Abstract
Several anti-cancer therapies target the epidermal growth factor receptor (EGFR). Radionuclide imaging of EGFR expression in tumours may aid in selection of optimal cancer therapy. The 111In-labelled DOTA-conjugated ZEGFR:2377 Affibody molecule was successfully used for imaging of EGFR-expressing xenografts in mice. An optimal combination of radionuclide, chelator and targeting protein may further improve the contrast of radionuclide imaging. The aim of this study was to evaluate the targeting properties of radiocobalt-labelled DOTA-ZEGFR:2377. DOTA-ZEGFR:2377 was labelled with 57Co (T1/2 = 271.8 d), 55Co (T1/2 = 17.5 h), and, for comparison, with the positron-emitting radionuclide 68Ga (T1/2 = 67.6 min) with preserved specificity of binding to EGFR-expressing A431 cells. The long-lived cobalt radioisotope 57Co was used in animal studies. Both 57Co-DOTA-ZEGFR:2377 and 68Ga-DOTA-ZEGFR:2377 demonstrated EGFR-specific accumulation in A431 xenografts and EGFR-expressing tissues in mice. Tumour-to-organ ratios for the radiocobalt-labelled DOTA-ZEGFR:2377 were significantly higher than for the gallium-labelled counterpart already at 3 h after injection. Importantly, 57Co-DOTA-ZEGFR:2377 demonstrated a tumour-to-liver ratio of 3, which is 7-fold higher than the tumour-to-liver ratio for 68Ga-DOTA-ZEGFR:2377. The results of this study suggest that the positron-emitting cobalt isotope 55Co would be an optimal label for DOTA-ZEGFR:2377 and further development should concentrate on this radionuclide as a label.
Introduction
A transmembrane epidermal growth factor receptor (EGFR) regulates cellular proliferation, motility and apoptosis1. Aberrant expression of EGFR has been detected in multiple cancers and linked to a malignant phenotype2. Overexpression of EGFR is a predictive biomarker for response of advanced non-small-cell lung cancer to tyrosine kinase inhibitor gefitinib3, 4 and to first-line chemotherapy plus anti-EGFR monoclonal antibody cetuximab5. In head and neck squamous cell carcinomas (HNSCC), overexpression of EGFR is associated with relapse after radiotherapy6 and can be used for selection of patients for hyperfractionated accelerated radiotherapy7. Preclinical studies suggest that determination of EGFR expression can be used for monitoring of response to combination of radiation therapy and cetuximab in HNSCC8 or to therapy using heat shock protein 90 inhibitors9. Radionuclide molecular imaging is a potential method for in vivo measurement of EGFR expression in malignant tumours. Unlike biopsy-based methods, molecular imaging is non-invasive and can be used repeatedly. In addition, radionuclide imaging enables imaging of receptor expression in multiple metastases addressing the heterogeneity of expression. Thus, the use of radionuclide molecular imaging of EGFR expression would make cancer treatment more personalized.
Approaches for development of probes for visualization of EGFR include the use of radiolabelled tyrosine kinase inhibitors, anti-EGFR monoclonal antibodies and their fragments, the natural ligand EGF and scaffold proteins10. A general challenge for development of EGFR-imaging agents is expression of EGFR in normal tissues, particularly in liver. Sequestering of radiolabelled probes in liver might result in their insufficient uptake in tumours11. However, a clinical study has demonstrated that it is possible to find an injected anti-EGFR antibody dose capable of providing a partial saturation of EGFR in the liver without target saturation in tumours enabling visualization of EGFR-expressing malignancies using radiolabelled antibodies11.
We develop EGFR-imaging probes based on Affibody molecules. Affibody molecules are small (7 kDa) engineered scaffold proteins, which can be selected by phage display for binding with high affinity to different proteins12. In vivo molecular imaging using radiolabelled Affibody molecules has been demonstrated in preclinical studies for several cancer-related molecular targets, e.g. HER2, EGFR, HER3, and IGF-1R. Clinical studies have demonstrated specific and high-contrast imaging of HER2-expression in metastatic breast cancer using a 111In- and 68Ga-labelled ABY-025 Affibody molecule13, 14. Earlier, we have shown that the anti-EGFR 111In-DOTA-ZEGFR:2377 Affibody molecule can visualize EGFR expression in murine xenografts15. Importantly, this Affibody molecule has similar affinity to both human and murine EGFR. According to surface plasmon resonance measurements, equilibrium dissociation constants (KD) were 0.8 and 28 nM for KD1 and KD2, respectively, in the case of murine EGFR. Corresponding values for human EGFR were 0.9 and 28 nM15. Therefore, a murine model takes into account the target-specific interaction of the tracer both in tumours and in normal tissues and should thus ensure good translational potential. Our studies showed that injection of 30–50 µg 111In-DOTA-ZEGFR:2377 provides partial saturation of EGFR in normal tissues without saturating the target in tumours15. Internalization of 111In-DOTA-ZEGFR:2377 by EGFR-expressing cells was slow, less than 20% after 24 h. Therefore, normal EGFR-expressing organs acted as depot that release 111In-DOTA-ZEGFR:2377 resulting in a relatively slow blood clearance. The tumour-to-blood ratios at optimal dosage were 7.0 ± 0.5 and 14 ± 4, at 4 and 24 h after injection, respectively.
A goal for the development of imaging agents is to obtain a probe with high uptake in tumour and low uptake in normal tissues. Earlier studies have demonstrated that different combinations of a chelator and a radionuclide can modify physico-chemical properties of a tumour-targeting peptide in different ways and influence its biodistribution16, 17. Moreover, the use of the same chelator in combination with different nuclides has resulted in altered imaging properties of somatostatin, RGD-peptides and bombesin analogues17–22. For example, Heppeler and co-workers concluded after comparison of 57Co- and 68Ga-labelled somatostatin analogue DOTA-TOC that “the physical features (size, charge) of the radiometal strongly influence receptor affinity, biodistribution and the pharmacokinetics of radiometal-labelled peptides”22. A strong influence of a radiometal/chelator combination on imaging contrast has been observed also for Affibody molecules. For example, biodistribution and tumour-to-organ ratios of DOTA-conjugated anti-HER2 Affibody molecules were altered appreciably by substitution of 68Ga by 111In or 44Sc and by substitution of 111In by 57Co23–25. Importantly, systematic studies concerning influence of radionuclides on biodistribution of tumour-targeting Affibody conjugates might help to select a probe with the optimal imaging characteristics.
Three cobalt radioisotopes, 55Co (T1/2 = 17.5 h), 57Co (T1/2 = 271.8 d) and 58mCo (T1/2 = 9.04 h) are of interest for radionuclide tumour targeting. 55Co is a long-lived positron emitter, which can be used for labelling of peptides for PET imaging26, 27. 58mCo emits Auger electrons and has been proposed for radionuclide therapy26, 28. The long-lived 57Co is a convenient surrogate radionuclide, which can be used for preclinical development of radiocobalt-labelled probes22, 27 in the same way as 125I is used as a substitute for 123I, 124I and 131I.
Development of a radiocobalt-labelled ZEGFR:2377 derivative with favourable targeting properties would open the way for the use of 55Co as a label. The increase of tumour-to-blood ratio of 111In-DOTA-ZEGFR:2377 with time indicates that performing the imaging at the next day after injection would provide better contrast. For this purpose, a positron-emitting radionuclide with a half-life of 10–20 h would be optimal. Besides, our studies on the previous generation of anti-EGFR Affibody molecules demonstrated that residualizing radiometal labels provide appreciably better tumour retention of the radionuclide at 24 h after injection29. 55Co can be produced by the 54Fe(d, n)55Co reaction on enriched 54Fe targets using low-energy cyclotrons available at PET-centres26, 30. Importantly, the DOTA chelator provides stable coupling of radiocobalt to targeting proteins and peptides22, 25, 26, 28. The use of a positron-emitting label for DOTA-ZEGFR:2377 would further improve detection of EGFR expression in vivo, since PET provides better imaging sensitivity compared with SPECT. A generator-produced positron emitter 68Ga (T1/2 = 67.7 min) is one obvious alternative to 55Co, although the time window for imaging would be limited to three-four hour after injection.
