Abstract
Background
Public access defibrillation programs can improve survival after out-of-hospital cardiac arrest (OHCA), but automated external defibrillators (AEDs) are rarely available for bystander use at the scene. Drones are an emerging technology that can deliver an AED to the scene of an OHCA for bystander use. We hypothesize that a drone network designed with the aid of a mathematical model combining both optimization and queuing can reduce the time to AED arrival.
Methods
We applied our model to 53,702 OHCAs that occurred in the eight regions of the Toronto Regional RescuNET between January 1st 2006 and December 31st 2014. Our primary analysis quantified the drone network size required to deliver an AED one, two, or three minutes faster than historical median 911 response times for each region independently. A secondary analysis quantified the reduction in drone resources required if RescuNET was treated as one large coordinated region.
Results
The region-specific analysis determined that 81 bases and 100 drones would be required to deliver an AED ahead of median 911 response times by three minutes. In the most urban region, the 90th percentile of the AED arrival time was reduced by 6 minutes and 43 seconds relative to historical 911 response times in the region. In the most rural region, the 90th percentile was reduced by 10 minutes and 34 seconds. A single coordinated drone network across all regions required 39.5% fewer bases and 30.0% fewer drones to achieve similar AED delivery times.
Conclusion
An optimized drone network designed with the aid of a novel mathematical model can substantially reduce the AED delivery time to an OHCA event.
Keywords: Resuscitation, cardiac arrest, drone, automated external defibrillators, optimization
Introduction
Public access defibrillation programs have demonstrated that significant improvements in survival from out-of-hospital cardiac arrest (OHCA) are possible, with the majority of the survival advantage accruing to patients who arrest in public settings.1-3 However, the majority of OHCAs occur in private settings4, 5 with correspondingly slower emergency response times,5-7 especially in rural settings. While deployment of automated external defibrillators (AEDs) may be cost-effective in certain public venues,8, 9 especially if locations are optimized,10 static AEDs deployed broadly for use in private OHCA emergencies are unlikely to be cost-effective.7, 11, 12 There is a fundamental coverage limit of cardiac arrest risk that cannot be overcome using static AEDs alone.13 Moreover, in part due to access and availability issues,14 static AEDs have low utilization historically.15 Improving AED access and reducing the time to defibrillation are important for improving survival from OHCA. Thus, a new approach is necessary to make a significant impact in OHCA survival, especially for rural and private locations.
Recently, several companies and researchers have developed prototype drone technology that can be used to deliver AEDs to the scene of a cardiac arrest.16, 17 Google has successfully obtained a patent for drone delivery of medical supplies including AEDs.18 AED delivery is only one of the many proposed applications for drones, formally known as unmanned aerial vehicles. Companies have proposed to use drones to deliver everything from pizza19 to official documents20 to medicine.21, 22 Although there are technical challenges to overcome, drone-delivered AEDs are a potential transformative innovation in the provision of emergency care to cardiac arrest patients, especially to those who arrest in a private or rural setting.
The goal of this study is to determine if a drone network designed with the aid of a mathematical model combining both optimization and queuing can reduce the time to AED arrival. Our mathematical model determines, for a given geographical area, the number and location of drone bases, along with the number of the drones required at each base, to meet any specified AED arrival time goal. We applied our model to a large area composed of rural and urban regions surrounding Toronto, Canada and quantified the size of the drone network required to achieve AED arrival times that improve upon historical 911 response times. We determine the reduction in time to AED arrival, relative to 911 first responders, by using drone networks determined by our model to deliver an AED for bystander use.
Methods
Study setting
The Toronto Regional RescuNET comprises eight regions in Southern Ontario, Canada: Toronto, Durham, Simcoe, Muskoka, Peel, Hamilton, Halton, and York, with a total population of 7.12 million in a total area of 26,364 km2. Each region is served by a single paramedic service, though neighboring services may respond to emergencies if they are closer. There is a tiered response to emergency calls, where fire fighter first responders are dispatched to all suspected OHCAs along with paramedics.
Data Sources
Cardiac arrest episodes
All non-traumatic, private and public, treated and untreated OHCA episodes throughout RescuNET from January 1st 2006 to December 31st 2014 were included in the study. Data was obtained from the Rescu Epistry cardiac arrest database,23, 24 which has research ethics board approval from all destination hospitals and from the institution providing oversight to the paramedic and fire services. Universal Transverse Mercator (UTM) coordinates were determined for each episode after applying various geocoding techniques (Supplemental Figure 1). Cardiac arrests that could not be accurately geocoded due to lack of sufficient location information were excluded.
Candidate base locations
All fire, paramedic, and police stations within RescuNET were considered as candidate drone base locations. Addresses for each station were obtained from the regional provider and converted to UTM coordinates.
Drone specifications
Drone parameters used in our model were based on specifications reflecting current technological capabilities. Vertical acceleration/deceleration was set to 9.81 m/s2 while horizontal acceleration/deceleration was set to 19.6m/s2.25, 26 Horizontal acceleration/deceleration is done simultaneously with vertical deceleration (Supplemental Figure 2). Maximum forward velocity was set at 27.8 m/s.16 Flying height was assumed to be 60 m, which is below the maximum height allowed in Canada.27, 28 Accounting for maximum speed and height, 10 seconds is required for takeoff and landing. The maximum distance a drone can reach – it's “radius” – is determined using the average regional dispatch time and the maximum flying time used in the optimization model (see Supplemental Methods).
Model
For each region, the OHCA data was split into two disjoint sets of equal size: a training set and a testing set. The training set was used as the input into our models while the testing set was used to evaluate the performance of the theoretical drone networks.
Our modeling approach consisted of two stages. The first stage used an integer optimization model (Supplemental Methods) to determine the minimum number and location of drone bases, chosen from the set of candidate base locations, required to improve the historical median response time by one, two, or three minutes. The coverage radius for each potential base was determined using the average regional dispatch time and the maximum flying time used in the optimization model (see Supplemental Methods). Each base defined a catchment area through its coverage radius and we treated each catchment area independently in the second stage.
