Abstract
Women who lack social support tend to have a higher risk of postpartum depression. The present study examined the traditional female role, understood here as the adoption of passive and submissive traits specific to Mexican women, as another risk factor for postpartum depressive symptomatology that interacts with social support. Using two waves of data from a longitudinal study of 210 adult Mexican women (20–44 years-old, Mage = 29.50 years, SD = 6.34), we found that lacking social support during the third trimester of their pregnancy was associated with greater depressive symptoms at 6 months in the postpartum, although this relationship depended on the level of endorsement of the traditional female role during pregnancy. Lower social support during pregnancy predicted greater postpartum depressive symptoms for women with higher endorsement of the traditional female role, even when accounting for prenatal depressive symptoms. These results suggest that Mexican women’s experience of social support may depend on their individual adherence to gender roles. Understanding the association between women’s traditional roles and social support in the risk for postpartum depression can improve prevention and educational programs for women at risk.
Keywords: sex roles, traditional female role, postpartum depression, social support
Society often expects motherhood to be joyful, yet 6–20% of women worldwide experience postpartum depression (PPD) or depressive symptoms (Fisher et al. 2012; Gaynes et al. 2005). Although most estimates come from developed countries, the prevalence of PPD is similar in developing countries. For example, in Mexico, a middle-income country with traditional gender roles, as many as 13.3–18% of women suffer from PPD (Almanza-Muñoz et al. 2011; Alvarado-Esquivel et al. 2010; de Castro et al. 2011; Gibbons et al. 1991; Lara et al. 2015; Stickney and Konrad 2007). PPD is a major depressive episode that begins during pregnancy or within 4 weeks of childbirth, although it is often studied clinically up to one year postpartum (American Psychiatric Association [APA] 2013; O’Hara and McCabe 2013). Women suffering from PPD experience at least 2 weeks of prevalent depressed mood, irritableness, loss of interest, and sleep problems (APA 2013).
PPD has deleterious effects on both mothers and infants. Incongruence between women’s expectations of motherhood and reality can result in overwhelming guilt, anxiety, and fear of not meeting social expectations (Beck et al. 2006). These emotions can trigger a dangerous downward spiral where women struggle to regain control of their emotions, cognition, and behavior (Beck et al. 2006; Mauthner 1999). Women may interpret their PPD symptoms as signs that they are bad mothers, further creating a cycle of distress (Mauthner 1999; Mickelson et al. 2016). PPD not only robs mothers of their expected motherhood experience (Beck 2002), but also is negative for infants. Infants whose mothers suffered from PPD formed less secure attachments and had greater difficulties with emotional and cognitive development (Field 2010; Paulson et al. 2006; Sohr-Preston 2006). Given the high prevalence and negative consequences of PPD on mothers and infants, it is important to identify factors that increase women’s risk.
Lack of Social Support
One of the most studied risk factors of PPD is a lack of social support. Internationally, women who lack social support during pregnancy tend to have a much greater risk of experiencing PPD (Beck 2002). This association has been documented among women in Latin America (Canaval et al. 2000; Rojas et al. 2010; Urdaneta et al. 2011), Latinas in the United States (Martinez-Schallmoser et al. 2003; Surkan et al. 2006), and Mexican women (de Castro et al. 2014; Navarrete et al. 2012). Social support during pregnancy includes instrumental, emotional, or informational assistance (Collins et al. 1993; Robertson et al. 2004). Instrumental support addresses practical challenges such as preparing food or gathering supplies for the infant, whereas emotional support includes positive social interaction and expression of esteem (Chojenta et al. 2012; Negron et al. 2013; Robertson et al. 2004). Lastly, informational support may include advice on proper nutrition or suggestions on how to care for the neonate (Collins et al. 1993). Although anyone within a new mother’s social network can provide social support, support from the partner or the woman’s own mother plays the most important role (Clark 2001; Özmen et al. 2014; Xie et al. 2010).
The existing literature suggests that social support has a direct effect on women’s risk of PPD (Beck 2008). Prenatal support provides women with social resources during a time of various psychological and lifestyle changes (Elsenbruch et al. 2007). These resources can ease the adjustment and reduce women’s stress, thereby reducing their risk for PPD (Elsebruch et al. 2007). Indeed, women who reported high support also reported experiencing less stress during pregnancy and were less likely to suffer from PPD (Collins et al. 1993). Similarly, social support helped women in Mexico regain a sense of control in their lives during the perinatal period and limited their risk of PPD (Canaval et al. 2000). The reviewed literature suggests that social support may reduce the risk of PPD by providing women with resources that help them cope with the stressors of pregnancy and childbirth. Given this past work, we expected lower social support to be associated with a higher risk of PPD symptoms.
Traditional Female Role
Gender is a socially constructed identity that is given meaning based on biological sex (Moradi and Parent 2013). Whereas biological sex is typically defined using biological markers, gender is socially created through gendered traits, stereotypes, and roles (Bem 1993; Eagly and Wood 1999; Saunders and Kashubeck-West 2006). The Traditional Female Role (TFR) describes the adoption of a passive and submissive feminine identity due to socialization within a structure that subordinates women’s role (Johannesen-Schmidt and Eagly 2002; Lara 1993). Lara (1993) defined the TFR through traits that are judged as more typical of females than of males and that are considered “socially undesirable.” TFR was operationalized based on the available literature examining the expectations and stereotypes of women’s behavior in Mexican culture. TFR is a part of the Inventory of Masculinity and Femininity [Inventario de masculinidad y feminidad] (IMAFE; Lara 1993), a multidimensional instrument with four independent scales that measure gendered identity. The development of TFR is part of the evolution of gender-role research within the past 40 years, which now emphasizes the social construction of gender through attitudinal and identity measures of gender (Moradi and Parent 2013). In the present study, we defined TFR as women’s self-descriptions in relation to items that reflect the traditional role expected for women in Mexican and Latin American culture (Lara 1989). In other words, in the present study we measured TFR as the degree to which women reported behaving according to the traditional role in Mexico. This role is similar in other Latin American countries that share a male-dominated society, and it has also been referred to as “marianismo” or self-sacrificing women syndrome (Díaz-Loving et al. 2001; Lara and Navarro 1986; Lara and Navarro 1987).
Despite ethnic, socioeconomic, and cultural heterogeneity in Mexico, TFR persists (DiGirolamo and Salgado de Snyder 2008; Hietanen and Pick 2015; Mendez-Luck et al. 2008). Although the rise of women in the work force, lower fertility rates, and greater schooling have affected Mexican women’s role, many women continue to adopt passive and submissive roles (Instituto Nacional de Estadística y Geografía [INEGI] 2010). For example, many Mexican women desire to have a male child in order to satisfy their partner (Navarrete 2012), and many depend on their partner to make important decisions, such as seeking mental health treatment (Lara et al. 2010a). Additionally, their primary role continues to be childbearing and caretaking, even for those women who work outside the home (Rocha-Sánchez and Cruz del Castillo 2013). The socialization of Mexican women as mothers and caregivers, as well as the demanding tasks they face in these roles, may encourage them to display submissive traits (i.e., indecisive, timid, or conforming) and adopt TFR (Díaz-Loving et al. 2001; DiGirolamo and Salgado de Snyder 2008; Lara 1989; Pérez Blasco and Serra Desfilis 1997).
