Abstract
Aims
Arginine metabolism via inducible nitric oxide synthase (iNOS) and arginase 2 (ARG2) is higher in asthmatics than in healthy individuals. We hypothesized that a sub-phenotype of asthma might be defined by the magnitude of arginine metabolism categorized on the basis of high and low fraction of exhaled nitric oxide (FENO).
Methods
To test this hypothesis, asthmatics (n = 52) were compared to healthy controls (n = 51) for levels of FENO, serum arginase activity, and airway epithelial expression of iNOS and ARG2 proteins, in relation to clinical parameters of asthma inflammation and airway reactivity. In parallel, bronchial epithelial cells were evaluated for metabolic effects of iNOS and ARG2 expression in vitro.
Results
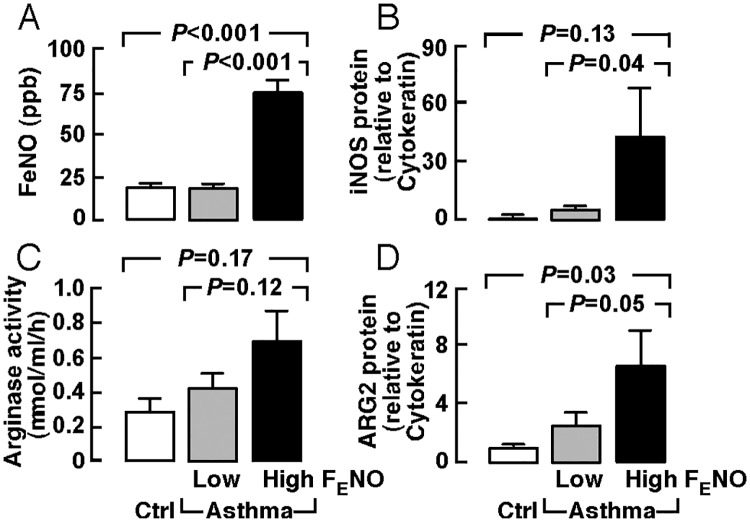
Asthmatics with high FENO (≥ 35 ppb; 44% of asthmatics) had higher expression of iNOS (P = 0.04) and ARG2 (P = 0.05) in the airway, indicating FENO is a marker of the high arginine metabolic endotype. High FENO asthmatics had the lowest FEV1% (P < 0.001), FEV1/FVC (P = 0.0002) and PC20 (P < 0.001) as compared to low FENO asthmatics or healthy controls. Low FENO asthmatics had near normal iNOS and ARG2 expression (both P > 0.05), and significantly higher PC20 (P < 0.001) as compared to high FENO asthmatics. In vitro studies to evaluate metabolic effects showed that iNOS overexpression and iNOS+ARG2 co-expression in a human bronchial epithelial cell line led to greater reliance on glycolysis with higher rate of pyruvate going to lactate.
Conclusions
The high FENO phenotype represents a large portion of the asthma population, and is typified by greater arginine metabolism and more severe and reactive asthma.
Introduction
Asthma is a chronic inflammation of the airways that is characterized by airway reactivity. Nitric oxide (NO), generated by inducible NO Synthase (iNOS; EC 1.14.13.39) expressed in the airway epithelium, where it catalyzes the conversion of arginine to NO and citrulline, is typically higher in asthmatics than in healthy populations [1–4]. We [1, 5, 6] and others [7–13] found that levels of arginine and arginase 2 (ARG2; EC 3.5.3.1), which catabolizes arginine to ornithine and urea, are also higher in the airway of asthmatics as compared to healthy controls. Recently we reported that sustained NO production in asthma is dependent upon the cell autonomous citrulline-arginine-NO cycle [6]. ARG2, by delivering ornithine into the mitochondria, provides nitrogen for the citrulline-arginine-NO cycle in order to sustain the high NO production while also supporting cellular bioenergetics and the inflammatory state [6].
In this context, although NO is higher in asthmatic populations, there is a wide variability in fraction of exhaled NO (FENO) in individuals with asthma; some have FENO levels in a normal range. Little is known of the high and low FENO endotypes, and the bioenergetic effects of high arginine metabolism on asthma. Guidelines for asthma care define a cut-point of 35 ppb FENO for asthma control and assessment of inflammation [4, 14]. Here, we hypothesized that a sub-phenotype of asthma could be defined by the magnitude of arginine metabolism identified on the basis of high and low FENO levels.
Materials and methods
Study population
The clinical characteristics of the study population are listed in Table 1. Some of the study subjects had participated in studies reported previously [5, 6]. Asthma was verified based upon American Thoracic Society guidelines, which include positive methacholine challenge test and/or reversible airflow obstruction. The severity of asthma was classified as mild intermittent/persistent (mild), moderate persistent (moderate) and severe persistent (severe) based on National Asthma Education and Prevention Program (NAEPP) guidelines [15]. Healthy controls lacked cardiopulmonary symptoms and had normal spirometry and negative methacholine challenge. Exclusion criteria for both asthmatics and healthy controls included age less than 18 years, pregnancy, current smoking, smoking within the past year, or former smokers with ≥ 5 pack-year total history. Spirometry was performed with an automated spirometer, and FENO was measured by an online method at a constant flow rate of 50 ml/second according to the standards published by the American Thoracic Society. A subgroup of participants underwent bronchoscopy for endobronchial brushing and for bronchoalveolar lavage (BAL). All studies were approved by the Cleveland Clinic Institutional Review Board (IRB # PPG8351). All subjects were recruited from Cleveland Clinic and gave written informed consent by signing a consent document approved by the Cleveland Clinic Institutional Review Board.
