Abstract
The binding of the human immunodeficiency virus (HIV-1) envelope glycoprotein (Env) trimer ((gp120/gp41)3) to the receptors CD4 and CCR5 triggers virus entry into host cells. To identify Env regions that respond to CCR5 binding, HIV-1 was serially passaged on a CD4-positive canine cell line expressing progressively lower levels of CCR5. HIV-1 replication was observed in cells expressing ~1300 CCR5 molecules/cell. Env changes that conferred this low-CCR5 replication phenotype were located outside of the known CCR5-binding region of the gp120 Env subunit and did not apparently increase CCR5 binding affinity. The adaptation-associated changes, located in the gp120 α1 helix and in the gp41 HR1 heptad repeat and membrane-proximal external region (MPER), enhanced HIV-1 replication in cells at all levels of CCR5 expression. The adapted Envs exhibited a greater propensity to undergo conformational changes, as evidenced by increased exposure of conserved regions near the CD4- and CCR5-binding sites.
Keywords: CD4, trigger, receptor, virus, entry, membrane fusion
Introduction
The metastable human immunodeficiency virus (HIV-1) envelope glycoprotein (Env) trimer ((gp120/gp41)3) mediates entry into target cells (Wyatt and Sodroski, 1998). Virus entry is triggered by Env binding sequentially to CD4 and a coreceptor, most often CCR5 but also CXCR4 (Klatzman et al., 1984; Dalgleish et al., 1984; Cocchi et al., 1995; Deng et al., 1996; Feng et al., 1996; Alkhatib et al., 1996; Choe et al., 1996; Doranz et al., 1996; Dragic et al., 1996). CD4 binding drives Env from its unliganded conformation (State 1) through an intermediate (State 2) to the full CD4-bound conformation (State 3) (Munro et al., 2014; Herschhorn et al., 2016). In State 3, Env assumes a pre-hairpin intermediate conformation in which the CCR5-binding site on gp120 and the heptad repeat (HR1) coiled coil on gp41 are formed and exposed (Wu et al., 1996; Trkola et al., 1996, Furuta et al., 1998; Si et al., 2004; He et al., 2003; Koshiba and Chan, 2003). The hydrophobic fusion peptide at the gp41 N-terminus is thought to interact with the target cell membrane during this process (Freed et al., 1990; Kowalski et al., 1987). CCR5 binding (for CCR5-tropic (R5) HIV-1) or CXCR4 binding (for CXCR4-tropic (X4) HIV-1) triggers the pre-hairpin intermediate (State 3) to form the gp41 six-helix bundle (Lu et al., 1995; Chan et al., 1997; Tan et al., 1997; Weissenhorn et al., 1997). The formation of this very stable, post-fusion six-helix bundle is thought to promote the fusion of the viral and target cell membranes (Melikyan et al., 2000).
HIV-1 variants with lower requirements for CD4, including viruses that are completely CD4-independent, have been generated in the laboratory (Kolchinsky et al., 1999; Edwards et al., 2001; Dumonceaux et al., 1998; Zhang et al., 2002). CD4-independent viruses exhibit the ability to sample downstream Env conformations (State 2 and/or State 3) spontaneously, a property dictated by determinants in both gp120 and gp41 subunits (Haim et al., 2011; Kolchinsky et al., 2001a,b; Edwards et al., 2002; LaBranche et al., 1999; Hoffman et al., 1999; Dumonceaux et al., 2001; Musich et al., 2011). Natural HIV-1 variants derived from the central nervous system often exhibit a reduced dependence on CD4 and efficiently infect macrophages and microglia, which express low levels of CD4 (Martin et al., 2001; Thomas et al., 2007; Peters et al., 2004; Gorry et al., 2002; O’Connell et al., 2013).
The vast majority of transmitted/founder HIV-1 and most HIV-1 strains in individuals with established infections are CCR5-tropic (Peters et al., 2004; Lin et al., 2012; Keele et al., 2008; Melby et al., 2006). Clinical observations suggest that blocking Env-CCR5 binding will suppress HIV-1 infection. For example, in 2009, an HIV-1-infected patient with acute myeloid leukemia received a stem cell transplant from a donor homozygous for CCR5Δ32, which encodes an N-terminally deleted CCR5 protein that does not support HIV-1 infection (Liu et al., 1996). Since then, this individual has had an undetectable viral load and a sustained reconstitution of his immune system in the absence of antiretroviral therapy (Hutter et al., 2009; Allers et al., 2011).
Small-molecule CCR5 antagonists have been used to treat HIV-1 infection (Anastassopoulou et al., 2011; Lalezari et al., 2005; Roche et al., 2011; Tilton et al., 2010a). Maraviroc (MVC) is an FDA-approved HIV-1 entry inhibitor that binds in the hydrophobic pocket formed by the CCR5 transmembrane helices and stabilizes a CCR5 conformation that resists efficient gp120 binding (Garcia-Perez et al., 2011; Tan et al., 2013). HIV-1-infected individuals treated with MVC exhibited reduced viral loads, followed by selection for previously undetected CXCR4-using viruses or the evolution of CCR5-tropic viruses capable of using MVC-bound CCR5 as a coreceptor (Lalezari et al., 2005; Tilton et al., 2010a,b; Westby et al., 2007; Jiang et al., 2015; Berro et al., 2011; Westby et al., 2007). These latter MVC-resistant viruses have altered residues in the gp120 V3 stem that enhance binding affinity to the CCR5 N-terminus and to the drug-bound extracellular loops, despite overall decreases in entry and replication capacity (Roche et al., 2011; Tilton et al., 2010a,b; Berro et al., 2012). HIV-1 adapted to vicriviroc, an investigational CCR5 antagonist, displayed altered residues in gp41 that have been proposed to lead to increased triggering of the fusion peptide as well as gp120 changes that enhanced affinity for the CCR5 N-terminus (Lalezari et al., 2005; Berro et al., 2012). These studies indicate that HIV-1 can evolve to use conformationally altered CCR5 for viral entry.
Strategies to interfere with CCR5 binding would benefit from additional knowledge about the structures of the CCR5-bound Env trimer and downstream intermediates, the Env determinants of these conformational transitions, and the molecular dynamics required for viral entry. Here, we generate HIV-1 isolates that infect cells with low levels of CCR5, hypothesizing that the adaptation-associated changes in Env will identify regions that are critical for CCR5 binding or CCR5-triggered membrane fusion. We tested the extent to which HIV-1 can evolve to adapt to limiting amounts of CCR5 by progressively reducing the levels of CCR5 expressed on target cells and monitoring the compensatory changes in the adapted HIV-1 Env. The starting virus for these studies was a chimeric HIV-1 with the envelope glycoproteins from HIV-1JR-FL, a macrophage-tropic brain-derived virus that was already able to infect cells with moderately low levels of CCR5 (O’Brien et al., 1990). After extensive passage, viruses that can infect cells with ~1300 CCR5 molecules per cell were generated. The adapted viruses demonstrated enhanced infectivity compared to the starting virus during cell-cell transmission, but cell-free infectivity was poor. The Env changes required for the adaptation to low CCR5 usage did not result in an increase in CCR5 binding. However, the adapted viruses were more sensitive to CD4 triggering and to neutralization by particular antibodies, indicating that the Env from these viruses is predisposed to make transitions from a State 1 conformation.
Results
Adaptation of HIV-1NL4.3(JR-FL) to replicate in cells expressing low levels of CCR5
We adapted an HIV-1 with the HIV-1JR-FL Env to infect cells with low levels of CCR5 by serially passaging the virus in cells in which the level of CCR5 expression was gradually decreased. Cf2Th canine cells constitutively expressing human CD4 and expressing human CCR5 in a Tet-regulated fashion were used as target cells for the adaptation (Fig. 1). Two Cf2Th clones that express high levels of CD4 and either low or high ranges of cell-surface CCR5 upon doxycycline treatment, herein called R5-Low and R5-High cells, were used for HIV-1 adaptation. An initial stock of HIV-1NL4.3(JR-FL) was prepared by transfecting 293T cells with the proviral plasmid and harvesting the cell supernatant three days later. Cf2Th-CD4/CCR5 cells, which constitutively express human CD4 and human CCR5, were incubated with the 293T cell supernatants and cultured. Reverse transcriptase activity was detected in the supernatants by 30 days of culture (data not shown). Cell supernatants with reverse transcriptase activity were used to reinfect Cf2Th-CD4/CCR5 in the presence of 2 μg/mL polybrene to enhance infection. Viruses in the supernatants of these cells were used for adaptation of HIV-1NL4.3(JR-FL) to CD4-expressing cells with low levels of CCR5.
Fig. 1.
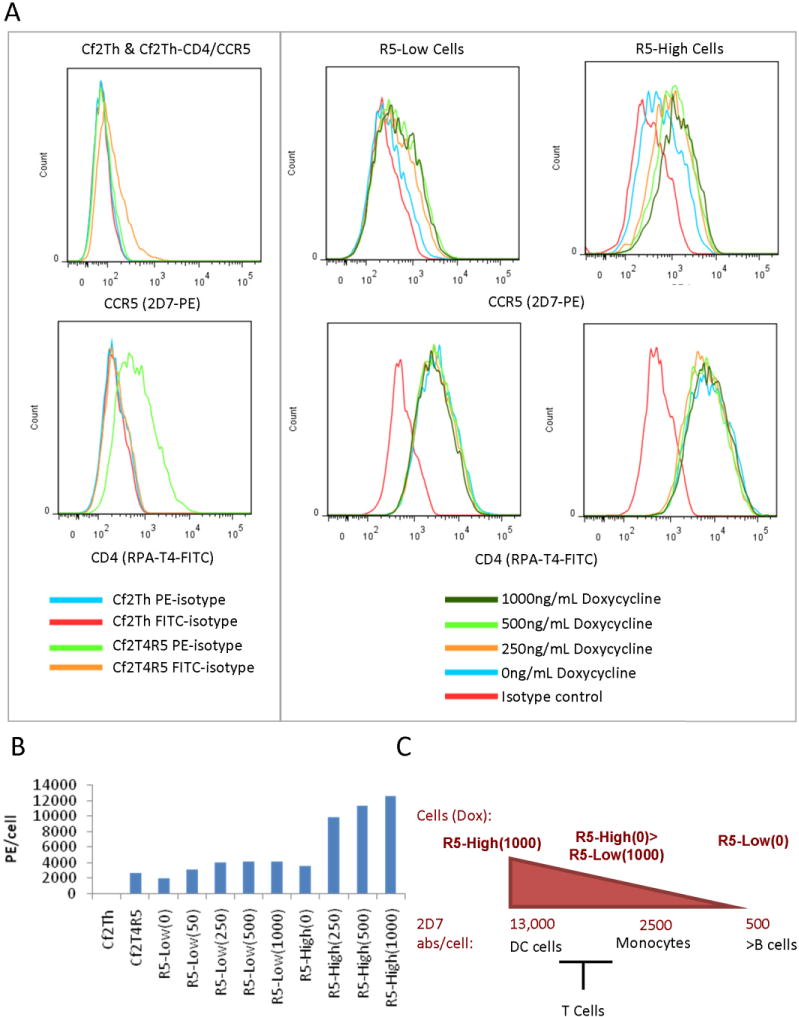
Characterization of CD4-positive cells with regulated CCR5 expression. (A) FACS analysis of doxycycline-regulated Cf2Th-CD4-CCR5(TetOn) cells. Cell clones were incubated with 0-1000 ng/ml doxycyline for 18 h, stained with anti-CCR5 (2D7-PE) or anti-CD4 (RPA-T4-FITC) fluorescent antibodies, and analyzed by FACS. One set of cells was stained with labeled mouse IgG2a, ĸ isotype control. (B) QuantiBrite PE quantification of 2D7 epitopes/cell. Two thaws of frozen cell stocks were independently analyzed in the presence of the doxycycline concentration (ng/ml) indicated in parentheses. Average values are shown. (C) Representation of the number of epitopes/cell of the 2D7 anti-CCR5 antibody compared with that on immune cells (Lee et al., 1999).
Cf2Th cells expressing human CD4 constitutively and human CCR5 in a Tet-regulated manner (Fig. 1) were incubated with the HIV-1NL4.3(JR-FL) virus and then passaged. By three rounds of passage, viruses emerged that replicated on a mixture of 70% R5-High cells and 30% R5-Low cells in 1 μg/mL doxycycline (Fig. 2A). By 9 rounds of passage, viruses that replicated on R5-Low cells in 75 ng/mL doxycycline were obtained.
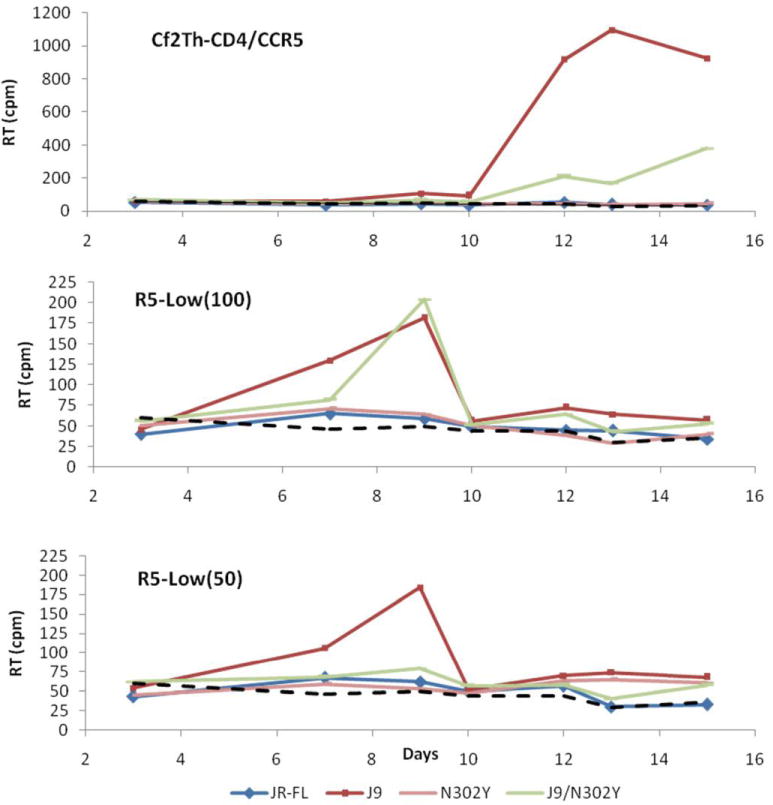
Fig. 2.
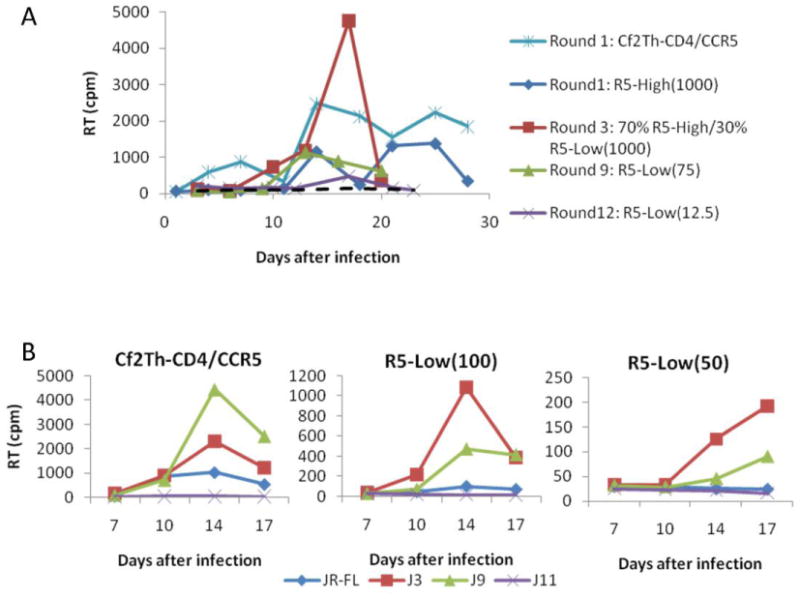
Adaptation of HIV-1NL4.3(JR-FL) to low levels of CCR5. (A) Replication kinetics of HIV-1NL4.3(JR-FL) at different rounds of adaptation in the indicated cell type and doxycycline concentrations. Cf2Th and Cf2Th-CD4/CCR5 cells were infected with HIV-1NL4.3(JR-FL). A 32P-reverse-transcriptase assay was performed on medium removed at each passage. Results are displayed as cpm of 32P -labeled nucleotides reverse transcribed. Viruses at peak reverse transcriptase activity were used to infect R5-High or R5-Low cells in the next round of adaptation. The dashed line represents reverse transcriptase activity in supernatants from CD4-negative, CCR5-negative Cf2Th cells incubated with virus in Round 12. Numbers in parentheses refer to the concentration of doxycycline in ng/ml. (B) Viruses were derived at various passages in R5-Low cells. Wild-type HIV-1JR-FL or viruses from passage 3 (J3), passage 9 (J9) and passage 11 (J11) were used to infect Cf2Th, Cf2Th-CD4/CCR5, and R5-Low cells. Viral pools were normalized for the amount of p24 Gag protein prior to infection. The reverse transcriptase activity in the culture supernatants is shown.
