ABSTRACT
Malnutrition leads to increased morbidity and is evident in almost half of all deaths in children under the age of 5 years. Mortality due to rotavirus diarrhea is common in developing countries where malnutrition is prevalent; however, the relationship between malnutrition and rotavirus infection remains unclear. In this study, gnotobiotic pigs transplanted with the fecal microbiota of a healthy 2-month-old infant were fed protein-sufficient or -deficient diets and infected with virulent human rotavirus (HRV). After human rotavirus infection, protein-deficient pigs had decreased human rotavirus antibody titers and total IgA concentrations, systemic T helper (CD3+ CD4+) and cytotoxic T (CD3+ CD8+) lymphocyte frequencies, and serum tryptophan and angiotensin I-converting enzyme 2. Additionally, deficient-diet pigs had impaired tryptophan catabolism postinfection compared with sufficient-diet pigs. Tryptophan supplementation was tested as an intervention in additional groups of fecal microbiota-transplanted, rotavirus-infected, sufficient- and deficient-diet pigs. Tryptophan supplementation increased the frequencies of regulatory (CD4+ or CD8+ CD25+ FoxP3+) T cells in pigs on both the sufficient and the deficient diets. These results suggest that a protein-deficient diet impairs activation of the adaptive immune response following HRV infection and alters tryptophan homeostasis.
KEYWORDS: ACE2, gnotobiotic, malnutrition, rotavirus, tryptophan, fecal microbiota
INTRODUCTION
Malnutrition leads to wasting and stunted growth and is associated with almost half of all under-5 deaths worldwide (1, 2). The causative association between malnutrition and infectious diseases has long been known (3, 4), and malnourished children frequently have increased diarrheal episodes resulting in exacerbated energy loss and death (1, 4, 5). It is estimated that enteric infections with overt diarrhea account for 25% of stunting cases in children (6), and exposure to multiple enteric pathogens over an extended period of time, with or without diarrhea, may account for up to 43% of stunting cases (7). The common enteric pathogen rotavirus (RV) is a major cause of gastroenteritis in children worldwide, leading to more than 215,000 deaths per year (8, 9). RV infection results in diarrhea due to intestinal net fluid secretion via mechanisms including malabsorption due to villous atrophy (10).
Previously, murine models have been used to show that the enteric pathogens Cryptosporidium (11) and enteroaggregative Escherichia coli (12) exacerbate growth impairment and intestinal damage associated with malnutrition. The neonatal piglet is similar to human infants in gastrointestinal physiology, micro- and macronutrient metabolism, and mucosal immunity. Further, like children, germfree (GF) pigs are susceptible to repeated infections by multiple RV serotypes with ensuing disease and intestinal lesions (13–15). Finally, pigs are outbred, eliminating the strain bias common in mouse model research. We have used the GF pig to study controlled exposure to microorganisms and physiologically relevant and economically feasible intervention strategies (15–22). Recently, investigators have successfully transplanted GF pigs with human gut microbiota (23) and used this model to examine the effects of probiotics on human rotavirus (HRV) pathogenesis and immunity (24–26). The pig has also been used as a translational model for malnutrition, which disrupted intestinal barrier function and exacerbated RV-induced disease in colostrum-deprived neonatal piglets (27–31).
Recently, we established a neonatal gnotobiotic (Gn) pig model of childhood protein malnutrition in conjunction with human infant fecal microbiota (HIFM) colonization that reproduces the effects of kwashiorkor protein malnutrition (26). In this model, stunting was evident at 1 week of age and clinical features mimicking kwashiorkor protein malnutrition (edema of the face, neck, feet, and abdomen) appeared, in addition to changes in blood parameters, including hypoglycemia, hypoproteinemia, and hypoalbuminemia, commonly seen in malnourished children (26). Analysis of fecal samples and the microbiome in multiple regions of the intestine 1 week following the HIFM transplant found that over 99% of the operational taxonomic units (OTUs) from the original HIFM sample were present in the pigs and that the microbial community structure of the transplanted HIFM was qualitatively representative of the original sample (A. Kumar, A. N. Vlasova, L. Deblais, H.-C. Huang, A. Wijeratne, S. Kandasamy, D. D. Fischer, S. N. Langel, F. C. Paim, M. A. Alhamo, L. Shao, L. J. Saif, and G. Rajashekara, submitted for publication). Additionally, HRV-infected, protein-deficient, HIFM-transplanted pigs (deficient HIFM/HRV) had increased diarrhea and shed virus at higher titers after virulent human rotavirus (virHRV) inoculation in comparison to their sufficient-diet, HIFM-transplanted, virHRV-infected (sufficient HIFM/HRV) counterparts (26). Furthermore, deficient HIFM/HRV pigs had increased microbiota diversity in systemic tissues in comparison to sufficient HIFM/HRV pigs, indicating increased translocation from the intestine (Kumar et al., submitted).
To better understand the relationship between malnutrition, immune activation and responses to RV, and homeostatic control of selected amino acids, we compared adaptive immune responses (antibody production and T cell frequencies), concentrations of angiotensin I-converting enzyme 2 (ACE2; a regulator of dietary amino acid homeostasis), and levels of the essential amino acid tryptophan. ACE2 is associated with the neutral amino acid transporter B0AT1 and is required for expression of B0AT1 on the luminal surface of intestinal epithelial cells (IECs) (32–34). Knockout of ACE2 in mice resulted in increased susceptibility to intestinal inflammation and colitis, decreased serum tryptophan, and alteration of the gut microbiome (35). Restoring tryptophan levels reduced inflammation and increased the production of antimicrobial peptides by the intestinal epithelium, showing that ACE2 regulates dietary amino acid homeostasis, innate immunity, inflammation, and gut microbial ecology in a tryptophan-dependent manner (35). Furthermore, children at high risk for stunting often have limited tryptophan in their diets (36), and it has been shown previously that stunted children have lower serum concentrations of all nine essential amino acids, including tryptophan (37). Low plasma tryptophan is a predictor of poorer subsequent growth in boys and is associated with biomarkers of barrier disruption and intestinal and systemic inflammation in children of both genders (38). Tryptophan catabolism via the indoleamine 2,3-dioxygenase (IDO) pathway has immunoregulatory effects, and its depletion has been well studied in the context of chronic infections (39); however, the interrelationship between tryptophan and the adaptive immune response to RV and other acute infections is less clear, particularly in the context of host protein malnutrition.
In this study, we report that protein deficiency affects the adaptive immune response to RV and disrupts tryptophan homeostasis and catabolism in the neonatal gnotobiotic (Gn) pig model of childhood malnutrition, involving transplantation of pigs with human infant fecal microbiota (HIFM).
RESULTS
Protein deficiency reduced HRV IgA and IgM antibody isotype titers and total IgA concentrations following HRV inoculation, but increased total IgG and IgM concentrations.
