Abstract
Background
Prescription opioid (PO) overdose deaths increased sharply over the last decade. Changes in PO deaths in combination with other psychoactive substances may provide a partial explanation.
Methods
PO deaths from the National Multiple-Cause-of-Death Files for 2002–03 (N=15,973) and 2014–15 (N=41,491) were analyzed. We calculated (1) changes in proportions of deaths in combination with benzodiazepines, antidepressants, heroin, alcohol, cocaine between the two periods, and (2) proportions of increase in deaths attributable to each substance among PO and synthetic opioids other than methadone (SO-M) deaths, by age, gender, race/ethnicity.
Results
Between 2002–03 and 2014–15, PO deaths increased 2.6 times; SO-M deaths 5.6 times, especially for ages 18–34, males, African-Americans. For PO deaths, most frequent combinations at both periods were with benzodiazepines; for SO-M, benzodiazepines, antidepressants in 2002–03, heroin, benzodiazepines in 2014–15. The largest increases occurred in combination with heroin among all PO (4.6% to 15.4%, change ratio=3.3[95%CI=3.1–3.6]), but especially SO-M deaths (1.2% to 24.5%, change ratio=21.3[95%CI=15.0–30.3]). Deaths involving cocaine decreased among PO, increased among SO-M deaths. One-fifth of increased PO or SO-M deaths were attributable to any of the five substances. Increased PO deaths were equally attributable to benzodiazepines and heroin; deaths attributable to heroin were higher among ages 18–49, males, and non-Hispanic whites. Increased SO-M deaths were attributable mostly to heroin among all groups.
Conclusions
Increased PO overdose deaths over the last decade may be partially explained by increased deaths in combination with other psychoactive substances. Use of other substances should be considered in efforts toward reducing prescription opioid overdoses.
Keywords: Prescription opioids, Overdose deaths, Benzodiazepines, Heroin, Synthetic opioids other than methadone
1. Introduction
Mortality and morbidity associated with prescription opioid analgesics increased sharply over the last decade (Centers for Disease Control and Prevention, 2017; Compton et al., 2015; Franklin et al., 2015; Kolata and Cohen, 2016; National Institute on Drug Abuse, 2017; Paulozzi, 2012; Rudd et al., 2016a; The White House, 2016; Volkow et al., 2014), leading the Centers for Disease Control to declare drug overdose deaths to be an epidemic (Rudd et al., 2016b). Prescription opioid (PO) overdose deaths increased more than two and a half times between 2002 and 2015 (National Institute on Drug Abuse, 2017). Increases in deaths occurred in the context of decreased prevalence of PO use but increased rates of heavy use and disorder among users (Han et al., 2015). Issues related to prescription opioids are worldwide, affecting European countries, Australia, and Canada (Berecki-Gisolf et al., 2017; Berterame et al., 2016; Degenhardt et al., 2013; Dhalla et al., 2011; European Monitoring Centre for Drugs and Addiction, 2014; Fischer et al., 2014; Shei et al., 2015; United Nations).
Determining the factors contributing to increased PO mortality is needed for informing prevention and intervention efforts. The director of the National Institute on Drug Abuse emphasized that increased prescriptions, greater social acceptability for using medications, and aggressive marketing by pharmaceutical companies helped create the “environmental availability” of prescription opioids and likely contributed to the current prescription drug abuse problem (Volkow, 2014). Increases in number of PO users could potentially explain increases in PO deaths. Everything else constant, changes in number of deaths should parallel changes in number of users. However, a relationship between users and deaths cannot be directly established nationally. Records do not distinguish deaths related to medical or nonmedical prescription opioid (NMPO) use. Furthermore, trend data are only available for nonmedical PO use. Prevalence of NMPO use in the population declined (Frenk et al., 2015; Han et al., 2015) from 4.7% in 2002 to 3.9% in 2014 (Hu et al., 2017). The 8% increase in number of persons prescribed opioid analgesics from 75 million in 2002 to 81 million in 2014 (Hwang et al., 2016) paralleled the concurrent 10% increase in the US population size (288 million in 2002, 319 million in 2014). Consequently, the prevalence of individuals prescribed opioid analgesics remained flat, 26.0% in 2002, 25.4% in 2014. The evidence suggests that increased PO deaths did not result from an increased number of medical or nonmedical PO users.
Changes in PO users’ behavior, including frequency of use, disorder, type of opioid used, prescription dosage, and concurrent use of other drugs, such as heroin or benzodiazepines, may account for increases in PO deaths (Compton et al., 2016; Drug Enforcement Administration, 2016; Hwang et al., 2016; Jones, 2012; 2013; Martins et al., 2017). High intensity NMPO use and disorder increased between 2002 and 2014 (Han et al., 2015; Hu et al., 2017; Jones, 2012). Prescription opioid dosage also increased since 1997 (Pain and Policy Studies Group/WHO Collaborating Center, 2015), and increased dosage is associated with increased morbidity and mortality (Bohnert et al., 2016; Dasgupta et al., 2016). Neither increasing intensity of use nor prescription dosage can be linked to population level PO overdose deaths because death records lack this information. Linkage can be implemented for one aspect of PO users’ behavior prior to death, use of other drugs, since death records list contributing drugs. Use of PO in combination with other substances, e.g., benzodiazepines, alcohol, fentanyl-mixed heroin or cocaine, has been associated with increased mortality from additive or synergistic adverse effects in the US (Babalonis and Walsh, 2015; Centers for Disease Control and Prevention, 2016; Jones et al., 2017; McCance-Katz et al., 2010; Oliver et al., 2007; Paone et al., 2016; Suzuki and El-Haddad, 2017), and Canada (Gomes et al., 2011), in part from pharmacokinetic and pharmacodynamic interactions resulting in respiratory depression and unintended rapid release of the opioid dose (Gudin et al., 2013; Jones et al., 2012; White and Irvine, 1999). Increased mortality associated with polydrug use involving opiates, cocaine, alcohol, or benzodiazepines in combination has been observed in New York City between 1990–98 (Coffin et al., 2003) and in Australia (Darke et al., 2010).
PO deaths involving other substances have been investigated at one time-point (Calcaterra et al., 2013; Dasgupta et al., 2016; Jann et al., 2014; Jones et al., 2013; 2014; Park et al., 2015; Saunders et al., 2012; Warner et al., 2016), but not over time, except for benzodiazepines (Chen et al., 2014; Jones and McAninch, 2015), which increased between 2004 and 2011 across age, gender and racial/ethnic groups (Jones and McAninch, 2015). Changes in overdose deaths from single substances, including heroin (Jones et al., 2015), psychostimulants (Calcaterra and Binswanger, 2013) and benzodiazepines (Bachhuber et al., 2016), have been examined separately up to 2009 or 2013. Using literal text analysis of information written on death certificates by medical certifiers (Trinidad et al., 2016; Warner et al., 2016), the National Center for Health Statistics and U.S. Food and Drug Administration recently identified specific drugs within classes of deaths in 2010–2014, and examined changes in all overdose deaths (not restricted to PO) for the ten most frequently mentioned specific drugs (Warner et al., 2016). Heroin deaths more than tripled; fentanyl deaths more than doubled.
The extent to which changes in PO deaths in combination with other substances contributed to the increase in PO deaths over the last decade and the relative contributions of different drug combinations to the increase remain to be specified.
We specify the extent to which changes in PO overdose deaths in combination with other substances contributed to increases in overall PO overdose deaths, and specifically synthetic opioids other than methadone (SO-M) overdose deaths which includes fentanyl, over the last twelve years in the population and in age, gender and race/ethnicity subgroups. We address three issues by analyzing national death records for 2002–03 and 2014–15 among all PO deaths, and among SO-M deaths, to capture indirectly changes related to fentanyl: (1) How has the proportion of PO deaths in combination with each of five central nervous system pharmaceutical or recreational psychoactive substances (benzodiazepines, antidepressants, heroin, alcohol, cocaine) changed in that interval? (2) What proportion of the increase in deaths is attributable to changes in deaths in combination with specific substances? (3) What are age, gender and racial/ethnic differences in these patterns?
