Abstract
Empathy is a complex cognitive and affective process that allows humans to experience concern for others, comprehend their emotions, and eventually help them. In addition to studies with healthy subjects and various neuropsychiatric populations, a few reports have examined this domain focusing on mental health workers, whose daily work requires the development of a saliently empathic character. Building on this research line, the present population-based study aimed to (a) assess different dimensions of empathy for pain in mental health workers relative to general-physicians and non-medical workers; and (b) evaluate their relationship with relevant factors, such as moral profile, age, gender, years of experience, and workplace type. Relative to both control groups, mental health workers exhibited higher empathic concern and discomfort for others’ suffering, and they favored harsher punishment to harmful actions. Furthermore, this was the only group in which empathy variability was explained by moral judgments, years of experience, and workplace type. Taken together, these results indicate that empathy is continuously at stake in mental health care scenarios, as it can be affected by contextual factors and social contingencies. More generally, they highlight the importance of studying this domain in populations characterized by extreme empathic demands.
Introduction
Empathy is a complex construct, which entails feeling concern for others, sharing and comprehending their emotions, prompting motivation to help them1, 2. Rather than a unified domain, empathy represents a complex socio- cognitive competence encompassing various interacting components, such as affective sharing and perspective taking3–5. Moreover, empathy is a flexible capacity which becomes modulated by different cognitive, social, and contextual determinants5, 6. In addition to studies on healthy subjects7–15 and various neuropsychiatric populations16–18, a few reports have examined this domain focusing on professionals whose daily work particularly taxes empathic abilities, such as social workers, nurses, and physicians19–21. Building on this research line, the present population-based study assessed different dimensions of empathy in mental health workers (MHWs) and their relationship with socio-cognitive, demographic, and work-related factors.
Empathy skills in medical practice are continuously at stake. The work of physicians requires understanding the patients’ thoughts and emotional experiences, as well as effectively communicating their comprehension19, 20, 22–24. In this context, empathic skills emerges as a highly desirable trait25, since they foster trust26, 27, patient satisfaction28, diagnosis efficacy21, and, ultimately, treatment adherence and success29–31.
This proves particularly critical for mental health workers32. Psychologists and psychiatrists require highly empathic communication to understand and address their patients’ suffering. Karl Jaspers introduced empathy as a tool for psychopathological assessment more than a century ago33. Indeed, such a skill constitutes a cornerstone of all psychotherapeutic approaches, including psychodynamic34, 35, cognitive-behavioral3, and group psychotherapy36 approaches.
In medical contexts, empathy is modulated by several factors. For instance, this domain may be sensitive to the physicians’ moral profile, as low levels empathic concern predict utilitarian moral judgment in this population37–39. Furthermore, moral competence physicians and nurses seems to decrease as a function of age and years of experience40, 41. Thus, moral profile may also emerge as a key modulator of empathic dimensions in mental health workers.
Empathy also varies as a function of demographic factors. In physicians, these include gender19, expertise13, and workplace type24, 42. For instance, female medical workers showed higher scores than their male counterparts in self-reports of empathy. Concerning expertise, empathic sensitivity seems to decrease in the last stages of medical training19, 43, although experienced doctors can then recover their empathic behavior, arguably due to a reduction of personal distress44, 45. Arguably, medical workers with more than 10 years of experience, which is a criterion for being considered as experts or proficient practitioners, might present changes in clinical empathy46, 47. Finally, previous studies in general-physicians and nurses have explored empathy levels associated to workplace type35, 36. Those studies have shown that physicians working at inpatient environments report lower empathic reactivity than those in ambulatory environments. Arguably, medical professionals that work at ambulatory environments have more private and confident spaces, favoring the trust and welfare of patients24, 42, 48. In addition, medical professionals at inpatient contexts experience enhanced stress levels and have more risk of burnout syndromes, which could eventually affect empathy skills24, 48–50.
In sum, while clinical empathy seems sensitive to various factors, no study has explored this issue with a focus on mental health workers. Moreover, available results stem from relatively small samples completing self-report empathy questionnaires (which may be strongly biased by social expectations)19, 51–53. To address this issue, we conducted a population-based study aimed to (a) assess different dimensions of empathy for pain in mental health workers (MHWs) relative to a group of physicians (general-physicians) and non-medical workers; and (b) evaluate their relationship with relevant factors, such a moral profile, age, gender, years of experience, and workplace type. In particular, to circumvent the biases inherent to self-report measures or empathy scales, we used a validated empathy-for-pain task (EPT)17, 18, 54–56 tapping into cognitive, affective, and moral aspects of empathy. The EPT evaluates various dimensions of empathy in scenarios featuring intentional and accidental harm. The EPT employed here comprises 11 animated scenarios (4 intentional, 4 accidental, 3 neutral) involving two individuals. In this version, participants were asked to respond five questions for each scenario, i.e., (a) purpose comprehension (was the action done on purpose?), (b) empathic concern (how sad do you feel for the victim?), (c) degree of discomfort (how upset do you feel for what happened in the situation?), (d) intention to harm (how bad was the intention?), and (e) punishment (how much penalty does this action deserve?) (see Supplementary information for a further review of the EPT).
We hypothesized that MHWs, compared to both other groups, would exhibit higher empathy scores in all empathic domains. Furthermore, we predicted that the empathic profile of MHWs would be sensitive to factors such as morality, gender, years of experience. In addition, we predicted that workplace type (i.e., working at inpatient vs. ambulatory environments) could affect the empathic profile of MHWs. Considering that previous studies in general-physicians and nurses showed that workplace type modulates empathy, MHWs working at ambulatory environments should exhibit enhanced empathic skills relative to those working at inpatient environments. In short, we aimed to illuminate the interplay between empathy and various socio-professional factors in a population characterized by critical reliance on this domain.
Materials and Methods
Participants
The study comprised 1,109 individuals (567 women) with a mean age of 37.61 (SD = 12.5). All participants were professionals who accessed Intramed (www.intramed.net), an online portal designed for the healthcare community. The sample of MHWs (n = 377) was composed of 185 psychiatrists and 192 psychologists from 9 (nine) Latin-American countries (Argentina, Mexico, Colombia, Peru, Ecuador, Uruguay, Chile, Paraguay, Bolivia). The group of general-physicians included 402 individuals without medical residence, and the group of non-medical workers comprised 330 workers with no clinical experience who work in the fields of administration, economy, engineering, and social service. The participant’s age across groups ranged from 21 to 70 years. No significant differences were observed between groups in terms of gender (X2 (1) = 1.2, p > 0.1), age (F (1, 1035) = 0.22, p = 0.79), years of experience (F (1, 1035) = 0.41, p = 0.66), or workplace type (X2 (1) = 0.7, p = 0.39).
In a separate small-scale experiment, we have assessed another group of empathy domains with the interpersonal reactivity index (IRI), a widely used tool tapping different dimensions of affective and cognitive empathy57. In particular, we examined the extent to which empathic concern is related to personal distress and whether empathic concern and discomfort domains measured with the EPT coincide with the measures tracked by the IRI. To this end, we tested a group of 30 mental health workers, a group of 42 general-physicians, and a group of 28 non-medical workers.
All participants completed the survey and the experimental tasks in full and within a reasonable time (approximately 25 min). All subjects participated voluntarily by accepting an invitation posted on the main page of their Intramed profiles, and they gave informed consent in accordance with the Declaration of Helsinki by pressing an “I agree” button beneath an explanatory letter. Potential respondents were informed of the anonymity of their responses. All procedures performed in this study were approved by research committee and Ethics Committee of Javeriana University (Bogotá, Colombia) and Institute of Cognitive Neurology INECO (Buenos Aires Argentina).
All procedures in this study were conducted in accordance with the relevant guidelines and regulations of the Declaration of Helsinki.
Instruments and procedure
On the first page of the online survey, participants reported their age, gender, occupation, workplace type (hospital or ambulatory service). Next, they completed a series of tasks, as described below.
Empathy for pain task
We used a modified version of a previously reported EPT16–18, 54–56, which evaluates various dimensions of empathy in scenarios featuring intentional and accidental harm (for a further review of EPT procedure see Supplementary Information section 1.1).
Moral judgment
Participants were also presented with two moral dilemmas58, 59, namely, an impersonal one (the standard trolley dilemma) and a personal one (the footbridge dilemma). We also included one non-moral dilemma for comparison purposes. In this dilemma participants were asked to choose whether to travel by bus or train given certain time constraints (see more details of moral judgment evaluation in Supplementary Information section 1.2).
