Abstract
Prostate cancer is one of the most prevalent cancers and the second leading cause of cancer-related deaths in men in the United States. A large number of patients undergo radiation therapy (RT) as a standard care of treatment; however, RT causes erectile dysfunction (radiation-induced erectile dysfunction; RiED) because of late side effects after RT that significantly affects quality of life of prostate cancer patients. Within 5 years of RT, approximately 50% of patients could develop RiED. Based on the past and current research findings and number of publications from our group, the precise mechanism of RiED is under exploration in detail. Recent investigations have shown prostate RT induces significant morphologic arterial damage with aberrant alterations in internal pudendal arterial tone. Prostatic RT also reduces motor function in the cavernous nerve which may attribute to axonal degeneration may contributing to RiED. Furthermore, the advances in radiogenomics such as radiation induced somatic mutation identification, copy number variation and genome-wide association studies has significantly facilitated identification of biomarkers that could be used to monitoring radiation-induced late toxicity and damage to the nerves; thus, genomic- and proteomic-based biomarkers could greatly improve treatment and minimize arterial tissue and nerve damage. Further, advanced technologies such as proton beam therapy that precisely target tumor and significantly reduce off-target damage to vital organs and healthy tissues. In this review, we summarize recent advances in RiED research and novel treatment modalities for RiED. We also discuss the possible molecular mechanism involved in the development of RiED in prostate cancer patients. Further, we discuss various readily available methods as well as novel strategies such as stem cell therapies, shockwave therapy, nerve grafting with tissue engineering, and nutritional supplementations might be used to mitigate or cure sexual dysfunction following radiation treatment.
Introduction
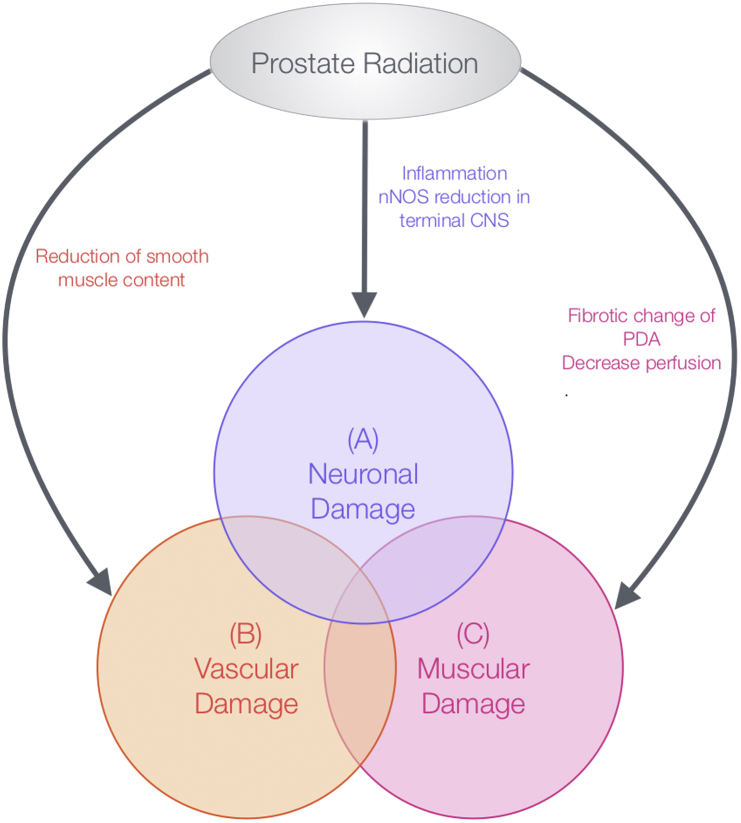
Prostate cancer is responsible for the second highest rate of cancer-related deaths in American men.1 Approximately one-half of prostate cancer patients undergo radiation therapy (RT) as a part of their primary treatment.2, 3 Over the past 15 years, clinical trials have demonstrated improved prostate cancer-related outcomes by increasing radiation doses to the prostate along with frequent addition of androgen deprivation therapy (ADT).4 Given the large variability in the number of patients experiencing erectile dysfunction (ED) (20%-90%), the major predictors of recovery are (1) age at the time of radiation: the younger the man is, the better erectile function at the time of treatment and the better the long-term function is going to be, (2) erectile function at or before the time of radiation, (3) type of RT causing less nerve damage of the prostate and the less amount of surrounding tissues exposed to radiation, the better the outcome, and (4) the health of erectile tissues. Although survival rates of prostate cancer patients are high, within 3-5 years of treatment completion, taking the previously discussed predictors into account, approximately one-half of these patients will develop ED depending on their age, baseline function, and comorbidities. Normal erections generally depend upon 3 processes: increased arterial blood flow into the penis by neurological initiation, cavernosal smooth muscle relaxation, and restriction of venous blood outflow from the penis.5 Impairment of any of these processes can lead to ED. The probable mechanisms of radiation-induced erectile dysfunction (RiED) are depicted in Fig 1.
Figure 1.
Probable mechanisms of radiation-induced erectile dysfunction. (A) Neuronal damage: there is inflammation and neuronal nitric oxid synthase (nNOS) reduction resulting from radiation therapy (RT) in cavernous nerve. Late RT-mediated effects on cavernous nerve can lead to erectile dysfunction after 3-5 years. (B) Vascular damage: fibrotic changes in blood vessels resulting from RT resulting in less blood flow in the erection chamber. (C) Smooth muscle atrophy: the corpus cavernosa undergoes atrophy similar to other muscles when they go unused.
ED affects the sexual health–related quality of life of cancer survivors; especially men younger than 70 years of age.6, 7, 8 One of the most important factors in predicting postintervention potency is the age of the patient's sexual partner as well. Possible loss of sexual function often plays an important role in treatment-related decisions made by patients after their initial prostate cancer diagnosis. Along with reducing radiation-induced toxicities, invention of new tools to mitigate and cure RiED through extensive research will reduce the financial burden on the health care systems for patients suffering from radiation-induced normal tissue injuries.
