Abstract
We investigate the geographic patterns of drug poisoning deaths involving heroin by county for the USA from 2000 to 2014. The county-level patterns of mortality are examined with respect to age-adjusted rates of death for different classes of urbanization and racial and ethnic groups, while rates based on raw counts of drug poisoning deaths involving heroin are estimated for different age groups and by gender. To account for possible underestimations in these rates due to small areas or small numbers, spatial empirical Baye’s estimation techniques have been used to smooth the rates of death and alleviate underestimation when analyzing spatial patterns for these different groups. The geographic pattern of poisoning deaths involving heroin has shifted from the west coast of the USA in the year 2000 to New England, the Mid-Atlantic region, and the Great Lakes and central Ohio Valley by 2014. The evolution over space and time of clusters of drug poisoning deaths involving heroin is confirmed through the SaTScan analysis. For this period, White males were found to be the most impacted population group overall; however, Blacks and Hispanics are highly impacted in counties where significant populations of these two groups reside. Our results show that while 35–54-year-olds were the most highly impacted age group by county from 2000 to 2010, by 2014, the trend had changed with an increasing number of counties experiencing higher death rates for individuals 25–34 years. The percentage of counties across the USA classified as large metro with deaths involving heroin is estimated to have decreased from approximately 73% in 2010 to just fewer than 56% in 2014, with a shift to small metro and non-metro counties. Understanding the geographic variations in impact on different population groups in the USA has become particularly necessary in light of the extreme increase in the use and misuse of street drugs including heroin and the subsequent rise in opioid-related deaths in the USA.
Keywords: Drug poisoning deaths, Heroin, Substance use, Spatiotemporal cluster analysis
Introduction
According to the US National Center for Health Statistics at the Centers for Disease Control and Prevention,1 the number of deaths from prescription drugs increased 227% between 2000 and 2014, with 25,760 deaths involving prescription drugs occurring in 2014. For this same period, there was an increase of approximately 329% for drug poisoning deaths involving natural opioid analgesics (such as oxycodone, hydrocodone), methadone, morphine, and other synthetic opioid analgesics, such as fentanyl. It is also reported that during this period, heroin initiation rose from 108,000 in the USA in 2005 to 178,000 in 2011 and to 435,000 in 2014 [1, 2]. Drug poisoning deaths involving heroin increased 474% from 2000 (1842 reported deaths) to 2014 (10,574 reported deaths). The recent spike in the number of overdose deaths involving the misuse of opioid analgesics has been reported widely and linked to the expanded use of prescription opioids [3, 4], and the pattern of shifting from prescription opioid use to heroin use has been a topic of investigation as researchers are seeking to understand the reasons underlying this shift. In one study, an increase in heroin overdoses was found to be linked to therapeutic errors (e.g., incorrect doses or the administration of an incorrect substance) that resulted in exposure to oxycodone [5]. And additional reporting found that increases in non-medical uses of pharmaceutical opioids (e.g., oxycodone) were occurring even as pharmaceutical companies were making formulations of some drugs that were more difficult to inject, where opioid users were resorting to different formulations that included intravenous use [6]. The increasing trend of non-medical uses, misuses, and fatal poisonings involving prescription opioids has led to an over 300% increase in mortality in the USA from 2000 to 2014.2
Prior research has used, for example, Multiple Cause of Death data from National Vital Statistics reporting to track trends in drug poisoning deaths in the USA; however, it is understood that localities may differ widely on the percentage of deaths reported [7, 8]. Keeping this potential reporting limitation in mind, this research differs from prior research by tracking deaths involving heroin at the county level. In this study, we use Centers for Disease Control and Prevention—Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) Multiple Cause of Death data to investigate the geographic patterns of drug poisoning deaths involving heroin by county for the USA from 2000 to 2014. The patterns are examined with respect to a set of key factors including urbanization, race and ethnicity, age, and gender in order to understand the impact from the rise in heroin use and related deaths on different population groups at county level. As part of this research, we investigate the geospatial patterns of overdose deaths involving heroin and the location and extent to which clusters of overdose deaths are identified. Through this study, we show the burden of heroin overdose deaths on US counties as well as on different population groups at key intervals during this 15-year period. This geographic-based research provides a perspective on how the rate of deaths varies over space and time and gives insights that can be useful for interventions and improved planning in relation to heroin misuse in the USA and to alleviate the burden of mortality in certain counties and states.
Background
A rise in overdoses involving heroin has been noted globally. A survey conducted in Australia between 2012 and 2013 among heroin users from either methadone maintenance treatments, drug-free residential rehabilitation, or detoxification programs noted that 67.5% of participants with heroin initiation had overdose records [9]. A growing risk from overdoses involving heroin was also found in a recent UK study by Strang [10] that reported life-threatening overdoses were experienced by half of heroin or opiate misusers in Scotland and England during 1993 and 2008. In Columbia, a 2010 study found a mean rate of 3.2 times of injections per day among heroin injectors, with this high rate of injection putting these users at greater risk of HIV infections [11].
Research on heroin use includes evidence that in certain locations, there has been an increase in heroin use by younger persons in recent years, where younger drug users have been more likely to use syringes multiple times for heroin injection [12]. In Seattle’s metropolitan area, for example, heroin has been a primary cause of death among younger individuals (age under 26) as a result of opioid overdoses and prescription opioid misuse [13, 14]. In a study investigating heroin use in North Carolina between 2007 and 2013, researchers found that overdose deaths have shifted from opioid analgesics to heroin, and researchers found that there was a decrease in the average age of deceased individuals from 38.7 years in 2007 to 35.5 years in 2013 [15].
Studies have also examined the impact of drug poisoning deaths on racial and ethnic groups. Research based on a nationwide survey during 2002 to 2011 shows non-Hispanic Whites were at high risk of heroin use during this period and there was an increasing trend among Hispanics in mid 2000s [16]. A more recent study in San Francisco reported that the opioid overdose mortality between 2010 and 2012 mostly occurred among middle-aged non-Hispanic White males (and over 9% of these deaths involved heroin) [17].
The distribution of drug poisoning deaths between urban and rural locations has also been a topic of study. Research has revealed that overdoses involving opioid use have severely impacted adults living in urban places compared to rural adults due to a higher usage of substances including prescription drugs [18, 19]. A case study in urban San Francisco found a consistently high injection frequency by heroin users since the late 2000s [20]. However, a rapid increase in prescription opioid use and drug poisoning deaths involving heroin among residents living in rural areas in the USA has also been reported to be on the rise due to the lower costs of heroin as well as increased accessibility to this drug [21–23]. Our study will investigate urban-rural spatial patterns of drug deaths involving heroin.
Geospatial analysis methods have been applied in substance use research [7, 8, 24]. As drug poisoning deaths at a county level across the USA are not a common event, small area estimation technique (e.g., mixed effect model) has been applied by Rossen [7, 8] to alleviate unstable results. In their research, major hot spots of deaths from drug poisoning were identified in North Pacific Coast, Southwest, Gulf Coast, and Appalachia during 2007–2009. Spatial accessibility to substance use treatment facilities has been analyzed using buffer analysis based on a 10-min driving distance in order to investigate whether the availability of these facilities possibly plays a negative role with respect to heroin injections due to decreasing concerns about access to injections in the future [25, 26]. Research into the associations between fatal prescription opioid poisonings and socioeconomic factors in NH used spatial regression analysis with a simultaneous autoregressive spatial error model to show that fatal poisonings were more likely to occur in areas with lower median household income or greater percentages of disabled workers [27]. In our research, we apply spatial methods including spatial and spatiotemporal cluster analysis and spatial smoothing techniques to investigate the impact of drug poisoning deaths involving heroin at the county level across the USA in order to identify how the impact on different population groups has changed over space and time, and locations in the USA where this impact is highest.