Interpersonal Reactivity Index
The IRI is a widely used tool for the multi-dimensional assessment of empathy57. This self-report instrument comprises 28 items answered on 5-point Likert scales ranging from “Does not describe me well” to “Describes me very well”. The tool is composed by four subscales, which explore different empathy domains, namely: (i) perspective taking (the tendency to spontaneously adopt the psychological point of view of others), (ii) fantasy (the tendency to imaginatively transpose oneself into the feelings and actions of fictitious characters in books, movies, and plays), (iii) empathic concern (“other-oriented” feelings of sympathy and concern for misfortunes befalling others), and (iv) personal distress (“self-oriented” feelings of personal anxiety and unease in tense interpersonal settings).
Data analysis
Demographic data were compared among groups with ANOVA tests, except for categorical variables, which were analyzed through X2 tests. MANOVAs were run to explore group differences in empathic domains (each domain was considered as a dependent variable).
The ratings for each empathic measure were analyzed with factorial ANOVAS.
In addition, as in previous studies16–18, 54, 55, after MANOVA analyses, the ratings for each empathy measure (i.e., purpose comprehension, empathic concern, discomfort, intention to hurt and punishment) were independently analyzed through a factorial ANOVA. In each ANOVA we introduced condition (intentional harm, accidental harm and neutral situations) as a within-subject factor, and group (MHWs, general-physicians and non-medical workers) as a between-subject factor. In addition, each demographic factor (gender, age, years of experience, and workplace type) was introduced as a between-subject factor. We ran an independent analysis for each demographical factor (age, gender, workplace type, years of experience) to avoid mixed effects attributed to interactions between demographic factors, which correlate with each other. We reported only those contrasts between condition, group, and demographical factors that reached significance. When a significant interaction between group and condition was found, we examined between-group differences in ratings using Tukey’s HSD post-hoc test. Differences among conditions (intentional harm, accidental harm, and neutral situations) for each rating (purpose comprehension, empathic concern, discomfort, intention to hurt, punishment) were also examined with Tukey’s HSD post-hoc tests. Eta squared (n2) was used as a measure of effect size for significant effects. In the results section we reported Eta squared (n2) values for each significant p-value. Note that Eta squared is only available for ANOVAS main effects of interactions, but not for their post hoc comparisons (because the values are already considering the sum of squares obtained with the all ANOVAs combined effects).
Following a procedure reported in previous studies18, 60, we conducted multiple regression analyses to explore whether context factors (including gender, age, years of experience, workplace type) and responses to moral judgments partially explained performance on the EPT in each group. We considered as dependent variables all measures yielding group differences across conditions (intentional harm, accidental harm, neutral situations). Thus, we ran independent models for purpose comprehension, empathic concern, discomfort, intention to hurt, and punishment. Different demographical factors, including gender, age, workplace type, years of experience, and responses to personal and impersonal moral dilemmas, were introduced as predictors in all regression models.
For multiple regression analyses, multicollinearity of independent variables was assessed using variance inflation factors (VIFs) with a reference value of 3 before interpreting the final output61. Moral judgments, workplace type, and years of experience were introduced as dummy variables in the regression models. Thus, the moral judgment in the personal and impersonal dilemmas was coded with 0 when participants assigned utilitarian responses. Thus, positive values of beta were interpreted as a positive relationship between deontological judgments in moral dilemmas and the empathic measures. For workplace type, the variable was coded with 0 when participants had mainly worked in an inpatient environment and coded with 1 when participants had mainly worked at ambulatory environments. Negative values of beta were interpreted as greater empathic scores in ambulatory environments. Finally, participants were classified depending on whether they had more or less than 10 years of experience. This criterion was used considering evidence that medical workers change their empathic skills after 10 years of experience46, 47. Thus, for years of experience, the variable was coded with 0 when participants reported less than 10 years of experience. Negative values of beta were interpreted as greater empathic scores in subjects with more than 10 years of experience. Participants were classified depending on whether they had more or less than 10 years of experience. This criterion was used considering evidence that medical workers change their empathic skills after 10 years of experience46, 47. (for a further review of data analysis see Supplementary Information section 2).
Results
Group differences in empathy measures
A MANOVA analysis using the empathy domains as dependent variables (Purposely, EC, discomfort, intention to hurt and punishment) and group as between factor (MHW, general-physicians and non-medical professionals) revealed that the groups of subjects in each profession exhibited significant differences in empathy domains tracked with EPT Wilk’s (Wilk’s Lambda = 12.71) (F (36, 372) = 25.51, p < 0.0001, η2 = 0.21). This result allowed us to perform additional ANOVAS over each dependent variable of the EPT.
ANOVA analyses over purpose comprehension revealed no interactions between group and condition (F (4, 2216) = 1.12, p = 0.35) nor triple interactions between empathy condition, group, and demographic measures [gender (F (2, 2216) = 0.18, p = 0.94), age (F (16, 2216) = 0.63, p = 0.85), years of experience (F (2, 2216) = 1.02, p = 0.43), or workplace type (F (2, 2216) = 1.46, p = 0.13)].
Regarding empathic concern, results revealed a significant interaction between group and condition (F (4, 2216) = 16.10, p = 0.001, η2 = 0.1) for intentional harm. A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that MHW provided higher empathic concern ratings for intentional harm than general-physicians group (p < 0.01) and non-medical workers (p < 0.01). No other differences were observed in scores for accidental harm and neutral situations between groups (all ps > 0.4) (see Fig. 1).
Figure 1.
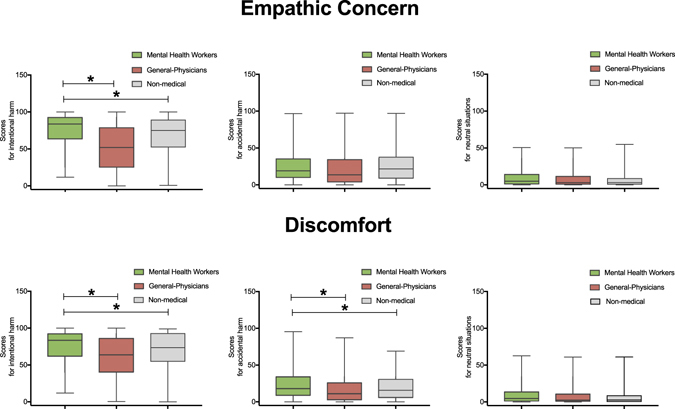
Ratings in empathic concern and discomfort domains in each group. This graph depicts ratings in two empathic measures (Empathic concern and Discomfort) by each condition (intentional and accidental harm and neutral situations) by each group. Stars indicate significant differences (p < 0.01).
Results for this empathy measure also revealed a triple interaction between empathy condition (intentional harm, accidental harm, neutral situations), group (MHWs, general-physicians, non-medical workers), and workplace type (F (2, 2216) = 2.46, p = 0.01, η2 = 0.06). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that MHWs provided higher empathic concern ratings for intentional harm in environments of ambulatory practice than in hospitals (p < 0.01). No differences due to workplace type were observed in general-physicians group or non-medical workers. No interactions were found when experience factor was analyzed.
As regards discomfort ratings, a significant interaction was observed between group and condition (F (4, 2216) = 11.59, p < 0.01, η2 = 0.11). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that MHWs provided higher ratings for intentional harm than general-physicians (p < 0.01) and non-medical workers (p < 0.01). Moreover, post-hoc analysis revealed that MHWs provided higher scores for accidental harm than general-physicians (p < 0.05) and non-medical workers (p < 0.05). No differences were observed between the latter two groups (p = 0.23 for intentional harm, and p = 0.33 for accidental harm) (see Fig. 1). No between-group differences were observed in scores for neutral situations (all ps > 0.3).
For the discomfort measure, an interaction emerged between condition (intentional harm, accidental harm and neutral situations), group (MHWs, general-physicians, non-medical workers), and years of experience (F (2, 2216) = 5.46, p = 0.01, η2 = 0.07). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that in the MHWs, those professionals with more than 10 years of experience provided lower discomfort ratings than workers with less than 10 years of experience (p < 0.01). Post-hoc analyses did not reveal other significant effects (no differences were observed for general-physicians or non-medical group (all ps > 0.3). In addition, a triple interaction was observed between condition, group, and workplace for this measure (F (2, 2216) = 4.16, p = 0.01, η2 = 0.08). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that workers in MHWs provided higher discomfort ratings for intentional and accidental harm in ambulatory environments than in hospitals (all ps < 0.01). Post hoc analyses did not reveal other significant effects (no differences were observed for general-physicians or non-medical workers (all ps > 0.5).