History of ED Treatment
The first documentation of ED dates back to 2000 BC when Hippocrates reported a number of cases among wealthy men of ancient Greece; early ED treatment involved therapies such as the injection of sheep testis extract.9 In the 1940s, testosterone was purified; however, the results of its use as a treatment for ED were disappointing.10, 11 Similarly, the use of androgens, when compared with placebo, did not increase the ability to obtain an erection. In 1960, the youth equivalence device, penis pump, was invented by Osbon and remains one of the most effective devices to treat ED. In 1995, the US Food and Drug Administration approved the prescription medication Caverject (alprostadil) for the treatment of ED. This drug is injected directly into the base of the penis 5 minutes before a sexual encounter, which increases blood flow and produces an erection. Prostaglandin, used as an intraurethral suppository, was introduced as a treatment for ED in 1997. Sildenafil (Viagra), the most common treatment for ED, was US Food and Drug Administration–approved in 1998, followed by vardenafil (Levitra) and tadalafil (Cialis) in 2003. There are new gels, pills, and injections in development, all of which aim to benefit patients experiencing ED. Notably, these drugs target relaxation of the corpus cavernosum and do not directly treat neurogenic ED.
Radiogenomics and RiED
Radiogenomics is the study of responses to RT and its relation to genomic variations.12 This approach has the ability to detect altered protein variants in the database and identify somatic and germline mutations as well as copy number variations (CNVs) in altered proteins.13 The genomic expression can predict intrinsic cellular radiosensitivity.14, 15 Genetic components, such as single nucleotide polymorphisms (SNPs) or CNVs, have recently been shown to cause variability in radiation sensitivity among individuals.16, 17 Integration of these two genetic components, along with dosimetric and clinical variables, significantly improved prediction of radiation-induced injuries such as rectal bleeding and ED. Coates et al demonstrated in a retrospective study that CNVs and SNPs may prove to be useful genetic variants in predicting associated radiation toxicities.18 Interestingly, the first radiogenomic genome-wide association study report was a small pilot study with a sample size of only 79 patients with ED following RT for prostate cancer.19 They identified a SNP associated with the FSHR gene that encodes the follicle stimulating hormone receptor, which is involved in gonad development and function.20 SNPs causing ED were found to be significantly associated with adverse reactions in patients treated with RT.21, 22 The predictive systems for cancer drug resistance, responses to RT or radiochemotherapy, and cellular toxicity to RT has shown great promise in advancement of radiogenomic cancer research.23
RT and RiED
Radiation is delivered through multiple methods and treatment recommendations are based on patient-related factors (comorbid conditions, urinary function, patient's preference), cancer-related factors (risk group, prostate size), and institutional preferences. All treatment modalities of RT carry a risk of ED. Radiation-based treatments lead to slowly declining erectile function over 1-3 years. Because of an overall survival at 5 and 10 years of around 90% and 65%, respectively, it is important to consider adverse effects and quality of life in addition to disease control.23
There are new techniques for RT that allow for the delivery of higher doses of radiation with better cancer control rates and fewer side effects. Intensity modulated RT (IMRT) minimizes the high-dose volume through precise targeting of the prostate. In addition, use of more advanced image guidance techniques including Calypso track the target in real time, whereas RT is delivered to increase precision and decrease expansions for setup uncertainty.24, 25, 26 In secondary analysis of erectile function for patients on a dose escalation trial testing 64 versus 74 Gy of 3-dimensional (3D) conformal RT along with 3-6 months of ADT, Mangar et al reported that in 51 patients, 12 remained potent, 22 had reduced potency, and 17 were impotent at 2 years. A total of 83.3% of impotent patients received a 50 Gy dose to the penile bulb (PB) compared with 29.4% of patients who maintained potency at 2 years. They suggested that 50 Gy dose is associated with a significant risk of ED and this should be considered while selecting dose constraints in future dose escalation studies.27 Van den Wielen et al found that the incidence of new-onset ED was 36% and 38% 2 and 3 years post-RT, respectively.28 Radiation Therapy Oncology Group (RTOG) 9406 trial data reported by Roach et al showed a greater risk of ED in patients who had a median PB exposure of >52.5 Gy.29 More recently, patient-reported outcomes from RTOG 0126, a trial powered to detect a survival benefit for dose escalation, demonstrated no difference in ED between IMRT and 3D conformal RT radiation, even though the PB dose was statistically lower in the IMRT cohort.30
Owing to their close proximity to the prostate, several nontarget structures such as the neurovascular bundles, Crura, and PB often receive significant radiation doses, and radiation injury to these structures has been postulated to be responsible for ED. Girelli et al reported treatment of 104 prostate cancer patients with IMRT using a hypofractionated schedule with an integrated boost.30 Men, who were potent at baseline, showed partial decrease in erectile function. Combining IMRT, hypofractionation, and a simultaneous integrated boost has been shown to be a safe and effective treatment option for prostate cancer patients. Prostate cancer patients treated with Cyberknife stereotactic body RT exhibited minimal acute toxicity.31 Prostate-specific antigen response, toxicity, preservation of erectile function, and improvement in urinary function compare favorably to data presented following radical prostatectomy, brachytherapy, or conventional external beam RT.32
Despite the high proportion of patients treated with brachytherapy, less is known about its lasting effects on erectile function. In available reports, rates of ED after permanent seed implantation have been as high as 50% within 6 years after treatment.33, 34, 35 Although long-term follow-up is valuable, interpretation of such findings can be further complicated by the effects of aging.36, 37 Keyes et al established multiple factors that had a negative long-term impact on erectile function, including ADT, age, and a history of hypertension. They also found that each successive 5-year cohort showed a decline in potency.38 High dose rate brachytherapy was developed as an alternative for patients who could not undergo combined low dose rate and external beam RT and has been used by a few groups with excellent results.39, 40, 41, 42, 43, 44, 45 A recent review of the high dose rate patient outcomes reports that erectile preservation was observed in 57%-89% of patients.46
Proton therapy (PT) is a cutting edge technique being used in the treatment of prostate cancer. It allows for less radiation exposure to the nontargeted normal tissues than photon-based external beam RT. Hoppe et al recently reported that potency rates remained high in younger patients 2 years after PT for prostate cancer and the risk of urinary incontinence was lowered when compared with effects of surgery; however, long-term effects are still unknown and will require further follow-up.47 The potential advantages of PT compared with IMRT are evolving. A proton beam transfers a minimal dose of radiation to the front of the tumor, a maximal dose to the tumor area itself and minimum off-target dose; hence, proton therapy is safer for healthy tissue surrounding the tumor. This may lead to a direct impact on the tumor leading to fewer harmful side effects and increased tumor control. Further research is awaited to elucidate the effects of PT on ED in prostate cancer patients.48, 49, 50, 51, 52
Current treatment options of RiED
Although treatment of prostate cancer confers increased risk of ED, there are many additional causes of ED, both medical and psychosocial, that can contribute to the sexual heath of an individual patient. Known factors include, but are not limited to, increasing age, diabetes mellitus, peripheral vascular disease, smoking, anxiety, and depression; therefore, treatment should be instituted using a multifaceted approach including an attempt to address comorbid conditions that could be exacerbating RiED. Table 1 demonstrates the current treatment options for ED patients and the benefits and limitations of each treatment.