The goal of this study was to confirm that the DOTA-conjugated ZEGFR:2377 can be labelled with 55Co with preserved binding specificity and to compare tumour-targeting properties of radiogallium- and radiocobalt-labelled DOTA-ZEGFR:2377. The long-lived cobalt radioisotope 57Co (T1/2 = 271.8 d) was used in a number of experiments as a convenient surrogate of 55Co.
Results
Tracer production and labelling
The C-terminal cysteine-containing anti-EGFR Affibody molecule ZEGFR:2377 was produced, conjugated with maleimido-derivative of DOTA and purified as described earlier15. Analytic reversed-phase high-performance liquid chromatography (RP-HPLC) demonstrated a purity for DOTA-ZEGFR:2377 of over 95% (Supplementary Fig. S1). The molecular mass of DOTA-ZEGFR:2377 was determined by mass spectrometric analysis and showed a good agreement with the theoretical value (expected 7916.9 Da, found 7918 Da) (Supplementary Fig. S2). Measuring of circular dichroism spectra (Supplementary Fig. S3) demonstrated a high-fidelity refolding of DOTA-ZEGFR:2377 after heating up to 90 °C.
Labelling of DOTA-ZEGFR:2377 with cobalt isotopes provided yields of over 99%. The identity of conjugates was confirmed by radio-SDS-PAGE. Initial experiments concerning labelling with 55Co were associated with precipitation of Affibody molecules. Exclusion of glassware from the radionuclide production solved this problem. Still, aggregation of 55Co-DOTA-ZEGFR:2377 remains to be an issue. Similar effect for 57Co-DOTA-ZEGFR:237 was observed only occasionally, e.g. in the case of prolonged (3 h) incubation at 85 °C. Remarkably, this phenomenon was observed only with Affibody molecules, but not during 55Co-labelling of somatostatin or bombesin analogues26–28. Labelling of DOTA-ZEGFR:2377 with 68Ga provided a yield of 98.9 ± 0.5%. A purification using NAP-5 column provided a purity of 100%. A summary of obtained yields and specific activities of imaging probes is provided in Supplementary Table S1. There was no measurable release of radionuclide from the conjugate after 4 h (57Co) or 2 h (68Ga) incubation with 500-fold excess of EDTA.
In vitro characterization of radiolabelled DOTA-ZEGFR:2377
Pre-treatment of EGFR-expressing A431 cells with an excess of non-labelled ZEGFR:2377 caused a more than fivefold reduction of binding of both 68Ga- and 55/57Co- DOTA-ZEGFR:2377 (p < 5 × 10−7). This demonstrates saturable receptor-mediated binding of all conjugates to EGFR-expressing cells. According to LigandTracer measurements, the equilibrium dissociation constant (KD) of 57Co-labelled DOTA-ZEGFR:2377 interaction with A431 cells (167 ± 18 pM) was lower than KD of 111In-DOTA-ZEGFR:2377 (744 ± 28 pM) (For sensorgrams see Supplementary Fig. S4). Both labelled variants had similar association rate, (4.8 ± 0.6) × 104 M−1s−1 and (3.7 ± 0.1) × 104 M−1s−1, for 57Co- DOTA-ZEGFR:2377 and 111In-DOTA-ZEGFR:2377, respectively. However, the dissociation rate for 57Co- DOTA-ZEGFR:2377, (7.8 ± 0.7) × 10−6 s−1, was appreciably lower than for 111In-DOTA-ZEGFR:2377, (2.8 ± 0.2) × 10−5 s−1. Unfortunately, KD of 68Ga-DOTA-ZEGFR:2377 could not be measured since the half-life of the radionuclide is much shorter than the assay time required for accurate determination of the off-rate. To evaluate the relative binding strength of not only cobalt and indium but also gallium-labelled variants, the half maximum inhibition concentrations (IC50) were measured (Fig. 1). In agreement with KD determination, the IC50 value of Co-DOTA-ZEGFR:2377 (533 ± 1pM) was lower than that of In-DOTA-ZEGFR:2377 (700 ± 1pM). IC50 values of Co-DOTA-ZEGFR:2377 and Ga-DOTA-ZEGFR:2377 (576 ± 1pM) were very close, but significantly different.
Figure 1.
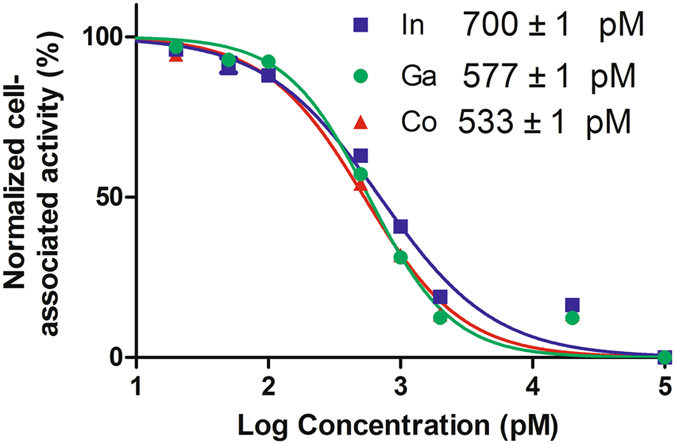
Inhibition of 111In-DOTA- ZEGFR:2377 binding to A431 cells with natGa-, natCo- or natIn- ZEGFR:2377. Data presented as mean ± SD of 3 culture dishes.
Data concerning internalization of 57Co-DOTA-ZEGFR:2377 and 68Ga-DOTA-ZEGFR:2377 by EGFR-expressing A431 cells are presented in Fig. 2. In agreement with previous data for 111In-DOTA-ZEGFR:2377 15, the internalization was slow, although the internalized fraction of the radioactivity increased over time. After 4-h incubation, the internalized fraction was less than 20% for both tracers. In the case of 57Co-DOTA-ZEGFR:2377, the cell-associated radioactivity reached maximum between 2 and 4 h with subsequent decline.
Figure 2.
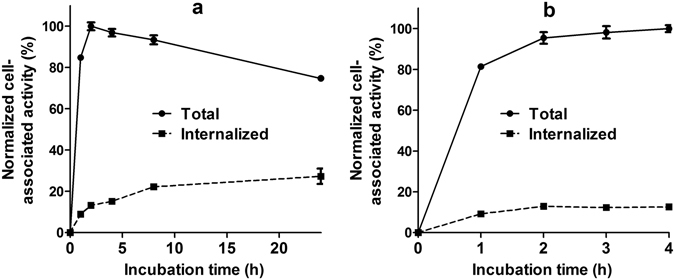
Cell-associated radioactivity as a function of time during continuous incubation of EGFR-expressing A431 cells with the 57Co-DOTA-ZEGFR:2377 (a) and 68Ga- DOTA-ZEGFR:2377 (b). Data are presented as mean from 3 dishes ± SD, and normalized to the maximum uptake. Due to small variability some error bars are hidden behind the symbols.
In vivo studies
Specificity of EGFR targeting in vivo was evaluated by pre-saturation of the receptors in normal murine tissues and A431 xenografts with high EGFR expression by pre-injection of a 10-fold excess of non-labelled ZEGFR:2377. In addition, mice bearing SKOV-3 xenografts with very low EGFR expression were used as negative control. The results of the in vivo specificity experiments are presented in Fig. 3. Pre-saturation of EGFR in A431 xenografts caused a significant (p < 0.0005) decrease in tumour uptake of both tracers. Besides, there was a statistically significant (p < 0.05) decrease in radioactivity concentration in blood and lung, and in EGFR-expressing tissues, such as salivary gland, liver, and colon. The uptake of both 57Co-DOTA-ZEGFR:2377 and 68Ga-DOTA-ZEGFR:2377 in SKOV-3 xenografts was much lower (p < 10−7) than in A431 xenografts.
Figure 3.