When additional rounds of virus passage were conducted at decreasing levels of target cell CCR5 expression, we observed decreasing reverse transcriptase activity in the cell supernatants (Fig. 2A). Viral replication was not detected beyond round 12, in which we detected reverse transcriptase activity in the supernatants of R5-Low cells in 12.5 ng/mL doxycycline. Cell-free viruses in the supernatant of the round 12 cultures did not detectably replicate in R5-Low cells maintained in the same levels of doxycycline (data not shown). QuantibritePE was used to estimate the number of CCR5 molecules/cell by quantifying the epitopes for the 2D7 anti-CCR5 antibody per cell (BD Biosciences). Replication of HIV-1NL4.3(JR-FL) was not detected in the CD4-expressing cells with less than ~1300 CCR5 molecules per cell (Fig. 1).
To confirm that the viruses generated by this adaptation procedure could replicate in cells expressing low levels of CCR5, we infected R5-Low cells at 50 and 100 ng/mL doxycycline, as well as Cf2Th-CD4/CCR5 cells, with cell supernatants from round 3 (J3), round 9 (J9) and round 11 (J11) that were normalized for the level of the p24 Gag protein. Fig. 2B compares the replication capacity of the J3 and J9 viruses with that of the parental HIV-1NL4.3(JR-FL) virus for each cell type and doxycycline concentration. In Cf2Th-CD4/CCR5 cells, J3 and J9 viruses infected 2-fold and 4-fold more efficiently than the parental HIV-1NL4.3(JR-FL), respectively. Both J3 and J9 viruses replicated better than HIV-1NL4.3(JR-FL) in R5-Low(100) and R5-Low(50) cells. The production of the J3 virus in R5-Low(100) cells was comparable to that of the parental HIV-1NL4.3(JR-FL) in Cf2Th-CD4/CCR5 cells; by contrast, HIV-1NL4.3(JR-FL) replicated only marginally in the R5-Low(100) cells. Both J3 and J9 viruses replicated in R5-Low(50) cells, whereas no HIV-1NL4.3(JR-FL) reverse transcriptase activity was detected in these cells. These observations indicate that the J3 and J9 viruses have adapted to replicate better than the parental HIV-1NL4.3(JR-FL) virus on cells expressing low levels of CCR5.
The J11 viral pool did not detectably replicate in any cell type, suggesting that some adaptive changes occurring after round 9 were deleterious to cell-free infection in this context.
Adaptive changes in the HIV-1JR-FL Env
We isolated the genomic DNA of the cells collected at the time point of peak reverse transcriptase activity in the supernatant at each round of adaptation, PCR amplified the integrated HIV-1 provirus, and sequenced the env gene. The wild-type HIV-1JR-FL env sequence was maintained throughout multiple rounds of replication in Cf2Th-CD4/CCR5 cells (data not shown). In the viruses adapted to replicate in R5-Low cells, multiple changes were observed. Changes that were retained through multiple rounds of adaptation are shown in Fig. 3A. Three changes, S115N, R564H, and E662K, were found in all three adapted viruses, J3, J9, and J12. Both J9 and J12 had, in addition, an S164N change, and J9 had an E831D change.
Fig. 3.
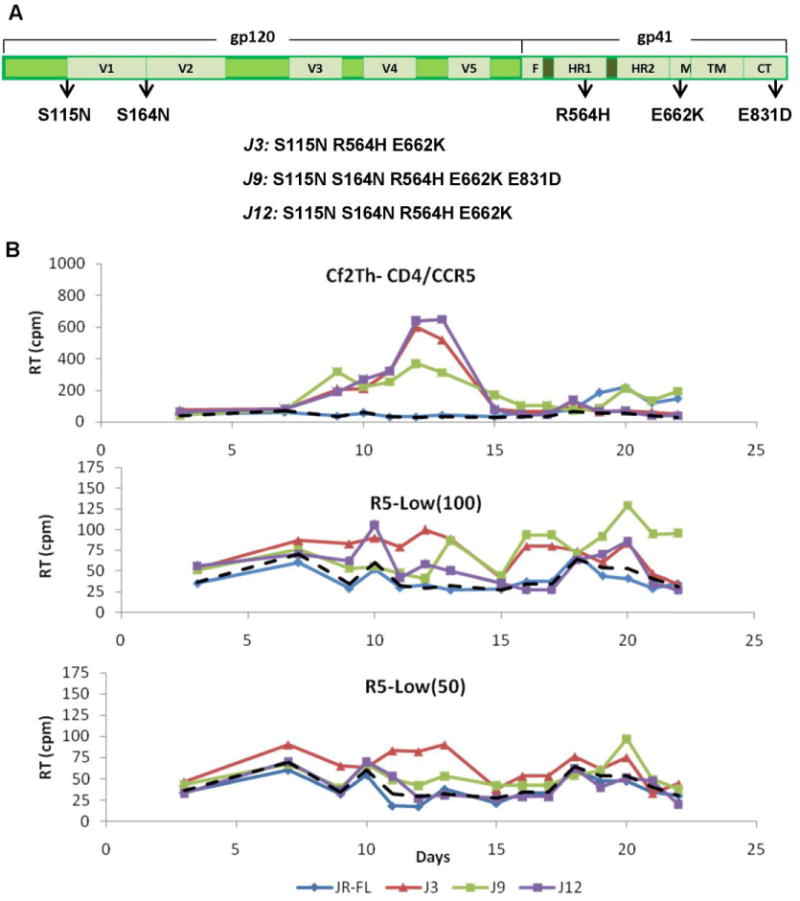
Env changes in adapted HIV-1NL4.3(JR-FL) permit viral replication in cells expressing low levels of CCR5. (A) The location of adaptation-associated changes in the HIV-1(JR-FL) Env is shown. V: Variable region; F: Fusion peptide; HR: Heptad repeat; M: Membrane Proximal External Region; TM: Transmembrane region; CT: Cytoplasmic Tail. The Env changes observed in the J3, J9 and J12 passaged viruses are listed beneath the diagram. (B) The indicated cells were transfected with the pNL4.3(JR-FL) proviral vector with the wild-type HIV-1JR-FL Env or with the J3, J9, or J12 Envs and passaged for 30 days. A 32P RT assay was performed on medium removed at each passage. Each point represents the average of duplicate samples of a representative replication kinetics assay. The dashed line represents average RT activity of supernatants from Cf2Th cells transfected with the proviral vectors, and represents the background of the assay.
None of the above passage-associated Env changes were observed in previous studies in which HIV-1 was adapted to replicate on Cf2Th cells lacking CD4 (Kolchinsky et al., 1999) or expressing New World monkey receptors (Pacheco et al., 2008). Thus, the observed Env changes apparently arose as an adaptation to the specific requirements imposed by the low-CCR5 cells. None of the observed Env changes has been previously implicated in the interaction of gp120 with CCR5. Based on crystal structures of gp120 bound to a CD4-induced antibody which binds gp120 near the coreceptor-binding site (Kwong et al., 1998), serine 115 is located in the membrane-distal end of the α1 helix, not far from the coreceptor-binding region (Rizzuto et al., 1998). Arginine 564 and glutamic acid 662 are located in the HR1 region and the MPER of gp41, respectively. The arginine 564 residue faces the N-terminal α1 helix of gp120 in the structure of the HIV-1JR-FL Env trimer bound to the PGT151 neutralizing antibody (Lee et al., 2016). Although S115N and E662K are not determinants of HIV-1 resistance to fusion-inhibitory gp41 peptides, these changes have been observed in viruses resistant to these antiviral agents (Shimura et al., 2010; Wang et al., 2011) (Table 1). Serine 164 is between the gp120 V1 and V2 regions; the S164G change has been shown along with other Env alterations to confer resistance to the entry inhibitor BMS-378806 (Zhou et al., 2010). A D164N change in HIV-1JR-CSF along with other Env alterations has been associated with viral replication in CD4-positive, CCR5-positive cells in which CCR5 binding was blocked by the 2D7 monoclonal antibody (Aarons et al., 2001). Finally, E831D is located within the cytoplasmic tail of Env that has been implicated in trafficking of Env into lipid rafts (Chan et al., 2005; Wyma et al., 2000).
Table 1.
Adaptation-associated Env changes and frequency in natural HIV-1 isolates. Source: Davey NE, et al. The HIV Mutation Browser: A Resource for Human Immunodeficiency Virus Mutagenesis and Polymorphism Data. PLoS Comput Biol. 2014 Dec 4;10(12):e1003951.
| Env amino acid change | Location | Frequency in natural HIV-1 isolates |
|---|---|---|
| S115N | C-terminus of the α1 helix (gp120) | S: 95.9%, 4.1% other, no Ns Identified with E662K in SC34EK-resistant HIV-1 (Shimura et al. 2010) |
| S164N | Between V1 & V2 (gp120) | E: 65.3%, 34.1% other, no Ns S164G seen with other mutations in BMS-378806 resistance (Zhou et al. 2010). D164N seen in JR-CSF resistance to 2D7 (Aarons et al., 2001) |
| R564H | Within HR1 (gp41) | H: 92.9%, 7.1% other |
| E662K | MPER (gp41) | E:22.9%/A:66.5%/other:10.6%/K in HIV-2 & SIV Identified with S115N in SC34EK-resistant HIV-1. E662A found in patients with resistance to Enfuvirtide (Shimura et al. 2010) |
| E831D | Cytoplasmic tail, Hydrophilic surface of LLP-1 (gp41) | E: 92.4%, E831D in strain KSM4001 |
Because the HIV-1 Gag polyprotein can influence in the incorporation of Env into viral particles (Wyma et al., 2000; Mammano et al., 1995; Murakami and Freed, 2000; Tedbury et al., 2015, 2016), we sequenced the gag gene of the adapted viruses to identify changes that potentially alter the low-CCR5 usage phenotype. No changes in gag were observed until round 11; the observed alterations (Gag S126N and M228I) have been seen in natural HIV-1 variants and are tolerated with respect to HIV-1 infectivity. We therefore focused on the contribution of changes in Env to the low-CCR5 usage phenotype.
To evaluate the sufficiency of the observed changes to account for the ability of HIV-1NL4.3(JR-FL) to replicate in cells with low CCR5, we generated proviruses with the Env changes observed in J3, J9, and J12. We transfected 100 ng of the proviral plasmids into R5-Low cells in 50 or 100 ng/mL doxycycline, or into Cf2Th-CD4/CCR5 cells (Fig. 3B). Transfection of the proviruses ensured that the initial rounds of infection could involve both cell-free and cell-to-cell transmission, mimicking the conditions of the adaptation procedure. In these experiments, which were carried out without the addition of polybrene, HIV-1NL4.3(JR-FL) exhibited detectable virus production in the Cf2Th-CD4/CCR5 cells only after several rounds of passaging. Relative to the parental HIV-1NL4.3(JR-FL), the viruses with adaptation-associated changes demonstrated more efficient replication in cells at all levels of CCR5 expression. The env gene was PCR amplified and sequenced from genomic DNA from all cells on the final day of the assay. No changes in env sequence were noted for samples in which viral replication was observed. A similar test of viral replication in which cells were transfected with twice as much proviral DNA demonstrated enhanced replication of J3, J9, and J12 compared to the parental HIV-1NL4.3(JR-FL) in cells in which viral replication was detected (data not shown). These results indicate that the Env changes associated with virus adaptation are sufficient to explain the enhanced ability to replicate on CD4-positive cells with low CCR5 expression.
Effect of changes in the HIV-1JR-FL Env on virion Env incorporation and cell-free viral infectivity
Changes that are associated with increased Env availability on the viral membrane or better Env processing may improve viral infectivity in low CCR5 conditions, as they allow more available functional glycoprotein per virus, therefore increasing the opportunity to bind receptors. To measure Env levels on the viral surface, we transiently expressed in 293T cells single-cycle recombinant HIV-1 pseudotyped with the wild-type HIV-1JR-FL Env, the adapted Envs, and an HIV-1JR-FL Env containing the E831D change. The viral particles in the 293T cell supernatants were concentrated by ultracentrifugation through a sucrose cushion. The lysed viral pellet was analyzed by SDS-PAGE and Western blotted for gp120 Env, p55 Gag, and p24 CA (Fig. 4A). The viruses containing the Envs with adaptation-associated changes displayed similar levels of gp120 relative to the viral Gag proteins, p55 and p24, as the parental virus.
Fig. 4.
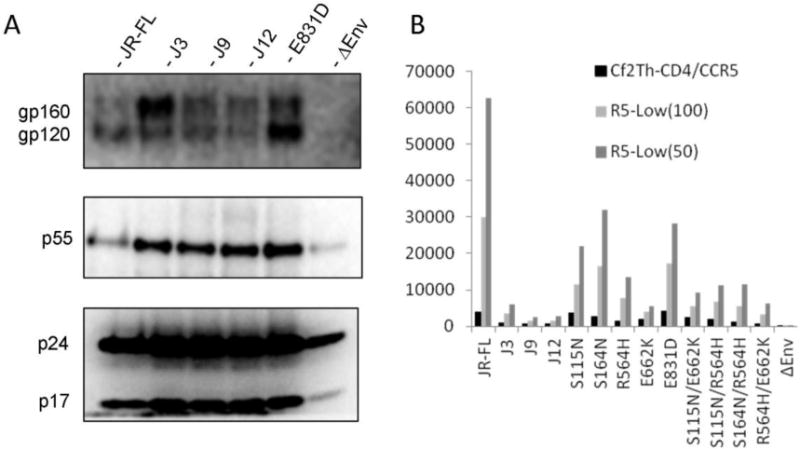
Composition and infectivity of single-round recombinant viruses with Envs from wild-type HIV-1JR-FL or from adapted viruses. (A) Immunoblots of viral proteins in recombinant viruses purified by ultracentrifugation through a 20% sucrose cushion. The recombinant viruses contain the wild-type HIV-1JR-FL Env or the indicated Envs from the adapted viruses; the ΔEnv control viruses lack Env. (B) Infectivity of recombinant, luciferase-expressing viruses containing the wild-type HIV-1JR-FL Env or the indicated variant Envs. Infectivity is indicated by the relative luciferase units (RLU) in the lysates of infected cells, after normalization of the input virus by reverse transcriptase activity (RT). The averages of the means from two experiments with duplicate samples are shown.
To evaluate whether the adapted virus Envs retain the ability to support entry, we incubated Cf2Th-CD4/CCR5 and R5-Low cells with equivalent reverse transcriptase units of recombinant single-round virus (Fig. 4B). In this assay, the expression of luciferase in the target cells is dependent on Env-mediated virus entry, as well as subsequent reverse transcription and integration of the viral vector (Helseth et al., 1990). We observed that viruses with the adapted Envs exhibited approximately a 5-fold reduced infectivity compared to viruses with the parental HIV-1JR-FL Env. Viruses with single and double-residue changes introduced into the wild-type HIV-1JR-FL Env did not demonstrate as great an attenuation in infectivity as the viruses with the adapted Envs. The low levels of infectivity of single-round viruses with adaptation-associated changes contrasts with the enhanced infection of Cf2Th-CD4/CCR5 or R5-Low cells by replication-competent viruses with the same changes. This result suggests that although the parental HIV-1JR-FL Env mediates better infection in a cell-free, single-round context (Fig. 4B), the adapted Envs display an enhanced replication capacity in a context in which cell-free and cell-cell infection occurs.