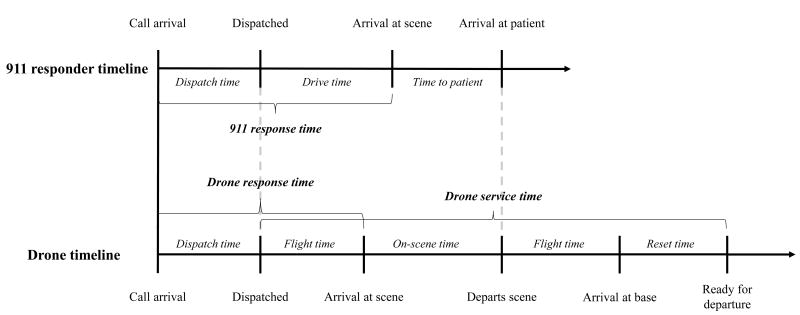
Once the base locations were determined by the optimization model, the second stage used a queuing model (Supplemental Methods) to determine the number of drones to be stationed at each base so there is a 99% chance a drone is free when an OHCA occurs inside that base's catchment area. The calculation is specific to each base, requiring two inputs: an average rate of OHCA occurrences in each catchment area and an average time interval between successive mission departures for the same drone (“drone busy time”). We calculated a separate rate of OHCA occurrences for daytime (8:00AM–7:59PM) and night time (8:00PM–7:59AM),29 and we used the daytime rate in the queuing model. The time interval required between successive departures by the same drone – drone busy time – comprises the outbound travel time, on-scene time, inbound travel time, and “reset” time. Supplemental Table 1 displays each of these computed time intervals. Figure 1 summarizes the relevant time intervals in the operationalization of the drone response.
Figure 1.
911 first responder and drone timelines. The on-scene time will be zero if 911 responders arrive prior to the drone. The drone may or may not arrive at the patient during the on-scene time interval, and this time point is not shown because it is not used in any calculations.
Analyses
Primary analysis: Delivery of drone AEDs prior to 911 responder arrival
We determined the historical median and 90th percentile 911 response times (i.e., dispatch plus drive time) from the training OHCA data for each region. For each region independently, we use our two-stage (optimization and queuing) approach to find the region-specific drone network that improves the median regional 911 response time by at least one minute; we repeated this process for two and three minutes. For each combination of drone response time improvement goal (one, two and three minutes faster than the median 911 response time) and region, we quantified the number of bases and drones required. Using the out-of-sample testing set OHCAs, we determined the response time distribution of the optimized drone network. We also determined the response time distribution of the combined drone and 911 network, by taking the minimum of the drone response time and historical 911 response time for each cardiac arrest. Finally, we calculated the proportion of testing set OHCAs in which the drone response time was shorter than the 911 response time.
Secondary analysis: The value of centrally coordinated drone response across regions
We repeated the primary analysis treating RescuNET as one large, integrated region. We computed the same metrics as in the primary analysis. To quantify the value of coordination, we computed the difference in the number of bases and total drones required by the “region-specific” versus the “integrated” network.
Statistical analysis
We use a right tailed Sign Test to determine if the observed median response time reductions were statistically significant at the 0.05 significance level. To do this, we tested the null hypothesis that the difference between the historical 911 response time distribution and the estimated response time distribution of a combined 911 and drone network had a zero median.
Sensitivity analysis
Variability in the drone busy time will influence the number of drone resources suggested by the mathematical model. To determine the impact of possible changes in drone busy time, we conducted a sensitivity analysis by varying the overall busy time by ±15 and ±30 minutes.
Results
After geocoding and eliminating OHCAs with missing data, 53,702 OHCAs remained (96% of OHCAs occurring during the study time frame) for our analysis. The training and testing sets both contained 26,851 OHCAs. Supplemental Table 2 provides information on historical 911 response times and annual OHCA incidence.
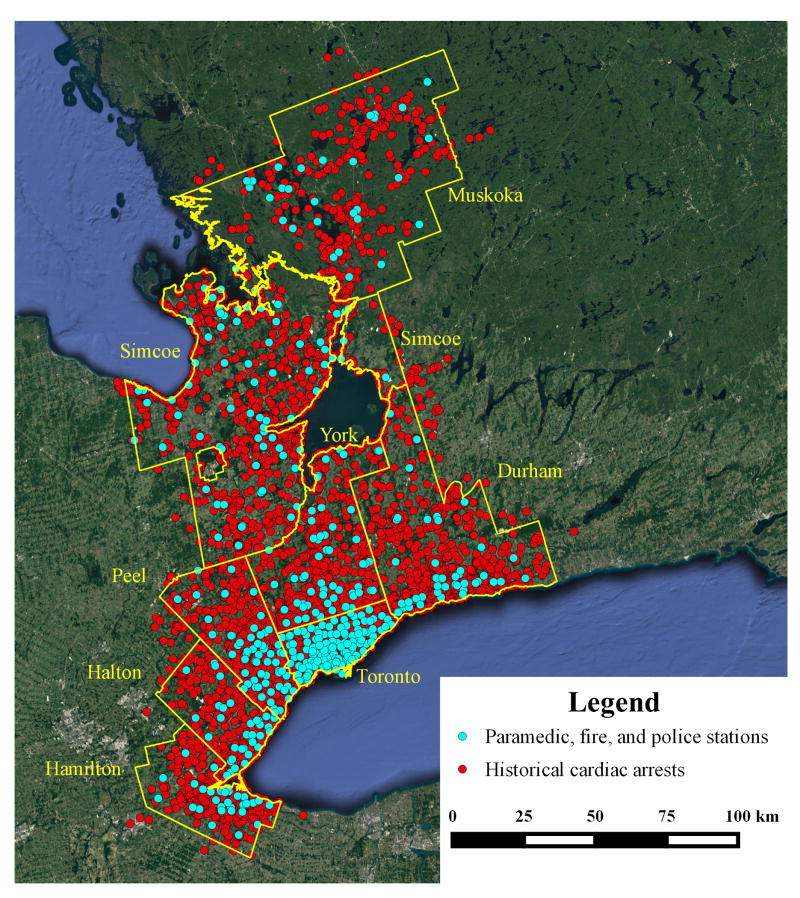
Table 1 provides a summary of the eight RescuNET regions. Figure 2 displays all geocoded cardiac arrests and the paramedic, fire, and police stations. A summary of the geocoding results is given in the Supplemental Material.
Table 1.
Summary statistics for the eight regions comprising RescuNET.