Table 1. Clinical features of study participants.
| Characteristics | Healthy Controls | All Asthmatics | P* | Asthma Severity | |||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | P** | ||||
| N | 51 | 52 | 27 | 18 | 3 | ||
| Mean age, yr | 37 ± 1 | 38 ± 1 | 0.8 | 37 ± 2 | 41 ± 1 | 36 ± 7 | 0.4 |
| Gender, M/F | 18/33 | 23/29 | 0.3 | 10/17 | 10/8 | 1/2 | 0.4 |
| BMI, kg/m2 | 27.8 ± 0.9 | 29.0 ± 0.8 | 0.17 | 27.4 ± 1.0 | 30.6 ± 1.1 | 34.5 ± 4.0 | 0.03 |
| Ethnicity, C/AA/other | 24/23/4 | 25/20/7 | 0.4 | 15/8/4 | 7/9/2 | 1/2/0 | 0.7 |
| Lung function | |||||||
| FEV1% predicted | 96 ± 1 | 82 ± 2 | <0.001 | 94 ± 1 | 71 ± 1 | 52 ± 4 | <0.001 |
| FEV1/FVC | 0.80 ± 0.01 | 0.74 ± 0.01 | 0.0002 | 0.77 ± 0.01 | 0.71 ± 0.02 | 0.54 ± 0.03 | <0.001 |
| PC20, mg/ml | NR# | 4.6 ± 1.3 | <0.001 | 6.3 ± 1.9 | 2.3 ± 1.5 | 0.26 ± 0 | 0.2 |
| IgE, IU/ml | 76 ± 21 | 291 ± 51 | 0.0004 | 278 ± 74 | 310 ± 86 | 290 ± 29 | 0.9 |
| Medication (n) | |||||||
| Corticosteroids (no/yes) | 51/0 | 22/30 | 15/12 | 3/15 | 0/3 | 0.006 | |
| Inhaled (no/yes) | 51/0 | 22/30 | 15/12 | 3/15 | 0/3 | 0.006 | |
| Oral (no/yes) | 51/0 | 52/0 | 27/0 | 18/0 | 3/0 | ||
| Injected (no/yes) | 51/0 | 52/0 | 27/0 | 18/0 | 3/0 | ||
| Xolair (no/yes) | 51/0 | 52/0 | 27/0 | 18/0 | 3/0 | ||
| Leukotriene receptor antagonists (no/yes) |
51/0 | 41/11 | 22/5 | 14/4 | 2/1 | 0.8 | |
Mean ± SEM;
Definition of abbreviations: Mild, mild intermittent/persistent; Moderate, moderate persistent; Severe, severe persistent; M, male; F, female; BMI, body mass index; C, Caucasian; AA, African American; FEV1, Forced expiratory volume in 1 second; FVC, Forced vital capacity; PC20, provocative concentration of methacholine causing a 20% fall in FEV1;
*P value, asthma vs. controls;
**P value, ANOVA of mild, moderate, severe asthma;
#non-reactive.
Arginase activity
Arginase activity was determined, using 50 μl aliquots of serum, by the conversion of [14C]guanidino-L-arginine to [14C]urea, which was converted to 14CO2 by urease and trapped as Na214CO3 [5, 16].
Western analyses
Whole cell lysates were prepared as previously described [17]. Total protein was measured using the Pierce Coomassie Plus Protein Assay (Thermo Fisher Scientific, Waltham, MA). For human bronchial epithelial cells, the volumes of whole cell lysate loaded per lane were adjusted to have similar Cytokeratin expression after 5 μl lysates were pre-run to measure Cytokeratin, because Cytokeratin confirms epithelial cells obtained by airway brushing. Equal amounts of protein (80 μg/lane) were loaded per lane for samples from BET1A cells, while Enolase was used as a loading control. Proteins were separated by electrophoresis on a 4–15% Tris-HCl precast gel (Bio-Rad Lab, Hercules, CA) and transferred onto polyvinylidene difluoride membranes (PVDF, Millipore Corporation, Bedford, MA). Rabbit anti-iNOS (sc-651, 1:400), ARG2 (sc-20151, 1:600) and Enolase (sc-15343, 1:1000) polyclonal Ab (Santa Cruz Biotechnology, Santa Cruz, CA), and mouse anti-Cytokeratin (M3515, 1:400) monoclonal Ab (DAKO North America, Carpinteria, California) were used in western analyses.
Cell culture
BET1A cells, a human bronchial cell line transformed by SV40 T antigen, were cultured in serum-free LHC-9 medium (Thermo Fisher Scientific) on pre-coated plates.
Transient transfection
Using Lipofectamine 2000 Reagent (Invitrogen Corp, Carlsbad, CA), BET1A cells were transiently transfected for 6 hours with human iNOS expression plasmid (iNOS, CCF37) [18, 19], ARG2 expression plasmid (ARG2, CCF88) [6], or an empty control vector, or co-transfected with iNOS plasmid and ARG2 plasmid (iNOS+ARG2). After transfection, cells were treated with 3 mM NO synthase inhibitor N-nitroarginine methyl ester (L-NAME) or left untreated. 48 hours after transfection, the cells were harvested for further analysis.
ATP and lactate content
ATP in cell lysates was measured by using a luciferase-based luminescence assay kit (PerkinElmer, Waltham, MA). Lactate concentration in BAL was determined with Lactate Assay Kit (BioVision, Milpitas, CA).
Measurement of oxygen consumption rate (OCR) in cells
OCR was measured using the Seahorse Extracellular Flux (XF24) Analyzer (Agilent Technologies, Santa Clara, CA). Seahorse assay media (DMEM without glucose, L-glutamine, phenol red, sodium pyruvate, and sodium bicarbonate [Sigma-Aldrich, St. Louis, MO] prepared with 6 mM glucose, 1.85 g/l sodium chloride, 1 mM sodium pyruvate, and 15 mg/l phenol red) was freshly supplemented with 2 mM L-glutamine and the pH adjusted to 7.35 with sodium hydroxide. BET1A cells were detached, washed 3 times with Seahorse assay medium, and resuspended in assay medium. 6×105 cells in 150 μl assay medium were added to the wells of a Seahorse cell plate and adhered using BD Cell-Tak (BD Biosciences, Bedford, MA) according to Seahorse protocol for nonadherent cells, with 2 or 4 wells per plate left empty for background correction. The plate was incubated in a 37°C non-CO2 incubator for 25 minutes. Additional assay medium was added to bring the final per-well volume to 500 μl and the plate incubated in a 37°C non-CO2 incubator for an additional 15 minutes. The plate was then transferred to the Seahorse XF24 Analyzer for analysis. Once in the XF24, BET1A cells underwent a MitoStress test (basal measurement of oxygen consumption followed by successive treatments with oligomycin A [0.5 μM], FCCP [carbonyl cyanide-ρ-trifluoromethoxyphenylhydrazone; 0.5 μM], and rotenone and antimycin A [1.5 μM]). All MitoStress OCR measures were done 3 times in a 3-2-3-minute mix-wait-measure cycle.
