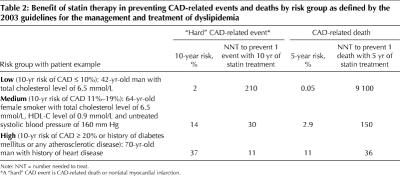
The recommendations of the 2003 Canadian guidelines for the management and treatment of dyslipidemia, if applied in clinical practice, will result in more people being screened and prescribed statin therapy.1,2 When compared with the 2000 guidelines, the 2003 guidelines recommend screening more people with fewer risk factors for coronary artery disease (CAD) and lower lipid level targets for people in all risk groups (Table 1). We are concerned that these changes will result in hundreds of thousands more people receiving treatment and a marked increase in costs to the Canadian health care system, with small overall improvements to CAD outcomes. Simple revisions to the new guidelines could reduce the number of people receiving treatment and at the same time prevent more CAD-related deaths.
Table 1
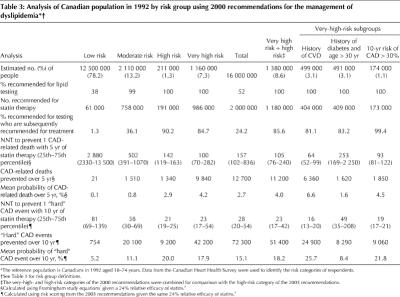
There is no doubt that statins are efficacious. They reduce CAD-related mortality by 15% to 30%.3,4 However, the absolute benefit provided by statins (and the number needed to treat to achieve that benefit) varies enormously, depending on whether patients are at high, medium or low risk of CAD (Table 2).5Under the 2003 recommendations, low-risk patients will be given statin therapy for many years with only a very small reduction in the number of CAD events.
Table 2
We used the approach of MacLean and colleagues6 and data from the Canadian Heart Health Survey (CHHS) to estimate how the 2003 guideline revisions would affect the Canadian population in terms of the number of people who would be screened and the people for whom treatment with statins would be recommended. Details about the methods are available at www.cmaj.ca/cgi/content/full/172/8/1027/DC1. In brief, we used CHHS data to identify the proportion of respondents aged 18–74 years who were eligible for screening according to both the 2000 and 2003 guidelines (e.g., respondents who had diabetes, CAD or 1 or more risk factors for CAD, men older than 40 years, women older than 50 years). Data on the lipid level profile, smoking status and blood pressure of CHHS respondents were also available. Using this information, we determined whether the CHHS respondents were at low, medium or high risk of experiencing a “hard” CAD event (i.e., CAD-related death or nonfatal myocardial infarction) in the next 10 years as determined by the Framingham-based risk point scoring system used in the respective guidelines. Since the Framingham scoring system applies only to people without known cardiovascular disease, we estimated the probability of CHHS respondents with existing cardiovascular disease experiencing a “hard” CAD event using the age-specific 10-year “hard” CAD event rates experienced by an Ontario cohort of patients aged 18–74 who were previously admitted to hospital because of cardiovascular disease between 1988 and 1992. CHHS sampling weights were applied to generate estimates for all Canadians 18–74 years of age.
We then evaluated the health impact of the 2000 and 2003 guidelines on the Canadian population in terms of the number of CAD events potentially prevented and the number needed to treat to prevent a CAD event with statin therapy. The number needed to treat to prevent 1 event was calculated as 1 over the absolute baseline risk of people receiving treatment in each guideline risk group multiplied by the relative effectiveness of statins (assumed to be a constant 24%3 for all risk groups and outcomes). The number needed to treat for some people in the low-risk groups was very large because their baseline risk was extremely low. The guidelines defined the low-risk group as anyone with a 10-year baseline risk of a "hard" CAD event less than 10% in 2000 and 10% or less in 2003. The number of deaths potentially prevented in each risk group was calculated by dividing the total number of people in a risk group by the number needed to treat in that group.