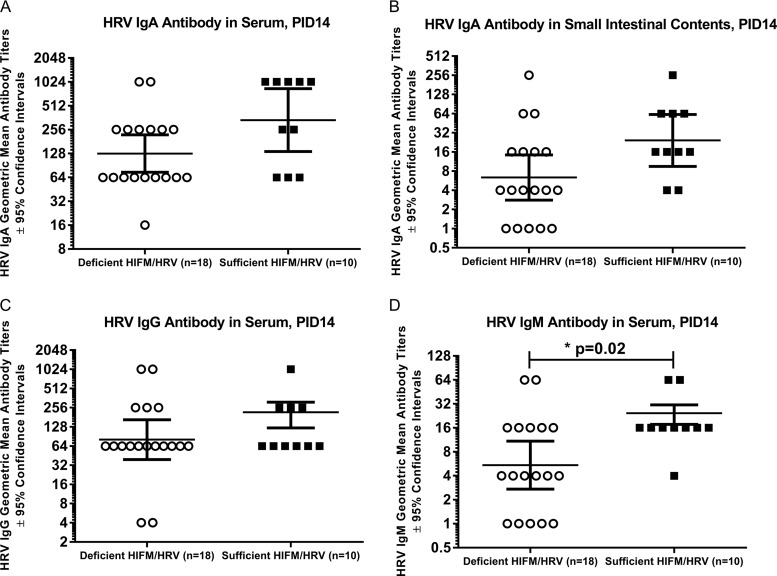
To evaluate the effect of protein deficiency on systemic and local antibody production, HRV-specific antibody titers and total IgA concentrations were measured. IgA HRV antibody titers were reduced in serum (Fig. 1A, P = 0.06) and significantly reduced in small intestinal contents (Fig. 1B, P < 0.05) of deficient HIFM/HRV pigs compared to sufficient HIFM/HRV pigs, suggesting that protein deficiency compromised mucosal and systemic viral antibody responses. Additionally, in deficient HIFM/HRV pigs, IgM HRV antibody titers (Fig. 1D, P < 0.05) were significantly decreased compared with those in sufficient HIFM/HRV pigs. IgG HRV antibody titers were not significantly decreased in the deficient HIFM/HRV pigs. Reductions in HRV antibodies were seen despite higher rotavirus shedding in the deficient HIFM/HRV pigs (26).
FIG 1.
Mean immunoglobulin isotype concentrations. HRV antibody isotype geometric mean titers in sufficient and deficient HIRM/HRV pigs at PID14 as measured by ELISA. (A and B) IgA antibody GMTs in serum (A) and small intestinal contents (B); (C) IgG antibody GMT in serum; (D) IgM antibody GMT in serum. The GMTs are shown ±95% confidence intervals. *, significant (P ≤ 0.05) decrease of deficient HIFM/HRV pigs compared to sufficient HIFM/HRV pigs (Mann-Whitney test).
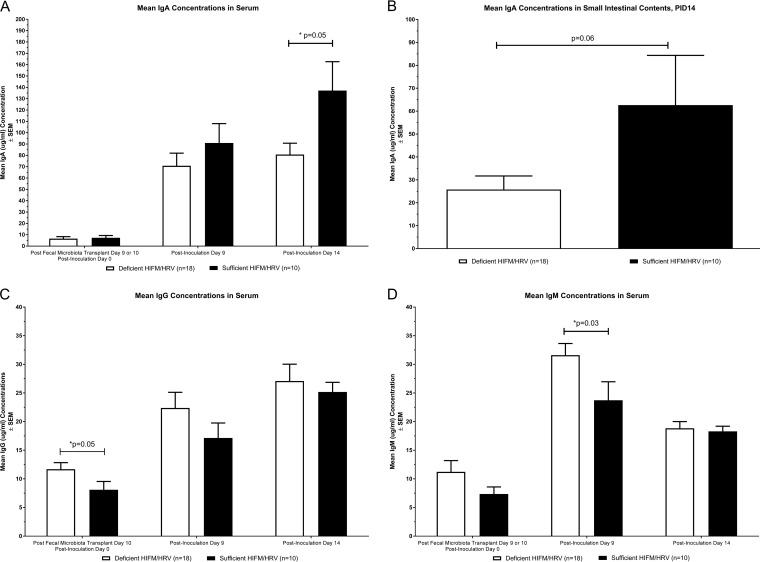
In deficient HIFM/HRV pigs, mean concentrations of total IgA in the serum were lower at post-virHRV inoculation day 9 (PID9) and were reduced at PID14 (Fig. 2A, P = 0.05) in comparison to sufficient HIFM/HRV pigs. Mean total IgA concentrations were also lower (Fig. 2B, P = 0.06) in the small intestinal contents of deficient HIFM/HRV pigs at PID14 compared with the sufficient HIFM/HRV pigs. In deficient HIFM/HRV pigs, mean total IgG and IgM concentrations were higher in the serum pre- and postinoculation, IgG at post-fecal microbiota transplant day 10 (PFMTD10)/PID0 (Fig. 2C, P = 0.05) and IgM at PID9 (Fig. 2D, P < 0.05).
FIG 2.
T helper and cytotoxic T cell frequencies at PID14. Total immunoglobulin concentrations in deficient and sufficient HIFM/HRV pigs. (A and B) IgA in the serum (A) and small intestinal contents (B); (C) IgG in serum; (D) IgM in serum. Concentrations were determined by ELISA. Results are ±standard errors of the means (SEM). *, significant (P < 0.05) change in deficient HIRM/HRV pigs compared to sufficient HIFM/HRV pigs (Mann-Whitney test).
Protein deficiency reduced systemic T helper and cytotoxic T cell frequencies.
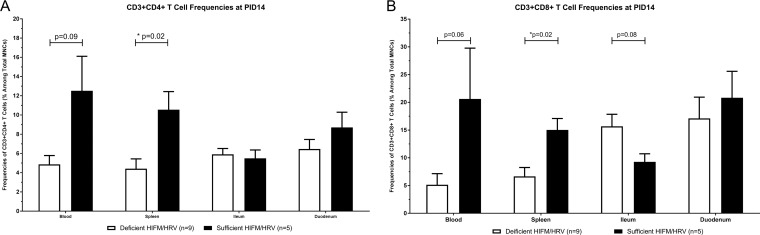
To evaluate the impact of protein deficiency on Th cells, the frequencies of CD3+ CD4+ Th cells in blood, spleen, duodenum, and ileum mononuclear cells (MNCs) were measured by flow cytometry at PID14 in deficient and sufficient pigs infected with HRV (Fig. 3A). Systemic CD3+ CD4+ Th cell frequencies were decreased systemically in the blood (P = 0.09, Fig. 3A) and significantly in the spleen (*, P = 0.02). No decreases or only slight decreases in Th frequencies were seen in the intestine (ileum or duodenum, respectively). Similarly, CD3+ CD8+ cytotoxic T lymphocyte (CTL) frequencies were decreased systemically in the spleen (P = 0.06) and significantly decreased in the blood (P = 0.02) but increased in the ileum (P = 0.08) in deficient HIFM/HRV pigs in comparison with the sufficient HIFM/HRV pigs (Fig. 3B).
FIG 3.
CD3+ CD4+ T helper cell and CD3+ CD8+ cytotoxic T cell frequencies as a percentage of total MNCs in the blood, spleen, ileum, and duodenum in deficient and sufficient HIFM/HRV pigs at PID14, determined by flow cytometry. (A) CD3+ CD4+ T helper cells. (B) CD3+ CD8+ cytotoxic T cells. Results are ±standard errors of the means (SEM). *, significant (P < 0.05) change in deficient HIRM/HRV pigs compared to sufficient HIFM/HRV pigs (Mann-Whitney test).
Dietary tryptophan supplementation increased regulatory T cell frequencies in deficient- and/or sufficient-diet pigs infected with HRV.