2. Methods
2.1. Data
Data are from the Multiple-Cause-of-Death Files, National Vital Statistics System Wonder files (CDC, 2016) for PO overdose deaths for the years 2002–03 (N=15,973) and 2014–15 (N=41,491). One underlying cause-of-death, based on mechanism (e.g., overdose) and intent, and up to 20 contributing causes-of-deaths are recorded in death certificates (Slavova et al., 2015; Trinidad et al., 2016; Warner et al., 2016). Overdose/poisoning deaths involving PO are coded into three broad classes as per International Classification of Diseases-Tenth Edition (ICD-10) (National Center for Health Statistics, 2017): natural/semisynthetic opioids; methadone; synthetic opioids other than methadone (SO-M). Between 2002–2015, 17.0% to 28.9% of drug overdose death certificates lacked information about contributing drugs (Rudd et al., 2016a; Trinidad et al., 2016; Warner et al., 2009; 2016).
The following ICD-10 codes were used for selecting cases:
Drug overdose deaths: underlying cause of death X40-X44 (unintentional), X60-X64 (suicide), X85 (assault), Y10-Y14 (undetermined intent).
PO overdose deaths: (1) and one contributing cause-of-death code T40.2 (natural and semisynthetic opioids, e.g., morphine, oxycodone, hydrocodone), T40.3 (methadone), T40.4 (SO-M, e.g., fentanyl, tramadol, propoxyphene, meperidine).
SO-M overdose deaths: (1) and code T40.4 (SO-M).
Heroin-related overdose: (1) and T40.1 (heroin).
Benzodiazepine-related overdose: (1) and T42.4 (benzodiazepine).
Antidepressant-related overdose: (1) and T43.0-T43.2 (antidepressant).
Cocaine-related overdose: (1) and T40.5 (cocaine).
Alcohol poisoning-related overdose: (1) and T51.0 (toxic ethanol effect), T51.9 (toxic effect of unspecified alcohol).
2.2. Variables
Gender: male, female.
Age: 0–17; 18–34; 35–49; 50 and older.
Race/ethnicity: non-Hispanic white; non-Hispanic African-American; Hispanic.
2.3. Analytical Strategy
We examined changes in proportions of PO deaths in combination with other substances between 2002–03 and 2014–15 for all PO deaths and for SO-M deaths. We calculated (1) changes in proportions of deaths in combination with benzodiazepines, antidepressants, heroin, alcohol, or cocaine between 2002–03 and 2014–15, and (2) the proportion of increase in deaths attributable to each substance in combination, as the difference between actual and expected number of deaths in combination with specific substances in 2014–15 divided by the total number of increased deaths between the two periods. Expected number of deaths was the 2014–15 number multiplied by the proportion of deaths in combination with other substances in 2002–03. Thus, in 2002–03, benzodiazepine-related deaths (N=2,682) constituted 16.791% of all PO deaths (N=15,973); in 2014–15, the expected number was 6,967=(16.791%×41,491 PO deaths). The difference between actual and expected numbers was 4,626=(11,593-6,967). Since PO deaths increased by 25,518 cases (41,491-15,973), the attributable proportion increase in PO-benzodiazepine deaths was 18.1%=(4,626/25,518).
For each substance, the attributable proportion of increase depends on the initial proportion among PO deaths in 2002–03, the percent change by 2014–15, and the increase in number of deaths between 2002–03 and 2014–15 for each group. Given the same percent change, the attributable proportions can be different, given differences in base number of deaths and the number of increased deaths for a particular group.
Statistical significance of differences in ratios of proportions and attributable proportions were evaluated by the log-linked Poisson model.
3. Results
3.1. Changes in PO Deaths by Opioid Class
Between 2002–03 and 2014–15, overall PO deaths increased 2.6 times (Table 1); methadone deaths increased 1.3 times; SO-M deaths increased 5.6 times. In 2002–03, 58.1% of PO deaths involved natural and semisynthetic opioids, 33.4% methadone, 16.9% SO-M versus 60.0%, 16.2%, 36.5%, respectively, in 2014–15.
Table 1.
Changes in proportions of prescription opioid deaths in combination with five other substances between 2002–03 and 2014–15 among all prescription opioid deaths and by class of prescription opioid deaths.
| Deaths in Combination With: | All Prescription Opioid Deaths | Natural and Semi-Synthetic Opioid Deaths | Methadone Deaths | Synthetic Opioids Other than Methadone Deaths | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| 2002–03 % |
2014–15 % |
Changes Between 2002–03 and
2014–15 Ratio (95%CI)a |
2002–03 % |
2014–15 % |
Changes Between 2002–03 and
2014–15 Ratio (95%CI)a |
2002–03 % |
2014–15 % |
Changes Between 2002–03 and
2014–15 Ratio (95%CI)a |
2002–03 % |
2014–15 % |
Changes Between 2002–03 and
2014–15 Ratio (95%CI)a |
|
| Benzodiazepines | 16.8 | 27.9 | 1.7 (1.6–1.7) | 18.3 | 33.7 | 1.8 (1.8–1.9)b | 17.1 | 30.7 | 1.8 (1.7–1.9)b | 17.5 | 20.0 | 1.1 (1.0–1.3)c |
| Antidepressants | 13.2 | 12.9 | 1.0 (0.9–1.0) | 13.0 | 15.2 | 1.2 (1.1–1.2)b | 13.2 | 12.7 | 1.0 (0.9–1.1)c | 17.4 | 10.1 | 0.6 (0.5–0.6)d |
| Heroin | 4.6 | 15.4 | 3.3 (3.1–3.6) | 6.9 | 10.6 | 1.5 (1.4–1.7)b | 1.8 | 9.6 | 5.3 (4.3–6.6)c | 1.2 | 24.5 | 21.3 (15.0–30.3)d |
| Alcohol | 8.5 | 13.7 | 1.6 (1.5–1.7) | 9.7 | 14.7 | 1.5 (1.4–1.6) | 5.8 | 9.2 | 1.6 (1.4–1.8) | 9.1 | 12.9 | 1.4 (1.3–1.6) |
| Cocaine | 12.6 | 10.1 | 0.8 (0.8–0.8) | 12.9 | 8.0 | 0.6 (0.6–0.7)b | 14.5 | 8.7 | 0.6 (0.5–0.7)b | 6.5 | 14.3 | 2.2 (1.9–2.6)c |
| Any of 5 substances | 44.3 | 57.9 | 1.3 (1.3–1.3) | 48.2 | 60.0 | 1.2 (1.2–1.3)b | 41.9 | 52.3 | 1.2 (1.2–1.3)b | 40.5 | 58.0 | 1.4 (1.4–1.5)c |
| Total Deaths (N) | (15,973) | (41,491) | 2.6 (=41,491/15,973) | (9,283) | (24,886) | 2.7 (=24,886/9,283) | (5,330) | (6,701) | 1.3 (=6,701/5,330) | (2,695) | (15,124) | 5.6 (=15,124/2,695) |
, where a and b equal the number of deaths in combination with other substances in 2002–03 and 2014–15.
For each substance-related death, different superscripts indicate statistically significant (p<0.05) differences between the classes of prescription opioids in change ratios.
3.2. Changes in PO Deaths in Combination with Other Substances
The proportion of all PO deaths in combination with any of the five psychoactive substances increased 1.3 times (95% CI=1.3–1.3), from 44.3% in 2002–03 to 57.9% in 2014–15 (Table 1). PO deaths in combination with specific substances increased for all drugs, except cocaine, which decreased (10.1%), and antidepressants, which remained the same. Extent of change varied by combination substance. Heroin-related deaths more than tripled (change ratio=3.3 [95% CI=3.1–3.6]). Benzodiazepine and alcohol-related deaths increased by factors of 1.7 (95% CI = 1.6–1.7) and 1.6 (95% CI = 1.5–1.7), respectively. Cocaine-related deaths decreased (0.8 [95% CI = 0.8–0.8]) (Table 1).
