Abstract
Objective
The purpose of this paper is to elucidate this little known cause of upper back pain through a narrative review of the literature and to discuss the possible role of the dorsal scapular nerve (DSN) in the etiopathology of other similar diagnoses in this area including cervicogenic dorsalgia (CD), notalgia paresthetica (NP), SICK scapula and a posterolateral arm pain pattern.
Background
Dorsal scapular nerve (DSN) neuropathy has been a rarely thought of differential diagnosis for mid scapular, upper to mid back and costovertebral pain. These are common conditions presenting to chiropractic, physiotherapy, massage therapy and medical offices.
Methods
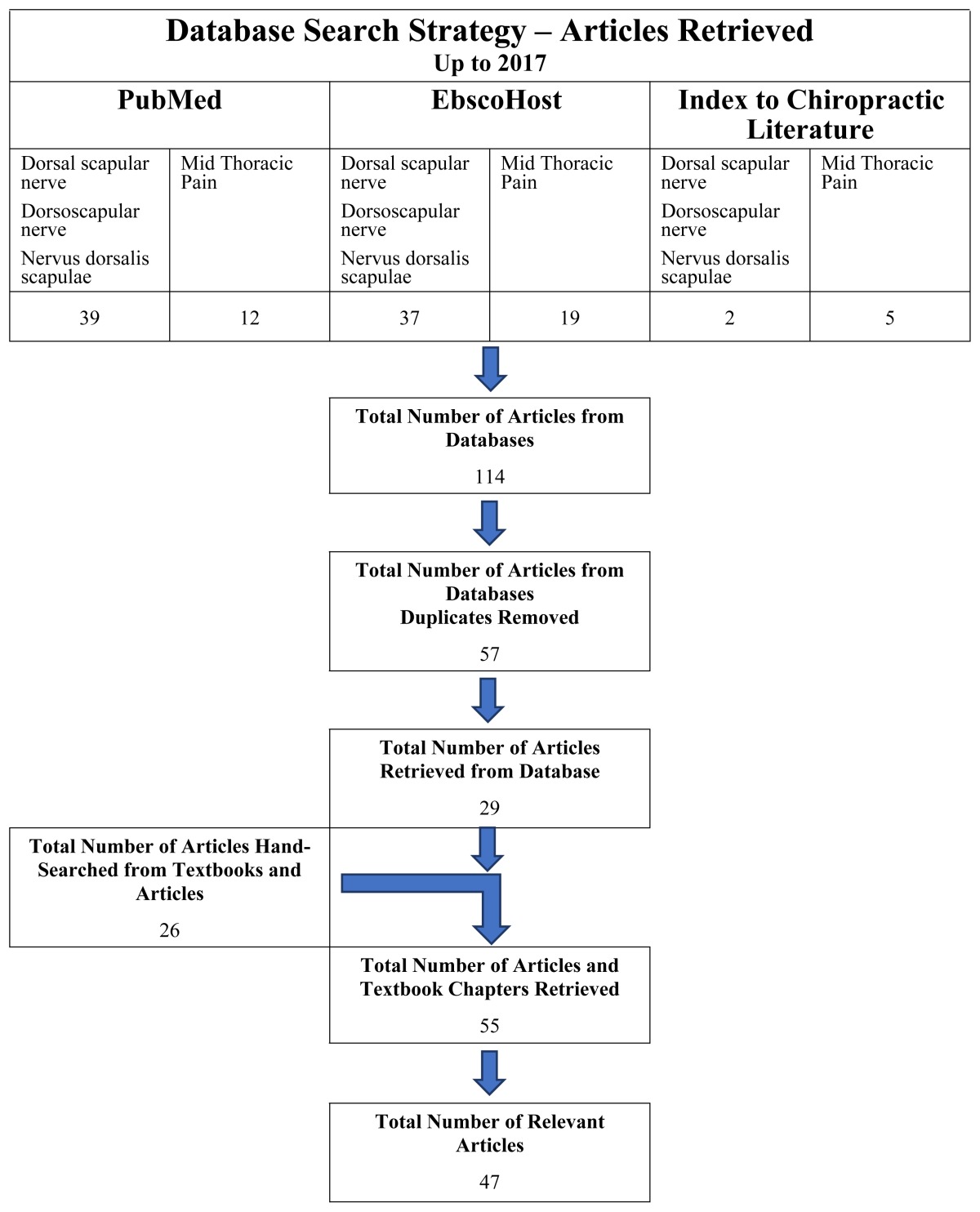
The methods used to gather articles for this paper included: searching electronic databases; and hand searching relevant references from journal articles and textbook chapters.
Results
One hundred-fourteen articles were retrieved. After removing duplicates, there were 57 articles of which 29 were retrieved. There were 26 articles and textbook chapters retrieved by hand searching equaling 55 articles retrieved of which 47 relevant articles were used in this report.
Discussion
The anatomy, pathway and function of the dorsal scapular nerve can be varied and exceptionally rarely may include a sensory component. The signs and symptoms, therefore, may include pain, atrophy, scapular winging, and dysesthesia. The mechanism of injury to the DSN is also quite varied ranging from postural to overuse in overhead work and sport. Other conditions in this area, including CD, NP, SICK scapula and a posterolateral arm pain pattern bear a striking resemblance to DSN neuropathy.
Conclusion
DSN neuropathy should be included in the list of common differential diagnoses of upper and mid-thoracic pain, stiffness, dysesthesia and dysfunction. The study also brings forward interesting connections between DSN neuropathy, CD, NP, SICK scapula and a posterolateral arm pain pattern.
Keywords: dorsal scapular nerve, nervus dorsalis scapulae, mid-thoracic pain, cervicogenic dorsalgia, notalgia paresthetica, SICK scapula, posterolateral arm pain pattern
Abstract
Objectif
Ce document a pour objectif d’élucider cette cause peu connue de douleur dans le haut du dos par un examen narratif de la littérature, ainsi que de discuter du rôle possible du nerf scapulaire dorsal (NSD) dans l’étiopathologie d’autres diagnostics semblables dans ce domaine, y compris la dorsalgie cervicogénique (DC), la notalgie paresthésique (NP), l’omoplate SICK et un schéma de douleur postérolatérale au bras.
Contexte
La neuropathie du nerf scapulaire dorsal (NSD) constitue un diagnostic différentiel rare pour la douleur mi-scapulaire, costo-vertébrale et au bas/haut du dos. Il s’agit de troubles communs qui surgissent dans les cabinets de chiropratique, de physiothérapie, de massothérapie et de médecin.
Méthodologie
Les méthodes utilisées pour rassembler les articles de ce document comprenaient la recherche dans des bases de données électroniques et la recherche manuelle de références pertinentes dans des articles de journaux et des chapitres de traités.
Résultats
On a extrait 114 articles. Une fois les dédoublements éliminés, il y avait 57 articles, desquels 29 ont été extraits. Il y avait 26 articles et chapitres de traités extraits à la main, ce qui donne 55 articles extraits, desquels 47 articles pertinents ont été utilisés pour ce rapport.
Discussion
L’anatomie, la voie et la fonction du nerf scapulaire dorsal peuvent être variées et, exceptionnellement, comprendre un facteur sensoriel. Par conséquent, les signes et symptômes peuvent comprendre la douleur, l’atrophie, le décollement scapulaire et la dysesthésie. Le mécanisme de blessure du NSD est lui aussi très varié, allant de la posture au travail/sport au-dessus de la tête. D’autres troubles dans ce domaine, dont la DC, la NP, l’omoplate SICK et un schéma de douleur postéro-latérale au bras, ressemblent étrangement à la neuropathie du NSD.
Conclusion
Il faut inclure la neuropathie du NSD dans la liste des diagnostics différentiels communs pour la douleur thoracique supérieure et médiane, la raideur, la dysesthésie et le dysfonctionnement. De plus, l’étude met en évidence d’intéressants liens entre la neuropathie du NSD, la DC, la NP, l’omoplate SICK et un schéma de douleur postéro-latérale au bras.
