ABSTRACT
High-grade chloroquine (CQ) resistance has emerged in both Plasmodium falciparum and P. vivax. The aim of the present study was to investigate the phenotypic differences of CQ resistance in both of these species and the ability of known CQ resistance reversal agents (CQRRAs) to alter CQ susceptibility. Between April 2015 and April 2016, the potential of verapamil (VP), mibefradil (MF), L703,606 (L7), and primaquine (PQ) to reverse CQ resistance was assessed in 46 P. falciparum and 34 P. vivax clinical isolates in Papua, Indonesia, where CQ resistance is present in both species, using a modified schizont maturation assay. In P. falciparum, CQ 50% inhibitory concentrations (IC50s) were reduced when CQ was combined with VP (1.4-fold), MF (1.2-fold), L7 (4.2-fold), or PQ (1.8-fold). The degree of CQ resistance reversal in P. falciparum was highly correlated with CQ susceptibility for all CQRRAs (R2 = 0.951, 0.852, 0.962, and 0.901 for VP, MF, L7, and PQ, respectively), in line with observations in P. falciparum laboratory strains. In contrast, no reduction in the CQ IC50s was observed with any of the CQRRAs in P. vivax, even in those isolates with high chloroquine IC50s. The differential effect of CQRRAs in P. falciparum and P. vivax suggests significant differences in CQ kinetics and, potentially, the likely mechanism of CQ resistance between these two species.
KEYWORDS: malaria, Plasmodium falciparum, Plasmodium vivax, drug resistance, chloroquine, chloroquine resistance reversal
INTRODUCTION
Malaria remains one of the most important infectious diseases in the world, with authorities being notified of 214 million new cases and 438,000 deaths in 2015 (1). Chloroquine (CQ) has been in use for treatment and prophylaxis since the 1940s, but CQ resistance in Plasmodium falciparum was first reported from the Thai-Cambodian border and Colombia within a decade of its deployment, and since then, CQ resistance has spread worldwide (2). Today, WHO recommends that the use of CQ is restricted to non-falciparum malaria in areas with CQ-susceptible infections and the prevention of P. vivax and P. ovale relapses in pregnant and breast-feeding women (3). CQ is still recommended for the treatment of P. vivax malaria in many areas, but its efficacy is threatened by the emergence and spread of CQ-resistant (CQr) P. vivax, with severe public health consequences (4).
Mutations in the pfcrt gene encoding the Plasmodium falciparum chloroquine resistance transporter (PfCRT) protein are a major molecular determinant of CQ resistance in P. falciparum (5). It is hypothesized that mutant PfCRT is capable of transporting CQ away from its heme target in the digestive vacuole (DV), thus reducing the level of CQ accumulation in CQr parasites. The debate as to whether mutant PfCRT acts as a saturable carrier or a voltage-gated channel (reviewed in reference 6) is ongoing. Whereas CQ resistance in P. falciparum has been well studied, little is known about its mechanisms in P. vivax. Candidate markers, such as pvcrt-o and pvmdr1, have been investigated; however, reports about the association between these molecular determinants and in vitro and in vivo CQr phenotypes are conflicting (7–10).
A number of CQ resistance reversal agents (CQRRAs), also known as chemosensitizers, have been identified in P. falciparum in vitro. The term “reversal agent” refers to compounds that restore the activity of another drug without having intrinsic activity against the organism (11). The majority of CQRRAs are licensed for use for other medical conditions, including the calcium channel blocker verapamil (VP) (12, 13), the antihistamines chlorpheniramine and cyproheptadine (14–17), the antidepressant desipramine (18, 19), and the neuroleptic compound chlorpromazine (20). Although the mechanisms by which CQRRAs reverse CQ resistance are not fully understood, recent in-depth kinetic studies suggest that VP interacts with multiple binding sites of mutant PfCRT and inhibits PfCRT-mediated CQ transport (21). In addition, the amino acid replacement from lysine to threonine at position 76 of pfcrt (K76T) appears to be critical in determining the presence or absence of CQ resistance reversibility by VP, whereas upstream mutations at positions 72 to 75 influence the degree of reversibility (22, 23). Furthermore, reduced reversal activity in the presence of plasma proteins has been reported for desipramine (24) and VP (25). Primaquine (PQ), an 8-aminoquinoline drug currently used to prevent P. vivax relapses and the radical clearance of gametocytes in falciparum malaria, is the only agent with a demonstrable potential to reverse CQ resistance at clinically relevant concentrations (26, 27). More recently, the antidiarrheal agent loperamide, the calcium channel blocker mibefradil (MF), and the neurokinin 1 (NK1) receptor antagonist L703,606 (L7) have been shown to possess even greater potency than VP for reversal of CQ resistance in P. falciparum (28).
Assessment of CQ resistance reversal activity has generally been conducted using P. falciparum laboratory strains or field isolates with well-defined CQ susceptibility phenotypes. This approach is more challenging for P. vivax, since it cannot as yet be sustained in continuous ex vivo culture. Hence, the investigation of reversal activity in P. vivax is restricted to the assessment of field isolates, with a single publication reporting a lack of VP reversal activity in a small number of isolates (10).
The current study aimed to investigate the mechanistic differences of CQ resistance-conferring determinants in the two species with a comparative assessment of the activity of VP, MF, L7, and PQ for the reversal of CQ resistance in clinical P. falciparum and P. vivax field isolates.
RESULTS
Susceptibility to CQ and CQRRAs.
A total of 80 clinical isolates from patients with single-species infections (46 P. falciparum isolates and 34 P. vivax isolates) were assessed between April 2015 and April 2016. CQ alone and CQ in combination with VP (CQV), MF (CQM), and L7 (CQL) were assessed in all isolates; but the assessment of the combination of CQ plus PQ (CQPQ) was restricted to 26 P. falciparum and 20 P. vivax isolates. CQV data for 14 P. falciparum and 5 P. vivax isolates were excluded from the analysis as the CQ-VP combination in one of the drug plate batches failed to pass the internal drug plate quality control (QC). Adequate growth for harvest (defined as ≥40% schizonts after ≥35 h of incubation) was achieved for 80% (37/46) of P. falciparum isolates and 59% (20/34) of P. vivax isolates. The baseline characteristics of the isolates processed are presented in Table 1.
