Abstract
This study aimed to evaluate the scientific evidence regarding the effectiveness of silver diamine fluoride (SDF) in preventing and arresting caries in the primary dentition and permanent first molars. A systematic review (SR) was performed by 2 independent reviewers using 3 electronic databases (PubMed, ScienceDirect, and Scopus). The database search employed the following key words: “topical fluorides” AND “children” AND “clinical trials”; “topical fluorides” OR “silver diamine fluoride” AND “randomized controlled trial”; “silver diamine fluoride” AND “children” OR “primary dentition” AND “tooth decay”; “silver diamine fluoride” OR “sodium fluoride varnish” AND “early childhood caries”; and “silver diamine fluoride” AND “children”. Inclusion criteria were articles published in English, from 2005 to January 2016, on clinical studies using SDF as a treatment intervention to evaluate caries arrest in children with primary dentition and/or permanent first molars. Database searches provided 821 eligible publications, of which 33 met the inclusion criteria. After the abstracts were prescreened, 25 articles were dismissed based on exclusion criteria. The remaining 8 full-text articles were assessed for eligibility. Of these, 7 publications were included in the SR. These included 1 study assessing the effectiveness of SDF at different concentrations; 3 studies comparing SDF with other interventions; 2 investigations comparing SDF at different application frequencies and with other interventions; and 1 study comparing semiannual SDF applications versus a control group. The literature indicates that SDF is a preventive treatment for dental caries in community settings. At concentrations of 30% and 38%, SDF shows potential as an alternative treatment for caries arrest in the primary dentition and permanent first molars. To establish guidelines, more studies are needed to fully assess the effectiveness of SDF and to determine the appropriate application frequency.
Dental caries is the most frequent childhood chronic disease worldwide.1–3 Early childhood caries (ECC), the presence of 1 or more decayed, missing, or filled tooth surfaces (dmfs) in any primary tooth in a preschool-aged child, has been recognized by the American Dental Association as an important public health issue.4
In recent years, a reduction in overall caries indicators has been reported; however, an increase in ECC has been documented.5–7 If ECC remains untreated, oral health–related quality of life, body weight, growth, school attendance, and school performance can be affected.8,9 In addition, children with ECC treated under general anesthesia have a higher predisposition to develop dental caries in the permanent dentition.10 Because a severe ECC experience is an important predictor for adult caries, strategies to prevent and control ECC are important to improve general and oral health.11–13
Feeding habits and a variety of biological, environmental, and socioeconomic factors are involved in the development of ECC.14,15 One important socioeconomic factor is the lack of child dental insurance. Access to dental insurance has been found to correlate with age and is inversely related to family income and the educational level of the mother.16 ECC is therefore exacerbated in children residing in underprivileged areas, where carious lesions remain untreated due to limited financial resources and facilities.17,18
Dental caries can be prevented or arrested.19 Moreover, preventive measures for ECC are more cost effective than emergency room visits or restorative treatments when the illness has been established.20,21 A variety of evidence-based approaches for caries prevention have been reported; however, these strategies demand significant financial investment and depend on the availability of oral health workforces and facilities.18 Effective ECC preventive measures include the use of fluoride varnish—such as 5% sodium fluoride (NaF)—and the use of fluoridated toothpaste.22–25 In the management of cavitated ECC, atraumatic restorative treatment (ART) has been recommended. ART is painless, is low cost, and can be applied outside the clinical setting or when conventional treatment is not available. A disadvantage of this treatment is its high rate of failure.26
Interest in the use of silver diamine fluoride (SDF) has been growing. SDF has been used as an alternative treatment for caries prevention and arrest.27 In 2014, SDF was approved by the US Food and Drug Administration as a treatment for dentinal sensitivity.28 SDF had been used off-label for caries arrest; however, it was recently approved (code D1354) as an interim cariesarresting medicament.29
In vitro studies have demonstrated that SDF increases the pH of biofilm, reduces dentin demineralization, and has antimicrobial action against cariogenic bacteria.30 However, treated teeth sometimes develop black stains as a result of silver phosphate precipitation.31 Ex vivo and in vivo studies on cavitated extracted teeth from children receiving semiannual applications of SDF have shown effectiveness in arresting lesions as well as higher fluoride uptake compared to fluoride varnish and acidulated phosphate fluoride gel.32,33
Clinical studies have demonstrated the effectiveness of SDF in childhood caries prevention and arrest. Semiannual applications of SDF at 38% concentration have been recommended.34 SDF has been suggested for difficult-to-treat lesions and patients with high caries risk, including those with medical or behavioral complications, those who require multiple treatment visits, or those without access to dental care.35
The purpose of this systematic literature review was to evaluate the scientific evidence regarding the effectiveness of SDF in preventing and arresting dental caries in the primary dentition and permanent first molars.
