Abstract
Objective
To compare the efficacy of embedded nurse-led versus conventional physician-led follow-up on disease activity in patients with rheumatoid arthritis (RA).
Methods
In a systematic literature search, we identified randomised controlled trials (RCTs) reporting on the efficacy of nurse-led follow-up on disease control in patients with RA compared with physician-led follow-up. Primary outcome was disease activity indicated by Disease Activity Score (DAS)-28. Secondary outcomes were: patient satisfaction, physical disability, fatigue, self-efficacy and quality of life. Outcomes were assessed after 1-year and 2 year follow-ups.
Results
Seven studies representing five RCTs, including a total of 723 participants, were included. All but one study included stable patients in low disease activity or remission at baseline. No difference in DAS-28 was found after 1 year (mean difference (MD) −0.07 (95% CI −0.23 to 0.09)). After 2 years, a statistically significant difference was seen in favour of nurse-led follow-up (MD −0.28 (95% CI −0.53 to −0.04)). However, the difference did not reach a clinically relevant level.
No difference was found in patient satisfaction after 1 year (standard mean difference (SMD) −0.17 (95 % CI −1.0 to 0.67), whereas a statistical significant difference in favour of nurse-led follow-up was seen after 2 years (SMD: 0.6 (95% CI –0.00 to 1.20)).
Conclusion
After 1 year no difference in disease activity, indicated by DAS-28, were found between embedded nurse-led follow-up compared with conventional physician-led follow-up, in RA patients with low disease activity or remission.
Keywords: rheumatoid arthritis, nursing, DAS28
Key messages.
What is already known about this subject?
In the recent years, evidence of the involvement of nurses in care and control of disease activity in patients with rheumatoid arthritis (RA) has increased.
What does this study add?
By conducting a meta-analysis, we have created an overview that can ease intrepretation of the evidence. After 1 year, there were no differences in disease activity between nurse-led and phycisian-led follow-up.
How might this impact on clinical practice?
Our findings may promote the implementation of nurse-led follow-up supervised by physicians in the future.
Introduction
Treatment of rheumatoid arthritis (RA) aims to achieve remission or low disease activity (treat-to-target) in order to stop or minimise joint erosion, normalise functioning and improve the patients’ quality of life.1 Hence, important elements in the RA treatment strategy such as early diagnosis and initiation of pharmacological treatment, quick escalation of drugs to a clinically effective level and adjustment of the dose when there are signs of disease activity are considered important.1 This requires close monitoring of disease activity and adjustments of the pharmacological therapy in patients with RA throughout the course of their disease. In patients with moderate or high disease activity, it is recommended that measurements of disease activity are obtained monthly and in patients with sustained low disease activity or remission every 6 months.1
Increased life expectancy means that more people will develop RA in the future and thus need treatment and follow-up. Even as treatment is generally becoming more effective and better tolerated, many countries experience an unmet demand for rheumatologists coinciding with a demand for greater cost-effectiveness. Thus, different alternatives to conventional outpatient physician-led follow-up have been investigated, for example, to allow nurse-led consultations to become embedded in the follow-up of RA in daily clinical practice.2–5 Furthermore, it has been recommended that nurses should participate in disease management to improve patient-preferred outcomes, such as fatigue, throughout the disease course.6 It has also been recommended that patients with RA should have access to a nurse throughout the course of their disease to improve their understanding and disease management and for enhanced satisfaction.6 Studies have shown that nurse-led care may contribute to promote patients’ self-management skills and thus their level of self-efficacy.7 The increasing involvement of nurses in the follow-up of patients with RA has been recognised and described in recent European treatment recommendations.1 The essential question remains, however, whether the involvement of nurses in the follow-up care can achieve the same degree of disease control, indicated by DAS-28, as when the follow-up is performed by physicians alone. In addition, it is interesting whether nurses can contribute to enhanced patient satisfaction and self-efficacy. These questions need a systematic evaluation of the evidence. Hence, our objective was to conduct a systematic review and meta-analysis to investigate the efficacy of embedded nurse-led versus conventional physician-led follow-up in the treat to target strategy in RA.
Methods
Search strategy
A systematic literature search was performed in the following electronic databases: MEDLINE (Ovid), Embase (Ovid), the Cochrane Central Register of Controlled Trials (CENTRAL), PsycINFO (ProQUEST), CINAHL (EBSCO), Web of Science (Thomson Reuters) and Scopus (Elsevier). There was no time limit back in time. The search ended in December 2016. We searched for all randomised controlled trials (RCTs) using the methodological filter for RCTs outlined in the Cochrane Handbook8; variations of this filter, or other validated filters, were used for other databases.
