Abstract
BACKGROUND
Patients with prostate cancer and their providers face uncertainty as they consider adjuvant radiotherapy (ART) or salvage radiotherapy (SRT) after undergoing radical prostatectomy. The authors prospectively evaluated the impact of the Decipher test, which predicts metastasis risk after radical prostatectomy, on decision making for ART and SRT.
METHODS
A total of 150 patients who were considering ART and 115 who were considering SRT were enrolled. Providers submitted a management recommendation before processing the Decipher test and again at the time of receipt of the test results. Patients completed validated surveys on prostate cancer (PCa)‐specific decisional effectiveness and PCa‐related anxiety.
RESULTS
Before the Decipher test, observation was recommended for 89% of patients considering ART and 58% of patients considering SRT. After Decipher testing, 18% (95% confidence interval [95% CI], 12%‐25%) of treatment recommendations changed in the ART arm, including 31% among high‐risk patients; and 32% (95% CI, 24%‐42%) of management recommendations changed in the salvage arm, including 56% among high‐risk patients. Decisional Conflict Scale (DCS) scores were better after viewing Decipher test results (ART arm: median DCS before Decipher, 25 and after Decipher, 19 [P<.001]; SRT arm: median DCS before Decipher, 27 and after Decipher, 23 [P<.001]). PCa‐specific anxiety changed after Decipher testing; fear of PCa disease recurrence in the ART arm (P = .02) and PCa‐specific anxiety in the SRT arm (P = .05) decreased significantly among low‐risk patients. Decipher results reported per 5% increase in 5‐year metastasis probability were associated with the decision to pursue ART (odds ratio, 1.48; 95% CI, 1.19‐1.85) and SRT (odds ratio, 1.41; 95% CI, 1.09‐1.81) in multivariable logistic regression analysis.
CONCLUSIONS
Knowledge of Decipher test results was associated with treatment decision making and improved decisional effectiveness among men with PCa who were considering ART and SRT. Cancer 2017;123:2850–59. © 2017 American Cancer Society.
Keywords: adjuvant therapy, Decipher, decisional conflict, prostate cancer, prostatectomy, quality of life, salvage therapy
Short abstract
Use of the Decipher test appears to result in a change in treatment decision making in a substantial percentage of men with prostate cancer who are considering adjuvant or salvage radiotherapy after radical prostatectomy. Decisional effectiveness improves for both patients and providers with use of the Decipher test.
INTRODUCTION
The majority of cases of prostate cancer are indolent, with a low risk of lethality. However, cases with aggressive pathology exhibit high rates of biochemical and clinical disease progression.1 Randomized controlled trials have demonstrated a progression‐free survival benefit for adjuvant radiotherapy (ART) for patients with aggressive pathology after radical prostatectomy, defined by extracapsular extension, seminal vesicle invasion, or a positive surgical margin.2, 3, 4 However, the impact of ART on overall survival is less clear. Moreover, RT in the early recovery trajectory after radical prostatectomy may arrest the return of sexual and urinary function and impose new bowel‐related side effects.5 In addition, the relative efficacy of immediate ART versus early salvage RT (SRT) has not been rigorously tested in the clinical trial setting. Because of these factors, many practitioners defer ART. Nationally representative prostate cancer registry data suggest a limited uptake of ART for patients with aggressive pathology at the time of radical prostatectomy.6 Similarly, men with a rising prostate‐specific antigen (PSA) level after prostatectomy may benefit from SRT.7 Nevertheless, although early SRT appears to improve prostate cancer‐specific outcomes,8 the PSA threshold at which SRT is most beneficial is unknown.
This clinical environment is an ideal forum for biomarkers that inform clinical decision making. The Decipher test is a genomic classifier that predicts the 5‐year risk of clinical metastases after radical prostatectomy.9, 10, 11, 12, 13 Decipher evaluates the activity of genes in the tumor that are shown to be involved in the progression of prostate cancer by measuring the expression levels of 22 RNA features involved in multiple biological pathways across the genome using a previously locked random forest algorithm.
We prospectively evaluated the impact of the Decipher test on patient and provider decision making regarding the adjuvant treatment of patients with aggressive pathology or salvage treatment of patients with a rising PSA after radical prostatectomy. We assessed the recommended management from the treating provider, as well as patient and provider decision effectiveness before and after viewing the results of a Decipher test. We hypothesized that information from the Decipher test would result in changes in recommended treatment pursuant to the Decipher risk category and with decreased decisional conflict observed in patients and providers.
MATERIALS AND METHODS
Study Participants
The current study was a multicenter, prospective study at 19 sites participating in the Society of Urologic Oncology Clinical Trials Consortium. Patients were recruited from May 2014 through February 2016. We used a 2‐arm cohort trial approach in which all patients received Decipher testing (Fig. 1). Eligible patients had prostate cancer that previously was treated with radical prostatectomy and were being considered for either ART or SRT. The target population was patients with clinicopathological characteristics for whom the decision for ART or SRT was not certain. Thus, we enrolled men with pathologically non‐organ‐confined prostate cancer (ie, pathological classification of T3 disease, including men with extraprostatic extension and/or seminal vesicle invasion) or positive surgical margins into the ART arm. Patients who were eligible for ART were required to have undergone surgery within the preceding 12 months before study enrollment. Patients with a PSA increase or definite biochemical disease recurrence (BCR), defined as a PSA ≥0.2 ng/mL with a confirmatory reading, were enrolled into the SRT arm. Patients who were eligible for SRT were allowed to have received adjuvant hormone therapy before their BCR. Patients with metastatic disease were excluded. Additional exclusions for both arms included failure of PSA to nadir to ≤0.1 ng/mL within 3 months of surgery, receipt of neoadjuvant androgen deprivation therapy (ADT) or, for patients in the ART arm, the receipt of adjuvant systemic therapy. There was no age restriction for participation in the study.