Table 1.
Current treatment options for RiED
| Treatments | Benefits | Limitations |
|---|---|---|
| PDE5-Is |
|
|
| Vacuum devices |
|
|
| Penile injections |
|
|
| Penile prostheses |
|
|
| Penile suppositories |
|
|
| Natural supplements |
|
|
ED, erectile dysfunction; PDE5-Is, phosphodiesterase type 5 inhibitors; RiED, radiation-induced erectile dysfunction.
Normally, the release of nitric oxide (NO) in the corpus cavernosum upon sexual stimulation initiates penile erection. The activation of autonomic nerves results from sexual stimulation and causes relaxation of vascular and cavernosal smooth muscle via the release of NO. Simultaneous release of acetylcholine from parasympathetic nerve fibers inhibits the sympathetic release of noradrenaline leading to an increase in blood flow into the cavernosal space. Activation of endothelial NOS increases blood flow and synthesis of NO. Synthesis of cyclic guanosine monophosphate, stimulated by the presence of NO, causes the relaxation of smooth muscle.
Phosphodiesterase type 5 inhibitors (PDE5Is), such as sildenafil, have been shown to have high efficacy and safety rates.53 Ilic et al performed a randomized control trial of nightly sildenafil versus placebo for 6 months in 27 men treated with radiation for prostate cancer, which did not demonstrate a benefit in potency.54 Zelefsky et al reported on 279 patients randomized to 50 mg sildenafil daily or placebo during and after RT for 6 months and found overall sexual function was significantly improved with the use of sildenafil at 6 and 12 months using the International Index of Erectile Function. At 24 months, men treated with sildenafil maintained significantly higher sexual desire and ability to achieve a functional erection.55 Although a significant proportion of men with RiED do respond to PDE5Is, a number of patients do not respond well to such pharmacological intervention, suggesting a need for further investigation into the mechanism and development of novel therapeutics.
Animal models evaluating RiED and the molecular mechanisms
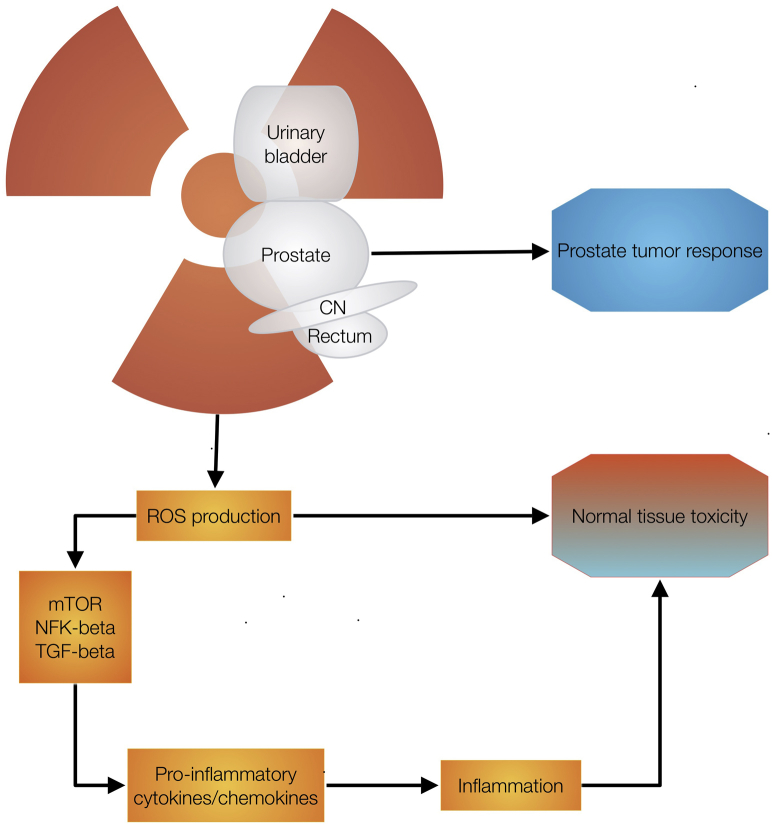
Because of challenges in developing an animal model that clearly demonstrates the human clinical RiED scenario, the etiology of RiED has not been entirely clear. Rat is the most common laboratory animal used for developing models of ED. It was demonstrated that RiED in rat models using irradiators, which are appropriate for human use, were not suitable for animal use to deliver accurate dose of radiation.56, 57, 58 Our recently published paper described the rat model of RiED after targeted radiation using a small animal image guided irradiation unit.59 Radiation-induced cell injury is primarily caused by DNA oxidation. Oxidative stress causes loss of smooth muscle, fibrosis of cavernous tissue, and dysfunction of the endothelium. Van der Wielen et al demonstrated alterations in corpora cavernosal arteries after fractionated prostate-targeted irradiation.60 Radiation damage to the arterial supply of the corpora cavernosa causes a chronic inflammatory response driven by oxidative stress that leads to ED.61 Further investigation is needed to explore the importance of oxidative stress within the cavernosa. Using penile Doppler ultrasonography, it has been postulated that the blood vessel damage occurs within the penile tissue.26, 62, 63 It is presumed that RiED is multifactorial (Fig 2). Furthermore, Nolan et al recently reported that prostatic irradiation in a canine model using stereotactic body RT causes morphologic arterial damage with altered internal pudendal arterial tone. There was decreased motor function in the pudendal nerve, which was attributed to axonal degeneration and loss.64 Overall, the mechanism of RiED is largely unknown and more intensive mechanistic studies are needed to develop novel and effective drugs.