The proportion of specific drug combinations varied substantially by class of PO deaths (Table 1). At both periods, the most frequent combination was with benzodiazepines: 16.8% in 2002–03, 27.9% in 2014–15. Antidepressants (13.2%) and cocaine (12.6%) were next in 2002–03, heroin (15.4%) and alcohol (13.7%) in 2014–15. In 2014–15, among (1) natural and semisynthetic opioids and (2) methadone deaths, benzodiazepines ranked first (27.9%), heroin was next but a third as prevalent (15.4%). Among SO-M deaths, heroin was first (24.5%) and benzodiazepines a close second (20.0%). Although heroin-related deaths increased more than any other drug combination among all three PO classes, the change ratio for heroin was strikingly higher among SO-M (21.3 [95% CI = 15.0–30.3]) than natural/semisynthetic opioids (1.5 [95% CI = 1.4–1.7]) and methadone (5.3 [95% CI = 4.3–6.6]) deaths. Cocaine-related deaths decreased among natural/semisynthetic opioids (0.6 [95% CI = 0.6–0.7]) and methadone (0.6 [95% CI = 0.5–0.7]) deaths, but doubled (2.2 [95% CI = 1.9–2.6]) among SO-M deaths.
3.2.1. Increases in PO Deaths Attributable to Other Substances
The proportions of increased deaths in 2014–15 attributable to combinations with each psychoactive substance exceeding those expected based on their proportions in 2002–03 were calculated.
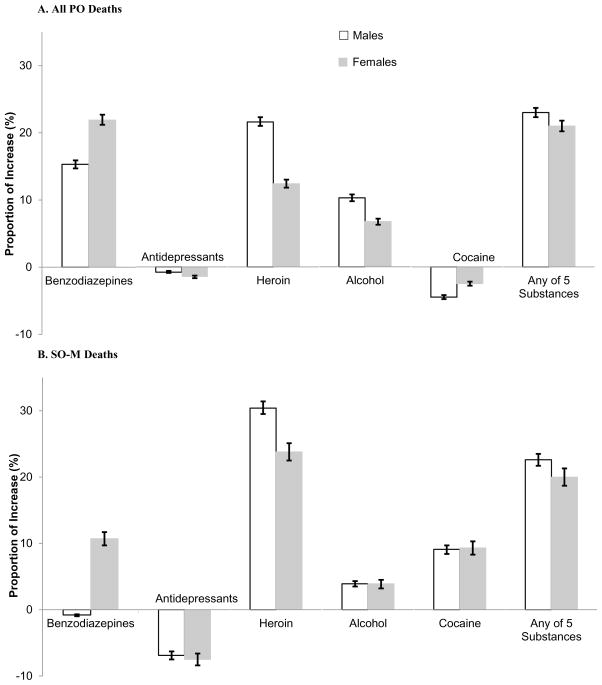
Of the increases in deaths, 22.1% (95% CI = 21.6%–22.6%) among all PO deaths and 21.3% (95% CI = 20.6%–22.0%) among SO-M deaths were attributable to deaths involving any of the five substances (Figure 1, Supplementary Table 11). Among all PO deaths, the largest increases were attributable to benzodiazepines and heroin (18.1% [95% CI = 17.7%–18.6%]; 17.5% [95% CI = 17.0%–18.0%]), followed by alcohol (8.5% [95% CI = 8.2%–8.8%]). Cocaine was associated with a 3.9% (95% CI = −4.2%–−3.7%) decrease in deaths and antidepressants with a −0.5% (95% CI = −0.6%–−0.4%) decrease. Among SO-M deaths, the largest increase was attributable to heroin (28.5% [95% CI = 27.7%–29.3%]); cocaine was second (9.6% [95% CI = 9.1%–10.1%]). Only 3% (95% CI = 2.7%–3.3%) of the increase was attributable to benzodiazepines.
Figure 1.
Attributable proportions of increases in prescription opioid (PO) deaths in combination with five other substances between 2002–03 and 2014–15 among (A) all prescription opioid (PO) deaths, and (B) synthetic opioids other than methadone (SO-M) deaths.
Because of multiple substance combinations, the increase in deaths attributable to each substance included a component uniquely attributable to that substance and one attributable to additional substances. Thus, in 2014–15, 67.0% of PO deaths in combination with one of the five psychoactive substances involved one substance, 28.0% a second substance, 4.6% a third one. Proportions attributable uniquely to one substance varied across type of PO death and substance. Among all PO deaths, the proportional increase attributable to only one substance in combination varied from 48.0% for benzodiazepines, 45.6% for heroin, to 26.7% for alcohol. Among SO-M deaths, these percentages were 54.3% for heroin, 5.9% for alcohol, 22.5% for cocaine (Supplementary Table 11).
3.3 PO Deaths by Age
3.3.1. Changes in PO Deaths in Combination with Other Substances by Age
Overall PO deaths increased most at ages 50 and older; SO-M deaths increased most at ages 18–34. Changes in deaths involving PO in combination with other substances were similar at all ages, with several exceptions (Table 2). Among all PO deaths, heroin-related deaths increased most at ages 18–34; alcohol-related deaths increased most at ages 50 and older. Among SO-M deaths, cocaine-related deaths increased more at ages 35 and older than ages 18–34.
Table 2.
Changes in proportions of prescription opioid deaths in combination with five other substances between 2002–03 and 2014–15 among all prescription opioid deaths and synthetic opioids other than methadone deaths, by age, gender and race/ethnicity.
| Deaths in Combination With: | All Prescription Opioid Deaths | Synthetic Opioids Other than Methadone Deaths | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 2002–03 % |
2014–15 % |
Changes Between 2002–03 and
2014–15 Ratio (95%CI)a |
2002–03 % |
2014–15 % |
Changes Between 2002–03 and
2014–15 Ratio (95%CI)a |
|
| AGEb | ||||||
| 18–34 | ||||||
| Benzodiazepines | 17.0 | 26.5 | 1.6 (1.4–1.7) | 18.8 | 17.7 | 0.9 (0.8–1.1)c |
| Antidepressants | 7.9 | 6.9 | 0.9 (0.8–1.0) | 12.4 | 5.0 | 0.4 (0.3–0.5)c |
| Heroin | 4.6 | 23.1 | 5.0 (4.3–5.7)c | 1.0 | 30.3 | 31.4 (14.1–69.7) |
| Alcohol | 8.6 | 12.3 | 1.4 (1.3–1.6)c | 8.0 | 10.7 | 1.3 (1.0–1.8) |
| Cocaine | 15.5 | 11.8 | 0.8 (0.7–0.8)c | 9.0 | 14.1 | 1.6 (1.2–2.0)c |
| Any of 5 substances | 43.5 | 58.4 | 1.3 (1.3–1.4) | 38.4 | 56.4 | 1.5 (1.3–1.6) |
| Total deaths (N) | (4,234) | (12,075) | 2.9 (=12,075/4,234) | (622) | (5,845) | 9.4 (=5,845/622) |
| 35–49 | ||||||
