Abstract
Objective
To evaluate the effects of heparin saline versus normal saline as locking solution for maintaining patency in peripheral venous catheters in Chinese patients.
Methods
This open-label, randomized controlled study was conducted in two hepatobiliary surgery wards, where patients received identical treatments, at a tertiary referral hospital. Patients were randomly divided into a normal saline group (NS, 3 ml) or a heparin saline group (HS, 50 IU/ml, 3 ml) for catheter sealing.
Results
The study enrolled 286 patients and 609 peripheral venous catheters were included in the analysis. The patients in the two groups had no local infections or catheter-related bloodstream infections. There were no significant differences between the two groups in terms of the rate of catheter obstruction, duration time, or the rates of phlebitis, infiltration, and accidental catheter removal.
Conclusions
No significant differences in the peripheral venous catheter sealing effects were observed between normal saline and heparin saline usage in Chinese patients.
Keywords: Heparin, peripheral venous catheter, catheter flushing, heparinized saline
Introduction
Peripheral venous catheters (PVCs) can be retained for a period of 72–96 hours to minimize the number of venipunctures. Thus, PVCs are widely used in various medical facilities for clinical interventions such as drug infusion, nutrition and blood product administration.1 Approximately 80% of patients in the USA have received intravenous administration via PVCs.2 In 2009, a survey was conducted in 47 hospitals in Beijing, China, and found that 95.7% of these hospitals used PVCs as venipuncture tools.3
For intermittent infusion, PVC flushing and sealing are required to maintain the patency of the PVCs. To date, heparin saline (HS) and normal saline (NS) solutions have been mainly used in catheter sealing for clinical applications. Heparin is an anticoagulant. Therefore, HS can be used to prevent thrombosis and maintain the patency of the catheter for intermittent infusion.4 However, adverse reactions caused by heparin can be significant, including allergic reactions,5 bleeding4 and heparin-induced thrombocytopenia,6 the latter of which has an incidence of 0.5%.7 Another disadvantage of using HS for catheter sealing is the possibility of administering the wrong dosage of HS.8 Compared with HS, NS is convenient and comparatively inexpensive.9
To date, results of studies that addressed the catheter sealing effects of NS and HS have remained controversial. In 1991, a meta-analysis was conducted to evaluate the effects of HS and NS in maintaining catheter patency, the incidence of phlebitis and catheter retention time.10 No significant differences were detected in the incidence of catheter blocking, phlebitis and catheter retention time.10 Research subjects in the meta-analysis were from the Departments of Medicine and Surgery and from the Intensive Care Unit.10 Based on this evidence, in 2011, the Infusion Nurses Society (INS) recommended the application of NS for flushing and sealing of catheters used in adult patients.11
Several studies that have been published in this field have reported inconsistent findings. One examination included 73 pregnant women and compared the catheter sealing effects of HS (10 IU/ml) and NS.12 No significant differences between the two groups were detected in maintaining catheter patency and the incidence of phlebitis.12 In contrast, in 2012, a non-blind randomized controlled trial that included 214 research subjects was conducted in a teaching hospital in Italy.13 Regardless of the numbers of patients or the number of catheters, the data analysis produced the findings, indicating that the utilization of HS as a catheter sealing solution resulted in catheter patency that was better than that obtained after the use of NS.13 The benefits included the reduction in both the total and individual incidence of phlebitis and catheter obstruction.13
The American Association of Critical Care Nurses conducted an international survey on catheter sealing solutions in randomized samples (n = 1072).14 Among the institutions surveyed, they reported that 77% of these institutions used HS for catheter sealing compared with 18% of institutions that used NS.14 In the remaining 5%, other diluents or solutions were employed for catheter sealing.14 A survey revealed that in the study hospital, 88.7% of patients received heparinized saline as a flush fluid, whereas 11.3% received normal saline.15
Although INS guidelines recommend using NS for catheter sealing,11 in China, there is a lack of guidelines or consensus on whether HS or NS is the optimal option as a flushing and locking solution. However, HS has been widely and commonly employed as a catheter flushing and sealing solution by Chinese nurses.16 Therefore, it is necessary to assess the effects of NS and HS used for catheter sealing in Chinese patients.
