Abstract
Purpose
To provide an overview of rehabilitation medicine– and physical modality–based approaches to cancer pain management, and to highlight the fact that these approaches are generally used in conjunction and that a majority are focused on minimizing pain during periods of mobility and the performance of activities of daily living.
Methods
We performed a nonsystematic literature review and provide a description of the current standard of care.
Results
Rehabilitative and physical modalities used to manage pain can be grouped into four categories: those that modulate nociception, stabilize or unload painful structures, influence physiological processes that indirectly influence nociception, or alleviate pain arising from the overloading of muscles and connective tissues that often occurs after surgery or with sarcopenia in late-stage cancer. Most modalities have been pragmatically refined over the years, and many have an evidence base, although few have been explicitly validated in the oncologic setting. With few exceptions, they are patient controlled and free of adverse effects.
Conclusion
Physical modalities and rehabilitation medicine offer a range of pain management approaches that may serve as beneficial adjuncts to the conventional systemic and interventional analgesic strategies used to control cancer-related pain. These approaches may be particularly beneficial to patients with movement-associated pain and those who are ambivalent regarding pharmacoanalgesia.
INTRODUCTION
Pain is a frequent aspect of cancer, for which treatment is often less effective and associated with more adverse effects than we would like. All pain is limiting, but bone pain is particularly problematic in that it is aggravated by movement and therefore has profound effects on an individual's mobility and independence.
Rehabilitation medicine, with its focus on optimizing function despite a patient's symptom burden or impairments, involves strategies that may be beneficial in pain of all types, but they are disproportionately targeted toward pain associated with movement. These approaches are often used in combination and, in almost all cases, serve as adjuncts to, rather than replacements for, conventional analgesic care. Most have been pragmatically refined over the years, and many have an evidence base. Although many have not been explicitly validated in the oncologic setting, common sense and extensive experience argue persuasively for their clinical effectiveness. In addition, with few exceptions, they are patient controlled and largely free of adverse effects.
Physical modalities used to manage pain can be grouped into four categories: those that modulate nociception, stabilize or unload painful structures, influence physiological processes that indirectly influence nociception, or alleviate pain arising from the overloading of muscles and connective tissues that often occurs after surgery or with sarcopenia in late-stage cancer. Table 1 lists the findings of systematic reviews since 2005 for the modalities discussed in this article, with ratings of evidence described according to GRADE1 and/or Cochrane levels of evidence, depending on the approach used. The evidence for specific body parts is listed separately, because systematic reviews seldom conflate findings from different anatomic regions. It will be noted that many modalities are used in conjunction and that a majority are focused on minimizing pain during periods of mobility and the performance of activities of daily living.
Table 1.
SRs and MAs Since 2005 of Rehabilitation and Physical Modalities Used to Manage Pain, Described in Terms of Grade and Cochrane Level of Evidence
| Condition | Grade | Cochrane | No. of SRs or MAs | Date of Most Recent Report | Evidence in Cancer | Authors |
|---|---|---|---|---|---|---|
|
Modulation of Nociception |
||||||
| Topical heat | No | |||||
| LBP | SE | 1 | 2006 | French et al1 | ||
| Shortwave diathermy | No | |||||
| LBP | Very low | 1 | 2007 | Chou and Huffman2 | ||
| Ultrasound | No | |||||
| LBP | Very low | IE | 3 | 2011 | Chou and Huffman,2 Seco et al,3 Poitras and Brosseau4 | |
| Shoulder | Low | 1 | 2010 | Alexander et al5 | ||
| Cold | No | |||||
| LBP | Very low | 1 | 2006 | French et al1 | ||
| Knee pain | Very low | 1 | 2011 | Lake and Wofford6 | ||
| Transcutaneous nerve stimulation | Robb et al7* | |||||
| LBP | Low | IE | 3 | 2009 | Poitras and Brosseau,4 Machado et al,8 Khadilkar et al9 | |
| Knee | Moderate | IE | 2 | 2009 | Rutjes et al10 | |
| Acute nociceptive pain | Moderate | IE | 2 | 2014 | Simpson et al,11 Walsh et al12 | |
| Neck | IE | 1 | 2013 | Kroeling et al13 | ||
| Neuropathic pain | Moderate | 3 | 2010 | Jin et al,14 Mulvey et al,15 Dubinsky and Miyasaki16 | ||
| Fracture | IE | 1 | 2011 | Abou-Setta et al17 | ||
| Chronic | Moderate | IE | 2 | 2008 | Johnson and Martinson,18 Nnoaham and Kumbang19 | |
| Interferential current therapy | ||||||
| Musculoskeletal | Low | 2 | 2010 | No | Poitras and Brosseau,4 Fuentes et al20 | |
|
Stabilization and Unloading of Painful Structures |
||||||
| Compensatory strategies and adaptive devices | ||||||
| Hand arthritis | High | 1 | 2010 | No | Valdes and Marik21 | |
| Orthotics | Lee et al22* | |||||
| Back | IE | 2 | 2012 | van Duijvenbode et al,23 Longo et al24 | ||
| Hand arthritis and CTS | High | SE | 2 | 2012 | Valdes and Marik,21 Page et al25 | |
| Knee | Low to moderate | IE | 4 | 2012 | Swart et al,26 Raja and Dewan,27 Brouwer et al,28 Beaudreuil et al29 | |
|
Influence on Local Physiologic Processes Affecting Nociception |
||||||
| Laser and light therapy | Bensadoun and Nair,30 Bjordal et al,31 Clarkson et al32† | |||||
| Arthritis | Moderate | SE | 3 | 2011 | Brosseau et al,33 Ye et al,34 Jamtvedt et al35 | |
| LBP | IE | 3 | 2011 | Chou and Huffman,2 van Middelkoop et al,36 Yousefi-Nooraie et al37 | ||
| Neck | Moderate to high | > 7 | 2013 | Graham et al,38 Leaver et al,39 Gross et al,40 Kadhim-Saleh et al,41 Chow and Barnsley,42 Chow et al,43 Hurwitz et al44 | ||
| Orofacial | Low | 2 | 2013 | He et al,45 Petrucci et al46 | ||
| Manual lymphatic drainage | Low | 1 | 2009 | No | Vairo et al47 | |
|
Reduction of Pain-Associated Muscle and Connective Tissue Pathology |
||||||
| Corticosteroid injections | No | |||||
| Knee | Moderate to high | SE | 3 | 2012 | Cheng et al,48 Bellamy et al,49 Hepper et al50 | |
| LBP | Moderate to high | IE | 3> 7 | 32013 | Ammendolia et al,51 Quraishi,52 Benny and Azari,53 Roberts et al,54 Buenaventura et al,55 Staal et al56,57 | |
| Shoulder | Moderate to high | 2009 | Gaujoux-Viala et al,58 Arroll and Goodyear-Smith,59 Koester et al60 | |||
| Trigger-point injections and dry needling | No | |||||
| Neck | SE | 1 | 2007 | Peloso et al61 | ||
| Nonspecific musculoskeletal | Low | 2 | 2009 | Scott et al,62 Tough et al63 | ||
| Massage | Ernst,64 Wilkinson et al,65 Bardia et al66* | |||||
| Shoulder | Low to moderate | 5 | 2013 | Koog et al,67 Kong et al,68 Ho et al,69 van den Dolder et al,70 Verhagen et al71 | ||
| Neck | Low to moderate | IE | > 7 | 2013 | Kong et al,68 Verhagen et al71 Brosseau et al,72 Patel et al,73 Bryans et al,74 Furlan et al,75 Vernon and Humphreys,76 Ezzo77 | |
| LBP | Low to moderate | IE | > 7 | 2013 | Chou and Huffman,2 van Middelkoop et al,36 Brosseau et al,72 Furlan et al,75 Bronfort et al,78 Kumar et al,79 Furlan et al80,81 | |
| Therapeutic exercise | Carvalho et al82‡ | |||||
| Hip | Moderate to high | SE | 4 | 2013 | Gill and McBurney,83 Fransen et al,84,85 Zhang et al,86 Hernández-Molina et al,87 Bartels et al88 | |
| Knee | High | > 7 | 2014 | Gill and McBurney,83 Juhl et al,89 Uthman et al,90 Tanaka et al,91 Wang et al,92 Gill SD 2013; Smith et al,93 Escalante et al94 | ||
| Shoulder | Moderate to high | > 7 | 2012 | Hanratty et al,95 Kromer et al,96 Littlewood et al,97 Brudvig et al,98 Marinko et al,99 Kuhn,100 Smidt et al101 | ||
| Neck | Moderate to high | SE | 4 | 2014 | Leaver et al,39 Hurwitz et al,44 O'Riordan et al,102 Kay et al,103 Miller et al104 | |
| LBP | Moderate to high | 6 | 2010 | Chou and Huffman,2 van Middelkoop et al,36,105 Hayden et al106–108 | ||
| Manipulation | No | |||||
| Shoulder | Low to moderate | 4 | 2011 | Brantingham et al,109 Maund et al,110 Pribicevic et al,111 McHardy et al112 | ||
| Spine (neck and low back) | Very low to moderate | IE to SE | > 7 | 2013 | Miller et al,104 Rubinstein et al,113–116 Posadzki,117 Goertz et al,118 Smith et al,119 Huisman et al,120 Vincent et al,121 Gross et al122 | |
Abbreviations: CTS, carpal tunnel syndrome; IE, insufficient evidence to recommend; LBP, low back pain; MA, meta-analysis; SE, sufficient evidence to recommend; SR, systematic review.