TABLE 1.
Baseline characteristics of isolates for which ex vivo assays were performed
| Baseline characteristic | P. falciparum (n = 46) | P. vivax (n = 34) |
|---|---|---|
| No. (%) of isolates reaching harvest | 37 (80) | 20 (59) |
| Median (range) delay from venipuncture to start of culture (min) | 150 (65–310) | 175 (100–330) |
| Median (range) duration of assay (h) | 43 (35–46) | 45 (42–50) |
| Geometric mean (95% CIa) parasitemia with asexual-form parasites/μl | 21,017 (13,955–31,652) | 8,555 (5,656–12,940) |
| Median (range) initial % parasites at ring stage | 100 | 93 (76–97) |
| Mean (95% CI) % schizonts at harvest | 52 (47–56) | 46 (42–49) |
CI, confidence interval.
The 50% inhibitory concentration (IC50) of each CQRRA against CQ-resistant (CQr) (K1 and W2) and CQ-sensitive (CQs) (FC27 and 3D7) P. falciparum laboratory strains resulted in intrinsic activities as well as reversal properties similar to those observed in previous studies (Table 2). All CQ resistance reversal agents (CQRRAs) tested possessed weak (micromolar range) intrinsic antimalarial properties across different parasite strains, with the median VP IC50s being between 6.5 and 28.5 μM, the median MF IC50s being between 1.5 and 8.9 μM, the median L7 IC50s being between 5.4 and 12.8 μM, and the median PQ IC50s being between 9.6 μM and 14.4 μM. The IC50s for these P. falciparum laboratory strains treated with CQ-CQRRAs are presented in Table 2. VP, MF, and L7 showed potent reversal activity against CQr isolates K1 and W2, reducing the median CQ IC50s by approximately 5.6- to 12-fold, 6.3- to 7.6-fold, and 5.1- to 22.7-fold, respectively. In contrast, PQ showed only a modest CQ IC50 reduction in K1 and W2 (i.e., 1.6- and 1.5-fold CQ IC50 reductions, respectively). CQ IC50s for the CQs strains FC27 and 3D7 were not affected by the addition of any of the CQRRAs tested.
TABLE 2.
Ex vivo drug susceptibility of P. falciparum laboratory strains to CQ and CQRRAs
| Drug or drug combination | FC27a |
3D7a |
K1b |
W2b |
||||
|---|---|---|---|---|---|---|---|---|
| Median (range) IC50 (nM)c | Fold changed | Median (range) IC50 (nM)c | Fold change | Median (range) IC50 (nM)c | Fold change | Median (range) IC50 (nM)c | Fold change | |
| VP | 27,270 (10,280–34.430) | 13,640 (13,630–18,380) | 28,530 (13,930–48.570) | 6,490 (5,820–6,530) | ||||
| MF | 8,962 (8,614–9,774) | 3,820 (3,760–3,920) | 1,544 (1,309–1,699) | 2,600 (2,540–2,610) | ||||
| L7 | 12,810 (11,860–24,350) | 8,550 (8,430–10,150) | 6,466 (5,098–12,372) | 5,400 (5,280–5,670) | ||||
| PQe | NAf | NA | 9,599 | 14,442 | ||||
| CQ | 9.3 (8.5–10.8) | 6.7 (6.6–7.8) | 138.9 (116.9–150.2) | 174.6 (173.6–181.0) | ||||
| CQV (1 μM) | 12.8 (11.9–24.3) | 0.73 | 7.3 (6.7–7.6) | 0.92 | 24.6 (20.9–33.1) | 5.65 | 14.6 (14.5–20.2) | 11.96 |
| CQM (0.35 μM) | 12.1 (11.2–13.9) | 0.77 | 7.8 (6.9–7.9) | 0.86 | 21.9 (14.0–39.3) | 6.34 | 22.9 (22.1–23.7) | 7.62 |
| CQL (1.5 μM) | 10.8 (10.6–14.9) | 0.86 | 6.9 (6.7–7.6) | 0.97 | 27.2 (14.9–41.9) | 5.11 | 7.7 (7.3–8.2) | 22.68 |
| CQPQ (0.5 μM) | 7.7 (7.1–7.7) | 1.21 | 11.9 (10.0–20.8) | 0.56 | 86.8 (81.0–96.8) | 1.6 | 120.0 (118.6–138.0) | 1.46 |
A chloroquine-sensitive laboratory strain.
A chloroquine-resistant laboratory strain.
Data are derived from three independent experiments unless indicated otherwise.
Fold change of the median CQ-CQRRA IC50 from the CQ IC50.
Derived from one experiment only.
NA, not tested in this strain.
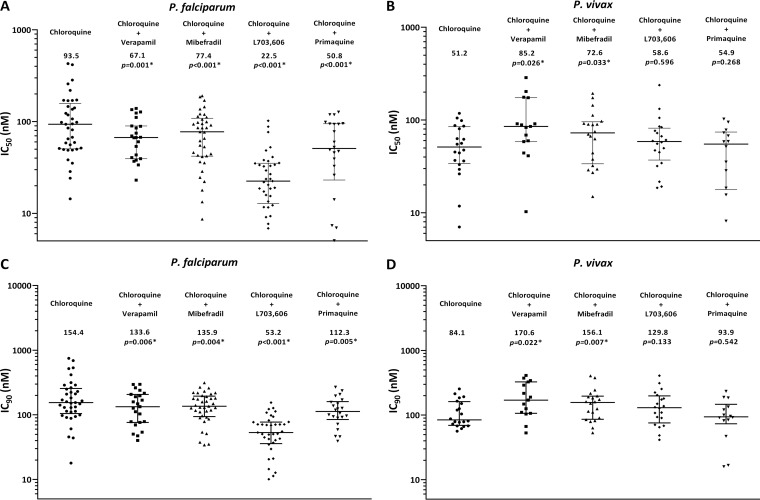
The CQ and CQ-CQRRA IC50s and IC90s of P. falciparum and P. vivax field isolates are presented in Table 3 and Fig. 1. The median IC50 of CQ for 37 P. falciparum isolates was 93.5 nM (range, 14.4 to 427.7 nM), and the median IC90 was 154.4 nM (range, 17.9 to 747.2 nM), with 14 isolates (54%) having an IC90 of greater than 150 nM. The ex vivo susceptibility of P. falciparum to all of the CQRRA combinations was significantly lower than that to CQ alone: 22.5 nM to 77.4 nM for the IC50 and 53.2 to 135.9 nM for the IC90 (P ≤ 0.006 for all comparisons).