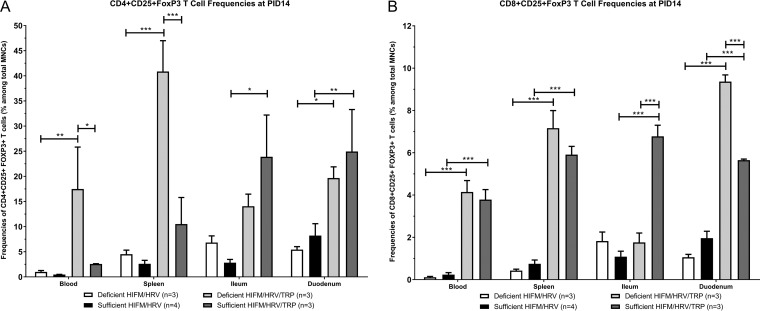
The frequencies of CD4+ CD25+ Foxp3+ (Fig. 4A) and CD8+ CD25+ Foxp3+ (Fig. 4B) regulatory T cells (Tregs) in blood, spleen, duodenum, and ileum MNCs were measured by flow cytometry at PID14 in tryptophan-supplemented and unsupplemented deficient and sufficient HIFM pigs infected with HRV. CD4+ CD25+ Foxp3+ cell frequencies were higher, but not significantly different, in the blood, spleen, and ileum of unsupplemented deficient HIFM/HRV pigs compared with unsupplemented sufficient HIFM/HRV pigs. Deficient HIFM/HRV pigs supplemented with tryptophan had significantly increased frequencies of CD4+ CD25+ Foxp3+ Tregs in the blood (P < 0.01), spleen (P < 0.001), and duodenum (P < 0.05) compared with unsupplemented deficient HIFM/HRV pigs. Sufficient HIFM/HRV pigs supplemented with tryptophan had significantly increased CD4+ CD25+ Foxp3+ Treg frequencies only in the gut (ileum [P < 0.05] and duodenum [P < 0.05]) compared to unsupplemented sufficient HIFM/HRV pigs. The overall frequencies of CD8+ CD25+ FoxP3+ Tregs were mostly lower in all tissues than those of CD4+ CD25+ FoxP3+ Tregs. As for CD4+ CD25+ Foxp3+ Tregs, deficient HIFM/HRV pigs supplemented with tryptophan had highly significant increases (P < 0.001) in the frequencies of CD8+ CD25+ Foxp3+ Tregs in the blood, spleen, and duodenum compared to unsupplemented deficient HIFM/HRV pigs. Also, sufficient HIFM/HRV pigs supplemented with tryptophan had highly significant increases (P < 0.001) in CD8+ CD25+ Foxp3+ cell numbers in the blood, spleen, ileum, and duodenum in comparison with their unsupplemented counterparts. Dietary tryptophan supplementation had no detectable effects on HRV antibody isotype titers, total antibody concentrations, CD3+ CD4+ Th cell frequencies, or CD3+ CD8+ CTL frequencies.
FIG 4.
T regulatory cell frequencies as a percentage of total MNCs in the blood, spleen, ileum, and duodenum of deficient and sufficient HIFM/HRV pigs with or without tryptophan supplementation at PID14, determined by flow cytometry. (A) CD4+ CD25+ FoxP3+ T cells (scale, 0 to 50%). (B) CD8+ CD25+ FoxP3+ T cells (scale, 0 to 12%). Results are ±standard errors of the means (SEM). Asterisks show significant (*, P < 0.05; **, P ≤ 0.01; ***, P ≤ 0.005) increases in tryptophan-supplemented compared to unsupplemented pigs (two-way ANOVA and Bonferroni's multiple-comparison test).
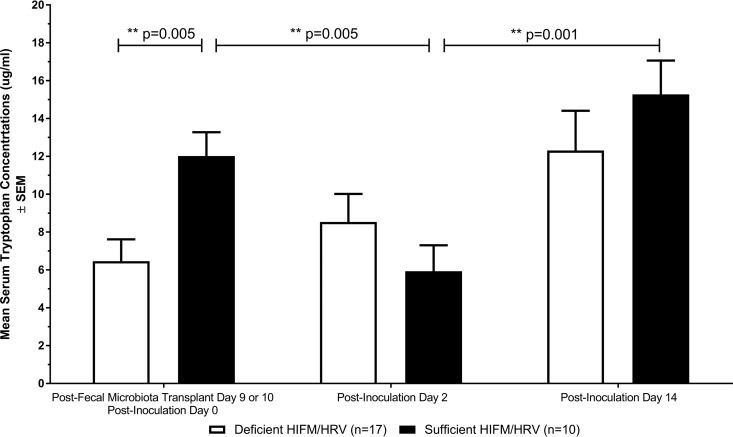
Protein deficiency altered serum tryptophan concentrations.
Serum tryptophan concentrations were measured (Fig. 5) preinoculation and during the acute and convalescent phases of virHRV infection. At 9 or 10 days PFMT, prior to virHRV inoculation (PFMTD9 or PFMTD10/PID0), deficient pigs had significantly lower (P = 0.005) levels of the essential amino acid tryptophan in serum than did sufficient HIFM/HRV pigs, indicating disruption in amino acid homeostasis consistent with hypoproteinemia (26). In the acute phase of virHRV infection (PID2) and convalescent phase (PID14), serum tryptophan levels rose steadily in deficient-diet pigs. In sufficient-diet pigs, serum tryptophan levels dropped significantly (**, P < 0.01) in the acute phase of virHRV infection and then rose significantly (**, P < 0.01) during the convalescent phase, consistent with immune activation and virus clearance.
FIG 5.
Serum tryptophan concentrations in deficient and sufficient HIFM/HRV pigs: preinfection (PFMTD9 or PFMTD10/PID0), post-virHRV inoculation (PID2), and 2 weeks post-virHRV inoculation (PID14), measured by ELISA. Results are ±standard errors of the means (SEM). ** (P ≤ 0.01), change at a single time point between deficient HIFM/HRV pigs and sufficient HIFM/HRV pigs or at different time points between sufficient HIFM/HRV pigs (unpaired t test).
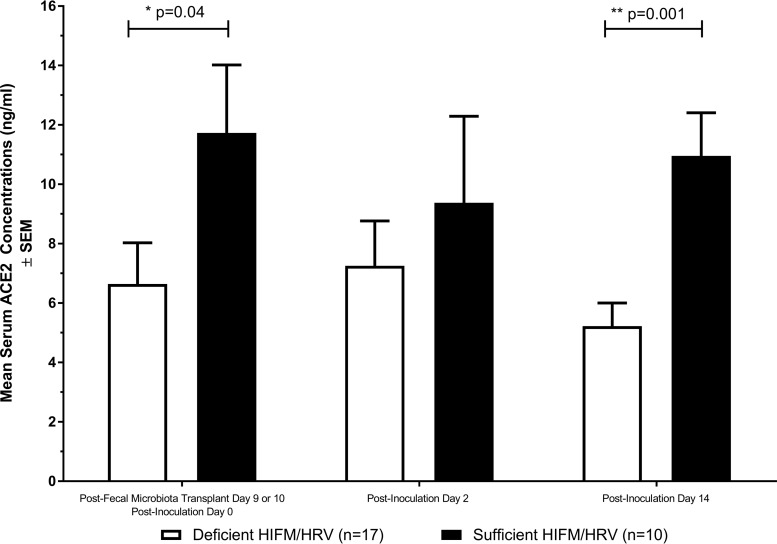
Protein deficiency decreased serum ACE2 concentrations.
Serum ACE2 concentrations were measured (Fig. 6) preinoculation and during the acute and convalescent phases of virHRV infection. Pre-virHRV inoculation (PFMTD9 or PFMTD10/PID0), serum ACE2 concentrations were significantly lower (P < 0.05) in deficient HIFM/HRV pigs than in sufficient HIFM/HRV pigs. Serum ACE2 levels were decreased in sufficient-diet pigs, but they remained higher than those in deficient-diet pigs during the acute phase (PID2) of virHRV infection (ACE2 levels also decreased in a manner coincident with that of tryptophan [Fig. 5]) and were restored to a significantly higher (P < 0.01) concentration during the convalescent (PID14) phase of infection. Deficient/HIFM pigs not challenged with virHRV had lower (but not statistically significantly lower) serum ACE2 concentrations than unchallenged sufficient/HIFM pigs at PID14 (data not shown).
