Abstract
BACKGROUND
Few studies have evaluated the relationship between changes in diet quality over time and the risk of death.
METHODS
We used Cox proportional-hazards models to calculate adjusted hazard ratios for total and cause-specific mortality among 47,994 women in the Nurses’ Health Study and 25,745 men in the Health Professionals Follow-up Study from 1998 through 2010. Changes in diet quality over the preceding 12 years (1986–1998) were assessed with the use of the Alternate Healthy Eating Index–2010 score, the Alternate Mediterranean Diet score, and the Dietary Approaches to Stop Hypertension (DASH) diet score.
RESULTS
The pooled hazard ratios for all-cause mortality among participants who had the greatest improvement in diet quality (13 to 33% improvement), as compared with those who had a relatively stable diet quality (0 to 3% improvement), in the 12-year period were the following: 0.91 (95% confidence interval [CI], 0.85 to 0.97) according to changes in the Alternate Healthy Eating Index score, 0.84 (95 CI%, 0.78 to 0.91) according to changes in the Alternate Mediterranean Diet score, and 0.89 (95% CI, 0.84 to 0.95) according to changes in the DASH score. A 20-percentile increase in diet scores (indicating an improved quality of diet) was significantly associated with a reduction in total mortality of 8 to 17% with the use of the three diet indexes and a 7 to 15% reduction in the risk of death from cardiovascular disease with the use of the Alternate Healthy Eating Index and Alternate Mediterranean Diet. Among participants who maintained a high-quality diet over a 12-year period, the risk of death from any cause was significantly lower — by 14% (95% CI, 8 to 19) when assessed with the Alternate Healthy Eating Index score, 11% (95% CI, 5 to 18) when assessed with the Alternate Mediterranean Diet score, and 9% (95% CI, 2 to 15) when assessed with the DASH score — than the risk among participants with consistently low diet scores over time.
CONCLUSIONS
Improved diet quality over 12 years was consistently associated with a decreased risk of death.
Some epidemiologic studies of nutrition focus on dietary patterns rather than single nutrients or foods to evaluate the association between diet and health outcomes.1 Accumulated evidence supports an association between healthy dietary patterns and a decreased risk of death.2–11 Results from recent studies suggest that improved diet quality, as assessed by means of the Alternate Healthy Eating Index–2010 score,12 the Alternate Mediterranean Diet score,10,13 and the Dietary Approaches to Stop Hypertension (DASH) diet score,14 was associated with reductions of 8% to 22% in the risk of death from any cause15,16 and reductions of 19% to 28% in the risk of death from cardiovascular disease and 11% to 23% in the risk of death from cancer.2–4,17
Given such consistent evidence, the 2015 Dietary Guidelines for Americans recommended the Alternate Healthy Eating Index, the Alternate Mediterranean Diet, and DASH as practical, understandable, and actionable diet plans for the public.18 Such guidelines are important in the United States and globally because unhealthy diets have been ranked as a major factor contributing to death and health complications.19 Evaluation of changes in diet quality over time in relation to the subsequent risk of death would be important. Here, we evaluated the association between 12-year changes (from 1986 through 1998) in the three diet-quality scores noted above and the subsequent risk of total and cause-specific death from 1998 through 2010 among participants in the Nurses’ Health Study and the Health Professionals Follow-up Study. We also examined short-term changes (baseline to 8-year follow-up, 1986–1994) and long-term changes (baseline to 16-year follow-up, 1986–2002) in diet quality in relation to total and cause-specific mortality.
METHODS
STUDY POPULATION AND DESIGN
The Nurses’ Health Study, a prospective study that was initiated in 1976, enrolled 121,700 registered nurses who were 30 to 55 years of age. The Health Professionals Follow-up Study, a prospective study that was initiated in 1986, enrolled 51,529 U.S. health professionals who were 40 to 75 years of age. Baseline and follow-up questionnaires were sent to participants every 2 years to update medical and lifestyle information over the follow-up period.20,21 In both studies, follow-up rates exceeded 90% in both cohorts.22
For the present study, the initial cycle was set at 1986, baseline was set at 1998 (changes in diet quality were calculated from 1986 through 1998), and the end of follow-up was 2010. We excluded participants who had a history of cardiovascular disease or cancer at or before baseline in 1998, missing information regarding diet and lifestyle covariates, or very low or high caloric intake (<800 kcal or >4200 kcal per day in men and <500 or >3500 kcal per day in women). We also excluded participants who died before 1998. The final analysis included 47,994 women and 25,745 men.
STUDY OVERSIGHT
The first author formulated the study question and design, performed the statistical analyses, interpreted the results, and wrote the first draft of the manuscript. The second and fifth authors contributed to the development of the study questions and statistical analyses. The seventh, eighth, and last authors contributed to the conception and design of the study and acquisition of the data. All the authors contributed to the interpretation of data and critical revision of the manuscript, approved the final version, and made the decision to submit the manuscript for publication. The first and last authors share primary responsibility for the final content and vouch for the accuracy and completeness of the data and analyses.
