Abstract
Objective
Gender and racial/ethnic disparities in sleep duration are well documented among the U.S. adult population, but we know little about how these disparities are shaped during the early course of adult life, a period marked by substantial changes in social roles that can influence time for sleep.
Methods
Prospective data was used from the National Longitudinal Survey of Youth 1997 (NLSY97), a U.S.-based representative sample of persons born between 1980 and 1984, who were first interviewed in 1997. Sleep duration was assessed in 2002, 2007/2008, 2009, 2010, and 2011. Random-coefficient models were estimated to examine gender and racial/ethnic disparities in trajectories of sleep duration across early adulthood as a function of educational experiences, employment, and family relationships.
Results
Sleep duration declined during early adulthood. Women reported shorter sleep than men from age 18 to 22, but slept longer than men by age 28. Young adults of black race/ethnnicity reported sleep durations similar to those of young adults of white race/ethnicity until age 24, after which blacks slept less than whites. Educational experiences and employment characteristics reduced gender and racial/ethnic disparities, but family relationships exacerbated them.
Conclusion
This study is the first to establish the emergence of gender and racial/ethnic disparities in sleep duration during early adulthood.
Keywords: Longitudinal, Education, Family, Work, Gender, Race/ethnicity
1. Introduction
Sleep problems are a major public health concern [1], affecting 50 to 70 million U.S. adults annually [1,2], and are associated with a number of adverse health conditions [3–9]. Several population-based studies of U.S. adults have reported gender and racial/ethnic disparities in sleep duration [10–12]. On average, women sleep longer than men, and individuals of black race/ethnicity are more likely to report short sleep durations compared to those of white race/ethnicity [13–15]. Moreover, sleep studies using national time use data have documented age-related changes in sleep duration across the life course [12,16,17]. Based on these cross-sectional studies, sleep duration appears to follow a U-shaped pattern, with longer sleep durations reported among persons 15–24 years old and adults over 75 years compared to those 45–54 years old. Furthermore, the steepest declines in sleep duration occur between ages 15 and 34 years [16].
These age-related patterns in sleep duration coincide with developmental and role-related changes that commonly occur during the early adult life course, including becoming a college student, worker, spouse/partner, and parent, among others [18,19]. Many of these social roles require substantial time commitments, which may displace time spent sleeping [12]. For example, working longer hours or multiple jobs [10,12,13,20], having young children in the home [10], or being a college student [12] all increase the risk of experiencing shorter sleep.
Studies suggest that these social roles may help to explain gender and racial/ethnic sleep disparities. Women, as compared to men, are often expected to take care of the emotional and practical needs of the family, especially children, during the night [21], leading to more interrupted sleep and possibly shorter sleep [22]. Conversely, some research finds that work responsibilities are more strongly associated with sleep problems among men than among women [23,24]. Employment and work-related factors may also explain the greater prevalence of shorter sleep among individuals of black race/ethnicity as compared to those of white race/ethnicity [14]. Among the employed, blacks are more likely to work longer hours and to be employed in multiple jobs [20], often jobs that require shift work that may make regular sleep more difficult [25–27]. As a result, the early adult life course may be a key developmental period when gender and racial/ethnic disparities in sleep duration emerge. No studies to our knowledge, however, have investigated how these social roles contribute to gender and racial/ethnic disparities in sleep duration during the early adult life course.
The purpose of our study was to estimate trajectories of sleep duration by gender and race/ethnicity over the early adult life course using prospective, population-based U.S. data. Furthermore, we examined the role of educational experiences, employment, and family relationships in patterning gender and racial/ethnic disparities in sleep duration. These are key factors influencing the social context of young adults, and we hypothesized that they would mediate the relationship between gender, race/ethnicity, and sleep duration during early adulthood. Because early adulthood is characterized by significant change [19], an important strength of our study is our use of time-varying measures of educational experiences, employment, and family relationships to more fully capture the dynamic relationship between these social roles and sleep duration.
2. Methods
2.1. Data and sample
We used prospective data from the National Longitudinal Survey of Youth 1997 (NLSY97), a nationally representative sample of individuals born between 1980 and 1984 (N = 8984). Baseline interviews were conducted in 1997, with annual follow-ups available through 2011. The retention rate over the 14-year period was 82.6%. The NLSY97 is a publicly available, de-identified dataset; thus, this study was classified as exempt from human subjects review.
We restricted our sample to those who were interviewed on at least one occasion when sleep duration was measured (n = 8536). We excluded respondents who were missing data on any of the covariates included in the analysis in the year they provided sleep data. We also excluded respondents who were pregnant at the time of the interview. These exclusions resulted in a sample of 8473 respondents providing 35,972 person-period observations. Over 93% of the analytic sample respondents provided data on sleep at least four times (minimum observations = 1; maximum observations = 5).
2.2. Measures
2.2.1. Sleep duration
Sleep duration data were collected in 2002, 2007/2008, 2009, 2010, and 2011. Respondents were asked, “On a typical weeknight, how many hours of sleep do you usually get?” Responses ranged from 0 to 24 hours, and were reported in 1-hour increments. The variable was normally distributed and used as a continuous variable. Distributions were similar for men and women and across racial/ethnic groups.
2.2.2 Demographics
Demographic characteristics included age (in years; minimum = 18, maximum = 31), race/ethnicity (self-reported as non-Hispanic white, non-Hispanic black, hispanic, and other), and gender (male or female).