Effect of adaptation-associated changes in HIV-1JR-FL Env on coreceptor use and virus entry requirements
The altered infectivity of the adapted Envs for CD4-positive, CCR5-positive target cells could result from changes in coreceptor tropism, e.g. with a switch to CXCR4 or to coreceptors present in Cf2Th cells. We tested this by incubating single-cycle recombinant viruses with the parental Cf2Th cell line, and with Cf2Th cells stably expressing human CCR5 alone, CD4 and CXCR4, or CD4 and CCR5. Detectable levels of infection were observed only in Cf2Th-CD4/CCR5 cells (Fig. 5A). These results indicate that the viruses with the adapted Envs remain dependent on the CCR5 coreceptor for efficient infection of target cells.
Fig. 5.
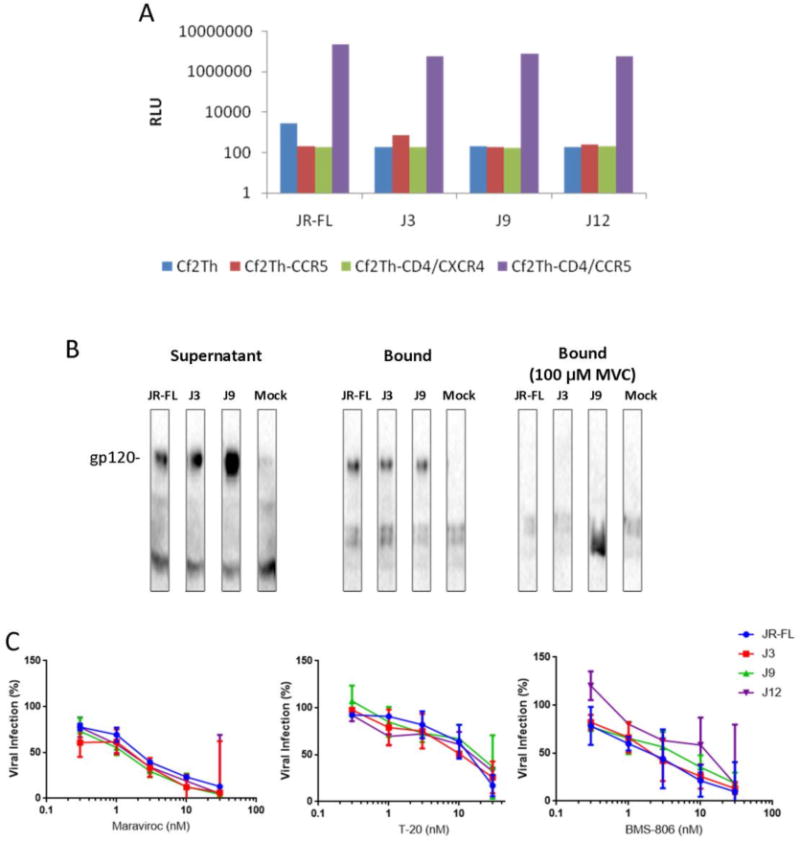
Cellular tropism, CCR5 binding and sensitivity to entry inhibitors of viruses containing wild-type HIV-1JR-FL Env or Envs from adapted viruses. (A) Infection of the indicated target cells by recombinant, luciferase-expressing viruses containing the wild-type HIV-1JR-FL Env or the Envs of the adapted viruses. The infectivity shown represents the ratio of relative luciferase units (RLU) in lysates of infected cells, normalized for the amount of input virus by reverse transcriptase activity (RT). The means of duplicate samples in a typical experiment are shown. (B) Binding of gp120 to CCR5. The gp120 glycoproteins from wild-type HIV-1JR-FL or from the adapted viruses, or supernatants of mock-transfected cells, were incubated with Cf2Th-CCR5 cells in the absence or presence of maraviroc (MVC). The gp120 glycoproteins in the supernatants or bound to the Cf2Th-CCR5 cells are shown. (C) Sensitivity of viruses with the indicated Envs to entry inhibitors, as a percentage of the infectivity observed in the absence of inhibitor. Shown are the means and standard deviations from duplicate samples (Maraviroc and T-20, n=1; BMS-806, n=3).
To evaluate the interaction of the adapted virus Envs with CCR5, we measured the binding of gp120 glycoproteins from these HIV-1 variants to CCR5 on the surface of Cf2Th-CCR5 cells. Soluble gp120 glycoproteins in the supernatants of cells expressing the parental or adapted HIV-1JR-FL Envs were incubated with sCD4 and Cf2Th-CCR5 cells, in the absence or presence of maraviroc (MVC). The binding of the J3 and J9 gp120 glycoproteins to the Cf2Th-CCR5 cells was comparable to that of the wild-type HIV-1JR-FL gp120 (Fig. 5B). MVC completely blocked the binding of gp120-sCD4 complexes to the Cf2Th-CCR5 cells, indicating that a CCR5 protein in the appropriate conformation is necessary for the observed interactions. These results indicate that the adaptation-associated changes in gp120 do not increase the affinity of gp120 for CCR5.
To investigate the dependence of virus infection mediated by the adapted Envs on the known events in the HIV-1 entry process, we tested the sensitivity of these Env variants to entry inhibitors. Differences in the affinity of the functional HIV-1 Env trimer for the receptors are typically accompanied by specific alterations in virus sensitivity to inhibitors of these interactions (Thali et al., 1991; Berro et al., 2011; Rizzuto et al., 1998). Previous HIV-1 adaptation experiments using CCR5 antagonists or suspension cells that regulate CCR5 expression have observed changes in HIV-1 Env that confer resistance to entry inhibitors (Anastassopoulou et al., 2009, 2011, 2012; Berro et al., 2012; Jiang et al., 2015; Westby et al., 2007; Garg et al., 2016). We compared the sensitivity of the wild-type and adapted Envs to the CCR5 antagonist Maraviroc, the gp41-directed fusion inhibitor T-20, and BMS-806, which blocks CD4-induced conformational changes in Env (Fatkenheuer et al., 2005; Kilby et al., 1998; Wang et al., 2003; Wild et al., 1994; Si et al., 2004; Herschhorn et al., 2016). Of note, viruses with the parental HIV-1JR-FL Env and the adapted Envs were inhibited comparably by all three antiviral agents (Fig. 5C). Taken together, the above results indicate that viruses adapted to low CCR5 expression retain dependence on CD4 and CCR5, and infect cells using Env conformational transitions inhibited by BMS-806 and T-20.
Contribution of individual Env changes to HIV-1NL4.3(JR-FL) replication in cells with low CCR5 expression
We sought to identify the changes responsible for the low-CCR5 usage phenotype by transfecting Cf2Th-CD4/CCR5 and R5-Low cells with proviral DNA containing single and double mutations observed in the adapted Envs (Fig. 6). The R564H change alone was able to allow detectable replication in cells expressing different levels of CCR5 expression. The addition of the E662K change to the R564H change enhanced infection in Cf2Th-CD4/CCR5 cells to levels as high as those seen for the adapted Envs (Fig. 6). S115N alone conferred a low level of replication in R5-Low(100) cells but replication was enhanced at each level of CCR5 tested when both the S115N and E662K changes were present. The S115N/R564H and S164N/R564H double mutants exhibited very low levels of infection that were detectable above the background in Cf2Th-CD4/CCR5 and R5-Low(100) cells. The sequences of the env gene determined at the end of a similar infectivity assay did not demonstrate any additional changes. These results indicate that the two gp41 changes, R564H and E662K, are sufficient to allow HIV-1NL4.3(JR-FL) to replicate in Cf2Th cells with low CCR5 expression.
Fig. 6.
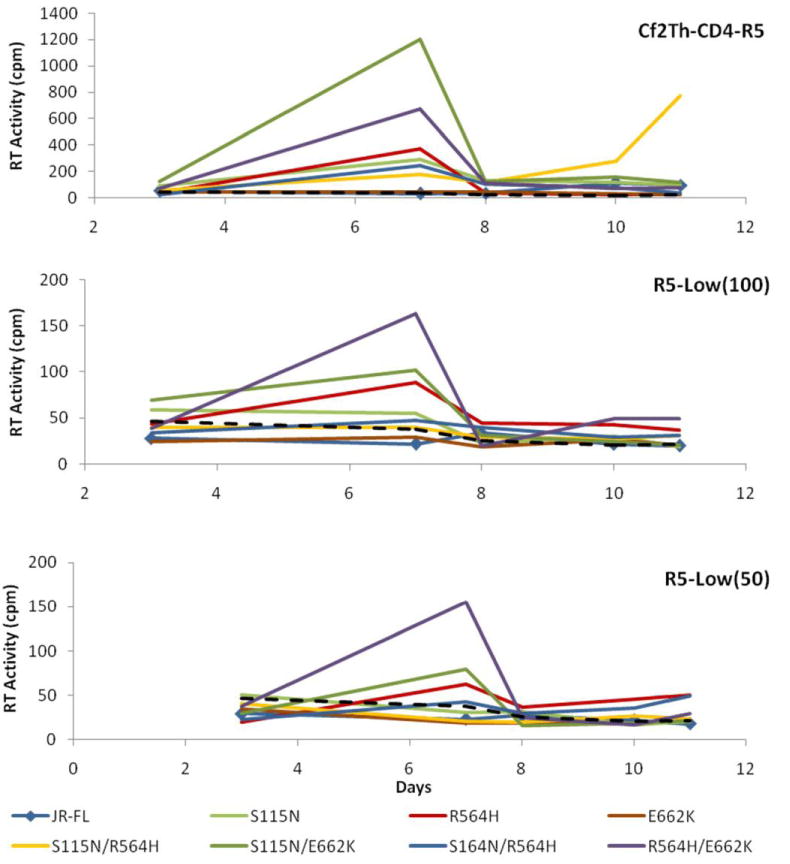
Replication kinetics of NL4.3 viruses containing wild-type or mutant HIV-1JR-FL Envs. The indicated cells were transfected with NL4.3 proviruses with the wild-type or mutant HIV-1JR-FL Envs and passaged for 11 days. A 32P RT assay was performed on medium removed at the time of each passage. The dashed line represents the average reverse transcriptase activity in supernatants of CD4-negative, CCR5-negative Cf2Th cells incubated with each virus. The results of one representative replication assay out of duplicate assays are shown.
Effect of the adaptation-associated changes on cell-to-cell transmission of HIV-1
None of the observed single or double Env changes in HIV-1NL4.3(JR-FL) conferring the low-CCR5 usage phenotype resulted in an enhanced level of single-cycle infection, compared with that of the wild-type HIV-1JR-FL Env (Fig. 4B). Because HIV-1 replication occurs in a context in which infected cells contact uninfected cells, we evaluated the adapted Envs in assays where Env-expressing cells interact with receptor-bearing cells. To determine if the observed adaptation-associated changes enhance Env-mediated cell-cell fusion, we evaluated the adapted Envs in an alpha-complementation assay (Holland et al., 2004). In this assay, COS-1 cells expressing Env are cocultivated with Cf2Th-CD4/CCR5 cells for 8 hours before measuring reporter activity (Fig. 7A). The J3, J9, and J12 Envs exhibited between 25–33% of the cell-cell fusion capacity of the wild-type HIV-1JR-FL Env. The reduced fusion capacity of the adapted Envs with respect to the HIV-1JR-FL Env mimics what we observed in the single-cycle viral assays. No difference in the inhibition of cell-cell fusion by Maraviroc was observed between the wild-type HIV-1JR-FL Env and the adapted Envs (Fig. 7B), consistent with the results seen in the single-cycle viral assays.
Fig. 7.
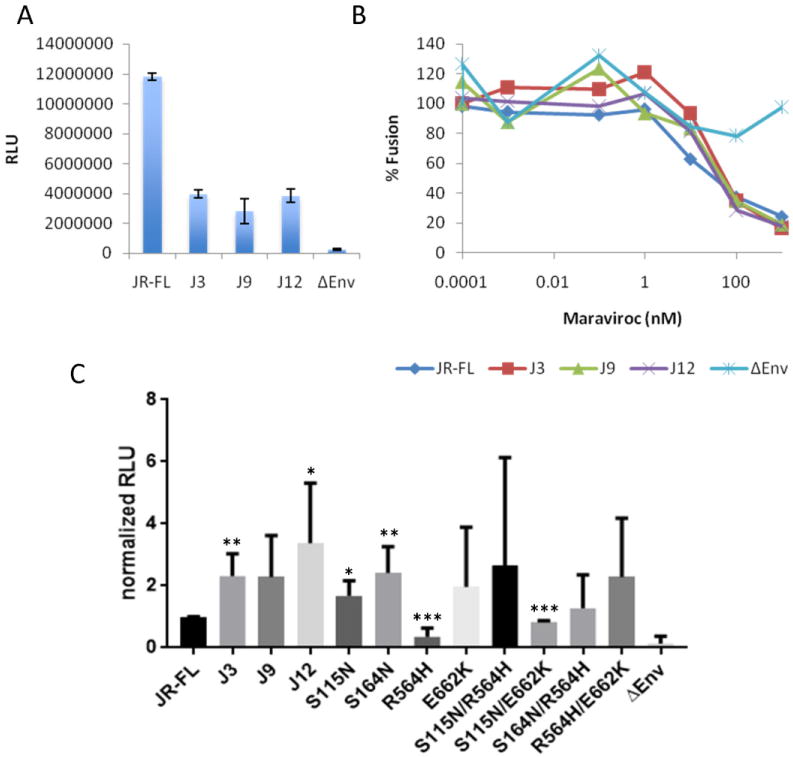
Syncytium-forming ability and cell-to-cell transmission of HIV-1JR-FL Env variants. (A) Cos-1 cells expressing the wild-type HIV-1JR-FL or the adapted virus Envs were incubated with Cf2Th-CD4/CCR5 cells in an alpha complementation assay, as described in the Materials and Methods. The relative light units (RLU) of luciferase activity reflect the degree of cell-cell fusion (syncytium formation) mediated by the Env. The ∆Env is a negative control. (B) Sensitivity of the alpha complementation assay to maraviroc, a CCR5 inhibitor. The % fusion for each Env is shown relative to the value seen in the absence of inhibitor.(C) 293T cells transiently expressing single-round recombinant HIV-1 with the indicated wild-type or variant HIV-1JR-FL Envs were cocultivated with Cf2Th-CD4/CCR5 cells and passaged for approximately 6 days. The luciferase activity (RLU) in the culture was then measured. Means and standard deviations derive from 2 or more coculture samples, normalized to the RLU of viruses with the wild-type HIV-1JR-FL Env. The ∆Env is a negative control virus lacking a functional Env. Student t-test as compared to wild-type HIV-1JR-FL Env: * P ≤ 0.05, ** P ≤ 0.01, and *** P ≤ 0.001.
The above results indicate that, in contrast to the presumed advantage of the adaptation-associated Env changes to HIV-1NL4.3(JR-FL) replication in Cf2Th cells expressing CD4 and low levels of CCR5, these changes do not improve cell-free infection or cell-cell fusion mediated by Env. We therefore utilized an assay in which cell-free and cell-to-cell transmission of HIV-1 occur (Helseth et al, 1990), potentially mimicking the conditions under which the viruses were adapted to the lower level of CCR5 expression. In this assay, transfected 293T cells expressing single-round luciferase-expressing viruses were cocultivated with Cf2Th-CD4/CCR5 cells. Thus, the Cf2Th-CD4/CCR5 target cells could be infected by single-cycle recombinant virus via cell-free infection or by cell-to-cell transfer. Because luciferase expression is initially high in the transfected 293T cells, the assay is conducted for at least 6 days, by which time luciferase expression in the transfected 293T cells diminishes; this decrease in luciferase is monitored by using an Env-deleted (ΔEnv) virus that cannot initiate new infections. If the cotransfected Env can support a new round of either cell-free or cell-to-cell transmission from the transfected 293T cells to the Cf2Th-CD4/CCR5 cells, the expression of luciferase from the integrated HIV-1 vector is sustained for long periods of time. Thus, we measured luciferase activity in the cocultures when the luciferase activity associated with the ΔEnv control returned to background levels.