| Characteristics | Region | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Toronto | Durham | Simcoe | Muskoka | Peel | Hamilton* | Halton* | York* | All | ||
| Population (2011) | 2,615,060 | 608,124 | 446,063 | 100,209 | 1,296,814 | 519,949 | 501,669 | 1,032,524 | 7,120,412 | |
|
| ||||||||||
| Population density (per square km, 2011) | 4149.5 | 241.0 | 91.8 | 7.6 | 1040.0 | 465.4 | 520.4 | 585.9 | 270.1 | |
|
| ||||||||||
| Average annual number of cardiac arrests | 2977 | 570 | 440 | 73 | 848 | 618 | 355 | 666 | 746 | |
|
| ||||||||||
| Female sex (%) | 38.3 | 36.2 | 34.4 | 29.3 | 37.7 | 36.1 | 36.6 | 38.9 | 37.4 | |
|
| ||||||||||
| Average age (yr.) | 68.4 | 65.1 | 64.9 | 66.5 | 65.6 | 66.0 | 67.2 | 68.9 | 67.2 | |
|
| ||||||||||
| Dispatch time (mm:ss) | Median | 1:34 | 0:39 | 1:00 | 0:20 | 0:45 | 1:00 | 0:51 | 0:32 | 1:00 |
| 90th percentile | 2:57 | 1:09 | 1:48 | 1:00 | 1:30 | 2:00 | 1:41 | 1:44 | 2:29 | |
|
| ||||||||||
| Response time (mm:ss) | Median | 6:12 | 5:33 | 7:00 | 8:00 | 5:41 | 6:00 | 6:00 | 6:44 | 6:00 |
| 90th percentile | 10:39 | 9:07 | 14:00 | 19:35 | 8:22 | 11:00 | 10:00 | 10:38 | 10:35 | |
|
| ||||||||||
| Access time† (mm:ss) | Median | 3:18 | 3:02 | 2:45 | 2:51 | 2:47 | 3:00 | 3:02 | 2:33 | 3:02 |
| 90th percentile | 7:24 | 6:28 | 6:00 | 7:33 | 6:28 | 6:36 | 6:20 | 5:34 | 6:55 | |
|
| ||||||||||
| Public location (%) | 9.6 | 8.2 | 10.8 | 16.1 | 11.7 | 7.5 | 11.1 | 8.9 | 9.8 | |
|
| ||||||||||
| Treated (%) | 54.5 | 56.9 | 59.2 | 54.0 | 64.1 | 57.9 | 57.0 | 66.5 | 57.5 | |
|
| ||||||||||
| Initial shockable cardiac rhythm* (%) | 19.3 | 25.2 | 24.4 | 27.8 | 22.7 | 19.3 | 24.2 | 20.8 | 21.2 | |
|
| ||||||||||
| Survival to hospital discharge* (%) | 6.9 | 10.2 | 7.7 | 8.5 | 8.5 | 6.0 | 11.0 | 8.9 | 7.8 | |
|
| ||||||||||
| Number of paramedic, fire, and police stations | 158 | 44 | 76 | 32 | 68 | 51 | 41 | 68 | 538 | |
Access time is defined as the time interval from arrival of the 911 responder (i.e., wheels stop) to patient contact.
Hamilton, Halton, and York reported data for only 8, 7, and 5 years, respectively. Initial shockable cardiac rhythm and survival to discharge include treated OHCAs only. The number of missing data points for each characteristic and region can be found in Supplemental Table 3.
Figure 2.
Historical OHCAs and paramedic, fire, and police station locations.
Table 2 shows the number of bases and drones in each region for both the region-specific and integrated drone networks for each response time improvement goal, along with corresponding response time metrics. For example, to deliver an AED via drone one minute prior to 911 arrival on average, the region-specific network required 23 bases and 37 drones, whereas the integrated network required 15 bases and 28 drones. For the two- and three-minute goals, a reduction in drone bases (15.0% and 39.5% reduction, respectively) and number of drones (10.5% and 30.0%, respectively) was also observed in the integrated network.
Table 2.
Region-specific and integrated drone network characteristics for the three response time improvement goals evaluated using the testing set OHCAs.
| Drone response time improvement goal | Region | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Toronto | Durham | Simcoe | Muskoka | Peel | Hamilton | Halton | York | All | |||
| Region-specific | Number of bases (number of total drones) | 1 min. | 3 (6) | 3 (6) | 5 (6) | 3 (3) | 2 (4) | 1 (2) | 3 (4) | 3 (6) | 23 (37) |
| 2 min. | 6 (12) | 5 (7) | 11 (12) | 5 (5) | 4 (8) | 1 (2) | 3 (4) | 5 (7) | 40 (57) | ||
| 3 min. | 13 (26) | 14 (16) | 20 (20) | 6 (6) | 10 (11) | 5 (7) | 5 (5) | 8 (9) | 81 (100) | ||
|
| |||||||||||
| Improvement in median time to AED on scene (mm:ss) | 1 min. | 1:07 | 1:00 | 1:01 | 1:06 | 1:11 | 1:00 | 1:05 | 1:05 | 0:59 | |