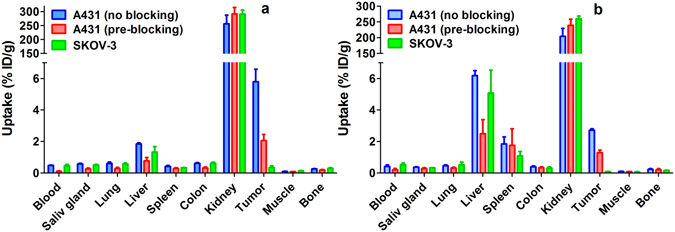
Specificity of 57Co-DOTA-ZEGFR:2377 (a) and 68Ga-DOTA-ZEGFR:2377 (b) uptake in tumours at 3 h after injection. An injected protein dose was adjusted to 40 µg for all animals. For pre-blocking, a group of animals bearing EGFR-positive A431 xenografts was pre-injected with 400 µg non-labelled ZEGFR:2377 40 min before injection of the radiolabelled conjugate. A group with SKOV-3 xenografts was used as a negative control. Data are presented as average %ID/g ± SD (n = 4).
Comparison of biodistribution of 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377 is presented in Table 1. The most prominent difference was between 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377 in hepatic, splenic and tumour uptake. The uptake of 68Ga-DOTA-ZEGFR:2377 was 3.3-fold higher than the uptake of 57Co-DOTA-ZEGFR:2377 in liver, and 4.4-fold higher in spleen. The tumour uptake of 57Co-DOTA-ZEGFR:2377 was 2.1-fold higher than the uptake of 68Ga-DOTA-ZEGFR:2377. Besides, the uptake of 57Co-DOTA-ZEGFR:2377 was 1.2–1.5 fold higher in salivary gland, lung, and colon. At 24 h after injection, the uptake of 57Co-DOTA-ZEGFR:2377 was reduced 1.3–1.6 fold in tumour as well as in salivary gland, lung, and liver.
Table 1.
Comparative biodistribution of 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377 after injection of 40 μg into BALB/C nu/nu mice bearing A431 xenografts.
| 3 h after injection | 24 h after injection | ||
|---|---|---|---|
| 68Ga-DOTA-ZEGFR:2377 | 57Co-DOTA-ZEGFR:2377 | 57Co-DOTA-ZEGFR:2377 | |
| Blood | 0.42 ± 0.09 | 0.48 ± 0.02 | 0.13 ± 0.03b |
| Salivary gland | 0.37 ± 0.02 | 0.57 ± 0.04a | 0.40 ± 0.03b |
| Lung | 0.46 ± 0.05 | 0.60 ± 0.09a | 0.37 ± 0.04b |
| Liver | 6.2 ± 0.3 | 1.85 ± 0.06a | 1.2 ± 0.1b |
| Spleen | 1.9 ± 0.4 | 0.42 ± 0.06a | 0.38 ± 0.04 |
| Colon | 0.39 ± 0.05 | 0.61 ± 0.05a | 0.47 ± 0.07b |
| Kidney | 204 ± 25 | 256 ± 30a | 218 ± 12 |
| Tumour | 2.7 ± 0.1 | 5.8 ± 0.8a | 4.04 ± 0.03b |
| Muscle | 0.10 ± 0.01 | 0.10 ± 0.01 | 0.09 ± 0.01 |
| Bone | 0.23 ± 0.04 | 0.25 ± 0.03 | 0.21 ± 0.05 |
| Gastrointestinal tract | 0.9 ± 0.1 | 1.1 ± 0.2 | 0.7 ± 0.2b |
| Carcass | 3.8 ± 0.5 | 4.9 ± 0.4a | 3.37 ± 0.08b |
Data are presented as average %ID/g ± SD (n = 4), except for the gastrointestinal tract and carcass which are presented as %ID per sample.
aSignificant (p < 0.05) difference between uptake of 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377;
bSignificant (p < 0.05) difference between uptake of 57Co-DOTA-ZEGFR:2377 at 3 and 24 h after injection.
The difference in the distribution profile resulted in significantly (p < 0.05) higher tumour-to-organ ratios of 57Co-DOTA-ZEGFR:2377 compared to 68Ga-DOTA-ZEGFR:2377 for all measured organs and tissues at 3 h after injection (Table 2). The most stunning was the difference in liver, where the use of 57Co-DOTA-ZEGFR:2377 provided a positive contrast (tumour-to-liver ratio of 3.1 ± 0.5), while the tumour-to-liver ratio of 68Ga-DOTA-ZEGFR:2377 was below one. At 24 h after injection, the tumour-to-blood ratio for 57Co-DOTA-ZEGFR:2377 increased 2.6-fold, to 32 ± 7. There was minor but significant decrease of tumour-to-spleen and tumour-to-kidney ratios.
Table 2.
Tumour-to-organ ratios of 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377 after injection of 40 μg into BALB/C nu/nu mice bearing A431 xenografts.
| 3 h after injection | 24 h after injection | ||
|---|---|---|---|
| 68Ga-DOTA-ZEGFR:2377 | 57Co-DOTA-ZEGFR:2377 | 57Co-DOTA-ZEGFR:2377 | |
| Blood | 7 ± 2a | 12 ± 2 | 32 ± 7b |
| Salivary gland | 7.3 ± 0.4a | 10 ± 2 | 10.2 ± 0.8 |
| Lung | 5.9 ± 0.7a | 10 ± 2 | 11 ± 1 |
| Liver | 0.44 ± 0.03a | 3.1 ± 0.5 | 3.3 ± 0.3 |
| Spleen | 1.5 ± 0.4a | 13.9 ± 0.7 | 11 ± 1b |
| Colon | 7.1 ± 0.8a | 10 ± 1 | 9 ± 1 |
| Kidney | 0.013 ± 0.002a | 0.023 ± 0.002 | 0.019 ± 0.001b |
| Muscle | 26 ± 3a | 56 ± 10 | 48 ± 7 |
| Bone | 12 ± 2a | 24 ± 5 | 21 ± 5 |
Data are average of four animals ± SD.
aSignificant (p < 0.05) difference between 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377.
bSignificant (p < 0.05) difference between values for 57Co-DOTA-ZEGFR:2377 at 3 and 24 h after injection.
Imaging using SPECT/CT and PET/CT devices for small animals, performed 3 h after injection (Fig. 4, full-scale image in Supplementary Fig. S5), confirmed the results of the biodistribution experiments. Kidneys were the organs with the highest uptake for both radionuclides. 68Ga-DOTA-ZEGFR:2377 provided a high contrast of A431 xenografts, even though the hepatic uptake was higher than the tumour uptake. On the other hand, the tumour uptake of 57Co-DOTA-ZEGFR:2377 was higher than the hepatic uptake.
Figure 4.
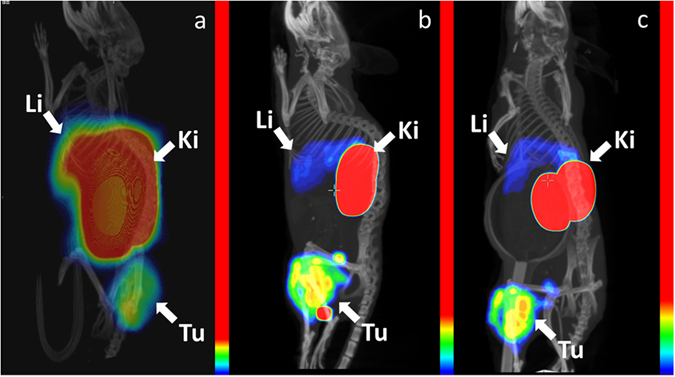
Imaging of mice bearing A431 xenografts. PET/CT using 68Ga-DOTA-ZEGFR:2377 at 3 h after injection (a) and SPECT/CT using 57Co-DOTA-ZEGFR:2377 at 3 h (b) and 24 h (c) after injection. The images show three-dimensional volume rendering of PET or SPECT data overlaid CT data. The images were rotated to provide view of liver. The relative colour scales were normalized to the highest activity and then adjusted to provide first red pixel in tumours (8, 13 and 17% of the full scale, for Fig. 4a,b and c, respectively). Arrows point at tumours (Tu), kidneys (Ki) and livers (Li).