2.2.3. Education measures
Education-related variables included enrollment status (a time-varying indicator categorized as not enrolled in college, enrolled in college, or enrolled in graduate school) and respondents’ highest degree attained (a time-varying indicator categorized as no degree, General Educational Development [GED], high school diploma, associate’s degree, bachelor’s degree, or higher).
2.2.4. Employment measures
Employment characteristics included a time-varying indicator of the average number of hours worked per week during the respective survey year (categorized as 0 hours, 1–39 hours, and 40 or more hours) and a time-varying indicator of the total number of jobs that the respondent held in the respective survey year (range 0–9; 88% held 0–2 jobs).
2.2.5. Family measures
Family relationship variables included a time-varying indicator of whether the respondent was living or not living with a romantic partner (ie, was married or cohabitating), a time-varying indicator of the count of children under age 18 years who were living in the household at the time of the interview (range 0–10; 92% had two or fewer children in the household), and a time-varying indicator for whether the respondent had a child under the age of 6 years residing in the household.
2.3. Statistical analysis
Random-coefficient linear models were estimated to account for repeated observations and varying numbers of observations per person. In our models, age represents time and was centered at 26, the mean age of our sample across the waves of observation. The following model was estimated:
| (Equation 1) |
where Yit is sleep duration for respondent i at time t and Yit to Ynt are independent; i = 1, … n respondents across t = 18,…t years of age; λ00 is the average sleep duration at age 26, Σλi1Xi1 is the sum of time invariant covariates; ΣαitZit is the sum of time-varying covariates and cross-level interactions; ζ0i and ζ1i are random effects that represent unobserved heterogeneity for respondent i and are assumed to be normally distributed with mean 0; and εit is random within-person error of prediction for respondent i at time t. We assume that the random effects are independent of εit, and all random components are independent of all covariates.
Random-coefficient linear models were estimated using mixed in Stata v14 software (Stata Corporation, College Station, TX). Analyses were weighted at the person-level using the custom weights provided by the NLSY97, which account for sampling design and attrition; however, unweighted analysis yielded similar inferences. We estimated four nested models to examine how gender and racial/ethnic disparities in sleep duration varied across early adulthood (model 1) as a function of educational experiences (model 2), employment (model 3), and family relationships (model 4). Sleep duration was converted to minutes so that regression coefficients represent the amount of minutes in sleep gained or lost.
We calculated predicted sleep duration across age by gender and race/ethnicity using the margins command in Stata v14 so we could visualize differences in graphical plots. We also determined whether the gender and racial/ethnic differences in predicted sleep duration at each age were statistically significant.
3. Results
3.1. Sample characteristics
Table 1 presents sample characteristics across the five waves of observations. Sleep duration declined from 7.1 hours in 2002 to 6.6 hours in 2011. Although 38.3% of participants were enrolled in college or graduate school in 2002, by 2011, this percentage was only 11.4%. Correspondingly, less than 2% had attained at least a college degree by 2002, whereas 29.9% had done so by 2011. Over this period, young adults held fewer jobs (mean = 1.9 in 2002; mean = 1.1 in 2011), perhaps because they switched from mostly part-time employment (57.3% in 2002) to mostly full-time employment (58.8% in 2011). More young adults were living with a partner by 2011 (56.0%) than they were in 2002 (17.1%), and had more children residing in the household (mean = 1.0 in 2011; mean = 0.7 in 2002).
Table 1.
Sample characteristics by survey year, National Longitudinal Survey of Youth 1997, weighted estimates, percentage or mean (SE). a
| 2002 n = 7464 |
2007/8 n = 7353 |
2009 n = 7129 |
2010 n = 7000 |
2011 n = 7026 |
|
|---|---|---|---|---|---|
|
|
|||||
| Sleep duration (h) | 7.1 (0.02) | 6.8 (0.02) | 6.8 (0.02) | 6.7 (0.02) | 6.6 (0.02) |
| Age (y) | 20.0 (0.02) | 24.9 (0.02) | 26.8 (0.02) | 27.9 (0.02) | 28.8 (0.02) |
| Female, % | 47.8 | 47.4 | 48.2 | 47.3 | 47.6 |
| Race/ethnicity, % | |||||
| Non-Hispanic white | 67.0 | 66.6 | 66.6 | 66.3 | 66.1 |
| Non-Hispanic black | 15.3 | 15.7 | 15.7 | 16.0 | 16.1 |
| Hispanic | 12.6 | 12.8 | 12.9 | 13.0 | 12.9 |
| Other | 5.1 | 4.9 | 4.8 | 4.7 | 4.8 |
| School enrollment, % | |||||
| Not enrolled in college | 61.7 | 84.3 | 86.3 | 86.8 | 88.6 |
| Enrolled in college | 37.8 | 11.5 | 9.0 | 8.8 | 7.8 |
| Enrolled in graduate school | 0.5 | 4.2 | 4.7 | 4.4 | 3.6 |
| Highest degree attained, % | |||||
| No degree | 21.2 | 9.6 | 8.7 | 8.5 | 8.2 |
| GED | 6.4 | 10.5 | 11.1 | 11.4 | 11.7 |
| High school diploma | 69.2 | 48.6 | 44.9 | 43.4 | 42.6 |
| Associate’s degree | 1.5 | 6.2 | 6.9 | 7.1 | 7.6 |
| Bachelor’s degree or higher | 1.7 | 25.1 | 28.4 | 29.6 | 29.9 |
| Number of jobs held (count) | 1.9 (0.02) | 1.5 (0.01) | 1.3 (0.01) | 1.2 (0.01) | 1.1 (0.01) |
| Hours worked, % | |||||
| None | 11.2 | 8.2 | 12.0 | 13.6 | 14.8 |
| Part-time (1–39 hours) | 57.3 | 30.9 | 30.1 | 27.5 | 26.4 |
| Full-time (40+ hours) | 31.5 | 60.9 | 57.9 | 58.9 | 58.8 |
| Living with partner, % | 17.1 | 44.2 | 51.4 | 53.6 | 56.0 |
| Number of children under age 18 in HH (count) | 0.7 (0.01) | 0.7 (0.01) | 0.5 (0.01) | 0.9 (0.02) | 1.0 (0.02) |
| Any child under age 6 in HH, % | 17.2 | 30.0 | 44.4 | 36.5 | 37.1 |
Means and standard errors are reported for continuous variables and their measurement units are indicated next to their variable name. GED, General Educational Development; SE, standard error; HH, household.
