Abstract
Ageing is associated with the deterioration of all cognitive functions, including attention, memory and psychomotor speed. It has not yet been clearly confirmed whether the effects of cognitive and physical interventions can improve activities of daily living (ADL). This study compared the effectiveness of cognitive and physical training on cognitive functions and the transfer to ADL. Eighty older people with mild cognitive impairment (mean age 67.07 ± 4.3 years) were randomly divided into an experimental group (n = 40) and a control group (n = 40). Data were collected in an outpatient psychiatric clinic in a randomised controlled trial. Primary outcome measures included the following: cognitive functions were evaluated using the mini mental state examination, the AVLT—Auditory verbal learning test, the Stroop test, the TMT—trail making test, the DRT—disjunctive reaction time and the NHPT—nine hole peg test. Secondary outcome measure was the Bristol activities of daily living scale. The experimental group underwent a CogniPlus and physical training; consisting of 20 training sessions over 10 weeks. Both groups went through 30 min of daily physical training for 10 weeks. After the training, significant differences in favour of the experimental group were found in almost all the tests. In memory (AVLT) (p ≤ 0.0001, effect size (ES) η 2 = 0.218. In reduction of the response time on attention tasks (Stroop tasks) (p ≤ 0.006, ES = 0.092–0.115). In lower error rates in all tests: Stroop tasks, DRT, TMT, NHPT (p ≤ 0.02–0.001, ES = 0.062–0.176). In ADL (p ≤ 0.0001, ES = 0.176). The combined cognitive and physical training had better efficacy for most cognitive functions and for ADL when compared with the physical training only.
Keywords: Attention, Memory, Activities of daily living
Introduction
Ageing is associated with the deterioration of all cognitive functions, including attention, memory and psychomotor speed, thus resulting in mental slowing down. The ability to concentrate and quickly respond to stimuli deteriorates with age. The largest share in the reduction of response speed is observed in the central processes associated with processing a stimulus and deciding on the response (Reinvang et al. 2012). Reaction time also increases with age. The overall psychomotor tempo, as well as perceptual—motoric functional coordination, experiences a slow-down because the nerve fibres transmit impulses more slowly (Chang et al. 2012). Attention is the basis for all cognitive functions. Dual-tasking, the ability to simultaneously perform more than just one activity, is significantly reduced among older people with mild cognitive impairment (MCI). However, it is necessary for carrying out many activities of daily life. There are various ways of improving dual-tasking in older people (Seçer and Satyen 2013).
The training of mental activity—learning new things—is associated with better brain function and reduced risk of cognitive decline and dementia, as has been confirmed by the following studies (Bahar-Fuchs et al. 2013; Kueider et al. 2012). The methods used for training cognitive functions have had positive effects on cognitive, visual-spatial abilities and psychomotor speed among older people (Clare and Woods 2004). Additionally, interventions to stimulate cognitive functions may be employed by various types of physical training (Lautenschlager et al. 2010). It is known that physical exercise (physical fitness training or various forms of physical activities) may improve the ability to learn and memorise. Uemura et al. (2013) and Brown et al. (2013) found significant improvements in cognitive function after physical training in older people with mild cognitive impairment.
However, the results from combination of cognitive and physical training studies have suggested that, despite performance improvements in trained tasks, the transfer effects into activities of daily life appear to be very limited in older people (Bherer 2015). In addition, systematic reviews recommend examining these transfer effects (Green and Bavelier 2012; Reijnders et al. 2013). Due to the lack of evidence regarding the transfer of the abilities and skills gained from cognitive and physical training sessions to ADL, we sought to investigate whether training in carefully selected combination of cognitive and physical exercises may improve the transfer of gained skills to ADL.
The aim of this study was to investigate whether cognitive training combined with physical-balance training not only improves basic cognitive functions, memory, attention, psychomotor speed and visual-motoric coordination as primary outcome measures, but also improves activities of daily living as secondary outcome measure more than physical-balance training alone in older people with mild cognitive impairment.
Methods
Sample and procedure
The study was performed in the Outpatient Psychiatric Clinic of the Highly Specialized Geriatric Institute of St. Lukas in Kosice, Slovak Republic, where older adults from the whole region are referred for diagnosis and treatment. One hundred patients were invited to participate by telephone interview in the study, which was conducted between June 2013 and March 2014. The sample consisted of patients who had mild cognitive impairment confirmed by their psychiatrist and psychologist based on standard clinical examination, in line with the criteria defined by ICD-9-CM 331.83.
To be included, participants had to have mild cognitive impairment with the presence of a subjective mild decrease in memory and attention and had to be over the age of 65. Participants were excluded if they had moderate or severe cognitive deficits (MMSE ≤23), major depressive or anxiety disorders (5 participants), cancer, significant visual or auditory damage, neurological diseases or brain injury or psychiatric disorders.