FIG 6.
Serum ACE2 concentrations in deficient and sufficient HIFM/HRV pigs: preinfection (PFMTD9 or PFMTD10), post-virHRV inoculation (PID2), and 2 weeks post-virHRV inoculation (PID14), measured by ELISA. Results are ±standard errors of the means (SEM). Asterisks indicate significant (*, P < 0.05; **, P ≤ 0.01) decreases of ACE2 in deficient HIRM/HRV pigs compared to sufficient HIFM/HRV pigs (Mann-Whitney test).
DISCUSSION
Because malnutrition and malnutrition-associated infections are a leading cause of childhood deaths, it is critical to distinguish the interrelated factors that lead to increased infections or impaired immune responses and to identify targets for intervention. In this study, we report that in HIFM-transplanted pigs, protein deficiency impairs adaptive immune responses to HRV, lowers serum levels of tryptophan, impairs its catabolism during the acute phase of HRV infection, and lowers serum ACE2 compared with sufficient-diet pigs. In addition, we found that whereas Th cells and CTLs were significantly decreased systemically only in the protein-deficient pigs, dietary tryptophan supplementation increased systemic and intestinal Treg frequencies in both deficient and sufficient animals.
The presence and titers of HRV-specific IgA antibodies in the feces/intestinal contents and serum of humans (40–43) and pigs (44–46) strongly correlate with protection from HRV infection in multiple studies (47). In this study, protein deficiency decreased HRV IgA antibodies in both the serum and small intestinal contents, despite HRV replicating to higher titers in deficient HIFM/HRV pigs, indicating impaired mucosal and systemic HRV antibody responses. Additionally, HRV IgM antibody titers and total IgA concentrations were reduced in serum at PID14 in the deficient HIFM/HRV pigs, further suggesting that protein deficiency compromises intestinal and systemic antibody responses to viral infection. Our findings showing that deficient HIFM/HRV pigs have decreased levels of total and HRV IgA antibody in the intestinal contents are in agreement with the previous findings that protein malnutrition impairs secretory IgA production in humans (48, 49) and mice (50, 51). It has been shown previously that total serum IgM, IgG, and IgA are elevated in humans with the protein malnutrition disorders kwashiorkor and marasmus (52–56). Our findings of increased total serum IgM and IgG concentrations in the deficient-diet pigs at PFMTD9 or PFMTD10/PID0 are consistent with these findings; however, it is unclear why we did not find elevated serum IgA at this time point, in contrast to the findings of others. The increased total concentrations of serum IgA postinoculation in the sufficient HIFM pigs post-HRV infection are likely due to the increased stimulation of mucosal IgA in response to HRV infection.
Protein deficiency also decreased the frequencies of systemic (blood and spleen) CD3+ CD4+ Th cells and CD3+ CD8+ CTLs among total MNCs in the HIFM/HRV pigs, confirming alterations of systemic T cell immune responses. The significant decrease in splenic Th cell frequencies and the downward trend in blood Th cells in deficient HIFM/HRV pigs are consistent with the decreased production of HRV antibodies and total IgA concentrations, as Th cells are necessary for activation of B cells and subsequent antibody production. The decrease in systemic CTLs in deficient HIFM/HRV pigs suggests an impaired response to extraintestinal RV. Our results indicating that protein deficiency does not affect the levels of CD3+ CD4+ Th cells in the ileum and duodenum or CD3+ CD8+ CTLs in the duodenum are consistent with the findings of Zijlstra and colleagues, who found that malnutrition did not significantly alter the numbers of CD4+ or CD8+ T cells in the jejunum of conventional pigs infected with porcine rotavirus (27). The increase of CTLs in the ileum in the deficient HIFM/HRV pigs might be due to the high replication of the rotavirus in the ileum of pigs (14) or the altered and less diverse gut microbiota in these pigs (Kumar et al., submitted). An additional possibility is that Turicibacter species, which can modulate CD8+ T cells (57), were found to be more abundant in the intestines of sufficient HIFM/HRV animals (Kumar et al., submitted). These decreases in T cells were also consistent with the decreased number and function of several innate immune cell types in deficient HIFM/HRV pigs (26), including CD103+ dendritic cells (DCs), which are necessary to prime and confer intestinal homing of B and T lymphocytes (58).
Serum tryptophan concentrations were reduced in deficient HIFM/HRV pigs pre-HRV inoculation and at 2 weeks postinoculation compared with sufficient-diet pigs, indicating disruption of tryptophan amino acid homeostasis during protein deficiency. In sufficient HIFM/HRV pigs, during the acute phase of HRV infection, serum tryptophan concentrations dropped significantly from preinoculation levels before rising significantly again at PID14. In contrast, serum tryptophan concentrations in deficient HIFM/HRV pigs rose steadily throughout the experiment, without a decrease in concentrations at PID2, suggesting that tryptophan was not catabolized efficiently during the antiviral response. Decreased tryptophan concentrations have been found to inhibit the growth of certain bacteria (59) and parasites (60) and are associated with antiviral immune responses during measles (61), herpes simplex virus (HSV) 1 and 2 (62, 63), and vaccinia virus (64) infections (39). To our knowledge, this study is the first to show that HRV infection decreased serum tryptophan concentrations. Tryptophan also decreases during chronic viral infection with hepatitis B and C, HIV, herpesvirus, and cytomegalovirus (reviewed in reference 39). During these instances where virus is not cleared, IDO is persistently activated and may serve to balance tissue damage by inhibiting antiviral T cell responses and enhancing Tregs, leading to removal of the virus from immune surveillance, creating tolerance (39).
Deficient HIFM/HRV pigs may have been unable to catabolize tryptophan post-HRV inoculation for a number of reasons (Fig. 5). First, gamma interferon (IFN-γ) production may be impaired in deficient HIFM/HRV pigs, not reaching concentrations high enough to trigger IDO1 and the tryptophan pathway. We measured IFN-γ concentrations in the serum and tested for IFN-γ-secreting T cells; however, the low sample sizes showed inconsistent trends. A second mechanism may be impaired Toll-like receptor (TLR) signaling/reduced antigen-presenting cells. Stimulation of TLR2, -3, -4, -7, -8, and -9 can induce kynurenine production via tryptophan catabolism, while stimulation of TLR3 (activated by double-stranded RNA, the component of RV genomes) can also increase the levels of downstream metabolites (65). In mice, protein malnutrition decreases the number of macrophages (66), and we found reduced plasmacytoid dendritic cells and CD103+ MNCs in deficient HIFM/HRV pigs (26). Finally, while during the initial stages of protein deficiency reserve proteins and amino acids are metabolized for energy, in extended periods of protein deficiency continued loss of cell proteins would be lethal. Therefore, protein turnover and amino acid degradation pathways are suppressed (reviewed in reference 67). In humans and rats who consume protein-deficient diets, there is a suppression of protein turnover and amino acid degradation in muscle (68–70). Furthermore, children with severe edematous malnutrition have been shown to have slowed breakdown of body protein, which decreases the availability of many amino acids, resulting in decreased production of plasma proteins involved in the acute phase of the immune response and nutrient transport (71).
Serum ACE2 concentrations were significantly higher in sufficient HIFM/HRV pigs pre-HRV inoculation and at PID14 than in deficient HIFM/HRV pigs. ACE2 concentrations decreased at PID2 in a similar manner as tryptophan in sufficient HIFM/HRV pigs. Results from our previous study (26) concerning the detrimental effects of protein and tryptophan deficiency on intestinal epithelial cell health in deficient HIFM/HRV pigs are consistent with the beneficial tryptophan-mediated effects through ACE2 (35). Others have shown that ACE2 deficiency results in increased angiotensin II-exacerbated H5N1 influenza virus-induced injury in the lungs of mice and that treatment with recombinant human ACE2 (rhACE2) ameliorated the injury (72). Our results are suggestive of tryptophan-ACE2 involvement in immune activation and homeostatic control in sufficient HIFM/HRV pigs that is altered in the deficient pigs.