DIETARY ASSESSMENT
At baseline and every 4 years thereafter, the participants reported information about their diets with the use of a validated food frequency questionnaire. They were asked how often, on average, they had consumed each food of a standard portion size in the past year. The reproducibility and validity of the food frequency questionnaires have been described previously.12,23,24
We calculated three diet-quality scores using food components and scoring criteria that have been described previously.25 Briefly, the Alternate Healthy Eating Index included 11 food components, each scored from 0 (unhealthy) to 10 (healthiest) and selected on the basis of evidence of an association with the risk of chronic disease.12 Total scores ranged from 0 to 110, with higher scores indicating a healthier diet. The Alternate Mediterranean Diet score included 9 components, each scored as 0 (unhealthy) or 1 (healthy) according to whether the participant’s intake was above or below the cohort-specific median levels.10,13 Total scores ranged from 0 to 9, with higher scores indicating a healthier diet. Finally, the DASH score included 8 components, each scored from 1 (unhealthy) to 5 (healthiest) according to a participant’s quintile of intake.14 Total DASH scores ranged from 8 to 40 points, with higher scores indicating a healthier diet. Further information is provided in Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org.
ASCERTAINMENT OF DEATHS
Deaths were identified from state vital statistics records and the National Death Index or reported by the participants’ families and the U.S. postal system.26 Using these methods, we could ascertain 98% of the deaths in each cohort.26 We attempted to obtain the death certificate of each participant who had died, and when appropriate, we requested permission from the participant’s next of kin to review medical records. The underlying cause of death, according to the International Classification of Diseases, Eighth Revision and Ninth Revision, was assigned by physicians after they had reviewed death certificates and medical records.
COVARIATES
Information on the participants’ lifestyle and risk factors for cardiovascular disease was assessed and updated every other year. This information included the following: the participant’s age; weight; smoking status; use of aspirin, multivitamins, postmenopausal hormone-replacement therapy, and oral contraceptives; menopausal status; physical activity; and hypertension, hypercholesterolemia, or diabetes that had been recently diagnosed by a physician. Alcohol use was assessed, and this information was updated from the food frequency questionnaires every 4 years. The participant’s height and weight were used to calculate the body-mass index (BMI; the weight in kilograms divided by the square of the height in meters). Detailed descriptions of the validity and reproducibility of body weight, physical activity, and alcohol consumption as reported by the participants have been published previously.27–29
STATISTICAL ANALYSIS
Changes in the three diet-quality scores were categorized into quintiles from the largest decrease (quintile 1) to the largest increase (quintile 5). Person-years were calculated from the date of return of the 1998 questionnaire to the date of death or the end of follow-up, whichever occurred first. Cox proportional-hazards models with time-varying covariates and age as the underlying time scale were used to estimate hazard ratios and 95% confidence intervals.
Model 1 was adjusted for the following factors: age; calendar year as the underlying time scale; initial diet-quality score (in quintiles); race; family history of myocardial infarction, diabetes, or cancer; use or nonuse of aspirin or multivitamins; initial BMI category; menopausal status and use or nonuse of hormone-replacement therapy in women; initial smoking status and changes in smoking status; initial smoking pack-year and changes in smoking pack-year (continuous variables) among participants with any history of smoking (ever smokers); and initial levels of physical activity and total energy intake and changes in these levels (in quintiles). In addition to these adjustments, model 2 was adjusted for a history of hypertension, hypercholesterolemia, or type 2 diabetes; change in weight; and the use or nonuse of cholesterol-lowering and antihypertensive medications. The model with the DASH score as the exposure was also adjusted for initial alcohol intake and changes in alcohol intake. Tests for trend were conducted by assigning a median value to each quintile. A 20-percentile increase in each score was calculated from the range of the diet score and the median value of each quintile. We also conducted restricted-cubic-spline regressions to flexibly model the association.
Shorter-term changes (baseline to 8-year follow-up, 1986–1994) and longer-term changes (baseline to 16-year follow-up, 1986–2002) in the three scores were tested for association with total and cause-specific mortality. We conducted several sensitivity analyses to test the robustness of our findings. First, we applied stratification analysis according to several potential confounding factors at baseline (e.g., age, BMI, diet, physical activity, and smoking status). Second, we conducted a 4-year lag analysis to account for the presence of any chronic diseases in the years after diagnosis that might have influenced dietary patterns. Third, because early detection and treatment of disease could confound results, in an additional model we adjusted for mammographic screening in women and physical checkups.
All analyses were performed separately for each cohort and then were pooled with the use of an inverse, variance-weighted meta-analysis with a fixed-effects model. Analyses were performed with the use of SAS software, version 9.4 for UNIX (SAS Institute). Statistical tests were two-sided, and P values of less than 0.05 were considered to indicate statistical significance.
RESULTS
LIFESTYLE CHARACTERISTICS OF THE PARTICIPANTS
Initial lifestyle characteristics and changes in these characteristics according to quintiles of change in the Alternate Healthy Eating Index score over 12 years are shown in Table 1. In both cohorts, participants with a greater increase in diet quality were younger, had a lower baseline diet score, engaged in more physical activity, and consumed less alcohol than participants with little change in diet quality. Participants with a greater increase in diet quality reported increased consumption of whole grains, vegetables, and n-3 fatty acids and decreased sodium intake over time (Table S2 in the Supplementary Appendix). Similar patterns were observed with assessments based on the Alternate Mediterranean Diet and DASH scores (Table S2 in the Supplementary Appendix). In general, participants with consistently high diet quality at baseline and 12 years later were older, had a lower BMI, were less likely to be current smokers, and were more physically active than those with a poor diet quality both at baseline and 12 years later (Table S3 in the Supplementary Appendix).