TABLE 3.
Ex vivo drug susceptibility of P. falciparum and P. vivax field isolates to CQ and CQRRAs
| Drug |
P. falciparum |
P. vivax |
||||||
|---|---|---|---|---|---|---|---|---|
| IC50 |
IC90 |
IC50 |
IC90 |
|||||
| Median (range) IC50 (nM) | P valuea | Median (range) IC50 (nM) | P value | Median (range) IC50 (nM) | P value | Median (range) IC50 (nM) | P value | |
| CQ | 93.5 (14.4–427.7) | 154.4 (17.9–747.2) | 51.2 (7.0–118.0) | 84.1 (56.3–254.2) | ||||
| CQV (1 μM) | 67.1 (4.9–139.0) | 0.001 | 133.6 (40.1–296.0) | 0.006 | 85.2 (10.3–286.6) | 0.026 | 170.6 (52.9–409.9) | 0.022 |
| CQM (0.35 μM) | 77.4 (8.7–190.7) | <0.001 | 135.9 (34.3–312.8) | 0.004 | 72.7 (14.9–193.8) | 0.033 | 156.1 (53.3–404.2) | 0.007 |
| CQL (1.5 μM) | 22.5 (2.8–102.0) | <0.001 | 53.2 (3.5–154.6) | <0.001 | 58.6 (18.6–237.6) | 0.596 | 129.8 (41.4–407.2) | 0.133 |
| CQPQ (0.5 μM) | 50.8 (3.1–127.0) | <0.001 | 112.3 (39.2–268.1) | 0.005 | 54.9 (2.6–102.5) | 0.268 | 93.9 (15.9–232.7 | 0.542 |
P values (determined by the Wilcoxon rank-sum test) denote the statistical significance of the difference in median IC50s between CQ-CQRRA and CQ.
FIG 1.
Ex vivo drug susceptibility of clinical P. falciparum (left) and P. vivax (right) field isolates. Numbers represent median IC50s (in nanomolar) (A and B) and IC90s (in nanomolar) (C and D), and error bars represent the interquartile range (IQR). P values were derived by the Wilcoxon rank-sum test.
In the 20 P. vivax isolates, the median ex vivo CQ susceptibility was 51.2 nM (range, 7.0 to 118.0 nM) for the IC50 and 84.1 nM (range, 56.3 to 254.2 nM) for the IC90, with both values being significantly lower than the respective values for the 37 P. falciparum isolates (P = 0.005 and P = 0.009, respectively) and with 6 isolates (30%) having an IC90 of greater than 150 nM. In contrast to the effects of the CQRRAs in P. falciparum, in P. vivax isolates there was no significant difference in the IC50s with compounds L7 and PQ and a small increase in the median IC50s with VP and MF (85.2 nM [P = 0.026] and 72.7 nM [P = 0.033], respectively; Table 3).
Association between degree of reversal activity and CQ susceptibility.
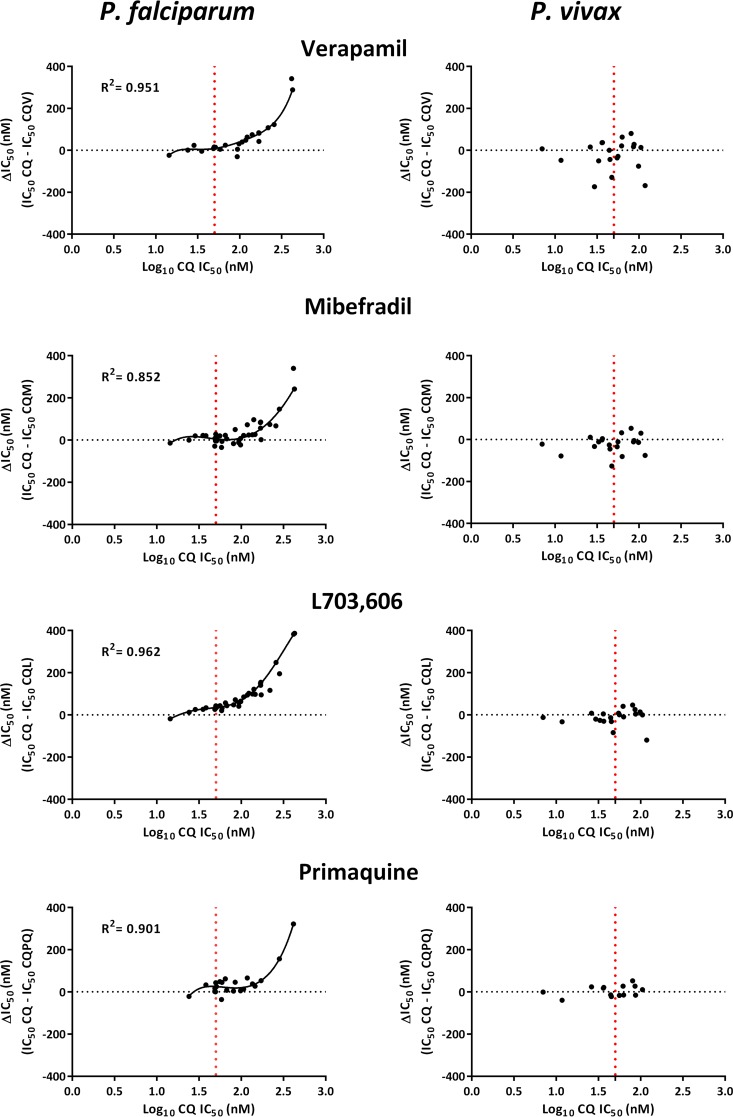
Overall, the CQ IC50 for the P. falciparum isolates was correlated with the change in the IC50 (ΔIC50) compared to the IC50s with CQV (R2 = 0.951), CQM (R2 = 0.852), CQL (R2 = 0.962), and CQPQ (R2 = 0.901) (P < 0.001 for all comparisons). The data were best fitted to a third-order polynomial regression model with inflection points at CQ IC50s of 44 nM for CQV and CQM, 42 nM for CQL, and 67 nM for CQPQ. In contrast, there was no correlation between the CQ IC50 for the P. vivax isolates and the ΔIC50 for any of the tested CQRRAs; this was also apparent in the 10 (50%) isolates with CQ IC50s above the inflection points (42 to 67 nM) observed in P. falciparum (Fig. 2).