Systemic CD4+ CD25+ Foxp3+ Treg frequencies were higher in the deficient HIFM/HRV pigs, which coincides with the decreased CD3+ CD4+ Th cell frequencies seen in these pigs. Supplementing deficient and sufficient HIFM/HRV pigs with dietary tryptophan resulted in increased frequencies of CD4+ CD25+ FoxP3+ and CD8+ CD25+ FoxP3+ Tregs in systemic or intestinal tissues at PID14, with the exception of the CD8+ CD25+ FoxP3+ cells in the ileum of deficient HIFM/HRV pigs. Systemically, tryptophan supplementation raised CD4+ CD25+ FoxP3+ Tregs to significantly higher frequencies in the deficient HIFM/HRV pigs than in the sufficient HIFM/HRV pigs (Fig. 4A). The lack of increased CD8+ CD25+ FoxP3+ cell frequencies in the ileum of the supplemented deficient HIFM/HRV pigs is consistent with the higher frequencies of CD3+ CD8+ CTLs in the unsupplemented deficient HIFM/HRV pigs, as tryptophan supplementation did not reduce HRV shedding (unpublished data). No other parameters tested, including Th cell or CTL frequencies, were affected by tryptophan supplementation. Supplemental tryptophan was likely available for catabolism by the IDO pathway, leading to kynurenine production and enhanced Treg activation. Increased frequencies of Tregs contribute to decreased proinflammatory cytokines and T effector cell responses, decreasing intestinal and systemic inflammation, intestinal permeability, and malabsorption and thereby alleviating the negative effects of malnutrition.
In conclusion, our results indicate that protein malnutrition in HIFM-transplanted pigs infected with HRV compromised adaptive immune responses and amino acid homeostasis. In future studies, this model will be used to test if intervention strategies such as nutritional supplements and immunomodulatory probiotics can be used to overcome the immune impairment.
MATERIALS AND METHODS
Human infant fecal microbiota.
The collection and use of infant fecal samples were approved by The Ohio State University Institutional Review Board (IRB). With parental consent, human infant fecal samples were collected from the soiled diapers of a healthy, 2-month-old, exclusively breastfed, vaginally delivered infant. The fecal samples were pooled, weighed, diluted 1:20 (wt/vol) in phosphate buffer solution containing 0.05% (wt/vol) cysteine and 30% sterile glycerol, and stored at −80°C as described previously (26).
Virus.
The Gn pig-adapted (passage 23) HRV Wa G1P[8] strain (virHRV) was administered orally to Gn pigs at a dose of 106 fluorescent focus units (FFU) in 3 ml of minimum essential medium (MEM; Thermo Fisher Scientific, Waltham, MA, USA), immediately after oral administration of 3 ml of 100 mM sodium bicarbonate to reduce gastric acidity as described previously (14).
Animal experiments.
All animal experiments were approved by the Institutional Animal Care and Use Committee at The Ohio State University. Near-term pregnant sows (Landrace × Yorkshire × Duroc cross-bred) from The Ohio State University swine center facility were used to derive the Gn pigs by cesarean section, and the Gn pigs were maintained in sterile isolators as described previously (73). Pigs were randomly assigned to one of four groups: (i) protein-sufficient diet (n = 10), (ii) protein-deficient diet (n = 18), (iii) protein-sufficient diet with 0.4-g/day tryptophan supplementation (n = 3), or (iv) protein-deficient diet with tryptophan supplementation (n = 3). T cell experiments were conducted in only a subset of pigs. Protein-sufficient pigs received 100% ultrahigh-temperature-pasteurized (UHT) bovine milk (Parmalat) that met or exceeded the National Research Council (NRC) Animal Care Committee's guidelines for calories, fat, protein, and carbohydrates in suckling piglets. Protein-deficient pigs were given a diet of 50% Parmalat and 50% sterile water, which fell within NRC standards for calories, fat, and carbohydrates, while protein levels were half the recommended levels (7.5% versus 15% of diet). To confirm sterility from bacterial or fungal contamination prior to HIFM transplant, aerobic and anaerobic cultures of rectal swabs were performed. Additionally, all piglets were confirmed negative for the enteric viruses—rotavirus, transmissible gastroenteritis virus, porcine epidemic diarrhea virus, calicivirus/sapovirus, astrovirus, and kobuvirus—prior to HIFM inoculation. Four days postderivation, Gn pigs were inoculated orally with HIFM. Nine to 10 days were allowed for the establishment and stabilization of the fecal microbiota transplant (26; also Kumar et al., submitted). At postfecal microbiota day 9 or 10 (PFMTD9 or PFMTD10, respectively), pigs were inoculated with virHRV (PID0). All pigs were humanely euthanized by electrocution following anesthesia at PID14.
Antibody, tryptophan, and ACE2 ELISAs.
IgM, IgG, and IgA HRV antibody geometric mean titers (GMTs) and total IgA concentrations in serum were measured by enzyme-linked immunosorbent assay (ELISA) pre-virHRV inoculation (PFMTD9 or PFMTD10/PID0), post-virHRV inoculation (PID9), and at the termination of the experiment (PID14) as described previously (16, 21, 74). The same parameters were measured in the small intestinal contents at PID14. Serum tryptophan and ACE2 concentrations were quantitatively determined by competitive ELISA pre-virHRV inoculation (PFMTD9 or PFMTD10/PID0), 48 to 72 h post-virHRV inoculation (PID2), and at PID14, by comparison of the absorbance of the unknown samples with a reference curve generated from known standards according to the manufacturer's instructions (tryptophan ELISA kit from Rocky Mountain Diagnostics, Colorado Springs, CO, and porcine ACE2 ELISA kit from NeoBioLab, Cambridge, MA).
Isolation of MNCs and flow cytometry.
Blood, duodenum, ileum, and spleen were collected to isolate mononuclear cells (MNCs) as described previously (17). Result acquisition was done using a MACSQuant Analyzer 10 (Miltenyi Biotec, Bergisch Gladbach, Germany), and analysis was performed using FlowJo software version 10 (FlowJo LLC, Ashland, OR). To determine Th cells (CD3+ CD4+) and cytotoxic T lymphocytes (CTLs [CD3+ CD8+]), we stained each sample with anti-porcine CD3− fluorescein isothiocyanate (FITC; clone PPT3; Southern Biotech, Birmingham, AL), CD4− phycoerythrin (PE; clone 74-12-4; BD Biosciences, San Jose, CA), and CD8-spectral red (SPRD; clone 76-2-11; BD Biosciences) for 15 min at 4°C. The frequency of T cells was expressed as the percentage among total MNCs (determined based on forward and side scatter characteristics). The frequencies of natural regulatory T cells (Tregs; CD4+ CD25+ Foxp3+ and CD8+ CD25+ Foxp3+) were determined as described previously (17).
Statistics.
Results were tested for normality using the D'Agostino-Pearson omnibus test. Differences in HRV antibody isotype titers, total IgA concentrations, CD3+ CD4+ Th cell and CD3+ CD8+ cytotoxic T cell frequencies, and ACE2 were analyzed by the Mann-Whitney test. Differences in tryptophan concentrations between and among groups were analyzed with unpaired t tests, and differences in CD4+ CD25+ FoxP3+/CD8+ CD25+ FoxP3+ frequencies were calculated using 2-way analysis of variance (ANOVA) and Bonferroni's multiple-comparison test. All statistical analyses were performed using GraphPad Prism version 5 (GraphPad Software, Inc., CA, USA). P values of <0.05 were considered statistically significant for all comparisons.