Figure 2.
Probable molecular mechanisms of radiation-induced erectile dysfunction. Radiation therapy causes increase in reactive oxygen species, leading to inflammation leading to tissue toxicities. CN, cavernous nerve; mTOR, mechanistic target of rapamycin; NFK, nuclear factor kappa; ROS, reactive oxygen; TGF, transforming growth factor.
Future treatments for RiED
Stem cells in rat model of RiED
Stem cells (SCs) are naturally occurring cells that repopulate healthy tissue and aid in the repair of damaged tissue. Qiu et al reported significant decrease in erectile function postradiation and found that injection of adipose-derived stem cells can ameliorate RiED in a rat model.65 Fandel et al were the first to provide evidence that intracavernosal (IC) injected SCs rapidly disappeared from the injection site and migrated to major pelvic ganglia (MPG) in rats with cavernous nerve (CN) injury.66 Later, Qiu et al established RiED as a target for SC therapy and showed that IC injection of stem cells was able to treat both acute and chronic CN injury-induced ED.65, 67 Kovanecz et al showed that IC injection of SkMSC (xenogeneic mouse mesenchymal stem cells) alone or in combination with oral sildenafil was able to normalize erectile function in rats with CN injury.68 There has been a lot of progress in this field of research. SC transplantation has mostly been done by IC injection, but more recent studies try alternative routes, such as intravenous injection, periprostatic injection, and scaffolding.69 To gain more of an understanding of how SCs exert their therapeutic effects postradiation treatment, research efforts need to shift the preference for functional outcomes toward the elucidation of mechanisms.
Shockwave therapy for the treatment of RiED
Low-intensity extracorporeal shock wave therapy (LiESWT) is a new technology used for the treatment of ED. It is a noninvasive therapy that induces localized angiogenesis, increasing the ability to push blood to the penis and keep it there, through the use of low-intensity shockwaves to increase penile hemodynamics. The goal of LiESWT is to restore natural erectile function by inducing neovascularization, and therefore enhance penile perfusion, improving erectile function.70 Recent studies have shown response to treatment in PDE5-I nonresponders and further evidence suggests that LiESWT to the corpora cavernosa is involved in regaining erectile function.71, 72 Interestingly, there is no study yet reported on radiation-induced ED and use of LiESWT to date. This is a novel avenue for future research.
Nutritional supplementation in RiED
Many cultures worldwide accept the use of natural products and herbal remedies for the improvement of male sexual health73, 74; however, many of these so-called “natural” products that claim to improve sexual function have been found to contain undisclosed amounts of prescription pharmaceuticals. A study testing readily available products found PDE5-I or its analogs in 81% of the samples tested, 20% of which contained >110% the highest approved dosage. Another study that analyzed sexual enhancement products found that 70% of samples marketed as “natural” contained sildenafil.75
Among thousands of natural products, those containing red ginseng have been found to have some efficacy. Red ginseng stimulates NO synthase, increasing the production of NO and blood flow into the corpora cavernosa. Studies in rabbit models have shown dose-dependent relaxation of smooth muscle within the corpora cavernosa as well as an increase in intracavernosal pressure.76 It has been proposed that Ginkgo biloba induces production of NO in endothelial cells while simultaneously relaxing vascular smooth muscle cells. In vitro data have shown G. biloba–mediated corpus cavernosal smooth muscle cell relaxation in a rabbit model.77
L-arginine is frequently used as a men's health supplement. It is the immediate precursor of NO, elevating NO production when consumed. A study by Medeiros et al on RiED and nutritional supplements reported that l-arginine or l-glutamine supplementation can have protective effects against the structural changes of the rat penis resulting from radiation. Using l-arginine or l-glutamine as nutritional supplements prevents these changes, and supplementation with l-arginine showed slightly more favorable results, making these amino acids a potential preventive treatment for RiED.78
Nerve graft and tissue engineering
During radical prostatectomy, there have recently been surgical nerve graft procedures that have had favorable outcomes, resulting in a rediscovered interest for the applications of neural repair in a urologic setting. Currently, the gold standard of treatment is using an autologous donor graft in the nerve repair procedure, but donor availability and site morbidity are still a problem. Connolly et al used an “off-the-shelf” acellular nerve graft, hoping it would be a viable substitute in a rat model and demonstrated significant improvement in erectile function.79 Chen and colleagues used a rabbit model to try to bioengineer entire pendular penile bodies by seeding endothelial cells and smooth muscle onto 3D corporal collagen matrices. They were able to create a neo corpora that showed good intracorporeal pressures needed to achieve an erection and the ability to induce relaxation when exposed to NO. They also performed mating assessments that revealed an 83% intravaginal ejaculation rate.80, 81
RT can cause ED via radiation-induced nerve damage. In the penis, a decrease in the number of erection-inducing nerves has been shown in response to radiation exposure. Although the cause of ED after RT is not understood fully, penile endothelial dysfunction within cavernosal tissue and cavernous nerve hypoxia and fibrosis is the likely mechanism.