A search for possible ongoing trials was performed through ClinicalTrials.gov, ISRCTN registry, UK Clinical, Research Network Study Portfolio and MRC Clinical Trials Unit. Dissertations and theses were located through ProQuest Dissertations & Theses Global. Reference lists of relevant articles and conference proceedings were searched manually, and the included studies were also made subject to citation analysis in Web of Science. No language restrictions were imposed, and databases were searched from inception date and forward. Protocol of the searches in the different databases can be found as online supplementary file 1 .
rmdopen-2017-000481supp001.docx (35.5KB, docx)
Selection of studies
All the included studies were RCTs reporting on the effect of nurse-led follow-up in managing disease control in RA compared with physician-led follow-up. Patients with RA were diagnosed according to the American College of Rheumatology 1997/2010 criteria.9 10 This implied nurse-led follow-up of outpatients with RA in hospitals where nurses performed assessment of tender and swollen joints, evaluated blood samples and monitored the medical treatment in order to assess the patients’ disease activity.
Outcome measures
The primary outcome was disease activity indicated by Disease Activity Score (DAS)-28 C reactive protein (CRP) or erythrocyte sedimentation rate (ESR) or DAS-44.11 12 The DAS-28 CRP/ESR combines single measures into an overall continuous measure of disease activity in RA and includes a 28 tender and swollen joint count together with either CRP or ESR and a patient global assessment of disease activity.12 DAS-44 includes a 44-swollen joint count, CRP/ESR and a patient global assessment.12
Secondary outcomes were patient satisfaction, physical disability, quality of life, fatigue and self-efficacy.
Data extraction and management
Each potentially relevant study was independently reviewed by two reviewers (all studies were reviewed by ADT and by JP, BAE or IKR). Disagreement was resolved through discussion until consensus was obtained. From each selected trial, the following data were collected: general study information (author information, affiliation, country and funding) number of randomised individuals for each treatment group, characteristics of the participants in the intervention and control groups, type of intervention, type of comparator, follow-up times (ie, longest follow-up period), disease activity, level of physical disability, level of fatigue, self-efficacy and patient satisfaction. We also extracted the number of subjects who withdrew from the study (dropouts) for each treatment group. Data were extracted using the web-based software platform Covidence (www.covidence.org).
Assessment of risk of bias and overall quality
We used the Cochrane 'Risk of Bias' tool13 to assess bias in six domains: random sequence generation, allocation concealment, blinding to participants, blinding to assessment, withdrawals (attrition bias) and selective outcome reporting.14 Risk of bias was assessed at the level of each outcome, independently by two reviewers (ADT and by JP, BAE or IKR). In addition to risk of bias, the ‘Grading of Recommendations Assessment, Development and Evaluation’ (GRADE) was used to evaluate the total body of evidence by further assessment of three domains: inconsistency (the variation across studies), indirectness (ie, differences in patient population) and imprecision (95% confidence interval (CI)).15
Statistical methods
Heterogeneity was tested using the χ2 test, and inconsistency was evaluated via the I2 index, which expresses the percentage of total variation across studies.16 Data were entered into Review Manager 5.3 (http://tech.cochrane.org), and a meta-analysis was performed as a random effect model by default, because we expected the study populations to vary regarding factors that might influence our primary outcome, DAS-28, that is, regarding underlying treatment.17 All outcomes were continuous. Disease activity was measured by DAS-28 in all studies allowing change from baseline until end of follow-up to be estimated by calculating mean difference (MD) with 95% CI. All secondary outcomes (patient satisfaction, self-efficacy, physical activity and fatigue) were measured on different scales across the studies (table 1) and were thus estimated by standard mean difference (SMD) with 95% CI. When outcomes within the same concept are measured on different scales, SMD treats effect as a unit less measure by dividing the difference in mean changes from baseline until the end of follow-up by the pooled SD.18
Table 1.