Materials and methods
A systematic literature database search was performed by 2 independent reviewers using PubMed, ScienceDirect, and Scopus. The search included the following sets of key words:
“Topical fluorides” AND “children” AND “clinical trials”
“Topical fluorides” OR “silver diamine fluoride” AND “randomized controlled trial”
“Silver diamine fluoride” AND “children” OR “primary dentition” AND “tooth decay”
“Silver diamine fluoride” OR “sodium fluoride varnish” AND “early childhood caries”
“Silver diamine fluoride” AND “children”
The following filters were applied to these terms: clinical trial, published in the last 10 years (or since 2005), English, and journal (or dental journal).
The search was conducted from August 2015 to January 2016. Inclusion criteria were a randomized controlled trial (RCT) using SDF as 1 of the interventions, a population of children with primary dentition and/or permanent first molars, and manuscripts published in English from 2005 to January 2016. Exclusion criteria included other study designs, manuscripts in different languages or published outside the target timeframe, RCTs not using SDF as 1 of the interventions, and/or adults or children with complete permanent dentitions. The research question addressed was: In children who have caries in primary teeth and/or permanent first molars, is the use of silver diamine fluoride more effective than other strategies in the prevention and/or arrest of carious lesions?
A database was developed to compare and assess each reviewer search. Three eligibility phases were employed: titles, abstracts, and full-text screening. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement guidelines were followed.36 The data extraction form included the study design, SDF concentration and frequency, other treatment interventions used, SDF application techniques, and SDF adverse events. The outcomes reported were mean number of surfaces with new, active, and inactive caries at baseline and follow-up; mean numbers of arrested surfaces; the percentage of caries arrested; and caries increment. The risk of bias was assessed using a simplified analysis adapted from recommendations in the Cochrane Handbook for Systematic Reviews of Interventions.37
Results
A total of 1136 manuscripts were initially identified in database searches: 395 articles from PubMed, 255 articles from ScienceDirect, and 486 articles from Scopus (Chart). After duplicate records were eliminated, 821 articles remained. Of these, 33 met the inclusion criteria. After the abstracts were prescreened, 25 articles were dismissed based on the exclusion criteria, and the reviewers agreed to include 8 publications in the full-text article assessment phase. After review of the full text, the reviewers decided, by consensus, to exclude 1 of the reports due to inconsistencies in the description of the study design and results. Finally, a total of 7 studies were included in the systematic review.
Chart.
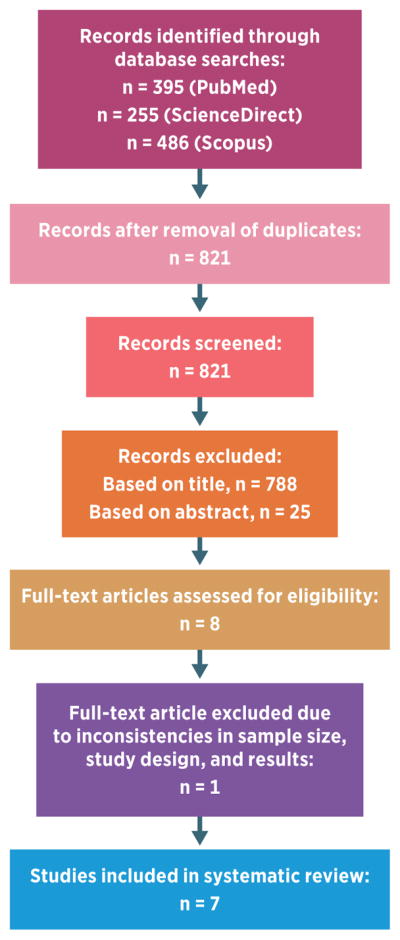
Selection of studies for the systematic review.
One study compared semiannual SDF applications versus a control group, 3 studies compared SDF with other treatment interventions, and 1 study assessed the effectiveness of SDF at different concentrations.38–42 The remaining 2 studies compared SDF at different application frequencies and with other treatment interventions.43,44
The RCTs had various durations (12–36 months) and were conducted in different countries. Two of the 7 studies were conducted in Brazil.39,41 The sample size was calculated according to the number of children or the number of carious surfaces. The caries diagnostic criteria used in these studies varied: decayed, missing, or filled teeth (dmft) or dmfs indices; International Caries Detection and Assessment System (ICDAS); visual criteria; or World Health Organization (WHO) criteria. The 7 selected studies could be categorized into 2 groups: children with primary dentition (4 studies) or children with primary dentition and at least 1 permanent first molar (3 studies).38–44 Studies in both groups evaluated the prevention and/or arrest of caries and compared SDF with other preventive measures: glass ionomer cement (GIC), cross-toothbrushing technique (CTT), interim restorative treatment, and fluoride varnish.
The articles included in this review were mainly conducted in school settings (kindergarten and primary schools). Only 1 of the studies was conducted in a dental school.39 Therefore, the context of these studies was basically outside the clinical setting (Table 1).
Table 1.
