Abstract
Study design: Longitudinal design.
Objectives: The study determined the effects of two forms of exercise training on the abundance of two proteins, (glucose transporter-4 [GLUT-4], adenosine monophosphate kinase [AMPK]) involved in glucose utilization and the transcriptional coactivator that regulates the genes involved in energy metabolism and mitochondrial biogenesis (peroxisome proliferator-activated receptor (PPAR) coactivator 1 alpha [PGC-1α]), in muscles in men with chronic motor-complete spinal cord injury (SCI).
Settings: Clinical trial at a Medical Center.
Methods: Nine men with chronic motor-complete SCI participated in functional electrical stimulation lower extremity cycling (FES-LEC; n = 4) or arm cycling ergometer (arm-cycling ergometer [ACE]; n = 5) 5 days/week for 16 weeks. Whole body composition was measured by dual energy X-ray absorptiometry. An intravenous glucose tolerance test was performed to measure glucose effectiveness (Sg) and insulin sensitivity (Si). Muscle biopsies of the right vastus lateralis (VL) and triceps muscles were collected one week prior to and post the exercise training intervention.
Results: Neither training intervention altered body composition or carbohydrate metabolism. GLUT-4 increased by 3.8 fold in the VL after FES training and increased 0.6 fold in the triceps after ACE training. PGC-1α increased by 2.3 fold in the VL after FES training and 3.8 fold in the triceps after ACE training. AMPK increased by 3.4 fold in the VL after FES training and in the triceps after ACE training.
Conclusion: FES-LEC and ACE training were associated with greater protein expressions in the trained muscles by effectively influencing the abundance of GLUT-4, AMPK and PGC-1α. Thus, FES-LEC training of paralyzed muscle can modulate protein expression similar to that of trained and innervated muscle.
Keywords: FES-LEC, ACE, Body composition, IVGTT, GLUT-4, PGC-1α, AMPK, Spinal cord injury
The American Diabetes Association reports that 27.6 million Americans have type 2 diabetes mellitus (DM) in 2012, which represents approximately 9% of the nation's population.1 Persons with spinal cord injury (SCI) are at heightened risk of developing type 2 DM.2–4 An early study noted that 40% of individuals with SCI had glucose intolerance and elevated insulin levels.2 When formal oral glucose tolerance testing was performed, Bauman and Spungen reported that 22% in a cohort with SCI were diabetic compared to 6% of the control group.3 Lavela et al. noted a step rise increase with aging in the prevalence of type 2 DM in Veterans with SCI compared to the general population.4
Skeletal muscle oxidative capacity is greatly impaired due to disuse atrophy associated with slow-to-fast fiber type transformation.5–8 These factors may further predispose those with SCI to impair glucose disposal, cardio-metabolic dysregulation and other disease risks.9–11,13–15 Enhancement of glucose disposal pathways may require special understanding of the different metabolic pathways involved in improvement of insulin sensitivity after SCI.9,16,17
Perturbations of intracellular metabolic pathways may have a role in decreased glucose disposal following SCI.18,19 Exercise interventions may correct these abnormalities and trigger the release of Ca++, which stimulates translocation of glucose transporter-4 (GLUT-4) following functional electrical stimulation-lower extremity cycling (FES-LEC) training in persons with SCI.20–23 Exercise may also improve glucose uptake through independently increasing the activity of 5-adenosine monophosphate kinase (AMPK).24 Upregulation of AMPK has been shown to be linked to exercise-induced expression of peroxisome proliferator-activated receptor (PPAR) coactivator 1 alpha (PGC-1 α),24–26 a transcriptional co-activator that is involved in mitochondrial biogenesis and the oxidative profile of skeletal muscle.26 Dysfunction in mitochondrial biogenesis has been associated with decreased expression of PGC-1α and results in decreased B- oxidation and insulin resistance.
Newly released guidelines have recommended exercise interventions as an important countermeasure for several of the chronic disorders observed after SCI.27–29 Both volitional and assisted exercise training modalities are recommended in SCI with arm-cycling ergometry prescribed for non-paralyzed muscles and FES-LEC for the paralyzed muscles. Both interventions improve parameters related to glucose tolerance and insulin sensitivity.30,31 However, it is unclear whether exercise training interventions using paralyzed or non-paralyzed muscles target similar molecular responses related to glucose disposal and oxidative phosphorylation.
Moreover, a direct comparison of the effects of ACE and FES-LEC on responses of skeletal muscle has not been performed. As such, in persons with SCI the effects of ACE compared to FES-LEC were investigated for changes to three vital skeletal muscle proteins which are known to be altered by exercise and involved in energy metabolism (GLUT-4, AMPK, and PGC-1) and that are likely to be involved in glucose disposal, energy regulation and mitochondrial biogenesis following exercise training. The primary hypothesis was that FES-LEC will yield similar changes in the abundance of these regulatory proteins to that of ACE. The rationale stemmed from previous work that showed that paralyzed skeletal muscle following SCI muscle remains both sensitive and responsive years after injury.20–22
Methods
Nine men with motor complete SCI (C5–T10; 38 ± 9 years old, 84 ± 14 kg, 1.8 ± 0.07 m and 25.7 ± 4.3 kg/m2) were enrolled. Participants were randomly assigned to either ACE (n = 5) or FES (n = 4). Each participant had two overnight stays: pre-training (baseline) and 16 weeks post-training (post-exercise) to perform body composition assessment, intravenous glucose tolerance test (IVGTT) and muscle biopsies. Muscles biopsies were performed for both the right vastus lateralis and right triceps muscles.
The study was conducted at the McGuire VA Medical Center in collaboration with the Clinical Research Unit at Virginia Commonwealth University (VCU) Medical Center. All participants were asked to read and sign consent forms that were approved by the local ethics committee at McGuire VA Medical Center and Virginia Commonwealth University. All study procedures were conducted according to the Declaration of Helsinki. Participants were recruited by word of mouth, posted flyers or from the associated SCI clinics at the participating institutions.