Figure 1.
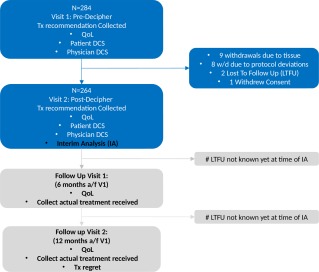
Study schema. DCS indicates Decisional Conflict Scale; Post‐Decipher, after Decipher testing; QoL, quality of life; Tx, treatment; w/d, withdrawal.
Study Procedures
Included patients were not randomized; enrollment was consecutive upon confirmation of eligibility. Stratification was planned 1:1 for the ART and SRT arms. All patient personal health information was blinded and all patients provided informed consent. This study received Institutional Review Board approval through Quorum (#29292) and through Institutional Review Boards as required by site practice. The study is registered on ClinicalTrials.gov (PRO‐IMPACT; ClinicalTrials.gov identifier NCT02080689). Data were collected through an electronic data capturing tool and monitored by a third‐party clinical research organization.
Eligible patients were enrolled between May 2014 and February 2016. Each patient was on study for 1 year. Overall, 265 patients completed visit 1 and visit 2. The intent of this interim report is to compare the treatment recommendations without the Decipher test results (visit 1) with those made after reviewing the Decipher test results (visit 2). This change in treatment recommendation is measured from observation to any treatment and vice versa or from a treatment to a higher magnitude treatment (eg, RT to RT with ADT). Visits 3 and 4 assess actual treatment received and will be presented when full data are available (Fig. 1).
During visit 1, a tumor specimen from the radical prostatectomy was sent to GenomeDx Biosciences Inc (San Diego, Calif). The recommended treatment based on clinical variables and collected baseline demographic and clinical information was recorded. Decision effectiveness using the Decisional Conflict Scale (DCS) for each patient‐provider pair and prostate cancer‐specific anxiety with the Memorial Anxiety Scale for Prostate Cancer (MAX‐PC) also was recorded. During visit 2, Decipher test results were reviewed. The updated treatment recommendation was recorded, and quality of life, decision effectiveness, and prostate cancer‐specific anxiety again were assessed.
The patient DCS is a validated14 16‐item instrument that assesses overall decision conflict as well as subdomains of decision uncertainty: Feeling Informed, Feeling That One's Personal Values Have Been Clarified, Feeling Supported in Decision Making, and Perception of Effective Decision Making. The DCS is scored from 0 to 100, with higher scores indicating greater decisional conflict. The provider‐oriented DCS was the Provider Decision Process Assessment Instrument,15, 16 which is a 12‐item survey that measures the level of confidence in a treatment decision on a scale from 1 (“strongly agree”) to 5 (“strongly disagree”). Total DCS scores range from 12 to 60, with higher scores indicating greater decisional conflict or lower decision effectiveness.15 The modified 18‐item MAX‐PC produces a summary score and also includes 3 subscales: Prostate Cancer Anxiety, PSA Anxiety, and Fear of Prostate Cancer Recurrence, with items scored on a rating scale of 0 to 3.17, 18 Individual items are summed, with higher scores representing higher levels of anxiety.18
Specimen Collection, Handling, and Decipher Test Scoring
Radical prostatectomy specimens were graded by expert genitourinary pathologists from originating institutions using the International Society of Urological Pathology (ISUP) 2005 Gleason grading criteria,19 and formalin‐fixed paraffin‐embedded blocks were selected based on the pathology report. Molecular analysis for Decipher testing was based on the formalin‐fixed paraffin‐embedded block containing the index prostate cancer lesion with the highest stage and tumor grade, and samples were obtained using a 1.5‐mm tissue punch tool provided in the specimen kit.
The Decipher score is based on the expression value of 22 prespecified biomarkers, which are extracted from the normalized data matrix and entered into a locked model as described previously.9 The Decipher test results were sent to the ordering providers and reported the patient's predicted 5‐year probability of developing metastasis after surgery. Decipher test results are grouped into low‐risk (<4%), intermediate‐risk (4%‐9%), and high‐risk (>9%) categories based on previously described thresholds.11
Statistical Analysis
The protocol‐defined primary objective of the current study was to determine the extent to which use of the Decipher test influences treatment recommendations immediately after radical prostatectomy and at the time of BCR. The primary endpoint was defined as any change in treatment plan from before to after the Decipher report. Although this interim report represents the study's primary analysis, data collection is ongoing to determine the consistency of the treatment plan with the actual treatment received within 12 months of radical prostatectomy or BCR.
The study protocol specified a sample size of 150 patients (150 patients after radical prostatectomy and 150 patients after BCR) to achieve a 2‐sided 95% confidence interval (95% CI) half‐width <9% when accounting for within‐physician correlation (ie, multiple recommendations per physician) and assuming results similar to previous work.20, 21
All statistical tests were 2‐sided, and are reported with a significance level of .05. Analyses were performed in R statistical software (version 3.1; R Foundation, Vienna, Austria). All analyses and results were confirmed by a third‐party statistician (D.J.S.T.) independent of GenomeDx Biosciences. We present descriptive statistics focused on medians and interquartile ranges (IQRs) or frequencies and percentages as appropriate. Treatment recommendations were analyzed as stratified by Decipher risk categories.22 Exact binomial CIs were constructed to measure changes in treatment recommendations, before and after the Decipher test results. The paired Wilcoxon test was used to compare continuous scores on decisional conflict and patient‐reported anxiety. Univariable and multivariable logistic regression models were constructed to assess the association between Decipher test results and treatment recommendations, independent of demographic and clinical variables. For these models, the response variable was classified as observation (ie, no further therapy) versus treatment (ie, ART or SRT or systemic therapy). Results were corroborated by mixed‐effect logistic regression models to account for the potential correlation of multiple patients seen by the same physician; results were similar without changes in significance.
