This multicenter study determines whether an emergency department–initiated intervention reduces subsequent suicidal behavior.
Key Points
Question
Do emergency department (ED)–initiated interventions reduce subsequent suicidal behavior among a sample of high-risk ED patients?
Findings
In this multicenter study of 1376 ED patients with recent suicide attempts or ideation, compared with treatment as usual, an intervention consisting of secondary suicide risk screening by the ED physician, discharge resources, and post-ED telephone calls focused on reducing suicide risk resulted in a 5% absolute decrease in the proportion of patients subsequently attempting suicide and a 30% decrease in the total number of suicide attempts over a 52-week follow-up period.
Meaning
For ED patients at risk for suicide, a multifaceted intervention can reduce future suicidal behavior.
Abstract
Importance
Suicide is a leading cause of deaths in the United States. Although the emergency department (ED) is an opportune setting for initiating suicide prevention efforts, ED-initiated suicide prevention interventions remain underdeveloped.
Objective
To determine whether an ED-initiated intervention reduces subsequent suicidal behavior.
Design, Setting, and Participants
This multicenter study of 8 EDs in the United States enrolled adults with a recent suicide attempt or ideation and was composed of 3 sequential phases: (1) a treatment as usual (TAU) phase from August 2010 to December 2011, (2) a universal screening (screening) phase from September 2011 to December 2012, and (3) a universal screening plus intervention (intervention) phase from July 2012 to November 2013.
Interventions
Screening consisted of universal suicide risk screening. The intervention phase consisted of universal screening plus an intervention, which included secondary suicide risk screening by the ED physician, discharge resources, and post-ED telephone calls focused on reducing suicide risk.
Main Outcomes and Measures
The primary outcome was suicide attempts (nonfatal and fatal) over the 52-week follow-up period. The proportion and total number of attempts were analyzed.
Results
A total of 1376 participants were recruited, including 769 females (55.9%) with a median (interquartile range) age of 37 (26-47) years. A total of 288 participants (20.9%) made at least 1 suicide attempt, and there were 548 total suicide attempts among participants. There were no significant differences in risk reduction between the TAU and screening phases (23% vs 22%, respectively). However, compared with the TAU phase, patients in the intervention phase showed a 5% absolute reduction in suicide attempt risk (23% vs 18%), with a relative risk reduction of 20%. Participants in the intervention phase had 30% fewer total suicide attempts than participants in the TAU phase. Negative binomial regression analysis indicated that the participants in the intervention phase had significantly fewer total suicide attempts than participants in the TAU phase (incidence rate ratio, 0.72; 95% CI, 0.52-1.00; P = .05) but no differences between the TAU and screening phases (incidence rate ratio, 1.00; 95% CI, 0.71-1.41; P = .99).
Conclusions and Relevance
Among at-risk patients in the ED, a combination of brief interventions administered both during and after the ED visit decreased post-ED suicidal behavior.
Introduction
Suicidal behavior is a significant public health issue. In 2015, there were 44 193 deaths by suicide in the United States. Suicide accounts for 1.2% of all deaths and is the tenth leading cause of death in the United States. Attempted suicide is an even more common event, with more than 1 million people per year attempting suicide.
Despite its significance, to our knowledge, few intervention trials have targeted and/or reduced suicidal behavior. Some psychotherapies have been found to reduce rates of suicide attempts, although there are concerns about publication bias. Additionally, these interventions require substantial training and are lengthy and costly to administer. Briefer, less intensive interventions (eg, follow-up letters and reminder postcards) have had mixed results. New interventions specifically developed to prevent suicidal behavior are clearly needed.
Because emergency departments (EDs) treat many patients who are at risk for suicidal behavior, they are particularly important locations for suicide prevention. More than 4% of all ED visits are attributable to psychiatric conditions, and there are approximately 420 000 visits every year for intentional self-harm. These high-risk individuals are susceptible to suicide attempts after their ED visit. Also, a significant proportion of those who die by suicide received care in an ED in the period prior to death.
To address these ongoing public health issues, we conducted a multicenter study of adult ED patients who screened positive for suicide attempts or ideation. In this article, we focus on the hypothesis that a multifaceted intervention delivered during and after the ED visit would decrease subsequent suicidal behaviors compared with usual care.
