Abstract
Background
Face-to-face cognitive testing is not always possible in large studies. We therefore assessed the telephone Montreal Cognitive Assessment (T-MoCA: MoCA items not requiring pencil and paper and/or visual stimulus) and the modified Telephone Interview of Cognitive Status (TICSm) against face-to-face cognitive tests in patients with TIA or stroke.
Methods
In a population-based study, consecutive community dwelling patients had the MoCA and neuropsychological battery ≥1 year after TIA or stroke followed by T-MoCA (22-points) and TICSm (39-points) at least one month later. Mild cognitive impairment (MCI) was diagnosed using modified Petersen criteria and the area under the ROC curve (AUC) determined for T-MoCA and TICSm.
Results
91 non-demented subjects completed neuropsychological testing (mean±sd age 72.9±11.6 years, 54 male, 49 stroke) and 73 had telephone follow-up. MoCA subtest scores for repetition, abstraction and verbal fluency were significantly worse (p<0.02) by phone than at face-to-face testing. Reliability of diagnosis for MCI (AUC) was: T-MoCA=0.75, 95% CI 0.63-0.87, TICSm=0.79,0.68-0.90 vs face-to-face MoCA=0.85, 0.76-0.94. Optimal cut-offs were 18/19 on T-MoCA and 24/25 on TICSm. Reliability of diagnosis for MCI (AUC) was greater when only multi-domain impairment was considered: T-MoCA=0.85,0.75-0.96; TICSm=0.83,0.70-0.96 vs face-to-face MoCA=0.87,0.76-0.97.
Conclusion
Both T-MoCA and TICSm are feasible and valid telephone tests of cognition after TIA and stroke but perform better in detecting multi- vs single-domain impairment. However, T-MoCA is limited in its ability to assess visuoexecutive and complex language tasks compared to face-to-face MoCA.
Keywords: MoCA, TICSm, telephone testing, vascular cognitive impairment, MCI
Search terms: [46] behavioural changes and stroke
Introduction
Cognitive impairment is prevalent after stroke.1,2 and there is thus a need for short tests of cognition including telephone tests since lengthy neuropsychological batteries are often not feasible in large studies.
The Montreal Cognitive Assessment3 recommended by the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network Vascular Cognitive Impairment (NINDS-CSN) Harmonization Standards working group4 is sensitive to MCI in TIA and stroke5–7 and may be administered by telephone but there are no published validations. The Telephone Interview of Cognitive Status (TICS) was originally developed as a short cognitive test for face-to-face or telephone administration8,9 but there are few reports after stroke.10,11
We therefore assessed the Telephone (T)-MoCA (items not requiring the use of a pencil and paper and/or visual stimulus) and the TICSm in community dwelling patients with TIA or stroke who had recently undergone face-to-face MoCA and NINDS-CSN neuropsychological battery.4
Methods
Patients were participants in the Oxford Vascular Study (OXVASC 2002-), a prospective population-based study of all acute vascular events12 approved by the local ethics committee. Between August 2009 and November 2010, consecutive community-dwelling patients were invited at their routine 1 or 5 year follow-up (at which they had the MoCA)3 to undergo the NINDS-CSN Harmonisation Standards Neuropsychological Battery4 which was used to define MCI by modified Petersen criteria: single-domain (amnestic and non-amnestic) and multiple-domain (amnestic and non-amnestic) as described previously.6
At least 1 month after neuropsychological testing, subjects were telephoned and invited to complete the T-MoCA and TICSm presented in counterbalanced order (supplementary table S1). For the MoCA sustained attention task in which subjects tap on the desk during face-to-face testing, subjects were instructed to tap the side of the phone with a pencil. Telephone testing was performed by researchers (SW, FC) blinded to face-to-face data.
Statistical Analyses
For MoCA data acquired by telephone, we considered the T-MoCA (total-22 points) and separately, the T-MoCA-Short (verbal fluency, recall and orientation total-12 points) recommended by the NINDS-CSN Harmonisation Standards Working Group.4 The additional point for low education3 was added to the face-to-face score but not to telephone scores.
Differences between scores on MoCA subtests performed over the telephone versus face-to-face were assessed using the Wilcoxon signed rank test. Prediction of MCI by T-MoCA, T-MoCA-Short and TICSm was assessed using the area under the receiver operating characteristic curve (AUC).
Results
91 non-demented patients (73.4±7 years, stroke 56%, NIHSS 0.95±1.5, 63% education<12 years) completed face-to-face MoCA and neuropsychological battery at a mean of 3.1±1.9 years after index event and 73 had telephone testing at least 1 month after face-to-face test. MoCA repetition, abstraction and verbal fluency were worse (all p<0.02) by phone than face-to-face (Supplementary table S1) even after exclusion of patients with overt hearing problems.