Regarding intention to hurt, we found a significant interaction between group and condition (F (4, 2216) = 7.43, p < 0.01, η2 = 0.07). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that MHWs provided higher ratings for intentional harm than general-physicians (p < 0.01) and non-medical workers (p < 0.01). No differences were observed between the latter two groups (p = 0.31) (see Fig. 2). No other differences were observed in scores for accidental harm and neutral situations between groups (all p > 0.2).
Figure 2.
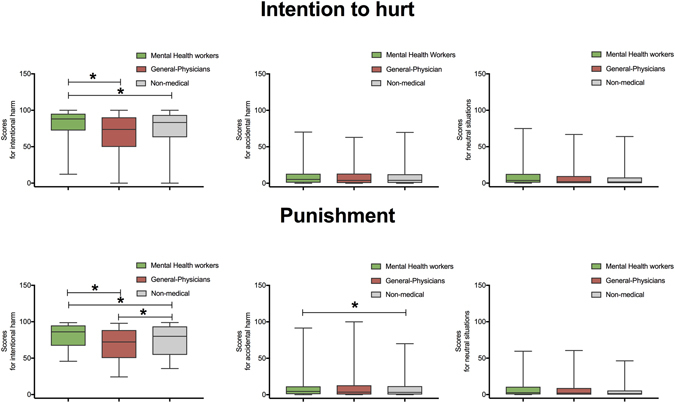
Ratings in intention to hurt and punishment domains in each group. This graph depicts ratings in two empathic measures (Intention to hurt and Punishment) by each condition (intentional and accidental harm and neutral situations) by each group. Stars indicate significant differences (p < 0.01).
For the intention to hurt measure, a triple interaction was observed between condition (intentional harm, accidental harm and neutral situations, group (MHWs, general-physicians and non-medical workers), and years of experience (F (2, 2216) = 2.46, p = 0.01, η2 = 0.06). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that in the MHWs, workers with more than 10 years of experience provided lower intention to hurt ratings for intentional harm than workers with less than 10 years of experience (p < 0.01). No other contrasts yielded significant effects (no differences were observed neither for general-physicians or non-medical workers (all ps > 0.2). Additionally, for this measure a triple interaction emerged between condition, group, and workplace type (F (2, 2216) = 3.16, p < 0.05, η2 = 0.06). Post-hoc analyses (Tukey HSD, MS = 108.76, df = 2216) showed that MHWs working in ambulatory environments had higher intention to hurt scores than those working at hospitals (all ps < 0.01). Post hoc-analyses did not reveal other significant effects (no differences were observed in general-physicians or in non-medical workers (all ps > 0.3).
Finally, regarding the punishment measure, we observed an interaction between group and condition (F (4, 2216) = 5.23, p < 0.01, η2 = 0.06). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that MHWs provided higher ratings for intentional harm than general-physicians (p < 0.001). In addition, non-medical workers provided higher scores than general-physicians (p < 0.01) (see Fig. 2). Moreover, post-hoc analyses revealed that MHWs provided higher punishment scores for accidental harm than non-medical workers (p < 0.05).
In addition, for the punishment measure, we observed a triple interaction between condition (intentional harm, accidental harm and neutral situations), group (MHWs, general-physicians, non-medical workers), and years of experience (F (2, 2216) = 6.32, p = 0.01, η2 = 0.07). A post-hoc analysis (Tukey HSD, MS = 108.76, df = 2216) showed that MHWs with more than 10 years of experience provided lower punishment ratings than workers with less of 10 years of experience (p < 0.01). No other analyses yielded significant effects (no differences were observed in general-physicians or in non-medical workers (all ps > 0.42). No interactions were found when workplace type was analyzed.
In sum, we observed higher scores for intentional harm in MHWs than in both other groups. This was the case in various measures, including empathic concern, discomfort, intention to hurt, and punishment. Also, more experienced MHWs presented lower scores in empathy than less-experienced ones. Finally, those working in ambulatory context presented higher empathy scores in discomfort and intention to hurt than those working at hospitals.
Group differences in empathy measures using IRI scale in a subsample of subjects
In a separate small-scale experiment, we have assessed another group of empathy domains with the interpersonal reactivity index (IRI). To this end, we tested 30 mental health workers, 42 general-physicians, and 28 non-medical participants. We calculated MANOVAs using the empathy domains of IRI as dependent variables (fantasy, EC, PD, and perspective-taking) and group as between factor (MHW, general-physicians and non-medical professionals). Results revealed between-group differences in empathy domains tracked with IRI (Wilk’s Lambda = 0.842) (F (8, 150) = 2.52, p < 0.05, η2 = 0.08). This result allowed us to perform additional ANOVAs over each dependent variable of the IRI. A one-way ANOVA revealed that MHWs exhibited higher EC scores than general-physicians and non-medical workers (F (2, 77) = 4.07, p < 0.05, η2 = 0.12). The analyses also showed higher perspective-taking scores in MHWs than in other groups (F (2, 77) = 2.07, p < 0.05, η2 = 0.06). Analyses over PD (F (2, 77) = 1.25, p = 0.27) and fantasy (F (2, 77) = 0.58, p = 0.71) scores did not reveal significant differences between groups.
Moral judgment among groups
Impersonal dilemma
Most participants (929 = 81.9%) delivered a utilitarian response (i.e., yes, flip the switch), and 106 (18.01%) delivered a non-utilitarian response. No significant differences were found between groups (X2 (2) = 1.72, p = 0.19, Cramer’s V = 0.02) (see Fig. 3).
Figure 3.
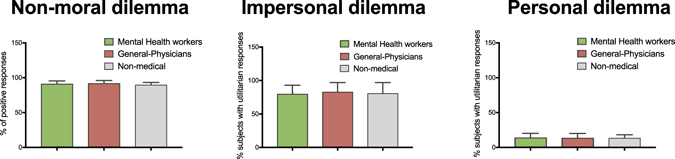
Responses to moral dilemmas in each group. This graph shows percentages of positive responses for the non-moral dilemma, utilitarian and no-utilitarian responses in impersonal and personal dilemmas according to group.
Personal dilemma
A small proportion of participants (158, 13.9%) delivered a utilitarian response (i.e., yes, push the man). Most of them (877, 86.01%) delivered a non-utilitarian response (i.e., no, don’t push the man). No significant differences were found between groups (X2 (2) = 1.34, p = 0.51, Cramer’s V = 0.02) (see Fig. 3).
Non-moral dilemma
A total of 1015 (91.3%) participants provided a positive response to the non-moral dilemma. No significant differences were found between groups (X2 (2) = 2.7, p = 0.24, Cramer’s V = 0.03) (see Fig. 3).
The relationship between moral judgment and empathy domains in each group
We analyzed the extent to which moral judgments determine empathy ratings in each group. First, we studied the relationship between empathy and moral judgment in MHWs. To this end, we implemented regression models using each significant empathic measure as a dependent variable, and responses to impersonal and personal dilemmas as independent variables. Models over purpose comprehension for intentional and accidental harm did not reveal significant effects. A multiple regression model using empathic concern ratings for intentional harm (F (1, 372) = 3.99, p < 0.01, R2 = 0.01) showed that responses to the personal dilemma (beta = 1.33, p < 0.01, η2 = 0.07) directly explained variance of empathic concern ratings. A model over empathic concern for accidental harm did not yield significant differences.
A new model (F (1, 372) = 4.21, p < 0.01, R2 = 0.02) revealed that responses to the impersonal dilemma (beta = 1.37, p < 0.01, η2 = 0.07) directly explained discomfort ratings for intentional harm. Models over discomfort ratings for accidental harm did not reveal significant differences. As regards intention to hurt, a model for intentional harm (F (1, 372) = 5.29, p < 0.01, R2 = 0.02) showed that responses to personal dilemma (beta = 1.42, p < 0.01, η2 = 0.08) directly explained intention to hurt ratings. Subjects who provided utilitarian responses to personal dilemma had lower scores in intention to hurt ratings than those with deontological responses.