Radioisotope studies of glucose metabolism in cells
The rate of oxidation of glucose to CO2 and the rate of glycolysis (glucose to lactate) were measured by incubating 1−2×106 BET1A cells in LHC9 medium containing 6 mM glucose with [14C]-glucose in an atmosphere of 95% O2 and 5% CO2 in an airtight Erlenmeyer flask [6]. Cells were incubated for 3 hours. The CO2 generated was flushed by adding sodium bicarbonate and sulfuric acid into the medium. CO2 trapped in hyamine was counted in a scintillation counter. Lactate was separated by ion exchange chromatography and radioactivity in the isolated organic acids, mostly lactate, was measured using a scintillation counter. The rate of conversion of glucose to lactate was calculated using precursor-product relationship.
Statistics
Data are shown as mean ± SEM. All statistical comparisons were performed using the Student’s t-test, Wilcoxon nonparametric analyses or ANOVA as appropriate. Relationships between groups were analyzed using Multivariate Pairwise Correlation. The level of significance for P was chosen at 0.05. All data were analyzed with statistical program JMP Pro 10 (SAS Institute, Cary, NC).
Results
Clinical population
The study population included 51 healthy controls and 52 individuals with asthma. The clinical characteristics of the study subjects are displayed in Table 1. Asthmatics had airway reactivity to methacholine and mild to moderate airflow limitation as measured by forced expiratory volume in 1 second (FEV1) and the ratio of FEV1 to forced vital capacity (FVC)(FEV1% predicted, Control 96 ± 1, Asthma 82 ± 2, P < 0.001; FEV1/FVC, Control 0.80 ± 0.01, Asthma 0.74 ± 0.01, P = 0.0002). Asthmatics were divided into mild, moderate and severe asthma according to FEV1 (FEV1% predicted, mild, ≥ 80, n = 27, moderate, > 60 but < 80, n = 18, severe, ≤ 60, n = 3)[15]. Individuals with severe asthma had the highest body mass index (BMI)(ANOVA P = 0.03) and worst lung function (P < 0.001) as compared with mild and moderate asthmatics (Table 1). Asthma was stable and controlled by inhaled corticosteroids without recent exacerbations and without recent systemic corticosteroids use (Table 1). Not all individuals underwent all experimental studies; the numbers of subjects assessed are provided with each experiment and result. Medications were withheld for one day prior to testing.
Arginine metabolic endotypes related to clinical asthma phenotypes
Previously, we [1–3, 5, 6] and others [7–12] reported that asthmatics had higher levels of serum arginase activity and had higher FENO. Using untargeted analysis, we observed a nitric oxide-related metabolomic endotype in asthma [3]. We also reported that the high rate of NO production was dependent upon induction of ARG2 and upon cell autonomous arginine-NO-citrulline cycle [6]. To examine whether arginine metabolic endotypes were informative of clinical asthma phenotypes, FENO levels, serum arginase activity, and the expression of iNOS and ARG2 in freshly obtained airway epithelium were evaluated in asthmatics and healthy controls. As reported previously [1–5], asthmatics had significantly higher FENO and greater serum arginase activity when compared with healthy controls [FENO ppb, Control 19 ± 1, n = 51, Asthma 43 ± 5, n = 52, P < 0.001; Arginase activity μmol/ml/h, Control 0.30 ± 0.07, n = 3, Asthma 0.52 ± 0.08, n = 14, P = 0.05](S1 Table). Both iNOS and ARG2 proteins were generally expressed at higher levels in the airway epithelium of asthmatics compared with healthy controls [iNOS protein expression relative to cytokeratin expression, control 1.1 ± 0.2, n = 5, asthma 23.9 ± 13.8, n = 10, P = 0.01; ARG2 protein expression relative to cytokeratin expression, control 1.0 ± 0.1, n = 5, asthma 3 ± 1.3, n = 9, P = 0.03](S1 Table). Severe asthmatics had the highest FENO levels (ANOVA P = 0.003), but similar expression of iNOS and ARG2 proteins in the airway epithelium (both ANOVA P > 0.05) as compared to individuals with mild and moderate asthma (S1 Table). Similar to previously reported suppressive effects of corticosteroids on iNOS/NO [1], asthmatics using inhaled corticosteroids tended to have lower FENO levels than asthmatics not on corticosteroids (P = 0.17)(S2 Table). However, serum arginase activity and airway expression of iNOS and ARG2 proteins were similar between asthmatics on corticosteroids and those not on corticosteroids (all P > 0.05)(S2 Table). As previously reported [4, 5], FENO was inversely related to lung function in asthma [FENO correlation to, FEV1% predicted, R = -0.414, P = 0.003; FEV1/FVC, R = -0.311, P = 0.02; PC20, R = -0.469, P = 0.01](Table 2). IgE levels in asthmatics were positively correlated with the expression of ARG2 and iNOS in the airway epithelium [IgE correlation to, ARG2, R = 0.730, P = 0.02; iNOS, R = 0.624, P = 0.05](Table 2). ARG2 expression and arginase activity were not related to lung function in asthmatics (all P > 0.05)(Table 2), which is consistent with our prior studies [5, 6]. FENO levels were inversely related to lung function in individuals grouped by mild or severe asthma (P < 0.05), but not in individuals with moderate asthma (P > 0.05)(S3 Table). In asthmatics on corticosteroids, FENO levels were inversely related to lung function (P < 0.05). IgE levels were positively correlated with the expression of iNOS in the airway epithelium in asthmatics not on corticosteroids (P = 0.01)(S4 Table).