This current study aimed to evaluate and compare the effects of NS and HS in PVC sealing in Chinese patients, provide evidence for clinical nurses that facilitate the proper choice of catheter sealing solutions, and achieve safe and effective patient care.
Patients and methods
Study design and setting
This was an open-label randomized controlled trial (RCT) performed at a tertiary referral hospital, Zhongshan Hospital Affiliated to Xiamen University, Xiamen, China, Fujian Province, between 3 March 2014 and 30 April 2014. This research hospital contains a total of 2000 beds and 38 clinical departments.
Study population
Patients from two hepatobiliary surgery wards, who had pairwise identical treatments and diseases, were included in this study. Patient inclusion criteria were as follows: (i) patients ≥18 years old; (ii) PVCs expect to be retained for more than 24 h. Exclusion criteria were as follows: (i) continuous infusion required without catheter sealing; (ii) presence of haematological diseases; (iii) peripheral parenteral nutrition required; (iv) administration of anticoagulant therapy; (v) existence of serious infections.
This study’s research proposal was approved by the Ethical Committee of Fudan University (Shanghai, China), Zhongshan Hospital Affiliated to Xiamen University (Xiamen, China) and the Centre of Chinese Clinical Trial Registry (ChiCTR-IOR-15007104; http://www.chictr.org.cn/index.aspx). All study participants were informed of the details of the investigation, the objective, and the possible outcomes before they were asked to sign a written informed consent prior to participation into the study.
Randomization
Eligible patients were randomly assigned to either the normal saline group (NS, experimental group) or a matching heparin saline group (HS, control group) for catheter sealing using the random number table method. The table of random numbers was generated using the Excel® random number macro. Patients were sequentially enrolled into the groups based on the order of the random number tables.
Materials used during intravenous catheterization
Venipuncture zones were disinfected using anerdian (Shanghai Likang Hi Tech, Shanghai, China) before performing the venipuncture. All catheters were purchased from Becton, Dickinson and Company (Suzhou, China). The closed intravenous catheters were made of polyurethane (gauge: 18–24). 3 M™ transparent dressings were used (3 M, Brookings, SD, USA). Heparin sodium in glass bottles (2 ml/12 500 IU) were purchased from Nanjing Xinbai Pharmaceutical (Nanjing, China). NS in plastic bags (0.9%; 250 ml/bag) were purchased from Cisen Pharmaceutical (Shandong, China). HS dilutions were formulated as follows: 2 ml of heparin sodium (2 ml/12 500 IU) was withdrawn from the bottle using a 5-ml syringe and diluted in 250 ml of NS. The HS solution (50 IU/ml) was placed in a sterile tray and replaced every 4 h. NS solutions were stored and replaced at the same time after opening, similar to that for HS. Before locking catheters, 3 ml flushing solution was extracted from the HS solution or NS solutions.
Catheter flushing techniques
Catheter flushing and sealing techniques complied with INS guidelines as follows.11 After each drug administration, a pulse flushing technique was used to irrigate the catheters (by alternatively flushing and pausing in flushing with locking solution to create a small vortex within the catheter), followed by administering positive pressure to seal the tube (by flushing the locking solution while simultaneously withdrawing the needle to remove the syringe needle). Volumes of 3 ml of 0.9% NS solution in the NS group and 3 ml of 50 IU/ml of HS solution in the HS group were used to seal the catheters using 5-ml syringes.