MOTS CLÉS: chiropratique, nerf scapulaire dorsal, nervus dorsalis scapulae, douleur thoracique médiane, dorsalgie cervicogénique, notalgie paresthésique, omoplate SICK, schéma de douleur postéro-latérale au bras
Introduction
Dorsal scapular nerve (DSN) (Latin: nervus dorsalis scapulae) neuropathy has been a rarely thought of differential diagnosis for mid scapular, upper to mid back pain.1 Upper to mid-thoracic and costovertebral pain and stiffness are a common entity presenting to chiropractic, physiotherapy, massage therapy and medical offices2–4 especially following motor vehicle accidents5. Patients may report pain, stiffness, dysesthesia and dysfunction (scapular, thoracic and costovertebral) of an acute or chronic nature in this area with only temporary relief following normal care by their health professional.1
In a study by Sultan et al.1, 55 patients with unilateral interscapular pain were evaluated. The diagnosis for these patients varied from no diagnosis to thoracic degenerative discogenic pain, costovertebral joint dysfunction, levator scapulae syndrome, thoracic facet syndrome, dorsal back strain, myofascial pain of the rhomboids and finally DSN entrapment.1 These are common diagnoses rendered for pain in this area and the referral for an electrophysiologic study would suggest a lack of progress with normal care. The study found that there was evidence of DSN neuropathy in 29 patients (52.7%) and another five were at the upper cutoff limit which would bring the total to 61.8% if these were counted as having DSN involvement.1 This would suggest that DSN neuropathy should be included in the differential diagnoses for upper to midback pain, stiffness and dysfunction. Its consideration may in fact add to, or change, the diagnosis and provide an avenue for longer lasting relief with an appropriate treatment strategy.
The signs and symptoms of DSN neuropathy bear a striking resemblance to several other diagnoses or findings in the cervicothoracic, scapular and posterolateral arm areas including cervicogenic dorsalgia (CD), notalgia paresthetica (NP), SICK scapula and a posterolateral arm pain pattern. First described by Maigne6,7, cervicogenic dorsalgia (CD) is not well recognized outside of chiropractic literature (a literature search in PubMed revealed no articles). Anatomically, the DSN provides that direct link from the mid to lower cervical spine to the mid-scapular region.8–10 Notalgia paresthetica (NP) is a condition of the upper to mid-thoracic spine that involves pruritis, numbness and tingling, and pain.11–15 The etiology of this condition is elusive, and its treatment using conservative therapies has also been met with mixed results. 11,13,16 In the paper by Sultan et al.1, two of the 29 patients that tested positive for DSN neuropathy had pruritis in the upper to mid-back area with one of those having a decreased ability to sense a pinprick over the area. This, along with a dissection report by AF Dixon in 1896 that showed cutaneous nerve fibres from the DSN innervating an area of the mid-thoracic spine17, suggests a possible connection between NP and DSN neuropathy. “SICK scapula”, an acronym for the condition Scapular malposition, Inferior medial border prominence, Coracoid pain and malposition, and dysKinesis of scapular movement18, is a condition that has been reported to have rhomboid related scapular winging which suggests DSN involvement. SICK scapula is speculated to be a component of several shoulder related diagnoses including impingement, labral tears and rotator cuff tendinopathies and tears.18 DSN neuropathy may cause scapular winging due to rhomboid atrophy19–20 and may need to be considered as a component of SICK scapula. Several authors mention that DSN neuropathy may be related to a posterolateral arm and forearm pain pattern21–23 that may include the neck, axilla and lateral thoracic wall21. This paper will explore the possibility that the pain pattern may be due to a peripheral nerve neuropathy that includes the DSN, suprascapular nerve, long thoracic and radial nerve with the C5 nerve root being a common thread. A possible mechanism that may explain the etiopathology behind these nerves being affected is explored. The mechanism behind these nerves combining to create this pain pattern while other C5 nerves including the axillary, median, or musculocutaneous nerve, are rarely affected, is unknown and not in the scope of this paper.
The purpose of this paper is to elucidate this little known, but emerging, cause of upper back pain. This paper will include a narrative review of the anatomy and function of the DSN, along with the epidemiology, signs and symptoms and possible mechanisms of injury of DSN neuropathy. It will also explore the possible role of DSN neuropathy in other diagnoses in this area including CD, NP, SICK scapula and a posterolateral arm pain pattern.
Methods
The methods used to gather articles for this paper included: searching several electronic databases and hand searching relevant references from journal articles and textbook chapters. Table 1 outlines the electronic databases used in the search. The following terms were used in the searches: dorsal scapular nerve, dorsoscapular nerve, nervus dorsalis scapulae, and mid-thoracic pain. It should be noted that “dorsoscapular nerve” is not recognized as a proper anatomic/medical term for the DSN but was found to be used while procuring articles during the literature search.
Table 1.
Sources used in the search for articles for this manuscript.
|
Due to a relative lack of articles found in the electronic database search, the bulk of the articles and textbook chapters were found by hand searching the references of each article and attempting to purchase or obtain these articles through available college and university libraries. Google Scholar was used to retrieve hand searched articles that were not otherwise retrievable and briefly examined to see if all relevant articles had been identified. Due to the lack of limiters, Google Scholar was not used as a main search engine source.
Results
Searching the electronic databases, 114 articles were found. Once duplicates were removed there were 57 articles of which twenty-nine were retrieved. There were 26 articles and textbook chapters retrieved by hand searching the articles that had been retrieved equaling 55 articles of which 47 relevant articles were used in this report.
Of the 57 articles from the database search, only 29 articles were retrieved from this list. The articles not retrieved were eliminated due to language issues, and a lack of relevance determined from the abstract, and due to an inability to procure the article. All of the articles retrieved by hand searching were used in this report. The remaining eight articles that were retrieved and not used was due to a lack of relevance to the subjects covered in the narrative review after reading the full article.
Discussion
Origin
The DSN is typically reported to arise from the anterior ramus of the C5 nerve root directly or as the first branch of the superior trunk of the brachial plexus.8 In a cadaveric study, Ballesteros and Ramirez8 found that this usual presentation was only in 17.9% of cadavers. In another 30.4%, it still arose from the usual position but shared a common branching trunk with the long thoracic nerve. The other reported variations included C4 in 28.4% and C4 and C5 in 23.1%. In a cadaveric case report by Shilal et al.9, the DSN was found to have input from the C6 nerve root. Interestingly, the long thoracic nerve on this individual arose from the C6 and C7 nerve roots only with an aberrant communicating branch between the dorsal scapular and the long thoracic nerves.
In another cadaveric study by Tubbs et al.10, the DSN originated from C5 in 19 of the 20 sides (10 cadavers) with one originating from the C5 and C6 spinal nerves. In a cadaveric study done by Lee et al.24, the DSN originated from the fifth cervical anterior ramus in 75.8% of the cases. In 9.0%, it arose from the superior trunk of the plexus while in 7.6% it was from the fourth and fifth cervical anterior rami and in another 7.6% from the sixth cervical anterior rami. In the anatomic study by Chen et al.21, one patient had bilateral input to the DSN from C3–4.
In a cadaveric study by Nguyen et al.25, they reported a C5 origin in 70% (16 of 23 cadavers), 22% from C4 and 8% from C6. No combination of nerve roots was reported in this study. In a study by Malessy et al.26 on four cadavers (one side only, two male and two female), the DSN arose from C4 and C5 in all specimens. It seems that the DSN has been erroneously reported as arising from C4 to T110,27,28, and from C8 only22.
Pathway
The course of the DSN as described by Chen et al.21, has it immediately pass obliquely and inferiorly through the middle scalene without innervating it. Classically, the middle scalene is described as acting to flex the cervical spine when contracting bilaterally, ipsilaterally laterally flex and contralaterally rotate the cervical spine when acting unilaterally, and to elevate the first and possibly the second rib with forced inspiration.29–31 Olinger and Homier29 and Buford et al.32 suggest that the scalenes have the ability to ipsilaterally rotate the cervical spine and can be stretched with both ipsi and contralateral rotation. The middle scalene is normally innervated by branches from the anterior rami of the third through eighth cervical spinal nerves33. The middle scalene is often described as an entrapment site of the DSN21 and thus its function may play a part in determining the role of the cervical spine in the tensioning of the DSN.