Conclusions
Overall, there have been very few published manuscripts on RiED, both original and review. There are several potential therapeutic candidates that demonstrate some promise in reducing ED without RT. However, there are still significant challenges to overcome before widespread human application. Important issues, such as reliable outcomes, safety risks regarding genomic or epigenetic changes in the longer term as well as potential immune reactions and infection risks need to be identified in more stringent clinical trials. Therefore, extensive research is required for developing novel strategies to mitigate RiED, which will lead to improved quality of life of prostate cancer patients.
Acknowledgment
We thank Dr. William F. Regine, the Department of Radiation Oncology, University of Maryland Medical Center.
Footnotes
Sources of support: This work was supported from the startup funds from the University of Maryland, School of Medicine to Dr. Zeljko Vujaskovic.
Conflicts of interest: None.
References
- 1.DeSantis C.E., Lin C.C., Mariotto A.B. Cancer treatment and survivorship statistics, 2014 CA. Cancer J Clin. 2014;64:252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 2.Bellavita R., Scricciolo M., Bini V. Radiotherapy for early-stage prostate cancer in men under 70 years of age. Tumori. 2015;102:209–216. doi: 10.5301/tj.5000433. [DOI] [PubMed] [Google Scholar]
- 3.Incrocci L., Jensen P.T. Pelvic radiotherapy and sexual function in men and women. J Sex Med. 2013;10(Suppl 1):53–64. doi: 10.1111/jsm.12010. [DOI] [PubMed] [Google Scholar]
- 4.Mendenhall W.M., Henderson R.H., Mendenhall N.P. Definitive radiotherapy for prostate cancer. Am J Clin Oncol. 2008;31:496–503. doi: 10.1097/COC.0b013e31816d1ca6. [DOI] [PubMed] [Google Scholar]
- 5.Wein A., Kavoussi L., Novick A., Partin A., Peters C. Saunders; USA: 2012. Physiology of Penile Erection and Pathophysiology of Erectile Dysfunction. 10th ed. Campbell-Walsh Urology. [Google Scholar]
- 6.Aytac I.A., McKinlay J.B., Krane R.J. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–56. doi: 10.1046/j.1464-410x.1999.00142.x. [DOI] [PubMed] [Google Scholar]
- 7.Zenger M., Hinz A., Stolzenburg J.U., Rabenalt R., Schwalenberg T., Schwarz R. Health-related quality of life of prostate cancer patients compared to the general German population: age-specific results. Urol Int. 2009;83:166–170. doi: 10.1159/000230018. [DOI] [PubMed] [Google Scholar]
- 8.Karakiewicz P.I., Scardino P.T., Kattan M.W. The impact of sexual and urinary dysfunction on health-related quality-of-life (HRQOL) following radical prostatectomy (RP) Prostate Cancer Prostatic Dis. 2000;3:S21. doi: 10.1038/sj.pcan.4500446. [DOI] [PubMed] [Google Scholar]
- 9.Valiquette L. A historical review of erectile dysfunction. Can J Urol. 2003;10(Suppl 1):7–11. [PubMed] [Google Scholar]
- 10.Sehmisch S., Boeckhoff J., Wille J. Vitex agnus castus as prophylaxis for osteopenia after orchidectomy in rats compared with estradiol and testosterone supplementation. Phytother Res. 2009;23:851–858. doi: 10.1002/ptr.2711. [DOI] [PubMed] [Google Scholar]
- 11.Tata J.R. Signalling through nuclear receptors. Nat Rev Mol Cell Biol. 2002;3:702–710. doi: 10.1038/nrm914. [DOI] [PubMed] [Google Scholar]
- 12.Angel T.E., Aryal U.K., Hengel S.M. Mass spectrometry-based proteomics: Existing capabilities and future directions. Chem Soc Rev. 2012;41:3912–3928. doi: 10.1039/c2cs15331a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shukla H.D., Mahmood J., Vujaskovic Z. Integrated proteo-genomic approach for early diagnosis and prognosis of cancer. Cancer Lett. 2015;369:28–36. doi: 10.1016/j.canlet.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Buffa M., Davidson S.E., Hunter R.D., Nahum A.E., West C.M. Incorporating biologic measurements (SF(2), CFE) into a tumor control probability model increases their prognostic significance: A study in cervical carcinoma treated with radiation therapy. Int J Radiat Oncol Biol Phys. 2001;50:1113–1122. doi: 10.1016/s0360-3016(01)01584-x. [DOI] [PubMed] [Google Scholar]
- 15.Williams J.R., Zhang Y., Zhou H. Overview radiosensitivity of human tumor cells to low dose rate irradiation. Int J Radiat Oncol Biol Phys. 2008;72:909–917. doi: 10.1016/j.ijrobp.2008.06.1928. [DOI] [PubMed] [Google Scholar]
- 16.Zhang F., Gu W., Hurles M.E. Copy number variation in human health, disease, and evolution. Annu Rev Genomics Hum Genet. 2009;10:451–481. doi: 10.1146/annurev.genom.9.081307.164217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langsenlehner T., Renner W., Gerger A. Association between single nucleotide polymorphisms in the gene for XRCC1 and radiation-induced late toxicity in prostate cancer patients. Radiother Oncol. 2011;98:387–393. doi: 10.1016/j.radonc.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 18.Coates J., Jeyaseelan A.K., Ybarra N. Contrasting analytical and data-driven frameworks for radiogenomic modeling of normal tissue toxicities in prostate cancer. Radiother Oncol. 2015;115:107–113. doi: 10.1016/j.radonc.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Themmen A.P.N., Huhtaniemi I.T. Mutations of gonadotropins and gonadotropin receptors: Elucidating the physiology and pathophysiology of pituitary-gonadal function. Endocr Rev. 2000;21:551–583. doi: 10.1210/edrv.21.5.0409. [DOI] [PubMed] [Google Scholar]
- 20.Kerns S.L., Stone N.N., Stock R.G., Rath L., Ostrer H., Rosenstein B.S. A 2-stage genome-wide association study to identify single nucleotide polymorphisms associated with development of urinary symptoms after radiotherapy for prostate cancer. J Urol. 2013;190:102–108. doi: 10.1016/j.juro.2013.01.096. [DOI] [PubMed] [Google Scholar]