| Benzodiazepines | 16.9 | 28.6 | 1.7 (1.6–1.8) | 16.5 | 20.6 | 1.2 (1.1–1.4)d |
| Antidepressants | 14.1 | 14.0 | 1.0 (0.9–1.1) | 18.0 | 11.0 | 0.6 (0.5–0.7)d |
| Heroin | 4.6 | 15.3 | 3.4 (3.0–3.7)d | 1.2 | 23.9 | 19.8 (12.3–31.8) |
| Alcohol | 9.2 | 14.8 | 1.6 (1.5–1.7)c | 10.2 | 14.6 | 1.4 (1.2–1.7) |
| Cocaine | 12.9 | 11.6 | 0.9 (0.8–1.0)d | 6.4 | 16.6 | 2.6 (2.1–3.2)d |
| Any of 5 substances | 45.6 | 59.9 | 1.3 (1.3–1.4) | 41.3 | 60.7 | 1.5 (1.4–1.6) |
| Total deaths (N) | (8,212) | (14,412) | 1.8 (=14,412/8,212) | (1,406) | (5,265) | 3.7 (=5,265/1,406) |
| 50 and older | ||||||
| Benzodiazepines | 16.7 | 28.7 | 1.7 (1.6–1.9) | 18.9 | 22.6 | 1.2 (1.0–1.4)c,d |
| Antidepressants | 18.5 | 16.9 | 0.9 (0.8–1.0) | 21.3 | 16.5 | 0.8 (0.7–0.9)e |
| Heroin | 5.1 | 9.4 | 1.8 (1.6–2.1)e | 1.3 | 17.1 | 13.7 (6.9–27.3) |
| Alcohol | 7.0 | 14.0 | 2.0 (1.8–2.3)d | 7.8 | 14.0 | 1.8 (1.4–2.4) |
| Cocaine | 8.3 | 7.6 | 0.9 (0.8–1.0)d | 4.1 | 11.9 | 2.9 (2.0–4.3)d |
| Any of 5 substances | 43.6 | 56.1 | 1.3 (1.2–1.3) | 41.6 | 57.2 | 1.4 (1.2–1.5) |
| Total deaths (N) | (3,292) | (14,726) | 4.5 (=14,726/3,292) | (639) | (3,951) | 6.2 (=3,951/639) |
| GENDER | ||||||
| Males | ||||||
| Benzodiazepines | 16.6 | 25.7 | 1.6 (1.5–1.6)f | 18.1 | 17.5 | 1.0 (0.8–1.1)f |
| Antidepressants | 9.1 | 8.6 | 0.9 (0.9–1.0) | 12.2 | 6.3 | 0.5 (0.4–0.6)f |
| Heroin | 6.2 | 19.1 | 3.1 (2.8–3.3)f | 1.6 | 27.6 | 17.3 (11.5–25.9) |
| Alcohol | 10.4 | 16.5 | 1.6 (1.5–1.7)f | 11.5 | 14.7 | 1.3 (1.1–1.5) |
| Cocaine | 14.5 | 11.8 | 0.8 (0.8–0.9) | 7.7 | 15.5 | 2.0 (1.7–2.4) |
| Any of 5 substances | 45.2 | 58.9 | 1.3 (1.3–1.3) | 39.1 | 58.4 | 1.5 (1.4–1.6) |
| Total deaths (N) | (10,039) | (24,781) | 2.5 (=24,781/10,039) | (1,438) | (10,025) | 7.0 (=10,025/1,438) |
| Females | ||||||
| Benzodiazepines | 17.1 | 31.2 | 1.8 (1.7–2.0) | 16.9 | 24.9 | 1.5 (1.3–1.7) |
| Antidepressants | 20.3 | 19.3 | 1.0 (0.9–1.0) | 23.3 | 17.7 | 0.8 (0.7–0.9) |
| Heroin | 2.0 | 10.0 | 5.0 (4.2–6.0) | 0.6 | 18.5 | 29.1 (14.6–58.2) |
| Alcohol | 5.2 | 9.6 | 1.8 (1.6–2.1) | 6.3 | 9.2 | 1.5 (1.2–1.9) |
| Cocaine | 9.2 | 7.6 | 0.8 (0.8–0.9) | 5.0 | 12.0 | 2.4 (1.9–3.1) |
| Any of 5 substances | 42.8 | 56.4 | 1.3 (1.3–1.4) | 42.2 | 57.2 | 1.4 (1.3–1.5) |
| Total deaths (N) | (5,934) | (16,710) | 2.8 (=16,710/5,934) | (1,257) | (5,099) | 4.1 (=5,099/1,257) |
| RACE/ETHNICITY | ||||||
| Whites | ||||||
| Benzodiazepines | 17.8 | 29.2 | 1.6 (1.6–1.7)e | 18.2 | 21.3 | 1.2 (1.1–1.3) |
| Antidepressants | 13.5 | 13.3 | 1.0 (0.9–1.0) | 17.3 | 10.5 | 0.6 (0.6–0.7) |
| Heroin | 3.5 | 14.5 | 4.2 (3.8–4.6)g | 0.9 | 23.5 | 24.8 (16.5–37.3)g |
| Alcohol | 8.2 | 12.9 | 1.6 (1.5–1.7)g | 8.6 | 11.7 | 1.4 (1.2–1.6) |
| Cocaine | 10.9 | 8.9 | 0.8 (0.8–0.9) | 5.8 | 12.8 | 2.2 (1.9–2.6)g |
| Any of 5 substances | 42.7 | 57.3 | 1.3 (1.3–1.4)g | 40.2 | 57.0 | 1.4 (1.3–1.5) |
| Total deaths (N) | (13,710) | (34,951) | 2.5 (=34,951/13,710) | (2,429) | (12,680) | 5.2 (12,680/2,429) |
| African-Americans | ||||||
| Benzodiazepines | 8.6 | 17.4 | 2.0 (1.6–2.6)g,h | 10.6 | 10.5 | 1.0 (0.5–1.8) |
| Antidepressants | 12.5 | 10.4 | 0.8 (0.7–1.0) | 18.6 | 7.0 | 0.4 (0.2–0.6) |
| Heroin | 10.6 | 21.5 | 2.0 (1.7–2.5)h | 3.5 | 32.5 | 9.2 (3.5–24.1) g,h |
| Alcohol | 7.3 | 17.9 | 2.5 (1.9–3.2)h | 11.5 | 20.5 | 1.8 (1.1–3.0) |
| Cocaine | 30.1 | 21.7 | 0.7 (0.6–0.8) | 21.2 | 26.0 | 1.2 (0.8–1.8)h |
| Any of 5 substances | 53.6 | 62.3 | 1.2 (1.1–1.2)h | 42.5 | 65.7 | 1.5 (1.2–1.9) |
| Total deaths (N) | (879) | (3,082) | 3.5 (=3,082/879) | (113) | (1,332) | 11.8 (=1,332/113) |
| Hispanics | ||||||
| Benzodiazepines | 11.0 | 23.9 | 2.2 (1.8–2.6)h | 13.0 | 16.8 | 1.3 (0.7–2.2) |
| Antidepressants | 10.0 | 10.4 | 1.0 (0.8–1.3) | 16.7 | 8.4 | 0.5 (0.3–0.8) |
| Heroin | 14.7 | 20.9 | 1.4 (1.2–1.7)i | 3.7 | 27.7 | 7.5 (2.8–19.7) i |
| Alcohol | 11.1 | 18.3 | 1.6 (1.4–2.0)g | 13.0 | 17.8 | 1.4 (0.8–2.3) |
| Cocaine | 20.2 | 14.3 | 0.7 (0.6–0.8) | 8.3 | 20.1 | 2.4 (1.3–4.6)g,h |
| Any of 5 substances | 55.5 | 60.9 | 1.1 (1.0–1.2)h | 46.3 | 62.1 | 1.3 (1.1–1.7) |
| Total deaths (N) | (1,072) | (2,492) | 2.3 (=2,492/1,072) | (108) | (826) | 7.6 (=826/108) |
, where a and b equal the number of deaths in combination with other substances in 2002–03 and 2014–15.
Aged <18 are not shown.
For each substance-related death, different superscripts indicate statistically significant (p<.05) differences between age groups in change ratios among all prescription opioid and synthetic opioids other than methadone deaths.
For each substance-related death, superscript indicates statistically significant (p<.05) differences by gender in change ratios among all prescription opioid and synthetic opioids other than methadone deaths.
For each substance-related death, different superscripts indicate statistically significant (p<.05) differences between race/ethnicity groups in change ratios among all prescription opioid and synthetic opioids other than methadone deaths.