Column percentages reported. Percentages may not add to 100 due to rounding.
3.2. Random-coefficient linear models
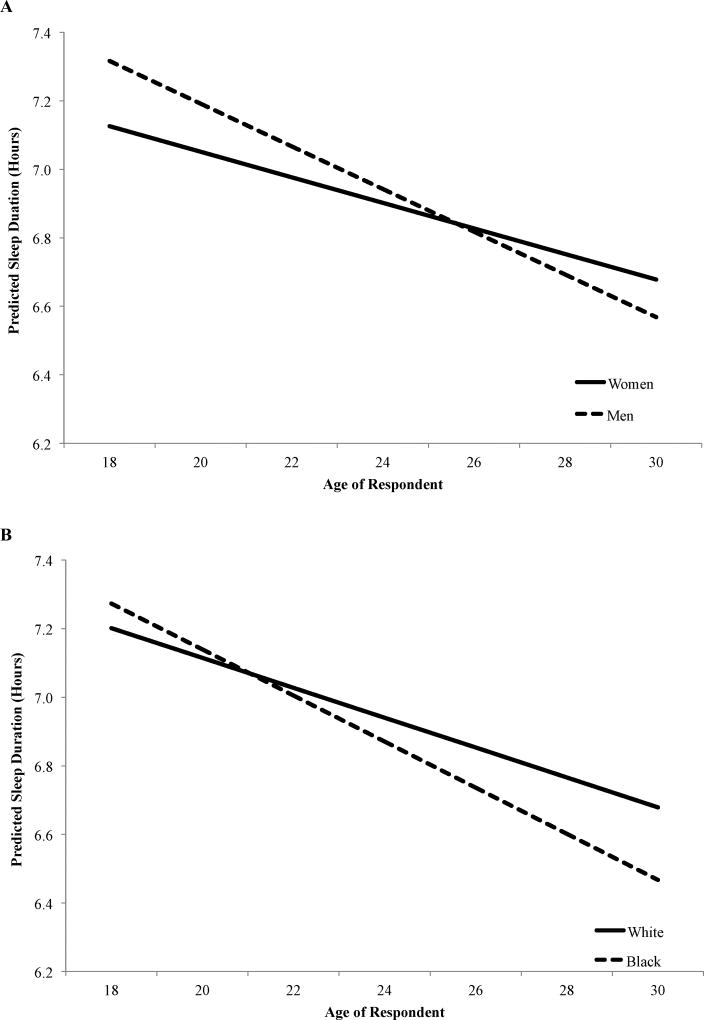
Table 2 presents estimates from the random-coefficient linear models. Model 1 shows estimates for gender and race/ethnicity. At age 26 years, women reported sleeping about the same amount as men, but blacks reported sleeping 7.0 fewer minutes than whites. Latinos and young adults of other races/ethnicities reported amounts of sleep similar to those of whites. A 1-year change in age was associated with a 3.3-minute decline in sleep duration. The age slope was shallower for women (b = 1.5, standard error [SE] = 0.3) than men, but was steeper for blacks (b = −1.4, SE = 0.4) than for whites. Thus, women reported sleeping about 11 fewer minutes than men at age 18, but reported sleeping almost 7 minutes longer than men by age 30 (Fig. 1A). The reversal in the gender disparity in sleep duration occurred between ages 24 and 26. Furthermore, at age 18 years there were no statistically significant racial/ethnic disparities in sleep duration (Fig. 1B); however, by age 24, blacks reported sleeping 4 fewer minutes than whites, a disparity that widened to almost 13 minutes at age 30.
Table 2.