27 (40%) of 68 patients with neuropsychological battery and telephone test had a diagnosis of MCI: single-domain=15, multiple-domain=12. MCI patients were older (77.8±9.1 vs 70.0+10.1 years,p=0.002), had low education (22/27 vs 23/41,p=0.03) and tended to have had stroke (17/27 vs 16/41, p=0.08). All telephone tests differentiated between no MCI, single domain and multiple domain MCI (Supplementary table S2).
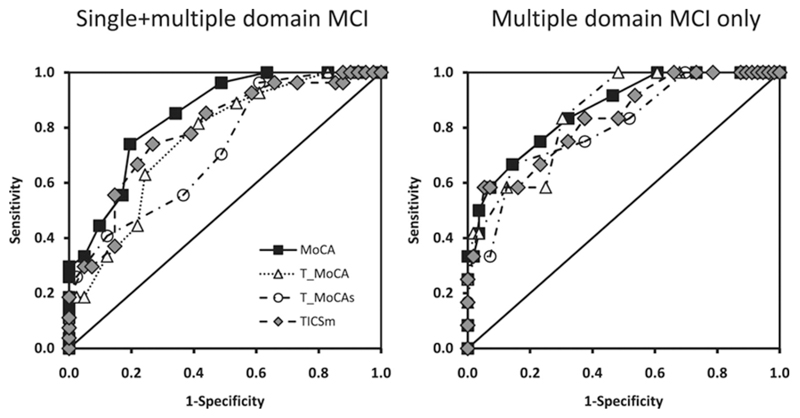
Reliability of detection of MCI (AUC) (figure) were: T-MoCA=0.75, 95%CI 0.64-0.87 (0.83, 0.73-0.92 for the same 22 items extracted from face-to-face MoCA); T-MoCA-Short=0.72, 0.60-0.84, TICSm=0.79, 0.68-0.90, face-to-face MoCA=0.85, 0.76-0.94. For multiple-domain MCI only, AUC were T-MoCA=0.85, 0.75-0.96, T-MoCA-Short=0.85, 0.75-0.96, TICSm=0.83, 0.70-0.96, face-to-face MoCA=0.87,0.76-0.97.
Figure.
AUC curves for face-to-face MoCA, TICSm, T-MoCA, and T-MoCA-Short for any (single+multiple domain) MCI and multiple-domain MCI only.
Optimal sensitivities and specificities for MCI were achieved for T-MoCA cut-offs around 18/19, T-MoCA-Short around 10/11 and TICsm around 24/25 with cut points around 1-2 points lower for multi-domain impairment (table).
Table.
Sensitivities, specificities, positive and negative predictive values (ppv and npv) for T-MoCA, T-MoCA-Short and TICSm for any MCI and multiple-domain MCI only.
|
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Any MCI (single + multi-domain) | Multi-domain MCI | |||||||
| Sensitivity % 95% CI | Specificity % 95% CI | Ppv, 95% CI | Npv, 95% CI | Sensitivity % 95% CI | Specificity % 95% CI | Ppv, 95% CI | Npv, 95% CI | |
| T-MoCA/22 | ||||||||
| <19 | 89,71-98 | 46,31-63 | 52,37-67 | 86,65-97 | 100,74-100 | 39,27-53 | 26,14-41 | 100,85-100 |
| <18 | 81,62-94 | 59,42-74 | 56,40-72 | 83,64-94 | 100,74-100 | 52,38-65 | 31,17-48 | 100,88-100 |
| <17 | 63,42-81 | 76,60-88 | 63,42-81 | 76,60-88 | 83,52-98 | 70,56-81 | 37,19-58 | 95,83-99 |
| <16 | 44,25-65 | 78,62-89 | 57,34-78 | 68,53-81 | 58,28-85 | 75,62-86 | 33,15-57 | 89,77-96 |
| T-MoCA-Short/12 | ||||||||
| <11 | 96,81-100 | 39,24-56 | 51,37-65 | 94,71-100 | 100,74-100 | 30,19-44 | 24,13-37 | 100,80-100 |
| <10 | 70,50-86 | 51,35-67 | 49,32-65 | 72,53-87 | 83,52-98 | 48,35-62 | 26,13-42 | 93,77-99 |
| <9 | 56,35-75 | 63,47-78 | 50,31-69 | 68,51-83 | 75,43-95 | 63,49-75 | 30,15-49 | 92,79-98 |
| <8 | 41,22-61 | 88,74-96 | 69,41-89 | 69,55-81 | 67,35-90 | 86,74-94 | 50,25-75 | 92,81-98 |
| TICSm/39 | ||||||||
| <25 | 85,66-96 | 56,40-72 | 56,40-72 | 85,66-96 | 92,62-100 | 46,33-60 | 27,14-43 | 96,81-100 |
| <24 | 78,58-91 | 61,45-76 | 57,39-73 | 81,63-93 | 83,52-98 | 52,38-65 | 27,14-44 | 94,79-99 |
| <23 | 74,54-89 | 73,57-86 | 65,45-81 | 81,65-92 | 83,52-98 | 63,49-75 | 32,17-51 | 95,82-99 |
| <22 | 67,46-83 | 78,62-89 | 67,46-83 | 78,62-89 | 75,43-95 | 68,54-80 | 33,17-54 | 93,80-98 |
|
| ||||||||
Discussion
The T-MoCA and the TICSm had similar AUC curves and reasonable sensitivity and specificity for MCI although the T-MoCA-Short performed less well and face-to-face MoCA was best. Performance was better and more similar for all tests in detecting multiple domain impairment.