IE.
Moderate.
High.
Modulation of Afferent Nociceptive Activity
Rehabilitation uses two approaches to modulate the input of nociceptive signals into the CNS. The first, the use of heat and cold, which is traditionally associated with rehabilitation medicine, is being de-emphasized but still has a roll. The second, epitomized by transcutaneous electronic nerve stimulation (TENS), uses benign afferent sensory input to modulate nociceptive activity, rather than attempting to block the input of painful stimuli. This latter approach, based on the gate theory of pain of Melzack and Wall,124 has been challenged but never seriously debunked, even though the precise neural pathways and biochemical reactions continue to be studied.
Heat and Cold
Heat and cold have clear effects on a variety of physiologic processes. As such, their main use has been for the control of pain, typically focused on the musculoskeletal system, where there is support for benefit of heat and cold as adjuncts to exercise.1,2,125,126 Metabolic and enzymatic processes are remarkably temperature sensitive; changes of only a few degrees Celsius are capable of altering nerve conduction, blood flow, and collagen extensibility.127–130 Systemic temperature changes of 0.3 to 0.4°C are possible in the clinical situation. However, local effects, as might be expected, are far more pronounced.131 Ice massage, for example, can reduce knee intra-articular temperatures by as much as 6°C,132 and ultrasound and short-wave diathermy can increase deep-tissue temperatures by similar amounts.132 Although the heating agents differ, most gain their effects by inducing analgesia or hyperemia or reducing muscle tone. Research into the effectiveness of heat and cold in the clinical setting has been limited by the variety of conditions studied and the specifics of the techniques used. However, the evidenced-based consensus supports the longstanding belief of the clinician that although heat and cold in and of themselves can be beneficial, in almost all cases their benefits are larger when combined with a well-planned program of exercise and mobilization.133–135
Electrical Stimulation
Electrical stimulation is used for a variety of indications that range from functional electric stimulation, where stimulation is used to assist a patient to move an impaired limb, to analgesia and even the healing of soft tissue injuries and fractures. However, this article is restricted to its analgesic applications. A number of electromagnetic approaches to pain control have been developed and continue to be studied in the field of rehabilitation. TENS is the best studied and most widely used of these agents, and as such, it is discussed here.
TENS was introduced in the early 1960s as a noninvasive means to provide the afferent sensory stimuli posited to block nociceptive signals.136 A few successful trials led to its rapid acceptance. However, acceptance and use have not completely clarified its benefits or best means of application.
TENS units are typically small and programmable with ≥ one signal generator. Although an infinite number of stimulation parameters are possible, all choices tend to involve output currents on the order of 100 mA, pulse rates < 100 to 120 Hz, and pulse widths from 10 to a few hundred microseconds. A variety of waveform modulation patterns are used, with the goal of increasing its effectiveness and comfort.
Electrodes are often placed over the painful area; however, positioning over the superficial portions of afferent nerves and acupuncture points is often trialed as well. Two stimulation approaches are the most common. In the first (ie, low-intensity or conventional TENS), stimulation is set at approximately 40 to 80 Hz and is barely perceptible by the patient (ie, benign afferent signal of gate theory) and hence generally more comfortable. The second, which some consider a counterirritant approach, is in many ways the reverse; frequencies are relatively slow, (ie, 1 to 8 Hz), and the intensity is moderately uncomfortable and must be tolerated for 20 to 30 minutes.
Response is difficult to predict, and TENS studies range in quality from well-designed, prospective, randomized controlled trials to (particularly in its earlier days) small inadequately blinded trials. Even today, trials comparing TENS with active controls remain rare.
Many of the earlier studies focused on postoperative and early labor pain and found that TENS use resulted in benefits comparable to those of limited amounts of narcotics.135–137 Subsequent research has yielded more mixed results, with recent evidence-based clinical guidelines and systematic reviews finding little evidence that TENS can lessen neck or back pain.138–141 The situation may be somewhat more positive for knee osteoarthritis.
Cancer-related pain has thus far received only limited attention. For example, although theoretic arguments can be made that TENS is capable of improving movement- or weight-bearing–associated cancer pain, a recent Cochrane review, despite casting a wide net for acceptable studies, found that only three met its criteria for inclusion. Issues with design heterogeneity and quality were noted, and although treatment was well tolerated by participants, the authors were unable to conclude that the evidence was strong enough to support the use of TENS.142
TENS relies on repetitive trains of stimuli, which raises concern that benefits may lessen with time as a result of habituation and tachyphylaxis. Although many have tried to avoid this issue by producing waveforms of varying shape, frequency, and packet size, newer approaches using rather intense stimuli with randomly varying waveforms may avoid this issue and become more effective than TENS, particularly for neuropathic pain.143
TENS has few safety issues other than skin irritation and mild discomfort during use. Cardiac pacemakers seem relatively resistant to TENS signals, but reasonable concerns about real or apparent introduction of dysrhythmias or malfunction restrict its use in that setting. It also seems prudent to avoid treatment near the carotid sinus and epiglottis and on the abdomen or low back of pregnant women.
Why have TENS units continued to be used despite equivocal evidence of effectiveness? The reasons may help oncologists in deciding whether to consider TENS for their patients. First, TENS assessment is limited by the myriad of differing conditions and stimulation settings reported. Thus, although systematic reviews have found limited evidence of effectiveness, the old adage that “the absence of evidence of efficacy does not necessarily mean evidence of absence of efficacy” holds true, and they have been unable to state that the approach is ineffective. Second, adverse effects are minimal. Third, efficacy in both nociceptive and neuropathic pain syndromes—a mixture of which is experienced by most patients with cancer144,145—is to some extent supported by reduced patient pain ratings. Fourth, a TENS trial can be incorporated into a course of physical therapy (PT) without significantly interfering with other potentially beneficial activities (eg, therapeutic exercise). Lastly, the prolonged use of TENS by a subgroup of patients suggests that it may benefit certain individuals. In all, reasonable candidates are patients whose localized pain is inadequately controlled by conventional treatments, who experience untenable medication adverse effects, or who prefer to try nonpharmacologic approaches.
Counterstimulation and Desensitization Techniques
There are a variety of other rehabilitation techniques designed to increase benign afferent sensory drive to attenuate pain intensity. Some, such as desensitization, have this as their sole objective. Others (eg, massage and compression garments) increase afferent sensory drive in conjunction with other treatment goals, such as the control of edema or decreasing muscle tone. Desensitization techniques in which tolerance for increasingly intense stimuli (initially benign and subsequently noxious) is systematically cultivated warrant particular mention, because they are a first-line rehabilitation medicine treatment for neuropathic and complex regional pain syndromes, including chemotherapy-induced peripheral neuropathy.146
STABILIZATION AND UNLOADING STRATEGIES
Cancer is often associated with a decreased ability of the body to bear weight, move, or tolerate the forces placed on it by even routine activities. As a consequence, the limbs, spine, and muscles frequently become pain generators, particularly with movement. The most prevalent example is metastatically induced bone pain. However, even intact musculoskeletal elements can become secondarily painful as a consequence of the biomechanical changes induced by cancer and its treatment.147
Four approaches are used to reduce the forces placed on painful bony or connective tissues: displacing painful forces onto external supports, improving the load-bearing capacity of intact anatomic elements, immobilizing painful joints, and reducing the physical effort required by an activity. It should be noted that although we present activities separately for the sake of clarity, their application in clinical treatment generally involves an integrated combination of approaches.
Assistive Devices for Mobility and Performance of Activities of Daily Living
Patients with cancer rank the maintenance of independent mobility as among their most important concerns, and loss of functionality is strongly associated with depression and desire for hastened death.148,149 A wide range of devices are available to enhance the safety and autonomy of a patient's mobility. Each, even the single-point cane, has its own strengths, limitations, and fitting requirements. Although loads can be reduced by ≥ 30% with these devices,150 there are times when mechanized or electrical alternatives may be required. For example, a Hoyer lift, scooter, or wheelchair may free a patient from pain during transfers and locomotion. The need for the guidance of a physical therapist and the importance of professionally supervised trials and fitting in all but the simplest situations cannot be overstated.
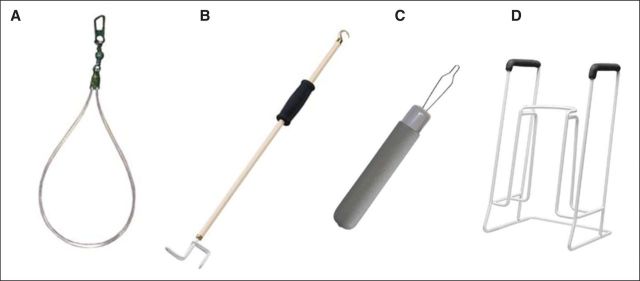
A diverse array of assistive devices can be used to protect inflamed or otherwise vulnerable structures from activities of daily living (ADL) –related forces. Figures 1A to 1D show a variety of possibilities. In contrast to assistive devices for mobility, those directed toward maintenance of ADL performance are generally designed to reduce the amount of reaching, bending, or twisting required to complete an activity. Often even a brief session with a knowledgeable occupational therapist and a few simple devices (eg, bath bench, built-up utensil) can preserve independence and reduce activity-related pain for a remarkable length of time.
