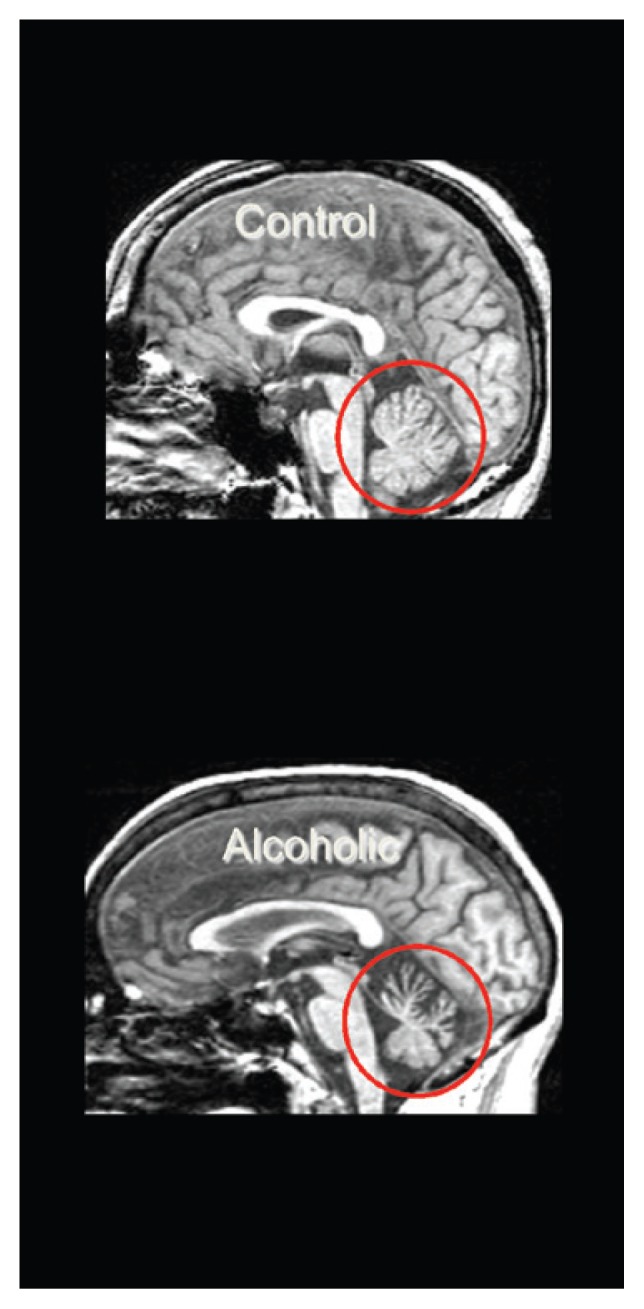
Cerebellar volume deficits in uncomplicated alcoholism. Midsagittal view of the brain, showing smaller volume of the anterior superior vermis of the cerebellum in an alcoholic man (bottom) compared with an age-matched control man (top).
The frontal cortex is notably damaged in ARD. With respect to cortical regions in uncomplicated alcoholism, various methods have shown significant, widespread shrinkage of both cortical gray and white matter with corresponding increases in CSF-filled spaces (Cardenas et al. 2007; Jang et al. 2007; Jernigan et al. 1991a; Mechtcheriakov et al. 2007; Pfefferbaum 1992). In particular, older (older than age 50) but not younger adult alcoholics show disproportionate deficits in both gray- and white-matter cortical volume, especially in the frontal lobes, when volumes are statistically adjusted for brain tissue decline associated with normal aging (Cardenas et al. 2005, 2007; Pfefferbaum et al. 1997). This is the case even in comparisons made in groups selected on alcohol consumption, where older alcoholics have consumed equivalent amounts over their lifetime as younger alcoholics.
Thinning of the corpus callosum occurs in uncomplicated alcoholics and is more prominent in the anterior than posterior regions (Estruch et al. 1997; Pfefferbaum et al. 1996). As with WE and KS, evidence for MBD-like pathology in uncomplicated alcoholism raises the possibility that brain damage occurs on a continuum. The following section examines how brain structures and function respond when drinking stops.
Structural MRI Findings in Recovery From Alcoholism
Longitudinal MRI investigations show that the ventricles become smaller following weeks (Schroth et al. 1988; Zipursky et al. 1989) or months (Shear et al. 1994) of drinking cessation. Reduction of lateral ventricles precedes reduction of third-ventricular volume (Pfefferbaum et al. 1995) and may be related to improvements in hematocrit, hemoglobin, and red blood cell counts (Pfefferbaum et al. 2004). The following brain structures increase in volume in response to abstinence: the entire cerebral cortex (Liu et al. 2000); temporal, insular, and anterior cingulate cortices (Cardenas et al. 2007); amygdala (Wrase et al. 2008) (a finding that would argue against a premorbid volume deficit); thalamus (Cardenas et al. 2007); hippocampus (Liu et al. 2000, Wrase et al. 2008); brainstem; and cerebellar cortex (Cardenas et al. 2007; Liu et al. 2000).
Sober alcoholics reveal several associations between brain-volume gain, as determined by MRI, and improvement in neuropsychological test performance: Reduced lateral-ventricle volume is related to improved memory performance (Rosenbloom et al. 2007), reduced third-ventricle volume is related to improved nonverbal short-term memory performance (Sullivan et al. 2000b), and reduced fourth-ventricle volume is related to improvement in measures of ataxia (Rosenbloom et al. 2007).
The brain’s capacity to return to “normal” following long-term sobriety is unknown. Short-term (6 weeks) abstinence seems sufficient to observe some brain-volume recovery but does not result in equivalent brain volumes between recovering chronic alcoholics and healthy controls (Mann et al. 2005). It is difficult to determine whether recovery is complete. Aging is a factor. That is, older alcoholics exhibit reduced capacity for recovery compared with younger alcoholics (Fein et al. 1990; Munro et al. 2000; Reed et al. 1992; Rourke and Grant 1999). Longer periods of abstinence may be required for follow-up investigations. Some brain damage, such as neuronal loss (Harper 2007), may be irreversible, even with extended abstinence.
Despite evidence for recovery of brain volume with abstinence, the mechanisms accounting for recovery remain unclear. One hypothesis, brain rehydration, was not supported by early human research studies (Schroth et al. 1988). An alternative explanation suggests that new neurons are created (i.e., neurogenesis) (e.g., Mandyam and Koob 2012): It is unlikely, however, that enough neurons could be made to replace the volume loss observed in chronic alcoholism. Nor is it clear that new neurons can migrate from neurogenic zones to distant areas of volume loss (Rakic 2002). On the other hand, adequate volume recovery may be explained by white-matter regeneration, because glial cells (i.e., oligodendroctyes) have the capacity to repair myelin and remyelinate neurons (Kipp et al. 2012), and oligodendrocyte progenitor cells have the potential to migrate long distances (Tirotta et al. 2010). Indeed, alcoholics who relapse have decreased white matter (Pfefferbaum et al. 1995), whereas continued abstinence is associated with increased white matter (Shear et al. 1994), notably in the corpus callosum and subcortical white matter (Cardenas et al. 2007).
Turning from studies with humans to animals, the following section examines imaging studies in models of alcoholism and related disorders.
Using Animal Models and Structural MRI to Study Alcoholism-Related Brain Disease
WE
There are two experimental approaches to model WE in rodents. The slower approach uses a thiamine-deficient diet (i.e., feeding with a thiamine-deficient chow), which can take 3–4 weeks to produce symptoms. Behavioral symptoms can be achieved in ~2 weeks using a combination of a thiamine-deficient chow and intraperitoneal (i.p.) administration of a thiamine pyrophosphokinase inhibitor such as pyrithiamine (Hazell and Butterworth 2009). Both models result in symptoms that mimic those observed in humans with WE (Pitkin and Savage 2001). Structural MRI findings in thiamine-deficient animals show similar patterns of brain changes, including hyperintense signals observed on T2-weighted images in thalamus, collicular bodies (Dror et al. 2010; Jordan et al. 1998; Pfefferbaum et al. 2007; Zahr et al. 2014a), hypothalamus, hippocampus (Jordan et al. 1998), mammillary bodies (Pfefferbaum et al. 2007), corpus callosum, and superior cerebellar peduncles (Dror et al. 2010). Thiamine deficiency may cause degeneration through neuroinflammatory mechanisms (Abbott 2000; Hazell and Butterworth 2009). In rats, inflammatory genes were highly expressed in vulnerable brain regions (Vemuganti et al. 2006). MRI in animal models permits further probing of the effects of thiamine deficiency on the brain and can be used to determine susceptible brain regions as a function of time of insult (Dror et al. 2010; Zahr et al. 2014a) as well as relationships between neuroinflammatory markers and brain insult (Zahr et al. 2014a). Such studies have also been used to confirm a mechanism of toxicity suspected based on research in humans (e.g., Harper 1980; Koguchi et al. 2004; Navarro et al. 2008): that glucose loading in a thiamine-deficient state can precipitate WE (Jordan et al. 1998; Zahr et al. 2014a), likely involving a breakdown of the blood–brain barrier (Nixon et al. 2008; Zelaya et al. 1995). In animals, postmortem followup can be used to confirm and extend in vivo findings. For example, electron microscopy showed a higher percentage of small fibers and myelin thinning in the corpus callosa of thiamine-deficient animals relative to controls (He et al. 2007).
Research with animals demonstrates that thiamine deficiency impairs several biochemical pathways requiring the thiamine derivative thiamine pyrophosphate (e.g., transketolase, pyruvate dehydrogenase, and α-ketoacid dehydrogenase) (Thomson et al. 2012), thereby interfering with carbohydrate metabolism (for energy production), lipid metabolism (for production and maintenance of myelin), and amino acid metabolism (for production of glucose-derived neurotransmitters; for example, glutamate and γ-aminobutyric acid [GABA]) (Sechi and Serra 2007; Vetreno et al. 2012). Consequently, the function of essential thiamine-requiring enzymes in the brain (e.g., transketolase, pyruvate dehydrogenase, and α-ketoacid dehydrogenase) is compromised, leading to oxidative stress, cellular energy impairment, and eventually neuronal loss (Thomson et al. 2012).
Evidence also shows that thiamine deficiency alters norepinephrine, dopamine (Mousseau et al. 1996), serotonin (Nakagawasai et al. 2007), and histamine (Langlais et al. 2002; McRee et al. 2000) synthesis and catabolism pathways. Thiamine deficiency may target focal brain areas such as the thalamus because, relative to other brain structures, it has lower levels of monocarboxylic acid transporters and acetyl-CoA-synthetase. This makes these areas less capable of generating energy from acetate (Qin and Crews 2014), which is a potential source of cellular energy in place of glucose in alcoholism (Volkow et al. 2013).
Current rodent models to study HE include models of acute and chronic liver failure (Butterworth et al. 2009; Diaz-Gomez et al. 2011). According to the International Society for Hepatic Encephalopathy, however, “At this time, there are no satisfactory animal models of Type C HE resulting from end-stage alcoholic liver disease or viral hepatitis, the most common etiologies encountered in patients” (Butterworth et al. 2009, p. 783). In addition, no MR-imaging studies to date have used rodent models of HE. Imaging studies in cats, dogs, and monkeys (Moon et al. 2012; Torisu et al. 2005; Zhou et al. 2012) typically recapitulate the human condition, showing nonspecific sulcal widening and hyperintensities in lentiform nuclei (i.e., putamen and globus pallidus of the basal ganglia) (Torisu et al. 2005; Zhou et al. 2012). Animal models of HE have been used to evaluate potential mechanisms of pathology, such as the contribution of excess ammonia in the blood (i.e., hyperammonemia) (Cauli et al. 2014) or lactate (Bosoi et al. 2014). Animal models of HE have also been used to explore treatment strategies for HE (e.g., hypothermia) (Barba et al. 2008).
CPM
Using a rat model of CPM to study white-matter degeneration, it was found that blood–brain barrier breakdown, detected with MRI, was associated with a higher risk of developing demyelination, as detected using postmortem histopathology (Adler et al. 2000). This study demonstrated that blood–brain barrier disruption exposes oligodendrocytes to substances normally excluded from the brain. This supports hypotheses from human postmortem studies suggesting that damage to the pons may be linked to reduced blood flow, as indicated by findings that basilar artery architecture is altered in CMP (De Reuck et al. 1975).
Although there are no known studies using structural MRI in animal models of ACD, ARD, or MBD, the following section examines animal studies in uncomplicated alcoholism.
Structural MRI Findings in Animal Models of Uncomplicated Alcoholism
An important initial report in the rodent MRI literature was the demonstration that brain growth continues beyond what would be considered adulthood in rats bred to prefer alcohol (i.e., alcohol-preferring rats, or P rats). Indeed, whole-brain volume in such rats continued to grow until approximately postnatal day 450 (Sullivan et al. 2006a), well past adulthood, which is typically considered as postnatal day 90 (Bell et al. 2013). Baseline studies (in the absence of alcohol [i.e., EtOH] exposure) also suggest that brains of alcohol-preferring rats are different relative to their wild-type counterparts, including reduced gray-matter volume in thalamus, ventral tegmental area, and insular and cingulate cortices (Gozzi et al. 2013).
One of the most consistent findings in alcohol-exposed rodents, ventricular enlargement, varies with timing and method of alcohol exposure. It is far more pronounced in rats achieving average blood alcohol levels (BALs) of 250 mg/dL in just 4 days of involuntary binge-type administration of EtOH (Zahr et al. 2010, 2013, 2014b) than in rats achieving average BALs of 200 mg/dL over 24 weeks using vapor EtOH exposure (Pfefferbaum et al. 2008) or P rats gradually achieving average BALs of 125 mg/dL with voluntary EtOH consumption (Pfefferbaum et al. 2006a), where only modest ventricular enlargement was noted (cf., Fadda and Rossetti 1998; Nixon 2006). Even repeated binge exposures (i.e., 5 cycles of 4 days of intragastric binge EtOH exposure with 1 week abstinence in between), do not result in persistent effects on the brain detectable with MRI (Zahr et al. 2015). Although ventricular size increases with each binge EtOH exposure, there is rapid recovery during each week of abstinence (Zahr et al. 2015). Such studies suggest that EtOH alone, at least in the exposure protocols evaluated with MRI, does not result in the characteristics observed in human alcoholics. Conversely, rats exposed to vaporized EtOH during adolescence are reported to show persistent effects (i.e., ventricular enlargement and deficits in hippocampal volume) into adulthood (Ehlers et al. 2013; Gass et al. 2014). Mice exposed to EtOH during adolescence are similarly purported to exhibit long-lasting regional brain-volume deficits in the olfactory bulb and basal forebrain (Coleman et al. 2011, 2014). These results suggest that the adolescent rodent brain may be more vulnerable to enduring toxic effects of EtOH than the adult rodent brain.
In monkeys trained to voluntarily consume alcohol, those that drank at least 3 g/kg EtOH per day for 15 months showed significant brain-volume shrinkage in the cerebral cortices (Kroenke et al. 2014). Because these animals were well nourished, these results suggest a direct relationship between oral EtOH intake and measures of decreased brain gray-matter volume.
Microstructural DTI
A number of sources provide extensive descriptions of the principles of DTI (Basser and Jones 2002; Chien et al. 1990; Gerig et al. 2005; Jones 2005; LeBihan 2001, 2003; Pierpaoli et al. 1996; Poupon et al. 1999; Sullivan and Pfefferbaum 2011). Briefly, DTI takes advantage of the fact that MR images of the brain are predominantly maps of water protons with contrast created by their immediate environment and their motility. In regions with few or no constraints imposed by physical boundaries, such as CSF in the ventricles, water movement is random and uniform in every direction and is therefore isotropic. In contrast to CSF, the path of a water molecule along a white-matter fiber is constrained by physical boundaries such as the axon sheath, causing greater movement along the long axis of the fiber than across it. This movement is called anisotropic; diffusion along the long axis of a fiber (axial or longitudinal diffusion) is greater than diffusion across the fiber (radial or transverse diffusion) (Song et al. 2002).
DTI findings are described in terms of diffusion. The magnitude of diffusion, referred to as mean diffusivity (MD) or the apparent diffusion coefficient (ADC), is calculated mathematically. Increased MD corresponds to white-matter damage. Fractional anisotropy (FA), ranging between 0 and 1, reflects axonal integrity, with lower integrity reflected by FA values closer to 0. Thus, disruption of white-matter microstructure detectable with DTI can reflect compromised myelin, cytoskeletal structure, or axonal density (Basser 1995; Basser and Pierpaoli 1996; Spielman et al. 1996).
Several approaches have been used to quantify DTI metrics. One of the more desirable approaches is the use of quantitative fiber tracking, which is able to evaluate fibers along their entire length and can thus detect compromised white matter. This technique can be used to depict selective commissures (e.g., corpus callosum), projection fibers, and association fibers.
DTI Findings in Alcoholism-Related Brain Disorders
In one study, DTI in alcoholics with (n = 7) and without (n = 20) WKS showed FA deficits in the fornix and cingulum bundle of the Papez or medial limbic circuit, measured using tract-based spatial statistics (TBSS). These FA effects were greater in alcoholics with WKS relative to those without it (Segobin et al. 2015). The number of tracts in the fornix appears to be reduced only in WKS patients (Nahum et al. 2015).
Studies of people who have alcohol-related cirrhosis with HE have reported elevated MD in several white-matter bundles, including the corpus callosum, internal capsule, and frontal white matter (Kale et al. 2006), and effects on both FA and MD of occipital white matter (Kumar et al. 2008). HE caused by alcoholism compared with other forms of HE (e.g., as a result of viral infection or primary biliary cirrhosis) appears to have different effects on DTI parameters (Miese et al. 2006), with more widespread changes in FA and MD in alcoholic relative to nonalcoholic cirrhosis (Ahluwalia et al. 2015). When researchers induced hyperammonemia in cirrhotic patients, an increase in ADC in brain white matter was observed, supporting excess ammonia in the blood as a mechanism driving cerebral edema (Mardini et al. 2011).
DTI showed elevated MD in the middle cerebellar peduncles with no effects on corticospinal tracts in a study participant with CPM relative to three healthy comparison participants (Min et al. 2012; Nair et al. 2012).
The largest DTI study of MBD to date included six study participants, five with a history of chronic alcoholism. All six showed hyperintense signals on diffusion images and low ADC of the corpus callosum. Researchers observed cortical lesions in frontoparietal regions in three of six study participants with the poorest outcomes (Menegon et al. 2005). Remaining DTI studies of MBD were case studies (e.g., Tuntiyatorn and Laothamatas 2008) showing low ADC along the entire corpus callosum (Bano et al. 2009; Wenz et al. 2014), with FA values diminishing progressively from front to back (Pacheco et al. 2014; Sair et al. 2006). No known DTI studies have been conducted in patients with ACD or ARD.