In adherence to TFR, many Mexican women chronically prioritize the needs of others over their own, which often takes a toll on their mental health (DiGiorlamo and Salgado de Snyder 2008; Rocha-Sánchez and Cruz del Castillo 2013). For example, high TFR was associated with greater depression and lower self-esteem among Mexican women (Lazarevich et al. 2013). Another Mexican study found an association between high TFR and greater neuroticism, psychoticism, and depression (Lara 1991). In adopting a passive and submissive personality, women may cede autonomy, self-efficacy, and self-esteem, thereby increasing their risk for depression (Pérez and Gaviña 2014; Rocha-Sánchez and Cruz del Castillo 2013). Women who highly endorse TFR may also have a well-developed sense of emotionality and guilt, as well as greater difficulty defending themselves and acting assertively (Lazarevich et al. 2013). TFR encourages women to care for the needs and desires of others while silently sacrificing their own needs, often leading to poor mental health.
Despite growing evidence of an association between TFR and depression in women (Lara 1991; Lara 1993; Lazarevich et al. 2013), there is a lack of research examining its relation to PPD in particular. Previous work has explored positively stereotyped masculine or feminine traits (i.e., instrumental-self-sufficient and warm-affective, respectively; Bem 1974) as risk factors of PPD. Using the Bem Sex Role Inventory (BSRI), some research has found no association between gender-role orientation and PPD (Berthiaume et al. 1996), whereas others have found an association between high affective femininity and low PPD (Dimitrovsky et al. 2000; Pfost et al. 1989). This inconsistency may be due to measurement at different times during the puerperal period. TFR represents negatively stereotyped traits, and it is rooted in beliefs that motherhood is central to a woman’s femininity, suggesting that pregnancy can strengthen the adoption of this role (Lara 1993). Given the association between TFR and major depression, and the conceptualization of PPD as an episode of major depression, we expected that higher TFR would be associated with greater PPD symptoms among pregnant women.
Endorsement of TFR may also restrict women’s social support and limit the benefits they derive from it. Because TFR emphasizes caretaking without demanding care from others, a Mexican woman who endorses this role may have a smaller social network that includes only her mother and husband (Rocha-Sánchez and Cruz del Castillo 2013). In addition to having a smaller social network, women who ascribe to TFR are more passive, so they may be less able to vocalize their needs and gather support from others (Lara 1993). Moreover, women who are high in TFR may benefit less from the support they do have because of stigmatization. Having emotional difficulties in the postpartum may signal to women that they are not fulfilling their role, thereby stigmatizing their experience of depressive symptoms (Abrams et al. 2009; Choi et al. 2005). Support seeking may also be stigmatized because it violates the prescription for women to be self-sacrificing (Lara 1993). Past work suggests that women who perceive depressive symptomatology to be stigmatized in society seek support through subtler requests (Mickelson et al. 2016) and perceive less social support available to them (Mickelson 2001; Mickelson and Williams 2008). By increasing passivity and feelings of stigmatization, TFR may make it more difficult for women high in TFR to gather and benefit from the support they need during the perinatal period.
Given women’s increased vulnerability and needs during the perinatal period, it follows that adherence to the TFR and its effects on social support may be especially important for PPD. Because the ability to gather and benefit from social support may depend on women’s adherence to TFR, we hypothesized an interactive relationship between social support and TFR as risk factors for PPD symptomatology. Specifically, we expected that women who lacked social support would have more PPD symptoms, but that this would be exacerbated for women who also reported strong endorsement of TFR.
Other Risk Factors
A large body of literature suggests that depressive symptomatology during pregnancy is a strong predictor of PPD (Beck 2001; O’Hara 2009; O’Hara and Swain 1996; Robertson et al. 2004). Given the significant changes that accompany pregnancy, women are often more vulnerable to depression during this time. Women who do express depressive symptoms during pregnancy may have difficulty coping with these changes and are more likely to continue experiencing depression after giving birth (Righetti-Veltema et al. 1998).
Socioeconomic factors also characterize women who are at a greater risk of PPD. Women with low resources may experience greater hardships and fewer opportunities to escape their subordinated position. For example, 28% of Mexico City residents are unable to meet their basic needs (CONEVAL 2014). This lack of resources often limits women’s access to health services and contributes to their stress during the perinatal period (Kimerling and Baumrind 2005). Indeed, among women in Latin America, low economic status (Almanza-Muñoz et al. 2011; Molero et al. 2014), low educational attainment (Alvarado-Esquivel et al. 2010), and being single (Tannous et al. 2008) are associated with higher PPD. Similar socioeconomic markers are associated with greater TFR as well (Lara 1993). Women from low socioeconomic backgrounds may have fewer resources to help them cope with pregnancy and childbirth, which in turn can increase their stress and risk for PPD (Goyal et al. 2010).
The Present Study
The objective of the present study is to explore the role of TFR as a moderator of the relationship between social support and PPD symptomatology through a secondary data analysis of a longitudinal study on the prevalence and risk factors of PPD among Mexican adult women (Lara et al. 2015; Lara et al. 2016). Because the present study utilized self-report measures rather than clinical interviews, diagnosis of depression is not appropriate and analyses are restricted to depressive symptoms. The present analysis reports data collected during pregnancy (demographics, prenatal depressive symptoms, social support, and TFR) and at 6 months postpartum (PPD symptoms). The study examines an original question among a diverse sample of women in a developing country through a longitudinal design.
The present study contributes to the literature by developing a nuanced understanding of social support as a risk factor for PPD symptoms that takes into account how women who endorse TFR may experience support differently. This also allows for a greater understanding of the association between gender roles and PPD: Whereas past work on socially desirable roles suggests they may promote social support and reduce PPD risk (Dimitrovsky et al. 2000), the effects of passive-submissive femininity remain unexplored. We hypothesized that low social support and high TFR would predict higher PPD symptoms (Hypothesis 1). Additionally, we hypothesized that a lack of social support would be a stronger predictor of PPD symptoms for women with higher TFR than for women with lower TFR (Hypothesis 2). We explored these relationships while controlling for key demographic variables (income, education, and partner status), and prenatal depressive symptoms.
Method
Participants
The sample included the 210 women who completed assessments both during pregnancy and at 6 months postpartum. Participants were recruited from two clinics that provide prenatal care in Mexico City, Mexico. Trained research assistants approached the women and invited them to participate while they waited for their prenatal appointment. In order to participate, the women had to be at least 20 years old, in the third trimester of their pregnancy, and not presenting manic symptoms. The participants’ mean age was 29.50 years (SD = 6.34, range = 20–44), and the average gestational age was 32.39 weeks (SD = 4.01). The average years of education was 13.01 years (SD = 3.83, range = 5–20), 131 (62.4%) women were employed, 169 (80%) lived with their partner, and 98 (46.7%) had low monthly family income. Family income information was categorized into either low income (< approximately US $350 per month) or medium and high income (> approximately US $350 per month). These categories represent the lowest 30% of incomes or the medium and upper 70% of incomes in Mexico, respectively (INEGI 2013). Nearly half (n = 95; 45.2%) of the women were primiparous (i.e., bearing their first child).
Measures
Depressive symptoms
Depressive symptomatology was measured both during the third trimester of pregnancy and 6 months postpartum via the Spanish version of the Patient Health Questionnaire-9 (PHQ-9; Spitzer et al. 1999; Wulsin et al. 2002; Zhong et al. 2014). The present study employed the first nine items of the scale, which address the DSM-5 depression diagnostic criteria and indicated adequate reliability (α = 0.78 in pregnancy and 0.85 at 6 months postpartum). Participants reported how often they were bothered by problems such as “little interest or pleasure in doing things” using a scale from 0 (not at all) to 3 (nearly every day). A summed score greater than 10, with possible scores ranging from 0–27, indicates a risk of depression (Kroenke et al. 2001). Past research has used the PHQ-9 with Mexican samples (Lazarevich et al. 2013) and has established the reliability of this instrument among postpartum women, including adequate sensitivity and specificity (Davis et al. 2013; Gjerdingen et al. 2009; Pawar et al. 2011). Although the PHQ-9 measures general depressive symptoms, it has shown concordance with PPD-specific measures such as the Edinburgh Postnatal Depression Scale (Flynn et al. 2011; Yawn et al. 2009) and the Postpartum Depression Screening Scale (Beck and Gable 2012). Moreover, the National Institute for Health and Care Excellence (NICE, 2007) guidelines list the PHQ-9 among the recommended self-report measures to use during screening and monitoring of PPD.