| 2 min. | 2:09 | 2:10 | 2:10 | 2:01 | 2:01 | 2:08 | 2:03 | 2:04 | 1:58 | ||
| 3 min. | 3:05 | 3:00 | 3:04 | 3:08 | 3:02 | 3:03 | 3:00 | 3:09 | 2:56 | ||
|
| |||||||||||
| Improvement in 90th percentile time to AED on scene (mm:ss) | 1 min. | 3:36 | 0:00 | 1:30 | 6:14 | 1:37 | 0:05 | 0:53 | 0:00 | 2:45 | |
| 2 min. | 5:28 | 3:09 | 5:43 | 9:06 | 2:43 | 1:57 | 0:00 | 3:15 | 4:47 | ||
| 3 min. | 6:43 | 4:37 | 7:47 | 10:34 | 4:21 | 3:24 | 4:30 | 4:50 | 6:05 | ||
|
| |||||||||||
| Proportion of cases where drone AED arrives prior to 911 (%) | 1 min. | 69.0 | 64.2 | 65.0 | 76.3 | 71.7 | 54.1 | 64.4 | 63.9 | 67.9 | |
| 2 min. | 87.6 | 82.1 | 78.6 | 79.7 | 84.7 | 75.3 | 73.9 | 79.5 | 84.6 | ||
| 3 min. | 96.1 | 94.6 | 89.6 | 84.2 | 94.6 | 92.2 | 92.7 | 89.2 | 94.6 | ||
|
| |||||||||||
| Integrated | Number of bases (Total drones) | 1 min. | 3 (7) | 2 (4) | 3 (4) | 0 (0) | 2 (4) | 1 (2) | 1 (2) | 3 (5) | 15 (28) |
| 2 min. | 6 (12) | 4 (6) | 7 (7) | 1 (1) | 4 (7) | 2 (4) | 4 (6) | 6 (8) | 34 (51) | ||
| 3 min. | 13 (26) | 5 (7) | 7 (7) | 0 (0) | 8 (10) | 4 (7) | 5 (5) | 7 (8) | 49 (70) | ||
|
| |||||||||||
| Improvement in median time to AED on scene (mm:ss) | 1 min. | 1:41 | 0:32 | 1:21 | 0:00 | 0:57 | 1:34 | 0:13 | 1:08 | 1:10 | |
| 2 min. | 2:37 | 1:47 | 3:34 | 0:00 | 1:32 | 2:11 | 2:11 | 2:12 | 2:12 | ||
| 3 min. | 3:35 | 2:48 | 3:43 | 0:00 | 2:34 | 3:09 | 2:57 | 3:25 | 3:09 | ||
|
| |||||||||||
| Improvement in 90th percentile time to AED on scene (mm:ss) | 1 min. | 4:39 | 0:00 | 0:00 | 0:00 | 1:30 | 1:49 | 0:00 | 0:00 | 3:28 | |
| 2 min. | 5:36 | 2:28 | 3:31 | 0:00 | 2:43 | 3:54 | 3:37 | 4:09 | 4:59 | ||
| 3 min. | 7:05 | 0:00 | 0:14 | 0:00 | 4:04 | 5:09 | 4:45 | 1:18 | 6:24 | ||
|
| |||||||||||
| Proportion of cases where drone AED arrives prior to 911 (%) | 1 min. | 79.5 | 53.1 | 59.1 | 0.0 | 68.4 | 68.9 | 48.1 | 61.3 | 70.2 | |
| 2 min. | 90.6 | 78.7 | 86.8 | 32.9 | 79.4 | 79.1 | 85.5 | 82.1 | 85.6 | ||
| 3 min. | 97.9 | 85.3 | 79.8 | 0.0 | 92.4 | 93.5 | 92.7 | 81.3 | 92.3 | ||
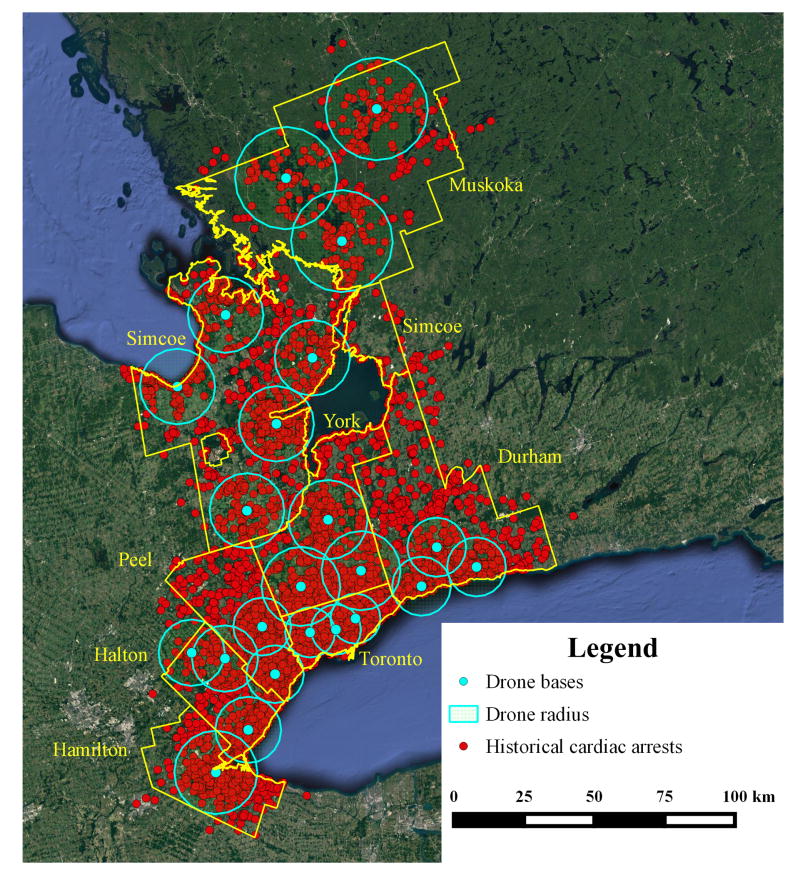
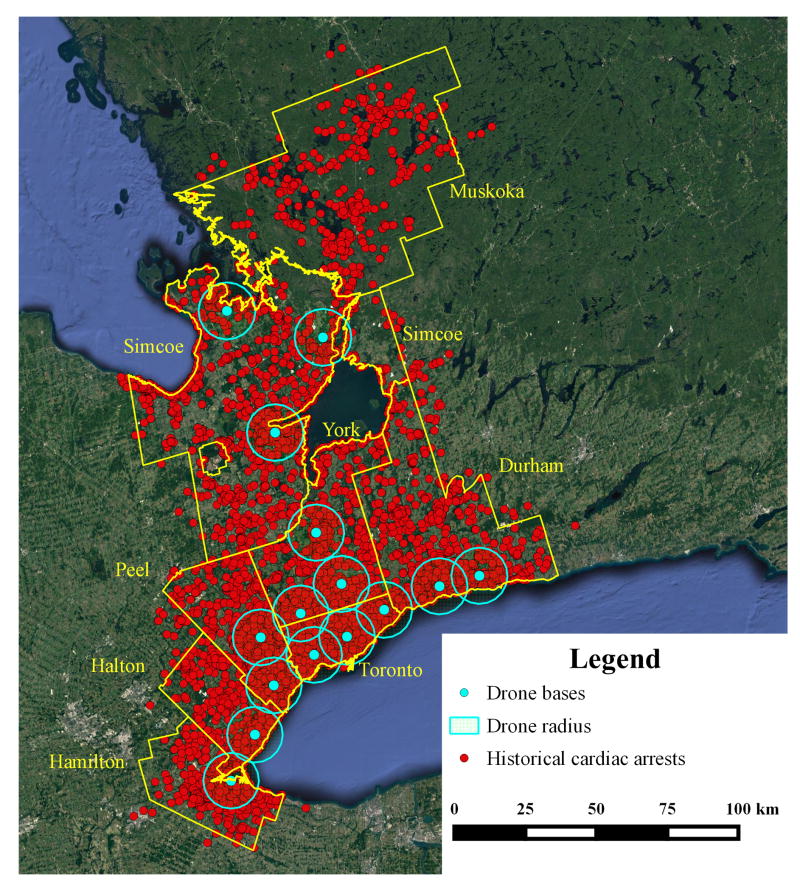
Figure 3 compares the region-specific and integrated drone networks for the one-minute improvement goal. In the region-specific network, there is broad geographical coverage across all regions. However, the integrated network chooses to concentrate most of the bases in the region surrounding the high cardiac arrest density areas (e.g., Toronto) in order to minimize the number of bases required. For example, in Figure 3, there are no drone bases located in Muskoka. Supplemental Figures 3 and 4 illustrate the drone network configurations for the two- and three-minute improvement goals.
Figure 3.
Geographic layout of the (a) region-specific and (b) integrated drone networks for the one-minute improvement goal. Radius of circle represents the maximum distance or available flying time of the drone in order to improve the median 911 response time by one minute in each region, taking into account region-specific dispatch and response times.
Figure 4 compares the historical 911 response time distribution to the estimated response time distribution of a combined 911 and drone network in both Toronto and Muskoka, the regions with the highest and lowest population density, respectively. In both regions, we see a marked shift of the response time distribution to the left (i.e., toward shorter response times) as the response time improvement goal increases. For the three-minute goal in Toronto, the 90th percentile of the combined 911 and drone response represents a 63.1% reduction of the 90th percentile of the historical 911 distribution. In Muskoka, the corresponding reduction was 54.0%. Across all regions, adding drones results in a similar improvement (Supplemental Figures 5 to 10).