RESULTS
Between May 2014 and February 2016 (the enrollment period), 159 and 125 patients, respectively, were enrolled in the ART and SRT arms. Of these, 150 patients (94%) and 114 patients (91%), respectively, completed the before and after Decipher visits (visits 1 and 2). Nine patients (6%) and 11 patients (9%), respectively, withdrew due to tissue availability, loss to follow‐up, protocol deviations, or withdrawal of consent before completing visit 2.
Patient Characteristics
Demographic, clinical, and pathological characteristics of the study cohort are shown in Table 1. Approximately one‐half of the patients in the ART arm had positive surgical margins and 67% had ≥pT3 prostate cancer; 47% had pathological ISUP grade 3 to 5 (Gleason scores of 4 + 3=7 or 8‐10). The median Decipher probability of metastasis at 5 years after radical prostatectomy was 6.2% (IQR, 2.4%‐11.2%). Decipher testing classified 46.0%, 22.0%, and 32.0% of patients, respectively, into low‐risk, intermediate‐risk, and high‐risk groups.
Table 1.
Clinicopathologic Characteristics of Patients in Each Study Arm
| Variables | Adjuvant Radiotherapy Arma | Salvage Radiotherapy Armb |
|---|---|---|
| No. of Patients | 150 | 115 |
| Age at RP, y | ||
| Median (range) | 64 (46‐76) | 63 (48‐75) |
| IQR (Q1‐Q3) | 59‐69 | 58‐67 |
| Race | ||
| White (non‐Hispanic) | 126 (84%) | 95 (82.6%) |
| White (Hispanic) | 9 (6%) | 8 (7%) |
| Black/African | 11 (7.3%) | 12 (10.4%) |
| Asian | 3 (2%) | ‐ |
| Unknown | 1 (0.7%) | ‐ |
| Preoperative PSA, ng/mL | ||
| Median (range) | 6.3 (0.9‐40.5) | 6.7 (0.8‐55.5) |
| IQR (Q1‐Q3) | 4.9‐10 | 4.7‐9.4 |
| <10 | 110 (73.3%) | 86 (74.8%) |
| 10‐20 | 30 (20%) | 20 (17.4%) |
| >20 | 8 (5.3%) | 5 (4.3%) |
| PSA at time of enrollment, ng/mL | ||
| Median (range) | 0.2 (0.0‐4.0) | |
| IQR (Q1‐Q3) | 0.1‐0.3 | |
| Extraprostatic extension, no. (%) | ||
| Present | 99 (66%) | 45 (39.1%) |
| Seminal vesicle invasion, no. (%) | ||
| Present | 22 (14.7%) | 14 (12.2%) |
| Surgical margin, no. (%) | ||
| Positive | 75 (50%) | 56 (48.7%) |
| Lymph node invasion, no. (%) | ||
| Positive | 2 (1.3%) | 2 (1.7%) |
| Pathologic Gleason score, no. (%) | ||
| 6 | 2 (1.3%) | 9 (7.8%) |
| 7 | ||
| 3+4 | 78 (52%) | 49 (42.6%) |
| 4+3 | 41 (27.3%) | 36 (31.3%) |
| 8 | 17 (11.3%) | 9 (7.8%) |
| 9 | 12 (8%) | 12 (10.4%) |
| Pathological T classification, no. (%) | ||
| T2 | 40 (26.7%) | 53 (46.1%) |
| T3a | 78 (52%) | 35 (30.4%) |
| T3b | 22 (14.7%) | 14 (12.2%) |
| Unknown | 10 (6.7%) | 13 (11.3%) |
| Decipher risk probability at 5 y after RP | ||
| Median (range) | 6.2% (0.5%‐44.2%) | 6.5% (0.5%‐62.8%) |
| IQR (Q1‐Q3) | 2.4%‐11.2% | 2.7%‐14.4% |
| Low | 69 (46%) | 38 (33%) |
| Intermediate | 33 (22%) | 29 (25.2%) |
| High | 48 (32%) | 48 (41.7%) |
Abbreviations: IQR, interquartile range; PSA, prostate‐specific antigen; Q, quartile; RP, radical prostatectomy.
In the adjuvant radiotherapy arm, unknown preoperative PSA, extraprostatic extension, seminal vesicle invasion, and lymph node invasion status for 2, 4, 9, and 21 patients, respectively.
In salvage radiotherapy arm, unknown preoperative PSA, extraprostatic extension, seminal vesicle invasion, and lymph node invasion status for 4, 10, 8, and 20 patients, respectively.
In the SRT arm, 49% of patients had positive surgical margins and 43% had ≥pT3 prostate cancer; 49.5% had pathological ISUP grade 3 to 5. The median Decipher probability of metastasis at 5 years after radical prostatectomy was 6.5% (IQR, 2.7%‐14.4%). Overall, Decipher testing classified 33.0%, 25.2%, and 41.7% of patients, respectively, into low‐risk, intermediate‐risk, and high‐risk groups.
Treatment Recommendations
Before Decipher, observation was recommended for 88.7% of patients in the ART arm (133 patients) and 11.3% (17 patients) received a recommendation for ART (Table 2). Observation was recommended for 58.3% of patients in the SRT arm (67 patients), and 32.2% (37 patients) received a recommendation for SRT and 9.6% (11 patients) received a recommendation for either ADT or SRT and ADT. After Decipher testing, we observed an 18% change (95% CI, 12%‐25%; 27 patients) in treatment recommendations in the ART arm and a 32% change (95% CI, 24%‐42%; 37 patients) in treatment recommendations in the SRT arm.