Table 1.
Characteristics of the Participants and Changes over Time, According to Quintiles of Change in the Alternate Healthy Eating Index–2010 Score over 12 Years.*
| Variable | Quintile of Change in Nurses’ Health Study | Quintile of Change in Health Professionals Follow-up Study | ||||
|---|---|---|---|---|---|---|
| Quintile 1 (Largest Decrease) (N = 9598) | Quintile 3 (Relatively No Change) (N = 9599) | Quintile 5 (Largest Increase) (N = 9599) | Quintile 1 (Largest Decrease) (N = 5149) | Quintile 3 (Relatively No Change) (N = 5149) | Quintile 5 (Largest Increase) (N = 5149) | |
| Diet score | ||||||
|
| ||||||
| Baseline | 60.1±10.1 | 50.8±9.8 | 44.7±9.7 | 60.8±10.5 | 52.1±10.5 | 46.3±10.2 |
|
| ||||||
| Change | −11.7±4.7 | 2.2±1.4 | 15.9±4.7 | −10.7±4.8 | 3.4±1.4 | 17.4±4.8 |
|
| ||||||
| Age (yr) | 65.4±7.1 | 63.5±7.0 | 62.4±6.7 | 64.6±9.2 | 63.6±8.9 | 63.2±8.7 |
|
| ||||||
| Initial body-mass index† | 25.1±4.4 | 25.2±4.6 | 24.9±4.7 | 25.5±3.1 | 25.3±3.1 | 25.1±3.0 |
|
| ||||||
| Weight change (kg) | 4.8±7.7 | 4.0±6.9 | 2.8±6.9 | 3.4±6.1 | 2.5±5.6 | 1.6±5.6 |
|
| ||||||
| Physical activity (MET-hr/wk) | ||||||
|
| ||||||
| Baseline | 15.1±20.6 | 13.2±18.7 | 12.8±18.8 | 24.0±37.0 | 21.9±27.0 | 20.9±28.3 |
|
| ||||||
| Change | 1.8±21.3 | 4.7±20.2 | 6.2±20.8 | 1.4±28.3 | 3.6±26.8 | 6.4±28.2 |
|
| ||||||
| Alcohol intake (g/day) | ||||||
|
| ||||||
| Baseline | 5.9±8.5 | 6.1±10.5 | 7.5±13.2 | 11.2±12.7 | 11.4±14.9 | 12.0±17.5 |
|
| ||||||
| Change | −0.4±7.6 | −1.0±6.9 | −2.3±9.3 | 1.8±12.1 | −0.5±10.2 | −2.1±12.7 |
|
| ||||||
| Energy intake (kcal/day) | ||||||
|
| ||||||
| Baseline | 1756±517 | 1798±506 | 1789±490 | 1962±600 | 2029±611 | 1972±573 |
|
| ||||||
| Change | −2.5±518 | −35.3±485 | −62.4±496 | 56.7±583 | −23.2±551 | −33.4±560 |
|
| ||||||
| White race (%)‡ | 99 | 98 | 97 | 97 | 96 | 95 |
|
| ||||||
| Smoking status (%) | ||||||
|
| ||||||
| Remained a never smoker | 42 | 48 | 47 | 44 | 48 | 50 |
|
| ||||||
| Change from current smoker to former smoker or remained former smoker | 47 | 42 | 44 | 46 | 43 | 43 |
|
| ||||||
| Change from never smoked or smoked in past to current smoker or remained current smoker | 10 | 10 | 9 | 5 | 5 | 4 |
|
| ||||||
| Smoking history among ever smokers (no. of pack-yr)§ | ||||||
|
| ||||||
| Baseline | 21.0±17.4 | 20.4±17.6 | 21.3±17.9 | 22.0±16.3 | 21.8±16.6 | 21.8±16.8 |
|
| ||||||
| Change | 2.7±5.0 | 2.7±5.0 | 2.7±4.8 | 1.2±3.6 | 1.2±3.7 | 1.1±3.7 |
|
| ||||||
| Past diagnoses (%) | ||||||
|
| ||||||
| Hypertension | 44 | 43 | 43 | 36 | 33 | 33 |
|
| ||||||
| High cholesterol | 56 | 56 | 59 | 44 | 47 | 49 |
|
| ||||||
| Diabetes | 6 | 6 | 8 | 5 | 6 | 7 |
|
| ||||||
| Current use of medication or supplements (%) | ||||||
|
| ||||||
| Aspirin | 53 | 54 | 55 | 64 | 66 | 64 |
|
| ||||||
| Multivitamins | 62 | 62 | 63 | 60 | 59 | 62 |
|
| ||||||
| Antihypertensive medication | 37 | 36 | 35 | 28 | 27 | 26 |
|
| ||||||
| Cholesterol-lowering medication | 14 | 14 | 15 | 13 | 14 | 14 |
|
| ||||||
| Family history (%) | ||||||
|
| ||||||
| Myocardial infarction | 25 | 25 | 25 | 33 | 32 | 32 |
|
| ||||||
| Diabetes | 30 | 30 | 29 | 23 | 23 | 24 |
Plus–minus values are means ±SD. All variables except age are age-standardized. Scores on the Alternate Healthy Eating Index–2010 range from 0 to 110, with higher scores indicating a healthier diet. MET denotes metabolic equivalent.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Race was reported by the participants.
