Publisher's Note: There is an Inside Blood Commentary on this article in this issue.
Key Points
R-CHOP results in excellent response rates and durable remissions in NLPHL.
Abstract
Nodular lymphocyte Hodgkin lymphoma (NLPHL) is a rare disease for which the optimal therapy is unknown. We hypothesized that rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) could decrease rates of relapse and transformation. We retrospectively reviewed patients with NLPHL diagnosed between 1995 and 2015 confirmed by central pathologic review. Fifty-nine had sufficient treatment and follow-up data for analysis. We described progression-free survival (PFS), overall survival (OS), and histologic transformation according to treatment strategy and explored prognostic factors for PFS and OS. The median age at diagnosis was 41 years; 75% were male, and 61% had a typical growth pattern. Twenty-seven patients were treated with R-CHOP with an overall response rate of 100% (complete responses 89%). The median follow-up was 6.7 years, and the estimated 5- and 10-year PFS rates for patients treated with R-CHOP were 88.5% (95% confidence interval [CI], 68.4% to 96.1%) and 59.3 (95% CI, 25.3% to 89.1%), respectively. Excluding patients with histologic transformation at diagnosis, the 5-year cumulative incidence of histologic transformation was 2% (95% CI, 87% to 100%). No patient treated with R-CHOP experienced transformation. A high-risk score from the German Hodgkin Study Group was adversely prognostic for OS (P = .036), whereas male sex and splenic involvement were adversely prognostic for PFS (P = .006 and .002, respectively) but not OS. Our data support a potential role for R-CHOP in patients with NLPHL. Larger prospective trials are needed to define the optimal chemotherapy regimen.
Introduction
Nodular lymphocyte–predominant Hodgkin lymphoma (NLPHL) is a rare type of lymphoma with an estimated incidence of 0.2 per 100 000 and an estimated 550 new cases in the United States in 2016.1 In contrast to classical Hodgkin lymphoma (cHL), NLPHL is characterized by indolent behavior and CD20 positive lymphocyte–predominant (LP) cells.2 Although NLPHL was historically viewed as being analogous to follicular lymphoma, gene expression profiling of microdissected LP cells indicates molecular similarity to T-cell-rich B-cell lymphoma (TCRBCL) and cHL despite differences in immunohistochemistry.3 In comparison with cHL patients, NLPHL patients have both a higher rate of delayed relapses and a transformation to aggressive B-cell lymphomas of TCRBCL or diffuse large-B-cell lymphoma (DLBCL). Investigators from the British Columbia Cancer Agency (BCCA) reported that 14% of 95 NLPHL patients experienced transformation after a median follow-up of 8.1 years, with a 20-year actuarial risk of transformation of 30%. Five of the 13 patients with transformation were treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP), and 6 patients received R-CHOP or other rituximab-containing chemotherapy and then underwent an autologous stem cell transplant (ASCT). The 10-year progression-free survival (PFS) and overall survival (OS) rates were 52% and 62%, respectively.4 By comparison the Mayo Clinic group identified a lower rate of transformation of 8% at an earlier median time point of 2.9 years in 222 NLPHL patients who were followed; 9 of the 17 patients who developed transformation were treated with R-CHOP or CHOP, and 2 patients underwent an ASCT with a similar 5-year OS of 76%.5 Clinical features including tumor size that was >5 cm and splenic involvement among patients with advanced stage have been associated with increased risk for transformation,6 and recent data indicate histopathologic variants may also carry increased risk.7 Building on this, the German Hodgkin Study Group (GHSG) defined a clinicopathologic prognostic score combining variant growth pattern, serum albumin of <4 g/dL, and male sex to stratify patients in 3 risk groups: patients with all 3 factors had the highest risk of disease relapse, approximately 22.3% at 5 years.8 Rituximab is established as being efficacious, but the optimal treatment of patients with newly diagnosed NLPHL remains difficult to define given the lack of randomized trials.9-11 Radiotherapy alone is often favored for early-stage disease, whereas data from the BCCA have shown potential for further improvement in PFS when utilizing a combined modality therapy (CMT) approach with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).12-15 The European Society for Medical Oncology and guidelines for advanced stage NLPHL suggest cHL-directed chemotherapy, whereas National Comprehensive Cancer Network guidelines suggest either cHL or B-cell non-Hodgkin lymphoma–directed chemotherapy regimens, including R-CHOP or rituximab plus cyclophosphamide, vincristine, and prednisone (R-CVP),16 though prospective data to support these recommendations are limited.17,18
In the hope of decreasing rates of relapse and transformation to aggressive B-cell lymphomas, our group started using R-CHOP for patients in need of systemic therapy.16,19,20 Some patients with early-stage disease were treated with R-CHOP at treating physician’s discretion. Here we present long-term outcomes of a large group of NLPHL patients treated at a single institution with a focus on the comparative outcomes of those treated with R-CHOP in relation to other treatment approaches.