Social support
The Spanish version of the Postpartum Depression Predictors Inventory-Revised (PDPI-R) social support subscale was used to measure social support during pregnancy (Genovez and Le 2011; Records et al. 2007). This instrument has been validated among a pregnant sample and has shown concurrent validity among postpartum samples (Records et al. 2007). The 12-item scale quantifies the presence of instrumental and emotional support from the partner, mother, and other family members and friends. Instrumental support was measured through items such as, “Do you think you receive adequate practical support from your partner? (For example, help with house chores or taking care of the kids),” whereas emotional support included items such as, “Do you think you receive adequate emotional support from your partner?” (Records et al. 2007). Each item was scored with a 0 (absent) or 1 (present), creating a possible summed range of scores from 0–12 where higher scores indicate greater support. This scale had adequate reliability in this sample (α = .76).
Traditional Female Role
Traditional Female Role was quantified during pregnancy via eight questions from the submissive subscale of the IMAFE (Lara 1993). The scale measures personality traits expected in many cultures but particularly of Mexican women (Lara 1993). Using a 0 (I’m never or almost never like this) to 7 (I’m always or almost always like this) scale, participants indicated how much certain traits described themselves such that higher scores represented higher levels of TFR. The items included in this study were: conformist, submissive, indecisive, of weak personality, resigned, cowardly, withdrawn, and shy. These had factor loadings of .40 or higher (range: .40–.49, N = 167 women), as reported in the IMAFE manual (Lara 1993). This short version demonstrated adequate reliability in the present study (α = .83). The submissive subscale has also shown adequate reliability in other Latin American countries, such as Colombia (Martínez-Gómez et al. 2012; Rey 2008).
Procedure
The women who consented to participate were interviewed during their third trimester in the waiting room of the community health center where they were seeking prenatal care. They completed all study measures at this time. The women were then contacted via phone to schedule subsequent interviews at 6 months postpartum. Participants selected the location for the follow-up interviews, including their home, workplace, health center, or another location. The interviews lasted approximately 30 minutes, during which each women again completed the measure of depressive symptoms. Most often, each woman was interviewed by the same person at each time point. The interviews were carried out by the research team, which was trained by two of the authors over the course of a month. Training included a review of the study’s background and instruments, role-play, supervision, and interviews during a pilot phase. At each time point, the women received self-help and parenting books, as well as bus tickets, travel reimbursement (< US $2), or calling cards as compensation. Following the NICE Guidelines (NICE 2007), women who reported PPD symptoms were recommended to seek treatment. However, at 6 months postpartum no women reported having done so. The study was approved by the Institutional Review Board (IRB) of the Ramón de la Fuente National Institute of Psychiatry.
Data Analysis
We conducted correlational and hierarchical linear regression analyses to test the associations among social support, TFR, and PPD symptoms, as well as the moderating effect of TFR. We regressed PPD symptoms on social support, TFR, prenatal depressive symptoms, and sociodemographic variables through four steps. In the first step, we regressed PPD symptoms on prenatal depressive symptoms and the following demographic variables: income, partner status, and education. Income and partner status were dummy coded to indicate low income (dummy code = 1) or medium and high income (0), and partnered (dummy code = 1) or single (0). Education was mean-centered (i.e., each response was recoded as a deviation from the grand mean) for ease of interpretation. At Step 2, we included social support (mean-centered) in the model, and in Step 3 we added TFR (mean-centered). In the fourth step, we included the social support × TFR interaction term. To probe the moderation effect, we plotted PPD symptoms at one standard deviation above and below the means of TFR and social support (Aiken and West 1991). We conducted all analyses using SPSS 22.
Results
Table 1 reports the means and frequencies of the key study variables. Correlational analyses revealed that lower social support was associated with higher prenatal and postpartum depressive symptoms as expected (see Table 2). Higher TFR was associated with higher depressive symptoms during pregnancy and during the postpartum. Additionally, higher TFR was also associated with lower social support, lower education, lower income, and being single. This suggests that TFR was more common among women who were of lower socioeconomic status.
Table 1.
Descriptive Statistics for Key Variables
| Variable | M | SD | Range |
f (% above cut off) |
|---|---|---|---|---|
| Prenatal depressive symptoms | 5.81 | 4.56 | 0–27 | 35 (16.7%) |
| Postpartum depressive symptoms | 5.62 | 5.45 | 0–27 | 42 (20%) |
| Social support | 9.65 | 2.57 | 0–12 | |
| Traditional Female Role | 17.59 | 8.26 | 0–56 |
Table 2.
Correlations Among Study Variables
| Variables | Social Support |
TFR | PPDS | Prenatal depressive symptoms |
Income | Education |
|---|---|---|---|---|---|---|
| Social Support | -- | |||||
| TFR | −.15* | -- | ||||
| PPDS | −.42*** | .29*** | -- | |||
| Prenatal depressive symptoms |
−.30*** | .47*** | .39*** | -- | ||
| Incomea | .10 | −.25*** | −.21** | −.18** | -- | |
| Education (in years) | .25*** | −.32*** | −.28*** | −.26*** | .54*** | -- |
| Partner Statusa | .27*** | −.17* | −.18** | −.12 | .15* | .17* |
Note. TFR = Traditional Female Role; PPDS = postpartum depressive symptoms. Income: medium/high = 0, low = 1; partner status: single = 0, partnered = 1.
point biserial correlations.
p < .05.
p < .01.
p < .001.
Our first hypothesis tested the direct effects of social support and TFR on PPD symptoms, and our second hypothesis tested the interaction between social support and TFR. We examined both hypotheses through hierarchical linear regression (see Table 3). The first step included the demographic variables and explained an adequate amount of variance (R2 = .20, p < .001). The only significant predictor was prenatal depressive symptoms. Women who reported more prenatal depressive symptoms also reported more postnatal depressive symptoms. At step 2, social support was included in the model, which improved its fit (R2 = .27, p < .001). In support of Hypothesis 1, lower social support was associated with greater PPD symptoms.
Table 3.