Designs of the studies included in the systematic review.
| Llodra et al (2005),38 Cuba |
|
|
| Design: 36 mo; RCT; blind |
| Site: 1 primary school |
| Visits: 7 (every 6 months) |
| Sample: N = 452 (95% CI, 80% power) |
| Randomization: individual random basis |
| Inclusion criteria: age ≥6 y |
| Diagnostic criteria: DMFS; caries activity: changes in dentin hardness and color |
| TX group: 38% SDF application every 6 mo |
| Control: no SDF; demographic characteristics not defined |
| SDF application technique: in primary teeth, no removal of carious tissue; in permanent teeth, removal of carious tissue |
| SDF adverse events: black stains; white lesions in oral mucosa in 3 participants (It is not clear whether these 3 children also developed black stains.) |
|
|
| Braga et al (2009),39 Brazil |
|
|
| Design: 30 mo; pilot RCT; blind |
| Site: Dental School of the University of São Paulo |
| Visits: baseline and 3, 6, 12, 18, and 30 mo |
| Sample: N = 66 first molars (22 children) |
| Randomization: assignment randomly selected and distributed in groups |
| Inclusion criteria: age 5–7 y with first molar with occlusal active initial caries without cavitation |
| Diagnostic criteria: modified Carvalho index (visual); radiographs at 6, 12, and 30 mo |
| TX groups: cross-toothbrushing technique; 10% SDF; glass ionomer cement |
| SDF application technique: applied in active caries lesions |
| SDF adverse events: black stains |
|
|
| Yee et al (2009),40 Nepal |
|
|
| Design: 24 mo; RCT; blind |
| Sites: kindergarten and primary schools |
| Visits: baseline and follow-up (6, 12, and 24 mo) |
| Sample: N = 976 (80% power, α = 0.05) |
|
Randomization: computer-generated list During randomization, sociodemographic characteristics were distributed homogenously between groups. |
| Inclusion criteria: age 3–9 y |
| Diagnostic criteria: DMFT and caries activity (changes in dentin hardness) |
| TX groups: 38% SDF without tea (SDF applied for 2 min); 38% SDF with tea (SDF applied for 2 min); 12% SDF without tea (SDF applied for 2 min) |
| Control: no treatment |
| SDF application technique: no caries removal |
| SDF adverse events: none reported |
|
|
| Dos Santos et al (2012),41 Brazil |
|
|
| Design: 12 mo; RCT |
| Sites: municipal schools |
| Visits: baseline, 6 mo, and 12 mo |
| Sample: N = 91 (90% CI, α = 0.05) |
| Randomization: by school |
| Inclusion criteria: age 5–6 y with primary teeth with active caries lesion with score of ICDAS 5 |
| Diagnostic criteria: ICDAS (code 5); Miller criteria; active caries lesions in the SDF group; failure of the sealant in the interim restorative treatment group (consistency of the dentin, resistance to probing) |
| TX groups: 30% SDF; interim restorative treatment |
| SDF application technique: in primary teeth, no removal of carious tissue |
| SDF adverse events: none reported |
|
|
| Monse et al (2012),42 Philippines |
|
|
| Design: 18 mo; RCT; blind |
| Sites: 8 public elementary schools |
| Visits: nonspecified |
| Sample: N = 1016 (80% power, α = 0.05) |
| Randomization: class list |
| Inclusion criteria: age 6–8 y with at least 1 erupted permanent first molar with a sound occlusal surface |
| Diagnostic criteria: WHO procedure tools and caries scores |
| TX groups: 38% SDF plus tannic acid (1 application); ART glass ionomer cement sealants plus high-viscosity material |
|
Control: no TX Due to noncompliance with the brushing program (3 schools), children were divided into nonbrushers and brushers during analysis. |
| SDF application technique: sound occlusal surfaces (or surfaces with enamel caries) of all erupted permanent first molars |
| SDF adverse events: none reported |
|
|
| Zhi et al (2012),43 China |
|
|
| Design: 24 mo; RCT; blind |
| Sites: 6 kindergartens |
| Visits: 6-mo intervals |
| Sample: N = 212 (80% power, α = 0.05) |
| Randomization: computer-generated list |
| Inclusion criteria: age 3–4 y with active dentin caries not involving the pulp |
| Diagnostic criteria: visual and tactile inspection |
| TX groups: 38% SDF every 12 mo; 38% SDF every 6 mo; glass ionomer cement every 12 mo |
| SDF application technique: removal of carious tissue by hand instruments |
| SDF adverse events: none reported |
|
|
| Duangthip et al (2016),44 Hong Kong |
|
|
| Design: 18 mo; RCT; blind |
| Sites: 16 kindergartens |
| Visits: baseline and 6, 12, and 18 mo |
| Sample: N = 304 (1670 lesions) (80% power, α = 0.05) |
| Randomization: stratified randomization |
| Inclusion criteria: age 3–4 y with at least 1 tooth with untreated active dentin caries not involving pulp |
| Diagnostic criteria: diagnosis of dentin caries by visual and tactile detection (ICDAS codes 5–6); visible plaque index |
| TX groups: 30% SDF at baseline every 12 mo; 30% SDF (3 applications at weekly intervals from baseline); 5% sodium fluoride varnish (3 applications at weekly intervals from baseline) |
| SDF application technique: no removal of carious tissue |
| SDF adverse events: black stains |
Abbreviations: ART, atraumatic restorative treatment; CI, confidence interval; DMFT, decayed, missing, and filled teeth; ICDAS, International Caries Detection and Assessment System; RCT, randomized controlled trial; SDF, silver diamine fluoride; TX, treatment; WHO, World Health Organization.