ACKNOWLEDGMENTS
This work was supported by the Bill and Melinda Gates Foundation (OPP 1117467), the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (R01 A1099451), and federal and state funds appropriated to the Ohio Agricultural Research and Development Center, The Ohio State University.
We thank Marcia Lee and John Blankenship for their technical assistance and Juliette Hanson, Ronna Wood, Jeffrey Ogg, Megan Strother, and Sara Tallmadge for animal care assistance.
REFERENCES
- 1.Brennhofer S, Reifsnider E, Bruening M. 2016. Malnutrition coupled with diarrheal and respiratory infections among children in Asia: a systematic review. Public Health Nurs doi: 10.1111/phn.12273. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. 9 September 2015. Child mortality rates plunge by more than half since 1990 but global MDG target missed by wide margin. World Health Organization, Geneva, Switzerland: http://www.who.int/mediacentre/news/releases/2015/child-mortality-report/en/. [Google Scholar]
- 3.Scrimshaw NS, Taylor CE, Gordon JE. 1968. Interactions of nutrition and infection. Monogr Ser World Health Organ 57:3–329. [PubMed] [Google Scholar]
- 4.Schaible UE, Kaufmann SH. 2007. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med 4:e115. doi: 10.1371/journal.pmed.0040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mukhopadhyay DK, Biswas R, Chakraborty M, Sadhukhan SK, Banik KK. 2009. Anthropometric failure, a new approach to measure undernutrition: an experience from a rural community of West Bengal, India. J Indian Med Assoc 107:211–214. [PubMed] [Google Scholar]
- 6.Checkley W, Buckley G, Gilman RH, Assis AM, Guerrant RL, Morris SS, Molbak K, Valentiner-Branth P, Lanata CF, Black RE, Childhood Malnutrition and Infection Network. 2008. Multi-country analysis of the effects of diarrhoea on childhood stunting. Int J Epidemiol 37:816–830. doi: 10.1093/ije/dyn099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guerrant RL, DeBoer MD, Moore SR, Scharf RJ, Lima AA. 2013. The impoverished gut—a triple burden of diarrhoea, stunting and chronic disease. Nat Rev Gastroenterol Hepatol 10:220–229. doi: 10.1038/nrgastro.2012.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atherly D, Dreibelbis R, Parashar UD, Levin C, Wecker J, Rheingans RD. 2009. Rotavirus vaccination: cost-effectiveness and impact on child mortality in developing countries. J Infect Dis 200(Suppl 1):S28–S38. doi: 10.1086/605033. [DOI] [PubMed] [Google Scholar]
- 9.Tate JE, Burton AH, Boschi-Pinto C, Parashar UD, World Health Organization-Coordinated Global Rotavirus Surveillance Network 2016. Global, regional, and national estimates of rotavirus mortality in children <5 years of age, 2000–2013. Clin Infect Dis 62(Suppl 2):S96–S105. doi: 10.1093/cid/civ1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lundgren O, Svensson L. 2001. Pathogenesis of rotavirus diarrhea. Microbes Infect 3:1145–1156. doi: 10.1016/S1286-4579(01)01475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costa LB, Noronha FJ, Roche JK, Sevilleja JE, Warren CA, Oria R, Lima A, Guerrant RL. 2012. Novel in vitro and in vivo models and potential new therapeutics to break the vicious cycle of Cryptosporidium infection and malnutrition. J Infect Dis 205:1464–1471. doi: 10.1093/infdis/jis216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bolick DT, Roche JK, Hontecillas R, Bassaganya-Riera J, Nataro JP, Guerrant RL. 2013. Enteroaggregative Escherichia coli strain in a novel weaned mouse model: exacerbation by malnutrition, biofilm as a virulence factor and treatment by nitazoxanide. J Med Microbiol 62:896–905. doi: 10.1099/jmm.0.046300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saif LJ, Ward LA, Yuan L, Rosen BI, To TL. 1996. The gnotobiotic piglet as a model for studies of disease pathogenesis and immunity to human rotaviruses. Arch Virol Suppl 12:153–161. [DOI] [PubMed] [Google Scholar]
- 14.Ward LA, Rosen BI, Yuan L, Saif LJ. 1996. Pathogenesis of an attenuated and a virulent strain of group A human rotavirus in neonatal gnotobiotic pigs. J Gen Virol 77:1431–1441. doi: 10.1099/0022-1317-77-7-1431. [DOI] [PubMed] [Google Scholar]
- 15.Gonzalez AM, Azevedo MS, Jung K, Vlasova A, Zhang W, Saif LJ. 2010. Innate immune responses to human rotavirus in the neonatal gnotobiotic piglet disease model. Immunology 131:242–256. doi: 10.1111/j.1365-2567.2010.03298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chattha KS, Vlasova AN, Kandasamy S, Esseili MA, Siegismund C, Rajashekara G, Saif LJ. 2013. Probiotics and colostrum/milk differentially affect neonatal humoral immune responses to oral rotavirus vaccine. Vaccine 31:1916–1923. doi: 10.1016/j.vaccine.2013.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chattha KS, Vlasova AN, Kandasamy S, Rajashekara G, Saif LJ. 2013. Divergent immunomodulating effects of probiotics on T cell responses to oral attenuated human rotavirus vaccine and virulent human rotavirus infection in a neonatal gnotobiotic piglet disease model. J Immunol 191:2446–2456. doi: 10.4049/jimmunol.1300678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kandasamy S, Vlasova AN, Fischer D, Kumar A, Chattha KS, Rauf A, Shao L, Langel SN, Rajashekara G, Saif LJ. 2016. Differential effects of Escherichia coli Nissle and Lactobacillus rhamnosus strain GG on human rotavirus binding, infection, and B cell immunity. J Immunol 196:1780–1789. doi: 10.4049/jimmunol.1501705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vlasova AN, Kandasamy S, Chattha KS, Rajashekara G, Saif LJ. 2016. Comparison of probiotic lactobacilli and bifidobacteria effects, immune responses and rotavirus vaccines and infection in different host species. Vet Immunol Immunopathol 172:72–84. doi: 10.1016/j.vetimm.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vlasova AN, Shao L, Kandasamy S, Fischer DD, Rauf A, Langel SN, Chattha KS, Kumar A, Huang HC, Rajashekara G, Saif LJ. 2016. Escherichia coli Nissle 1917 protects gnotobiotic pigs against human rotavirus by modulating pDC and NK-cell responses. Eur J Immunol 46:2426–2437. doi: 10.1002/eji.201646498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang W, Azevedo MS, Gonzalez AM, Saif LJ, Van Nguyen T, Wen K, Yousef AE, Yuan L. 2008. Influence of probiotic lactobacilli colonization on neonatal B cell responses in a gnotobiotic pig model of human rotavirus infection and disease. Vet Immunol Immunopathol 122:175–181. doi: 10.1016/j.vetimm.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kandasamy S, Chattha KS, Vlasova AN, Rajashekara G, Saif LJ. 2014. Lactobacilli and bifidobacteria enhance mucosal B cell responses and differentially modulate systemic antibody responses to an oral human rotavirus vaccine in a neonatal gnotobiotic pig disease model. Gut Microbes 5:639–651. doi: 10.4161/19490976.2014.969972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pang X, Hua X, Yang Q, Ding D, Che C, Cui L, Jia W, Bucheli P, Zhao L. 2007. Inter-species transplantation of gut microbiota from human to pigs. ISME J 1:156–162. doi: 10.1038/ismej.2007.23. [DOI] [PubMed] [Google Scholar]