Methods
Patients
Patient data were collected from our departmental new-patient referral database for initial appointments from 1995 to 2010 in accordance with the guidelines of a retrospective institutional review board–approved protocol. Responses to treatment were determined using 1999 International Working Group criteria.21 Departmental policy during the time period covered by the study was for 3 monthly reviews for the first 2 years following completion of primary therapy, then 6 monthly reviews thereafter. Surveillance CT scans were performed at the discretion of the treating physician. Slides of biopsy specimens were centrally reviewed by our lymphoma hematopathologists (A.R., L.J.M.) and the diagnosis of NLPHL was established using World Health Organization criteria.22 On the basis of criteria established by Fan and colleagues, tumor growth pattern was defined as typical or a morphologic variant, and the GHSG risk score was calculated.7,8 The diagnosis of DLBCL required the presence of sheets of large B cells replacing normal architecture. Patients with TCRLBCL had diffuse replacement with the large lymphoma cells representing <10% of all cells in the specimen, with the background cells being T cells (often CD8+, often with a cytotoxic immunophenotype) as well as histocytes.
Of 83 patients referred with external diagnoses of NLPHL to our center during the study period, 63 patients had NLPHL without transformation, 6 had NLPHL with transformation to DLBCL or TCRLBCL, 3 had alternative diagnoses, and 11 lacked sufficient immunophenotyping to confirm diagnosis. Thus, 69 patients who were seen at our institution and provided with treatment recommendations were confirmed to have NLPHL. Of these 69, 10 patients received treatment and follow-up elsewhere, leaving 59 patients who were included in the subsequent analysis.
Statistical methods
The focus of this study was to determine clinical outcomes (PFS and OS) according to primary treatment strategy. A secondary aim was exploratory analysis of candidate prognostic factors for PFS and OS. We defined PFS and OS as the time (in months) from the date of diagnosis to disease progression or death from any cause and as the time (in months) from the date of diagnosis to death from any cause, respectively. Patients alive at last follow-up were censored. Unadjusted event time distributions were estimated using the method of Kaplan and Meier,23 and groups were compared using the log-rank test. A Cox proportional hazard model24 was used to determine univariate associations between candidate prognostic factors and PFS and OS. Continuous variables were summarized using descriptive statistics such as median and range. Categorical variables were summarized using frequency tables and 95% confidence intervals. The homogeneity of response rate across groups was tested using the χ squared test. We used STATA (version 12.1; StataCorp, College Station, TX) to perform all statistical analyses. P values were 2-sided, and we considered values of <.05 to be significant.
Results
Patient characteristics and treatment
The median age at diagnosis was 41 (range, 16-73), and 50 (72%) were male. The majority of NLPHL patients (65%) had a typical histologic pattern (A or B) rather than a variant (non-A, B). Evidence of histologic transformation at diagnosis was present in 6 (9%) cases, DLBCL in 4, and TCRBCL in 2. Among patients without transformation, the distribution of GHSG risk scores was 14 (24%), 28 (48%), and 17 (29%) in low, intermediate, and high risk, respectively. Approximately two-thirds of patients had stage I/II disease (62%), and all patients had Eastern Cooperative Oncology Group (ECOG) performance status of ≤1. However, B symptoms, extranodal sites of involvement, low serum albumin, and spleen or bone marrow disease were infrequent (Table 1).
Table 1.