Regression coefficients and standard errors from random-coefficient models predicting self-reported sleep duration (in minutes), National Longitudinal Survey of Youth 1997, weighted estimates. a,b
| Model 1 b (SE) |
Model 2 b (SE) |
Model 3 b (SE) |
Model 4 b (SE) |
|
|---|---|---|---|---|
|
|
||||
| Status at age 26 y | ||||
| Intercept | 410.9 (1.1)* | 408.6 (1.4)* | 418.6 (2.3)* | 420.9 (2.4)* |
| Female | 0.6 (1.4) | −0.1 (1.4) | −1.4 (1.4) | 1.1 (1.4)* |
| Race/ethnicity | ||||
| Non-Hispanic black | −7.0 (1.8)* | −5.9 (1.9)* | −6.8 (1.9)* | −4.3 (1.9)* |
| Hispanic | −1.0 (1.7) | 0.2 (1.8) | 0.2 (1.8) | 2.1 (1.8) |
| Other | −12.5 (3.6)* | −13.4 (3.6)* | −14.1 (3.6)* | −13.9 (3.6)* |
| School enrollment | ||||
| Enrolled in college | −3.9 (1.5)* | −5.6 (1.6)* | −6.5 (1.6)* | |
| Enrolled in graduate school | −10.1 (2.3)* | −12.5 (2.3)* | −13.2 (2.3)* | |
| Highest degree attained | ||||
| No degree | 6.1 (2.6)* | 4.0 (2.6) | 5.9 (2.6)* | |
| GED | −3.4 (2.5) | −4.3 (2.5) | −3.2 (2.5) | |
| Associate’s degree | −2.5 (2.7) | −2.1 (2.6) | −3.3 (2.6) | |
| Bachelor’s degree or higher | 13.2 (1.7)* | 14.7 (1.7)* | 11.1 (1.7)* | |
| Number of jobs | −1.0 (0.6) | −1.3 (0.6)* | ||
| Hours worked | ||||
| Part-time work | −4.0 (2.1) | −4.3 (2.1)* | ||
| Full-time work | −11.3 (2.1)* | −12.1 (2.1)* | ||
| Living with partner | 7.6 (1.2)* | |||
| Number of children <18 y in HH | −2.7 (0.6)* | |||
| Any child age <6 y in HH | −11.7 (1.4)* | |||
| Rate of change | ||||
| Age | −3.3 (0.2)* | −4.0 (0.3)* | −5.2 (0.6)* | −4.9 (0.6)* |
| Age × female | 1.5 (0.3)* | 1.2 (0.3)* | 1.2 (0.3)* | 1.4 (0.3)* |
| Age × non-Hispanic black | −1.4 (0.4)* | −0.9 (0.4)* | −0.7 (0.4) | −0.8 (0.4)* |
| Age × Hispanic | −0.6 (0.4) | −0.1 (0.4) | −0.1 (0.4) | −0.1 (0.4) |
| Age × other race | −2.3 (0.9)* | −2.6 (0.8)* | −2.4 (0.8)* | −2.6 (0.8)* |
| Age × no degree | −0.8 (0.5) | −0.5 (0.5) | −0.5 (0.5) | |
| Age × GED | 0.7 (0.6) | 0.6 (0.6) | 0.5 (0.6) | |
| Age × associate’s degree | 0.9 (0.8) | 0.7 (0.8) | 0.9 (0.8) | |
| Age × bachelor’s degree or higher | 0.5 (0.5) | 0.4 (0.5) | 0.5 (0.5) | |
| Age × enrolled in college | 0.9 (0.4)* | 1.2 (0.4)* | 1.0 (0.4)* | |
| Age × enrolled in graduate school | 2.5 (0.9)* | 2.8 (1.0)* | 2.8 (1.0)* | |
| Age × number of jobs | −0.1 (0.1) | −0.1 (0.1) | ||
| Age × part-time work | 1.2 (0.6)* | 1.3 (0.6)* | ||
| Age × full-time work | 1.6 (0.6)* | 1.7 (0.6)* | ||
| Age × living with partner | −0.2 (0.4) | |||
| Age × number of children <18 y in HH | −0.1 (0.2) | |||
| Age × any child <6 y in HH | –0.1 (0.4) | |||
| Random effects | ||||
| ζ0i | 49.1 | 48.9 | 48.4 | 48.4 |
| ζ1i | 8.0 | 7.8 | 7.8 | 7.7 |
|
|
||||
| Number of respondents | 8473 | |||
| Person-period observations | 35,972 | |||
GED, General Educational Development; HH, household; SE, standard error.
p < 0.05 (two-tailed test).
Reference categories: Male, non-Hispanic white, not enrolled in college; high school diploma, no hours worked, not living with a partner, no child <6 y in HH.
Age is centered at 26 y.
Fig. 1.
(A) Predicted sleep duration (hours) by gender (model 1), NLSY97. (B) Predicted sleep duration (hours) by race/ethnicity (model 1), National Longitudinal Survey of Youth 1997 (NLSY97).
Model 2 adjusts for education-related variables. At age 26 years, individuals enrolled in college (b = −3.9, SE = 1.5) or graduate school (b = −10.1, SE = 2.3) reported sleeping less than young adults not enrolled in college. College-educated (b = 13.2, SE = 1.7) individuals and those with no degree (b = 6.1, SE = 2.6) reported sleeping longer than high school graduates. The age slope was shallower for individuals enrolled in college (b = 0.9, SE = 0.4) or graduate school (b = 2.5, SE = 0.9). The inclusion of education-related variables reduced the gender and black–white disparity in the age slope by 20% ([(1.5–1.2)/1.5] × 100) and 35.7%, respectively.
