Abstract
Expanded use of nurse practitioners (NPs) and physician assistants (PAs) is a potential solution to workforce issues, but little is known about how NPs and PAs can best be used. Our study examines whether medical and social complexity of patients is associated with whether their primary care provider (PCP) type is a physician, NP, or PA. In this national retrospective cohort study, we use 2012-2013 national Veterans Administration (VA) electronic health record data from 374 223 veterans to examine whether PCP type is associated with patient, clinic, and state-level factors representing medical and social complexity, adjusting for all variables simultaneously using a generalized logit model. Results indicate that patients with physician PCPs are modestly more medically complex than those with NP or PA PCPs. For the group having a Diagnostic Cost Group (DCG) score >2.0 compared with the group having DCG <0.5, odds of having an NP or a PA were lower than for having a physician PCP (NP odds ratio [OR] = 0.83, 95% confidence interval [CI]: 0.79-0.88; PA OR = 0.85, CI: 0.80-0.89). Social complexity is not consistently associated with PCP type. Overall, we found minor differences in provider type assignment. This study improves on previous work by using a large national dataset that accurately ascribes the work of NPs and PAs, analyzing at the patient level, analyzing NPs and PAs separately, and addressing social as well as medical complexity. This is a requisite step toward studies that compare patient outcomes by provider type.
Keywords: Veterans Administration, nurse practitioner, physician assistant, primary care, health workforce
Background
New approaches to caring for patients with diabetes are needed due to projected increases in diabetes prevalence, suboptimal quality of diabetes care, the heavy cost burden of diabetes, and expected insufficient numbers of primary care physicians in coming years. In 2012, 12% of the US adult population had diabetes, and this figure is expected to reach 20% to 33% by 2050.1,2 Most patients receive care for their diabetes in primary care settings,3,4 but estimates of primary care physician shortfalls range as high as 31 000 by 2025.5 Many patients with diabetes do not meet quality standards for routine preventive care2 or achieve recommended disease control targets.6-8 Meanwhile, complications such as heart disease, kidney failure, amputations, and loss of vision contribute to the human and financial costs of the disease.9 In 2012, direct medical costs in the United States for diabetes care were approximately $176 billion.9
Innovative approaches to primary care, such as patient-centered medical home (PCMH) models and expanded use of nurse practitioners (NPs) and physician assistants (PAs), are being implemented to address these access, quality, and cost problems.10-15 PCMH models are a multifaceted approach to primary care designed to better meet the needs of patients with chronic disease. Expanded use of PAs and NPs is a common approach to address workforce deficiencies, both within and outside of PCMH models, but research demonstrating the most effective utilization of these professionals in primary care is scant.16
The Veterans Health Administration (VHA) system is in the vanguard of implementation of both strategies discussed above: adopting a PCMH model and expanding use of NPs and PAs in primary care. It is the largest US employer of PAs and NPs and has been a pioneer in adopting expansive roles for NPs and PAs.17-19 The VHA’s version of the medical home approach, called the Patient-Aligned Care Team (PACT) model, has now been implemented nationwide.14,20 Each PACT is led by an NP, PA, or physician who is responsible for the medical care of a panel of veterans.21,22
Patient characteristics might lead to preferential assignment to a PACT led by a particular type of provider. For example, it is possible that the most medically complex patients might be assigned to physicians due to physicians’ advanced medical training, or that patients with significant psychosocial needs might be assigned to NPs due to the NP profession’s training emphasis on psychosocial aspects of well-being.23,24 Previous research in the VHA and in other settings regarding associations of provider type with patient demographic and medical complexity factors has produced mixed results,16 but a number of studies have found that patients seeing physicians are slightly older and slightly more medically complex and that NPs are substantially more likely to see female patients.25-30
Patient assignment to a particular provider type might also be affected by facility or state-level contextual factors. There are no standard criteria for assigning veterans to particular primary care provider (PCP) types. Wide variations in use of NPs and PAs across VHA facilities are well documented,19,29 including by our 2010 analysis showing that the proportion of primary care visits attended by PAs or NPs varied across regional Veterans Integrated Service Networks (VISNs) from 14% to 42%.27 As a number of studies have shown that PAs and NPs are more likely to provide care in rural areas than are physicians,25,27,30,31 patients attending rural clinics might be more likely to be assigned to an NP or PA. There is also variation in the use of PAs and NPs by region and state. In an analysis of National Ambulatory Health Care Survey data, the proportion of nonfederal primary care physicians who reported working with an NP or PA in 2012 varied from as low as 35% in Georgia to as high as 90% in South Dakota and was higher in practices with more physicians and in multispecialty practices.32 State scope of practice (SOP) regulations may also affect the degree to which PAs and NPs are used in the VHA even though federal supremacy rules grant NPs and PAs somewhat wider SOP in the VHA than in other settings. PAs and NPs are more concentrated in states with less restrictive SOP regulations, although the causal direction of this relationship is unclear.33,34 The increased availability of NPs and PAs in these states might facilitate their uptake in the VHA, thereby affecting patients’ likelihood of receiving care from them.
New Contribution
This article analyzes patient, facility, and state characteristics associated with having a physician, NP, or PA as the VHA PCP for patients with diabetes, with a particular focus on the association between patient medical and social complexity and assigned provider type. Understanding factors associated with having a particular type of PCP is essential for primary care workforce planning. Although other studies have examined patient and facility characteristics associated with provider type, our study differs by being conducted within the largest integrated delivery system in the United States, which explicitly includes NPs and PAs as leaders of primary care teams. Unlike most other studies, our study examines continuous care of chronic disease over the course of 2 years and evaluates social complexity in addition to medical complexity and demographic factors.
Although the VHA population is predominantly male and on average older, sicker, and of lower socioeconomic status than the general population,35,36 our use of VHA data overcomes a number of obstacles to research comparing provider types. Most importantly, VHA electronic health record (EHR) data are the only longitudinal national data source that accurately ascribes care to PAs and NPs.37 In contrast, Medicare and Medicaid data are inaccurate for studying primary care PAs and NPs because their care is frequently subsumed under physician care due to billing practices (“incident to” billing).37 Use of a national data source was essential so that the effect of state-level factors, such as SOP regulations, could be examined.38 Finally, VHA data provide a broad range of variables for our examination and sufficient sample size (N = 377 579) to support statistical procedures.39,40
Examination of the similarities and differences of patients whose PCPs are physicians, NPs, or PAs is a requisite step toward conduct of studies comparing access, quality, and cost outcomes across provider types. Taken together, these studies may contribute to improvements in primary care of patients with diabetes.
Methods
Data Sources and Sample Construction
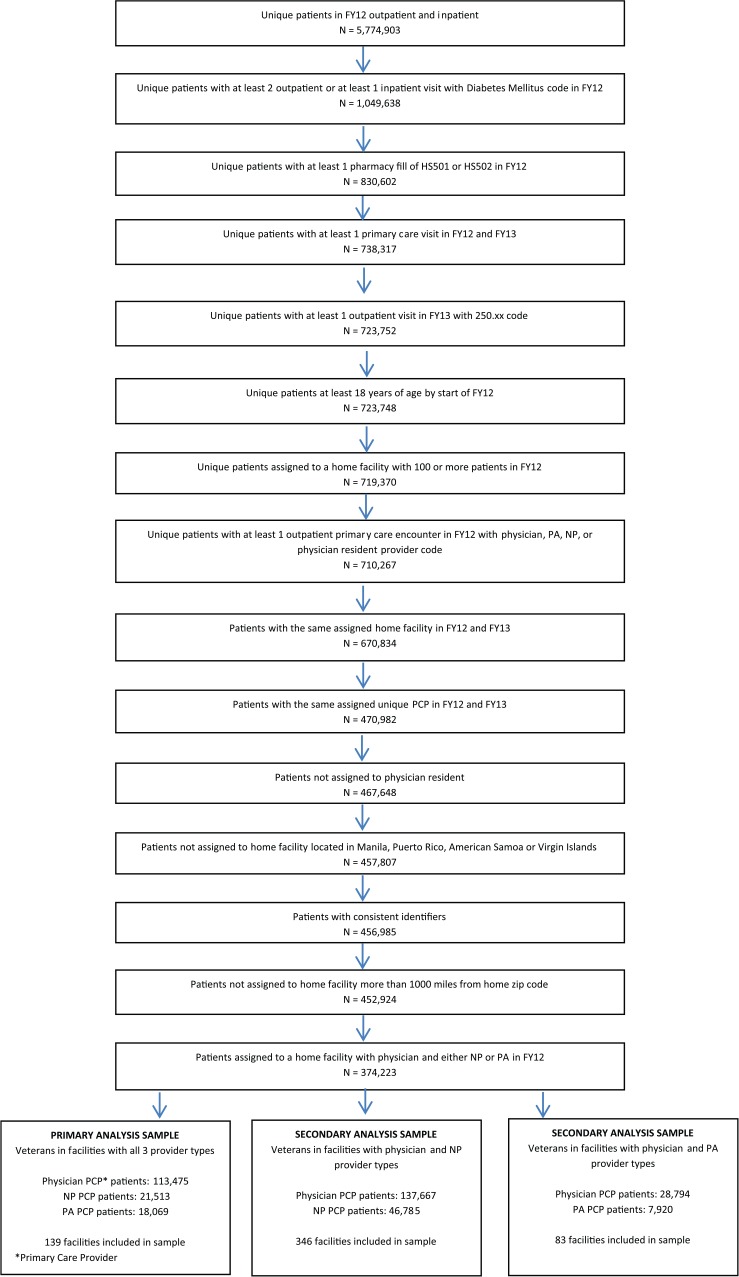
This cohort study used centrally available national VHA EHR data. The construction of the cohort is summarized in Figure 1. Our national sample consisted of adult, pharmaceutically treated diabetes patients seen within VHA primary care clinics. Specifically, patients must have had a diabetes diagnosis (International Classification of Diseases, Ninth revision [ICD-9] codes 250.xx) associated with at least 1 VHA inpatient visit and/or at least 2 VHA outpatient visits in fiscal year (FY) 2012 (October 1, 2011, to September 30, 2012; N = 1 049 638) and a filled prescription for insulin and/or an oral hyperglycemic agent (VHA drug classes HS501 or HS502) the same year (N = 830 602). These individuals had to have at least 1 VHA primary care visit in FY 2012 using VHA administrative codes indicating a primary care clinic (VHA stop codes 322, 323, 342, and 348). Patients were excluded if they did not also have an outpatient visit with a diabetes diagnosis in FY 2013 or were younger than 18 at the beginning of FY 2012. Each patient was assigned a “home” facility as the clinic most frequently visited for primary care in FY 2012. To be retained in the cohort, patients had to have a “home” facility with at least 100 cohort members in FY 2012 (remaining N = 719 370). The provider most often visited in the home VHA’s primary care clinic in FY 2012 was considered to be the veteran’s PCP. The same procedure was used to determine home clinic and PCP in FY 2013. To ensure consistency in the patient-provider relationship, we excluded veterans whose PCP assignment changed between 2012 and 2013. As our primary interest was on factors associated with type of nontrainee provider seen by VHA diabetic patients, we excluded patients who most frequently saw a physician resident. We also excluded patients whose home facility (whether a traditional facility or a community-based outpatient clinic [CBOC]) was over 1000 miles from their home zip code or was not in one of the 50 U.S. states or the District of Columbia (remaining N = 456 985).