Inclusion and exclusion criteria
Participants were included if they were between the ages of 18 and 65, had a visible tetanic contraction of the knee extensor muscle group in response to electrical stimulation and had motor complete SCI (C5–L2; AIS A & B). Participants who were injured for less than one year were excluded to ensure that any changes in body composition as a result of acute injury will have been completed.9,32 Participants with motor complete SCI were studied to exclude the inevitable variability of body composition changes that would have been found in individuals with motor incomplete SCI. Participants with pre-existing medical conditions (uncontrolled hypertension, uncontrolled hyperglycemia or a hemoglobin A1C level >7.0%, chronic arterial diseases, recent deep vein thrombosis, uncontrolled autonomic dysreflexia, severe spasticity, fractures, or history of fractures, pressure ulcers greater than Grade II, documented osteoporosis, untreated thyroid disease, or renal disease) were excluded from study participation.9,32–35
Measurements for both groups (n = 9)
All participants underwent a complete physical examination, including a neurological assessment and International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) examination followed by a resting electrocardiogram (EKG). The participant was then transferred to the Clinical Research Center located at Virginia Commonwealth University for an overnight stay. After a 10–12 hour overnight fast, percutaneous muscle biopsies of the right Vastus lateralis and Triceps groups were performed (see below).
Body mass and height. Each participant was asked to void his bladder and then to propel himself onto a wheelchair weighing scale (PW-630U; Tanita)a with total body weight determined by subtracting the weight of the wheelchair. After properly aligning the head, trunk and the legs, the height of each participant was determined along left side with the participant in the supine position.9,32–35 Two smooth wooden boards were placed at the participant's head and heels and the distance between them corresponded to the height in nearest cm. Every effort was taken to maintain the knees in an extended position. The BMI (kg/m2) was then calculated as the weight divided by the height squared.
Graded exercise test. Maximal graded exercise testing using a Lode arm crank ergometer (Groningen, The Netherlands) was performed before and after the sixteen weeks of exercise, as described previously.32,33 A TrueMax 2400 computerized metabolic measurement system (ParvoMedics, Salt Lake, UT, USA) was used to determine peak VO2 and HR during the graded exercise tests. Participants were tested in their own wheelchair. Heart rate and blood pressure were measured using a Polar® HR monitor (automatic) and manual blood pressure (BP) cuff, respectively. The HR monitor was placed on the subject's chest below the xyphoid process. After a warm up period of two minutes, participant cycled at a pace of 50 revolutions per minute (RPM). The initial resistance was set at 36 watts and a pace of 50 revolutions per minute (RPM), followed by incremental increases in workload of 12 watts every 2 min. VO2 peak was determined once respiratory exchange ratio (RER) exceeded 1.1 and the participant was unable to maintain a pace of 50 RPM.
Dual energy X-ray absorptiometry (DXA). DXA was used to measure body composition, total percentage and absolute fat mass (FM) and fat-free mass (FFM). The scans were performed one week before and three to four days after the end of the 16-week exercise intervention. Every effort was taken to mimic the original participants’ positioning on the scanner between the baseline and post-intervention measurements. Both legs were strapped together proximal to the knee joint to allow the participant to maintain a neutral position and reduce external rotation. The scans were performed after lying flat for at least 20 minutes to minimize the effect of fluid shift on body composition parameters.9,32–35 Total body DXA scans were performed using a Lunar Prodigy Advance (Lunar Inc., Madison, WI, USA)b located at the VAMC hospital.
Intravenous Glucose Tolerance Tests (IVGTT). Following a 12-hour fast, a standard 3-hour intravenous glucose tolerance test (IVGTT) was performed to determine insulin sensitivity and glucose effectiveness.33 The IVGTT used in this study is considered a more highly sensitive test for detecting Si or Sg compared to that of standard oral glucose tolerance testing used in previous studies.23,36,37 IVGTTs were performed between the hours of 8:00 and 8:30 after fasting overnight. Briefly, an indwelling catheter was placed in an antecubital vein and with an intravenous saline drip (0.9% NaCl) was initiated to maintain the patency of the catheter, and another intravenous line was placed in a contralateral hand vein to facilitate infusion of glucose and blood sampling during the IVGTT. Glucose samples were taken at –6, −4, −2, 0, 2, 3, 4, 5, 6, 8, 10, 12, 14, 16, 19, 22, 23, 24, 25, 27, 30, 35, 40, 50, 60, 70, 80, 90, 100, 120, 140, 160, and 180 minutes after a rapid glucose injection (0.3 gm/kg IV over 30 seconds at time zero). In addition, 20 minutes after the glucose injection, a bolus of insulin (0.02 U/kg) was injected. The results of the IVGTT were modeled using MinMod analysis (MinMod Inc., Pasadena, CA, USA). Fasting glucose, fasting insulin, insulin sensitivity (Si) and glucose effectiveness (Sg) were calculated prior to 16 weeks of training and 72 hours following the final exercise bout of each of the interventions.
Muscle Biopsy of Vastus Lateralis and Triceps. Muscle biopsies were obtained from the right-side long head of the triceps and VL immediately after performing an IVGTT in the clinical research center. The area overlying the muscles was prepped and draped in sterile fashion, and 3 ml of 2% lidocaine were locally administered. A 5-mm skin incision was then made with a #10 scalpel and the biopsy was obtained using a percutaneous muscle biopsy needle (Bergström needle) inserted through the incision and into the muscle; suction was simultaneously applied using a 60 CC syringe. The incision was closed with Steristrips and an overlying sterile adhesive dressing, with a pressure dressing administered for at least 10 minutes. The biopsy sample was immediately frozen in liquid nitrogen and stored at –70 °C until analyzed.
Muscle homogenization and protein quantification
Muscle tissue was placed in a 1:10 weight-to-volume ratio using 1x RIPA buffer supplemented with protease and phosphatase inhibitors. The tissue was homogenized with an electric tissue homogenizer, briefly sonicated, and centrifuged at 4 °C for 10 minutes at 10,000 g. The supernatant was collected and analyzed for protein content with a microBCA kit (Pierce).