Out of 100 patients, five were excluded due to symptoms of major depressive and anxiety disorders. Fifteen patients refused to participate during the baseline examination. They were not able complete the initial testing. Eighty patients were enrolled in the study by one member of the research team not involved in the assessment or interventions. The baseline sample thus consisted of 80 participants who were randomly divided into two groups with a 1:1 allocation. The project data analyst generated a random sequence of numbers for random selection for the experimental group and the control group using the computer programme Microsoft Office Excel 2010. These numbers were placed in a sealed envelope. The project manager opened the envelope and informed the participating persons upon assignment to one of the two groups.
Data were collected in an outpatient psychiatric clinic. Data collection consisted of two measurements: baseline and a follow-up after 10 weeks of training sessions. The participants were informed about their division into two groups, but they were not given any detailed information about the differences between the interventions they would undergo or the expected results. The only information given was that the trainings are similar.
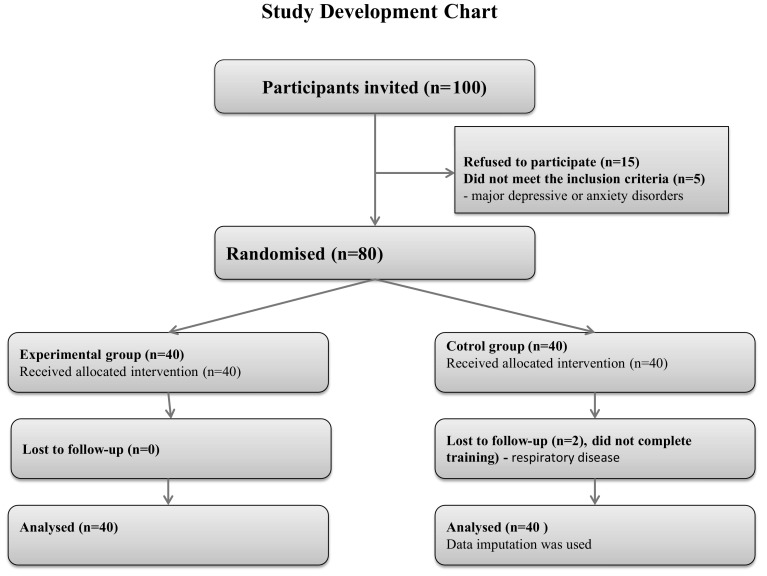
The training staffs were not blinded, but assessors were blinded to the intervention. In the experimental group, all of the included persons completed the programme. In the control group, two individuals did not complete the training programme due to respiratory disease. They developed acute symptoms in the middle of the running programme and they were unable to finish the programme. All of those included signed an informed consent form. The study was approved by the local ethics committee of the Highly Specialized Geriatric Institute of St. Lukas in Kosice, Slovakia. The research protocol and study approval documents (No. 1/2013) are available in Slovak language and can be obtained upon request from the local ethics committee (Fig. 1).
Fig. 1.
Study development chart
Interventions
Both groups—the control and intervention groups—received physical training as a foundation to which CogniPlus was added in the experimental group.
Physical training
The frequency was 30 min daily lasting for 10 weeks. Our programme contained the following elements of exercise:
Walking over obstacles, 5 min: participants walked over 5 boxes and then they turned and walked back. First they walked slowly, and then they sped up their walking. During the walk, they had to avoid hitting the box and they had to maintain balance.
Walking with a directional change, 6 min: walk with a directional change (right, left, for 2 min, turning 360°, walk backwards for 2 min), walk with a speed change (speeding up, slowing down for 2 min).
Change of walking base, 6 min: change of walking base, that is, stride-width change (for 2 min), walking with a change in step length and stride length change (5 long, 5 short steps, for 2 min), tandem walk (for 2 min).
Speed walking, 3 min.
Walking with a load, 5 min: they walked while carrying a load in one hand and then in both hands.
Walking up and down the stairs, 5 min: participants walked up and down stairs (ten steps).
The objective was to strengthen leg muscles and maintain balance (NICE 2011; Patla 2003).
Cognitive training
CogniPlus and physical training
For the experimental group, the cognitive training battery CogniPlus, developed by the company Schuhfried GmbH, Austria, was used. The training sub-programmes were designed for patients with mild cognitive impairment. CogniPlus is a training programme with a scientific background. The training programme is listed with recommendation ‘strength A’ in the guidelines of the Society for Neuropsychology (Gesellschaft für Neuropsychologie—GNP 2009).
We used the sub-programmes:
Alert—for increasing attention intensity. The training was performed by means of driving a virtual car (18 difficulty levels).
Nback—working memory, newly obtained information and its continuous update. Probands were shown pictures of animals, people, country, etc. and they had to remember 2–3 pictures previously presented (15 difficulty levels).