Methods
Study Design and Settings
This article is part of the Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE) study (clinicaltrials.gov identifier: NCT01150994). The ED-SAFE study was designed to examine the effect of universal screening and an intervention on individuals at risk for suicide in the ED setting. Description of the methods and effect of screening on risk detection have been reported previously. Participants with suicidal ideation or recent attempt were recruited from 8 EDs across 7 states in the United States, ranging from small community hospitals to large academic centers. To increase generalizability, no participating ED had psychiatric services located within or adjacent to the ED. The ED-SAFE study consisted of 3 sequential phases at each site: (1) the treatment as usual (TAU) phase, (2) the universal screening (screening) phase, and (3) the universal screening plus intervention (intervention) phase.
For all phases, following the index ED visit, enrolled participants were observed for 1 year using telephone assessments and medical record reviews. Trained blinded interviewers at a centralized call center conducted outcome assessments at 6, 12, 24, 36, and 52 weeks. If suicide risk was detected, the participant was immediately connected to the Boys Town Suicide Prevention Hotline. Additionally, using a standardized form, trained medical record abstractors at each site conducted medical record reviews 6 and 12 months after enrollment.
In the TAU phase, participants were treated according to the usual and customary care at each site, serving as the control for the subsequent study phases. In the screening phase, sites implemented clinical protocols with universal suicide risk screening (the Patient Safety Screener) for all ED patients. In the intervention phase, in addition to universal screening, all sites implemented a 3-component intervention: (1) a secondary suicide risk screening designed for ED physicians to evaluate suicide risk following an initial positive screen, (2) the provision of a self-administered safety plan and information to patients by nursing staff, and (3) a series of telephone calls to the participant, with the optional involvement of their significant other (SO), for 52 weeks following the index ED visit. The structure and content of these calls were based on the Coping Long Term with Active Suicide Program (CLASP) protocol, an adjunctive intervention designed to reduce suicide risk that is composed of a unique combination of case management, individual psychotherapy, and SO involvement. The clinician’s primary role as the CLASP contact was more of a treatment advisor than therapist. The CLASP-ED protocol consisted of up to 7 brief (10- to 20-minute) telephone calls to the participant and up to 4 calls to an SO identified by the participant, if available (eTable 1 in the Supplement). The calls focused on identifying suicide risk factors, clarifying values and goals, safety and future planning, facilitating treatment engagement/adherence, and facilitating patient-SO problem-solving. Multiple attempts were made to complete each scheduled call, and voicemails were left if the participant did not pick up. If a call could not be completed, the advisor sent a personalized letter expressing concern for the patient and inviting them to call.
Calls following CLASP-ED protocol were centralized at Butler Hospital in Providence, Rhode Island, and were administered by 10 advisors (6 PhD psychologists, 3 psychology fellows, and 1 masters-level counselor). All advisors were trained to criteria by the developers of CLASP and received weekly supervision.
Institutional review boards at each site approved the study. All ED participants gave written consent. Because SOs in the intervention phase were only contacted by telephone, these participants gave verbal consent. The National Institute of Mental Health Data and Safety Monitoring Board conducted overall study oversight and monitoring.
Participants
Adults presenting to one of the EDs with a suicide attempt or ideation within the week prior to the ED visit were eligible for inclusion. Patients in the ED with any level of self-harm behavior or ideation were identified via real-time medical record review and approached for eligibility screening. Patients were enrolled if they confirmed either a suicide attempt or active suicidal ideation within the past week and agreed to study requirements. Exclusion criteria included (1) being medically or cognitively unable to participate in study procedures, (2) living in a noncommunity setting, (3) being under state custody or pending legal action, (4) being without permanent residence or reliable telephone service, and (5) having an insurmountable language barrier.
Outcomes
Outcomes were assessed by a combination of telephone interviews using the Columbia Suicide Severity Rating Scale and medical record review over the 52-week follow-up period. The occurrence and timing of each outcome variable were assessed using data collected from all possible sources. Research team members reviewed data from all sources to reconcile discrepancies and to eliminate overlap in identified events.
Consistent with other suicide prevention trials, the primary outcome variable was suicide attempts (both fatal and nonfatal) based on Columbia Suicide Severity Rating Scale definitions. We analyzed both the proportion of patients who made a suicide attempt and the total number of suicide attempts occurring during the 52-week follow-up period.