Figure 1.
Primary care providers for veterans with diabetes mellitus cohort construction flow chart.
Note. PA = physician assistant; NP = nurse practitioner; PCP = primary care provider.
Our original planned analysis was to examine facilities in which all 3 provider types served as PCP for cohort patients. This remains our primary analysis. However, because only 139 of 823 facilities had patients with all 3 PCP types based on our algorithm of determining PCP, we decided to additionally examine associations within facilities that had only 2 PCP types as secondary analyses. Thus, in total, our analytic sample consisted of N = 374 223 patients from 568 facilities with at least 2 of 3 provider types. We created 3 nonoverlapping cohorts of patients in facilities with at least 2 types of providers serving PCP roles for patients in our cohort: (1) primary analysis—all 3 provider types (N = 153 057 from 139 facilities); (2) secondary analysis—physician and NP only (N = 184 452 from 346 facilities), and (3) secondary analysis—physician and PA only (N = 36 714 from 83 facilities).
Outcome
The outcome of interest is the type of PCP most frequently seen in FYs 2012-2013. This provider type could be an attending physician, NP, or PA. A patient’s PCP was considered to be the individual to whom the patient had the most primary care visits in FYs 2012-2013. If no PCP could be assigned (i.e., the patient saw multiple providers equally), the patient was excluded from the analysis.
Explanatory Variables Included in Multivariable Regression Analyses
Our choice of patient-level variables to examine for association with PCP type was informed by the determinants of health model developed by Evans and Stoddart.41 In Table 1, we map each of the patient-level variables in our study to the Evans and Stoddart categories and then modify the model by mapping the variables to the concepts of medical and social complexity that are central to our research question. The measures most relevant to medical complexity were age and the Diagnostic Cost Group (DCG) score, while most of the remaining variables measured social complexity. The DCG comorbidity measure was originally designed to predict cost of care but has been validated to measure medical complexity within the VHA population.42,43 The algorithm uses demographic and diagnostic information to assign each patient a DCG score, normed so that the average Medicare patient has a score equal to 1.44 All patient-level variables were constructed using VHA EHR data from FY 2012.
Table 1.
Rationale for Patient-Level Variable Selection.
| Determinants of health41 | Variables in our studya | Measures of medical complexity | Measures of social complexity |
|---|---|---|---|
| Social environment | Age | + | |
| Sex | |||
| Race | + | ||
| Ethnicity | + | ||
| Marital status | + | ||
| Distance from assigned station | + | ||
| Physical environment | Homelessness | + | |
| Prosperity | Copayment status based on povertyb | + | |
| Disease | + | ||
| Physical disease | VA medical complexity score (DCG)44 | + | |
| Mental disease | Psychiatric conditions (non-PTSD and nonmood disorders) | + | |
| PTSD | + | ||
| Mood disorders | + | ||
| Dementia | + | ||
| Behavior | Substance abuse | + | |
| Health and function | Copayment status based on disability | + |
Note. VA = Veterans Administration; DCG = Diagnostic Cost Group; PTSD = posttraumatic stress disorder.
The Evans and Stoddart model also includes categories for genetic factors and well-being. Variables representing these categories were not available for use in our study.
For determination of VA patient copay status, patients are first considered for exemption from copay on the basis of disability. If they do not qualify for exemption based on disability, they are considered for exemption based on poverty. Therefore, the group classified as “low income” variable does not represent low income disabled veterans.
Facility- and state-level contextual variables including multispecialty (vs single-specialty) nature of facilities, rural-urban status, and region have been associated with use of NPs and PAs.27,32 The proportion of providers in the facility who were PAs or NPs would also obviously affect the chance of a patient being assigned to NP or PA care. Variables representing these characteristics were examined, as shown in Table 2. The availability of endocrinology referrals within the facility was included as a proxy for facility complexity and multispecialty availability for diabetes care. The proportion of providers who were PAs or NPs and the presence of endocrinology and/or specialty diabetes services at a facility (defined as providing 500 or more such visits in FY 2012) were calculated using our analytic dataset. Facility-level rural-urban status was based on the ZIP code version of the Rural Urban Community Area (RUCA) codes.45 Region of facility is designated as assigned by the VHA.
Table 2.
Characteristics of VHA Patients With Diabetes by Primary Care Provider Type Assigned in Facilities With Physicians, NPs, and PAs.
| Category | Physician-assigned provider (n = 113 475) | NP-assigned provider (n = 21 513) | PA-assigned provider (n = 18 069) | Total (N = 153 057) |
|---|---|---|---|---|
| Patient-level factors | ||||
| Male | 109 746 (96.71) | 20 100 (93.43) | 17 600 (97.40) | 147 446 (96.33) |
| Age group | ||||
| Less than 40 | 1068 (0.94) | 274 (1.27) | 193 (1.07) | 1535 (1.00) |
| 40 to less than 65 | 58 634 (51.67) | 11 076 (51.49) | 9118 (50.46) | 78 828 (51.50) |
| 65 to less than 80 | 43 190 (38.06) | 8178 (38.01) | 7055 (39.04) | 58 423 (38.17) |
| 80 and above | 10 583 (9.33) | 1985 (9.23) | 1703 (9.42) | 14 271 (9.32) |
| Race | ||||
| White | 76 326 (67.26) | 15 235 (70.82) | 13 074 (72.36) | 104 635 (68.36) |
| American Indian | 864 (0.76) | 206 (0.96) | 130 (0.72) | 1200 (0.78) |
| Asian | 453 (0.40) | 119 (0.55) | 51 (0.28) | 623 (0.41) |
| Black | 25 664 (22.62) | 3950 (18.36) | 3268 (18.09) | 32 882 (21.48) |
| Native Hawaiian | 1260 (1.11) | 209 (0.97) | 132 (0.73) | 1601 (1.05) |
| Unknown or Missing | 8908 (7.85) | 1794 (8.34) | 1414 (7.83) | 12 116 (7.92) |
| Hispanic | 5870 (5.17) | 786 (3.65) | 711 (3.93) | 7367 (4.81) |
| Marital status | ||||
| Currently married | 66 521 (58.62) | 12 439 (57.82) | 10 951 (60.61) | 89 911 (58.74) |
| Never married | 13 532 (11.93) | 2556 (11.88) | 1880 (10.40) | 17 968 (11.74) |
| Previously married | 33 218 (29.27) | 6436 (29.92) | 5197 (28.76) | 44 851 (29.30) |
| Unknown marital status | 204 (0.18) | 82 (0.38) | 41 (0.23) | 327 (0.21) |
| Homeless at any time during year | 2395 (2.11) | 517 (2.40) | 298 (1.65) | 3210 (2.10) |
| Copay status | ||||
| No copay due to disability | 62 865 (55.40) | 11 520 (53.55) | 9674 (53.54) | 84 059 (54.92) |
| No copay due to low income | 30 228 (26.64) | 5656 (26.29) | 4750 (26.29) | 40 634 (26.55) |
| Must pay copay | 18 843 (16.61) | 3871 (17.99) | 3420 (18.93) | 26 134 (17.07) |
| Copay status unknown | 1539 (1.36) | 466 (2.17) | 225 (1.25) | 2230 (1.46) |
| Mental health diagnoses | ||||
| Mood disorder | 27 424 (24.17) | 5372 (24.97) | 4233 (23.43) | 37 029 (24.19) |
| Posttraumatic stress disorder | 16 106 (14.19) | 3169 (14.73) | 2494 (13.80) | 21 769 (14.22) |
| Dementia | 3669 (3.23) | 611 (2.84) | 560 (3.10) | 4840 (3.16) |
| Substance abuse | 9142 (8.06) | 1736 (8.07) | 1260 (6.97) | 12 138 (7.93) |
| Other mental health diagnosis | 6888 (6.07) | 1396 (6.49) | 1088 (6.02) | 9372 (6.12) |
| DCG score category | ||||
| Less than or equal to 0.5 | 54 258 (47.81) | 10 732 (49.89) | 9199 (50.91) | 74 189 (48.47) |
| Greater than 0.5 to 1 | 18 439 (16.25) | 3650 (16.97) | 2966 (16.41) | 25 055 (16.37) |
| Greater than 1 to 1.5 | 15 305 (13.49) | 2932 (13.63) | 2386 (13.20) | 20 623 (13.47) |
| Greater than 1.5 to 2 | 8772 (7.73) | 1502 (6.98) | 1303 (7.21) | 11 577 (7.56) |
| Greater than 2 | 16 701 (14.72) | 2697 (12.54) | 2215 (12.26) | 21 613 (14.12) |
| Distance from VHA primary care clinic | ||||
| Less than 5 miles | 22 697 (20.00) | 4885 (22.71) | 4070 (22.52) | 31 652 (20.68) |
| 5 to less than 25 miles | 61 486 (54.18) | 10 486 (48.74) | 8633 (47.78) | 80 605 (52.66) |