Names—long-term memory, effective strategies for learning and remembering names of people in connection with their faces (17 difficulty levels).
Pland—3 forms for training of executive functions and planning of daily activities. Probands had to solve various tasks with little time and overlapping tasks (16–28 difficulty levels).
Vismo—training of visual-motor abilities. Probands followed a spaceship on the screen and they had to keep it inside a circle (22 difficulty levels).
The aim of the training was to gradually achieve the maximum level of performance in different types of training. At the start of treatment, the lowest level of training intensity was adjusted and was automatically increased or decreased according to individual abilities of the seniors.
The exercises in Alert, Names and Pland 1 and 2 were quickly mastered up to the maximum level of difficulty, so it was possible to combine them with motor exercises into a dual task. The training involved with sub-programmes Nback, Vismo and Pland 3 was not possible to combine with any physical exercise, because all attention had to be concentrated on the tasks.
Probands in the experimental group performed the following exercises:
Alert (both forms)—while driving a virtual car, probands were standing and changing their position from the left foot to the right foot and standing on their toes.
Names—while learning names, the probands were repeatedly standing up from their chair and then sitting down on their chairs.
Pland (Form 1 and 2)—while planning their virtual daily activities, like shopping, doctor visits and social life according to a priority timetable, the participants were alternately taking steps forward and backward, to the left and to the right.
Participants completed 20 training sessions, two sessions during each week. Each training session lasted 30 min. Each type of cognitive sub-programme lasted for 5–10 min during a single session. During one session, only attention, short-term and long-term memory were trained; then at the following session, the executive functions and visual-motoric coordination were trained. All of the cognitive functions were trained during each week.
Both groups underwent 30 min of daily physical training with balance components.
Outcome measures
Primary outcome measures: cognitive and psychomotor abilities
Mini mental state examination (MMSE)—an examination of basic cognitive functions. This is a valid and reliable 30-point questionnaire that is used in clinical and research settings to measure cognitive impairment. A MMSE ≤23 was used to indicate cognitive impairment (Folstein et al. 1975).
Auditory verbal learning test (AVLT) (McMinn et al. 1988; Preiss 1994)—this uses 15 words repeated five times, followed by the interference of another set of 15 words. Word recognition of words from the first set was assessed after 30 min. We separately considered each of 5 attempts and then all together. At follow-up examination, a set of another 15 words was used. We evaluated the number of remembered words in the first attempt, word recognition, and the total number of words (1–5 attempts).
Stroop test (Stroop 1935; Daniel 1983)—assesses psychomotor and personal speed. The Stroop test was presented with a list of 100 words (black and colour) and a list of 100 colours. The time in seconds and the total number of errors in naming the colours and words were evaluated. The shorter the time, the better the performance.
(Words)—the category assesses personal tempo. In this task, participants have to name the words in black colour as quickly as possible.
(Colours)—the category assesses the perception factor. In this task, participants have to name different colours as quickly as possible.
(Colours, words)—the category assesses the perception load score. In this task, participants have to name words in different colours as quickly as possible.
(Colour, words, colours)—the category assesses the increased load score. In this task, participants have to name the different colours of a word that spells a colour name as quickly as possible. When the colour and the word are congruent (e.g. the word ‘red’ in red letters), the task is easy. However, when the colour and the word are incongruent (e.g. the word ‘blue’ in red letters), the subjects experience interference.
Trail making test (TMT), Form A (Reitan and Wolfson 1985; Bezdicek et al. 2012)—tests attention, psychomotor speed and visual search capability. Version A contains 25 numerals. The patient tries to combine numerals from one to two up to numeral 25 as quickly as possible. The time in seconds and the number of errors are rated.
Disjunctive reaction time (DRT-II) (Vonkomer 1992)—the outcome provides an overview of mental speed, concentration of attention and space orientation. Participants filled in a reflecting picture of 2 circular formations into a marked space within a standard time of 1 min. We evaluated the number of correct and incorrect pictures.
Nine hole peg test (NHPT) (Mathiowetz et al. 1985)—measures psychomotor coordination and fine motor movements of the dominant hand, i.e. hand–eye coordination. Assessment concerned the time in seconds and the number of errors when inserting pins into holes.
Secondary outcome measures: activities of daily living
Bristol activities of daily living scale (BADLS) (Bucks et al. 1996)—is a carer-rated scale that comprises 20 questions designed to measure the ability to perform everyday activities in people with mild to advanced dementia. It evaluates the ability to prepare meals and drink, dressing, hygiene, toilet, mobility, orientation, communication, house work, shopping and social life. Each item is scored between zero and three. The lower the score, the better the result. A total score of 0 shows independence in all activities; the proband is self-sufficient. The maximum score is 60 and means that the proband is not at all self-sufficient. The BADLS has been shown to be valid, reliable and responsive to change over time (Bucks et al. 1996, Bartos et al. 2010).