Fig 1.
Assistive devices for performance of activities of daily living: (A) zipper pull, (B) dressing stick/sock aid, (C) weighted button aid, and (D) sock donner.
Compensatory Strategies
Compensatory strategies use the same principle as assistive devices, offloading the forces required to perform a painful activity. In fact, these strategies so often rely on assistive devices that it becomes almost contrived to separate them. Nonetheless, there are important distinctions, which, if appreciated, may help clinicians generate more effective and comprehensive PT and occupational therapy plans.
Our daily activities consist of orchestrated combinations of coordinated movements. Often, only a limited number of the movements required to execute an activity produce pain. By deconstructing painful activities to their constituent movements, physical and occupational therapists can isolate those that are painful and devise alternative, compensatory strategies to achieve a patient's goal. Simply helping patients recognize the movements that trigger pain frequently enables them to develop their own strategies. Activities that can be deconstructed in this manner vary widely, from getting into or out of a vehicle, to using the toilet, to putting on a bra. Engaging caregivers, using architectural supports and durable medical equipment, and altering the home environment can be combined to optimize patients' nonpainful functioning.
Therapeutic Exercise
Therapeutic exercise, often in conjunction with other modalities and designed to assist in obtaining specific goals, may be the most effective treatment in the rehabilitation armamentarium. For example, although there may be specific restrictions to the approach (eg, unstable spine), muscles are dynamic and often provide the most effective means of stabilization and immobilization. In fact, their use in this manner, often termed dynamic stabilization, has been a mainstay in sports medicine and the treatment of low back pain for years. As a result, therapeutic exercises aimed at enhancing the strength and stamina of the core musculature and muscles capable of splinting a painful body part can be remarkably effective adjuncts to conventional analgesia. Furthermore, consideration of the translation of these techniques into the realm of cancer rehabilitation seems warranted, given the promising results of unloading painful areas and mobilizing patients with metastatic disease.151
Therapeutic exercises should be chosen and implemented by a therapist with the skills and time to design a program that can effectively splint or constrain the movement of pain-generating structures. For the most part, muscles should be strengthened in a fixed position through isometric contractions that avoid pain-producing positional changes. Common examples of exercises used to stabilize pain-generating bony structures include isometric strengthening of the abdominal and hip abductor muscles to unload painful vertebrae and hip joints, respectively.133
Orthotics
Orthotics are used to stabilize, unload, and protect compromised musculoskeletal structures. Orthotics that perform this function come in many forms, but typically, they either immobilize the entire affected body part or apply pressure at select points to restrict the motion of a specific joint or joints. Many are commercially available, whereas others may require custom construction. Those used with the goal of avoiding pain in cancer care are, in large part, directed at stabilizing the neck, trunk, and low back. However, orthotics for the extremities, such as molded-ankle foot orthoses and spica or hand and wrist splints, may benefit patients with distal limb pain.
Spinal braces warrant specific mention. Often their prescription is initiated and coordinated by an orthopedist or neurosurgeon when a patient's spine is deemed unstable. Molded body jackets, which require custom fabrication, are most frequently prescribed in these cases because of their superior immobilizing properties.152 Although body jackets unquestionably limit motion better than other spinal orthoses, they are costly, hot, uncomfortable, and poorly tolerated. In these cases, it may be necessary to consider a less ideal alternative, such as the semirigid braces that are often commercially available and are also capable of restricting spinal motion.153
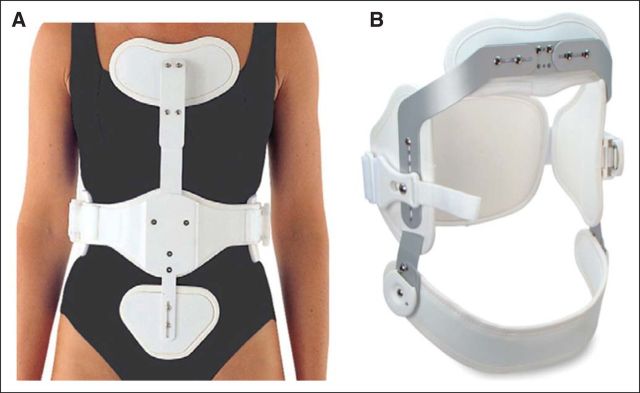
Less expensive, and more tolerable, alternatives include modular and prefabricated orthoses that encompass different segments of the spine. Thoracolumbosacral orthoses, such as the widely available CASH and Jewett braces (Figs 2A and 2B), are generally well tolerated. These three-point braces apply pressure at two points on the anterior upper and lower trunk and at a third posteriorly on the midback. A nice attribute of these off-the-shelf orthoses is that they can be tried to assess their benefits without the need for an expensive investment in either purchase or custom fabrication. It should be noted that although these braces do limit spinal flexion, they do little or nothing to constrain truncal extension. However, because the anterior vertebral column is the most common site of metastatic involvement,154 anterior support is what is needed. However, if the posterior columns of the spine are unstable, surgical consultation and a molded body jacket should be considered.
Fig 2.
Prefabricated thoracolumbosacral orthoses to limit spinal flexion: (A) CASH and (B) Jewett braces.
Lumbosacral orthoses (LSOs) control spinal motion from roughly the epigastrium to the lower lumber area. LSOs are, for the most part, variations on the abdominal corset, with rigid struts and other support. The mechanisms of their benefits, whether from unloading the spine through compression of the abdominal contents, restriction of movement, or simply the warmth they produce, remain surprisingly unclear.153 LSOs are generally well tolerated, can be easily tried with a physical therapist or orthotist without financial outlay, and are relatively inexpensive. A number of LSOs have a drawstring or one-handed cinching mechanism to facilitate easy donning, removal, and adjustment.
Cervical orthoses also offer a continuum of support, ranging from the fixed immobilization of a halo brace to the essentially tactile feedback and limited support of a soft cervical collar.155 Between the two extremes are a range of prefabricated options, including the Miami J, Philadelphia, and sterno-occipital mandibular immobilizer braces. All provide variable amounts of movement restriction and comfort.156 If pain control, rather than stabilization, is the impetus for considering a cervical orthotic, a trial of the differing options as well as a soft collar is warranted, because patient preferences and degree of benefit are difficult to predict.
Coordinating an orthotic trial is generally straightforward and within the practice scope of most physical and occupational therapists. Patients can also be sent directly to an orthotist, but this may require prior determination of which brace will be dispensed. Many medical centers have established alliances with orthotic suppliers. However, it should be remembered that (as is true for much durable medical equipment) payers may restrict provider choice, and coverage should be explored before initiating an assessment or fitting.
Positioning
The strategic use of pillows, bolsters, hospital beds, and adaptive equipment to support patients and constrain them to a pain-free range of motion is so common sense that it almost does not warrant mention. However, these effective approaches receive little attention in the formal guidance given to both professional and lay caregivers. For patients with severe weakness and motor deficits, stabilizing at-rest positions can not only reduce pain but also protect vulnerable skin over bony prominences. Like orthotics, pillows and bolsters can be used to reduce the forces placed on compromised muscles and tissue. For example, use of pillows and arm rests to support the arms of patients with head and neck disease with weakened cervical and shoulder stability after neck dissections can radically reduce pain and discomfort in the residual musculature. Figures 3A to 3D illustrate a range of widely available and inexpensive positioning aids.
Fig 3.
Positioning aids: (A) bed bolster, (B) armrest bolster, (C) contracture cushion, and (D) positioning wedge.
MODALITIES WITH PHYSIOLOGIC EFFECTS THAT INDIRECTLY INFLUENCE NOCICEPTION
Light and Laser Therapies
Low-power lasers were first used in the mid 1960s, and early reports of benefits, albeit often anecdotal, were enthusiastic and rapidly led to the application of lasers to a wide variety soft tissue injuries and conditions. With time, lasers have for the most part been replaced with a variety of nonlaser monochromatic and often infrared light sources. However, treatment parameters have remained relatively stable and typically involve the use of 30- to ≥ 150-mW devices and energy intensities of a few joules per square centimeter. As such, tissue temperatures are not elevated more than a few tenths of 1°C, and the theoretic support for effectiveness lies in the fact that irradiation at these wavelengths and intensities is known to alter a variety of cellular and metabolic processes. Light therapy was accepted by the US Food and Drug Administration via a 510K process for use primarily as an adjunct to the treatment of pain roughly 10 years ago.
As is true for many modalities, the clinical benefits of light and laser therapies remain difficult to quantitate. A large number of clinical trials have evaluated the efficaciousness of laser therapy over the years, with mixed results. Although many results are quite encouraging, systematic assessment has been limited, with recent evidence-based reviews on nonspecific low back pain and venous stasis ulcers unable to support benefit.37,157 However, the situation seems somewhat better for patients with rheumatoid arthritis, shoulder pain,134 or cancer receiving treatment for oral mucositis,32,158 although even here, the need has been voiced for additional trials to ensure an adequate evaluation.