Methods
Data
The annual numbers of drug poisoning deaths involving heroin for each US county for the period 2000–2014 were collected from CDC WONDER.3 The data collected are for cases corresponding to poisoning codes representing categories for Underlying Cause of Deaths (UCD) that are classified using the International Classification of Disease, Tenth Revision (UCD-ICD-10). This category includes X40–X44 (accidental poisoning); X60–X64 (intentional poisoning); X85 (assault); Y10–Y14 (poisoning undetermined intent); and the type of drug involved indicated by the classifications under Multiple Cause of Deaths (MCD) MCD-ICD-10, for this study, T40.1 (heroin). Raw number of deaths by county and year were collected for the 48 contiguous states in the USA. In the CDC WONDER dataset, when the number of deaths in a county is lower than 10, the data are suppressed and values are not presented for use. In fact, the data (age-adjusted rates for total population and racial and ethnic groups and raw counts for the remaining groups) are suppressed for most US counties for each population category. The number of counties where data are available is summarized in Table 1. Our study area covers the 48 contiguous states in the USA with 3109 counties.
Table 1.
Number of counties with data (raw counts or age-adjusted rates) on the number of deaths by drug poisoning involving heroin
| 2000 | 2005 | 2010 | 2014 | |
|---|---|---|---|---|
| Total populationa | 21 | 21 | 31 | 136 |
| Whitea | 14 | 16 | 27 | 121 |
| Blacka | 3 | 1 | 0 | 8 |
| Hispanica | 1 | 2 | 2 | 9 |
| Female | 4 | 5 | 10 | 64 |
| Male | 37 | 39 | 63 | 199 |
| 18–24 years | 1 | 1 | 8 | 31 |
| 25–34 years | 6 | 4 | 19 | 90 |
| 35–54 years | 26 | 26 | 31 | 119 |
| 55 years and above | 1 | 1 | 4 | 23 |
aAge-adjusted rates
In order to understand the impact and geographic patterns of poisoning deaths involving heroin in the USA, we also acquired the data by age, gender, racial group, and ethnicity. We categorized age groups as the following: ages 18–24, 25–34, 35–54, and 55 years and above. In the CDC WONDER database, reportable data exists for two racial groups, African American and White, and for Hispanic and non-Hispanic counts. As poisoning deaths involving heroin are relatively rare and involve small numbers, GeoDa’s tools (GeoDa 1.6.7, Anselin, Luc, IL, 2015) for spatial empirical Baye’s estimation have been used to smooth the rate of deaths and alleviate small area problems across the country when analyzing spatial patterns in terms of the total population and these sociodemographic variables. For this estimation, we used raw counts (for age and gender patterns) and age-adjusted drug poisoning death rates (for spatial, racial, and urbanization pattern analyses) as event data and county population as base data, and spatial weights were defined based on queen contiguity (i.e., counties that share at least one boundary are considered as neighbors). The smoothed rates were estimated for the entire study time period. The rates that are mapped, including rates for 2000, 2005, 2010, and 2014, are presented using a natural breaks classification method.
Each county was assigned an urban-rural classification that follows the scheme used by the National Center for Health Statistics.4 In this research, we aggregated counties into four categories: large metro (population ≥1 million), medium metro (population 250,000–999,999), small metro (population <250,000), and non-metro (including micropolitan and non-core counties). The urban-rural classification for 2006 is used for analysis of the period 2000–2009, while the classification for 2013 is applied for the period 2010–2014.
Geostatistical Analysis
Spatial Autocorrelation
To investigate the geographic pattern of drug poisoning deaths involving heroin in the USA, a global Moran’s I test [28] was performed using ArcGIS 10.3 (ESRI, Redlands, CA, 2014) to examine whether there is a possibility that the spatial pattern of poisoning deaths is clustered. This test was applied on the spatial empirical Baye’s estimated rates of deaths involving heroin in the USA for 2000 to 2014. In addition, to better explore the spatial pattern of deaths involving heroin among neighboring counties, Local Indicators of Spatial Association (LISA statistic) [29] was performed to measure the local spatial autocorrelation and clustering tendency of these deaths. From this analysis, counties with higher rates of drug deaths involving heroin can be identified. As a counterpart of global Moran’s I, local Moran’s I index for each county was also generated using ArcGIS. This statistic indicates whether each county has a positive or negative spatial autocorrelation based on the pattern of deaths. A clustered or dispersed spatial pattern is illustrated by a positive or negative Moran’s I value along with a z-score falling between −1.96 and 1.96. This test was applied to the spatial empirical Baye’s estimated rates of deaths from 2000 to 2014.
Space-Time Scan Statistics
To understand how geographic patterns of clustering have emerged and evolved between 2000 and 2014, a scan statistic was applied using the SaTScan software (SaTScan 9.4, Kulldorff, Martin, 2015). For this evaluation, the SaTScan analysis was undertaken for raw counts of deaths based on a Poisson probability model, scanning for areas with high numbers of deaths involving heroin and using a null hypothesis that the expected number of drug poisoning deaths involving heroin in each county is proportional to the population size of the county [30]. This analysis is performed using a likelihood ratio test, and the function is equal to the following:
where C denotes the total number of deaths, c is the observed number of deaths within the scanning window, and E[c] refers to the covariate adjusted expected number of deaths within the test window. I() is an indicator function equal to 1 since this test is set to scan only for clusters with high numbers of deaths, i.e., more deaths within the window than expected [31]. The maximum size of the scanning window is defined as 5% of the population at risk since deaths involving heroin typically comprise a low percentage of the causes of deaths in a population (e.g., about 0.3% of the population died from heroin poisoning in 2014).5 However, this size of window could hide small clusters of deaths. In order to detect stable counties within core clusters, we applied a sensitivity analysis [32, 33] and investigated a range of eight maximum-sized scanning windows: 0.2% of population at risk, 0.4, 0.6, 0.8, 1, 2, 4, and 5%. The maximum temporal cluster size is always defined as 1 year since the datasets we are working with are annual counts of drug poisoning deaths involving heroin. The criteria for reporting hierarchical clusters are that no cluster centers are in less likely clusters, which indicates there could be clusters that overlap each other. In this sensitivity analysis, we defined a core cluster as a cluster that has a low percentage of counties with a low relative risk. In this test, the relative risk index in each county indicates how much more common poisoning deaths involving heroin are in a county compared to other counties, following the equation below:
where RR >1 reveals a high risk of death. In this sensitivity analysis, low risk refers to counties where RR <1. Based on the results, a threshold of 33% is used to represent what is considered a low percentage of counties with low risk. To qualify as a statistically significant cluster, p values of each core cluster have to be lower than 0.01, where the significance of these clusters was determined by the Monte Carlo simulation with 999 random replications. To detect the stability of a county belonging to a core cluster, we applied the reliability index computation as follows [32]:
where R i denotes the stability value for county i, S is the total number of scans (in this case, eight scans), and C i refers to the number of deaths when county i falls in a core cluster. Since there is the possibility that clusters overlap, this reliability index could be larger than 1. The reliability index reveals stable core clusters but also reveals possible heterogeneous patterns within core clusters.