Regression models for intention to hurt for accidental harm did not reach significant values. Models for punishment ratings for intentional and accidental harm did not reveal significant effects. In sum, results from models revealed an inverse relationship between responses to empathy measures including empathic concern, discomfort, intention to hurt, and utilitarian responses to moral dilemmas.
The relationship between moral judgments and empathy was also analyzed in both control groups (general-physicians and non-medical). Results in general-physicians revealed an inverse relationship between responses to empathic concern and utilitarian responses to impersonal moral dilemmas. Results in non-medical workers did not reach significant differences (for a further description see Supplementary Information section 3.1).
Factors determining empathy ratings in MHWs
Different regression models were run using each significant empathic measure as a dependent variable and demographic variables (age, gender, years of experience, and workplace type) as independent variables. A first regression model over purpose comprehension ratings (F (4, 372) = 0.46, p = 0.64, R2 = 0.001) yielded no significant effects. The same was true of models analyzing purpose comprehension ratings for accidental harm and neutral situations.
A multiple regression model (F (4, 372) = 4.22, p < 0.01, R2 = 0.08) showed that years of experience (beta = −0.27, p < 0.01, η2 = 0.09) and workplace type (beta = −0.17, p < 0.05, η2 = 0.06) were associated with empathic concern ratings for intentional harm. Analyses revealed that those subjects with more years of experience (>10 years) had lower empathic concern scores than those with less experience (<10 years). In addition, subjects working at hospitals had lower empathic concern scores than those working in ambulatory settings. No significant differences were revealed by models of empathic concern ratings for accidental harm or for neutral situations (see Figs 4 and 5).
Figure 4.
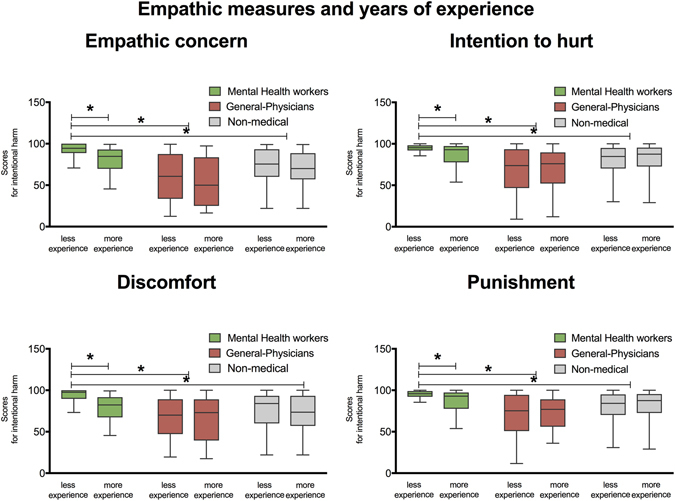
Relationship between empathic domains and years of experience. This graph shows the interaction between empathy measures and years of experience (i.e., less experience: (less than 10 years); high experience: (more than 10 years). Left part of graph shows differences between groups in affective empathy measures: Empathic Concern and Discomfort. The right of the graph shows group differences in moral-cognitive empathy measures: Intention to hurt and Punishment. Stars indicate significant differences at p < 0.01.
Figure 5.
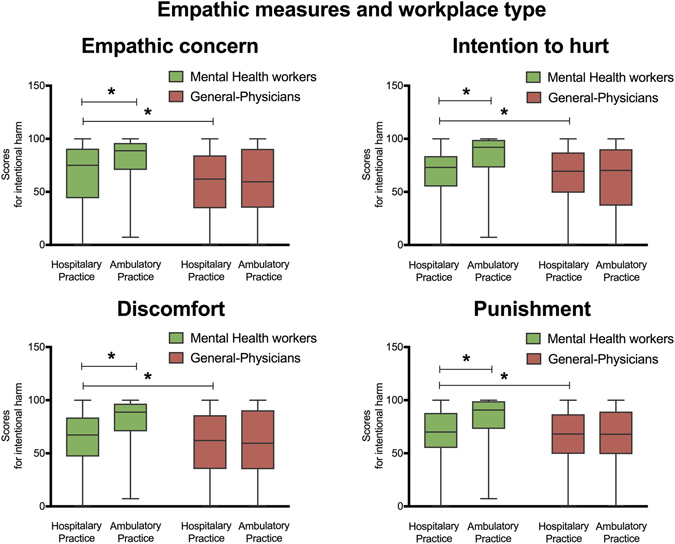
Relationship between empathic domains and workplace type. Graph shows the interaction between empathy measures and workplace type (i.e., hospital practice and ambulatory practice). Left part of graph shows differences between groups in affective empathy measures: Empathic Concern and Discomfort. The right of the graph shows group differences in moral-cognitive empathy measures: Intention to hurt and Punishment. Stars indicate significant differences at p < 0.01.
A model over discomfort ratings for intentional harm (F (4, 372) = 4.89, p < 0.001, R2 = 0.09) showed that such a variable was explained by years of experience (beta = −0.22, p < 0.001, η2 = 0.07) and workplace type (beta = −0.19, p < 0.05, η2 = 0.07). Subjects with more years of experience and working at hospitals had lower discomfort scores. Regression models over discomfort ratings for accidental harm and for neutral situations did not reach significant values (see Figs 4 and 5).
As regards intention to hurt ratings, a multiple regression model (F (4, 372) = 5.04, p < 0.001, R2 = 0.09) showed that years of experience (beta = −0.23, p < 0.001, η2 = 0.07) and workplace type (beta = −0.21, p < 0.01, η2 = 0.07) were associated with intention to hurt ratings for intentional harm. An additional model over accidental harm (F (4, 372) = 2.38, p < 0.05, R2 = 0.04) revealed that intention to hurt ratings were explained by workplace type (beta = −0.13, p < 0.05, η2 = 0.04). Subjects with more years of experience and working at hospitals had lower intention to hurt scores. Models over neutral situations revealed no significant effects (see Figs 4 and 5).
A model over punishment ratings (F (4, 372) = 4.58, p < 0.001, R2 = 0.1) revealed that factors like gender (beta = 0.11, p < 0.02, η2 = 0.04), years of experience (beta = −0.27, p < 0.001, η2 = 0.08), and workplace type (beta = −0.17, p < 0.01, η2 = 0.06) were associated with punishment ratings for intentional harm (see Figs 4 and 5). As in previous measures, the more experienced subjects working at hospitals provided the lowest empathy scores. An additional model over punishment (F (4, 372) = 3.18, p < 0.05, R2 = 0.02) revealed that workplace type (beta = −0.12, p < 0.05, η2 = 0.04) was associated with ratings for accidental harm. A model for neutral situations did not reveal significant differences. VIF analyses revealed no evidence of multicollinearity between years of experience and age in multiple regression models (VIF values below 1.12).
In sum, for MHWs, years of experience and workplace type were the most crucial factors associated with the ratings for many empathic measures for intentional harm (see Figs 4 and 5).
Results in general-physicians revealed that only years of experience was associated to ratings of empathic concern for intentional harm. In addition, results in the non-medical workers did not reach significant values (for a further description see Supplementary Information section 3.2) (see Figs 4 and 5).
Discussion
In this population-based study, we examined the empathic profile of MHWs and its relationship with potential modulating factors19–21. Relative to general-physicians and non-medical workers, MHWs exhibited higher scores for intentional harm in empathic concern, discomfort, intention to hurt, and punishment measures (see Figs 1 and 2). They were also characterized by higher empathic concern and discomfort scores for accidental harm.
The higher empathy ratings reported by MHWs highlight the distinctive role of empathic skills in their daily practice1, 26. Since early stages of training, psychologists and psychiatrists are encouraged to work on their empathic abilities to enhance rapport and improve success in clinical practice3, 34, 35, 62. In this sense, the differences observed relative to general-physicians suggest that the fine-tuned empathic profile of MHWs is not merely a reflection of a general effect of clinical experience.
Three major explanations might be listed for these effects. First, empathy scores in MHWs could be a consequence of the differential emphasis placed on particular skills during their training, such as patient comprehension, rapport, and communicative skills. Although empathy skills are developed across medical specialties, students in the mental health field are often more sensitized to the critical role of those communicative and supportive skills for daily practice29, 63. Our results are compatible with this possibility, as general-physicians assigned lower scores than MHWs in most empathy measures for intentional and accidental harm. Second, greater empathy in this group could be a response to their constant dealings with human suffering26, 64. In the case of MHWs, empathy may be modulated by keeping in touch with others’ pain. This interpretation aligns with evidence that perspective taking and emotional reactivity are modulated by others’ emotional experience1, 6, 65. Third, it is also conceivable that people with higher empathic skills are more prone to following a medical career as psychiatrists or psychologists. Moreover, it is plausible that the high empathy skills help MHW in keeping their interest in the profession and achieve longer-running careers. Nevertheless, offering definite accounts of this phenomenon transcends the aims of this study.