In summary, evidence for the benefits of light therapy remains mixed, although there is some level of support above that of an individual study. Treatment is associated with minimal adverse effects, and a recent review of the literature revealed not only acceptance for use in cancer treatment–related conditions, such as mucositis,32,159 but also no evidence of an increase in the frequency of cancer recurrence or metastatic disease.160
Manual Lymphatic Drainage
Manual lymphatic drainage, lymphatic massage, or Vodder-type massage is a highly specialized technique designed to reduce edema. Gentle and rhythmic movements are used to stimulate the contraction of lymphatic vessel smooth muscles, decongest tissues, and reduce inflammation through an enhanced removal of potentially inflammatory macromolecules.161 Massage is limited to finger or hand pressures of approximately 30 to 45 mmHg, with treatments initiated proximal to lymphostatic regions and gradually progressing distally.
The analgesic properties of manual lymphatic drainage have been well recognized through its extensive use in the management of lymphedema, with the consequence that it is increasingly being applied in pain syndromes in which lymph congestion is thought to play a role.162,163 Treatment tends to be well tolerated, even among patients with moderate to severe allodynia. Benefits depend on the skill of the practitioner, and the recommendation of a knowledgeable person or use of a registry, such as the Lymphology Association of North America164 and the Vodder School,165 is highly recommended.
REHABILITATION APPROACHES TO MANAGING MUSCULOSKELETAL PAIN
Cancer-related musculoskeletal pain arises from four principal mechanisms: direct tumor invasion, maladaptive changes induced by cancer treatment or local tumor effects, exacerbation of pre-existing musculoskeletal pain, and hypertonicity and spasm related to any of the above. Although to our knowledge it never seems to have been subjected to epidemiologic study, the third mechanism (ie, exacerbation of pre-existing pain) seems surprisingly common across all cancer populations. Common approaches to the treatment of musculoskeletal pain are outlined here, with several often integrated in a unified treatment plan. Pain arising from tumor invasion is far more likely to definitively respond to treatment with antineoplastic therapies; however, even here, rehabilitation medicine approaches may be attempted once tumor control has been optimized.
Principles of Rest, Ice Compression, and Elevation
The roles of heat and cold were reviewed to some extent earlier in this article. However, the principles of rest, ice compression, and elevation (PRICE), although simple, continue to be widely used despite some concern about the effectiveness of cold in controlling pain and acute inflammation.166 Musculoskeletal pain of abrupt onset or with a clear precipitant (eg, overuse or trauma) warrants a trial, with or without nonsteroidal anti-inflammatory drugs, of as many PRICE components as possible.
Deep-Heat Modalities
Although cold is generally administered topically, with ice packs or massage, heating modalities that target deeper tissues (eg, muscles and joints) are commonly used as adjuncts in PT practice. Ultrasound, in particular, continues to be a mainstay for enhancing tissue elasticity before range-of-motion activities and fibrous-release techniques. Systematic reviews and meta-analyses have established the efficacy of ultrasound in a range of benign pain states.167
Injections
Injections share the common goal of delivering an analgesic or anti-inflammatory agent at high concentration to a localized pain generator to maximize therapeutic effect while minimizing systemic toxicity. An impressive array of pharmaceuticals are injected, but steroids, local anesthetics, and, more recently, botulinum toxin are the most common. Ultrasound guidance is increasingly used to optimize localization; however, the benefits of this approach, particularly with more mobile lipophilic injectates, have not been clearly established.168 Inflamed tendons, bursae, and synovium are the most common targets.
When the long-term benefits of steroid injections have been scrutinized, they have seemed less effective than PT alone, although benefits are slower to accrue with PT.169,170 To date, some of the most definitive work has been done in lateral epicondylitis or tennis elbow. There seems to be a rebound effect after the near-term anti-inflammatory benefits of the injection, with eventual worsening.171 This is relevant to patients with cancer, because their prognoses and involvement with cancer treatments vary radically. For a disease-free survivor with a good prognosis, PT in conjunction with or independent of an injection may offer greater collective benefit than an injection alone. In contrast, patients with far advanced cancer need near-term relief and may not survive to experience the more delayed and sustained benefits offered by PT. The role of botulinum toxin in treating mucloskeletal pain sources, such as myofascial pain, given its newer introduction, remains unclear but intriguing.172
Injections are relatively safe and toxicity free. Patients should not receive > three intra-articular injections per year. Most physiatrists, orthopedists, and rheumatologists, as well as many primary care practitioners, perform these procedures. However, for more specialized injections (eg, involving smaller structures of the hand), the involvement of specialists who frequently target these joints is recommended.
Myofascial Release Techniques and Trigger Points
Myofascial pain is a syndrome that affects millions of people and is most commonly located in upper back musculature.173,174 Its most salient findings include tenderness on palpation and the presence of taut bands of increased muscle tone and trigger points (ie, small areas of increased tenderness that when pressed generated stereotypical patterns of referred pain). Although the nature and cause of the syndrome remain controversial, its effects on patients can be large. Massage, exercise, and trigger-point or botulinum injections are the mainstays of treatment.
Massage, often accompanied with heat, muscle tension–release techniques, and relaxation exercises, is frequently employed. Like most approaches to myofascial pain, multiple treatment sessions are required for sustained benefit. Trigger-point injections and dry needling mechanically stimulate the discreet taut bands that are the hallmark of myofascial pain. Controversy persists as to the benefits of introducing an injectate (eg, local anesthetic, botulinum toxin,172 or steroid) versus simply penetrating taut bands with a needle. No direct comparisons offer an empiric basis to choose one over the other. However, because positive benefits have been reported for approaches using narrow-gauge (eg, > 30) needles that inflect less trauma and discomfort, these approaches may be preferred for initial needling trials.
As we have discussed, therapeutic exercise, alone or combined with other approaches, plays a critical role in normalizing the derangements that predispose patients to develop musculoskeletal pain in general. Overuse is the most common source of myofascial pain among patients with cancer and occurs when muscles, for whatever reason, must work harder or differently than they customarily do. It may not be possible to reverse the precipitating cancer-associated injuries that created the symptoms. However, the severity and chronicity of the resultant pain can generally be improved through therapeutic exercise. Evaluation by a physician or therapist familiar with cancer treatment–related changes, as well as comprehensive myofascial pain management, offers the best chance of developing an appropriate and individualized exercise program targeting all implicated muscle groups.
Massage and Body Work
Definitive research on massage as a pain-relieving modality has been hampered, similar to other modalities, by the heterogeneity of types and treatment schedules. As a stand-alone treatment, massage provides immediate or short-term pain relief for mechanical neck and low back pain.73,79 Accupuncture-like, structural, and relaxation massages may offer greater or more sustained benefit, although the evidence base is limited.80,175 Massage in isolation does not seem to yield sustained benefit and should be incorporated into an integrated program of exercise.36 A similar limitation of benefit to the near term has characterized trials evaluating massage for cancer pain.176
Therapeutic Exercise
In addition to its role in optimizing control of myofascial pain and enhancing the stabilization of painful body areas, it cannot be overemphasized that therapeutic exercise is the cornerstone of all rehabilitative approaches to pain arising from muscles, tendons, and ligaments. The structured application of specific demands to muscle and connective tissues reliably elicits desirable physiologic changes. Such demands may be resistive, aerobic, or tensile, depending on the desired alterations in muscle anatomy and physiology.
DISCUSSION
Physical modalities and rehabilitation medicine offer a range of pain management approaches that may serve as beneficial adjuncts to the conventional systemic and interventional analgesic strategies used to control cancer-related pain. These approaches may be particularly beneficial to patients with movement-associated pain and those who are ambivalent regarding pharmacoanalgesia.