Table 2.
Effect of the Decipher Test Result on Urologists' Treatment Recommendations After RP
| Adjuvant Radiotherapy Arm | Salvage Radiotherapy Arm | ||||||
|---|---|---|---|---|---|---|---|
| Without Decipher | With Decipher | No. Without Decipher | Change No. (%) | 95% CI | No. Without Decipher | Change No. (%) | 95% CI |
| Overall | Any change | 150 | 27 (18%) | 12%‐25% | 115 | 37 (32%) | 24%‐42% |
| Observation | Any treatment | 133 | 19 (14%) | 9%‐21% | 67 | 18 (27%) | 17%‐39% |
| Observation | RT | 133 | 17 (13%) | 8%‐20% | 67 | 12 (18%) | 10%‐29% |
| Observation | RT plus ADT | 133 | 2 (2%) | 0%‐5% | 67 | 5 (7%) | 2%‐17% |
| Observation | ADT | ‐ | ‐ | ‐ | 67 | 1 (1%) | 0%‐8% |
| Any treatment | Any change | 17 | 8 (47%) | 23%‐72% | 48 | 19 (40%) | 26%‐55% |
| RT | Observation | 17 | 6 (35%) | 14%‐62% | 37 | 10 (27%) | 14%‐44% |
| RT | RT plus ADT | 17 | 2 (12%) | 1%‐36% | 37 | 6 (16%) | 6%‐32% |
| RT plus ADT | Observation | ‐ | ‐ | ‐ | 9 | 1 (11%) | ‐ |
| RT plus ADT | RT | ‐ | ‐ | ‐ | 9 | 1 (11%) | ‐ |
| ADT | RT | ‐ | ‐ | ‐ | 2 | 1 (50%) | ‐ |
Abbreviations: 95% CI, 95% confidence interval; ADT, androgen deprivation therapy; RP, radical prostatectomy; RT, radiotherapy.
Stratified by Decipher risk category, 91% (63 patients) and 96% (66 patients) of patients in the ART arm and Decipher low‐risk group were recommended to undergo observation before and after the addition of information from the Decipher test, respectively. Fewer patients retained recommendations for observation after the addition of information from the Decipher test in both the intermediate‐risk (79% [26 patients] before to 73% [24 patients] after receiving Decipher results) and high‐risk (92% [44 patients] before to 63% [30 patients] after receiving Decipher results) groups. After Decipher, 37% (18 patients) of Decipher high‐risk patients were recommended to receive more intense therapy (ART instead of observation or ART and ADT instead of RT alone) compared with 8% (4 patients) when only clinical and pathological characteristics were considered (Fig. 2A).
Figure 2.
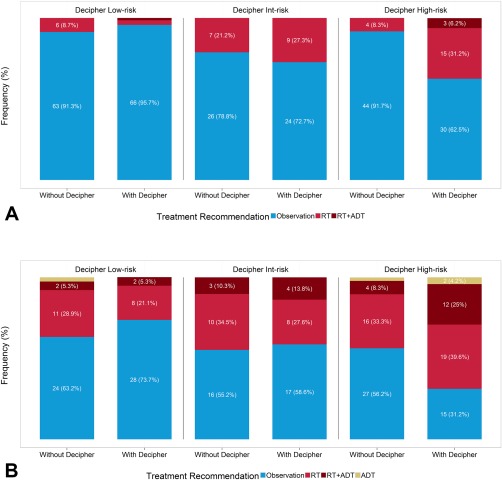
(A) Changes in treatment recommendation by Decipher risk category in the adjuvant radiotherapy arm. (B) Changes in treatment recommendation by Decipher risk category in the salvage radiotherapy arm. ADT indicates androgen deprivation therapy; Int, intermediate; RT, radiotherapy.
Among patients in the SRT arm, 63% (24 patients) and 74% (28 patients) of Decipher low‐risk patients were recommended to undergo observation before and after Decipher testing, respectively. Observation recommendations increased for Decipher intermediate‐risk patients as well: 55% (16 patients) before Decipher and 59% (17 patients) after Decipher. After Decipher testing, 69% (33 patients) of Decipher high‐risk patients were recommended to receive more intense therapy (SRT instead of observation, SRT and ADT instead of RT alone, or ADT) compared with 44% of patients (21 patients) when only clinical and pathological characteristics were considered (Fig. 2B).
Figure 3 displays changes in treatment recommendations at intervals of Decipher probability of clinical metastases 5 years after radical prostatectomy in the ART (Figs. 3A and 3B) and SRT (Figs. 3C and 3D) arms. Patients with higher probabilities of metastasis were more often recommended more intense therapy (P<.001 for both the ART and SRT arms).
Figure 3.
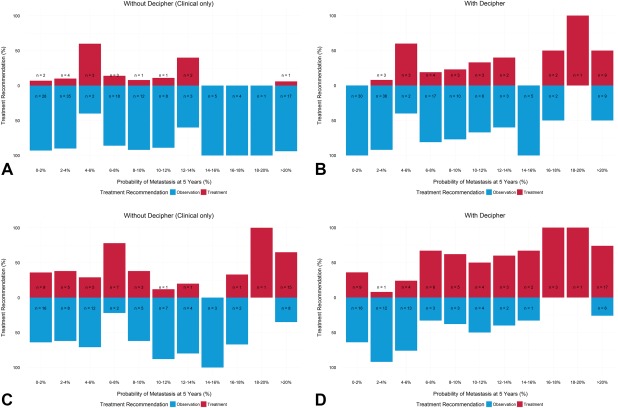
(A) Treatment recommendation in the adjuvant radiotherapy arm without Decipher by use of clinical features only. (B) Treatment recommendation in the adjuvant radiotherapy arm once exposed to Decipher testing. (C) Treatment recommendation in the salvage radiotherapy arm without Decipher by use of clinical features only. (D) Treatment recommendation in the salvage radiotherapy arm once exposed to Decipher testing.