Our findings show that both the T-MoCA and the TICSm are valid tests for assessing cognition after TIA and stroke although certain MoCA subtests (abstraction, verbal fluency and repetition) appeared to be adversely affected by telephone administration. Sensitivity/specificity of the T-MoCA for MCI was thus better when the same 22 items were extracted from the face-to-face MoCA and this would be a valid test for face-to-face assessment of visually impaired patients. The T-MoCA-Short performed less well than the other tests in detection of single domain MCI.
Our study has several limitations. First, we included only community-dwelling subjects who were tested some time after a relatively mild cerebrovascular event and telephone testing may be more difficult in patients with more severe stroke. Second, optimal cut-offs on the T-MoCA and TICSm will vary with different definitions of MCI.6 Finally, our sample size was relatively small and further large studies are needed to confirm our findings.
In conclusion, both the T-MoCA and the TICSm appear to be valid telephone tests of cognition but perform better in detecting multiple vs single-domain MCI in community-dwelling patients with TIA and stroke. The T-MoCA is limited by inability to test visuoexecutive items and by the impact of telephone administration and face-to-face MoCA is to be preferred where clinic assessment is feasible.
Supplementary Material
Acknowledgments
Funding
The Oxford vascular study is funded by the UK Stroke Association, the Dunhill Medical Trust, the National Institute of Health Research (NIHR), the Medical Research Council and the NIHR Biomedical Research Centre, Oxford. Dr Pendlebury is supported by the NIHR Biomedical Research Centre, Oxford.
Footnotes
Disclosures/ Competing interests: None
References
- 1.Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8:1006–1018. doi: 10.1016/S1474-4422(09)70236-4. [DOI] [PubMed] [Google Scholar]
- 2.Narasimhalu K, Ang S, De Silva DA, Wong MC, Chang HM, Chia KS, et al. Severity of CIND and MCI predict incidence of dementia in an ischemic stroke cohort. Neurology. 2009;73:1866–72. doi: 10.1212/WNL.0b013e3181c3fcb7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 4.Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37:2220–2241. doi: 10.1161/01.STR.0000237236.88823.47. [DOI] [PubMed] [Google Scholar]
- 5.Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, Rothwell PM. Underestimation of Cognitive Impairment by Mini-Mental State Examination Versus the Montreal Cognitive Assessment in Patients With Transient Ischemic Attack and Stroke. A Population-Based Study. Stroke. 2010;41:1290–1293. doi: 10.1161/STROKEAHA.110.579888. [DOI] [PubMed] [Google Scholar]
- 6.Pendlebury ST, Mariz J, Bull L, Mehta Z, Rothwell PM. MoCA, ACE-R, and MMSE versus the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards Neuropsychological Battery after TIA and stroke. Stroke. 2012;43:464–9. doi: 10.1161/STROKEAHA.111.633586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pendlebury ST, Markwick A, de Jager CA, Zamboni G, Wilcock GK, Rothwell PM. Differences in cognitive profile between TIA, stroke and elderly memory research subjects: a comparison of the MMSE and MoCA. Cerebrovasc Dis. 2012;34:48–54. doi: 10.1159/000338905. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Brandt J, Spencer M, Folstein M. The Telephone Interview for Cognitive Status. Neuropsychiatry Neuropsychol Behavioral Neurol. 1988;1:111–117. [Google Scholar]
- 9.de Jager CA, Budge MM, Clarke R. Utility of TICS-M for the assessment of cognitive function in older adults. Int J Geriatr Psychiatry. 2003;18:318–24. doi: 10.1002/gps.830. [DOI] [PubMed] [Google Scholar]
- 10.Desmond DW, Tatemichi T, Hanzawa L. The Telephone Interview for Cognitive Status (TICS): reliability and validity in a stroke sample. Int J Geriatr Psychiatry. 1994;9:803–807. [Google Scholar]
- 11.Barber M, Stott DJ. Validity of the Telephone Interview for Cognitive Status (TICS) in post-stroke subjects. Int J Geriatr Psychiatry. 2004;19:75–9. doi: 10.1002/gps.1041. [DOI] [PubMed] [Google Scholar]
- 12.Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM, et al. Oxford Vascular Study. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study) Lancet. 2004;363:1925–33. doi: 10.1016/S0140-6736(04)16405-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.