DTI Findings in Uncomplicated Alcoholism
DTI has revealed microstructural damage related to alcoholism in cerebral areas that appear intact in structural MRI analyses (e.g., Pfefferbaum and Sullivan 2002; Pfefferbaum et al. 2006b; Sullivan et al. 2003). Corpus callosum findings in uncomplicated alcoholics are common and, as observed for MBD, show greater anterior than posterior effects (e.g., Arnone et al. 2006; Konrad et al. 2012; Liu et al. 2010; Pitel et al. 2010; Schulte et al. 2005). Quantitative fiber tracking has demonstrated greater FA deficits in anterior than in posterior fibers of supratentorial and infratentorial white-matter bundles in alcoholics compared with healthy controls, as well as low FA in tracts of the corpus callosum, centrum semiovale, internal and external capsules, fornix, superior cingulate, and longitudinal fasciculi (Fortier et al. 2014; Müller-Oehring et al. 2009; Pfefferbaum and Sullivan 2005; Pfefferbaum et al. 2000, 2002a, 2009a; Trivedi et al. 2013). Frontolimbic (Harris et al. 2008; Monnig et al. 2013), fronto-parietal (Maksimovskiy et al. 2014), fronto-occipital (Bagga et al. 2014), fronto-cerebellar (Sullivan and Pfefferbaum 2005), cortico-striatal (Yeh et al. 2009), and cortico-pontine (Chanraud et al. 2009b) fibers are also affected in alcoholics relative to healthy controls.
Studies have also examined DTI- function relationships in alcoholism. FA in anterior cingulate and motor areas correlates with executive and psychomotor performance (Konrad et al. 2012), FA in the splenium correlates with working memory (Pfefferbaum et al. 2000), and FA in several regions (corpus callosum, parietal, occipital, and frontal white-matter) correlates with performance on the Iowa Gambling Task (Zorlu et al. 2013). A double dissociation was found showing that higher diffusivity in sensory- motor and parietal bundles was associated with poorer balance but not psychomotor speed, whereas higher diffusivity in prefrontal and temporal bundles was associated with slower psychomotor speed but not balance (Pfefferbaum et al. 2010). DTI changes in multiple supratentorial and infratentorial fiber systems in alcoholics correlated with impairment in speeded performance and postural stability (Pfefferbaum et al. 2009b), frontal fiber integrity connecting left and right hemispheres predicted performance on a coordinated psychomotor task (Rosenbloom et al. 2008), and number of reconstructed fibers running between the pons and the midbrain was related to cognitive flexibility performance (Chanraud et al. 2009b). Gray-matter diffusivity in the hippocampus, which is lower in alcoholics than in healthy controls, is related to episodic memory impairment (Chanraud et al. 2009a).
DTI Findings in Recovery from Alcoholism
Similar to structural MRI findings demonstrating pronounced tissue- volume shrinkage of orbitofrontal cortices in abstinent alcoholics who were likely to resume drinking (e.g., Beck et al. 2012; Cardenas et al. 2011; Durazzo et al. 2011), DTI identified alcoholic individuals more likely to resume drinking 6 months following initial evaluation based on lower FA and higher diffusivity in frontal white matter at baseline (Sorg et al. 2012). Increases in FA and decreases in diffusivity have been interpreted as evidence for white-matter recovery with abstinence. Studies have shown recovery in corpus callosum at 1 year compared with 2 weeks of abstinence (Alhassoon et al. 2012) and in frontal white matter at 1 month compared with 1 week of abstinence, at least in nonsmoking, sober alcoholics (Gazdzinski et al. 2010). Other reports suggest that some white-matter impairments persist after 6 to 30 months of recovery in alcoholics relative to healthy controls (Zorlu et al. 2014). In a seminal longitudinal study of 47 alcoholic and 56 healthy controls study participants, Pfefferbaum and colleagues (2014) reported that, despite abnormally low FA, age trajectories of the alcoholics who abstained were positive and progressing toward normality, whereas those of the relapsing alcoholics and control subjects were negative.
DTI Findings in Animal Models of WE
DTI data have been collected in animal models of WE but not in other concomitants of alcoholism.
In the study in which WE was induced by thiamine deficiency, animals were imaged at baseline, presymptomatic stage (day 10), symptomatic stage (days 12 and 14), and after recovery on days 31 and 87. A decrease in FA in the inferior colliculi was first noted on day 10 but showed recovery on day 87. On the other hand, the FA decrease in the thalamus first noted on day 12 persisted through day 87 (Dror et al. 2010). This model was also used in a pharmacological DTI study in which animals were exposed to rasagiline, a selective monamine oxidase B inhibitor, as a potential protective agent against thiamine-deficiency–induced brain damage (Dror et al. 2014). In addition to reducing ventricular enlargement, rasagiline appeared to ameliorate the effects of thiamine deficiency on the FA decrease in the thalamus (Dror et al. 2014). Histopathology showed that treatment with rasagiline reduced the lesions in thalamus and colliculi observed in the thiamine-deficient brain (Eliash et al. 2009). Rasagiline has not been evaluated in human patients with WE.
DTI Findings in Animal Models of Uncomplicated Alcoholism
Adolescent animals exposed to intermittent EtOH and evaluated postmortem showed no effects on FA but reduced axial diffusivity (hippocampus, cortex, and cerebellum), reduced radial diffusivity (hippocampus and cortex), and reduced MD (cerebellum and corpus callosum) in several brain regions (Vetreno et al. 2016). Adult rats exposed to a single dose of EtOH showed a slight and transient reduction, relative to unaffected rats, in ADC in brainstem (Kong et al. 2013), frontal lobe, hippocampus, thalamus, and cerebellum (Liu et al. 2014). These findings were interpreted as reflecting the development of cytotoxic brain edema, as histological analysis showed cell swelling and narrowed extracellular spacing (Kong et al. 2013).
Whereas chronic exposure to vaporized EtOH did not result in detectable effects on FA or MD, binge EtOH exposure resulted in transient decreases in FA and transient increases in MD (Pfefferbaum et al. 2015). Together, these results suggest that DTI can detect acute and subchronic effects on the brain, but that chronic exposure to EtOH can result in brain adaptations such that effects on FA and MD are no longer discernable.
Magnetic Resonance Spectroscopy
Although MRI primarily depicts the distribution of water protons, similar technology can also be used to obtain information about chemical constituents other than water, primarily due to a small frequency shift, or “chemical shift,” relative to the water signal. The acquisition of MR-detectable signals other than those of water and fat is referred to as MRS and is an in vivo application of traditional laboratory-based NMR spectroscopy.
MRS reveals information about several biochemicals, or metabolites, in the brain. The largest signals arise from N-acetylaspartate (NAA), creatine and phosphocreatine (i.e., total creatine [tCr]), and choline-containing compounds (Cho). Signals from the combined resonances of glutamate (Glu) and glutamine (Gln) (i.e., Glx) are also sometimes reported, as are myo-inositiol (mI) and lactate (lac). Signals from Glu and GABA can also be detected under certain conditions.
MRI and Signals for Four Prominent Metabolites
NAA
The predominant in vivo proton signal is NAA, with contributions from other N-acetyl compounds, especially N-acetyl aspartyl glutamate. NAA is found almost exclusively in neurons (Petroff et al. 1995; Urenjak et al. 1992, 1993) and, thus, is considered a measure of neuronal integrity. Postmortem (Cooper 1972; Koller et al. 1984; Nadler and Cooper 1972) and MRS (Kwo-On-Yuen et al. 1994; Petroff et al. 1995) studies have shown NAA levels to be higher in gray than in white matter in healthy study participants, as have in vivo studies (Doyle et al. 1995; Lim and Spielman 1997; Lim et al. 1998; Moyher et al. 1995; Narayana et al. 1989; Pouwels and Frahm 1998; Schuff et al. 1999; Wang et al. 1998).
tCr
The tCr signal, generated by creatine and phosphocreatine, is influenced by the state of high-energy phosphate metabolism (Tedeschi et al. 1995). In spectroscopy studies, it often is used as a reference for other peaks based on the incorrect assumption that its concentration is relatively constant (cf. Zahr et al. 2008, 2009, 2014b).
Cho
The in vivo MRS-visible Cho peak is generated primarily by water-soluble choline-containing compounds (free choline, phosphocholine, and glycerophosphocholine) (Barker et al. 1994) and is associated with cell-membrane synthesis and turnover. The Cho resonance also provides an index of cellular density in brain tumors (Gupta et al. 1999) and may be a marker of increases in glial density with age and disease. MRS-measured Cho concentration is higher in white than gray matter (Pfefferbaum et al. 1999) and increases with normal aging (Chang et al. 1996; Kreis et al. 1993; Moats et al. 1994; Pfefferbaum et al. 1999; Soher et al. 1996).
mI
Myo-inositiol is present in glial but not neuronal cell cultures (Brand et al. 1993; Petroff et al. 1995) and plays a role in maintaining cell volume (Ernst et al. 1997; Lien et al. 1990). The concentration of mI is higher in gray than in white matter (Michaelis et al. 1993; Pouwels and Frahm 1998).
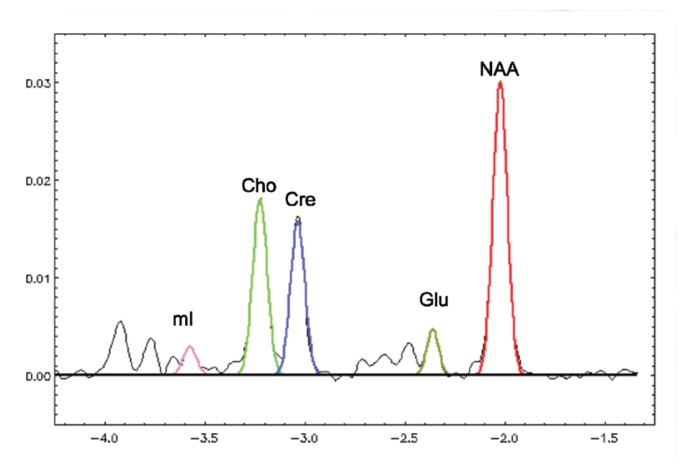
Figure 7 shows a graph of MR spectra from the thalamus of a 55-year-old nonalcoholic woman. The major metabolites are color coded.
Figure 7.
Magnetic resonance spectroscopy spectra from the thalamus of a 55-year-old nonalcoholic control woman, with a gaussian fit of the major metabolites that has been color coded.
MRS Findings in Alcoholism-Related Brain Disorders
As with the other imaging modalities, MRS reports of WE are primarily case studies. For example, a Japanese man who had consumed alcohol for 50 years and had eaten poorly for several days as a result of a cold presented with gait disturbances and incoherent speech. MRS before and after thiamine treatment found an initial low level of NAA/tCr in the thalamus, which appeared to increase with thiamine replacement. NAA/tCr levels in the cerebellum did not increase, although a lactate peak initially present in the cerebellum resolved (Murata et al. 2001). MRS conducted in two patients with non–alcohol-related thiamine deficiency (i.e., caused by gastric and pancreatic cancer) compared with five healthy study participants showed similar results: relatively low NAA/tCr levels in the thalamus resolved after treatment with thiamine (Mascalchi et al. 2002).
In a variety of brain regions, MRS findings in alcohol-related cirrhosis and HE are remarkably consistent and comparable with findings in nonalcoholic HE (e.g., Cordoba et al. 2001; Gupta et al. 1993; Häussinger et al. 1994), showing lower levels of Cho/tCr and mI/tCr and higher levels of Gln/tCr (Ahluwalia et al. 2015; Binesh et al. 2006; Chavarria et al. 2013; Jain et al. 2013; Kreis et al. 1992; Laubenberger et al. 1997; Miese et al. 2006; Pujol et al. 1996; Singhal et al. 2010; Taylor-Robinson et al. 1994, 1999; Thomas et al. 1998). Levels of mI and Cho are lowest and Glx highest in patients with HE (Geissler et al. 1997; Lee et al. 1999; Poveda et al. 2010; Ross et al. 1994; Tarasow et al. 2003).
Mild swelling of astrocytes is proposed as the key event in the pathogenesis of HE (e.g., Takahashi et al. 1991). In cirrhosis, elevated blood level of ammonia is thought to result in elevated brain ammonia, which can be toxic (Weissenborn et al. 2007). It often has been proposed that the brain’s response to elevated ammonia levels is to combine ammonia and glutamate to make glutamine using glutamine synthetase, found primarily in astrocytes (Yamamoto et al. 1987). Thus, brain swelling in cirrhosis is thought to reflect an increase in astrocytic glutamine formation. The decrease in mI is thought to be a compensatory mechanism to counterbalance the osmotic effect of cerebral glutamine accumulation (Balata et al. 2003; Mardini et al. 2011). Although some articles claim to measure in vivo glutamine (e.g., Binesh et al. 2006; Chavarria et al. 2013; Jain et al. 2013; Kreis et al. 1992; McConnell et al. 1995), it is unlikely that the MRS method used in these cases permitted the separate detection of glutamate and glutamine, which are strongly coupled and difficult to detect independently, even with very short echo times (Adalsteinsson et al. 2002). A single study measured GABA levels in five alcoholics without HE and five study participants with both alcohol and non–alcohol-related HE. GABA levels were lower in the two patient groups relative to 10 comparison participants (Behar et al. 1999).
In the only report of MRS conducted in a case of alcoholism-associated CPM, elevated Cho/tCr was found and interpreted as reflecting edema or demyelination in a 53-year-old man with gait disturbances and hearing loss (Nomoto et al. 2004). In 12 patients with chronic hyponatremia (nonalcohol etiology), MRS showed reduced Cho and mI relative to unaffected study participants, reflecting osmolyte disturbances (Videen et al. 1995).
Research also has found compromised NAA/tCr levels in patients with cerebellar degeneration (Tedeschi et al. 1996; Terakawa et al. 1999). Two MRS case studies of MBD showed reduced NAA/tCr and elevated Cho/tCr in corpus callosum splenium (Gambini et al. 2003; Tuntiyatorn and Laothamatas 2008), findings consistent with demyelination (elevated Cho) and axonal injury (reduced NAA).
MRS Findings in Uncomplicated Alcoholism
Most MRS studies show lower levels of NAA in recently sober alcoholics relative to healthy controls in several brain regions, including frontal areas (Bendszus et al. 2001; Durazzo et al. 2004, 2010; Fein et al. 1994; Jagannathan et al. 1996; Meyerhoff et al. 2004; Schweinsburg et al. 2003; Seitz et al. 1999) and cerebellum (Bendszus et al. 2001; Durazzo et al. 2010; Jagannathan et al. 1996; Parks et al. 2002; Seitz et al. 1999). Similarly, studies in AUD patients shortly following detoxification have found low levels of Cho (Bendszus et al. 2001; Durazzo et al. 2004; Ende et al. 2005; Fein et al. 1994; Parks et al. 2002; Seitz et al. 1999), although Cho findings in AUD are less consistent (e.g., Hermann et al. 2012; Modi et al. 2011). Because these findings are prominent in white matter, it is thought that the effects of alcoholism are greater in white than in gray matter (De la Monte 1988; Harper et al. 2003).
MRS Findings in Recovery from Alcoholism
MRS studies suggest that NAA (e.g., Bartsch et al. 2007; Bendszus et al. 2001; Parks et al. 2002), particularly in frontal (Bartsch et al. 2007; Bendszus et al. 2001; Durazzo et al. 2006) and cerebellar (Bendszus et al. 2001; Fein et al. 1994; Parks et al. 2002) regions and Cho levels (e.g., Bartsch et al. 2007; Bendszus et al. 2001; Durazzo et al. 2006; Ende et al. 2005; Martin et al. 1995) show normalization (i.e., increase) with abstinence. Elevations in mI are not seen in long-term sober alcoholics (Schweinsburg et al. 2000). These findings suggest that low NAA levels initially observed in recently sober alcoholics reflect neurodegeneration without cell death, and increases with abstinence may reflect healing without cell generation. The disruption and recovery of Cho and mI levels suggest white-matter recovery with sobriety and the potential for remyelination.
MRS Findings in Animal Models of Syndromes Associated With Alcoholism
In rat models of WE induced using pyrithiamine, the dominant MRS pattern is a reduction in both NAA and Cho in several brain regions (Lee et al. 1995, 2001; Rose et al. 1993), including the thalamus (Navarro et al. 2008, 2005; Pfefferbaum et al. 2007). Researchers also frequently report elevations in lactate (Navarro et al. 2005, 2008). Precipitation of WE with glucose (resulting in seizures) is associated with further decreases in NAA and Cho and, significantly, an elevation in lactate (Zahr et al. 2014a). Treatment with thiamine is associated with recovery in Cho levels (Lee et al. 1995).
MRS has been used to evaluate models of HE achieved using various methods (Cudalbu 2013) and most reports show similar findings. Hepatic devascularization (Barba et al. 2008; Zwingmann et al. 2004), carbon tetrachloride treatment (Bates et al. 1989), bile-duct ligations (Bosoi et al. 2014; Rackayova et al. 2015), and other means of promoting hyperammonemia (e.g., acute liver ischemia, urease, or methionine sulfoximine treatment) (Bosman et al. 1990; de Graaf et al. 1991) result in elevated levels of Gln and frequently lactate in rat brain (e.g., cortex). Additional effects reported include lower levels of NAA, mI, Cho, and Glu (Barba et al. 2008; Bates et al. 1989; Bosman et al. 1990; de Graaf et al. 1991; Peeling et al. 1993; Rackayova et al. 2015; Zwingmann et al. 2004). As in the human condition, a similar caveat holds: that is, it is not clear if Glu and Gln are clearly discriminated in many of these studies, and, often, reports more likely reflect Glx levels.
Although in vivo MRS studies in both humans and animals have persisted in interpreting elevations in brain Gln as reflecting elevations in peripheral ammonia and brain edema (Venkatasubramanian et al. 2001), ex vivo carbon 13 nuclear MR studies have challenged the convention that glutamine accumulation is the major cause of brain edema in acute HE. Such studies instead indicate limited metabolic pathway reactions and capacity of astrocytes to detoxify ammonia by glutamine synthesis and emphasize distortions of energy and neurotransmitter metabolism (Zwingmann 2007).