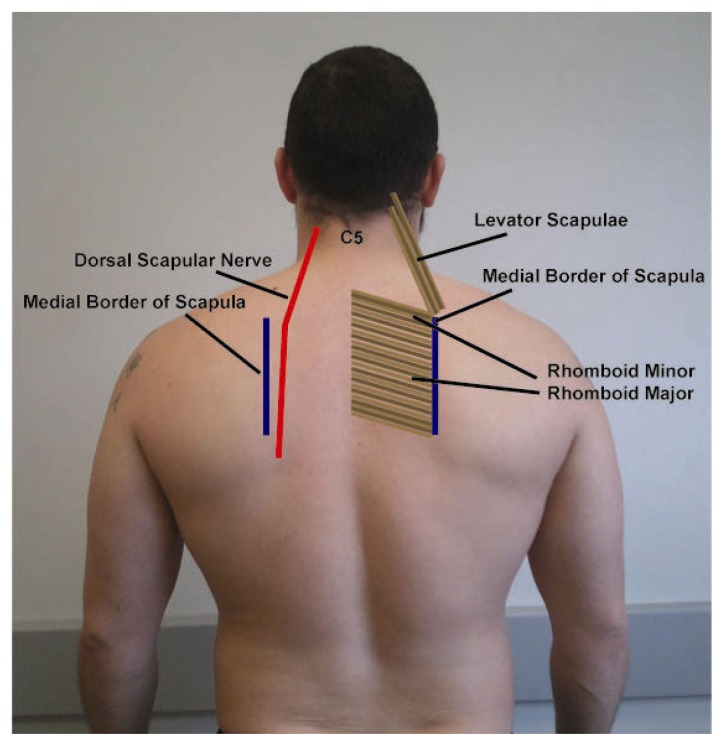
The DSN then runs inferiorly and slightly laterally between the superior fibres of the upper trapezius medially and the levator scapulae laterally. It then passes deep to the upper trapezius fibres as they curve/course laterally toward the acromion, lying anterior to the rhomboid major and minor but posterior to the serratus posterior superior muscle (SPS). The main trunk of the DSN lies medial to the medial border of the scapula as it travels inferiorly to the inferior medial border of the scapula that typically ends at the level of the T7 spinous process31 (see Figure 1 and 2).
Figure 1.
Pathway of the dorsal scapular nerve
Figure 2.
Dissection showing the dorsal scapular nerve.
The dorsal scapular nerve is shown innervating the levator scapulae, rhomboid minor and rhomboid major muscles. The rhomboid major and minor are reflected from the midline showing the DSN attached to the anterior aspect of each. Also shown is the C3 and C4 nerves innervating the upper portion of the levator scapulae
A case report by George and Nayak34 described a variation of the pathway. They found that the DSN came from the anterior ramus of C5 and made a loop around the deep branch of the cervical artery suggesting a possible mechanism of compression. It then continued along its normal path as described above. In the Tubbs et al.10 study, they reported that in all twenty sides, the DSN was intertwined with the dorsal scapular artery and was found along the anterior border of the rhomboid major and minor muscles. In the study by Lee et al.24, the DSN pierced both the middle and posterior scalene in 6.4% of the cases. Martin and Fish35 report the DSN piercing the levator scapulae as it travelled inferiorly in nine of their 35 dissected specimens suggesting a possible area of compression.
In the cadaveric study by Nguyen et al.25, the DSN pierced the middle scalene in 74% of their cases, while passing anterior and posterior to the middle scalene in 26% (13% each).
Function
The DSN’s main function is the innervation of the rhomboid major and minor which retract, elevate and stabilize the scapula. It also acts to rotate the lateral border of the scapula downward.35
The DSN will also innervate the levator scapulae (LS) muscle. In a cadaveric study, eleven of the thirty-five specimens showed DSN innervation of the LS.36 The other source of innervation to the LS is C3 and C4 via the cervical plexus.36 The LS mainly acts to elevate the scapula, rotate the glenoid cavity inferiorly by rotating the scapula and will retract the scapula.31 It also acts as an accessory breathing muscle during dysfunctional breathing.37
The DSN was reported to innervate the LS only in 48% of the cases described by Nguyen et al.25 In the other 52% of the cases, the DSN innervated the LS and the rhomboid minor and major muscles combined. This is the first study found that describes the DSN as only innervating the LS and no mention was made of what was providing innervation to the rhomboids in these cases.
In the cadaveric study by Malessy et al.26, they report that the cranial aspect of LS was innervated by a branch from C3, with the caudal aspect innervated by C4 that combined with a C5 branch to supply the rhomboids in all four specimens.
Kida and Tani38, in a cadaveric case report showed the DSN sending a branch to innervate the SPS muscle. Vilensky et al.39 describe the medial origin of the SPS as the spinous process of the sixth cervical to the second thoracic. It traverses obliquely, laterally and inferiorly to insert on the upper border of ribs two to five just lateral to their angle. Its normal innervation is the intercostal nerves ranging from T1 to T4 or T5.39 According to Vilensky et al.39, most textbooks describe the SPS as having a respiratory function due to its location on the ribs. They suggest that it may not in fact be active during respiration but may have a proprioceptive function for the thoracic spine possibly during respiration.
Normally, the dorsal scapular nerve contains only motor fibres, but an old dissection case report17 describes sensory fibres from the nerve that innervated a small area of skin at the level of the fifth and sixth thoracic vertebrae. This finding may suggest a connection from the cervical spine to notalgia parasthetica, an elusive diagnosis of pruritis and/or pain and dysesthesia in an area of the mid scapular region.
Epidemiology
Musculoskeletal thoracic pain is common in the general population. The annual prevalence of thoracic spine pain in adults ranges from 15.0% in Swedish adults (aged 35 to 45 years) to 34.8% in Swedish working adults (aged 16 to 65 years).2–4 The lifetime prevalence for thoracic spine pain in adolescents was 15.6 to 19.5%.3 In a study by Briggs et al.3, it was reported that factors associated with thoracic spine pain in children and adolescents includes female gender, postural changes associated with backpack use, backpack weight, participation in specific sports, chair height at school, and difficulty with homework. In adults, thoracic spine pain was associated with concurrent musculoskeletal symptoms and difficulty performing activities of daily living. Thoracic pain is also commonly associated (65.5%) with neck pain in individuals injured in motor vehicle accidents.5
Pain and dysfunction arising from compression of the DSN has often been reported as rare23,40, or not included as a cause of neurologic related shoulder injuries41, or as a differential diagnosis in posterior upper thoracic pain42. However, a report by Sultan et al.1 suggests that this may not be the case. In their study, 55 patients with unilateral interscapular pain were evaluated. The diagnosis for these patients varied from no diagnosis to thoracic degenerative discogenic pain, costovertebral joint dysfunction, levator scapulae syndrome, thoracic facet syndrome, dorsal back strain, myofascial pain of the rhomboids and finally DSN entrapment. They found that there was evidence of DSN neuropathy in 29 patients (52.7%) and another five were at the upper cutoff limit which would bring the total to 61.8% if these were counted as having DSN involvement.1
In the study by Chen et al.21, they examined and treated 36 patients with dorsal scapular nerve compression. There were 28 female and eight male patients whose ages ranged from 29 to 52 years with an average age of 34 years. Of the 36 patients, symptoms were unilateral in 34, two were bilateral, 20 were on the right side and 16 on the left. Sultan et al.1 included 42 women and 13 men, and an age range of 22 to 52 years (average 40.2). There were 29 patients that had symptoms on the right side and 26 on the left. Only 29 of these patients were considered testing positive for DSN neuropathy on electrophysiologic evaluation but these were not broken down into gender.
Signs and Symptoms
DSN neuropathy may present on a spectrum from complete function to complete atrophy of the muscles it innervates. This spectrum would include varying levels of: pain intensity and character along a portion of or its entire pathway; and tightness and weakness in the muscles it innervates.1 Other symptoms may include dysesthesia and pruritis in the midscapular region1, and radiation of the pain along the posterolateral aspect of the shoulder, arm, and forearm21–23,43. Chen et al.21 also report DSN involvement in neck, axilla, and lateral thoracic wall pain.
Other findings may include a loss of pinprick sensation medial to the scapular border1, and varying levels of loss of range of motion of the cervical spine, typically ipsilateral rotation and contralateral lateral flexion22,40. A loss of range of motion of the affected side shoulder has also been outlined although no specific movements were described.1,40 Cervical flexion, ipsilateral lateral flexion1, and extension19 have also been reported to aggravate the pain along the DSN. Pain on palpation of the thoracic spinous21, thoracic facet and costotransverse joints may also be present1. Relative hypertrophy and spasm of the neck musculature has also been reported.40 An elongated C7 transverse process has been reported in association with this condition by a few authors.1,21,40
Weakness of the rhomboids may cause varying levels of winging of the scapula. Ravindran20 describes two cases of suprascapular neuropathy in a brother and sister that played volleyball at a high level. Each had electromyographical confirmation of chronic neurogenic changes in the supraspinati, infraspinati and rhomboid muscles with normal findings in the trapezius, deltoid and serratus anterior. The neurogenic changes mentioned presented as muscle weakness and wasting of the infraspinatus, as well as weakness in the supraspinatus and rhomboids. Both had mild winging of the scapula that didn’t change with shoulder ranges. It was postulated that they either had a concurrent DSN neuropathy or an anatomical variation of the suprascapular nerve innervating the rhomboids – which has not been reported in cadaveric studies.20 Moderate to more severe cases of scapular winging due to DSN injury are reported by several authors.19,28,43–47
Benedetti et al.43 describe the case of a 24 year old woman that presented four years after a crash in which she sustained a pelvic fracture as well as abdominal and chest trauma. For the past year, she had been experiencing upper back pain with constant left shoulder pain with radiation and weakness of the left upper limb. An MRI showed no sign of a C5 radiculopathy. She presented with left scapular winging along with severe global loss of range, tingling and numbness in the left upper limb and tremor with the initiation of active movment. There was no mention of range of motion findings of the cervical spine. An EMG study was performed confirming signs of denervation of the left rhomboid suggestive of a DSN lesion.