Description of included studies
| Study ID/year | N/duration* | Baseline characteristics | Intervention/comparison | |||
| Nurse-led follow-up |
Physician-led follow-up |
Nurse-led follow-up |
Physician-led follow-up | Included outcomes | ||
| Hill/2003 (3) | 80/12 | RA, 79% ♀, mean age 57 (SD 48.1), DD† 12, mean DAS-28: N/A | RA, 78% ♀, mean age 57 (SD 49.3), DD 17, mean DAS-28: N/A | FU by rheum. nurse, week: 0, 4, 12 24, 36, 48. AT:30 min CER:>20 |
FU by rheumatologist week 0, 4, 12 24, 36, 48. AT: 30 min CER: >2 |
PD (AIMS), Satisfaction (LSQ) |
| Koksvig/2013 (21) | 68/21 | % RA: 54, 71% ♀, mean age 49 (SD 13.3), DD 8, mean DAS-28: 3.05 (SD 0.94) | % RA: 52, 64% ♀, mean age 51 (SD 12.6), DD 9, mean DAS-28 2.87 (SD 0.79) | FU by rheum. nurse once a year. AT: 30 min CER: >10 |
FU by rheumatologist once a year. AT: 30 min CER: N/A |
DAS-28 Fatigue (VAS-fatigue) Satisfaction (LSQ) QoL (SF-36) PD (SF-36) |
| Larsson/2014 (22) | 107/21 | % RA: 53, 55% ♀, mean age 55 (SD 12.3), DD 17.3, mean DAS-28: 2.43 (SD 0.58) | % RA: 70, 56% ♀, mean age 55.8 (SD 13.2), DD 16.2, mean DAS-28 2.53 (SD 0.64) | FU by rheum. nurse once a week 26 weeks AT: 30 min CER: >20 |
FU by rheumatologist weeks 26 and 56 AT: 30 min CER: not described |
DA (DAS-28) PD (HAQ) Satisfaction (NRS) |
| Ndosi/2014 (23) | 181/12 | RA, 73.6% ♀, mean age 60.2 (SD 11.26), DD 9.6, mean DAS-28: 3.65 (SD 1.24) | RA, 74.4% ♀, mean age 57.3 (SD 12.2), DD 10.21, mean DAS-28 3.89 (SD 1.54) | FU by rheum nurse, week 13, 26, 39, 52 AT: 30 min CER: >10 |
FU by rheumatologist week 13, 26, 39, 52 AT: 30 min CER: median of 9 at consultant level |
DA (DAS-28) PD (HAQ) QoL (RAQoL) FRAQoLe (Fatigue VAS) Satisfaction (LSQ) Self-efficacy (ASES) |
| Primdahl/ 2012 and 2014 Sørensen/2014 (2,19,20) | 287/24 | RA, 51.5% ♀, mean age 60.8 (SD 12.4), DD 9.6, mean DAS-28: 2.1 (SD 0.51) | RA, 51% ♀, mean age 61.1 (SD 11.2), DD 7, mean DAS-28: 2.2 (SD 0.55) | FU by rheum nurse every 3 months. AT: 30 min CER: rheum. nurse, trained in joint assessment |
FU by rheumatologist with various frequency based on doctors judgement AT: 20–30 min CER: junior or senior |
DA (DAS-28) PD (HAQ) QoL (EQ-5D) Fatigue (Fatigue VAS) Satisfaction (LSQ) Self-efficacy (ASE) |
*Follow-up time (months).
†DiseaseDisease duration (DD), years.
FU, follow-up; AT, allocation time; CER, clinical experience within rheumatology; DAS28, Disease Activity Score-28; PD, physical disability; AIMS, Arthritis Impact Measurement Scale; ; LSQ, Leeds Satisfaction Questionnaire; QoL, quality of life; SF-36, Short-Form 36; NRS, Numeric Rating Scale; RAQoL, rheumatoid arthritis quality of life; ASES, Arthritis Self-Efficacy Scale; ; ; EQ-5D, European Quality of Life-5 dimensions; ; HAQ, Health Assessment Questionnaire
Stratified analyses were performed according to the duration of the observation period (12 months vs >12 months). Forest plots were used to assess the results. A two-sided p value<0.05 was considered to be statistically significant.
Results
Description of studies
A total of 1052 studies were identified, and seven RCTs representing five studies were finally included in the meta-analysis (figure 1).2 3 19–23 Three of the included studies comprised data from the same study cohort, the AMBRA (AMBulant behandling af Reumatoid Artrit – Outpatient care of established RA) study.2 19 20 Nurses in the included studies were described as: nurses, rheumatology nurses, clinical nurse specialists or experienced rheumatology nurses trained in joint assessment (table 1). Most studies included patients with RA; however, one study included patients with RA, ankylosing spondylitis (AS), psoriatic arthritis (PsA) and juvenile idiopathic arthritis or undifferentiated polyarthritis,21 and one study included patients with RA and PsA.22 The percentages of patients with RA in these two studies were 53% and 62%, respectively. Due to the relatively low number of studies included in the meta-analysis, we chose to depart from our protocol and included these studies in the primary analysis in order to provide sufficient power to the meta-analysis; instead we downgraded the quality of evidence for indirectness according to the GRADE methodology24 and performed a sensitivity analysis without these two studies.21 22 Only one study included patients with a DAS-28 ESR >3.2.23 In all studies, the nurse-led follow-up was supervised by physicians.
Figure 1.

Flow diagram showing the selection of studies.
One study described the mean change in DAS-28 graphically3 but did not provide data for the meta-analysis. We contacted the authors, but unfortunately, data were no longer available.