Figure 4.
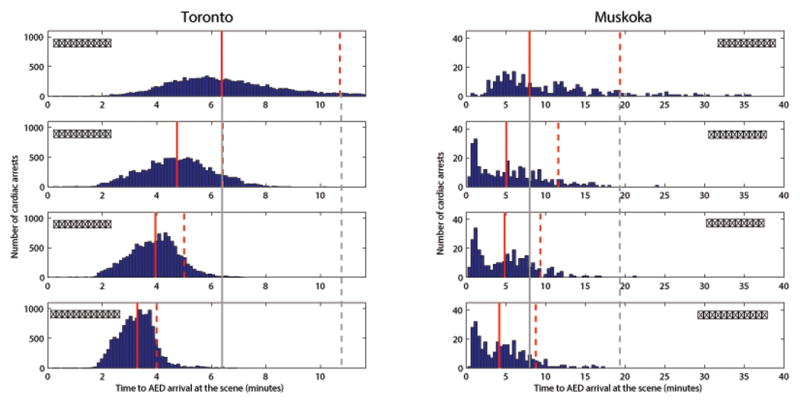
The first row, labelled “Historical”, shows the distribution of historical 911 response times in Toronto (the most urban region in the Toronto RescuNET) and Muskoka (the most rural region in the Toronto RescuNET). The second row, labelled “One-minute”, shows the estimated response time distribution corresponding to the drone network configuration designed to improve the historical median response time by one minute. The third and fourth rows show the response time distributions corresponding to the drone network configurations designed to improve the historical median response by two and three minutes, respectively. The solid line is the median of the distribution and the dashed line is the 90th percentile. The historical distribution is extended in grey across all three distributions as a reference.
Our statistical analysis found that for region-specific drone networks the reduction in median response time was statistically significant across all regions and all response time improvement goals. For the integrated drone networks, the reduction in median response time was statistically significant for all regions except Muskoka (1, 2, and 3 minute goal) and Halton (1 minute goal)
Table 3 summarizes our sensitivity analysis, which reveals that the drone busy time is critical in determining the drone network size. In particular, when the drone busy time is decreased by 30 minutes, almost all bases require only a single drone, except for the busiest bases in Toronto, which still require several. However, when the drone busy time is increased by 30 minutes, then many regions, especially the denser ones, have bases requiring multiple drones, sometimes double the number from before.
Table 3.
Summary of the sensitivity analysis.
| Change in busy time | Drone response time improvement goal | Region | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Toronto | Durham | Simcoe | Muskoka | Peel | Hamilton | Halton | York | All | |||
| Region-specific | -30 minutes | 1 min. | 6 | 3 | 5 | 3 | 2 | 2 | 3 | 3 | 27 |
| 2 min. | 10 | 5 | 11 | 5 | 4 | 2 | 3 | 5 | 45 | ||
| 3 min. | 14 | 14 | 20 | 6 | 10 | 5 | 5 | 8 | 82 | ||
|
| |||||||||||
| -15 minutes | 1 min. | 6 | 5 | 5 | 3 | 4 | 2 | 4 | 5 | 34 | |
| 2 min. | 12 | 6 | 11 | 5 | 7 | 2 | 3 | 6 | 52 | ||
| 3 min. | 20 | 15 | 20 | 6 | 10 | 6 | 5 | 8 | 90 | ||
|
| |||||||||||
| 0 minutes | 1 min. | 6 | 6 | 6 | 3 | 4 | 2 | 4 | 6 | 37 | |
| 2 min. | 12 | 7 | 12 | 5 | 8 | 2 | 4 | 7 | 57 | ||
| 3 min. | 26 | 16 | 20 | 6 | 11 | 7 | 5 | 9 | 100 | ||
|
| |||||||||||
| +15 minutes | 1 min. | 7 | 6 | 6 | 3 | 4 | 2 | 4 | 6 | 38 | |
| 2 min. | 12 | 7 | 13 | 5 | 8 | 2 | 5 | 8 | 60 | ||
| 3 min. | 26 | 16 | 21 | 6 | 13 | 8 | 6 | 12 | 108 | ||
|
| |||||||||||
| +30 minutes | 1 min. | 9 | 6 | 6 | 3 | 4 | 2 | 4 | 6 | 40 | |
| 2 min. | 13 | 7 | 13 | 5 | 8 | 2 | 5 | 8 | 61 | ||
| 3 min. | 26 | 17 | 22 | 6 | 18 | 8 | 8 | 12 | 117 | ||
|
| |||||||||||
| Integrated | -30 minutes | 1 min. | 6 | 2 | 3 | 0 | 4 | 2 | 1 | 4 | 22 |
| 2 min. | 11 | 4 | 7 | 1 | 4 | 2 | 4 | 6 | 39 | ||
| 3 min. | 16 | 5 | 7 | 0 | 8 | 4 | 5 | 7 | 52 | ||
|
| |||||||||||
| -15 minutes | 1 min. | 6 | 4 | 3 | 0 | 4 | 2 | 2 | 5 | 26 | |
| 2 min. | 12 | 5 | 7 | 1 | 7 | 4 | 4 | 7 | 47 | ||
| 3 min. | 26 | 6 | 7 | 0 | 9 | 5 | 5 | 7 | 65 | ||
|
| |||||||||||
| 0 minutes | 1 min. | 7 | 4 | 4 | 0 | 4 | 2 | 2 | 5 | 28 | |
| 2 min. | 12 | 6 | 7 | 1 | 7 | 4 | 6 | 8 | 51 | ||
| 3 min. | 26 | 7 | 7 | 0 | 10 | 7 | 5 | 8 | 70 | ||
|
| |||||||||||
| +15 minutes | 1 min. | 8 | 4 | 4 | 0 | 4 | 2 | 2 | 6 | 30 | |
| 2 min. | 13 | 6 | 8 | 1 | 7 | 4 | 6 | 9 | 54 | ||
| 3 min. | 26 | 8 | 8 | 0 | 14 | 7 | 6 | 9 | 78 | ||
|
| |||||||||||
| +30 minutes | 1 min. | 8 | 4 | 4 | 0 | 4 | 2 | 2 | 6 | 30 | |
| 2 min. | 13 | 6 | 8 | 1 | 7 | 4 | 6 | 9 | 54 | ||
| 3 min. | 26 | 9 | 8 | 0 | 16 | 7 | 8 | 11 | 85 | ||
The numbers represent the total number of drones required for each improvement goal and reset time pair. The number of drone bases is unaffected by the busy time and is omitted for clarity (See Table 2 for results on drone bases). Note that the “0 minutes” case corresponds to the results in Table 2.