Sociodemographic, clinical and descriptive data
Baseline sociodemographic and clinical data were obtained from patient records. Age was treated as a continuous variable. The highest level of education completed was coded as primary (elementary completed or not completed), secondary (vocational education or general secondary education) or tertiary (college or university education). For descriptive purposes, but not in analyses, we used the test of intellectual potential (TIP), Form A, a non-verbal test of the intellect. It contains 29 test tasks with increasing levels of difficulty (Rican 1971).
Statistical analyses
The primary analysis was based on the intention-to-treat principle. In order to analyse the data, descriptive and inferential statistics were used. Independent t-tests for continuous variables and Chi square tests for categorical variables were used to compare the experimental and control groups at baseline.
The differences between the control and the experimental groups at the time before (Time 1—baseline) and 10 weeks after the intervention (Time 2—follow-up) were evaluated by using the general linear model (GLM)—repeated measures with Greenhouse-Geisser correction. The GLM–repeated measures (alternative names: Split-plot ANOVA or mixed design ANOVA) is a statistical test specifically designed to deal with multiple comparisons, in particular with a set of repeated measures. In our study, we are comparing only 2 groups (intervention and control) and therefore, in this case, the standard post hoc tests for multiple comparisons (such as Bonferroni or Scheffe) do not need to be performed. Instead, what needs to be tested is the violation of sphericity. Thus, we had to correct for sphericity, which can carried out by Greenhouse-Geisser correction or the Huynh and Feldt correction.
According to Cohen’s (1988) specifications for ANOVA analyses, effect size (ES) is reported as the Partial Eta Squared (η 2) − η 2: 0.00–0.003: no effect; η 2: 0.010–0.039: small effect; η 2: 0.060–0.110: medium effect; η 2: 0.140– 0.200: large effect.
Missing values at follow-up (n = 2) were imputed by the previous observation. Calculations were performed using IBM SPSS 22 for Windows (IBM, Chicago, Illinois, USA). The level of statistical significance was set at p < 0.05.
Results
Descriptive data
The baseline measures of the basic demographic variables—such as age, gender, education as well as intelligence and the duration of mild mental ailments—were similar in both groups. MMSE confirmed mild cognitive impairment (with a mild decrease in memory and attention domains). The mean values of non-verbal intelligence tests (TIP-A) indicated average intelligence. The sociodemographic and clinical characteristics are summarised in Table 1. No significant differences were found between the groups for any outcome measures before the training.
Table 1.
Demographic and baseline characteristics of study participants (n = 80)
| Experimental group n/%; mean ± SD |
Control group n/%; mean ± SD |
t test; chi square test |
p valuea | |
|---|---|---|---|---|
| N | 40 | 40 | ||
| Age | 68.22 ± 6.78 | 65.95 ± 5.68 | 2.021 | 0.108 |
| Gender | ||||
| Males | 22/55.0 | 19/47.5 | 0.450 | 0.502 |
| Females | 18/45.0 | 21/52.5 | ||
| Education | ||||
| Secondary | 30/75.0 | 25/62.5 | 1.455 | 0.228 |
| University | 10/25.0 | 15/37.5 | ||
| Duration of mild mental ailments (months) | 16.98 ± 7.37 | 17.45 ± 6.38 | −0.308 | 0.759 |
| TIP—test of intellectual potential | 16.40 ± 6.22 | 16.88 ± 5.06 | −0.374 | 0.709 |
| Primary outcome measures | ||||
| MMSE—Mini Mental State Examination | 25.98 ± 2.57 | 26.03 ± 1.47 | −0.106 | 0.915 |
| AVLT—auditory verbal learning test—a set | ||||
| 1. trial | 4.15 ± 1.57 | 3.75 ± 1.62 | 1.115 | 0.268 |
| 1. to 5. Trial—sum of words | 32.73 ± 8.60 | 32.58 ± 11.58 | 0.066 | 0.948 |
| Recognition | 4.35 ± 2.92 | 4.30 ± 4.06 | 0.063 | 0.950 |
| Stroop test | ||||
| Words—personal tempo, time (s) | 78.11 ± 27.91 | 69.95 ± 19.43 | 1.518 | 0.133 |
| Colours—perception factor, time (s) | 82.32 ± 26.67 | 72.53 ± 19.47 | 1.874 | 0.065 |
| Words, colours—perception load score, time (s) | 107.50 ± 65.34 | 86.53 ± 49.57 | 1.617 | 0.110 |
| Words, colours, words—increased load score, time (s) | 217.94 ± 56.68 | 204.28 ± 73.48 | 0.930 | 0.355 |
| Errors—number | 6.53 ± 8.29 | 5.00 ± 6.98 | 0.890 | 0.376 |
| Psychomotor tempo | ||||
| DRT(A)—number of correct reactions | 8.85 ± 5.80 | 6.98 ± 4.19 | 1.655 | 0.102 |
| DRT(N)—number of incorrect reactions | 4.98 ± 3.18 | 5.98 ± 3.54 | −1.327 | 0.188 |
| TMT—trail making test A—time (s) | 104.58 ± 24.07 | 92.92 ± 33.56 | 1.785 | 0.078 |
| TMT—trail making test A—errors | 0.65 ± 1.07 | 0.60 ± 0.63 | 0.253 | 0.801 |
| The hand–eye coordination | ||||
| Nine hole peg test—right hand time (s) | 19.83 ± 3.91 | 18.35 ± 3.35 | 1.815 | 0.073 |
| Nine hole peg test—errors | 0.45 ± .78 | 0.30 ± .60 | 0.957 | 0.341 |
| Secondary outcome measures | ||||
| BADLS—activities of daily living | 4.70 ± 5.41 | 5.28 ± 7.19 | −0.404 | 0.687 |
a p values are based on independent t-test for continuous and chi square test for categorical variables
DRT disjunctive reactive time, BADLS Bristol activities of daily living scale
Comparisons of experimental and control groups before and after the training
In the mini mental state examination (MMSE) and auditory verbal learning test (AVLT), significant differences were noted in favour of the experimental group (p < 0.0001). The effect size was large.