Here we observed a positive relationship between EC and discomfort. Some studies show dissociable effects between EC and personal distress (PD)66–68, an empathic domain potentially related to discomfort. Along these lines, the degree of EC depends on controlling the degree of pain’ perception of others, i.e., EC depends on how PD is regulated69, 70. The inhibition of bottom-up processing of the perception of pain in others can be associated to a major EC in some populations.
Despite of these evidences, we consider that the positive relationship between EC and discomfort in our study is explained by two main reasons. First, our results are in line with studies indicating that PD is a type of vicarious distress, which lead to more prosocial choices and it is necessary to generate intention to help others5, 67, 71–73. Evidence of such vicarious distress (PD) is often taken as an indication that subjects are experiencing EC14, 74–76. In addition, a positive association between PD and EC is also supported with evidences of neural activations in a reliable ‘empathy for pain’ network, which includes brain areas involved in processing physical pain14, 74. Such results indicate an intimate association between self-pain and pain in others14, 74–76.
Second, although PD and discomfort are considered self-oriented constructs each of them is measured through different tasks eliciting different emotional-empathic responses. PD has been usually measured with the Interpersonal Reactivity Index (IRI)57. PD refers to the disposition to being overwhelmed by intense negative feelings when facing emergency situations (e.g., a natural disaster). This domain has been usually tracked through the Interpersonal Reactivity Index (IRI), which taps self-perception of feelings of anxiety and unease in a group of tense interpersonal settings. By contrast, discomfort refers to the degree of inconformity that subjects feel when facing images of others in pain77. In our study discomfort was assessed through the EPT60, 77, which explicitly taps the degree of discomfort triggered by a painful situation rather than exploring feelings of anxiety or unease facing a situation60, 77. The positive relationship we found between EC and discomfort in MHWs replicates previous results18, 60, 77. In these studies, both EC and discomfort are considered as affective empathy measures and usually have been reported as enhanced in intentional harms.
Moreover, in an additional small experiment we explored other empathy domains using the IRI scale. Those results revealed higher EC and perspective-taking skills in MHWs relative to general-physicians and non-medical workers. In addition, those analyses did not reveal significant differences in PD scores between groups. Importantly, those results support the explanation that discomfort and PD are different empathic tendencies. Furthermore, it suggests that empathy abilities in MHWs depend on sharing affective experiences, which includes sharing concern and inconformity in presence of other’s suffering. However, empathic skills in MHWs seem to be less related to the degree of anxiety and personal stress that they feel when others face painful situations. These patterns of results should be corroborated in future studies that combine different approaches to assess EC, PD, and discomfort in large-sample populations and in groups where empathy is crucial for daily working.
Crucially, IRI results also showed higher perspective-taking scores in MHWs compared to control groups. Perspective-taking requires a temporary interruption of one’s own point-of-view in an attempt to view a situation as someone else might4, 78, 79. Our results suggest that MHWs were more prone to adopting alternative viewpoints, which is understandable given that MHWs need to hone such skills to improve diagnostic and treatment outcomes26, 80. These results align with previous studies in social workers showing better treatment results in individuals more capable to assume the needs of others81. Higher perspective-taking scores for MHWs may be related with the increased scores observed for this group in intention to hurt and punishment measures of the EPT, which are considered cognitive components of empathy18, 82. Together, results from EPT analyses and the IRI scales suggest that MHWs have enhanced affective and cognitive empathy skills.
Previous studies exploring empathy in other medical groups (acupuncturist and internal medicine physicians) have reported a dissociable pattern between EC and PD, suggesting that they might down-regulate their pain response by dampening negative arousal in response to the pain of others and thus freeing up cognitive resources necessary to assist others69, 70. This pattern is expected in such groups, because their profession requires inhibiting bottom-up processing of others’ pain to perform well in scenarios marked by physical pain. In contrast, MHWs in our study showed increased EC and discomfort for intentional harms. These results could be explained because empathy is continuously at stake for in MHWs19, 21, 64. In this field, empathy is critical during training, in daily clinical practice34, 35, 63, and in psychotherapeutic interventions3. Thus, while acupuncturists and internal medicine workers can be expected to evidence reductions of anxiety and discomfort for others’ physical pain as an adaptive or coping mechanism, MHWs are likely to develop enhanced experiences of EC and discomfort. Future studies should explore the relationship between EC, PD, EC and discomfort in different medical populations exposed to physical and psychological suffering in others.
Multiple regression analyses revealed that in MHWs and general-physicians empathy dimensions are explained by judgments to moral dilemmas. In particular, responses to the personal dilemma were associated with empathic concern, intention to hurt, and punishment for intentional harm in MHWs. Furthermore, in general-physicians, the responses to the impersonal dilemma were associated with empathic concern. Our results indicate that empathy dimensions are shaped by moral behavior in line with previous studies e.g. refs 37–39, 83. The existence of an inverse relationship between affective empathy dimension such as empathic concern and moral judgment has been already reported in medical workers84, 85. Our results extend the previous evidences by showing that moral judgment is curved by affective empathy measures including empathic concern and discomfort and by cognitive measures such as intention to hurt and punishment. The interplay between empathy skills and moral judgment seems to be crucial in supporting usual clinical practices in MHWs, including counseling and psychotherapy19, 52. Explorations of this assumption transcend our aims and should be further explored in future research.
In addition, we observed that scores in empathy domains were also modulated by years of experience in MHWs. In particular, subjects with more than 10 years of experience showed a reduction of empathy scores for discomfort, intention to hurt, and punishment measures for intentional harm. Although empathic concern scores for intentional harm were also modulated by years of experience in general-physicians, this factor seems to be main determinant for mental health empathy as it was a crucial factor in explaining empathy variance in different empathy domains. Previous studies have reported two types of relationship between empathy and years of experience. While a sort of studies reported that empathic sensitivity decreases in the last stages of medical training19, 43, other studies indicated that experienced doctors recover their empathic behavior, an effect explained as a consequence of reduction of personal distress44, 45. Our results agree with previous studies that showed an inverse relationship between experience and clinical empathy13, 43. Empathy scores in experienced MHWs seem to discard that higher empathy skills are a direct consequence of clinical experience. Conceivably, reductions in empathy scores in MHWs may be a consequence of a progressive desensitization to psychological and mental suffering as they are continuously facing painful situations (see Fig. 4).
Results also revealed that workplace type is a critical in modulating empathy in MHWs. In particular, we observed higher scores of affective empathy measures (i.e., empathic concern and discomfort) in MHWs working at ambulatory environments. This may reflect the comparatively lower quality of care in hospital contexts (see refs 16, 42, 86). Indeed, inpatient scenarios are highly stressful, as there, time and privacy for interaction with patients is limited and medical workers usually lack an appropriate environment to favor intimate communication87. By contrast, high empathy scores in MHW at ambulatory environments may be due to in these context professionals would have more time to devote attention to their patients24, 42 (see Fig. 5).
Environmental conditions seem to play a particularly distinctive role in MHWs, as this factor did not affect empathy ratings in general-physicians. Empathy with psychological suffering could be favored by particular contextual conditions such as intimate, close and warm environments and time to dedicate to others, which are more probably found in ambulatory environments36, 42. Changes in affective empathy due to workplace type could suggest that emotional sharing depends on formal circumstances that foster practitioner-patient rapport and closer communication.
The dissimilarities in affective empathic skills in MHWs according to workplace type could have an alternative explanation. It is possible that MHWs working at inpatient environments are more exposed to painful situations than those working at ambulatory settings. Considering this aspect, our results might suggest that MHWs have empathic attitudes that generalize to painful situations irrespective of whether these occur in medical or non-medical contexts. This explanation aligns with evidence from other populations indicating that specific social cognition tendencies, including moral cognition and empathy, go beyond the particular cognitive domain in which they are rooted and generalize to other particular cognitive and situational settings88, 89.