Baseline characteristics of patients with NLPHL
| Characteristic | Result | Data available |
|---|---|---|
| Median age at diagnosis (range), years | 41 (16-73) | 59 |
| Male (%) | 44 (75) | 59 |
| Histologic type (%) | 59 | |
| Typical (A/B) | 36 (61) | |
| Variant (non-A/B) | 19 (32) | |
| Histologic transformation at diagnosis | 4 (7) | |
| DLBCL | 3 (75) | |
| TCRBCL | 1 (25) | |
| Albumin <4.0 g/dL (%) | 7 (13) | 55 |
| GHSG score | 59 | |
| Low risk (0-1) | 14 (24%) | |
| Intermediate risk (2) | 28 (48%) | |
| High risk (3-4) | 17 (29%) | |
| Stage (%) | 59 | |
| I | 12 (20) | |
| II | 25 (42) | |
| III | 14 (24) | |
| IV | 8 (14) | |
| ECOG performance status (%) | 53 | |
| 0 | 33 (62) | |
| 1 | 20 (38) | |
| B symptoms (%) | 8 (14) | 59 |
| Extranodal sites of involvement (%) | 9 (15) | 59 |
| Spleen involved (%) | 8 (14) | 59 |
| Bone marrow involved (%) | 5 (8) | 59 |
The most common approach for patients with stage I/II disease was radiotherapy alone (31 to 40 Gy), delivered to 19 patients (43%). The remainder received chemotherapy ± rituximab, either with (n = 11, 25%) or without involved field radiation therapy (IFRT) (n = 7, 16%). Among the 22 patients with stage III/IV disease, 20 (65%) received chemotherapy ± rituximab as a single modality, and 2 received systemic therapy and radiation therapy (RT). Of the 39 patients who received systemic therapy, 27 received R-CHOP (median 6 cycles [range 4–8]), 3 received ABVD with rituximab (all 6 cycles), 3 ABVD without rituximab (4 cycles, n = 1, 6 cycles, n = 2), 4 received rituximab monotherapy (all weekly × 4 doses), and 1 patient each was treated with cyclophosphamide, doxorubicin, procarbazine, prednisone, and mitoxantrone, vinblastine, vincristine, and prednisone (NOVP) (Table 2). Two patients with advanced-stage disease also received radiotherapy. One received 24 Gy of IFRT to a retroperitoneal lymph node that was 6 cm in size at time of diagnosis; they had achieved complete remission (CR) after R-CHOP, prior to the delivery of RT. Another patient received 35 Gy to the mantle, with boosts to the neck and axilla following NOVP as part of an investigational protocol.
Table 2.
Initial treatment strategy for patients by disease stage
| Treatment | Stage I | Stage II | Stage III/IV | Total |
|---|---|---|---|---|
| Radiation alone | 19 | |||
| 31 Gy | 2 | |||
| 36 Gy | 5 | 3 | ||
| 40 Gy | 6 | 2 | ||
| Dose unknown | 1 | |||
| Total | 14 | 5 | 0 | |
| Combined modality | 12 | |||
| R-CHOP + IFRT (24 Gy, n = 1; 30.6 Gy, n = 5; 36 Gy, n = 1) | 2 | 4 | 1 | |
| R + IFRT (30 Gy, n=1; 40 Gy, n=1) | 1 | 1 | 0 | |
| ABVD + STNI (40 Gy) | 0 | 1 | 0 | |
| COPP + IFRT (40 Gy) | 0 | 1 | 0 | |
| NOVP + IFRT (35 Gy) | 0 | 0 | 1 | |
| Total | 3 | 7 | 2 | |
| Chemotherapy alone | 27 | |||
| R-CHOP | 2 | 3 | 15 | |
| R-ABVD | 0 | 1 | 2 | |
| ABVD | 0 | 0 | 2 | |
| R | 0 | 1 | 1 | |
| Total | 2 | 5 | 20 | |
| Observation | 1 | 0 | 0 | 1 |
| Total | 20 | 17 | 22 | 59 |
COPP, cyclophosphamide, doxorubicin, procarbazine, prednisone; R, rituximab; STNI, subtotal nodal irradiation.