FIG 2.
Polynomial regression analysis between ΔIC50 (the CQ IC50 minus the CQ-CQRRA IC50) and the CQ IC50. Data were analyzed using a third-order polynomial regression model. The vertical dotted lines denote the inflection point of the CQ IC50 in P. falciparum and the corresponding concentration in P. vivax. In P. vivax, the data failed to fit a polynomial regression model of any order. R2 values represent the coefficients of determination.
DISCUSSION
Our comparative study confirms the ability of four known CQRRAs to reverse CQ resistance in P. falciparum laboratory strains, and this was also apparent in the CQr P. falciparum clinical isolates (Fig. 1). The reduction in CQ susceptibility with MF and VP was more modest in the clinical isolates (1.2- and 1.4-fold, respectively) than the laboratory strains (10- and 6-fold, respectively). Whereas PQ showed similar reversal activity in both laboratory strains and clinical isolates (∼1.5-fold), L7 had the most potent reversal activity in clinical isolates (almost 4-fold). In contrast, none of these CQRRAs significantly increased CQ susceptibility in the P. vivax isolates under similar experimental conditions.
In P. falciparum, the reversal of CQ resistance is associated with increased levels of accumulation of CQ in the parasite's digestive vacuole (DV) and a reduction of CQ IC50s, and this is most apparent in CQr strains (13, 29). The potency of CQRRAs in reversing CQ resistance is influenced by the genetic background of the parasites, with pfCRT variants playing a critical role (23, 30). Although pfCRT is a key determinant of both CQ resistance and the ability of chemosensitizers to reverse this resistance, both mechanisms are likely to be modulated by other factors, including variability at other genetic loci (31, 32). All of the P. falciparum isolates in this study had a CQr pfcrt isoform (i.e., CVIET and SVMNT; data not shown), and this may, in part, explain the differences in the potential to reverse CQ resistance observed between the laboratory strains and the clinical isolates. Furthermore, whereas laboratory strains presented CQ susceptibility phenotypes at the extreme ends of the spectrum, the clinical isolates were much more diverse and showed a range of IC50s. Clinical infections can be caused by a complex mixture of parasites, with up to 10 parasite clones being found per infection (33, 34). Our clinical isolates were specifically selected for ex vivo phenotyping, all came from patients with moderate to high levels of parasitemia, and a majority of the parasites were at the ring stage. Approximately 20% of P. falciparum infections and 35% of P. vivax infections were polyclonal (unpublished data), and these isolates are more likely to consist of a mixture of CQr and CQs parasite clones than monoclonal isolates or laboratory strains are. This may have accounted for the greater variability in the potential to reverse CQ resistance that we observed in this field study.
The relationship between CQ susceptibility and the potential of verapamil, mibefradil, L703,606, and primaquine to reverse CQ resistance was explored using polynomial regression. Whereas the degree of CQ resistance reversibility was a function of CQ susceptibility in P. falciparum, no apparent relationship between CQ resistance reversal potential and baseline CQ susceptibility was observed in P. vivax, even in isolates with IC50s greater than the inflection point observed in P. falciparum.
Clinical studies have demonstrated a high degree of CQ resistance in Papua, Indonesia, and Papua New Guinea (35, 36). In a study in Timika, Papua, Indonesia, conducted in 2005, 65% of patients had a recrudescent infection within 28 days of treatment with chloroquine monotherapy, with early failure occurring in 15% of patients (37). In view of this high level of CQ resistance, antimalarial treatment policy was changed to dihydroartemisinin-piperaquine in 2006, and it has not been ethical to repeat a clinical trial of CQ therapy since that time. Thus, continued surveillance for CQ resistance has relied on monitoring of clinical isolates for ex vivo drug susceptibility. The definition of ex vivo CQ resistance using a universal threshold for the IC50 has significant limitations, particularly when comparing different drug susceptibility assays, such as the [3H]hypoxanthine incorporation and schizont maturation assays. We have shown previously that the ex vivo CQ susceptibility in Papua (where there are known P. vivax isolates with high-grade CQ resistance in vivo) and Thailand (where CQ is clinically effective against P. vivax), determined using the same assay methodology, differed accordingly, with the isolates in Papua having significantly higher IC50s than those in Thailand (10).
Our ongoing ex vivo surveillance of CQ susceptibility suggests that while IC50s have fallen slightly and are indeed lower than those documented for P. falciparum (Table 3), a significant proportion of the P. vivax clinical isolates remain CQ resistant. Clinical and pharmacology studies suggest that the growth of parasites in whole-blood concentrations of greater than 100 ng/ml is indicative of CQ resistance (38). If it is assumed that the MIC corresponds to an ex vivo IC90 of approximately 150 nM, then at least 6 of the 20 (30%) P. vivax isolates assessed in the current study would be categorized as highly CQ resistant. There was no significant difference in either the IC50 or the IC90 in these isolates when any of the CQRRAs was added to CQ ex vivo.