| 25 to less than 50 miles | 18 766 (16.54) | 3903 (18.14) | 3440 (19.04) | 26 109 (17.06) |
| 50 miles and more | 9845 (8.68) | 1941 (9.02) | 1822 (10.08) | 13 608 (8.89) |
| Missing | 681 (0.60) | 298 (1.39) | 104 (0.58) | 1083 (0.71) |
| Facility-level factors | ||||
| Endocrinology referral capacitya | 81 168 (71.53) | 12 596 (58.55) | 9748 (53.95) | 103 512 (67.63) |
| Percent of providers in primary care clinic who are PAs | ||||
| Lowest tertile | 57 330 (50.52) | 10 381 (48.25) | 2911 (16.11) | 70 622 (46.14) |
| Middle tertile | 39 196 (34.54) | 6701 (31.15) | 6170 (34.15) | 52 067 (34.02) |
| Highest tertile | 16 949 (14.94) | 4431 (20.60) | 8988 (49.74) | 30 368 (19.84) |
| Percent of providers in primary care clinic who are NPs | ||||
| Lowest tertile | 56 452 (49.75) | 2729 (12.69) | 7696 (42.59) | 66 877 (43.69) |
| Middle tertile | 39 556 (34.86) | 8310 (38.63) | 7104 (39.32) | 54 970 (35.91) |
| Highest tertile | 17 467 (15.39) | 10 474 (48.69) | 3269 (18.09) | 31 210 (20.39) |
| Rural-urban commuting area status | ||||
| Metropolitan area core | 99 992 (88.12) | 18 798 (87.38) | 14 037 (77.69) | 132 827 (86.78) |
| Metropolitan area core—remaining levels | 8992 (7.92) | 1343 (6.24) | 1882 (10.42) | 12 217 (7.98) |
| Micropolitan area core | 3948 (3.48) | 1208 (5.62) | 1810 (10.02) | 6966 (4.55) |
| Small town or rural | 543 (0.48) | 164 (0.76) | 340 (1.88) | 1047 (0.68) |
| State-level factors | ||||
| Region | ||||
| Northeast | 15 259 (13.45) | 3420 (15.90) | 3500 (19.37) | 22 179 (14.49) |
| West | 13 465 (11.87) | 4997 (23.23) | 2404 (13.30) | 20 866 (13.63) |
| Midwest | 33 050 (29.13) | 7181 (33.38) | 5116 (28.31) | 45 347 (29.63) |
| South | 51 701 (45.56) | 5915 (27.50) | 7049 (39.01) | 64 665 (42.25) |
| Percent of primary care physicians who work with NPs/PAs | ||||
| Lowest tertile | 61 335 (54.05) | 8945 (41.58) | 7982 (44.18) | 78 262 (51.13) |
| Middle tertile | 28 495 (25.11) | 7006 (32.57) | 5426 (30.03) | 40 927 (26.74) |
| Highest tertile | 23 645 (20.84) | 5562 (25.85) | 4661 (25.80) | 33 868 (22.13) |
| Physician assistant scope of practice regulations | ||||
| Least restrictive | 18 390 (16.21) | 3762 (17.49) | 3221 (17.83) | 25 373 (16.58) |
| Moderately restrictive | 21 307 (18.78) | 4600 (21.38) | 3564 (19.72) | 29 471 (19.25) |
| Most restrictive | 73 778 (65.02) | 13 151 (61.13) | 11 284 (62.45) | 98 213 (64.17) |
| Nurse practitioner scope of practice regulations | ||||
| Least restrictive | 14 084 (12.41) | 5226 (24.29) | 2824 (15.63) | 22 134 (14.46) |
| Moderately restrictive | 15 546 (13.70) | 2905 (13.50) | 2385 (13.20) | 20 836 (13.61) |
| Most restrictive | 83 845 (73.89) | 13 382 (62.20) | 12 860 (71.17) | 110 087 (71.93) |
Note. Data for patient-level variables are from the VA electronic health record files. Other data sources are described in the “Methods” section. PCP is assigned as the physician, NP, or PA seen most during FY 2012 and 2013. VA = Veterans Administration; NP = nurse practitioner; PA = physician assistant; DCG = Diagnostic Cost Group; VHA = Veterans Health Administration; PCP = primary care provider; FY = fiscal year.
Endocrinology referral capacity is defined as either present (endocrinology or other diabetes mellitus specialty clinics provided 500 or more visits to cohort patients in FY 2012) or absent (fewer than 500 visits to cohort patients).
Additional state-level contextual variables were examined. The proportion of primary care physicians within a state who report working with NPs or PAs was obtained from an analysis of the National Ambulatory Medical Care Survey by Hing and Hsiao.32 This variable was included to reflect the level of acceptance and uptake of PAs and NPs in the state. NP SOP ratings were obtained from the 2012 Pearson Report, with the most restrictive SOP environment requiring physician involvement for an NP to prescribe, diagnose, or treat, the moderately restrictive environment requiring physician involvement for an NP to prescribe medications, and the least restrictive environment requiring no physician involvement.46 PA SOP regulation scores were calculated by the authors using a tabulation of recommended key elements (“licensure” as the regulatory term, full prescriptive authority, SOP and chart cosignature requirements determined at the practice level, adaptable collaboration rules, and no restriction on the number of PAs a physician can supervise) assembled by the American Academy of Physician Assistants, with presence of 3 key elements indicating the most restrictive SOP, 4 elements indicating moderately restrictive SOP, and 5 to 6 elements categorized as the least restrictive SOP.47
Statistical Analysis
We examined the association of PCP types (ie, physicians, NP, or PA) with all patient-level, facility-level, and state-level variables simultaneously using a generalized logit model for the main analysis with all 3 provider types; logistic regression was used for the 2 secondary analyses. In all models, a facility-level random intercept was included to account for clustering within clinics. Covariates were specified a priori and entered into the model simultaneously after examination for collinearity by evaluating frequency cross-tabulations and cluster analysis results using the SAS VARCLUS procedure. All analyses set statistical significance at P < .05 and were conducted using SAS 9.4 (Copyright 2013, SAS Institute Inc., Cary, North Carolina).
The study was approved by the Institutional Review Board of the Durham Veterans Affairs Medical Center.
Results
Providers and Clinics of VHA Patients With Diabetes Mellitus
Among 5,774,903 VHA patients seen in FY 2012, 830,602 (14.4%) individuals met our diagnostic criteria for pharmacologically treated diabetes mellitus. Among diabetic patients for whom we could assign a nonresident PCP (456,985 patients in 823 facilities), physicians were the most frequent PCP type (78%), followed by NPs (16%) and PAs (6%).Among these 823 facilities, 17% (n = 139) had all 3 types of providers, 42% (n = 346) had only physicians and NPs, and 10% (n = 83) had only physicians and PAs (see Figure 1). Patients in the remaining 255 facilities were excluded from our analytic sample because they only had 1 provider type represented and/or did not have any physicians represented in the data. It is important to remember that these clinics might have employed physicians or other provider types who did not appear in our study because none of their patients met our study inclusion criteria.
Characteristic of Diabetic Patients in Our Analytic Sample
Our primary analysis was among the subset of clinics that had all 3 provider types (physician, NP, and PA) serving as PCPs for patients. This subset comprised 139 clinics with 153,057 patients, representing 41% of patients in our analytic sample. Among these clinics, physicians were the PCP for 74% of cohort patients, NPs were the PCP for 14%, and PAs were the PCP for 12%. Characteristics of the patients in this subset are shown in Table 2, and characteristics of the remaining 2 subsets in our secondary analyses (patients attending clinics with only physicians and NPs serving as PCPs for cohort patients and patients attending clinics with only physicians and PAs serving as PCPs for cohort patients) are presented in the appendix.
Like the general VHA population, the patients with diabetes who attended clinics with all 3 provider types are predominantly male (96%) and older (47% aged 65 and above) than the general US population. They are medically and socially complex, with relatively high rates of mental health disorders (mood disorders 24%, posttraumatic stress disorder [PTSD] 14%, and substance abuse 8%), homelessness (2%), and exemption from copays due to disability (55%) or due to low income (26%). Compared with patients attending clinics with only 2 provider types serving as PCPs for cohort patients (Appendix A), patients attending clinics with all 3 provider types serving as PCPs for cohort patients are more urban (87%), more likely to be located in the South (42%) and Midwest (30%), and more likely to be African American (21%).