Response and long-term outcomes
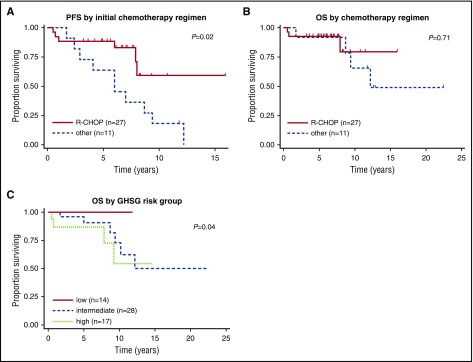
R-CHOP therapy for the 27 treated patients induced a 100% overall response rate (ORR) of 100% (89% CR). In contrast, R-ABVD and ABVD for the 3 patients treated with each regimen induced an ORR of 100% with CR rates (CRR) ranging from 67% to 100%, respectively. Rituximab monotherapy in the 4 treated patients led to an ORR of 100% and CRR of 50% (Table 3). Among the 6 patients with histologic transformation at diagnosis, all received R-CHOP. Two returned to have therapy at other institutions and were lost to follow-up. Of the remaining 4 included in our final analysis, all achieved a response (3 CR, 1 partial remission [PR]). A 46-year-old female patient with NLPHL and TCRBCL at diagnosis experienced disease progression 1 year after initiation of treatment (with TCRBCL). The other 3 patients remain in continuous remission at 6.7, 7.0, and 15.9 years of follow-up. The median follow-up for all patients was 6.7 years (range, 0.2-22.4) and the median follow-up of R-CHOP-treated patients (n = 27) was 6.6 years (range, 3.2-15.9). The estimated 5- and 10-year PFS for patients treated with R-CHOP was 88.5% (95% CI, 68.4% to 96.1%) and 59.3 (95% CI, 25.3% to 89.1%), respectively (Figure 1A). Excluding the 4 patients with NLPHL and histologic transformation, the estimated 5- and 10-year PFS for the 23 patients treated with R-CHOP was 91.3% (95% CI, 69.5% to 97.8%) and 76.1% (95% CI, 33.4% to 93.4%). When considering only patients with stage III/IV NLPHL without histologic transformation (n = 14), the 5- and 10-year PFS were both 85.7% (95% CI, 53.9% to 96.2%). Among patients treated with R-CHOP, neither the use of radiotherapy (P = .85; data not shown) nor disease stage (P = .65; data not shown) were associated with PFS. An analysis limited to patients with early stage revealed no significant difference in PFS for patients treated with CMT in relation to chemotherapy or RT alone (data not shown). Among patients treated with systemic therapy, those who received R-CHOP had a superior PFS in comparison with those who received all other regimens (P = .02; Figure 1A). There was no significant difference in OS (Figure 1B). No patients treated with R-CHOP experienced histologic transformation, while by comparison, patients treated with subtotal nodal irradiation (n = 1) and R-ABVD (n = 1) experienced histologic transformation at 8.8 and 2.9 years, respectively. Of the PFS events occurring after 5 years, 4 were deaths in remission (second primary malignancy [n = 1], invasive pulmonary aspergillosis [n = 1], unknown [n = 2]), and the remainder were lymphoma relapses. Of the patients treated with R-CHOP, 2 patients had late-disease progression at 6 and 8 years. One patient in complete remission at last follow-up died after 7.9 years of follow-up (cause of death unknown). There were 8 patients over the age of 60 years: among these patients, the 5-year estimated PFS was 85.7% (95% CI, 33.4% to 97.8%), and OS was 85.7% (95% CI, 38.7% to 8.1%). These results did not significantly differ from the patients under the age of 60 (P = .37 and P = .59, respectively). There were 2 early deaths (both in R-CHOP–treated patients)—one was diagnosed with metastatic gastric adenocarcinoma 6 months after completion of therapy (patient died following CMT; cause of death unavailable). The second early death occurred at 8 months after R-CHOP because of necrotizing viral myocarditis.
Table 3.
Overall response rates according to chemotherapy regimen (all stages)
| Treatment regimen | CR (%) | PR (%) | ORR (%) |
|---|---|---|---|
| R-CHOP | 17/20 (85) | 3/20 (15) | 20/20 (100) |
| R-CHOP + RT | 7/7 (100) | 0 (0) | 7/7 (100) |
| R-CHOP all RT | 24/27 (89) | 3/27 (11) | 27/27 (100) |
| R-ABVD | 2/3 (67) | 1/3 (33) | 3 (100) |
| R-ABVD + RT | 0 | 0 | 0 |
| R-ABVD all RT | 2 (67) | 1/3 (33) | 3 (100) |
| ABVD | 2/2 (100) | 0 (0) | 2/2 (100) |
| ABVD + RT | 1/1 (100) | 0 (0) | 1/1 (100) |
| ABVD all RT | 3/3 (100) | 0 (0) | 3/3 (100) |
| R | 0 (0) | 1/1 (100) | 1/1 (100) |
| R + RT | 2/3 (67) | 1/3 (33) | 3/3 (100) |
| R all RT | 2/4 (50) | 2/4 (50) | 4/4 (100) |
| Other regimens | 2 (100) | 0 (0) | 2 (100) |
| All systemic therapy ± RT | 33/39 (85%) | 6/39 (15%) | 39/39 (100) |
Boldface type indicates subtotal.