Multivariable models assessing the independent association between Decipher test results and a change in treatment recommendation, adjusting for demographic, clinical, and pathological variables, demonstrated a statistically significant association between Decipher results and treatment in both the ART and SRT arms (Table 3). All other variables held constant: a 5% increase in the Decipher 5‐year probability of clinical metastases was associated with significantly higher odds of ART (odds ratio, 1.48; 95% CI, 1.19‐1.85 [P<.001]) and SRT (odds ratio, 1.41; 95% CI, 1.09‐1.81 [P = .01]) versus observation.
Table 3.
MVA of Decision to Pursue ART or SRT After Decipher Test Report
| MVA | |||
|---|---|---|---|
| Arm | Variables | OR (95% CI) | P |
| Adjuvant radiotherapy | Age, y | 1.01 (0.94‐1.08) | .83 |
| Preoperative PSAa | 1.03 (0.60‐1.78) | .91 | |
| Extraprostatic extension | 0.67 (0.23‐1.95) | .46 | |
| Seminal vesicle invasion | 1.99 (0.55‐7.14) | .29 | |
| Surgical margin | 2.22 (0.71‐6.99) | .17 | |
| Pathological Gleason score of 4+3 (vs ≤3+4) | 1.77 (0.59‐5.31) | .31 | |
| Pathological Gleason score ≥8 (vs ≤3+4) | 1.26 (0.35‐4.55) | .72 | |
| Decipher riskb | 1.48 (1.19‐1.85) | <.001 | |
| Salvage radiotherapy | Age, y | 0.99 (0.92‐1.06) | .8 |
| Preoperative PSAa | 1.09 (0.68‐1.74) | .73 | |
| Extraprostatic extension | 2.31 (0.77‐6.92) | .13 | |
| Seminal vesicle invasion | 2.13 (0.49‐9.16) | .31 | |
| Surgical margin | 0.56 (0.21‐1.45) | .23 | |
| Pathological Gleason score of 4+3 (vs ≤3+4) | 0.55 (0.18‐1.68) | .29 | |
| Pathological Gleason score ≥8 (vs ≤3+4) | 1.24 (0.33‐4.59) | .75 | |
| Time to BCR or PSA rise, y | 0.99 (0.78‐1.26) | .96 | |
| Decipher riskb | 1.30 (1.03‐1.65) | .03 | |
Abbreviations: 95% CI, 95% confidence interval; ART, adjuvant radiotherapy; BCR, biochemical disease recurrence; MVA, multivariable analysis; OR, odds ratio; PSA, prostate‐specific antigen; SRT, salvage radiotherapy.
Preoperative PSA values were log2 transformed.
Decipher risk was reported for a 5% increase in the 5‐year probability of metastasis.
Decision Effectiveness
Among patients in both the ART and SRT arms, use of the Decipher test was associated with decreased decisional conflict overall (ART arm: median DCS before Decipher, 25 [IQR, 8‐44] and median DCS after Decipher, 19 [IQR, 2‐30] [P<.001]; and SRT: median DCS before Decipher, 27 [IQR, 16‐41] and median DCS after Decipher, 23 [IQR, 4‐30] [P<.001]) and improved decision effectiveness in the DCS subdomains of Decisional Uncertainty and Feeling Supported in Your Decision (Table 4). Among providers, the decisional conflict exhibited a statistically significant decrease of similar magnitude in both the ART (median DCS before Decipher, 32 [IQR, 28‐36] and median DCS after Decipher, 28 [IQR, 23‐34] [P<.001]) and SRT (median DCS before Decipher, 33 [IQR, 26‐36] and median DCS after Decipher, 29 [IQR, 22‐34] [P<.001]) arms.
Table 4.
Decisional Conflict Scale
| Without Decipher | With Decipher | |||||||
|---|---|---|---|---|---|---|---|---|
| Arm | DCS | No. | Median (Range) | IQR | No. | Median (Range) | IQR | P a |
| Adjuvant radiotherapy | DCS (patient) | 125 | 25 (0‐81) | 8‐44 | 125 | 19 (0‐86) | 2‐30 | <.001 |
| DCS uncertainty | 128 | 33 (0‐100) | 17‐50 | 128 | 25 (0‐100) | 0‐42 | ||
| DCS informed | 126 | 25 (0‐75) | 0‐50 | 126 | 25 (0‐75) | 0‐25 | ||
| DCS values clarity | 127 | 25 (0‐92) | 0‐50 | 127 | 25 (0‐100) | 0‐25 | ||
| DCS support | 128 | 25 (0‐75) | 0‐33 | 128 | 17 (0‐75) | 0‐25 | ||
| DCS effective decision | 126 | 25 (0‐81) | 6‐50 | 126 | 25 (0‐100) | 0‐31 | ||
| DCS (provider) | 150 | 32 (12‐42) | 28‐36 | 150 | 28 (12‐42) | 23‐34 | <.001 | |
| Salvage radiotherapy | DCS (patient) | 95 | 27 (0‐91) | 16‐41 | 95 | 23 (0‐81) | 4‐30 | <.001 |
| DCS uncertainty | 98 | 33 (0‐100) | 25‐50 | 98 | 25 (0‐100) | 0‐42 | ||
| DCS informed | 100 | 25 (0‐100) | 17‐50 | 100 | 25 (0‐100) | 0‐25 | ||
| DCS values clarity | 99 | 25 (0‐100) | 17‐50 | 99 | 25 (0‐100) | 0‐25 | ||
| DCS support | 99 | 25 (0‐75) | 4‐25 | 99 | 17 (0‐67) | 0‐25 | ||
| DCS effective decision | 97 | 25 (0‐100) | 12‐38 | 97 | 25 (0‐100) | 0‐25 | ||
| DCS (provider) | 115 | 33 (12‐46) | 26‐36 | 115 | 29 (12‐41) | 22‐34 | <.001 | |
Abbreviations: DCS, Decisional Conflict Scale; IQR, interquartile range.