Hierarchical Linear Regression Analysis Predicting Depressive Symptomatology
| Step 1 | Step 2 | Step 3 | Step 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | β | b | t | β | b | t | β | b | t | β | b | t |
| Income | 0.06 | 0.66 | 0.83 | 0.07 | .71 | 0.93 | 0.05 | 0.59 | 0.77 | 0.06 | 0.65 | 0.87 |
| Education | −0.14 | −0.20 | −1.95 | −0.10 | −.14 | −1.37 | −0.84 | −0.12 | −1.17 | −0.08 | −0.11 | −1.11 |
| Partner Status | −0.11 | −1.45 | −1.65 | −0.04 | −.60 | −0.70 | −0.04 | −0.51 | −0.59 | −0.06 | −.074 | −0.88 |
| Prenatal depressive symptoms |
0.33 | 0.40 | 5.17*** | 0.27 | .32 | 4.16*** | 0.23 | 0.28 | 3.29** | 0.21 | 0.25 | 2.98** |
| Social Support | −0.29 | −.62 | −4.45*** | −0.29 | −0.62 | −4.51*** | −0.29 | −0.62 | −4.54*** | |||
| TFR | 0.09 | 0.06 | 1.26 | 0.04 | 0.03 | 0.63 | ||||||
| Social Support × TFR |
−0.18 | −0.04 | −2.98** | |||||||||
| F | 13.10*** | 15.41*** | 13.14*** | 12.97*** | ||||||||
| df | 4 | 5 | 6 | 7 | ||||||||
| dferror | 205 | 204 | 203 | 202 | ||||||||
| R2 | .20 | .27** | .28*** | .31*** | ||||||||
| ΔR2 | .07*** | .01 | .03** | |||||||||
Note. Income: medium/high = 0, low = 1; partner status: single = 0, partnered = 1. df = degrees of freedom.
p < .05.
p < .01.
p < .001.
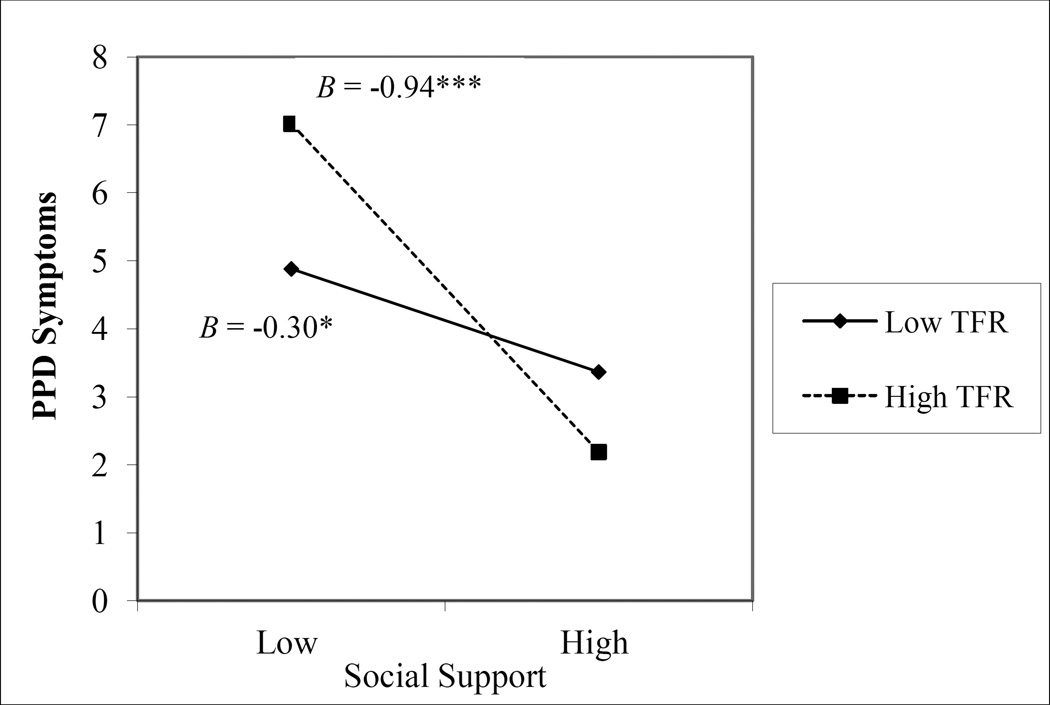
We added TFR in the third step (R2 = .28, p < .001). Unexpectedly, a greater endorsement of TFR did not significantly predict PPD symptoms and did not improve the fit of the model. In the fourth step, the social support × TFR interaction term was included. In support of Hypothesis 2, the interaction was significant, and significantly increased the amount of variance explained by the model, thereby indicating moderation (R2 = .31, p < .001, ΔR2 = .03, ΔF(1, 202) = 8.86, p = .003). This finding suggests that the association between social support and PPD symptoms varied by level of TFR. Simple slopes analyses confirmed that the negative relationship between social support and depressive symptomatology was stronger for women with higher TFR (β = −.94, t = −7.71, p < .001) than lower TFR (β = −0.30, t = −2.17, p = .032, see Fig. 1). Because the psychosocial variables explained a significant amount of variance beyond the demographic variables, the results suggest the psychosocial variables are stronger predictors of PPD symptoms.
Figure 1.
Postpartum depression as a function of Traditional Female Role and social support.
B = standardized regression coefficient; TFR = Traditional Female Role; PPD = postpartum depression.
* p < .05. ** p < .01. *** p < .001.
Discussion
Our study examined the association between social support and postpartum depressive symptoms at differing levels of traditionalism (Traditional Feminine Role) through a longitudinal design that accounted for prenatal depressive symptoms. In support of a large body of existing work, pregnant women who reported lower social support during pregnancy also indicated greater depressive symptoms in the postpartum. However, this association varied by level of TFR. Women who had lower levels of social support were at a greater risk of PPD symptoms if they also espoused more TFR. In other words, the less support a woman had and the more strongly she endorsed TFR, the more likely she was to not benefit from the support she did have, leading to a higher risk of PPD. The results imply that the degree of social support a woman has may not be experienced similarly by all women. Rather, a woman’s benefits from support appear to depend on individual differences in each woman’s adherence to TFR.
Also consistent with past work, greater depressive symptoms during pregnancy was associated with greater depressive symptoms in the postpartum, providing some evidence of the continuity of depression across the perinatal period (Gjerdingen et al. 2011). PPD symptoms were also related to lower socioeconomic status in our sample, but the relationship between social support and TFR predicted PPD symptoms above and beyond these factors. TFR was implicated in the sociodemographic variables and did not predict PPD symptoms beyond social support. As in past work (Lara 1993), the women who adhered to TFR were from lower, compared to higher, socioeconomic backgrounds.
Although the present study is the first known to test the interactive effect of social support and TFR, our results are consistent with previous work exploring the barriers women face in the postpartum period. Mothers who are higher in TFR have been socialized to act in a passive way and to support others without seeking help for themselves. This socialization may make it more difficult for them to gather help in the postpartum because they engage in such agentic behaviors less often and have a smaller network (Dennis and Chung-Lee 2006; Negron et al. 2013; Rocha-Sánchez and Cruz del Castillo 2013). Additionally, women who are higher in TFR may be more likely to consider their depressive symptoms and help-seeking to be stigmatizing. This stigmatization can deter further support-seeking and limit the assistance they receive from their existing support system (Mickelson and Williams 2008). Our study’s longitudinal design and large and diverse sample allow unique insight into how gender roles influence women’s access to and benefits from social support, ultimately altering their risk of PPD.
Our results also promote a more nuanced conceptualization of gender roles. Whereas past work indicates that positively stereotyped gender-role traits, such as highly affective femininity, aided the procurement of social support and thus reduced the risk of PPD (Dimitrovsky et al. 2000; Pfost et al. 1989), the current study suggests that higher adoption of TFR showed the opposite pattern. Our study is among the first known to test TFR with perinatal women and to examine its relationship to social support and PPD. As such, it advances our understanding of gender-role attitudes and highlights the need to study various dimensions of gender roles. Current studies of women (although often not perinatal women) have centered around the concept of gender, which addresses the inequalities of women in society compared to men, as in Seedat et al. (2009) and the World Health Report (World Health Organization 1998). TFR, as measured here, emphasizes the endorsement of passive-submissive traits that is associated with women’s subordinate position in society. Gender inequalities call for changes in social structures and public policies, whereas attitudes toward gender roles such as TFR call for actions that are more individualized.