Plezbert and Nicholson47 report on a case of a 28 year old with persistent cervical and thoracic pain along the medial border of the scapula and left shoulder weakness. The patient had been originally diagnosed with cervical-thoracic myofascitis but was re-examined due to little progress. The re-exam noted weakness in the rhomboid (3/5) and posterior deltoid (4/5) with mild inferior scapular angle winging. Reflexes and sensory testing was found to be within normal limits. Restrictions on palpation were noted in the cervical, upper thoracic and left upper costovertebral joints. Deep palpation of the anterior and middle scalenes, as well as, left cervical rotation and cervical extension recreated the pain along the medial border of the scapula. The patient’s diagnosis was subsequently revised to having a left DSN entrapment neuropathy secondary to scalene myofascitis. Radiographs of this patient showed a flattened thoracic kyphosis and a congenital block vertebrae at C2–3.
Etiology
The main etiology described for DSN entrapment is hypertrophy of the middle scalene muscle causing compression of the nerve as it passes through.21 Mondelli et al.48 describes the case of DSN neuropathy in a bodybuilder whom they felt had tractioned the nerve in a hypertrophied middle scalenus muscle during exercises of neck flexion and heavy shoulder raises and lowers.
There are several other case reports in the literature that outline a variety of different mechanisms. In a case of repetitive lifting, Argyriou et al.44 describe rhomboid atrophy and scapular winging secondary to DSN neuropathy in a worker required to manually handle and carry bags weighing eight kilograms across his body. Haim and Urban49 describe the case of a rhomboid dystonia following thoracic disc surgery that required DSN blocks to resolve. Debeer et al.28 report on a case involving a 15 year old girl. The girl was being treated for three years for idiopathic scoliosis utilizing a corrective brace that the authors felt caused a compressive neuropraxia to the DSN and subsequent, severe shoulder dysfunction secondary to scapular winging. Ravindran20, as mentioned, describes siblings with suspected DSN neuropathy due to repetitive overhead activity related to volleyball. Kugler et al.50 mention an estimate by Dubotzky and Leistner that a highly skilled volleyball attacker practicing 16 to 20 hours per week will spike the ball approximately 40 000 times per year. Kaplan et al.45 describe a case of an 18 year old female with a one year history of right scapular pain and mild scapular winging. Denervation of her right rhomboid major and levator scapulae were found and attributed to 30 months of continuous studying (four to five hours per day) for a weekly three hour exam. This case suggests that continuous stretch of the DSN secondary to poor posture may be enough to cause a chronic neuropathy. Akgun et al.19 describes a more acute case of DSN injury in a 51 year old man that felt a sharp pain in the right shoulder after lifting a heavy box overhead. In another case report, Jerosch et al.51 describes the case of a 19 year old female that anteriorly dislocated her right shoulder following a fall in judo. Two surgeries to stabilize the shoulder were unsuccessful and upon presentation to a new clinic, winged scapula with atrophy of the rhomboids and serratus anterior were noted. EMG confirmed damage to both the long thoracic and DSN.
In the study by Sultan et al.1, two of the 29 patients with DSN neuropathy developed the condition acutely after lifting heavy objects overhead in a manner similar to Akgun et al.19. The remainder described a gradual, insidious onset of the condition. In nine of these patients, they related the onset of their symptoms to frequent, repetitive use of their dominant side in overhead activities related to work, recreation and sport. Of these nine patients, three were teachers, two were painters, two electricians, one was a volleyball player and one a basketball player1.
Brower22 also suggests that a traction injury to the nerve secondary to a whiplash event is a possible etiology although no specific cases were discussed. Benedetti et al.43, describe a DSN lesion following a crash although there was no mention of it being a car or other vehicle. They felt her DSN injury was likely due to the chest trauma sustained in the accident. No mechanism of injury was mentioned in the case reported by Plezbert and Nicholson.47
In summary, the DSN may be injured due to overhead activity during work and sport/recreation that may be repetitive and in some cases involve heavy loads, chronic postural strain, iatrogenic (either post-surgical or post bracing), or following a crash involving a motor vehicle of some kind.
Possible role of DSN neuropathy in other conditions
Cervicogenic dorsalgia
Maigne suggests that 70% of common dorsal pain originates from the lower cervical spine.6,52 This compares to the estimate by Sultan et al.1 who found that 53% to 62% of patients in their study with unilateral interscapular pain had DSN neuropathy. Maigne6 and Terrett52 both report that women are more affected than men with Terrett52 estimating it at a 6:1 ratio. This ratio is slightly higher than the DSN gender ratio of 3.5:1 in Chen et al.21 No mention of side to side differences was mentioned in Maigne6, Terrett52 or Engel and Gatterman7 or how often the condition may be bilateral.
Engel and Gatterman7 suggest that the cause of the cervical spine irritation that’s creating the thoracic spine pain may lie in a variety of structures including the disc and the facet and the diagnosis should include these as the primary diagnosis with the thoracic pain mentioned as an associated symptom. The difficulty in diagnosing this condition is the patient may consistently deny any associated neck pain especially in the subacute and chronic stages7,52 which is similar to DSN neuropathy1.
Maigne6 and Terrett52 describes the interscapular pain of CD as well localized or diffuse, a cramping sensation, the sensation of a weight, a burning or painful tension, a feeling of fatigue and/or a deep-seated intrathoracic pain. They also suggest that cervical ROM may range from normal, to minimally to markedly decreased in certain directions. Again, similar to DSN neuropathy, the interscapular pain in the cases described by Terrett52 were recreated by ipsilateral cervical spine rotation and further increased by cervical extension from the rotated position. The pain usually decreases with rest, however, it may be aggravated during sleeping especially if the patient’s preferred position is prone with rotation to the affected side.6,7,52 There is no mention of radiation of the pain across the scapula and along the posterolateral arm with CD unlike in DSN neuropathy.21–23
Maigne6 also describes a “cervical point of the back” found during the physical exam for CD. Maigne6 suggests that this point is a consistent point of pain just lateral to the spinous processes (2 cm) which is found with palpation between the T5 and T6 spinous in a large percentage of patients. This is very similar to the pain at the thoracic spinous described by Chen et al.21 in patients with DSN neuropathy. Maigne6 also describes a mid-thoracic “cellulalgic band” found by skinrolling. This feature has not been described in the literature pertaining to DSN irritation although it has been mentioned with regard to notalgia paresthetica.11
Radiographic findings of the cervical and thoracic spine are often negative similar to those taken in patients with DSN neuropathy. Similar to a DSN neuropathy, CD is often misdiagnosed as a subluxated rib or a trigger point7,52, thoracic posterior facet syndrome, thoracic subluxation, T4 syndrome, discogenic disease, costovertebral lesion, intercostal muscle spasm, interscapular or scapular muscle spasm1.
The “anterior doorbell sign” described by Maigne6 consists of recreating the intrathoracic pain by applying pressure to the “responsible level and at the anterolateral part of the spine”. Maigne2 suggests it is an inconstant finding and is positive in six of ten cases of thoracic pain of cervical origin. He also suggests that to find the “cervical doorbell point” you may have to vary the palpation point by a few centimetres6. Engel and Gatterman7 suggest that the “cervical doorbell point is the location of the emergence of the anterior nerve root and is often mistaken for a “scalene trigger point”. The location of the structure described by Maigne6, and Engel and Gatterman7 may be the location of the DSN as it pierces the middle scalene as it branches from the anterior rami21.