The SDF concentrations and sources in the selected studies are detailed in Table 2. A summary of the results of each study is presented in Table 3. The majority of the studies agreed that both 30% and 38% solutions were more effective for caries arrest than other interventions. In 4 studies, the effectiveness of 38% SDF in caries prevention and/or arrest was determined. 38,40,42,43 One of the clinical trials reported that a 38% SDF solution was significantly more effective for caries prevention in primary teeth (80% fewer new caries lesions; P < 0.05) and first molars (65% fewer new caries lesions; P < 0.001) compared to a control group.38 Also, children who received SDF treatment exhibited significantly more surfaces with inactive caries. Another study found that the caries arrest rate was significantly higher (53%) when 38% SDF was applied semiannually than when 38% SDF (37%) or GIC (28.6) was applied annually (P < 0.001).43 Another investigation showed that 38% SDF, with or without tea, was significantly more efficient in caries arrest in the primary dentition, both at 6 months and at 12 months, than 12% SDF and a control group (P < 0.001).40 Only 1 study reported that SDF was less effective than ART sealants; however, the trial design and follow-up showed deviations from the original protocol.42
Table 2.
Concentrations and source of silver diamine fluoride in the studies included in the systematic review.
| Concentration | Product | Manufacturer | Country | Studies |
|---|---|---|---|---|
| 38% | Fluoroplat | NAF Laboratorios | Argentina | Llodra et al38 |
| 10% | Cariostatic | Inodon Laborotório | Brazil | Braga et al39 |
| 12% | SDF | PROBEM Laboratório de Produtos Farmacêuticos Odontológicos | Brazil | Yee et al40 |
| 30% | Cariestop | Biodinâmica | Brazil | Dos Santos et al41; Duangthip et al44 |
| 38% | Saforide | Bee Brand Medical/Toyo Seiyaku Kasei | Japan | Yee et al40; Monse et al42; Zhi et al43 |
Table 3.
Results of the studies included in the systematic review.
| Study (year) | Objective | Statistical analysis | Results |
|---|---|---|---|
| Llodra et al (2005)38 | Assess the effectiveness of 6-month application of 38% SDF in preventing and arresting caries in primary and permanent teeth and compare with results in a control group | Student t test Multiple linear regression |
N = 452 Drop-out: n = 79 SDF was more effective for caries reduction in primary teeth (80%) and first molars (65%) than a control group. |
| Braga et al (2009)39 | Compare the effectiveness of SDF in arresting occlusal caries in erupting permanent first molars with the effectiveness of other noninvasive approaches (CTT and GIC) | Kruskal-Wallis test Friedman test |
N = 66 first molars (22 children) Drop-out: n = 8 (molars) After 3 and 6 months, 10% SDF showed a significantly higher capacity than CTT and GIC for arresting caries. A general reduction in active lesions was noted in all groups (P < 0.05). |
| Yee et al (2009)40 | Compare the effectiveness of a single application of 38% or 12% SDF, with or without the use of a reducing agent (tea), in arresting caries | ANOVA Student t test |
N = 976 Drop-out: n = 342 The number of arrested carious surfaces was significantly higher in 38% SDF and 38% SDF plus tea groups at 6 and 12 months (P < 0.001) and 24 months (P < 0.01) than it was in 12% SDF and control groups. |
| Dos Santos et al (2012)41 | Compare the caries-arresting properties of 30% SDF with those of IRT using GIC | Descriptive statistics Chi-square test Fisher exact test |
N = 91 (345 teeth) Drop-out: n = 23 teeth After 12 months, SDF was 1.73 (95% CI, 1.38–2.18) times more effective in arresting caries (RR, 66.9%) than IRT (RR, 38.6%) (P < 0.05). |
| Monse et al (2012)42 | Compare the effectiveness of 1 application of 38% SDF with that of ART sealants and no treatment in the prevention of dentinal caries (D3 lesions) | Chi-square test Cox proportional hazard model |
N = 1016 children Drop-out: n = 312 children The caries increment was lower in toothbrushing children than in nontoothbrushing children. HR was statistically significant for the nontreated children (HR, 0.43; CI, 0.21–0.87; P < 0.02) and the sealant-treated children (HR, 0.15; CI, 0.03–0.072; P < 0.02). |
| Zhi et al (2012)43 | Compare the effectiveness of annual and semiannual topical application of SDF solution with that of annual application of GIC in arresting active dentin caries in primary teeth | Chi-square test ANOVA Multilevel nonlinear logistic regression model |
N = 212 (719 lesions) Drop-out: n = 31 The group receiving 6-month applications of SDF showed higher caries arrest rates (OR, 2.98; CI, 1.35–6.69; P = 0.007) than groups receiving annual applications of SDF or GIC. |