Limitations
Some aspects of our study’s design restrict the generalizability of our results. The sample was drawn from two public clinics, which may limit the socioeconomic variability of the participants. Nearly half of the sample (46.7%) reported incomes that categorize them into the lowest 30% of the Mexican wealth distribution. Despite this limitation, socioeconomic characteristics did not influence women’s risk of PPD, although they were related to TFR. Nonetheless, these findings must be interpreted cautiously when considering women from different socioeconomic backgrounds. Additionally, though 280 women were interviewed during pregnancy, only 75% completed the follow-up at 6 months postpartum. However, this attrition rate is comparable to other longitudinal studies with puerperal women (Lara et al. 2010b). Differences between these groups (see Lara et al. 2015) indicate that the present sample is missing women who were at highest risk for depression and perhaps more likely to have high TRF. This difference may be because women with the highest risk of PPD experience greater difficulties receiving care and may face greater stressors that prevent their continued participation in our study. This limitation suggests our analysis may underestimate PPD and TFR among perinatal Mexican women. Additionally, TFR was measured via self-report, meaning concerns about social desirability could have influenced women’s responses. Lastly, women presenting manic symptoms were not included, which limits the generalizability of our results to women who may have comorbid mental health problems.
Future Research Directions
The PPD literature would benefit from further investigation into the aspects of TFR that most strongly influence PPD. For example, women may be socialized to adhere to TFR but experience conflict in doing so because it can limit their potential (Moradi and Parent 2013). Future research should examine the role of TFR-related stress in increasing women’s distress during the postpartum. Similarly, because TFR is theorized to be a result of socialization in a patriarchal society, future research should account for the demographic makeup of women’s support network. TFR may influence social support more strongly if a woman relies largely on her husband for support rather than on a female family member or friend.
Future research should also examine women’s desire to uphold the traditional role and be mothers as a risk for PPD. Additionally, given the similarities within Latin American cultural values, our findings may prove to be especially important in the United States, where Latinos comprise 16% of the national population and 63% of Latinos are of Mexican origin (Ennis et al. 2011). Though gender roles may differ between Mexican and Mexican American or other Latina women (Lega and Procel 2013), past work suggests that Mexican American gender-role development is largely influenced by parental beliefs and cultural values shared with Mexican culture (Gowan and Trevio 1998; Knight et al. 2010; Lam et al. 2012; Updegraff et al. 2014). Future work may benefit from a greater integration of Latin American and U.S. Latina studies that incorporate the unique stressors many Latina immigrants often experience through the process of acculturation (Davila et al. 2009; Urquia et al. 2012).
Practice Implications
Our findings emphasize the need for increased awareness of TFR and empowerment to seek support for women at risk of PPD. We suggest psychologists, nurses, and doctors educate pregnant women about TFR and its association with depression and social support. Without seeking to alter women’s value systems, raising awareness of TFR may reduce the stigma surrounding PPD and help-seeking (Lara et al. 2010a; Muñoz et al. 2007). Moreover, interventions for women high in TFR may empower them by helping them increase their network of social support (Rocha-Sánchez and Cruz del Castillo 2013). Indeed, existing PPD interventions often include lessons on increasing social support, but these can be improved by also including information on how TFR may influence support-seeking (Lara et al. 2010a; Muñoz et al. 2007). Our results also imply the need for early screening of PPD symptoms, especially for high-risk women such as those lower in social support and higher in TFR. For many women, experiencing depressive symptoms during the third trimester carried into the postpartum, which underscores the continuity of depression during the perinatal period. Given this finding, practitioners need to expand prenatal screening of depressive symptoms and risk factors (Austin 2014; Bales et al. 2015; Segre et al. 2014). The use of the PHQ-9 measure in our study further corroborates the reliability and validity of using this brief and accessible measure to screen for depression (Kroenke et al. 2001; NICE 2007).
Conclusions
Our study examined the role of social support and the Traditional Female Role in the risk of PPD, a serious mental health problem that is especially understudied among Mexican and other Latina women. Specifically, we found that women with both lower social support and higher self-reported adherence to the Traditional Female Role were at the highest risk of experiencing postpartum depressive symptoms. The present findings extend past research through a longitudinal design with a large sample size of an understudied population. The women’s varied economic background and the sociocultural context of Mexico provide a unique sample to examine this question. The pervasiveness of TFR in many aspects of Mexican and other Latino societies, as well as the high prevalence of PPD and the negative effects on mother and child, underscore the need for such research and its potential to have broadly beneficial outcomes.
Acknowledgments
The present study was supported by the Consejo Nacional de Ciencia y Tecnología (CONACyT, CB-2009-01 133923) and by the National Institute on Minority Health and Health Disparities. We are grateful to Dr. José Luis Navarro, Director of the Centro de Salud Dr. Ángel Brioso Vasconcelos and to Dr. Juan Pablo Barba Martín, Coordinator of Obstetrics and Gynecology of the Hospital Regional del ISSSTE Lic. Adolfo López Mateos. Thanks are also due to the research team: Yadira Ramos, Karla Alcántara and Valeria Zempoalteca, and to Ricardo Orozco for his statistical assistance.
Contributor Information
Analia F. Albuja, Department of Psychology, Rutgers University
M. Asunción Lara, Department of Epidemiology and Psychosocial Research, Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz.
Laura Navarrete, Department of Epidemiology and Psychosocial Research, Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz.
Lourdes Nieto, Department of Epidemiology and Psychosocial Research, Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz.