Results
Spatial and Temporal Pattern of Drug Poisoning Deaths Involving Heroin
In terms of raw counts of deaths involving heroin, a total of 37,088 deaths are reported for the period 2000 and 2014. Between 2000 and 2011, the highest number of deaths in the USA occurred in Los Angeles County, CA (169 deaths in 2000 with a peak number in 2002 of 182). In 2012, the highest number had shifted to Cuyahoga County, OH (135 deaths). In 2013 and 2014, the highest number of drug poisoning deaths involving heroin occurred in Cook County, IL (291 and 323 deaths respectively).
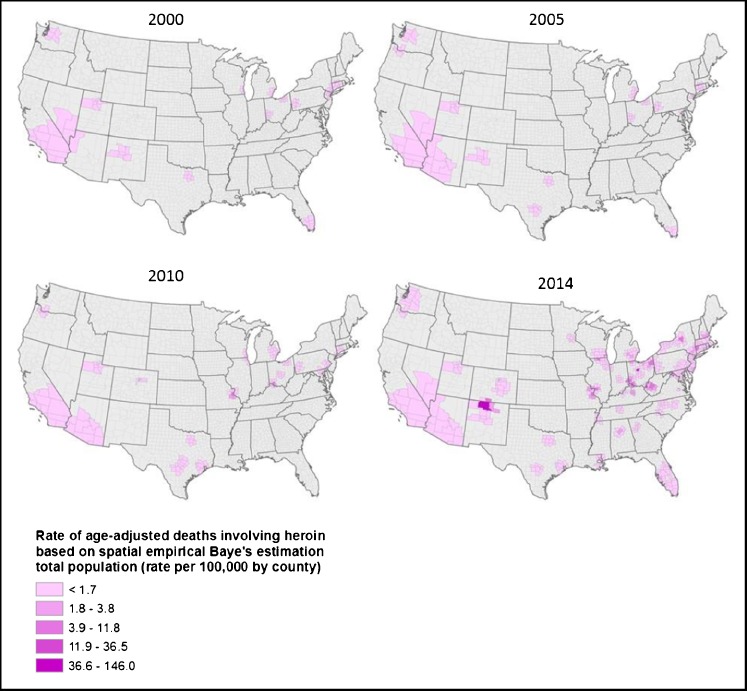
Spatial empirical Baye’s estimation techniques were applied to spatially smooth age-adjusted death rates for four different time points including 2000, 2005, 2010, and 2014. This analysis returns a spatial pattern that started in 2000 with counties on both the east and west coasts of the USA, expanding into the central USA (e.g., MO and OH) by 2010 and then spreading rapidly from 2010 to 2014 throughout New England, the Mid-Atlantic, and Great Lakes and Ohio Valley regions (Fig. 1). In 2000, 103 counties in the USA had spatially smoothed age-adjusted rates, with the highest rate being estimated for Passaic County, NJ, and the second and third highest rates in Valencia County, NM, and Kern County, CA, respectively. In 2005, the highest spatially smoothed rate had shifted to Baltimore City, MD, followed by Miami County, OH. Since 2005, the spatially smoothed age-adjusted rates have remained high in the Ohio Valley region. By 2010, 160 counties were impacted in the USA, an approximately 55% increase from 2000, with the highest age-adjusted death rates estimated for Jefferson County, MO, followed by Clermont County, OH, and Bracken County, KY. Four years later, in 2014, 511 counties have spatially smoothed age-adjusted deaths. The highest rate is estimated for Rio Arriba County, NM. Four counties in the Ohio Valley region comprise the highest two categories of death rates including Berkeley and Cabell Counties, WV; Campbell County, KY; and Marion County, OH. Note that no spatially smoothed rate based on age-adjusted deaths involving heroin was estimated for Rio Arriba County, NM prior to 2014.
Fig. 1.
Spatial empirical Baye’s estimation of rate of age-adjusted deaths involving heroin for 2000, 2005, 2010, and 2014
Racial and Ethnic Patterns of Deaths Involving Heroin
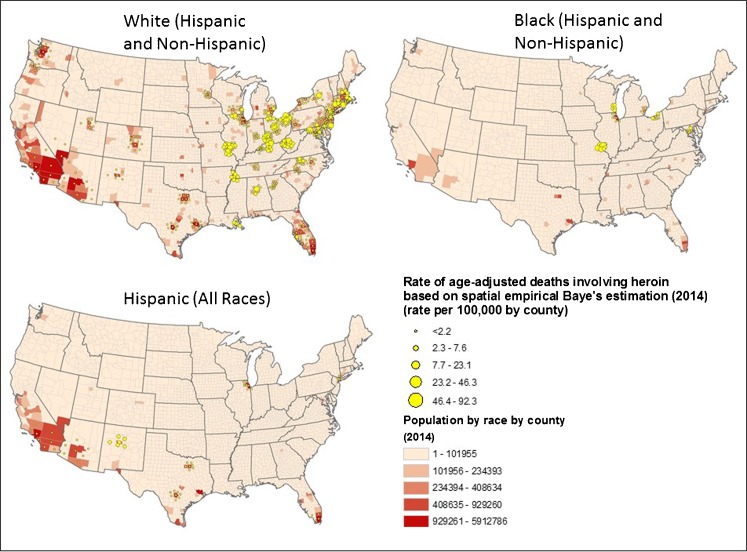
There were 31,701 deaths (approximately 92.3% of total deaths) from drug poisoning overdoses involving heroin among Whites during the period 2000 to 2014, compared to 2646 (7.7%) deaths for Blacks and 3297 (about 9.6%) for Hispanic individuals. In 2000, after spatial smoothing using age-adjusted rates, Whites comprised 56.9% of the total rates (based on White and Black deaths). This percentage increased to 88% in 2005, approached 100% of the estimated rates in 2010, and then decreased to 87.7% in 2014. Black spatially smoothed and age-adjusted death rates decreased from 43.1% in 2000 to 12% in 2005, further declined to less than 1% in 2010, and then increased to 12.3% in 2014. For Hispanics, the percentage of spatially smoothed age-adjusted rates increased from 0.8% in 2000 to 15.6% in 2005 and then declined to 4.9% in 2010 and 3.3% in 2014.
In 2000, Kern County, CA, appeared to have the highest spatially smoothed age-adjusted rate for Whites (rate of 1.1 per 100,000). The high rates shifted to counties around Bernalillo County, NM, and into the Great Lakes region (e.g., northern Pennsylvania and eastern MI) in 2005. In 2010, four counties in OH and MO had spatially smoothed age-adjusted death rates for Whites that exceeded 60 per 100,000. By 2014, the upward trend increased even more sharply for Whites, with most of these deaths occurring in counties in the northeast, Mid-Atlantic, and Great Lakes regions of the USA (a total of 488 counties) (Fig. 2). Together, these 488 counties represent approximately 15% of the total US White population. The highest spatially smoothed age-adjusted rate of 92.3 per 100,000 in 2014 was found in Marion County, OH, followed by a rate of 46.3 per 100,000 in Cabell County, WV (Fig. 2).
