Abstract
Background
Greater provider volume is associated with better outcomes. There is, however, a paucity of evidence on volume-outcome associations for surgical complications and 30-day all-cause rehospitalization after free tissue transfer (FTT) or free flap. Surgical complications and frequent rehospitalization are important quality indicators that substantially hinder appropriate healthcare spending. We hypothesized that increased provider volume and surgeon experience are associated with lower complication and hospital readmission rates.
Methods
We conduct a retrospective cohort study of adults 18–64 years of age who underwent FTT. We examined 100% of all FTT operations between 2001 and 2012 using Taiwan’s national data. We used regression modeling to examine associations between volume and outcome. All of our models were adjusted for patient, surgeon, and hospital characteristics.
Results
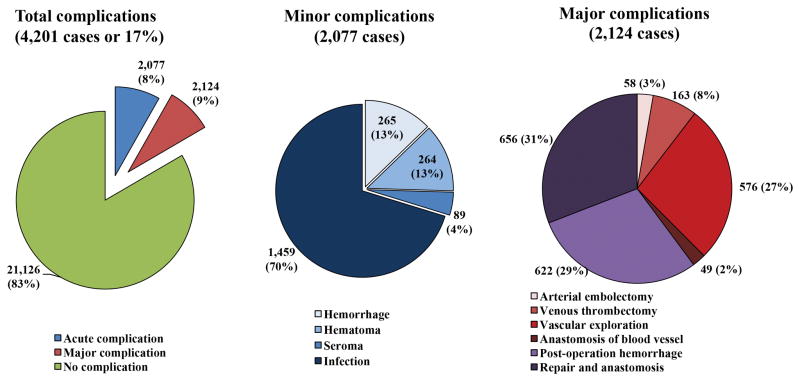
Seventeen percent of FTT operations (4,201 out of 25,327) had complications. Infection was the most prevalent complication after FTT (70%) and 30-day rehospitalization rate was about 20%. Hospital volume was associated with small decrease in complications in FTT (OR=0.99; CI:0.99–0.99; p < 0.01). For surgeons, years of experience and not annual case volume decreased surgical complications (OR=0.98; CI=0.97–0.99; p=0.01). We did not find any association between hospital or surgeon volume, or surgeon’s years of experience and 30-day rehospitalization.
Conclusions
Higher-volume hospitals and more experienced surgeons were shown to have lower likelihood of complications after surgery. Hospital process and structure affect outcomes and reduce surgical complications. Reducing a 30-day rehospitalization may require a payment reform as it demands a coordinated care pre and post hospital discharge.
Surgical complication and hospital readmission shortly after discharge have plagued our inpatient healthcare system for far too long, causing higher cost for healthcare and adverse health events for patients.1 Median hospital cost are substantially higher for both minor ($14k) and major complications ($28K) compared with similar procedures without any complications ($5K).2 Thus, over the last decade, there have been increasing efforts in the U.S. to reduce complications (any minor or major deviations from the normal post-surgery process) and 30-day all-cause rehospitalization. For example, a bundled payment, introduced in 2010 as part of the Affordable Care Act (ACA), acting as an alternative between fee-for-service and capitation payment systems. Bundled payments have been proposed to improve quality of care and reduce healthcare costs.3 Furthermore in 2012, to encourage efforts and incentivize hospitals to reduce hospital readmissions, Congress passed the Hospital Readmissions Reduction Program (HRRP).4 Accordingly, the Centers for Medicare and Medicaid Services (CMS) will penalize hospitals by 1–3% with higher-than-expected risk-adjusted hospital readmissions for myocardial infarction, congestive heart failure, and pneumonia.
A large body of research indicates that there are better surgical outcomes and fewer complications from procedures performed in higher-volume hospitals. For example, Goodney et al. examined volume-outcome associations among six cardiovascular and eight cancer resection procedures.5 They found statistically significant associations between hospital volume and 30-day readmission among four of the studied procedures.5 High-volume providers show substantially better outcomes for complex surgical procedures, such as endarterectomies or pancreatic resections, when compared with low-volume providers. Whether a higher provider volume translates into a safer choice for complex but low risk surgeries is unknown and may vary depending on the procedure. Examining demographic, preoperative condition, and provider characteristics that can be predictive of complications and/or 30-day rehospitalization can help patient, payers, and providers in developing effective strategies to reduce them. To date, only a handful of studies have examined associations between surgeon- or hospital-volume and complications after FTT.6,7 To the best of our knowledge, none of these studies used the entire national data on FTT, examining the association of both surgeon and hospital volumes with complications and 30-day readmission.