3.3.2. Increases in PO Deaths Attributable to Other Substances by Age
Proportional increases in PO deaths attributable to specific substance combinations varied by age (Figure 2, Supplementary Table 22). Among all PO deaths, those in combination with heroin contributed most to increased deaths at ages 18–34 (28.5% [95% CI = 27.5%–29.5%]) and 35–49 (25.0% [95% CI = 24.0%–26.1%]). Benzodiazepines did so at ages 35–49 (27.1% [95% CI = 26.0%–28.2%). There was a reversal with increasing age in the relative increases in deaths attributable to heroin and benzodiazepines. At ages 18–34, increases attributable to heroin (28.5%) contributed 1.9 times as much as benzodiazepines (14.6% [95% CI=13.8%–15.4%]); at ages 35–49, both drugs contributed equally; at ages 50+, increases attributable to benzodiazepines (15.5% [95% CI=14.8%–16.1%]) were almost three times higher than heroin (5.5% [95% CI=5.1%–5.9%]). Among all PO deaths, the largest increases attributable to alcohol occurred at ages 35–49; the largest decrease associated with cocaine occurred at ages 18–34. Among SO-M deaths, the largest proportion of increased deaths was attributable to heroin at all ages, but especially ages 18–49. The proportion of increased deaths attributable to cocaine was highest at ages 35–49.
Figure 2.
Attributable proportions of increases in prescription opioid (PO) deaths in combination with five other substances between 2002–03 and 2014–15 among (A) all prescription opioid (PO) deaths, and (B) synthetic opioids other than methadone (SO-M) deaths, by age.
3.4. PO Deaths by Gender
3.4.1. Changes in PO Deaths in Combination with Other Substances by Gender
While increases in number of overall PO deaths from 2002–03 to 2014–15 did not differ by gender, the increases in number of SO-M deaths were 70% higher among males (increased 7 times) than females (increased 4.1 times) (Table 2). Increases in proportions of deaths involving all PO and SO-M in combination with any of the five psychoactive substances were similar for males and females (change ratios=1.3–1.5). However, among PO and SO-M deaths, deaths in combination with benzodiazepines increased more for females than males (Table 2).
3.4.2. Increases in PO Deaths Attributable to Other Substances by Gender
The largest proportion of increased overall PO deaths was attributable to heroin among males, benzodiazepines among females. The largest proportion of increased SO-M deaths was attributable to heroin among both genders, but especially males (Figure 3, Supplementary Table 23).
Figure 3.
Attributable proportions of increases in prescription opioid (PO) deaths in combination with five other substances between 2002–03 and 2014–15 among (A) all prescription opioid (PO) deaths, and (B) synthetic opioids other than methadone (SO-M) deaths, by gender.
3.5. PO Deaths by Race/Ethnicity
3.5.1. Changes in PO Deaths in Combination with Other Substances by Race/Ethnicity
Increases in overall PO deaths, those in combination with other substances, and patterns of change differed by race/ethnicity. PO deaths, especially SO-M deaths, increased more among African-Americans (3.5 times all PO deaths, 11.8 times SO-M deaths) than whites or Hispanics (Table 2). The proportion of PO deaths in combination with any of five psychoactive substances in 2002–03 was higher among minorities than whites (Table 2). By 2014–15, PO deaths involving other substances had increased among all groups, and racial/ethnic differences were attenuated.
Among all PO deaths in 2002–03, the proportions of benzodiazepine-related deaths were higher than other combinations among whites, cocaine-related deaths were higher among minorities. By 2014–15, the proportions of heroin-related deaths had increased more among whites than minorities: change ratio=4.2 (95% CI = 3.8–4.6) among whites, 2.0 (95% CI = 1.7–2.5) among African-Americans, 1.4 (95% CI = 1.2–1.7) among Hispanics. Proportions of benzodiazepine-related deaths increased more among Hispanics than whites; alcohol-related deaths increased the most among African-Americans. In 2014–15, PO deaths in combination with benzodiazepines were most prevalent among whites, those involving heroin and cocaine among African-Americans, those involving heroin and benzodiazepines among Hispanics.
Among SO-M deaths, the proportions of heroin-related deaths increased more among whites (change ratio=24.8 [95% CI =16.5–37.3]) than African-Americans (9.2 [95% CI = 3.5–24.1]) and Hispanics (7.5 [95% CI = 2.8–19.7]). The proportions of cocaine-related deaths increased more among whites than African-Americans (Table 2). In 2014–15, the most prevalent combination was with heroin across race/ethnicity groups.
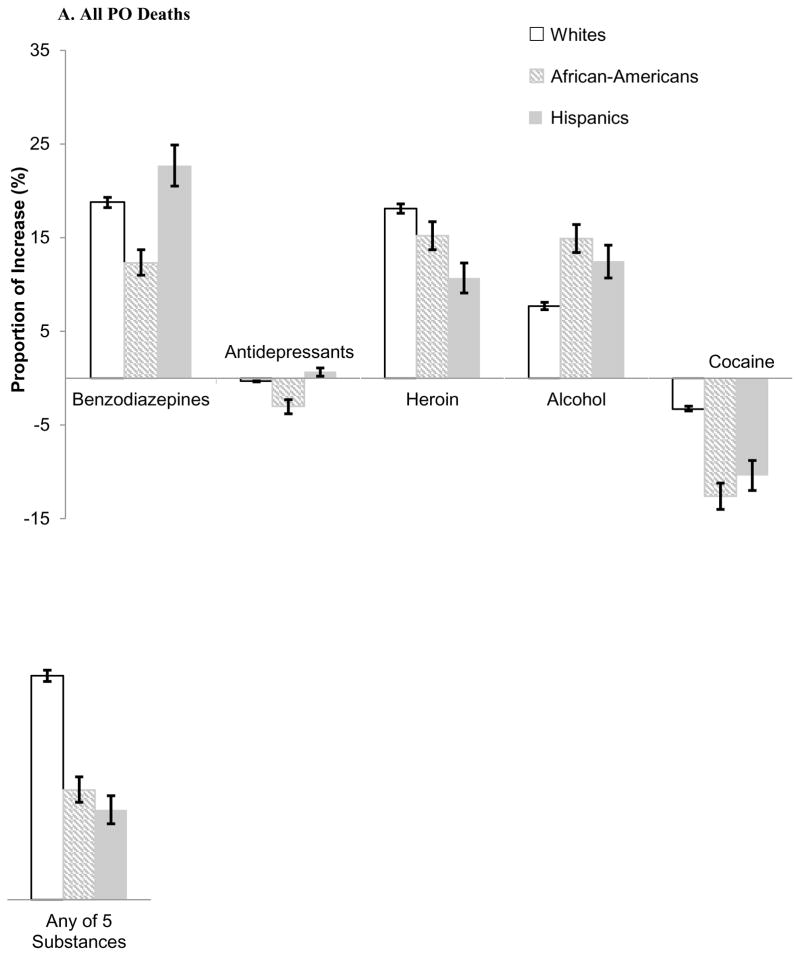
3.5.2. Increases in PO Deaths Attributable to Other Substances by Race/Ethnicity
The proportional increase in all PO deaths attributable to any of the five psychoactive substances was much higher for whites (24.0% [95% CI = 23.3%–24.5%] than African-Americans (12.2% [95% CI = 10.3%–13.0%]) or Hispanics (9.6% [95% CI = 8.1%–11.1%]). Among SO-M deaths, the increase attributable to substances in combination was highest among African-Americans (Figure 4, Supplementary Table 24).
Figure 4.
Attributable proportions of increases in prescription opioid (PO) deaths in combination with five other substances between 2002–03 and 2014–15 among (A) all prescription opioid (PO) deaths, and (B) synthetic opioids other than methadone (SO-M) deaths, by race/ethnicity.
Among all PO deaths, the increase attributable to heroin was higher among whites (18.1% [95% CI = 17.6%–18.6%]) than African-Americans (15.3% [95% CI = 13.7%–16.7%]) and Hispanics (10.8% [95% CI = 9.2%–12.4%]). The decrease in deaths attributable to cocaine was highest among minorities. Among SO-M deaths, the increase attributable to heroin was similar for all racial/ethnic groups; the increase attributable to cocaine was highest among Hispanics.