MRS Findings in Animal Models of Uncomplicated Alcoholism (and Recovery)
MRS can be used in animals to detect and quantify in vivo and real-time brain EtOH kinetics (e.g., rats: Sullivan et al. 2005c; monkeys: Kaufman et al. 1994). Unlike findings in long-term sober human alcoholics, nonabstinent chronic heavy drinkers (Meyerhoff et al. 2004) and social and moderate drinkers (Ende et al. 2006) show elevated levels of brain Cho. Elevated levels of Cho are also reported in the thalamus of rodents between weeks 16 and 40 of alcohol exposure (Lee et al. 2003). Neuroimaging research has been conducted with rodent models of binge (Zahr et al. 2010, 2013, 2014b), repeated binge (Zahr et al. 2015), and chronic alcohol exposure (Zahr et al. 2009). In vivo MRS studies have consistently shown that a single 4-day binge exposure with BALs approaching 300 mg/dL is associated with reversible changes to the brain: levels of NAA are lower and those of Cho are higher following binge EtOH exposure (Zahr et al. 2010, 2013, 2014b). In the repeated-binge experiment, animals were exposed to 5 cycles of 4 days of intragastric EtOH treatment and 10 days of recovery. Changes in MRS metabolite levels again were transient: levels of NAA decreased, whereas those of Cho increased with each binge EtOH exposure cycle but then recovered during each abstinence period. Changes in response to EtOH were in expected directions based on the previous, single-binge EtOH exposure experiments but did not accrue with repeated-binge EtOH exposure (Zahr et al. 2015). In the chronic EtOH exposure study, NAA levels were lower in the EtOH-exposed relative to the comparison group but did not attain statistical significance, whereas levels of Cho appeared to demonstrate a dose-response curve (i.e., increasing levels with higher and longer EtOH exposure) (Zahr et al. 2009).
Conclusion
Imaging investigations of alcohol-related brain disorders show unique neuropathology (as outlined in table 1), offering a framework for examining pathology in uncomplicated alcoholism. Because brains affected by AUD can show mild effects in the regions aggressively targeted by overt disease, animal models have been useful in distinguishing the etiology of pathology and differentiating brain regions specifically targeted by thiamine deficiency versus hyperammonemia, for example. Individuals with AUD may show more prominent effects in some regions compared with others, suggesting a propensity for one diagnosis over another (e.g., an alcoholic may be more vulnerable to thiamine deficiency than to liver damage). What remains unresolved, and what animal models can help determine, is why certain brain regions are differentially vulnerable to certain pathologies. For example, are the colliculi sensitive to thiamine deficiency because of their relatively high metabolic rate (Landau et al. 1955; Sokoloff et al. 1977)? Is the pons susceptible to CPM because of its proximity to the basilar artery? Does dopamine explain why basal ganglia are targets of liver disease (Mousseau et al. 1993)?
In vivo imaging studies in humans and animal models will continue to provide an evolving picture of the course of alcoholic brain disease through remissions and exacerbations as long-term studies follow human alcoholics as they age and as new initiatives evaluate adolescents before they are exposed to alcohol.
Acknowledgments
Supported by National Institutes of Health Grants AA–005965, AA–012388, AA–017347, and AA–013521-INIA.
Footnotes
WE and KS are neurological disorders caused by thiamine deficiency. HE is a decline in brain function as a result of severe liver disease. CPM is a neurological disorder resulting from the destruction of the myelin layer that covers nerve cells in the pons. ACD occurs when neurons in the cerebellum are damaged due to alcohol use. MBD is a neurological disease associated with alcoholism, caused by damage to the corpus callosum.
Researchers use different MRI techniques to highlight different aspects of the brain. Techniques mentioned in this article include T1 weighted, T2 weighted, and FLAIR.
The cerebral aqueduct and third ventricle are part of the brain’s ventricular system—a set of cavities in the brain that produce, transport, and remove cerebrospinal fluid. This system also includes the lateral ventricles and fourth ventricle.
Financial Disclosure
The authors declare they have no competing financial interests.
References
- Abbott NJ. Inflammatory mediators and modulation of blood-brain barrier permeability. Cellular and Molecular Neurobiology. 2000;20(2):131–147. doi: 10.1023/A:1007074420772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adalsteinsson E, Sullivan EV, Pfefferbaum A. Biochemical, functional and microstructural magnetic resonance imaging (MRI) In: Liu Y, Lovinger DM, editors. Methods in Alcohol-Related Neuroscience Research. Boca Raton, FL: CRC Press; 2002. pp. 345–372. [Google Scholar]
- Adler S, Martinez J, Williams DS, Verbalis JG. Positive association between blood brain barrier disruption and osmotically-induced demyelination. Multiple Sclerosis. 2000;6(1):24–31. doi: 10.1177/135245850000600106. [DOI] [PubMed] [Google Scholar]
- Agartz I, Momenan R, Rawlings RR, et al. Hippocampal volume in patients with alcohol dependence. Archives of General Psychiatry. 1999;56(4):356–363. doi: 10.1001/archpsyc.56.4.356. [DOI] [PubMed] [Google Scholar]
- Ahluwalia V, Wade JB, Moeller FG, et al. The etiology of cirrhosis is a strong determinant of brain reserve: A multimodal magnetic resonance imaging study. Liver Transplantation. 2015;21(9):1123–1132. doi: 10.1002/lt.24163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhassoon OM, Sorg SF, Taylor MJ, et al. Callosal white matter microstructural recovery in abstinent alcoholics: A longitudinal diffusion tensor imaging study. Alcoholism: Clinical and Experimental Research. 2012;36(11):1922–1931. doi: 10.1111/j.1530-0277.2012.01808.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman AI, Tarter RE. Relationship between familial alcoholism and head injury. Journal of Studies on Alcohol. 1985;46(3):256–258. doi: 10.15288/jsa.1985.46.256. [DOI] [PubMed] [Google Scholar]
- Andersen AM, Novovic S, Ersboll AK, Hansen MB. Mortality in alcohol and biliary acute pancreatitis. Pancreas. 2008;36(4):432–434. doi: 10.1097/MPA.0b013e31815ceae5. [DOI] [PubMed] [Google Scholar]
- Antunez E, Estruch R, Cardenal C, et al. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke’s encephalopathy. AJR American Journal of Roentgenology. 1998;171(4):1131–1137. doi: 10.2214/ajr.171.4.9763009. [DOI] [PubMed] [Google Scholar]
- Arbelaez A, Pajon A, Castillo M. Acute Marchiafava-Bignami disease: MR findings in two patients. AJNR American Journal of Neuroradiology. 2003;24(10):1955–1957. [PMC free article] [PubMed] [Google Scholar]
- Arnone D, Abou-Saleh MT, Barrick TR. Diffusion tensor imaging of the corpus callosum in addiction. Neuropsychobiology. 2006;54(2):107–113. doi: 10.1159/000096992. [DOI] [PubMed] [Google Scholar]
- Bagga D, Sharma A, Kumari A, et al. Decreased white matter integrity in fronto-occipital fasciculus bundles: Relation to visual information processing in alcohol- dependent subjects. Alcohol. 2014;48(1):43–53. doi: 10.1016/j.alcohol.2013.10.009. [DOI] [PubMed] [Google Scholar]
- Bajaj JS. Minimal hepatic encephalopathy matters in daily life. World Journal of Gastroenterology. 2008;14(23):3609–3615. doi: 10.3748/wjg.14.3609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balata S, Olde Damink SW, Ferguson K, et al. Induced hyperammonemia alters neuropsychology, brain MR spectroscopy and magnetization transfer in cirrhosis. Hepatology. 2003;37(4):931–939. doi: 10.1053/jhep.2003.50156. [DOI] [PubMed] [Google Scholar]
- Bano S, Mehra S, Yadav SN, Chaudhary V. Marchiafava-Bignami disease: Role of neuroimaging in the diagnosis and management of acute disease. Neurology India. 2009;57(5):649–652. doi: 10.4103/0028-3886.57811. [DOI] [PubMed] [Google Scholar]
- Barba I, Chatauret N, Garcia-Dorado D, Cordoba J. A 1H nuclear magnetic resonance-based metabonomic approach for grading hepatic encephalopathy and monitoring the effects of therapeutic hypothermia in rats. Liver International. 2008;28(8):1141–1148. doi: 10.1111/j.1478-3231.2008.01801.x. [DOI] [PubMed] [Google Scholar]
- Barker PB, Breiter SN, Soher BJ, et al. Quantitative proton spectroscopy of canine brain: In vivo and in vitro correlations. Magnetic Resonance in Medicine. 1994;32(2):157–163. doi: 10.1002/mrm.1910320202. [DOI] [PubMed] [Google Scholar]
- Bartsch AJ, Homola G, Biller A, et al. Manifestations of early brain recovery associated with abstinence from alcoholism. Brain. 2007;130(Part 1):36–47. doi: 10.1093/brain/awl303. [DOI] [PubMed] [Google Scholar]
- Basser PJ. Inferring microstructural features and the physiological state of tissues from diffusion-weighted images. NMR in Biomedicine. 1995;8(7–8):333–344. doi: 10.1002/nbm.1940080707. [DOI] [PubMed] [Google Scholar]
- Basser PJ, Jones DK, Diffusion-tensor MRI. Theory, experimental design and data analysis—A technical review. NMR in Biomedicine. 2002;15(7):456–467. doi: 10.1002/nbm.783. [DOI] [PubMed] [Google Scholar]
- Basser PJ, Pierpaoli C. Microstructural and physiological features of tissues elucidated by quantitative-diffusion-tensor MRI. Journal of Magnetic Resonance, Series B. 1996;111(3):209–219. doi: 10.1006/jmrb.1996.0086. [DOI] [PubMed] [Google Scholar]
- Bates TE, Williams SR, Kauppinen RA, Gadian DG. Observation of cerebral metabolites in an animal model of acute liver failure in vivo: A 1H and 31P nuclear magnetic resonance study. Journal of Neurochemistry. 1989;53(1):102–110. doi: 10.1111/j.1471-4159.1989.tb07300.x. [DOI] [PubMed] [Google Scholar]
- Beck A, Wustenberg T, Genauck A, et al. Effect of brain structure, brain function, and brain connectivity on relapse in alcohol-dependent patients. Archives of General Psychiatry. 2012;69(8):842–852. doi: 10.1001/archgenpsychiatry.2011.2026. [DOI] [PubMed] [Google Scholar]
- Behar KL, Rothman DL, Petersen KF, et al. Preliminary evidence of low cortical GABA levels in localized 1H-MR spectra of alcohol-dependent and hepatic encephalopathy patients. American Journal of Psychiatry. 1999;156(6):952–954. doi: 10.1176/ajp.156.6.952. [DOI] [PubMed] [Google Scholar]
- Bell RL, Franklin KM, Hauser SL, Engleman EA. Next stop dependence—Binge drinking on the road to alcoholism: Preclinical findings on its neurobiology from rat animal models. In: Harris SB, editor. Binge Eating and Binge Drinking: Psychological, Social, and Medical Implications. Hauppauge, NY: Nova Science Publishers; 2013. pp. 1–60. [Google Scholar]
- Bellentani S, Saccoccio G, Costa G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage: The Dionysos Study Group. Gut. 1997;41(6):845–850. doi: 10.1136/gut.41.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendszus M, Weijers HG, Wiesbeck G, et al. Sequential MR imaging and proton MR spectroscopy in patients who underwent recent detoxification for chronic alcoholism: Correlation with clinical and neuropsychological data. AJNR American Journal of Neuroradiology. 2001;22(10):1926–1932. [PMC free article] [PubMed] [Google Scholar]
- Benegal V, Antony G, Venkatasubramanian G, Jayakumar PN. Gray matter volume abnormalities and externalizing symptoms in subjects at high risk for alcohol dependence. Addiction Biology. 2007;12(1):122–132. doi: 10.1111/j.1369-1600.2006.00043.x. [DOI] [PubMed] [Google Scholar]
- Beresford TP, Arciniegas DB, Alfers J, et al. Hippocampus volume loss due to chronic heavy drinking. Alcoholism: Clinical and Experimental Research. 2006;30(11):1866–1870. doi: 10.1111/j.1530-0277.2006.00223.x. [DOI] [PubMed] [Google Scholar]
- Bienia A, Sodolski W, Luchowska E. The effect of chronic alcohol abuse on gastric and duodenal mucosa. Annales Universitatis Mariae Curie-Sklodowska. Sectio D: Medicina. 2002;57(2):570–582. [PubMed] [Google Scholar]
- Binesh N, Huda A, Thomas MA, et al. Hepatic encephalopathy: A neurochemical, neuroanatomical, and neuropsychological study. Journal of Applied Clinical Medical Physics. 2006;7(1):86–96. doi: 10.1120/jacmp.v7i1.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich S, Sperling W, Degner D, et al. Lack of association between hippocampal volume reduction and first-onset alcohol withdrawal seizure: A volumetric MRI study. Alcohol and Alcoholism. 2003;38(1):40–44. doi: 10.1093/alcalc/agg017. [DOI] [PubMed] [Google Scholar]
- Bosman DK, Deutz NE, De Graaf AA, et al. Changes in brain metabolism during hyperammonemia and acute liver failure: Results of a comparative 1H-NMR spectroscopy and biochemical investigation. Hepatology. 1990;12(2):281–290. doi: 10.1002/hep.1840120215. [DOI] [PubMed] [Google Scholar]
- Bosoi CR, Zwingmann C, Marin H, et al. Increased brain lactate is central to the development of brain edema in rats with chronic liver disease. Journal of Hepatology. 2014;60(3):554–560. doi: 10.1016/j.jhep.2013.10.011. [DOI] [PubMed] [Google Scholar]
- Boutte D, Calhoun VD, Chen J, et al. Association of genetic copy number variations at 11 q14.2 with brain regional volume differences in an alcohol use disorder population. Alcohol. 2012;46(6):519–527. doi: 10.1016/j.alcohol.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand A, Richter-Landsberg C, Leibfritz D. Multinuclear NMR studies on the energy metabolism of glial and neuronal cells. Developmental Neuroscience. 1993;15(3–5):289–298. doi: 10.1159/000111347. [DOI] [PubMed] [Google Scholar]
- Brun A, Andersson J. Frontal dysfunction and frontal cortical synapse loss in alcoholism—the main cause of alcohol dementia? Dementia and Geriatric Cognitive Disorders. 2001;12(4):289–294. doi: 10.1159/000051271. [DOI] [PubMed] [Google Scholar]
- Buis CI, Wijdicks EF. Serial magnetic resonance imaging of central pontine myelinolysis. Liver Transplantation. 2002;8(7):643–645. doi: 10.1053/jlts.2002.34023. [DOI] [PubMed] [Google Scholar]
- Butterworth RF. Thiamine deficiency-related brain dysfunction in chronic liver failure. Metabolic Brain Disease. 2009;24(1):189–196. doi: 10.1007/s11011-008-9129-y. [DOI] [PubMed] [Google Scholar]
- Butterworth RF, Norenberg MD, Felipo V, et al. Experimental models of hepatic encephalopathy: ISHEN guidelines. Liver International. 2009;29(6):783–788. doi: 10.1111/j.1478-3231.2009.02034.x. [DOI] [PubMed] [Google Scholar]
- Caine D, Halliday GM, Kril JJ, Harper CG. Operational criteria for the classification of chronic alcoholics: Identification of Wernicke’s encephalopathy. Journal of Neurology, Neurosurgery, and Psychiatry. 1997;62(1):51–60. doi: 10.1136/jnnp.62.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardenas VA, Durazzo TC, Gazdzinski S, et al. Brain morphology at entry into treatment for alcohol dependence is related to relapse propensity. Biological Psychiatry. 2011;70(6):561–567. doi: 10.1016/j.biopsych.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardenas VA, Studholme C, Gazdzinski S, et al. Deformation-based morphometry of brain changes in alcohol dependence and abstinence. NeuroImage. 2007;34(3):879–887. doi: 10.1016/j.neuroimage.2006.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardenas VA, Studholme C, Meyerhoff DJ, et al. Chronic active heavy drinking and family history of problem drinking modulate regional brain tissue volumes. Psychiatry Research. 2005;138(2):115–130. doi: 10.1016/j.pscychresns.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Carlen PL, McAndrews MP, Weiss RT, et al. Alcohol-related dementia in the institutionalized elderly. Alcoholism: Clinical and Experimental Research. 1994;18(6):1330–1334. doi: 10.1111/j.1530-0277.1994.tb01432.x. [DOI] [PubMed] [Google Scholar]
- Carrilho PE, Santos MB, Piasecki L, Jorge AC. Marchiafava-Bignami disease: A rare entity with a poor outcome. Revista Brasileira de Terapia Intensiva. 2013;25(1):68–72. doi: 10.1590/S0103-507X2013000100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauli O, Llansola M, Agusti A, et al. Cerebral oedema is not responsible for motor or cognitive deficits in rats with hepatic encephalopathy. Liver International. 2014;34(3):379–387. doi: 10.1111/liv.12258. [DOI] [PubMed] [Google Scholar]
- Cederbaum AI. Alcohol metabolism. Clinics in Liver Disease. 2012;16(4):667–685. doi: 10.1016/j.cld.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L, Ernst T, Poland RE, Jenden DJ. In vivo proton magnetic resonance spectroscopy of the normal aging human brain. Life Sciences. 1996;58(22):2049–2056. doi: 10.1016/0024-3205(96)00197-x. [DOI] [PubMed] [Google Scholar]
- Chanraud S, Leroy C, Martelli C, et al. Episodic memory in detoxified alcoholics: Contribution of grey matter microstructure alteration. PLoS One. 2009a;4(8):e6786. doi: 10.1371/journal.pone.0006786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanraud S, Martelli C, Delain F, et al. Brain morphometry and cognitive performance in detoxified alcohol-dependents with preserved psychosocial functioning. Neuropsycho-pharmacology. 2007;32(2):429–438. doi: 10.1038/sj.npp.1301219. [DOI] [PubMed] [Google Scholar]
- Chanraud S, Reynaud M, Wessa M, et al. Diffusion tensor tractography in mesencephalic bundles: Relation to mental flexibility in detoxified alcohol-dependent subjects. Neuropsychopharmacology. 2009b;34(5):1223–1232. doi: 10.1038/npp.2008.101. [DOI] [PubMed] [Google Scholar]