Using 100% of the 2001 to 2012 data from Taiwan’s National Health Insurance Research Database (NHIRD), we examined complications and 30-day hospital readmissions after FFT operations. Because of the multi-payer healthcare system in the U.S. and related lack of access to population-level national data, a study of this magnitude was not possible in the U.S. Taiwan’s single payer healthcare program, however, enabled us to perform this analysis. Owing to the similarity of microvascular surgical procedures among developed nations, results of this study can be used to determine whether any associations exist between provider volume and postoperative complications for FTT. In this context, we aimed to examine: (1) associations of surgeon-volume with complications and 30-day hospital readmissions; (2) associations of hospital-volume with complications and 30-day hospital readmissions; and (3) variations in complication rates between high-volume surgeons working in high-volume hospitals compared with other combinations of hospital- and surgeon-volumes. We hypothesized that both surgeon- and hospital-volume had decreasing association with postoperative complication and 30-day all-cause rehospitalization.
Methods
Data
For this study, we used 100% of all FTTs performed in Taiwan between 2001 and 2012. We examined the National Health Insurance Research Database (NHIRD) of Taiwan, which includes all inpatient, outpatient, prescription drug, and clinical encounters for more than 23 million residents of Taiwan (or more than 99% of Taiwan’s population). Starting in 1995, after extensive research, Taiwan switched from a multi-payer system to a universal, single-payer healthcare system. Thus, using the NHIRD, we were able to measure 100% of all FTT operations and cluster them by hospital and surgeon volumes. Additionally, we used unique hospital and surgeon identifiers to merge the NHIRD with hospital and surgeon registries in Taiwan.
Study Sample
We included all patients who underwent FTT surgery between 2001 and 2012 (procedure codes 62032B to 62038B, except 62034B). Our initial sample included 41,761 patients in 133 hospitals. We excluded free bone transfers from our sample because of the extended time period needed to detect a compromised bone transfer. After excluding patients who underwent free bone transfers (procedure code 62034 – 3,925 individuals) and patients with missing values (183), our final sample size included 30,133 patients. In order to link FTT related complications to the original surgery, we excluded any additional FTT operations that were performed during the same hospitalization episode. In addition, we excluded patients younger than 18 years or older than 64 years. Our final sample included 25,327 patients, 877 surgeons and 127 hospitals for the analysis. Supplemental Digital Content 1, Figure, shows the schematic flow of our sample, INSERT LINK. Supplemental Digital Content 2, table, shows a list of potential FTT complications for this study, INSERT LINK. Due to the fact that there is only one large medical center in TaoYuan City, Taiwan, we were able to validate our data by comparing medical chart data of all free flap patients in CGMH with their corresponding records in NHIRD in 2012. No significant variation was observed (Supplemental Digital Content 3, Table shows the List of Complications and codes, * International Classification of Disease, Ninth Revision, Clinical Modification, INSERT LINK).
Variables
Dependent Variables
The two main outcomes of this study were: (1) surgical complications and (2) 30-day readmission after discharge from the hospital. Surgical complication (a binary variable) had to happen after FTT operation but before discharge (See Supplemental Digital Content 3, Table, for the List of Complications and codes, INSERT LINK). Acute complications that may or may not need reoperation included (1) hemorrhage, (2) hematoma, (3) seroma, and (4) infection. Major complications – those that had to undergo reoperation - happened because of repair and anastomosis of peripheral vessel, post-operation hemorrhage, anastomosis of blood vessel, vascular exploration, venous thrombectomy, and arterial embolectomy. We also measured 30-day all-cause hospital readmission (also a binary variable) within 30-days of FTT discharge from the hospital. These two variables have been used in previously published literature to examine hospital-volume associations for other surgical procedures.8–11
Independent Variables
The main explanatory variables were surgeon and hospital volume. We ran our models using volume as continuous and categorical variables. To categorize continuous volume variables, using unique hospital and surgeon identification numbers, we sorted their annual number of operations in ascending order into three equal groups among hospitals (≤ 94, 95–156, > 156) and into three equal groups among the surgeons (≤ 10, 11–25, > 25). This approach has been used previously in the literature.12,13 In our regression models, we controlled for patient, surgeon, and hospital characteristics. For patients, we included age at the time of operation, gender, number of comorbid conditions (based on Elixhauser’s algorithm),14 and whether it was an emergency vs. planned operation. For hospitals, we included whether it was public vs. private, geographic location, teaching vs. non-teaching, number of beds, number of plastic surgeons and hospital annual replantation volume. The main geographic areas were defined as the Northern, Southern, Eastern, and Central regions of Taiwan. We also controlled for each surgeon’s years of experience, and surgeon’s annual replantation volume.