| Duangthip et al (2016)44 | Compare the effectiveness of 3 topical fluoride application protocols (weekly SDF [3×], annual SDF, and NaF [3×]) in arresting dentin caries in the primary dentition | Chi-square test ANOVA Survival analysis (Bayesian approach) |
N = 304 (1670 lesions) Drop-out: n = 29 At 6 and 12 months, groups receiving intensive application of SDF had higher caries arrest rates than other treatment groups (annual SDF and weekly NaF varnish applications). At 18 months, the group receiving an annual SDF application presented a higher caries arrest rate (40%) than the groups receiving intensive SDF and NaF treatments (P < 0.001). |
Abbreviations: ANOVA, analysis of variance; ART, atraumatic restorative treatment; CI, confidence interval; CTT, cross-toothbrushing technique; GIC, glass ionomer cement; HR, hazard ratio; IRT, interim restorative technique; NaF, sodium fluoride; OR, odds ratio; RR, relative risk; SDF, silver diamine fluoride.
Two studies compared the effectiveness of SDF with temporary restorations in the arrest of caries.41,42 One of the studies found that 30% SDF was 1.73 times more effective to arrest caries (relative risk, 66.9%) than an interim restorative technique (relative risk, 38.6%) after 6 and 12 months (P < 0.05).41 The other study reported caries increments in toothbrushing and nontoothbrushing children treated with ART sealants or SDF as well as control groups. The hazard ratio (HR) was significantly lower in both sealant groups—with toothbrushing (HR, 0.12; confidence interval [CI], 0.02–0.61; P < 0.01) and without toothbrushing (HR, 0.33; CI, 0.20–0.54; P < 0.001)—than in the groups treated with SDF or the control groups.42
One of the selected studies compared the effectiveness of 30% SDF versus fluoride varnish in caries arrest rates.44 One group received SDF at baseline and again after 1 year; another group received 3 SDF applications at weekly intervals; and the third group received 3 applications of 5% NaF fluoride varnish at weekly intervals. After 1 year, the group receiving 3 SDF applications exhibited significantly higher caries arrest rates than did the other 2 treatments (P < 0.001). However, after 18 months the caries arrest rate of those receiving annual SDF application was significantly higher (40%) than that of those receiving intensive SDF or NaF varnish applications (35% and 27%, respectively).44
Another study compared the effectiveness of SDF with GIC and CTT.39 After 3 and 6 months, applications of 10% SDF showed a significantly greater capacity for arresting caries than both GIC and CTT. Additionally, a general reduction in active lesions was noted in all study groups (P < 0.05).39
Reports of adverse events in the present systematic review (SR) were uncommon. The presence of black discoloration in the arrested lesions was disclosed in 2 studies.38,44 One of these studies also reported the development of reversible, small, white lesions in the oral mucosa.38
As stated previously, the evaluation of the risk of bias for the studies included in this review was based on the recommendations from the Cochrane Handbook for Systematic Reviews of Interventions.37 Due to incomplete data or information omission, biases were difficult to identify clearly. Corresponding authors were not contacted; therefore, a general analysis was conducted. Inclusion and exclusion criteria were not defined in all studies. The randomization and allocation processes were not clearly stated in most of these studies. One of the manuscripts stated that “the authors were unable to perform a double- or single-blind study because it was impossible to mask the examiner for the materials.”41 In another study, caries arrest was not recorded if the lesion was not totally arrested.44 Overall, the determination of the arrested caries was not consistent. Results reporting based on the aims and outcomes was not clearly stated. With regard to the study design, the type of study (such as split-mouth design) and any changes due to lack of compliance (as reported in 1 study) are relevant issues to be considered. The most relevant biases found were selection (concealment of allocation sequence) and detection (failure to blind participants and personnel).
Discussion
A solution of 38% SDF has been reported as an effective treatment for caries arrest.45 SDF is usually recommended for children with a high risk of developing caries, often those living in poor conditions or developing countries.34,46 As reported previously, SDF was recently accepted in the United States as a temporary treatment to promote caries arrest; therefore, it is necessary to evaluate the current evidence about this product.29 Such information could improve the delivery of oral healthcare services for dental caries, especially in children.