Discussion
Main Findings
This study investigated the theoretical benefit of drone-delivered AEDs using a mathematical model to optimize drone base locations and fleet size. The primary analysis determined the size and structure of the network needed to achieve AED delivery time improvement goals of one, two, and three minutes relative to historical median 911 response times in the Toronto Regional RescuNET. We found that drones not only improve the median time to defibrillator arrival on scene, but reduce the entire response time distribution. Our statistical analysis found that all observed reductions in median response time greater than 13 seconds were statistically significant.
The secondary analysis demonstrated that the performance of an integrated drone network can achieve the same overall performance as eight independent regional networks but with substantially fewer resources. However, the trade-off for this efficiency gain was a loss in geographical coverage in more rural areas. For example, in certain regions and for certain response time improvement goals, there was near elimination of drone coverage, which illustrates the potential inequality that can arise between regions if we simply optimize for all of RescuNet as one integrated region. Such an efficiency-equity trade-off arises because the majority of OHCAs are concentrated in a few regions and our models optimize with respect to median response time; optimizing for the 90th percentile instead of the median would result in more bases in rural areas.
Potential benefits
Drone-delivered AEDs have the potential to improve survival for patients with OHCA because the probability of ventricular fibrillation and survival decays with time.30 Our analysis has demonstrated that, in theory, a drone network can be optimized to allow delivery of AEDs ahead of 911 response. Currently, less than 3% of all cardiac arrests have a public access defibrillator used.15 If drone networks are designed with the goal to deliver AEDs to every cardiac arrest in the region and achieve earlier defibrillation of patients with OHCA, then they are very likely to have a meaningful impact on cardiac arrest survival.
There are numerous benefits to using drones to augment the current 911 system and static public access defibrillators. First, drones offer the potential to actively mobilize defibrillators along with the traditional 911 response. In contrast, the current approach to public access defibrillation is passive. Static defibrillators are deployed in the community with the hope that one is nearby when needed. Most communities do not have systems to mobilize public access defibrillators to the scene of an emergency in a targeted way. Second, drone technology offers many potential tactical advantages. For example, rapid AED delivery may be possible due to straight line travel and traffic avoidance. Drone-delivered AEDs could in principle be available 24/7, unlike most static AEDs.14 Drones may be able to deliver AEDs at height via a balcony or roof for cardiac arrests that occur in high rise buildings, which are known to suffer a survival disadvantage.31 The drone's camera, which is used for navigation, could also be leveraged by the 911 dispatcher to visually assess the patient and support bystander CPR and AED application. Third, drones may be able to quickly reach private location cardiac arrests, which comprise the vast majority of all cardiac arrests and are typically associated with worse outcomes.4 Currently, static public access defibrillators are almost never used for private location cardiac arrests.
Previous literature
Prior work on drone delivery of AEDs is limited to a single preliminary study that found drone-delivered AEDs have the potential to reduce response times in Salt Lake county, Utah.32 However, the study was limited by the fact that they did not use actual cardiac arrest data to inform the drone network design, and omitted several technical and realistic details about drone operation such as dispatch time, busy time, and drone acceleration/deceleration. Moreover, the model used did not consider the need to have multiple drones per base, tacitly assuming that no OHCAs occur when a drone is busy. Our sensitivity analysis showed that the drone busy time is an important operational parameter that heavily influences the number of drones per base.
Limitations
Our modeling approach includes both the determination of drone base locations and the number of drones per base. The latter depends on the estimated incidence of cardiac arrests in each base's catchment area; bases located in high call volume areas will be busier and require more drones. Our parameter choices are meant to induce a more conservative solution, so our drone network size is generally an overestimate. We applied daytime OHCA occurrence rates to determine the number of drones required at each base, which will overestimate the numbers of drones needed because OHCAs occur less frequently at night.29 We used current drone specifications rather than projecting future advances in speed and acceleration, which are progressing rapidly. One factor that may contribute to an underestimation of required drone resources is that we used 911 responder-assessed OHCA for our analysis; we did not have access to all 911 calls that were identified to be potential cardiac arrests at the time of dispatch but were unconfirmed on arrival of the 911 response team, for which a drone would have also been dispatched. In contrast, we used both treated and untreated arrests to test the effectiveness of the drone networks, which may contribute to an overestimation in the required drone resources because in practice, a small fraction of cases may be ruled out for drone deployment. Lastly, response time data was missing for 7.8% of the cases and access time was missing for 49% of cases (see Supplemental Table 3). Access time is hand recorded or estimated by 911 responders and as such, is often left blank or difficult to validate. However, given that we only use this data to determine the median access time, the impact of the missing data is likely small.
Implementation factors
Our sensitivity analysis focused on the drone busy time (Figure 1). The two components of the overall busy time that are the largest and most uncertain are the reset time and on-scene time. The reset time is associated with uncertainty because it depends on how the drone system is operationalized, along with technological impacts such as battery and AED swap-out/recharge, and drone maintenance. The possibilities range from automated status checks and battery swaps to manual inspection by base staff.33-35 Scene time is also uncertain, since the drone could be sent home as soon as the AED is dropped off, or only after the 911 responders arrive, or only when the 911 responders depart the scene, depending on how drone operations would be integrated with standard 911 response procedures.
Vertical delays for OHCAs in high-rise buildings are an important factor for determining AED availability.36 As shown in Table 1, “Access time” adds an additional three-minute delay to patient contact after the 911 responders have arrived at the scene (i.e., wheels stop). To account for this delay, our tacit modelling assumption is that the drone will suffer a similar delay to patient contact as the 911 responders. For instance, for the AED to be applied in most cases there must be two bystanders on scene; one to call 911 and stay with the patient doing CPR, and another to retrieve and apply the AED. In this scenario, we assume the bystander can provide building access and therefore, the time delay to patient contact should be essentially the same between the 911 responder and the bystander. Given the assumption that access time is equal for drones and 911 responders, comparing response time is analogous to comparing patient arrival time. However, for cases where the drone is able to land directly on the balcony, access delays can be mitigated and as a result, our assumption of equal access delay may be conservative. In either case, it is important to note that for both drones and 911 responders, there may be additional access delays that increase the time to AED application
Many regulatory and technical challenges must be addressed before drone-delivered AED systems can be realized. Drones would require permission to fly beyond operator line-of-sight, which is currently permitted in some countries (e.g., Canada) but not others (e.g., United States). It is expected that over time, as drone applications become more widespread and the technology is advanced, such restrictions will be loosened. Inclement weather may adversely impact drone operation. Drone navigation will need to avoid no fly zones (e.g., airports) and negotiate around high-rise buildings. A vigorous public awareness campaign will need to accompany any implementation to ease apprehension and discourage mischievous behavior towards the drones. Most importantly, drones will need to be integrated with the 911 response and such integration will be critical in determining the network scope. Our secondary analysis, which highlights the efficiency-equity trade-off, is a first step towards exploring this issue.