Model 3 adjusts for employment-related variables. At age 26 years, those who were working full-time reported sleeping 11.3 fewer minutes than those who were not working. The age slope was shallower for part-time (b = 1.2, SE = 0.6) and full-time (b = 1.6, SE = 0.6) workers than for nonworkers. The number of jobs held was unrelated to sleep duration. Inclusion of employment variables had no effect on the gender disparity in the age slope (model 3 vs model 2), but reduced the black–white disparity in the age slope by 22.2%.
Model 4 adjusts for family relationship variables. At age 26 years, young adults who lived with a partner reported sleeping 7.6 minutes longer than those who lived without a partner. Having any children under age 6 years residing in the household was associated with 11.7 fewer minutes of sleep. Every additional child under the age of 18 in the household was associated with 2.7 fewer minutes of sleep. The age slope in sleep duration did not differ by partner status or having children in the household. Inclusion of family relationship variables increased the gender disparity in the age slope by 16.7% (model 4 vs model 3) and the black–white disparity in the age slope by 14.3%.
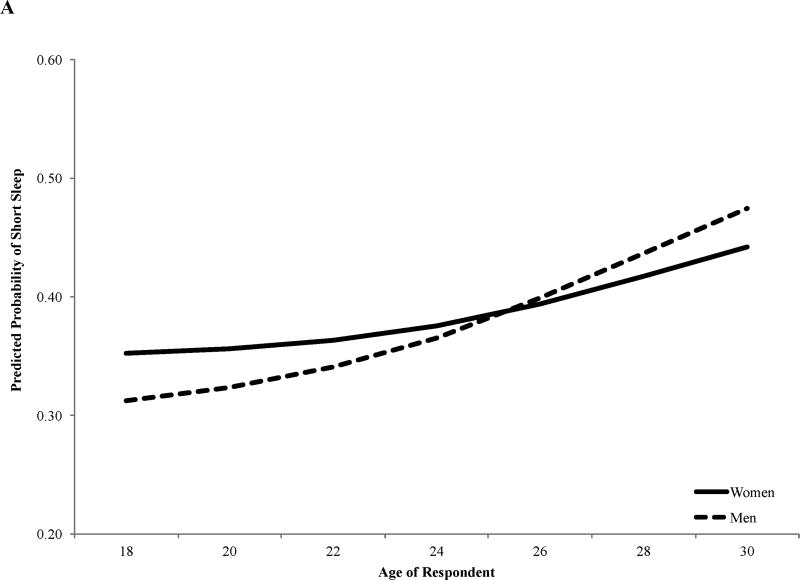
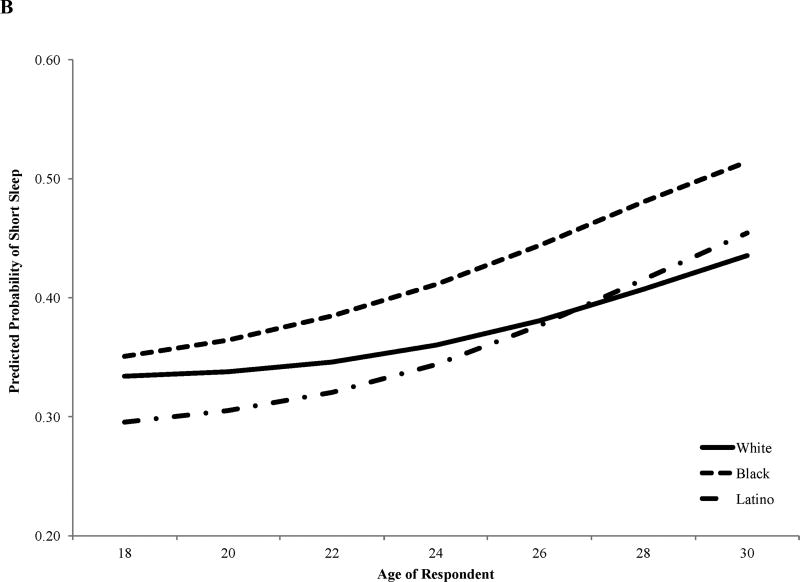
3.3. Random-coefficient logit models
Because both short sleep and long sleep have been shown to increase the risk of morbidity and premature mortality, and because prior studies have found that different factors predict short versus long sleep, we also estimated random-coefficient logit models predicting short (≤6 hours) versus adequate sleep (≥7 hours) following the same model progression that we used when estimating continuous sleep duration. We plotted the predicted probabilities of short sleep across age by gender (Fig. 2A) and race/ethnicity (Fig. 2B) using estimates from Model 4, which adjusts for education, employment, and family relationship variables.
Fig. 2.
(A) Predicted probabilities of short sleep by gender (model 4), NLSY97. (B) Predicted probabilities of short sleep by race/ethnicity (model 4), National Longitudinal Survey of Youth 1997 (NLSY97).
Similar to our findings using the continuous measure of sleep duration, gender disparities in short sleep reversed around age 26 years. Specifically, at age 18 years, women had a higher predicted probability (PP) of short sleep than men (PP = 0.35 vs PP = 0.31, respectively), but by age 30, women had a lower predicted probability of short sleep than men (PP = 0.44 vs PP = 0.47).
Likewise, racial/ethnic disparities in short sleep were similar to those found when estimating continuous sleep duration, with one exception: Latino young adults had statistically significantly lower predicted probabilities of short sleep than whites from age 18 to 22 years. Blacks had statistically significantly higher predicted probabilities of short sleep compared to whites after age 19 years, which mirrors results from models estimating continuous sleep duration.