Table 2. Correlation between arginine metabolic endotype and clinical asthma sub-phenotype.
| Characteristics | Statistics* | FEV1 % predicted |
FEV1/FVC | IgE IU/ml |
PC20 mg/ml |
|---|---|---|---|---|---|
| FENO, ppb | R | -0.414 | -0.311 | 0.242 | -0.469 |
| P | 0.003 | 0.02 | 0.18 | 0.01 | |
| iNOS/CK | R | 0.184 | 0.327 | 0.624 | -0.082 |
| P | 0.6 | 0.3 | 0.05 | 0.8 | |
| Arginase activity, μmol/ml/h | R | -0.011 | -0.093 | 0.418 | -0.083 |
| P | 0.9 | 0.7 | 0.15 | 0.8 | |
| ARG2/CK | R | 0.400 | 0.226 | 0.730 | 0.089 |
| P | 0.2 | 0.5 | 0.02 | 0.8 |
Definition of abbreviations: FEV1, Forced expiratory volume in 1 second; FVC, Forced vital capacity; PC20, provocative concentration of methacholine causing a 20% fall in FEV1; FENO, fractional exhaled nitric oxide; iNOS, inducible nitric oxide synthase; CK, Cytokeratin; ARG2, arginase 2; iNOS/CK and ARG2/CK determined in the airway epithelium;
*R and P values represent Multivariate Pairwise correlation and significance, respectively; Values in bold indicate R values with significant P ≤ 0.05.
Asthmatics had higher levels of FENO than controls (P < 0.001), but 56% of asthmatics actually had FENO within the normal range. When we stratified asthmatics by high and low FENO [high FENO, ≥ 35 ppb, n = 23, low FENO, < 35 ppb, n = 29] [4, 14], asthmatics with high FENO had higher expression of iNOS (P = 0.04) and ARG2 (P = 0.05) in the airway epithelium (Table 3)(Fig 1). These data suggest that FENO can be used as a marker of high arginine metabolism in asthmatic airways. Serum arginase activity, although higher in asthmatics, was not significantly different in asthmatics with high or low FENO (P = 0.12)(Table 3)(Fig 1). With all three severe asthmatics stratified to high FENO phenotype, high FENO asthmatics tended to be more severe than low FENO asthmatics (Asthma severity, mild/moderate/severe, low FENO, 17/11/0, high FENO, 10/7/3, P = 0.06)(Table 3). Because arginine metabolism influences cellular bioenergetics [6, 20], we measured the concentration of lactate in the bronchoalveolar lavage (BAL). Asthmatics with high FENO had higher levels of lactate in the BAL (ANOVA P = 0.02), lower FEV1% predicted (ANOVA P < 0.001), lower FEV1/FVC (ANOVA P = 0.0002) and lower PC20 (ANOVA P < 0.001) as compared to low FENO asthmatics or healthy controls. Importantly, asthmatics with low FeNO, whose airway expression of iNOS and ARG2 were similar to healthy controls (all P > 0.05), had significantly higher PC20 (P < 0.001) and lower IgE (P = 0.04) as compared to high FENO asthmatics (Table 3)(Fig 1). There was no difference in proportion of asthmatics receiving corticosteroids or not on corticosteroids between high FENO and low FENO groups (P > 0.05)(Table 3).
Table 3. Features in healthy controls and asthmatics stratified by NO levels.
| Characteristics | Healthy Controls |
Asthmatics | P** | ||
|---|---|---|---|---|---|
| Low FENO (< 35 ppb) |
High FENO (≥ 35 ppb) |
P* | |||
| N | 51 | 29 | 23 | ||
| Mean age, yr | 37 ± 1 | 38 ± 1 | 38 ± 2 | 0.9 | 0.9 |
| Gender, M/F | 18/33 | 12/17 | 11/12 | 0.6 | 0.5 |
| BMI | 27.8 ± 0.9 | 28.5 ± 1.1 | 29.5 ± 1.0 | 0.5 | 0.5 |
| Ethnicity, C/AA/other | 24/23/4 | 15/11/3 | 10/9/4 | 0.8 | 0.7 |
| Asthma Severity | |||||
| Mild/Moderate/Severe | 17/11/0 | 10/7/3 | 0.06 | ||
| Lung function | |||||
| FEV1% predicted | 96 ± 1 | 86 ± 3 | 78 ± 3 | 0.04 | <0.001 |
| FEV1/FVC | 0.80 ± 0.01 | 0.76 ± 0.01 | 0.72 ± 0.02 | 0.11 | 0.0002 |
| PC20, mg/ml | NR# | 8.2 ± 2.2 | 0.9 ± 0.2 | <0.001 | <0.001 |
| FENO, ppb | 19 ± 1 | 19 ± 1 | 75 ± 7 | <0.001 | <0.001 |
| Blood | |||||
| IgE, IU/ml | 76 ± 21 | 221 ± 60 | 377 ± 84 | 0.04 | 0.0002 |
| Arginase activity, μmol/ml/h | 0.30 ± 0.07 | 0.43 ± 0.08 | 0.70 ± 0.17 | 0.12 | 0.17 |
| BAL | |||||
| Lactate, μM | 11 ± 1 | 11 ± 1 | 25 ± 6 | 0.01 | 0.02 |
| Airway epithelium | |||||
| iNOS/CK | 1.1 ± 0.2 | 4.9 ± 2.0 | 42.8 ± 25.9 | 0.04 | 0.13 |
| ARG2/CK | 1.0 ± 0.1 | 2.5 ± 1.0 | 6.6 ± 2.3 | 0.05 | 0.03 |
| Medication (n) | |||||
| Corticosteroids (no/yes) | 51/0 | 11/18 | 11/12 | 0.4 | |
| Inhaled (no/yes) | 51/0 | 11/18 | 11/12 | 0.4 | |
| Oral (no/yes) | 51/0 | 29/0 | 23/0 | ||
| Injected (no/yes) | 51/0 | 29/0 | 23/0 | ||
| Xolair (no/yes) | 51/0 | 29/0 | 23/0 | ||
| Leukotriene receptor antagonists (no/yes) |
51/0 | 23/6 | 18/5 | 0.9 | |
Mean ± SEM;
Definition of abbreviations: M, male; F, female; BMI, body mass index; C, Caucasian; AA, African Amirican; Mild, mild intermittent/persistent; Moderate, moderate persistent; Severe, severe persistent; FEV1, Forced expiratory volume in 1 second; FVC, Forced vital capacity; PC20, provocative concentration of methacholine causing a 20% fall in FEV1; FENO, fractional exhaled nitric oxide; BAL, bronchoalveolar lavage; iNOS, inducible nitric oxide synthase; CK, Cytokeratin; ARG2, arginase 2;
*P value, asthmatics with high FENO vs. asthmatics with low FENO;
**P value, ANOVA of asthmatics with high FENO, asthmatics with low FENO, controls;
#non-reactive.