Moreover, empathic profile was unaffected by age or gender in MHWs. Notably, the same was true in general-physicians, but not in non-medical workers. As regards age, our results align with previous studies reporting changes in empathy skills mediated by age6. Moreover, our results showed that gender modulated empathy scores only in the non-medical group. These results support previous studies19, 90, 91 that reported no gender differences when empathy is assessed via experimental approaches, as opposed to self-report measures. The stronger evidence regarding gender differences in empathy has been reported in studies measuring empathy by means of self-report questionnaires e.g., refs 91–95. However, such differences are absent when empathy is assessed with experimental tasks91 or physiological measures53, 96. The fact of age and gender factors counted only for the non-medical group suggests that empathy in MHWs and general-physicians is more mediated by experiential factors such as years of experience and workplace type. Furthermore, our results showed that only in medical groups empathy seems to be more modulated by judgments about the correctness of social actions and moral dispositions.
Our results have important implications to understand how empathy skills are modulated in workers for whom this domain is continuously at stake. Crucially, our results suggest that empathy in MHWs is dynamically sensitive to external influences rather than a static and predetermined social-cognitive skill. The more empathic MHWs seem to be women with less than 10 years of experience working at ambulatory settings and with a more deontological moral profile. Awareness of this pattern could help administrators of medical services to facilitate external conditions that might improve empathy skills in their MHWs. In addition, this knowledge could help to develop educational and assistance plans to those MHWs that have external features associated to reductions of empathy, avoiding negative consequences in patient care.
Second, our results suggest that empathy may be a modifiable cognitive domain even in subjects that use it in their daily working life. Previous initiatives have started to develop plans to improve empathy skills, including affective sharing and perspective taking abilities88. Empathy training can impact on social decision-making processes and prosocial behavior88, processes which are usually modulated by emotional empathy and perspective-taking skills97. Considering empathy as a modifiable factor opens the door to design interventions that may impact on patient care. Future studies should explore which cognitive processes and social factors could favor empathy modifications. In addition, new studies are needed to explore the extent to which changes in empathy skills can foster caring behavior in clinical practice, and whether those changes favor prosocial behavior in other contexts.
Our results seem to deal with a well-documented problem in current science, i.e., the low rates of replicability across studies98. The usage of larger samples has been advised for increasing the reproducibility and the precision of estimated effects in psychological studies98. Along these lines, our large-scale population-based study gives solidity and allows more robustness the results. Larger samples, as the sample analyzed in this study, increase the statistical power of the estimates concerning social cognitive processes including empathy.
Despite its contributions, our study has some limitations. First, as noted earlier, our work does not determine whether higher empathy skills lead to choosing mental health as a career path or whether they are developed in mental health settings as a consequence of training and sensitization to others’ pain. This consideration should be studied in future research. Second, future population-based studies including larger sets of moral dilemmas, more ecological moral scenarios, self-reported measures, and neurophysiological measures should be explored and related to empathy dimensions in MHWs, to establish the meaningfulness of these findings. Future studies with representative samples from all over the world are needed to determine the generalizability of the present results.
Karl Jaspers introduced empathy as a tool for psychopathological assessment more than a century ago. Jaspers heralded the discovery of empathy as one of most important advances in modern social sciences33. This population-based study showed high responses in all empathy domains in MHWs. Furthermore, the empathic profile of these subjects seems sensitive to moral judgment, years of experience, and workplace type. Together, our results indicate that empathy is flexible and modifiable by external factors. Future research should be conducted to elucidate the interaction between empathy and moral decision making in other professions in which good practice hinges on empathy, such as law or social assistance.
Electronic supplementary material
Acknowledgements
This work was partially supported by grants from CONICET, CONICYT/FONDECYT Regular (1170010), FONCYT-PICT 2012-0412, FONCyT-PICT 2012-1309, FONDAP 15150012, and the INECO Foundation. Pontificia Universidad Javeriana. Hospital Universitario San Ignacio. Grant 617-2014 APS Colciencias.
Author Contributions
H.S.G.: Principal Investigator, performed statistical analysis and drafted the manuscript. A.I.: Principal Investigator and Corresponding Author, obtained the grant for the research program and drafted the manuscript. S.B.: contributed with analysis of data and revision of manuscript. A.G.: contributed with conceptualization and revision of manuscript. D.F.: contributed with analysis and collected the information. M.P.: contributed with analysis and collected the information. R.M.: contributed with analysis and collected the information. M.S.: contributed with conceptualization and revision of manuscript. D.M.: contributed with analysis of data and revision of manuscript. M.C.: contributed with analysis of data and revision of manuscript. All authors contributed to conceptualization, drafting and revising of the final version of the manuscript, as well as revising the manuscript for content. The final manuscript was approved by all coauthors.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-06775-y
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Decety J. Empathy, sympathy and the perception of pain. Pain. 2009;145:365–366. doi: 10.1016/j.pain.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Decety J, Jackson PL. The functional architecture of human empathy. Behavioral and cognitive neuroscience reviews. 2004;3:71–100. doi: 10.1177/1534582304267187. [DOI] [PubMed] [Google Scholar]
- 3.Carlozzi AF, Bull KS, Stein LB, Ray K, Barnes L. Empathy theory and practice: a survey of psychologists and counselors. The Journal of psychology. 2002;136:161–170. doi: 10.1080/00223980209604147. [DOI] [PubMed] [Google Scholar]
- 4.de Waal FBM. The antiquity of empathy. Science (New York, N.Y.) 2012;336:874–876. doi: 10.1126/science.1220999. [DOI] [PubMed] [Google Scholar]
- 5.Singer T, Lamm C. The social neuroscience of empathy. Annals of the New York Academy of Sciences. 2009;1156:81–96. doi: 10.1111/j.1749-6632.2009.04418.x. [DOI] [PubMed] [Google Scholar]
- 6.Decety J. The neuroevolution of empathy. Annals of the New York Academy of Sciences. 2011;1231:35–45. doi: 10.1111/j.1749-6632.2011.06027.x. [DOI] [PubMed] [Google Scholar]
- 7.Chen DC, Pahilan ME, Orlander JD. Comparing a self-administered measure of empathy with observed behavior among medical students. Journal of general internal medicine. 2010;25:200–202. doi: 10.1007/s11606-009-1193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cikara M, Fiske ST. Bounded empathy: neural responses to outgroup targets’ (mis)fortunes. Journal of cognitive neuroscience. 2011;23:3791–3803. doi: 10.1162/jocn_a_00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daily, P. & Behavior, P. The Neural Components of Empathy. 1–27 (2014).