In this assay, the adapted Envs supported cell-to-cell infection better than the parental JR-FL Env (Fig. 7C). The S115N, S164N and E662K mutants, as well as some of the combined mutants, also were very efficient in this assay. The activity of the single and double mutant Envs did not correlate with the level of enhancement seen for these Envs in the virus replication assay. Thus, although this single-round cell-to-cell infection assay does not fully reproduce all of the features of the virus replication assay, the results suggest that the adaptation-associated Env changes can enhance HIV-1 infection when cell-to-cell transmission is allowed.
Effects of adaptation-associated changes in Env on HIV-1 sensitivity to antibody neutralization
HIV-1 variants with decreased dependence on CD4 typically demonstrate an increased sensitivity to antibodies targeting the CD4-binding and coreceptor-binding sites, such as F105 and 17b, respectively (Haim et al., 2011; Hoffman et al., 1999; Kolchinsky et al., 2001a,b). Therefore, we measured the neutralization sensitivity of our adapted Envs by infecting Cf2Th-CD4/CCR5 cells with single-round luciferase-expressing viruses that had been pre-incubated with a panel of antibodies.
Viruses with the J3, J9 and J12 Envs were slightly more sensitive to inhibition by sCD4 and small-molecule CD4-mimetic compounds than the wild-type HIV-1JR-FL (Table 2). The viruses with the adapted Envs exhibited significant increases in sensitivity to neutralization by the F105, 17b, 830A, 19b, and 1.4E antibodies, which did not inhibit the viruses with the wild-type HIV-1JR-FL Env. These anti-gp120 antibodies against the CD4-binding site (F105), CD4-induced gp120 epitopes (17b), V2 region (830A), and V3 region (19b and 1.4E) recognize an intermediate Env conformation (State 2) that is on the HIV-1 entry pathway (Munro et al., 2014; Herschhorn et al., 2016). The adapted Envs apparently sample conformations similar to State 2 more readily than the parental HIV-1JR-FL Env. We observed no significant difference in the inhibition of viruses containing the parental HIV-1JR-FL and adapted Envs by the broadly neutralizing antibodies VRC01, PGT121, and 35O22.
Table 2.
Inhibition of viruses with wild-type and mutant HIV-1JR-FL Envs. Recombinant, luciferase-expressing viruses with wild-type or mutant HIV-1JR-FL Envs were incubated with sCD4, small- molecule entry inhibitors or antibodies for one hour at room temperature. The virus-inhibitor mixtures were then incubated with Cf2Th-CD4/CCR5 cells for 2 days prior to cell lysis and measurement of luciferase activity. Viral infection was plotted as a percentage of the relative luciferase activity observed in the absence of inhibitor. The concentration of inhibitors required to inhibit virus infection by 50% (IC50) is reported. The IC50 values for all of the antibodies are in μg/mL. The values shown are means and standard deviations from one or more sets of duplicate samples in typical experiment. N/A – not applicable.
| IC50
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inhibitor | Binding Site | WT JR-FL |
J3 | J9 | J12 | ΔV1V2 | S115N | R564H | E662K | S115N S164N |
S115N R564H |
S115N E662K |
R564H E662K |
| sCD4 (in μg/mL) | CD4 | 3.7±0.6 | 1.3±0.1 | 1.0±0.1 | 1.6±0.2 | >100 | 0.9±0.2 | ||||||
| BMS-806 (in nM) | β20–β21 compound | 3.0±.7 | 3.9±0.6 | 7.5±2.2 | 4.1±0.6 | >100 | 9.2±2.8 | 6.0±2.6 | 3.5±0.7 | 28.5±5.0 | 5.4±1.3 | 21.1±7.1 | 2.3±0.2 |
| DMJ-I-228 (in uM) | CD4BS compound | 43±7.0 | 12±2.8 | 13±4.1 | 2.0±0.5 | 9.1±1.0 | |||||||
| JP-III-48 (in uM) | CD4BS compound | 33.9±10.5 | 7.7±1.8 | 9.5±2.0 | 7.0±1.6 | 1.3±0.2 | |||||||
| VRC01 | CD4BS | 0.6±0.1 | 0.6±0.2 | 0.7±0.1 | 0.7±0.2 | 15.9±7.9 | 0.9±0.2 | 0.4±0.1 | 0.6±0.1 | 0.7±0.2 | 0.6±0.1 | 0.9±0.2 | 0.8±0.2 |
| F105 | CD4BS | >100 | 8.3±1.7 | 4.6±0.8 | 8.7±2.5 | 7.7±4.3 | 35.1±14.5 | >100 | >100 | 22.8±5.6 | >100 | 5.5±1.6 | >50 |
| 17b | CD4i | >100 | 16.4±4.3 | 16.1±3.7 | 28.0±8.5 | 6.8±8.3 | >100 | >100 | >100 | >50 | >50 | >100 | >100 |
| 830A | V2 | >50 | 6.1±2.8 | 2.4±1.2 | 0.6±0.3 | N/A | |||||||
| 902090 | V2 | >100 | 34±14 | >50 | >100 | >100 | |||||||
| 19b | V3 | >50 | 13.7±2.4 | 5.4±1.0 | 5.1±+1.4 | 0.03±0.04 | 21.1±5.4 | >100 | >100 | >50 | 40.6±15.6 | 5.6±1.1 | >50 |
| 1.4E | V3 | >50 | 4.0±1.2 | 4.9±1.0 | 2.7±0.6 | 8.3±10.6 | |||||||
| PGT121 | V3 Glycan | 2.6±0.4 | 1.3±0.1 | 3.2±0.7 | 1.8±0.3 | 25.1±49.8 | |||||||
| 35O22 | gp120-gp41 | 3.2±1.7 | 7.7±3.9 | 6.9±3.6 | 3.1±1.6 | 0.05±0.02 | |||||||
To identify the specific Env changes responsible for this phenotype, we assayed the sensitivity of single and double Env mutants to VRC01, F105, 17b, and 19b. The mutants R564H, E662K, and R564H/E662K exhibited a neutralization profile similar to that of the parental HIV-1JR-FL virus (Fig. 8A, Table 2). The S115N mutant was more sensitive to F105 and 19b neutralization than the wild-type HIV-1JR-FL virus, although not as sensitive as the viruses with the adapted Envs. The virus with the S115N and E662K changes was as sensitive as the viruses with the J3, J9, and J12 Envs to neutralization by F105 and 19b. These results indicate that the S115N change makes a major contribution to the sampling of State 2-like conformations, in which the CD4-binding site and V3 region of gp120 is more exposed (Herschhorn et al., 2016). Other changes, like E662K in gp41, contribute to the degree of this phenotype. Apparently, multiple Env changes in the adapted viruses result in greater sampling of a State 2-like conformation with increased exposure of two epitopes (V3 and CD4-induced) near the CCR5-binding region.
Fig. 8.
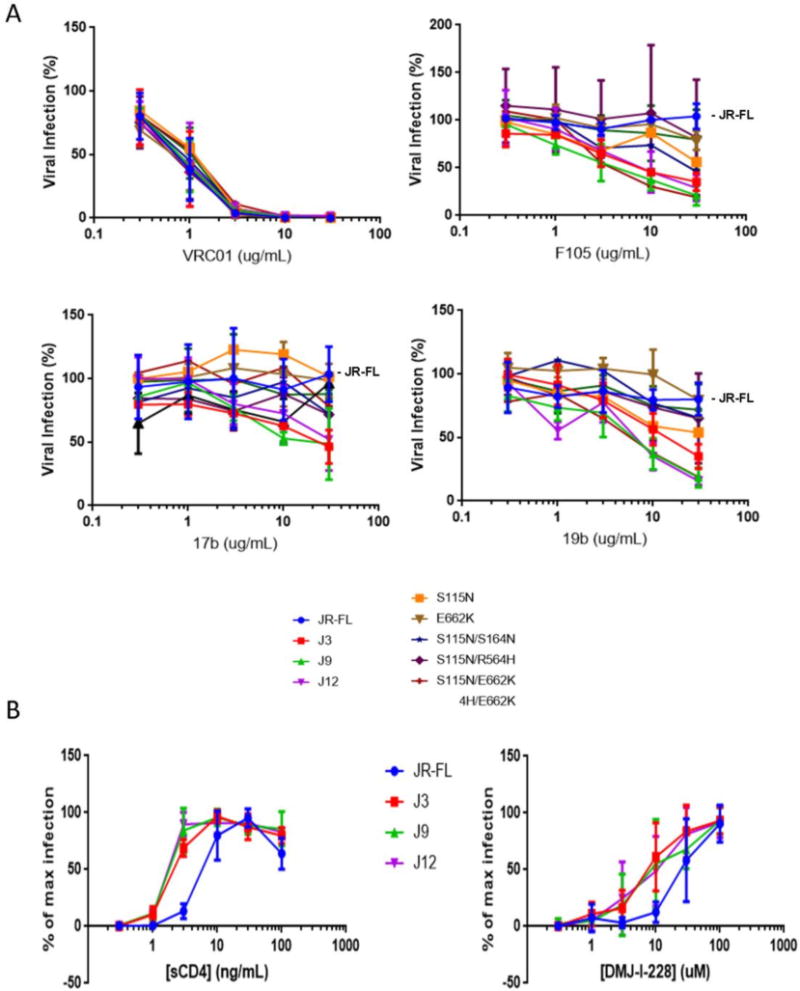
Sensitivity of viruses with wild-type and variant HIV-1JR-FL Envs to neutralization by antibodies and activation by CD4-mimetic molecules. (A) Recombinant, luciferase-expressing viruses with the wild-type HIV-1JR-FL Env or variant Envs with adaptation-associated changes were incubated with antibody at room temperature. The virus-antibody mixtures were then incubated with Cf2Th-CD4/CCR5 cells for 2 days prior to cell lysis and measurement of luciferase activity. Viral infection is shown as a percentage of the luciferase activity observed in the absence of antibody. The means and standard deviations from duplicate samples in a typical experiment are shown. (B) Recombinant viruses with the wild-type HIV-1JR-FL Env or the adapted virus Envs were incubated with CD4-negative Cf2Th-CCR5 cells in the presence of the indicated concentrations of sCD4 or the CD4-mimetic compound DMJ-I-228. Luciferase activity was measured in the cells two days later and is reported as the percentage of the maximum luciferase activity observed for each virus variant.
The neutralization assays with sCD4 and small-molecule CD4-mimetic compounds suggested that the adapted Envs might be slightly more susceptible to the induction of conformational changes by these ligands. To test this hypothesis, the activation of infection of CD4-negative Cf2Th-CCR5 cells by sCD4 and two CD4-mimetic compounds was evaluated for viruses with the adapted and parental HIV-1JR-FL Envs (Herschhorn et al., 2016; Madani et al., 2016). The infection of Cf2Th-CCR5 cells by the viruses with J3, J9 and J12 Envs was activated at 2-3-fold lower concentrations of sCD4, JP-III-48 and DMJ-I-228 than the wild-type HIV-1JR-FL infection (Fig. 8B and data not shown). These results are consistent with a slight increase in the ability of the adapted viruses to be triggered by CD4.
Effect of the N302Y change on the HIV-1JR-FL low-R5 replication phenotype
The adaptation of HIV-1 to infect cells expressing low levels of CCR5 has been recently reported (Garg et al., 2016). In this system, SupT1 T lymphocytes (L23 cells) stably expressing low levels of human CCR5 were infected with HIV-1YU2, followed by passage for 70 days. The resulting virus contained an N302Y change in the gp120 V3 region that enhanced virus replication in the L23 cells and conferred 5-fold resistance to Maraviroc.
We introduced the N302Y change into the wild-type and J9 mutant Envs in the HIV-1NL4.3(JR-FL) provirus to determine whether the V3 change would enhance replication in R5-Low cells. The N302Y change did not enhance the replication of HIV-1NL4.3(JR-FL) (Fig. 9). We observed no significant improvement in the replication of the J9/N302Y virus in R5-Low cells, compared with that of the J9 virus. The replication of the J9/N302Y virus in Cf2Th-CD4/CCR5 cells was attenuated relative to that of the J9 virus. These results indicate that the N302Y change is not sufficient to confer the ability to replicate efficiently on cells with low CCR5 to HIV-1NL4.3(JR-FL).
Fig. 9.
Replication kinetics of viruses with the wild-type HIV-1JR-FL Env or mutant Envs. Cells were transfected with NL4.3 proviruses with the wild-type HIV-1JR-FL Env or the indicated variant Env, and passaged for 15 days. A 32P RT assay was performed on medium removed at each passage. Each point represents an average of duplicate samples from a representative replication kinetics assay. The dashed line represents the average reverse transcriptase activity in supernatants of CD4-negative, CCR5-negative Cf2Th cells incubated with each virus.
Introduction of adaptation-associated changes into HIV-1AD8
The R564H change in the HIV-1JR-FL Env contributed to the replication of the virus in cells with low levels of CCR5. HIV-1AD8 and 92.7 percent of all HIV-1 strains have a histidine residue at position 564. Since the wild-type HIV-1AD8 Env already has a histidine at position 564, we hypothesized that the addition of the other single-residue changes that arose in the adapted HIV-1JR-FL Env would allow HIV-1AD8 to infect cells expressing low CCR5 levels. The addition of these single-residue changes to the Env of the HIV-1NL4.3(AD8) provirus resulted in a virus that did not detectably replicate in Cf2Th-CD4/CCR5 or R5-Low cells (data not shown). Introduction of S115N in single-cycle recombinant HIV-1AD8 with the AD8 Env resulted in increased infectivity in Cf2Th-CD4/CCR5 cells and an increased sensitivity to the 17b and 19b antibodies (Fig. 10). Apparently, some but not all of the phenotypes resulting from the adaptation-associated changes in the HIV-1JR-FL Env can be reproduced in the context of the HIV-1AD8 Env. The adaptation-associated changes may contribute to the ability of a subset of naturally occurring HIV-1 variants to infect cells with different levels of CCR5.
Fig. 10.
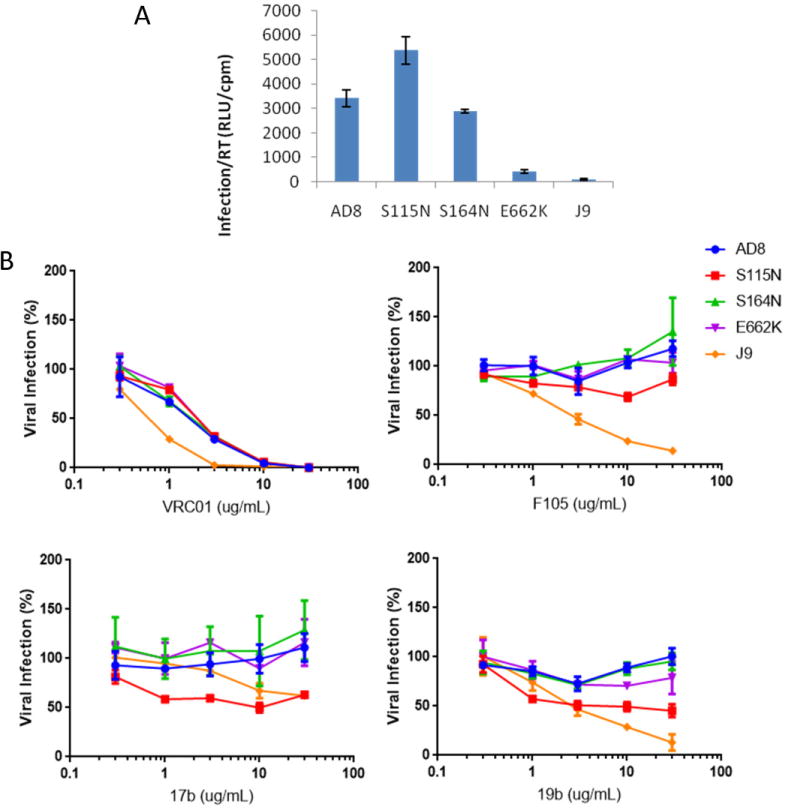
Sensitivity of viruses with the wild-type HIV-1AD8 Env or mutant Envs to antibody neutralization. (A) Recombinant single-round luciferase-expressing viruses with the wild-type HIV-1AD8 Env or mutant Envs were incubated with Cf2Th-CD4/CCR5 cells for 2 days. For comparison, the infectivity of recombinant luciferase-expressing virus containing the HIV-1JR-FL J9 mutant Env is shown. The infectivity is expressed as the ratio of relative luciferase units (RLU) of infected cells normalized to the reverse transcriptase activity (cpm). (B) The recombinant, luciferase-expressing viruses with the indicated HIV-1AD8 Env variants (or the HIV-1JR-FL J9 mutant Env) were incubated with antibody prior to addition of the virus-antibody mixture to Cf2Th-CD4/CCR5 cells. Viral infection is measured as a percentage of the luciferase activity observed in the absence of antibody. Shown are means and standard deviations from duplicate samples in a typical experiment.