Statistical Analysis
We used a Generalized Linear Mixed Model (GLMM)15 with logistic link function for both outcomes of interest. In our regression models, we specified random effects for both hospitals and surgeons to account for repeated measures and to adjust for the effect of clustering of patients (level 1) within surgeons (level 2) and clustering of surgeons within hospitals (level 3). All analyses were done at the patient level. We used the SAS statistical package (version 9.3; SAS Institute, Inc., Cary, N.C) for all analyses.
Results
Table 1 shows the characteristics of 25,327 patients 18 to 64 years of age who underwent free flap surgery between 2001 and 2012 in Taiwan. The average age of patients was 46 and they had an average of two chronic conditions. The majority of FTT procedures in Taiwan are scheduled ahead of time, with only 3% performed on emergency admissions.
Table 1.
Characteristics of Individuals (18–64 Years) with Free Flap Procedures
| Patient Characteristics (N of patients=25,327) | # (%) | Mean (SD) |
|---|---|---|
| Male | 21,884(86%) | |
| Age (Year) | 46 (11) | |
| Elixhauser Comorbidity | 1.74 (1.39) | |
| Income | ||
| Low | 6,479 (26%) | |
| Middle | 12,235 (48%) | |
| High | 2,773 (11%) | |
| Family | 3,840 (15%) | |
| Emergency Admission | 867 (3%) | |
From Taiwan’s National Health Insurance Research Database 2001–2012
Significantly different among hospital volume groups at the 95% confidence interval.
Table 2 shows characteristics of 877 surgeons working in 127 hospitals that performed at least one FTT operation in Taiwan. The average annual FTT volume was 6 cases for surgeons and 30 cases for hospitals. Surgeons performing FTT had on average 9 years of experience. About 36% of hospitals in Taiwan were public and 87% were teaching hospitals. The majority of these hospitals were located in the northern area (39%), followed by 32% in the southern region and 24% in the central area of Taiwan. The average number of hospital beds was 1,411.
Table 2.
Characteristics of Hospitals and Surgeons Performing Free Flap Procedures
| Characteristics | # (%) | Mean (SD) |
|---|---|---|
|
Surgeon Characteristics (N of surgeons=877)
| ||
| Mean of surgeon annual volume | 6 (10) | |
| Surgeon Experience (Year) | 9 (6) | |
|
| ||
|
Hospital Characteristics (N of hospitals=127)
| ||
| Mean of hospital annual volume | 30 (80) | |
| Ownership | ||
| Public | 46 (36%) | |
| Private | 81 (64%) | |
| Teaching hospital | 110 (87%) | |
| Geographic location | ||
| Northern | 50 (39%) | |
| Central | 31 (24%) | |
| Southern | 40 (32%) | |
| Eastern | 6 (5%) | |
| Average number of beds | 1,411 (991) | |
| Average number of plastic surgeons | 22 (18) | |
|
| ||
|
Outcomes
| ||
| Surgical Complication | ||
| Yes | 4,201 (17%) | |
| No | 21,126 (86%) | |
| 30-day Readmission | ||
| Yes | 5,124 (20%) | |
| No | 20,203 (80%) | |
From Taiwan’s National Health Insurance Research Database 2001–2012
Significantly different among hospital volume groups at the 95% confidence interval.
Figure 1 demonstrates the frequency of surgical complications. Seventeen percent (4,201 out of 25,327) of FTT operations had surgical complications (acute: 2,027; major: 2,124). The most common acute complication was infection.
Figure 1.
Frequency of Surgical Complications for Free Flap Procedure
Source: 2001–2012 National Health Insurance Research Database in Taiwan
Note: Percentages show the frequency of each complication over total number of complications in each category (each patient may have more than one complication); Major complications are those that had to undergo reoperation.