We did not predict long sleep (≥10 hours) because so few observations fell into the category of long sleep (<2%), and estimates of long sleep would likely be unstable. Moreover, unlike other studies that include a larger age range of adults, long sleep is less likely to be driven by poor health in our sample because our respondents were young adults who are relatively healthy.
3.4. Sensitivity analysis
We considered the possibility that sleep trajectories depended upon both gender and race/ethnicity by re-estimating our models after inclusion of gender × race and gender × race × age interactions. We found no evidence that sleep trajectories by gender depended upon race/ethnicity. We also estimated a model that adjusted for obesity and self-rated health; however, their inclusion had little impact on the overall gender and racial/ethnic disparities in trajectories of sleep duration. Finally, we re-estimated all models after adjustment for survey year (in addition to age) as a way to account for potential period effects that may have occurred in response to the recession. The results were similar to those that we have presented. Given the correlation between age and survey year in the NLSY97 sample, we chose to present results using age as our measure of time because we believe that it better captures life course processes.
4. Discussion
The purpose of our study was to examine gender and racial/ethnic disparities in sleep duration during the early adult life course and to identify the educational experiences, employment characteristics, and family relationships that explained these sleep disparities across this developmental period. Results indicated that sleep duration declined across early adulthood; young adults reported sleeping approximately 3.3 fewer minutes with each additional year, from age 18 to age 31 years. Our results are consistent with cross-sectional studies that have reported declining sleep duration with increasing age [12,16,28], with some finding the steepest declines between 15 and 34 years of age [16].
Prior studies have documented a sleep advantage for women compared to men [10,12,16]. For example, Basner et al. found that, among a U.S. adult population, men slept less than women [12], a finding that was also documented using the National Health Interview Survey [10]. Our results suggest that this gender disparity emerges in early adulthood. As individuals in our sample transitioned into adulthood (~18–20 years of age), women reported sleeping less than men. The gender difference in sleep duration, however, narrowed during the early to mid-20s, and by age 28 years women reported sleeping longer than men. Being a student explained, in part, the gender disparities in reported sleep duration. In the United States, women are more likely than men to be enrolled in college during early adulthood [29]. Prior studies have found that college students often report inadequate and erratic sleep [30,31]. Being a college student may also increase stress, which has been linked to shorter and poorer quality sleep [31–33].
Conversely, accounting for being a parent, particularly of a young child, increased gender disparities in sleep duration. Social norms around child care suggest that women are expected to be responsible for the needs of others, especially children, and this caregiving responsibility often extends from the waking hours into the nighttime [21,23,34]. Parents’ sleep is often disrupted to address the needs of their children, and research has shown these disruptions occur at a higher rate for women than men [22]. Women also tend to go to bed earlier than men, perhaps because women set aside more time for sleep, knowing that they may be awakened in the night to care for others in the household [35]. Thus, women may begin to report longer sleep duration than men in early adulthood as they employ strategies to accommodate life changes, such as new parenthood, that impinge on their ability to have uninterrupted sleep.
Mounting evidence indicates that blacks tend to sleep less than whites [13–15]. We found that the well-documented black–white disparity in sleep duration emerges in early adulthood. At age 18 years, no significant racial/ethnic sleep disparities were observed, but by age 24, black young adults were sleeping about 4 fewer minutes, on average, than white young adults. This disparity widened to almost 13 minutes by age 30 years. College enrollment, educational attainment, and employment characteristics explained approximately 50% of the black–white disparity in sleep duration over early adulthood. Compared to whites, black young adults are less likely to be enrolled in college, to have a college degree, or to be employed full-time [36,37]. This corresponds to the black–white disparities that we found in trajectories of sleep duration; at the ages when college participation was higher, full-time employment was less common, and the black–white disparity in college degree attainment was at its narrowest (results available upon request): black young adults in our sample reported sleeping about the same amount as white young adults. As young adults transitioned out of college, completed their degrees, and began full-time employment, blacks reported less sleep than whites.
Living with a spouse/partner or child/children exacerbated black–white disparities in sleep duration. Across early adulthood, black respondents were more likely to have children residing in the household than white respondents, but were less likely to be living with a spouse/partner (results available upon request). This is consistent with black−white differences in family structure patterns observed in the broader U.S. population [38]. Having children in the household increases the risk for disrupted sleep [22,35], and this risk may be greater for blacks who are more likely to reside in single-parent households [38,39] where they are the only nighttime caregiver.
Black parents may also face greater stress from living with their children in unsafe places. Blacks are more likely to reside in adverse environments where they feel unsafe and are at greater risk for witnessing or experiencing violence and criminal activity [40]. Although adverse residential environmental conditions likely influence sleep in all populations, parents may be at greater risk as a result of their concerns for their children. One study of mothers of children 5 years of age and less who were living in a large urban area found that high exposure to neighborhood violence was associated with increased risk for sleeping fewer than 7 hours per night [41]. In a qualitative study of black mothers with infants, some of the mothers discussed the need to maintain active vigilance during the night to protect their children from the dangers and violence present in their living environments [42]. The additional stress of parenting in adverse environments may contribute to sleep disparities among young parents. In contrast to the well-documented black−white sleep disparity, population-based studies have not consistently found Latino−white sleep disparities. In our study, Latinos reported sleeping about the same amount as whites across early adulthood, but were less likely than whites to experience short sleep between 18 and 22 years of age. Ram et al. also found that Latinos and whites reported comparable levels of sleep duration [43], whereas Knutson et al. reported lower odds of short sleep for Latinos compared to whites [44]. Other studies, however, have documented higher odds of short sleep among some Latino ethnic groups compared to whites [10,11,45]. None of these studies focused exclusively on young adults, suggesting a need for additional studies that focus on the younger adult Latino population.