Patient satisfaction was measured on both the Leeds Satisfaction Scale25 and a visual analog scale (VAS) confidence and satisfaction scale.26
One study assessed physical disability by the Arthritis Impact Measurement Scale.27 The remaining studies used the Health Assessment Questionnaire for assessment of physical disability.28
Quality of life was assessed by the SF-36 (mental part),29 the RA quality of life scale30 and the European Quality of Life-5 Dimensions.31 Fatigue was measured by a VAS fatigue scale,32 except in one study,3 where it was measured in minutes, and these data were not included in the analysis. Self-efficacy was measured by the Arthritis Self-Efficacy Scale33 and two studies also reported data from the Rheumatoid Arthritis Self-Efficacy Questionnaire (RASE).2 34 Results from the RASE were, however, not used in the meta-analyses. A description of the included studies is shown in table 1, and a list of excluded studies can be found in online supplementary file 2 .
rmdopen-2017-000481supp002.docx (25.3KB, docx)
Critical appraisal
All included studies were RCTs and. in general, the quality was moderate to low. An evidence table showing the grading of the evidence for each outcome is shown in online supplementary file 3 . None of the studies were double blinded due to the type of intervention. Two of the included studies had ensured assessor blinding of the assessment of disease activity,2 23 and all but one22 performed intention-to-treat analyses. Risk of bias assessments across all outcomes are summarised in figure 2.
Figure 2.

Risk of bias for each reported outcome across the included studies.
rmdopen-2017-000481supp003.docx (29KB, docx)
Effect of nurse-led versus physician-led follow-up
Disease activity
Data concerning disease activity were based on 534 patients in four studies that all reported a DAS-28 CRP/ESR.2 21–23 There was no statistically or clinically significant difference in disease activity between nurse-led versus physician-led follow-up after 1 year (MD −0.07 (95% CI −0.23 to 0.09)) (figure 3.1). The quality of the evidence was moderate (online supplementary file 3). Leaving out the two studies that included patients with other types of inflammatory arthritis (IA) than RA21 22 did not alter the estimates (−0.15 (95% CI −0.40 to 0.10); however. it did, as expected, increase imprecision.35
Figure 3.
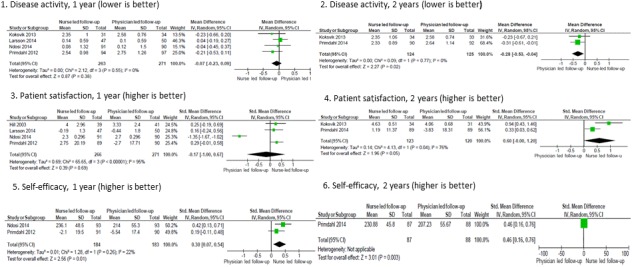
Forest plots showing pooled mean and standard mean differences (SMDs) for disease activity, patient satisfaction and self-efficacy in trials comparing nurse-led with physician-led follow-up among patients with rheumatoid arthritis (RA) after 1 and 2 years. Disease activity measured by DAS-28 CRP/ESR, patient satisfaction measured by Leeds Satisfaction Questionnaire or NRS Satisfaction Scale and self-efficacy measured by Arthritis Self-Efficacy Scale (ASES) and RASE. DAS-28, Disease Activity Score; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; RASE, Rheumatoid Arthritis Self-Efficacy Questionnaire.
Two of the studies addressed the effect after 2 years.2 21 These studies included a total of 249 patients, and both included patients with low disease activity or in remission. A statistically but not clinically relevant difference was found in favour of nurse-led follow-up (MD −0.28 (95% CI −0.53 to 0.04)). Furthermore, the CIs were wide including both no difference (0.04) and nurse-led follow-up being more effective than physician-led follow-up (−0.53) and thus, the quality of the evidence was downgraded due to imprecision35 (figure 3.2) (online supplementary file 3). The between variance was low with I2 values of 0% at both 1-year and 2-year follow-ups.
In the study that could not be included in the meta-analysis due to missing data,3 no statistically significant difference was found between the two groupssupporting the overall estimate of the meta-analysis.
Patient satisfaction
Data concerning patient satisfaction after 1 year was based on 537 patients from four different studies.2 3 22 23 No statistically significant difference was found in patients’ satisfaction between nurse-led versus physician-led follow-up (SMD −0.17 (95% CI −1.0 to 0.67)) (figure 3.3). Heterogeneity was high for this outcome (I2=95%). When leaving out the one study that included patients with a baseline DAS-28 >3.2,23 no heterogeneity was found (I2=0%), and a small statistically significant difference in favour of nurse-led follow-up was seen (SMD 0.24 (95% CI 0.03 to 0.45)). We performed the analyses again without the studies that included patients with other types of IA.22 This did not alter the overall estimates (−0.27 95% CI −1.38 to 0.83).
At 2-year follow-up, a statistically significant difference in patient satisfaction was seen in favour of nurse-led follow-up (SMD: 0.60 (95% CI 0.00 to 1.20)). However, only two studies reported data from 2-year follow-up,2 21 and heterogeneity was high (I2=76%) (figure 3.4). When omitting the study with other types of patients with IA,21 the effect size decreased from strong to moderate (0.33 (95% CI 0.03 to 0.62)). The quality of evidence was low due to heterogeneity and imprecision (online supplementary file 3).