References
- Abrams LS, Dornig K, Curran L. Barriers to service use for postpartum depression symptoms among low-income ethnic minority mothers in the United States. Qualitative Health Research. 2009;19:535–551. doi: 10.1177/1049732309332794. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Almanza-Muñoz JJ, Salas-Cruz CL, Olivares-Morales AS. Prevalencia de depresión posparto y factores asociados en pacientes puérperas de la Clínica de Especialidades de la Mujer [Prevalence and risk factors of postpartum depression among new mothers in the Clínica de Especialidades de la Mujer] Revista de Sanidad Militar. 2011;65:78–86. [Google Scholar]
- Alvarado-Esquivel C, Sifuentes-Alvarez A, Estrada-Martinez S, Salas-Martinez C, Hernandez-Alvarado AB, Ortiz-Rocha SG, Sandoval-Herrera F. Prevalencia de depresión posnatal en mujeres atendidas en hospitales públicos de Durango, México [Prevalence of postpartum depression among women in the public hospitals of Durango, Mexico] Gaceta Médica de México. 2010;146:1–9. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing, Inc.; 2013. [Google Scholar]
- Austin MP. Marcé International Society position statement on psychosocial assessment and depression screening in perinatal women. Best Practice & Research Clinical Obstetrics and Gynaecology. 2014;28:179–187. doi: 10.1016/j.bpobgyn.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Bales M, Pambrun E, Melchior M, Glangeaud-Freudenthal NM-C, Charles M-A, Verdoux H, Sutter-Dallay A-L. Prenatal psychological distress and access to mental health care in the ELFE cohort. European Psychiatry. 2015;30:322–328. doi: 10.1016/j.eurpsy.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Beck CT. Predictors of postpartum depression: An update. Nursing Research. 2001;50:275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Beck CT. Postpartum depression: A metasynthesis. Qualitative Health Research. 2002;22:453–472. doi: 10.1177/104973202129120016. [DOI] [PubMed] [Google Scholar]
- Beck CT. State of the science on postpartum depression: What nurse researchers have contributed. American Journal of Maternal/Child Nursing. 2008;33:121–126. doi: 10.1097/01.NMC.0000313421.97236.cf. [DOI] [PubMed] [Google Scholar]
- Beck CT, Records K, Rice M. Further development of the Postpartum Depression Predictors Inventory-Revised. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2006;35:735–745. doi: 10.1111/j.1552-6909.2006.00094.x. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Concordance and discordance of the Postpartum Depression Screening Scale and the Patient Health Questionniare-9 in an ethnically diverse sample. Journal of Social Service Research. 2012;38:439–450. [Google Scholar]
- Bem SL. The measurement of psychological androgyny. Journal of Consulting and Clinical Psychology. 1974;42:155–162. [PubMed] [Google Scholar]
- Bem SL. The lenses of gender: Transforming the debate on sexual inequality. New Haven, CT: Yale University Press; 1993. [Google Scholar]
- Berthiaume M, David H, Saucier J. Correlates of gender role orientation during pregnancy and the postpartum. Sex Roles. 1996;35:781–800. [Google Scholar]
- Canaval GE, González MC, Martínez-Schallmoser L, Tovar MC, Valencia C. Depresión postparto, apoyo social y calidad de vida en mujeres de Cali, Colombia [Postpartum depression, social support, and quality of life of women in Cali, Colombia] Colombia Médica. 2000;31:4–10. [Google Scholar]
- Choi P, Henshaw C, Baker S, Tree J. Supermum, superwife, supereverything: Performing femininity in the transition to motherhood. Journal of Reproductive and Infant Psychology. 2005;23:167–180. [Google Scholar]
- Chojenta C, Loxton D, Lucke J. How do previous mental health, social support, and stressful life events contribute to postnatal depression in a representative sample of Australian women? Journal of Midwifery and Women’s Health. 2012;57:145–150. doi: 10.1111/j.1542-2011.2011.00140.x. [DOI] [PubMed] [Google Scholar]
- Clark L. La familia: Methodological issues in the assessment of perinatal social support for Mexicanas living in the United States. Social Science and Medicine. 2001;53:1303–1320. doi: 10.1016/s0277-9536(00)00411-1. [DOI] [PubMed] [Google Scholar]
- Collins NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC. Social support in pregnancy: Psychosocial correlates of birth outcomes and postpartum depression. Journal of Personality and Social Psychology. 1993;65:1243–1258. doi: 10.1037//0022-3514.65.6.1243. [DOI] [PubMed] [Google Scholar]
- Consejo Nacional de Evaluación de la Política de Desarrollo Social [CONEVAL] Medición de pobreza: Distrito Federal [Measurement of poverty: Federal District] 2014 Retrieved from http://www.coneval.org.mx/coordinacion/entidades/DistritoFederal/Paginas/pobreza-2014.aspx. [Google Scholar]
- Davila M, McFall SL, Cheng D. Acculturation and depressive symptoms among pregnant and postpartum Latinas. Maternal Child Health Journal. 2009;13:318–325. doi: 10.1007/s10995-008-0385-6. [DOI] [PubMed] [Google Scholar]
- Davis K, Pearlstein T, Stuart S, O'Hara M, Zlotnick C. Analysis of brief screening tools for the detection of postpartum depression: Comparisons of the PRAMS 6-item instrument, PHQ-9, and structured interviews. Archives of Women’s Mental Health. 2013;16:271–277. doi: 10.1007/s00737-013-0345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Castro F, Hinojosa-Ayala N, Hernandez-Prado B. Risk and protective factors associated with postnatal depression in Mexican adolescents. Journal of Psychosomatic Obstetrics and Gynecology. 2011;32:210–217. doi: 10.3109/0167482X.2011.626543. [DOI] [PubMed] [Google Scholar]
- de Castro F, Place JMS, Billings DL, Rivera L, Frongillo EA. Risk profiles associated with postnatal depressive symptoms among women in a public sector hospital in Mexico: The role of sociodemographic and psychosocial factors. Archives of Women's Mental Health. 2014;18:463–471. doi: 10.1007/s00737-014-0472-1. [DOI] [PubMed] [Google Scholar]
- Dennis C, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth. 2006;33:323–331. doi: 10.1111/j.1523-536X.2006.00130.x. [DOI] [PubMed] [Google Scholar]
- Díaz-Loving R, Aragón SR, Aragón RS. Rasgos instrumentales (masculinos) y expresivos (femininos), normativos (tipicos e ideales) en Mexico. Revista Latinoamericana de Psicologìa. 2001;33:131–139. [Google Scholar]
- DiGirolamo AM, Salgado de Snyder VN. Women as primary caregivers in Mexico: Challenges to well-being. Salud Publica de Mexico. 2008;50:516–522. doi: 10.1590/s0036-36342008000600013. [DOI] [PubMed] [Google Scholar]
- Dimitrovsky L, Levy-Shiff R, Perl G. Effect of gender-role orientation of primiparous mothers on their cognitive appraisals, coping strategies, and mood postpartum. Sex Roles. 2000;43:593–604. [Google Scholar]
- Eagly AH, Wood W. The origins of sex differences: Evolution versus social structure. American Psychologist. 1999;54:408–423. [Google Scholar]
- Elsenbruch S, Benson S, Rucke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, Arck PC. Social support during pregnancy: Effects on maternal depressive symptoms, smoking and pregnancy outcome. Human Reproduction. 2007;22:869–877. doi: 10.1093/humrep/del432. [DOI] [PubMed] [Google Scholar]
- Ennis SR, Rios-Vargas M, Albert NG. The Hispanic population: 2010. 2011 Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior and Development. 2010;33:1–9. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J, Mello MCD, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bulletin of the World Health Organization. 2012;90:139–149. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn HA, Sexton M, Ratliff S, Porter K, Zivin K. Comparative performance of the Edinburgh Postnatal Depression Scale and the Patient Health Questionnaire-9 in pregnant and postpartum women seeking psychiatric services. Psychiatry Research. 2011;187:130–134. doi: 10.1016/j.psychres.2010.10.022. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Miller WC. AHRQ Publication Number 05-E006-1. Rockville, MD: Agency for Healthcare Research and Quality; 2005. Perinatal depression: Prevalence, screening accuracy, and screening outcomes: Summary. Retrieved from http://www.ahrq.gov/clinic/epcsums/peridepsum.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genovez MG, Le HN. Identification of Salvadoran pregnant women at risk for postpartum depression. Poster presented at the 25th Annual Conference of Postpartum Support International; Seattle, WA. 2011. [Google Scholar]