SDS-PAGE and Western immunoblotting
The supernatant was mixed 1:1 in Laemlli sample buffer, boiled for 3 min, and briefly centrifuged down at room temperature. Approximately 50 µg of protein was loaded into 10% polyacrylamide gels and run for 60 min at 185 V. A 60 min semi-dry transfer (Trans-blot; Bio-Rad) at 20 V was used to transfer protein from the gel to a PVDF membrane. The membrane was stained with a Ponceau S solution after the transfer to visualize equal protein loading and destained with 0.1 M NaOH. Membranes were quickly rinsed in Tris-buffered saline with 0.05% Tween 20 (TBS-T) and placed in a blocking solution of 5% milk and TBS-T for an hour. Membranes were incubated at 4 °C overnight with one of the following primary antibodies after dilution in 1% milk and TBS-T solution: GLUT4 (sc-7938) or PGC-1α (sc-13067) obtained from Santa Cruz Biotechnology; AMPK (#2532) from Cell Signalin. The primary antibody dilutions used were 1:1000. Membranes were rinsed in TBS-T 3 times for 10 min each before being placed in a 1:2000 solution of a horseradish peroxidase-conjugated secondary antibody (Cell Signalin) and 1% milk and TBS-T for an hour at room temperature. Membranes were rinsed with TBS-T 3 times for 10 min each, then incubated with a horseradish peroxidase chemiluminescence (ECL Prime; Amersham) detection reagent for 5 min and imaged using a digital imager (A600; Amersham). Densitometry was analyzed with iQuant software and all samples were normalized to the pre-value for each muscle group.
Interventions over the course of 16 weeks
Arm-Crank Ergometer (n = 5). Training was performed at the VA Medical Center SCI Exercise Physiology Laboratory and consisted of exercising the arms on an upper body ergometer (Monarch Rehab Trainer 881E). Each session began with a ten-minute warmup, followed by 40 minutes of training, and finished with a 10-minute cool-down. Warm-up and cool-down periods consisted of arm cycling without resistance. During the 16-week training period, the workload was adjusted from 20 to 40 watts to maintain a peak heart rate (HR) at 75% of their maximum HR.32 The participant was encouraged to maintain an exercise rate of 50 revolutions per minute.
Functional Electrical Stimulation (FES; n = 4). FES cycling performed on an ERGYS 2 ergometer (Therapeutic Alliances, Fairborn, OH, USA) with bilateral stimulation of the quadriceps, hamstrings, and gluteal muscles.32,33 Muscles were stimulated sequentially at 60 Hz with current amplitude (140 mA) necessary to complete 40 minutes of cycling at 50 RPM with progressively greater resistance over the course of training. Participants started cycling against no resistance (0/8 kiloponds, kp). However, once the subject was able to cycle without fatigue or dropping of the cadence below 50 RPM, the resistance of the bike was progressed manually to 0.125 kp. The target of the FES-LEC training was to complete an exercise session for 40 minutes at 50 RPM without fatigue. Each session included 10-minutes of passive warm-up and cool-down, and heart rate was monitored and recorded throughout the training using a Polar RS400 watch. The passive cycling was performed by one of the research investigators to maintain a cadence of 5 RPM less than the target cadence. Fatigue threshold was set at 10 RPM to allow for a longer cycling time despite the fact that muscle fatigue may ensue.32,33
Statistical analysis
Independent t-tests were used to evaluate differences in subjects’ demographics between FES-LEC and ACE groups. Repeated measure ANOVA within (pre-and post-interventions) and between (FES-LEC vs. ACE) subject factors were used to analyze body composition and metabolic data. Due to the nature of the difficulties with muscle biopsies in those with chronic SCI and the low sample size, we have chosen to present the data qualitatively as a series of case studies (Figs. 1–3). All values were reported as mean ± SD and statistical significance was set at alpha less than 0.05. Statistical analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
Figure 1.
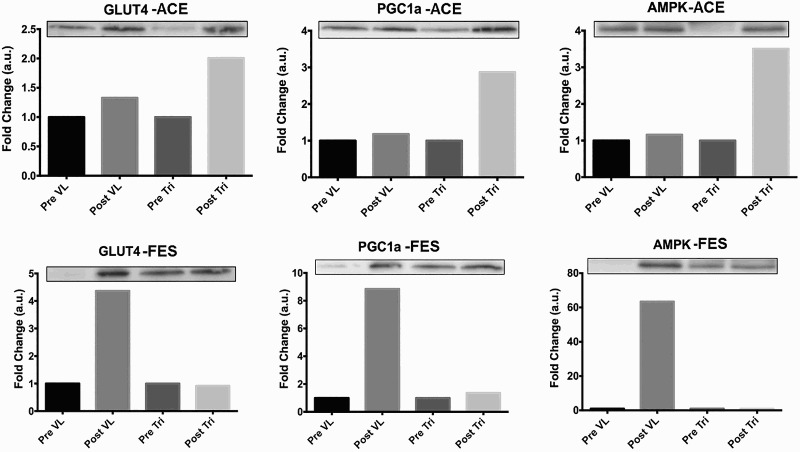
Panel of representative protein immunoblots for GLUT-4, PGC-1α and AMPK protein signaling expressions in one person following 16 weeks of ACE (upper panel) and another person following FES-LEC (lower panel) with motor-complete SCI
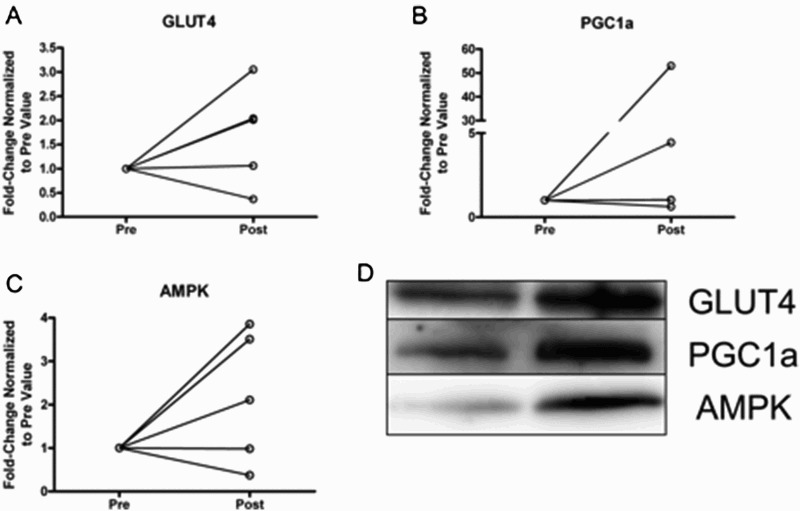
Figure 3.
Spaghetti plots of individual changes in protein expression of a) GLUT-4, b) PGC-1α, c) AMPK and d) immunoblots of the three proteins pre-and post- FES-LEC training for 16 weeks
Results
Physical characteristics and cardiovascular response
The physical characteristics of the 9 participants with motor-complete SCI are presented (Table 1). There was no statistical difference in any of the physical characteristics between the ACE and FES-LEC groups. The compliance rates for the 80 sessions were 95% for ACE (72–80 sessions) and 98% for FES-LES (77–80 sessions).