Self-efficacy
Data on self-efficacy after 1 year were based on a total of 367 patients from two studies.2 23 After 1 year, a small but statistically significant difference was seen in favour of nurse-led follow-up (SMD: 0.30 (95% CI 0.07 to 0.53)) (figure 3.5). Heterogeneity was low (I222%), and the quality of evidence was moderate (online supplementary file 3). Only one study assessed self-efficacy after 2 years.2 However, the results stayed more or less the same but became more imprecise (SMD: 0.46 (95% CI 0.16 to 0.76)) (figure 3.6).
Other secondary outcomes
Common for the remaining three secondary outcomes (physical disability, fatigue and quality of life) was that very small non-statistically significant differences were seen between the two groups. Forest plots for these outcomes can be found in online supplementary file 4 .
rmdopen-2017-000481supp004.docx (209.5KB, docx)
Discussion
In this meta-analysis, we found no differences in the efficacy to achieve or sustain disease control by embedded nurse-led follow-up compared with conventional physician-led follow-up in patients with RA with low disease activity or in remission.
To the best of our knowledge, this is the first meta-analysis evaluating the effect of nurse-led care in RA. A recent systematic review found nurse-led care to be effective and safe. However, the authors decided not to carry out a meta-analysis with heterogenerity as their argument.36 A previous systematic review from 2011 was inconclusive due to lack of power (only few studies could provide data for the primary outcome).37
We have shown that for most outcomes heterogenerity was generally low and further, the body of evidence has markedly improved since 2011. This has enabled us to include more relevant studies and allowed us to perform a useful meta-analysis. By calculating SMDs when outcomes within the same concept were measured on different scales18 and by using random effect model by default, we have taken into account the possible variations among studies.17
Unlike the previous studies, we excluded the multicentre study by Tijhuis et al38 as it compared inpatient care with nurse-led follow-up, while our study compared nurse-led with physician-led follow-up for outpatients. We also excluded the study of Ryan et al39 as it dealt with drug monitoring rather than monitoring of disease activity.
Our findings is consistent with findings within other chronic diseases, that is, a Cochrane review regarding the benefits from adding a nurse specialist to routine care in the management of type 1 or type 2 diabetes,40 an RCT regarding the management of childhood asthma by a paediatrician or asthma nurse41 and a Cochrane review regarding nurse-led versus physician-led in adult asthma care.42
Apart from disease control, nurse-led follow-up may contribute with additional value in the overall treatment and care in RA. Nurse-led follow-up provides the opportunity to use the scarce rheumatology resources in a more efficient way by offering patients different types of follow-up throughout their disease course. Rheumatologists will therefore be able to focus on diagnostics, medical prescription and treatment of patients with continuing high disease activity or comorbidities.
In the past years, we have seen an increasing tendency to involve nurses in the care and control of disease activity in patients with RA.6 43 44 Based on the additional professional perspectives nurses add to RA treatment and care, consideration should be given to involve them in routine follow-up, independently of whether rheumatologist resources are scarce or not. Studies have shown that patients value nurse-led follow-up, because it provides continuity of the healthcare provider, makes patients feel secure and makes them feel that they have easy access to help.19 45–48 Furthermore, a mixed-method study found that nurses focus more on socioemotional issues, whereas physicians tend to be more task focused.49 Nurses also focus on supporting the patients to manage life with their disease, which may explain why nurses’ support may increase the patients’ self-efficacy.6
Still, it is important to point out that, in most of the included studies, nurses had many years of experience with rheumatology (10+ years). This indicates that less-experienced nurses will need proper training and supervision by both rheumatologists and senior nurses before they can take over some of the follow-up consultations in RA and undertake extended roles such as examinations of the joints and identification of signs of flare-ups and insufficient pharmacological treatment.
Strengths and limitations
The internal validity of our meta-analysis was ensured by the application of a systematic and strict methodology throughout the whole review process. An experienced research librarian (TF) undertook a systematic, thorough search of the literature to identify all studies meeting the inclusion criteria for this review. A priori, our review protocol was made permanently available online (http://www.crd.york.ac.uk/PROSPERO/, PROSPERO id no. 42015026151), allowing other researchers to check that the review has been performed according to the protocol. The general quality of the evidence of the included studies was moderate. By using the well-recommended GRADE methodology to assess the overall quality of the studies, we ensured a systematic and transparent process of the review.35 In this connection, it is important to underline that in general the included studies were well conducted and of high quality. However, the nature of the intervention renders blinding, which was not possible in the included studies. Thus, the quality of the evidence will a priori be downgraded due to the possibility of information bias.35 Despite this, we have high confidence that the true effect was likely to be close to the estimated effect.35 However, our study has some limitations that merit further discussion. The meta-analytic approach creates an overview that can ease interpretation. However, although our selection criteria were strict, the interventions in the included studies were not exactly the same with respect to the frequency of follow-up and supervision provided by rheumatologists to the nurses. In addition, the content in the nurse-led and physician-led follow-ups is not described in detail in the included studies and may vary based on local culture and legislation.