We also analyzed a broader suicide composite based on the occurrence of any of 5 types of suicidal behavior: death by suicide, suicide attempt, interrupted or aborted attempts, and suicide preparatory acts. The time-to-event for each participant was defined as the period from the index ED visit to when the outcome occurred within the 52-week follow-up period. Participants who did not have an outcome were censored at time of withdrawal (suicide attempt) or their last follow-up interview (suicide composite).
Statistical Analysis
The sample-size calculation was based on an assumed rate of the primary outcome over the 52-week period in the TAU phase of 20%. Thus, enrollment of 1440 patients has a power of 80% (at a 2-sided α level of .05) to detect an absolute risk reduction of 7 percentage points (or a relative risk reduction of 35%) in the intervention phase, allowing for an expected 20% loss to follow-up over the 52-week follow-up period. Continuous variables were reported as medians and interquartile ranges (IQRs) and categorical variables as proportions. Kruskal-Wallis, χ2, and Fisher exact tests were used to analyze between-phase baseline differences.
Analyses included all enrolled participants, with no exclusions (intention-to-treat). To test for potential differences in the proportion of patients making a suicide attempt, we first calculated absolute risk reduction, relative risk reduction, and number needed to treat (NNT). We then conducted survival analyses with Kaplan-Meier method and log-rank test. To test for differences in the total number of suicide attempts, and because our outcomes were overly dispersed, we conducted negative binomial regression.
These primary analyses were followed by several additional analyses. First, because our study was a sequential design, we were aware of the potential for patient-level confounding across study phases. Therefore, consistent with our a priori data analytic plans, to control for potential differences between study phases, we created both Cox proportional hazards and negative binomial models adjusting for potential confounders that were selected based on clinical knowledge and demonstrated predictive relationship with suicide outcomes as well as dummy variables for participating site (Table 1). We detected no violation of the proportionality of hazards assumption using log cumulative hazards plots, Schoenfeld residual plots, and time-dependent variables.
Table 1. Characteristics of the Participants at Baseline by Study Phase.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Phase 1: Treatment as Usual (n = 497) | Phase 2: Universal Screening (n = 377) | Phase 3: Universal Screening Plus Intervention (n = 502) | |
| Demographic information | |||
| Age, median (IQR), ya | 37 (26-46) | 36 (28-48) | 36 (24-47) |
| Femalea | 278 (55.9) | 210 (55.7) | 281 (56.0) |
| Race/ethnicity | |||
| Non-Hispanic white | 340 (68.4) | 242 (64.2) | 346 (68.9) |
| Non-Hispanic black | 72 (14.5) | 60 (15.9) | 73 (14.5) |
| Hispanic | 63 (12.7) | 50 (13.3) | 58 (11.6) |
| Other | 22 (4.4) | 25 (6.6) | 25 (5.0) |
| Not married | 407 (81.9) | 295 (78.3) | 415 (82.7) |
| Lives alonea,b | 151 (30.4) | 86 (22.8) | 124 (24.7) |
| Served in the militarya | 38 (7.7) | 20 (5.3) | 27 (5.4) |
| Education (≤high school) | 251 (50.5) | 192 (50.9) | 260 (51.8) |
| Unemployed | 304 (61.2) | 247 (65.5) | 289 (57.6) |
| Coexisting medical disordera | 350 (70.4) | 274 (72.7) | 328 (65.3) |
| Heart disease | 29 (5.8) | 29 (7.7) | 33 (6.6) |
| Cancer | 10 (2.0) | 12 (3.2) | 19 (3.8) |
| HIV infection | 10 (2.0) | 7 (1.9) | 8 (1.6) |
| Diabetes | 58 (11.7) | 40 (10.6) | 60 (12.0) |
| Stroke | 3 (0.6) | 5 (1.3) | 11 (2.2) |
| Chronic pain | 130 (26.2) | 261 (69.2) | 307 (61.2) |
| Coexisting psychiatric disordera | 432 (86.9) | 334 (88.6) | 436 (86.9) |