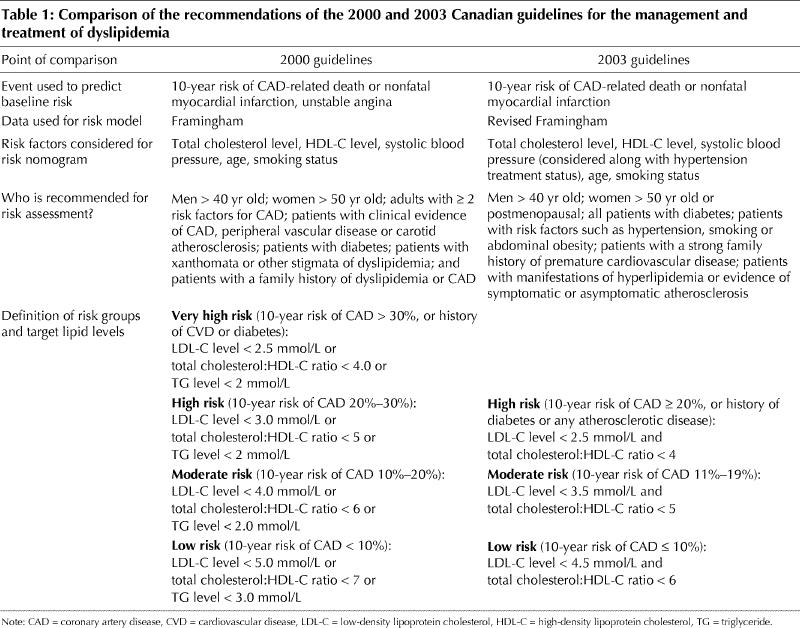
Using the Canadian population aged 18–74 years in 1992 as the reference population, the number of people for whom statin therapy is recommended increased by 27%, from 2 million using the 2000 guidelines to 2.53 million using the 2003 guidelines (Table 3andTable 4). Almost all of the increase consisted of patients in the low-risk category. The number of low-risk people for whom statins are recommended if lifestyle modification fails to achieve target lipid levels increased 10-fold, from 61 000 to 595 000. Yet, the relative benefit of statin therapy for many people in the low-risk group is incredibly small. By our estimates, among the 149 000 Canadians who fall within the highest-risk quartile in this group, the number needed to treat with 5 years of statin therapy to prevent 1 CAD-related death would be 19 600. The number needed to treat to prevent 1 CAD-related death in the low-risk group recommended for statin therapy (n = 595 000) would be 1550.
Table 3
Table 4
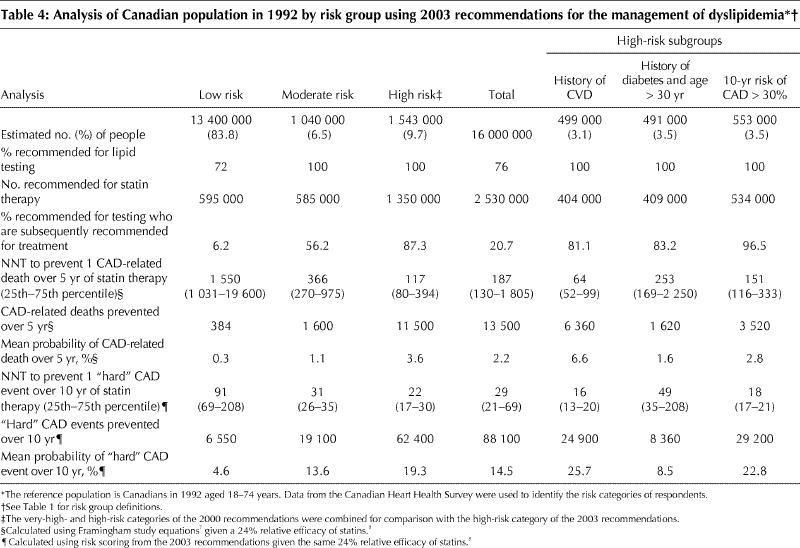
Conversely, according to CHHS data, about 12.5% (193 000/1 543 000) (Table 4) of high-risk people have low-density lipoprotein cholesterol levels below the recommended target. According to the 2003 guidelines, these people would not be recommended for statin treatment. However, the Heart Protection Study4 is widely cited as providing evidence for the benefit of statin therapy for most of these people. The 2003 guidelines acknowledge the evidence of this and other studies. In our estimate, the number needed to treat for 5 years to prevent 1 death is 10 times more favourable for high-risk people currently not recommended therapy than for low-risk people who are recommended therapy (141 v. 1550).