Fig. 2.
Spatial empirical Baye’s estimation of age-adjusted rate of deaths involving heroin per 100,000 for 2014 by race and ethnicity. Each map depicts the population data for the corresponding racial and ethnic group (i.e., White, Black, and Hispanic)
In 2000, the spatially smoothed age-adjusted rate was as high as 3.9 per 100,000 for Blacks in Essex County, NJ, with no spatially smoothed White age-adjusted death rates being estimated for this county. In 2005, Macomb County, MI (north of Detroit), had the highest spatially smoothed age-adjusted rate for Blacks, with a rate of 0.7 per 100,000, which is higher than the rate for Whites in this county. In 2010, due to small numbers and corresponding data suppression in CDC WONDER, no spatially smoothed age-adjusted rates were estimated for Blacks for any counties. Eight counties in the USA did have deaths including the Wayne County, MI, with a raw count of 18 deaths in this year. In 2014, however, the rates had increased, and 41 counties that together represent approximately 14% of the US Black population and 7% of total deaths involving heroin had spatially smoothed age-adjusted death rates for Blacks. The highest rate of 24.9 per 100,000 occurred in St. Louis, MO (an independent city administered as a county). Twenty-five out of these 41 counties had spatially smoothed rates that exceeded the rates found for Whites, including counties in WI, MO (including the city of St. Louis, with a rate of 24.9 per 100,000), IL (the smoothed rate for Black deaths in Cook County was three times that of White deaths), MI, MD (Baltimore City and Montgomery County, MD), OH, VA, and the District of Columbia (Fig. 2).
For Hispanics, a significant increase in percentage of spatially smoothed age-adjusted rate from 2000 to 2005 (0.8 to 15.6%) was found in three counties surrounding Los Angeles, CA, with a total rate as low as 0.3 per 100,000 in 2000, shifting to eight counties surrounding San Antonio in TX, total rate of 4.3 per 100,000 in 2005. A similar pattern existed in 2010 for Hispanics. In 2014, 45 counties in the Southwest, Great Lakes, and Mid-Atlantic regions that together represent approximately 24% of the US Hispanic population had smoothed age-adjusted death rates per 100,000. These counties include Bernalillo County, NM, with spatially smoothed age-adjusted death rate of 5.8 per 100,000 and Bronx, NY, with a rate of 0.7 per 100,000. Twenty-six of these counties had spatially smoothed age-adjusted death rates for Hispanics that exceeded the rates for both Black and White populations. Among these, 15 counties were in TX, six in NM (including Bernalillo County that had the highest spatially smoothed rate), and four in AZ and Miami-Dade County, FL.
Urban-Rural Patterns of Drug Poisoning Deaths Involving Heroin
We investigated whether drug poisoning deaths involving heroin have impacted urban or rural counties more frequently for the period 2000–2014 and found that approximately 82% of the raw counts of deaths (45,228 deaths) occurred in counties that are categorized as large metro (i.e., population >1 million), significantly exceeding the number of deaths in small metro counties (population 50,000–249,999) (529 deaths). The percentage of counties that are classified as large metro with a spatially smoothed death rate increased from 56.3% in 2000 to 62.4% in 2005 and to 73.1% in 2010 and then decreased to approximately 55.8% in 2014 (285 out of 511 counties found to have a spatially smoothed age-adjusted death rate per 100,000 are classified as large metro in 2014) (Fig. 3). Based on the spatial empirical Baye’s estimated age-adjusted rates, the mean spatially smoothed rates for deaths involving heroin are actually lower in large metro counties than small metro or non-metro counties in each year from 2000 to 2014. While only 12 small metro counties had spatially smoothed age-adjusted death rates before 2011, in 2014, spatially smoothed age-adjusted death rates were found for 34 small metro counties (approximately 5% of total deaths involving heroin). A similar, increasing pattern was found to exist for counties classified as non-metro, representing more rural locations. In 2014, there were 92 non-metro counties with a spatially smoothed age-adjusted rate of deaths involving heroin, while before 2012, only 25 were non-metro counties (12 non-metro counties in 2000, 14 in 2005, and 17 in 2010. Note that some of these counties had rates in each of these years). In 2014, the mean spatially smoothed age-adjusted rate for non-metro locations was as high as 3.2 per 100,000 while the rate was only 0.8 per 100,000 for large metro counties. Figure 3 shows that in 2014, only one out of the four counties that fall into the highest two classes of rates (spatially smoothed age-adjusted rate >18.9 per 100,000) is classified as large metro (Campbell County, KY), while one county, Cabell County, WV, is categorized as medium metro, and two counties, Marion County, OH, and Rio Arriba County, NM, are non-metro counties (Fig. 3).
Fig. 3.
Spatial empirical Baye’s estimated rate of deaths involving heroin per 100,000 by county (2014) and urbanization classification (2013)
Patterns of Drug Poisoning Deaths Involving Heroin by Age and Gender
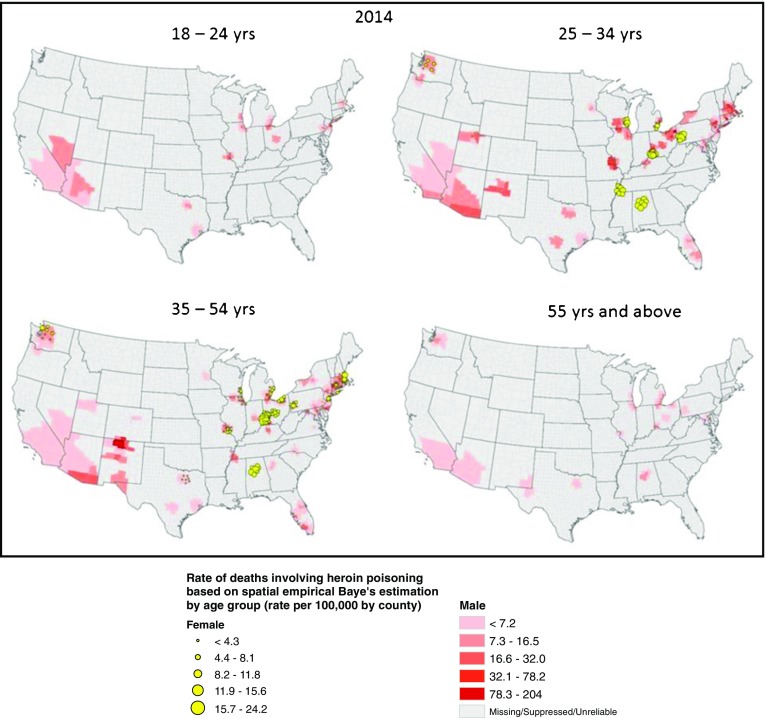
For an analysis of the trends in deaths involving heroin by age and gender, we examined four age categories, 18–24, 25–34, 35–54, and over 55 years, and used spatial empirical Baye’s estimation of the rate of deaths involving heroin poisoning per 100,000. Due to data suppression in the CDC WONDER dataset when raw counts are lower than 10, many counties had suppressed counts pertaining to either age or gender groups. We found that in 2000, 72.3% of the spatially smoothed death rates (applied to raw counts) occurred among 35–54-year-olds while 21.7% were 25–34-year-olds and were located in the Mountain region (e.g., Salt Lake City, UT) and in New England, respectively. In 2005, the percentage for 35–54-year-olds increased to approximately 78%, involving 35 counties in the Mountain, Great Lakes, New England, and Mid-Atlantic regions. While these spatially smoothed rates remain high for this age group in the following 10 years until 2014, the percentage of deaths for this group decreases to around 40% in 2010 and 37% in 2014. Meanwhile, the age groups of impacted individuals shift towards younger ages. In 2005, about 14% of spatially smoothed death rates applied to 25–34-year-olds in 10 counties near Pittsburgh, PA, and Detroit, MI. In 2010, the percentage increased sharply to 41% for this age group (108 counties mainly in the Great Lakes region), and in 2014, the 25–34-year-old group accounted for almost 45% of the spatially smoothed death rates (381 counties impacted). Of these impacted counties, 20 counties in New England, Mid-Atlantic, and the Ohio Valley region had spatially smoothed death rates over 31.5 per 100,000 (which ranks in the highest 5% of rates for this group). For the youngest age group, 18–24 years, there was also an increase in spatially smoothed rates from 6.8% and 7 counties in 2005 (around Dallas, TX) to 11.4% and 43 counties in 2010 (impacting counties near Los Angeles, Phoenix, New York City, Cleveland, Chicago, Dallas, and San Antonio) and to 12% and 163 counties in 2014 (impacting the Southwest, the Great Lakes region, Ohio Valley, and New England).