Treatment of CD is focused on the cervical spine6,7,52 with the predominant therapeutic modality being manipulation and less often exercise and massage or soft tissue therapy to the thoracic and cervical spine musculature. Manipulation of the thoracic facet and costovertebral joints is often met with temporary relief only and should tip the practitioner to a different primary cause of the intrathoracic pain.52 Plezbert and Nicholson47 describe the successful treatment of a case of DSN neuropathy secondary to scalene myofascitis. The patient was treated with trigger point therapy of the scalene musculature, high-volt galvanized current to the rhomboid muscle utilizing muscle strengthening settings, as well as chiropractic manipulation to the cervical, thoracic and upper posterior ribs.
There is no mention of scapular winging in any of the cases or papers by Engel and Gatterman7, Maigne6, or Terrett52 and none of them mention the possibility of the thoracic pain being the result of a DSN neuropathy.
Considering the few differences, the similarities in presentation of DSN neuropathy and CD suggest that further investigations should be carried out to see if they are in fact one and the same.
Notalgia paresthetica
Notalgia paresthetica (NP) is a condition characterized mainly by unilateral pruritis in an area medial to the scapula and lateral to the thoracic spine.11–15 It is often accompanied by pain, numbness or tingling, paresthesia, or hyperesthesia and is commonly found to have local hyper-pigmentation thought to be the result of chronic scratching. 13 One author suggests that it may be that “unreachable itch” that led not only humans but primates (apes in particular) to develop back scratchers to deal with it.13 Ellis13 also suggests that “pruritis is an often unrecognized symptom of nerve damage”. This condition was first described by Astwazaturow in 1934 but remains difficult to treat even today.14
The condition is thought to be neurogenic in origin due to the relative, short term effectiveness of drugs used to aid in the treatment of nerve pain including topical capsaicin, botox, nerve blocks and gabapentin.13 Most often NP has been attributed to the entrapment of the T2–T6 posterior rami that supply cutaneous innervation to the area but its true etiology remains elusive.16 Some authors suggest that the entrapment may be due to spasms of the paraspinal musculature, mainly the multifidus, the scapular stabilizers including the rhomboid and trapezius, or impingement due to degenerative changes in the thoracic spine and/or thoracic herniated discs.53 Other treatments aimed at the proposed neuromusculoskeletal pathologies have also had some success at treating NP including exercise, acupuncture, and osteopathic treatment including muscle energy, soft tissue, inhibition and fascial release of the area11 as well as ultrasound and radiation physiotherapy54. Another case series of patients with long thoracic nerve injury or of the C5–7 cervical roots found that muscle stimulation (EMS) of the serratus anterior was helpful in the treatment of NP.12
The findings of AF Dixon17 in 1896 that the DSN had cutaneous branches that innervated the skin in the mid-scapular area suggests a possible direct link of NP and DSN neuropathy. Sultan et al.1 in fact describes two patients with DSN entrapment that have a concurrent itching sensation along with pain and one of the two patients had reduced pinprick sensation in the area just medial to the scapular border. Along with the pruritis, pain along the medial scapular border seems to be a feature of NP13 which has already been discussed previously with respect to DSN neuropathy1.
Notalgia paresthetica, like DSN neuropathy, is predominantly a chronic condition found in middle to older aged women at a 2:1 or 3:1 ratio versus men.54 In a review by Perez-Perez15, the author’s personal observation suggests NP may be as high as 9:1. In a study by Wallengren55, their patient distribution was 4:1 women to men, age range 35 to 70 years with a mean age of 59 years, with a unilateral distribution in 19 of the 20 (left side 13, right side six) with one patient having the condition bilaterally.
The DSN has a known anatomical and functional link to the long thoracic nerve8,9,21 so EMS of the serratus anterior may be beneficial to DSN neuropathy although this has not previously been shown in the literature12. The aforementioned cases of NP did not note any assessment of the cervical spine or any exacerbation of symptoms with neck movement, although neck related injury or surgery to the C5–7 area were described in two of the four cases by Wang et al.12 Also, an NP case of two years duration was reported by Alai et al.56 to have a decreased range of motion in the neck (specific directions were not reported) associated with noticeable bilateral cervical muscle spasm greater on the left. The patient did have a history of multiple motor vehicle accidents resulting in whiplash associated injuries to the neck and infrascapular back area 15 to 20 years prior. The patient’s cervical spine MRI revealed degenerative changes and mild disc protrusions of C4 through C7 which were felt to be contributing factors to the NP.56 Richardson11 also reports a case of NP with associated neck, upper back and low back pain of approximately two years duration with symptoms that began following a rear-end motor vehicle accident. Their patient also demonstrated decreased cervical range of motion as well as tissue texture changes in vertebrae T2 through T7 with tenderness of the corresponding spinous processes and “an appreciable ropy and fibrotic texture at the left scapula”11. The tissue texture changes sound similar to those described by Maigne6 with regard to changes found in CD. In two cases of exercises being used to treat NP, rhomboid weakness was noted causing protracted scapula.57 It was postulated that the NP was caused by a constant stretch of the T2 to T6 spinal nerves. This mechanism, however, may also cause a constant tension on the DSN resulting in DSN neuropathy and increasing rhomboid weakness if prolonged.1
One area where the comparison between DSN neuropathy and NP requires further study is a small portion of the affected area itself. The T6 dermatome falls below the level of the inferior border of the scapula58 and thus below the level of the rhomboid attachment on the inferior medial border of the scapula. This would suggest that the DSN neuropathy alone would not affect this area although a possible combination of DSN neuropathy and thoracic cutaneous nerve neuropathy, as outlined later in the discussion, may be the potential cause.
SICK scapula
SICK scapula is an acronym that stands for Scapular malposition, Inferior medial border prominence, Coracoid pain and malposition, and dysKinesis of scapular movement. 18 SICK scapula is a complex of scapular issues affecting overhead athletes. Certain components of SICK scapula bear a striking resemblance to the findings of DSN neuropathy. Burkhart, Morgan and Kibler18 report that patients with an isolated SICK scapula “may complain of anterior shoulder pain, posterosuperior scapular pain, superior shoulder pain, proximal lateral arm pain or any combination of the above. In addition, posterosuperior scapular pain may radiate into the ipsilateral paraspinous cervical region or the patient may complain of radicular/thoracic outlet type symptoms into the affected arm, forearm, and hand …”. In particular, the type II pattern of dynamic scapular dyskinesis has entire medial border winging of the affected scapula at rest that becomes more prominent with the cocking and elevation phase of pitching. They suggest that it is associated with upper and lower trapezius and rhomboid muscle weakness.18 They also suggest that continued SICK scapula can lead to rotator cuff impingement, SLAP lesions and possible “dead arm”.18
DSN neuropathy should be considered in these patients especially with scapular winging, interscapular pain, and radiation along the posterolateral arm and forearm.1 DSN neuropathy has been shown to be associated with overuse injuries sustained in overhead athletes.1,20
Posterolateral Arm Pain – C5 Peripheral Nerve Neuropathy
Many authors report a posterior shoulder/posterolateral arm pain pattern associated with DSN neuropathy, scapular dysfunction and shoulder injuries.1,18,20–23,43,59 This may be accompanied by occasional pain to the forearm and posterior hand22,23 and the axilla and lateral thoracic wall21.
There is debate in the literature surrounding the existence of active and latent trigger points and their ability to refer pain versus the pain being of peripheral nerve origin.60,61 If you briefly examine the pain pattern from both sides, there are some interesting similarities and omissions when it comes to this particular pain pattern. From a peripheral nerve standpoint, the pain pattern outlined above would suggest involvement of the DSN, long thoracic (lateral thoracic wall), suprascapular (scapular) and radial nerves (posterolateral arm and forearm) and possibly the axillary (posterolateral shoulder) and musculocutaneous nerves (posterolateral forearm). The common thread for these nerves would be the C5 nerve root suggesting a C5 peripheral nerve neuropathy. Anecdotally, the DSN, suprascapular, long thoracic and radial nerves are more commonly involved as a group.59 The axillary and/or musculocutaneous nerves are rarely combined with the other four when this pain pattern is present. The median nerve also shares a C5 nerve root but again, anecdotally, is rarely involved. The reason for the inclusion or exclusion of particular C5 related peripheral nerves is unknown.