Footnotes
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: Jeffrey R. Basford
Data analysis and interpretation: Jeffrey R. Basford
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.French SD Cameron M Walker BF, etal: A Cochrane review of superficial heat or cold for low back pain Spine Phila Pa 1976 31:998–1006,2006 [DOI] [PubMed] [Google Scholar]
- 2.Chou R, Huffman LH: Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline Ann Intern Med 147:492–504,2007 [DOI] [PubMed] [Google Scholar]
- 3.Seco J, Kovacs FM, Urrutia G: The efficacy, safety, effectiveness, and cost-effectiveness of ultrasound and shock wave therapies for low back pain: A systematic review Spine J 11:966–977,2011 [DOI] [PubMed] [Google Scholar]
- 4.Poitras S, Brosseau L: Evidence-informed management of chronic low back pain with transcutaneous electrical nerve stimulation, interferential current, electrical muscle stimulation, ultrasound, and thermotherapy Spine J 8:226–233,2008 [DOI] [PubMed] [Google Scholar]
- 5.Alexander LD Gilman DR Brown DR, etal: Exposure to low amounts of ultrasound does not improve soft tissue shoulder pathology: A systematic review Phys Ther 90:14–25,2010 [DOI] [PubMed] [Google Scholar]
- 6.Lake DA, Wofford NH: Effect of therapeutic modalities on patients with patellofemoral pain syndrome: A systematic review Sports Health 3:182–189,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robb K Oxberry SG Bennett MI, etal: A Cochrane systematic review of transcutaneous electrical nerve stimulation for cancer pain J Pain Symptom Manage 37:746–753,2009 [DOI] [PubMed] [Google Scholar]
- 8.Machado LA Kamper SJ Herbert RD, etal: Analgesic effects of treatments for non-specific low back pain: A meta-analysis of placebo-controlled randomized trials Rheumatology (Oxford) 48:520–527,2009 [DOI] [PubMed] [Google Scholar]
- 9.Khadilkar A Odebiyi DO Brosseau L, etal: Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain Cochrane Database Syst Rev 4:CD003008,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rutjes AW Nüesch E Sterchi R, etal: Transcutaneous electrostimulation for osteoarthritis of the knee Cochrane Database Syst Rev 4:CD002823,2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simpson PM Fouche PF Thomas RE, etal: Transcutaneous electrical nerve stimulation for relieving acute pain in the prehospital setting: a systematic review and meta-analysis of randomized-controlled trials Eur J Emerg Med 21:10–17,2014 [DOI] [PubMed] [Google Scholar]
- 12.Walsh DM Howe TE Johnson MI, etal: Transcutaneous electrical nerve stimulation for acute pain Cochrane Database Syst Rev 2:CD006142,2009 [DOI] [PubMed] [Google Scholar]
- 13.Kroeling P Gross A Graham N, etal: Electrotherapy for neck pain Cochrane Database Syst Rev 8:CD004251,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jin DM Xu Y Geng DF, etal: Effect of transcutaneous electrical nerve stimulation on symptomatic diabetic peripheral neuropathy: a meta-analysis of randomized controlled trials Diabetes Res Clin Pract 89:10–15,2010 [DOI] [PubMed] [Google Scholar]
- 15.Mulvey MR Bagnall AM Johnson MI, etal: Transcutaneous electrical nerve stimulation (TENS) for phantom pain and stump pain following amputation in adults Cochrane Database Syst Rev 5:CD007264,2010 [DOI] [PubMed] [Google Scholar]
- 16.Dubinsky RM, Miyasaki J: Assessment: efficacy of transcutaneous electric nerve stimulation in the treatment of pain in neurologic disorders (an evidence-based review): Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology Neurology 74:173–176,2010 [DOI] [PubMed] [Google Scholar]
- 17.Abou-Setta AM Beaupre LA Rashiq S, etal: Comparative effectiveness of pain management interventions for hip fracture: A systematic review Ann Intern Med 155:234–245,2011 [DOI] [PubMed] [Google Scholar]
- 18.Johnson M, Martinson M: Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: A meta-analysis of randomized controlled trials Pain 130:157–165,2007 [DOI] [PubMed] [Google Scholar]
- 19.Nnoaham KE, Kumbang J: Transcutaneous electrical nerve stimulation (TENS) for chronic pain Cochrane Database Syst Rev 3:CD003222,2008 [DOI] [PubMed] [Google Scholar]
- 20.Fuentes JP Armijo Olivo S Magee DJ, etal: Effectiveness of interferential current therapy in the management of musculoskeletal pain: A systematic review and meta-analysis Phys Ther 90:1219–1238,2010 [DOI] [PubMed] [Google Scholar]
- 21.Valdes K, Marik T: A systematic review of conservative interventions for osteoarthritis of the hand J Hand Ther 23:334–350,2010 [DOI] [PubMed] [Google Scholar]
- 22.Lee SH Cox KM Grant R, etal: Patient positioning (mobilisation) and bracing for pain relief and spinal stability in metastatic spinal cord compression in adults Cochrane Database Syst Rev 3:CD007609,2012 [DOI] [PubMed] [Google Scholar]
- 23.van Duijvenbode IC Jellema P van Poppel MN, etal: Lumbar supports for prevention and treatment of low back pain Cochrane Database Syst Rev 2:CD001823,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Longo UG Loppini M Denaro L, etal: Conservative management of patients with an osteoporotic vertebral fracture: A review of the literature J Bone Joint Surg Br 94:152–157,2012 [DOI] [PubMed] [Google Scholar]
- 25.Page MJ Massy-Westropp N O'Connor D, etal: Splinting for carpal tunnel syndrome Cochrane Database Syst Rev 7:CD010003,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swart NM van Linschoten R Bierma-Zeinstra SM, etal: The additional effect of orthotic devices on exercise therapy for patients with patellofemoral pain syndrome: A systematic review Br J Sports Med 46:570–577,2012 [DOI] [PubMed] [Google Scholar]
- 27.Raja K, Dewan N: Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: A systematic review Am J Phys Med Rehabil 90:247–262,2011 [DOI] [PubMed] [Google Scholar]
- 28.Brouwer RW Jakma TS Verhagen AP, etal: Braces and orthoses for treating osteoarthritis of the knee Cochrane Database Syst Rev 1:CD004020,2005 [DOI] [PubMed] [Google Scholar]
- 29.Beaudreuil J Bendaya S Foucher M, etal: Clinical practice guidelines for rest orthosis, knee sleeves, and unloading knee braces in knee osteoarthritis Joint Bone Spine 76:629–636,2009 [DOI] [PubMed] [Google Scholar]
- 30.Bensadoun RJ, Nair RG: Low-level laser therapy in the prevention and treatment of cancer therapy-induced mucositis: 2012 state of the art based on literature review and meta-analysis Curr Opin Oncol 24:363–370,2012 [DOI] [PubMed] [Google Scholar]
- 31.Bjordal JM Bensadoun RJ Tunèr J, etal: A systematic review with meta-analysis of the effect of low-level laser therapy (LLLT) in cancer therapy-induced oral mucositis Support Care Cancer 19:1069–1077,2011 [DOI] [PubMed] [Google Scholar]
- 32.Clarkson JE Worthington HV Furness S, etal: Interventions for treating oral mucositis for patients with cancer receiving treatment Cochrane Database Syst Rev 8:CD001973,2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brosseau L Robinson V Wells G, etal: Low level laser therapy (classes I, II and III) for treating rheumatoid arthritis Cochrane Database Syst Rev 4:CD002049,2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ye L Kalichman L Spittle A, etal: Effects of rehabilitative interventions on pain, function and physical impairments in people with hand osteoarthritis: A systematic review Arthritis Res Ther 13:R28,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jamtvedt G Dahm KT Christie A, etal: Physical therapy interventions for patients with osteoarthritis of the knee: An overview of systematic reviews Phys Ther 88:123–136,2008 [DOI] [PubMed] [Google Scholar]
- 36.van Middelkoop M Rubinstein SM Kuijpers T, etal: A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain Eur Spine J 20:19–39,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yousefi-Nooraie R Schonstein E Heidari K, etal: Low level laser therapy for nonspecific low-back pain Cochrane Database Syst Rev 16:CD005107,2008 [DOI] [PubMed] [Google Scholar]
- 38.Graham N Gross AR Carlesso LC, etal: An ICON overview on physical modalities for neck pain and associated disorders Open Orthop J 7:440–460,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leaver AM Refshauge KM Maher CG, etal: Conservative interventions provide short-term relief for non-specific neck pain: a systematic review J Physiother 56:73–85,2010 [DOI] [PubMed] [Google Scholar]
- 40.Gross AR Dziengo S Boers O, etal: Low level laser therapy (LLLT) for neck pain: A systematic review and meta-regression Open Orthop J 7:396–419,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kadhim-Saleh Maganti H Ghert M, etal: Is low-level laser therapy in relieving neck pain effective? Systematic review and meta-analysis Rheumatol Int 33:2493–2501,2013 [DOI] [PubMed] [Google Scholar]