An examination of gender using spatial empirical Baye’s estimation found that males were impacted more than females from overdose deaths involving heroin during 2000–2014, but the estimated rates of male deaths show a decrease over time. In 2000, 96.3% of the estimated poisoning deaths involving heroin occurred among males in 160 counties across the USA. In 2005, this had decreased to 94.6% but expanded to 181 counties. Before 2010, Allegheny County, PA, was the most impacted county for male deaths, with Baltimore City, MD, and Passaic County, NJ, also belonging to the category with the highest spatially smoothed male death rates. In 2010, the spatially smoothed rates for male deaths decreased to 91.3% while expanding to 277 counties, with the highest rates estimated for Clermont County, OH, and St. Louis City, MO. In 2014, male deaths decreased further to 85.3% while expanding to 674 counties. The highest spatially smoothed rate in 2014 occurred in Rio Arriba County, NM, while counties in New England, the Ohio Valley, and the Great Lakes regions were also impacted by high rates of male deaths.
In contrast, while remaining low, the spatially smoothed rate of deaths for females gradually increased from 5% in 2005 to 8.7% in 2010 and reached 14.6% in 2014. The spatial pattern of deaths among females shifted from 22 counties in southern CA and Great Lakes region in 2000 to 60 counties in the Midwest in 2010 and to 282 counties in 2014, including counties in the Mountain region, New England, and Mid-Atlantic areas. In 2014, the estimated rates suggest that while females were impacted more than males in less than 1 % of counties, two counties, Sandoval County, NM, and St. Clair County, IL, had estimated death rates that exceeded the rates for males. The spatially smoothed rate for Sandoval County, NM, was estimated at 1.9 per 100,000 (exceeding the rate for males by more than 50%) and St. Clair County, IL, where the spatially smoothed rate for female deaths is estimated to be 2.5 per 100,000 (exceeding the rate for males by almost 38%).
Combining age and gender, we found in general that the spatially smoothed rate is higher for males aged 35–54 than for other age-gender groups for the study period. The highest estimated rate for this group occurred in Rio Arriba County, NM (a spatially smoothed rate of 204 per 100,000), followed by St. Louis City, MO (spatially smoothed rate of 78.2 per 100,000).In 2000, males aged 35–54 on the west coast of the USA were the most impacted group. By 2010, the highest impact had shifted to males aged 25–34 in the Midwest and Great Lakes regions where St. Louis County, MO; Monroe County, IL; and Macomb and St. Clair Counties, MI, had spatially smoothed estimated death rates over 20 per 100,000. In 2010, due to data suppression and small numbers, no counties returned spatially smooth death rates for females for any of the age categories. In 2014, a more diverse age-gender pattern was returned with a higher spatially smoothed death rate found for males aged 18–24 (highest in Monmouth County, NJ, with an estimated rate of 42.3 per 100,000) and over 55 years (highest in St. Louis City, MO). Additionally in 2014, spatially smoothed death rates suggest that females are impacted more among younger age groups including those aged 25–34 (highest in Hamilton County, OH, with a spatially smoothed rate of 24.2 per 100,000) as well as women aged 35–54 (highest in Butler County, OH, with an estimated rate of 21.4 per 100,000) (Fig. 4).
Fig. 4.
Spatial empirical Baye’s estimated rates per 100,000 per county for four age-gender groups for 2014
Spatiotemporal Patterns of Drug Poisoning Deaths Involving Heroin
To learn more about the evolution and patterns of deaths involving heroin in the USA and to identify locations where concentrations of deaths may exist, spatial cluster analysis was undertaken using global Moran’s I and LISA statistics. Cluster analysis of summed age-adjusted death rates using spatial empirical Baye’s smoothing during 2000 to 2014 shows it is unlikely that the spatial pattern is random as illustrated by a positive Moran’s I of 0.364. In addition, a p value smaller than 0.001 indicates the result is statistically significant. The result of local Moran’s I for the summed spatially smoothed deaths rate during the study period found 301 counties that belong to high-high clusters (i.e., counties with high spatially smoothed rates of drug poisoning deaths involving heroin that are adjacent to counties with similarly high counts) are located in New England, the Mid-Atlantic, and central Ohio Valley regions, as well as in the Mountain region and on the west coast, for example, counties around Seattle, WA. The analysis also returned low-high outliers (where low to no spatially smoothed death rates adjacent to counties with high spatially smoothed rates for these counties during this period) including Costilla County, CO, near Rio Arriba County, NM, and 33 counties in central Ohio Valley near Cincinnati and Toledo, OH, as well as Greene County, IL, near St. Louis, MO. These clusters have p values lower than 0.05, indicating a statistical significance with 95% confidence interval. There is one high-low outlier (counties with high spatially smoothed rates adjacent to counties with low counts) in Davidson County, TN, near Nashville. No statistically significant cold spots were found to exist during the study period.