A review of the particular trigger point referral patterns outlined in Travell and Simons upper limb trigger point manual62 revealed the following: the rhomboids (innervated by the DSN) refer locally as well as over the scapula; the levator scapula (innervated by the DSN in 31%–100%25,36) refers to the rhomboid, scapula and posterior shoulder area; the serratus anterior (innervated by the long thoracic nerve) refers to the rhomboid area as well as the medial arm, forearm and hand (in the distribution of the ulnar nerve); the scalenes (innervated segmentally), supra and infraspinatus (innervated by the suprascapular nerve) and the tricep brachii (innervated by the radial nerve) refer pain along the upper back, across the scapula, down the posterolateral arm to the hand in the exact pain pattern described. The posterior deltoid (innervated by the axillary nerve) will refer locally and into the posterior upper arm while the coracobrachialis (innervated by the musculocutaneous nerve) will refer in the posterolateral arm and forearm.62 The bicep brachii and brachialis (also innervated by the musculocutaneous nerve) will refer locally and to the cubital fossa.62
Neither the trigger point nor the peripheral nerve theories seem to completely explain the posterolateral pain pattern described in DSN neuropathy and further study to determine the cause is suggested.
Etiopathology
Sultan et al.1 suggests three possible mechanisms for the cause of pain in patients with a known DSN neuropathy. The first is entrapment or stretch, whether acute or prolonged, of the nerve can induce neuropathic trunk pain which involves the nervi nervorum. The second mechanism is the presence of myofascial pain syndrome with subsequent DSN entrapment in the taut bands of the rhomboids containing the trigger points. The third mechanism is the pain is caused by the stretching of the cutaneous nerves from the thoracic posterior primary rami to the area due to scapula winging – similar to the mechanism proposed to explain NP – even though the pain may be there in the absence of scapular winging.1
The first mechanism outlined by Sultan et al.1 is a plausible initiating factor of the neuropathic trunk pain and subsequent pain pattern. This is due to the activation of the nervi nervorum that are nociceptive63,64 and irritated with stretching of the nerve they innervate. With nerve compression, Mackinnon65 describes a process by which there is an interruption in the blood-nerve barrier that allows a leakage of fluid from the microvessels, or vasa nervorum, supplying the nerve. The blood-nerve barrier breakdown allows entry to, and an accumulation of, inflammation related mediators that causes edema and eventually scar formation.65 Sultan et al.1 outlines a mechanism proposed by Ellis66 to explain thoracic outlet syndrome that suggests that this type of trauma to the nervi nervorum creates a cycle of inflammation within the perineurium that results in an individual nerve “internal compartment syndrome”. Mackinnon describes a similar process calling it a “mini-compartment” syndrome within the nerve.65 With repeated or continued trauma, there is a vicious cycle of neural desensitization that causes more inflammation with even less trauma.
Along with the inflammation within the nerve, Ellis66 suggests that highly innervated and inflammatory fibrous bands and persistent adhesions are formed that adhere the nerve to adjacent structures which further limits the movement of the nerve. This seemingly describes the mechanism behind the double crush syndrome as outlined by Upton and McComas.67 They originally hypothesized that proximal level nerve compression could cause more distal sites to become compressed65,67 calling it a “double crush”. This was further expanded to suggest that it was more of a multiple crush situation and also that more distal compression sites could cause proximal site compression, a reverse double crush.65 The development of the fibrous bands along the route of the nerve would create individual tension sites adding to the inflammation and suggesting the need to evaluate the nerve along its entire route prior to treatment. This could also help explain the estimated 1% to 25% failure rate for carpal tunnel release surgery.68
The increasing compartment pressure in the nerve causes more compression of the nervi nervorum causing further pain and fibroblast proliferation, and continued fibrosis. The inflammation, if not identified and treated appropriately, can spread both perineurally (within the nerve) and endoneurally causing activation of the CNS.66 Ellis66 suggests that this can then cause the subsequent inflammation of other adjacent/connected nerves, and can lead to mirror symptoms in the opposite limb.
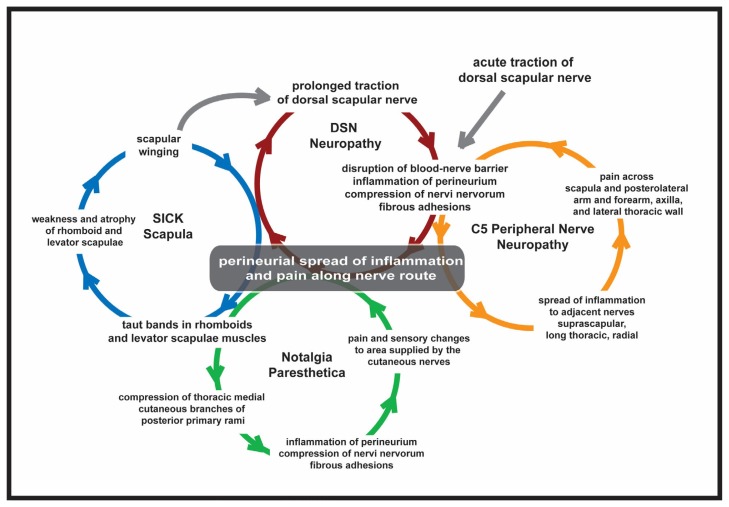
Although there is debate in the literature regarding the existence of active and latent trigger points60,61 as a theory of myofascial pain syndrome, most manual therapists would agree that taut, palpable, painful bands in muscle can be found in all areas of the musculoskeletal system. It is conceivable that these taut bands could be initiated by DSN neuropathy and not the reverse. In 21 of the 29 patients with DSN neuropathy in the paper by Sultan et al.1, the primary diagnosis was myofascial pain syndrome of the rhomboid major with identified taut bands. Further to this, the taut bands could cause entrapment of the thoracic medial cutaneous nerves from the thoracic posterior primary rami that supply this area as they pass directly through the rhomboid and trapezius on their way to the skin.12 To continue this argument, if DSN neuropathy causes scapular winging in these individuals, traction of these cutaneous branches could occur causing both compression and traction. This would create continued inflammation and nervi nervorum irritation within these nerves causing both pain and sensory changes in the area. (See Figure 3).
Figure 3.
Proposed mechanism of dorsal scapular nerve neuropathy, notalgia paresthetica, C5 peripheral nerve neuropathy and SICK scapula/scapular winging.
This may help to explain the mechanism behind NP. It is interesting to note that two of the patients with DSN neuropathy in the paper by Sultan et al.1 had both pruritis, (one of the two had diminished pinprick sensation) and scapular winging. This may also be the cause of the pain associated with skin rolling in the area as reported by Maigne6 with regard to CD, as discussed. Interestingly, the “cervical point of the back” outlined by Maigne6 could also be due to irritation of the skin at the spinous innervated by the medial branch of the posterior primary rami. It may also help to explain the limited therapeutic value of the use of topical applications in NP55 in that the cutaneous nerves may only play a partial role. (See Figure 3).
The spread of the inflammation into adjacent nerves as outlined by Ellis66, would help to explain the posterolateral arm pain pattern (suggested C5 peripheral nerve neuropathy) as outlined above. As the inflammation spreads to the other nerves, intuitively, they also become susceptible to fibrosis and persistent adhesions – their own multiple crush situation.65 This becomes very important clinically, as Mackinnon further states, “this concept of double or multiple crush is important clinically in patients who demonstrate multiple levels of nerve compression, as failure to diagnose and treat these multiple levels of injury will result in a failure to relieve the patients’ symptoms.” 65. The effectiveness of treating some or all of the C5 nerves (DSN, suprascapular, long thoracic and radial) and the effect on outcomes should be investigated. (See Figure 3).
DSN neuropathy, like other neuropathies, may exist on a spectrum that includes various levels of pain intensity, dysesthesia and tingling and atrophy of the supplied musculature. It may also show various levels of spread to other adjacent nerves. Anecdotally, most patients reach a particular level of pain only and do not progress to dysesthesia/numbness/tingling or atrophy or irrecoverable nerve damage. It is assumed that the Etiopathology as proposed (in Figure 3) must reach an “equilibrium” of sorts and the patient’s pain will wax and wane within a defined range (ie. a 2 to a 4 on the pain scale). How or why this equilibrium is reached in some patients and not others is not within the scope of this paper but may be due to the level of the initial trauma, the length of time of the chronic compressive/traction cycle and/or the nerve fibre type affected by the inflammatory cycle. The cycle could also be affected by further acute trauma (such as a new or second motor vehicle accident) or a change in the overuse related trauma to the affected area (such as a new (or a change) in job description ie. overhead lifting, or constant sitting with poor posture).
Conclusion
This article provides a review of the origin, pathway, and function of the DSN along with the epidemiology, clinical presentation and proposed etiologies of DSN neuropathy.
DSN neuropathy may be associated with or may be the entity known as cervicogenic dorsalgia. It may also play a role in notalgia paresthetica, SICK scapula and a commonly reported pain pattern along the posterolateral arm and forearm associated with neck, upper back and shoulder pain. Further study is recommended to explore the possible role of DSN neuropathy in these conditions and the possible etiopathology theorized.