- Chavarria L, Alonso J, Garcia-Martinez R, et al. Brain magnetic resonance spectroscopy in episodic hepatic encephalopathy. Journal of Cerebral Blood Flow and Metabolism. 2013;33(2):272–277. doi: 10.1038/jcbfm.2012.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CJ, Huang CC, Ro LS. Evolution of pontine and extrapontine myelinolysis: Clinical correlation with serial CT and MRI studies. European Neurology. 1996;36(3):179–180. doi: 10.1159/000117242. [DOI] [PubMed] [Google Scholar]
- Chen CM, Yi HY, Yoon YH, Dong C. Alcohol use at time of injury and survival following traumatic brain injury: Results from the National Trauma Data Bank. Journal of Studies on Alcohol and Drugs. 2012;73(4):531–541. doi: 10.15288/jsad.2012.73.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien D, Buxton RB, Kwong KK, et al. MR diffusion imaging of the human brain. Journal of Computer Assisted Tomography. 1990;14(4):514–520. doi: 10.1097/00004728-199007000-00003. [DOI] [PubMed] [Google Scholar]
- Chua GC, Sitoh YY, Lim CC, et al. MRI findings in osmotic myelinolysis. Clinical Radiology. 2002;57(9):800–806. [PubMed] [Google Scholar]
- Clarke TK, Treutlein J, Zimmermann US, et al. HPA-axis activity in alcoholism: Examples for a gene-environment interaction. Addiction Biology. 2008;13(1):1–14. doi: 10.1111/j.1369-1600.2007.00084.x. [DOI] [PubMed] [Google Scholar]
- Clavier E, Thiebot J, Delangre T, et al. Marchiafava-Bignami disease. A case studied by CT and MR imaging. Neuroradiology. 1986;28(4):376. doi: 10.1007/BF00333454. [DOI] [PubMed] [Google Scholar]
- Coleman LG, Jr, He J, Lee J, et al. Adolescent binge drinking alters adult brain neurotransmitter gene expression, behavior, brain regional volumes, and neurochemistry in mice. Alcoholism: Clinical and Experimental Research. 2011;35(4):671–688. doi: 10.1111/j.1530-0277.2010.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman LG, Jr, Liu W, Oguz I, et al. Adolescent binge ethanol treatment alters adult brain regional volumes, cortical extracellular matrix protein and behavioral flexibility. Pharmacology, Biochemistry, and Behavior. 2014;116:142–151. doi: 10.1016/j.pbb.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordoba J, Alonso J, Rovira A, et al. The development of low-grade cerebral edema in cirrhosis is supported by the evolution of (1)H-magnetic resonance abnormalities after liver transplantation. Journal of Hepatology. 2001;35(5):598–604. doi: 10.1016/s0168-8278(01)00181-7. [DOI] [PubMed] [Google Scholar]
- Cordoba J, Sanpedro F, Alonso J, Rovira A. 1H magnetic resonance in the study of hepatic encephalopathy in humans. Metabolic Brain Disease. 2002;17(4):415–429. doi: 10.1023/a:1021926405944. [DOI] [PubMed] [Google Scholar]
- Cudalbu C. In vivo studies of brain metabolism in animal models of hepatic encephalopathy using 1H magnetic resonance spectroscopy. Metabolic Brain Disease. 2013;28(2):167–174. doi: 10.1007/s11011-012-9368-9. [DOI] [PubMed] [Google Scholar]
- Day E, Bentham PW, Callaghan R, et al. Thiamine for prevention and treatment of Wernicke-Korsakoff syndrome in people who abuse alcohol. Cochrane Database of Systematic Reviews. 2013;7:CD004033. doi: 10.1002/14651858.CD004033.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, Narasimhan A, Thatcher DL, et al. Prefrontal cortex, thalamus, and cerebellar volumes in adolescents and young adults with adolescent-onset alcohol use disorders and comorbid mental disorders. Alcoholism: Clinical and Experimental Research. 2005;29(9):1590–1600. doi: 10.1097/01.alc.0000179368.87886.76. [DOI] [PubMed] [Google Scholar]
- de Graaf AA, Deutz NE, Bosman DK, et al. The use of in vivo proton NMR to study the effects of hyperammonemia in the rat cerebral cortex. NMR in Biomedicine. 1991;4(1):31–37. doi: 10.1002/nbm.1940040106. [DOI] [PubMed] [Google Scholar]
- de la Monte S, Derdak Z, Wands JR. Alcohol, insulin resistance and the liver-brain axis. Journal of Gastroenterology and Hepatology. 2012;27(Suppl 2):33–41. doi: 10.1111/j.1440-1746.2011.07023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Monte SM. Disproportionate atrophy of cerebral white matter in chronic alcoholics. Archives of Neurology. 1988;45(9):990–992. doi: 10.1001/archneur.1988.00520330076013. [DOI] [PubMed] [Google Scholar]
- de los Rios F, Kleindorfer DO, Khoury J, et al. Trends in substance abuse preceding stroke among young adults: A population-based study. Stroke. 2012;43(12):3179–3183. doi: 10.1161/STROKEAHA.112.667808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Reuck J, Vander Eecken H, Thiery E, Crevits L. Central pontine myelinolysis and its arterial blood supply. Acta Neurologica Belgica. 1975;75(5):193–204. [PubMed] [Google Scholar]
- de Souza A, Desai PK. More often striatal myelinolysis than pontine? A consecutive series of patients with osmotic demyelination syndrome. Neurological Research. 2012;34(3):262–271. doi: 10.1179/1743132812Y.0000000009. [DOI] [PubMed] [Google Scholar]
- DeWitt LD, Buonanno FS, Kistler JP, et al. Central pontine myelinolysis: Demonstration by nuclear magnetic resonance. Neurology. 1984;34(5):570–576. doi: 10.1212/wnl.34.5.570. [DOI] [PubMed] [Google Scholar]
- Diaz-Gomez D, Jover M, del-Campo JA, et al. Experimental models for hepatic encephalopathy. Revista Espanola de Enfermedades Digestivas. 2011;103(10):536–541. doi: 10.4321/s1130-01082011001000006. [DOI] [PubMed] [Google Scholar]
- Doyle TJ, Bedell BJ, Narayana PA. Relative concentrations of proton MR visible neurochemicals in gray and white matter in human brain. Magnetic Resonance in Medicine. 1995;33(6):755–759. doi: 10.1002/mrm.1910330603. [DOI] [PubMed] [Google Scholar]
- Draper B, Karmel R, Gibson D, et al. Alcohol-related cognitive impairment in New South Wales hospital patients aged 50 years and over. Australian and New Zealand Journal of Psychiatry. 2011a;45(11):985–992. doi: 10.3109/00048674.2011.610297. [DOI] [PubMed] [Google Scholar]
- Draper B, Karmel R, Gibson D, et al. The Hospital Dementia Services Project: Age differences in hospital stays for older people with and without dementia. International Psychogeriatrics. 2011b;23(10):1649–1658. doi: 10.1017/S1041610211001694. [DOI] [PubMed] [Google Scholar]
- Dror V, Eliash S, Rehavi M, et al. Neurodegeneration in thiamine deficient rats—A longitudinal MRI study. Brain Research. 2010;1308:176–184. doi: 10.1016/j.brainres.2009.10.032. [DOI] [PubMed] [Google Scholar]
- Dror V, Rehavi M, Biton IE, Eliash S. Rasagiline prevents neurodegeneration in thiamine deficient rats— A longitudinal MRI study. Brain Research. 2014;1557:43–54. doi: 10.1016/j.brainres.2013.12.030. [DOI] [PubMed] [Google Scholar]
- Duell EJ, Sala N, Travier N, et al. Genetic variation in alcohol dehydrogenase (ADH1A, ADH1B, ADH1C, ADH7) and aldehyde dehydrogenase (ALDH2), alcohol consumption and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Carcinogenesis. 2012;33(2):361–367. doi: 10.1093/carcin/bgr285. [DOI] [PubMed] [Google Scholar]
- Durazzo TC, Gazdzinski S, Banys P, Meyerhoff DJ. Cigarette smoking exacerbates chronic alcohol-induced brain damage: A preliminary metabolite imaging study. Alcoholism: Clinical and Experimental Research. 2004;28(12):1849–1860. doi: 10.1097/01.alc.0000148112.92525.ac. [DOI] [PubMed] [Google Scholar]
- Durazzo TC, Gazdzinski S, Rothlind JC, et al. Brain metabolite concentrations and neurocognition during short-term recovery from alcohol dependence: Preliminary evidence of the effects of concurrent chronic cigarette smoking. Alcoholism: Clinical and Experimental Research. 2006;30(3):539–551. doi: 10.1111/j.1530-0277.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- Durazzo TC, Pathak V, Gazdzinski S, et al. Metabolite levels in the brain reward pathway discriminate those who remain abstinent from those who resume hazardous alcohol consumption after treatment for alcohol dependence. Journal of Studies on Alcohol and Drugs. 2010;71(2):278–289. doi: 10.15288/jsad.2010.71.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Tosun D, Buckley S, et al. Cortical thickness, surface area, and volume of the brain reward system in alcohol dependence: Relationships to relapse and extended abstinence. Alcoholism: Clinical and Experimental Research. 2011;35(6):1187–1200. doi: 10.1111/j.1530-0277.2011.01452.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Liu W, Wills DN, Crews FT. Periadolescent ethanol vapor exposure persistently reduces measures of hippocampal neurogenesis that are associated with behavioral outcomes in adulthood. Neuroscience. 2013;244:1–15. doi: 10.1016/j.neuroscience.2013.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias S, Dror V, Cohen S, Rehavi M. Neuroprotection by rasagiline in thiamine deficient rats. Brain Research. 2009;1256:138–148. doi: 10.1016/j.brainres.2008.11.097. [DOI] [PubMed] [Google Scholar]
- Ende G, Walter S, Welzel H, et al. Alcohol consumption significantly influences the MR signal of frontal choline-containing compounds. NeuroImage. 2006;32(2):740–746. doi: 10.1016/j.neuroimage.2006.03.049. [DOI] [PubMed] [Google Scholar]
- Ende G, Welzel H, Walter S, et al. Monitoring the effects of chronic alcohol consumption and abstinence on brain metabolism: A longitudinal proton magnetic resonance spectroscopy study. Biological Psychiatry. 2005;58(12):974–980. doi: 10.1016/j.biopsych.2005.05.038. [DOI] [PubMed] [Google Scholar]
- Ernst T, Chang L, Melchor R, Mehringer CM. Frontotemporal dementia and early Alzheimer disease: Differentiation with frontal lobe H-1 MR spectroscopy. Radiology. 1997;203(3):829–836. doi: 10.1148/radiology.203.3.9169712. [DOI] [PubMed] [Google Scholar]
- Estruch R, Nicolas JM, Salamero M, et al. Atrophy of the corpus callosum in chronic alcoholism. Journal of the Neurological Sciences. 1997;146(2):145–151. doi: 10.1016/s0022-510x(96)00298-5. [DOI] [PubMed] [Google Scholar]
- Eyer F, Schuster T, Felgenhauer N, et al. Risk assessment of moderate to severe alcohol withdrawal—Predictors for seizures and delirium tremens in the course of withdrawal. Alcohol and Alcoholism. 2011;46(4):427–433. doi: 10.1093/alcalc/agr053. [DOI] [PubMed] [Google Scholar]
- Fadda F, Rossetti ZL. Chronic ethanol consumption: From neuroadaptation to neurodegeneration. Progress in Neurobiology. 1998;56(4):385–431. doi: 10.1016/s0301-0082(98)00032-x. [DOI] [PubMed] [Google Scholar]
- Fein G, Bachman L, Fisher S, Davenport L. Cognitive impairments in abstinent alcoholics. Western Journal of Medicine. 1990;152(5):531–537. [PMC free article] [PubMed] [Google Scholar]
- Fein G, Landman B, Tran H, et al. Brain atrophy in long-term abstinent alcoholics who demonstrate impairment on a simulated gambling task. NeuroImage. 2006;32(3):1465–1471. doi: 10.1016/j.neuroimage.2006.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Meyerhoff D, Di Sclafani V, et al. 1H magnetic resonance spectroscopic imaging separates neuronal from glial changes in alcohol-related brain atrophy. In: Lancaster F, editor. Alcohol and Glial Cells: NIAAA Research Monograph No. 27. Bethesda, MD: U.S. Government Printing Office; 1994. pp. 227–241. [Google Scholar]
- Feuerlein W. Neuropsychiatric disorders of alcoholism. Annals of Nutrition and Metabolism. 1977;21(1–3):163–174. doi: 10.1159/000175761. [DOI] [PubMed] [Google Scholar]
- Fields JZ, Turk A, Durkin M, et al. Increased gastrointestinal symptoms in chronic alcoholics. American Journal of Gastroenterology. 1994;89(3):382–386. [PubMed] [Google Scholar]
- Fitzpatrick LE, Jackson M, Crowe SF. Characterization of cerebellar ataxia in chronic alcoholics using the International Cooperative Ataxia Rating Scale (ICARS) Alcoholism: Clinical and Experimental Research. 2012;36(11):1942–1951. doi: 10.1111/j.1530-0277.2012.01821.x. [DOI] [PubMed] [Google Scholar]
- Fortier CB, Leritz EC, Salat DH, et al. Widespread effects of alcohol on white matter microstructure. Alcoholism: Clinical and Experimental Research. 2014;38(12):2925–2933. doi: 10.1111/acer.12568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambini A, Falini A, Moiola L, et al. Marchiafava-Bignami disease: Longitudinal MR imaging and MR spectroscopy study. AJNR American Journal of Neuroradiology. 2003;24(2):249–253. [PMC free article] [PubMed] [Google Scholar]
- Gass JT, Glen WB, Jr, McGonigal JT, et al. Adolescent alcohol exposure reduces behavioral flexibility, promotes disinhibition, and increases resistance to extinction of ethanol self-administration in adulthood. Neuropsychopharmacology. 2014;39(11):2570–2583. doi: 10.1038/npp.2014.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazdzinski S, Durazzo TC, Mon A, et al. Cerebral white matter recovery in abstinent alcoholics—a multimodality magnetic resonance study. Brain. 2010;133(Pt 4):1043–1053. doi: 10.1093/brain/awp343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geissler A, Lock G, Frund R, et al. Cerebral abnormalities in patients with cirrhosis detected by proton magnetic resonance spectroscopy and magnetic resonance imaging. Hepatology. 1997;25(1):48–54. doi: 10.1053/jhep.1997.v25.pm0008985263. [DOI] [PubMed] [Google Scholar]
- Gerard E, Healy ME, Hesselink JR. MR demonstration of mesencephalic lesions in osmotic demyelination syndrome (central pontine myelinolysis) Neuroradiology. 1987;29(6):582–584. doi: 10.1007/BF00350448. [DOI] [PubMed] [Google Scholar]
- Gerig G, Corouge I, Vachet C, et al. Quantitative analysis of diffusion properties of white matter fiber tracts: A validation study. Proceedings of the 13th International Society for Magnetic Resonance in Medicine, Abstract No. 1337; Miami, FL. 2005. [Google Scholar]
- Gloria L, Cravo M, Camilo ME, et al. Nutritional deficiencies in chronic alcoholics: Relation to dietary intake and alcohol consumption. American Journal of Gastroenterology. 1997;92(3):485–489. [PubMed] [Google Scholar]
- Goebel HH, Herman-Ben Zur P. Central pontine myelinolysis. In: Vinken PJ, Bruyn GW, editors. Handbook of Clinical Neurology. Vol. 28. Amsterdam: North-Holland Publishing Company; 1976. pp. 285–316. [Google Scholar]
- Goldman JE, Horoupian DS. Demyelination of the lateral geniculate nucleus in central pontine myelinolysis. Annals of Neurology. 1981;9(2):185–189. doi: 10.1002/ana.410090213. [DOI] [PubMed] [Google Scholar]
- Gozzi A, Agosta F, Massi M, et al. Reduced limbic metabolism and fronto-cortical volume in rats vulnerable to alcohol addiction. NeuroImage. 2013;69:112–119. doi: 10.1016/j.neuroimage.2012.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graff-Radford J, Fugate JE, Kaufmann TJ, et al. Clinical and radiologic correlations of central pontine myelinolysis syndrome. Mayo Clinic Proceedings. 2011;86(11):1063–1067. doi: 10.4065/mcp.2011.0239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta RK, Saraswat VA, Poptani H, et al. Magnetic resonance imaging and localized in vivo proton spectroscopy in patients with fulminant hepatic failure. American Journal of Gastroenterology. 1993;88(5):670–674. [PubMed] [Google Scholar]
- Gupta RK, Sinha U, Cloughesy TF, Alger JR. Inverse correlation between choline magnetic resonance spectroscopy signal intensity and the apparent diffusion coefficient in human glioma. Magnetic Resonance in Medicine. 1999;41(1):2–7. doi: 10.1002/(sici)1522-2594(199901)41:1<2::aid-mrm2>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Gupta S, Warner J. Alcohol-related dementia: A 21st-century silent epidemic? British Journal of Psychiatry. 2008;193(5):351–353. doi: 10.1192/bjp.bp.108.051425. [DOI] [PubMed] [Google Scholar]
- Ha ND, Weon YC, Jang JC, et al. Spectrum of MR imaging findings in Wernicke encephalopathy: Are atypical areas of involvement only present in nonalcoholic patients? AJNR American Journal of Neuroradiology. 2012;33(7):1398–1402. doi: 10.3174/ajnr.A2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara K, Okada Y, Shida N, Yamashita Y. Extensive central and extrapontine myelinolysis in a case of chronic alcoholism without hyponatremia: A case report with analysis of serial MR findings. Internal Medicine. 2008;47(5):431–435. doi: 10.2169/internalmedicine.47.0634. [DOI] [PubMed] [Google Scholar]
- Harding AJ, Wong A, Svoboda M, et al. Chronic alcohol consumption does not cause hippocampal neuron loss in humans. Hippocampus. 1997;7(1):78–87. doi: 10.1002/(SICI)1098-1063(1997)7:1<78::AID-HIPO8>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Harlan WR, Landis JR, Flegal KM, et al. Secular trends in body mass in the United States, 1960–1980. American Journal of Epidemiology. 1988;128(5):1065–1074. doi: 10.1093/aje/128.5.1065. [DOI] [PubMed] [Google Scholar]
- Harper C. Thiamine (vitamin B1) deficiency and associated brain damage is still common throughout the world and prevention is simple and safe! European Journal of Neurology. 2006;13(10):1078–1082. doi: 10.1111/j.1468-1331.2006.01530.x. [DOI] [PubMed] [Google Scholar]
- Harper C. The neurotoxicity of alcohol. Human & Experimental Toxicology. 2007;26(3):251–257. doi: 10.1177/0960327107070499. [DOI] [PubMed] [Google Scholar]
- Harper C, Dixon G, Sheedy D, Garrick T. Neuropathological alterations in alcoholic brains: Studies arising from the New South Wales Tissue Resource Centre. Progress in Neuro-psychopharmacology & Biological Psychiatry. 2003;27(6):951–961. doi: 10.1016/S0278-5846(03)00155-6. [DOI] [PubMed] [Google Scholar]
- Harper C, Rodriguez M, Gold J, Perdices M. The Wernicke-Korsakoff syndrome in Sydney—A prospective necropsy study. Medical Journal of Australia. 1988;149(11–12):718–720. doi: 10.5694/j.1326-5377.1988.tb120846.x. [DOI] [PubMed] [Google Scholar]