| Depression | 409 (82.3) | 315 (83.6) | 406 (80.9) |
| Bipolar disorder | 202 (40.6) | 175 (46.4) | 194 (38.6) |
| Anxiety | 296 (59.6) | 236 (62.6) | 285 (56.8) |
| Schizophreniab | 62 (12.5) | 38 (10.1) | 49 (9.8) |
| Lifetime suicide-related historya | |||
| Suicide attempt | 351 (70.6) | 268 (71.1) | 368 (73.3) |
| Aborted attempt | 296 (59.6) | 241 (63.9) | 301 (60.0) |
| Interrupted attemptb | 272 (54.7) | 238 (63.1) | 285 (56.8) |
| Nonsuicidal self-injury | 222 (44.7) | 186 (49.3) | 230 (45.8) |
| Severity of suicide ideation (C-SSRS), median (IQR)a | 0 (0-5) | 2 (0-5) | 0 (0-5) |
| Health care use | |||
| ED visit for psychiatric problems within the past 6 moa | 168 (33.8) | 125 (33.2) | 150 (29.9) |
| Hospitalization for psychiatric problems within past 6 moa | 110 (22.1) | 88 (23.3) | 110 (21.9) |
| Suicide attempt within past wka | 183 (36.8) | 114 (30.2) | 162 (32.3) |
| Substance use | |||
| Current alcohol misusea | 181 (36.4) | 117 (31.0) | 173 (34.5) |
| Current drug usea | 245 (49.3) | 182 (48.3) | 237 (47.2) |
| Psychological distress (GSI score), median (IQR)a | 14 (9-18) | 15 (10-19) | 14 (8-18) |
| Quality of life (SF-6D score), median (IQR)a | 17 (15-18) | 16 (15-18) | 17 (15-18) |
Abbreviations: C-SSRS, Columbia Suicide Severity Rating Scale; ED emergency department; GSI, Global Severity Index; HIV, human immunodeficiency virus; IQR, interquartile range; SF-6D, Short Form 6D Health Survey.
Variable included in covariate analyses.
P < .05.
We also conducted a pair of additional analyses to examine secular effects, including seasonality and site experience with the intervention. In the first, we controlled for calendar month to address possible seasonality effects. In another, we adjusted for the effect of the relative length of time a site was engaged in a particular study phase (ranging from −0.5 for the first patient in a given phase to +0.5 for the last patient in a phase) to control for effects of experience and comfort with the study procedures. All analyses were performed with SAS version 9.4 (SAS Institute) or STATA version 14.1 (StataCorp). All P values were 2-tailed, with P < .05 considered statistically significant.
Results
Participant Characteristics
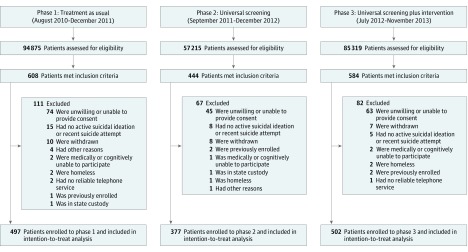
Of 1636 patients who met the study inclusion criteria, we enrolled 1376 participants, including 497 in the TAU phase, 377 in the screening phase, and 502 in the intervention phase (Figure 1). The median (IQR) age was 37 (26-47) years; 769 (55.9%) were female and 928 (67.4%) were non-Hispanic white. A total of 987 (71.7%) of the sample had a history of suicide attempts, and 459 (33.4%) had made an attempt in the week prior to ED visit; 1202 (87.4%) had a psychiatric disorder and 952 (69.2%) also had a coexisting medical disorder. See Table 1 for other demographic and clinical characteristics. Of 1376 enrolled participants, 1089 patients (79.1%) had at least 1 completed telephone interview through 52 weeks; medical record reviews were completed on all participants.
Figure 1. CONSORT Diagram.
Interventions
Secondary Suicide Screening
Medical record review indicated that 449 of 502 participants (89.4%) had received a suicide risk assessment from their physician, but only 17 (3.9%) had documentation of the ED-SAFE standardized secondary screening was used.
Safety Plan
Among those participants who completed the initial CLASP call, 114 (37.4%) reported having received a written safety plan in the ED.
CLASP
Among 502 participants in the intervention phase, 305 participants (60.8%) completed at least 1 CLASP telephone call. Of those participants who completed at least 1 call, the median (IQR) number of completed calls was 6 (2-7). One hundred participants (19.9%) had an SO who completed at least 1 call. Significant others completed a median (IQR) of 4 (3-4) calls.