Conclusion
In summary, strategically locating and using drones has the potential to substantially reduce the time to defibrillator arrival at the scene of a cardiac arrest. Drone-delivered AEDs represent a logical progression for both drone applications and technology-enabled emergency response. An integrated drone network can achieve the same overall performance as eight independent regional networks but with substantially fewer resources. Cost-effectiveness of an eventual drone network should be evaluated and weighed against the potential benefits outlined in this paper.
Supplementary Material
Clinical Perspective.
What is new?
We demonstrate, using data from over 50,000 historical OHCAs covering over 26,000 square kilometers in Ontario, Canada, that a theoretical drone network designed with the aid of a mathematical model has the potential to significantly reduce the AED delivery time for bystander use.
We found that a drone network designed to reduce the median AED arrival time by 3 minutes relative to the historical 911 response, also reduced the 90th percentile of the AED arrival time by between 6 minutes and 43 seconds (most urban region) and 10 minutes and 34 seconds (most rural region).
What are the clinical implications?
Drone-delivered AEDs have the potential to be a transformative innovation in the provision of emergency care to cardiac arrest patients, especially those who arrest in a private or rural setting.
Drones require careful integration with 911 response and future clinical research is needed to understand the challenges associated with implementation and to determine the cost-effectiveness of such a system.
Acknowledgments
The authors gratefully acknowledge Prof. Armann Ingolfsson for pointers to helpful references and Ervin Ruci of geocoder.ca for providing us with free access to geocoder.ca's services. The authors would like to thank the Rescu Epistry investigators and all emergency medical service operators, providers and medical directors as well as the in-hospital staff in the SPARC network hospitals working together in the front line of emergency patient care for their continued commitment contributions to high quality care and primary data collection in resuscitation research at Rescu, Li Ka Shing Knowledge Institute, St Michael's Hospital, Toronto Ontario, Canada. The Rescu Epistry database is made possible through grants from the Canadian Institute of Health Research, the Laerdal Medical Foundation and Heart and Stroke Foundation of Canada.
Sources of Funding: The Resuscitation Outcomes Consortium Epistry study is supported by a cooperative agreement (5U01 HL077863) with the National Heart, Lung, and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, Canadian Institutes of Health Research–Institute of Circulatory and Respiratory Health, Defense Research and Development Canada, Heart and Stroke Foundation of Canada, and American Heart Association. Rescu Epistry is funded by a centre grant from the Laerdal Foundation, and knowledge translation collaborative grants and operating grants from Canadian Institutes of Health Research and the Heart and Stroke Foundation of Canada.
Footnotes
Rescu Epistry Investigators Index List: Barto Nascimiento - barto.nascimento@sunnybrook.ca, Damon Scales - damon.scales@sunnybrook.ca, Dennis Ko - dennis.ko@ices.on.ca, Jamie Hutchison - jamie.hutchison@sickkids.ca, Katie Dainty - daintyk@smh.ca, Laurie Morrison - morrisonl@smh.ca, Paul Dorian - dorianp@smh.ca, Richard Swartz - rick.swartz@sunnybrook.ca, Richard Verbeek - rverbeek@socpc.ca, Sandro Rizoli - rizolis@smh.ca, Sheldon Cheskes - scheskes@socpc.ca, Steven Brooks - brookss1@kgh.kari.net, Steve Lin - lins@smh.ca, Timothy C.Y. Chan - tcychan@mie.utoronto.ca
Disclosures: None.
References
- 1.Aufderheide T, Hazinski MF, Nichol G, Steffens SS, Buroker A, McCune R, Stapleton E, Nadkarni V, Potts J, Ramirez RR, Eigel B, Epstein A, Sayre M, Halperin H, Cummins RO. Community lay rescuer automated external defibrillation programs: Key state legislative components and implementation strategies: A summary of a decade of experience for healthcare providers, policymakers, legislators, employers, and community leaders from the american heart association emergency cardiovascular care committee, council on clinical cardiology, and office of state advocacy. Circulation. 2006;113:1260–1270. doi: 10.1161/CIRCULATIONAHA.106.172289. [DOI] [PubMed] [Google Scholar]
- 2.Hazinski MF, Idris AH, Kerber RE, Epstein A, Atkins D, Tang W, Lurie K, American Heart Association Emergency Cardiovascular C, Council on Cardiopulmonary P, Critical C, Council on Clinical C. Hazinski MF, Idris AH, Kerber RE, Epstein A, Atkins D, Tang W, Lurie K. Lay rescuer automated external defibrillator (“public access defibrillation”) programs: Lessons learned from an international multicenter trial: Advisory statement from the american heart association emergency cardiovascular committee; the council on cardiopulmonary, perioperative, and critical care; and the council on clinical cardiology. Circulation. 2005;111:3336–3340. doi: 10.1161/CIRCULATIONAHA.105.165674. [DOI] [PubMed] [Google Scholar]
- 3.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M, Public Access Defibrillation Trial I Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 4.Weisfeldt ML, Everson-Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, Bigham B, Brooks SC, Foerster C, Gray R, Ornato JP, Powell J, Kudenchuk PJ, Morrison LJ. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–321. doi: 10.1056/NEJMoa1010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swor RA, Jackson RE, Compton S, Domeier R, Zalenski R, Honeycutt L, Kuhn GJ, Frederiksen S, Pascual RG. Cardiac arrest in private locations: Different strategies are needed to improve outcome. Resuscitation. 2003;58:171–176. doi: 10.1016/s0300-9572(03)00118-7. [DOI] [PubMed] [Google Scholar]
- 6.Eisenburger P, Sterz F, Haugk M, Scheinecker W, Holzer M, Koreny M, Kaff A, Laggner A, Herkner H. Cardiac arrest in public locations--an independent predictor for better outcome? Resuscitation. 2006;70:395–403. doi: 10.1016/j.resuscitation.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Folke F, Gislason GH, Lippert FK, Nielsen SL, Weeke P, Hansen ML, Fosbol EL, Andersen SS, Rasmussen S, Schramm TK, Kober L, Torp-Pedersen C. Differences between out-of-hospital cardiac arrest in residential and public locations and implications for public-access defibrillation. Circulation. 2010;122:623–630. doi: 10.1161/CIRCULATIONAHA.109.924423. [DOI] [PubMed] [Google Scholar]