The mechanisms of CQ action and resistance in P. vivax and, hence, the potential to reverse CQ resistance in this species remain unknown. Sà et al. have demonstrated that the 3D7 P. falciparum strain transformed with the pfcrt orthologue pvcrt-o showed 2.2-fold increased CQ IC50s and this effect could be reversed with VP (9). More recently, the activities of two “reversed chloroquine” (RCQ) compounds (PL69 and PL106) were assessed against P. falciparum and P. vivax isolates collected from the same area where the isolates for the current study were collected, and the two species showed different profiles of susceptibility to the two compounds (39). Whereas the IC50s of both compounds were significantly lower than the IC50 of CQ alone in P. falciparum, only PL69 showed some, albeit weak, reversal activity in P. vivax, suggesting that the imipramine-like moiety of PL69 may have an effect on CQ activity in P. vivax. Further investigations on CQ kinetics will be needed to elucidate how P. vivax evades CQ toxicity.
In conclusion, all CQRRAs tested in this study demonstrated reversal activity in CQr P. falciparum isolates, with the recently identified pharmacophore L703,606 being the most potent. There was no corresponding reduction in chloroquine susceptibility in P. vivax. The results of the study suggest differences in CQ kinetics between the two Plasmodium species, with the lack of reversal activity in P. vivax supporting a growing body of work suggesting that the molecular determinants of CQ resistance in these two species may be different (40, 41).
MATERIALS AND METHODS
Study area and field sample collection.
The study was conducted in Timika, Papua Province, Indonesia, between April 2015 and April 2016. Patients presenting to the Rumah Sakit Mitra Masyarakat (RSMM) Hospital were enrolled into the study if they were diagnosed with a microscopically confirmed P. falciparum or P. vivax monospecies infection with a level of parasitemia of between 2,000 and 80,000 parasites/μl. Plasmodium isolates were processed only if at least 60% of asexual forms were at the ring stage. Patients were excluded if they had been treated with CQ in the last 30 days or any other antimalarial treatments in the last 2 weeks or had a hemoglobin concentration below 5 g/dl. After written informed consent was obtained, 5 ml of venous blood was collected and processed immediately. Host white blood cells were removed using commercially available Plasmodipur filters (Europroxima B.V., Arnhem, The Netherlands) according to the manufacturer's instructions, and the packed infected red blood cells (iRBC) were used for the ex vivo drug susceptibility assays.
Evaluation of intrinsic antimalarial activities of CQRRAs.
Verapamil hydrochloride (VP; Sigma-Aldrich, Australia), mibefradil hydrochloride (MF; Tocris Bioscience, UK), L703,606 (L7; Sigma-Aldrich, Australia), and primaquine (PQ; World Wide Antimalarial Resistance Network [WWARN] QA/QC Reference Material Programme [42]) were selected as CQ resistance reversal agents (CQRRAs) in this study. The intrinsic antimalarial activities of the recently reported MF and L7 had hitherto been tested only in the CQr strain K1 (28). Therefore, prior to the experiments in field isolates, the intrinsic antimalarial properties of these reversal agents, in addition to those of VP and PQ, were assessed in CQr (K1 and W2) and CQs (3D7 and FC27) P. falciparum laboratory strains (BEI Resources, ATCC, Manassas, VA, USA).
Drug compounds and drug plate preparation.
Each drug plate (96 wells) contained 11 serial concentrations (2-fold dilutions) in duplicate. Predosed drug plates were made by adding 25 μl of drug dilutions to each well, followed by lyophilization and storage at 4°C. The maximum concentration of CQ (provided by the WWARN QA/QC Reference Material Programme [42]) was 2,993 nM. In order to minimize the intrinsic antimalarial activities of the CQRRAs but retain their reversal activities, the concentrations of CQRRAs in experiments with multiple laboratory strains and P. falciparum and P. vivax field isolates were set as follows. For VP, the concentration added to each serial CQ dilution was derived from previous experiments performed by Martin et al. (13) and Martiney et al. (43) (i.e., 1,000 nM), and for PQ, it was derived from previous findings by Bray and colleagues (i.e., 500 nM) (26). The fixed concentrations of MF (0.355 μM) and L7 (1.5 μM) added to each serial CQ dilution were based on the lowest IC50s observed across the multiple parasite strains tested (Table 2).
Ex vivo drug susceptibility assay.
The drug susceptibilities of the Plasmodium isolates were measured using a modified schizont maturation assay as described previously (39, 44). Drug susceptibility profiles were presented as inhibition of parasite growth from the ring stage to the schizont stage. Two hundred microliters of a 2% hematocrit blood medium mixture (BMM), consisting of RPMI 1640 medium supplemented with 10% human serum (P. falciparum) or McCoy's 5A medium supplemented with 20% human serum (P. vivax), was added to each well of the predosed 96-well drug plates. The parasites were cultured in a candle jar at 37.0°C for 35 to 50 h. Incubation was stopped when more than 40% of the ring-stage parasites had reached the mature schizont stage in the drug-free control well. The plates were harvested by preparing thick blood films from each well of the plates. Thick blood films were stained with 5% Giemsa solution for 25 min and examined microscopically. Differential counts of 200 asexual-form parasites in the test slides were classified into ring, trophozoite, and mature schizont stages. To reduce parasite classification error and to standardize parasite identification between readers, only schizonts with at least 5 or more well-defined chromatin dots were classified as mature schizonts at harvest. Free merozoites and gametocytes were not included in the count. To determine the effect of each antimalarial drug, the schizont count at each drug concentration was normalized with that of the corresponding drug-free control well.
Data analysis.
Drug response data were analyzed using the in vitro analysis and reporting tool (IVART), a free and automated online platform to produce IC50 estimates by applying nonlinear regression analysis (45). Final data analysis was performed using STATA (version 14.1; Stata Corp., College Station, TX) and GraphPad Prism (version 6; GraphPad Software, Inc.) software. The Wilcoxon signed-rank test, polynomial regression analysis, and Spearman rank correlation were used for nonparametric comparisons.
Ethical approval.