Table 1.
Physical characteristics of 9 individuals with motor complete SCI who were randomly assigned to either 16 weeks of ACE (n = 5) or FES-LEC (n = 4)
| Groups | Sex | Age | Ethnicity | Weight (kg)-Pre | Weight (kg)-Post | Height (m) | BMI (Kg/m2)-Pre | BMI (Kg/m2)-Post | TSI | LOI | AIS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ACE | M | 61 | Native Hawaiian | 78.9 | 76.2 | 1.7 | 28.1 | 27.1 | 10 | T8-T9 | A |
| ACE | M | 46 | White | 67.4 | 68.3 | 1.7 | 24.0 | 23.6 | 26 | T4 | A |
| ACE | F | 30 | White | 76.2 | 76.6 | 1.7 | 29.3 | 30.0 | 2 | T6 | A |
| M | 34 | African American | 79.2 | 76.3 | 1.8 | 25.1 | 24.2 | 5 | T7 | A | |
| ACE | M | 34 | African American | 100.61 | 103.4 | 1.7 | 34.4 | 35.3 | 13 | T10 | A |
| Mean + SD | 41 ± 13 | 80 ± 12 | 80 ± 13 | 1.72 ± 0.04 | 28 ± 4 | 28 ± 5 | 11 ± 9 | T4-T10 | 5A | ||
| FES | M | 29 | White | 80.1 | 91.6 | 1.8 | 25.1 | 28.9 | 4 | T5-T6 | A |
| FES | M | 45 | African American | 76.5 | 76.3 | 1.7 | 26.8 | 27.4 | 4 | T5-T6 | B |
| FES | M | 34 | African American | 93.4 | 86 | 1.7 | 32.9 | 30.2 | 5 | T6 | A |
| FES | M | 41 | African American | 64.4 | Missing | 1.8 | 19.8 | Missing | 14 | C8-T1 | A |
| Mean + SD | 4M | 37 ± 7 | 79 ± 12 | 85 ± 8 | 1.75 ± 0.06 | 26 ± 5 | 29 ± 1.4 | 7 ± 5 | C8-T6 | 4A/1B |
Resting systolic and diastolic blood pressures did not change following either ACE (systolic: 119 ± 13 to 118 ± 12 mmHg and diastolic: 75 ± 5 to 77 ± 6 mmHg; P > 0.5) or FES-LES training (systolic: 123 ± 8 to 127 ± 10 mmHg and diastolic: 79 ± 5 to 83 ± 15 mmHg; P > 0.5). Similarly, resting heart rate did not change following ACE (76.5 ± 10 to 78 ± 12 bpm; P = 0.7) or FES-LEC training (76 ± 3 to 80.5 ± 25 bpm; P = 0.8), nor did peak HR following ACE (170 ± 23 to 180 ± 11 bpm; P = 0.8) or FES-LEC training (138 ± 2 to 155 ± 9 bpm; P = 0.3). There was trend for a greater peak oxygen uptake following ACE training (16.5 ± 3 to 20.0 ± 5.0 ml/kg/min; P = 0.09) but with not after FES-LEC training (14.0 ± 0.7 to 14.5 ± 3 ml/kg/min; P = 0.9).
Body composition and carbohydrate metabolism
Total body weight, body composition and the metabolic profile prior to and 16 weeks after each exercise training intervention are summarized in Table 2. Neither intervention influenced whole body composition or carbohydrate profile. Fasting glucose did not change following ACE training (95 ± 9 to 94 ± 14 mg/dl; P = 0.9), although there was a non-significant 7% increase following FES-LEC training (90 ± 2 to 96 ± 13 mg/dl; P = 0.4). Peak plasma glucose was unchanged (–4%) after ACE training (P = 0.6), but there was a non-significant increase of 27% after FES-LEC training (P = 0.5). Fasting insulin decreased 30.5% (P = 0.5) and peak plasma insulin increased 14% (P = 0.6) after ACE training. Fasting insulin decreased 60% after ACE training (P = 0.4) and decreased by 5% (P = 0.8) after FES-LEC training.
Table 2.
Body composition and carbohydrate metabolism profile in individuals with motor complete SCI following 16 weeks of either FES-LEC or ACE training
| Groups | %Fat Mass-Pre | %Fat Mass-Post | Fat- Pre (kg) | Fat- Post (kg) | Fat-Free Mass (kg)-Pre | Fat-Free Mass (kg)-Post | Fasting glucose (mg/dl)-Pre | Fasting glucose (mg/dl)-Post | Sg-Pre (min-1) | Sg-Post (min−1) | Fasting Insulin (μu/ml)-Pre | Fasting Insulin (μu/ml-Post | Si-Pre (μu/l)−1.min−1 | Si-Post (μu/l)−1.min−1 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACE | 37.1 | 38.4 | 28.4 | 27.8 | 50.9 | 47.4 | 104 | 115 | 0.013 | 0.012 | 14 | 10 | 1.84 | 0.82 |
| ACE | 39.0 | 35.6 | 25.3 | 23.2 | 42.1 | 44.3 | 92 | 92 | 0.017 | 0.035 | 6.5 | 5 | 2.74 | 7.5 |
| ACE | 44.2 | 45.2 | 32.2 | 33.0 | 43.2 | 42.6 | 103 | 96 | 0.03 | 0.023 | 5.5 | 1.3 | 1.17 | 3 |
| ACE | 36.7 | 34.5 | 27.3 | 24.8 | 50.9 | 51.0 | 81 | 78. | 0.008 | 0.037 | 3 | 2.2 | 1.67 | 3.9 |