Table 3 displays the results for our two regression models, analyzing the associations of hospital- and surgeon-volume with complications after surgery and 30-day hospital re-admission (for any reason) after hospital discharge. Being female was associated with lower odds of complication (OR=0.89; CI: 0.79–1.00; P=0.05). In contrast, having more chronic conditions increased the odds of complication (OR=1.06; CI: 1.03–1.09; P<0.01).
Table 3.
Generalized Linear Mixed Model for Probability of Surgical Complication and 30-day Readmission of Free Flap, 2001–2012 in Taiwan †
| Outcome | Surgical Complication | 30-day Readmission | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Parameter | Odds Ratio | 95% CI | P-value | Odds Ratio | 95% CI | P-value |
| No of patients, 25,327 | ||||||
| Gender | ||||||
| Female | 0.89 | 0.79–1.00 | 0.05* | 0.93 | 0.84–1.03 | 0.20 |
| Male (ref) | ||||||
| Patient age | 0.99 | 0.99–1.00 | <.01* | 0.99 | 0.99–0.99 | <.01* |
| Elixhauser | 1.06 | 1.03–1.09 | <.01* | 1.20 | 1.17–1.23 | <.01* |
| Emergency | ||||||
| Yes | 1.08 | 0.87–1.33 | 0.48 | 0.93 | 0.75–1.15 | 0.53 |
| No (ref) | ||||||
| Surgeon experience (year) | 0.98 | 0.97–0.99 | <.01* | 1.00(4) | 0.99–1.01 | 0.09 |
| Surgeon volume | 1.00(1) | 1.00–1.01 | 0.07 | 0.99 | 0.99–1.00 | 0.64 |
| Hospital type | ||||||
| Public | 0.73 | 0.54–0.98 | 0.04* | 0.95 | 0.74–1.23 | 0.73 |
| Private (ref) | ||||||
| Teaching hospital | ||||||
| Yes | 0.90 | 0.37–2.16 | 0.81 | 0.67 | 0.33–1.38 | 0.28 |
| No (ref) | ||||||
| Geographic location | ||||||
| Central | 0.95 | 0.67–1.34 | 0.75 | 0.76 | 0.57–1.03 | 0.08 |
| Eastern | 1.00(2) | 0.53–1.91 | 1.00 | 1.25 | 0.72–2.16 | 0.42 |
| Southern | 1.15 | 0.85–1.54 | 0.37 | 0.74 | 0.57–0.95 | 0.02* |
| Northern (ref) | ||||||
| Average number of beds | 1.00(3) | 1.00–1.00 | <.01* | 1.00(5) | 1.00–1.00 | 0.88 |
| Average number of plastic surgeons | 1.04 | 1.02–1.05 | <.01* | 0.99 | 0.98–1.00 | 0.56 |
| Hospital volume | 0.99 | 0.99–1.00 | <.01* | 0.99 | 0.99–1.00 | 0.07 |
From Taiwan’s National Health Insurance Research Database 2001–2012
Significantly at the 95% confidence interval.
Odds Ratio=1.0036;
Odds Ratio = 1.0014;
Odds Ratio=1.0003;
Odds Ratio=1.008;
Odds Ratio= 1.000007
Among surgeon’s characteristics, having one more year of the experience was associated with lower odds of complication (OR=0.98; CI: 0.97–0.99; P=0.01). However, surgeon volume was not associated with the probability of any complications. Hospitals with more number of plastic surgeons were associated with a slightly higher probability of complication (OR=1.04; CI: 1.02–1.05; P<0.01). Finally, greater hospital volume was associated with lower likelihood of any complication (OR=0.99; CI:0.99–1.00; p <0.01).
For 30-day rehospitalization after discharge, we found that a higher number of comorbidities increased the odds of 30-day readmission (OR=1.20; CI: 1.17–1.23; P<0.01). Additionally, being older (between 18 and 64) reduced the probability of 30-day readmission (OR=0.99; CI: 0.99–0.99; p < 0.01). Being in Southern Taiwan decreased the odds of readmission (OR=0.74; CI: 0.57–0.95; p=0.02). It is plausible that complex free flap cases are being routinely performed in larger hospitals, which are mostly located in Northern Taiwan.16 Although higher volume hospitals were associated with slightly less likelihood of 30-day rehospitalization, the results were not statistically significant.