4. Discussion
Between 2002–03 and 2014–15, overall PO overdose deaths more than doubled; those involving SO-M increased over five times. To provide some insight into these increases, we implemented a novel analysis in which we examined concomitantly five psychoactive substances (benzodiazepines, antidepressants, heroin, alcohol, cocaine) listed in death records as contributing to PO deaths. We estimated the proportions of increase in overdose deaths over a twelve-year period attributable to increases in combination with specific substances. SO-M deaths were examined separately to capture indirectly the consequences of changing patterns of fentanyl deaths included in these deaths, since only broad drug classes, but not specific drugs, are identified in the Multiple-Cause-of-Death Files. Using this approach, we found that increases of almost one-fifth of all PO and SO-M deaths were attributable to substances in combination.
In 2014–15, 57.9% of all PO deaths involved one of five other psychoactive substances versus 44.3% in 2002–03. Benzodiazepines and heroin each contributed similar increases to all PO deaths, while heroin contributed to a much larger proportion of increased SO-M deaths than benzodiazepines (28.5% vs. 3.0%). However, cocaine-related deaths decreased among all PO deaths, but increased among SO-M deaths, and tempered the overall increase in all PO deaths. Cocaine was next in importance to heroin in its association with increased SO-M deaths. There were age, gender and racial/ethnic differences. At ages 50 and over, PO deaths in combination with benzodiazepines contributed more to all PO deaths than heroin. Heroin contributed more to increased deaths at ages 18–49 and among males than females for all PO and SO-M deaths. The proportion of heroin-related deaths was consistently lower among whites than minorities but increased substantially among whites. Despite the small number of heroin users in the population, increases in heroin-related deaths contributed markedly to the overall increase in PO deaths. Recent reports document that the increase in SO-M deaths is from increases in illicit fentanyl in combination with heroin (Gladden et al., 2016; Peterson et al., 2016) and cocaine (Tomassoni et al., 2017).
Increases in PO deaths involving other substances might be partially explained by increases in intensive nonmedical prescription use, since heavy users are more likely to use other substances (Han et al., 2015; Jones, 2013). Whether this is also the case for medical users cannot be ascertained, since trend data are unavailable. Our analyses of national 2015 data from the National Survey on Drug Use and Health (SAMHSA, 2016) indicate that past-year nonmedical benzodiazepine, cocaine and heroin use by exclusive medical users was only slightly higher than among non-PO users and much lower than among NMPO users (Supplementary Table 35). Thus, deaths in combination with other substances may be less prevalent among medical than nonmedical PO deaths. However, the respective proportions of PO deaths due to medical or nonmedical use are unknown. Many causes of increased PO mortality, besides deaths in combination with other substances, remain to be understood. These factors include increases in specific opioids used, intensity of use, opioid use disorder, medical, psychiatric or drug-disorder co-morbidities (Bohnert et al., 2016; Han et al., 2015), drug strength and purity (Pain and Policy Studies Group/WHO Collaborating Center, 2015), addition of toxic compounds, such as illicit fentanyl in heroin and cocaine (CDC, 2016, 2017; DEA, 2016; Gladden et al., 2016; Paone et al., 2016; Suzuki and El-Haddad, 2017). Number of prescriptions (Hwang et al., 2016; Volkow, 2014), variations in prescribing across states (CDC, 2014), changes in drug market, availability, and price may have also contributed to changing mortality patterns, as have broader societal changes, such as economic downturns (Carpenter et al., 2016). Except for combinations with other substances, these factors cannot be linked to death records, and their contributions to increased PO deaths cannot be evaluated.
Understanding the causes of PO deaths would be enhanced if medical and nonmedical PO users could be compared and if deaths could be linked to users’ behaviors prior to death, such as patterns of opioid use, use of other substances, or mental and physical health status. Longitudinal data from large cohorts sampled at different historical periods necessary to establish these linkages are unavailable.
Death records have limitations that may have affected our conclusions, including variations in the determination of causes of deaths, in testing or reporting, drug misidentification, missing data on specific drugs in different parts of the United States and at different periods, and the undercount of Hispanics (Arias et al., 2016; Hedegaard et al., 2014; Rudd et al., 2016a; Warner et al., 2009; 2016). The quality and completeness of reporting of specific substances involved in drug overdose deaths have varied substantially across time, as noted under Methods. Thus, increased PO overdose deaths may be due to improved post-mortem testing and overdose certification practices (Davis, 2014; Goldberger et al., 2013; Warner et al., 2016), as well as to increased use of other substances.
The findings highlight that one-fifth of the increase in PO overdose deaths over the last decade involved other substances in combination, particularly benzodiazepines and heroin, that a lower percentage among overall PO deaths involved cocaine, counterbalancing the increase among SO-M deaths, and that combinations with other substances vary among different age, gender and racial/ethnic groups. The greatest increases in heroin-related deaths occurred at ages 18–49 and for males among all PO and SO-M deaths.
Different groups of prescription opioid users will require different approaches to reduce morbidity and mortality. For populations in treatment for chronic pain, recommendations issued by the CDC for primary care physicians (Dowell et al., 2016) include reducing concurrent prescribing of opioids and benzodiazepines; educating patients regarding the risk of respiratory depression and overdose when prescription opioids are taken with benzodiazepines, alcohol, or illicit drugs, including heroin; addressing substance use, mental health and other comorbidities that increase the risk for polysubstance use; and drug testing to monitor the use of controlled and illicit substances. From public health and developmental perspectives, preventing polysubstance use may reduce morbidity and mortality associated with PO. Prevention and intervention efforts targeted toward reducing mortality associated with PO needs to take into account the type of opioid used, the frequency of opioid use and disorder, and use of other substances in different groups in the population.
Supplementary Material
Highlights.
22% of increased prescription opioid (PO) deaths are attributable to 5 other drugs.
Benzodiazepines and heroin contribute equally to increased PO deaths.
Heroin contributes most to increased PO deaths at ages 18–49, among males, whites.
Increased non-methadone synthetic opioid deaths are mostly attributable to heroin.
Acknowledgments
Role of Funding Source
This research was supported by grant R01 DA036748 from the National Institute on Drug Abuse (D. Kandel, PI). Support was also provided by the New York State Psychiatric Institute (Griesler). The funding agency had no part in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
We thank the reviewers for their insightful comments. We would also like to acknowledge Benjamin Jenkins’ assistance in the preparation of the manuscript.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
D. Kandel conceptualized the analysis. M. Hu conducted the data analysis. M. Wall provided statistical consultation. All of the authors contributed to the design of the analysis, reviewed the analysis, and participated in the writing of the manuscript.