Our study has several limitations. First, sleep duration was self-reported, and the study assessed typical weeknight sleep but did not examine weekend sleep. Though U.S. adults often make up sleep on the weekends, this is especially the case among U.S. young adults [12]. Self-reported sleep duration has been shown to result in imprecise estimates of actual time spent sleeping compared to measured sleep obtained from actigraphy [26]. Thus, we may have underestimated sleep duration in our sample. Errors in self-reported sleep may be due to the cognitive complexity involved in determining one’s “typical” weeknight sleep duration. Some researchers have, however, found that sleep duration from self-reports of usual time spent sleeping on a weeknight and actigraphy are significantly correlated [46,47], and furthermore, that actigraphy and self-reported sleep measures are similarly correlated with polysomnography in healthy populations [48]. Comparing individuals with themselves over time likely minimizes the effects of underestimating sleep duration, particularly as it relates to our study’s objective: describing gender and racial/ethnic disparities in sleep trajectories. Second, our measure of sleep duration does not account for napping. Prior studies have found that women tend to make up for lost sleep during the day through naps [35]; thus, our results may have underestimated the amount of time that women slept overall. Third, data collection occurred before, during, and after the economic recession. Unemployment has been associated with longer sleep, and some groups were particularly hard hit during the recession, including young black men [49,50]. As a result, we may have underestimated gender and black–white sleep disparities, although supplemental analyses accounting for survey year did not alter our findings. Finally, the NLSY97 does not include detailed information on mental and physical health conditions that may contribute to shorter sleep or selection into specific roles, such as paid employment. We did include an adjustment for obesity status and self-rated health in supplemental analysis and found similar results to those we report. Our sample, however, is relatively young and healthy, so it is unlikely that underlying mental and physical health problems are contributing to our findings.
Despite these limitations, our study also has a number of strengths. We use a large, diverse, and nationally representative sample of individuals who were followed up across early adulthood. This allowed us to examine differences in sleep trajectories over time to determine when gender and racial/ethnic disparities emerge in the course of early adult life. We also focused on the key social roles and experiences that young adults must navigate during this developmental period that can alter sleeping patterns and habits and that may contribute to emerging disparities.
5. Conclusions
Although young adults are at high risk for inadequate sleep, few sleep studies have focused on this important period in the life course [30], and no studies, to our knowledge, have used prospective, population-based data to investigate the timing and explanations for the emergence of gender and racial/ethnic disparities in adulthood. Our study provides evidence that early adulthood is an important developmental period for understanding emerging gender and racial/ethnic sleep disparities, because it is in this stage of the life course when individuals are often exposed to new social activities (eg, college, work) and social roles (eg, spouse/partner, parenthood) that displace time for sleep.
Supplementary Material
Highlights.
Racial/ethnic and gender disparities in sleep duration are well documented.
Little is known about when these disparities in sleep duration emerge.
We estimated trajectories of sleep duration from ages 18 to 31 years among U.S. adults.
Women slept less than men until age 28 years, and thereafter slept more than men.
Racial/ethnic differences emerged at age 24 years, at which time individuals of black race/ethnicity slept less than those of white race/ethnicity.
ABBREVIATIONS
- GED
General Educational Development
- NLSY97
National Longitudinal Survey of Youth 1997
- SE
standard error
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Center for Sleep Disorders Research. National Institutes of Health: Sleep disorders research plan. Bethesda, MD: US Department of Health and Human Services; 2011. [Google Scholar]
- 2.National Research Council. Sleep disorders and sleep deprivation: An unmet public health problem. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 3.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–69. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 4.Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402–12. doi: 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knutson K, Ryden A, Mander B, et al. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006;166:1768–74. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- 6.Cappuccio FP, Cooper D, D'Elia L, et al. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Euro Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 7.Irwin M, Wang M, Campomayor C, et al. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med. 2006;166:1756–62. doi: 10.1001/archinte.166.16.1756. [DOI] [PubMed] [Google Scholar]
- 8.Kronholm E, Sallinen M, Suutama T, et al. Self-reported sleep duration and cognitive functioning in the general population. J Sleep Res. 2009;18:436–46. doi: 10.1111/j.1365-2869.2009.00765.x. [DOI] [PubMed] [Google Scholar]