| ACE | 43.9 | 37.2 | 42.9 | 37.2 | 57.8 | 65.6 | 93 | 88 | 0.035 | 0.029 | 25.5 | 20 | 2.56 | 1 |
| Mean ± SD | 40 ± 3.7 | 38 ± 4 | 31 ± 7 | 29 ± 6 | 49 ± 6.5 | 50 ± 9 | 95 ± 9 | 94 ± 14 | 0.020 ± 0.01 | 0.027 ± 0.01 | 11 ± 9 | 7.6 ± 7.5 | 2 ± 0.65 | 3.25 ± 2.7 |
| FES | 38.4 | 40.8 | 28.7 | 35.9 | 48.9 | 54.7 | 88 | 110 | 0.017 | 0.023 | 4.5 | 3.4 | 6 | 20 |
| FES | 39.4 | 36.9 | 27.7 | 27.0 | 46.1 | 49.6 | 91 | 95 | 0.025 | 0.024 | 3.7 | 6.6 | 3.4 | 3.6 |
| FES | 44.5 | 41.3 | 40.0 | 34.2 | 53.1 | 51.9 | 91.4 | 84 | 0.032 | 0.028 | 33 | 6.5 | 2 | 2.5 |
| FES | 30.7 | 32.0 | 19.0 | 20.3 | 46.0 | 46.1 | Missing | Missing | Missing | Missing | Missing | Missing | Missing | Missing |
| Mean + SD | 38 ± 5.7 | 38 ± 4 | 29 ± 8.6 | 29 ± 7 | 48.5 ± 3.3 | 50.6 ± 3.6 | 90 ± 2 | 96 ± 13 | 0.024 ± 0.007 | 0.025 ± 0.003 | 14 ± 17 | 5.5 ± 1.8 | 3.8 ± 1.9 | 8.7 ± 9.8 |
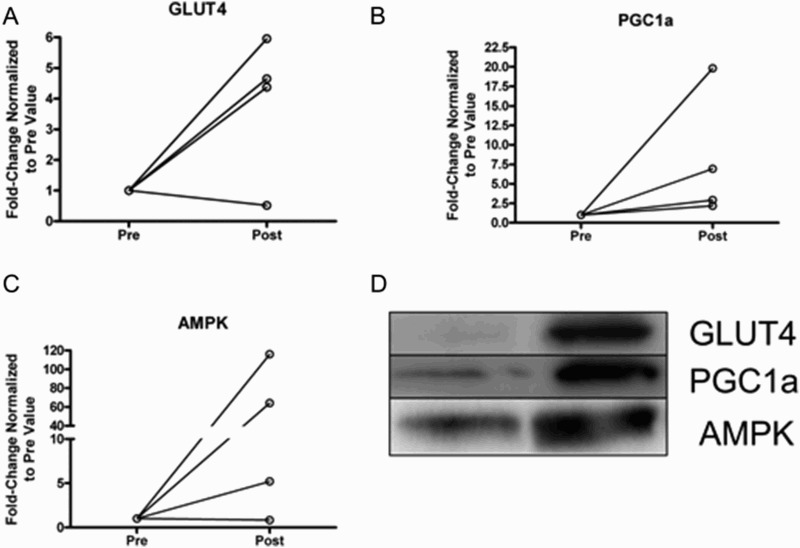
Protein expressed
The data for the ACE shows a general trend for greater levels of expression for GLUT4, PGC1-a and AMPK after 16 weeks of training (Fig. 2, A-C) and this is similar to the response seen following the FES-LEC training of the paralyzed muscle after a similar duration (Fig. 3, A-C). Please note that the outliers (greater than 3 SD) for certain proteins for individuals were due to the limited detection of the protein of interest at the pre-training muscle biopsy (Figs. 1–3). We include this data points because Ponceau staining was considered to ensure equal loading condition and troponin immunoblotting suggested that these tissues were largely muscle tissue.
Figure 2.
Spaghetti plots of individual changes in protein expression of a) GLUT-4, b) PGC-1, c) AMPK and d) immunoblots of the three proteins pre-and post-ACE training for 16 weeks
In VL, there was a minimal increase in GLUT-4 protein expressed following ACE (n = 4; 1.3 fold) and FES-LEC (n = 4; 3.8 fold) training, respectively, after 16 weeks. In triceps muscle, GLUT-4 protein expressed increased following ACE (0.6 fold; P = 0.18) and FES-LEC (0.5 fold; n = 2), respectively (Figs. 2 and 3). The samples of the triceps muscles in the FES-LEC group was reduced to 2 participants instead of 4 participants for protein analysis because sample was not obtained from one participant and sample quality from the other participant's muscle biopsy was too poor to quantify protein content or perform immunoblotting due to extensive protein degradation. In VL, PGC-1α protein expressed was not altered after ACE (n = 4; 1.1 fold) but increased 2.3 fold by FES (n = 4). In the triceps, PGC-1α protein expressed increased by 3.8 fold after ACE (n = 5) but decreased (0.6 fold) following FES (n = 2; Figs. 2 and 3).
In VL, there was a minimal increase in AMPK protein expressed after ACE (n = 4; 1.22 fold) and a greater increase after FES (n = 4; 3.4 fold). In the triceps muscle, AMPK protein expressed greatly increased after ACE (n = 5; 3.4 fold) but decreased by 0.4 fold after FES (Figs. 2 and 3).
Discussion
To our knowledge, this is the first study that has compared the training effects of ACE or FES-LEC on both paralyzed (VL) and non-paralyzed (triceps) muscle groups in persons with motor-complete SCI. This study design allows one to evaluate the possibility that training of a paralyzed muscle has benefits for the non-paralyzed muscle or vice-versa. Despite the lack of significant change in any parameter following either FES-LEC and ACE training interventions (body composition, glucose effectiveness and insulin sensitivity) over the 16-week exercise training period, ACE and FES exercise training showed positive trends in protein expression of GLUT-4, AMPK and PGC-1α in their respectively exercise muscle group. However, these benefits appeared to be limited to the muscle being trained.