Discussion
Anti-EGFR DOTA-ZEGFR:2377 Affibody molecule was successfully labelled with the nuclides 68Ga and 55/57Co. Both gallium- and cobalt-loaded DOTA-ZEGFR:2377 had subnanomolar IC50 values (Fig. 1). 57Co-DOTA-ZEGFR:2377 and 68Ga-DOTA-ZEGFR:2377 showed specific binding to EGFR-expressing cells in vitro and in vivo (Fig. 3). Cellular processing of both 57Co-DOTA-ZEGFR:2377 and 68Ga-DOTA-ZEGFR:2377 was characterized by slow internalization (Fig. 2). Both conjugates enabled imaging of EGFR-expressing xenografts in vivo (Fig. 4). However, there was a striking difference in their biodistribution profile (Table 2). A common feature was a prominent hepatic uptake. The biodistribution profile of 68Ga-DOTA-ZEGFR:2377 was quite similar to the profile reported for 111In-DOTA-ZEGFR:2377 15. The hepatic uptake was much higher than uptake in tumour or EGFR-expressing tissues, i.e. colon and salivary gland. In the case of 57Co-DOTA-ZEGFR:2377, the hepatic uptake was 3.4-fold lower and the tumour uptake was 2-fold higher compared to 68Ga-DOTA-ZEGFR:2377 at 3 h after injection of the same protein dose. This resulted in significantly higher tumour-to-organ ratios for all measured tissues. Most importantly, the tumour uptake of 57Co-DOTA-ZEGFR:2377 was significantly higher than the hepatic uptake (tumour-to-liver ratio of 3.1 ± 0.5), which is a precondition for successful imaging of hepatic metastases. This is essential, as liver is the major metastatic site for many cancers. The tumour-to-bone ratio for 57Co-DOTA-ZEGFR:2377 was also twice as high as for 68Ga-DOTA-ZEGFR:2377. At 24 h after injection, the tumour-to-blood ratio for 57Co-DOTA-ZEGFR:2377 increased 2.7-fold compared with 3 h time point.
The exact nature of this phenomenon is not quite clear. An important insight is provided by the fact that hepatic uptake of 68Ga-DOTA-ZEGFR:2377 was three-fold higher than uptake of 57Co-DOTA-ZEGFR:2377 (Fig. 3), when a blocking dose of non-labelled ZEGFR:2377 was pre-injected. Data for 111In-DOTA-ZEGFR:2377 show that saturation of liver uptake by non-labelled ZEGFR:2377 was much less efficient than saturation of uptake in other EGFR-expressing tissues15. This suggests that there are at least two different mechanisms of DOTA-ZEGFR:2377 hepatic uptake: one is dependent on EGFR expression (and can be saturated) and one is independent. The use of 57Co-DOTA-ZEGFR:2377 might reduce the hepatic uptake by the EGFR-independent mechanism. This is quite surprising, as the difference between 57Co-DOTA-ZEGFR:2377 and 68Ga-DOTA-ZEGFR:2377 is very subtle. Both Co2+ and Ga3+ have a six-coordination sphere and form DOTA complexes with distorted octahedral coordination geometry22. The major difference between Co-DOTA and Ga-DOTA complexes is that the cobalt complex carries a negative charge while the gallium complex is neutral. The literature data suggest that such small difference might have dramatic effect on affinity of radiolabelled peptides. For example, affinity of 68Ga and 57Co-DOTATOC to somatostatin receptors differs by one order of magnitude22. It is conceivable that the complex charge could also have an appreciable effect on DOTA-ZEGFR:2377 affinity to “scavenger receptors” in liver. The reduced liver binding of 57Co-DOTA-ZEGFR:2377 makes it more available for binding to EGFR-expressing tumours and tissues, which is in agreement with experimental observations.
The findings of this study suggest that the positron-emitting 55Co (T1/2 = 17.5 h) might be a suitable label for DOTA-ZEGFR:2377 and further development should concentrate on this radionuclide as a label. The half-life is long enough for imaging at 24 h after injection, but is not exceedingly long. The use of a positron-emitting label for DOTA-ZEGFR:2377 would further improve detection of EGFR expression in vivo, since PET provides better imaging sensitivity compared with SPECT.
Earlier, several approaches for preclinical development of PET probes specific to the extracellular domain of EGFR were evaluated. Labelling of the natural ligand, EGF, with 68Ga31 or 18F 32 enabled specific imaging of EGFR-expressing xenografts with tumour-to-blood ratios in the range of 2–5. At low doses, both tracers had liver uptake exceeding tumour uptake several fold. In mice, the hepatic uptake has been reduced appreciably at higher injected protein doses. However, this approach is not feasible clinically because of adverse side effects associated with injection of high doses of EGF (nausea, vomiting, hypotension)33. Anti-EGFR therapeutic monoclonal antibodies cetuximab and panitumumab were labelled with long-lived positron emitters 64Cu (T1/2 = 12.7 h), 86Y (T1/2 = 14.7 h), and 89Zr (T1/2 = 78.4 h)34–39. The maximum tumour-to-blood ratio (range of 2–8) was obtained at 3–4 days after injection due to slow clearance of antibodies from blood. 57Co-DOTA-ZEGFR:2377 provided a higher tumour-to-blood ratio already at 3 h after injection than any of these antibody-based agents at the best imaging time point. Labelling and preclinical in vivo evaluation of another clone of anti-EGFR Affibody molecule, ZEGFR:1907, with 18F and 64Cu has been reported40–42. ZEGFR:1907 had an apparent cross-reactivity with murine EGFR, which made the murine model adequate. These probes provided tumour-to-blood ratios of 2–10, depending on the labelling approach. Still, tumour-to-liver ratios were around 1.4 at best. Recently, we performed pre-clinical evaluation of ZEGFR:2377, which was site-specifically labelled with a long-lived positron emitter 89Zr (T1/2 = 78.4 h) using a maleimido derivative of a deferoxamine (DFO) chelator43. Direct comparison with 89Zr-labelled anti-EGFR antibody cetuximab demonstrated that 89Zr-DFO-Z EGFR:2377 provided appreciably higher tumour-to-blood, tumour-to-liver, and tumour-to-bone ratios. Yet, 57Co-DOTA-ZEGFR:2377 provided 2-5-fold higher tumour-to-organ ratios compared to 89Zr-DFO- EGFR:2377. Taken together, these data indicate that the radiocobalt-labelled DOTA-ZEGFR:2377 demonstrated the best tumour-to-non-tumour ratios among all pre-clinically tested affibody-based agents for imaging of EGFR.
A clinical translation of the finding of this study would require considering the dosimetry difference between 68Ga and 55Co. Although the longer half-life of 55Co permits a substantial improvement of tumour-to-organ ratios, it results in longer residence time and, therefore, higher dose burden on patients, compared to 68Ga. Another issue is that the decay scheme of 55Co includes a number of gamma emissions besides positrons, which increases whole-body dose (See Supplementary Table S2). These features are a common concern for all long-lived positron emitters. Still, the much more long-lived positron emitter 89Zr (T1/2 = 78.4 h) is used to label antibodies for clinical imaging44, and clinical studies show acceptable absorbed dose levels45, 46. It has to be noted that 55Co provides a better ratio between numbers of annihilation photons and co-emitted gamma photons compared to 89Zr and the majority of other long-lived positron emitters (Supplementary Table S2). Compared to the long-lived positron emitter 64Cu (T1/2 = 12.7 h), 55Co has higher positron abundance and does not emit beta particles. 55Co also provides a better image quality compared to the long-lived positron-emitting radiometal 86Y (T1/2 = 14.7 h)47.