A pack-year is defined as the equivalent of smoking one pack of cigarettes (20 cigarettes) per day for 1 year.
In the Nurses’ Health Study, we documented 5967 deaths, including 1115 deaths from cardiovascular disease and 2089 deaths from cancer over 544,973 person-years of follow-up. In the Health Professionals Follow-up Study, we documented 3979 deaths, including 1226 deaths from cardiovascular disease and 1192 deaths from cancer during 286,402 person-years of follow-up.
TOTAL MORTALITY AND DIET QUALITY
Multivariable analyses showed a significant inverse association across quintiles of change over 12 years between each of the three diet-quality scores and total mortality (P<0.05 for trend) (Table S4 in the Supplementary Appendix). The pooled hazard ratios among participants with the greatest improvement in diet quality (13 to 33% improvement), as compared with those whose diet quality remained relatively stable (0 to 3% improvement) in the 12-year period, were the following: 0.91 (95% confidence interval [CI], 0.85 to 0.97) according to changes in the Alternate Healthy Eating Index score; 0.84 (95% CI, 0.78 to 0.91) according to changes in the Alternate Mediterranean Diet score; and 0.89 (95% CI, 0.84 to 0.95) according to changes in the DASH score (Table 2). In contrast, a decrease in diet quality, as compared with no change in diet quality, was associated with increased total mortality (pooled hazard ratio, 1.12; 95% CI, 1.05 to 1.19) when assessed with the Alternate Healthy Eating Index score, 1.06 (95% CI, 0.99 to 1.13) when assessed with the Alternate Mediterranean Diet score, and 1.06 (95% CI, 1.00 to 1.12) when assessed with the DASH score. Restricted-cubic-spline analyses showed no evidence of nonlinearity in women (P = 0.005 for linearity) and men (P<0.001 for linearity) (Fig. S1A and S1B in the Supplementary Appendix), and for the other two dietary indexes (data not shown).
Table 2.
Pooled Results for the Association of Changes in Diet-Quality Scores during the 12-Year Period (1986–1998) with the Subsequent Risk of Death from Any Cause.*
| Variable | Quintile of Change | P Value for Trend | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Alternate Healthy Eating Index score† | ||||||
|
| ||||||
| Median change in the score in the NHS (%) | −10.4 (−9.5) | −2.8 (−2.6) | 2.2 (2.0) | 7.3 (6.6) | 14.8 (13.4) | |
|
| ||||||
| Median change in the score in the HPFS (%) | −9.4 (−8.5) | −1.7 (−1.5) | 3.4 (3.1) | 8.5 (7.7) | 16.2 (14.7) | |
|
| ||||||
| No. of deaths | 2452 | 2150 | 1914 | 1754 | 1676 | |
|
| ||||||
| Age-adjusted hazard ratio (95% CI) | 1.24 (1.16 to 1.32) | 1.10 (1.03 to 1.17) | 1.00 (ref) | 0.93 (0.87 to 0.99) | 0.88 (0.82 to 0.94) | <0.001 |
|
| ||||||
| Model 1: multivariable-adjusted hazard ratio (95% CI) | 1.11 (1.04 to 1.18) | 1.05 (0.99 to 1.12) | 1.00 (ref) | 0.95 (0.89 to 1.01) | 0.94 (0.88 to 1.00) | <0.001 |
|
| ||||||
| Model 2: multivariable-adjusted hazard ratio (95% CI) | 1.12 (1.05 to 1.19) | 1.06 (1.00 to 1.13) | 1.00 (ref) | 0.94 (0.88 to 1.01) | 0.91 (0.85 to 0.97) | <0.001 |
|
| ||||||
| Alternate Mediterranean Diet score‡ | ||||||
|
| ||||||
| Median change in the score in the NHS (%) | −2 (−22.2) | −1 (−11.1) | 0 | 1 (11.1) | 3 (33.3) | |
|
| ||||||
| Median change in the score in the HPFS (%) | −2 (−22.2) | −1 (−11.1) | 0 | 1 (11.1) | 2 (22.2) | |
|
| ||||||
| No. of deaths | 2325 | 1805 | 2114 | 2522 | 1180 | |
|
| ||||||
| Age-adjusted hazard ratio (95% CI) | 1.15 (1.08 to 1.22) | 1.00 (0.94 to 1.07) | 1.00 (ref) | 0.89 (0.84 to 0.95) | 0.77 (0.72 to 0.83) | <0.001 |
|
| ||||||
| Model 1: multivariable-adjusted hazard ratio (95% CI) | 1.05 (0.98 to 1.12) | 0.97 (0.91 to 1.03) | 1.00 (ref) | 0.93 (0.87 to 0.98) | 0.86 (0.79 to 0.92) | <0.001 |
|
| ||||||
| Model 2: multivariable-adjusted hazard ratio (95% CI) | 1.06 (0.99 to 1.13) | 0.97 (0.91 to 1.04) | 1.00 (ref) | 0.93 (0.87 to 0.98) | 0.84 (0.78 to 0.91) | <0.001 |
|
| ||||||
| DASH score§ | ||||||
|
| ||||||
| Median change in the score in the NHS (%) | −5 (−15.6) | −2 (−6.3) | 0 | 2 (6.3) | 5 (15.6) | |
|
| ||||||
| Median change in the score in the HPFS (%) | −5 (−15.6) | −2 (−6.3) | 0 | 2 (6.3) | 6 (18.8) | |
|
| ||||||
| No. of deaths | 2425 | 1605 | 2694 | 1390 | 1832 | |
|
| ||||||
| Age-adjusted hazard ratio (95% CI) | 1.16 (1.10 to 1.23) | 1.04 (0.97 to 1.10) | 1.00 (ref) | 0.91 (0.86 to 0.98) | 0.87 (0.82 to 0.93) | <0.001 |
|
| ||||||