Figure 1.
Progression-free survival and overall survival according to treatment strategies. Progression-free survival (A) and overall survival (B) according to treatment strategy (R-CHOP vs other) and overall survival by GHSG risk-factor group (C).
Treatment at relapse and outcomes
Data regarding second-line treatment were available for 9 patients who experienced relapse during follow-up. Among 7 patients who relapsed with NLPHL, 5 received single-agent rituximab, and 1 patient each received R-ABVD and R-CVP; all achieved CR. Two patients relapsed with transformed disease: one (described above) with both NLPHL and TCRBCL at diagnosis relapsed with TCRBCL and was treated with rituximab, ifosfamide, carboplatin, and etoposide. The other experienced histologic transformation from NLPHL to TCRBCL at 2.9 years and received rituximab, hyperfractionated cyclophosphamide, doxorubicin, vincristine, and dexamethasone (PR), followed by rituximab, ifosfamide, and etoposide (CR). Both patients underwent high-dose therapy and autologous stem cell transplant. With a median of 4.1 years (range, 0.1-16.4) follow-up after first relapse, the estimated 4-year survival from first relapse was 90% (95% CI, 47.3% to 98.5%).
Table 4 summarizes an exploratory univariate analysis examining impact of multiple candidate factors on PFS and OS. When comparing patients by GHSG risk scores, a significantly inferior OS (P = .04) was noted for those in the intermediate- or high-risk group in comparison with those in the low-risk group (Figure 1C). Males had inferior PFS (P = .008) and OS (P = .006) in comparison with females. Furthermore, splenic involvement was adverse prognostic for PFS (P = .002) but not OS. Although GHSG score and male sex were adversely prognostic for OS, low albumin or histologic variant alone were not.
Table 4.
Univariate analysis for candidate prognostic factors using Cox proportional hazards model
| Candidate factor | PFS | OS | ||
|---|---|---|---|---|
| Hazard ratio (95% CI) | P | Hazard ratio (95% CI) | P | |
| GHSG risk score | .036 | |||
| Low | Reference group | Reference group | ||
| Intermediate | 6.72 (0.87-52.01) | .068 | No events | |
| High | 6.02 (0.72-50.45) | .098 | No events | |
| ECOG performance status (1 vs 0) | 0.97 (0.90-2.40) | .94 | 1.19 (0.33-4.23) | .79 |
| Stage III/IV vs I/II | 1.22 (0.50-3.00) | .66 | 1.17 (0.33-4.41) | .81 |
| Male sex | 5.08 (1.17-22.00) | .008 | >100* | .006 |
| B symptoms | 1.76 (0.63-4.94) | .28 | 1.20 (0.25-5.70) | .82 |
| Splenic involvement | 6.94 (2.07-23.26) | .002 | 1.57 (0.33-7.50) | .57 |
| Bone marrow involvement | 1.60 (0.46-5.61) | .46 | 0.77 (0.10-6.20) | .81 |
| Transformed histology at diagnosis | 0.49 (0.06-3.80) | .50 | <0.01* | .21 |
| Albumin < 4.0 g/dL | 1.41 (0.46-4.31) | .54 | 0.92 (0.19-4.42) | .92 |
| Histologic variant (non-A/B†) | 1.04 (0.39-2.77) | .94 | 10.4 (0.27-4.04) | .95 |
Analysis of PFS is restricted to patients for whom treatment details are known. OS analysis includes all patients with follow-up data. Boldface type indicates a significant P value.
Unable to generate 95% CI.