Conflicts of Interest
The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arias E, Heron M, Hakes JK. Vital Health Stat. 176. Vol. 2. U.S. Census Bureau, National Center for Health Statistics; 2016. The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. [PubMed] [Google Scholar]
- Babalonis S, Walsh SL. Warnings unheeded: the risks of co-prescribing opioids and benzodiazepines. Pain Clin Updates. 2015;23:1–7. [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. 2016;106:686–88. doi: 10.2105/AJPH.2016.303061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berecki-Gisolf J, Hassani-Mahmooei B, Clapperton A, McClure R. Prescription opioid dispensing and prescription opioid poisoning: population data from Victoria, Australia 2006 to 2013. Aust N Z J Public Health. 2017;41:85–91. doi: 10.1111/1753-6405.12568. http://dx.doi.org/10.1111/1753-6405.12568. [DOI] [PubMed] [Google Scholar]
- Berterame S, Erthal J, Thomas J, Fellner S, Vosse B, Clare P, Hao W, Johnson DT, Mohar A, Pavadia J, Samak AKE, Sipp W, Sumyai V, Suryawati S, Toufiq J, Yans R, Mattick RP. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387:1644–56. doi: 10.1016/S0140-6736(16)00161-6. http://dx.doi.org/10.1016/S0140-6736(16)00161-6. [DOI] [PubMed] [Google Scholar]
- Bohnert A, Logan JE, Ganoczy D, Dowell D. A detailed exploration into the association of prescribed opioid dosage and overdose deaths among patients with chronic pain. Med Care. 2016;54:435–41. doi: 10.1097/MLR.0000000000000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcaterra S, Binswanger IA. Psychostimulant-related deaths as reported by a large national database. Subst Abuse. 2013;34:129–36. doi: 10.1080/08897077.2012.726959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcaterra S, Glanz J, Binswanger IA. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug Alcohol Depend. 2013;131:263–70. doi: 10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CS, McClellen CB, Rees DI. Economic conditions, illicit drug use, and substance use disorders in the United States. Working Paper 22051, NBER Working Paper Series; National Bureau of Economic Research; Cambridge, MA. 2016. pp. 1–38. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Opioid painkiller prescribing: where you live makes a difference. CDC, National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention; Atlanta, GA: 2014. [Accessed January 18, 2017]. https://www.cdc.gov/vitalsigns/opioid-prescribing/ [Google Scholar]
- Centers for Disease Control and Prevention. What is fentanyl? 2017. CDC, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention; Atlanta, GA: 2016. https://www.cdc.gov/drugoverdose/opioids/fentanyl.html. [Google Scholar]
- Centers for Disease Control and Prevention. CDC, Data are from the Multiple Cause of Death Files, 1999–2015, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. National Center for Health Statistics; 2016. [Accessed: December 20, 2016]. Multiple Cause of Death 1999–2015 on CDC WONDER Online Database. http://wonder.cdc.gov/mcd-icd10.html. [Google Scholar]
- Centers for Disease Control and Prevention. Opioid data analysis: categories of opioids. Vol. 2017. CDC; Atlanta, GA: 2017. https://www.cdc.gov/drugoverdose/data/analysis.html. [Google Scholar]
- Chen LH, Hedegaard H, Warner M. NCHS Data Brief. National Center for Health Statistics; Hyattsvill, MD: 2014. Drug-poisoning deaths involving opioid analgesics: United States, 1999–2011; p. 166. [PubMed] [Google Scholar]
- Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 2003;98:739–47. doi: 10.1046/j.1360-0443.2003.00376.x. http://dx.doi.org/10.1046/j.1360-0443.2003.00376.x. [DOI] [PubMed] [Google Scholar]
- Compton WM, Boyle M, Wargo E. Prescription opioid abuse: problems and responses. Prev Med. 2015;80:5–9. doi: 10.1016/j.ypmed.2015.04.003. http://www.dx.doi.org/10.1016/j.ypmed.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154–63. doi: 10.1056/NEJMra1508490. http://www.dx.doi.org/10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Duflou J, Path MM, Torok M. Comparative toxicology of intentional and accidental heroin overdose. J Forensic Sci. 2010;55:1015–8. doi: 10.1111/j.1556-4029.2010.01385.x. http://dx.doi.org/10.1111/j.1556-4029.2010.01385.x. [DOI] [PubMed] [Google Scholar]
- Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisi KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2016;17:85–98. doi: 10.1111/pme.12907. http://dx/doi.org/10.1111/pme.12907. [DOI] [PubMed] [Google Scholar]
- Davis G. Complete republication: National Association of Medical Examiners position paper: recommendations for the investigations, diagnosis, and certification of deaths related to opioid drugs. J Med Toxicol. 2014;10:100–6. doi: 10.1007/s13181-013-0323-x. http://dx.doi.org/10.1007/s13181-013-0323-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Whiteford HA, Ferrari AJ, Charlson FJ, Hall WD, Freedman G, Burstein R, Johns N, Engell RE, Flaxman A, Murray CJ, Vos T. Global burden of disease attributable to illicit drug use and dependence: findings from the global burden of disease study 2010. Lancet. 2013;382:1564–74. doi: 10.1016/S0140-6736(13)61530-5. http://dx.doi.org/10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- Dhalla IA, Persaud N, Juurlink DN. Facing up to the prescription opioid crisis. BMJ. 2011;343:d5142. doi: 10.1136/bmj.d5142. http://dx.doi.org/10.1136/bmj.d5142. [DOI] [PubMed] [Google Scholar]
- Drug Enforcement Administration. National heroin threat assessment summary. [Accessed: January 18, 2017];DEA Intelligence Report, U.S Department of Justice (DOJ), Drug Enforcement Administration: Strategic Intelligence Section. 2016 https://www.dea.gov/divisions/hq/2016/hq062716_attach.pdf.
- European Monitoring Centre for Drugs and Addiction. European drug report. EMCDDA; Lisbon, Portugal: 2014. http://www.emcdda.europa.eu/edr2014. [Google Scholar]
- Fischer B, Jones W, Urbanoski K, Skinner R, Rehm J. Correlations between prescription opioid analgesic dispensing levels and related mortality in Ontario, Canada, 2005–2011. Drug Alcohol Rev. 2014;33:19–26. doi: 10.1111/dar.12089. http://dx.doi.org/10.1111/dar.12089. [DOI] [PubMed] [Google Scholar]
- Franklin G, Sabel J, Jones CM, Mai J, Baumgartner C, Banta-Green CJ, Neven D, Tauben DJ. A comprehensive approach to address the prescription opioid epidemic in Washington State: Milestones and lessons learned. Am J Public Health. 2015;105:463–9. doi: 10.2105/AJPH.2014.302367. http://www.dx.doi.org/10.2105/AJPH.2014.302367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenk SM, Porter KS, Paulozzi LJ. Prescription opioid analgesic use among adults: United States 1999–2012. 189. National Center for Health Statistics (NCHS); Hyattsville, MD: 2015. [PubMed] [Google Scholar]
- Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths - 27 states, 2013–2014. MMWR. 2016;65:837–43. doi: 10.15585/mmwr.mm6533a2. http://dx.doi.org/10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- Goldberger BA, Maxwell JC, Campbell A, Wilford BB. Uniform standards and case definitions for classifying opioid-related deaths: Recommendations by a SAMHSA concensus panel. J Addict Dis. 2013;32:231–43. doi: 10.1080/10550887.2013.824334. http://dx.doi.org/10.1080/10550887.2013.824334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171:686–91. doi: 10.1001/archinternmed.2011.117. http://dx.doi.org/10.1001/archinternmed.2011.117. [DOI] [PubMed] [Google Scholar]
- Gudin JA, Mogali S, Jones JD, Comer SD. Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgrad Med. 2013;125:115–30. doi: 10.3810/pgm.2013.07.2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314:1468–78. doi: 10.1001/jama.2015.11859. http://www.dx.doi.org/10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, Paulozzi L, Johnson R. Excerpts from: Issues to consider when analyzing ICD-10 coded data on drug poisoning (overdose) deaths. National Center for Health Statistics (NCHS), and the National Center for Injury Prevention and Control; 2014. [Google Scholar]
- Hu MC, Griesler PC, Wall M, Kandel DB. Age-related patterns and trends in nonmedical prescription opioid use in the US population from 2002 to 2014. Drug Alcohol Depend. 2017;177:237–43. doi: 10.1016/j.drugalcdep.2017.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang CS, Kang EM, Kornegay CJ, Staffa JA, Jones CM, McAninch JK. Trends in the concomitant prescribing of opioids and benzodiazepines, 2002–2014. Am J Prev Med. 2016;51:151–60. doi: 10.1016/j.amepre.2016.02.014. [DOI] [PubMed] [Google Scholar]
- Jann M, Kennedy WH, Lopez G. Benzodiazepines: A major component in unintentional prescription drug overdoses with opioid analgesics. J Pharm Prac. 2014;27:5–16. doi: 10.1177/0897190013515001. [DOI] [PubMed] [Google Scholar]