| Model 1: multivariable-adjusted hazard ratio (95% CI) | 1.04 (0.98 to 1.10) | 0.99 (0.93 to 1.05) | 1.00 (ref) | 0.95 (0.88 to 1.01) | 0.93 (0.88 to 0.99) | 0.003 |
|
| ||||||
| Model 2: multivariable-adjusted hazard ratio (95% CI) | 1.06 (1.00 to 1.12) | 1.01 (0.94 to 1.07) | 1.00 (ref) | 0.93 (0.87 to 1.00) | 0.89 (0.84 to 0.95) | <0.001 |
The multivariable-adjusted model 1 was adjusted for age; initial diet-quality score (in quintiles); race (white vs. nonwhite); family history of myocardial infarction, diabetes, or cancer; use or nonuse of aspirin or multivitamins; initial BMI (<23.0, 23.0 to 24.9, 25.0 to 29.9, 30.0 to 34.9, and =35.0); initial smoking status and changes in smoking status; initial smoking pack-years and changes in smoking pack-years (continuous variable) among participants with any history of smoking (ever smokers); initial levels of physical activity and total energy intake and changes in these levels (all in quintiles); and menopausal status and use or nonuse of hormone-replacement therapy in women. The multivariable-adjusted model 2 had the same adjustments as model 1 plus history of hypertension, hypercholesterolemia, or type 2 diabetes (all yes vs. no); weight change (in quintiles); and use or nonuse of cholesterol-lowering and antihypertensive medications. The Dietary Approaches to Stop Hypertension (DASH) score models were also adjusted for initial intake of alcohol and change in this intake (in quintiles). Results from the Nurses’ Health Study (NHS) and Health Professionals Follow-up Study (HPFS) were combined with the use of the fixed-effects model. CI denotes confidence interval.
Scores on the Alternate Healthy Eating Index–2010 range from 0 to 110, with higher scores indicating a healthier diet.
Scores on the Alternate Mediterranean Diet range from 0 to 9, with higher scores indicating a healthier diet.
Scores on the DASH range from 8 to 40, with higher scores indicating a healthier diet.
DIET SCORES AND REDUCTION IN MORTALITY
In continuous analyses, a 20-percentile increase in diet-quality scores was associated with a reduction of 8 to 17% in the risk of death from any cause (Table 3, and Table S5 in the Supplementary Appendix). A 20-percentile increase in the Alternate Healthy Eating Index and Alternate Mediterranean Diet scores, but not the DASH score, was associated with a significantly reduced risk of death from cardiovascular disease (pooled hazard ratio, 0.85; 95% CI, 0.76 to 0.96) when assessed with the Alternate Healthy Eating Index score; 0.93 (95% CI, 0.88 to 0.99) when assessed with the Alternate Mediterranean Diet score, and 0.96 (95% CI, 0.88 to 1.05) when assessed with the DASH score. A significant inverse association between diet quality and the risk of death from cancer was seen only when the DASH score was used (0.91; 95% CI, 0.84 to 0.98) (Table 3); this was attributable mainly to a decreased risk of death from lung cancer (Table S6 in the Supplementary Appendix).
Table 3.
Pooled Results for the Relationships between Changes in Diet-Quality Scores and the Risk of Death from Any Cause, Death from Cardiovascular Disease, and Death from Cancer per 20-Percentile Increase in Each Score during the 12-Year Period (1986–1998).*
| Diet-Quality Scores | Death from Any Cause | Death from Cardiovascular Disease | Death from Cancer |
|---|---|---|---|
| Hazard Ratio (95% CI) | |||
|
| |||
| Alternate Healthy Eating Index score | |||
|
| |||
| Age-adjusted model | 0.73 (0.69–0.78) | 0.74 (0.66–0.83) | 0.91 (0.86–0.95) |
|
| |||
| Multivariable-adjusted model 1 | 0.85 (0.80–0.90) | 0.89 (0.79–1.00) | 0.94 (0.85–1.04) |
|
| |||
| Multivariable-adjusted model 2 | 0.83 (0.78–0.88) | 0.85 (0.76–0.96) | 0.94 (0.85–1.04) |
|
| |||
| Alternate Mediterranean Diet score | |||
|
| |||
| Age-adjusted model | 0.86 (0.84–0.89) | 0.86 (0.81–0.91) | 0.91 (0.86–0.95) |
|
| |||
| Multivariable-adjusted model 1 | 0.93 (0.90–0.96) | 0.95 (0.89–1.01) | 0.98 (0.93–1.03) |
|
| |||
| Multivariable-adjusted model 2 | 0.92 (0.89–0.95) | 0.93 (0.88–0.99) | 0.98 (0.93–1.03) |
|
| |||
| DASH score | |||
|
| |||
| Age-adjusted model | 0.84 (0.80–0.87) | 0.89 (0.82–0.97) | 0.83 (0.77–0.89) |
|
| |||
| Multivariable-adjusted model 1 | 0.94 (0.90–0.98) | 1.02 (0.93–1.11) | 0.91 (0.85–0.98) |
|
| |||
| Multivariable-adjusted model 2 | 0.90 (0.86–0.94) | 0.96 (0.88–1.05) | 0.91 (0.84–0.98) |
The 20-percentile increase in each score was calculated from the median value of each quintile. Results of the NHS and HPFS were combined with the use of the fixed-effects model.