- 10.Decety J, Michalska KJ, Akitsuki Y, Lahey BB. Atypical empathic responses in adolescents with aggressive conduct disorder: a functional MRI investigation. Biological psychology. 2009;80:203–211. doi: 10.1016/j.biopsycho.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Decety J. Dissecting the neural mechanisms mediating empathy. Emotion Review. 2011;3:92–108. doi: 10.1177/1754073910374662. [DOI] [Google Scholar]
- 12.Morelli SA, Rameson LT, Lieberman MD. The neural components of empathy: predicting daily prosocial behavior. Social cognitive and affective neuroscience. 2014;9:39–47. doi: 10.1093/scan/nss088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rameson LT, Morelli SA, Lieberman MD. The neural correlates of empathy: experience, automaticity, and prosocial behavior. Journal of cognitive neuroscience. 2012;24:235–245. doi: 10.1162/jocn_a_00130. [DOI] [PubMed] [Google Scholar]
- 14.Singer T, et al. Empathic neural responses are modulated by the perceived fairness of others. Nature. 2006;439:466–469. doi: 10.1038/nature04271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van den Brink D, et al. Empathy matters: ERP evidence for inter-individual differences in social language processing. Social cognitive and affective neuroscience. 2012;7:173–183. doi: 10.1093/scan/nsq094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baez S, et al. Contextual social cognition impairments in schizophrenia and bipolar disorder. PloS one. 2013;8:e57664. doi: 10.1371/journal.pone.0057664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baez S, et al. Impairments in negative emotion recognition and empathy for pain in Huntington’s disease families. Neuropsychologia. 2015;68:158–167. doi: 10.1016/j.neuropsychologia.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 18.Baez S, et al. Primary empathy deficits in frontotemporal dementia. Front Aging Neurosci. 2014;6:262. doi: 10.3389/fnagi.2014.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PloS one. 2013;8:e61526. doi: 10.1371/journal.pone.0061526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halpern J. What is clinical empathy? Journal of general internal medicine. 2003;18:670–674. doi: 10.1046/j.1525-1497.2003.21017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. Jama. 2005;293:1100–1106. doi: 10.1001/jama.293.9.1100. [DOI] [PubMed] [Google Scholar]
- 22.Benbassat J, Baumal R. What is empathy, and how can it be promoted during clinical clerkships? Academic Medicine. 2004;79:832–839. doi: 10.1097/00001888-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Hojat M, et al. Physicians’ empathy and clinical outcomes for diabetic patients. Academic Medicine. 2011;86:359–364. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 24.McIlfatrick S, Sullivan K, McKenna H. Nursing the clinic vs. nursing the patient: nurses’ experience of a day hospital chemotherapy service. Journal of clinical nursing. 2006;15:1170–1178. doi: 10.1111/j.1365-2702.2006.01495.x. [DOI] [PubMed] [Google Scholar]
- 25.Riess H. Empathy in medicine—a neurobiological perspective. JAMA. 2010;304:1604–1605. doi: 10.1001/jama.2010.1455. [DOI] [PubMed] [Google Scholar]
- 26.Brown NW, Hunter A. Empathy scores of nurses, psychiatrists and hospital administrators on the California Psychological Inventory. Psychological reports. 1987;60:295–300. doi: 10.2466/pr0.1987.60.1.295. [DOI] [PubMed] [Google Scholar]
- 27.Charon R. Narrative medicine: a model for empathy, reflection, profession, and trust. Jama. 2001;286:1897–1902. doi: 10.1001/jama.286.15.1897. [DOI] [PubMed] [Google Scholar]
- 28.Blatt B, LeLacheur SF, Galinsky AD, Simmens SJ, Greenberg L. Does perspective-taking increase patient satisfaction in medical encounters? Academic Medicine. 2010;85:1445–1452. doi: 10.1097/ACM.0b013e3181eae5ec. [DOI] [PubMed] [Google Scholar]
- 29.Bonvicini KA, et al. Impact of communication training on physician expression of empathy in patient encounters. Patient Education and Counseling. 2009;75:3–10. doi: 10.1016/j.pec.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Evaluation & the health professions. 2004;27:237–251. doi: 10.1177/0163278704267037. [DOI] [PubMed] [Google Scholar]
- 31.Nightingale SD, Yarnold PR, Greenberg MS. Sympathy, empathy, and physician resource utilization. Journal of General Internal Medicine. 1991;6:420–423. doi: 10.1007/BF02598163. [DOI] [PubMed] [Google Scholar]
- 32.Hojat M, et al. Physician empathy: definition, components, measurement, and relationship to gender and specialty. American Journal of Psychiatry. 2002;159:1563–1569. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 33.Jaspers, K. General psychopathology. (Manchester University Press, 1963).
- 34.Marci CD, Ham J, Moran E, Orr SP. Physiologic correlates of perceived therapist empathy and social-emotional process during psychotherapy. The Journal of nervous and mental disease. 2007;195:103–111. doi: 10.1097/01.nmd.0000253731.71025.fc. [DOI] [PubMed] [Google Scholar]
- 35.Marci, C. & Riess, H. The clinical relevance of psychophysiology: support for the psychobiology of empathy and psychodynamic process. American journal of psychotherapy59 (2005). [DOI] [PubMed]
- 36.Truax CB, et al. Therapist empathy, genuineness, and warmth and patient therapeutic outcome. Journal of Consulting Psychology. 1966;30:395. doi: 10.1037/h0023827. [DOI] [PubMed] [Google Scholar]
- 37.Decety J, Cowell JM. The complex relation between morality and empathy. Trends in cognitive sciences. 2014;18:337–339. doi: 10.1016/j.tics.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Decety J, Michalska KJ, Kinzler KD. The contribution of emotion and cognition to moral sensitivity: a neurodevelopmental study. Cerebral cortex. 2012;22:209–220. doi: 10.1093/cercor/bhr111. [DOI] [PubMed] [Google Scholar]
- 39.Escobar MJ, et al. Brain signatures of moral sensitivity in adolescents with early social deprivation. Scientific reports. 2014;4:5354. doi: 10.1038/srep05354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hegazi I, Wilson I. Medical education and moral segmentation in medical students. Medical education. 2013;47:1022–1028. doi: 10.1111/medu.12252. [DOI] [PubMed] [Google Scholar]
- 41.Slovackova B, Slovacek L. Moral judgement competence and moral attitudes of medical students. Nursing ethics. 2007;14:320–328. doi: 10.1177/0969733007075867. [DOI] [PubMed] [Google Scholar]
- 42.Sharma G, et al. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. Jama. 2009;301:1671–1680. doi: 10.1001/jama.2009.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hojat, M., Gonnella, J. S., Mangione, S., Nasca, T. J. & Magee, M. In Seminars in Integrative Medicine. 25–41 (Elsevier).
- 44.Handford C, Lemon J, Grimm MC, Vollmer-Conna U. Empathy as a function of clinical exposure-Reading emotion in the eyes. PloS one. 2013;8:e65159. doi: 10.1371/journal.pone.0065159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peisah C, Latif E, Wilhelm K, Williams B. Secrets to psychological success: why older doctors might have lower psychological distress and burnout than younger doctors. Aging and Mental Health. 2009;13:300–307. doi: 10.1080/13607860802459831. [DOI] [PubMed] [Google Scholar]
- 46.Waterman AD, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. The Joint Commission Journal on Quality and Patient Safety. 2007;33:467–476. doi: 10.1016/S1553-7250(07)33050-X. [DOI] [PubMed] [Google Scholar]
- 47.Rikers R, Winkel WT, Loyens S, Schmidt H. Clinical case processing by medical experts and subexperts. The Journal of psychology. 2003;137:213–223. doi: 10.1080/00223980309600609. [DOI] [PubMed] [Google Scholar]
- 48.Lee RT, Seo B, Hladkyj S, Lovell BL, Schwartzmann L. Correlates of physician burnout across regions and specialties: a meta-analysis. Human resources for health. 2013;11:48. doi: 10.1186/1478-4491-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taleghani F, Ashouri E, Saburi M. Empathy, Burnout, Demographic Variables and their Relationships in Oncology Nurses. Iranian journal of nursing and midwifery research. 2017;22:41–45. doi: 10.4103/ijnmr.IJNMR_79_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lamothe M, Boujut E, Zenasni F, Sultan S. To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Family Practice. 2014;15:15. doi: 10.1186/1471-2296-15-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eisenberg N, Lenon R. Sex Differences in Empathy and Related Capacities. Psychological bulletin. 1983;94:100–131. doi: 10.1037/0033-2909.94.1.100. [DOI] [Google Scholar]
- 52.Gleichgerrcht E, Decety J. The relationship between different facets of empathy, pain perception and compassion fatigue among physicians. Frontiers in behavioral neuroscience. 2014;8:243. doi: 10.3389/fnbeh.2014.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Michalska KJ, Kinzler KD, Decety J. Age-related sex differences in explicit measures of empathy do not predict brain responses across childhood and adolescence. Developmental cognitive neuroscience. 2013;3:22–32. doi: 10.1016/j.dcn.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baez S, et al. Orbitofrontal and limbic signatures of empathic concern and intentional harm in the behavioral variant frontotemporal dementia. Cortex; a journal devoted to the study of the nervous system and behavior. 2016;75:20–32. doi: 10.1016/j.cortex.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 55.Baez S, et al. Integrating intention and context: assessing social cognition in adults with Asperger syndrome. Frontiers in human neuroscience. 2012;6:302. doi: 10.3389/fnhum.2012.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hesse E, et al. Early detection of intentional harm in the human amygdala. Brain: a journal of neurology. 2016;139:54–61. doi: 10.1093/brain/awv336. [DOI] [PubMed] [Google Scholar]
- 57.Davis, M. H. Interpersonal reactivity index. (Edwin Mellen Press, 1980).