- 9.Cappuccio FP, D'Elia L, Strazzullo P, et al. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krueger PM, Friedman EM. Sleep duration in the United States: A cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hale L, Do DP. Race differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basner M, Spaeth AM, Dinges DF. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep. 2014;37:1889–1906. doi: 10.5665/sleep.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams NJ, Grandner MA, Wallace DM, et al. Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep Med. 2016;18:103–7. doi: 10.1016/j.sleep.2015.02.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petrov ME, Lichstein KL. Differences in sleep between black and white adults: An update and future directions. Sleep Med. 2016;18:74–81. doi: 10.1016/j.sleep.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: The MultiEthnic Study of Atherosclerosis (MESA) Sleep. 2015;38:877–88. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basner M, Fomberstein KM, Razavi FM, et al. American Time Use Survey: Sleep time and its relationship to waking activities. Sleep. 2007;30:1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grandner MA, Schopfer EA, Sands-Lincoln M, et al. Relationship between sleep duration and body mass index depends on age. Obesity. 2015;23:2491–8. doi: 10.1002/oby.21247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shanahan MJ. Pathways to adulthood in changing societies: Variability and mechanisms in life course perspective. Annu Rev Sociol. 2000;26:667–92. [Google Scholar]
- 19.Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–80. [PubMed] [Google Scholar]
- 20.Grandner MA, Williams NJ, Knutson KL, et al. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Venn S, Arber S, Meadows R, et al. The fourth shift: Exploring the gendered nature of sleep disruption among couples with children. Br J Sociol. 2008;59:79–97. doi: 10.1111/j.1468-4446.2007.00183.x. [DOI] [PubMed] [Google Scholar]
- 22.Burgard SA. The needs of others: Gender and sleep interruptions for caregivers. Soc Forces. 2011;89:1189–1215. [Google Scholar]
- 23.Maume DJ, Sebastian RA, Bardo AR. Gender, work-family responsibilities, and sleep. Gend Soc. 2010;24:746–68. [Google Scholar]
- 24.Maume DJ, Sebastian RA, Bardo AR. Gender differences in sleep disruption among retail food workers. Am Sociol Rev. 2009;74:989–1007. [Google Scholar]
- 25.Jackson CL, Redline S, Kawachi I, et al. Racial disparities in short sleep duration by occupation and industry. Am J Epidemiol. 2013;178:1442–51. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 27.Ohayon MM, Smolensky MH, Roth T. Consequences of shiftworking on sleep duration, sleepiness, and sleep attacks. Chronobiol Int. 2010;27:575–89. doi: 10.3109/07420521003749956. [DOI] [PubMed] [Google Scholar]
- 28.Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 29.Buchmann C, DiPrete TA, McDaniel A. Gender inequalities in education. Annu Rev Sociol. 2008;34:319–37. [Google Scholar]
- 30.Wolfson AR. Adolescents and emerging adults' sleep patterns: New developments. J Adolesc Health. 2010;46:97–9. doi: 10.1016/j.jadohealth.2009.11.210. [DOI] [PubMed] [Google Scholar]
- 31.Lund HG, Reider BD, Whiting AB, et al. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124–32. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 32.Astill RG, Verhoeven D, Vijzelaar RL, et al. Chronic stress undermines the compensatory sleep efficiency increase in response to sleep restriction in adolescents. J Sleep Res. 2013;22:373–9. doi: 10.1111/jsr.12032. [DOI] [PubMed] [Google Scholar]
- 33.Linton SJ, Kecklund G, Franklin KA, et al. The effect of the work environment on future sleep disturbances: A systematic review. Sleep Med Rev. 2015;23:10–9. doi: 10.1016/j.smrv.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 34.Arber S, Hislop J, Bote M, et al. Gender roles and women's sleep in mid and later life: A quantitative approach. Sociol Res Online. 2007;12:3. [Google Scholar]
- 35.Burgard SA, Ailshire JA. Gender time for sleep among U.S. adults. Am Sociol Rev. 2013;78:51–69. doi: 10.1177/0003122412472048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Charles CZ, Roscigno VJ, Torres KC. Racial inequality and college attendance: The mediating role of parental investments. Soc Sci Res. 2007;36:329–52. [Google Scholar]
- 37.U.S. Bureau of Labor Statistics. Labor force characteristics by race and ethnicity, 2015. Washington, DC: U.S. Department of Labor; 2016. [Google Scholar]
- 38.Ruggles S. The origins of African-American family structure. Am Sociol Rev. 1994;59:136–51. [Google Scholar]
- 39.McLanahan S, Percheski C. Family structure and the reproduction of inequalities. Annu Rev Sociol. 2008;34:257–76. [Google Scholar]
- 40.Gee GC, Payne-Sturgis DC. Environmental health disparities: A framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112:1645–53. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnson SL, Solomon BS, Shields WC, et al. Neighborhood violence and its association with mothers’ health: Assessing the relative importance of perceived safety and exposure to violence. J Urban Health. 2009;86:538–50. doi: 10.1007/s11524-009-9345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joyner BL, Oden RP, Ajao TI, et al. Where should my baby sleep: A qualitative study of African American infant sleep location decisions. J Natl Med Assoc. 2010;102:881. doi: 10.1016/s0027-9684(15)30706-9. [DOI] [PubMed] [Google Scholar]
- 43.Ram S, Seirawan H, Kumar SK, et al. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14:63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 44.Knutson KL, Van Cauter E, Rathouz PJ, et al. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Whinnery J, Jackson N, Rattanaumpawan P, et al. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–7. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 47.Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: The Sleep Heart Health Study (SHHS) J Clin Sleep Med. 2007;3:622–30. [PMC free article] [PubMed] [Google Scholar]
- 48.Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med Rev. 2011;15:259–67. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 49.Engemann K, Wall HJ. The effects of recessions across demographic groups. Fed Reserve Bank of St. Louis Rev. 2010;92:1–26. [Google Scholar]
- 50.Kuehn D. The labor market performance of young black men in the great recession. Washington, DC: Urban Institute; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.