- 21.Akita S. Treatment of radiation injury. Adv Wound Care (New Rochelle) 2014;3:1–11. doi: 10.1089/wound.2012.0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J.C., Shen W.C., Shih T.C. The current progress and future prospects of personalized radiogenomic cancer study. Biomedicine (Taipei) 2015;5:2. doi: 10.7603/s40681-015-0002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michalski J.M., Moughan J., Purdy J.A. Initial results of a phase 3 randomized study of high dose 3DCRT/IMRT versus standard dose 3D-CRT/IMRT in patients treated for localized prostate cancer (RTOG 0126) Int J Radiat Oncol Biol Phys. 2014;90:1263. [Google Scholar]
- 24.Cozzarini C., Fiorino C., Di Muzio N. Significant reduction of acute toxicity following pelvic irradiation with helical tomotherapy in patients with localized prostate cancer. Radiother Oncol. 2007;84:164–170. doi: 10.1016/j.radonc.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 25.Cozzarini C., Fiorino C., Di Muzio N. Hypofractionated adjuvant radiotherapy with helical tomotherapy after radical prostatectomy: Planning data and toxicity results of a phase I-II study. Radiother Oncol. 2008;88:26–33. doi: 10.1016/j.radonc.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 26.Budäus L., Bolla M., Bossi A. Functional outcomes and complications following radiation therapy for prostate cancer: a critical analysis of the literature. Eur Urol. 2012;61:112–127. doi: 10.1016/j.eururo.2011.09.027. [DOI] [PubMed] [Google Scholar]
- 27.Mangar S.A., Sydes M.R., Tucker H.L. Evaluating the relationship between erectile dysfunction and dose received by the penile bulb: Using data from a randomised controlled trial of conformal radiotherapy in prostate cancer (MRC RT01, ISRCTN47772397) Radiother Oncol. 2006;80:355–362. doi: 10.1016/j.radonc.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 28.van der Wielen G.H., van Putten W.L., Incrocci L. Sexual function after three-dimensional conformal radiotherapy for prostate cancer: Results from a dose-escalation trial. Int J Radiat Oncol Biol Phys. 2007;68:479–484. doi: 10.1016/j.ijrobp.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 29.Roach M., Winter K., Michalski J.M. Penile bulb dose and impotence after 3-dimensional conformal radiotherapy for prostate cancer on RTOG 9406: Findings from a prospective, multi-institutional, phase I/II dose-escalation study. Int J Radiat Oncol Biol Phys. 2004;60:1351–1356. doi: 10.1016/j.ijrobp.2004.05.026. [DOI] [PubMed] [Google Scholar]
- 30.Bruner D.W., Hunt D., Michalski J.M. Preliminary patient-reported outcomes analysis of 3-dimensional radiation therapy versus intensity-modulated radiation therapy on the high-dose arm of the Radiation Therapy Oncology Group (RTOG) 0126 prostate cancer trial. Cancer. 2015;121:2422–2430. doi: 10.1002/cncr.29362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rana Z., Hong R.L., Abugideiri M. Sexual, irritative, and voiding outcomes, following stereotactic body radiation therapy for prostate cancer. Radiat Oncol. 2015;10:182. doi: 10.1186/s13014-015-0488-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Girelli G., Franco P., Sciacero P. Image-guided Intensity-modulated radiotherapy for prostate cancer employing hypofractionation and simultaneous integrated boost: Results of a consecutive case series with focus on erectile function. Anticancer Res. 2015;35:4177–4182. [PubMed] [Google Scholar]
- 33.Potters L., Morgenstern C., Calugaru E. 12-year outcomes following permanent prostate brachytherapy in patients with clinically localized prostate cancer. J Urol. 2008;179(5 Suppl):S20–S24. doi: 10.1016/j.juro.2008.03.133. [DOI] [PubMed] [Google Scholar]
- 34.Stock R., Cesaretti J., Stone N. Disease-specific survival following the brachytherapy management of prostate cancer. Int J Radiat Oncol Biol Phys. 2006;64:810–816. doi: 10.1016/j.ijrobp.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 35.Cesaretti J.A., Kao J., Stone N.N. Effect of low dose-rate prostate brachytherapy on the sexual health of men with optimal sexual function before treatment: Analysis at ≥7 years of follow-up. BJU Int. 2007;100:362–367. doi: 10.1111/j.1464-410X.2007.07016.x. [DOI] [PubMed] [Google Scholar]
- 36.Merrick G., Butler W., Wallner K. Erectile function after prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2005;62:437–447. doi: 10.1016/j.ijrobp.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 37.Macdonald A., Keyes M., Kruk A. Predictive factors for erectile dysfunction in men with prostate cancer after brachytherapy: Is dose to the penile bulb important? Int J Radiat Oncol Biol Phys. 2005;63:155–163. doi: 10.1016/j.ijrobp.2004.12.056. [DOI] [PubMed] [Google Scholar]
- 38.Keyes M., Pickles T., Crook J. Effect of aging and long-term erectile function after iodine-125 prostate brachytherapy. Brachytherapy. 2015;14:334–341. doi: 10.1016/j.brachy.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Hauswald H., Kamrava M.R., Fallon J.M. High-dose-rate monotherapy for localized prostate cancer: 10-year results. Int J Radiat Oncol Biol Phys. 2016;94:667–674. doi: 10.1016/j.ijrobp.2015.07.2290. [DOI] [PubMed] [Google Scholar]
- 40.Mark R, Anderson P, Akins R, et al. Interstitial high dose rate brachytherapy as monotherapy for early stage prostate cancer: Median 8-year results in 301. Mark R, Anderson P, Akins R. patients. [abstract]. Brachytherapy. 2010;9:76.