In conclusion, the chemical nature of a radionuclide can appreciable influence the biodistribution and targeting properties of Affibody molecules. In vivo studies using 57Co as a model nuclide suggest that radiocobalt-labelled DOTA-ZEGFR:2377 is a very promising tracer for imaging of EGFR expression in vivo. Labelling of DOTA-ZEGFR:2377 with 55Co providing a conjugate with preserved specificity of binding to EGFR-expressing cells is feasible. This justifies further preclinical development of 55Co-labelled Affibody molecules for PET-imaging of EGFR expression in malignant tumours. Future studies should concentrate on development of large-scale production of 55Co-DOTA-ZEGFR:2377 and quantitative PET imaging of xenografts with different EGFR expression levels.
Methods
General
Maleimido-mono-amide-DOTA (1,4,7,10-tetraazacyclododecane-1,4,7-tris-acetic acid-10-maleimidoethylacetamide) was purchased from Macrocyclics (Dallas, TX). [57Co] cobalt chloride was purchased from PerkinElmer Sweden, (Upplands Väsby, Sweden). [111In] indium chloride was purchased from Mallinckrodt Pharmaceuticals (Chesterfield, United Kingdom). The EGFR-rich squamous carcinoma cell line A431 was obtained from American Type Culture Collection (ATCC, Rockville, MD). Buffers, used for conjugation and labelling, were purified from free metals using Chelex 100 resin (Bio-Rad Laboratories, Hercules, CA, USA).
The 68Ge/68Ga generator (50 mCi) was from Eckert and Ziegler (Vienna, Austria). Hydrochloric acid (0.1 M, prepared from 30% ultrapure HCl from Merck) was used for fractionated elution of the generator. The fraction containing the maximum radioactivity was used for labelling.
Labelling yield and radiochemical purity of the labelled DOTA-ZEGFR:2377 molecule were determined by radio-ITLC using 150–771 DARK GREEN strips (Biodex Medical Systems, New York, NY, USA) eluted with 0.2 M citric acid. In this system, free 68Ga and 55/57Co migrate with the solvent front and the radiolabelled DOTA-ZEGFR:2377 stays at the application point. The radio-ITLC was cross-validated by SDS-PAGE. The distribution of radioactivity along the thin layer chromatography strips and SDS-PAGE gels was measured using a Cyclone Storage Phosphor System (PerkinElmer, Wellesey, MA, USA).
Ketalar (ketamine, 50 mg/mL, Pfizer), Rompun (xylazin, 20 mg/mL, Bayer) and heparin (5000 IE/mL, Leo Pharma) were obtained commercially. The euthanasia was performed by an intra-peritoneal injection of Ketalar-Rompun solution (20 µL of solution/g body weight: Ketalar, 10 mg/mL; Rompun, 1 mg/mL).
The radioactivity uptake in the cellular processing and the biodistribution studies was measured using an automated gamma-counter with 3 inch NaI(TI) detector (1480 WIZARD, Wallac, Turku).
Statistics
Data on cellular uptake and biodistribution were analysed by unpaired, two-tailed t-test using GraphPad Prism (version 4.00 for Windows GraphPad Software) in order to determine significant differences (p < 0.05).
Tracer production and labelling
The C-terminal cysteine-containing anti-EGFR Affibody molecule Zegfr:2377 was produced, conjugated with maleimido-derivative of DOTA and purified as described earlier15. Before conjugation, a solution of Affibody molecules was treated with dithiothreitol (DTT; E. Merck, Darmstadt, Germany) in order to reduce spontaneously formed intermolecular disulfide bonds. For this purpose, a stock solution of Affibody molecules (2 ml, 2.3 mg/ml in PBS) was mixed with 100 µl 1 M Tris-HCl buffer, pH 8.0, and 63 µl DTT solution (0.5 M in water). The mixture was incubated at 40 °C for 30 min. The reduced Affibody molecules were then purified and the buffer was changed according to the manufacturer’s instructions using a disposable PD-10 column (GE Healthcare) pre-equilibrated with 0.2 M sodium acetate, pH 5.5. Maleimido-mono-amide-DOTA (2 mg) was added and the mixture incubated for 1 h at 40 °C.
The Affibody molecule was purified and analysed by high-performance liquid chromatography and on-line mass spectrometry (HPLC-MS) using an Agilent 1100 LC/MSD system equipped with electrospray ionization and a single quadrupole (Agilent Technologies, Palo Alto, CA). For purification, a Zorbax 300SB C18 9.4 × 250 mm, 5 µm column was used. The analysis was performed using a Zorbax 300SB-C18 2.1 × 150 mm, 3.5 µm column. Solvent A comprised 0.1% trifluoroacetic acid (TFA) in water, and solvent B comprised 0.1% TFA in acetonitrile. The column oven temperature was set to 30 °C. For analysis, the column was eluted with a linear gradient of 35% to 60% solvent B over 18 min, with a flow rate of 0.5 ml/min. The purified conjugate (further designated as DOTA-ZEGFR:2377) was freeze-dried. Chemstation Rev. B.02.01 software (Agilent) was used for analysis and evaluation of HPLC data. The conjugate was aliquoted (50 µg/aliquot) and lyophilized.
The thermal stability and secondary structure of DOTA- ZEGFR:2377 were determined using a JASCO J-810 spectropolarimeter (JASCO, Tokyo, Japan). The samples were diluted in PBS to concentrations of 0.5 mg/mL and melting temperatures were assessed by measuring the ellipticity at 221 nm during a temperature gradient ranging from 25–90 °C. The secondary structural content was assessed by measuring the degree of ellipticity from 250 to 195 nm at 25 °C before and after the thermal stability measurement.
55Co for labelling of Affibody molecules was produced via the 54Fe(d,n)55Co nuclear reaction as described earlier26. Briefly, the electroplated 54Fe target (99.84% enriched, Campro Scientific) was irradiated by 8.5 MeV deuterons using a GE PETtrace cyclotron. After the irradiation the produced 55Co was separated from the target material on an anion exchange column (Dowex 1∙8) using 4 M hydrochloric acid as eluent and further purified using a Chromafix 30-PS-HCO3 cartridge28 before evaporation to dryness. Labelling with radiocobalt has been performed according to previously described method25. Briefly, the lyophilized DOTA-ZEGFR:2377 (50 µg) was reconstituted in 40 µL of 0.2 M ammonium acetate, pH 5.5, mixed with radiocobalt stock solution (for 57Co: up to 18 µL, 4–15 MBq; for 55Co: 30–50 µL, 21–46 MBq) and incubated at 60°C for 30 min. The conjugate was purified using a NAP-5 size-exclusion column equilibrated with PBS.
For labelling with 68Ga, the 68Ge/68Ga generator was eluted with 0.1 M hydrochloric acid as eluent, and fractions containing 500 µL were collected. The fraction containing the maximum radioactivity was used for labelling. The lyophilized DOTA-ZEGFR:2377 (50 µg) was reconstituted in 100 µL 1.25 M sodium acetate buffer, pH 3.6. 68Ga-containing eluate, up to 3 MBq per microgram of DOTA-ZEGFR:2377, was added to the mixture. The mixture was incubated at 95 °C for 15 min. Thereafter, 1000-fold excess of Na4EDTA was added, and the mixture was incubated at 95 °C for 10 min. After labelling, the conjugate was purified using a NAP-5 size-exclusion column equilibrated with PBS.
Labelling of DOTA-ZEGFR:2377 with 111In for affinity measurements using LigandTracer and for determination of the half maximum inhibition concentration (IC50) was performed as described earlier15. For IC50 measurements, the conjugates were loaded with cobalt, indium and gallium of natural isotopic composition using the same conditions as for radiolabelling.
The yield and radiochemical purity of the conjugates were evaluated using ITLC eluted with 0.2 M citric acid, pH 2.0. To cross-validate the ITLC data, a radio-SDS page analysis was performed. The samples were treated with sample buffer (10 min at 70 °C) and analyzed using SDS-PAGE (at 200 V using NuPAGE 4–12% Bis-Tris Gels (Invitrogen AB, Sweden) in MES buffer (Invitrogen AB, Sweden). To provide a marker for low-molecular weight radioactivity, a sample of 68Ga or 57Co acetate was applied next to the analytes on the same gel.
To evaluate stability of labelling, the labelled conjugates were incubated with 500-fold excess of EDTA for 2 h at room temperature and then analysed using ITLC.