As defined by Hartmann et al.8
Discussion
Defining the optimal management of NLPHL remains a significant challenge, given that management strategies are typically based on small, single-center studies. The goals of treatment have been to decrease the risks of relapse and histologic transformation. Prior experience has suggested the potential of improved benefit from the inclusion of an alkylating agent such as cyclophosphamide.25 Numerous strategies have been explored for early-stage NLPHL. A series of 202 Australian patients treated with radiation therapy alone (median dose of 36 Gy) showed an OS rate of 83% and freedom from progression of 82% with a median of 15 years of follow-up.13 Chen et al described 113 early-stage patients with treatment limited to extended field radiation with 10-year PFS rates for stage I and II being 85% and 61%, respectively. Neither the addition of chemotherapy nor the radiation field changed outcomes, but 86% patients treated with chemotherapy alone experienced disease relapse. In contrast, investigators from the BCCA demonstrated that treatment with ABVD paired with RT improved outcomes in comparison with RT alone. In this study, the 10-year PFS was 91% and OS was 93% for ABVD-like therapy plus RT versus 65% and 84%, respectively, for RT alone. Rituximab monotherapy also has been evaluated for patients with early-stage NLPHL. Advani et al treated patients with induction followed by maintenance dosing with median PFS of 3 to 5.6 years.11 Finally, an analysis of 256 patients with stage IA NLPHL treated on successive GHSG protocols indicated that long-term disease control was excellent with multiagent chemotherapy, extended field, and involved field radiotherapy with 8-year PFS of 88.5%, 84.3%, and 91.9%, respectively, and not significantly different between these modalities (P = .43). Patients treated with single-agent rituximab had a shorter median follow-up of 4 years but were more likely to experience disease progression than the other modalities (hazard ratio, 4.99 [95% CI, 1.88-13.21]).26 The range of treatments applied to patients with early-stage disease in our cohort reflect the variety of options available. We observed a lower PFS for limited-stage-disease patients at 10 years in comparison with historical comparisons for RT alone and CMT. R-CHOP-treated patients had a 5-year PFS of 100%, but there was no statistically significant difference in PFS between patients treated with RT alone versus CMT versus chemotherapy alone. However, interpreting differences between different therapeutic modalities and regimens is challenging because of the low patient numbers treated with each approach.
There is no defined optimal therapy for patients with advanced-stage disease. The Princess Margaret Hospital group described a high relapse rate of over 50% at 5 years for NLPHL patients treated with ABVD, including 4 patients who developed transformation.27 The BCCA group recently conducted a 1:2 matched-pair analysis for advanced-stage NLPHL and cHL patients.6 The median follow-up was 10.7 and 11.3 years, respectively; most patients received ABVD-like chemotherapy. Although the 10-year OS was similar, time to progression including transformation to aggressive lymphomas was shorter for NLPHL patients than for cHL patients (41% vs 71%), supporting the concept that ABVD may have limitations. In our study patients treated with R-CHOP for advanced-stage disease had a 5-year OS of 81%, and we did not observe histologic transformation, comparing favorably to historical data using ABVD. The risk of histologic transformation varies between studies. Data from a French registry of 164 patients with NLPHL followed for a median of 9.5 years indicated a cumulative risk of histologic transformation of 12%, with the median time to transformation of 4.7 years after NLPHL diagnosis.28 Similar results were noted by investigators from the BCCA, who followed 95 patients and observed a 14% risk of transformation at the median follow-up of 8.1 years, with an actuarial risk of 30% at 20 years; the 10-year PFS for patients who developed transformed lymphoma was 52%. Initial therapies for the patients with NLPHL who subsequently developed transformation included ABVD or equivalent therapies in 54% of the patients; none received R-CHOP.4 Investigators from the Mayo Clinic reviewed 220 NLPHL patients with a median follow-up of 16 years and described a transformation rate of 7.7%, with a median time to transformation of 35 months and a 5-year OS following histologic transformation of 76.4%.5 The most common chemotherapy regimens used for initial diagnosis of NLPHL were ABVD ± R or mustargen, oncovin, procarbazine, and prednisone; none received R-CHOP. In both studies the treatments that were given at time of transformation centered on CHOP-based therapies with 62% of the BCCA patients and 53% of the Mayo Clinic patients receiving CHOP-based chemotherapies ± rituximab at time of transformation. In our cohort, none of the patients treated with R-CHOP experienced transformation. However, transformation has been reported as late as 20 years after initial diagnosis,4 and the numbers of patients treated with R-CHOP are modest; thus further observations are needed to confirm this impression. We were unable to directly compare toxicities from R-CHOP and ABVD ± R owing to the retrospective nature of this study. In relation to ABVD, R-CHOP causes more peripheral neuropathy (with vincristine in relation to vinblastine), has a higher cumulative steroid exposure, and has a potentially greater likelihood of infertility (cyclophosphamide vs dacarbazine). In contrast, ABVD results in more pulmonary toxicity (bleomycin) but is, in our experience, more difficult to deliver to elderly patients.