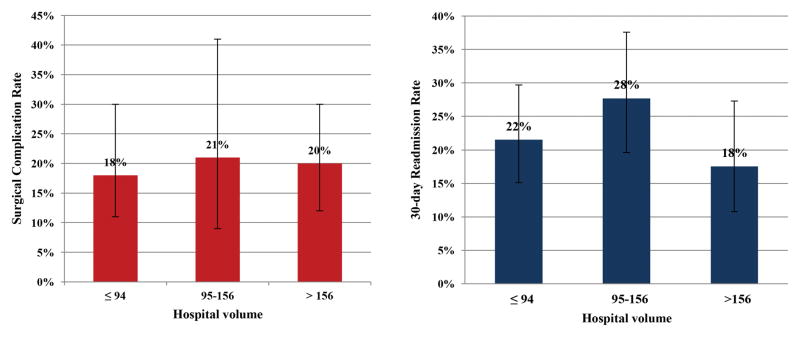
Adjusted predicted probabilities for (1) complications after surgery and (2) 30-day all-cause hospitalization indicate lower probability for both outcomes among hospitals with higher case volume (Figure 2). High-volume hospitals compared with medium-volume hospitals had lower probability of 30-day readmission by 10 percentage points (P=0.016), but our results did not indicate any significant variations in adjusted predicted surgical complications based on hospital volume.
Figure 2.
Adjusted Predicted Surgical Complication and 30-day Readmission Rates Based on Hospital Volume
-
Adjusted Predicted Complication Rate(ANOVA test, p<0.001Difference between ≤ 94 and 95–156, P=0.7231Difference between ≤ 94 and >156, P=0.6933Difference between 95–156 and >156, P=0.9039)
-
Adjusted Predicted 30-day Readmission Rate(ANOVA test, p<0.001Difference between ≤ 94 and 95–156, P=0.017Difference between ≤ 94 and >156, P=0.291Difference between 95–156 and >156, P=0.016)
Source: 2001–2012 National Health Insurance Research Database in Taiwan
Sensitivity Analysis
In the regression model for complications using categorical surgeon and hospital volume (instead of continuous volume variable) (See Supplemental Digital Content 4, Table shows the Generalized Linear Mixed Model for Probability of Complication and 30-day Readmission of Free Flap, 2001–2012, INSERT LINK), compared with being treated in low-volume hospitals (≤ 94 cases), being treated in medium-volume hospitals (95–156 cases) was associated with lower odds of complications after surgery, but it was not significant (OR=0.91; CI: 0.58–1.43; P=0.69). For hospital readmission model using categorical variables for providers’ volume show mixed results for hospital volume. Although compared with low-volume hospitals, high-volume hospitals showed lower odds of re-admission, the results were not statistically significant. Further, medium-volume hospitals (95–156 cases) were associated with higher odds of readmission (OR=1.39; CI: 1.06–1.84; p=0.02), compared with low-volume hospitals (≤ 94 cases). Finally, our regression models with interaction terms between hospital and surgeon volume did not show any significant association with our outcome variables.
Discussion
Our study yielded three notable findings. First, greater hospital case volume slightly decreased the likelihood of surgical complications in hospital after FTT. Seventeen percent of FTT operations in Taiwan had surgical complications, with 51% of them having to undergo reoperation. Although probability of complication was lower among high-volume hospitals and experienced surgeons, we failed to observe a strong association between volume and surgical complications. Second, neither hospital nor surgeon volume (nor surgeon’s years of experience) was associated with a 30-day hospital readmission. On average, hospital readmission happens to 20% of all discharged patients who underwent an FTT operation. Finally, our findings indicate that in Taiwan patient demographics such as their age, sex, and most importantly their number of chronic conditions are stronger predictors of complications or 30-day hospital readmission than provider characteristics.