Fig 1. Arginine metabolic endotype of asthma.
Fractional exhaled nitric oxide (FENO), serum arginase activity, and airway protein expression of inducible nitric oxide synthase (iNOS) and arginase 2 (ARG2) were dichotomized by high FENO (≥ 35 ppb, n = 23) and low FENO (< 35 ppb, n = 29).
These findings indicate that high arginine metabolism in asthma is associated with the high FENO phenotype, which is characterized clinically by greater airflow obstruction and airway reactivity and more severe asthma.
Greater reliance on glycolysis in bronchial epithelial cells with iNOS overexpression
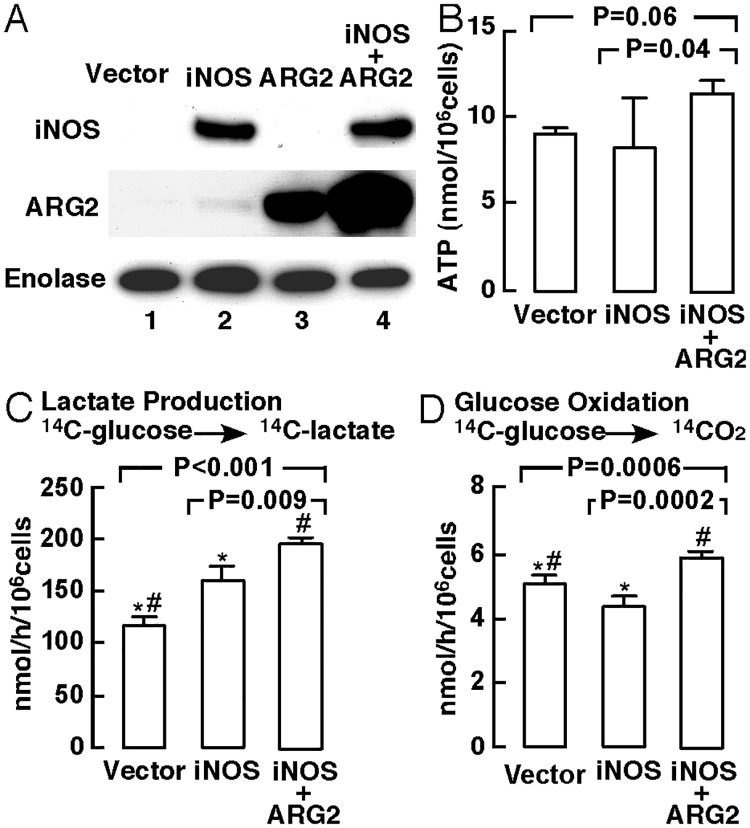
In our recent study [6], we reported that greater arginine flux through ARG2 can support cellular mitochondrial bioenergetics. In order to understand the impact of increased arginine metabolism via high expression of iNOS or high co-expression of iNOS and ARG2 in asthmatic bronchial epithelial cells, we analyzed immortalized human bronchial epithelial cells (BET1A) in vitro. BET1A cells were transiently transfected with iNOS expression vector, ARG2 expression vector, co-transfected with iNOS vector and ARG2 vector (iNOS+ARG2), or control vector. iNOS expression is not detectable in BET1A cells at baseline culture [21]. When transfected with iNOS vector alone or co-transfected with iNOS and ARG2 vectors, high-level expression of iNOS and ARG2 were observed (Fig 2A). High nitrate levels accumulated in the culture medium of cells transfected with iNOS vector or with iNOS+ARG2 vectors, and this was suppressed by N-nitroarginine methyl ester (L-NAME), a non-selective inhibitor of NO synthase, confirming iNOS activity [nitrate μM, vector alone 2.6 ± 0.1, n = 26, iNOS 52.5 ± 3.3, n = 15, iNOS+L-NAME 3.6 ± 0.2, n = 4, iNOS+ARG2 41.0 ± 3.3, n = 22, iNOS+ARG2+L-NAME 5.6 ± 0.9, n = 9, ANOVA P < 0.001].
Fig 2. Protein expression and bioenergetics of bronchial epithelial cells with iNOS expression.
(A) Western analyses of BET1A cells transfected with iNOS vector, ARG2 vector, co-transfected with iNOS+ARG2, or control vector (n ≥ 3 replicate experiments). Enolase was used as a loading control. (B) ATP production determined in BET1A cells transfected with iNOS vector, co-transfected with iNOS+ARG2, or control vector (n ≥ 3 replicate experiments). (C–D) Radioisotope studies of glucose metabolism in BET1A cells with iNOS expression. The rates of production of lactate (C) and oxidation of glucose (D) using radioactive glucose tracer were analyzed in BET1A cells transfected with iNOS vector, control vector, or co-transfected with iNOS+ARG2 vectors (n ≥ 3 replicate experiments). *P < 0.05, iNOS-expressing cells vs. control vector-transfected cells; #P < 0.05, iNOS+ARG2 co-transfected cells vs. control-transfected cells.