- Harper CG. Sudden, unexpected death and Wernicke’s encephalopathy: A complication of prolonged intravenous feeding. Australian and New Zealand Journal of Medicine. 1980;10(2):230–235. doi: 10.1111/j.1445-5994.1980.tb03720.x. [DOI] [PubMed] [Google Scholar]
- Harris GJ, Jaffin SK, Hodge SM, et al. Frontal white matter and cingulum diffusion tensor imaging deficits in alcoholism. Alcoholism: Clinical and Experimental Research. 2008;32(6):1001–1013. doi: 10.1111/j.1530-0277.2008.00661.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey RJ, Skelton-Robinson M, Rossor MN. The prevalence and causes of dementia in people under the age of 65 years. Journal of Neurology, Neurosurgery, and Psychiatry. 2003;74(9):1206–1209. doi: 10.1136/jnnp.74.9.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häussinger D, Laubenberger J, vom Dahl S, et al. Proton magnetic resonance spectroscopy studies on human brain myo-inositol in hypo-osmolarity and hepatic encephalopathy. Gastroenterology. 1994;107(5):1475–1480. doi: 10.1016/0016-5085(94)90552-5. [DOI] [PubMed] [Google Scholar]
- Hazell AS, Butterworth RF. Update of cell damage mechanisms in thiamine deficiency: Focus on oxidative stress, excitotoxicity and inflammation. Alcohol and Alcoholism. 2009;44(2):141–147. doi: 10.1093/alcalc/agn120. [DOI] [PubMed] [Google Scholar]
- He DY, McGough NN, Ravindranathan A, et al. Glial cell line-derived neurotrophic factor mediates the desirable actions of the anti-addiction drug ibogaine against alcohol consumption. Journal of Neuroscience. 2005;25(3):619–628. doi: 10.1523/JNEUROSCI.3959-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X, Sullivan EV, Stankovic RK, et al. Interaction of thiamine deficiency and voluntary alcohol consumption disrupts rat corpus callosum ultrastructure. Neuropsycho-pharmacology. 2007;32(10):2207–2216. doi: 10.1038/sj.npp.1301332. [DOI] [PubMed] [Google Scholar]
- Helenius J, Tatlisumak T, Soinne L, et al. Marchiafava-Bignami disease: Two cases with favourable outcome. European Journal of Neurology. 2001;8(3):269–272. doi: 10.1046/j.1468-1331.2001.00212.x. [DOI] [PubMed] [Google Scholar]
- Hermann D, Weber-Fahr W, Sartorius A, et al. Translational magnetic resonance spectroscopy reveals excessive central glutamate levels during alcohol withdrawal in humans and rats. Biological Psychiatry. 2012;71(11):1015–1021. doi: 10.1016/j.biopsych.2011.07.034. [DOI] [PubMed] [Google Scholar]
- Hillbom M, Saloheimo P, Fujioka S, et al. Diagnosis and management of Marchiafava-Bignami disease: A review of CT/MRI confirmed cases. Journal of Neurology, Neurosurgery, and Psychiatry. 2014;85(2):168–173. doi: 10.1136/jnnp-2013-305979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyumpa AM., Jr Mechanisms of thiamin deficiency in chronic alcoholism. American Journal of Clinical Nutrition. 1980;33(12):2750–2761. doi: 10.1093/ajcn/33.12.2750. [DOI] [PubMed] [Google Scholar]
- Ihn YK, Hwang SS, Park YH. Acute Marchiafava-Bignami disease: Diffusion-weighted MRI in cortical and callosal involvement. Yonsei Medical Journal. 2007;48(2):321–324. doi: 10.3349/ymj.2007.48.2.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagannathan NR, Desai NG, Raghunathan P. Brain metabolite changes in alcoholism: An in vivo proton magnetic resonance spectroscopy (MRS) study. Magnetic Resonance Imaging. 1996;14(5):553–557. doi: 10.1016/0730-725x(96)00048-3. [DOI] [PubMed] [Google Scholar]
- Jain L, Sharma BC, Srivastava S, et al. Serum endotoxin, inflammatory mediators, and magnetic resonance spectroscopy before and after treatment in patients with minimal hepatic encephalopathy. Journal of Gastroenterology and Hepatology. 2013;28(7):1187–1193. doi: 10.1111/jgh.12160. [DOI] [PubMed] [Google Scholar]
- Jang DP, Namkoong K, Kim JJ, et al. The relationship between brain morphometry and neuropsychological performance in alcohol dependence. Neuroscience Letters. 2007;428(1):21–26. doi: 10.1016/j.neulet.2007.09.047. [DOI] [PubMed] [Google Scholar]
- Jernigan TL, Butters N, DiTraglia G, et al. Reduced cerebral grey matter observed in alcoholics using magnetic resonance imaging. Alcoholism: Clinical and Experimental Research. 1991a;15(3):418–427. doi: 10.1111/j.1530-0277.1991.tb00540.x. [DOI] [PubMed] [Google Scholar]
- Jernigan TL, Schafer K, Butters N, Cermak LS. Magnetic resonance imaging of alcoholic Korsakoff patients. Neuropsychopharmacology. 1991b;4(3):175–186. [PubMed] [Google Scholar]
- Johkura K, Naito M, Naka T. Cortical involvement in Marchiafava-Bignami disease. AJNR American Journal of Neuroradiology. 2005;26(3):670–673. [PMC free article] [PubMed] [Google Scholar]
- Jones DK. Fundamentals of diffusion MR imaging. In: Gillard J, Waldman AD, Barker P, editors. Clincal MR Neuroimaging. Cambridge, UK: Cambridge University Press; 2005. pp. 54–85. [Google Scholar]
- Jordan LR, Zelaya FO, Rose SE, et al. Changes in the hippocampus induced by glucose in thiamin deficient rats detected by MRI. Brain Research. 1998;791(1–2):347–351. doi: 10.1016/s0006-8993(98)00203-0. [DOI] [PubMed] [Google Scholar]
- Kale RA, Gupta RK, Saraswat VA, et al. Demonstration of interstitial cerebral edema with diffusion tensor MR imaging in type C hepatic encephalopathy. Hepatology. 2006;43(4):698–706. doi: 10.1002/hep.21114. [DOI] [PubMed] [Google Scholar]
- Kamarajan C, Porjesz B, Jones K, et al. Event-related oscillations in offspring of alcoholics: Neurocognitive disinhibition as a risk for alcoholism. Biological Psychiatry. 2006;59(7):625–634. doi: 10.1016/j.biopsych.2005.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman MJ, Chiu TM, Mendelson JH, et al. In vivo proton magnetic resonance spectroscopy of alcohol in rhesus monkey brain. Magnetic Resonance Imaging. 1994;12(8):1245–1253. doi: 10.1016/0730-725x(94)90089-a. [DOI] [PubMed] [Google Scholar]
- Kawamura M, Shiota J, Yagishita T, Hirayama K. Marchiafava-Bignami disease: Computed tomographic scan and magnetic resonance imaging. Annals of Neurology. 1985;18(1):103–104. doi: 10.1002/ana.410180123. [DOI] [PubMed] [Google Scholar]
- Khaw AV, Heinrich A. Marchiafava-Bignami disease: Diffusion-weighted MRI in corpus callosum and cortical lesions. Neurology. 2006;66(8):1286. doi: 10.1212/01.wnl.0000222494.86571.3c. author reply 1286. [DOI] [PubMed] [Google Scholar]
- Kipp M, Victor M, Martino G, Franklin RJ. Endogeneous remyelination: Findings in human studies. CNS & Neurological Disorders—Drug Targets. 2012;11(5):598–609. doi: 10.2174/187152712801661257. [DOI] [PubMed] [Google Scholar]
- Kleinschmidt-Demasters BK, Rojiani AM, Filley CM. Central and extrapontine myelinolysis: Then . . . and now. Journal of Neuropathology and Experimental Neurology. 2006;65(1):1–11. doi: 10.1097/01.jnen.0000196131.72302.68. [DOI] [PubMed] [Google Scholar]
- Koguchi K, Nakatsuji Y, Abe K, Sakoda S. Wernicke’s encephalopathy after glucose infusion. Neurology. 2004;62(3):512. doi: 10.1212/01.wnl.0000099189.56741.a7. [DOI] [PubMed] [Google Scholar]
- Koller KJ, Zaczek R, Coyle JT. N-Acetyl-aspartyl-glutamate: Regional levels in rat brain and the effects of brain lesions as determined by a new HPLC method. Journal of Neurochemistry. 1984;43(4):1136–1142. doi: 10.1111/j.1471-4159.1984.tb12854.x. [DOI] [PubMed] [Google Scholar]
- Kong L, Lian G, Zheng W, et al. Effect of alcohol on diffuse axonal injury in rat brainstem: Diffusion tensor imaging and aquaporin-4 expression study. BioMed Research International. 2013;2013;798261 doi: 10.1155/2013/798261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A, Vucurevic G, Lorscheider M, et al. Broad disruption of brain white matter microstructure and relationship with neuropsychological performance in male patients with severe alcohol dependence. Alcohol and Alcoholism. 2012;47(2):118–126. doi: 10.1093/alcalc/agr157. [DOI] [PubMed] [Google Scholar]
- Korbo L. Glial cell loss in the hippocampus of alcoholics. Alcoholism: Clinical and Experimental Research. 1999;23(1):164–168. [PubMed] [Google Scholar]
- Kreis R, Ernst T, Ross BD. Development of the human brain: In vivo quantification of metabolite and water content with proton magnetic resonance spectroscopy. Magnetic Resonance in Medicine. 1993;30(4):424–437. doi: 10.1002/mrm.1910300405. [DOI] [PubMed] [Google Scholar]
- Kreis R, Ross BD, Farrow NA, Ackerman Z. Metabolic disorders of the brain in chronic hepatic encephalopathy detected with H-1 MR spectroscopy. Radiology. 1992;182(1):19–27. doi: 10.1148/radiology.182.1.1345760. [DOI] [PubMed] [Google Scholar]
- Kroenke CD, Rohlfing T, Park B, et al. Monkeys that voluntarily and chronically drink alcohol damage their brains: A longitudinal MRI study. Neuropsychopharmacology. 2014;39(4):823–830. doi: 10.1038/npp.2013.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R, Gupta RK, Elderkin-Thompson V, et al. Voxel-based diffusion tensor magnetic resonance imaging evaluation of low-grade hepatic encephalopathy. Journal of Magnetic Resonance Imaging. 2008;27(5):1061–1068. doi: 10.1002/jmri.21342. [DOI] [PubMed] [Google Scholar]
- Kumar S, Fowler M, Gonzalez-Toledo E, Jaffe SL. Central pontine myelinolysis, an update. Neurological Research. 2006;28(3):360–366. doi: 10.1179/016164106X110346. [DOI] [PubMed] [Google Scholar]
- Kurth C, Wegerer V, Reulbach U, et al. Analysis of hippocampal atrophy in alcoholic patients by a Kohonen feature map. NeuroReport. 2004;15(2):367–371. doi: 10.1097/00001756-200402090-00031. [DOI] [PubMed] [Google Scholar]
- Kwo-On-Yuen PF, Newmark RD, Budinger TF, et al. Brain N-acetyl-l-aspartic acid in Alzheimer’s disease: A proton magnetic resonance spectroscopy study. Brain Research. 1994;667(2):167–174. doi: 10.1016/0006-8993(94)91494-x. [DOI] [PubMed] [Google Scholar]
- Laakso MP, Vaurio O, Savolainen L, et al. A volumetric MRI study of the hippocampus in type 1 and 2 alcoholism. Behavioural Brain Research. 2000;109(2):177–186. doi: 10.1016/s0166-4328(99)00172-2. [DOI] [PubMed] [Google Scholar]
- Landau WM, Freygang WH, Jr, Roland LP, et al. The local circulation of the living brain; values in the unanesthetized and anesthetized cat. Transactions of the American Neurological Association 80th Meeting; 1955. pp. 125–129. [PubMed] [Google Scholar]
- Langlais PJ, McRee RC, Nalwalk JA, Hough LB. Depletion of brain histamine produces regionally selective protection against thiamine deficiency-induced lesions in the rat. Metabolic Brain Disease. 2002;17(3):199–210. doi: 10.1023/a:1019930206196. [DOI] [PubMed] [Google Scholar]
- Laubenberger J, Haussinger D, Bayer S, et al. Proton magnetic resonance spectroscopy of the brain in symptomatic and asymptomatic patients with liver cirrhosis. Gastroenterology. 1997;112(5):1610–1616. doi: 10.1016/s0016-5085(97)70043-x. [DOI] [PubMed] [Google Scholar]
- Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nature Reviews Neuroscience. 2003;4(6):469–480. doi: 10.1038/nrn1119. [DOI] [PubMed] [Google Scholar]
- Le Bihan D, Mangin JF, Poupon C, et al. Diffusion tensor imaging: Concepts and applications. Journal of Magnetic Resonance Imaging. 2001;13(4):534–546. doi: 10.1002/jmri.1076. [DOI] [PubMed] [Google Scholar]
- Lee H, Holburn GE, Price RR. In vivo and in vitro proton NMR spectroscopic studies of thiamine-deficient rat brains. Journal of Magnetic Resonance Imaging. 2001;13(2):163–166. doi: 10.1002/1522-2586(200102)13:2<163::aid-jmri1025>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Lee H, Holburn GH, Price RR. Proton MR spectroscopic studies of chronic alcohol exposure on the rat brain. Journal of Magnetic Resonance Imaging. 2003;18(2):147–151. doi: 10.1002/jmri.10335. [DOI] [PubMed] [Google Scholar]
- Lee H, Tarter J, Holburn GE, et al. In vivo localized proton NMR spectroscopy of thiamine-deficient rat brain. Magnetic Resonance in Medicine. 1995;34(3):313–318. doi: 10.1002/mrm.1910340306. [DOI] [PubMed] [Google Scholar]
- Lee JH, Seo DW, Lee YS, et al. Proton magnetic resonance spectroscopy (1H-MRS) findings for the brain in patients with liver cirrhosis reflect the hepatic functional reserve. American Journal of Gastroenterology. 1999;94(8):2206–2213. doi: 10.1111/j.1572-0241.1999.01228.x. [DOI] [PubMed] [Google Scholar]
- Lee SH, Kim SS, Kim SH, Lee SY. Acute Marchiafava-Bignami disease with selective involvement of the precentral cortex and splenium: A serial magnetic resonance imaging study. Neurologist. 2011;17(4):213–217. doi: 10.1097/NRL.0b013e31821a25ae. [DOI] [PubMed] [Google Scholar]
- Lenz V, Vargas MI, Bin JF, et al. Value of MRI findings in Gayet-Wernicke encephalopathy. [Article in French.] Journal of Neuroradiology. 2002;29(3):153–160. [PubMed] [Google Scholar]
- Levy S, Herve C, Delacoux E, Erlinger S. Thiamine deficiency in hepatitis C virus and alcohol-related liver diseases. Digestive Diseases and Sciences. 2002;47(3):543–548. doi: 10.1023/a:1017907817423. [DOI] [PubMed] [Google Scholar]
- Lien Y, Shapiro J, Chan L. Effects of hypernatremia on organic brain osmoles. Journal of Clinical Investigation. 1990;85(5):1427–1435. doi: 10.1172/JCI114587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim KO, Spielman DM. Estimating NAA in cortical gray matter with applications for measuring changes due to aging. Magnetic Resonance in Medicine. 1997;37(3):372–377. doi: 10.1002/mrm.1910370313. [DOI] [PubMed] [Google Scholar]
- Lim KO, Adalsteinsson E, Spielman D, et al. Proton magnetic resonance spectroscopic imaging of cortical gray and white matter in schizophrenia. Archives of General Psychiatry. 1998;55(4):346–352. doi: 10.1001/archpsyc.55.4.346. [DOI] [PubMed] [Google Scholar]
- Liou KC, Kuo SF, Chen LA. Wernicke encephalopathy with atypical magnetic resonance imaging. American Journal of Emergency Medicine. 2012;30(9):2086.e1–2086.e3. doi: 10.1016/j.ajem.2011.12.013. [DOI] [PubMed] [Google Scholar]
- Liu H, Zheng W, Yan G, et al. Acute ethanol-induced changes in edema and metabolite concentrations in rat brain. BioMed Research International. 2014;2014;351903 doi: 10.1155/2014/351903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu IC, Chiu CH, Chen CJ, et al. The microstructural integrity of the corpus callosum and associated impulsivity in alcohol dependence: A tractography-based segmentation study using diffusion spectrum imaging. Psychiatry Research. 2010;184(2):128–134. doi: 10.1016/j.pscychresns.2010.07.002. [DOI] [PubMed] [Google Scholar]
- Liu RS, Lemieux L, Shorvon SD, et al. Association between brain size and abstinence from alcohol. Lancet. 2000;355(9219):1969–1970. doi: 10.1016/s0140-6736(00)02332-1. [DOI] [PubMed] [Google Scholar]
- Makris N, Oscar-Berman M, Jaffin SK, et al. Decreased volume of the brain reward system in alcoholism. Biological Psychiatry. 2008;64(3):192–202. doi: 10.1016/j.biopsych.2008.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maksimovskiy AL, McGlinchey RE, Fortier CB, et al. White matter and cognitive changes in veterans diagnosed with alcoholism and PTSD. Journal of Alcoholism and Drug Dependence. 2014;2(1):144. doi: 10.4172/2329-6488.1000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandyam CD, Koob GF. The addicted brain craves new neurons: Putative role for adult-born progenitors in promoting recovery. Trends in Neurosciences. 2012;35(4):250–260. doi: 10.1016/j.tins.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann KF, Ackermann K, Croissant B, et al. Neuroimaging of gender differences in alcohol dependence: Are women more vulnerable? Alcoholism: Clinical and Experimental Research. 2005;29(5):896–901. doi: 10.1097/01.alc.0000164376.69978.6b. [DOI] [PubMed] [Google Scholar]
- Mann RE, Smart RG, Govoni R. The epidemiology of alcoholic liver disease. Alcohol Research & Health. 2003;27(3):209–219. [PMC free article] [PubMed] [Google Scholar]
- Mardini H, Smith FE, Record CO, Blamire AM. Magnetic resonance quantification of water and metabolites in the brain of cirrhotics following induced hyper-ammonaemia. Journal of Hepatology. 2011;54(6):1154–1160. doi: 10.1016/j.jhep.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Martin PJ, Young CA. Central pontine myelinolysis: Clinical and MRI correlates. Postgraduate Medical Journal. 1995;71(837):430–432. doi: 10.1136/pgmj.71.837.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin PR, Gibbs SJ, Nimmerrichter AA, et al. Brain proton magnetic resonance spectroscopy studies in recently abstinent alcoholics. Alcoholism: Clinical and Experimental Research. 1995;19(4):1078–1082. doi: 10.1111/j.1530-0277.1995.tb00992.x. [DOI] [PubMed] [Google Scholar]
- Martindale JL, Goldstein JN, Pallin DJ. Emergency department seizure epidemiology. Emergency Medicine Clinics of North America. 2011;29(1):15–27. doi: 10.1016/j.emc.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Mascalchi M, Belli G, Guerrini L, et al. Proton MR spectroscopy of Wernicke encephalopathy. AJNR American Journal of Neuroradiology. 2002;23(10):1803–1806. [PMC free article] [PubMed] [Google Scholar]
- Matthews RAJ. Medical progress depends on animal models—doesn’t it? Journal of the Royal Society of Medicine. 2008;101(2):95–98. doi: 10.1258/jrsm.2007.070164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride WJ. Central nucleus of the amygdala and the effects of alcohol and alcohol-drinking behavior in rodents. Pharmacology, Biochemistry, and Behavior. 2002;71(3):509–515. doi: 10.1016/s0091-3057(01)00680-3. [DOI] [PubMed] [Google Scholar]