Our findings on hospital volume and surgeon experience with the likelihood of complications after FTT surgery were consistent with the previous literature.17,18 Owing to a regionalized and highly competitive system of care for complex surgeries in Taiwan,19,20 our findings indicate a small but significant association between hospital volume and likelihood of surgical complications. Lower complication rates in higher volume hospitals may be due to a better prevention system throughout an episode of inpatient care in the hospital.17,21 It may also because of a more thorough implementation of standard processes of care (or “formalization of the care process”) for complex surgeries.21 For example, Bach et al. investigated the association between hospital volume and outcome after surgery for lung cancer; they found a strong association between greater hospital volume and lower likelihood of operative or pulmonary complications.9 The authors concluded that on average, postoperative care in low-volume hospitals is less systematic, causing higher likelihood of complications after complex surgeries.9
Additionally, our results indicate that among surgeons, having more years of experience (not having performed more procedures) was associated with a likelihood of fewer complications. These results suggest that surgical techniques based on surgeon’s experience may lead to variations in complications after FTT. In this context, outcomes of FTT operations may be more sensitive to differences in surgeons’ performance and experience, than in surgeons’ volume. In the majority of studies conducted on volume-outcome associations, surgeons’ years of experience was not adjusted for in the analysis. Further, surgeons’ experience might be measured by number of specific operations (volume) or by years of experience as a surgeon.22 This could be explained by a lack of data on years of experience or to different interpretations of “experience.” Regardless, when “years of experience” has been adjusted for in analytical models, it has been found to be strongly associated with better outcomes. For example, Schmidt and colleagues, examining volume-outcome associations for pancreaticoduodenectomy, revealed that experienced surgeons achieved comparable outcomes regardless of their annual volume.23 Learning curves predict that when surgeons with less experience perform up to a certain annual volume, they could achieve similar mortality and morbidity outcomes compared to those of experienced surgeons.23 The potential substitutability of surgeons’ experience and surgeons’ annual volume has important implications for how to distribute hospital surgical volume among a pool of surgeons with different experience levels to optimize outcomes with regard to surgical complications.
Furthermore, our findings indicate no association between hospital or surgeon volume, or surgeon experience and 30-day rehospitalization. Although evidence strongly suggests that high-volume providers have better outcomes for many complex surgical procedures, results for a 30-day hospital readmission were inconclusive.21 Although not all hospital readmissions can or should be prevented, there is a unanimous agreement among policy makers, payers, and hospital administrators that preventable rehospitalization should be reduced. Lack of association between provider volume and 30-day readmission can be explained in different ways. Hospital readmission is a complex and multifactorial issue negatively affecting the quality of care and healthcare expenditures.24 More than anything, hospital readmission is associated with transition of care after hospital discharge. For example, providing integrated low-cost services such as phone contact, home visits, or telemedicine, especially for high-risk individuals such as those with multiple chronic conditions, might reduce preventable rehospitalizations substantially.25,26
Most notably, under a prospective fee-for-service (FFS) payment system, where payment is made based on a predetermined fixed amount, high- or low-volume hospitals are not financially incentivized to provide additional services to prevent complications or rehospitalization.27 In Taiwan, all healthcare providers, including hospitals, follow a prospective FFS payment system. In 2002, after the implementation of Global Budget capitation system, hospitals share a limited budget and thus rigorously compete to increase their market share.28 Although hospitals may provide additional services to attract more patients, there has not been any policy initiative, such as value-based payment or bundled payment, directly targeting reduction in complications or hospital readmission.
Over the last decade, there have been increasing efforts in the U.S. to reduce preventable hospital readmissions. For example, in 2008, the CMS developed a model to estimate risk-standardized 30-day all-cause readmission rates for patients hospitalized with heart failure.29 In 2009, CMS began publishing hospitals’ risk-standardized 30-day readmission rates for heart failure from all acute care nonfederal hospitals in the U.S.30 Two thirds of all U.S. hospitals received penalties because their readmission rates were found to be higher than the predicted CMS models.31 Since 2012, the original model has been modified and improved, including more conditions and adjusting for scheduled hospitalization.32 Although reducing rehospitalization is still a work-in-progress in the U.S. and a complete discussion of this topic is beyond the scope of this paper, suffice it to say that readmission rates in the U.S. have slowly started to decline since 2012.33
Additionally, bundled payment expanded the definition of an episode of care for certain surgical procedures to post-operative care after hospital discharge, 3 hospitals will not be paid extra if rehospitalization is related to the same episode of care.34 Thus, bundled payment incentivizes all involved providers and healthcare services, from hospitals to rehabilitation services to home healthcare providers, to deliver a coordinated care. Although CMS is still testing these new alternative payment methods, early evaluations of these reforms have shown some encouraging results.35
This study had several limitations. First, using claims data, we were unable to measure and adjust for complexity of FTT surgeries. It is plausible that more complicated cases were admitted to higher-volume or higher-quality hospitals. We limited our sample to younger adults (< 65 years) to avoid biased results regarding higher probability of complications and rehospitalization among frail and elderly adults, regardless of place of service. Although we adjusted for chronic conditions and other patient demographics in our models, we were unable to adjust for severity of patient’s condition; this might have overstated both complications and 30-day hospital readmission in higher-volume hospitals. Second, we did not distinguish between preventable and other types of rehospitalization in our study. Although 30-day all-cause-rehospitalization is commonly used in literature, one should note that a 100% reduction in rehospitalization cannot and should not happen. Finally, we used Taiwan’s national data for our study because under our current multi-payer health system in the U.S. no national data on entire population are available. Although the implications of volume-outcome studies are universal, national healthcare policies and hospital reimbursement systems (as we discussed above) would have much stronger effects on these outcomes. Thus, in this context, carrying the analysis in the U.S. our results could have been different. We covered some related policies, affecting surgical complications and rehospitalization in both countries to make our findings more transparent.