Discussion
Although some primary human immunodeficiency viruses can utilize low levels of CCR5 to enter cells (Sterjovski et al., 2010), there are no reports of coreceptor-independent HIV-1 in the literature. In this work, by extensive passaging of HIV-1NL4.3(JR-FL), a virus that can efficiently use modest levels of CCR5 for entry into host cells, we obtained virus variants that could detectably replicate in cells with less than ~1300 CCR5 molecules on the surface. Additional passaging of the adapted virus failed to generate viruses capable of replicating on cells with lower or no CCR5 expression. This outcome contrasts with the multiple successes in generating CD4-independent HIV-1 variants (Kolchinsky et al., 1999; Edwards et al., 2001; Dumonceaux et al., 1998; Zhang et al., 2002). The stringent requirement for CCR5, CXCR4 or related chemokine receptors is consistent with the notion that these coreceptors likely served as the primary receptor for primordial lentiviruses (Willett et al., 1998; Poeschla and Looney, 1998; Dealwis et al., 1998). In this scenario, viruses evolved to bind CD4 as a means of forming and exposing the coreceptor-binding site. Therefore, in State 1, the highly conserved coreceptor-binding site on gp120 is unavailable to host antibodies. When Env binding to target cell CD4 exposes the coreceptor-binding site, steric factors limit the access of host antibodies to this element (Labrijn et al., 2003). Thus, the use of two receptors provides significant advantages for lentiviruses that establish persistent infections in the host.
The mechanistic contributions of CCR5 binding to the HIV-1 entry process are incompletely understood. Inferences about the structural influence of CCR5 on Env have centered on the physical interactions of CCR5 with gp120. Crystal structures of gp120 cores bound to sCD4 and 17b Fab revealed a highly conserved gp120 surface element composed of the bridging sheet and V3 base and tip that is thought to interact with the N-terminus and second extracellular loop of CCR5 (Kwong et al., 1998; Rizzuto et al., 1998; Wyatt et al., 1998). The interaction of this gp120 element with CCR5 serves to bring the CD4-bound Env trimer close to the host cell membrane. In addition to this attachment function, CCR5 binding serves to orient the Env spike. Mixing studies of HIV-1 Env mutants have suggested that at least two gp120 subunits in the Env trimer must engage CCR5 to allow virus entry (Yang et al., 2006; Salzwedel et al., 2009). Analogous to the events that occur after CD4 binding, CCR5 binding has been proposed to trigger additional conformational changes in Env that drive the formation of the gp41 six-helix bundle. How gp120-CCR5 binding leads to conformational changes in gp41 is still a matter of speculation. Presumably, CCR5-induced triggering of Env function involves a release of restraints that allows the gp41 to refold into a highly stable six-helix bundle.
Insights into the interaction of HIV-1 Env with CCR5 have been obtained by generating HIV-1 variants that escape from inhibitors of CCR5 binding. In these cases, the virus does not switch tropism, but rather adapts to use the inhibitor-bound CCR5 as a coreceptor. Adaptation of HIV-1D1/85.16 to replicate in the presence of maraviroc involved changes in the gp120 V3 region that influence CCR5 binding, as well as changes in the gp41 fusion peptide (G516V, M518V and F519I) that enhance viral membrane fusion with the target cell membrane (Anastassopoulou et al., 2012). HIV-1JR-CSF and HIV-111-121 adapted readily to escape the inhibitory effects of the 2D7 antibody against the second extracellular loop of CCR5, with the resistant viruses exhibiting a change (D167N) in the gp120 V2 region (Aarons et al., 2001). These studies indicate that HIV-1 can adapt to an inhibitor-bound CCR5 by making changes within as well as outside the V3 region.
HIV-1 has also been adapted to replicate in cells that express low levels of CCR5. HIV-1YU2 was adapted to replicate in SupT1 cells expressing a low level of CCR5 from a transfected gene (Garg et al., 2016). The adapted virus continued to use CCR5 as a coreceptor, and exhibited changes in V3 (N302Y), which made a large contribution to the phenotype, and in V2 (E172K), which added to the N302Y phenotype. The N302Y and N302Y/E172K viruses were ~5-fold more resistant to maraviroc than the parental HIV-1YU2. HIV-1KP-5 adapted to replicate in PM1 cells expressing low CCR5 levels without a switch in coreceptors (Yoshimura et al., 2014). Changes in V3 (D321E) as well as outside of V3 (D141N in V1 and I463T in V5) were associated with the adaptation. The adapted viruses were ~10-fold more resistant to maraviroc than the parental HIV-1KP-5, and exhibited increased sensitivity to a CD4-induced antibody and a slight increase in sensitivity to b12, a CD4-binding site antibody. The adapted virus was as sensitive to neutralization by a V3-directed antibody as the parental virus. These two studies suggest that one adaptive approach to low CCR5 levels is to increase CCR5-binding affinity through V3 changes, with auxiliary changes in the gp120 V1/V2 region. The gp120 V1/V2 region has been suggested to mask the coreceptor-binding site in primary Envs in State 1 (Wyatt et al., 1993; Kolchinsky et al., 2001b; Binley et al., 1998). Changes in the V1/V2 region can lead to increased Env transitions to State 2 (Herschhorn et al., 2016).
Our study generated HIV-1JR-FL variants that replicated in Cf2Th-CD4/CCR5 cells with ~1300 CCR5 molecules per cell. As seen in the Garg et al. and Yoshimura et al. studies, the adapted virus did not switch coreceptors. In contrast to the outcomes of these earlier studies, the adapted HIV-1JR-FL exhibited no V3 changes and did not exhibit altered sensitivity to maraviroc; we found no evidence for an increase in the affinity of the adapted virus gp120 for CCR5. In fact, Env changes in gp41 (R564H or E662K) were essential for the adapted virus’ ability to replicate on cells with low CCR5 levels. The adapted viruses exhibited an increased sensitivity to neutralization by F105 (a CD4-binding site antibody), 17b (a CD4-induced antibody) and 19b (a V3 antibody); thus, the adapted viruses are more prone to expose normally cryptic epitopes near the receptor-binding regions. Compared with the parental HIV-1JR-FL, the adapted viruses were slightly more sensitive to neutralization by sCD4 and small-molecule CD4-mimetic compounds; consistent with this observation, the activation of infection of CD4-negative CCR5-positive cells by sCD4 and CD4-mimetic compounds was slightly more efficient for the adapted viruses than for wild-type HIV-1JR-FL. The adapted viruses did not appreciably differ from the parental virus in T20 sensitivity.
Mechanistic insights into the HIV-1JR-FL adaptation to low-CCR5 utilization were obtained by assessing the contribution of Env changes, both individually and in combination, to this phenotype. The molecularly cloned J3 virus with three Env changes (S115N, R564H and E662K) replicated in low-CCR5 cells, demonstrating the sufficiency of these three changes to account for this phenotype. Two combinations, S115N + E662K and R564H + E662K, also allowed HIV-1JR-FL to replicate in cells with low CCR5 expression. The E662K change alone was insufficient to allow virus replication in low-CCR5 cells, indicating the importance of the S115N and R564H changes to the phenotype. Of interest, the S115N + E662K and R564H + E662K Envs differed in a number of ways, suggesting that distinct, parallel pathways of replication in low-CCR5 cells can be utilized by HIV-1JR-FL. In the first pathway, exemplified by the S115N + E662K virus, the activation barriers separating State 1 from downstream Env conformations are apparently lowered. These Envs are more prone to opening receptor-binding gp120 Env regions, as evidenced by the increased susceptibility to sCD4, CD4-mimetic compounds and antibodies. An expected consequence of these Env changes is an increase in the amount of the CD4-bound Env intermediate (State 3) present in the virus-target cell synapse. Thus, an increased concentration of coreceptor-binding-competent Envs is available to utilize low CCR5 levels efficiently. In the second pathway, exemplified by the R564H + E662K virus, the Env does not exhibit phenotypes associated with a more “open” conformation. Rather than increasing the overall amount of State 3 Env potentially available for CCR5 binding or increasing Env-CCR5 binding affinity, these gp41 changes apparently affect the responsiveness of Env to CCR5 binding.
What might account for the different strategies used by HIV-1 to adapt to low CCR5 levels in our study and in previous studies, where Envs with increased affinity for CCR5 were selected (Garg et al., 2016; Yoshimura et al., 2014)? One possibility is the nature of the starting virus. The HIV-1YU2 used by Garg and colleagues is more readily triggered by CD4 and CD4-mimetic compounds than HIV-1JR-FL (Madani et al., 2017), so the latter virus’ infectivity in low-CCR5 cells could benefit more from an increase in CD4 responsiveness. Another explanation relates to the cells used for virus adaptation. The Cf2Th-CD4/CCR5 cells used in our experiments are adherent and thus allow significant cell-cell transmission to occur as a result of cellular contact. Both Garg et al. and Yoshimura et al. used lymphocyte target cells grown in suspension, where cell-free virus transmission may be the predominant mode of infection. Optimizing Env binding to scarce CCR5 may be more important in increasing the efficiency of encounters between cell-free virions and target cells. In adherent cells, the budding virions have a greater opportunity to interact with target cells regardless of CCR5 levels; the rate-limiting factor in this case may be the efficiency with which each Env encounter with CCR5 actually triggers functional membrane fusion events leading to infection.
The gp120 and gp41 changes responsible for HIV-1JR-FL adaptation to low-CCR5 cells potentially involve dynamic regions of Env involved in receptor-induced conformational changes. Structural explanations for the effects of these changes are complicated by the possibility that the different observed Env changes may operate at distinct stages of the HIV-1 entry process. Given the considerable gaps in our structural information on the different stages of HIV-1 entry, our interpretation of the Env determinants of low-CCR5 utilization must be considered tentative. With that caveat, we examined the location of these determinants in available HIV-1 Env structures. The S115N change contributed to the increased sensitivity of the adapted viruses to inhibition by antibodies directed against the receptor-binding sites of gp120. Ser 115 is located at the carboxy-terminal end of the α1 helix of gp120 (Kwong et al., 1998); based on current Env structures, any consequences of the S115N change on neutralization sensitivity would be mediated by indirect mechanisms. Although Ser 164 is predicted to make interprotomeric gp120 contacts in structures of the HIV-1BG505 sgp140 SOSIP.664 Env trimer (Julien et al., 2013; Lyumkis et al, 2013; Pancera et al., 2014), we found that the S164N change is not essential for the ability of the adapted HIV-1JR-FL to use low levels of CCR5. Another study failed to observe the viral phenotypes predicted by the sgp140 SOSIP.664 Env trimer structure for changes in this interprotomer region (Madani et al., 2016), adding to uncertainty about the relationship of this structure to functional Env conformations (Alsahafi et al., 2015; Kesavardhana and Varadarajan, 2014; Pacheco et al., 2017). The gp41 residue Arg 564 faces the amino-terminal end of the gp120 α1 helix in the structure of the HIV-1JR-FL Env trimer bound to the PGT151 neutralizing antibody (Lee et al., 2016). Therefore, alteration of Arg 564 could potentially influence gp120-gp41 interaction and the triggering of Env conformational changes by CCR5 binding. Because the membrane-proximal region of gp41 is either missing or disordered in current Env structures (Julien et al., 2013; Lyumkis et al., 2013; Pancera et al., 2014), the consequences of the E662K change on HIV-1 Env structure are not interpretable. A full understanding of the mechanistic basis for the low-CCR5 replication phenotype awaits additional structural information on the functional Env conformations.
Natural variation in the ability of HIV-1 to use different levels of target cell CCR5 has been suggested to influence viral tropism and sensitivity to inhibitors (Etemad et al., 2009; Gorry et al., 2002; Karlsson et al., 2004; Koning et al., 2003; Pfaff et al., 2010; Repits et al, 2005; Taylor et al., 2008). Understanding the mechanisms whereby HIV-1 modulates CCR5 requirements will assist intervention efforts.
Conclusion
Adaptation of HIV-1NL4.3(JR-FL) to replicate on CD4-positive cells expressing low levels of CCR5 has revealed residues in gp120 and gp41 responsible for this phenotype. The Env changes do not apparently increase gp120 affinity for CCR5, but promote two parallel pathways of adaptation: 1) increased propensity of Env to assume a more open coreceptor binding-competent conformation; and 2) increased Env responsiveness to CCR5 binding.
Materials and Methods
Generation of cell lines
293T and Cf2Th cells were obtained from the American Type Culture Collection and grown in Dulbecco’s modified Eagle’s medium with 10% tetracycline-free fetal bovine serum (DMEM-10, Clontech). Cf2Th cell lines stably expressing human CD4 and CCR5 (Cf2Th-CD4-R5) were grown in DMEM-10 in the presence of 400 μg/mL G418 and 200 μg/mL hygromycin (Invitrogen).
Cf2Th cell lines with regulatable CCR5 expression were generated in the following manner: Cf2Th cells were transfected with Tet-On® Advanced Vector (Clontech), passaged in DMEM-10 and 0.6 ug/mL puromycin, and single cells selected by limiting dilution in 96-well plates. Single-cell clones were expanded and tested for expression of the tTA protein after treatment with 0–1 ug/mL doxycyline by Western blotting of whole cell lysates with a monoclonal antibody against TetR (Clontech). tTA-expressing cells were transfected with pGL422-tetO-CCR5, passaged in the presence of 0.6 μg/mL G418, and selected for single cells. Cells were expanded and tested for doxycycline-regulated CCR5 expression via flow cytometry as follows: after incubation with R-Phycoerythrin-conjugated mouse anti-human CCR5 (PE-anti-CD195, BD Biosciences), ~1 × 106 cells were analyzed with a BD FACSCanto II flow cytometer (BD Biosciences). Clones with the least background and greatest dynamic range of induced CCR5 expression were then transfected with the pcDNA-CD4 plasmid expressing human CD4, passaged in the presence of 0.025 μg/mL zeocin, and cloned. Cells were tested for doxycycline regulation of CCR5 expression and stable expression of CD4 using flow cytometry with PE-anti-CD195 and fluorescein isothiocyanate-conjugated mouse anti-human CD4, clone RPA-T4 (FITC-anti-CD4, BD Biosciences), respectively.
Two clones that express high levels of CD4 and low or high ranges of cell-surface CCR5 expression upon doxycycline treatment, herein called R5-Low and R5-High, were selected for HIV-1 adaptation to low levels of CCR5 (Fig. 1A). Levels of CCR5 were measured by QuantiBritePE (Fig. 1B, BD Biosciences) and vary within a physiological range (Fig. 1C).
Generation of replication-competent HIV-1 and adaptation of virus to low levels of CCR5 in R5-Low cells
Replication-competent HIV-1 was generated by transfecting 2 million 293T cells with 20 μg of a plasmid containing the pNL4.3 provirus with the HIV-1JR-FL env (between the SalI and BamHI sites) using Effectene transfection reagent (Qiagen). The supernatant was harvested after two days and frozen in aliquots. Reverse transcriptase (RT) activity in the supernatant was measured using 3H-labelled nucleotide triphosphates for initial viral production assays and 32P-labelled nucleotide triphosphates for all viral adaptation assays, by a previously described method (Rho et al., 1981). To produce the virus in the Cf2Th cell line, 100,000 Cf2-T4R5 cells were infected with 3000 cpm (3H) of HIV-1NL4.3(JR-FL) virus made in 293T cells as described above. Cells were passaged every 3–4 days by lifting them from the plate using 5 mM EDTA in PBS and diluting them 1:5. Supernatants were collected at each passage to measure RT. Additional studies of virus replication in Cf2Th-CD4/CCR5 cells used 6600 cpm (32P) of virus from the time point with peak RT in the presence of 2 μg/mL polybrene.