- McConnell JR, Antonson DL, Ong CS, et al. Proton spectroscopy of brain glutamine in acute liver failure. Hepatology. 1995;22(1):69–74. [PubMed] [Google Scholar]
- McMurtray A, Clark DG, Christine D, Mendez MF. Early-onset dementia: Frequency and causes compared to late-onset dementia. Dementia and Geriatric Cognitive Disorders. 2006;21(2):59–64. doi: 10.1159/000089546. [DOI] [PubMed] [Google Scholar]
- McRee RC, Terry-Ferguson M, Langlais PJ, et al. Increased histamine release and granulocytes within the thalamus of a rat model of Wernicke’s encephalopathy. Brain Research. 2000;858(2):227–236. doi: 10.1016/s0006-8993(99)02309-4. [DOI] [PubMed] [Google Scholar]
- Mechtcheriakov S, Brenneis C, Egger K, et al. A widespread distinct pattern of cerebral atrophy in patients with alcohol addiction revealed by voxel-based morphometry. Journal of Neurology, Neurosurgery, and Psychiatry. 2007;78(6):610–614. doi: 10.1136/jnnp.2006.095869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menegon P, Sibon I, Pachai C, et al. Marchiafava-Bignami disease: Diffusion-weighted MRI in corpus callosum and cortical lesions. Neurology. 2005;65(3):475–477. doi: 10.1212/01.wnl.0000171348.55820.89. [DOI] [PubMed] [Google Scholar]
- Messert B, Orrison WW, Hawkins MJ, Quaglieri CE. Central pontine myelinolysis. Considerations on etiology, diagnosis, and treatment. Neurology. 1979;29(2):147–160. doi: 10.1212/wnl.29.2.147. [DOI] [PubMed] [Google Scholar]
- Meyerhoff DJ, Blumenfeld R, Truran D, et al. Effects of heavy drinking, binge drinking, and family history of alcoholism on regional brain metabolites. Alcoholism: Clinical and Experimental Research. 2004;28(4):650–661. doi: 10.1097/01.ALC.0000121805.12350.CA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaelis T, Merboldt KD, Bruhn H, et al. Absolute concentrations of metabolites in the adult human brain in vivo: Quantification of localized proton MR spectra. Radiology. 1993;187(1):219–227. doi: 10.1148/radiology.187.1.8451417. [DOI] [PubMed] [Google Scholar]
- Miese F, Kircheis G, Wittsack HJ, et al. 1H-MR spectroscopy, magnetization transfer, and diffusion-weighted imaging in alcoholic and nonalcoholic patients with cirrhosis with hepatic encephalopathy. AJNR American Journal of Neuroradiology. 2006;27(5):1019–1026. [PMC free article] [PubMed] [Google Scholar]
- Mignini LE, Khan KS. Methodological quality of systematic reviews of animal studies: A survey of reviews of basic research. BMC Medical Research Methodology. 2006;6:10. doi: 10.1186/1471-2288-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min Y, Park SH, Hwang SB. Corticospinal tract and pontocerebellar fiber of central pontine myelinolysis. Annals of Rehabilitation Medicine. 2012;36(6):887–892. doi: 10.5535/arm.2012.36.6.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moats RA, Ernst T, Shonk TK, Ross BD. Abnormal cerebral metabolite concentrations in patients with probable Alzheimer disease. Magnetic Resonance in Medicine. 1994;32(1):110–115. doi: 10.1002/mrm.1910320115. [DOI] [PubMed] [Google Scholar]
- Modi S, Bhattacharya M, Kumar P, et al. Brain metabolite changes in alcoholism: Localized proton magnetic resonance spectroscopy study of the occipital lobe. European Journal of Radiology. 2011;79(1):96–100. doi: 10.1016/j.ejrad.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Monnig MA, Caprihan A, Yeo RA, et al. Diffusion tensor imaging of white matter networks in individuals with current and remitted alcohol use disorders and comorbid conditions. Psychology of Addictive Behaviors. 2013;27(2):455–465. doi: 10.1037/a0027168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon SJ, Kim JW, Kang BT, et al. Magnetic resonance imaging findings of hepatic encephalopathy in a dog with a portosystemic shunt. Journal of Veterinary Medical Science. 2012;74(3):361–366. doi: 10.1292/jvms.11-0198. [DOI] [PubMed] [Google Scholar]
- Morgan MY. Alcohol and nutrition. British Medical Bulletin. 1982;38(1):21–29. doi: 10.1093/oxfordjournals.bmb.a071727. [DOI] [PubMed] [Google Scholar]
- Mousseau DD, Perney P, Layrargues GP, Butterworth RF. Selective loss of pallidal dopamine D2 receptor density in hepatic encephalopathy. Neuroscience Letters. 1993;162(1–2):192–196. doi: 10.1016/0304-3940(93)90593-a. [DOI] [PubMed] [Google Scholar]
- Mousseau DD, Rao VL, Butterworth RF. Vesicular dysfunction during experimental thiamine deficiency is indicated by alterations in dopamine metabolism. European Journal of Pharmacology. 1996;317(2–3):263–267. doi: 10.1016/s0014-2999(96)00842-4. [DOI] [PubMed] [Google Scholar]
- Moyher SE, Nelson SJ, Wald LL, et al. High spatial resolution MRS and segmented MRI to study NAA in cortical gray matter and white matter of the human brain [abstract] Proceedings of the Society of Magnetic Resonance. 1995;1:332. [Google Scholar]
- Müller-Oehring EM, Schulte T, Fama R, et al. Global-local interference is related to callosal compromise in alcoholism: A behavior-DTI association study. Alcoholism: Clinical and Experimental Research. 2009;33(3):477–489. doi: 10.1111/j.1530-0277.2008.00858.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro CA, Saxton J, Butters MA. The neuropsychological consequences of abstinence among older alcoholics: A cross-sectional study. Alcoholism: Clinical and Experimental Research. 2000;24(10):1510–1516. [PubMed] [Google Scholar]
- Murata T, Fujito T, Kimura H, et al. Serial MRI and (1)H-MRS of Wernicke’s encephalopathy: Report of a case with remarkable cerebellar lesions on MRI. Psychiatry Research. 2001;108(1):49–55. doi: 10.1016/s0925-4927(01)00304-3. [DOI] [PubMed] [Google Scholar]
- Nadler JV, Cooper JR. N-acetyl-l-aspartic acid content of human neural tumours and bovine peripheral nervous tissues. Journal of Neurochemistry. 1972;19(2):313–319. doi: 10.1111/j.1471-4159.1972.tb01341.x. [DOI] [PubMed] [Google Scholar]
- Naegele T, Grodd W, Viebahn R, et al. MR imaging and (1)H spectroscopy of brain metabolites in hepatic encephalopathy: Time-course of renormalization after liver transplantation. Radiology. 2000;216(3):683–691. doi: 10.1148/radiology.216.3.r00se27683. [DOI] [PubMed] [Google Scholar]
- Nahum L, Pignat JM, Bouzerda-Wahlen A, et al. Neural correlate of anterograde amnesia in Wernicke–Korsakoff syndrome. Brain Topography. 2015;28(5):760–770. doi: 10.1007/s10548-014-0391-5. [DOI] [PubMed] [Google Scholar]
- Nair SR, Ramli NM, Rahmat K, Mei-Ling ST. Central pontine and extrapontine myelinolysis: Diffusion weighted imaging and diffusion tensor imaging on follow-up. Neurology India. 2012;60(4):426–428. doi: 10.4103/0028-3886.100712. [DOI] [PubMed] [Google Scholar]
- Nakagawasai O, Murata A, Arai Y, et al. Enhanced head-twitch response to 5-HT-related agonists in thiamine-deficient mice. Journal of Neural Transmission. 2007;114(8):1003–1010. doi: 10.1007/s00702-007-0655-2. [DOI] [PubMed] [Google Scholar]
- Namekawa M, Nakamura Y, Nakano I. Cortical involvement in Marchiafava-Bignami disease can be a predictor of a poor prognosis: A case report and review of the literature. Internal Medicine. 2013;52(7):811–813. doi: 10.2169/internalmedicine.52.9336. [DOI] [PubMed] [Google Scholar]
- Narayana PA, Fotedar LK, Jackson EF, et al. Regional in vivo proton magnetic resonance spectroscopy of brain. Journal of Magnetic Resonance. 1989;83(1):44–52. [Google Scholar]
- Nardelli A, Lebel C, Rasmussen C, et al. Extensive deep gray matter volume reductions in children and adolescents with fetal alcohol spectrum disorders. Alcoholism: Clinical and Experimental Research. 2011;35(8):1404–1417. doi: 10.1111/j.1530-0277.2011.01476.x. [DOI] [PubMed] [Google Scholar]
- Navarro D, Zwingmann C, Chatauret N, Butterworth RF. Glucose loading precipitates focal lactic acidosis in the vulnerable medial thalamus of thiamine-deficient rats. Metabolic Brain Disease. 2008;23(1):115–122. doi: 10.1007/s11011-007-9076-z. [DOI] [PubMed] [Google Scholar]
- Navarro D, Zwingmann C, Hazell AS, Butterworth RF. Brain lactate synthesis in thiamine deficiency: A re-evaluation using 1H-13C nuclear magnetic resonance spectroscopy. Journal of Neuroscience Research. 2005;79(1–2):33–41. doi: 10.1002/jnr.20290. [DOI] [PubMed] [Google Scholar]
- Needs CJ, Brooks PM. Antirheumatic medication in pregnancy. British Journal of Rheumatology. 1985;24(3):282–290. doi: 10.1093/rheumatology/24.3.282. [DOI] [PubMed] [Google Scholar]
- Newell KL, Kleinschmidt-DeMasters BK. Central pontine myelinolysis at autopsy: A twelve year retrospective analysis. Journal of Neurological Sciences. 1996;142(1–2):134–139. doi: 10.1016/0022-510x(96)00175-x. [DOI] [PubMed] [Google Scholar]
- Nixon K. Alcohol and adult neurogenesis: Roles in neurodegeneration and recovery in chronic alcoholism. Hippocampus. 2006;16(3):287–295. doi: 10.1002/hipo.20162. [DOI] [PubMed] [Google Scholar]
- Nixon K, Crews FT. Temporally specific burst in cell proliferation increases hippocampal neurogenesis in protracted abstinence from alcohol. Journal of Neuroscience. 2004;24(43):9714–9722. doi: 10.1523/JNEUROSCI.3063-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon PF, Jordan L, Zimitat C, et al. Choroid plexus dysfunction: The initial event in the pathogenesis of Wernicke’s encephalopathy and ethanol intoxication. Alcoholism: Clinical and Experimental Research. 2008;32(8):1513–1523. doi: 10.1111/j.1530-0277.2008.00723.x. [DOI] [PubMed] [Google Scholar]
- Nomoto N, Arasaki K, Tamaki M. Central pontine myelinolysis in chronic alcoholism demonstrated by magnetic resonance imaging and spectroscopy. European Neurology. 2004;51(3):179–180. doi: 10.1159/000077668. [DOI] [PubMed] [Google Scholar]
- Oslin DW, Cary MS. Alcohol-related dementia: Validation of diagnostic criteria. American Journal of Geriatric Psychiatry. 2003;11(4):441–447. [PubMed] [Google Scholar]
- Pacheco FT, Rego MM, do Rego JI, da Rocha AJ. “Ears of the lynx” sign in a Marchiafava-Bignami patient: Structural basis and fiber-tracking DTI contribution to the understanding of this imaging abnormality. Journal of Neuroimaging. 2014;24(2):205–207. doi: 10.1111/j.1552-6569.2012.00714.x. [DOI] [PubMed] [Google Scholar]
- Parks MH, Dawant BM, Riddle WR, et al. Longitudinal brain metabolic characterization of chronic alcoholics with proton magnetic resonance spectroscopy. Alcoholism: Clinical and Experimental Research. 2002;26(9):1368–1380. doi: 10.1097/01.ALC.0000029598.07833.2D. [DOI] [PubMed] [Google Scholar]
- Peeling J, Shoemaker L, Gauthier T, et al. Cerebral metabolic and histological effects of thioacetamide-induced liver failure. American Journal of Physiology. 1993;265(3 Pt. 1):G572–G578. doi: 10.1152/ajpgi.1993.265.3.G572. [DOI] [PubMed] [Google Scholar]
- Peters JL, Sutton AJ, Jones DR, et al. A systematic review of systematic reviews and meta-analyses of animal experiments with guidelines for reporting. Journal of Environmental Science and Health. Part B, Pesticides, Food Contaminants, and Agricultural Wastes. 2006;41(7):1245–1258. doi: 10.1080/03601230600857130. [DOI] [PubMed] [Google Scholar]
- Petroff OA, Pleban LA, Spencer DD. Symbiosis between in vivo and in vitro NMR spectroscopy: The creatine, N-acetylaspartate, glutamate, and GABA content of the epileptic human brain. Magnetic Resonance Imaging. 1995;13(8):1197–1211. doi: 10.1016/0730-725x(95)02033-p. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A. Use of MRI to evaluate structural changes in addictive medicine. Proceedings of the American Society of Addiction Medicine’s 23rd Annual Medical-Scientific Conference; 1992. [Google Scholar]
- Pfefferbaum A, Sullivan EV. Microstructural but not macrostructural disruption of white matter in women with chronic alcoholism. NeuroImage. 2002;15(3):708–718. doi: 10.1006/nimg.2001.1018. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV. Disruption of brain white matter microstructure by excessive intracellular and extracellular fluid in alcoholism: Evidence from diffusion tensor imaging. Neuropsychopharmacology. 2005;30(2):423–432. doi: 10.1038/sj.npp.1300623. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Adalsteinsson E, Bell RL, Sullivan EV. Development and resolution of brain lesions caused by pyrithiamine- and dietary-Induced thiamine deficiency and alcohol exposure in the alcohol-preferring rat: A longitudinal magnetic resonance imaging and spectroscopy study. Neuropsychopharmacology. 2007;32(5):1159–1177. doi: 10.1038/sj.npp.1301107. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Adalsteinsson E, Sood R, et al. Longitudinal brain magnetic resonance imaging study of the alcohol-preferring rat: Part II: Effects of voluntary chronic alcohol consumption. Alcoholism: Clinical and Experimental Research. 2006a;30(7):1248–1261. doi: 10.1111/j.1530-0277.2006.00146.x. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Adalsteinsson E, Spielman D, et al. In vivo spectroscopic quantification of the N-acetyl moiety, creatine, and choline from large volumes of brain gray and white matter: Effects of normal aging. Magnetic Resonance in Medicine. 1999;41(2):276–284. doi: 10.1002/(sici)1522-2594(199902)41:2<276::aid-mrm10>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Adalsteinsson E, Sullivan EV. Supratentorial profile of white matter microstructural integrity in recovering alcoholic men and women. Biological Psychiatry. 2006b;59(4):364–372. doi: 10.1016/j.biopsych.2005.06.025. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Lim KO, Desmond JE, Sullivan EV. Thinning of the corpus callosum in older alcoholic men: A magnetic resonance imaging study. Alcoholism: Clinical and Experimental Research. 1996;20(4):752–757. doi: 10.1111/j.1530-0277.1996.tb01682.x. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Lim KO, Rosenbloom MJ. Structural imaging of the brain in chronic alcoholism. In: Zakhari S, Witt E, editors. Imaging in Alcohol Research: NIAAA Research Monograph No. 21. Rockville, MD: U.S. Department of Health and Human Services; 1992. pp. 99–120. [Google Scholar]
- Pfefferbaum A, Rohlfing T, Rosenbloom MJ, et al. Variation in longitudinal trajectories of regional brain volumes of healthy men and women (ages 10 to 85 years) measured with atlas-based parcellation of MRI. NeuroImage. 2013;65:176–193. doi: 10.1016/j.neuroimage.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom M, Chu W, et al. White matter microstructural recovery with abstinence and decline with relapse in alcohol dependence interacts with normal ageing: A controlled longitudinal DTI study. Lancet Psychiatry. 2014;1(3):202–212. doi: 10.1016/S2215-0366(14)70301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom M, Deshmukh A, Sullivan E. Sex differences in the effects of alcohol on brain structure. American Journal of Psychiatry. 2001;158(2):188–197. doi: 10.1176/appi.ajp.158.2.188. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom M, Rohlfing T, Sullivan EV. Degradation of association and projection white matter systems in alcoholism detected with quantitative fiber tracking. Biological Psychiatry. 2009a;65(8):680–690. doi: 10.1016/j.biopsych.2008.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom M, Sullivan EV. Alcoholism and AIDS: Magnetic resonance imaging approaches for detecting interactive neuropathology. Alcoholism: Clinical and Experimental Research. 2002a;26(7):1031–1046. doi: 10.1097/01.ALC.0000021146.01778.55. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom MJ, Fama R, et al. Transcallosal white matter degradation detected with quantitative fiber tracking in alcoholic men and women: Selective relations to dissociable functions. Alcoholism: Clinical and Experimental Research. 2010;34(7):1201–1211. doi: 10.1111/j.1530-0277.2010.01197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom MJ, Rohlfing T, Sullivan EV. Degradation of association and projection white matter systems in alcoholism detected with quantitative fiber tracking. Biological Psychiatry. 2009b;65(8):680–690. doi: 10.1016/j.biopsych.2008.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom MJ, Serventi K, Sullivan EV. Corpus callosum, pons and cortical white matter in alcoholic women. Alcoholism: Clinical and Experimental Research. 2002b;26(3):400–406. [PubMed] [Google Scholar]
- Pfefferbaum A, Rosenbloom MJ, Serventi KL, Sullivan EV. Brain volumes, RBC status, and hepatic function in alcoholics after 1 and 4 weeks of sobriety: Predictors of outcome. American Journal of Psychiatry. 2004;161(7):1190–1196. doi: 10.1176/appi.ajp.161.7.1190. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV, Hedehus M, et al. In vivo detection and functional correlates of white matter microstructural disruption in chronic alcoholism. Alcoholism: Clinical and Experimental Research. 2000;24(8):1214–1221. [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV, Mathalon DH, Lim KO. Frontal lobe volume loss observed with magnetic resonance imaging in older chronic alcoholics. Alcoholism: Clinical and Experimental Research. 1997;21(3):521–529. doi: 10.1111/j.1530-0277.1997.tb03798.x. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV, Mathalon DH, et al. Longitudinal changes in magnetic resonance imaging brain volumes in abstinent and relapsed alcoholics. Alcoholism: Clinical and Experimental Research. 1995;19(5):1177–1191. doi: 10.1111/j.1530-0277.1995.tb01598.x. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Zahr NM, Mayer D, et al. Ventricular expansion in wild-type Wistar rats after alcohol exposure by vapor chamber. Alcoholism: Clinical and Experimental Research. 2008;32(8):1459–1467. doi: 10.1111/j.1530-0277.2008.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Zahr NM, Mayer D, et al. Dynamic responses of selective brain white matter fiber tracts to binge alcohol and recovery in the rat. PLoS One. 2015;10(4):e0124885. doi: 10.1371/journal.pone.0124885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfister HW, Einhaupl KM, Brandt T. Mild central pontine myelinolysis: A frequently undetected syndrome. European Archives of Psychiatry and Neurological Sciences. 1985;235(3):134–139. doi: 10.1007/BF00380982. [DOI] [PubMed] [Google Scholar]