- Gibbons JL, Stiles DA, Shkodriani GM. Adolescents’ attitudes toward family and gender roles: An international comparison. Sex Roles. 1991;25:625–643. [Google Scholar]
- Gjerdingen D, Crow S, McGovern P, Miner M, Center B. Postpartum depression screening at well-child visits: Validity of a 2-question screen and the PHQ-9. Annals of Family Medicine. 2009;7:63–70. doi: 10.1370/afm.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjerdingen D, Crow S, McGovern P, Miner M, Center B. Changes in depressive symptoms over 0–9 months postpartum. Journal of Women’s Health. 2011;20:381–386. doi: 10.1089/jwh.2010.2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowan M, Trevio M. An examination of gender differences in Mexican-American attitudes toward family and career roles. Sex Roles. 1998;38:1079–1093. [Google Scholar]
- Goyal D, Gay C, Lee KA. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first time mothers? Women’s Health Issues. 2010;20:96–104. doi: 10.1016/j.whi.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hietanen AE, Pick S. Gender stereotypes, sexuality, and culture in Mexico. In: Safdar S, Kosakowska-Berezecka N, editors. Psychology of gender through the lens of culture. New York, NY: Springer International; 2015. pp. 285–306. [Google Scholar]
- Instituto Nacional de Estadística y Geografía. Los hombres y las mujeres en México [Men and women in Mexico] México City, Mexico: INEGI; 2010. [Google Scholar]
- Instituto Nacional de Estadística y Geografía. Encuesta nacional de ingresos y gastos de los hogares [National survey of income and spenditure in homes] 2013 Retrieved from www.inegi.org.mx. [Google Scholar]
- Johannesen-Schmidt MC, Eagly AH. Another look at sex differences in preferred mate characteristics: The effects of endorsing the traditional female role. Psychology of Women Quarterly. 2002;26:322–328. [Google Scholar]
- Kimerling R, Baumrind N. Access to specialty mental health services among women in California. Psychiatric Services. 2005;56:729–734. doi: 10.1176/appi.ps.56.6.729. [DOI] [PubMed] [Google Scholar]
- Knight GP, Gonzales NA, Saenz DS, Bonds DD, Germán M, Deardorff J, Updegraff KA. The Mexican American Cultural Values scales for adolescents and adults. Journal of Early Adolescence. 2010;30:444–481. doi: 10.1177/0272431609338178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam CB, McHale SM, Updegraff KA. Gender dynamics in Mexican American families: Connecting mothers’, fathers’, and youths’ experiences. Sex Roles. 2012;67:17–28. doi: 10.1007/s11199-012-0137-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara MA. A sex role inventory with scales for “machismo” and “self-sacrificing woman”. Journal of Cross-Cultural Psychology. 1989;20:386–398. [Google Scholar]
- Lara MA. Masculinidad-feminidad y salud mental. Importancia de las características no deseables de los roles de género [Masculinity, femininity and mental health: The importance of undesirable traits in gender roles] Salud Mental. 1991;14:12–18. Retrieved from http://www.inprf-cd.gob.mx/revista_sm/ [Google Scholar]
- Lara MA. Inventario de masculinidad y feminidad (IMAFE) [Inventory of masculity and femininity] México, DF: El Manual Moderno; 1993. [Google Scholar]
- Lara MA, Navarrete L. Internal report of"prevalence and risk factors of postpartum depression in perinatal health services” pilot study. México City, Mexico: National Institute of Psychiatry Ramón de la Fuente Muñiz; 2013. [Google Scholar]
- Lara MA, Navarrete L, Nieto L. Prenatal predictors of postpartum depression and postpartum depressive symptoms in Mexican mothers: A longitudinal study. Archives of Women’s Mental Health. 2016;19:825–834. doi: 10.1007/s00737-016-0623-7. [DOI] [PubMed] [Google Scholar]
- Lara MA, Navarrete L, Nieto L, Martín JPB, Navarro JL, Lara-Tapia H. Prevalence and incidence of perinatal depression and depressive symptoms among Mexican women. Journal of Affective Disorders. 2015;175:18–24. doi: 10.1016/j.jad.2014.12.035. [DOI] [PubMed] [Google Scholar]
- Lara MA, Navarro R. Positive and negative factors in the measurement of sex roles: Findings from a Mexican sample. Hispanic Journal of Behavioral Sciences. 1986;8:143–155. [Google Scholar]
- Lara MA, Navarro R. Self-descriptions of Mexican college students in response to the Bem Sex Role Inventory and other sex role ítems. Journal of Cross-Cultural Psychology. 1987;18:331–344. [Google Scholar]
- Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: A randomized control trial. Journal of Affective Disorders. 2010a;122:109–117. doi: 10.1016/j.jad.2009.06.024. [DOI] [PubMed] [Google Scholar]
- Lara MA, Navarro C, Navarrete L, Le H. Retention rates and potential predictors in a longitudinal randomized control trial to prevent postpartum depression. Salud Mental. 2010b;33:429–436. [Google Scholar]
- Lazarevich I, Delgadillo-Gutiérrez HJ, Mora-Carrasco F, Martínez-González AB. Depresión, autoestima y características de personalidad asociadas al género en estudiantes rurales de México [Depression, self-esteem, and personality traits associated with gender among students in rural Mexico] Alternativas en Psicologia. 2013;29:44–57. [Google Scholar]
- Lega L, Procel S. Acculturation and generational differences in the irrational beliefs about traditional female roles in Ecuadorian mothers and daughters living in Ecuador and the United States. Revista Colombiana de Psicologia. 2013;22:35–40. [Google Scholar]
- Martínez-Gómez J, Guerrero-Rodríguez SM, Rey-Anacona CA. Assessment of construct validity and reliability of the Inventory of Masculinity and Femininity in adolescents and young Colombian adults. Avances en Psicología Latinoamericana. 2012;30:170–181. [Google Scholar]
- Martinez-Schallmoser L, Telleen S, MacMullen NJ. The effects of social support and acculturation on postpartum depression in Mexican American women. Journal of Transcultural Nursing. 2003;14:329–338. doi: 10.1177/1043659603257162. [DOI] [PubMed] [Google Scholar]
- Mauthner NS. “Feeling low and feeling really bad about feeling low”: Women’s experiences of motherhood and postpartum depression. Canadian Psychology. 1999;40:143–161. [Google Scholar]
- Mendez-Luck CA, Kennedy DP, Wallace SP. Concepts of burden in giving care to older relatives: A study of female caregivers in a Mexico City neighbourhood. Journal of Cross Cultural Gerontology. 2008;23:265–282. doi: 10.1007/s10823-008-9058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mickelson KD. Perceived stigma, social support, and depression. Personality and Social Psychology Bulletin. 2001;27:1046–1056. [Google Scholar]
- Mickelson KD, Biehle SN, Chong A, Gordon A. Perceived stigma of postpartum depression symptoms in low-risk first-time parents: Gender differences in a dual-pathway model. Sex Roles. 2016 Advance online publication. [Google Scholar]
- Mickelson KD, Williams SL. Perceived stigma of poverty and depression: Examination of interpersonal and intrapersonal mediators. Journal of Social and Clinical Psychology. 2008;27:903–930. [Google Scholar]
- Molero KL, Urdaneta Machado JR, Baabel Zambrano N, Contreras Benítez A, Azuaje Quiroz E, Baabel Romero N. Prevalencia de depresión posparto en puérperas adolescentes y adultas [Prevalence of postpartum depression in new adolescent and adult mothers] Revista Chilena de Obstetricia y Ginecología. 2014;79:294–304. [Google Scholar]
- Moradi B, Parent MC. Assessment of gender-related traits, attitudes, roles, norms, identity, and experiences. In: Geisinger KF, editor. APA handbook of testing and assessment in psychology: Testing and assessment in clinical and counseling psychology. Vol. 2. Washington, DC: American Psychological Association; 2013. pp. 467–488. [Google Scholar]
- Muñoz RF, Huynh-Nhu L, Chandra GI, Manuela AD, Guido GU, Soto J, Lieberman AF. Prevention of postpartum depression in low-income women: Development of the mamás y bebés/ Mothers and Babies course. Cognitive and Behavioral Practice. 2007;14:70–83. [Google Scholar]