The effect of iNOS on bioenergetics of BET1A cells was assessed by quantifying the rate of production of ATP and metabolism of glucose using radioactive tracer (n ≥ 3 replicate experiments)(Fig 2B–2D). BET1A cells transfected with iNOS+ARG2 had a trend towards higher production of ATP [nmol/106 cells, vector alone 9.1 ± 0.3, n = 8, iNOS 8.2 ± 2.2, n = 4, iNOS+ARG2 11.4 ± 0.7, n = 10, ANOVA P = 0.06](Fig 2B). The production of ATP was significantly higher by cells transfected with iNOS+ARG2 when compared with those transfected with iNOS alone (P = 0.04). Both iNOS transfected cells (P < 0.001) and iNOS+ARG2 transfected cells (P = 0.0002) had high rate of glycolysis, as evidenced by high rate of production of [14C]lactate from [14C]glucose, as compared with vector alone [lactate production nmol/h/106 cells, vector alone 117 ± 8, n = 18, iNOS 159 ± 14, n = 9, iNOS+ARG2 195 ± 4 n = 16, ANOVA P < 0.001]. The rate of oxidation of glucose was lower in the iNOS alone expressing cells (P = 0.04) and was higher in the iNOS+ARG2 co-transfected cells (P = 0.01)[glucose oxidation nmol/h/106 cells, vector alone 5.0 ± 0.2, n = 18, iNOS 4.3 ± 0.2, n = 9, iNOS+ARG2 5.8 ± 0.1, n = 16, ANOVA P = 0.0006](Fig 2C and 2D). Parallel experiments were performed for the measurement of oxygen consumption rate (OCR) using Seahorse XF system (n ≥ 3 replicate experiments). As compared with vector alone, iNOS transfected cells had a trend towards lower basal OCR (basal OCR pmol O2/min, vector alone 132 ± 16, n = 13, iNOS 103 ± 8, n = 13, P = 0.09), and significantly lower coupling efficiency, which is defined as the proportion of the oxygen consumed to drive ATP synthesis compared to proton leak (coupling efficiency, %, vector alone 82 ± 3, n = 13, iNOS 75 ± 2, n = 13, P = 0.04)(S1 Fig) [22]. Cells co-transfected with ARG2+iNOS had similar basal OCR (P > 0.05) and coupling efficiency (P > 0.05) as compared to vector alone. Both iNOS transfected cells (P = 0.02) and iNOS+ARG2 co-transfected cells (P = 0.04) had lower spare respiratory capacity than control vector-transfected cells (S1 Fig). Taken together, these data suggest a higher rate of aerobic glycolysis by iNOS transfected cells that was ameliorated by co-expression of ARG2.
Discussion
The presence of high levels of iNOS, which produces NO and citrulline from arginine, and of arginase, which converts arginine to ornithine and urea, suggests that some asthma phenotypes are in a state of very high arginine catabolism. Important to identification of this high arginine metabolic sub-phenotype, we found that asthmatics with high FENO had higher expression of iNOS and higher expression of ARG2 in the airway epithelium than the low FENO group. As compared to low FENO asthmatics, high FENO asthmatics had a more severe clinical phenotype, which confirms prior report of high FENO being an at-risk phenotype for reactivity and exacerbations of asthma [4]. The high FENO group had higher airway lactate levels, suggesting other metabolic changes may be present in this group. The in vitro studies of immortalized bronchial epithelial cells showed that high co-expression of iNOS and ARG2 shifted cellular metabolism to greater oxidative metabolism of glucose and higher rate of ATP production. Altogether, the high FENO group is characterized by greater arginine metabolism and greater oxidative glucose metabolism, which is associated with a more severe clinical phenotype.
Inhaled corticosteroids are considered to be the most effective medications for asthma control. Previously we reported suppressive effects of corticosteroids on iNOS induction [1]. We [14, 23] and others [24–27] have shown that FENO levels decrease when asthmatics are treated with corticosteroids. Here, asthmatics receiving inhaled corticosteroids tended to have lower FENO levels than asthmatics not on corticosteroids, however, there was no difference in proportion of asthmatics receiving corticosteroids or not on corticosteroids between high FENO and low FENO groups, suggesting that high FENO and low FENO groups are phenotypes which represent arginine metabolic endotypes and not only a reflection of corticosteroid use.
The greater reliance of iNOS-expressing cells on glycolysis has been reported previously. NO binds to several targets and inhibits their functions within the mitochondrial respiratory chain (e.g., complexes I, III and IV)[28–31]. Inhibition of the respiratory chain by NO consequently decreases oxygen consumption and cellular respiration and results in an increase in the rate of aerobic glycolysis and an increase in the production of pyruvate and lactate [31, 32]. Here, iNOS transfected cells had greater lactate production, significantly reduced coupling efficiency and spare respiratory capacity, most likely as a result of the inhibition of cellular respiration by NO. Expression of ARG2 reversed suppressive effects of iNOS/NO on glucose oxidative metabolism, which suggests that ARG2 arginine metabolism may protect against some of the adverse effects of NO on mitochondrial respiratory function.
Many studies support a link between metabolism and asthma. Prior studies have identified metabolic changes in the airway in the murine model of asthma [33]. Furthermore, mitochondria numbers and oxygen consumption in airway smooth muscle of asthmatics are greater than in healthy controls [34]. Platelets from asthmatic individuals have less reliance on glycolysis and greater tricarboxylic acid (TCA) cycle turnover [35]. Greater arginine flux through ARG2 in the mitochondria has recently been shown to drive TCA cycle and cellular respiration [6]. Metabolism of arginine regulates T cell function and fate, with higher levels of arginine increasing T cell survival and anti-tumor responses [20]. Thus, this work suggests that identification of the high NO sub-phenotype of asthma may enable strategies to target metabolic pathways for personalized asthma care.