Outcomes
Suicide Attempts
Overall, of 1376 participants, 288 (20.9%) made at least 1 suicide attempt during the 12-month period. In the TAU phase, 114 of 497 participants (22.9%) made a suicide attempt, compared with 81 of 377 participants (21.5%) in the screening phase and 92 of 502 participants (18.3%) in the intervention phase. Five attempts were fatal, with fatalities observed in the TAU phase (n = 2) and intervention phase (n = 3).
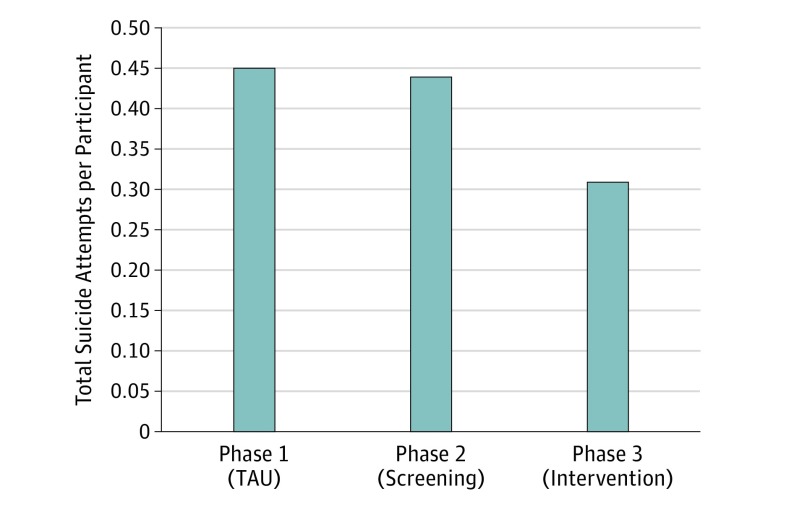
Of participants who reported an attempt, 164 (56.9%) made 1 attempt during the follow-up period, 53 (18.4%) made 2 attempts, and 67 (23.3%) made 3 or more. When combined, there were 548 total suicide attempts among participants, including 224 in the TAU phase (0.45 per participant), 167 in the screening phase (0.44 per participant), and 157 in the intervention phase (0.31 per participant).
Primary Analyses
There were no meaningful differences in risk reduction between the TAU and screening phases (Table 2). In contrast, compared with the TAU phase, participants in the intervention phase showed small but meaningful reductions in suicide risk (Table 2), with a relative risk reduction of 20% and NNT of 22. Participants in the intervention phase had 30% fewer total suicide attempts than participants in the TAU or screening phases (Figure 2).
Table 2. Risk Reduction.
| Suicidal Behavior | Proportions | Absolute Risk Reduction (95% CI) | Relative Risk (95% CI) | Relative Risk Reduction (95% CI) | NNT |
|---|---|---|---|---|---|
| TAU vs SO | |||||
| Suicide attempts | TAU, 22.9% (114/497); SO, 21.5% (81/377) | 0.15 (−0.04 to 0.07) | 0.94 (0.73 to 1.20) | −0.06 (−0.20 to 0.27) | 69 |
| Suicide composite | TAU, 48.9% (243/497); SO, 49.6% (187/377) | 0.07 (−0.06 to 0.07) | 0.99 (0.89 to 1.17) | −0.01 (−0.16 to 1.10) | 141 |
| TAU vs INT | |||||
| Suicide attempts | TAU, 22.9% (114/497); INT, 18.3% (92/502) | 0.05 (0 to 0.10) | 0.80 (0.63 to 1.02) | 0.20 (0.02 to 0.38) | 22 |
| Suicide composite | TAU, 48.9% (243/497); INT, 41.4% (208/502) | 0.08 (0.01 to 0.14) | 0.85 (0.74 to 0.97) | 0.15 (0.03 to 0.26) | 13 |
Abbreviations: INT, intervention; NNT, number needed to treat; SO, screening only; TAU, treatment as usual.
Figure 2. Total Suicide Attempts per Participant by Phase.
TAU indicates treatment as usual.