Factors Associated With PCP Type
In facilities where all 3 provider types cared for cohort patients, after adjustment for all other factors, the odds of having an NP or PA as PCP steadily declined as complexity and age increased (Table 3). For the group with the highest DCG score (>2.0) compared with the group with the lowest (0-0.5), the odds ratio (OR) of having an NP PCP compared with a physician was 0.83 (95% confidence interval [CI]: 0.79-0.88) and for having a PA compared with a physician was also 0.85 (CI: 0.80-0.89). For the oldest age group compared with the youngest, the OR for having an NP PCP was 0.67 (CI: 0.57-0.79) and the OR for having a PA PCP was 0.67 (CI: 0.56-0.79). Similar patterns were found in the clinics with only 2 provider types (Appendix A).
Table 3.
ORs for Predicting Assignment to a Primary Care Provider Who Is an NP or PA, Compared With Physician Among Facilities With Physician, NP, and PA Provider Types.
| Effect and level | OR for assignment to NP | 95% CI for assignment to NP | P value for assignment to NP | OR for assignment to PA | 95% CI for assignment to PA | P value for assignment to PA |
|---|---|---|---|---|---|---|
| Patient-level factors | ||||||
| Male | 0.42 | 0.39-0.45 | <.001 | 1.28 | 1.14-1.43 | <.001 |
| Age group | ||||||
| Less than 40 | Reference | Reference | Reference | Reference | ||
| 40 to less than 65 | 0.74 | 0.63-0.85 | <.001 | 0.75 | 0.63-0.88 | <.001 |
| 65 to less than 80 | 0.72 | 0.62-0.83 | <.001 | 0.73 | 0.62-0.87 | <.001 |
| 80 and above | 0.67 | 0.57-0.79 | <.001 | 0.67 | 0.56-0.79 | <.001 |
| Race | ||||||
| White | Reference | Reference | Reference | Reference | ||
| American Indian | 1.00 | 0.84-1.18 | .956 | 1.00 | 0.82-1.21 | .962 |
| Asian | 1.04 | 0.83-1.30 | .730 | 1.05 | 0.77-1.42 | .768 |
| Black | 1.01 | 0.96-1.06 | .705 | 1.09 | 1.04-1.15 | <.001 |
| Native Hawaiian | 1.00 | 0.85-1.18 | .979 | 0.81 | 0.67-0.98 | .033 |
| Unknown or Missing | 1.02 | 0.96-1.09 | .431 | 1.02 | 0.95-1.09 | .620 |
| Hispanic | 0.95 | 0.87-1.04 | .273 | 1.03 | 0.95-1.13 | .449 |
| Marital status | ||||||
| Currently married | Reference | Reference | Reference | Reference | ||
| Never married | 1.02 | 0.96-1.07 | .539 | 1.02 | 0.96-1.08 | .447 |
| Previously married | 1.04 | 1.00-1.07 | .068 | 1.04 | 1.00-1.08 | .048 |
| Unknown marital status | 1.49 | 1.13-1.97 | .005 | 1.23 | 0.86-1.76 | .254 |
| Homeless at any time during year | 1.16 | 1.04-1.29 | .007 | 1.09 | 0.95-1.24 | .225 |
| Copay status | ||||||
| Must pay copay | Reference | Reference | Reference | Reference | ||
| No copay due to disability | 0.94 | 0.90-0.98 | .008 | 0.94 | 0.90-0.99 | .013 |
| No copay due to low income | 0.96 | 0.91-1.01 | .130 | 0.96 | 0.91-1.01 | .093 |
| Unknown copay status | 1.04 | 0.89-1.21 | .600 | 0.92 | 0.77-1.10 | .356 |
| Mental health diagnoses | ||||||
| Mood disorder | 1.01 | 0.96-1.05 | .785 | 0.99 | 0.95-1.04 | .747 |
| PTSD | 1.05 | 1.00-1.10 | .076 | 1.02 | 0.96-1.07 | .538 |
| Dementia | 0.89 | 0.80-0.98 | .021 | 0.99 | 0.89-1.10 | .808 |
| Substance abuse | 1.11 | 1.04-1.18 | .001 | 1.01 | 0.94-1.08 | .827 |
| Other mental health diagnosis | 1.19 | 1.11-1.28 | <.001 | 1.09 | 1.01-1.17 | .035 |
| DCG score category | ||||||
| Less than or equal to 0.5 | Reference | Reference | Reference | Reference | ||
| Greater than 0.5 to 1 | 1.00 | 0.95-1.04 | .880 | 0.96 | 0.92-1.01 | .110 |
| Greater than 1 to 1.5 | 0.95 | 0.91-1.00 | .060 | 0.95 | 0.90-1.00 | .041 |
| Greater than 1.5 to 2 | 0.86 | 0.81-0.92 | <.001 | 0.92 | 0.86-0.99 | .022 |
| Greater than 2 | 0.83 | 0.79-0.88 | <.001 | 0.85 | 0.80-0.89 | <.001 |
| Distance from VHA primary care clinic | ||||||
| Less than 5 miles | Reference | Reference | Reference | Reference | ||
| 5 to less than 25 miles | 1.00 | 0.96-1.04 | .982 | 1.04 | 0.99-1.09 | .082 |
| 25 to less than 50 miles | 1.04 | 0.99-1.10 | .121 | 1.09 | 1.03-1.15 | .003 |
| 50 miles or greater | 1.00 | 0.94-1.07 | .982 | 1.15 | 1.07-1.23 | <.001 |
| Missing | 1.72 | 1.40-2.11 | <.001 | 1.37 | 1.05-1.79 | .021 |
| Facility-level factors | ||||||
| Endocrinology referral capacitya | 0.87 | 0.68-1.12 | .284 | 0.80 | 0.62-1.04 | .097 |
| Percent of providers in the primary care clinic who are PAs | ||||||
| Lowest tertile | Reference | Reference | Reference | Reference | ||
| Middle tertile | 1.05 | 0.79-1.40 | .724 | 4.40 | 3.29-5.89 | <.001 |
| Highest tertile | 1.63 | 1.20-2.22 | .002 | 18.19 | 13.32-24.84 | <.001 |
| Percent of providers in the primary care clinic who are NPs | ||||||
| Lowest tertile | Reference | Reference | Reference | Reference | ||
| Middle tertile | 6.35 | 4.65-8.66 | <.001 | 1.14 | 0.84-1.55 | .413 |
| Highest tertile | 21.54 | 15.80-29.38 | <.001 | 1.71 | 1.26-2.33 | <.001 |
| Rural-urban commuting area status | ||||||
| Metropolitan area core | Reference | Reference | Reference | Reference | ||
| Metropolitan area core—remaining levels | 0.97 | 0.63-1.48 | .884 | 0.90 | 0.59-1.37 | .620 |
| Micropolitan area core | 1.07 | 0.69-1.65 | .773 | 1.10 | 0.71-1.70 | .662 |
| Small town or rural | 1.32 | 0.60-2.88 | .492 | 1.47 | 0.66-3.29 | .345 |
| State-level factors | ||||||
| Region | ||||||
| Northeast | Reference | Reference | Reference | Reference | ||
| West | 0.72 | 0.46-1.11 | .137 | 0.60 | 0.38-0.93 | .024 |
| Midwest | 0.69 | 0.48-0.98 | .039 | 0.79 | 0.55-1.13 | .193 |
| South | 0.86 | 0.60-1.22 | .389 | 0.88 | 0.62-1.26 | .483 |
| Percent of primary care physicians who work with NPs/PAs | ||||||
| Lowest tertile | Reference | Reference | Reference | Reference | ||
| Middle tertile | 1.07 | 0.76-1.53 | .687 | 0.84 | 0.59-1.19 | .330 |
| Highest tertile | 1.35 | 0.91-2.00 | .139 | 1.03 | 0.69-1.54 | .869 |
| Nurse practitioner scope of practice regulations | ||||||
| Lowest tertile | Reference | Reference | Reference | Reference | ||
| Moderately restrictive | 0.75 | 0.45-1.26 | .276 | 1.05 | 0.63-1.76 | .852 |
| Most restrictive | 1.12 | 0.74-1.71 | .592 | 0.90 | 0.59-1.38 | .623 |
| Physician assistant scope of practice regulations | ||||||
| Lowest tertile | Reference | Reference | Reference | Reference | ||
| Moderately restrictive | 1.20 | 0.78-1.83 | .402 | 1.13 | 0.74-1.74 | .561 |
| Most restrictive | 1.15 | 0.79-1.66 | .460 | 1.15 | 0.79-1.67 | .457 |
Note. Data for patient-level variables are from the VA electronic health record files. Other data sources are described in the “Methods” section. PCP is assigned as the physician, NP, or PA seen most during FY 2012 and 2013. OR = odds ratio; NP = nurse practitioner; CI = confidence interval; PA = physician assistant; PTSD = posttraumatic stress disorder; DCG = Diagnostic Cost Group; VHA = Veterans Health Administration; PCP = primary care provider; FY = fiscal year.
Endocrinology referral capacity is defined as either present (endocrinology or other diabetes mellitus specialty clinics provided 500 or more visits to cohort patients in FY 2012) or absent (fewer than 500 visits to cohort patients).