- 42.Chow RT, Barnsley L: Systematic review of the literature of low-level laser therapy (LLLT) in the management of neck pain Lasers Surg Med 37:46–52,2005 [DOI] [PubMed] [Google Scholar]
- 43.Chow RT Johnson MI Lopes-Martins RA, etal: Efficacy of low-level laser therapy in the management of neck pain: A systematic review and meta-analysis of randomised placebo or active-treatment controlled trials Lancet 374:1897–1908,2009 [DOI] [PubMed] [Google Scholar]
- 44.Hurwitz EL Carragee EJ van der Veide G, etal: Treatment of neck pain: Noninvasive interventions—Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders J Manipulative Physiol Ther 32:S141–S175,2009suppl 2 [DOI] [PubMed] [Google Scholar]
- 45.He WL Li CJ Liu ZP, etal: Efficacy of low-level laser therapy in the management of orthodontic pain: A systematic review and meta-analysis Lasers Med Sci 28:1581–1589,2013 [DOI] [PubMed] [Google Scholar]
- 46.Petrucci A Sgolastra F Gatto R, etal: Effectiveness of low-level laser therapy in temporomandibular disorders: A systematic review and meta-analysis J Orofac Pain 25:298–307,2011 [PubMed] [Google Scholar]
- 47.Vairo GL Miller SJ McBrier NM, etal: Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: An evidence-based practice approach J Man Manip Ther 17:e80–e89,2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cheng OT Souzdalnitski D Vrooman B, etal: Evidence-based knee injections for the management of arthritis Pain Med 13:740–753,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bellamy N Campbell J Robinson V, etal: Intraarticular corticosteroid for treatment of osteoarthritis of the knee Cochrane Database Syst Rev 2:CD005328,2006 [DOI] [PubMed] [Google Scholar]
- 50.Hepper CT Halvorson JJ Duncan ST, etal: The efficacy and duration of intra-articular corticosteroid injection for knee osteoarthritis: A systematic review of level I studies J Am Acad Orthop Surg 17:638–646,2009 [DOI] [PubMed] [Google Scholar]
- 51.Ammendolia C Stuber KJ Rok E, etal: Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication Cochrane Database Syst Rev 8:CD010712,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Quraishi NA: Transforaminal injection of corticosteroids for lumbar radiculopathy: Systematic review and meta-analysis Eur Spine J 21:214–219,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Benny B, Azari P: The efficacy of lumbosacral transforaminal epidural steroid injections: A comprehensive literature review J Back Musculoskelet Rehabil 24:67–76,2011 [DOI] [PubMed] [Google Scholar]
- 54.Roberts ST Willick SE Rho ME, etal: Efficacy of lumbosacral transforaminal epidural steroid injections: A systematic review PM R 1:657–668,2009 [DOI] [PubMed] [Google Scholar]
- 55.Buenaventura RM Datta S Abdi S, etal: Systematic review of therapeutic lumbar transforaminal epidural steroid injections Pain Physician 12:233–251,2009 [PubMed] [Google Scholar]
- 56.Staal JB de Bie RA de Vet HC, etal: Injection therapy for subacute and chronic low back pain: An updated Cochrane review Spine 34:49–59,2009 [DOI] [PubMed] [Google Scholar]
- 57.Staal JB de Bie R de Vet HC, etal: Injection therapy for subacute and chronic low-back pain Cochrane Database Syst Rev 3:CD001824,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gaujoux-Viala C, Dougados M, Gossec L: Efficacy and safety of steroid injections for shoulder and elbow tendonitis: A meta-analysis of randomised controlled trials Ann Rheum Dis 68:1843–1849,2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arroll B, Goodyear-Smith F: Corticosteroid injections for painful shoulder: A meta-analysis Br J Gen Pract 55:224–228,2005 [PMC free article] [PubMed] [Google Scholar]
- 60.Koester MC Dunn WR Kuhn JE, etal: The efficacy of subacromial corticosteroid injection in the treatment of rotator cuff disease: A systematic review J Am Acad Orthop Surg 15:3–11,2007 [DOI] [PubMed] [Google Scholar]
- 61.Peloso P Gross A Haines T, etal: Medicinal and injection therapies for mechanical neck disorders Cochrane Database Syst Rev 3:CD000319,2007 [DOI] [PubMed] [Google Scholar]
- 62.Scott NA Guo B Barton PM, etal: Trigger point injections for chronic non-malignant musculoskeletal pain: A systematic review Pain Med 10:54–69,2009 [DOI] [PubMed] [Google Scholar]
- 63.Tough EA White AR Cummings TM, etal: Acupuncture and dry needling in the management of myofascial trigger point pain: A systematic review and meta-analysis of randomised controlled trials Eur J Pain 13:3–10,2009 [DOI] [PubMed] [Google Scholar]
- 64.Ernst E: Massage therapy for cancer palliation and supportive care: A systematic review of randomised clinical trials Support Care Cancer 17:333–337,2009 [DOI] [PubMed] [Google Scholar]
- 65.Wilkinson S, Barnes K, Storey L: Massage for symptom relief in patients with cancer: Systematic review J Adv Nurs 63:430–439,2008 [DOI] [PubMed] [Google Scholar]
- 66.Bardia A Barton DL Prokop LJ, etal: Efficacy of complementary and alternative medicine therapies in relieving cancer pain: A systematic review J Clin Oncol 24:5457–5464,2006 [DOI] [PubMed] [Google Scholar]
- 67.Koog YH Jin SS Yoon K, etal: Interventions for hemiplegic shoulder pain: Systematic review of randomised controlled trials Disabil Rehabil 32:282–291,2010 [DOI] [PubMed] [Google Scholar]
- 68.Kong LJ Zhan HS Cheng YW, etal: Massage therapy for neck and shoulder pain: A systematic review and meta-analysis Evid Based Complement Alternat Med [epub ahead of print on February 28, 2013] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ho CY, Sole G, Munn J: The effectiveness of manual therapy in the management of musculoskeletal disorders of the shoulder: A systematic review Man Ther 14:463–474,2009 [DOI] [PubMed] [Google Scholar]
- 70.van den Dolder PA, Ferreira PH, Refshauge KM: Effectiveness of soft tissue massage and exercise for the treatment of non-specific shoulder pain: A systematic review with meta-analysis Br J Sports Med [epub ahead of print on July 26, 2012] [DOI] [PubMed] [Google Scholar]
- 71.Verhagen AP Karels C Bierma-Zeinstra SM, etal: Ergonomic and physiotherapeutic interventions for treating work-related complaints of the arm, neck or shoulder in adults: A Cochrane systematic review Eura Medicophys 43:391–405,2007 [PubMed] [Google Scholar]
- 72.Brosseau L Wells GA Poitras S, etal: Ottawa Panel evidence-based clinical practice guidelines on therapeutic massage for low back pain J Bodyw Mov Ther 16:424–455,2012 [DOI] [PubMed] [Google Scholar]
- 73.Patel KC Gross A Graham N, etal: Massage for mechanical neck disorders Cochrane Database Syst Rev 9:CD004871,2012 [DOI] [PubMed] [Google Scholar]
- 74.Bryans R Decina P Descarreaux M, etal: Evidence-based guidelines for the chiropractic treatment of adults with neck pain J Manipulative Physiol Ther 37:42–63,2014 [DOI] [PubMed] [Google Scholar]
- 75.Furlan AD Yazdi F Tsertsvadze A, etal: A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain Evid Based Complement Alternat Med [epub ahead of print on November 24, 2011] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vernon H, Humphreys BK: Chronic mechanical neck pain in adults treated by manual therapy: A systematic review of change scores in randomized controlled trials of a single session J Man Manip Ther 16:E42–E52,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ezzo J Haraldsson BG Gross AR, etal: Massage for mechanical neck disorders: A systematic review Spine (Phila Pa 1976) 32:353–362,2007 [DOI] [PubMed] [Google Scholar]
- 78.Bronfort G Haas M Evans R, etal: Effectiveness of manual therapies: The UK evidence report Chiropr Osteopat 18:3,2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kumar S, Beaton K, Hughes T: The effectiveness of massage therapy for the treatment of nonspecific low back pain: A systematic review of systematic reviews Int J Gen Med 6:733–741,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Furlan AD Imamura M Dryden T, etal: Massage for low back pain: An updated systematic review within the framework of the Cochrane Back Review Group Spine (Phila Pa 1976) 34:1669–1684,2009 [DOI] [PubMed] [Google Scholar]
- 81.Furlan AD Imamura M Dryden T, etal: Massage for low-back pain Cochrane Database Syst Rev 4:CD001929,2008 [DOI] [PubMed] [Google Scholar]
- 82.Carvalho AP, Vital FM, Soares BG: Exercise interventions for shoulder dysfunction in patients treated for head and neck cancer Cochrane Database Syst Rev 4:CD008693,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gill SD, McBurney H: Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials Arch Phys Med Rehabil 94:164–176,2013 [DOI] [PubMed] [Google Scholar]
- 84.Fransen M McConnell S Hernandez-Molina G, etal: Exercise for osteoarthritis of the hip Cochrane Database Syst Rev 3:CD007912,2009 [DOI] [PubMed] [Google Scholar]
- 85.Fransen M McConnell S Hernandez-Molina G, etal: Does land-based exercise reduce pain and disability associated with hip osteoarthritis? A meta-analysis of randomized controlled trials Osteoarthritis Cartilage 18:613–620,2010 [DOI] [PubMed] [Google Scholar]