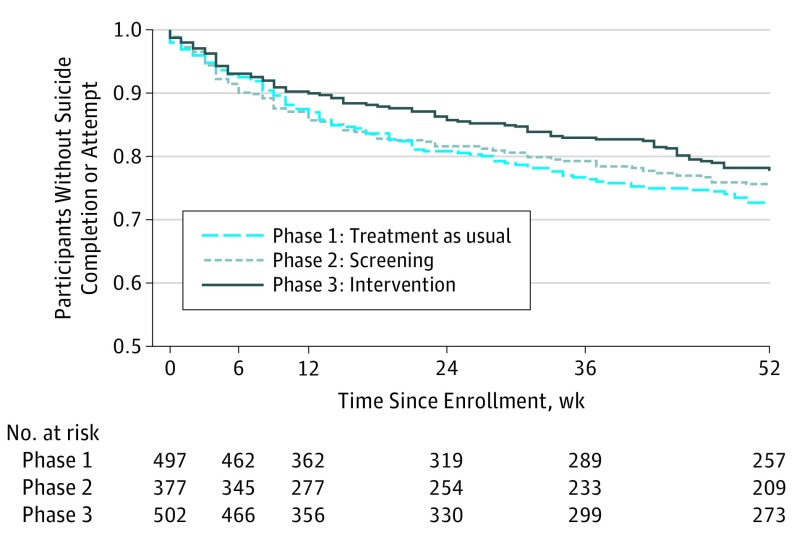
The survival curves for suicide attempts can be seen in Figure 3. Log-rank tests indicated no significant differences between the TAU and screening phases. Comparisons of TAU and Intervention were associated with a P value of .08. Negative binomial regression analysis indicated that the participants in the intervention phase had significantly fewer total suicide attempts than participants in the TAU phase (incidence rate ratio [IRR], 0.72; 95% CI, 0.52-1.00; P = .05) but no differences between the TAU and screening phases (IRR, 1.00; 95% CI, 0.71-1.41; P = .99). There were no significant site effects or site-by-treatment interactions.
Figure 3. Proportion of Participants Who Did Not Make a Suicide Attempt Over Time.
The screening phase (phase 2) vs the treatment as usual phase (phase 1): P = .56 by log-rank test. The intervention phase (phase 3) vs the treatment as usual phase (phase 1): P = .08 by log-rank test.
Secondary Analyses
Results from the multivariable Cox proportional hazards model indicated that compared with participants in the TAU phase, those in the screening phase had no significant difference in the proportion of participants making suicide attempts (eTable 2 in the Supplement). However, compared with participants in the TAU phase, participants in the intervention phase had a significant reduction in risk of suicide attempts (hazard ratio, 0.73; 95% CI, 0.55-0.97; P = .03). Multivariable negative binomial regression analysis also indicated that participants in the intervention phase had fewer total suicide attempts than those in the TAU phase (IRR, 0.75; 95% CI, 0.57-0.98; P = .04) (eTable 3 in the Supplement).
There were no significant effects for either of the secular trend analyses (both P > .05). Adding calendar month to the Cox models did not yield significant seasonal effects nor change the results of these models. Similarly, there was no evidence of trends within each phase (eTables 4 and 5 in the Supplement).
Suicide Composite
There were 637 participants (46.3%) who had 1 or more of the behaviors comprising the suicide composite. In the TAU phase, 243 participants (48.9%) had a suicide composite outcome, compared with 187 (49.6%) in the screening phase and 208 (41.4%) in the intervention phase. Results of analyses of the suicide composite largely mirrored those of the suicide attempt variable. We found no significant differences in the suicide composite between TAU and screening phases. By contrast, survival (Z = −2.17; P = .03), multivariate Cox (hazard ratio, 0.78; 95% CI, 0.64-0.94; P = .01), and negative binomial (IRR, 0.78; 95% CI, 0.65-0.93; P = .01) analyses indicated participants in the intervention phase had significantly lower risk of overall suicidal behavior than those in the TAU phase (eFigure and eTables 6 and 7 in the Supplement).
Discussion
To our knowledge, this study is the largest suicide intervention trial ever conducted in the United States. More than 1300 participants with significant suicide risk from 8 EDs received either TAU, universal screening, or universal screening plus an intervention consisting of an expanded suicide screening and provision of a self-administered safety plan in the ED followed by a telephone-based intervention delivered over 52 weeks. The results indicated that the provision of universal screening, while successful in identifying more participants, did not significantly affect subsequent suicidal behavior compared with that experienced by participants in the TAU phase. By contrast, those participants who received the intervention had lower rates of suicide attempts and behaviors and fewer total suicide attempts over a 52-week period. These results are consistent with other studies demonstrating the utility of contact following discharge from EDs.