Ethical approval for this project was obtained from the Human Research Ethics Committee of the NT Department of Health & Families and the Menzies School of Health Research, Darwin, Australia (HREC 2010-1396), and the Eijkman Institute Research Ethics Commission, Jakarta, Indonesia (EIREC 47 and EIREC 67).
ACKNOWLEDGMENTS
We are grateful to Lembaga Pengembangan Masyarakat Amungme Kamoro and the staff of the Rumah Sakit Mitra Masyarakat (RSMM) Hospital for their support in conducting this study. We thank all the study participants and their parents or legal guardians who made themselves available for the study and the laboratory staff members of the Research Facility at the Papuan Health and Community Development Foundation (PHCDF) in Timika, Papua, Indonesia, for their support. We thank the Australian Red Cross blood transfusion service for the supply of human serum.
We declare that we have no conflicts of interest.
G.W., R.N.P., and J.M. conceived and designed the experiments. G.W., I.H., P.P., L.L., D.A., R.W., and B.G. performed field laboratory experiments and the corresponding QC procedures. E.K., J.R.P., R.N., D.E.K., and Q.C. contributed reagents, materials, and analysis tools. G.W., I.H., and J.M. analyzed the data. G.W., R.N.P., and J.M. wrote the paper. All authors read and approved the final manuscript.
The study was funded by the Wellcome Trust (senior research fellowship in clinical science 200909 to R.N.P., research training fellowship 099875 to J.R.P.), the National Health and Medical Research Council (project grant 1023438 to R.N.P. and J.M., program grant 1037304 to R.N.P.), and the Swiss National Science Foundation (fellowship for advanced researchers PA00P3_134195/1 to J.M.).
REFERENCES
- 1.World Health Organization. 2015. World malaria report 2015. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2.Payne D. 1987. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol Today 3:241–246. doi: 10.1016/0169-4758(87)90147-5. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. 2015. Guidelines for the treatment of malaria, 3rd ed World Health Organization, Geneva, Switzerland. [Google Scholar]
- 4.Price RN, von Seidlein L, Valecha N, Nosten F, Baird JK, White NJ. 2014. Global extent of chloroquine-resistant Plasmodium vivax: a systematic review and meta-analysis. Lancet Infect Dis 14:982–991. doi: 10.1016/S1473-3099(14)70855-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, Ursos LM, Sidhu AB, Naude B, Deitsch KW, Su XZ, Wootton JC, Roepe PD, Wellems TE. 2000. Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell 6:861–871. doi: 10.1016/S1097-2765(05)00077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ecker A, Lehane AM, Clain J, Fidock DA. 2012. PfCRT and its role in antimalarial drug resistance. Trends Parasitol 28:504–514. doi: 10.1016/j.pt.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baro NK, Pooput C, Roepe PD. 2011. Analysis of chloroquine resistance transporter (CRT) isoforms and orthologues in S. cerevisiae yeast. Biochemistry 50:6701–6710. doi: 10.1021/bi200922g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orjuela-Sanchez P, de Santana Filho FS, Machado-Lima A, Chehuan YF, Costa MRF, Alecrim MDGG, del Portillo HA. 2009. Analysis of single-nucleotide polymorphisms in the crt-o and mdr1 genes of Plasmodium vivax among chloroquine-resistant isolates from the Brazilian Amazon region. Antimicrob Agents Chemother 53:3561–3564. doi: 10.1128/AAC.00004-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sà JM, Yamamoto MM, Fernandez-Becerra C, de Azevedo MF, Papakrivos J, Naude B, Wellems TE, Del Portillo HA. 2006. Expression and function of pvcrt-o, a Plasmodium vivax ortholog of pfcrt, in Plasmodium falciparum and Dictyostelium discoideum. Mol Biochem Parasitol 150:219–228. doi: 10.1016/j.molbiopara.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Suwanarusk R, Russell B, Chavchich M, Chalfein F, Kenangalem E, Kosaisavee V, Prasetyorini B, Piera KA, Barends M, Brockman A, Lek-Uthai U, Anstey NM, Tjitra E, Nosten F, Cheng Q, Price RN. 2007. Chloroquine resistant Plasmodium vivax: in vitro characterisation and association with molecular polymorphisms. PLoS One 2:e1089. doi: 10.1371/journal.pone.0001089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egan TJ, Kaschula CH. 2007. Strategies to reverse drug resistance in malaria. Curr Opin Infect Dis 20:598–604. doi: 10.1097/QCO.0b013e3282f1673a. [DOI] [PubMed] [Google Scholar]
- 12.van Schalkwyk DA, Walden JC, Smith PJ. 2001. Reversal of chloroquine resistance in Plasmodium falciparum using combinations of chemosensitizers. Antimicrob Agents Chemother 45:3171–3174. doi: 10.1128/AAC.45.11.3171-3174.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin SK, Oduola AM, Milhous WK. 1987. Reversal of chloroquine resistance in Plasmodium falciparum by verapamil. Science 235:899–901. doi: 10.1126/science.3544220. [DOI] [PubMed] [Google Scholar]
- 14.Basco LK, Ringwald P, Le Bras J. 1991. In vivo-in vitro test for chloroquine potentiation by cyproheptadine against Plasmodium falciparum. Trans R Soc Trop Med Hyg 85:206–207. doi: 10.1016/0035-9203(91)90021-P. [DOI] [PubMed] [Google Scholar]