- 86.Zhang W Nuki G Moskowitz RW, etal: OARSI recommendations for the management of hip and knee osteoarthritis: Part III—Changes in evidence following systematic cumulative update of research published through January 2009 Osteoarthritis Cartilage 18:476–499,2010 [DOI] [PubMed] [Google Scholar]
- 87.Hernández-Molina G Reichenbach S Zhang B, etal: Effect of therapeutic exercise for hip osteoarthritis pain: Results of a meta-analysis Arthritis Rheum 59:1221–1228,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bartels EM Lund H Hagen KB, etal: Aquatic exercise for the treatment of knee and hip osteoarthritis Cochrane Database Syst Rev 4:CD005523,2007 [DOI] [PubMed] [Google Scholar]
- 89.Juhl C Christensen R Roos EM, etal: Impact of exercise type and dose on pain and disability in knee osteoarthritis: A systematic review and meta-regression analysis of randomized controlled trials Arthritis Rheumatol 66:622–636,2014 [DOI] [PubMed] [Google Scholar]
- 90.Uthman OA van der Windt DA Jordan JL, etal: Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis BMJ 347:f5555,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tanaka R Ozawa J Kito N, etal: Efficacy of strengthening or aerobic exercise on pain relief in people with knee osteoarthritis: A systematic review and meta-analysis of randomized controlled trials Clin Rehabil 27:1059–1071,2013 [DOI] [PubMed] [Google Scholar]
- 92.Wang SY Olson-Kellogg B Shamliyan TA, etal: Physical therapy interventions for knee pain secondary to osteoarthritis: A systematic review Ann Intern Med 157:632–644,2012 [DOI] [PubMed] [Google Scholar]
- 93.Smith TO, King JJ, Hing CB: The effectiveness of proprioceptive-based exercise for osteoarthritis of the knee: A systematic review and meta-analysis Rheumatol Int 32:3339–3351,2012 [DOI] [PubMed] [Google Scholar]
- 94.Escalante Y Saavedra JM García-Hermoso A, etal: Physical exercise and reduction of pain in adults with lower limb osteoarthritis: A systematic review J Back Musculoskelet Rehabil 23:175–186,2010 [DOI] [PubMed] [Google Scholar]
- 95.Hanratty CE McVeigh JG Kerr DP, etal: The effectiveness of physiotherapy exercises in subacromial impingement syndrome: A systematic review and meta-analysis Semin Arthritis Rheum 42:297–316,2012 [DOI] [PubMed] [Google Scholar]
- 96.Kromer TO Tautenhahn UG de Bie RA, etal: Effects of physiotherapy in patients with shoulder impingement syndrome: A systematic review of the literature J Rehabil Med 41:870–880,2009 [DOI] [PubMed] [Google Scholar]
- 97.Littlewood C Ashton J Chance-Larsen K, etal: Exercise for rotator cuff tendinopathy: A systematic review Physiotherapy 98:101–109,2012 [DOI] [PubMed] [Google Scholar]
- 98.Brudvig TJ, Kulkarni H, Shah S: The effect of therapeutic exercise and mobilization on patients with shoulder dysfuction: A systematic review with meta-analysis J Orthop Sports Phys Ther 41:734–748,2011 [DOI] [PubMed] [Google Scholar]
- 99.Marinko LN Chacko JM Dalton D, etal: The effectiveness of therapeutic exercise for painful shoulder conditions: A meta-analysis J Shoulder Elbow Surg 20:1351–1359,2011 [DOI] [PubMed] [Google Scholar]
- 100.Kuhn JE: Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol J Shoulder Elbow Surg 18:138–160,2009 [DOI] [PubMed] [Google Scholar]
- 101.Smidt N de Vet HC Bouter LM, etal: Effectiveness of exercise therapy: A best-evidence summary of systematic reviews Aust J Physiother 51:71–85,2005 [DOI] [PubMed] [Google Scholar]
- 102.O'Riordan C Clifford A Van De Ven P, etal: Chronic neck pain and exercise interventions: Frequency, intensity, time, and type principle Arch Phys Med Rehabil 95:770–783,2014 [DOI] [PubMed] [Google Scholar]
- 103.Kay TM Gross A Goldsmith C, etal: Exercises for mechanical neck disorders Cochrane Database Syst Rev 3:CD004250,2005 [DOI] [PubMed] [Google Scholar]
- 104.Miller J Gross A D'Sylva J, etal: Manual therapy and exercise for neck pain: A systematic review Man Ther 15:334–354,2010 [PubMed] [Google Scholar]
- 105.van Middelkoop M Rubinstein SM Verhagen AP, etal: Exercise therapy for chronic nonspecific low-back pain Best Pract Res Clin Rheumatol 24:193–204,2010 [DOI] [PubMed] [Google Scholar]
- 106.Hayden JA van Tulder MW Malmivaara A, etal: Exercise therapy for treatment of non-specific low back pain Cochrane Database Syst Rev 3:CD000335,2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hayden JA, van Tulder MW, Tomlinson G: Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain Ann Intern Med 142:776–785,2005 [DOI] [PubMed] [Google Scholar]
- 108.Hayden JA van Tulder MW Malmivaara AV, etal: Meta-analysis: Exercise therapy for nonspecific low back pain Ann Intern Med 142:765–775,2005 [DOI] [PubMed] [Google Scholar]
- 109.Brantingham JW Cassa TK Bonnefin D, etal: Manipulative therapy for shoulder pain and disorders: Expansion of a systematic review J Manipulative Physiol Ther 34:314–346,2011 [DOI] [PubMed] [Google Scholar]
- 110.Maund E Craig D Suekarran S, etal: Management of frozen shoulder: A systematic review and cost-effectiveness analysis Health Technol Assess 16:1–264,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pribicevic M Pollard H Bonello R, etal: A systematic review of manipulative therapy for the treatment of shoulder pain J Manipulative Physiol Ther 33:679–689,2010 [DOI] [PubMed] [Google Scholar]
- 112.McHardy A Hoskins W Pollard H, etal: Chiropractic treatment of upper extremity conditions: A systematic review J Manipulative Physiol Ther 31:146–159,2008 [DOI] [PubMed] [Google Scholar]
- 113.Rubinstein SM van Middelkoop M Kuijpers T, etal: A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain Eur Spine J 19:1213–1228,2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rubinstein SM van Middelkoop M Assendelft WJ, etal: Spinal manipulative therapy for chronic low-back pain Cochrane Database Syst Rev 2:CD008112,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rubinstein SM Terwee CB Assendelft WJ, etal: Spinal manipulative therapy for acute low-back pain Cochrane Database Syst Rev 9:CD008880,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rubinstein SM Terwee CB Assendelft WJ, etal: Spinal manipulative therapy for acute low back pain: An update of the Cochrane review Spine (Phila Pa 1976) 38:E158–E177,2013 [DOI] [PubMed] [Google Scholar]
- 117.Posadzki P: Is spinal manipulation effective for pain? An overview of systematic reviews Pain Med 13:754–761,2012 [DOI] [PubMed] [Google Scholar]
- 118.Goertz CM Pohlman KA Vining RD, etal: Patient-centered outcomes of high-velocity, low-amplitude spinal manipulation for low back pain: A systematic review J Electromyogr Kinesiol 22:670–691,2012 [DOI] [PubMed] [Google Scholar]
- 119.Smith JS, Bolton PS: What are the clinical criteria justifying spinal manipulative therapy for neck pain? A systematic review of randomized controlled trials Pain Med 14:460–468,2013 [DOI] [PubMed] [Google Scholar]
- 120.Huisman PA, Speksnijder CM, de Wijer A: The effect of thoracic spine manipulation on pain and disability in patients with non-specific neck pain: A systematic review Disabil Rehabil 35:1677–1685,2013 [DOI] [PubMed] [Google Scholar]
- 121.Vincent K Maigne JY Fischhoff C, etal: Systematic review of manual therapies for nonspecific neck pain Joint Bone Spine 80:508–515,2013 [DOI] [PubMed] [Google Scholar]
- 122.Gross A Miller J D'Sylva J, etal: Manipulation or mobilisation for neck pain Cochrane Database Syst Rev 1:CD004249,2010 [DOI] [PubMed] [Google Scholar]
- 123.Guyatt GH Oxman AD Vist GE, etal: GRADE: An emerging consensus on rating quality of evidence and strength of recommendations BMJ 336:924–926,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Melzack R, Wall PD: Pain mechanisms: A new theory Science 150:971–979,1965 [DOI] [PubMed] [Google Scholar]
- 125.Lin YH: Effects of thermal therapy in improving the passive range of knee motion: Comparison of cold and superficial heat applications Clin Rehabil 17:618–623,2003 [DOI] [PubMed] [Google Scholar]
- 126.Brosseau L Robinson V Pelland L, etal: Efficacy of thermotherapy for rheumatoid arthritis: A meta-analysis Phys Ther Rev 7:5–15,2002 [Google Scholar]
- 127.Knight KL: Cryotherapy: Theory, Technique and Physiology (ed 1) 1985Chattanooga, TN: Chattanooga Corporation [Google Scholar]
- 128.Guyton AC: Textbook of Medical Physiology (ed 7) 1986Philedelphia, PA: WB Saunders [Google Scholar]
- 129.Denys EH: AAEM minimonograph #14: The influence of temperature in clinical neurophysiology Muscle Nerve 14:795–811,1991 [DOI] [PubMed] [Google Scholar]
- 130.Lehmann JF Silverman DR Baum BR, etal: Temperature distributions in the human thigh, produced by infrared, hot pack and microwave applications Arch Phys Med Rehabil 47:291–299,1966 [PubMed] [Google Scholar]