In the Stroop attention tasks, significant differences were observed in favour of the experimental group in personal tempo, perception factor (p < 0.002), and the effect size was medium. In number of errors in favour of the experimental group (p < 0.0001), the effect size was large. No significant differences were found between the groups in the assessment of the perception load score and the increased load score.
With regard to psychomotor tempo, the disjunctive reaction time (DRT) showed significant differences, with an increased number of incorrect reactions in the control group (p < 0.005); the effect size was medium. No significant differences in the assessment of number of correct reactions between the groups were found. The trail making test (TMT) Form A showed significant differences in favour of the experimental group (p < 0.01). The effect size was medium.
Visual-motoric coordination, as assessed by the nine hole peg test (NHPT) (performed with dominant hand), also showed significant differences in favour of the experimental group (p < 0.01). The effect size was medium.
In the assessment of ADL by the Bristol activities of daily living scale (BADLS), significant differences were observed in favour of the experimental group (p < 0.0001), and the effect size was large.
There were no adverse events or side effects recorded during or after the training (Table 2).
Table 2.
Mean scores and statistical comparison of interventions groups before and after the training (10 weeks)
| Group | T1—baseline | T2—follow-up | F | p value | Effect size | |||
|---|---|---|---|---|---|---|---|---|
| Estimated marginal means | SD | Estimated marginal means | SD | Partial Eta squared (η 2) | Interpretation | |||
| Primary outcome measures | ||||||||
| MMSE—mini mental state examination | ||||||||
| Experimental | 25.98 | 2.57 | 26.97 | 2.21 | 18.140 | 0.001 | 0.189 | Large |
| Control | 26.03 | 1.47 | 26.02 | 1.44 | ||||
| AVLT—auditory verbal learning test—A set | ||||||||
| 1. trial | ||||||||
| Experimental | 4.15 | 1.57 | 5.30 | 1.88 | 13.072 | 0.001 | 0.144 | Large |
| Control | 3.75 | 1.62 | 3.55 | 1.67 | ||||
| 1.–5. trial—sum of words | ||||||||
| Experimental | 32.73 | 8.60 | 38.70 | 12.60 | 21.782 | 0.0001 | 0.218 | Large |
| Control | 32.57 | 11.58 | 31.33 | 13.65 | ||||
| Recognition | ||||||||
| Experimental | 4.35 | 2.92 | 6.30 | 3.96 | 16.325 | 0.0001 | 0.173 | Large |
| Control | 4.30 | 4.04 | 4.42 | 3.93 | ||||
| Stroop test | ||||||||
| Words—personal tempo, time (s) | ||||||||
| Experimental | 78.11 | 27.91 | 64.16 | 23.05 | 10.146 | 0.002 | 0.115 | Medium |
| Control | 69.95 | 19.43 | 66.03 | 20.10 | ||||
| Colours—perception factor, time (s) | ||||||||
| Experimental | 82.32 | 26.67 | 70.60 | 21.81 | 7.891 | 0.006 | 0.092 | Medium |
| Control | 72.53 | 19.47 | 73.06 | 19.67 | ||||
| Words, colours—perception load score, time (s) | ||||||||
| Experimental | 107.50 | 65.34 | 84.69 | 29.91 | 0.722 | 0.398 | 0.009 | No effect |
| Control | 86.53 | 49.57 | 72.06 | 27.53 | ||||
| Words, colours, words—increased load score, time (s) | ||||||||
| Experimental | 217.94 | 56.68 | 211.66 | 67.00 | 0.002 | 0.966 | 0.000 | No effect |
| Control | 204.28 | 73.48 | 197.62 | 77.48 | ||||
| Errors-number | ||||||||
| Experimental | 6.52 | 8.29 | 2.43 | 5.44 | 16.705 | 0.0001 | 0.176 | Large |
| Control | 5.00 | 6.98 | 6.68 | 8.75 | ||||
| Psychomotor tempo | ||||||||
| DRT(A)—number of correct reactions | ||||||||
| Experimental | 8.85 | 5.80 | 11.75 | 6.36 | 2.669 | 0.106 | 0.033 | No effect |
| Control | 6.98 | 4.19 | 11.57 | 6.82 | ||||
| DRT(N)—number of incorrect reactions | ||||||||
| Experimental | 4.98 | 3.18 | 3.53 | 3.09 | 8.547 | 0.005 | 0.099 | Medium |