Previous systematic reviews have reported that silver compounds are useful in caries management to prevent and arrest lesions in the primary and permanent dentition.27,31,47 SDF is an alternative treatment for controlling dental caries when other approaches are not available. It is a minimally invasive, low-cost, and simple method that can reduce fear and anxiety in young children. In addition, it could be applied in community settings.48,49
The selected studies in this SR used a variety of SDF concentrations, application frequencies, follow-up intervals, and outcomes. Different SDF concentrations (10%, 12%, 30%, and 38%) are available. SDF review articles have recommended the use of a 38% concentration intervention for prevention and arrest of dental caries in children.34,35,45,46,50 In the present SR, the use of SDF at concentrations of 30% and 38% was more effective for arresting caries. However, the determination of an optimal SDF application frequency was hindered due to differences in study design among the selected studies.
The main adverse events associated with SDF applications are pulpal irritation, dental staining, and oral soft tissue irritation.47 SDF has been reported as innocuous to the dental pulp.31,46 Several studies have highlighted the black dental stains that appear after SDF application as one of its disadvantages.31,35 An in vitro study demonstrated that tooth discoloration could be reduced by the incorporation of potassium iodide to SDF during application.51 On the other hand, minor oral mucosal irritation, a reversible, rare event, is not commonly reported by investigators. Few side effects were reported in the studies reviewed for the present SR. In the selected studies that used 30% and 38% SDF, adverse events such as black stains and oral lesions were reported.38,44 This finding suggests that lower SDF concentrations might reduce the onset of adverse events; however, these levels are less effective in arresting caries.
This SR has some limitations. For example, the review analyzed only manuscripts written in English; however, results of additional SDF clinical trials conducted in countries where SDF is available have been published in other languages. This filter could have introduced bias into the analysis. Moreover, an analysis of bias was not conducted, because the authors were unable to contact the primary authors of the studies and clarify issues related to the risks assessed or adverse events and side effects (publication bias). Trial reporting of the assessed studies could suggest additional biases such as selection (concealment of allocation sequence), detection (failure to blind participants and personnel), and other biases. In addition, differences between examiner criteria or stringency of the examiner limited a comparative analysis of caries arrest detection.
Trial reporting is heterogenous; therefore, the use of a standardized protocol for reporting SDF clinical trials is necessary. The Consolidated Standards of Reporting Trials (CONSORT) Statement may be useful to prevent deficiencies during result dissemination.52 In addition, a qualitative SR to determine other important factors, such as parents’ perception and children’s acceptance of treatment, should be part of the comprehensive assessment of the potential public health impact of SDF.53
None of the studies in this review compared the effectiveness of 30% versus 38% concentrations of SDF in caries arrest; such studies are necessary to help in determining an ideal (effective and safe) SDF concentration. More studies using standardized protocols for study designs, detection criteria, outcomes, and statistical designs are needed to enable a full assessment of the effectiveness of SDF in caries prevention and control, determine the appropriate application frequency, and establish treatment guidelines.
Conclusion
A systematic review of 7 studies indicated that SDF, at concentrations of 30% and 38%, is more effective than other preventive management strategies for arresting dentinal caries in the primary dentition. Additionally, 30% and 38% concentrations of SDF show potential as a caries preventive treatment in primary teeth and permanent first molars. Standardized SDF protocols must be developed to allow meaningful study comparisons and establish treatment guidelines.
Acknowledgments
The authors would like to thank Dr Lydia M. Lopez del Valle at the School of Dental Medicine, University of Puerto Rico, for her support during the study.
This study was partially supported by National Institutes of Health Award No. HCTRECD R25MD007607 and HiREC S21MD001830 from the National Institute on Minority Health and Health Disparities. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Dr. Violeta Contreras, Postdoctoral scholar, Master of Science in Clinical and Translational Research, and a research resident.
Dr. Milagros J. Toro, Assistant professor, School of Dental Medicine, Medical Sciences Campus, University of Puerto Rico, San Juan.
Dr. Augusto R. Elías-Boneta, Assistant dean of research and a professor, School of Dental Medicine, Medical Sciences Campus, University of Puerto Rico, San Juan.
Ms. Angeliz Encarnación-Burgos, Former associate director of research affairs, School of Dental Medicine, University of Puerto Rico, and is currently a doctoral student, Community and Regional Planning, School of Architecture, the University of Texas at Austin.
References
- 1.Ozdemir D. Dental caries: the most common disease worldwide and preventive strategies. Int J Biol. 2013;5(4):55. [Google Scholar]
- 2.Benjamin RM. Oral health: the silent epidemic. Public Health Rep. 2010;125(2):158–159. doi: 10.1177/003335491012500202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. [Accessed February 28, 2017];Dental Diseases and Oral Health. 2003 http://www.who.int/oral_health/publications/en/orh_fact_sheet.pdf.
- 4.American Dental Association. Statement on Early Childhood Caries. [Accessed March 30, 2017];Trans. 2000 :454. http://www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-early-childhood-caries.