- 15.Okonkwo CA, Coker HA, Agomo PU, Ogunbanwo JA, Mafe AG, Agomo CO, Afolabi BM. 1999. Effect of chlorpheniramine on the pharmacokinetics of and response to chloroquine of Nigerian children with falciparum malaria. Trans R Soc Trop Med Hyg 93:306–311. doi: 10.1016/S0035-9203(99)90033-0. [DOI] [PubMed] [Google Scholar]
- 16.Sowunmi A, Oduola AM, Ogundahunsi OA, Falade CO, Gbotosho GO, Salako LA. 1997. Enhanced efficacy of chloroquine-chlorpheniramine combination in acute uncomplicated falciparum malaria in children. Trans R Soc Trop Med Hyg 91:63–67. doi: 10.1016/S0035-9203(97)90399-0. [DOI] [PubMed] [Google Scholar]
- 17.Basco LK, Le Bras J. 1994. In vitro reversal of chloroquine resistance with chlorpheniramine against African isolates of Plasmodium falciparum. Jpn J Med Sci Biol 47:59–63. doi: 10.7883/yoken1952.47.59. [DOI] [PubMed] [Google Scholar]
- 18.Bitonti AJ, Sjoerdsma A, McCann PP, Kyle DE, Oduola AM, Rossan RN, Milhous WK, Davidson DE Jr. 1988. Reversal of chloroquine resistance in malaria parasite Plasmodium falciparum by desipramine. Science 242:1301–1303. doi: 10.1126/science.3057629. [DOI] [PubMed] [Google Scholar]
- 19.Basco LK, Le Bras J. 1990. Reversal of chloroquine resistance with desipramine in isolates of Plasmodium falciparum from Central and West Africa. Trans R Soc Trop Med Hyg 84:479–481. doi: 10.1016/0035-9203(90)90006-Z. [DOI] [PubMed] [Google Scholar]
- 20.Basco LK, Le Bras J. 1992. In vitro activities of chloroquine in combination with chlorpromazine or prochlorperazine against isolates of Plasmodium falciparum. Antimicrob Agents Chemother 36:209–213. doi: 10.1128/AAC.36.1.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bellanca S, Summers RL, Meyrath M, Dave A, Nash MN, Dittmer M, Sanchez CP, Stein WD, Martin RE, Lanzer M. 2014. Multiple drugs compete for transport via the Plasmodium falciparum chloroquine resistance transporter at distinct but interdependent sites. J Biol Chem 289:36336–36351. doi: 10.1074/jbc.M114.614206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lakshmanan V, Bray PG, Verdier-Pinard D, Johnson DJ, Horrocks P, Muhle RA, Alakpa GE, Hughes RH, Ward SA, Krogstad DJ, Sidhu AB, Fidock DA. 2005. A critical role for PfCRT K76T in Plasmodium falciparum verapamil-reversible chloroquine resistance. EMBO J 24:2294–2305. doi: 10.1038/sj.emboj.7600681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehlotra RK, Fujioka H, Roepe PD, Janneh O, Ursos LMB, Jacobs-Lorena V, McNamara DT, Bockarie MJ, Kazura JW, Kyle DE, Fidock DA, Zimmerman PA. 2001. Evolution of a unique Plasmodium falciparum chloroquine-resistance phenotype in association with pfcrt polymorphism in Papua New Guinea and South America. Proc Natl Acad Sci U S A 98:12689–12694. doi: 10.1073/pnas.221440898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boulter MK, Bray PG, Howells RE, Ward SA. 1993. The potential of desipramine to reverse chloroquine resistance of Plasmodium falciparum is reduced by its binding to plasma protein. Trans R Soc Trop Med Hyg 87:303. doi: 10.1016/0035-9203(93)90137-F. [DOI] [PubMed] [Google Scholar]
- 25.Gbotosho GO, Ogundahunsi OA, Happi CT, Kyle DE, Gerena L, Milhous WK, Sowunmi A, Oduola AM, Salako LA. 2006. The effects of alpha1-acid glycoprotein on the reversal of chloroquine resistance in Plasmodium falciparum. Ann Trop Med Parasitol 100:571–578. doi: 10.1179/136485906X118486. [DOI] [PubMed] [Google Scholar]
- 26.Bray PG, Deed S, Fox E, Kalkanidis M, Mungthin M, Deady LW, Tilley L. 2005. Primaquine synergises the activity of chloroquine against chloroquine-resistant P. falciparum. Biochem Pharmacol 70:1158–1166. doi: 10.1016/j.bcp.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 27.Lehane AM, Kirk K. 2010. Efflux of a range of antimalarial drugs and ‘chloroquine resistance reversers’ from the digestive vacuole in malaria parasites with mutant PfCRT. Mol Microbiol 77:1039–1051. doi: 10.1111/j.1365-2958.2010.07272.x. [DOI] [PubMed] [Google Scholar]
- 28.Ch'ng JH, Mok S, Bozdech Z, Lear MJ, Boudhar A, Russell B, Nosten F, Tan KS. 2013. A whole cell pathway screen reveals seven novel chemosensitizers to combat chloroquine resistant malaria. Sci Rep 3:1734. doi: 10.1038/srep01734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krogstad DJ, Gluzman IY, Kyle DE, Oduola A, Martin SK, Milhous WK, Schlesinger PH. 1987. Efflux of chloroquine from Plasmodium falciparum: mechanism of chloroquine resistance. Science 238:1283–1285. doi: 10.1126/science.3317830. [DOI] [PubMed] [Google Scholar]
- 30.Chen N, Kyle DE, Pasay C, Fowler EV, Baker J, Peters JM, Cheng Q. 2003. pfcrt allelic types with two novel amino acid mutations in chloroquine-resistant Plasmodium falciparum isolates from the Philippines. Antimicrob Agents Chemother 47:3500–3505. doi: 10.1128/AAC.47.11.3500-3505.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mu J, Ferdig MT, Feng X, Joy DA, Duan J, Furuya T, Subramanian G, Aravind L, Cooper RA, Wootton JC, Xiong M, Su XZ. 2003. Multiple transporters associated with malaria parasite responses to chloroquine and quinine. Mol Microbiol 49:977–989. doi: 10.1046/j.1365-2958.2003.03627.x. [DOI] [PubMed] [Google Scholar]