Outcome measurements
The rate of catheter obstruction was regarded as the primary outcome in the investigation. Catheter obstruction was defined as the inability of the catheter to flush (not able to intravenously inject 1 ml of NS within 30 s).13
Secondary outcome measures were as follows: (i) duration time (h), starting with catheterization and continuing through catheter application that required catheter sealing until the removal of the catheter, the requirement for continuous infusion, or death of the patient; (ii) phlebitis, defined as the emergence of two or more symptoms at the puncture site including erythema, swelling, pain, or tenderness, or palpable venous cord beyond the puncture site;17 (iii) infiltration, defined as the infusion of non-blistering drug leaking through the normal vascular channel and resulting in the swelling of tissue peripheral to the puncture site;12 (iv) local venous infection, defined as microorganisms grown from purulent discharge at the puncture site;18 (v) catheter-related bloodstream infection, defined as positive blood culture from a peripheral vein, clinical signs of infection (i.e. fever, chills, or hypotension), with no other apparent source for the bloodstream infection except for the intravenous catheter (in situ within 48 h of the bloodstream infection), and a colonized intravenous catheter tip culture with the same organism as that identified in the blood;18 (vi) accidental catheter removal; and (vii) patency time (h), defined as the time from catheterization to the occurrence of an occlusion.
Data collection
Records designed by the research team were used for data collection and comparison between the sealing effects of NS and HS. Data included basic patient information (e.g. age, sex, presence or absence of complications, vascular quality, PVC specification, puncture site, infused liquid/drug delivery), duration time and the incidence of complications.
Two weeks before the study, all nurses in the research wards were trained to perform operations, including the insertion of indwelling catheters, catheter flushing, catheter sealing according to INS guidelines,11 and to evaluate the complications. In addition, nurses were trained to collect data. The skills of all nurses who performed the PVC puncture and catheter maintenance, and evaluated the complications were assessed. Nurses in the two wards were qualified for PVC puncture and maintenance.
An undergraduate nursing student was recruited at the end of their internship as a research assistant in each ward to confirm the integrity of the data collection. These students were not involved in PVC catheterization and extubation. Clinical nurses in the research wards recorded the basic patient information and PVC condition after the puncture, and the presence or absence of complications were also recorded in a timely manner for making decisions regarding extubation or PVC replacement. After extubation or PVC replacement, duration time, reason for extubation and condition of the complication were recorded for each patient. During their stay in the hospital, patients were monitored after the first indwelling puncture until PVC extubation or replacement. Further catheterization(s) (no more than five times altogether) were also investigated in this study.
In order to ensure the quality of the study data and maximize the validity and reliability of the conclusions drawn, clinical nurses were instructed to ask nurses specialized in intravenous therapy to help in the assessment of the complication and decide on the necessity of extubation, if they were not certain regarding the signs of phlebitis and catheter obstruction. This double assessment reduced the potential bias in the study. The researchers periodically visited and communicated with the research assistants and the clinical nurses to help resolve any problem during the period of the investigation.
Statistical analyses
Assuming a value of two-sided type I error of 0.05, a randomization ratio of 1:1 was achieved between the experimental NS group and control HS group using the random number table method. Based on data for the entire study population, each patient had a median of two PVCs. The sample size was calculated to detect significant differences in the incidence of catheter obstruction between the compared groups, with a power of 80% to detect a difference of 10% based on the 15% incidence rate in the control HS group19 and a withdrawal rate of 10%, accounting for 140 cases and 280 PVCs in each group.
All statistical analyses were performed using the SPSS® statistical package, version 18.0 (SPSS Inc., Chicago, IL, USA) for Windows®. Measurement data are presented as mean ± SD for data descriptions, frequency measurements and proportion descriptions. Student’s t-test and Kruskal–Wallis test were used for continuous variables, and χ2-test for categorical variables. Kaplan–Meier survival analysis and log rank test were used to compare differences in patency time between the two groups. A P-value ≤ 0.05 was considered statistically significant.