- 41.Zamboglou N., Tselis N., Baltas D. High-dose-rate interstitial brachytherapy as monotherapy for clinically localized prostate cancer: treatment evolution and mature results. Int J Radiat Oncol Biol Phys. 2013;85:672–678. doi: 10.1016/j.ijrobp.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 42.Yoshioka Y., Konishi K., Sumida I. Monotherapeutic high-dose-rate brachytherapy for prostate cancer: Five-year results of an extreme hypofractionation regimen with 54 Gy in nine fractions. Int J Radiat Oncol Biol Phys. 2011;80:469–475. doi: 10.1016/j.ijrobp.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 43.Rogers C.L., Alder S.C., Rogers R.L. High dose brachytherapy as monotherapy for intermediate risk prostate cancer. J Urol. 2012;187:109–116. doi: 10.1016/j.juro.2011.09.050. [DOI] [PubMed] [Google Scholar]
- 44.Barkati M., Williams S.G., Foroudi F. High-dose-rate brachytherapy as a monotherapy for favorable-risk prostate cancer: A phase II trial. Int J Radiat Oncol Biol Phys. 2012;82:1889–1896. doi: 10.1016/j.ijrobp.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Potharaju M., Subramanaiam R., Venkataraman M. A report on the clinical outcome after high-dose rate (HDR) brachytherapy as monotherapy in early prostate cancer. Cureus. 2015;7:e303. doi: 10.7759/cureus.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jeffrey Demanes D., Ghilezan M.I. High-dose-rate brachytherapy as monotherapy for prostate cancer. Brachytherapy. 2014;13:529e541. doi: 10.1016/j.brachy.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 47.Hoppe B.S., Nichols R.C., Henderson R.H. Erectile function, incontinence, and other quality of life outcomes following proton therapy for prostate cancer in men 60 years old and younger. Cancer. 2012;118:4619–4626. doi: 10.1002/cncr.27398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goozner M. The proton beam debate: are facilities outstripping the evidence? J Natl Cancer Inst. 2010;102:450–453. doi: 10.1093/jnci/djq112. [DOI] [PubMed] [Google Scholar]
- 49.StatBite StatBite: Particle beam therapy facilities worldwide. J Natl Cancer Inst. 2010;102:450–453. doi: 10.1093/jnci/djq108. [DOI] [PubMed] [Google Scholar]
- 50.Zietman A.L. The Titanic and the iceberg: Prostate proton therapy and health care economics. J Clin Oncol. 2007;25:3565–3566. doi: 10.1200/JCO.2007.11.9768. [DOI] [PubMed] [Google Scholar]
- 51.Trofimov A., Nguyen P.L., Coen J.J. Radiotherapy treatment of early-stage prostate cancer with IMRT and protons: A treatment planning comparison. Int J Radiat Oncol Biol Phys. 2007;69:444–453. doi: 10.1016/j.ijrobp.2007.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tepper J.E. Protons and parachutes. J Clin Oncol. 2008;26:2436–2437. doi: 10.1200/JCO.2008.17.1165. [DOI] [PubMed] [Google Scholar]
- 53.Cellek S., Cameron N.E., Cotter M.A., Fry C.H., Ilo D. Microvascular dysfunction and efficacy of PDE5 inhibitors in BPH-LUTS. Nat Rev Urol. 2014;11:231–241. doi: 10.1038/nrurol.2014.53. [DOI] [PubMed] [Google Scholar]
- 54.Ilic D., Hindson B., Duchesne G., Millar J.L. A randomised, double-blind, placebo-controlled trial of nightly sildenafil citrate to preserve erectile function after radiation treatment for prostate cancer. J Med Imaging Radiat Oncol. 2013;57:81–88. doi: 10.1111/j.1754-9485.2012.02461.x. [DOI] [PubMed] [Google Scholar]
- 55.Zelefsky M.J., Shasha D., Branco R.D. Prophylactic sildenafil citrate improves select aspects of sexual function in men treated with radiotherapy for prostate cancer. J Urol. 2014;192:868–874. doi: 10.1016/j.juro.2014.02.097. [DOI] [PubMed] [Google Scholar]
- 56.Kimura M., Rabbani Z.N., Zodda A.R. Role of oxidative stress in a rat model of radiation-induced erectile dysfunction. J Sex Med. 2012;9:1535–1549. doi: 10.1111/j.1743-6109.2012.02716.x. [DOI] [PubMed] [Google Scholar]
- 57.Kimura M., Yan H., Rabbani Z. Radiation-induced erectile dysfunction using prostate-confined modern radiotherapy in a rat model. J Sex Med. 2011;8(8):2215–2226. doi: 10.1111/j.1743-6109.2011.02351.x. [DOI] [PubMed] [Google Scholar]
- 58.Koontz B.F., Yan H., Kimura M., Vujaskovic Z., Donatucci C., Yin F.F. Feasibility study of an intensity-modulated radiation model for the study of erectile dysfunction. J Sex Med. 2011;8:411–418. doi: 10.1111/j.1743-6109.2010.02125.x. [DOI] [PubMed] [Google Scholar]
- 59.Kimura M., Zodda A.R., Mahmood J. Pilot study evaluating a rat model of radiation-induced erectile dysfunction using an image-guided microirradiator. Urology. 2015;85:1214.e1–1214.e6. doi: 10.1016/j.urology.2014.12.020. [DOI] [PubMed] [Google Scholar]
- 60.Van der Wielen G.J., Mulhall J.P., Incrocci L. Erectile dysfunction after radiotherapy for prostate cancer and radiation dose to the penile structures: A critical review. Radiother Oncol. 2007;84:107–113. doi: 10.1016/j.radonc.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 61.Oberley-Deegan R.E., Steffan J.J., Rove K.O. The antioxidant, MnTE-2-PyP, prevents side-effects incurred by prostate cancer irradiation. PLoS One. 2012;7:e44178. doi: 10.1371/journal.pone.0044178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goldstein I., Feldman M.I., Deckers P.J., Babayan R.K., Krane R.J. Radiation-associated impotence. A clinical study of its mechanism. JAMA. 1984;251:903–910. doi: 10.1001/jama.251.7.903. [DOI] [PubMed] [Google Scholar]