ACE vs. FES-LEC on body composition and glucose metabolism
In contrast to our most recent findings from our lab,32 in the current study, neither ACE nor FES-LEC had an effect upon parameters of body composition and carbohydrate metabolism.32 In the former study, ACE (n = 3) or FES-LEC (n = 3) increased whole body and leg lean mass by 8% and 9%, respectively, following 16 weeks of training. Griffin et al. noted positive changes in carbohydrate metabolism following 8 weeks of FES-LEC.23 The lack of effect of ACE or FES-LEC on body composition or carbohydrate metabolism in the current study may reflect the rapid loss of exercise effects on glucose uptake, the small sample size or, possibly, subject characteristics. Of note, FES-LEC training using the same protocol as that of the current study resulted in an improvement of Si without improvement in parameters of body composition in a single person with motor-complete SCI,33 suggesting discordant benefits of exercise training that may not be influenced by anthropometric outcomes. Other factors such as increases in visceral adiposity,17 failure to control for dietary habits35 may have contributed to the lack of major changes in Sg or Si in our study. Persons with SCI are likely to consume a high fat diet (∼40%) and 56% of the SCI population are not able to meet the daily caloric intake requirements.35
Differences between ACE and FES-LEC training
The interest in the current work has stemmed from the possibility that paralyzed VL may demonstrate reduced molecular and cellular responses to training by FES-LEC compared to the innervated triceps muscle. Previous reports noted that skeletal muscles in persons with SCI are more sensitive to loading than the muscles in the able-bodied.39,40 These studies demonstrated the sensitivity of the paralyzed VL to an acute bout of surface neuromuscular electrical stimulation. Our report suggests that FES-LEC may lead to greater responsiveness compared to ACE in paraplegics. One interpretation of these findings is that in paralyzed VL the training reverses the deterioration in cellular and molecular processes that support the muscle contraction, glucose uptake and energy utilization, which have extensively decayed following SCI.39,40
Effects of ACE and FES-LEC on protein expression
Our findings suggest greater changes in relative protein expression levels of GLUT-4, PGC-1α, and AMPK following FES-LEC training compared to ACE. This is most likely due to greatly reduced levels of these vital proteins in chronically paralyzed muscle. Moreover, greater protein expression following both interventions may be related to reductions in the levels of serum and muscle-derived cytokine expression, which are increased following SCI13,14 and can have deleterious effects on both the paralyzed and non-paralyzed muscles. Our findings suggest that GLUT-4, AMPK and PGC-1α are responsive to exercise training in the paralyzed muscles, consistent with prior reports.41 The increase in GLUT-4 protein expression may be explained by chronic exercise-induced, non-insulin-mediated increased GLUT-4 gene transcription likely stimulated by a calcium-dependent mechanism in response to skeletal muscle contractions.18–22 Moreover, increased AMPK expression may facilitate contraction-induced translocation of GLUT-424 and improve glucose disposal.20
We have recently shown that following an acute bout of FES-LEC that persons with SCI predominantly rely on carbohydrate utilization with little fat utilization.42 Those with SCI have an increase in intramuscular fat and glucose intolerance, which may be a marker of the decreased oxidative capacity and mitochondrial activity common in those with SCI.43–45 PGC-1α is considered an important factor for mitochondrial biogenesis and oxidative metabolism. Reduced expression of PGC-1α results in diminished expression of proteins necessary for mitochondrial biogenesis, beta oxidization and oxidative phosphorylation.43 PGC-1α expression is reduced following denervation as well as at 42 days after SCI, associated with reductions in the size and number of mitochondria.25,26 The state of mitochondrial health and function play a significant role in altered metabolic profiles.43,44 Individuals with SCI occupy the lowest end of the physical activity spectrum, with a VO2 peak as low as 0.9 l/min.45 Martin et al. reported a 48–67% lower SDH activity per unit fiber volume in tibialis anterior muscle fibers of patients 2–11 years after injury compared with AB controls.46
PGC-1α expression is known to influence fiber type phenotype and enhance the shift from fast to slow myosin heavy chain. Muscle in those with SCI is predominantly transformed to fast twitch fibers within the first 6 weeks after SCI in humans.8 The greater expression of PGC-1α after training by FES-LES suggests at least the potential for a fast-to-slow fiber type transition and increased capability for oxidative phosphorylation and beta oxidation. Our study also agrees with recent findings that showed upregulation of PGC-1 α gene expression following an acute bout of electrical stimulation in a person with complete SCI (47), and increased expression of PGC-1a and genes for oxidative metabolism and beta-oxidation in a chronically FES-trained soleus muscle compared to the contralateral untrained control.41,47
Limitations
The small sample size is the major limitation of our study. Moreover, missing data on one of the participants in the FES-LES group further reduced statistical power. In addition, the size of muscle biopsy samples limited us to analysis of total levels of three proteins. However, the metabolic signaling events that determine glucose uptake, insulin action and energy metabolism are complex. For example, evidence suggests that calcium related mechanisms involving CaMKII acting on AMPK, may be involved in the substrate utilization during exercise. Signal transduction involves phosphorylation of multiple kinases and downstream targets; examples include phosphorylation of AMPK (thr 172), CaMKII (thr 286) and Akt (Ser 473). The design of the current study collected muscle biopsies 72 hours after the last exercise session whereas most of the phosphorylation events are expected to be resolved after 24–48 hours.
The study groups may have included both responders and non-responders with respect to changes in body composition and carbohydrate metabolism. Non-responders may have achieved lower exertional intensity or have had co-morbidities that were not excluded by the trial design. We have previously shown that a person with SCI who participated in the identical study protocol (4 days per week for 21 weeks) failed to achieve any positive endpoints because of several confounding factors.33
Conclusions
In individuals with chronic motor-complete SCI, FES-LEC training for 16 weeks resulted in qualitatively similar protein expressions changes in the VL as compared to those observed in triceps after ACE. Effects of exercise of VL did not alter protein expression in triceps, and vice-versa. Up-regulation of GLUT-4 levels in the muscle in response to ACE or FES-LEC was not associated with improvements in whole body carbohydrate metabolism. Further study is required to understand the relationships between changes in biochemical parameters in muscle and insulin responses/glucose uptake in persons with SCI. This discrepancy between proteins’ abundance and carbohydrate metabolism, may suggest that other factors similar to diet, medication use and level of physical activity are responsible for improvement in whole body carbohydrate metabolism after exercise training.
Acknowledgements
Supported by VHA RR&D number B3918R, VHA RR&D number B6757R, VHA RR&D number B-9212-C, VHA RR&D number B2020-C, and award number UL1RR031990 from the National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Veterans Health Administration, National Center for Research Resources, or the National Institutes of Health.
Disclaimer statements
Contributors None.
Funding None.
Conflict of interest None.
Ethics approval None.
References
- 1.American Diabetes Association http://www.diabetes.org/. Last visited on 04/20/2016.