- 131.Doering TJ Aaslid R Steuernagel B, etal: Cerebral autoregulation during whole-body hypothermia and hyperthermia Am J Phys Med Rehabil 78:33–38,1999 [DOI] [PubMed] [Google Scholar]
- 132.Oosterveld FG, Rasker JJ: Effects of local heat and cold treatment of surface and articular temperature of arthritic knees Arthritis Rheum 37:1578–1582,1994 [DOI] [PubMed] [Google Scholar]
- 133.Almeida MO Silva BN Andriolo RB, etal: Conservative interventions for treating exercise-related musculotendinous, ligamentous and osseous groin pain Cochrane Database Syst Rev 6:CD009565,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Green S, Buchbinder R, Hetrick S: Physiotherapy interventions for shoulder pain Cochrane Database Syst Rev 2:CD004258,2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for knee pain Phys Ther 81:1675–1699,2001Philadelphia Panel [PubMed] [Google Scholar]
- 136.Chen L Tang J White PF, etal: The effect of location of transcutaneous electrical nerve stimulation on postoperative opioid analgesic requirement: Acupoint versus nonacupoint stimulation Anesth Analg 87:1129–1134,1998 [PubMed] [Google Scholar]
- 137.Hamza MA White PF Ahmed HE, etal: Effect of the frequency of transcutaneous electrical nerve stimulation on the postoperative opioid analgesic requirement and recovery profile Anesthesiology 91:1232–1238,1999 [DOI] [PubMed] [Google Scholar]
- 138.Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain Phys Ther 81:1641–1674,2001Philadelphia Panel [PubMed] [Google Scholar]
- 139.Khadilkar A Milne S Brosseau L, etal: Transcutaneous electrical nerve stimulation for the treatment of chronic low back pain: A systematic review Spine 30:2657–2666,2005 [DOI] [PubMed] [Google Scholar]
- 140.Vernon HT, Humphreys BK, Hagino CA: A systematic review of conservative treatments for acute neck pain not due to whiplash J Manipulative Physiol Ther 28:443–448,2005 [DOI] [PubMed] [Google Scholar]
- 141.Pengel HM Maher CG Refshauge KM, etal: Systematic review of conservative interventions for subacute low back pain Clin Rehabil 16:811–820,2002 [DOI] [PubMed] [Google Scholar]
- 142.Hurlow A Bennett MI Robb KA, etal: Transcutaneous electric nerve stimulation (TENS) for cancer pain in adults Cochrane Database Syst Rev 3:CD006276,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Marineo G Iorno V Gandini C, etal: Scrambler therapy may relieve chronic neuropathic pain more effectively than guideline-based drug management: Results of a pilot, randomized, controlled trial J Pain Symptom Manage 43:87–95,2012 [DOI] [PubMed] [Google Scholar]
- 144.Caraceni A, Portenoy RK: An international survey of cancer pain characteristics and syndromes: IASP Task Force on Cancer Pain—International Association for the Study of Pain Pain 82:263–274,1999 [DOI] [PubMed] [Google Scholar]
- 145.Zech DF Grond S Lynch J, etal: Validation of World Health Organization guidelines for cancer pain relief: A 10-year prospective study Pain 63:65–76,1995 [DOI] [PubMed] [Google Scholar]
- 146.Stanton-Hicks M Baron R Boas R, etal: Complex regional pain syndromes: Guidelines for therapy Clin J Pain 14:155–166,1998 [DOI] [PubMed] [Google Scholar]
- 147.Jimenez-Andrade JM Mantyh WG Bloom AP, etal: Bone cancer pain Ann N Y Acad Sci 1198:173–181,2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Axelsson B, Sjödén PO: Quality of life of cancer patients and their spouses in palliative home care Palliat Med 12:29–39,1998 [DOI] [PubMed] [Google Scholar]
- 149.O'Mahony S Goulet J Kornblith A, etal: Desire for hastened death, cancer pain and depression: Report of a longitudinal observational study J Pain Symptom Manage 29:446–457,2005 [DOI] [PubMed] [Google Scholar]
- 150.Blount WP: Don't throw away the cane J Bone Joint Surg Am 38-A:695–708,1956 [PubMed] [Google Scholar]
- 151.Cheville AL Kollasch J Vandenberg J, etal: A home-based exercise program to improve function, fatigue, and sleep quality in patients with stage IV lung and colorectal cancer: A randomized controlled trial J Pain Symptom Manage 45:811–821,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Vander Kooi D Abad G Basford JR, etal: Lumbar spine stabilization with a thoracolumbosacral orthosis: Evaluation with video fluoroscopy Spine 29:100–104,2004 [DOI] [PubMed] [Google Scholar]
- 153.Utter A Anderson ML Cunniff JG, etal: Video fluoroscopic analysis of the effects of three commonly-prescribed off-the-shelf orthoses on vertebral motion Spine 35:E525–E529,2010 [DOI] [PubMed] [Google Scholar]
- 154.Rose PS, Buchowski JM: Metastatic disease in the thoracic and lumbar spine: Evaluation and management J Am Acad Orthop Surg 19:37–48,2011 [DOI] [PubMed] [Google Scholar]
- 155.Sandler AJ Dvorak J Humke T, etal: The effectiveness of various cervical orthoses: An in vivo comparison of the mechanical stability provided by several widely used models Spine 21:1624–1629,1996 [DOI] [PubMed] [Google Scholar]
- 156.Tescher AN Rindflesch AB Youdas JW, etal: Range-of-motion restriction and craniofacial tissue-interface pressure from four cervical collars J Trauma 63:1120–1126,2007 [DOI] [PubMed] [Google Scholar]
- 157.Flemming K, Cullum N: Laser therapy for venous leg ulcers Cochrane Database Syst Rev 2:CD001182,2000 [DOI] [PubMed] [Google Scholar]
- 158.Brosseau L Welch V Wells G, etal: Low level laser therapy (classes I, II and III) in the treatment of rheumatoid arthritis Cochrane Database Syst Rev 2:CD002049,2000 [DOI] [PubMed] [Google Scholar]
- 159.Migliorati C Hewson I Lalla RV, etal: Systematic review of laser and other light therapy for the management of oral mucositis in cancer patients Support Care Cancer 21:333–341,2013 [DOI] [PubMed] [Google Scholar]
- 160.Zimin AA Zhevago NA Buĭniakova AI, etal: Application of low-power visible and near infrared radiation in clinical oncology[in Russian] Vopr Kurortol Fizioter Lech Fiz Kult 6:49–52,2009 [PubMed] [Google Scholar]
- 161.Casley-Smith JR, Casley-Smith JR: The pathophysiology of lymphedema and the action of benzo-pyrones in reducing it Lymphology 21:190–194,1988 [PubMed] [Google Scholar]
- 162.Ebert JR Joss B Jardine B, etal: Randomized trial investigating the efficacy of manual lymphatic drainage to improve early outcome after total knee arthroplasty Arch Phys Med Rehabil 94:2103–2111,2013 [DOI] [PubMed] [Google Scholar]
- 163.Ekici G Bakar Y Akbayrak T, etal: Comparison of manual lymph drainage therapy and connective tissue massage in women with fibromyalgia: A randomized controlled trial J Manipulative Physiol Ther 32:127–133,2009 [DOI] [PubMed] [Google Scholar]
- 164.LANA. Lymphoma Association of North America. http://www.clt-lana.org.
- 165.Dr Vodder School International. http://www.vodderschool.com.
- 166.Adie S Kwan A Naylor JM, etal: Cryotherapy following total knee replacement Cochrane Database Syst Rev 9:CD007911,2012 [DOI] [PubMed] [Google Scholar]
- 167.Loyola-Sánchez A, Richardson J, MacIntyre NJ: Efficacy of ultrasound therapy for the management of knee osteoarthritis: A systematic review with meta-analysis Osteoarthritis Cartilage 18:1117–1126,2010 [DOI] [PubMed] [Google Scholar]
- 168.Bloom JE Rischin A Johnston RV, etal: Image-guided versus blind glucocorticoid injection for shoulder pain Cochrane Database Syst Rev 8:CD009147,2012 [DOI] [PubMed] [Google Scholar]
- 169.Barr S, Cerisola FL, Blanchard V: Effectiveness of corticosteroid injections compared with physiotherapeutic interventions for lateral epicondylitis: A systematic review Physiotherapy 95:251–265,2009 [DOI] [PubMed] [Google Scholar]
- 170.Blanchard V, Barr S, Cerisola FL: The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: A systematic review Physiotherapy 96:95–107,2010 [DOI] [PubMed] [Google Scholar]
- 171.Coombes BK Bisset L Brooks P, etal: Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: A randomized controlled trial JAMA 309:461–469,2013 [DOI] [PubMed] [Google Scholar]
- 172.Soares A Andriolo RB Atallah AN, etal: Botulinum toxin for myofascial pain syndromes in adults Cochrane Database Syst Rev 4:CD007533,2012 [DOI] [PubMed] [Google Scholar]
- 173.Alvarez DJ, Rockwell PG: Trigger points: Diagnosis and management Am Fam Physician 65:653–660,2002 [PubMed] [Google Scholar]
- 174.Gerwin RD: Classification, epidemiology, and natural history of myofascial pain syndrome Curr Pain Headache Rep 5:412–420,2001 [DOI] [PubMed] [Google Scholar]
- 175.Cherkin DC Sherman KJ Kahn J, etal: A comparison of the effects of 2 types of massage and usual care on chronic low back pain: A randomized, controlled trial Ann Intern Med 155:1–9,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Kutner JS Smith MC Corbin L, etal: Massage therapy versus simple touch to improve pain and mood in patients with advanced cancer: A randomized trial Ann Intern Med 149:369–379,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]