The NNT to prevent future suicidal behavior ranged between 13 and 22. This level of risk reduction compares favorably with other interventions to prevent major health issues, including statins to prevent heart attack (NNT = 104), antiplatelet therapy for acute ischemic stroke (NNT = 143), and vaccines to prevent influenza in elderly individuals (NNT = 20).
Because our intervention phase had 3 components, we cannot identify their respective contributions to the observed reduction in suicidal behavior. Indeed, the implementation/compliance with all components of the intervention was less than optimal, with some participants not receiving portions of the intervention, either due to lack of implementation (standardized secondary screening and safety plan) or patient noncompliance (CLASP calls). In this report, we used conservative intent-to-treat analyses that included all participants regardless of their compliance. However, it should be noted that all participants in the intervention phase received substantial outreach via telephone messages and letters from CLASP advisors. It is possible that these nonspecific expressions of concern and caring may have had a beneficial effect in the absence of completed telephone calls.
Although the procedures of this study did improve suicide risk detection rates, we found no evidence that universal screening alone improved outcomes after the ED visit. However, the patients recruited for inclusion in the longitudinal follow-up of this study had all been identified clinically as having suicide risk and represent only a small subset of actual screen-positive patients among the entire ED population. Potential advantages of universal screening may be seen with larger, population-based studies.
We also note that for research and ethical reasons, participants in all phases, including the TAU phase, received assessment calls to assess suicide risk, followed by potential referral to a suicide hotline. It is possible that these safety procedures decreased subsequent suicidal behavior across all phases. We believe that this insurmountable challenge of suicide prevention research may have reduced the potential differences between the TAU and intervention phases.
Limitations
Our study has several limitations. First, we used a sequential design instead of a randomized clinical trial. While our design allowed investigation of system-based interventions that would have been impossible with a traditional randomized clinical trial, it is possible that time or other nonstudy systemic changes may have produced differences in participant samples or other unknown factors across phases. While we controlled statistically for potential differences in samples and time by using multiple covariates and analyses of seasonality and experience with study procedures (eTables 1, 2, and 3 in the Supplement), other factors may have influenced outcomes. However, there were no major changes in treatment of suicidal individuals during the time of our study, both at the sites and nationwide, and national suicide rates remained constant or even increased over the study period. Second, consistent with virtually every other suicide intervention trial, we did not have sufficient power to detect differences in actual deaths by suicide. While suicide attempts are an important public health issue, much larger trials will be necessary to adequately study the effect of interventions on suicide deaths.
Conclusions
In this multicenter study of ED patients with elevated suicide risk, we found that a multifaceted intervention (composed of brief in-ED interventions and a series of telephone calls after ED discharge) produced a small but meaningful reduction (5%) in the proportion of participants who attempted suicide over the 12-month observation period. Moreover, the intervention led to a 30% reduction in the overall number of suicide attempts.
eTable 1. Timing of CLASP-ED telephone contacts.
eTable 2. Cox proportional hazards model for the suicide attempts.
eTable 3. Negative binomial regression model for suicide attempts as a count variable.
eTable 4. Cox proportional hazards model for the suicide attempts including calendar month.
eTable 5. Cox proportional hazards model for the effect of time on suicide attempts within each study phase.
eTable 6. Cox proportional hazards model for the suicide composite.
eTable 7. Negative binomial regression model for the suicide composite as a count variable.
eFigure. Proportion of participants who remained suicide composite–free over time.
References
- 1.Drapeau CW, McIntosh JL; American Association of Suicidology USA suicide: 2015 official final data. http://www.floridasuicideprevention.org/PDF/2015%20US%20Suicide%20Official%20Final%20Data%20AAS.pdf. Accessed February 20, 2017.