It is recommended that DSN neuropathy be considered as a potential contributor to upper to mid thoracic pain and may be the sole cause in some cases. It is hoped that practitioners will begin to include it in their list of differentials in this group of patients.
Table 2.
Flowchart outlining the search strategy and article aquisition
Acknowledgment
Thank you to Dr. Guy Sovak for the preparation and pictures of the dissection used in this paper.
Footnotes
The author does not have any conflicts of interest to declare with regard to the writing of this manuscript.
References
- 1.Sultan HE, El-Tantawi GA. Role of dorsal scapular nerve entrapment in unilateral interscapular pain. Arch Phys Med Rehab. 2013;94(6):1118–1125. doi: 10.1016/j.apmr.2012.11.040. [DOI] [PubMed] [Google Scholar]
- 2.Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness and presenteeism. J Epidemiol Community Health. 2000;54:502–509. doi: 10.1136/jech.54.7.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Briggs AM, Smith AJ, Straker LM, Bragge P. Thoracic spine pain in the general population: prevalence, incidence and associated factors in children, adolescents and adults. A systematic review. BMC Musculoskel Dis. 2009;10(1):77. doi: 10.1186/1471-2474-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Linton SJ, Hellsing AL, Hallden K. A population-based study of spinal pain among 35–45-year-old individuals. Prevalence, sick leave, and health care use. Spine. 1998;23:1457–1463. doi: 10.1097/00007632-199807010-00006. [DOI] [PubMed] [Google Scholar]
- 5.Hincapié CA, Cassidy JD, Côté P, Carroll LJ, Guzmán J. Whiplash injury is more than neck pain: a population-based study of pain localization after traffic injury. J Occupation Environ Med. 2010;52(4):434–440. doi: 10.1097/JOM.0b013e3181bb806d. [DOI] [PubMed] [Google Scholar]
- 6.Maigne R. Orthopedic Medicine: a New Approach to Vertebral Manipulations. Springfield, IL: Charles C. Thomas; 1972. pp. 255–266. [Google Scholar]
- 7.Engel G, Gatterman M. Cervicogenic Dorsalgia. In: Gatterman M, editor. Foundations of Chiropractic: Subluxation. Elsevier Heatlh Sciences; 2005. pp. 448–456. [Google Scholar]
- 8.Ballesteros LE, Ramirez LM. Variations of the origin of collateral branches emerging from the posterior aspect of the brachial plexus. J Brachial Plex Peripher Nerve Inj. 2007;2:14. doi: 10.1186/1749-7221-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shilal P, Sarda RK, Chhetri K, Lama P, Tamang BK. Aberrant dual origin of the dorsal scapular nerve and its communication with long thoracic nerve: an unusual variation of the brachial plexus. J Clin Diagnost Res. 2015;9(6):AD01. doi: 10.7860/JCDR/2015/13620.6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tubbs RS, Tyler-Kabara EC, Aikens AC, Martin JP, Weed LL, Salter EG, Oakes WJ. Surgical anatomy of the dorsal scapular nerve. J Neurosurg. 2005;102(5):910–911. doi: 10.3171/jns.2005.102.5.0910. [DOI] [PubMed] [Google Scholar]
- 11.Richardson BS, Way BV, Speece AJ. Osteopathic manipulative treatment in the management of notalgia paresthetica. J Am Osteopath Assoc. 2009;109(11):605–608. [PubMed] [Google Scholar]
- 12.Wang CK, Gowda A, Barad M, Mackey SC, Carroll IR. Serratus muscle stimulation effectively treats notalgia paresthetica caused by long thoracic nerve dysfunction: a case series. J Brachial Plex Peripher Nerve Inj. 2009;4:17. doi: 10.1186/1749-7221-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellis C. Notalgia paresthetica: the unreachable itch. Dermatol Pract Concept. 2013;3(1):3. doi: 10.5826/dpc.0301a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shin J, Kim YC. Neuropathic itch of the back: a case of notalgia paresthetica. Ann Dermatol. 2014;26(3):392–394. doi: 10.5021/ad.2014.26.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pérez-Pérez LC. General features and treatment of notalgia paresthetica. Skinmed. 2011;9(6):353–358. [PubMed] [Google Scholar]
- 16.Tacconi P, Manca D, Tamburini G, Cannas A, Giagheddu M. Notalgia paresthetica following neuralgic amyotrophy: a case report. Neurolog Sci. 2004;25(1):27–29. doi: 10.1007/s10072-004-0223-9. [DOI] [PubMed] [Google Scholar]
- 17.Dixon AF. Abnormal distribution of the nervus dorsalis scapulæ, and of certain of the intercostal nerves. J Anat Physiol. 1896;30(Pt 2):209–210. [PMC free article] [PubMed] [Google Scholar]
- 18.Burkhart SS, Morgan CD, Ben Kibler W. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641–661. doi: 10.1016/s0749-8063(03)00389-x. [DOI] [PubMed] [Google Scholar]
- 19.Akgun K, Aktas I, Terzi Y. Winged scapula caused by a dorsal scapular nerve lesion: a case report. Arch Phys Med Rehabil. 2008;89:2017–2020. doi: 10.1016/j.apmr.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Ravindran M. Two cases of suprascapular neuropathy in a family. Br J Sports Med. 2003;37:539–541. doi: 10.1136/bjsm.37.6.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen D, Gu Y, Lao J, Chen L. Dorsal scapular nerve compression. Atypical thoracic outlet syndrome. Chin Med Journ. 1995;108(8):582–585. [PubMed] [Google Scholar]
- 22.Brower RS. Differential diagnosis of cervical radiculopathy and myelopathy. In: Clark CR, editor. The Cervical Spine. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 995–1008. [Google Scholar]
- 23.Hammer WI, editor. Functional Soft-Tissue Examination and Treatment by Manual Methods Third Edition. Sudbury, MA: Jones and Bartlett Publishers; 2007. pp. 140–141. [Google Scholar]
- 24.Lee HY, Chung IH, Seok W, Kang HS, Lee HS, Ko JS, Lee MS, Park SS. Variations of the ventral rami of the brachial plexus. J Kor Med Sci. 1992;7(1):19–24. doi: 10.3346/jkms.1992.7.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen VH, Liu HH, Rosales A, Reeves R. A cadaveric investigation of the dorsal scapular nerve. Anat Res Intl. 2016 Aug 1; doi: 10.1155/2016/4106981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malessy MJ, Thomeer RT, Marani E. The dorsoscapular nerve in traumatic brachial plexus lesions. Clin Neurol Neurosurg. 1993;95:17–23. doi: 10.1016/0303-8467(93)90029-g. [DOI] [PubMed] [Google Scholar]
- 27.Pecina MM, Krmpotic-Nemanie J, Markiewitz AD. Tunnel syndrome: peripheral nerve compression syndromes. Boca Raton: CRC Press, Inc; 1997. pp. 59–61. [Google Scholar]
- 28.Debeer P, Van Den Eede E, Moens P. Case report: scapular winging: an unusual complication of bracing in idiopathic scoliosis. Clin Orthoped Rel Res. 2007;461:258–261. [PubMed] [Google Scholar]
- 29.Olinger AB, Homier P. Functional anatomy of human scalene musculature: rotation of the cervical spine. J Manip Physiol Ther. 2010;33(8):594–602. doi: 10.1016/j.jmpt.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 30.Dahlstrom KA, Olinger AB. Descriptive anatomy of the interscalene triangle and the costoclavicular space and their relationship to thoracic outlet syndrome: a study of 60 cadavers. J Manip Physiol Ther. 2012;35(5):396–401. doi: 10.1016/j.jmpt.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 31.Moore KL. Clinically oriented anatomy. 2nd Edition. Vol. 664. Baltimore: Williams & Wilkins; 1985. p. 994. [Google Scholar]
- 32.Buford JA, Yoder SM, Heiss DG, Chidley JV. Actions of the scalene muscles for rotation of the cervical spine in macaque and human. J Orthop Sports Phys Ther. 2002;32(10):488–496. doi: 10.2519/jospt.2002.32.10.488. [DOI] [PubMed] [Google Scholar]