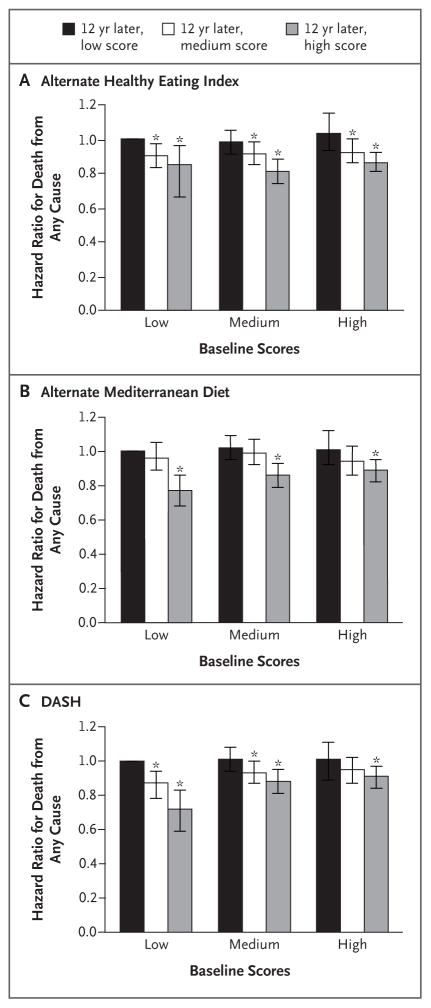
As compared with participants who had consistently low diet scores over time, those with the poorest score at baseline but the largest improvements 12 years later had a 15% (95% CI, 3 to 25) lower risk of death from any cause when diet quality was assessed with the Alternate Healthy Eating Index score, 23% (95% CI, 12 to 32) when assessed with the Alternate Mediterranean Diet score, and 28% (95% CI, 16 to 38) when assessed with the DASH score (Fig. 1). Those who had consistently high diet scores over time had a 14% (95% CI, 8 to 19) lower risk of death from any cause according to the Alternate Healthy Eating Index score, 11% (95% CI, 5 to 18) according to the Alternate Mediterranean Diet score, and 9% (95% CI, 2 to 15) according to the DASH score (Fig. 1, and Table S7 in the Supplementary Appendix). We did not observe consistent evidence to support an association between improvement in diet-quality scores and a decreased risk of death from cancer (Table S6 in the Supplementary Appendix).
Figure 1. Risk of Death from Any Cause, According to Scores on Three Measures of Diet Quality at Baseline and 12 Years Later.
The multivariable-adjusted risk of death from any cause according to the Alternate Healthy Eating Index–2010 score (Panel A), the Alternate Mediterranean Diet score (Panel B), and the Dietary Approaches to Stop Hypertension (DASH) score (Panel C) at baseline and 12 years later is shown. Baseline scores are shown as low, medium, and high, with higher scores indicating a healthier diet. At 12 years, a participant may have had a consistently low score over time, a change from a low score to a medium or high score, a consistently medium score over time, a change from a medium score to a low or high score, a consistently high score over time, or a change from a high score to a low or medium score. The reference group (hazard ratio, 1.00) was the low score at both baseline and the 12-year follow-up period. Results of the Nurses’ Health Study and the Health Professionals Follow-up Study were combined with the use of the fixed-effects model. I bars represent 95% confidence intervals. Asterisks indicate P<0.05.
TIMING OF DIETARY CHANGES
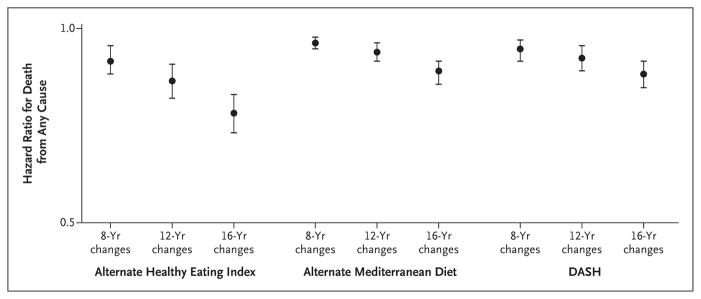
In multivariable analysis, a 20-percentile increase during the first 8, 12, and 16 years in any of the three diet scores was significantly associated with a reduced risk of death from any cause (Fig. 2). Associations were strengthened when changes over a longer duration were evaluated. For example, a 20-percentile increase in the Alternate Healthy Eating Index score over 8 years was associated with a reduction in mortality of 11% (95% CI, 6 to 15), whereas among participants with the same degree of improvement over 16 years, the reduction in mortality was 26% (95% CI, 21 to 31) (Tables S8 and S9 in the Supplementary Appendix). A 20-percentile increase over 16 years in any of the three diet scores was significantly associated with a decreased risk of death from cardiovascular disease (Table S10 and Fig. S2A in the Supplementary Appendix). Neither short-term nor long-term changes in dietary patterns were associated with a decreased risk of death from cancer (Fig. S2B in the Supplementary Appendix).