Two‐sided P value was derived from the Wilcoxon signed rank test.
Among patients in the ART arm whose treatment recommendation did not change after Decipher, DCS exhibited a statistically significant decrease in patients (median DCS before Decipher, 25 [IQR, 6‐43] and median DCS after Decipher, 18 [IQR, 2‐29] [P<.001]) and providers (median DCS before Decipher, 32 [IQR, 28‐36] and median DCS after Decipher, 28 [IQR, 23‐35] [P<.001]) (see Supporting Information Table 1). Changes in DCS were not significant for patients and providers among patients in the ART arm whose treatment recommendation changed (see Supporting Information Table 1).
Among patients in the SRT arm whose treatment recommendation changed after Decipher testing, DCS exhibited a statistically significant decrease in patients (median DCS before Decipher, 25 [IQR, 16‐50] and median DCS after Decipher, 20 [IQR, 2‐28] [P = .001]) and providers (median DCS before Decipher, 33 [IQR, 25‐36] and median DCS after Decipher, 26 [IQR, 19‐32] [P<.001]) (see Supporting Information Table 1). Statistically significant changes in the DCS of patients and providers also were observed among patients in the SRT arm whose treatment recommendations did not change after Decipher (both P≤.02) (see Supporting Information Table 1).
Considering all patients, prostate cancer‐specific anxiety did not exhibit statistically significant changes in the ART and SRT arms (Table 5). However, changes were observed among patients found to be at low risk of clinical metastases by Decipher (see Supporting Information Table 2). Among patients judged to be at low risk by Decipher testing in the ART arm, anxiety decreased in the majority of patients, and fear of prostate cancer recurrence exhibited a statistically significant decrease (P = .02). Among Decipher low‐risk patients in the SRT arm, anxiety decreased in the majority of patients, and prostate cancer‐specific anxiety exhibited a marginally statistically significant decrease (P = .05). Anxiety did not increase significantly among Decipher high‐risk patients.
Table 5.
Quality of Life: MAX‐PC Questionnaire
| QOL | Adjuvant Radiotherapy Arm | Salvage Radiotherapy Arm | ||||
|---|---|---|---|---|---|---|
| 18‐Item MAX‐PC | No. | No. Change (%) | P a | No. | No. Change (%) | P a |
| Total MAX‐PC | 134 | .48 | 104 | .14 | ||
| Decreased | 63 (47%) | 52 (50%) | ||||
| No change | 14 (10.4%) | 11 (10.6%) | ||||
| Increased | 57 (42.5%) | 41 (39.4%) | ||||
| PC anxiety | 134 | .34 | 105 | .38 | ||
| Decreased | 57 (42.5%) | 48 (45.7%) | ||||
| No change | 27 (20.1%) | 20 (19%) | ||||
| Increased | 50 (37.3%) | 37 (35.2%) | ||||
| PSA anxiety | 138 | .6 | 105 | .63 | ||
| Decreased | 18 (13%) | 21 (20%) | ||||
| No change | 96 (69.6%) | 65 (61.9%) | ||||
| Increased | 24 (17.4%) | 19 (18.1%) | ||||
| Fear of disease recurrence | 138 | .33 | 104 | .24 | ||
| Decreased | 58 (42%) | 43 (41.3%) | ||||
| No change | 34 (24.6%) | 27 (26%) | ||||
| Increased | 46 (33.3%) | 34 (32.7%) | ||||
Abbreviations: MAX‐PC, Memorial Anxiety Scale for Prostate Cancer; PSA, prostate‐specific antigen.
Two‐sided P value was derived from the Wilcoxon signed rank test.
DISCUSSION
Use of a genomic test that delineates a patient's risk of clinical metastasis after radical prostatectomy is associated with changes in recommended adjuvant and salvage treatment and improved decisional effectiveness. Treatment recommendations were found to align with Decipher risk category: Decipher low‐risk patients were more likely to receive recommendations for observation, whereas Decipher high‐risk patients were more likely to receive recommendations for ART.
The magnitude of change in treatment recommendations was more pronounced for men in the SRT arm of the current study. This relates in part to the finding that the default recommendation for men with adverse pathology at the time of radical prostatectomy is observation. Only 10% of men found to have adverse pathology on prostatectomy were recommended for ART.
Although ART has been associated with improved progression‐free survival, the comparative effectiveness of ART compared with early SRT is uncertain, and the impact of ART on overall survival has not been established to date. This may leave providers reluctant to pursue a clinical course that may compromise functional recovery.23
The changes in treatment recommendations that we observed in the current study were more pronounced among men with higher risk Decipher scores suggesting a higher genomic risk for clinical metastases. Decipher low‐risk patients were more likely to receive observation recommendations after use of the test. Decipher high‐risk patients were more likely to receive ART or SRT recommendations or to receive recommendations for interventions of a greater magnitude (eg, patients may receive a recommendation for ART and ADT instead of ART alone). The degree to which provider recommendations changed was more pronounced among patients in the SRT arm, which may reflect the differences in clinical scenarios. In the SRT arm, providers are confronted with men whose prostate cancer has definitively recurred. In the ART arm, patients are instead at a conceptual risk of a future disease recurrence based on the adverse features of their prostatectomy specimen.