- 2.Duckworth WC, Jallepalli P, Solomon SS.. Glucose intolerance in spinal cord injury. Arch Phys Med Rehabil 1983;64(3):107–10. [PubMed] [Google Scholar]
- 3.Bauman WA, Spungen AM.. Disorders of Carbohydrate and Lipid-Metabolism in Veterans with Paraplegia or Quadriplegia - a Model of Premature Aging. Metabolism-Clinical and Experimental 1994;43(6):749–56. doi: 10.1016/0026-0495(94)90126-0 [DOI] [PubMed] [Google Scholar]
- 4.Lavela SL, Weaver FM, Goldstein B, Chen K, Miskevics S, Rajan S, Gater DR Jr. Diabetes mellitus in individuals with spinal cord injury or disorder. J Spinal Cord Med 2006;29(4):387–95. doi: 10.1080/10790268.2006.11753887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA.. Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol 1999;80(4):373–8. doi: 10.1007/s004210050606 [DOI] [PubMed] [Google Scholar]
- 6.Gorgey AS, Dudley GA.. Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord 2007;45(4):304–9. [DOI] [PubMed] [Google Scholar]
- 7.Talmadge RJ, Castro MJ, Apple DF Jr, Dudley GA.. Phenotypic adaptations in human muscle fibers 6 and 24 wk after spinal cord injury. J Appl Physiol 200;92(1):147–54. doi: 10.1152/japplphysiol.000247.2001 [DOI] [PubMed] [Google Scholar]
- 8.Castro MJ, Apple DF Jr, Staron RS, Campos GE, Dudley GA.. Influence of complete spinal cord injury on skeletal muscle within 6 mo of injury. J Appl Physiol 1999;86(1):350–8. [DOI] [PubMed] [Google Scholar]
- 9.Gorgey AS, Gater DR.. Regional and relative adiposity patterns in relation to carbohydrate and lipid metabolism in men with spinal cord injury. Appl Physiol Nutr Metab 2011;36(1):107–14. doi: 10.1139/H10-091 [DOI] [PubMed] [Google Scholar]
- 10.Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR.. Effects of spinal cord injury on body composition and metabolic profile - part I. J Spinal Cord Med 2014;37(6):693–702. doi: 10.1179/2045772314Y.0000000245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gater DR. Obesity after spinal cord injury. Phys Med Rehabil Clin N Am 2007;18(2):331–51. doi: 10.1016/j.pmr.2007.03.004 [DOI] [PubMed] [Google Scholar]
- 12.Elder CP, Apple DF, Bickel CS, Meyer RA, Dudley GA.. Intramuscular fat and glucose tolerance after spinal cord injury—a cross-sectional study. Spinal Cord 2004;42(12):711–6. doi: 10.1038/sj.sc.3101652 [DOI] [PubMed] [Google Scholar]
- 13.Kern PA, Ranganathan S, Li CL, Wood L, Ranganathan G.. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab 2001;280(5):E745–51. [DOI] [PubMed] [Google Scholar]
- 14.Yu C, Chen Y, Cline GW, Zhang D, Zong H, Wang Y, et al. . Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem 2002;277(52):50230–6. doi: 10.1074/jbc.M200958200 [DOI] [PubMed] [Google Scholar]
- 15.Sidossis LS, Stuart CA, Shulman GL, Lopaschuk GD, Robert RW.. Glucose plus insulin regulate fat oxidation by controlling the rate of fatty acid entry in the mitochondria. J Clin Invest 1996;98(10):2244–50. doi: 10.1172/JCI119034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aksnes AK, Hjeltnes N, Wahlstrom EO, Katz A, Zierath JR, Wallberg-Henriksson H.. Intact glucose transport in morphologically altered denervated skeletal muscle from quadriplegic patients. Am J Physiol 1996;271(3 Pt 1):E593–E600. [DOI] [PubMed] [Google Scholar]
- 17.Gorgey AS, Mather KJ, Gater DR.. Central adiposity associations to carbohydrate and lipid metabolism in individuals with complete motor spinal cord injury. Metabolism 2011;60(6):843–51. doi: 10.1016/j.metabol.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 18.Bennegard GM, Karlsson AK.. Higher glucose uptake in paralysed spastic leg. Spinal Cord 2008;46(2):103–106. doi: 10.1038/sj.sc.3102083 [DOI] [PubMed] [Google Scholar]
- 19.Hjeltnes N, Galuska D, Björnholm M, Aksnes A-K, Lannem A, Zierath J, et al. . Exercise-induced overexpression of key regulatory proteins involved in glucose uptake and metabolism in tetraplegic persons: molecular mechanism for improved glucose homeostasis. FASEB J 1998;12(15):1701–12. [DOI] [PubMed] [Google Scholar]
- 20.Chilibeck PD, Bell G, Jeon J, Weiss CB, Murdoch G, MacLean I, et al. . Functional electrical stimulation exercises increases GLUT-1 and GLUT-4 in paralyzed skeletal muscle. Metabolism 1999;48(11):1409–13. doi: 10.1016/S0026-0495(99)90151-8 [DOI] [PubMed] [Google Scholar]
- 21.Jeon JY, Weiss CB, Steadward RD, Ryan E, Burnham RS, Bell G, et al. . Improved glucose tolerance and insulin sensitivity after electrical stimulation-assisted cycling in people with spinal cord injury. Spinal Cord 2002;40(3):110–7. doi: 10.1038/sj.sc.3101260 [DOI] [PubMed] [Google Scholar]
- 22.Mohr T, Dela F, Handberg A, Biering-Sørensen F, Galbo H, Kjaer M.. Insulin action and long-term electrically induced training in individuals with spinal cord injuries. Med Sci Sports Exerc 2001;33(8):1247–52. doi: 10.1097/00005768-200108000-00001 [DOI] [PubMed] [Google Scholar]
- 23.Griffin L, Decker MJ, Hwang JY, Wang B, Kitchen K, Ding Z, et al. . Functional electrical stimulation cycling improves body composition, metabolic and neural factors in persons with spinal cord injury. J Electromyogr Kinesiol 2009;19(4):614–22. doi: 10.1016/j.jelekin.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 24.Coughlan KA, Valentine RJ, Ruderman NB, Saha AK.. AMPK activation: a therapeutic target for type 2 diabetes? Diabetes Metab Syndr Obes 2014;7:241–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scarpulla RC. Metabolic control of mitochondrial biogenesis through the PGC-1 family regulatory network. Biochim Biophys Acta 2011;1813(7):1269–78. doi: 10.1016/j.bbamcr.2010.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arany Z. PGC-1 coactivators and skeletal muscle adaptations in health and disease. Curr Opin Genet Dev 2008;18(5):426–34. doi: 10.1016/j.gde.2008.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haskell WL, et al. Physical activity and public health: updated recommendation for adults from the american college of sports medicine and the american heart association. Med Sci Sports Exerc 2007;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27 [DOI] [PubMed] [Google Scholar]