In vitro characterization of radiolabelled DOTA-ZEGFR:2377
The EGFR-expressing A431 epidermoid carcinoma cell line (ATCC) was used. Ovarian carcinoma SKOV-3 cell line (ATCC) with very low EGFR expression was used as a negative control in in vivo studies. Cells were cultured using Ham’s F10-medium supplemented with 10% foetal bovine serum (Flow, Stockholm, Sweden), L-glutamine (2 mM) and PEST (penicillin 100 IU/mL and streptomycin 100 mg/mL).
The in vitro binding specificity was verified by receptor pre-saturation with unlabelled Affibody molecules as described15. To test the binding specificity, 8 nM of radiolabelled DOTA-ZEGFR:2377 was added to 6 petri dishes containing 7 × 105 A431 cells/dish. A 50-fold molar excess of non-labelled DOTA-ZEGFR:2377 was added to groups of three petri dishes 15 min before the labelled conjugate to saturate the receptors. The dishes were incubated at 37 °C for 1 h in a humidified incubator. The media was collected, the cells were detached using trypsin-EDTA solution and radioactivity was measured. Percent of cell-bound radioactivity was calculated for both the pre-saturated and unsaturated cells.
The dissociation constant (KD) of 111In and 57Co-labelled DOTA-ZEGFR:2377 binding to living A431 cells was measured by using LigandTracer Yellow (Ridgeview Instruments AB, Uppsala, Sweden) and analysed using InteractionMap software (Ridgeview Diagnostics AB, Uppsala, Sweden) as described earlier48. This device records kinetic binding and dissociation of radiolabelled tracers on living cells. In order to cover the concentration span needed for proper affinity estimation, three increasing concentrations of the radioconjugate (0.33, 1, and 3 nM) were added in each affinity assay. Analysis was performed in duplicates.
To evaluate the relative binding strength of gallium, cobalt and indium-labelled ZEGFR:2377, the half maximum inhibition concentration (IC50) were measured using 111In-DOTA- ZEGFR:2377. Monolayers of A431 cells were incubated for 4 h at 4 °C with natGa-, natCo- or natIn-DOTA-ZEGFR:2377 (0–100 nM) in the presence of 10 nM 111In-DOTA- ZEGFR:2377. After incubation, the cells were washed with media and detached with trypsin. The detached cells were collected, and the cell-associated radioactivity was measured. The IC50 values were determined using GraphPad Prism software.
The rate of internalization of 68Ga-DOTA-ZEGFR:2377 and 57Co-DOTA-ZEGFR:2377 by EGFR-expressing A431 squamous carcinoma cell during continuous incubation was studied using the acid wash method49. The labelled compound (protein concentration of 8 nM) was added to 15 petri dishes containing approximately 7 × 105 cells/dish. The cells were incubated at 37 °C in a humidified incubator. At pre-determined time points (1, 2, 3, and 4 h after incubation start for 68Ga-DOTA-ZEGFR:2377; 1, 2, 4, 8 and 24 h for 57Co-DOTA-ZEGFR:2377), the medium from a set of three dishes was removed. The cells were washed with 1 mL of ice-cold serum free medium. To collect the membrane-bound radioactivity, the cells were treated with 0.5 mL of 0.2 M glycine buffer containing 4 M urea, pH 2.0, for 5 min on ice. Dishes were washed with 0.5 mL acidic buffer followed by 1 mL PBS, and the fractions were pooled. To collect radioactivity internalized by the cells, treatment with 0.5 mL of 1 M NaOH at 37 °C for 30 min was performed. Dishes were additionally washed with 0.5 mL NaOH solution followed by 1 mL PBS, and the alkaline fractions were pooled. The percentage of internalized radioactivity was calculated for each time point.
In vivo studies
The animal experiments were planned and performed in accordance with the national regulation on laboratory animals’ protection and were approved by the Ethics Committee for Animal Research in Uppsala. Euthanasia was performed under Rompun/Ketalar anaesthesia. Female BALB/c nu/nu mice were purchased from Taconic M&B (Ry, Denmark). At the time of experiment, the animals were 10 weeks old and the average weight was 21.3 ± 0.8 g. EGFR-expressing xenografts were established by subcutaneous injection of 107 A431 cells in the right hind leg. The tumours were grown for 10–14 d. At the time of the study, the average tumour weight was 0.8 ± 0.3 g. The animals were randomized into groups of four. To test if the tumour uptake depends on EGFR expression, an additional group of mice was implanted with 107 SKOV-3 cells having very low EGFR expression. A biodistribution experiment was performed 14 days after implantation. At the time of the study, the average animal weight was 19.7 ± 0.8 g and the average tumour weight was 0.16 ± 0.03 g.
For biodistribution measurements, one group of mice was intravenously injected with 68Ga-DOTA-ZEGFR:2377 (700 kBq in 100 µL PBS per mouse) and two groups with 57Co-DOTA-ZEGFR:2377 (30 kBq in 100 µL PBS per mouse). The injected protein dose was adjusted to 40 µg/mouse by non-labelled DOTA-ZEGFR:2377. The animals were sacrificed at 3 h after injection of 68Ga-DOTA-ZEGFR:2377 and at 3 and 24 h after injection of 57Co-DOTA-ZEGFR:2377. Blood and organ samples were collected and weighed, and their radioactivity was measured. Tissue uptake was calculated as percent of injected dose per gram (% ID/g). To check the specificity of in vivo EGFR targeting, groups of four mice were subcutaneously pre-injected with 400 μg non-labelled recombinant ZHER2:342 affibody molecule before injecting 40 μg 68Ga-DOTA-ZEGFR:2377 or 57Co-DOTA-ZEGFR:2377. The control groups were sacrificed at 3 h p.i. A group of mice bearing SKOV-3 xenografts with low EGFR expression was injected with a mixture of 57Co-DOTA-ZEGFR:2377 (10 kBq per mouse) and 68Ga-DOTA-ZEGFR:2377 (700 kBq per mouse). The injected protein dose was adjusted to 40 µg/mouse by non-labelled DOTA-ZEGFR:2377. These mice were euthanized at 3 h after injection. Spectra of each sample and a standard were recorded. For each samples, radioactivity of 57Co and 68Ga were calculated by integration of counts in the energy range 10–160 keV and 300–160 keV, respectively. The data were corrected for background, gamma spectrometer dead time for each sample, 68Ga decay during measurement and spillover of 68Ga counts into 57Co energy window.
Imaging was performed to obtain a visual confirmation of the biodistribution data. Mice bearing A431 xenografts were injected with 7 MBq 68Ga-DOTA-ZEGFR:2377 or 9 MBq 57Co-DOTA-ZEGFR:2377. The injected protein dose was 40 µg/mouse. PET imaging was performed at 3 h after injection using Triumph™ Trimodality system (Gamma Medica) PET/CT device for small rodents. The CT scan was performed at the following parameters: field of view (FOV), 8 cm; magnification, 1.48; one frame and 512 projections for 2.13 min. PET data were acquired in list mode during 30 min and reconstructed using OSEM-3D. CT raw files were reconstructed by filter back projection (FBP). SPECT/CT imaging was performed using nanoScan SC (Mediso Medical Imaging Systems, Hungary) at 3 and 24 h after injection at the following parameters: CT-energy peak of 50 keV, 670 μA, 480 projections, 2.29 min acquisition time. Helical SPECT acquisition was performed using 57Co energy window (109.89 keV–134.31 keV), 110 projection and matrix of 256 × 256. The time per projection was 32 sec (totally 60 min) for imaging at 3 h and 65 sec (totally 12 min) for imaging at 24 h. CT raw files were reconstructed using Nucline 2.03 Software (Mediso Medical Imaging Systems, Hungary). SPECT raw data were reconstructed using Tera-Tomo™ 3D SPECT reconstruction technology.