Results
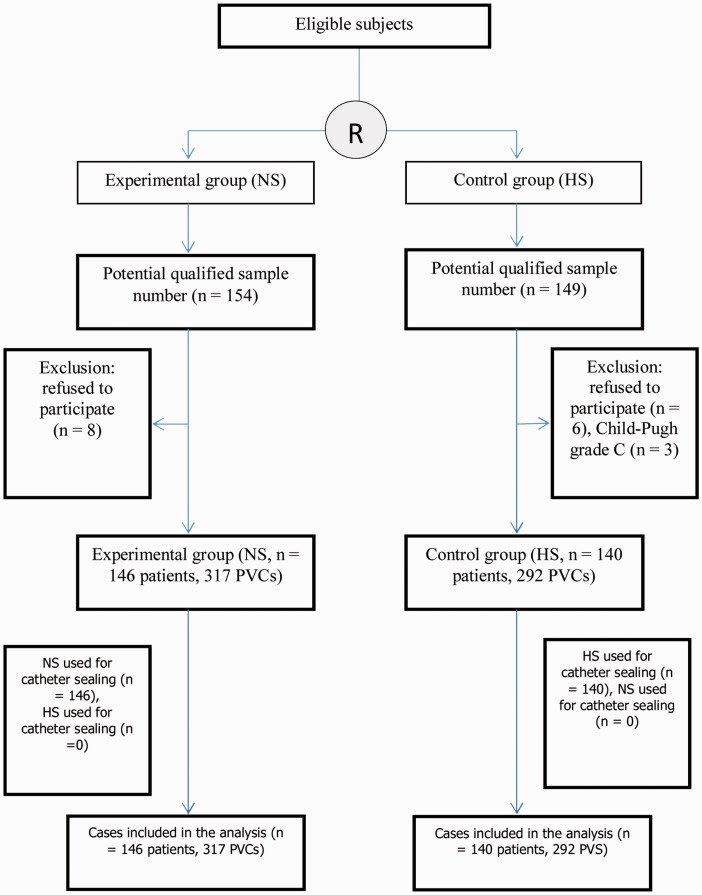
A total of 303 patients met the inclusion criteria, of which 289 patients agreed to participate in the study. Of these, three patients were excluded due to severe illness (Child-Pugh grade C); thus, only 286 patients were involved in the data analysis (146 patients [a total of 317 PVCs] who received NS for catheter sealing and 140 patients [a total of 292 PVCs] who received HS for catheter sealing) (Figure 1). None of the patients dropped out during the study. Each patient had a median of 2.13 PVCs. Table 1 summarizes the baseline clinical and demographic characteristics of the patients in the two groups. There were no significant differences between the two groups.
Figure 1.
Flow chart showing the patient numbers at various stages of this prospective, open-label randomized controlled trial that aimed to evaluate and compare the effects of normal saline (NS) and heparin saline (HS) in peripheral venous catheter (PVC) sealing in Chinese patients. R, randomization.
Table 1.
Baseline clinical and demographic characteristics of two groups of Chinese patients who were randomized to receive either normal saline (NS) and heparin saline (HS) in peripheral venous catheter (PVC) sealing.