Furthermore, it can be regarded as a limitation that we did not predefine factors of importance regarding safety, that is, with respect to reported drug adverse events and that we did not include the frequency of follow-up as an outcome in order to be able to control for these variables.
Variability in study populations with respect to disease activity is likely to be the main cause for the high interstudy heterogeneity discovered in the outcome for patient satisfaction.
All the included studies had dropouts <10%. Different reasons for dropouts were given (including comorbidity, death and non-compliance). All but one of the included studies22 did, however, use intention-to-treat analysis, by which they took a possible selection bias into account. Only one study included patients with RA and with high disease activity.23 Thus, it remains unresolved whether nurse-led follow-up is applicable in patients with high or uncontrolled disease activity. In recent years, the prevalence of patients with low disease activity or remission has, however, increased markedly due to the improved pharmacological treatment and the implementation of the treat to target strategy. Hence, overall, approximately two-thirds of the patients with RA in daily clinical practice will fall into this category, and thus support this type of intervention.1 Finally, it must be regarded a limitation that some of the included studies included patients with other diagnoses than RA.21 22 In order to take this into account, we have downgraded the evidence quality due to indirectness in line with the GRADE methodology24 and have provided sensitivity analysis excluding these studies. In conclusion, after 1 year, no clinical or significant differences were found in the efficacy of embedded nurse-led follow-up compared with physician-led follow-up on disease activity, indicated by DAS-28 in RA patients with low disease activity or remission.
Given that the quality of the evidence was low for disease activity measured after 2 years, we recommended that nurse-led follow-up is always implemented in tandem with physicians. However, based on our study, we conclude that it is feasible to involve nurses in disease management in patients with RA with low disease activity or in remission.
Acknowledgments
All contributors meet the criteria for authorship.
Acknowledgments
All contributors meet the criteria for authorship.
Footnotes
Contributors: All authors fulfil the ICMJE authorship criteria, and all have read and approved the final draft.
Funding: No specific funding was received from any funding bodies in the public, commercial or non-profit sectors to carry out the work described in this manuscript.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: This study involved only published reports and no unpublished information. No database was used for this study
References
- 1.Smolen JS, Breedveld FC, Burmester GR, et al. . Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis 2016;75:3–15. 10.1136/annrheumdis-2015-207524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Primdahl J, Sørensen J, Horn HC, et al. . Shared care or nursing consultations as an alternative to rheumatologist follow-up for rheumatoid arthritis outpatients with low disease activity--patient outcomes from a 2-year, randomised controlled trial. Ann Rheum Dis 2014;73:357–64. 10.1136/annrheumdis-2012-202695 [DOI] [PubMed] [Google Scholar]
- 3.Hill J, Thorpe R, Bird H. Outcomes for patients with RA: a rheumatology nurse practitioner clinic compared to standard outpatient care. Musculoskeletal Care 2003;1:5–20. 10.1002/msc.35 [DOI] [PubMed] [Google Scholar]
- 4.Lillicrap M, Otter S, Haq I. Rising to the challenge: rheumatology can lead in multi-professional education and training globally in the 21st century. Rheumatology 2016;55:1932–7. 10.1093/rheumatology/kev430 [DOI] [PubMed] [Google Scholar]
- 5.Emamifar A, van Bui Hansen MH, Jensen Hansen IM. The ratio of nurse consultation and physician efficiency index of senior rheumatologists is significantly higher than junior physicians in rheumatology residency training: a new efficiency measure in a cohort, exploratory study. Medicine 2017;96:e6601 10.1097/MD.0000000000006601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Eijk-Hustings Y, van Tubergen A, Boström C, et al. . EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Ann Rheum Dis 2012;71:13–19. 10.1136/annrheumdis-2011-200185 [DOI] [PubMed] [Google Scholar]
- 7.Bandura A. Social foundations of thought and action.A social cognitive theory. 1st ed New Jersey: Prentice-Hall, Inc.: Englewood Cliffs, 1986. [Google Scholar]
- 8.Lefebvre C, Manheimer E, Glanville J. Chapter 6. searching for studies In: Higgins J, Green S, eds The Cochrane Handbook, 2011. [Google Scholar]
- 9.Aletaha D, Neogi T, Silman AJ, et al. . 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum 20102010 Sep;;62:2569–81. 10.1002/art.27584 [DOI] [PubMed] [Google Scholar]
- 10.Arnett FC, Edworthy SM, Bloch DA, et al. . The American Rheumatism Association 1987 revised criteria for the classification of Rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. 10.1002/art.1780310302 [DOI] [PubMed] [Google Scholar]
- 11.Prevoo ML, van 't Hof MA, Kuper HH, et al. . Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8. 10.1002/art.1780380107 [DOI] [PubMed] [Google Scholar]
- 12.Anderson JK, Zimmerman L, Caplan L, et al. . Measures of rheumatoid arthritis disease activity: patient (PtGA) and provider (PrGA) Global Assessment of Disease Activity, Disease Activity score (DAS) and disease activity score with 28-Joint counts (DAS28), Simplified Disease Activity Index (SDAI), Clinical disease activity index (CDAI), Patient activity score (PAS) and patient activity Score-II (PASII), Routine Assessment of Patient Index Data (RAPID), Rheumatoid Arthritis Disease Activity Index (RADAI) and rheumatoid Arthritis Disease Activity Index-5 (RADAI-5), Chronic Arthritis systemic index (CASI), Patient-Based disease activity score with ESR (PDAS1) and Patient-Based disease activity score without ESR (PDAS2), and mean overall index for rheumatoid Arthritis (MOI-RA). Arthritis Care Res 2011;63 Suppl 11(Suppl 11):S14–36. 10.1002/acr.20621 [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Altman DG, Gøtzsche PC, et al. . The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins J, Altman D. Chapter 8. assessing risk of bias in included studies In: Higgins J, Green S, eds Cochrane handbook for systematic reviews of intervention, 2011. [Google Scholar]
- 15.Guyatt GH, Oxman AD, Vist GE, et al. . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, Thompson SG, Deeks JJ, et al. . Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deeks J, Higgins JPT, Altman DC. Identifying and measuring heterogenity In: Higgins J, Green S, eds . 1, 2011.