Many of the variables indicating social complexity (race, ethnicity, marital status, not being required to pay a VHA copayment due to low income, rural clinic locations, and diagnosis of a mood disorder, PTSD, or dementia) did not show statistically significant differences in the odds of having a particular provider type after adjustment for the other variables. Among variables that did have statistically significant differences, the differences were relatively small. For example, the odds of a patient seeing either an NP or a PA as his or her PCP were about 6% lower than the odds of seeing a physician for patients exempt from copays due to disability compared with those making copayments (NP OR = 0.94, CI: 0.90-0.98; PA OR = 0.94, CI: 0.90-0.99). Similarly, the odds of a patient seeing an NP as his or her PCP were 15% higher than those of seeing a physician for homeless patients (OR = 1.16, CI: 1.04-1.29) and 11% higher for patients with a substance abuse diagnosis (OR = 1.11, CI: 1.04-1.18). PAs were more likely than physicians to see patients with long commutes to their primary care clinic compared with those who lived within 5 miles (OR = 1.15, CI: 1.07-1.23).
In clinics with all 3 provider types caring for cohort patients, NPs were notably less likely to be the PCP for male patients than were physicians (OR = 0.42, CI: 0.39-0.45) and PAs were more likely than physicians to be the PCP for males (OR = 1.28, CI: 1.14-1.43). This pattern held in the secondary analysis of the subset of clinics that had only NPs and physicians as PCPs (OR for males vs females seeing an NP PCP compared with a physician = 0.46, CI: 0.43-0.49). In clinics without NPs, however, this pattern changed, with PAs much less likely than physicians to be the PCP for men (OR = 0.65, CI: 0.54-0.78; Appendix B).
The largest ORs in our regression models were for the proportions of NPs and PAs in the facilities, an obvious result of the necessity of a provider type being present in order for them to be the PCP for a patient. In our primary analysis, the other facility-level factors we examined (availability of endocrine referrals and rural-urban status) did not show statistically significant differences in the odds of having an NP or PA PCP compared with physicians.
Among the state-level variables, we found a lower odds of having an NP than physician provider in the midwest compared with the northeast (OR = 0.69, CI: 0.48-0.98) and a lower odds of having a PA than physician provider in the west, compared with the northeast (OR = 0.60, CI: 0.38-0.93). Neither the percent of primary care physicians in the state who work with NPs or PAs nor state-level SOP regulations were associated with provider type after controlling for all of the factors in our model.
Discussion
The VHA uses NPs and PAs extensively as PCPs for patients with chronic diseases such as diabetes, many of whom are medically and socially complex. NPs are used to a greater extent than PAs as PCPs for veterans with diabetes, a trend that mirrors national primary care staffing patterns and might also reflect the larger size of the NP workforce compared with the PA workforce.48 We found substantial variation among facilities in provider types used, with many facilities having only NPs and physicians as PCPs for patients in our cohort while others had only PAs and physicians.
The modest magnitude of the differences we found in PCP type assignment is consistent with previous research suggesting that physicians, NPs, and PAs functioning in similar roles in similar environments tend to care for similar types of patients and provide similar types of care.27,30,49-51 For example, although we found that the most medically complex VHA primary care patients with diabetes mellitus (DCG score >2.0) had about 15% higher odds of having a physician PCP than an NP or PA, there was considerable overlap of patient complexity scores among provider types. While 15% of physician patients were in the most medically complex group, 12% to 13% of PA and NP patients were also in this most complex category.
After controlling for all other factors, including medical complexity, older patients were more likely to have a physician PCP. It is possible that this is due to components of medical complexity that are not completely captured by the DCG score. Alternative explanations are that they might have had a physician PCP for years, before NPs and PAs were commonly used as PCPs, or that older patients prefer physician care. Our study did not address patient preference, but there is some evidence that older patients may be more inclined to choose a physician over an NP or PA when they are given an option.52
Social complexity factors were not consistently associated with a particular PCP type. While some statistically significant differences were observed, the magnitude of such differences was small, indicating that social complexity is not a major driver of PCP type.
Although not related to medical or social complexity directly, the gender differences in PCP type are notable. The VHA has women’s health clinics which serve as primary care clinics for many women veterans.53 Due to evidence that outcomes are best when women providers provide primary care to women veterans,54 these clinics might have been preferentially staffed by NPs, who are overwhelmingly female (93% female in 2012).55 Perhaps NPs are also preferentially hired to staff these clinics due to the traditional strong role of NPs in women’s health. It is not clear why PAs seem to fill the role of PCP for women veterans when NPs are not present, although the PA profession has a larger proportion of female providers (66%)56 compared with the physician profession (33%).57
Other than some minimal regional associations, state-level factors were not associated with PCP provider type. Our finding that the type of PCP assigned to a patient was not affected by state SOP is consistent with recent findings that SOP regulations were not associated with productivity in the VHA58 or with practice patterns and care quality in Community Health Centers.59
Strengths and Limitations
Unlike most previous studies which analyze discrete patient encounters or episodes of care for acute uncomplicated conditions, our study evaluated PCP type for chronic disease care over the course of 2 years. This approach is appropriate as analyzing isolated patient encounters or discrete episodes of care is inherently limited for studying primary care for chronic conditions—an enterprise which is by nature continuous and comprehensive. Our approach is also timely as provision of continuous and comprehensive chronic disease care is a central challenge facing the VHA and US health care system as a whole.60 Strengths of our data source include accurate attribution of care of each patient to a particular provider, an attribute missing in many commonly used data sources.37
Our study analyzed only face-to-face visits with the PCP, but PACT implementation in the VHA has been associated with large increases in non-face-to-face encounters such as phone and electronic communication.61 While it is possible that inclusion of these encounters might have affected our assignment of patients to providers, many of the non-face-to-face encounters are provided by nurses or other clinicians not acting in a PCP role.61 In addition, PCMH models such as the PACT model emphasize care by the entire team, while our study focuses only on the presumptive team leader. Finally, our study did not have information on some factors that might affect PCP type assignment, such as patient preferences.62
Conclusions
The question of how to best use physicians, NPs, and PAs in primary care is of key importance in the VHA as well as in other health organizations. This study contributes a crucial first step in addressing this question, by examining factors associated with patient assignment by provider type. We found that more medically complex patients had slightly higher odds of having a physician as compared with an NP or PA PCP, but associations of social complexity factors with provider type were modest and inconsistent. Future work will compare quality and cost outcomes by provider type, controlling for the case mix factors we have identified.