| NS group n = 146 | HS group n = 140 | |
|---|---|---|
| Age, years | 55.69 ± 19.51 | 52.38 ± 18.99 |
| Sex | ||
| Male | 82 (56.16%) | 76 (54.29%) |
| Female | 64 (43.84%) | 64 (45.71%) |
| Number of PVCs | 317 | 292 |
| Complications | ||
| No | 80 (54.79%) | 76 (54.29%) |
| 1 type | 45 (30.82%) | 44 (31.43%) |
| ≥2 types | 21 (14.38%) | 20 (14.29%) |
| Wound infection | ||
| No | 144 (98.63%) | 139 (99.29%) |
| Yes | 2 (1.37%) | 1 (0.71%) |
| Catheter specifications | ||
| ≤20 G | 7 (2.21%) | 11 (3.77%) |
| 22G | 67 (21.14%) | 66 (22.60%) |
| 24G | 243 (76.66%) | 215 (73.63%) |
| Left/right hand | ||
| Left hand | 171 (53.94%) | 153 (52.40%) |
| Right hand | 146 (46.06%) | 139 (47.60%) |
| Puncture site | ||
| Opisthenar | 170 (53.63%) | 163 (55.82%) |
| Inner forearm | 45 (14.20%) | 39 (13.36%) |
| Forearm | 82 (25.87%) | 75 (25.68%) |
| Wrist | 17 (5.36%) | 13 (4.45%) |
| Cubital fossa | 3 (0.95%) | 2 (0.68%) |
| Vascular quality | ||
| Good | 41 (28.08%) | 31 (22.14%) |
| Moderate | 73 (50.00%) | 85 (60.71%) |
| Poor | 32 (21.92%) | 24 (17.14%) |
| Drug delivery | ||
| Potassium chloride | 83 (26.18%) | 86 (29.45%) |
| Anti-inflammatory drugs | 48 (15.14%) | 37 (12.67%) |
| Vasoactive drugs | 50 (15.77%) | 44 (15.07%) |
| Hypertonic drugs | 13 (4.10%) | 16 (5.48%) |
| Others | 171 (53.94%) | 153 (52.40%) |
Data presented as mean ± SD, n of patients (%) or n of PVCs (%).
No significant between-group differences (P > 0.05); Student’s t-test for continuous variables and χ2-test for categorical variables.
There was no significant difference between the two groups in terms of the primary outcome of the rate of catheter obstruction; 18.61% (59/317) for the NS group compared with and 15.07% (44/292) for the HS group (Table 2). Patients in the two groups had no local infections or catheter-related bloodstream infections. There were no significant differences in the median duration time and rates of phlebitis, infiltration and accidental catheter removal between the two groups. No serious adverse events occurred during the observations undertaken in this study.
Table 2.
Comparison of clinical outcomes of two groups of Chinese patients who were randomized to receive either normal saline (NS) and heparin saline (HS) in peripheral venous catheter (PVC) sealing.
| NS group n = 317 PVCs | HS group n = 292 PVCs | |
|---|---|---|
| Primary outcome measure | ||
| Catheter obstruction | 59 (18.61%) | 44 (15.07%) |
| Secondary outcome measures | ||
| Median duration time, h | 72 (24–216) | 72 (24–216) |
| Phlebitis | 37 (11.67%) | 43 (14.73%) |
| Infiltration | 94 (29.65%) | 80 (27.40%) |
| Accidental removal | 8 (2.52%) | 3 (1.03%) |
Data presented as n of PVCs (%) or median (min–max).
No significant between-group differences (P > 0.05); Kruskal–Wallis test for continuous variables and χ2-test for categorical variables.
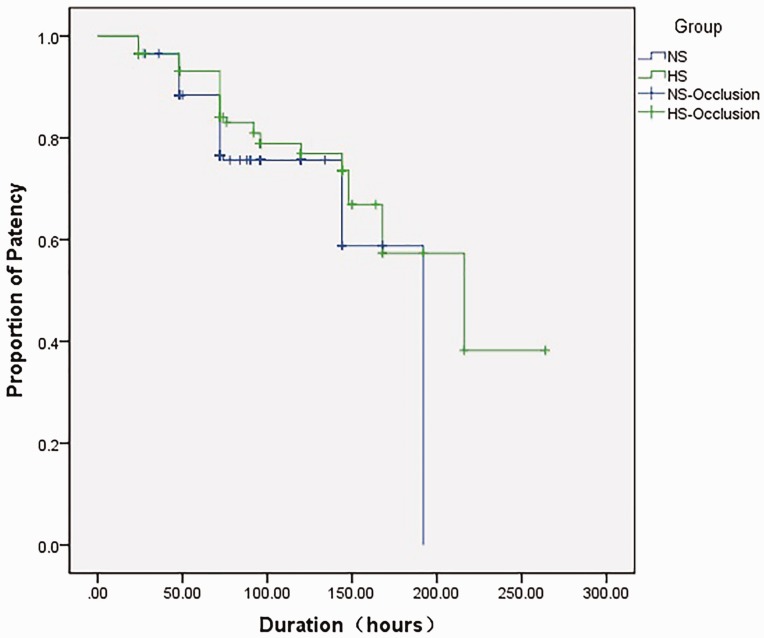
Kaplan–Meier survival analysis was used to compare the difference in patency time between the two groups. There was no significant difference in the patency time observed between the two groups (Figure 2).