- 24.Wang H, Gao K, Wen K, Allen IC, Li G, Zhang W, Kocher J, Yang X, Giri-Rachman E, Li GH, Clark-Deener S, Yuan L. 2016. Lactobacillus rhamnosus GG modulates innate signaling pathway and cytokine responses to rotavirus vaccine in intestinal mononuclear cells of gnotobiotic pigs transplanted with human gut microbiota. BMC Microbiol 16:109. doi: 10.1186/s12866-016-0727-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang H, Wang H, Shepherd M, Wen K, Li G, Yang X, Kocher J, Giri-Rachman E, Dickerman A, Settlage R, Yuan L. 2014. Probiotics and virulent human rotavirus modulate the transplanted human gut microbiota in gnotobiotic pigs. Gut Pathog 6:39. doi: 10.1186/s13099-014-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vlasova AN, Paim FC, Kandasamy S, Alhamo MA, Fischer DD, Langel SN, Deblais L, Kumar A, Chepngeno J, Shao L, Huang HC, Candelero-Rueda RA, Rajashekara G, Saif LJ. 2017. Protein malnutrition modifies innate immunity and gene expression by intestinal epithelial cells and human rotavirus infection in neonatal gnotobiotic pigs. mSphere 2:e00046-17. doi: 10.1128/mSphere.00046-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zijlstra RT, McCracken BA, Odle J, Donovan SM, Gelberg HB, Petschow BW, Zuckermann FA, Gaskins HR. 1999. Malnutrition modifies pig small intestinal inflammatory responses to rotavirus. J Nutr 129:838–843. [DOI] [PubMed] [Google Scholar]
- 28.Fabiansen C, Lykke M, Hother AL, Koch J, Nielsen OB, Hunter I, Goetze JP, Friis H, Thymann T. 2015. Cardiac dysfunction in a porcine model of pediatric malnutrition. PLoS One 10:e0140472. doi: 10.1371/journal.pone.0140472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lykke M, Hother AL, Hansen CF, Friis H, Molgaard C, Michaelsen KF, Briend A, Larsen T, Sangild PT, Thymann T. 2013. Malnutrition induces gut atrophy and increases hepatic fat infiltration: studies in a pig model of childhood malnutrition. Am J Transl Res 5:543–554. [PMC free article] [PubMed] [Google Scholar]
- 30.Garas LC, Feltrin C, Hamilton MK, Hagey JV, Murray JD, Bertolini LR, Bertolini M, Raybould HE, Maga EA. 2016. Milk with and without lactoferrin can influence intestinal damage in a pig model of malnutrition. Food Funct 7:665–678. doi: 10.1039/C5FO01217A. [DOI] [PubMed] [Google Scholar]
- 31.Jacobi SK, Moeser AJ, Blikslager AT, Rhoads JM, Corl BA, Harrell RJ, Odle J. 2013. Acute effects of rotavirus and malnutrition on intestinal barrier function in neonatal piglets. World J Gastroenterol 19:5094–5102. doi: 10.3748/wjg.v19.i31.5094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Camargo SM, Singer D, Makrides V, Huggel K, Pos KM, Wagner CA, Kuba K, Danilczyk U, Skovby F, Kleta R, Penninger JM, Verrey F. 2009. Tissue-specific amino acid transporter partners ACE2 and collectrin differentially interact with hartnup mutations. Gastroenterology 136:872–882. doi: 10.1053/j.gastro.2008.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kowalczuk S, Broer A, Tietze N, Vanslambrouck JM, Rasko JE, Broer S. 2008. A protein complex in the brush-border membrane explains a Hartnup disorder allele. FASEB J 22:2880–2887. doi: 10.1096/fj.08-107300. [DOI] [PubMed] [Google Scholar]
- 34.Singer D, Camargo SM. 2011. Collectrin and ACE2 in renal and intestinal amino acid transport. Channels (Austin) 5:410–423. doi: 10.4161/chan.5.5.16470. [DOI] [PubMed] [Google Scholar]
- 35.Hashimoto T, Perlot T, Rehman A, Trichereau J, Ishiguro H, Paolino M, Sigl V, Hanada T, Hanada R, Lipinski S, Wild B, Camargo SM, Singer D, Richter A, Kuba K, Fukamizu A, Schreiber S, Clevers H, Verrey F, Rosenstiel P, Penninger JM. 2012. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature 487:477–481. doi: 10.1038/nature11228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nuss ET, Tanumihardjo SA. 2011. Quality protein maize for Africa: closing the protein inadequacy gap in vulnerable populations. Adv Nutr 2:217–224. doi: 10.3945/an.110.000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Semba RD, Shardell M, Sakr Ashour FA, Moaddel R, Trehan I, Maleta KM, Ordiz MI, Kraemer K, Khadeer MA, Ferrucci L, Manary MJ. 2016. Child stunting is associated with low circulating essential amino acids. EBioMedicine 6:246–252. doi: 10.1016/j.ebiom.2016.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guerrant RL, Leite AM, Pinkerton R, Medeiros PH, Cavalcante PA, DeBoer M, Kosek M, Duggan C, Gewirtz A, Kagan JC, Gauthier AE, Swann J, Mayneris-Perxachs J, Bolick DT, Maier EA, Guedes MM, Moore SR, Petri WA, Havt A, Lima IF, Prata MM, Michaleckyj JC, Scharf RJ, Sturgeon C, Fasano A, Lima AA. 2016. Biomarkers of environmental enteropathy, inflammation, stunting, and impaired growth in children in northeast Brazil. PLoS One 11:e0158772. doi: 10.1371/journal.pone.0158772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mehraj V, Routy JP. 2015. Tryptophan catabolism in chronic viral infections: handling uninvited guests. Int J Tryptophan Res 8:41–48. doi: 10.4137/IJTR.S26862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coulson BS, Grimwood K, Hudson IL, Barnes GL, Bishop RF. 1992. Role of coproantibody in clinical protection of children during reinfection with rotavirus. J Clin Microbiol 30:1678–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matson DO, O'Ryan ML, Herrera I, Pickering LK, Estes MK. 1993. Fecal antibody responses to symptomatic and asymptomatic rotavirus infections. J Infect Dis 167:577–583. doi: 10.1093/infdis/167.3.577. [DOI] [PubMed] [Google Scholar]
- 42.O'Ryan ML, Matson DO, Estes MK, Pickering LK. 1994. Acquisition of serum isotype-specific and G type-specific antirotavirus antibodies among children in day care centers. Pediatr Infect Dis J 13:890–895. doi: 10.1097/00006454-199410000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Hjelt K, Grauballe PC, Paerregaard A, Nielsen OH, Krasilnikoff PA. 1987. Protective effect of preexisting rotavirus-specific immunoglobulin A against naturally acquired rotavirus infection in children. J Med Virol 21:39–47. doi: 10.1002/jmv.1890210106. [DOI] [PubMed] [Google Scholar]
- 44.Yuan L, Ward LA, Rosen BI, To TL, Saif LJ. 1996. Systematic and intestinal antibody-secreting cell responses and correlates of protective immunity to human rotavirus in a gnotobiotic pig model of disease. J Virol 70:3075–3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Azevedo MS, Yuan L, Iosef C, Chang KO, Kim Y, Nguyen TV, Saif LJ. 2004. Magnitude of serum and intestinal antibody responses induced by sequential replicating and nonreplicating rotavirus vaccines in gnotobiotic pigs and correlation with protection. Clin Diagn Lab Immunol 11:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.To TL, Ward LA, Yuan L, Saif LJ. 1998. Serum and intestinal isotype antibody responses and correlates of protective immunity to human rotavirus in a gnotobiotic pig model of disease. J Gen Virol 79:2661–2672. doi: 10.1099/0022-1317-79-11-2661. [DOI] [PubMed] [Google Scholar]