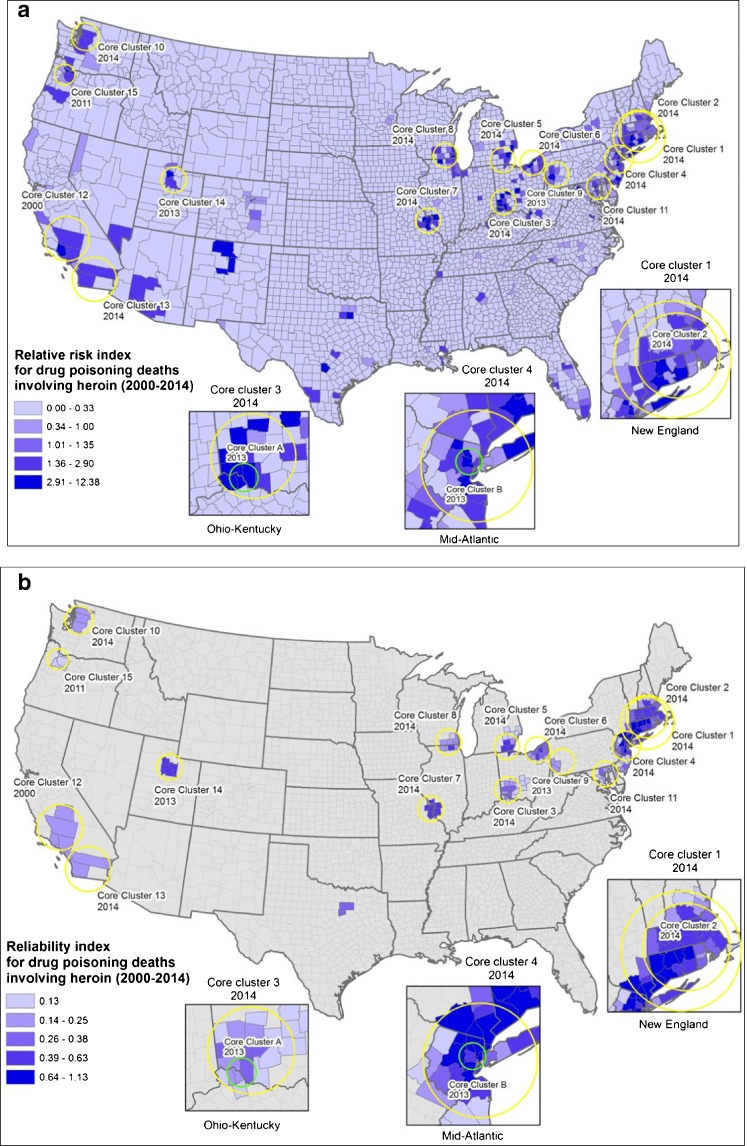
Cluster analysis using spatial and temporal scan statistics (SaTScan) was performed to understand more clearly the evolution of hotspots or clusters of drug poisoning deaths involving heroin over space and time. Based on raw counts of deaths, the SaTScan statistical algorithm returns a relative risk index for each county (Fig. 5a). This analysis revealed 13 spatiotemporal core clusters ordered by a likelihood ratio. As SaTScan has a tendency to generate clusters that are broad in spatial extent and include a large number of low-risk counties, a set of core clusters are defined as low percentage of counties with low risk (below 33% in this research) and where the likelihood ratio of a cluster is higher than 80 [32] (Fig. 5a). As indicated by p values <0.01, all the core clusters are statistically significant. The high-risk counties (relative risk index >2.9) are in New England and central Ohio Valley. Approximately 63% of counties with the highest risk indices are found in core clusters 1 to 8. The highest risk index is associated with St. Louis City, MO, in 2014, corresponding to core cluster 7.
Fig. 5.
a Relative risk of drug poisoning deaths involving heroin by county and core clusters (2000–2014) and b reliability index by county and core clusters (2000–2014)
Based on the complete dataset for 2000–2014, 15 core clusters are identified and ranked by the value of likelihood ratio. In Fig. 5a, relative risk indexes are classified using natural breaks, but with breaking value 1 to separate high- and low-risk counties. The two core clusters with the highest likelihood ratios (core clusters 1 and 2) are linked to the year 2014 for counties in New England and the Mid-Atlantic states, shown in the inset map. The first of these, core cluster 1, contains 34 counties in MA, NH, CT, RI, and NY, where approximately 70% of the counties have relative risk index over 1 (highest index value of 4.6 in Hartford County, CT). Core cluster 2 is within core cluster 1 and is comprised of 27 counties in these five states. Both these core clusters have high likelihood ratios (1310.3 and 1203.4, respectively). Core cluster 3 is located around Cincinnati, OH, and contains 14 counties, with 7 falling in the highest class (relative risk >2.91) and a likelihood ratio approaching 883. The next 8 core clusters, appear in the Mid-Atlantic and Great Lakes region, except core cluster 10 that is composed of 6 counties near Seattle, WA. The highest relative risk index appeared in St. Louis City, MO, which belongs to core cluster 7 in 2014. Nine of these 11 core clusters are all linked to data from 2014, except for core cluster 9 that occurred in 2013 and that covered three counties near Pittsburg, PA, where Allegheny County is identified with the second highest relative risk index 7.7 in the USA. Within core clusters 3 and 4, there are also three counties in each of these clusters (near Cincinnati, OH, and New York City, NY, respectively) that were found to be core clusters in 2013, shown as core clusters A and B in the inset maps in Fig. 5a. Core cluster 12 is located near Los Angeles County, CA, and is linked to data from the year 2000. Core cluster 13 is located in San Diego, CA, spatially close to Los Angeles albeit temporally distant, as this cluster emerges in 2014. Based on this analysis, it can be noted that Los Angeles County did not maintain an association with a core cluster after 2000. Core cluster 14 is located near Salt Lake City, UT, in 2013. Core cluster 15 appeared in three counties near Portland, OR, in 2011. Each of these four core clusters (core cluster 12–15) contains three counties.
A sensitivity analysis using SaTScan shows the reliability of a county belonging to one of the core clusters, where while adjusting the maximum size of risk population (based on 0.2% of the county population at risk, 0.4, 0.6, 0.8, 1, 2, 4, and 5%), the likelihood ratio remains higher than 80 through the eight sensitivity runs (Fig. 5b). This analysis identifies which counties continue to be detected as clusters using these different percentages of population at risk and based on the numbers of drug poisoning deaths involving heroin across the USA for 2000–2014. The highest reliability index is higher than 1 and corresponds to Passaic County, NJ (reliability index 1.13). Throughout the different runs of the sensitivity analysis, it was found that this county appears in two of the identified core clusters (clusters 1 and 4). Seventeen counties in the New England and Mid-Atlantic states (6 counties in CT, 5 in NY, and 6 in NJ) have scores in the highest class of reliability (index between 0.64 and 1.13). Thirteen counties located in the first two core clusters and 5 counties in New Jersey in core cluster 4 have scores in the second highest class (index between 0.39 and 0.63). The remaining counties in this category are located in core clusters 5, 6, 7, and 8 located mainly in the Great Lakes region and Ohio Valley and cluster 14 in Utah. The results show that while many counties in the USA have experienced an impact from drug poisoning involving heroin, few counties are part of a core cluster for multiple years until 2013, when counties in New England, the Mid-Atlantic, and Great Lakes regions form core clusters that continue through 2014.
Discussion
Analyzing the spatial and spatiotemporal pattern of drug poisoning deaths involving heroin in the USA during 2000–2014 shows the pattern of an increasing impact of overdose deaths involving heroin in the USA with varying impacts among different population groups by urbanization, age, gender, race, and ethnicity. Research on prescription opioid misuse in 2011 and 2012 found that urban residents were more likely to misuse prescription opioids than individuals living in rural locations. In our study, we found that while higher spatially smoothed age-adjusted rates for drug poisoning deaths involving heroin were estimated for counties classified as large metro, data from more recent years shows a growing number of small metro and non-metro counties to be impacted by drug poisoning overdoses involving heroin. This finding coincides with previous research that heroin use extends to Whites living outside urban areas, where heroin may be more available and less costly and used by individuals who misuse opioids [13, 21, 22].Our research finds that the spatially smoothed estimated rate of deaths among Whites is significantly higher than for other racial groups. However, we found that the spatially smoothed Black death rates are estimated to be high in certain urban locations (exceeding the rate of other population groups) with a corresponding high Black population (e.g., Baltimore, MD, and St Louis, MO). Previous research for 1990–2005 found that heroin overdoses particularly impacted Hispanic males in NM [34]. We also found a high rate of deaths (a total of 4.3 per 100,000 per county) for Hispanics in 2005, which corresponds to an increasing trend of heroin use among Hispanics during mid 2000s [16]. In 2014, six counties in NM were estimated to be impacted by a high age-adjusted spatially smoothed rates (a total of 26.9 per 100,000 per county) among Hispanics, higher than the spatially smoothed rates estimated for Whites and Blacks in those counties.