- 5.Lagerweij MD, van Loveren C. Declining caries trends: are we satisfied? Curr Oral Health Rep. 2015;2(4):212–217. doi: 10.1007/s40496-015-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dye BA, Thornton-Evans G. Trends in oral health by poverty status as measured by Healthy People 2010 objectives. Public Health Rep. 2010;125(6):817–830. doi: 10.1177/003335491012500609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dye BA, Thornton-Evans G, Li X, Iafolla TJ. Dental caries and sealant prevalence in children and adolescents in the United States, 2011–2012. NCHS Data Brief. 2015;(191):1–8. [PubMed] [Google Scholar]
- 8.Sheiham A. Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J. 2006;201(10):625–626. doi: 10.1038/sj.bdj.4814259. [DOI] [PubMed] [Google Scholar]
- 9.Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Almeida AG, Roseman MM, Sheff M, Huntington N, Hughes CV. Future caries susceptibility in children with early childhood caries following treatment under general anesthesia. Pediatr Dent. 2000;22(4):302–306. [PubMed] [Google Scholar]
- 11.Jordan AR, Becker N, Jöhren HP, Zimmer S. Early childhood caries and caries experience in permanent dentition: a 15-year cohort study. Swiss Dent J. 2016;126(2):114–119. doi: 10.61872/sdj-2016-02-141. [DOI] [PubMed] [Google Scholar]
- 12.Colak H, Dülgergil CT, Dalli M, Hamidi MM. Early childhood caries update: a review of causes, diagnoses, and treatments. J Nat Sci Biol Med. 2013;4(1):29–38. doi: 10.4103/0976-9668.107257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sachdev J, Bansal K, Chopra R. Effect of comprehensive dental rehabilitation on growth parameters in pediatric patients with severe early childhood caries. Int J Clin Pediatr Dent. 2016;9(1):15–20. doi: 10.5005/jp-journals-10005-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berkowitz RJ. Causes, treatment and prevention of early childhood caries: a microbiologic perspective. J Can Dent Assoc. 2003;69(5):304–307. [PubMed] [Google Scholar]
- 15.Kawashita Y, Kitamura M, Saito T. Early childhood caries. Int J Dent. 2011;2011:725320. doi: 10.1155/2011/725320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramos-Gomez FJ, Weintraub JA, Gansky SA, Hoover CI, Featherstone JD. Bacterial, behavioral and environmental factors associated with early childhood caries. J Clin Pediatr Dent. 2002;26(2):165–173. doi: 10.17796/jcpd.26.2.t6601j3618675326. [DOI] [PubMed] [Google Scholar]
- 17.Mouradian WE, Wehr E, Crall JJ. Disparities in children’s oral health and access to dental care. JAMA. 2000;284(20):2625–2631. doi: 10.1001/jama.284.20.2625. [DOI] [PubMed] [Google Scholar]
- 18.US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Accessed February 28, 2017]. Chapter 9: provision of oral health care. Last updated March 7, 2014. http://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/chap9.htm. [Google Scholar]
- 19.Chu CH, Mei ML, Lo EC. Use of fluorides in dental caries management. Gen Dent. 2010;58(1):37–43. [PubMed] [Google Scholar]
- 20.Ramos-Gomez FJ, Crystal YO, Ng MW, Crall JJ, Featherstone JD. Pediatric dental care: prevention and management protocols based on caries risk assessment. J Calif Dent Assoc. 2010;38(10):746–761. [PMC free article] [PubMed] [Google Scholar]
- 21.Savage MF, Lee JY, Kotch JB, Vann WF., Jr Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4):e418–e423. doi: 10.1542/peds.2003-0469-F. [DOI] [PubMed] [Google Scholar]
- 22.Weintraub JA, Ramos-Gomez F, Jue B, et al. Fluoride varnish efficacy in preventing early childhood caries. J Dent Res. 2006;85(2):172–176. doi: 10.1177/154405910608500211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Dental Association Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. J Am Dent Assoc. 2006;137(8):1151–1159. doi: 10.14219/jada.archive.2006.0356. [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Pediatric Dentistry. Policy on Early Childhood Caries (ECC): classification, consequences, and preventive strategies. Pediatr Dent. 2014;37(6 Reference Manual):50–52. [PubMed] [Google Scholar]
- 25.Walsh T, Worthington HV, Glenny AM, Appelbe P, Marinho VC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010;(1):CD007868. doi: 10.1002/14651858.CD007868.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Smales RJ, Yip HK. The atraumatic restorative treatment (ART) approach for primary teeth: review of literature. Pediatr Dent. 2000;22(4):294–298. [PubMed] [Google Scholar]
- 27.Peng JJ, Botelho MG, Matinlinna JP. Silver compounds used in dentistry for caries management: a review. J Dent. 2012;40(7):531–541. doi: 10.1016/j.jdent.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 28.US Food and Drug Administration. [Accessed February 28, 2017];Diammine Silver Fluoride Dental Hypersensitivity Varnish [510(k) premarket notification] 2017 http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K102973.