- 18.Normand SL, Formulating Meta-analysis:. Evaluating, combining, and reporting. Stat Med 1999;18:321–59. [DOI] [PubMed] [Google Scholar]
- 19.Primdahl J, Wagner L, Holst R, et al. . The impact on self-efficacy of different types of follow-up care and disease status in patients with rheumatoid arthritis--a randomized trial. Patient Educ Couns 2012;88:121–8. 10.1016/j.pec.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 20.Sørensen J, Primdahl J, Horn HC, et al. . Shared care or nurse consultations as an alternative to rheumatologist follow-up for rheumatoid arthritis (RA) outpatients with stable low disease-activity RA: cost-effectiveness based on a 2-year randomized trial. Scand J Rheumatol 2015;44:13–21. 10.3109/03009742.2014.928945 [DOI] [PubMed] [Google Scholar]
- 21.Koksvik HS, Hagen KB, Rødevand E, et al. . Patient satisfaction with nursing consultations in a rheumatology outpatient clinic: a 21-month randomised controlled trial in patients with inflammatory arthritides. Ann Rheum Dis 2013;72:836–43. 10.1136/annrheumdis-2012-202296 [DOI] [PubMed] [Google Scholar]
- 22.Larsson I, Fridlund B, Arvidsson B, et al. . Randomized controlled trial of a nurse-led rheumatology clinic for monitoring biological therapy. J Adv Nurs 2014;70:164–75. 10.1111/jan.12183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ndosi M, Lewis M, Hale C, et al. . The outcome and cost-effectiveness of nurse-led care in people with rheumatoid arthritis: a multicentre randomised controlled trial. Ann Rheum Dis 2014;73:1975–82. 10.1136/annrheumdis-2013-203403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guyatt GH, Oxman AD, Kunz R, et al. . GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol 2011;64:1303–10. 10.1016/j.jclinepi.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 25.Hill J, Bird HA, Hopkins R, et al. . Survey of satisfaction with care in a rheumatology outpatient clinic. Ann Rheum Dis 1992;51:195–7. 10.1136/ard.51.2.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kirwan JR, Mitchell K, Hewlett S, et al. . Clinical and psychological outcome from a randomized controlled trial of patient-initiated direct-access hospital follow-up for rheumatoid arthritis extended to 4 years. Rheumatology 2003;42:422–6. 10.1093/rheumatology/keg130 [DOI] [PubMed] [Google Scholar]
- 27.Meenan RF, Gertman PM, Mason JH. Measuring health status in arthritis. the arthritis impact measurement scales. Arthritis Rheum 1980;23:146–52. [DOI] [PubMed] [Google Scholar]
- 28.Fries JF, Spitz P, Kraines RG, et al. . Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137–45. 10.1002/art.1780230202 [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 30.de Jong Z, van der Heijde D, McKenna SP, et al. . The reliability and construct validity of the RAQoL: a rheumatoid arthritis-specific quality of life instrument. Br J Rheumatol 1997;36:878–83. 10.1093/rheumatology/36.8.878 [DOI] [PubMed] [Google Scholar]
- 31.Hurst NP, Kind P, Ruta D, et al. . Measuring health-related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D). Br J Rheumatol 1997;36:551–9. 10.1093/rheumatology/36.5.551 [DOI] [PubMed] [Google Scholar]
- 32.Hewlett S, Hehir M, Kirwan JR. Measuring fatigue in rheumatoid arthritis: a systematic review of scales in use. Arthritis Rheum 2007;57:429–39. 10.1002/art.22611 [DOI] [PubMed] [Google Scholar]
- 33.Lorig K, Chastain RL, Ung E, et al. . Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum 1989;32:37–44. 10.1002/anr.1780320107 [DOI] [PubMed] [Google Scholar]
- 34.Primdahl J, Wagner L, Hørslev-Petersen K. Self-efficacy in rheumatoid arthritis: translation and test of validity, reliability and sensitivity of the danish version of the rheumatoid Arthritis Self-Efficacy Questionnaire (RASE). Musculoskeletal Care 2010;8:123–35. 10.1002/msc.172 [DOI] [PubMed] [Google Scholar]