Males aged 35–54 years are the gender-age group most impacted overall, while spatially smoothed death rates for younger age groups showed an increase since 2005. These results correspond with the findings from studies on heroin use in Seattle where it was found that younger heroin and opioid injectors were more at risk than older heroin injectors [35] and that 39% of heroin users in a study using data collected for 2010–2014 were ages 18–29 years [12]. The major causes of this upward trend of overdoses among younger users include recent increased access to prescription opioids, injection behaviors and networks, HIV-risk perceptions, and sharing of syringes [13, 14, 36]. In addition, our study revealed an increase in the estimated rate of deaths of males aged over 55 years in New England, the Ohio Valley, CA, and NM in 2014. Smoothed age-adjusted death rates for females were significantly lower than for males overall. However, in 2014, hotspots for females based on spatially smoothed estimated rates were found in NM and OH, where smoothed death rates were estimated to exceed the rates for males. Similar findings also appeared in research using data from 1990 to 2005 on overdoses involving heroin; White females in NM were found to be a highly impacted group [34].
The spatiotemporal cluster analysis of drug poisoning deaths involving heroin using SaTScan indicates the counties that comprise core clusters in New England, Mid-Atlantic, and Great Lakes region corresponded to the two highest categories of spatially smoothed rates of deaths in 2014. The counties in these regions also correspond to the highest two categories of spatially smoothed rates of deaths among males aged 25–54 in 2014. According to our analysis, the 15 core clusters in Fig. 5 contain 62.5% of counties that fall in the three highest classes of spatially smoothed rate of deaths for Whites and 80% of counties that fall in this same group of classes for Blacks. Approximately 65% of counties in the core clusters are categorized as large metro areas while 6.4% are small metro. Our analysis revealed a significant hotspot using both Moran’s I and SaTScan in the Seattle region in 2014 that is also discussed in studies on drug use in Seattle [12, 35]. Although the risk index is high (between 2.90 and 12.38) in three counties in NM and two counties in TX, these counties do not belong to any of the core clusters mapped in Fig. 5a. These counties do show up in the results of local Moran’s I test as statistically significant high-low outliers that contribute to a spatially variable impact from deaths involving heroin for these areas.
Limitations
Previous studies have pointed out that drug poisoning deaths data may be underestimated as classifying drug poisoning deaths relies heavily on the professional judgment of medical examiners and coroners and that methods and expertise may vary widely across jurisdictions and this could have a substantial impact when analyzing county-level drug deaths data [7, 8]. This limitation should be acknowledged regarding the data on drug overdose (poisoning deaths) involving heroin used for this research as well and could mean that although we have used spatial empirical Bayes estimation techniques, our results may still be underrepresenting the possible number of deaths. Also, due to the small number of counties with reportable data (raw counts or age-adjusted rates) for certain population groups before 2010, the spatially smoothed estimates for these years may benefit from further sensitivity analysis. In addition, regarding the use of drug-specific (i.e., heroin) drug-involved poisoning deaths, there may be variability in attributing drug type to drug poisoning deaths. For example, one research study noted that 25% of drug poisoning deaths did not have drug type available [8]. Finally, since county size is so variable, the calculation of weights based on neighboring counties used in the geostatistical analyses, for example, Moran’s I, may be overestimated for some counties. Some studies have examined this in more detail [8], and alternative weighting approaches using K-nearest neighbors have been proposed.
Conclusions
The analysis of the geographic distribution and spatiotemporal clustering of drug poisoning deaths involving heroin in the USA during 2000–2014 provides a comprehensive view of the variations in the patterns of mortality rate from these overdoses involving heroin based on race and ethnicity, urbanization, age, and gender. Our research reveals significant clusters of deaths existed in southern CA in 2000, emerging again in 2013 in counties in New England, the Mid-Atlantic, and Great Lakes region and persisting in these counties through 2014. In general, while White populations are impacted the most overall by drug poisoning deaths involving heroin, both Black and Hispanic population groups are estimated to also be significantly impacted in counties where these populations are higher. With respect to urbanization, our study shows a significant decrease in the spatially smoothed rate of deaths per 100,000 by county in large metro areas from 2010 to 2014 and a shift to small metro and non-metro counties. From the perspective of age and gender, our study revealed an increasing trend over time of drug poisoning deaths involving heroin among younger ages (18–24 and 25–34 years), as well as female populations in the northeast and central states of the USA, especially in 2014 based on spatially smoothed rates. This study provides both a spatial and temporal understanding of the evolving pattern of deaths from overdoses involving heroin across the country for this time period. The variation of impacts and burden on different population groups is important for developing strategies and policies regarding substance use and misuse interventions for a range of different urbanization classes (e.g., small metro and non-metro) and population groups (e.g., Blacks, Hispanics, younger individuals, and females). A better understanding of these dynamics is critical to intervention and reductions in mortality in high-risk counties. Solutions could include planning for nasal naloxone distribution that is considered worldwide as a highly effective antidote for intervening deaths from heroin overdoses [10, 37]. Future work will examine geographic patterns associated with the use and misuse of other opioids including fentanyl in the USA.
Acknowledgments
Research reported in this publication was supported by the NIDA-funded National Drug Early Warning System (NDEWS). NDEWS is supported by the National Institute on Drug Abuse of the National Institutes of Health, under Cooperative Agreement U01DA038360, awarded to the Center for Substance Abuse Research (CESAR) at the University of Maryland, College Park. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
References
- 1.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. Rockville. 2012.
- 2.Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. Rockville. 2015.