- 47.Desselberger U, Huppertz HI. 2011. Immune responses to rotavirus infection and vaccination and associated correlates of protection. J Infect Dis 203:188–195. doi: 10.1093/infdis/jiq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reddy V, Raghuramulu N, Bhaskaram C. 1976. Secretory IgA in protein-calorie malnutrition. Arch Dis Child 51:871–874. doi: 10.1136/adc.51.11.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sirisinha S, Suskind R, Edelman R, Asvapaka C, Olson RE. 1975. Secretory and serum IgA in children with protein-calorie malnutrition. Pediatrics 55:166–170. [PubMed] [Google Scholar]
- 50.McGee DW, McMurray DN. 1988. The effect of protein malnutrition on the IgA immune response in mice. Immunology 63:25–29. [PMC free article] [PubMed] [Google Scholar]
- 51.Nikawa T, Odahara K, Koizumi H, Kido Y, Teshima S, Rokutan K, Kishi K. 1999. Vitamin A prevents the decline in immunoglobulin A and Th2 cytokine levels in small intestinal mucosa of protein-malnourished mice. J Nutr 129:934–941. [DOI] [PubMed] [Google Scholar]
- 52.Suliman OS, Salih MA, Karrar ZA, Mohammed AO, Helsing C. 2011. Infection and immunoglobulin levels in Sudanese children with severe protein-energy malnutrition. Sudan J Paediatr 11:32–42. [PMC free article] [PubMed] [Google Scholar]
- 53.Chandra RK, Chakraburty S, Chandra S. 1976. Malnutrition, humoral immunity and infection. Indian J Pediatr 43:159–171. doi: 10.1007/BF02894341. [DOI] [PubMed] [Google Scholar]
- 54.Najjar SS, Stephan M, Asfour RY. 1969. Serum levels of immunoglobulins in marasmic infants. Arch Dis Child 44:120–123. doi: 10.1136/adc.44.233.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chandra RK, Ghai OP. 1972. Serum immunoglobulins in healthy children from birth to adolescence. Indian J Med Res 60:89–96. [PubMed] [Google Scholar]
- 56.Omer HO, Omer MI, Khalifa OO. 1975. Pattern of protein-energy malnutrition in Sudanese children and comparison with some other Middle East countries. J Trop Pediatr Environ Child Health 21:329–333. [DOI] [PubMed] [Google Scholar]
- 57.Presley LL, Wei B, Braun J, Borneman J. 2010. Bacteria associated with immunoregulatory cells in mice. Appl Environ Microbiol 76:936–941. doi: 10.1128/AEM.01561-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johansson-Lindbom B, Svensson M, Pabst O, Palmqvist C, Marquez G, Forster R, Agace WW. 2005. Functional specialization of gut CD103+ dendritic cells in the regulation of tissue-selective T cell homing. J Exp Med 202:1063–1073. doi: 10.1084/jem.20051100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schmidt SV, Schultze JL. 2014. New insights into IDO biology in bacterial and viral infections. Front Immunol 5:384. doi: 10.3389/fimmu.2014.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Daubener W, Spors B, Hucke C, Adam R, Stins M, Kim KS, Schroten H. 2001. Restriction of Toxoplasma gondii growth in human brain microvascular endothelial cells by activation of indoleamine 2,3-dioxygenase. Infect Immun 69:6527–6531. doi: 10.1128/IAI.69.10.6527-6531.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Obojes K, Andres O, Kim KS, Daubener W, Schneider-Schaulies J. 2005. Indoleamine 2,3-dioxygenase mediates cell type-specific anti-measles virus activity of gamma interferon. J Virol 79:7768–7776. doi: 10.1128/JVI.79.12.7768-7776.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adams O, Besken K, Oberdorfer C, MacKenzie CR, Russing D, Daubener W. 2004. Inhibition of human herpes simplex virus type 2 by interferon gamma and tumor necrosis factor alpha is mediated by indoleamine 2,3-dioxygenase. Microbes Infect 6:806–812. doi: 10.1016/j.micinf.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 63.Adams O, Besken K, Oberdorfer C, MacKenzie CR, Takikawa O, Daubener W. 2004. Role of indoleamine-2,3-dioxygenase in alpha/beta and gamma interferon-mediated antiviral effects against herpes simplex virus infections. J Virol 78:2632–2636. doi: 10.1128/JVI.78.5.2632-2636.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Terajima M, Leporati AM. 2005. Role of indoleamine 2,3-dioxygenase in antiviral activity of interferon-gamma against vaccinia virus. Viral Immunol 18:722–729. doi: 10.1089/vim.2005.18.722. [DOI] [PubMed] [Google Scholar]
- 65.Orhan F, Bhat M, Sandberg K, Stahl S, Piehl F, Karolinska Schizophrenia Project (KaSP) Consortium, Svensson C, Erhardt S, Schwieler L. 2016. Tryptophan metabolism along the kynurenine pathway downstream of Toll-like receptor stimulation in peripheral monocytes. Scand J Immunol 84:262–271. doi: 10.1111/sji.12479. [DOI] [PubMed] [Google Scholar]
- 66.Redmond HP, Gallagher HJ, Shou J, Daly JM. 1995. Antigen presentation in protein-energy malnutrition. Cell Immunol 163:80–87. doi: 10.1006/cimm.1995.1101. [DOI] [PubMed] [Google Scholar]
- 67.Lecker SH, Solomon V, Mitch WE, Goldberg AL. 1999. Muscle protein breakdown and the critical role of the ubiquitin-proteasome pathway in normal and disease states. J Nutr 129:227S–237S. [DOI] [PubMed] [Google Scholar]
- 68.May RC, Piepenbrock N, Kelly RA, Mitch WE. 1991. Leucine-induced amino acid antagonism in rats: muscle valine metabolism and growth impairment. J Nutr 121:293–301. [DOI] [PubMed] [Google Scholar]
- 69.Tawa NE Jr, Goldberg AL. 1992. Suppression of muscle protein turnover and amino acid degradation by dietary protein deficiency. Am J Physiol 263:E317–E325. [DOI] [PubMed] [Google Scholar]
- 70.Young V. 1986. Some metabolic and nutritional considerations of dietary protein restriction, p 263–283. In Mitch W. (ed), Contemporary issues in nephrology: the progressive nature of renal disease. Churchill Livingstone, New York, NY. [Google Scholar]
- 71.Jahoor F, Badaloo A, Reid M, Forrester T. 2008. Protein metabolism in severe childhood malnutrition. Ann Trop Paediatr 28:87–101. doi: 10.1179/146532808X302107. [DOI] [PubMed] [Google Scholar]
- 72.Zou Z, Yan Y, Shu Y, Gao R, Sun Y, Li X, Ju X, Liang Z, Liu Q, Zhao Y, Guo F, Bai T, Han Z, Zhu J, Zhou H, Huang F, Li C, Lu H, Li N, Li D, Jin N, Penninger JM, Jiang C. 2014. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nat Commun 5:3594. doi: 10.1038/ncomms4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Meyer RC, Bohl EH, Kohler EM. 1964. Procurement and maintenance of germ-free swine for microbiological investigations. Appl Microbiol 12:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parreno V, Hodgins DC, de Arriba L, Kang SY, Yuan L, Ward LA, To TL, Saif LJ. 1999. Serum and intestinal isotype antibody responses to Wa human rotavirus in gnotobiotic pigs are modulated by maternal antibodies. J Gen Virol 80:1417–1428. doi: 10.1099/0022-1317-80-6-1417. [DOI] [PubMed] [Google Scholar]