For all subsequent rounds of adaptation, 25,500 cpm (32P) RT units of supernatant, collected at the time point with peak RT activity, was used to infect R5-High cells and then R5-Low cells at decreasing expression levels of CCR5 (i.e., lower concentrations of doxycycline). Serial passage of the virus was continued until three independent assays with triplicate samples containing cells expressing the lowest amount of CCR5 yielded no detectable RT activity.
Quantification of p24 levels in cell supernatants was performed using a p24 ELISA kit (Advanced BioScience Laboratories).
Sequencing env from genomic DNA of infected cells
Proviruses were sequenced from the genomic DNA of infected cells. Genomic DNA was isolated from cells frozen at peak RT using the GIAamp DNA blood minikit (Qiagen) followed by genome amplification using a published protocol (Gall et al., 2012). In summary, the HIV-1 genome was PCR-amplified by primers SK145 and OFM19 using the PrimeSTAR GXL DNA polymerase (Clontech). The viral env was then amplified from the PCR reaction using the Pan-HIV-1_4 forward and reverse primers. PCR fragments were purified using the QIAquick PCR Purification kit (Qiagen) and sequenced by the Sanger method.
Env cloning and mutagenesis
Changes in the HIV-1JR-FL env that arose during passage of the virus were introduced into the pNL4.3(JR-FL) proviral DNA or the Env expressor plasmid pSVIIIenv(JR-FL) by site-directed mutagenesis using the PfuUltra II Hotstart PCR Master Mix (Agilent). Mutagenesis was confirmed by automated DNA sequencing.
Gp120-CCR5 binding assay
293T cells were transfected with pSVIIIenv (JR-FL) plasmids using Qiagen Effectene and supernatants were harvested after 2 days. Approximately 0.5 ml of supernatant was incubated with 30 ng/mL sCD4 with or without 1uM Maraviroc for 30 minutes at 37 degrees. Two T-175 flasks of confluent Cf2Th-CCR5 cells were lifted using 5 mM EDTA, spun down and resuspended in 20 mL DMEM-10. One ml of the Cf2Th-CCR5 cell suspension was incubated with the gp120-containing supernatants for 1 hour at 37°C. Cells were washed twice with DMEM-10 and lysed in 500 μL 10 mM Tris pH 7.5, 0.5 M NaCl, 5% Igepal. Cell lysates were spun at 14,000 rpm for 30 minutes at 4°C and the supernatants were incubated on a rotating platform overnight with 4 μL serum from HIV-1-infected individuals and 80 μL 1:1 resuspended Protein A-Sepharose beads. Beads were washed twice with 10 mM Tris pH 7.5, 0.5 M NaCl, 5% Igepal and then washed once with 10 mM Tris pH 7.5, 1.5 mM NaCl. Proteins were eluted by boiling beads in 30 uL 4x NuPAGE LDS Sample Buffer plus ß-mercaptoethanol at 100°C. Samples were run on SDS-polyacrylamide gels, transferred to Hybond ECL nitrocellulose membranes (GE Healthcare Life Sciences) using a Trans-blot semi-dry transfer cell (Bio-rad), and blotted with 1:200 anti-gp120 antibody-HRP (Abcam). Blots were developed with SuperSignal West Femto Maximum Sensitivity Substrate (Thermo Fisher) and imaged on the GelDoc XR+ System (Bio-rad).
Viral replication assay
To test the replication capacity of NL4.3 viruses expressing wild-type HIV-1JR-FL Env or the adapted virus Envs, we introduced mutations into the HIV-1NL4.3(JR-FL) proviral DNA and transfected them into target cells. Site-directed mutagenesis was performed using the QuikChange II XL Site-Directed Mutagenesis protocol (Agilent) and the PfuUltra Hotstart DNA Polymerase (Agilent). Approximately 4×104 Cf2Th-CD4/CCR5 or R5-Low cells preincubated with 50 or 100 ng/mL doxycycline were transfected with 100 μg proviral DNA and passaged for 3 weeks. Supernatants of each cell sample were collected regularly throughout the culture period and evaluated for RT activity.
Generation and purification of single-round recombinant viruses expressing luciferase
Single-round recombinant HIV-1 expressing firefly luciferase was generated by transfecting 293T cells with pSVIIIenv(JR-FL) constructs, pLuciferase, and the pCMVΔP1ΔenvpA HIV-1 Gag-Pol packaging construct at a ratio of 1:2:1 micrograms of DNA using Effectene transfection reagent. The virus-containing supernatant was harvested after 3 days and used in all assays without freezing.
To test viral infectivity, virus-containing supernatants were incubated with target cells in 96-well plates for three days in a 37°C CO2 incubator. The activation of HIV-1 infection of CD4-negative Cf2Th-CCR5 cells by sCD4 or CD4-mimetic compounds was assessed as described (Madani et al., 2016). Cells were lysed with 30 μL passive lysis buffer (Promega) and luciferase activity was measured with a Mithras LB 940 luminometer (Berthold Technologies).
To test levels of Env expression on virions, viral particles were pelleted by ultracentrifugation through a 20-percent sucrose cushion at 4°C for 2 hours in a Beckman SW55 rotor at 30,000 rpm. Pellets were lysed in 4x NuPAGE LDS Sample Buffer plus ß-mercaptoethanol and frozen. Samples were run on SDS-polyacrylamide gels, transferred to Hybond ECL nitrocellulose membranes (GE Healthcare Life Sciences) using a Trans-blot semi-dry transfer cell (Bio-rad), and blotted with a 1:200 dilution of an anti-HIV-1 gp120 antibody-HRP. Blots were developed with SuperSignal West Femto Maximum Sensitivity Substrate (Thermo Fisher) and imaged on the GelDoc XR+ System (Bio-rad). Membranes were stripped with Western Blot Stripping Buffer (Thermo Fisher) and then blotted with a 1:2000 dilution of anti-HIV-1 p55 + p24 + p17 antibody (Abcam) and secondary HRP-Protein A/G, redeveloped and imaged.
Cell fusion assays
To test the capacity of wild-type HIV-1JR-FL Env and the adapted virus Envs to initiate cell fusion (syncytium formation), we used an alpha complementation assay (Holland 2004). In this assay, COS-1 cells were plated in a 96-well plate and transfected the next day with 0.1 μg/well pSVIIIenv(JR-FL), 0.01 μg/well pTat, and 1.1 μg/well of a plasmid containing the N-terminal fragment of beta-galactosidase, using the Effectene protocol. Cf2Th-CD4/CCR5 cells were plated in a T-75 flask and transfected with 10 μg of a plasmid containing the C-terminal fragment of β-galactosidase using the Effectene protocol. After 2 days of incubation at 37°C, Cf2Th-CD4/CCR5 cells were lifted with 5 mM EDTA in PBS and diluted to 2×105 cells per mL DMEM-10. To each well of COS-1 cells preincubated with increasing concentrations of Maraviroc was added 100 μL Cf2Th-CD4/CCR5 cells. Cells were incubated at 37°C for 8 hours, washed in PBS, and lysed with 20 μL Galactostar Lysis Buffer (ThermoFisher). Plates were frozen and thawed three times at −20°C to improve cell lysis. Plates were then warmed to room temperature and incubated with 100 μL 1:100 Galactostar substrate in Reaction Buffer Diluent. β-galactosidase enzymatic activity was measured in the luminometer, reading 1 second per well.
Cell-to-cell HIV-1 transmission assay
293T cells producing single-round luciferase recombinant virus were lifted with 5 mM EDTA in PBS and added to cultured Cf2Th-CD4/CCR5 cells. Cocultures were passaged every 3–4 days. At passaging, the remaining cells were diluted in DMEM-10 on a 96-well plate and incubated overnight. At various time points, cells were lysed with 30 μL passive lysis buffer (Promega) and luciferase activity was measured with a Mithras LB 940 luminometer (Berthold Technologies).
Neutralization assays
Single-round luciferase-expressing recombinant viruses were incubated with antibodies for 1 hour at room temperature and then incubated with Cf2Th-CD4/CCR5 cells in a 96-well plate for 2 hours at 37°C. The virus and antibody mixtures were incubated with the cells in DMEM-10 for 3 days in a 37°C CO2 incubator. Cells were lysed with 30 μL passive lysis buffer (Promega) and luciferase activity was measured with a Mithras LB 940 luminometer (Berthold Technologies).
Data representation and statistical analysis
Microsoft Excel and Prism 6.0 (GraphPad Software, L1 Jolla CA) was used to graph and analyze numerical data. Statistical tests as reported in the figure legends were performed using Prism software.
Research Highlights.
HIV-1 can adapt to CD4-positive cells expressing progressively lower levels of CCR5.
The adapted virus’ Env changes are located outside of the gp120 CCR5-binding region.
The gp120 of the adapted virus did not increase its affinity for CCR5.
The Env changes enhance HIV-1 replication at all levels of CCR5 expression.
The adapted virus Envs exhibit increased propensity to change conformation.
Acknowledgments
We thank Elizabeth Carpelan for manuscript preparation. We thank Vlad Novitsky for providing the protocol for proviral sequencing from genomic DNA. This study was supported by the National Institutes of Health (AI24982, GM56550 and AI100645) and the late William F. McCarty-Cooper. N.E. was supported by a predoctoral fellowship from the National Institutes of Health (AI112404).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aarons EJ, Beddows S, Willingham T, Wu L, Koup RA. Adaptation to blockade of human immunodeficiency virus type 1 entry imposed by the anti-CCR5 monoclonal antibody 2D7. Virology. 2001;287:382–390. doi: 10.1006/viro.2001.1046. [DOI] [PubMed] [Google Scholar]
- Agrawal-Gamse C, Lee FH, Haggarty B, Jordan AP, Yi Y, Lee B, Collman RG, Hoxie JA, Doms RW, Laakso MM. Adaptive mutations in a human immunodeficiency virus type 1 envelope protein with a truncated V3 loop restore function by improving interactions with CD4. J Virol. 2009;83:11005–11015. doi: 10.1128/JVI.01238-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhatib G, Combadiere C, Broder CC, Feng Y, Kennedy PE, Murphy PM, Berger EA. CC CKR5: a RANTES, MIP-1alpha, MIP-1beta receptor as a fusion cofactor for macrophage-tropic HIV-1. Science. 1996;272:1955–1958. doi: 10.1126/science.272.5270.1955. [DOI] [PubMed] [Google Scholar]
- Allers K, Hutter G, Hofmann J, Loddenkemper C, Rieger K, Thiel E, Schneider T. Evidence for the cure of HIV infection by CCR5Delta32/Delta32 stem cell transplantation. Blood. 2011;117:2791–2799. doi: 10.1182/blood-2010-09-309591. [DOI] [PubMed] [Google Scholar]
- Alsahafi N, Debbeche O, Sodroski J, Finzi A. Effects of the I559P gp41 change on the conformation and function of the human immunodeficiency virus (HIV-1) membrane envelope glycoprotein trimer. PLoS One. 2015;10:e0122111. doi: 10.1371/journal.pone.0122111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastassopoulou CG, Ketas TJ, Depetris RS, Thomas AM, Klasse PJ, Moore JP. Resistance of a human immunodeficiency virus type 1 isolate to a small molecule CCR5 inhibitor can involve sequence changes in both gp120 and gp41. Virology. 2011;413:47–59. doi: 10.1016/j.virol.2010.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastassopoulou CG, Ketas TJ, Klasse PJ, Moore JP. Resistance to CCR5 inhibitors caused by sequence changes in the fusion peptide of HIV-1 gp41. Proc Natl Acad Sci U S A. 2009;106:5318–5323. doi: 10.1073/pnas.0811713106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastassopoulou CG, Ketas TJ, Sanders RW, Klasse PJ, Moore JP. Effects of sequence changes in the HIV-1 gp41 fusion peptide on CCR5 inhibitor resistance. Virology. 2012;428:86–97. doi: 10.1016/j.virol.2012.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berro R, Klasse PJ, Jakobsen MR, Gorry PR, Moore JP, Sanders RW. V3 determinants of HIV-1 escape from the CCR5 inhibitors Maraviroc and Vicriviroc. Virology. 2012;427:158–165. doi: 10.1016/j.virol.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berro R, Klasse PJ, Lascano D, Flegler A, Nagashima KA, Sanders RW, Sakmar TP, Hope TJ, Moore JP. Multiple CCR5 conformations on the cell surface are used differentially by human immunodeficiency viruses resistant or sensitive to CCR5 inhibitors. J Virol. 2011;85:8227–8240. doi: 10.1128/JVI.00767-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binley JM, Wyatt R, Desjardins E, Kwong PD, Hendrickson W, Moore JP, Sodroski J. Analysis of the interaction of antibodies with a conserved enzymatically deglycosylated core of the HIV type 1 envelope glycoprotein 120. AIDS Res Hum Retroviruses. 1998;14:191–198. doi: 10.1089/aid.1998.14.191. [DOI] [PubMed] [Google Scholar]
- Chan DC, Fass D, Berger JM, Kim PS. Core structure of gp41 from the HIV envelope glycoprotein. Cell. 1997;89:263–273. doi: 10.1016/s0092-8674(00)80205-6. [DOI] [PubMed] [Google Scholar]
- Chan WE, Lin HH, Chen SS. Wild-type-like viral replication potential of human immunodeficiency virus type 1 envelope mutants lacking palmitoylation signals. J Virol. 2005;79:8374–8387. doi: 10.1128/JVI.79.13.8374-8387.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath PD, Wu L, Mackay CR, LaRosa G, Newman W, Gerard N, Gerard C, Sodroski J. The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996;85:1135–1148. doi: 10.1016/s0092-8674(00)81313-6. [DOI] [PubMed] [Google Scholar]
- Cocchi F, DeVico AL, Garzino-Demo A, Arya SK, Gallo RC, Lusso P. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- Dalgleish AG, Beverley PC, Clapham PR, Crawford DH, Greaves MF, Weiss RA. The CD4 (T4) antigen is an essential component of the receptor for the AIDS retrovirus. Nature. 1984;312:763–767. doi: 10.1038/312763a0. [DOI] [PubMed] [Google Scholar]
- Dealwis C, Fernandez EJ, Thompson DA, Simon RJ, Siani MA, Lolis E. Crystal structure of chemically synthesized [N33A] stromal cell-derived factor 1alpha, a potent ligand for the HIV-1 “fusin” coreceptor. Proc Natl Acad Sci U S A. 1998;95:6941–6946. doi: 10.1073/pnas.95.12.6941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, Di Marzio P, Marmon S, Sutton RE, Hill CM, Davis CB, Peiper SC, Schall TJ, Littman DR, Landau NR. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996;381:661–666. doi: 10.1038/381661a0. [DOI] [PubMed] [Google Scholar]
- Doranz BJ, Rucker J, Yi Y, Smyth RJ, Samson M, Peiper SC, Parmentier M, Collman RG, Doms RW. A dual-tropic primary HIV-1 isolate that uses fusin and the beta-chemokine receptors CKR-5, CKR-3, and CKR-2b as fusion cofactors. Cell. 1996;85:1149–1158. doi: 10.1016/s0092-8674(00)81314-8. [DOI] [PubMed] [Google Scholar]