- 32.Patel JJ, Thacker D, Tan JC, Pleeter P, Checkley L, Gonzales JM, Deng B, Roepe PD, Cooper RA, Ferdig MT. 2010. Chloroquine susceptibility and reversibility in a Plasmodium falciparum genetic cross. Mol Microbiol 78:770–787. doi: 10.1111/j.1365-2958.2010.07366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robinson T, Campino SG, Auburn S, Assefa SA, Polley SD, Manske M, MacInnis B, Rockett KA, Maslen GL, Sanders M, Quail MA, Chiodini PL, Kwiatkowski DP, Clark TG, Sutherland CJ. 2011. Drug-resistant genotypes and multi-clonality in Plasmodium falciparum analysed by direct genome sequencing from peripheral blood of malaria patients. PLoS One 6:e23204. doi: 10.1371/journal.pone.0023204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Schalkwyk DA, Burrow R, Henriques G, Gadalla NB, Beshir KB, Hasford C, Wright SG, Ding XC, Chiodini PL, Sutherland CJ. 2013. Culture-adapted Plasmodium falciparum isolates from UK travellers: in vitro drug sensitivity, clonality and drug resistance markers. Malar J 12:320. doi: 10.1186/1475-2875-12-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karunajeewa HA, Mueller I, Senn M, Lin E, Law I, Gomorrai PS, Oa O, Griffin S, Kotab K, Suano P, Tarongka N, Ura A, Lautu D, Page-Sharp M, Wong R, Salman S, Siba P, Ilett KF, Davis TM. 2008. A trial of combination antimalarial therapies in children from Papua New Guinea. N Engl J Med 359:2545–2557. doi: 10.1056/NEJMoa0804915. [DOI] [PubMed] [Google Scholar]
- 36.Sumawinata IW, Bernadeta Leksana B, Sutamihardja A, Purnomo Subianto B, Sekartuti Fryauff DJ, Baird JK. 2003. Very high risk of therapeutic failure with chloroquine for uncomplicated Plasmodium falciparum and P. vivax malaria in Indonesian Papua. Am J Trop Med Hyg 68:416–420. [PubMed] [Google Scholar]
- 37.Ratcliff A, Siswantoro H, Kenangalem E, Wuwung M, Brockman A, Edstein MD, Laihad F, Ebsworth EP, Anstey NM, Tjitra E, Price RN. 2007. Therapeutic response of multidrug-resistant Plasmodium falciparum and P. vivax to chloroquine and sulfadoxine-pyrimethamine in southern Papua, Indonesia. Trans R Soc Trop Med Hyg 101:351–359. doi: 10.1016/j.trstmh.2006.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baird JK, Leksana B, Masbar S, Fryauff DJ, Sutanihardja MA, Suradi Wignall FS, Hoffman SL. 1997. Diagnosis of resistance to chloroquine by Plasmodium vivax: timing of recurrence and whole blood chloroquine levels. Am J Trop Med Hyg 56:621–626. doi: 10.4269/ajtmh.1997.56.621. [DOI] [PubMed] [Google Scholar]
- 39.Wirjanata G, Sebayang BF, Chalfein F, Prayoga Handayuni I, Noviyanti R, Kenangalem E, Poespoprodjo JR, Burgess SJ, Peyton DH, Price RN, Marfurt J. 2015. Contrasting ex vivo efficacies of “reversed chloroquine” compounds in chloroquine-resistant Plasmodium falciparum and P. vivax isolates. Antimicrob Agents Chemother 59:5721–5726. doi: 10.1128/AAC.01048-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nomura T, Carlton JM, Baird JK, del Portillo HA, Fryauff DJ, Rathore D, Fidock DA, Su X, Collins WE, McCutchan TF, Wootton JC, Wellems TE. 2001. Evidence for different mechanisms of chloroquine resistance in 2 Plasmodium species that cause human malaria. J Infect Dis 183:1653–1661. doi: 10.1086/320707. [DOI] [PubMed] [Google Scholar]
- 41.Pearson RD, Amato R, Auburn S, Miotto O, Almagro-Garcia J, Amaratunga C, Suon S, Mao S, Noviyanti R, Trimarsanto H, Marfurt J, Anstey NM, William T, Boni MF, Dolecek C, Tran HT, White NJ, Michon P, Siba P, Tavul L, Harrison G, Barry A, Mueller I, Ferreira MU, Karunaweera N, Randrianarivelojosia M, Gao Q, Hubbart C, Hart L, Jeffery B, Drury E, Mead D, Kekre M, Campino S, Manske M, Cornelius VJ, MacInnis B, Rockett KA, Miles A, Rayner JC, Fairhurst RM, Nosten F, Price RN, Kwiatkowski DP. 2016. Genomic analysis of local variation and recent evolution in Plasmodium vivax. Nat Genet 48:959–964. doi: 10.1038/ng.3599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lourens C, Watkins WM, Barnes KI, Sibley CH, Guerin PJ, White NJ, Lindegardh N. 2010. Implementation of a reference standard and proficiency testing programme by the World Wide Antimalarial Resistance Network (WWARN). Malar J 9:375. doi: 10.1186/1475-2875-9-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martiney JA, Cerami A, Slater AF. 1995. Verapamil reversal of chloroquine resistance in the malaria parasite Plasmodium falciparum is specific for resistant parasites and independent of the weak base effect. J Biol Chem 270:22393–22398. doi: 10.1074/jbc.270.38.22393. [DOI] [PubMed] [Google Scholar]
- 44.Wirjanata G, Sebayang BF, Chalfein F, Prayoga Handayuni I, Trianty L, Kenangalem E, Noviyanti R, Campo B, Poespoprodjo JR, Mohrle JJ, Price RN, Marfurt J. 2015. Potent ex vivo activity of naphthoquine and methylene blue against drug-resistant clinical isolates of Plasmodium falciparum and Plasmodium vivax. Antimicrob Agents Chemother 59:6117–6124. doi: 10.1128/AAC.00874-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Woodrow CJ, Dahlström S, Cooksey R, Flegg JA, Le Nagard H, Mentré F, Murillo C, Ménard D, Nosten F, Sriprawat K. 2013. High-throughput analysis of antimalarial susceptibility data by the WWARN in vitro analysis and reporting tool (IVART). Antimicrob Agents Chemother 57:3121–3130. doi: 10.1128/AAC.02350-12. [DOI] [PMC free article] [PubMed] [Google Scholar]