Electronic supplementary material
Acknowledgements
This research was financially supported by grants from Swedish Cancer Society (Cancerfonden) and Swedish Research Council (Vetenskapsrådet). The molecular imaging work in this publication has been supported by the Wallenberg infrastructure for PET-MRI (WIPPET), a Swedish nationally available imaging platform at Uppsala University, Sweden, financed by Knut and Alice Wallenberg Foundation.
Author Contributions
J.G. - participated in production of affibody molecules, their conjugation to the chelator, radiolabelling, in vitro and in vivo characterization, in data acquisition, drafted the first version of the manuscript; K.G.A., J.L., S.S.-participated in design of conjugate, production of affibody molecules, conjugation to the chelator, purification of the conjugate, performed biochemical and biophysical characterization of non-labelled conjugate; J.H.D., B.B.O., H.T. -performed production of cobalt-55, labelling of affibody molecules with cobalt-55 and evaluation of specificity of their binding to EGFR-expressing cells, B.M., A.O.- participated in planning and performing in vivo studies, including radionuclide imaging, J.B.- performed analysis of LigandTracer data, V.T.- participated in the study design, in vivo studies, data treatment and interpretation, and coordination of the project. All co-authors revised the manuscript and approved the final variant.
Competing Interests
V.T., J.L., A.O., and S.S. are the members of the scientific advisory board of Affibody A.B. S.S. is a minority share owner of Affibody A.B. V.T., A.O. own stock in Affibody A.B. Affibody A.B. holds intellectual property rights and trademarks for Affibody molecules. J.G., K.G.A., J.H.D., B.B.O., H.T., J.B. and B.M. declare no potential conflict of interest.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-05700-7
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Avraham R, Yarden Y. Feedback regulation of EGFR signalling: decision making by early and delayed loops. Nat. Rev. Mol. Cell Biol. 2011;12:104–117. doi: 10.1038/nrm3048. [DOI] [PubMed] [Google Scholar]
- 2.Carlsson, J. EGFR-Family Expression and Implications for Targeted Radionuclide Therapy in Targeted Radionuclide Tumor Therapy-Biological Aspects (ed. Stigbrand, T. et al.) 25–58 (Springer, 2008).
- 3.Cappuzzo F, et al. Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J. Natl. Cancer Inst. 2005;97:643–655. doi: 10.1093/jnci/dji112. [DOI] [PubMed] [Google Scholar]
- 4.Hirsch FR, et al. Molecular predictors of outcome with gefitinib in a phase III placebo-controlled study in advanced non-small-cell lung cancer. J. Clin. Oncol. 2006;24:5034–5042. doi: 10.1200/JCO.2006.06.3958. [DOI] [PubMed] [Google Scholar]
- 5.Pirker R, et al. EGFR expression as a predictor of survival for first-line chemotherapy plus cetuximab in patients with advanced non-small-cell lung cancer: analysis of data from the phase 3 FLEX study. Lancet. Oncol. 2012;13:33–42. doi: 10.1016/S1470-2045(11)70318-7. [DOI] [PubMed] [Google Scholar]
- 6.Ang KK, et al. Impact of epidermal growth factor receptor expression on survival and pattern of relapse in patients with advanced head and neck carcinoma. Cancer Res. 2002;62:7350–7356. [PubMed] [Google Scholar]
- 7.Bentzen SM, et al. Epidermal growth factor receptor expression in pretreatment biopsies from head and neck squamous cell carcinoma as a predictive factor for a benefit from accelerated radiation therapy in a randomized controlled trial. J. Clin. Oncol. 2005;23:5560–5567. doi: 10.1200/JCO.2005.06.411. [DOI] [PubMed] [Google Scholar]
- 8.van Dijk LK, Boerman OC, Franssen GM, Kaanders JH, Bussink J. 111In-cetuximab-F(ab’)2 SPECT and 18F-FDG PET for prediction and response monitoring of combined-modality treatment of human head and neck carcinomas in a mouse model. J. Nucl. Med. 2015;56:287–292. doi: 10.2967/jnumed.114.148296. [DOI] [PubMed] [Google Scholar]
- 9.Niu G, Cai W, Chen K, Chen X. Non-invasive PET imaging of EGFR degradation induced by a heat shock protein 90 inhibitor. Mol. Imaging Biol. 2008;10:99–106. doi: 10.1007/s11307-007-0123-2. [DOI] [PubMed] [Google Scholar]
- 10.Corcoran EB, Hanson RN. Imaging EGFR and HER2 by PET and SPECT: a Review. Med. Res. Rev. 2014;4:596–643. doi: 10.1002/med.21299. [DOI] [PubMed] [Google Scholar]
- 11.Divgi CR, et al. Phase I and imaging trial of indium 111-labeled anti-epidermal growth factor receptor monoclonal antibody 225 in patients with squamous cell lung carcinoma. J. Natl. Cancer Inst. 1991;83:97–104. doi: 10.1093/jnci/83.2.97. [DOI] [PubMed] [Google Scholar]
- 12.Ahlgren. S, Tolmachev V. Radionuclide molecular imaging using Affibody molecules. Curr. Pharm. Biotechnol. 2010;11:581–589. doi: 10.2174/138920110792246609. [DOI] [PubMed] [Google Scholar]
- 13.Sörensen J, et al. First-in-human molecular imaging of HER2 expression in breast cancer metastases using the 111In-ABY-025 affibody molecule. J. Nucl. Med. 2014;55:730–735. doi: 10.2967/jnumed.113.131243. [DOI] [PubMed] [Google Scholar]
- 14.Sörensen J, et al. Measuring HER2-Receptor Expression In Metastatic Breast Cancer Using [68Ga]ABY-025 Affibody PET/CT. Theranostics. 2016;6:262–271. doi: 10.7150/thno.13502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tolmachev V, et al. Imaging of EGFR expression in murine xenografts using site-specifically labelled anti-EGFR 111In-DOTA-Z EGFR:2377 Affibody molecule: aspect of the injected tracer amount. Eur. J. Nucl. Med. Mol. Imaging. 2010;37:613–622. doi: 10.1007/s00259-009-1283-x. [DOI] [PubMed] [Google Scholar]
- 16.Tolmachev V, Orlova A. Influence of labelling methods on biodistribution and imaging properties of radiolabelled peptides for visualisation of molecular therapeutic targets. Curr. Med. Chem. 2010;17:2636–2655. doi: 10.2174/092986710791859397. [DOI] [PubMed] [Google Scholar]
- 17.Eisenwiener KP, et al. NODAGATOC, a new chelator-coupled somatostatin analogue labeled with [67/68Ga] and [111In] for SPECT, PET, and targeted therapeutic applications of somatostatin receptor (hsst2) expressing tumors. Bioconjug. Chem. 2002;13:530–541. doi: 10.1021/bc010074f. [DOI] [PubMed] [Google Scholar]
- 18.Antunes P, et al. Are radiogallium-labelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur. J. Nucl. Med. Mol. Imaging. 2007;34:982–993. doi: 10.1007/s00259-006-0317-x. [DOI] [PubMed] [Google Scholar]
- 19.Decristoforo C, et al. 68Ga- and 111In-labelled DOTA-RGD peptides for imaging of alphavbeta3 integrin expression. Eur. J. Nucl. Med. Mol. Imaging. 2008;35:1507–1515. doi: 10.1007/s00259-008-0757-6. [DOI] [PubMed] [Google Scholar]
- 20.Dumont RA, et al. Novel (64)Cu- and (68)Ga-labeled RGD conjugates show improved PET imaging of α(ν)β(3) integrin expression and facile radiosynthesis. J. Nucl. Med. 2011;52:1276–1284. doi: 10.2967/jnumed.111.087700. [DOI] [PubMed] [Google Scholar]
- 21.Varasteh Z, et al. Synthesis and characterization of a high-affinity NOTA-conjugated bombesin antagonist for GRPR-targeted tumor imaging. Bioconjug. Chem. 2013;24:1144–1153. doi: 10.1021/bc300659k. [DOI] [PubMed] [Google Scholar]