- Jones CM. Frequency of prescription pain reliever nonmedical use: 2002–2003 and 2009–2010. Arch Intern Med. 2012;172:1265–7. doi: 10.1001/archinternmed.2012.2533. [DOI] [PubMed] [Google Scholar]
- Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers–United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132:95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Jones CM, Baldwin GT, Compton WM. Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health. 2017;107:430–2. doi: 10.2105/AJPH.2016.303627. http://dx.doi.org/10.2105/AJPH.2016.303627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden M, Bohm MK. Vital signs: Demographic and substance use trends among heroin users – United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 2015;64:719–25. [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States 2010. JAMA. 2013;309:657–9. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- Jones CM, McAninch JK. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am J Prev Med. 2015;49:493–501. doi: 10.1016/j.amepre.2015.03.040. [DOI] [PubMed] [Google Scholar]
- Jones CM, Paulozzi LJ, Mack KA. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths -- United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63:881–5. [PMC free article] [PubMed] [Google Scholar]
- Jones JD, Mogali S, Comer SD. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125:8–18. doi: 10.1016/j.drugalcdep.2012.07.004. http://dx.doi.org/10.1016/j.drugalcdep.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolata G, Cohen S. Drug overdoses propel rise in mortality rates of whites. New York Times; New York, NY: 2016. Jan 17, [Accessed: January 18, 2016]. www.nytimes.com/2016/01/17/science/drug-overdoses-propel-rise-in-mortality-rates-of-young-whites.html. [Google Scholar]
- Martins SS, Segura LE, Santaella-Tenorio J, Perimutter A, Fenton MC, Cerdá M, Keyes KM, Ghandour LA, Storr CL, Hasin DS. Prescription opioid use disorder and heroin use among 12–34 year-olds in the United States from 2002 to 2014. Addict Behav. 2017;65:236–41. doi: 10.1016/j.addbeh.2016.08.033. http://dx.doi.org/10.1016/j.addbeh.2016.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCance-Katz EF, Sullivan L, Nallani S. Drug interactions of clinical important among the opioids, Methadone and Buprenorphine, and other frequently prescribed medications: A review. Am J Addict. 2010;19:4–16. doi: 10.1111/j.1521-0391.2009.00005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. International Classification of Diseases, tenth revision, clinical modification (ICD-10-CM), 2017 update. NCHS; 2017. Jan 23, https://www.cdc.gov/nchs/icd/icd10cm.htm. [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Supporting data document on national overdose deaths from prescription and illicit drugs. NIDA, U.S Department of Health and Human Services; 2017. [Accessed: January 17, 2017]. Overdose death rates. www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. [Google Scholar]
- Oliver P, Forrest R, Keen J. Research Briefing: 31. National Treatment Agency for Substance Misuse; London, UK: 2007. Benzodiazepines and cocaine as risk factors in fatal opioid overdoses. http://www.nta.nhs.uk/uploads/nta_rb31_benzos_cocaine_in_fatal_opioid_overdose.pdf. [Google Scholar]
- Pain and Policy Studies Group/WHO Collaborating Center. [Accessed: February 26, 2016];United States of America - Opioid consumption in morphine equivalence (ME) 2016 www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/country_files/morphine_equivalence/unitedstatesofamerica_me_methadone.pdf.
- Paone D, Tuazon E, Nolan M, Mantha S. Unintentional drug poisoning (overdose) deaths involving heroin and/or fentanyl in New York City, 2000–2015. Department of Health and Mental Hygiene: Epi Data Brief. 2016;74:1–3. [Google Scholar]
- Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert AS. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ. 2015:350. doi: 10.1136/bmj.h2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ. Prescription drug overdoses: A review. J Safety Res. 2012;43:283–9. doi: 10.1016/j.jsr.2012.08.009. [DOI] [PubMed] [Google Scholar]
- Peterson AB, Gladden M, Delcher C, Spies E, Garcia-Williams A, Wang Y, Halpin J, Zibbell J, McCarty CL, DeFiore-Hyrmer J, DiOrio M, Goldberger BA. Increases in fentanyl-related overdose deaths - Florida and Ohio, 2013–2015. MMWR Morb Mortal Wkly Rep. 2016;65:844–49. doi: 10.15585/mmwr.mm6533a3. http://dx.doi.org/10.15585/mmwr.mm6533a3. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden M. Increases in drug and opioid overdose deaths – United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016b;64:1378–82. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths – United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016a;65:1445–52. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- Saunders KW, Von Korff M, Campbell CI, Banta-Green CJ, Sullivan MD, Merrill JO, Weisner C. Concurrent use of alcohol and sedatives among persons prescribed chronic opioid therapy: Prevalence and risk factors. J Pain. 2012;13:266–75. doi: 10.1016/j.jpain.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shei A, Hirst M, Kirson NY, Enloe CJ, Birnbaum HG, Dunlop WCN. Estimating the health care burden of prescription opioid abuse in five European countries. Clin Econ Outcomes Res. 2015;15:477–88. doi: 10.2147/CEOR.S85213. http://dx.doi.org/10.2147/CEOR.S85213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S, O’Brien DB, Creppage K, Dao D, Fondario A, Haile E, Hume B, Largo TW, Nguyen C, Sabel JC, Wright D. Drug overdose deaths: Let’s get specific. Pub Health Rep. 2015;130:339–42. doi: 10.1177/003335491513000411. http://dx.doi.org/10.1177/003335491513000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health (NSDUH - 2015) Center for Behavioral Health Statistics and Quality, CBHSQ; Rockville, MD: 2016. https://www.datafiles.samhsa.gov/study/national-survey-drug-use-and-health-nsduh-2015-nid16893. [Google Scholar]
- Suzuki J, El-Haddad S. A review: Fentanyl and non-pharmaceutical fentanyls. Drug Alcohol Depend. 2017;171:107–16. doi: 10.1016/j.drugalcdep.2016.11.033. [DOI] [PubMed] [Google Scholar]
- The White House. Fact Sheet: Obama administration announces additional actions to address the prescription opioid abuse and heroin epidemic. Office of the Press Secretary; Washington, DC: 2016. Mar 29, [Accessed: March 31, 2016]. https://www.whitehouse.gov/the-press-office/2016/03/29/fact-sheet-obama-administration-announces-additional-actions-address. [Google Scholar]
- Tomassoni AJ, Hawk KF, Jubanyik K, Nogee DP, Durant T, Lynch KL, Patel R, Dinh D, Ulrich A, D’Onofrio G. Multiple fentanyl overdoses - New Haven, Connecticut, June 23, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:107–11. doi: 10.15585/mm6604a4. http://dx.doi.org/10.15585/mm6604a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad JP, Warner M, Bastian BA, Miniño AM, Hedegaard H. Using literal text from the death certificate to enhance mortality statistics: characterizing drug involvement in deaths. National Vital Statistics Reports; National Center for Health Statistics (NCHS); Hyattsville, MD: 2016. p. 65. [PubMed] [Google Scholar]
- United Nations. 2006 world drug report. United Nations Office on Drugs and Crime; Vienna, Austria: [Google Scholar]
- Volkow ND. Senate Caucus on International Narcotics Control hearing America’s Addiction to Opioids: Heroin and Prescription Drug Abuse. Washington, D.C Senate: 2014. [Accessed: October 30, 2016]. America’s addiction to opioids: heroin and prescription drug abuse. https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse. [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies – tackling the opioid-overdose epidemic. N Engl J Med. 2014;370:2063–6. doi: 10.1056/NEJMp1402780. http://www.dx.doi.org/10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Warner M, Chen LH, Makuc DM. NCHS Data Brief. National Center for Health Statistics (NCHS); Hyattsville, MD: 2009. Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006; p. 22. [PubMed] [Google Scholar]
- Warner M, Trinidad JP, Bastian BA, Miniño AM, Hedegaard H. National Vital Statistics Reports. National Center for Health Statistics (NCHS); Hyattsville, MD: 2016. Drugs most frequently involved in drug overdose deaths: United States, 2010–2014; p. 65. [PubMed] [Google Scholar]
- White JM, Irvine RJ. Mechanisms of fatal opioid overdose. Addiction. 1999;94:961–72. http://dx.doi.org/10.1046/j.1360-0443.1999.9479612.x. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.