Arginine bioavailability may impact nitric oxide production and potentially FENO. We previously reported an increase in whole body metabolism of arginine in asthmatics as compared to healthy controls using stable isotope–labeled tracers [6]. Extracellular arginine levels do not reflect arginine metabolism or its cellular compartmentalization. Arginine is taken into cells by cationic amino acid transporter (CAT) proteins, and arginine and other urea cycle amino acids are highly compartmentalized in tissues and within intracellular pools, and do not equilibrate rapidly with extracellular pools. A recent study showed that intracellular arginine is critical in the control of glycolysis and mitochondrial activity [20], and intracellular arginine flux and mitochondrial arginine metabolism is a critical determinant of cell bioenergetics and function [6, 20]. In the present study, we assessed airway epithelial enzyme levels and airway exhaled NO. However, we did not evaluate plasma arginine and arginine/ornithine ratios, or intracellular arginine.
Taken together, this study shows that the high FENO phenotype represents a greater arginine metabolism endotype that is clinically characterized by greater airflow obstruction and airway reactivity. This new understanding is important to plan metabolic interventions and provide therapeutic options separate from corticosteroids and other anti-inflammatories.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Basal OCR (A), coupling efficiency (B) and spare respiratory capacity (C) were analyzed in BET1A cells transfected with iNOS vector, co-transfected with iNOS+ARG2, or control vector (n ≥ 3 replicate experiments). *P < 0.05, iNOS-expressing cells vs. control vector-transfected cells; #P < 0.05, iNOS+ARG2 co-transfected cells vs. control-transfected cells.
(TIF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by HL081064, HL103453, and HL109250; SCE was supported in part by the Alfred Lerner Chair for Biomedical Research.
References
- 1.Guo FH, Comhair SA, Zheng S, Dweik RA, Eissa NT, Thomassen MJ, et al. Molecular mechanisms of increased nitric oxide (NO) in asthma: evidence for transcriptional and post-translational regulation of NO synthesis. Journal of immunology. 2000; 164: 5970–5980. [DOI] [PubMed] [Google Scholar]
- 2.Dweik RA, Comhair SA, Gaston B, Thunnissen FB, Farver C, Thomassen MJ, et al. NO chemical events in the human airway during the immediate and late antigen-induced asthmatic response. Proceedings of the National Academy of Sciences of the United States of America. 2001; 98: 2622–2627. doi: 10.1073/pnas.051629498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Comhair SA, McDunn J, Bennett C, Fettig J, Erzurum SC, Kalhan SC. Metabolomic Endotype of Asthma. Journal of immunology. 2015; 195: 643–650. doi: 10.4049/jimmunol.1500736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dweik RA, Sorkness RL, Wenzel S, Hammel J, Curran-Everett D, Comhair SA, et al. Use of exhaled nitric oxide measurement to identify a reactive, at-risk phenotype among patients with asthma. American journal of respiratory and critical care medicine. 2010; 181: 1033–1041. doi: 10.1164/rccm.200905-0695OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lara A, Khatri SB, Wang Z, Comhair SA, Xu W, Dweik RA, et al. Alterations of the Arginine Metabolome in Asthma. American journal of respiratory and critical care medicine. 2008; 178: 673–681. doi: 10.1164/rccm.200710-1542OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu W, Ghosh S, Comhair SA, Asosingh K, Janocha AJ, Mavrakis DA, et al. Increased mitochondrial arginine metabolism supports bioenergetics in asthma. The Journal of clinical investigation. 2016; 126: 2465–2481. doi: 10.1172/JCI82925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bratt JM, Franzi LM, Linderholm AL, Last MS, Kenyon NJ, Last JA. Arginase enzymes in isolated airways from normal and nitric oxide synthase 2-knockout mice exposed to ovalbumin. Toxicol Appl Pharmacol. 2009; 234: 273–280. doi: 10.1016/j.taap.2008.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bratt JM, Zeki AA, Last JA, Kenyon NJ. Competitive metabolism of L-arginine arginase as a therapeutic target in asthma. Journal of Biomedical Research. 2011; 25: 299–308. doi: 10.1016/S1674-8301(11)60041-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ckless K, Lampert A, Reiss J, Kasahara D, Poynter ME, Irvin CG, et al. Inhibition of arginase activity enhances inflammation in mice with allergic airway disease, in association with increases in protein S-nitrosylation and tyrosine nitration. Journal of immunology. 2008; 181: 4255–4264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maarsingh H, Zaagsma J, Meurs H. Arginase: a key enzyme in the pathophysiology of allergic asthma opening novel therapeutic perspectives. Br J Pharmacol. 2009; 158: 652–664. doi: 10.1111/j.1476-5381.2009.00374.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morris CR, Poljakovic M, Lavrisha L, Machado L, Kuypers FA, Morris SM Jr. Decreased arginine bioavailability and increased serum arginase activity in asthma. American journal of respiratory and critical care medicine. 2004; 170: 148–153. doi: 10.1164/rccm.200309-1304OC [DOI] [PubMed] [Google Scholar]
- 12.Zimmermann N, King NE, Laporte J, Yang M, Mishra A, Pope SM, et al. Dissection of experimental asthma with DNA microarray analysis identifies arginase in asthma pathogenesis. The Journal of clinical investigation. 2003; 111: 1863–1874. doi: 10.1172/JCI17912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reinke SN, Gallart-Ayala H, Gomez C, Checa A, Fauland A, Naz S, et al. Metabolomics analysis identifies different metabotypes of asthma severity. The European respiratory journal. 2017; 49 doi: 10.1183/13993003.01740-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. American journal of respiratory and critical care medicine. 2011; 184: 602–615. doi: 10.1164/rccm.9120-11ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda (MD): National Heart, Lung, and Blood Institute. 2007; NIH publication no. 07–4051.