- 33.Rusnak-Smith S, Moffat M, Rosen E. Anatomical variations of the scalene triangle: dissection of 10 cadavers. J Orthop Sports Phys Ther. 2001;31(2):70–80. doi: 10.2519/jospt.2001.31.2.70. [DOI] [PubMed] [Google Scholar]
- 34.George BM, Nayak SB. Neuromuscular variations in the posterior triangle of the neck–a case report. Neuroanat. 2008;7:8–9. [Google Scholar]
- 35.Martin RM, Fish DE. Scapular winging: anatomical review, diagnosis, and treatments. Curr Rev Musculoskelet Med. 2008;1:1–11. doi: 10.1007/s12178-007-9000-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frank DK, Wenk E, Stern JC, Gottlieb RD, Moscatello AL. A cadaveric study of the motor nerves to the levator scapulae muscle. Otolaryngol Head Neck Surg. 1997;117(6):671–80. doi: 10.1016/S0194-59989770051-2. [DOI] [PubMed] [Google Scholar]
- 37.Perri MA, Halford E. Pain and faulty breathing: a pilot study. J Bodywork Move Ther. 2004;8(4):297–306. [Google Scholar]
- 38.Kida MY, Tani M. The human superior posterior serratus muscle supplied by both the intercostal and dorsal scapular nerves. Kaibogaku zasshi. J Anat. 1993;68(2):162–168. [PubMed] [Google Scholar]
- 39.Vilensky JA, Baltes M, Weikel L, Fortin JD, Fourie LJ. Serratus posterior muscles: anatomy, clinical relevance, and function. Clin Anat. 2001;14(4):237–241. doi: 10.1002/ca.1039. [DOI] [PubMed] [Google Scholar]
- 40.Wood VE, Marchinski L. Congenital anomalies of the shoulder. In: Rockwood CA, Matsen FA, editors. The Shoulder. Vol. 1. Philadelphia: WB Saunders; 1998. pp. 99–163. [Google Scholar]
- 41.Duralde XA. Neurologic injuries in the athlete’s shoulder. J Athl Train. 2000;35(3):316. [PMC free article] [PubMed] [Google Scholar]
- 42.Fruth SJ. Differential diagnosis and treatment in a patient with posterior upper thoracic pain. Phys Ther. 2006;86(2):254–268. [PubMed] [Google Scholar]
- 43.Benedetti MG, Zati A, Stagni SB, Fusaro I, Monesi R, Rotini R. Winged scapula caused by rhomboid paralysis: a case report. Joints. 2016 Oct;4(4):247. doi: 10.11138/jts/2016.4.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Argyriou AA, Karanasios P, Makridou A, Makris N. Dorsal scapular neuropathy causing rhomboids palsy and scapular winging. J Back Musculoskel Rehabil. 2015;28(4):883–885. doi: 10.3233/BMR-140583. [DOI] [PubMed] [Google Scholar]
- 45.Kaplan Y, Kurt S, Karaer H. Isolated dorsal scapular neuropathy associated with repetitive minor trauma: a case report. Arch Neuropsychiatry. 2008;45:107–109. [Google Scholar]
- 46.Lee SG, Kim JH, Lee SY, et al. Winged scapula caused by rhomboideus and trapezius muscle rupture associated with repetitive minor trauma: a case report. J Korean Med Sci. 2006;21:581–584. doi: 10.3346/jkms.2006.21.3.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Plezbert JA, Nicholson CV. Dorsal scapular nerve entrapment neuropathy: a unique clinical syndrome. J Neuromusculoskel System. 1994;2(4):206–211. [Google Scholar]
- 48.Mondelli M, Cioni R, Federico A. Rare mononeuropathies of the upper limb in bodybuilders. Muscle Nerve. 1998;21(6):809–812. doi: 10.1002/(sici)1097-4598(199806)21:6<809::aid-mus17>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 49.Haim K, Urban BJ. Dorsal scapular nerve block: description of technique and report of a case. Anesthesiology. 1993;78:361–363. doi: 10.1097/00000542-199302000-00021. [DOI] [PubMed] [Google Scholar]
- 50.Kugler A, Krüger-Franke M, Reininger S, Trouillier HH, Rosemeyer B. Muscular imbalance and shoulder pain in volleyball attackers. Br J Sports Med. 1996;30(3):256–259. doi: 10.1136/bjsm.30.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jerosch J, Castro WH, Geske B. Damage of the long thoracic and dorsal scapular nerve after traumatic shoulder dislocation: case report and review of the literature. Acta Orthop Belg. 1990;56:625–627. [PubMed] [Google Scholar]
- 52.Terrett AG, Terrett RG. Referred posterior thoracic pain of cervical posterior rami origin: a Ccause of much misdirected treatment. Chiropr J Austral. 2002;32(2):42–51. [Google Scholar]
- 53.Savk O, Savk E. Investigation of spinal pathology in notalgia paresthetica. J Amer Acad Dermatol. 2005;52(6):1085–1087. doi: 10.1016/j.jaad.2005.01.138. [DOI] [PubMed] [Google Scholar]
- 54.Raison-Peyron N, Meunier L, Acevedo M, Meynadier J. Notalgia paresthetica: clinical, physiopathological and therapeutic aspects. A study of 12 cases. J Euro Acad Dermatol Venereol. 1999;12(3):215–221. [PubMed] [Google Scholar]
- 55.Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Amer Acad Dermatol. 1995;32(2):287–289. doi: 10.1016/0190-9622(95)90152-3. [DOI] [PubMed] [Google Scholar]
- 56.Alai NN, Skinner HB, Nabili ST, Jeffes E, Shahrokni S, Saemi AM. Notalgia paresthetica associated with cervical spinal stenosis and cervicothoracic disk disease at C4 through C7. Cutis. 2010;85(2):77–81. [PubMed] [Google Scholar]
- 57.Fleischer AB, Meade TJ, Fleischer AB. Notalgia paresthetica: successful treatment with exercises. Acta Dermato-Venereologica. 2011;91(3):356–357. doi: 10.2340/00015555-1039. [DOI] [PubMed] [Google Scholar]
- 58.Lee MW, McPhee RW, Stringer MD. An evidence-based approach to human dermatomes. Clin Anat. 2008;21(5):363–373. doi: 10.1002/ca.20636. [DOI] [PubMed] [Google Scholar]
- 59.Muir B, Kissel JA, Yedon DF. Intraosseous ganglion cyst of the humeral head in a competitive flat water paddler: case report. J Can Chiropr Assoc. 2011;55(4):294. [PMC free article] [PubMed] [Google Scholar]
- 60.Quintner JL, Cohen ML. Referred pain of peripheral nerve origin: an alternative to the “myofascial pain” construct. Clin J Pain. 1994;10:243–251. doi: 10.1097/00002508-199409000-00012. [DOI] [PubMed] [Google Scholar]
- 61.Dommerholt J, Gerwin RD. A critical evaluation of Quintner et al: Missing the point. J Bodywork Movement Ther. 2015;19(2):193–204. doi: 10.1016/j.jbmt.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 62.Simons DG, Travell JG. The upper extremities. Vol. 1. Williams & Wilkins; 1983. Myofascial pain and dysfunction: the trigger point manual; p. 335.p. 345.p. 369.p. 378.p. 428.p. 432.p. 441.p. 448.p. 457.p. 464.p. 623. [Google Scholar]
- 63.Bove GM, Light AR. The nervinervorum: missing link for neuropathic pain? J Pain. 1997;6:181–190. [Google Scholar]
- 64.Sauer SK, Bove GM, Averbeck B, Reeh PW. Rat peripheral nerve components release calcitonin gene-related peptide and prostaglandin E 2 in response to noxious stimuli: evidence that nervi nervorum are nociceptors. Neurosci. 1999;92(1):319–325. doi: 10.1016/s0306-4522(98)00731-3. [DOI] [PubMed] [Google Scholar]
- 65.Mackinnon SE. Pathophysiology of nerve compression. Hand Clin. 2002;18(2):231–241. doi: 10.1016/s0749-0712(01)00012-9. [DOI] [PubMed] [Google Scholar]
- 66.Ellis W. Thoracic outlet syndrome as a disorder of neurogenic inflammation. Vasc Endovasc Surg. 2006;40:251–244. doi: 10.1177/153857440604000312. [DOI] [PubMed] [Google Scholar]
- 67.Upton AM, Mccomas A. The double crush in nerve-entrapment syndromes. Lancet. 1973;302(7825):359–362. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 68.Neuhaus V, Christoforou D, Cheriyan T, Mudgal CS. Evaluation and treatment of failed carpal tunnel release. Orthoped Clin North Am. 2012;43(4):439–447. doi: 10.1016/j.ocl.2012.07.013. [DOI] [PubMed] [Google Scholar]