| Control | 5.97 | 3.54 | 7.28 | 6.36 | ||||
| TMT—trail making test A—time (s) | ||||||||
| Experimental | 104.58 | 24.07 | 89.98 | 24.70 | 5.803 | 0.018 | 0.069 | Medium |
| Control | 92.92 | 33.56 | 93.47 | 37.66 | ||||
| TMT—trail making test A—errors | ||||||||
| Experimental | 0.65 | 1.07 | 0.25 | 0.74 | 5.186 | 0.026 | 0.062 | Medium |
| Control | 0.60 | 0.63 | 0.85 | 1.05 | ||||
| The hand–eye coordination | ||||||||
| Nine hole peg test—right hand time (s) | ||||||||
| Experimental | 19.83 | 3.91 | 16.87 | 4.18 | 5.889 | 0.018 | 0.070 | Medium |
| Control | 18.35 | 3.35 | 17.69 | 3.38 | ||||
| Nine hole peg test—errors | ||||||||
| Experimental | 0.45 | 0.78 | 0.15 | 0.36 | 6.134 | 0.015 | 0.073 | Medium |
| Control | 0.30 | 0.60 | 0.45 | 0.67 | ||||
| Secondary outcome measures | ||||||||
| BADLS—activities of daily living | ||||||||
| Experimental | 4.70 | 5.41 | 3.93 | 4.79 | 16.636 | 0.001 | 0.176 | Large |
| Control | 5.27 | 7.19 | 5.35 | 7.61 | ||||
T1, T2; time 1—baseline, time 2—after 10 weeks
p values are based on mixed design ANOVA
Effect size (ES) is reported as Partial Eta Squared (η 2). η 2: 0.00–0.003: no effect; η 2: 0.010–0.039: small effect; η 2: 0.060–0.110: medium effect; η 2: 0.140–0.200: large effect (Cohen 1988)
The auditory verbal learning test. 15 words is a maximum number in one trial set
Stroop tasks, trail making test A, nine hole peg test—time in seconds. The shorter the time, the better the performance
Stroop tasks, disjunctive reactive time (DRT), Trail making test A, nine hole peg test—number of errors. The lower the score, the better the result
Disjunctive Reactive Time (DRT)—number of correct reactions. The higher the score, the better the result
BADLS—Bristol activities of daily living scale. The lower the score, the better the functioning
Discussion
The results of this randomised controlled study indicated that cognitive training (CogniPlus) combined with physical training showed significantly greater improvement for basic cognitive functions, memory, attention—especially in lower number of errors in all tests—and visual-motoric coordination compared with physical training alone, as well as better transfer to the performance of activities of daily living (ADL) in older people with mild cognitive impairment. In the assessment of the perception load and increased load scores in the Stroop test and in the number of correct reactions in disjunctive reaction time, there were no significant differences between the groups. Hiyamizu et al. (2011) performed a similar study, in which they also found no significant differences in tests assessing psychomotor speed between two groups of older people after 3 months of strength and balance training with dual tasks and without dual task.
With regard to the assessment of basic cognitive functions (assessed by MMSE) and memory (assessed by AVLT) after the training, significant differences were noted in favour of the experimental group. Our results indicate that physical training alone was not sufficient for improvements. These findings are not consistent with the findings of Uemura et al. (2013) who found that general cognitive functions were improved after physical exercise intervention in subjects with mild cognitive impairment. However, in their study, only the MMSE was used to assess general cognitive function. In a meta-analysis of RCTs, Gates et al. (2013) evaluated the effect of exercise on cognitive functions in older people with mild cognitive impairment. They did not find any significant benefit for additional executive measures, memory or information processing. The results of our study are consistent with these findings.