- Dragic T, Litwin V, Allaway GP, Martin SR, Huang Y, Nagashima KA, Cayanan C, Maddon PJ, Koup RA, Moore JP, Paxton WA. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996;81:667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- Dumonceaux J, Nisole S, Chanel C, Quivet L, Amara A, Baleux F, Briand P, Hazan U. Spontaneous mutations in the env gene of the human immunodeficiency virus type 1 NDK isolate are associated with a CD4-independent entry phenotype. J Virol. 1998;72:512–519. doi: 10.1128/jvi.72.1.512-519.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumonceaux J, Goujon C, Joliot V, Briand P, Hazan U. Determination of essential amino acids involved in the CD4-independent tropism of the X4 human immunodeficiency virus type 1 m7NDK isolate: role of potential N glycosylations in the C2 and V3 regions of gp120. J Virol. 2001;75:5425–5428. doi: 10.1128/JVI.75.11.5425-5428.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards TG, Hoffman TL, Baribaud F, Wyss S, LaBranche CC, Romano J, Adkinson J, Sharron M, Hoxie JA, Doms RW. Relationships between CD4 independence, neutralization sensitivity, and exposure of a CD4-induced epitope in a human immunodeficiency virus type 1 envelope protein. J Virol. 2001;75:5230–5239. doi: 10.1128/JVI.75.11.5230-5239.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards TG, Wyss S, Reeves JD, Zolla-Pazner S, Hoxie JA, Doms RW, Baribaud F. Truncation of the cytoplasmic domain induces exposure of conserved regions in the ectodomain of human immunodeficiency virus type 1 envelope protein. J Virol. 2002;76:2683–2691. doi: 10.1128/JVI.76.6.2683-2691.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etemad B, Fellows A, Kwambana B, Kamat A, Feng Y, Lee S, Sagar M. Human immunodeficiency virus type 1 V1-to-V5 envelope variants from the chronic phase of infection use CCR5 and fuse more efficiently than those from early after infection. J Virol. 2009;83:9694–9708. doi: 10.1128/JVI.00925-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatkenheuer G, Pozniak AL, Johnson MA, Plettenberg A, Staszewski S, Hoepelman AI, Saag MS, Goebel FD, Rockstroh JK, Dezube BJ, Jenkins TM, Medhurst C, Sullivan JF, Ridgway C, Abel S, James IT, Youle M, van der Ryst E. Efficacy of short-term monotherapy with maraviroc, a new CCR5 antagonist, in patients infected with HIV-1. Nature medicine. 2005;11:1170–1172. doi: 10.1038/nm1319. [DOI] [PubMed] [Google Scholar]
- Feng Y, Broder CC, Kennedy PE, Berger EA. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272:872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- Freed EO, Myers DJ, Risser R. Characterization of the fusion domain of the human immunodeficiency virus type 1 envelope glycoprotein gp41. Proc Natl Acad Sci U S A. 1990;87:4650–4654. doi: 10.1073/pnas.87.12.4650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta RA, Wild CT, Weng Y, Weiss CD. Capture of an early fusion-active conformation of HIV-1 gp41. Nat Struct Biol. 1998;5:276–279. doi: 10.1038/nsb0498-276. [DOI] [PubMed] [Google Scholar]
- Gall A, Ferns B, Morris C, Watson S, Cotten M, Robinson M, Berry N, Pillay D, Kellam P. Universal amplification, next-generation sequencing, and assembly of HIV-1 genomes. J Clin Microbiol. 2012;50:3838–3844. doi: 10.1128/JCM.01516-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Perez J, Rueda P, Staropoli I, Kellenberger E, Alcami J, Arenzana-Seisdedos F, Lagane B. New insights into the mechanisms whereby low molecular weight CCR5 ligands inhibit HIV-1 infection. J Biol Chem. 2011;286:4978–4990. doi: 10.1074/jbc.M110.168955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg H, Lee RT, Maurer-Stroh S, Joshi A. HIV-1 adaptation to low levels of CCR5 results in V3 and V2 loop changes that increase envelope pathogenicity, CCR5 affinity and decrease susceptibility to Maraviroc. Virology. 2016;493:86–99. doi: 10.1016/j.virol.2016.03.010. [DOI] [PubMed] [Google Scholar]
- Gorry PR, Taylor J, Holm GH, Mehle A, Morgan T, Cayabyab M, Farzan M, Wang H, Bell JE, Kunstman K, Moore JP, Wolinsky SM, Gabuzda D. Increased CCR5 Affinity and Reduced CCR5/CD4 Dependence of a Neurovirulent Primary Human Immunodeficiency Virus Type 1 Isolate. Journal of Virology. 2002;76:6277–6292. doi: 10.1128/JVI.76.12.6277-6292.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haim H, Strack B, Kassa A, Madani N, Wang L, Courter JR, Princiotto A, McGee K, Pacheco B, Seaman MS, Smith AB, 3rd, Sodroski J. Contribution of intrinsic reactivity of the HIV-1 envelope glycoproteins to CD4-independent infection and global inhibitor sensitivity. PLoS Pathog. 2011;7:e1002101. doi: 10.1371/journal.ppat.1002101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y, Vassell R, Zaitseva M, Nguyen N, Yang Z, Weng Y, Weiss CD. Peptides trap the human immunodeficiency virus type 1 envelope glycoprotein fusion intermediate at two sites. J Virol. 2003;77:1666–1671. doi: 10.1128/JVI.77.3.1666-1671.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helseth E, Kowalski M, Gabuzda D, Olshevsky U, Haseltine WA, Sodroski J. Rapid complementation assays measuring replicative potential of HIV-1 envelope glycoprotein mutants. J Virol. 1990;64:2416–2420. doi: 10.1128/jvi.64.5.2416-2420.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herschhorn A, Ma X, Gu C, Ventura JD, Castillo-Menendez L, Melillo B, Terry DS, Smith AB, 3rd, Blanchard SC, Munro JB, Mothes W, Finzi A, Sodroski J. Release of gp120 Restraints Leads to an Entry-Competent Intermediate State of the HIV-1 Envelope Glycoproteins. mBio. 2016;7 doi: 10.1128/mBio.01598-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman TL, LaBranche CC, Zhang W, Canziani G, Robinson J, Chaiken I, Hoxie JA, Doms RW. Stable exposure of the coreceptor-binding site in a CD4-independent HIV-1 envelope protein. Proc Natl Acad Sci U S A. 1999;96:6359–6364. doi: 10.1073/pnas.96.11.6359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland AU, Munk C, Lucero GR, Nguyen LD, Landau NR. Alpha-complementation assay for HIV envelope glycoprotein-mediated fusion. Virology. 2004;319:343–352. doi: 10.1016/j.virol.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Hutter G, Nowak D, Mossner M, Ganepola S, Mussig A, Allers K, Schneider T, Hofmann J, Kucherer C, Blau O, Blau IW, Hofmann WK, Thiel E. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. The New England Journal of Medicine. 2009;360:692–698. doi: 10.1056/NEJMoa0802905. [DOI] [PubMed] [Google Scholar]
- Jiang X, Feyertag F, Meehan CJ, McCormack GP, Travers SA, Craig C, Westby M, Lewis M, Robertson DL. Characterizing the Diverse Mutational Pathways Associated with R5-Tropic Maraviroc Resistance: HIV-1 That Uses the Drug-Bound CCR5 Coreceptor. J Virol. 2015;89:11457–11472. doi: 10.1128/JVI.01384-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julien JP, Cupo A, Sok D, Stanfield RL, Lyumkis D, Deller MC, Klasse PJ, Burton DR, Sanders RW, Moore JP, Ward AB, Wilson IA. Crystal structure of a soluble cleaved HIV-1 envelope trimer. Science. 2013;342:1477–1483. doi: 10.1126/science.1245625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson I, Antonsson L, Shi Y, Oberg M, Karlsson A, Albert J, Olde B, Owman C, Jansson M, Fenyo EM. Coevolution of RANTES sensitivity and mode of CCR5 receptor use by human immunodeficiency virus type 1 of the R5 phenotype. J Virol. 2004;78:11807–11815. doi: 10.1128/JVI.78.21.11807-11815.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keele BF, Giorgi EE, Salazar-Gonzalez JF, Decker JM, Pham KT, Salazar MG, Sun C, Grayson T, Wang S, Li H, Wei X, Jiang C, Kirchherr JL, Gao F, Anderson JA, Ping LH, Swanstrom R, Tomaras GD, Blattner WA, Goepfert PA, Kilby JM, Saag MS, Delwart EL, Busch MP, Cohen MS, Montefiori DC, Haynes BF, Gaschen B, Athreya GS, Lee HY, Wood N, Seoighe C, Perelson AS, Bhattacharya T, Korber BT, Hahn BH, Shaw GM. Identification and characterization of transmitted and early founder virus envelopes in primary HIV-1 infection. Proc Natl Acad Sci U S A. 2008;105:7552–7557. doi: 10.1073/pnas.0802203105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesavardhana S, Varadarajan R. Stabilizing the native trimer of HIV-1 Env by destabilizing the heterodimeric interface of the gp41 postfusion six-helix bundle. J Virol. 2014;88:9590–9604. doi: 10.1128/JVI.00494-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilby JM, Hopkins S, Venetta TM, DiMassimo B, Cloud GA, Lee JY, Alldredge L, Hunter E, Lambert D, Bolognesi D, Matthews T, Johnson MR, Nowak MA, Shaw GM, Saag MS. Potent suppression of HIV-1 replication in humans by T-20, a peptide inhibitor of gp41-mediated virus entry. Nature Medicine. 1998;4:1302–1307. doi: 10.1038/3293. [DOI] [PubMed] [Google Scholar]
- Klatzmann D, Champagne E, Chamaret S, Gruest J, Guetard D, Hercend T, Gluckman JC, Montagnier L. T-lymphocyte T4 molecule behaves as the receptor for human retrovirus LAV. Nature. 1984;312:767–768. doi: 10.1038/312767a0. [DOI] [PubMed] [Google Scholar]
- Kolchinsky P, Kiprilov E, Sodroski J. Increased neutralization sensitivity of CD4-independent human immunodeficiency virus variants. J Virol. 2001a;75:2041–2050. doi: 10.1128/JVI.75.5.2041-2050.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolchinsky P, Kiprilov E, Bartley P, Rubinstein R, Sodroski J. Loss of a single N-linked glycan allows CD4-independent human immunodeficiency virus type 1 infection by altering the position of the gp120 V1/V2 variable loops. J Virol. 2001b;75:3435–3443. doi: 10.1128/JVI.75.7.3435-3443.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolchinsky P, Mirzabekov T, Farzan M, Kiprilov E, Cayabyab M, Mooney LJ, Choe H, Sodroski J. Adaptation of a CCR5-using, primary human immunodeficiency virus type 1 isolate for CD4-independent replication. J Virol. 1999;73:8120–8126. doi: 10.1128/jvi.73.10.8120-8126.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koning FA, Kwa D, Boeser-Nunnink B, Dekker J, Vingerhoed J, Hiemstra H, Schuitemaker H. Decreasing sensitivity to RANTES (regulated on activation, normally T cell-expressed and -secreted) neutralization of CC chemokine receptor 5-using, non-syncytium-inducing virus variants in the course of human immunodeficiency virus type 1 infection. The Journal of infectious diseases. 2003;188:864–872. doi: 10.1086/377105. [DOI] [PubMed] [Google Scholar]
- Koshiba T, Chan DC. The prefusogenic intermediate of HIV-1 gp41 contains exposed C-peptide regions. J Biol Chem. 2003;278:7573–7579. doi: 10.1074/jbc.M211154200. [DOI] [PubMed] [Google Scholar]
- Kowalski M, Potz J, Basiripour L, Dorfman T, Goh WC, Terwilliger E, Dayton A, Rosen C, Haseltine W, Sodroski J. Functional regions of the envelope glycoprotein of human immunodeficiency virus type 1. Science. 1987;237:1351–1355. doi: 10.1126/science.3629244. [DOI] [PubMed] [Google Scholar]
- Kwong PD, Wyatt R, Robinson J, Sweet RW, Sodroski J, Hendrickson WA. Structure of an HIV gp120 envelope glycoprotein in complex with the CD4 receptor and a neutralizing human antibody. Nature. 1998;393:648–659. doi: 10.1038/31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBranche CC, Hoffman TL, Romano J, Haggarty BS, Edwards TG, Matthews TJ, Doms RW, Hoxie JA. Determinants of CD4 independence for a human immunodeficiency virus type 1 variant map outside regions required for coreceptor specificity. J Virol. 1999;73:10310–10319. doi: 10.1128/jvi.73.12.10310-10319.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrijn AF, Poignard P, Raja A, Zwick MB, Delgado K, Franti M, Binley J, Vivona V, Grundner C, Huang CC, Venturi M, Petropoulos CJ, Wrin T, Dimitrov DS, Robinson J, Kwong PD, Wyatt RT, Sodroski J, Burton DR. Access of antibody molecules to the conserved coreceptor binding site on glycoprotein gp120 is sterically restricted on primary human immunodeficiency virus type 1. J Virol. 2003;77:10557–10565. doi: 10.1128/JVI.77.19.10557-10565.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalezari J, Thompson M, Kumar P, Piliero P, Davey R, Patterson K, Shachoy-Clark A, Adkison K, Demarest J, Lou Y, Berrey M, Piscitelli S. Antiviral activity and safety of 873140, a novel CCR5 antagonist, during short-term monotherapy in HIV-infected adults. AIDS (London, England) 2005;19:1443–1448. doi: 10.1097/01.aids.0000183633.06580.8a. [DOI] [PubMed] [Google Scholar]
- Lee B, Sharron M, Montaner LJ, Weissman D, Doms RW. Quantification of CD4, CCR5, and CXCR4 levels on lymphocyte subsets, dendritic cells, and differentially conditioned monocyte-derived macrophages. Proc Natl Acad Sci U S A. 1999;96:5215–5220. doi: 10.1073/pnas.96.9.5215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Ozorowski G, Ward AB. Cryo-EM structure of a native, fully glycosylated, cleaved HIV-1 envelope trimer. Science. 2016;351:1043–1048. doi: 10.1126/science.aad2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin NH, Becerril C, Giguel F, Novitsky V, Moyo S, Makhema J, Essex M, Lockman S, Kuritzkes DR, Sagar M. Env sequence determinants in CXCR4-using human immunodeficiency virus type-1 subtype C. Virology. 2012;433:296–307. doi: 10.1016/j.virol.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R, Paxton WA, Choe S, Ceradini D, Martin SR, Horuk R, MacDonald ME, Stuhlmann H, Koup RA, Landau NR. Homozygous defect in HIV-1 coreceptor accounts for resistance of some multiply-exposed individuals to HIV-1 infection. Cell. 1996;86:367–377. doi: 10.1016/s0092-8674(00)80110-5. [DOI] [PubMed] [Google Scholar]
- Lu M, Blacklow SC, Kim PS. A trimeric structural domain of the HIV-1 transmembrane glycoprotein. Nat Struct Biol. 1995;2:1075–1082. doi: 10.1038/nsb1295-1075. [DOI] [PubMed] [Google Scholar]
- Lyumkis D, Julien JP, de Val N, Cupo A, Potter CS, Klasse PJ, Burton DR, Sanders RW, Moore JP, Carragher B, Wilson IA, Ward AB. Cryo-EM structure of a fully glycosylated soluble cleaved HIV-1 envelope trimer. Science. 2013;342:1484–1490. doi: 10.1126/science.1245627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madani N, Princiotto AM, Zhao C, Jahanbakhshsefidi F, Mertens M, Herschhorn A, Melillo B, Smith AB, 3rd, Sodroski J. Activation and inactivation of primary human immunodeficiency virus envelope glycoprotein trimers by CD4-mimetic compounds. J Virol. 2017;91 doi: 10.1128/JVI.01880-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mammano F, Kondo E, Sodroski J, Bukovsky A, Gottlinger HG. Rescue of human immunodeficiency virus type 1 matrix protein mutants by envelope glycoproteins with short cytoplasmic domains. J Virol. 1995;69:3824–3830. doi: 10.1128/jvi.69.6.3824-3830.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin J, LaBranche CC, Gonzalez-Scarano F. Differential CD4/CCR5 utilization, gp120 conformation, and neutralization sensitivity between envelopes from a microglia-adapted human immunodeficiency virus type 1 and its parental isolate. J Virol. 2001;75:3568–3580. doi: 10.1128/JVI.75.8.3568-3580.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melby T, Despirito M, Demasi R, Heilek-Snyder G, Greenberg ML, Graham N. HIV-1 coreceptor use in triple-class treatment-experienced patients: baseline prevalence, correlates, and relationship to enfuvirtide response. The Journal of Infectious Diseases. 2006;194:238–246. doi: 10.1086/504693. [DOI] [PubMed] [Google Scholar]