- 35.Balshem H, Helfand M, Schünemann HJ, et al. . GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–6. 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 36.Garner S, Lopatina E, Rankin JA, et al. . Nurse-led care for patients with Rheumatoid Arthritis: a Systematic Review of the effect on Quality of Care. J Rheumatol 2017;44:757–65. 10.3899/jrheum.160535 [DOI] [PubMed] [Google Scholar]
- 37.Ndosi M, Vinall K, Hale C, et al. . The effectiveness of nurse-led care in people with rheumatoid arthritis: a systematic review. Int J Nurs Stud 2011;48:642–54. 10.1016/j.ijnurstu.2011.02.007 [DOI] [PubMed] [Google Scholar]
- 38.Tijhuis GJ, Kooiman KG, Zwinderman AH, et al. . Validation of a novel satisfaction questionnaire for patients with rheumatoid arthritis receiving outpatient clinical nurse specialist care, inpatient care, or day patient team care. Arthritis Rheum 2003;49:193–9. 10.1002/art.10994 [DOI] [PubMed] [Google Scholar]
- 39.Ryan S, Hassell AB, Lewis M, et al. . Impact of a rheumatology expert nurse on the wellbeing of patients attending a drug monitoring clinic. J Adv Nurs 2006;53:277–86. 10.1111/j.1365-2648.2006.03725.x [DOI] [PubMed] [Google Scholar]
- 40.Loveman E, Royle P, Waugh N. Specialist nurses in diabetes mellitus. Cochrane Database Syst Rev 2003;2:CD003286. 10.1002/14651858.CD003286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamps AW, Brand PL, Kimpen JL, et al. . Outpatient management of childhood asthma by paediatrician or asthma nurse: randomised controlled study with one year follow up. Thorax 2003;58:968–73. 10.1136/thorax.58.11.968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kuethe MC, Vaessen-Verberne AA, Elbers RG, et al. . Nurse versus physician-led care for the management of asthma. Cochrane Database Syst Rev 2013;22:CD009296, CD009296. [DOI] [PubMed] [Google Scholar]
- 43.Starz TW, Young B. The rheumatology nurse. The Rheumatologist 2016:11–12. [Google Scholar]
- 44.Solomon DH, Fraenkel L, Lu B, et al. . Comparison of Care provided in Practices with nurse practitioners and physician assistants Versus Subspecialist Physicians only: a Cohort Study of Rheumatoid Arthritis. Arthritis Care Res 2015;67:1664–70. 10.1002/acr.22643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bala SV, Samuelson K, Hagell P, et al. . The experience of care at nurse-led rheumatology clinics. Musculoskeletal Care 2012;10:202–11. 10.1002/msc.1021 [DOI] [PubMed] [Google Scholar]
- 46.Arthur V, Clifford C. Rheumatology: a study of patient satisfaction with follow-up monitoring care. J Clin Nurs 2004;13:325–31. 10.1046/j.1365-2702.2003.00872.x [DOI] [PubMed] [Google Scholar]
- 47.Arvidsson SB, Petersson A, Nilsson I, et al. . A nurse-led rheumatology clinic's impact on empowering patients with rheumatoid arthritis: A qualitative study. Nurs Health Sci 2006;8:133–9. 10.1111/j.1442-2018.2006.00269.x [DOI] [PubMed] [Google Scholar]
- 48.Primdahl J, Wagner L, Hørslev-Petersen K. Being an outpatient with rheumatoid arthritis--a focus group study on patients' self-efficacy and experiences from participation in a short course and one of three different outpatient settings. Scand J Caring Sci 2011;25:394–403. 10.1111/j.1471-6712.2010.00854.x [DOI] [PubMed] [Google Scholar]
- 49.Vinall-Collier K, Madill A, Firth J. A multi-centre study of interactional style in nurse specialist- and physician-led Rheumatology clinics in the UK. Int J Nurs Stud 2016;59:41–50. 10.1016/j.ijnurstu.2016.02.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2017-000481supp001.docx (35.5KB, docx)
rmdopen-2017-000481supp002.docx (25.3KB, docx)
rmdopen-2017-000481supp003.docx (29KB, docx)
rmdopen-2017-000481supp004.docx (209.5KB, docx)