- 58.Foot P. The problem of abortion and the doctrine of double effect. Oxford Review. 1967;5:5–15. [Google Scholar]
- 59.Thomson J. The Trolley Problem. The Yale Law Journal. 1985;94:1395–1415. doi: 10.2307/796133. [DOI] [Google Scholar]
- 60.Baez S, et al. Integrating intention and context: assessing social cognition in adults with Asperger syndrome. Frontiers in human neuroscience. 2012;6:302. doi: 10.3389/fnhum.2012.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mansfield ER, Helms BP. Detecting multicollinearity. The American Statistician. 1982;36:158–160. [Google Scholar]
- 62.Lebowitz MS, Ahn W-K. Effects of biological explanations for mental disorders on clinicians’ empathy. Proceedings of the National Academy of Sciences. 2014;111:17786–17790. doi: 10.1073/pnas.1414058111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Academic medicine: journal of the Association of American Medical Colleges. 2013;88:1171–1177. doi: 10.1097/ACM.0b013e318299f3e3. [DOI] [PubMed] [Google Scholar]
- 64.Gateshill G, Kucharska-Pietura K, Wattis J. Attitudes towards mental disorders and emotional empathy in mental health and other healthcare professionals. The Psychiatrist. 2011;35:101–105. doi: 10.1192/pb.bp.110.029900. [DOI] [Google Scholar]
- 65.Akitsuki Y, Decety J. Social context and perceived agency affects empathy for pain: an event-related fMRI investigation. NeuroImage. 2009;47:722–734. doi: 10.1016/j.neuroimage.2009.04.091. [DOI] [PubMed] [Google Scholar]
- 66.Batson CD, Fultz J, Schoenrade PA, Paduano A. Critical self-reflection and self-perceived altruism: when self-reward fails. Journal of personality and social psychology. 1987;53:594–602. doi: 10.1037/0022-3514.53.3.594. [DOI] [PubMed] [Google Scholar]
- 67.Cialdini RB, et al. Empathy-based helping: is it selflessly or selfishly motivated? Journal of personality and social psychology. 1987;52:749–758. doi: 10.1037/0022-3514.52.4.749. [DOI] [PubMed] [Google Scholar]
- 68.Batson CD, O’Quin K, Fultz J, Vanderplas M, Isen AM. Influence of self-reported distress and empathy on egoistic versus altruistic motivation to help. Journal of personality and social psychology. 1983;45:706. doi: 10.1037/0022-3514.45.3.706. [DOI] [Google Scholar]
- 69.Cheng Y, et al. Expertise modulates the perception of pain in others. Current Biology. 2007;17:1708–1713. doi: 10.1016/j.cub.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 70.Decety J, Yang CY, Cheng Y. Physicians down-regulate their pain empathy response: an event-related brain potential study. NeuroImage. 2010;50:1676–1682. doi: 10.1016/j.neuroimage.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 71.Cialdini RB, Brown SL, Lewis BP, Luce C, Neuberg SL. Reinterpreting the empathy-altruism relationship: when one into one equals oneness. Journal of personality and social psychology. 1997;73:481–494. doi: 10.1037/0022-3514.73.3.481. [DOI] [PubMed] [Google Scholar]
- 72.FeldmanHall O, Dalgleish T, Evans D, Mobbs D. Empathic concern drives costly altruism. NeuroImage. 2015;105:347–356. doi: 10.1016/j.neuroimage.2014.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hein G, Lamm C, Brodbeck C, Singer T. Skin conductance response to the pain of others predicts later costly helping. PloS one. 2011;6:e22759. doi: 10.1371/journal.pone.0022759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Singer T, et al. Empathy for pain involves the affective but not sensory components of pain. Science (New York, N.Y.) 2004;303:1157–1162. doi: 10.1126/science.1093535. [DOI] [PubMed] [Google Scholar]
- 75.Singer T, Frith C. The painful side of empathy. Nature neuroscience. 2005;8:845–846. doi: 10.1038/nn0705-845. [DOI] [PubMed] [Google Scholar]
- 76.Preston, S. D. & de Waal, F. B. Empathy: Its ultimate and proximate bases. The Behavioral and brain sciences25, 1–20; discussion 20–71 (2002). [DOI] [PubMed]
- 77.Baez S, et al. Primary empathy deficits in frontotemporal dementia. Frontiers in aging neuroscience. 2014;6:262. doi: 10.3389/fnagi.2014.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Morelli, S. A., Rameson, L. T. & Lieberman, M. D. The neural components of empathy: Predicting daily prosocial behavior. Social cognitive and affective neuroscience, doi:10.1093/scan/nss088 (2012). [DOI] [PMC free article] [PubMed]
- 79.Epley, N. & Caruso, E. M. 20 Perspective Taking: Misstepping Into Others’ Shoes. Handbook of imagination and mental simulation, 295 (2008).
- 80.Marsh, D. T., Serafica, F. C. & Barenboim, C. Effect of perspective-taking training on interpersonal problem solving. Child development, 140–145 (1980).
- 81.Kinman G, Grant L. Exploring stress resilience in trainee social workers: The role of emotional and social competencies. British Journal of Social Work. 2011;41:261–275. doi: 10.1093/bjsw/bcq088. [DOI] [Google Scholar]
- 82.Decety J, Michalska KJ, Kinzler KD. The contribution of emotion and cognition to moral sensitivity: a neurodevelopmental study. Cerebral Cortex. 2012;22:209–220. doi: 10.1093/cercor/bhr111. [DOI] [PubMed] [Google Scholar]
- 83.Yoder KJ, Decety J. Spatiotemporal neural dynamics of moral judgment: A high-density ERP study. Neuropsychologia. 2014;60:39–45. doi: 10.1016/j.neuropsychologia.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gleichgerrcht E, Young L. Low levels of empathic concern predict utilitarian moral judgment. PLoS One. 2013;8:e60418. doi: 10.1371/journal.pone.0060418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Patil, I. & Silani, G. Reduced empathic concern leads to utilitarian moral judgments in trait alexithymia. Frontiers in Psychology5, doi:10.3389/fpsyg.2014.00501 (2014). [DOI] [PMC free article] [PubMed]
- 86.Gonzalez-Gadea ML, et al. Emotion recognition and cognitive empathy deficits in adolescent offenders revealed by context-sensitive tasks. Front Hum Neurosci. 2014;8:850. doi: 10.3389/fnhum.2014.00850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality of care: cross-national findings. Nursing outlook. 2002;50:187–194. doi: 10.1067/mno.2002.126696. [DOI] [PubMed] [Google Scholar]
- 88.Kok BE, Singer T. Effects of contemplative dyads on engagement and perceived social connectedness over 9 months of mental training: a randomized clinical trial. Jama psychiatry. 2017;74:126–134. doi: 10.1001/jamapsychiatry.2016.3360. [DOI] [PubMed] [Google Scholar]
- 89.Baez, S. et al. Outcome-oriented moral evaluation in terrorists. Nature Human Behaviour, doi:10.1038/s41562-017-0118 (2017).
- 90.Batson, C. D., Early, S. & Salavarani, G. Perspective Taking: Imagining How Another Feels Versus Imaging How You Would Feel. Personality & social psychology bulletin23, doi:10.1177/0146167297237008 (1997).
- 91.Derntl B, et al. Multidimensional assessment of empathic abilities: neural correlates and gender differences. Psychoneuroendocrinology. 2010;35:67–82. doi: 10.1016/j.psyneuen.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 92.Baron-Cohen S, Wheelwright S. The empathy quotient: an investigation of adults with Asperger syndrome or high functioning autism, and normal sex differences. Journal of autism and developmental disorders. 2004;34:163–175. doi: 10.1023/B:JADD.0000022607.19833.00. [DOI] [PubMed] [Google Scholar]
- 93.Davis MH, Franzoi SL. Stability and change in adolescent selfconsciousness and empathy. Journal of Research in Personality. 1991;25:70–87. doi: 10.1016/0092-6566(91)90006-C. [DOI] [Google Scholar]
- 94.Rueckert L, Branch B, Doan T. Are Gender Differences in Empathy Due to Differences in Emotional Reactivity? Psychology. 2011;12:574–578. doi: 10.4236/psych.2011.26088. [DOI] [Google Scholar]
- 95.Toussaint L, Webb JR. Gender differences in the relationship between empathy and forgiveness. The Journal of social psychology. 2005;145:673–685. doi: 10.3200/SOCP.145.6.673-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Christov-Moore L, et al. Empathy: gender effects in brain and behavior. Neuroscience and biobehavioral reviews. 2014;46(Pt 4):604–627. doi: 10.1016/j.neubiorev.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Takagishi H, et al. The role of cognitive and emotional perspective taking in economic decision making in the ultimatum game. PloS one. 2014;9:e108462. doi: 10.1371/journal.pone.0108462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Anderson CJ, et al. Response to Comment on “Estimating the reproducibility of psychological science”. Science. 2016;351:1037. doi: 10.1126/science.aad9163. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