- 3.Ford M, Dulaney AR. Prescription drug overdose: data from Carolinas Poison Center. N C Med J. 2014;74(3):74316. http://www.cdc.gov/psr/prescriptiondrug/. Accessed Aug 2016 [PubMed]
- 4.Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. “Every ‘never’ I Ever Said Came True”: transitions from opioid pills to heroin injecting. Int J Drug Policy. 2014;25(2):257–266. doi: 10.1016/j.drugpo.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coplan PM, Kale H, Sandstrom L, Landau C, Chilcoat HD. Changes in oxycodone and heroin exposures in the National Poison Data System after introduction of extended-release oxycodone with abuse-deterrent characteristics. Pharmacoepidemiol Drug Saf. 2013;22:1274–1282. doi: 10.1002/pds.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dertadian GC, Maher L. From oxycodone to heroin: two cases of transitioning opioid use in young Australians. Drug Alcohol Rev. 2014;33(1):102–104. doi: 10.1111/dar.12093. [DOI] [PubMed] [Google Scholar]
- 7.Rossen LM, Khan D, Warner M. Trends and geographic patterns in drug-poisoning death rates in the U.S., 1999–2009. Am J Prev Med. 2013;45(6):e19–e25. doi: 10.1016/j.amepre.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rossen LM, Khan D, Warner M. Hot spots in mortality from drug poisoning in the United States, 2007-2009. Heal Place. 2014;26:14–20. doi: 10.1016/j.healthplace.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Darke S, Marel C, Mills KL, et al. Patterns and correlates of non-fatal heroin overdose at 11-year follow-up: findings from the Australian Treatment Outcome Study. Drug Alcohol Depend. 2014;144:148–152. doi: 10.1016/j.drugalcdep.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Strang J. Death matters: understanding heroin/opiate overdose risk and testing potential to prevent deaths. Addiction. 2015;110:27–35. doi: 10.1111/add.12904. [DOI] [PubMed] [Google Scholar]
- 11.Mateu-Gelabert P, Harris S, Berbesi D, et al. Heroin use and injection risk behaviors in Colombia: implications for HIV/AIDS prevention. Subst Use Misuse. 2016;51(2):230–240. doi: 10.3109/10826084.2015.1092989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cedarbaum ER, Banta-green CJ. Health behaviors of young adult heroin injectors in the Seattle area. Drug Alcohol Depend. 2016;158:102–109. doi: 10.1016/j.drugalcdep.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 13.Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO. “Hooked on” prescription-type opiates prior to using heroin: results from a survey of syringe exchange clients. J Psychoactive Drugs. 2012;44(3):259–265. doi: 10.1080/02791072.2012.704591. [DOI] [PubMed] [Google Scholar]
- 14.Jenkins LM, Banta-Green CJ, Maynard C, et al. Risk factors for nonfatal overdose at seattle-area syringe exchanges. J Urban Heal. 2011;88(1):118–128. doi: 10.1007/s11524-010-9525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dasgupta N, Creppage K, Austin A, Ringwalt C, Sanford C, Proescholdbell SK. Observed transition from opioid analgesic deaths toward heroin. Drug Alcohol Depend. 2014;145:238–241. doi: 10.1016/j.drugalcdep.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Martins SS, Santaella-Tenorio J, Marshall BDL, Maldonado A, Cerdá M. Racial/ethnic differences in trends in heroin use and heroin-related risk behaviors among nonmedical prescription opioid users. Drug Alcohol Depend. 2015;151:278–283. doi: 10.1016/j.drugalcdep.2015.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visconti AJ, Santos G-M, Lemos NP, Burke C, Coffin PO. Opioid overdose deaths in the city and county of San Francisco: prevalence, distribution, and disparities. J Urban Health. 2015;92(4):758–72. doi:10.1007/s11524-015-9967-y. [DOI] [PMC free article] [PubMed]
- 18.Rigg KK, Monnat SM. Urban vs. rural differences in prescription opioid misuse among adults in the United States: informing region specific drug policies and interventions. Int J Drug Policy. 2015;26(5):484–491. doi: 10.1016/j.drugpo.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Day C, Conroy E, Lowe J, Page J, Dolan K. Original article patterns of drug use and associated harms among rural injecting drug users: comparisons with metropolitan injecting drug users. Aust J Rural Health. 2006;14:120–125. doi: 10.1111/j.1440-1584.2006.00775.x. [DOI] [PubMed] [Google Scholar]
- 20.Wenger LD, Lopez AM, Comfort M, Kral AH. The phenomenon of low-frequency heroin injection among street-based urban poor: drug user strategies and contexts of use. Int J Drug Policy. 2014;25(3):471–479. doi: 10.1016/j.drugpo.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meiman J, Tomasallo C, Paulozzi L. Trends and characteristics of heroin overdoses in Wisconsin, 2003-2012. Drug Alcohol Depend. 2015;152:177–184. doi: 10.1016/j.drugalcdep.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA psychiatry. 2014;71(7):821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- 23.Cicero TJ, Surratt H, Inciardi JA, Munoz A. Relationship between therapeutic use and abuse of opioid analgesics in rural, suburban, and urban locations in the United States. Pharmacoepidemiol Drug Safety2. 2007;16:827–840. doi: 10.1002/pds.1452. [DOI] [PubMed] [Google Scholar]
- 24.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010-2015. Morb Mortal Wkly Rep. 2016;65:1445–1452. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 25.Kao D, Torres LR, Guerrero EG, Mauldin RL, Bordnick PS. Spatial accessibility of drug treatment facilities and the effects on locus of control, drug use, and service use among heroin-injecting Mexican American men. Int J Drug Policy. 2014;25(3):598–607. doi: 10.1016/j.drugpo.2013.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beardsley K, Wish ED, Fitzelle DB, O’Grady K, Arria AM. Distance traveled to outpatient drug treatment and client retention. J Subst Abus Treat. 2003;25(4):279–285. doi: 10.1016/S0740-5472(03)00188-0. [DOI] [PubMed] [Google Scholar]
- 27.Hester L, Shi X, Morden N. Characterizing the geographic variation and risk factors of fatal prescription opioid poisoning in New Hampshire, 2003-2007. Ann GIS. 2012;18(2):99–108. doi: 10.1080/19475683.2012.668558. [DOI] [Google Scholar]
- 28.Moran PA. The interpretation of statistical maps. J R Statisitcal Soc Ser B. 1948;10(2):243–251. [Google Scholar]
- 29.Anselin L. Local indicators of spatial association: LISA. Geogr Anal. 1995;27(2):93–115. doi: 10.1111/j.1538-4632.1995.tb00338.x. [DOI] [Google Scholar]
- 30.Kulldorff M. A spatial scan statistic. Commun Stat - Theory Methods. 1997;26(6):1481–96. doi:10.1080/03610929708831995.
- 31.Kulldorff M, Heffernan R, Hartman J, Assuncao R, Mostashari F. A space-time permutation scan statistic for disease outbreak detection. PLoS Med. 2005;2(3):0216–0224. doi: 10.1371/journal.pmed.0020059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen J, Roth RE, Naito AT, Lengerich EJ, Maceachren AM. Geovisual analytics to enhance spatial scan statistic interpretation: an analysis of U.S. cervical cancer mortality. Int J Health Geogr. 2008;7:57. doi: 10.1186/1476-072X-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barro AS, Kracalik IT, Malania L, Tsertsvadze N, Manvelyan J, Imnadze P, et al. Identifying hotspots of human anthrax transmission using three local clusering techniques. Appl Geogr. 2015;60:29–36. doi:10.1016/j.apgeog.2015.02.014.
- 34.Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990-2005: combinations of heroin, cocaine, prescription opioids and alcohol. Addiction. 2008;103(1):126–136. doi: 10.1111/j.1360-0443.2007.02054.x. [DOI] [PubMed] [Google Scholar]
- 35.Banta-Green C, Jackson TR, Freng S, et al. Drug abuse trends in the Seattle-King County area: 2014. Alcohol & Drug Abuse Institute, Univ. of Washington, June 17, 2015. adai.uw.edu/pubs/cewg/DrugTrends_2014_final.pdf. Accessed Aug 2016.
- 36.Pollini RA, Banta-Green CJ, Cuevas-Mota J, Metzner M, Teshale E, Garfein RS. Problematic use of prescription-type opioids prior to heroin use among young heroin injectors. Subst Abuse Rehabil. 2011;2(1):173–180. doi: 10.2147/SAR.S24800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346(January):f174. doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]