In brief, higher volume hospitals are associated with better quality and less surgical complications. However, a more integrated healthcare system (beyond individual hospitals) for a complete episode of care (including 30- or 90-day post hospital discharge) and perhaps a different payment system that incentivizes hospitals to avoid unfavorable outcomes might be more effective in reducing complications or hospital readmissions.
Conclusions
Higher-volume hospitals and more experienced surgeons were shown to have lower likelihood of complications after surgery. Hospital processes and structures affect outcomes and reduce surgical complications. Performing complex surgical procedures – such as free flap – in higher-volume hospitals might reduce surgical complications. Reducing the rate of 30-day rehospitalization, however, may require payment reform, as it demands coordinated care pre- and post-hospital discharge.
Supplementary Material
Supplemental Digital Content 1. Figure shows the Flowchart for Patient Selection
Source: 2001–2012 National Health Insurance Research Database in Taiwan.
Supplemental Digital Content 2. Table shows the Overall Statistics for all Free Flap Operations in Chang Gung Memorial Hospital Compared with National Health Insurance Data in 2012.
Supplemental Digital Content 3. Table shows the List of Complications and codes
* International Classification of Disease, Ninth Revision, Clinical Modification
Supplemental Digital Content 4. Table shows the Generalized Linear Mixed Model for Probability of Complication and 30-day Readmission of Free Flap, 2001–2012 †
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval.
(1)Odds Ratio= 1.0006; (2) Odds Ratio= 0.999
Acknowledgments
Funding: This work was supported by the Plastic Surgery Foundation National Endowment for Plastic Surgery Grant (to Dr. Elham Mahmoudi), a Midcareer Investigator Award in Patient-Oriented Research from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2 K24-AR053120-06) (to Dr. Kevin C. Chung), ), and The Integration and Maintenance Program of Health Information Application and Collaborative Research (to Drs. Ming-Huei Cheng and Chee Jen Chang) (CIRPD1D0032)
References
- 1.Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Annals of surgery. 2013;258(1):10–18. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
- 2.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. Journal of the American College of Surgeons. 2004;199(4):531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 3.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Affairs. 2011;30(11):2107–2115. doi: 10.1377/hlthaff.2011.0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA : the journal of the American Medical Association. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 5.Goodney PP, Stukel TA, Lucas FL, Finlayson EV, Birkmeyer JD. Hospital volume, length of stay, and readmission rates in high-risk surgery. Annals of surgery. 2003;238(2):161–167. doi: 10.1097/01.SLA.0000081094.66659.c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei F-c, Celik N, Yang W-g, Chen I-h, Chang Y-m, Chen H-c. Complications after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plastic and reconstructive surgery. 2003;112(1):37–42. doi: 10.1097/01.PRS.0000065911.00623.BD. [DOI] [PubMed] [Google Scholar]
- 7.Lee C-C, Ho H-C, Chou P. Multivariate analyses to assess the effect of surgeon volume on survival rate in oral cancer: a nationwide population-based study in Taiwan. Oral oncology. 2010;46(4):271–275. doi: 10.1016/j.oraloncology.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Janakiraman V, Lazar J, Joynt KE, Jha AK. Hospital volume, provider volume, and complications after childbirth in US hospitals. Obstetrics & Gynecology. 2011;118(3):521–527. doi: 10.1097/AOG.0b013e31822a65e4. [DOI] [PubMed] [Google Scholar]
- 9.Bach PB, Cramer LD, Schrag D, Downey RJ, Gelfand SE, Begg CB. The influence of hospital volume on survival after resection for lung cancer. New England Journal of Medicine. 2001;345(3):181–188. doi: 10.1056/NEJM200107193450306. [DOI] [PubMed] [Google Scholar]
- 10.Freeman JV, Wang Y, Curtis JP, Heidenreich PA, Hlatky MA. The relation between hospital procedure volume and complications of cardioverter-defibrillator implantation from the implantable cardioverter-defibrillator registry. Journal of the American College of Cardiology. 2010;56(14):1133–1139. doi: 10.1016/j.jacc.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86(9):1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. New England Journal of Medicine. 2002;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 13.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. New England Journal of Medicine. 2003;349(22):2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 15.McCulloch CE, Neuhaus JM. Generalized linear mixed models. Wiley Online Library; 2001. [Google Scholar]