By these calculations, if the 2003 guidelines were modified to recommend statins for all high-risk people and no low-risk people, 1010 more deaths over 5 years might be prevented and 398 000 fewer people (2.5% of the total population) given treatment. Although the guidelines recommend screening the entire adult population, in practice not everyone will be screened or offered treatment or will persist on statin therapy. Thus, the actual impact in terms of the potential number of deaths prevented or people treated would be considerably lower.9,10,11,12,13
In Canada, statin prescriptions increased over 3-fold between 1996 and 2000 to 11 million prescriptions at a cost of $1.1 billion annually.11 The further 27% increase incurred if the revised recommendations are followed would contribute an additional $250 million in drug costs each year. On the other hand, recommending statins for all high-risk people and no low-risk people, using the 2003 definitions for the risk groups, would reduce the number of people recommended statins by 16% and avoid more deaths (Fig. 1). The New Zealand approach of recommending treatment for all people with a history of CAD or a 10-year risk of CAD-related death greater than 15%14 is even more efficient. Applying the New Zealand guidelines in Canada would result in the prevention of slightly more CAD-related deaths, treatment of 37% fewer people and savings of $100 million compared with using the revised 2003 guidelines (Fig. 1).14
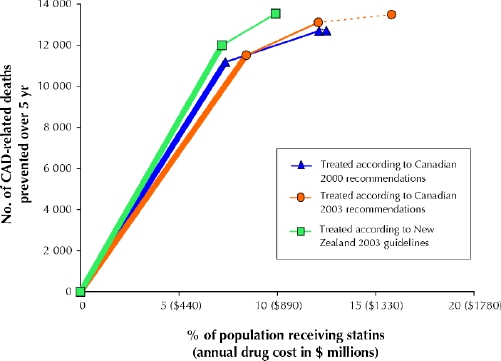
Fig. 1: No. of deaths from coronary artery disease (CAD) prevented over 5 years among people aged 18–74 years receiving statin therapy according to the 2000 and 2003 Canadian recommendations and the 2003 New Zealand guidelines. This assumes that all eligible people were screened and were compliant with the statin therapy recommended and that the drug cost was $1.52 per day. Thick solid rules represent people at high risk for CAD, thinner solid rules represent people at moderate risk, and dotted rules represent people at low risk; for the 2000 Canadian recommendations, the categories of high and very high risk have been combined.
These calculations have implications for patients, clinicians, funding agencies and those interested in population health. Fully informed patients are often less aggressive about therapy than their clinicians.15 As well, low-risk patients will paradoxically sometimes receive more aggressive treatment than high-risk patients.13,16 The very small absolute benefits associated with statin therapy in low-risk patients highlights the importance of informing these patients about the absolute benefits and risks of statins. Our analysis reinforces the importance of ensuring that clinicians offer statin therapy to high-risk patients, since they are the patients with the most to gain. Even high-risk patients whose low-density lipoprotein cholesterol levels are below the target given in the 2003 guidelines should be considered for statin therapy.
It is important to remember that a drug that is efficacious in high-risk patients is also typically efficacious in very-low-risk patients, but the absolute benefits and cost-effectiveness are almost always lower. Costs for the individual (including costs related to the drug, testing, doctor and clinic visits, being labeled as “sick” or carrying a risk factor) and for society (drug and treatment costs) suggest that the funds spent on statins for low-risk patients may be better used elsewhere. Including information on the absolute benefits and cost-effectiveness of statin therapy in dyslipidemia guidelines — as New Zealand and European guidelines do14,17 — allows for more meaningful discussions about who should receive the therapy. Our analysis demonstrates that estimating absolute benefit can improve guidelines by more clearly identifying who will benefit most from statins. Since there is no clear threshold of benefit or cost-effectiveness of statins, societal views should be elicited before expanding recommendations to a large number of low-risk people. The editors and reviewers of CMAJ should call on guideline authors to include measures of absolute benefit and to address resource implications of recommendations that are published in the journal.18 We urge the authors of the Canadian dyslipidemia guidelines to consider our analysis and revise their recommendations.
β See related articles pages 1033 and 1037
Supplementary Material
Acknowledgments
We thank Jenny Lim for her contribution to the additional analysis and assistance in preparing the manuscript.