- 22.Heppeler A, et al. Metal-ion-dependent biological properties of a chelator-derived somatostatin analogue for tumour targeting. Chemistry. 2008;14:3026–3034. doi: 10.1002/chem.200701264. [DOI] [PubMed] [Google Scholar]
- 23.Honarvar, H. et al. Position for site-specific attachment of a DOTA chelator to synthetic affibody molecules has a different influence on the targeting properties of 68Ga- compared to 111in-labeled conjugates. Mol. Imaging13 (2014). [DOI] [PubMed]
- 24.Honavar H, et al. Evaluation of the first 44Sc-labeled Affibody molecule for imaging of HER2-expressing tumors. Nucl. Med. Biol. 2016;45:15–21. doi: 10.1016/j.nucmedbio.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Wållberg H, Ahlgren S, Widström C, Orlova A. Evaluation of the radiocobalt-labeled [MMA-DOTA-Cys61]-Z HER2:2395(-Cys) affibody molecule for targeting of HER2-expressing tumors. Mol. Imaging Biol. 2010;12:54–62. doi: 10.1007/s11307-009-0238-8. [DOI] [PubMed] [Google Scholar]
- 26.Thisgaard H, Olesen ML, Dam JH. Radiosynthesis of 55Co- and 58mCo-labelled DOTATOC for positron emission tomography imaging and targeted radionuclide therapy. J. Label. Compd. Radiopharm. 2011;54:758–762. doi: 10.1002/jlcr.1919. [DOI] [Google Scholar]
- 27.Dam JH, Olsen BB, Baun C, Høilund-Carlsen PF, Thisgaard H. In Vivo Evaluation of a Bombesin Analogue Labeled with Ga-68 and Co-55/57. Mol. Imaging. Biol. 2016;18:368–376. doi: 10.1007/s11307-015-0911-z. [DOI] [PubMed] [Google Scholar]
- 28.Thisgaard H, et al. F. Evaluation of cobalt-labeled octreotide analogs for molecular imaging and auger electron-based radionuclide therapy. J. Nucl. Med. 2014;55:1311–1316. doi: 10.2967/jnumed.114.137182. [DOI] [PubMed] [Google Scholar]
- 29.Tolmachev V, et al. Affibody molecules for epidermal growth factor receptor targeting in vivo: aspects of dimerization and labeling chemistry. J. Nucl. Med. 2009;50:274–283. doi: 10.2967/jnumed.108.055525. [DOI] [PubMed] [Google Scholar]
- 30.Zaman MR, Spellerberg S, Qaim SM. Production of 55Co via the 54Fe(d, n)-process and excitation functions of 54Fe(d, t)53Fe and 54Fe(d, α)52mMn reactions from threshold up to 13.8MeV. Radiochim. Acta. 2003;91:105–108. doi: 10.1524/ract.91.2.105.19991. [DOI] [Google Scholar]
- 31.Velikyan I, et al. Preparation and evaluation of (68)Ga-DOTA-hEGF for visualization of EGFR expression in malignant tumors. J. Nucl. Med. 2005;46:1881–1888. [PubMed] [Google Scholar]
- 32.Li W, et al. PET imaging of EGF receptors using [18F]FBEM-EGF in a head and neck squamous cell carcinoma model. Eur. J. Nucl. Med. Mol. Imaging. 2012;39:300–308. doi: 10.1007/s00259-011-1969-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cuartero-Plaza A, et al. Radiolocalization of squamous lung carcinoma with 131I-labeled epidermal growth factor. Clin. Cancer Res. 1996;2:13–20. [PubMed] [Google Scholar]
- 34.Cai W, et al. Quantitative PET of EGFR expression in xenograft-bearing mice using 64Cu labeled cetuximab, a chimeric anti-EGFR monoclonal antibody. Eur. J. Nucl. Med. Mol. Imaging. 2007;34:850–858. doi: 10.1007/s00259-006-0361-6. [DOI] [PubMed] [Google Scholar]
- 35.Li WP, Meyer LA, Capretto DA, Sherman CD, Anderson CJ. Receptor-binding, biodistribution, and metabolism studies of 64Cu-DOTAcetuximab, a PET-imaging agent for epidermal growth-factor receptor-positive tumors. Cancer Biother. Radiopharm. 2008;23:158–171. doi: 10.1089/cbr.2007.0444. [DOI] [PubMed] [Google Scholar]
- 36.Nayak TK, et al. PET imaging of HER1-expressing xenografts in mice with 86Y-CHX-A”-DTPA-cetuximab. Eur. J. Nucl. Med. Mol. Imaging. 2010;37:1368–1376. doi: 10.1007/s00259-009-1370-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nayak TK, Garmestani K, Baidoo KE, Milenic DE, Brechbiel MW. Preparation, biological evaluation, and pharmacokinetics of the human anti-HER1 monoclonal antibody panitumumab labeled with 86Y for quantitative PET of carcinoma. J. Nucl. Med. 2010;51:942–950. doi: 10.2967/jnumed.109.071290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aerts HJ, et al. Disparity between in vivo EGFR expression and 89Zr-labeled cetuximab uptake assessed with PET. J. Nucl. Med. 2009;50:123–31. doi: 10.2967/jnumed.108.054312. [DOI] [PubMed] [Google Scholar]
- 39.Chang AJ, De Silva RA, Lapi SE. Development and characterization of 89Zr-labeled panitumumab for immuno-positron emission tomographic imaging of the epidermal growth factor receptor. Mol. Imaging. 2013;12:17–27. [PMC free article] [PubMed] [Google Scholar]
- 40.Miao Z, Ren G, Liu H, Jiang L, Cheng Z. Small-animal PET imaging of human epidermal growth factor receptor positive tumor with a 64Cu labeled affibody protein. Bioconjug. Chem. 2010;21:947–954. doi: 10.1021/bc900515p. [DOI] [PubMed] [Google Scholar]
- 41.Miao Z, et al. PET of EGFR expression with an 18F-labeled affibody molecule. J. Nucl. Med. 2012;53:1110–1118. doi: 10.2967/jnumed.111.100842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Su X, et al. Comparison of two site-specifically (18)F-labeled affibodies for PET imaging of EGFR positive tumors. Mol. Pharm. 2014;11:3947–3956. doi: 10.1021/mp5003043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garousi J, et al. PET imaging of epidermal growth factor receptor expression in tumours using 89Zr-labelled ZEGFR:2377 affibody molecules. Int. J. Oncol. 2016;48:1325–32. doi: 10.3892/ijo.2016.3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jauw YW, et al. Immuno-Positron Emission Tomography with Zirconium-89-Labeled Monoclonal Antibodies in Oncology: What Can We Learn from Initial Clinical Trials? Front. Pharmacol. 2016;7:131. doi: 10.3389/fphar.2016.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Makris NE, et al. PET/CT-derived whole-body and bone marrow dosimetry of 89Zr-cetuximab. J. Nucl. Med. 2015;56:249–254. doi: 10.2967/jnumed.114.147819. [DOI] [PubMed] [Google Scholar]
- 46.Laforest R, et al. [89Zr]Trastuzumab: Evaluation of Radiation Dosimetry, Safety, and Optimal Imaging Parameters in Women with HER2-Positive Breast Cancer. Mol. Imaging. Biol. 2016;18:952–959. doi: 10.1007/s11307-016-0951-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Braad PE, Hansen SB, Thisgaard H, Høilund-Carlsen PF. PET imaging with the non-pure positron emitters: (55)Co, (86)Y and (124)I. Phys. Med. Biol. 2015;60:3479–3497. doi: 10.1088/0031-9155/60/9/3479. [DOI] [PubMed] [Google Scholar]
- 48.Barta P, et al. Protein interactions with HER-family receptors can have different characteristics depending on the hosting cell line. Int. J. Oncol. 2012;40:1677–1682. doi: 10.3892/ijo.2011.1307. [DOI] [PubMed] [Google Scholar]
- 49.Wållberg H, Orlova A. Slow internalization of anti-HER2 synthetic affibody monomer 111In-DOTA-ZHER2:342-pep2: implications for development of labeled tracers. Cancer Biother. Radiopharm. 2008;23:435–442. doi: 10.1089/cbr.2008.0464. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