Both clinical scenarios clearly present prostate cancer care providers with decisional uncertainty. In both the ART and SRT settings, providers had DCS scores >30, reflecting substantial decisional conflict. Although use of Decipher testing was associated with a statistically significant reduction in DCS, the median DCS after Decipher still was high, indicating residual decisional uncertainty. Although we believe that Decipher has the potential to improve clinical decision making for patients considering ART and SRT, additional decision aids may be required to clarify which patients are optimally selected for observation or additional therapy.
This provider uncertainty likely impacts patient‐reported decisional conflict. A patient DCS score >25 is considered to indicate clinically significant decisional conflict.24 Decipher testing was found to be associated with reduced patient decisional conflict with notable reductions in the subdomains of Decisional Uncertainty and Decisional Support. Overall DCS scores as well as the Decisional Uncertainty and Decisional Support subscales decreased from levels consistent with clinically significant decisional conflict to scores considered to be nonsignificant.
It is interesting to note that the ART and SRT arms exhibited inverse associations between DCS reductions and whether the treatment recommendation changed after use of the Decipher test. Among patients in the ART arm, it appeared that Decipher testing most effectively reassured patients and providers about observation. Among patients in the SRT arm, Decipher testing reassured patients and providers regarding the need to change the treatment recommendation, which most commonly meant pursuit of SRT. In both arms, anxiety was most robustly and significantly decreased in men found to be categorized as low risk by Decipher testing. In demonstrating improved decisional effectiveness, we highlight the impact of Decipher on patient‐centered health outcomes beyond clinical impact.
The current study has several limitations. First, we are presenting interim data regarding treatment recommendations, which may not correlate with the actual treatment received. Final analysis of the current study will identify treatments received within 12 months of Decipher testing. Second, patients are their own controls; we do not include a group unexposed to Decipher testing. Patients who have additional time to consider their clinical and pathological characteristics may have decisional effectiveness changes parallel with the current study findings. Third, patients in the SRT arm have heterogeneous time since prostatectomy, which may influence treatment recommendations independent of Decipher testing results. Last, to the best of our knowledge, no genomic test to date has been validated against a control to demonstrate that use of the test improves prostate cancer‐specific outcomes.
Despite these limitations, we identified significant associations between Decipher genomic testing and both the treatment recommendations and decisional effectiveness underlying those recommendations. Patients determined to be at low risk of metastasis by Decipher had higher rates of observation recommendations and patients determined to be at high risk of metastasis had higher rates of ART and SRT recommendations. Decisional conflict was lower after viewing Decipher test results for both patient and providers. The Decipher test has the potential to be an important adjunct to clinical decision making in men with adverse pathology or a rising PSA after undergoing radical prostatectomy for prostate cancer.
FUNDING SUPPORT
Sponsored by GenomeDx Biosciences Inc.
CONFLICT OF INTEREST DISCLOSURES
Marguerite du Plessis has received fees from GenomeDx Biosciences Inc for work performed as part of and outside of the current study. María Santiago‐Jiménez and Kasra Yousefi are employees of GenomeDx Biosciences Inc. Darby J. S. Thompson's institution has a statistical support contract with GenomeDx Biosciences Inc. Lawrence Karsh has acted as a paid consultant and speaker and received research funding to his institution from Astellas, Janssen, and Medivation; has acted as a paid consultant and received research funding to his institution from Bayer, Spectrum, Ferring Pharmaceuticals, Precision Biopsy, Argos, Tokai, Takeda, Heat Biologics, Augmenix, and Dendreon; acted as a paid consultant for Sanofi and 3D Biopsy; and received research funding to his institution from GenomeDx Biosciences Inc and Genomic Health for work performed outside of the current study. Adam S. Kibel has acted as a member of the advisory boards of Sanofi Aventis, Dendreon, Profound, MTG, Tokai, and Bayer for work performed outside of the current study. Hyung Kim received a grant from GenomeDx Biosciences Inc for work performed as part of the current study. William Lowrance has received funds from Myriad Genetics for work performed outside of the current study and acted as an advisory board member for MDxHealth. Elai Davicioni is an employee of GenomeDx Biosciences Inc. Yair Lotan has received grants from GenomeDx Biosciences Inc for work performed as part of and outside of the current study.
AUTHOR CONTRIBUTIONS
John L. Gore: Conceptualization‐equal and writing‐original draft. Marguerite du Plessis: Conceptualization‐equal, data curation, and project administration. María Santiago‐Jiménez: Formal analysis. Kasra Yousefi: Validation. Darby J. S. Thompson: Methodology. Lawrence Karsh: Investigation‐supporting. Brian R. Lane: Investigation‐supporting. Michael Franks: Investigation‐supporting. David Y. T. Chen: Investigation‐supporting. Mark Bandyk: Investigation‐supporting. Fernando J. Bianco Jr: Investigation‐supporting. Gordon Brown: Investigation‐supporting. William Clark: Investigation‐supporting. Adam S. Kibel: Investigation‐supporting. Hyung L. Kim: Investigation‐supporting. William Lowrance: Investigation‐supporting. Murugesan Manoharan: Investigation‐supporting. Paul Maroni: Investigation‐supporting. Scott Perrapato: Investigation‐supporting. Paul Sieber: Investigation‐supporting. Edouard J. Trabulsi: Investigation‐supporting. Robert Waterhouse: Investigation‐supporting. Elai Davicioni: Funding acquisition. Yair Lotan: Investigation‐supporting. Daniel W. Lin: Investigation‐lead and writing‐review and editing.
Supporting information
Additional supporting information may be found in the online version of this article.