In summary, within the limits of a retrospective study, our data suggest that R-CHOP may be a highly effective treatment of patients with advanced-stage NLPHL. Despite the rarity of the disease, both randomized studies to establish a standard of care and phase I/II clinical trials evaluating targeted agents should be performed to further improve outcomes for patients with this rare B-cell lymphoma.
Footnotes
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: M.A.F. and A.Y. conceived the study; C.-M.L., M.A.F., C.Y.C., A.R., and L.J.M. collected data; C.Y.C. analyzed data and created the tables and figures; M.A.F. wrote the first draft of the manuscript; and all of the authors critically reviewed and approved the final manuscript.
Conflict-of-interest disclosure: C.Y.C. received research funding from Celgene, Roche, and Abbvie; is on the Speakers Bureau for Roche, Janssen-Cilag, Takeda, and Gilead; is an Advisory Board member for Janssen-Cilag and Bristol Myers Squibb; and has received travel expenses from Bristol Myers Squibb. M.A.F. has received research funding from Roche. The remaining authors declare no competing financial interests.
Francesco Turturro died on 2 May 2017.
Correspondence: Michelle A. Fanale, Department of Lymphoma and Myeloma, University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 429, Houston, TX 77030; e-mail: mfanale@mdanderson.org.
References
- 1.Teras LR, DeSantis CE, Cerhan JR, Morton LM, Jemal A, Flowers CR. 2016 US lymphoid malignancy statistics by World Health Organization subtypes. CA Cancer J Clin. 2016;66(6):443-459. [DOI] [PubMed] [Google Scholar]
- 2.Isaacson PG. Malignant lymphomas with a follicular growth pattern. Histopathology. 1996;28(6):487-495. [DOI] [PubMed] [Google Scholar]
- 3.Brune V, Tiacci E, Pfeil I, et al. . Origin and pathogenesis of nodular lymphocyte-predominant Hodgkin lymphoma as revealed by global gene expression analysis. J Exp Med. 2008;205(10):2251-2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Mansour M, Connors JM, Gascoyne RD, Skinnider B, Savage KJ. Transformation to aggressive lymphoma in nodular lymphocyte-predominant Hodgkin’s lymphoma. J Clin Oncol. 2010;28(5):793-799. [DOI] [PubMed] [Google Scholar]
- 5.Kenderian SS, Habermann TM, Macon WR, et al. . Large B-cell transformation in nodular lymphocyte-predominant Hodgkin lymphoma: 40-year experience from a single institution. Blood. 2016;127(16):1960-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xing KH, Connors JM, Lai A, et al. . Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis. Blood. 2014;123(23):3567-3573. [DOI] [PubMed] [Google Scholar]
- 7.Fan Z, Natkunam Y, Bair E, Tibshirani R, Warnke RA. Characterization of variant patterns of nodular lymphocyte predominant hodgkin lymphoma with immunohistologic and clinical correlation. Am J Surg Pathol. 2003;27(10):1346-1356. [DOI] [PubMed] [Google Scholar]
- 8.Hartmann S, Eichenauer DA, Plütschow A, et al. . The prognostic impact of variant histology in nodular lymphocyte-predominant Hodgkin lymphoma: a report from the German Hodgkin Study Group (GHSG). Blood. 2013;122(26):4246-4252, quiz 4292. [DOI] [PubMed] [Google Scholar]
- 9.Ekstrand BC, Lucas JB, Horwitz SM, et al. . Rituximab in lymphocyte-predominant Hodgkin disease: results of a phase 2 trial. Blood. 2003;101(11):4285-4289. [DOI] [PubMed] [Google Scholar]
- 10.Schulz H, Rehwald U, Morschhauser F, et al. . Rituximab in relapsed lymphocyte-predominant Hodgkin lymphoma: long-term results of a phase 2 trial by the German Hodgkin Lymphoma Study Group (GHSG). Blood. 2008;111(1):109-111. [DOI] [PubMed] [Google Scholar]