- 16.Morris SM Jr., Kepka-Lenhart D, Chen LC. Differential regulation of arginases and inducible nitric oxide synthase in murine macrophage cells. The American journal of physiology. 1998; 275: E740–747. [DOI] [PubMed] [Google Scholar]
- 17.Xu W, Comhair SA, Zheng S, Chu SC, Marks-Konczalik J, Moss J, et al. STAT-1 and c-Fos interaction in nitric oxide synthase-2 gene activation. American journal of physiology Lung cellular and molecular physiology. 2003; 285: L137–148. doi: 10.1152/ajplung.00441.2002 [DOI] [PubMed] [Google Scholar]
- 18.Xu W, Kaneko FT, Zheng S, Comhair SA, Janocha AJ, Goggans T, et al. Increased arginase II and decreased NO synthesis in endothelial cells of patients with pulmonary arterial hypertension. Faseb J. 2004; 18: 1746–1748. doi: 10.1096/fj.04-2317fje [DOI] [PubMed] [Google Scholar]
- 19.Panda K, Chawla-Sarkar M, Santos C, Koeck T, Erzurum SC, Parkinson JF, et al. Visualizing inducible nitric-oxide synthase in living cells with a heme-binding fluorescent inhibitor. Proceedings of the National Academy of Sciences of the United States of America. 2005; 102: 10117–10122. doi: 10.1073/pnas.0408972102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geiger R, Rieckmann JC, Wolf T, Basso C, Feng Y, Fuhrer T, et al. L-Arginine Modulates T Cell Metabolism and Enhances Survival and Anti-tumor Activity. Cell. 2016; 167: 829–842 e813. doi: 10.1016/j.cell.2016.09.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uetani K, Arroliga ME, Erzurum SC. Double-stranded rna dependence of nitric oxide synthase 2 expression in human bronchial epithelial cell lines BET-1A and BEAS-2B. Am J Respir Cell Mol Biol. 2001; 24: 720–726. doi: 10.1165/ajrcmb.24.6.4297 [DOI] [PubMed] [Google Scholar]
- 22.Dranka BP, Benavides GA, Diers AR, Giordano S, Zelickson BR, Reily C, et al. Assessing bioenergetic function in response to oxidative stress by metabolic profiling. Free radical biology & medicine. 2011; 51: 1621–1635. doi: 10.1016/j.freeradbiomed.2011.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cowan DC, Taylor DR, Peterson LE, Cowan JO, Palmay R, Williamson A, et al. Biomarker-based asthma phenotypes of corticosteroid response. The Journal of allergy and clinical immunology. 2015; 135: 877–883 e871. doi: 10.1016/j.jaci.2014.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cowan DC, Cowan JO, Palmay R, Williamson A, Taylor DR. Effects of steroid therapy on inflammatory cell subtypes in asthma. Thorax. 2010; 65: 384–390. doi: 10.1136/thx.2009.126722 [DOI] [PubMed] [Google Scholar]
- 25.Silkoff PE, McClean P, Spino M, Erlich L, Slutsky AS, Zamel N. Dose-response relationship and reproducibility of the fall in exhaled nitric oxide after inhaled beclomethasone dipropionate therapy in asthma patients. Chest. 2001; 119: 1322–1328. [DOI] [PubMed] [Google Scholar]
- 26.Smith AD, Cowan JO, Brassett KP, Filsell S, McLachlan C, Monti-Sheehan G, et al. Exhaled nitric oxide: a predictor of steroid response. American journal of respiratory and critical care medicine. 2005; 172: 453–459. doi: 10.1164/rccm.200411-1498OC [DOI] [PubMed] [Google Scholar]
- 27.Szefler SJ, Martin RJ, King TS, Boushey HA, Cherniack RM, Chinchilli VM, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. The Journal of allergy and clinical immunology. 2002; 109: 410–418. [DOI] [PubMed] [Google Scholar]
- 28.Brown GC, Borutaite V. Inhibition of mitochondrial respiratory complex I by nitric oxide, peroxynitrite and S-nitrosothiols. Biochimica et biophysica acta. 2004; 1658: 44–49. doi: 10.1016/j.bbabio.2004.03.016 [DOI] [PubMed] [Google Scholar]
- 29.Ramachandran A, Levonen AL, Brookes PS, Ceaser E, Shiva S, Barone MC, et al. Mitochondria, nitric oxide, and cardiovascular dysfunction. Free radical biology & medicine. 2002; 33: 1465–1474. [DOI] [PubMed] [Google Scholar]
- 30.Antunes F, Boveris A, Cadenas E. On the mechanism and biology of cytochrome oxidase inhibition by nitric oxide. Proceedings of the National Academy of Sciences of the United States of America. 2004; 101: 16774–16779. doi: 10.1073/pnas.0405368101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iglesias DE, Bombicino SS, Valdez LB, Boveris A. Nitric oxide interacts with mitochondrial complex III producing antimycin-like effects. Free radical biology & medicine. 2015; 89: 602–613. doi: 10.1016/j.freeradbiomed.2015.08.024 [DOI] [PubMed] [Google Scholar]
- 32.Dranka BP, Hill BG, Darley-Usmar VM. Mitochondrial reserve capacity in endothelial cells: The impact of nitric oxide and reactive oxygen species. Free radical biology & medicine. 2010; 48: 905–914. doi: 10.1016/j.freeradbiomed.2010.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mabalirajan U, Dinda AK, Sharma SK, Ghosh B. Esculetin restores mitochondrial dysfunction and reduces allergic asthma features in experimental murine model. Journal of immunology. 2009; 183: 2059–2067. doi: 10.4049/jimmunol.0900342 [DOI] [PubMed] [Google Scholar]
- 34.Trian T, Benard G, Begueret H, Rossignol R, Girodet PO, Ghosh D, et al. Bronchial smooth muscle remodeling involves calcium-dependent enhanced mitochondrial biogenesis in asthma. J Exp Med. 2007; 204: 3173–3181. doi: 10.1084/jem.20070956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu W, Cardenes N, Corey C, Erzurum SC, Shiva S. Platelets from Asthmatic Individuals Show Less Reliance on Glycolysis. PloS one. 2015; 10: e0132007 doi: 10.1371/journal.pone.0132007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Basal OCR (A), coupling efficiency (B) and spare respiratory capacity (C) were analyzed in BET1A cells transfected with iNOS vector, co-transfected with iNOS+ARG2, or control vector (n ≥ 3 replicate experiments). *P < 0.05, iNOS-expressing cells vs. control vector-transfected cells; #P < 0.05, iNOS+ARG2 co-transfected cells vs. control-transfected cells.
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.