- 8.Cram P, Vijan S, Fendrick AM. Cost-effectiveness of automated external defibrillator deployment in selected public locations. J Gen Intern Med. 2003;18:745–754. doi: 10.1046/j.1525-1497.2003.21139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gold LS, Eisenberg M. Cost-effectiveness of automated external defibrillators in public places: Pro. Curr Opin Cardiol. 2007;22:1–4. doi: 10.1097/HCO.0b013e32801173c1. [DOI] [PubMed] [Google Scholar]
- 10.Chan TCY, Demirtas D, Kwon RH. Optimizing the deployment of public access defibrillators. Manage Sci. 2016;62:3617–3635. [Google Scholar]
- 11.Winkle RA. The effectiveness and cost effectiveness of public-access defibrillation. Clin Cardiol. 2010;33:396–399. doi: 10.1002/clc.20790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pell JP, Walker A, Cobbe SM. Cost-effectiveness of automated external defibrillators in public places: Con. Curr Opin Cardiol. 2007;22:5–10. doi: 10.1097/HCO.0b013e3280118fec. [DOI] [PubMed] [Google Scholar]
- 13.Siddiq AA, Brooks SC, Chan TC. Modeling the impact of public access defibrillator range on public location cardiac arrest coverage. Resuscitation. 2013;84:904–909. doi: 10.1016/j.resuscitation.2012.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sun CLF, Demirtas D, Brooks SC, Morrison LJ, Chan TCY. Overcoming spatial and temporal barriers to public access defibrillators via optimization. J Am Coll Cardiol. 2016;68:836–845. doi: 10.1016/j.jacc.2016.03.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weisfeldt ML, Sitlani CM, Ornato JP, Rea T, Aufderheide TP, Davis D, Dreyer J, Hess EP, Jui J, Maloney J. Survival after application of automatic external defibrillators before arrival of the emergency medical system: Evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Webredactie Communication. TU Delft's ambulance drone drastically increases chances of survival of cardiac arrest patients. [Accessed January 30, 2017];Delft University of Technology. 2014 Oct 27; http://www.tudelft.nl/en/current/latest-news/article/detail/ambulance-drone-tu-delft-vergroot-overlevingskans-bij-hartstilstand-drastisch/
- 17.Reece P. Drones that save lives. [Accessed January 30, 2017];Salt Spring Island Exchange. 2014 Jun 26; http://saltspringexchange.com/2014/06/26/drones-that-save-lives/
- 18.Patrick WG. Request apparatus for delivery of medical support implemented by UAV. U.S. Patent 9,307,383. 2016 Apr 5;
- 19.India: Police investigate pizza deliveries by drone. [Accessed January 30, 2017];BBC News. 2014 May 23; http://www.bbc.com/news/blogs-news-from-elsewhere-27537120.
- 20.Kannan P. UAE develops delivery drones to improve government services. [Accessed January 30, 2017];The National. 2014 Feb 10; http://www.thenational.ae/uae/government/uae-develops-delivery-drones-to-improve-government-services.
- 21.Hackman M, Nicas J. Drone delivers medicine to rural virginia clinic. [Accessed January 30, 2017];The Wall Street Journal. 2015 Jul 27; https://www.wsj.com/articles/drone-delivers-medicine-to-rural-virginia-clinic-1437155114.
- 22.D'Onfro J. Meet The Startup That's Using Drones To Change The World. [Accessed January 30, 2017];Business Insider. 2014 Nov 8; http://www.businessinsider.com/matternet-uav-delivery-drones-2014-11.
- 23.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, Pirrallo RG, Atkins DL, Davis DP, Idris AH, Newgard C, ROC Investigators Rationale, development and implementation of the resuscitation outcomes consortium epistry-cardiac arrest. Resuscitation. 2008;78:161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin S, Morrison LJ, Brooks SC. Development of a data dictionary for the strategies for post arrest resuscitation care (sparc) network for post cardiac arrest research. Resuscitation. 2011;82:419–422. doi: 10.1016/j.resuscitation.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 25.Schollig A, Hehn M, Lupashin S, D'Andrea R. Feasiblity of motion primitives for choreographed quadrocopter flight. Proc Am Control Conf. 2011:3843–3849. [Google Scholar]
- 26.Kumar V, Michael N. Opportunities and challenges with autonomous micro aerial vehicles. Int J Rob Res. 2012;31:1279–1291. [Google Scholar]
- 27.Van Hoeyweghen RJ, Bossaert LL, Mullie A, Calle P, Martens P, Buylaert WA, Delooz H. Quality and efficiency of bystander cpr. Belgian cerebral resuscitation study group. Resuscitation. 1993;26:47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- 28.King RL. Drones should get their own airspace, says amazon. [Accessed January 30, 2017];The Toronto Star. 2015 Jul 28; https://www.thestar.com/business/2015/07/28/drones-should-get-their-own-airspace-says-amazon.html.
- 29.Brooks SC, Schmicker RH, Rea TD, Aufderheide TP, Davis DP, Morrison LJ, Sahni R, Sears GK, Griffiths DE, Sopko G. Out-of-hospital cardiac arrest frequency and survival: Evidence for temporal variability. Resuscitation. 2010;81:175–181. doi: 10.1016/j.resuscitation.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, Taylor SE. Probability of a shockable presenting rhythm as a function of ems response time. Prehosp Emerg Care. 2014;18:224–230. doi: 10.3109/10903127.2013.851308. [DOI] [PubMed] [Google Scholar]
- 31.Drennan IR, Strum RP, Byers A, Buick JE, Lin S, Cheskes S, Hu S, Morrison LJ, ROC Investigators Out-of-hospital cardiac arrest in high-rise buildings: Delays to patient care and effect on survival. CMAJ. 2016;188:413–419. doi: 10.1503/cmaj.150544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pulver A, Wei R, Mann C. Locating aed enabled medical drones to enhance cardiac arrest response times. Prehosp Emerg Care. 2016;20:378–389. doi: 10.3109/10903127.2015.1115932. [DOI] [PubMed] [Google Scholar]
- 33.Ure NK, Chowdhary G, Toksoz T, How JP, Vavrina MA, Vian J. An automated battery management system to enable persistent missions with multiple aerial vehicles. IEEE ASME Trans Mechatron. 2015;20:275–286. [Google Scholar]
- 34.Kemper FP, Suzuki KA, Morrison JR. Uav consumable replenishment: Design concepts for automated service stations. Journal of Intelligent & Robotic Systems. 2011;61:369–397. [Google Scholar]
- 35.Valenti M, Dale D, How J, Vian J. Mission health management for 24/7 persistent surveillance operations. AIAA Guidance, Navigation and Control Conference and Exhibit. 2007:6508. [Google Scholar]
- 36.Chan TC. Rise and shock: Optimal defibrillator placement in a high-rise building. Prehosp Emerg Care. doi: 10.1080/10903127.2016.1247202. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.