Appendix
Appendix A.
Characteristics of VA Patients With Diabetes by Primary Care Provider Type Assigned in Facilities With Either Physicians and NPs or Physicians and PAs Assigned.
| Category | Clinics with only physicians and NPs assigned as PCPs |
Clinics with only physicians and PAs assigned as PCPs |
||||
|---|---|---|---|---|---|---|
| Physician-assigned provider (n = 137 667) | NP-assigned provider (n = 46 785) | Total (N = 184 452) | Physician-assigned provider (n = 28 794) | PA-assigned provider (n = 7920) | Total (N = 36 714) | |
| Patient-level factors | ||||||
| Male | 133 933 (97.3) | 44 778 (95.7) | 178 711 (96.9) | 28 004 (97.3) | 7655 (96.7) | 35 659 (97.1) |
| Age group | ||||||
| Less than 40 | 1219 (0.89) | 450 (0.96) | 1669 (0.90) | 214 (0.74) | 67 (0.85) | 281 (0.77) |
| 40 to less than 65 | 70 337 (51.1) | 23 393 (50.0) | 93 730 (50.8) | 14 235 (49.4) | 3743 (47.3) | 17 978 (49.0) |
| 65 to less than 80 | 53 202 (38.6) | 18 256 (39.0) | 71 458 (38.7) | 11 459 (39.8) | 3221 (40.7) | 14 680 (40.0) |
| 80 and above | 12 909 (9.38) | 4686 (10.0) | 17 595 (9.54) | 2886 (10.0) | 889 (11.2) | 3775 (10.3) |
| Race | ||||||
| White | 97 508 (70.8) | 34 284 (73.3) | 131 792 (71.5) | 22 222 (77.2) | 6393 (80.7) | 28 615 (77.9) |
| American Indian | 890 (0.65) | 273 (0.58) | 1163 (0.63) | 192 (0.67) | 66 (0.83) | 258 (0.70) |
| Asian | 1067 (0.78) | 171 (0.37) | 1238 (0.67) | 48 (0.17) | 26 (0.33) | 74 (0.20) |
| Black | 24 544 (17.8) | 7797 (16.7) | 32 341 (17.5) | 3826 (13.3) | 715 (9.03) | 4541 (12.4) |
| Native Hawaiian | 1657 (1.20) | 404 (0.86) | 2061 (1.12) | 295 (1.02) | 98 (1.24) | 393 (1.07) |
| Unknown or Missing | 12 001 (8.72) | 3856 (8.24) | 15 857 (8.60) | 2211 (7.68) | 622 (7.85) | 2833 (7.72) |
| Hispanic | 6544 (4.75) | 1786 (3.82) | 8330 (4.52) | 900 (3.13) | 210 (2.65) | 1110 (3.02) |
| Marital status | ||||||
| Currently married | 82 405 (59.9) | 28 156 (60.2) | 110 561 (59.9) | 18 452 (64.1) | 5113 (64.6) | 23 565 (64.2) |
| Never married | 14 795 (10.7) | 5174 (11.1) | 19 969 (10.8) | 2507 (8.71) | 643 (8.12) | 3150 (8.58) |
| Previously married | 39 968 (29.0) | 13 316 (28.5) | 53 284 (28.9) | 7736 (26.9) | 2148 (27.1) | 9884 (26.9) |
| Unknown marital status | 499 (0.36) | 139 (0.30) | 638 (0.35) | 99 (0.34) | 16 (0.20) | 115 (0.31) |
| Homeless at any time during year | 2410 (1.75) | 735 (1.57) | 3145 (1.71) | 279 (0.97) | 68 (0.86) | 347 (0.95) |
| Copay status | ||||||
| No copay due to disability | 75 781 (55.0) | 24 059 (51.4) | 99 840 (54.1) | 15 318 (53.2) | 3944 (49.8) | 19 262 (52.5) |
| No copay due to low income | 35 955 (26.1) | 12 448 (26.6) | 48 403 (26.2) | 7293 (25.3) | 1972 (24.9) | 9265 (25.2) |
| Must pay copay | 24 068 (17.5) | 9580 (20.5) | 33 648 (18.2) | 5790 (20.1) | 1879 (23.7) | 7669 (20.9) |
| Copay status unknown | 1863 (1.35) | 698 (1.49) | 2561 (1.39) | 393 (1.36) | 125 (1.58) | 518 (1.41) |
| Mental health diagnoses | ||||||
| Mood disorder | 32 842 (23.9) | 11 177 (23.9) | 44 019 (23.9) | 6513 (22.6) | 1747 (22.1) | 8260 (22.5) |
| Posttraumatic stress disorder | 19 787 (14.4) | 6253 (13.4) | 26 040 (14.1) | 4085 (14.2) | 961 (12.1) | 5046 (13.7) |
| Dementia | 4317 (3.14) | 1254 (2.68) | 5571 (3.02) | 844 (2.93) | 187 (2.36) | 1031 (2.81) |
| Substance abuse | 10 765 (7.82) | 3556 (7.60) | 14 321 (7.76) | 1669 (5.80) | 416 (5.25) | 2085 (5.68) |
| Other mental health diagnosis | 8101 (5.88) | 2836 (6.06) | 10 937 (5.93) | 1665 (5.78) | 402 (5.08) | 2067 (5.63) |
| DCG score category | ||||||
| Less than or equal to 0.5 | 69 438 (50.4) | 24 832 (53.1) | 94 270 (51.1) | 15 668 (54.4) | 4662 (58.9) | 20 330 (55.4) |
| Greater than 0.5 to 1 | 23 807 (17.3) | 8219 (17.6) | 32 026 (17.4) | 4892 (17.0) | 1273 (16.1) | 6165 (16.8) |
| Greater than 1 to 1.5 | 17 338 (12.6) | 5830 (12.5) | 23 168 (12.6) | 3470 (12.1) | 897 (11.3) | 4367 (11.9) |
| Greater than 1.5 to 2 | 9640 (7.00) | 2968 (6.34) | 12 608 (6.84) | 1846 (6.41) | 454 (5.73) | 2300 (6.26) |
| Greater than 2 | 17 444 (12.7) | 4936 (10.6) | 22 380 (12.1) | 2918 (10.1) | 634 (8.01) | 3552 (9.67) |
| Distance from VHA primary care clinic | ||||||
| Less than 5 miles | 33 844 (24.6) | 12 386 (26.5) | 46 230 (25.1) | 6833 (23.7) | 2143 (27.1) | 8976 (24.4) |
| 5 to less than 25 miles | 70 610 (51.3) | 23 630 (50.5) | 94 240 (51.1) | 13 673 (47.5) | 3949 (49.9) | 17 622 (48.0) |
| 25 to less than 50 miles | 21 539 (15.6) | 7250 (15.5) | 28 789 (15.6) | 6374 (22.1) | 1448 (18.3) | 7822 (21.3) |
| 50 miles and more | 10 663 (7.75) | 3032 (6.48) | 13 695 (7.42) | 1747 (6.07) | 332 (4.19) | 2079 (5.66) |
| Missing | 1011 (0.73) | 487 (1.04) | 1498 (0.81) | 167 (0.58) | 48 (0.61) | 215 (0.59) |
| Facility-level factors | ||||||
| Endocrinology referral capacitya | 65 407 (47.5) | 15 476 (33.1) | 80 883 (43.9) | 7288 (25.3) | 1555 (19.6) | 8843 (24.1) |
| Percent of providers in primary care clinic who are NPs/PAs | ||||||
| Lowest tertile | 77 020 (55.9) | 7479 (16.0) | 84 499 (45.8) | 17 320 (60.2) | 1147 (14.5) | 18 467 (50.3) |
| Middle tertile | 45 587 (33.1) | 18 141 (38.8) | 63 728 (34.5) | 7561 (26.3) | 2972 (37.5) | 10 533 (28.7) |
| Highest tertile | 15 060 (10.9) | 21 165 (45.2) | 36 225 (19.6) | 3913 (13.6) | 3801 (48.0) | 7714 (21.0) |
| Rural-urban commuting area status | ||||||
| Metropolitan area core | 99 340 (72.2) | 31 927 (68.2) | 131 267 (71.2) | 17 590 (61.1) | 3366 (42.5) | 20 956 (57.1) |
| Metropolitan area core—remaining levels | 18 647 (13.5) | 4361 (9.32) | 23 008 (12.5) | 6190 (21.5) | 2334 (29.5) | 8524 (23.2) |
| Micropolitan area core | 14 532 (10.6) | 7478 (16.0) | 22 010 (11.9) | 3755 (13.0) | 1711 (21.6) | 5466 (14.9) |
| Small town or rural | 5148 (3.74) | 3019 (6.45) | 8167 (4.43) | 1259 (4.37) | 509 (6.43) | 1768 (4.82) |
| State-level factors | ||||||
| Region | ||||||
| Northeast | 21 738 (15.8) | 11 576 (24.7) | 33 314 (18.1) | 4329 (15.0) | 2337 (29.5) | 6666 (18.2) |
| West | 32 153 (23.4) | 9314 (19.9) | 41 467 (22.5) | 1710 (5.94) | 761 (9.61) | 2471 (6.73) |
| Midwest | 29 297 (21.3) | 12 317 (26.3) | 41 614 (22.6) | 5411 (18.8) | 1997 (25.2) | 7408 (20.2) |
| South | 54 479 (39.6) | 13 578 (29.0) | 68 057 (36.9) | 17 344 (60.2) | 2825 (35.7) | 20 169 (54.9) |
| Percent of primary care physicians who work with NPs/PAs | ||||||
| Lowest tertile | 81 267 (59.0) | 23 057 (49.3) | 104 324 (56.6) | 14 456 (50.2) | 4886 (61.7) | 19 342 (52.7) |
| Middle tertile | 38 486 (28.0) | 16 108 (34.4) | 54 594 (29.6) | 5573 (19.4) | 1301 (16.4) | 6874 (18.7) |
| Highest tertile | 17 914 (13.0) | 7620 (16.3) | 25 534 (13.8) | 8765 (30.4) | 1733 (21.9) | 10 498 (28.6) |
| Physician assistant scope of practice regulations | ||||||
| Least restrictive | 20 500 (14.9) | 8386 (17.9) | 28 886 (15.7) | 5785 (20.1) | 1112 (14.0) | 6897 (18.8) |
| Moderately restrictive | 22 218 (16.1) | 9165 (19.6) | 31 383 (17.0) | 1394 (4.84) | 956 (12.1) | 2350 (6.40) |
| Most restrictive | 94 949 (69.0) | 29 234 (62.5) | 124 183 (67.3) | 21 615 (75.1) | 5852 (73.9) | 27 467 (74.8) |
Note. Data for patient-level variables are from the VA electronic health record files. Other data sources are described in the “Methods” section. PCP is assigned as the physician, NP, or PA seen most during FY 2012 and 2013. VA = Veterans Administration; OR = odds ratio; NP = nurse practitioner; PA = physician assistant; DCG = Diagnostic Cost Group; VHA = Veterans Health Administration; PCP = primary care provider; FY = fiscal year.
Endocrinology referral capacity is defined as either present (endocrinology or other diabetes mellitus specialty clinics provided 500 or more visits to cohort patients in FY 2012) or absent (fewer than 500 visits to cohort patients).
Appendix B.
ORs for Predicting Assignment to a Primary Care Provider Who Is an NP or PA, Compared With Physician Among Facilities With Physician and NP or Physician and PA.