With regard to attention, in our study, the main significant differences after the training were noted in the number of errors in the Stroop task in favour of the experimental group, due to the application of targeted interventions on attention and executive functions. In the control group, a significantly greater number of errors were observed. The study of Hiyamizu et al. (2011) presented similar results in correct answering rates in the Stroop tasks in healthy seniors after similar interventions. After comparing the results of the study of Hyamizu et al. with our results, it can be stated that physical training in combination with dual tasks may have a positive effect, especially on attention in older people with and without mild cognitive impairment.
After the training, a significant shortening of the response time in the TMT test was also observed in favour of the experimental group and a significantly higher error rate in the control group was observed. The study provides empirical support for the fact that training of executive functions plays a significant role in these improvements.
Significant differences in hand–eye coordination (assessed using the nine hole peg test) were noted in favour of the experimental group. The sub-programme from CogniPlus for training hand–eye coordination, which was very demanding, was shown to have a positive impact on improving visual-motoric coordination.
Next, we attempted to determine the transfer effect to activities of daily living as evaluated by the BADLS. Significant differences were observed in favour of the experimental group, which demonstrate the better transfer to ADL. Reijnders et al. (2013) report in their systematic review that cognitive training can be effective in improving various aspects of objective cognitive functioning, but they recorded only weak improvements in the execution of ADL in healthy older adults and people with mild cognitive impairment. Our findings were only partially congruent with the outcomes of a study by Reijnders et al. (2013). Regarding the transfer of gained skills into ADL, we found that properly chosen cognitive exercises, which are important for the execution of ADL, combined with physical training, produced better results in the transfer of gained skills into daily life, whereas in the mentioned study by Reijnders et al. (2013), only weak improvements in the execution of ADL were observed.
Strengths and limitations, future recommendations
The strengths of this study include the relatively high response rate within our sample (85 %) and the low number lost to follow-up. Limitations of the study include the small sample size. The evaluation of the effect of the training programmes listed, cognitive and physical training, or similar types of interventions should be interpreted with caution. Many older people live an active way of life and try to keep themselves physically and mentally fit and active in their own way, which can also influence the improvements shown in our study. Future recommendations would be to carry out an intervention study over a longer period of time to test the effects of those interventions and their transfer to the specific ADL. Practical implications include cognitive training being added to physical interventions, with the aim of improving cognitive functions and ADL.
Conclusions
The combined cognitive and physical training showed a significantly greater improvement in most of the cognitive functions—memory, attention, psychomotor tempo and hand–eye coordination. The study also demonstrated a better transfer to ADL compared with physical training alone. This therapeutic combination may be effective for a better transfer to improvement of execution of daily living activities in older people with mild cognitive impairment.
Acknowledgments
This work was supported by the Slovak Research and Development Agency under contract No. APVV-0220-10. The authors also wish thank all patients who agreed to participate in this study.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Compliance with ethical standards
Conflict of interests
The authors declare that they have no conflict of interest.
References
- Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database Syst Rev. 2013;6:CD003260. doi: 10.1002/14651858.CD003260.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartos A, Martinek P, Ripova D. Bristolska skala aktivit kazdodenniho zivota (BADLS-CZ) [Bristol Activities of Daily Living Scale—Czech version] Cesk Slov Neurol N. 2010;73:673. [Google Scholar]
- Bezdicek O, Motak L, Axelrod BN, Preiss M, Nikolai T, Vyhnalek M, Ruzicka E. Czech version of the trail making test: normative data and clinical utility. Arch Clin Neuropsychol. 2012;27:906–914. doi: 10.1093/arclin/acs084. [DOI] [PubMed] [Google Scholar]
- Bherer L. Cognitive plasticity in older adults: effects of cognitive training and physical exercise. Ann NY Acad Sci. 2015;1337:1–6. doi: 10.1111/nyas.12682. [DOI] [PubMed] [Google Scholar]