- National Institute for Health and Care Excellence. Antenatal and postnatal mental health: The NICE Guideline on clinical management and service guidance. 2007 Retrieved from http://www.nice.org.uk/guidance/cg192. [PubMed] [Google Scholar]
- Navarrete LE. Unpublished master’s thesis. México City, Mexico: Universidad Nacional Autónoma de México; 2012. La experiencia psicológica del embarazo de alto riesgo en mujeres con sintomatología depresiva [The psychological experience of high risk pregnancy among women with depressive symptoms] [Google Scholar]
- Navarrete LE, Lara MA, Navarro C, Gómez ME, Morales F. Factores psicosociales que predicen síntomas de ansiedad posnatal y su relación con los síntomas depresivos en el posparto [Psychosocial factors predicting postnatal anxiety symptoms and their relation to symptoms of postpartum depression] Revista de Investigación Clínica. 2012;64:625–633. [PubMed] [Google Scholar]
- Negron R, Martin A, Almog M, Balbierz A, Howell E. Social support during the postpartum period: Mothers' views on needs, expectations, and mobilization of support. Maternal and Child Health Journal. 2013;17:616–623. doi: 10.1007/s10995-012-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara MW. Postpartum depression: What we know. Journal of Clinical Psychology. 2009;65:1258–1269. doi: 10.1002/jclp.20644. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, McCabe JE. Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, Swain AM. Rates and risk of postpartum depression: A meta-analysis. International Review of Psychiatry. 1996;8:37–54. [Google Scholar]
- Özmen D, Çetinkaya A, Ulaş S, Özmen E. Association between perceived social support and postpartum depression in Turkey. British Journal of Medicine and Medical Research. 2014;4:2025–2036. [Google Scholar]
- Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118:659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- Pawar G, Wetzker C, Gjerdingen D. Prevalence of depressive symptoms in the immediate postpartum period. Journal of the American Board Family Medicine. 2011;24:258–261. doi: 10.3122/jabfm.2011.03.100249. [DOI] [PubMed] [Google Scholar]
- Pérez P, Gaviña J. Affective disorders. In: Sáenz-Herrero M, editor. Psychopathology in women: Incorporating gender perspective into descriptive psychopathology. New York, NY: Springer International Publishing; 2014. pp. 527–559. [Google Scholar]
- Pérez Blasco J, Serra Desfilis E. Influencia del rol tradicional femenino en la sintomatología ansiosa en una muestra de mujeres adultas [The effect of the traditional female role on anxiety symptoms in a sample of adult women] Anales de Psicología. 1997;13:155–161. [Google Scholar]
- Pfost K, Stevens M, Lum C. Femininity and work plans protect women against postpartum dysphoria. Sex Roles. 1989;21:423–431. [Google Scholar]
- Records K, Rice M, Beck CT. Psychometric assessment of the Postpartum Depression Predictors Inventory-Revised. Journal of Nursing Measurement. 2007;15:189–202. doi: 10.1891/106137407783095775. [DOI] [PubMed] [Google Scholar]
- Rey CA. Pro-social skills, gender personality traits and acceptance of violence toward women in adolescents who have witnessed violence in their parents. Acta Colombiana de Psicologia. 2008;11:107–118. [Google Scholar]
- Righetti-Veltema M, Conne-Perréard E, Bousquet A, Manzano J. Risk factors and predictive signs of postpartum depression. Journal of Affective Disorders. 1998;49:167–180. doi: 10.1016/s0165-0327(97)00110-9. [DOI] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: A synthesis of recent literature. General Hospital Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Rocha-Sánchez T, Cruz del Castillo C. Structural and subjective barriers in the role transition of Mexican women and their emotional distress. Acta Colombiana de Psicologia. 2013;16:123–135. [Google Scholar]
- Rojas G, Fritsch R, Guajardo V, Rojas F, Barroilhet S, Jadresic E. Characterization of depressed mothers in the postpartum. Revista Medica de Chile. 2010;138:536–542. [PubMed] [Google Scholar]
- Saunders KJ, Kashubeck-West S. The relations among feminist identity development, gender-role orientation, and psychological well-being in women. Psychology of Women Quarterly. 2006;30:199–211. [Google Scholar]
- Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Kessler RC. Cross-national associations between gender and mental disorders in the WHO World Mental Health Surveys. Archives of General Psychiatry. 2009;66:785–795. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segre LS, Pollack LO, Brock RL, Andrew JR, O’Hara MW. Depression screening on a maternity unit: A mixed-methods evaluation of nurses’ view and implementation strategies. Issues in Mental Health Nursing. 2014;35:444–454. doi: 10.3109/01612840.2013.879358. [DOI] [PubMed] [Google Scholar]
- Sohr-Preston SV. Implications of timing of maternal depressive symptoms for early cognitive and language development. Clinical Child and Family Psychology Review. 2006;9:65–83. doi: 10.1007/s10567-006-0004-2. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stickney LT, Konrad AM. Gender role attitudes and earnings: A multinational study of married women and men. Sex Roles. 2007;57:801–811. [Google Scholar]
- Surkan PJ, Peterson KE, Hughes MD, Gottlieb BR. The role of social networks and support in postpartum women’s depression: A multi-ethnic urban sample. Maternal and Child Health Journal. 2006;10:375–383. doi: 10.1007/s10995-005-0056-9. [DOI] [PubMed] [Google Scholar]
- Tannous L, Gigante LP, Fuchs SC, Busnello EDA. Postnatal depression in Southern Brazil: Prevalence and demographic and socioeconomic determinants. BMC Psychiatry. 2008;8:1–8. doi: 10.1186/1471-244X-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Updegraff KA, McHale SM, Zeider KH, Umaña-Taylor AJ, Perez-Brena NJ, Wheeler LA, Rodríguez De Jesús SA. Mexican-American adolescents’ gender role attitude development: The role of adolescents’ gender and nativity and parents’ gender role attitudes. Journal of Youth and Adolescence. 2014;43:2041–2053. doi: 10.1007/s10964-014-0128-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urdaneta J, Rivera A, García JI, Guerra M, Baabel NZ, Contreras AB. Factores de riesgo de depression posparto en puérperas venezolanas volaradas por medio de la escala Edimburgo [Risk factors for postpartum depression in new Venezuelan mothers using the Edinburgh scale.] Revista Chilena de Obstetricia y Ginecología. 2011;76:102–112. [Google Scholar]
- Urquia ML, O’Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: The roles of duration of residence and ethnicity. Social Science & Medicine. 2012;74:1610–1621. doi: 10.1016/j.socscimed.2012.02.013. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The World Health report 1998: Life in the 21st century. A vision for all. 1998 Retrieved from http://www.who.int/whr/1998/en/whr98_en.pdf.
- Wulsin L, Somoza E, Heck J. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Primary Care Companion to the Journal of Clinical Psychiatry. 2002;4:191–195. doi: 10.4088/pcc.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie R, Yang J, Liao S, Xie H, Walker M, Wen S. Prenatal family support, postnatal family support and postpartum depression. Australian and New Zealand Journal of Obstetrics and Gynecology. 2010;50:340–345. doi: 10.1111/j.1479-828X.2010.01185.x. [DOI] [PubMed] [Google Scholar]
- Yawn BP, Pace W, Wollan PC, Bertram S, Kurland M, Graham D, Dietrich A. Concordance of Edinburgh Postnatal Depression Scale (EPDS) and Patient Health Questionnaire (PHQ-9) to assess increased risk of depression among postpartum women. Journal of the American Board of Family Medicine. 2009;22:483–491. doi: 10.3122/jabfm.2009.05.080155. [DOI] [PubMed] [Google Scholar]
- Zhong Q, Gelaye B, Fann JR, Sanchez SE, Williams MA. Cross-cultural validity of the Spanish version of the PHQ-9 among pregnant Peruvian women: A Rasch item response analysis. Journal of Affective Disorders. 2014;158:148–153. doi: 10.1016/j.jad.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]