| Effect and level | Clinics with only physicians and NPs assigned as PCPs |
Clinics with only physicians and PAs assigned as PCPs |
|||||
|---|---|---|---|---|---|---|---|
| OR for assignment to NP | 95% CI for assignment to NP | P value for assignment to NP | Blank | OR for assignment to PA | 95% CI for assignment to PA | P value for assignment to PA | |
| Patient-level factors | 1 | ||||||
| Male | 0.46 | 0.43-0.49 | <.001 | 2 | 0.65 | 0.54-0.78 | <.001 |
| Age group | 3 | ||||||
| Less than 40 | Reference | Reference | 4 | Reference | Reference | ||
| 40 to less than 65 | 0.86 | 0.76-0.98 | .021 | 5 | 0.77 | 0.55-1.06 | .107 |
| 65 to less than 80 | 0.86 | 0.75-0.97 | .016 | 6 | 0.77 | 0.56-1.07 | .123 |
| 80 and above | 0.85 | 0.74-0.96 | .012 | 7 | 0.80 | 0.57-1.12 | .191 |
| Race | 8 | ||||||
| White | Reference | Reference | 9 | Reference | Reference | ||
| American Indian | 0.91 | 0.78-1.06 | .232 | 10 | 0.88 | 0.62-1.25 | .473 |
| Asian | 0.98 | 0.81-1.18 | .820 | 11 | 0.89 | 0.49-1.60 | .697 |
| Black | 1.06 | 1.02-1.10 | .005 | 12 | 0.92 | 0.83-1.02 | .103 |
| Native Hawaiian | 0.92 | 0.81-1.04 | .184 | 13 | 1.13 | 0.86-1.48 | .379 |
| Unknown or Missing | 1.02 | 0.97-1.06 | .496 | 14 | 0.99 | 0.88-1.10 | .803 |
| Hispanic | 1.07 | 1.00-1.14 | .050 | 15 | 1.17 | 0.97-1.42 | .092 |
| Marital status | 16 | ||||||
| Currently married | Reference | Reference | 17 | Reference | Reference | ||
| Never married | 1.02 | 0.98-1.07 | .270 | 18 | 0.93 | 0.84-1.04 | .201 |
| Previously married | 0.99 | 0.96-1.01 | .296 | 19 | 1.02 | 0.95-1.09 | .651 |
| Unknown marital status | 0.87 | 0.70-1.08 | .204 | 20 | 0.60 | 0.33-1.07 | .084 |
| Homeless at any time during year | 1.07 | 0.97-1.18 | .155 | 21 | 1.17 | 0.86-1.60 | .323 |
| Copay status | 22 | ||||||
| Must pay copay | Reference | Reference | 23 | Reference | Reference | ||
| No copay due to disability | 0.91 | 0.88-0.94 | <.001 | 24 | 0.97 | 0.90-1.05 | .420 |
| No copay due to low income | 0.97 | 0.93-1.01 | .098 | 25 | 0.94 | 0.87-1.03 | .171 |
| Copay status unknown | 0.95 | 0.85-1.07 | .394 | 26 | 1.15 | 0.87-1.52 | .330 |
| Mental health diagnoses | 27 | ||||||
| Mood disorder | 1.06 | 1.03-1.09 | <.001 | 28 | 1.01 | 0.94-1.10 | .707 |
| PTSD | 0.97 | 0.93-1.01 | .122 | 29 | 0.95 | 0.86-1.04 | .267 |
| Dementia | 0.86 | 0.80-0.93 | <.001 | 30 | 0.86 | 0.71-1.04 | .115 |
| Substance abuse | 1.07 | 1.02-1.12 | .010 | 31 | 1.05 | 0.92-1.19 | .506 |
| Other mental health diagnosis | 1.09 | 1.03-1.15 | .002 | 32 | 0.91 | 0.79-1.04 | .158 |
| DCG score category | 33 | ||||||
| Less than or equal to 0.5 | Reference | Reference | 34 | Reference | Reference | ||
| Greater than 0.5 to 1 | 0.99 | 0.95-1.02 | .460 | 35 | 0.88 | 0.81-0.95 | .002 |
| Greater than 1 to 1.5 | 0.97 | 0.93-1.01 | .107 | 36 | 0.92 | 0.84-1.01 | .088 |
| Greater than 1.5 to 2 | 0.87 | 0.83-0.91 | <.001 | 37 | 0.83 | 0.73-0.94 | .003 |
| Greater than 2 | 0.84 | 0.81-0.88 | <.001 | 38 | 0.80 | 0.72-0.89 | <.001 |
| Distance from VHA primary care clinic | 39 | ||||||
| Less than 5 miles | Reference | Reference | 40 | Reference | Reference | ||
| 5 to less than 25 miles | 1.03 | 1.00-1.06 | .060 | 41 | 0.99 | 0.93-1.07 | .866 |
| 25 to less than 50 miles | 1.05 | 1.01-1.09 | .023 | 42 | 0.95 | 0.87-1.04 | .251 |
| 50 miles or greater | 1.05 | 0.99-1.11 | .094 | 43 | 0.95 | 0.82-1.10 | .513 |
| Missing | 0.88 | 0.74-1.06 | .177 | 44 | 0.52 | 0.33-0.83 | .005 |
| Facility-level factors | 45 | ||||||
| Endocrinology referral capacitya | 0.92 | 0.72-1.18 | .520 | 46 | 0.96 | 0.48-1.93 | .916 |
| Percent of providers in the primary care clinic who are NPs/PAs | 47 | ||||||
| Lowest tertile | Reference | Reference | 48 | Reference | Reference | ||
| Middle tertile | 5.36 | 4.28-6.71 | <.001 | 49 | 7.80 | 4.89-12.45 | <.001 |
| Highest tertile | 24.37 | 19.26-30.85 | <.001 | 50 | 23.88 | 14.56-39.18 | <.001 |
| Rural-urban commuting area status | 51 | ||||||
| Metropolitan area core | Reference | Reference | 52 | Reference | Reference | ||
| Metropolitan area core—remaining levels | 1.09 | 0.83-1.43 | .522 | 53 | 1.36 | 0.78-2.37 | .274 |
| Micropolitan area core | 1.12 | 0.89-1.42 | .329 | 54 | 1.21 | 0.76-1.95 | .423 |
| Small town or rural | 1.43 | 1.03-1.98 | .033 | 55 | 4.30 | 1.87-9.86 | <.001 |
| State-level factors | 56 | ||||||
| Region | 57 | ||||||
| Northeast | Reference | Reference | 58 | Reference | Reference | ||
| West | 0.81 | 0.59-1.10 | .171 | 59 | 1.03 | 0.50-2.14 | .927 |
| Midwest | 1.21 | 0.91-1.62 | .182 | 60 | 1.20 | 0.69-2.11 | .520 |
| South | 0.80 | 0.62-1.04 | .097 | 61 | 0.66 | 0.40-1.08 | .097 |
| Percent of primary care physicians who work with NPs/PAs | 62 | ||||||
| Lowest tertile | Reference | Reference | 63 | Reference | Reference | ||
| Middle tertile | 0.94 | 0.75-1.18 | .592 | 64 | 0.43 | 0.26-0.73 | .002 |
| Highest tertile | 0.94 | 0.72-1.24 | .686 | 65 | 0.65 | 0.37-1.15 | .137 |
| Physician assistant scope of practice regulations | 66 | ||||||
| Least restrictive | Reference | Reference | 67 | Reference | Reference | ||
| Moderately restrictive | 1.25 | 0.89-1.77 | .199 | 68 | 0.54 | 0.25-1.17 | .117 |
| Most restrictive | 0.93 | 0.69-1.25 | .621 | 69 | 0.65 | 0.37-1.17 | .149 |
Note. Data for patient-level variables are from the VA electronic health record files. Other data sources are described in the “Methods” section. PCP is assigned as the physician, NP, or PA seen most during FY 2012 and 2013. OR = odds ratio; NP = nurse practitioner; CI = confidence interval; PA = physician assistant; PTSD = posttraumatic stress disorder; DCG = Diagnostic Cost Group; VHA = Veterans Health Administration; PCP = primary care provider.
Endocrinology referral capacity is defined as either present (endocrinology or other diabetes mellitus specialty clinics provided 500 or more visits to cohort patients in FY 2012) or absent (fewer than 500 visits to cohort patients).
Footnotes
Authors’ Note: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Veterans Affairs Health Services Research and Development Service (IIR 13-063).
References
- 1. Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Diabetes Report Card 2014. 2014. http://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf. Accessed July 31, 2015.
- 3. DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. JAMA. 2003;289(17):2254-2264. [DOI] [PubMed] [Google Scholar]
- 4. Rothman AA, Wagner EH. Chronic illness management: what is the role of primary care? Ann Intern Med. 2003;138(3):256-261. [DOI] [PubMed] [Google Scholar]
- 5. Association of American Medical Colleges. The complexities of physician supply and demand: Projections from 2013 to 2025. 2015. https://www.aamc.org/download/426242/data/ihsreportdownload.pdf?cm_mmc=AAMC-_-ScientificAffairs-_-PDF-_-ihsreport. Accessed May 31, 2017.
- 6. Jackson GL, Edelman D, Weinberger M. Simultaneous control of intermediate diabetes outcomes among Veterans Affairs primary care patients. J Gen Intern Med. 2006;21(10):1050-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36(8):2271-2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ali MK, Bullard KM, Gregg EW. Achievement of goals in U.S. Diabetes Care, 1999-2010. N Engl J Med. 2013;369(3):287-288. [DOI] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention. National diabetes statistics report, 2014: estimates of diabetes and its burden in the United States. 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed July 29, 2015.
- 10. Grumbach K, Bodenheimer T. A primary care home for Americans: putting the house in order. JAMA. 2002;288(7):889-893. [DOI] [PubMed] [Google Scholar]
- 11. American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, Association AO. Joint principles of the patient-centered medical home. 2007http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Accessed May 23, 2017.