- Pierpaoli C, Jezzard P, Basser PJ, et al. Diffusion tensor MR imaging of the human brain. Radiology. 1996;201(3):637–648. doi: 10.1148/radiology.201.3.8939209. [DOI] [PubMed] [Google Scholar]
- Piguet O, Cramsie J, Bennett HP, et al. Contributions of age and alcohol consumption to cerebellar integrity, gait and cognition in non-demented very old individuals. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(8):504–511. doi: 10.1007/s00406-006-0671-5. [DOI] [PubMed] [Google Scholar]
- Pitel AL, Chanraud S, Sullivan EV, Pfefferbaum A. Callosal microstructural abnormalities in Alzheimer’s disease and alcoholism: Same phenotype, different mechanisms. Psychiatry Research. 2010;184(1):49–56. doi: 10.1016/j.pscychresns.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitel AL, Chetelat G, Le Berre AP, et al. Macrostructural abnormalities in Korsakoff syndrome compared with uncomplicated alcoholism. Neurology. 2012;78(17):1330–1333. doi: 10.1212/WNL.0b013e318251834e. [DOI] [PubMed] [Google Scholar]
- Pitkin SR, Savage LM. Aging potentiates the acute and chronic neurological symptoms of pyrithiamine-induced thiamine deficiency in the rodent. Behavioural Brain Research. 2001;119(2):167–177. doi: 10.1016/s0166-4328(00)00350-8. [DOI] [PubMed] [Google Scholar]
- Poordad FF. Review article: The burden of hepatic encephalopathy. Alimentary Pharmacology & Therapeutics. 2007;25(Suppl 1):3–9. doi: 10.1111/j.1746-6342.2006.03215.x. [DOI] [PubMed] [Google Scholar]
- Pound P, Ebrahim S, Sandercock P, et al. Where is the evidence that animal research benefits humans? BMJ. 2004;328(7438):514–517. doi: 10.1136/bmj.328.7438.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poupon C, Clark CA, Frouin V, et al. Tracking white matter fascicles with diffusion tensor imaging. Proceedings of the Seventh International Society for Magnetic Resonance in Medicine. 1999;325 [Google Scholar]
- Pouwels PJ, Frahm J. Regional metabolite concentrations in human brain as determined by quantitative localized proton MRS. Magnetic Resonance in Medicine. 1998;39(1):53–60. doi: 10.1002/mrm.1910390110. [DOI] [PubMed] [Google Scholar]
- Poveda MJ, Bernabeu A, Concepción L, et al. Brain edema dynamics in patients with overt hepatic encephalopathy: A magnetic resonance imaging study. NeuroImage. 2010;52(2):481–487. doi: 10.1016/j.neuroimage.2010.04.260. [DOI] [PubMed] [Google Scholar]
- Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nature Reviews. Gastroenterology & Hepatology. 2010;7(9):515–525. doi: 10.1038/nrgastro.2010.116. [DOI] [PubMed] [Google Scholar]
- Price DB, Kramer J, Hotson GC, Loh JP. Central pontine myelinolysis: Report of a case with distinctive appearance on MR imaging. AJNR American Journal of Neuroradiology. 1987;8(3):576–577. [PMC free article] [PubMed] [Google Scholar]
- Pujol J, Kulisevsky J, Moreno A, et al. Neurospectroscopic alterations and globus pallidus hyperintensity as related magnetic resonance markers of reversible hepatic encephalopathy. Neurology. 1996;47(6):1526–1530. doi: 10.1212/wnl.47.6.1526. [DOI] [PubMed] [Google Scholar]
- Qin L, Crews FT. Focal thalamic degeneration from ethanol and thiamine deficiency is associated with neuroimmune gene induction, microglial activation, and lack of monocarboxylic acid transporters. Alcoholism: Clinical and Experimental Research. 2014;38(3):657–671. doi: 10.1111/acer.12272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rackayova V, Braissant O, McLin VA, et al. 1H and 31P magnetic resonance spectroscopy in a rat model of chronic hepatic encephalopathy: In vivo longitudinal measurements of brain energy metabolism. Metabolic Brain Disease. 2016;31(6):1303–1314. doi: 10.1007/s11011-015-9715-8. [DOI] [PubMed] [Google Scholar]
- Rakic P. Neurogenesis in adult primates. Progress in Brain Research. 2002;138:3–14. doi: 10.1016/S0079-6123(02)38067-1. [DOI] [PubMed] [Google Scholar]
- Rando K, Hong KI, Bhagwagar Z, et al. Association of frontal and posterior cortical gray matter volume with time to alcohol relapse: A prospective study. American Journal of Psychiatry. 2011;168(2):183–192. doi: 10.1176/appi.ajp.2010.10020233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raz N, Ghisletta P, Rodrigue KM, et al. Trajectories of brain aging in middle-aged and older adults: Regional and individual differences. NeuroImage. 2010;51(2):501–511. doi: 10.1016/j.neuroimage.2010.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed RJ, Grant I, Rourke SB. Long-term abstinent alcoholics have normal memory. Alcoholism: Clinical and Experimental Research. 1992;16(4):677–683. doi: 10.1111/j.1530-0277.1992.tb00660.x. [DOI] [PubMed] [Google Scholar]
- Ridley NJ, Draper B, Withall A. Alcohol-related dementia: An update of the evidence. Alzheimers Research & Therapy. 2013;5(1):3. doi: 10.1186/alzrt157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riethdorf L, Warzok R, Schwesinger G. Alcoholic encephalopathies in autopsy material. [Article in German] Zentralblatt für Pathologie. 1991;137(1):48–56. [PubMed] [Google Scholar]
- Ritchie K, Villebrun D. Epidemiology of alcohol-related dementia. Handbook of Clinical Neurology. 2008;89:845–850. doi: 10.1016/S0072-9752(07)01273-0. [DOI] [PubMed] [Google Scholar]
- Roerecke M, Greenfield TK, Kerr WC, et al. Heavy drinking occasions in relation to ischaemic heart disease mortality—an 11–22 year follow-up of the 1984 and 1995 US National Alcohol Surveys. International Journal of Epidemiology. 2011;40(5):1401–1410. doi: 10.1093/ije/dyr129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohlfing T. Transformation model and constraints cause bias in statistics on deformation fields. Medical Image Computing and Computer-Assisted Intervention: International Conference on Medical Image Computing and Computer-Assisted Intervention. 2006;9(Pt. 1):207–214. doi: 10.1007/11866565_26. [DOI] [PubMed] [Google Scholar]
- Rose SE, Nixon PF, Zelaya FO, et al. Application of high field localised in vivo 1H MRS to study biochemical changes in the thiamin deficient rat brain under glucose load. NMR in Biomedicine. 1993;6(5):324–328. doi: 10.1002/nbm.1940060507. [DOI] [PubMed] [Google Scholar]
- Rosenbloom MJ, Rohlfing T, O’Reilly AW, et al. Improvement in memory and static balance with abstinence in alcoholic men and women: Selective relations with change in brain structure. Psychiatry Research: Neuroimaging. 2007;155(2):91–102. doi: 10.1016/j.pscychresns.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbloom MJ, Sassoon SA, Fama R, et al. Frontal callosal fiber integrity selectively predicts coordinated psychomotor performance in chronic alcoholism. Brain Imaging and Behavior. 2008;2(2):74–83. doi: 10.1007/s11682-007-9017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross BD, Jacobson S, Villamil F, et al. Subclinical hepatic encephalopathy: Proton MR spectroscopic abnormalities. Radiology. 1994;193(2):457–463. doi: 10.1148/radiology.193.2.7972763. [DOI] [PubMed] [Google Scholar]
- Ross LJ, Wilson M, Banks M, et al. Prevalence of malnutrition and nutritional risk factors in patients undergoing alcohol and drug treatment. Nutrition. 2012;28(7–8):738–743. doi: 10.1016/j.nut.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Rourke SB, Grant I. The interactive effects of age and length of abstinence on the recovery of neuropsychological functioning in chronic male alcoholics: A 2-year follow-up study. Journal of the International Neuropsychological Society. 1999;5(3):234–246. doi: 10.1017/s1355617799533067. [DOI] [PubMed] [Google Scholar]
- Rovira A, Alonso J, Cordoba J. MR imaging findings in hepatic encephalopathy. AJNR American Journal of Neuroradiology. 2008;29(9):1612–1621. doi: 10.3174/ajnr.A1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovira A, Cordoba J, Sanpedro F, et al. Normalization of T2 signal abnormalities in hemispheric white matter with liver transplant. Neurology. 2002;59(3):335–341. doi: 10.1212/wnl.59.3.335. [DOI] [PubMed] [Google Scholar]
- Rumboldt Z, Castillo M, Huang B, Rossi A, editors. Brain Imaging with MRI and CT: An Image Pattern Approach. Cambridge, UK: Cambridge University Press; 2010. [Google Scholar]
- Sair HI, Mohamed FB, Patel S, et al. Diffusion tensor imaging and fiber-tracking in Marchiafava-Bignami disease. Journal of Neuroimaging. 2006;16(3):281–285. doi: 10.1111/j.1552-6569.2006.00041.x. [DOI] [PubMed] [Google Scholar]
- Sandercock P, Roberts I. Systematic reviews of animal experiments. Lancet. 2002;360(9333):586. doi: 10.1016/S0140-6736(02)09812-4. [DOI] [PubMed] [Google Scholar]
- Schaeffner E, Ritz E. Alcohol and kidney damage: A Janus-faced relationship. Kidney International. 2012;81(9):816–818. doi: 10.1038/ki.2012.14. [DOI] [PubMed] [Google Scholar]
- Schmidt KS, Gallo JL, Ferri C, et al. The neuropsychological profile of alcohol-related dementia suggests cortical and subcortical pathology. Dementia and Geriatric Cognitive Disorders. 2005;20(5):286–291. doi: 10.1159/000088306. [DOI] [PubMed] [Google Scholar]
- Scholz E, Diener H, Dichgans J, et al. Incidence of peripheral neuropathy and cerebellar ataxia in chronic alcoholics. Journal of Neurology. 1986;233(4):212–217. doi: 10.1007/BF00314021. [DOI] [PubMed] [Google Scholar]
- Schroth G, Naegele T, Klose U, et al. Reversible brain shrinkage in abstinent alcoholics, measured by MRI. Neuroradiology. 1988;30(5):385–389. doi: 10.1007/BF00404102. [DOI] [PubMed] [Google Scholar]
- Schuff N, Amend DL, Knowlton R, et al. Age-related metabolite changes and volume loss in the hippocampus by magnetic resonance spectroscopy and imaging. Neurobiology of Aging. 1999;20(3):279–285. doi: 10.1016/s0197-4580(99)00022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte T, Sullivan EV, Muller-Oehring EM, et al. Corpus callosal microstructural integrity influences interhemispheric processing: A diffusion tensor imaging study. Cerebral Cortex. 2005;15(9):1384–1392. doi: 10.1093/cercor/bhi020. [DOI] [PubMed] [Google Scholar]
- Schweinsburg BC, Alhassoon OM, Taylor MJ, et al. Effects of alcoholism and gender on brain metabolism. American Journal of Psychiatry. 2003;160(6):1180–1183. doi: 10.1176/appi.ajp.160.6.1180. [DOI] [PubMed] [Google Scholar]
- Schweinsburg BC, Taylor MJ, Videen JS, et al. Elevated myo-inositol in gray matter of recently detoxified but not long-term abstinent alcoholics: A preliminary MR spectroscopy study. Alcoholism: Clinical and Experimental Research. 2000;24(5):699–705. [PubMed] [Google Scholar]
- Sechi G, Serra A. Wernicke’s encephalopathy: New clinical settings and recent advances in diagnosis and management. Lancet Neurology. 2007;6(5):442–455. doi: 10.1016/S1474-4422(07)70104-7. [DOI] [PubMed] [Google Scholar]
- Segobin S, Ritz L, Lannuzel C, et al. Integrity of white matter microstructure in alcoholics with and without Korsakoff’s syndrome. Human Brain Mapping. 2015;36(7):2795–2808. doi: 10.1002/hbm.22808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seitz D, Widmann U, Seeger U, et al. Localized proton magnetic resonance spectroscopy of the cerebellum in detoxifying alcoholics. Alcoholism: Clinical and Experimental Research. 1999;23(1):158–163. [PubMed] [Google Scholar]
- Seok J, Warren HS, Cuenca AG, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(9):3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear PK, Jernigan TL, Butters N. Volumetric magnetic resonance imaging quantification of longitudinal brain changes in abstinent alcoholics. Alcoholism: Clinical and Experimental Research. 1994;18(1):172–176. doi: 10.1111/j.1530-0277.1994.tb00899.x. [DOI] [PubMed] [Google Scholar]
- Shear PK, Sullivan EV, Lane B, Pfefferbaum A. Mammillary body and cerebellar shrinkage in chronic alcoholics with and without amnesia. Alcoholism: Clinical and Experimental Research. 1996;20(8):1489–1495. doi: 10.1111/j.1530-0277.1996.tb01153.x. [DOI] [PubMed] [Google Scholar]
- Sheedy D, Lara A, Garrick T, Harper C. Size of mamillary bodies in health and disease: Useful measurements in neuroradiological diagnosis of Wernicke’s encephalopathy. Alcoholism: Clinical and Experimental Research. 1999;23(10):1624–1628. [PMC free article] [PubMed] [Google Scholar]
- Singh N, Yu VL, Gayowski T. Central nervous system lesions in adult liver transplant recipients: Clinical review with implications for management. Medicine. 1994;73(2):110–118. doi: 10.1097/00005792-199403000-00004. [DOI] [PubMed] [Google Scholar]
- Singhal A, Nagarajan R, Hinkin CH, et al. Two-dimensional MR spectroscopy of minimal hepatic encephalopathy and neuropsychological correlates in vivo. Journal of Magnetic Resonance Imaging. 2010;32(1):35–43. doi: 10.1002/jmri.22216. [DOI] [PubMed] [Google Scholar]
- Soher BJ, Hurd RE, Sailasuta N, Barker PB. Quantitation of automated single-voxel proton MRS using cerebral water as an internal reference. Magnetic Resonance in Medicine. 1996;36(3):335–339. doi: 10.1002/mrm.1910360302. [DOI] [PubMed] [Google Scholar]
- Sokoloff L, Reivich M, Kennedy C, et al. The [14C] deoxyglucose method for the measurement of local cerebral glucose utilization: Theory, procedure, and normal values in the conscious and anesthetized albino rat. Journal of Neurochemistry. 1977;28(5):897–916. doi: 10.1111/j.1471-4159.1977.tb10649.x. [DOI] [PubMed] [Google Scholar]
- Song SK, Sun SW, Ramsbottom MJ, et al. Dysmyelination revealed through MRI as increased radial (but unchanged axial) diffusion of water. NeuroImage. 2002;17(3):1429–1436. doi: 10.1006/nimg.2002.1267. [DOI] [PubMed] [Google Scholar]
- Sorensen TI, Orholm M, Bentsen KD, et al. Prospective evaluation of alcohol abuse and alcoholic liver injury in men as predictors of development of cirrhosis. Lancet. 1984;2(8397):241–244. doi: 10.1016/s0140-6736(84)90295-2. [DOI] [PubMed] [Google Scholar]
- Sorg SF, Taylor MJ, Alhassoon OM, et al. Frontal white matter integrity predictors of adult alcohol treatment outcome. Biological Psychiatry. 2012;71(3):262–268. doi: 10.1016/j.biopsych.2011.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielman D, Butts K, de Crespigny A, Moseley M. Diffusion-weighted imaging of clinical stroke. International Journal of Neuroradiology. 1996;1:44–55. [Google Scholar]
- Squire LR, Amaral DG, Press GA. Magnetic resonance imaging of the hippocampal formation and mammillary nuclei distinguish medial temporal lobe and diencephalic amnesia. Journal of Neuroscience. 1990;10(9):3106–3117. doi: 10.1523/JNEUROSCI.10-09-03106.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JT. The frontal/subcortical dementias: Common dementing illnesses associated with prominent and disturbing behavioral changes. Geriatrics. 2006;61(8):23–27. [PubMed] [Google Scholar]
- Stork J. Atrophy of the cerebellar vermis and chronic alcoholism. Clinical-anatomical study of 44 cases. [Article in German] Schweizer Archiv für Neurologie, Neurochirurgie und Psychiatrie. 1967;99(1):40–82. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2013. Rockville, MD: SAMHSA; 2013. [Google Scholar]
- Sullivan EV. Compromised pontocerebellar and cerebellothalamocortical systems: Speculations on their contributions to cognitive and motor impairment in nonamnesic alcoholism. Alcoholism: Clinical and Experimental Research. 2003;27(9):1409–1419. doi: 10.1097/01.ALC.0000085586.91726.46. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Marsh L. Hippocampal volume deficits in alcoholic Korsakoff’s syndrome. Neurology. 2003;61(12):1716–1719. doi: 10.1212/01.wnl.0000098940.31882.bb. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Pfefferbaum A. Neurocircuitry in alcoholism: A substrate of disruption and repair. Psychopharmacology. 2005;180(4):583–594. doi: 10.1007/s00213-005-2267-6. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Pfefferbaum A. Neuroimaging of the Wernicke-Korsakoff syndrome. Alcohol and Alcoholism. 2009;44(2):155–165. doi: 10.1093/alcalc/agn103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan EV, Pfefferbaum A. Diffusion tensor imaging in aging and age-related neurodegenerative disorders. In: Jones DK, editor. Diffusion MRI: Theory, Methods and Applications. New York: Oxford University Press; 2011. pp. 624–643. [Google Scholar]