- 11.Advani RH, Hoppe RT. How I treat nodular lymphocyte predominant Hodgkin lymphoma. Blood. 2013;122(26):4182-4188. [DOI] [PubMed] [Google Scholar]
- 12.Chen RC, Chin MS, Ng AK, et al. . Early-stage, lymphocyte-predominant Hodgkin’s lymphoma: patient outcomes from a large, single-institution series with long follow-up. J Clin Oncol. 2010;28(1):136-141. [DOI] [PubMed] [Google Scholar]
- 13.Wirth A, Yuen K, Barton M, et al. . Long-term outcome after radiotherapy alone for lymphocyte-predominant Hodgkin lymphoma: a retrospective multicenter study of the Australasian Radiation Oncology Lymphoma Group. Cancer. 2005;104(6):1221-1229. [DOI] [PubMed] [Google Scholar]
- 14.Schlembach PJ, Wilder RB, Jones D, et al. . Radiotherapy alone for lymphocyte-predominant Hodgkin’s disease. Cancer J. 2002;8(5):377-383. [DOI] [PubMed] [Google Scholar]
- 15.Savage KJ, Skinnider B, Al-Mansour M, Sehn LH, Gascoyne RD, Connors JM. Treating limited-stage nodular lymphocyte predominant Hodgkin lymphoma similarly to classical Hodgkin lymphoma with ABVD may improve outcome. Blood. 2011;118(17):4585-4590. [DOI] [PubMed] [Google Scholar]
- 16.Shankar A, Hall GW, Gorde-Grosjean S, et al. . Treatment outcome after low intensity chemotherapy [CVP] in children and adolescents with early stage nodular lymphocyte predominant Hodgkin’s lymphoma—an Anglo-French collaborative report. Eur J Cancer. 2012;48(11):1700-1706. [DOI] [PubMed] [Google Scholar]
- 17.Eichenauer DA, Engert A, André M, et al. ; ESMO Guidelines Working Group. Hodgkin’s lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(Suppl 3):iii70-iii75. [DOI] [PubMed] [Google Scholar]
- 18.National Comprehensive Cancer Network. NCCN guidelines version 1. Hodgkin lymphoma. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 1 May 2017. [Google Scholar]
- 19.Fanale M. Lymphocyte-predominant Hodgkin lymphoma: what is the optimal treatment? Hematology Am Soc Hematol Educ Program. 2013;2013:406-413. [DOI] [PubMed] [Google Scholar]
- 20.Fanale MA, Lai C-M, McLaughlin P, et al. . Outcomes of nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) patients treated with R-CHOP. Blood. 2010;116(21):2812.20585043 [Google Scholar]
- 21.Cheson BD, Horning SJ, Coiffier B, et al. ; NCI Sponsored International Working Group. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. J Clin Oncol. 1999;17(4):1244. [DOI] [PubMed] [Google Scholar]
- 22.Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumors of the Hematopoeitic and Lymphoid Tissues. Lyon, France: International Agency for Research on Cancer; 2008. [Google Scholar]
- 23.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457-481. [Google Scholar]
- 24.Cox DR. Regression models and life-tables. J R Stat Soc B. 1972;34(2):187-220. [Google Scholar]
- 25.Canellos GP, Mauch P. What is the appropriate systemic chemotherapy for lymphocyte-predominant Hodgkin’s lymphoma? J Clin Oncol. 2010;28(1):e8. [DOI] [PubMed] [Google Scholar]
- 26.Eichenauer DA, Plütschow A, Fuchs M, et al. . Long-term course of patients with stage IA nodular lymphocyte-predominant Hodgkin lymphoma: a report from the German Hodgkin Study Group. J Clin Oncol. 2015;33(26):2857-2862. [DOI] [PubMed] [Google Scholar]
- 27.Ames J, Maganti M, Monteith BE, et al. . Outcomes of nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) vs. classical Hodgkin lymphoma (cHL) at Princess Margaret Cancer Centre. Blood. 2015;126(23):3863. [Google Scholar]
- 28.Biasoli I, Stamatoullas A, Meignin V, et al. . Nodular, lymphocyte-predominant Hodgkin lymphoma: a long-term study and analysis of transformation to diffuse large B-cell lymphoma in a cohort of 164 patients from the Adult Lymphoma Study Group. Cancer. 2010;116(3):631-639. [DOI] [PubMed] [Google Scholar]