- 12. van Hasselt M, McCall N, Keyes V, Wensky SG, Smith KW. Total cost of care lower among Medicare fee-for-service beneficiaries receiving care from patient-centered medical homes. Health Serv Res. 2015;50(1):253-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hebert PL, Liu CF, Wong ES, et al. Patient-centered medical home initiative produced modest economic results for Veterans Health Administration, 2010-12. Health Aff (Millwood). 2014;33(6):980-987. [DOI] [PubMed] [Google Scholar]
- 14. Nelson KM, Helfrich C, Sun H, et al. Implementation of the patient-centered medical home in the veterans health administration: associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Intern Med. 2014;174(8):1350-1358. [DOI] [PubMed] [Google Scholar]
- 15. Jackson G, Powers B, Chatergee R, et al. The patient-centred medical home: a systematic review. Ann Intern Med. 2013;158(3):169-178. [DOI] [PubMed] [Google Scholar]
- 16. Everett C, Thorpe C, Carayon P, Palta M, Gilchrist V, Smith M. Physician assistant and nurse practitioners perform effective roles on teams caring for Medicare patients with diabetes. Health Aff (Millwood). 2013;32(11):1942-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Woodmansee DJ, Hooker RS. Physician assistants working in the Department of Veterans Affairs. JAAPA. 2010;23(11):41-44. [DOI] [PubMed] [Google Scholar]
- 18. Robinson KR. Roles of nurse practitioners in the U.S. Department of Veterans Affairs. In: Sullivan-Marx EM, McGivern DO, Fairman JA, Greenberg SA, eds. Nurse Practitioners: The Evolution and Future of Advanced Practice. 5th ed. New York, NY: Springer; 2010:223-238. [Google Scholar]
- 19. Huang PY, Yano EM, Lee ML, Chang BL, Rubenstein LV. Variations in nurse practitioner use in Veterans Affairs primary care practices. Health Serv Res. 2004;39(4, Pt 1):887-904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. U.S. Department of Veterans Affairs. Patient Aligned Care Team (PACT). 2010. http://www.va.gov/primarycare/pcmh/. Accessed May 23, 2017.
- 21. Piette JD, Holtz B, Beard AJ, et al. Improving chronic illness care for veterans within the framework of the patient-centered medical home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1:615-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yano B, Stark R, Fihn S, et al. Patient-Aligned Care Teams (PACT) Demonstration Lab Initiative. Veterans Affairs Health Services Research and Development Meeting; Washington, DC; February 17, 2011. [Google Scholar]
- 23. Hass V. Physician assistants and nurse practitioners are not interchangeable. JAAPA. 2016;29(4):9-12. [DOI] [PubMed] [Google Scholar]
- 24. George JB. Nursing Theories: The Base for Professional Nursing Practice. 6th ed. New York, NY: Pearson; 2011. [Google Scholar]
- 25. Everett CM, Schumacher JR, Wright A, Smith MA. Physician assistants and nurse practitioners as a usual source of care. J Rural Health. 2009;25(4):407-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Newhouse RP, Stanik-Hutt J, White KM, et al. Advanced practice nurse outcomes 1990-2008: a systematic review. Nurs Econ. 2011;29(5):230-250; quiz 251. [PubMed] [Google Scholar]
- 27. Morgan P, Abbott D, McNeill R, Fisher D. Characteristics of primary care office visits to nurse practitioners, physician assistants and physicians in United States Veterans Health Administration facilities, 2005-2010: a retrospective cross-sectional analysis. Hum Resour Health. 2012;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hing E, Hooker RS. Community Health Centers: Providers, Patients, and Content of Care. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- 29. Fletcher CE, Copeland LA, Lowery JC, Reeves PJ. Nurse practitioners as primary care providers within the VA. Mil Med. 2011;176(7):791-797. [DOI] [PubMed] [Google Scholar]
- 30. Morgan P, Everett C, Hing E. Nurse practitioners, physician assistants, and physicians in community health centers, 2006-2010. Healthcare (Amsterdam, Netherlands). 2015;3(2):102-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Grumbach K, Hart LG, Mertz E, Coffman J, Palazzo L. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003;1(2):97-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hing E, Hsiao C-J. In which states are physician assistants or nurse practitioners more likely to work in primary care? JAAPA. 2015;28(9):46-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Barnes H, Maier CB, Altares Sarik D, Germack HD, Aiken LH, McHugh MD. Effects of regulation and payment policies on nurse practitioners’ clinical practices [published online ahead of print May 13, 2016]. Med Care Res Rev. doi: 10.1177/1077558716649109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kuo Y, Loresto F, Rounds L, Goodwin J. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Aff (Millwood). 2013;32(7):1236-1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Med Care. 2011;49(1):76-88. [DOI] [PubMed] [Google Scholar]
- 36. Trivedi AN, Grebla RC. Quality and equity of care in the veterans affairs health-care system and in Medicare advantage health plans. Med Care. 2011;49(6):560-568. [DOI] [PubMed] [Google Scholar]
- 37. Morgan P, Strand J, Ostbye T, Albanese M. Missing in action: care by physician assistants and nurse practitioners in national health surveys. Health Serv Res. 2007;42(5):2022-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dower C, Moore J, Langelier MH. It is time to restructure health professions scope-of-practice regulations to remove barriers to care. Health Aff (Millwood). 2013;32(11):1971-1976. [DOI] [PubMed] [Google Scholar]
- 39. Brown SH, Lincoln MJ, Groen PJ, Kolodner RM. VistA—U.S. Department of Veterans Affairs national-scale HIS. Int J Med Inform. 2003;69(2-3):135-156. [DOI] [PubMed] [Google Scholar]
- 40. Jackson GL, Krein SL, Alverson DC, et al. Defining core issues in utilizing information technology to improve access: evaluation and research agenda. J Gen Intern Med. 2011;26(suppl 2):623-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Evans RG, Stoddart GL. Producing health, consuming health care. Soc Sci Med. 1990;31(12):1347-1363. [DOI] [PubMed] [Google Scholar]
- 42. Maciejewski ML, Liu C-F, Derleth A, McDonell M, Anderson S, Fihn SD. The performance of administrative and self-reported measures for risk adjustment of Veterans Affairs expenditures. Health Serv Res. 2005;40(3):887-904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ellis RP, Ash A. Refinements to the Diagnostic Cost Group (DCG) model. Inquiry. 1995;32(4):418-429. [PubMed] [Google Scholar]
- 44. Ash A, Porell F, Gruenberg L, Sawitz E, Beiser A. Adjusting Medicare capitation payments using prior hospitalization data. Health Care Financ Rev. 1989;10(4):17-29. [PMC free article] [PubMed] [Google Scholar]
- 45. U.S. Department of Agriculture. 2010 Rural-Urban Commuting Area (RUCA) Codes. 2010. http://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation.aspx. Accessed August 13, 2016.
- 46. Pearson LJ. The 2012 Pearson Report: A National Overview of Nurse Practitioner Legislation and Health Care Issues. Monroe Township, NJ: NP Communications; 2012. [Google Scholar]
- 47. American Academy of Physician Assistants. The six key elements of a Modern Physician Assistant Practice Act. 2014. Alexandria, VA: AAPA. [Google Scholar]
- 48. Agency for Healthcare Research and Quality. Primary care workforce facts and stats no 2: The Number of Nurse Practitioners and Physician Assistants Practicing Primary Care in the United States. 2011. https://www.ahrq.gov/sites/default/files/publications/files/pcwork2.pdf. Accessed May 23, 2017.
- 49. Mills AC, McSweeney M. Nurse practitioners and physician assistants revisited: do their practice patterns differ in ambulatory care? J Prof Nurs. 2002;18(1):36-46. [DOI] [PubMed] [Google Scholar]
- 50. Cipher DJ, Hooker RS, Guerra P. Prescribing trends by nurse practitioners and physician assistants in the United States. J Am Acad Nurse Pract. 2006;18(6):291-296. [DOI] [PubMed] [Google Scholar]
- 51. Laurant M, Harmsen M, Wollersheim H, Grol R, Faber M, Sibbald B. The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S-89S. [DOI] [PubMed] [Google Scholar]
- 52. Everett CM, Leach B, Strand de, Oliveira J, Gradison M, Dill MJ, Morgan P. Patient factors that predict preference for primary care provider type. Association of American Medical Colleges Health Workforce Conference; Chicago, IL; May 5, 2016. [Google Scholar]
- 53. Washington DL, Caffrey C, Goldzweig C, Simon B, Yano EM. Availability of comprehensive women’s health care through Department of Veterans Affairs Medical Center. Womens Health Issues. 2003;13(2):50-54. [DOI] [PubMed] [Google Scholar]
- 54. Bean-Mayberry BA, Chang CC, McNeil MA, Scholle SH. Ensuring high-quality primary care for women: predictors of success. Womens Health Issues. 2006;16(1):22-29. [DOI] [PubMed] [Google Scholar]
- 55. U.S. Department of Health & Human Services, Health Resources and Services Administration, Analysis NCfHW. Highlights from the 2012 National Sample Survey of Nurse Practitioners. 2014. https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/npsurveyhighlights.pdf. Accessed January 20, 2015.
- 56. National Commission on Certification of Physician Assistants. 2013 statistical profile of recently certified physician assistants. 2014. http://www.nccpa.net/Upload/PDFs/RecentlyCertifiedReport2013.pdf. Accessed September 1, 2016.
- 57. Association of American Medical Colleges. 2012 physician specialty data book. 2012. https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Accessed September 1, 2016.
- 58. Moran EA, Basa E, Gao J, Woodmansee D, Almenoff PL, Hooker RS. PA and NP productivity in the Veterans Health Administration. JAAPA. 2016;29(7):1-6. [DOI] [PubMed] [Google Scholar]
- 59. Kurtzman ET, Barnow BS, Johnson JE, Simmens SJ, Infeld DL, Mullan F. Does the regulatory environment affect nurse practitioners’ patterns of practice or quality of care in health centers? Health Serv Res. 2017;52(suppl 1):437-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511-544. [PubMed] [Google Scholar]
- 61. Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263-e272. [PubMed] [Google Scholar]
- 62. Dill MJ, Pankow S, Erikson C, Shipman S. Survey shows consumers open to a greater role for physician assistants and nurse practitioners. Health Aff (Millwood). 2013;32(6):1135-1142. [DOI] [PubMed] [Google Scholar]