Supporting Information
REFERENCES
- 1. Ross AE, Yousefi K, Davicioni E, et al. Utility of risk models in decision making after radical prostatectomy: lessons from a natural history cohort of intermediate‐ and high‐risk men. Eur Urol. 2016;69:496‐504. [DOI] [PubMed] [Google Scholar]
- 2. Thompson IM, Tangen CM, Paradelo J, et al. Adjuvant radiotherapy for pathologically advanced prostate cancer: a randomized clinical trial. JAMA. 2006;296:2329‐2335. [DOI] [PubMed] [Google Scholar]
- 3. Swanson GP, Hussey MA, Tangen CM, et al; SWOG 8794 . Predominant treatment failure in postprostatectomy patients is local: analysis of patterns of treatment failure in SWOG 8794. J Clin Oncol. 2007;25:2225‐2229. [DOI] [PubMed] [Google Scholar]
- 4. Bolla M, van Poppel H, Tombal B, et al; European Organisation for Research and Treatment of Cancer , Radiation Oncology and Genito‐Urinary Groups . Postoperative radiotherapy after radical prostatectomy for high‐risk prostate cancer: long‐term results of a randomised controlled trial (EORTC trial 22911). Lancet. 2012;380:2018‐2027. [DOI] [PubMed] [Google Scholar]
- 5. Suardi N, Gallina A, Lista G, et al. Impact of adjuvant radiation therapy on urinary continence recovery after radical prostatectomy. Eur Urol. 2014;65:546‐551. [DOI] [PubMed] [Google Scholar]
- 6. Sineshaw HM, Gray PJ, Efstathiou JA, Jemal A. Declining use of radiotherapy for adverse features after radical prostatectomy: results from the National Cancer Data Base. Eur Urol. 2015;68:768‐774. [DOI] [PubMed] [Google Scholar]
- 7. Freedland SJ, Choeurng V, Howard L, et al. Utilization of a genomic classifier for prediction of metastasis following salvage radiation therapy after radical prostatectomy. Eur Urol. 2016;70:588‐596. [DOI] [PubMed] [Google Scholar]
- 8. Tendulkar RD, Agrawal S, Gao T, et al. Contemporary update of a multi‐institutional predictive nomogram for salvage radiotherapy after radical prostatectomy [published online ahead of print August 15, 2016]. J Clin Oncol. doi:10.1200/JCO.2016.67.9647. [DOI] [PubMed] [Google Scholar]
- 9. Erho N, Crisan A, Vergara IA, et al. Discovery and validation of a prostate cancer genomic classifier that predicts early metastasis following radical prostatectomy. PLoS One. 2013;8:e66855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ross A, Feng FY, Ghadessi M, et al. A genomic classifier predicting metastatic disease progression in men with biochemical recurrence after prostatectomy. Prostate Cancer Prostatic Dis. 2014;17:64‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karnes RJ, Bergstralh EJ, Davicioni E, et al. Validation of a genomic classifier that predicts metastasis following radical prostatectomy in an at risk patient population. J Urol. 2013;190:2047‐2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Den RB, Feng FY, Showalter TN, et al. Genomic prostate cancer classifier predicts biochemical failure and metastases in patients after postoperative radiation therapy. Int J Radiat Oncol Biol Phys. 2014;89:1038‐1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Den RB, Yousefi K, Trabulsi EJ, et al. Genomic classifier identifies men with adverse pathology after radical prostatectomy who benefit from adjuvant radiation therapy. J Clin Oncol. 2015;33:944‐951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25‐30. [DOI] [PubMed] [Google Scholar]
- 15. Dolan JG. A method for evaluating health care providers' decision making: the Provider Decision Process Assessment Instrument. Med Decis Making. 1999;19:38‐41. [DOI] [PubMed] [Google Scholar]
- 16. Sheridan SL, Golin C, Bunton A, et al. Shared decision making for prostate cancer screening: the results of a combined analysis of two practice‐based randomized controlled trials. BMC Med Inform Decis Mak. 2012;12:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Roth A, Nelson CJ, Rosenfeld B, et al. Assessing anxiety in men with prostate cancer: further data on the reliability and validity of the Memorial Anxiety Scale for Prostate Cancer (MAX‐PC). Psychosomatics. 2006;47:340‐347. [DOI] [PubMed] [Google Scholar]
- 18. Roth AJ, Rosenfeld B, Kornblith AB, et al. The Memorial Anxiety Scale for prostate cancer: validation of a new scale to measure anxiety in men with prostate cancer. Cancer. 2003;97:2910‐2918. [DOI] [PubMed] [Google Scholar]
- 19. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL; ISUP Grading Committee . The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2005;29:1228‐1242. [DOI] [PubMed] [Google Scholar]
- 20. Badani K, Thompson DJ, Buerki C, et al. Impact of a genomic classifier of metastatic risk on postoperative treatment recommendations for prostate cancer patients: a report from the DECIDE study group. Oncotarget. 2013;4:600‐609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Badani KK, Thompson DJ, Brown G, et al. Effect of a genomic classifier test on clinical practice decisions for patients with high‐risk prostate cancer after surgery. BJU Int. 2015;115:419‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ross AE, Johnson MH, Yousefi K, et al. Tissue‐based genomics augments post‐prostatectomy risk stratification in a natural history cohort of intermediate‐ and high‐risk men. Eur Urol. 2016;69:157‐165. [DOI] [PubMed] [Google Scholar]
- 23. Hu JC, Elkin EP, Krupski TL, Gore J, Litwin MS. The effect of postprostatectomy external beam radiotherapy on quality of life: results from the Cancer of the Prostate Strategic Urologic Research Endeavor. Cancer. 2006;107:281‐288. [DOI] [PubMed] [Google Scholar]
- 24. Thompson‐Leduc P, Turcotte S, Labrecque M, Legare F. Prevalence of clinically significant decisional conflict: an analysis of five studies on decision‐making in primary care. BMJ Open. 2016;6:e011490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional supporting information may be found in the online version of this article.
Supporting Information