Figure 2.
Kaplan–Meier survival analysis of patency times compared between the two groups of Chinese patients who were randomized to receive either normal saline (NS) and heparin saline (HS) in peripheral venous catheter sealing. Patency time was defined as the time from catheterization to the occurrence of an occlusion. X2 = 2.95, P = 0.086. The colour version of this figure is available at: http://imr.sagepub.com.
Discussion
This present open-label RCT demonstrated that there were no significant differences between the catheter sealing effects of NS and HS in a population of Chinese patients. The use of NS as a catheter locking solution did not increase catheter obstruction and did not increase the incidence of other complications. According to the above results, HS has no significant advantage, but it carries certain risk factors such as thrombocytopenia,6 haemorrhage4 and dosage errors caused by the HS dilution procedure.8 Thus, in order to avoid the adverse reactions of HS, this study supports using NS for catheter sealing. Performing NS catheter sealing is simple and convenient. It does not require solvent dilution, which facilitates the avoidance of dilution-related contamination during the procedure.
Although INS guidelines recommend the use of NS for catheter sealing,11 there are no guidelines or consensus for regulating the use HS or NS as a locking solution in China. The results of the present RCT indicate that the effects of NS used for catheter sealing are similar to those of HS, which is consistent with the recommendations of the INS guidelines.11
The results of this study reach the same conclusions as previous reports.12,16 The median catheter duration time was 72 hours in both groups, with no statistically significant difference between the two groups. Moreover, there was a lower incidence of phlebitis in the NS group (37/317; 11.67%) compared with the HS group (43/292; 14.73%), but the difference was not statistically significant. For other complications, the NS group had a higher incidence of obstruction, infiltration, and accidental catheter removal compared with the HS group, but none of the differences were statistically significant. The usefulness of using HS as a catheter sealing solution has been questioned since the 1980s.20,21 A study in 1992 demonstrated that there was no significant difference between the catheter sealing effect in surgical inpatients receiving HS and NS, while NS decreased the stimulation of blood vessels and reduced the incidence of phlebitis.22 Furthermore, two RCTs were conducted in 201123 and 200724; and both reported that paediatric patients who received HS did not experience any significant catheter sealing benefit compared with paediatric patients who received NS.
This present study did not provide any evidence of significantly better catheter sealing effects and safety of HS compared with those of NS. However, many domestic studies in China have supported the use of HS as a catheter sealing solution.25–27 In 2011, a meta-analysis performed in China evaluated the catheter sealing effects of NS and HS for peripheral venous catheterization.28 The study included nine RCTs and a total of 1770 patients.28 The results indicated that HS, as a catheter sealing solution, had a better effect in reducing the rate of intravenous catheter obstruction than NS.28 Used as a catheter sealing solution in paediatric patients, HS extended catheter retention time compared with NS.28 However, no significant difference in phlebitis prevention was noted between these two catheter sealing solutions.28 Nevertheless, the studies included in the Chinese meta-analysis did not specify the randomization methods and processes used; and they did not detail the reasons for sample loss.28 Therefore, it is not possible to completely rule out that the randomization processes used in the nine RCTs may have had an impact on the study outcomes.