- 29.American Dental Association. CDT 2017 Dental Procedures Codes. Chicago: American Dental Association Publishing; 2017. [Google Scholar]
- 30.Chu CH, Mei L, Seneviratne CJ, Lo EC. Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int J Paediatr Dent. 2012;22(1):2–10. doi: 10.1111/j.1365-263X.2011.01149.x. [DOI] [PubMed] [Google Scholar]
- 31.Chu CH, Lo EC. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent. 2008;6(4):315–321. [PubMed] [Google Scholar]
- 32.Mei ML, Ito L, Cao Y, Lo EC, Li QL, Chu CH. An ex vivo study of arrested primary teeth caries with silver diamine fluoride therapy. J Dent. 2014;42(4):395–402. doi: 10.1016/j.jdent.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Shah SG, Bhaskar V, Chawla S, et al. Efficacy of silver diamine fluoride as a topical fluoride agent compared to fluoride varnish and acidulated phosphate fluoride gel: an in vivo study. J Pediatr Dent. 2014;2(1):5–12. doi: 10.4103/0970-9290.123374. [DOI] [PubMed] [Google Scholar]
- 34.Sharma G, Puranik MP, KRS Approaches to arresting dental caries: an update. J Clin Diagn Res. 2015;9(5):ZE08–ZE11. doi: 10.7860/JCDR/2015/12774.5943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horst JA, Ellenikiotis H, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 2016;44(1):16–28. [PMC free article] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PloS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration; 2011. [Accessed February 28, 2017]. Version 5.1.0. Updated March 2011. http://handbook.cochrane.org. [Google Scholar]
- 38.Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005;84(8):721–724. doi: 10.1177/154405910508400807. [DOI] [PubMed] [Google Scholar]
- 39.Braga MM, Mendes FM, De Benedetto MS, Imparato JC. Effect of silver diammine fluoride on incipient caries lesions in erupting permanent first molars: a pilot study. J Dent Child (Chic) 2009;76(1):28–33. [PubMed] [Google Scholar]
- 40.Yee R, Holmgren C, Mulder J, Lama D, Walker D, van Palenstein Helderman W. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res. 2009;88(7):644–647. doi: 10.1177/0022034509338671. [DOI] [PubMed] [Google Scholar]
- 41.Dos Santos VE, Jr, de Vasconcelos FM, Ribeiro AG, Rosenblatt A. Paradigm shift in the effective treatment of caries in schoolchildren at risk. Int Dent J. 2012;62(1):47–51. doi: 10.1111/j.1875-595X.2011.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Monse B, Heinrich-Weltzien R, Mulder J, Holmgren C, van Palenstein Helderman WH. Caries preventive efficacy of silver diammine fluoride (SDF) and ART sealants in a school-based daily fluoride toothbrushing program in the Philippines. BMC Oral Health. 2012;12:52. doi: 10.1186/1472-6831-12-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhi QH, Lo EC, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012;40(11):962–967. doi: 10.1016/j.jdent.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 44.Duangthip D, Chu CH, Lo EC. A randomized clinical trial on arresting dentine caries in preschool children by topical fluorides—18 month results. J Dent. 2016;44:57–63. doi: 10.1016/j.jdent.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 45.Gao SS, Zhao S, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Translat Res. 2016;1(3):201–210. doi: 10.1177/2380084416661474. [DOI] [PubMed] [Google Scholar]
- 46.Shah S, Bhaskar V, Venkatraghavan K, Choudhary P, Ganesh M, Trivedi K. Silver diamine fluoride: a review and current applications. J Adv Oral Res. 2014;5(1):25–35. [Google Scholar]
- 47.Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res. 2009;88(2):116–125. doi: 10.1177/0022034508329406. [DOI] [PubMed] [Google Scholar]
- 48.Chu CH, Lo EC. Dental caries prevention and treatment for preschool children in China. Chinese J Dent Res. 2007;10(Suppl):56–62. [Google Scholar]
- 49.Lo EC, Chu CH, Lin HC. A community-based caries control program for pre-school children using topical fluorides: 18-month results. J Dent Res. 2001;80(12):2071–2074. doi: 10.1177/00220345010800120901. [DOI] [PubMed] [Google Scholar]
- 50.Fung MHT, Wong MCM, Lo EC, Chu CH. Arresting early childhood caries with silver diamine fluoride-a literature review. J Oral Hyg Health. 2013;1(3):117. [Google Scholar]
- 51.Knight GM, McIntyre JM, Craig GG, Zilm PS, Gully NJ. An in vitro model to measure the effect of a silver fluoride and potassium iodide treatment on the permeability of demineralized dentine to Streptococcus mutans. Aust Dent J. 2005;50(4):242–245. doi: 10.1111/j.1834-7819.2005.tb00367.x. [DOI] [PubMed] [Google Scholar]
- 52.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2012;10(1):28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 53.Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention—WHO recommendations for improved evidence in public health practice. Community Dent Health. 2004;21(4 Suppl):319–329. [PubMed] [Google Scholar]