Figure 2. Risk of Death from Any Cause per 20-Percentile Increase in Diet-Quality Scores.
The multivariable-adjusted risk of death from any cause per 20-percentile increase in the score (indicating improvement in the quality of the diet) on three measures of diet quality is shown. The 20-percentile increase in each score was calculated from the median value of each quintile. I bars represent 95% confidence intervals.
SENSITIVITY ANALYSES
In sensitivity analyses, the significant inverse association between changes in the three scores and total and cause-specific mortality remained similar when we further adjusted for mammographic screening (in women only) and physical checkups (Table S11 in the Supplementary Appendix), when we stratified the analyses according to major confounding factors (Table S12 in the Supplementary Appendix), when we added a 4-year lag period after changes in diet-quality scores (Table S13 in the Supplementary Appendix), when alcohol was removed from the Alternate Healthy Eating Index score and the Alternate Mediterranean Diet score (Table S14 in the Supplementary Appendix), or when smoking duration and dose instead of smoking pack-years were adjusted in the multivariable models (Table S15 in the Supplementary Appendix).
DISCUSSION
In the present study, we found consistent associations between improved diet quality over 12 years as assessed by the Alternate Healthy Eating Index, Alternate Mediterranean Diet, and DASH scores and a reduced risk of death in the subsequent 12 years. A 20-percentile increase in diet-quality scores was associated with an 8 to 17% reduction in mortality. In contrast, worsening diet quality over 12 years was associated with an increase in mortality of 6 to 12%. The risk of death from any cause was significantly lower (by 9 to 14%) among participants who maintained a high-quality diet than among those who had consistently low diet scores over time.
Our results are consistent with those of recent meta-analyses showing that higher diet-quality scores measured with the Alternate Healthy Eating Index, Alternate Mediterranean Diet, DASH, and the Healthy Eating Index–2010 were associated with a 17 to 26% reduction in the risk of death from any cause.15,16 We found a dose-dependent relationship between changes in diet quality over 12 years and total mortality. These results underscore the concept that moderate improvements in diet quality over time could meaningfully decrease the risk of death, and conversely, worsening diet quality may increase the risk. The change in the risk of death was more pronounced when longer-term (16 years) rather than shorter-term (8 years) changes in diet quality were considered.
Taken together, our findings provide support for the recommendations of the 2015 Dietary Guidelines Advisory Committee that it is not necessary to conform to a single diet plan to achieve healthy eating patterns.18 These three dietary patterns, although different in description and composition, capture the essential elements of a healthy diet. Common food groups in each score that contributed most to improvements were whole grains, vegetables, fruits, and fish or n-3 fatty acids.
To improve our comparison of associations between the three scores that differ in scoring criteria and range, we evaluated the association with mortality using a 20-percentile increase in each score as a common unit for improving diet. For example, if we assume a causal relationship, a person with an increase of 22 of 110 points in the Alternate Healthy Eating Index score over a 12-year period could reduce his or her risk of death by nearly 20% in the subsequent 12 years. An increase in consumption of nuts and legumes from no servings to 1 serving per day and a reduction in consumption of red and processed meats from 1.5 servings per day to little consumption will result in an improvement of 20 points in the score. These findings are broadly consistent with those of previous meta-analyses of the association between consumption of nuts30 and red meat31 and mortality.
In line with other studies, stronger associations were seen when overall deaths and deaths from cardiovascular causes were analyzed, and null or weaker associations were observed for death from cancer.2,3,8,12,32 Our results with respect to improvement in the Alternate Healthy Eating Index and a reduction in the risk of death from cardiovascular disease were expected, given that the Alternate Healthy Eating Index is based on current knowledge of dietary factors contributing to cardiovascular disease.12 Evidence supports the inverse association between higher scores in the Alternate Healthy Eating Index2–4,6,8,16 or the Mediterranean-style diet10,11,13,32–34 and a lower risk of death from cardiovascular disease in various populations. We did not find significant associations between changes in the DASH score and death from cardiovascular causes. Although the DASH score shares some food and nutrient components with the two other scores, it does not include fish or specific fatty acids, which have been consistently associated with a reduced risk of cardiovascular disease.21,33 In addition, previous findings have shown that moderate alcohol intake is associated with a reduction in the risk of death from cardiovascular disease,21,35 and this component is not included in the DASH score. Although some studies have shown a significantly reduced risk of death from cancer with good adherence to some dietary patterns,4–6 other studies have not shown such associations.2,8,32 Our study did not provide consistent evidence that improving diet quality had a substantial effect on overall mortality from cancer.