This present RCT had several limitations. First, it did not monitor prothrombin time, because a previous study demonstrated that there was no significant difference in prothrombin time between NS and HS groups.29 Future investigations that include the monitoring of prothrombin time would be necessary. Secondly, the present RCT employed an open-label design to reduce study costs. Thirdly, selection bias was difficult to completely exclude in this open-label study.
In conclusion, no significant differences in reducing the incidence of catheter obstruction and the other complications (e.g. phlebitis) between patients receiving NS and HS for catheter sealing were observed in this open-label RCT. As a result of these findings, NS is recommended as a sealing solution for PVCs, because it is safe, effective and easy to use. Moreover, NS is inexpensive and requires no configuration or a dilution step, as compared with HS; minimizing the workload of clinical nurses, the risk of contamination and the chances for error in dose configuration.
Acknowledgements
We would like to thank the head nurses and all clinical nurses in the two wards for their support. We would also like to thank two undergraduate nursing students of Fujian Medical University, Jiani Chen and Yanhuang Su, for their great efforts in data collection.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This study was a key programme funded by the Nursing Research Foundation of Fudan University, 2012 (no: FNF201201).
References
- 1.McCallum L, Higgins D. Care of peripheral venous cannula sites. Nurs Times 2012; 108: 12, 14–15. [PubMed] [Google Scholar]
- 2.Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents 2009; 34(Suppl 4): S38–S42. [DOI] [PubMed] [Google Scholar]
- 3.Li CY, Jing H, Li L. A survey of the status of infusion therapy in Beijing. Chinese Journal of Nursing 2009; 44: 607–609. [in Chinese]. [Google Scholar]
- 4.Malloy MH, Cutter GR. The association of heparin exposure with intraventricular hemorrhage among very low birth weight infants. J Perinatol 1995; 15: 185–191. [PubMed] [Google Scholar]
- 5.Schindewolf M, Lindhoff-Last E, Ludwig RJ, et al. Heparin-induced skin lesions. Lancet 2012; 380: 1867–1879. [DOI] [PubMed] [Google Scholar]
- 6.Miller PL. Heparin-induced thrombocytopenia–recognition and treatment. AORN J 2003; 78: 79–86,89. [DOI] [PubMed] [Google Scholar]
- 7.Rice L, Nguyen PH, Vann AR. Preventing complications in heparin-induced thrombocytopenia. Alternative anticoagulants are improving patient outcomes. Postgrad Med 2002; 112: 85–89. [DOI] [PubMed] [Google Scholar]
- 8.Otoya M. Heparin safety in the neonatal intensive care unit: are we learning from mistakes of others? Newborn Infant Nurs Rev 2009; 9: 53–61. [Google Scholar]
- 9.Shu DJ, Min Z. Comparison of the effect of obstruction between two kinds of locking solution for PICC. International Journal of Nursing 2010; 8: 1256–1258. [in Chinese]. [Google Scholar]
- 10.Goode CJ, Titler M, Rakel B, et al. A meta-analysis of effects of heparin flush and saline flush: quality and cost implications. Nurs Res 1991; 40: 324–330. [PubMed] [Google Scholar]
- 11.Infusion Nursing Society. Infusion Nursing Standards of Practice. J Infus Nurs 2011; 34: S1–S34. Available at: http://engage.ahima.org/HigherLogic/System/DownloadDocumentFile.ashx?DocumentFileKey=2238ee0a-c2df-4d1a-affa-f69f2ce41856. [Google Scholar]
- 12.Niesen KM, Harris DY, Parkin LS, et al. The effects of heparin versus normal saline for maintenance of peripheral intravenous locks in pregnant women. J Obstet Gynecol Neonatal Nurs 2003; 32: 503–508. [DOI] [PubMed] [Google Scholar]