- Melikyan GB, Markosyan RM, Hemmati H, Delmedico MK, Lambert DM, Cohen FS. Evidence that the transition of HIV-1 gp41 into a six-helix bundle, not the bundle configuration, induces membrane fusion. J Cell Biol. 2000;151:413–423. doi: 10.1083/jcb.151.2.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro JB, Gorman J, Ma X, Zhou Z, Arthos J, Burton DR, Koff WC, Courter JR, Smith AB, 3rd, Kwong PD, Blanchard SC, Mothes W. Conformational dynamics of single HIV-1 envelope trimers on the surface of native virions. Science. 2014;346:759–763. doi: 10.1126/science.1254426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami T, Freed EO. Genetic evidence for an interaction between human immunodeficiency virus type 1 matrix and alpha-helix 2 of the gp41 cytoplasmic tail. J Virol. 2000;74:3548–3554. doi: 10.1128/jvi.74.8.3548-3554.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musich T, Peters PJ, Duenas-Decamp MJ, Gonzalez-Perez MP, Robinson J, Zolla-Pazner S, Ball JK, Luzuriaga K, Clapham PR. A conserved determinant in the V1 loop of HIV-1 modulates the V3 loop to prime low CD4 use and macrophage infection. J Virol. 2011;85:2397–2405. doi: 10.1128/JVI.02187-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien WA, Koyanagi Y, Namazie A, Zhao JQ, Diagne A, Idler K, Zack JA, Chen IS. HIV-1 tropism for mononuclear phagocytes can be determined by regions of gp120 outside the CD4-binding domain. Nature. 1990;348:69–73. doi: 10.1038/348069a0. [DOI] [PubMed] [Google Scholar]
- O’Connell O, Repik A, Reeves JD, Gonzalez-Perez MP, Quitadamo B, Anton ED, Duenas-Decamp M, Peters P, Lin R, Zolla-Pazner S, Corti D, Wallace A, Wang S, Kong XP, Lu S, Clapham PR. Efficiency of bridging-sheet recruitment explains HIV-1 R5 envelope glycoprotein sensitivity to soluble CD4 and macrophage tropism. J Virol. 2013;87:187–198. doi: 10.1128/JVI.01834-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacheco B, Alsahafi N, Debbeche O, Prevost J, Ding S, Chapleau JP, Herschhorn A, Madani N, Princiotto A, Melillo B, Gu C, Zeng X, Mao Y, Smith AB, 3rd, Sodroski J, Finzi A. Residues in the gp41 ectodomain regulate HIV-1 envelope glycoprotein conformational transitions induced by gp120-directed inhibitors. J Virol. 2017;91 doi: 10.1128/JVI.02219-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pancera M, Zhou T, Druz A, Georgiev IS, Soto C, Gorman J, Huang J, Acharya P, Chuang GY, Ofek G, Stewart-Jones GB, Stuckey J, Bailer RT, Joyce MG, Louder MK, Tumba N, Yang Y, Zhang B, Cohen MS, Haynes BF, Mascola JR, Morris L, Munro JB, Blanchard SC, Mothes W, Connors M, Kwong PD. Structure and immune recognition of trimeric pre-fusion HIV-1 Env. Nature. 2014;514:455–461. doi: 10.1038/nature13808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters PJ, Bhattacharya J, Hibbitts S, Dittmar MT, Simmons G, Bell J, Simmonds P, Clapham PR. Biological analysis of human immunodeficiency virus type 1 R5 envelopes amplified from brain and lymph node tissues of AIDS patients with neuropathology reveals two distinct tropism phenotypes and identifies envelopes in the brain that confer an enhanced tropism and fusigenicity for macrophages. J Virol. 2004;78:6915–6926. doi: 10.1128/JVI.78.13.6915-6926.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaff JM, Wilen CB, Harrison JE, Demarest JF, Lee B, Doms RW, Tilton JC. HIV-1 resistance to CCR5 antagonists associated with highly efficient use of CCR5 and altered tropism on primary CD4+ T cells. J Virol. 2010;84:6505–6514. doi: 10.1128/JVI.00374-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poeschla EM, Looney DJ. CXCR4 is required by a nonprimate lentivirus: heterologous expression of feline immunodeficiency virus in human, rodent, and feline cells. J Virol. 1998;72:6858–6866. doi: 10.1128/jvi.72.8.6858-6866.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repits J, Oberg M, Esbjornsson J, Medstrand P, Karlsson A, Albert J, Fenyo EM, Jansson M. Selection of human immunodeficiency virus type 1 R5 variants with augmented replicative capacity and reduced sensitivity to entry inhibitors during severe immunodeficiency. J Gen Virol. 2005;86:2859–2869. doi: 10.1099/vir.0.81111-0. [DOI] [PubMed] [Google Scholar]
- Rho HM, Poiesz B, Ruscetti FW, Gallo RC. Characterization of the reverse transcriptase from a new retrovirus (HTLV) produced by a human cutaneous T-cell lymphoma cell line. Virology. 1981;112:355–360. doi: 10.1016/0042-6822(81)90642-5. [DOI] [PubMed] [Google Scholar]
- Rizzuto CD, Wyatt R, Hernandez-Ramos N, Sun Y, Kwong PD, Hendrickson WA, Sodroski J. A conserved HIV gp120 glycoprotein structure involved in chemokine receptor binding. Science. 1998;280:1949–1953. doi: 10.1126/science.280.5371.1949. [DOI] [PubMed] [Google Scholar]
- Roche M, Jakobsen MR, Sterjovski J, Ellett A, Posta F, Lee B, Jubb B, Westby M, Lewin SR, Ramsland PA, Churchill MJ, Gorry PR. HIV-1 escape from the CCR5 antagonist maraviroc associated with an altered and less-efficient mechanism of gp120-CCR5 engagement that attenuates macrophage tropism. J Virol. 2011;85:4330–4342. doi: 10.1128/JVI.00106-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzwedel K, Berger EA. Complementation of diverse HIV-1 Env defects through cooperative subunit interactions: a general property of the functional trimer. Retrovirology. 2009;6:75. doi: 10.1186/1742-4690-6-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimura K, Nameki D, Kajiwara K, Watanabe K, Sakagami Y, Oishi S, Fujii N, Matsuoka M, Sarafianos SG, Kodama EN. Resistance profiles of novel electrostatically constrained HIV-1 fusion inhibitors. The Journal of biological chemistry. 2010;285:39471–39480. doi: 10.1074/jbc.M110.145789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si Z, Madani N, Cox JM, Chruma JJ, Klein JC, Schon A, Phan N, Wang L, Biorn AC, Cocklin S, Chaiken I, Freire E, Smith AB, 3rd, Sodroski JG. Small-molecule inhibitors of HIV-1 entry block receptor-induced conformational changes in the viral envelope glycoproteins. Proc Natl Acad Sci U S A. 2004;101:5036–5041. doi: 10.1073/pnas.0307953101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterjovski J, Roche M, Churchill MJ, Ellett A, Farrugia W, Gray LR, Cowley D, Poumbourios P, Lee B, Wesselingh SL, Cunningham AL, Ramsland PA, Gorry PR. An altered and more efficient mechanism of CCR5 engagement contributes to macrophage tropism of CCR5-using HIV-1 envelopes. Virology. 2010;404:269–278. doi: 10.1016/j.virol.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K, Liu J, Wang J, Shen S, Lu M. Atomic structure of a thermostable subdomain of HIV-1 gp41. Proc Natl Acad Sci U S A. 1997;94:12303–12308. doi: 10.1073/pnas.94.23.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan Q, Zhu Y, Li J, Chen Z, Han GW, Kufareva I, Li T, Ma L, Fenalti G, Li J, Zhang W, Xie X, Yang H, Jiang H, Cherezov V, Liu H, Stevens RC, Zhao Q, Wu B. Structure of the CCR5 chemokine receptor-HIV entry inhibitor maraviroc complex. Science. 2013;341:1387–1390. doi: 10.1126/science.1241475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor BM, Foulke JS, Flinko R, Heredia A, DeVico A, Reitz M. An alteration of human immunodeficiency virus gp41 leads to reduced CCR5 dependence and CD4 independence. J Virol. 2008;82:5460–5471. doi: 10.1128/JVI.01049-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedbury PR, Mercredi PY, Gaines CR, Summers MF, Freed EO. Elucidating the mechanism by which compensatory mutations rescue an HIV-1 matrix mutant defective for gag membrane targeting and envelope glycoprotein incorporation. J Mol Biol. 2015;427:1413–1427. doi: 10.1016/j.jmb.2015.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedbury PR, Novikova M, Ablan SD, Freed EO. Biochemical evidence of a role for matrix trimerization in HIV-1 envelope glycoprotein incorporation. Proc Natl Acad Sci U S A. 2016;113:E182–190. doi: 10.1073/pnas.1516618113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thali M, Olshevsky U, Furman C, Gabuzda D, Li J, Sodroski J. Effects of changes in gp120-CD4 binding affinity on human immunodeficiency virus type 1 envelope glycoprotein function and soluble CD4 sensitivity. J Virol. 1991;65:5007–5012. doi: 10.1128/jvi.65.9.5007-5012.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas ER, Dunfee RL, Stanton J, Bogdan D, Taylor J, Kunstman K, Bell JE, Wolinsky SM, Gabuzda D. Macrophage entry mediated by HIV Envs from brain and lymphoid tissues is determined by the capacity to use low CD4 levels and overall efficiency of fusion. Virology. 2007;360:105–119. doi: 10.1016/j.virol.2006.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilton JC, Amrine-Madsen H, Miamidian JL, Kitrinos KM, Pfaff J, Demarest JF, Ray N, Jeffrey JL, Labranche CC, Doms RW. HIV type 1 from a patient with baseline resistance to CCR5 antagonists uses drug-bound receptor for entry. AIDS Res Hum Retroviruses. 2010a;26:13–24. doi: 10.1089/aid.2009.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilton JC, Wilen CB, Didigu CA, Sinha R, Harrison JE, Agrawal-Gamse C, Henning EA, Bushman FD, Martin JN, Deeks SG, Doms RW. A maraviroc-resistant HIV-1 with narrow cross-resistance to other CCR5 antagonists depends on both N-terminal and extracellular loop domains of drug-bound CCR5. J Virol. 2010b;84:10863–10876. doi: 10.1128/JVI.01109-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trkola A, Dragic T, Arthos J, Binley JM, Olson WC, Allaway GP, Cheng-Mayer C, Robinson J, Maddon PJ, Moore JP. CD4-dependent, antibody-sensitive interactions between HIV-1 and its co-receptor CCR-5. Nature. 1996;384:184–187. doi: 10.1038/384184a0. [DOI] [PubMed] [Google Scholar]
- Wang T, Zhang Z, Wallace OB, Deshpande M, Fang H, Yang Z, Zadjura LM, Tweedie DL, Huang S, Zhao F, Ranadive S, Robinson BS, Gong YF, Ricarrdi K, Spicer TP, Deminie C, Rose R, Wang HG, Blair WS, Shi PY, Lin PF, Colonno RJ, Meanwell NA. Discovery of 4-benzoyl-1-[(4-methoxy-1H-pyrrolo[2,3-b]pyridin-3-yl)oxoacetyl]-2-(R)-methylpiperazine (BMS-378806): a novel HIV-1 attachment inhibitor that interferes with CD4-gp120 interactions. Journal of Medicinal Chemistry. 2003;46:4236–4239. doi: 10.1021/jm034082o. [DOI] [PubMed] [Google Scholar]
- Wang W, De Feo CJ, Zhuang M, Vassell R, Weiss CD. Selection with a peptide fusion inhibitor corresponding to the first heptad repeat of HIV-1 gp41 identifies two genetic pathways conferring cross-resistance to peptide fusion inhibitors corresponding to the first and second heptad repeats (HR1 and HR2) of gp41. J Virol. 2011;85:12929–12938. doi: 10.1128/JVI.05391-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissenhorn W, Dessen A, Harrison SC, Skehel JJ, Wiley DC. Atomic structure of the ectodomain from HIV-1 gp41. Nature. 1997;387:426–430. doi: 10.1038/387426a0. [DOI] [PubMed] [Google Scholar]
- Westby M, Smith-Burchnell C, Mori J, Lewis M, Mosley M, Stockdale M, Dorr P, Ciaramella G, Perros M. Reduced maximal inhibition in phenotypic susceptibility assays indicates that viral strains resistant to the CCR5 antagonist maraviroc utilize inhibitor-bound receptor for entry. J Virol. 2007;81:2359–2371. doi: 10.1128/JVI.02006-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild CT, Shugars DC, Greenwell TK, McDanal CB, Matthews TJ. Peptides corresponding to a predictive alpha-helical domain of human immunodeficiency virus type 1 gp41 are potent inhibitors of virus infection. Proc Natl Acad Sci U S A. 1994;91:9770–9774. doi: 10.1073/pnas.91.21.9770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett BJ, Adema K, Heveker N, Brelot A, Picard L, Alizon M, Turner JD, Hoxie JA, Peiper S, Neil JC, Hosie MJ. The second extracellular loop of CXCR4 determines its function as a receptor for feline immunodeficiency virus. J Virol. 1998;72:6475–6481. doi: 10.1128/jvi.72.8.6475-6481.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Gerard NP, Wyatt R, Choe H, Parolin C, Ruffing N, Borsetti A, Cardoso AA, Desjardin E, Newman W, Gerard C, Sodroski J. CD4-induced interaction of primary HIV-1 gp120 glycoproteins with the chemokine receptor CCR-5. Nature. 1996;384:179–183. doi: 10.1038/384179a0. [DOI] [PubMed] [Google Scholar]
- Wyatt R, Kwong PD, Desjardins E, Sweet RW, Robinson J, Hendrickson WA, Sodroski JG. The antigenic structure of the HIV gp120 envelope glycoprotein. Nature. 1998;393:705–711. doi: 10.1038/31514. [DOI] [PubMed] [Google Scholar]
- Wyatt R, Sodroski J. The HIV-1 envelope glycoproteins: fusogens, antigens, and immunogens. Science. 1998;280:1884–1888. doi: 10.1126/science.280.5371.1884. [DOI] [PubMed] [Google Scholar]
- Wyatt R, Sullivan N, Thali M, Repke H, Ho D, Robinson J, Posner M, Sodroski J. Functional and immunologic characterization of human immunodeficiency virus type 1 envelope glycoproteins containing deletions of the major variable regions. J Virol. 1993;67:4557–4565. doi: 10.1128/jvi.67.8.4557-4565.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyma DJ, Kotov A, Aiken C. Evidence for a stable interaction of gp41 with Pr55(Gag) in immature human immunodeficiency virus type 1 particles. J Virol. 2000;74:9381–9387. doi: 10.1128/jvi.74.20.9381-9387.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X, Kurteva S, Ren X, Lee S, Sodroski J. Subunit stoichiometry of human immunodeficiency virus type 1 envelope glycoprotein trimers during virus entry into host cells. J Virol. 2006;80:4388–4395. doi: 10.1128/JVI.80.9.4388-4395.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimura K, Harada S, Boonchawalit S, Kawanami Y, Matsushita S. Impact of maraviroc-resistant and low-CCR5-adapted mutations induced by in vitro passage on sensitivity to anti-envelope neutralizing antibodies. J Gen Virol. 2014;95:1816–1826. doi: 10.1099/vir.0.062885-0. [DOI] [PubMed] [Google Scholar]
- Zhang PF, Bouma P, Park EJ, Margolick JB, Robinson JE, Zolla-Pazner S, Flora MN, Quinnan GV., Jr A variable region 3 (V3) mutation determines a global neutralization phenotype and CD4-independent infectivity of a human immunodeficiency virus type 1 envelope associated with a broadly cross-reactive, primary virus-neutralizing antibody response. J Virol. 2002;76:644–655. doi: 10.1128/JVI.76.2.644-655.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou N, Fan L, Ho HT, Nowicka-Sans B, Sun Y, Zhu Y, Hu Y, McAuliffe B, Rose B, Fang H, Wang T, Kadow J, Krystal M, Alexander L, Colonno R, Lin PF. Increased sensitivity of HIV variants selected by attachment inhibitors to broadly neutralizing antibodies. Virology. 2010;402:256–261. doi: 10.1016/j.virol.2010.03.033. [DOI] [PubMed] [Google Scholar]