The strengths of our study include the prospective design, large sample sizes, high rates of follow-up, repeated assessment of diet and lifestyle, and use of multiple diet-quality scores. However, the study has certain limitations. Because dietary data were reported by the participants, measurement errors were inevitable. However, our food frequency questionnaires were extensively validated against diet records and biomarkers. Although we were able to adjust for many potential confounders, residual and unmeasured confounding could not be completely ruled out. We did not examine the association of each component of the scores and mortality because we considered that a high diet quality is a combination of multiple components that act synergistically. Finally, generalizability may be limited because participants were mostly white health professionals and we only included one third of the initial population because of our study design. However, our findings are broadly consistent with those from other populations.
In conclusion, among U.S. adults, we observed consistent associations between increasing diet quality over 12 years and a reduced risk of death.
Supplementary Material
Acknowledgments
Funded by the National Institutes of Health.
Supported by grants (HL034594, HL088521, HL35464, HL60712, P01 CA055075, P01 CA87969, UM1 CA167552, and UM1 CA186107) from the National Institutes of Health.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Cespedes EM, Hu FB. Dietary patterns: from nutritional epidemiologic analysis to national guidelines. Am J Clin Nutr. 2015;101:899–900. doi: 10.3945/ajcn.115.110213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.George SM, Ballard-Barbash R, Manson JE, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. Am J Epidemiol. 2014;180:616–25. doi: 10.1093/aje/kwu173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harmon BE, Boushey CJ, Shvetsov YB, et al. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: the Dietary Patterns Methods Project. Am J Clin Nutr. 2015;101:587–97. doi: 10.3945/ajcn.114.090688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144:881–9. doi: 10.3945/jn.113.189407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu D, Sonderman J, Buchowski MS, et al. Healthy eating and risks of total and cause-specific death among low-income populations of African-Americans and other adults in the southeastern United States: a prospective cohort study. PLoS Med. 2015;12(5):e1001830. doi: 10.1371/journal.pmed.1001830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mursu J, Steffen LM, Meyer KA, Duprez D, Jacobs DR., Jr Diet quality indexes and mortality in postmenopausal women: the Iowa Women’s Health Study. Am J Clin Nutr. 2013;98:444–53. doi: 10.3945/ajcn.112.055681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boggs DA, Ban Y, Palmer JR, Rosenberg L. Higher diet quality is inversely associated with mortality in African-American women. J Nutr. 2015;145:547–54. doi: 10.3945/jn.114.195735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akbaraly TN, Ferrie JE, Berr C, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr. 2011;94:247–53. doi: 10.3945/ajcn.111.013128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. High diet quality is associated with a lower risk of cardiovascular disease and all-cause mortality in older men. J Nutr. 2014;144:673–80. doi: 10.3945/jn.113.186486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093–100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–90. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 12.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–18. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 14.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–20. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 15.Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17:2769–82. doi: 10.1017/S1368980013003169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780–800. e5. doi: 10.1016/j.jand.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Liese AD, Krebs-Smith SM, Subar AF, et al. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145:393–402. doi: 10.3945/jn.114.205336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: Department of Agriculture; Feb, 2015. ( https://health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics — 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 20.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health. 1997;6:49–62. doi: 10.1089/jwh.1997.6.49. [DOI] [PubMed] [Google Scholar]
- 21.Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet. 1991;338:464–8. doi: 10.1016/0140-6736(91)90542-w. [DOI] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semi-quantitative food frequency questionnaire. Am J Epidemiol. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 24.Salvini S, Hunter DJ, Sampson L, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol. 1989;18:858–67. doi: 10.1093/ije/18.4.858. [DOI] [PubMed] [Google Scholar]
- 25.Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation. 2015;132:2212–9. doi: 10.1161/CIRCULATIONAHA.115.017158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol. 1994;140:1016–9. doi: 10.1093/oxfordjournals.aje.a117191. [DOI] [PubMed] [Google Scholar]
- 27.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–73. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Giovannucci E, Colditz G, Stampfer MJ, et al. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol. 1991;133:810–7. doi: 10.1093/oxfordjournals.aje.a115960. [DOI] [PubMed] [Google Scholar]
- 29.Chasan-Taber S, Rimm EB, Stampfer MJ, et al. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996;7:81–6. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Aune D, Keum N, Giovannucci E, et al. Nut consumption and risk of cardiovascular disease, total cancer, all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective studies. BMC Med. 2016;14:207. doi: 10.1186/s12916-016-0730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larsson SC, Orsini N. Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol. 2014;179:282–9. doi: 10.1093/aje/kwt261. [DOI] [PubMed] [Google Scholar]
- 32.Buckland G, Agudo A, Travier N, et al. Adherence to the Mediterranean diet reduces mortality in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain) Br J Nutr. 2011;106:1581–91. doi: 10.1017/S0007114511002078. [DOI] [PubMed] [Google Scholar]
- 33.Knoops KTB, Groot de LC, Fidanza F, Alberti-Fidanza A, Kromhout D, van Staveren WA. Comparison of three different dietary scores in relation to 10-year mortality in elderly European subjects: the HALE project. Eur J Clin Nutr. 2006;60:746–55. doi: 10.1038/sj.ejcn.1602378. [DOI] [PubMed] [Google Scholar]
- 34.Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol. 2014;25:20–6. doi: 10.1097/MOL.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 35.Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.