- 13.Bertolino G, Pitassi A, Tinelli C, et al. Intermittent flushing with heparin versus saline for maintenance of peripheral intravenous catheters in a medical department: a pragmatic cluster-randomized controlled study. Worldviews Evid Based Nurs 2012; 9: 221–226. [DOI] [PubMed] [Google Scholar]
- 14.Goode CJ, Titler M, Rakel B, et al. A meta-analysis of effects of heparin flush and saline flush: quality and cost implications. Nurs Res 1991; 40: 324–330. [PubMed] [Google Scholar]
- 15.Thamlikitkul V, Indranoi A. Switching from heparinized saline flush to normal saline flush for maintaining peripheral venous catheter patency. Int J Qual Health Care 2006; 18: 183–185. [DOI] [PubMed] [Google Scholar]
- 16.Wang R, Luo O, He L, et al. Preservative-free 0.9% sodium chloride for flushing and locking peripheral intravenous access device: a prospective controlled trial. J Evid Based Med 2012; 5: 205–208. [DOI] [PubMed] [Google Scholar]
- 17.Rickard CM, McCann D, Munnings J, et al. Routine resite of peripheral intravenous devices every 3 days did not reduce complications compared with clinically indicated resite: a randomised controlled trial. BMC Med 2010; 8: 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 2011; 52: e162–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bao ZW, Zu YL, Sha SW. Effect of the two different solution used to seal up the tube of intravenous indwelling needle in old patients. Jilin Medication 2010; 30: 3146–3147. [in Chinese]. [Google Scholar]
- 20.Epperson EL. Efficacy of 0.9% sodium chloride injection with and without heparin for maintaining indwelling intermittent injection sites. Clin Pharm 1984; 3: 626–629. [PubMed] [Google Scholar]
- 21.Hamilton RA, Plis JM, Clay C, et al. Heparin sodium versus 0.9% sodium chloride injection for maintaining patency of indwelling intermittent infusion devices. Clin Pharm 1988; 7: 439–443. [PubMed] [Google Scholar]
- 22.Shoaf J, Oliver S. Efficacy of normal saline injection with and without heparin for maintaining intermittent intravenous site. Appl Nurs Res 1992; 5: 9–12. [DOI] [PubMed] [Google Scholar]
- 23.Arnts IJ, Heijnen JA, Wilbers HT, et al. Effectiveness of heparin solution versus normal saline in maintaining patency of intravenous locks in neonates: a double blind randomized controlled study. J Adv Nurs 2011; 67: 2677–2685. [DOI] [PubMed] [Google Scholar]
- 24.Mok E, Kwong TK, Chan MF. A randomized controlled trial for maintaining peripheral intravenous lock in children. Int J Nurs Pract 2007; 13: 33–45. [DOI] [PubMed] [Google Scholar]
- 25.Zhu YM. Observation of the effect of two kinds of sealing fluid on sealing venous indwelling needle in perioperative patients. Journal of Aerospace Medicine 2015; 26: 785–786. [in Chinese]. [Google Scholar]
- 26.Chen LJ. Comparison of two kinds of sealing liquid on venous indwelling needle in patients with pneumocardial disease. Jilin Medication 2008; 29: 795–796. [in Chinese]. [Google Scholar]
- 27.Yang GY. Study on the effect of the different liquids of a vein detains the needle. Chinese Primary Health Care 2007; 121: 82–83. [in Chinese]. [Google Scholar]
- 28.Xin TW, Zhi ML, Yue HZ. Effects of venous remaining needle sealing with heparin vs. Saline in China: a meta-analysis. Chin J Evid-based Med 2011; 11: 96–100. [in Chinese]. [Google Scholar]
- 29.Meyer BA, Little CJ, Thorp JA, et al. Heparin versus normal saline as a peripheral line flush in maintenance of intermittent intravenous lines in obstetric patients. Obstet Gynecol 1995; 85: 433–436. [DOI] [PubMed] [Google Scholar]