- 63.Mittal B. A study of penile circulation before and after radiation in patients with prostate cancer and its effect on impotence. Int J Radiat Oncol Biol Phys. 1985;11:1121–1125. doi: 10.1016/0360-3016(85)90059-8. [DOI] [PubMed] [Google Scholar]
- 64.Nolan M.W., Marolf A.J., Ehrhart E.J. Pudendal nerve and internal pudendal artery damage may contribute to radiation-induced erectile dysfunction. Int J Radiat Oncol Biol Phys. 2015;91:796–806. doi: 10.1016/j.ijrobp.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 65.Qiu X., Villalta J., Ferretti L. Effects of intravenous injection of adipose-derived stem cells in a rat model of radiation therapy-induced erectile dysfunction. J Sex Med. 2012;9:1834–1841. doi: 10.1111/j.1743-6109.2012.02753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fandel T.M., Albersen M., Lin G. Recruitment of intracavernously injected adipose-derived stem cells to the major pelvic ganglion improves erectile function in a rat model of cavernous nerve injury. Eur Urol. 2012;61:201–210. doi: 10.1016/j.eururo.2011.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Qiu X., Fandel T.M., Ferretti L. Both immediate and delayed intracavernous injection of autologous adipose-derived stromal vascular fraction enhances recovery of erectile function in a rat model of cavernous nerve injury. Eur Urol. 2012;62:720–727. doi: 10.1016/j.eururo.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kovanecz I., Rivera S., Nolazco G. Separate or combined treatments with daily sildenafil, molsidomine, or muscle derived stem cells prevent erectile dysfunction in a rat model of cavernosal nerve damage. J Sex Med. 2012;9:2814–2826. doi: 10.1111/j.1743-6109.2012.02913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lin C.S., Xin Z., Dai J., Huang Y.C., Lue T.F. Stem-cell therapy for erectile dysfunction. Expert Opin Biol Ther. 2013;13:1585–1597. doi: 10.1517/14712598.2013.847085. [DOI] [PubMed] [Google Scholar]
- 70.Chung E., Cartmill R. Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: An Australian first open-label single-arm prospective clinical trial. BJU Int. 2015;115(Suppl 5):46–49. doi: 10.1111/bju.13035. [DOI] [PubMed] [Google Scholar]
- 71.Gruenwald I., Appel B., Kitrey N.D., Vardi Y. Shockwave treatment of erectile dysfunction. Ther Adv Urol. 2013;5:95–99. doi: 10.1177/1756287212470696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yee C.H., Chan E.S., Hou S.S., Ng C.F. Extracorporeal shockwave therapy in the treatment of erectile dysfunction: A prospective, randomized, double-blinded, placebo controlled study. Int J Urol. 2014;21:1041–1045. doi: 10.1111/iju.12506. [DOI] [PubMed] [Google Scholar]
- 73.Regan K.S., Wambogo E.A., Haggans C.J. NIH and USDA funding of dietary supplement research, 1999-2007. J Nutr. 2011;141:1–3. doi: 10.3945/jn.110.134106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cui T., Kovell R.C., Brooks D.C., Terlecki R.P. A urologist's guide to ingredients found in top-selling nutraceuticals for men's sexual health. J Sex Med. 2015;12:2105–2117. doi: 10.1111/jsm.13013. [DOI] [PubMed] [Google Scholar]
- 75.Low M.Y., Zeng Y., Li L. Safety and quality assessment of 175 illegal sexual enhancement products seized in red-light districts in Singapore. Drug Saf. 2009;32:1141–1146. doi: 10.2165/11316690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 76.Cho K.S., Park C.W., Kim C.K. Effects of Korean ginseng berry extract (GB0710) on penile erection: Evidence from in vitro and in vivo studies. Asian J Androl. 2013;15:503–507. doi: 10.1038/aja.2013.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paick J.S., Lee J.H. An experimental study of the effect of ginkgobiloba extract on the human and rabbit corpus cavernosumtissue. J Urol. 1996;156:1876–1880. [PubMed] [Google Scholar]
- 78.Medeiros J.L., Jr., Costa W.S., Felix-Patricio B., Sampaio F.J., Cardoso L.E. Protective effects of nutritional supplementation with arginine and glutamine on the penis of rats submitted to pelvic radiation. Andrology. 2014;2:943–950. doi: 10.1111/andr.134. [DOI] [PubMed] [Google Scholar]
- 79.Connolly S.S., Yoo J.J., Abouheba M., Soker S., McDougal W.S., Atala A. Cavernous nerve regeneration using acellular nerve grafts. World J Urol. 2008;26:333–339. doi: 10.1007/s00345-008-0283-y. [DOI] [PubMed] [Google Scholar]
- 80.Chen K., Eberli D., Yoo J., Atala A. Bioengineered corporal tissue for structural and functional restoration of the penis. Proc Natl Acad Sci U S A. 2010;107:3346–3350. doi: 10.1073/pnas.0909367106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stein M.J., Lin H., Wang R. New advances in erectile technology. Ther Adv Urol. 2014;6:15–24. doi: 10.1177/1756287213505670. [DOI] [PMC free article] [PubMed] [Google Scholar]