- 2.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570. [DOI] [PubMed] [Google Scholar]
- 3.Linehan MM, Comtois KA, Murray AM, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757-766. [DOI] [PubMed] [Google Scholar]
- 4.Rudd MD, Bryan CJ, Wertenberger EG, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172(5):441-449. [DOI] [PubMed] [Google Scholar]
- 5.Tarrier N, Taylor K, Gooding P. Cognitive-behavioral interventions to reduce suicide behavior: a systematic review and meta-analysis. Behav Modif. 2008;32(1):77-108. [DOI] [PubMed] [Google Scholar]
- 6.Milner AJ, Carter G, Pirkis J, Robinson J, Spittal MJ. Letters, green cards, telephone calls and postcards: systematic and meta-analytic review of brief contact interventions for reducing self-harm, suicide attempts and suicide. Br J Psychiatry. 2015;206(3):184-190. [DOI] [PubMed] [Google Scholar]
- 7.Owens P, Mutter R, Stocks C Mental health and substance abuse-related emergency department visits among adults, 2007: statistical brief #92. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2010. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb92.pdf. Accessed February 20, 2017. [PubMed] [Google Scholar]
- 8.Ting SA, Sullivan AF, Boudreaux ED, Miller I, Camargo CA Jr. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. Gen Hosp Psychiatry. 2012;34(5):557-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olfson M, Marcus SC, Bridge JA. Focusing suicide prevention on periods of high risk. JAMA. 2014;311(11):1107-1108. [DOI] [PubMed] [Google Scholar]
- 10.Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry. 2003;183:28-33. [DOI] [PubMed] [Google Scholar]
- 12.Da Cruz D, Pearson A, Saini P, et al. Emergency department contact prior to suicide in mental health patients. Emerg Med J. 2011;28(6):467-471. [DOI] [PubMed] [Google Scholar]
- 13.Boudreaux ED, Miller I, Goldstein AB, et al. The Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE): method and design considerations. Contemp Clin Trials. 2013;36(1):14-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boudreaux ED, Camargo CA Jr, Arias SA, et al. Improving suicide risk screening and detection in the emergency department. Am J Prev Med. 2016;50(4):445-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arias SA, Sullivan AF, Miller I, Camargo CA Jr, Boudreaux ED. Implementation and use of a crisis hotline during the treatment as usual and universal screening phases of a suicide intervention study. Contemp Clin Trials. 2015;45(pt B):147-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller IW, Gaudiano BA, Weinstock LM. The Coping Long Term with Active Suicide Program: description and pilot data. Suicide Life Threat Behav. 2016;46(6):752-761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawton K, Townsend E, Arensman E, et al. Psychosocial versus pharmacological treatments for deliberate self harm. Cochrane Database Syst Rev. 2000;(2):CD001764. [DOI] [PubMed] [Google Scholar]
- 19.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm: systematic review. Br J Psychiatry. 2002;181:193-199. [DOI] [PubMed] [Google Scholar]
- 20.Hess KR. Graphical methods for assessing violations of the proportional hazards assumption in Cox regression. Stat Med. 1995;14(15):1707-1723. [DOI] [PubMed] [Google Scholar]
- 21.Fleischmann A, Bertolote JM, Wasserman D, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ. 2008;86(9):703-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vaiva G, Vaiva G, Ducrocq F, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ. 2006;332(7552):1241-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ray KK, Seshasai SR, Erqou S, et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170(12):1024-1031. [DOI] [PubMed] [Google Scholar]
- 24.Sandercock PA, Counsell C, Gubitz GJ, Tseng MC. Antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev. 2008;(3):CD000029. [DOI] [PubMed] [Google Scholar]
- 25.Demicheli V, Rivetti D, Deeks JJ, Jefferson TO. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev. 2000;(2):CD001269. [DOI] [PubMed] [Google Scholar]
- 26.Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge: 24-month outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry. 2007;191:548-553. [DOI] [PubMed] [Google Scholar]
- 27.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828-833. [DOI] [PubMed] [Google Scholar]
- 28.Wortzel HS, Gutierrez PM, Homaifar BY, Breshears RE, Harwood JE. Surrogate endpoints in suicide research. Suicide Life Threat Behav. 2010;40(5):500-505. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Timing of CLASP-ED telephone contacts.
eTable 2. Cox proportional hazards model for the suicide attempts.
eTable 3. Negative binomial regression model for suicide attempts as a count variable.
eTable 4. Cox proportional hazards model for the suicide attempts including calendar month.
eTable 5. Cox proportional hazards model for the effect of time on suicide attempts within each study phase.
eTable 6. Cox proportional hazards model for the suicide composite.
eTable 7. Negative binomial regression model for the suicide composite as a count variable.
eFigure. Proportion of participants who remained suicide composite–free over time.