- Sullivan EV, Adalsteinsson E, Sood R, et al. Longitudinal brain magnetic resonance imaging study of the alcohol-preferring rat. Part I: Adult brain growth. Alcoholism: Clinical and Experimental Research. 2006a;30(7):1234–1247. doi: 10.1111/j.1530-0277.2006.00145.x. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Deshmukh A, De Rosa E, et al. Striatal and forebrain nuclei volumes: Contribution to motor function and working memory deficits in alcoholism. Biological Psychiatry. 2005a;57(7):768–776. doi: 10.1016/j.biopsych.2004.12.012. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Deshmukh A, Desmond JE, et al. Cerebellar volume decline in normal aging, alcoholism, and Korsakoff’s syndrome: Relation to ataxia. Neuropsychology. 2000a;14(3):341–352. doi: 10.1037//0894-4105.14.3.341. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Harding AJ, Pentney R, et al. Disruption of frontocerebellar circuitry and function in alcoholism. Alcoholism: Clinical and Experimental Research. 2003;27(2):301–309. doi: 10.1097/01.ALC.0000052584.05305.98. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Lane B, Deshmukh A, et al. In vivo mammillary body volume deficits in amnesic and nonamnesic alcoholics. Alcoholism: Clinical and Experimental Research. 1999;23(10):1629–1636. [PubMed] [Google Scholar]
- Sullivan EV, Marsh L, Mathalon DH, et al. Anterior hippocampal volume deficits in nonamnesic, aging chronic alcoholics. Alcoholism: Clinical and Experimental Research. 1995;19(1):110–122. doi: 10.1111/j.1530-0277.1995.tb01478.x. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Marsh L, Mathalon DH, et al. Relationship between alcohol withdrawal seizures and temporal lobe white matter volume deficits. Alcoholism: Clinical and Experimental Research. 1996;20(2):348–354. doi: 10.1111/j.1530-0277.1996.tb01651.x. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Marsh L, Pfefferbaum A. Preservation of hippocampal volume throughout adulthood in healthy men and women. Neurobiology of Aging. 2005b;26(7):1093–1098. doi: 10.1016/j.neurobiolaging.2004.09.015. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Rose J, Pfefferbaum A. Effect of vision, touch and stance on cerebellar vermian-related sway and tremor: A quantitative physiological and MRI study. Cerebral Cortex. 2006b;16(8):1077–1086. doi: 10.1093/cercor/bhj048. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Rose J, Pfefferbaum A. Physiological and focal cerebellar substrates of abnormal postural sway and tremor in alcoholic women. Biological Psychiatry. 2010;67(1):44–51. doi: 10.1016/j.biopsych.2009.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan EV, Rosenbloom MJ, Lim KO, Pfefferbaum A. Longitudinal changes in cognition, gait, and balance in abstinent and relapsed alcoholic men: Relationships to changes in brain structure. Neuropsychology. 2000b;14(2):178–188. [PubMed] [Google Scholar]
- Sullivan EV, Rosenbloom MJ, Pfefferbaum A. Pattern of motor and cognitive deficits in detoxified alcoholic men. Alcoholism: Clinical and Experimental Research. 2000c;24(5):611–621. [PubMed] [Google Scholar]
- Sullivan EV, Sable HJ, Strother WN, et al. Neuroimaging of rodent and primate models of alcoholism: Initial reports from the Integrative Neuroscience Initiative on Alcoholism. Alcoholism: Clinical and Experimental Research. 2005c;29(2):287–294. doi: 10.1097/01.alc.0000153546.39946.ec. [DOI] [PubMed] [Google Scholar]
- Suzuki K, Izumi M. Alcohol is a risk factor not for thalamic but for putaminal hemorrhage: The Akita Stroke Registry. Journal of Stroke and Cerebrovascular Diseases. 2013;22(7):1064–1069. doi: 10.1016/j.jstrokecerebrovasdis.2012.07.009. [DOI] [PubMed] [Google Scholar]
- Takahashi H, Koehler RC, Brusilow SW, Traystman RJ. Inhibition of brain glutamine accumulation prevents cerebral edema in hyperammonemic rats. American Journal of Physiology. 1991;261(3 Pt. 2):H825–H829. doi: 10.1152/ajpheart.1991.261.3.H825. [DOI] [PubMed] [Google Scholar]
- Tarasow E, Panasiuk A, Siergiejczyk L, et al. MR and 1H MR spectroscopy of the brain in patients with liver cirrhosis and early stages of hepatic encephalopathy. Hepato-Gastroenterology. 2003;50(54):2149–2153. [PubMed] [Google Scholar]
- Taylor-Robinson SD, Buckley C, Changani KK, et al. Cerebral proton and phosphorus-31 magnetic resonance spectroscopy in patients with subclinical hepatic encephalopathy. Liver. 1999;19(5):389–398. doi: 10.1111/j.1478-3231.1999.tb00067.x. [DOI] [PubMed] [Google Scholar]
- Taylor-Robinson SD, Oatridge A, Hajnal JV, et al. MR imaging of the basal ganglia in chronic liver disease: Correlation of T1-weighted and magnetisation transfer contrast measurements with liver dysfunction and neuropsychiatric status. Metabolic Brain Disease. 1995;10(2):175–188. doi: 10.1007/BF01991864. [DOI] [PubMed] [Google Scholar]
- Taylor-Robinson SD, Sargentoni J, Marcus CD, et al. Regional variations in cerebral proton spectroscopy in patients with chronic hepatic encephalopathy. Metabolic Brain Disease. 1994;9(4):347–359. doi: 10.1007/BF02098881. [DOI] [PubMed] [Google Scholar]
- Tedeschi G, Bertolino A, Massaquoi SG, et al. Proton magnetic resonance spectroscopic imaging in patients with cerebellar degeneration. Annals of Neurology. 1996;39(1):71–78. doi: 10.1002/ana.410390111. [DOI] [PubMed] [Google Scholar]
- Tedeschi G, Bertolino A, Righini A, et al. Brain regional distribution pattern of metabolite signal intensities in young adults by proton magnetic resonance spectroscopic imaging. Neurology. 1995;45(7):1384–1391. doi: 10.1212/wnl.45.7.1384. [DOI] [PubMed] [Google Scholar]
- Terakawa H, Abe K, Watanabe Y, et al. Proton magnetic resonance spectroscopy (1H MRS) in patients with sporadic cerebellar degeneration. Journal of Neuroimaging. 1999;9(2):72–77. doi: 10.1111/jon19999272. [DOI] [PubMed] [Google Scholar]
- Thomas MA, Huda A, Guze B, et al. Cerebral 1H MR spectroscopy and neuropsychologic status of patients with hepatic encephalopathy. AJR American Journal of Roentgenology. 1998;171(4):1123–1130. doi: 10.2214/ajr.171.4.9763008. [DOI] [PubMed] [Google Scholar]
- Thomson AD. Mechanisms of vitamin deficiency in chronic alcohol misusers and the development of the Wernicke-Korsakoff syndrome. Alcohol and Alcoholism. 2000;35(Suppl 1):2–7. doi: 10.1093/alcalc/35.supplement_1.2. [DOI] [PubMed] [Google Scholar]
- Thomson AD, Cook CC, Guerrini I, et al. Wernicke’s encephalopathy: “Plus ça change, plus c’est la même chose”. Alcohol and Alcoholism. 2008;43(2):180–186. doi: 10.1093/alcalc/agm149. [DOI] [PubMed] [Google Scholar]
- Thomson AD, Cook CC, Touquet R, et al. The Royal College of Physicians report on alcohol: Guidelines for managing Wernicke’s encephalopathy in the accident and emergency department. Alcohol and Alcoholism. 2002;37(6):513–521. doi: 10.1093/alcalc/37.6.513. [DOI] [PubMed] [Google Scholar]
- Thomson AD, Guerrini I, Marshall EJ. The evolution and treatment of Korsakoff’s syndrome: Out of sight, out of mind? Neuropsychology Review. 2012;22(2):81–92. doi: 10.1007/s11065-012-9196-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorarinsson BL, Olafsson E, Kjartansson O, Blondal H. Wernicke’s encephalopathy in chronic alcoholics. [Article in Icelandic] Laeknabladid. 2011;97(1):21–29. doi: 10.17992/lbl.2011.01.338. [DOI] [PubMed] [Google Scholar]
- Tirotta E, Carbajal KS, Schaumburg CS, et al. Cell replacement therapies to promote remyelination in a viral model of demyelination. Journal of Neuroimmunology. 2010;224(1–2):101–107. doi: 10.1016/j.jneuroim.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torisu S, Washizu M, Hasegawa D, Orima H. Brain magnetic resonance imaging characteristics in dogs and cats with congenital portosystemic shunts. Veterinary Radiology & Ultrasound. 2005;46(6):447–451. doi: 10.1111/j.1740-8261.2005.00082.x. [DOI] [PubMed] [Google Scholar]
- Torvik A, Torp S. The prevalence of alcoholic cerebellar atrophy: A morphometric and histological study of an autopsy material. Journal of Neurological Sciences. 1986;75(1):43–51. doi: 10.1016/0022-510x(86)90049-3. [DOI] [PubMed] [Google Scholar]
- Trivedi R, Bagga D, Bhattacharya D, et al. White matter damage is associated with memory decline in chronic alcoholics: A quantitative diffusion tensor tractography study. Behavioural Brain Research. 2013;250:192–198. doi: 10.1016/j.bbr.2013.05.001. [DOI] [PubMed] [Google Scholar]
- Tuntiyatorn L, Laothamatas J. Acute Marchiafava-Bignami disease with callosal, cortical, and white matter involvement. Emergency Radiology. 2008;15(2):137–140. doi: 10.1007/s10140-007-0640-y. [DOI] [PubMed] [Google Scholar]
- Urenjak J, Williams SR, Gadian DG, Noble M. Specific expression of N-acetylaspartate in neurons, oligodendrocyte-type-2 astrocyte progenitors, and immature oligodendrocytes in vitro. Journal of Neurochemistry. 1992;59(1):55–61. doi: 10.1111/j.1471-4159.1992.tb08875.x. [DOI] [PubMed] [Google Scholar]
- Urenjak J, Williams SR, Gadian DG, Noble M. Proton nuclear magnetic resonance spectroscopy unambiguously identifies different neural cell types. Journal of Neuroscience. 1993;13(3):981–989. doi: 10.1523/JNEUROSCI.13-03-00981.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Holst RJ, de Ruiter MB, van den Brink W, et al. A voxel-based morphometry study comparing problem gamblers, alcohol abusers, and healthy controls. Drug and Alcohol Dependence. 2012;124(1–2):142–148. doi: 10.1016/j.drugalcdep.2011.12.025. [DOI] [PubMed] [Google Scholar]
- Vaquero J, Chung C, Cahill ME, Blei AT. Pathogenesis of hepatic encephalopathy in acute liver failure. Seminars in Liver Disease. 2003;23(3):259–269. doi: 10.1055/s-2003-42644. [DOI] [PubMed] [Google Scholar]
- Vemuganti R, Kalluri H, Yi JH, et al. Gene expression changes in thalamus and inferior colliculus associated with inflammation, cellular stress, metabolism and structural damage in thiamine deficiency. European Journal of Neuroscience. 2006;23(5):1172–1188. doi: 10.1111/j.1460-9568.2006.04651.x. [DOI] [PubMed] [Google Scholar]
- Venkatasubramanian PN, Tom B, Blei AT, Wyrwicz AM. Monitoring of brain water by chemical shift imaging during ammonia-induced brain swelling in rats after portacaval anastomosis. Artificial Organs. 2001;25(7):551–557. doi: 10.1046/j.1525-1594.2001.025007551.x. [DOI] [PubMed] [Google Scholar]
- Vetreno RP, Ramos RL, Anzalone S, Savage LM. Brain and behavioral pathology in an animal model of Wernicke’s encephalopathy and Wernicke-Korsakoff Syndrome. Brain Research. 2012;1436:178–192. doi: 10.1016/j.brainres.2011.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetreno RP, Yaxley R, Paniagua B, Crews FT. Diffusion tensor imaging reveals adolescent binge ethanol-induced brain structural integrity alterations in adult rats that correlate with behavioral dysfunction. Addiction Biology. 2016;21(4):939–953. doi: 10.1111/adb.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor M, Adams RD, Collins GH. The Wernicke-Korsakoff Syndrome. Philadelphia: F.A. Davis Company; 1971. [Google Scholar]
- Victor M, Adams RD, Collins GH. The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders Due to Alcoholism and Malnutrition. 2nd ed. Philadelphia: F.A. Davis Company; 1989. [Google Scholar]
- Videen JS, Michaelis T, Pinto P, Ross BD. Human cerebral osmolytes during chronic hyponatremia. A proton magnetic resonance spectroscopy study. Journal of Clinical Investigation. 1995;95(2):788–793. doi: 10.1172/JCI117728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Kim SW, Wang GJ, et al. Acute alcohol intoxication decreases glucose metabolism but increases acetate uptake in the human brain. NeuroImage. 2013;64:277–283. doi: 10.1016/j.neuroimage.2012.08.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Fowler JS, et al. Regional cerebral metabolism in female alcoholics of moderate severity does not differ from that of controls. Alcoholism: Clinical and Experimental Research. 1998;22(8):1850–1854. [PubMed] [Google Scholar]
- Waragai M, Satoh T. Serial MRI of extrapontine myelinolysis of the basal ganglia: A case report. Journal of the Neurological Sciences. 1998;161(2):173–175. doi: 10.1016/s0022-510x(98)00275-5. [DOI] [PubMed] [Google Scholar]
- Weissenborn K, Ahl B, Fischer-Wasels D, et al. Correlations between magnetic resonance spectroscopy alterations and cerebral ammonia and glucose metabolism in cirrhotic patients with and without hepatic encephalopathy. Gut. 2007;56(12):1736–1742. doi: 10.1136/gut.2006.110569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenz H, Eisele P, Artemis D, et al. Acute Marchiafava-Bignami disease with extensive diffusion restriction and early recovery: Case report and review of the literature. Journal of Neuroimaging. 2014;24(4):421–424. doi: 10.1111/j.1552-6569.2012.00755.x. [DOI] [PubMed] [Google Scholar]
- Wilhelm J, Frieling H, Hillemacher T, et al. Hippocampal volume loss in patients with alcoholism is influenced by the consumed type of alcoholic beverage. Alcohol and Alcoholism. 2008;43(3):296–299. doi: 10.1093/alcalc/agn002. [DOI] [PubMed] [Google Scholar]
- Wrase J, Makris N, Braus DF, et al. Amygdala volume associated with alcohol abuse relapse and craving. American Journal of Psychiatry. 2008;165(9):1179–1184. doi: 10.1176/appi.ajp.2008.07121877. [DOI] [PubMed] [Google Scholar]
- Yamamoto H, Konno H, Yamamoto T, et al. Glutamine synthetase of the human brain: Purification and characterization. Journal of Neurochemistry. 1987;49(2):603–609. doi: 10.1111/j.1471-4159.1987.tb02906.x. [DOI] [PubMed] [Google Scholar]
- Yeh PH, Simpson K, Durazzo TC, et al. Tract-based spatial statistics (TBSS) of diffusion tensor imaging data in alcohol dependence: Abnormalities of the motivational neurocircuitry. Psychiatry Research. 2009;173(1):22–30. doi: 10.1016/j.pscychresns.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeligar SM, Harris FL, Hart CM, Brown LA. Ethanol induces oxidative stress in alveolar macrophages via upregulation of NADPH oxidases. Journal of Immunology. 2012;188(8):3648–3657. doi: 10.4049/jimmunol.1101278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshizaki T, Hashimoto T, Fujimoto K, Oguchi K. Evolution of callosal and cortical lesions on MRI in Marchiafava-Bignami disease. Case Reports in Neurology. 2010;2(1):19–23. doi: 10.1159/000296705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Alt C, Mayer D, et al. Associations between in vivo neuroimaging and postmortem brain cytokine markers in a rodent model of Wernicke’s encephalopathy. Experimental Neurology. 2014a;261:109–119. doi: 10.1016/j.expneurol.2014.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Kaufman KL, Harper CG. Clinical and pathological features of alcohol-related brain damage. Nature Reviews Neurology. 2011;7(5):284–294. doi: 10.1038/nrneurol.2011.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Mayer D, Pfefferbaum A, Sullivan EV. Low striatal glutamate levels underlie cognitive decline in the elderly: Evidence from in vivo molecular spectroscopy. Cerebral Cortex. 2008;18(10):2241–2250. doi: 10.1093/cercor/bhm250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Mayer D, Rohlfing T, et al. Brain injury and recovery following binge ethanol: Evidence from in vivo magnetic resonance spectroscopy. Biological Psychiatry. 2010;67(9):846–854. doi: 10.1016/j.biopsych.2009.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Mayer D, Rohlfing T, et al. A mechanism of rapidly reversible cerebral ventricular enlargement independent of tissue atrophy. Neuropsychopharmacology. 2013;38(6):1121–1129. doi: 10.1038/npp.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Mayer D, Rohlfing T, et al. Rat strain differences in brain structure and neurochemistry in response to binge alcohol. Psychopharmacology. 2014b;231(2):429–445. doi: 10.1007/s00213-013-3253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Mayer D, Vinco S, et al. In vivo evidence for alcohol-induced neurochemical changes in rat brain without protracted withdrawal, pronounced thiamine deficiency, or severe liver damage. Neuropsychopharmacology. 2009;34(6):1427–1442. doi: 10.1038/npp.2008.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr NM, Rohlfing T, Mayer D, et al. Transient CNS responses to repeated binge ethanol treatment. Addiction Biology. 2016;21(6):1199–1216. doi: 10.1111/adb.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelaya FO, Rose SE, Nixon PF, et al. MRI demonstration of impairment of the blood-CSF barrier by glucose administration to the thiamin-deficient rat brain. Magnetic Resonance Imaging. 1995;13(4):555–561. doi: 10.1016/0730-725x(95)00020-h. [DOI] [PubMed] [Google Scholar]
- Zhou P, Xia J, Guo G, et al. A Macaca mulatta model of fulminant hepatic failure. World Journal of Gastroenterology. 2012;18(5):435–444. doi: 10.3748/wjg.v18.i5.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zipursky RB, Lim KO, Pfefferbaum A. MRI study of brain changes with short-term abstinence from alcohol. Alcoholism: Clinical and Experimental Research. 1989;13(5):664–666. doi: 10.1111/j.1530-0277.1989.tb00401.x. [DOI] [PubMed] [Google Scholar]
- Zorlu N, Gelal F, Kuserli A, et al. Abnormal white matter integrity and decision-making deficits in alcohol dependence. Psychiatry Research. 2013;214(3):382–388. doi: 10.1016/j.pscychresns.2013.06.014. [DOI] [PubMed] [Google Scholar]
- Zorlu N, Karavul Ucman T, Gelal F, et al. Abnormal white matter integrity in long-term abstinent alcohol dependent patients. Psychiatry Research. 2014;224(1):42–48. doi: 10.1016/j.pscychresns.2014.07.006. [DOI] [PubMed] [Google Scholar]
- Zwingmann C. Nuclear magnetic resonance studies of energy metabolism and glutamine shunt in hepatic encephalopathy and hyperammonemia. Journal of Neuroscience Research. 2007;85(15):3429–3442. doi: 10.1002/jnr.21445. [DOI] [PubMed] [Google Scholar]
- Zwingmann C, Chatauret N, Rose C, et al. Selective alterations of brain osmolytes in acute liver failure: Protective effect of mild hypothermia. Brain Research. 2004;999(1):118–123. doi: 10.1016/j.brainres.2003.11.048. [DOI] [PubMed] [Google Scholar]