- 28.Jacobs PL, Nash MS.. Exercise recommendations for individuals with spinal cord injury. Sports Med. 2004;34(11):727–51. doi: 10.2165/00007256-200434110-00003 [DOI] [PubMed] [Google Scholar]
- 29.Evans N, Wingo B, Sasso E, Hicks A, Gorgey AS, Harness E.. Exercise recommendations and considerations for persons with spinal cord injury. Arch Phys Med Rehabil 2015;96(9):1749–50. doi: 10.1016/j.apmr.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 30.Rosety-Rodriguez M, Camacho A, Rosety I, Fornieles G, Rosety MA, Diaz AJ, et al. . Low-grade systemic inflammation and leptin levels were improved by arm cranking exercise in adults with chronic spinal cord injury. Arch Phys Med Rehabil 2014;95(2):297–302. doi: 10.1016/j.apmr.2013.08.246 [DOI] [PubMed] [Google Scholar]
- 31.El-Sayed MS, Younesian A.. Lipid profiles are influenced by arm cranking exercise and training in individuals with spinal cord injury. Spinal Cord 2005;43(5):299–305. doi: 10.1038/sj.sc.3101698 [DOI] [PubMed] [Google Scholar]
- 32.Gorgey AS, Martin H, Metz A, Khalil RE, Dolbow DR, Gater DR.. Longitudinal changes in body composition and metabolic profile between exercise clinical trials in men with chronic spinal cord injury. J Spinal Cord Med 2016 Mar;17:1–14. [Epub ahead of print]. doi: 10.1080/10790268.2016.1229397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gorgey AS, Harnish CR, Daniels JA, Dolbow DR, Keeley A, Moore J, et al. . A report of anticipated benefits of functional electrical stimulation after spinal cord injury. J Spinal Cord Med 2012;35(2):107–12. doi: 10.1179/204577212X13309481546619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gorgey AS, Mather KJ, Cupp HR, Gater DR.. Effects of resistance training on adiposity and metabolism after spinal cord injury. Medicine & Science in Sports & Exercise 2012;44(1):165–74. doi: 10.1249/MSS.0b013e31822672aa [DOI] [PubMed] [Google Scholar]
- 35.Gorgey AS, Caudill C, Sistrun S, Khalil RE, Gill R, Castillo T, et al. . Frequency of dietary recalls, nutritional assessment, and body composition assessment in men with chronic spinal cord injury. Arch Phys Med Rehabil 2015;96(9):1646–53. doi: 10.1016/j.apmr.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 36.Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, DeFronzo RA.. San Antonio Metabolism Study. Beta-cell dysfunction and glucose intolerance: results from the San Antonio metabolism (SAM) study. Diabetologia 2004;47(1):31–39. doi: 10.1007/s00125-003-1263-9 [DOI] [PubMed] [Google Scholar]
- 37.Sharoff CG, Hagobian TA, Malin SK, et al. . Combining short-term metformin treatment and one bout of exercise does not increase insulin action in insulin-resistant individuals. Am J Physiol Endocrinol Metab 2010;298(4):E815Y23. doi: 10.1152/ajpendo.00517.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gregory CM, Bickel CS.. Recruitment patterns in human skeletal muscle during electrical stimulation. Phys Ther 2005;85(4):358–64. [PubMed] [Google Scholar]
- 39.Yarar-Fisher C, Bickel CS, Windham ST, McLain AB, Bamman MM.. Skeletal muscle signaling associated with impaired glucose tolerance in spinal cord-injured men and the effects of contractile activity. J Appl Physiol (1985) 2013;115(5):756–64. doi: 10.1152/japplphysiol.00122.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yarar-Fisher C, Bickel CS, Kelly NA, Windham ST, Mclain AB, Bamman MM.. Mechanosensitivity may be enhanced in skeletal muscles of spinal cord-injured versus able-bodied men. Muscle Nerve 2014;50(4):599–601. doi: 10.1002/mus.24248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adams CM, Suneja M, Dudley-Javoroski S, Shields RK.. Altered mRNA expression after long-term soleus electrical stimulation training in humans with paralysis. Muscle Nerve 2011;43(1):65–75. doi: 10.1002/mus.21831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gorgey AS, Lawrence J.. Acute Responses of Functional Electrical Stimulation Cycling on the Ventilation-to-CO2 Production Ratio and Substrate Utilization after Spinal Cord Injury. PM R 2016;8(3):225–34. doi: 10.1016/j.pmrj.2015.10.006 [DOI] [PubMed] [Google Scholar]
- 43.Puigserver P, Spiegelman BM.. Peroxisome proliferator-activated receptor-gamma coactivator 1 alpha (PGC-1 alpha): transcriptional coactivator and metabolic regulator. Endocr Rev 2003;24(1):78–90. doi: 10.1210/er.2002-0012 [DOI] [PubMed] [Google Scholar]
- 44.Adhihetty PJ, O'Leary MF, Chabi B, Wicks KL, Hood DA.. Effect of denervation on mitochondrially mediated apoptosis in skeletal muscle. Appl Physiol 2007;102(3):1143–51. doi: 10.1152/japplphysiol.00768.2006 [DOI] [PubMed] [Google Scholar]
- 45.Hagerman F, Jacobs P, Backus D, Dudley GA.. Exercise responses and adaptations in rowers and spinal cord injury individuals. Med Sci Sports Exerc 2006;38(5):958–62. doi: 10.1249/01.mss.0000218131.32162.ce [DOI] [PubMed] [Google Scholar]
- 46.Martin TP, Stein RB, Hoeppner PH, Reid DC.. Influence of electrical stimulation on the morphological and metabolic properties of paralyzed muscle. J Appl Physiol 1992;72(4):1401–6. [DOI] [PubMed] [Google Scholar]
- 47.Petrie M, Suneja M, Shields RK.. Low-frequency stimulation regulates metabolic gene expression in paralyzed muscle. J Appl Physiol (1985) 2015;118(6):723–31. doi: 10.1152/japplphysiol.00628.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]