- 16.Kreng VB, Yang C-T. The equality of resource allocation in health care under the National Health Insurance System in Taiwan. Health Policy. 2011;100(2):203–210. doi: 10.1016/j.healthpol.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Gouma DJ, Van Geenen RC, van Gulik TM, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Annals of surgery. 2000;232(6):786–795. doi: 10.1097/00000658-200012000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Surgical volume and quality of care for esophageal resection: do high-volume hospitals have fewer complications? The Annals of thoracic surgery. 2003;75(2):337–341. doi: 10.1016/s0003-4975(02)04409-0. [DOI] [PubMed] [Google Scholar]
- 19.Cheng T-M. Reflections on the 20th anniversary of Taiwan’s single-payer national health insurance system. Health Affairs. 2015;34(3):502–510. doi: 10.1377/hlthaff.2014.1332. [DOI] [PubMed] [Google Scholar]
- 20.Wu T-Y, Majeed A, Kuo KN. An overview of the healthcare system in Taiwan. London journal of primary care. 2010;3(2):115–119. doi: 10.1080/17571472.2010.11493315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen NT, Paya M, Stevens CM, Mavandadi S, Zainabadi K, Wilson SE. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Annals of surgery. 2004;240(4):586–594. doi: 10.1097/01.sla.0000140752.74893.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Annals of surgery. 1998;228(3):320. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt CM, Turrini O, Parikh P, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Archives of surgery. 2010;145(7):634–640. doi: 10.1001/archsurg.2010.118. [DOI] [PubMed] [Google Scholar]
- 24.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Annals of internal medicine. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 25.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. Journal of the American College of Surgeons. 2012;215(3):322–330. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Medical care. 2010;48(11):981–988. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 27.Morley M, Bogasky S, Gage B, Flood S, Ingber MJ. Medicare post-acute care episodes and payment bundling. Medicare & medicaid research review. 2014;4(1) doi: 10.5600/mmrr.004.01.b02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheng S-H, Chen C-C, Chang W-L. Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy. 2009;92(2):158–164. doi: 10.1016/j.healthpol.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 29.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circulation Cardiovascular quality and outcomes. 2008;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 30.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circulation: Heart Failure. 2010;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joynt KE, Jha AK. A path forward on Medicare readmissions. The New England journal of medicine. 2013;368(13):1175–1177. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Medicare and Medicaid Services. [Accessed August 15, 2016];Readmissions Reduction Program (HRRP) 2016 https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html.
- 33.Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. [Accessed Jan 29, 2015]; [Google Scholar]
- 34.Press MJ, Rajkumar R, Conway PH. Medicare’s new bundled payments: design, strategy, and evolution. JAMA : the journal of the American Medical Association. 2016;315(2):131–132. doi: 10.1001/jama.2015.18161. [DOI] [PubMed] [Google Scholar]
- 35. [Accessed September 15, 2016];CMS Bundled Payment for Care Improvement Initiative Models 2–4: Year 2 Evaluation and Monitoring Annual Report. 2016 https://innovation.cms.gov/Files/reports/bpci-models2-4-yr2evalrpt.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Figure shows the Flowchart for Patient Selection
Source: 2001–2012 National Health Insurance Research Database in Taiwan.
Supplemental Digital Content 2. Table shows the Overall Statistics for all Free Flap Operations in Chang Gung Memorial Hospital Compared with National Health Insurance Data in 2012.
Supplemental Digital Content 3. Table shows the List of Complications and codes
* International Classification of Disease, Ninth Revision, Clinical Modification
Supplemental Digital Content 4. Table shows the Generalized Linear Mixed Model for Probability of Complication and 30-day Readmission of Free Flap, 2001–2012 †
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval.
(1)Odds Ratio= 1.0006; (2) Odds Ratio= 0.999