Footnotes
Contributors: Douglas Manuel was the primary author and was responsible for the design of the study and the analysis and interpretation of the data. All authors provided advice and assistance for the initial design of the study. Peter Tanuspetro and Susan Schultz performed the analysis. All authors participated in revising the manuscript and approved the final version for submission.
Douglas Manuel is a Career Scientist with the Ontario Ministry of Health and Long-Term Care. David Alter holds a New Investigator Award from the Canadian Institutes of Health Research and the Heart and Stroke Foundation of Canada. Cameron Mustard held an Investigator Award from 1999 to 2003, and Andreas Laupacis holds a Senior Scientist Award from the Canadian Institutes of Health Research. Support for this project was received from the Canadian Population Health Initiative. The opinions expressed are those of the authors and not necessarily those of the institutions with which they are affiliated.
Competing interests: None declared.
Correspondence to: Dr. Douglas G. Manuel, Institute for Clinical Evaluative Sciences, Rm. G106, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-6048; doug.manuel@ices.on.ca
References
- 1.Fodor JG, Frohlich JJ, Genest JJ, Jr., McPherson PR. Recommendations for the management and treatment of dyslipidemia. Report of the Working Group on Hypercholesterolemia and Other Dyslipidemias. CMAJ 2000;162(10):1441-7. [PMC free article] [PubMed]
- 2.Genest J, Frohlich J, Fodor G, McPherson R (the Working Group on Hypercholesterolemia and Other Dyslipidemias). Recommendations for the management of dyslipidemia and the prevention of cardiovascular disease: summary of the 2003 update. CMAJ 2003;169(9):921-4. [PMC free article] [PubMed]
- 3.LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA 1999;282(24):2340-6. [DOI] [PubMed]
- 4.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002;360(9326):7-22. [DOI] [PubMed]
- 5.Alter DA, Manuel DG, Gunraj N, Anderson G, Naylor CD, Laupacis A. Age, risk-benefit trade-offs, and the projected effects of evidence-based therapies. Am J Med 2004;116(8):540-5. [DOI] [PubMed]
- 6.MacLean DR, Petrasovits A, Connelly PW, Little JA, O'Connor B. Impact of different blood lipid evaluation and treatment guidelines on the proportion of Canadians identified and treated for elevated blood cholesterol. Canadian Heart Health Surveys Research Group. Can J Cardiol 1999;15(4):445-51. [PubMed]
- 7.Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J 1991;121:293-8. [DOI] [PubMed]
- 8.Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med 1998;339:1349-57. [DOI] [PubMed]
- 9.Alzahrani T, Marrat S, Haider A. Management of dyslipidemia in primary care. Can J Cardiol 2003;19(13):1499-502. [PubMed]
- 10.Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA 2002;288(4):462-7. [DOI] [PubMed]
- 11.Jackevicius CA, Tu K, Filate WA, Brien SE, Tu JV. Trends in cardiovascular drug utilization and drug expenditures in Canada between 1996 and 2001. Can J Cardiol 2003;19(12):1359-66. [PubMed]
- 12.Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA 2002;288(4):455-61. [DOI] [PubMed]
- 13.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA 2004;291(15):1864-70. [DOI] [PubMed]
- 14.New Zealand Guidelines Group. The assessment and management of cardiovascular risk. December 2003. Wellington, New Zealand. Available: www.nzgg.org.nz/index.cfm?fuseaction=fuseaction_10&fusesubaction=docs&documentID=22 (accessed 09 Mar 05).
- 15.McAlister FA, O'Connor AM, Wells G, Grover SA, Laupacis A. When should hypertension be treated? The different perspectives of Canadian family physicians and patients. CMAJ 2000;163(4):403-8. [PMC free article] [PubMed]
- 16.Rutten FH, Hak E, Stalman WA, Verheij TJ, Hoes AW. Is treatment of atrial fibrillation in primary care based on thromboembolic risk assessment? Fam Pract 2003;20(1):16-21. [DOI] [PubMed]
- 17.De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003;24(17):1601-10. [DOI] [PubMed]
- 18.Laupacis A. Osteoporosis guidelines [letter]. CMAJ 2003;168(13):1644-5. [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.