- Brown BM, Peiffer JJ, Martins RN. Multiple effects of physical activity on molecular and cognitive signs of brain aging: can exercise slow neurodegeneration and delay Alzheimer’s disease? Mol Psychiatr. 2013;18:864–874. doi: 10.1038/mp.2012.162. [DOI] [PubMed] [Google Scholar]
- Bucks RS, Ashworth DL, Wilcock GK, Siegfried K. Assessment of activities of daily living in dementia: development of Bristol activities of daily living scale. Age Ageing. 1996;25:113–120. doi: 10.1093/ageing/25.2.113. [DOI] [PubMed] [Google Scholar]
- Chang YK, Pan ChY, Chen FT, Tsai CHL, Huang CHCH. Effect of resistance-exercise training on cognitive function in healthy older adults: a review. J Aging Phys Act. 2012;20:497–517. doi: 10.1123/japa.20.4.497. [DOI] [PubMed] [Google Scholar]
- Clare L, Woods RT. Cognitive training and cognitive rehabilitation for people with early-stage Alzheimer’s disease: a review. Neuropsychol Rehabil. 2004;14(1):385–401. doi: 10.1080/09602010443000074. [DOI] [Google Scholar]
- CogniPlus: Training cognitive functions (2013) http://www.schuhfried.at/fileadmin/content/2_Kataloge_en/CogniPlus_en_Katalog_SCHUHFRIED_3.2.pdf. Accessed 05 May 2016
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Erlbaum; 1988. [Google Scholar]
- Daniel J (1983) Stroopov test (Stroop test). Psychodiagnosticke a didakticke testy n.p. (Psychodiagnostic and didactic tests), Bratislava
- Folstein MF, Folstein SE, Mchugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gates N, Fiatarone Singh MA, Valenzuela M. The effect of exercise training on cognitive function in older adults with mild cognitive impairment: a meta-analysis of randomized controlled trials. Am J Geriat Psychiatr. 2013;21:1086–1097. doi: 10.1016/j.jagp.2013.02.018. [DOI] [PubMed] [Google Scholar]
- Green CS, Bavelier D. Learning, attentional control, and action video games. Curr Biol. 2012;22(6):R197–R206. doi: 10.1016/j.cub.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiyamizu M, Morioka SAK, Shimada T. Effects of dual task balance training on dual task performance in elderly people: a randomized controlled trial. Clin Rehabil. 2011;26:58–67. doi: 10.1177/0269215510394222. [DOI] [PubMed] [Google Scholar]
- Kueider AM, Parisi JM, Gross AL, Rebok GW. Computerized cognitive training with older adults: a systematic review. PLoS One. 2012;7:e40588. doi: 10.1371/journal.pone.0040588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lautenschlager NT, Cox K, Kurz AF. Physical activity and mild cognitive impairment and Alzheimer’s disease. Curr Neurol Neurosci Rep. 2010;10:352–358. doi: 10.1007/s11910-010-0121-7. [DOI] [PubMed] [Google Scholar]
- Mathiowetz V, Weber K, Kashman N, Volland G. Adult norms for the nine hole peg test of finger dexterity. Occup Ther J Res. 1985;5:24–33. doi: 10.5014/ajot.39.6.386. [DOI] [PubMed] [Google Scholar]
- McMinn MR, Wiens AN, Crossen JR. Rey Auditory Verbal Learning Test: developmental norms for healthy young adults. Clin Neuropsychol. 1988;2(1):67–87. doi: 10.1080/13854048808520087. [DOI] [Google Scholar]
- NICE—National Institute for Health and Clinical Excellence, Social Care Institute for Excellence (2011) Dementia: The NICE–SCIE guideline on supporting people with dementia and their careers in health and social care. National Institute for Health and Clinical Excellence website. http://www.scie.org.uk/publications/misc/dementia/dementia-fullguideline.pdf?res=true. Accessed 05 May 2016
- Patla AE. Strategies for dynamic stability during adaptive human locomotion. IEEE Eng Med Biol Mag. 2003;22:48–52. doi: 10.1109/MEMB.2003.1195695. [DOI] [PubMed] [Google Scholar]
- Preiss M. Pametovy test uceni pro klinickou praxi (Memory test learning for clinical practice) Czechoslovak Psychol. 1994;38:257–265. [Google Scholar]
- Reijnders J, van Heugten C, van Boxtel M. Cognitive interventions in healthy older adults and people with mild cognitive impairment: a systematic review. Ageing Res Rev. 2013;12:263–275. doi: 10.1016/j.arr.2012.07.003. [DOI] [PubMed] [Google Scholar]
- Reinvang I, Grambaite R, Espeseth T. Executive dysfunction in MCI: subtype or early symptom. Int J Alzheimers Dis. 2012;936272:1–8. doi: 10.1155/2012/936272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitan RM, Wolfson D (1985) The Halstead—reitan neuropsychological test battery. Neuropsychology Press
- Rican P (1971) Test intelektoveho potencialu (test of intellectual potential). Psychodiagnosticke a Didakticke testy (Psychodiagnostic and didactic tests), Bratislava
- Seçer I, Satyen L. Training skills of divided attention among older adults. J Artic Support Null Hypothesis. 2013;9:62–78. [Google Scholar]
- Stroop J. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–662. doi: 10.1037/h0054651. [DOI] [Google Scholar]
- Uemura K, Shimada H, Makizako H, Doi T, Yoshida D, Tsutsumimoto K, Anan Y, Suzuki T. Cognitive function affects trainability for physical performance in exercise intervention among older adults with mild cognitive impairment. Clin Interv Aging. 2013;8:97–102. doi: 10.2147/CIA.S39434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vonkomer J (1992) DRC—II, Disjunktivny reakcny cas (Disjunctive reaction time) Psychodiagnostika, s.r.o. (Psychodiagnostics), Bratislava