Abstract
Purpose
Increasing in prevalence, food allergy (FA) is becoming an important public health concern. In Korean adults, however, clinical phenotypes and causes of FA have not been studied. We aimed to study common causative allergens and clinical manifestations of FA in Korean adults.
Methods
This study was conducted as a retrospective review of medical records for 95 patients (≥19 years old) diagnosed with FA from September 2014 to August 2015 at a single university hospital.
Results
In the 95 patients, 181 FA events were recorded. The mean age of first onset of FA symptoms was 34.7±15.8 years. The most frequent causative food was seafood (34.8%); shrimp and crab allergies ranked highest, regardless of age and sex. Among all FA events, there were 47 (26.0%) cases of anaphylaxis and 26 (14.4%) cases of oral allergy syndrome (OAS). Seafood (51.1%) was the most frequent cause of anaphylaxis, followed by grains (14.9%). Most OAS cases were associated with fruits (95.7%). The frequency of fruit-induced FA was significantly higher in males than in females (23.0% vs 8.4%, P=0.011). While no cases of vegetables-induced FA were noted in younger individuals (19 to 30 years), vegetables accounted for 20.5% of FA symptoms in older subjects (≥51 years, P<0.001). Allergic rhinitis (44.2%) and drug allergy (20.0%) were major comorbidities associated with FA. Overall, 29 FA events had cofactors, of which 10 were combined with exercise.
Conclusions
The major causes of FA in Korean adults were crustacean, fruits, and grains. Interestingly, the clinical manifestations of FA and demographics varied according to type of food allergen.
Keywords: Food allergy, adults, Korea
INTRODUCTION
FA is an emerging public health concern that affects children and adults worldwide. A number of studies have indicated an increased prevalence of FA over the last decade.1,2,3,4,5 A survey conducted by the Centers for Disease Control and Prevention in 2007 estimated that FA affects 5% of children under the age of 5 years and 4% of children aged 5 to 17 years and adults in the US.5
The present standard for treating FA involves strict restriction from causative foods and the use of antihistamines and epinephrine auto-injectors to treat reactions upon accidental exposure to allergenic foods. Although clinical studies on the efficacy of allergen-specific immunotherapy for patients with FA have recently been conducted, the treatment modality has yet to be included in clinical practice for FA treatment.6 A low rate of conducting confirmative tests to determine causative allergens and a lack of education may contribute to increasing frequencies of FA reactions in the same patient. The only confirmative test to determine causative allergens of FA is a double-blind, placebo-controlled, food challenge test; however, it is time consuming and has potential risks of developing allergic reactions.7,8 Therefore, studies on additive clinical information that is easily accessible may provide important clues for clinicians to determine causative food allergens.
Considering rapid changes in the environment and eating habits in Korea, investigating common causes and clinical manifestations of FA in adults is of growing importance. In addition, to aid physicians in determining potential causative food allergens without the need to conduct complicated and costly tests, we aimed to investigate common food allergens of FA among Korean adults according to age, sex, and clinical manifestations of FA.
MATERIALS AND METHODS
Study design
We retrospectively reviewed the medical records of 95 Korean adults patients (≥19 years old) who were diagnosed with FA between September 2014 and October 2015 at the Allergy Clinic of a university hospital in Korea. Subjects with FA were defined as individuals who have been diagnosed by physicians with FA based on clinical manifestations that developed within 2 hours after ingestion of specific foods and immunologic test results.
Considering the diversity of food allergens, we simplified and grouped the food allergens. Fruits, grains, nuts, seeds, beans, and vegetables were classified as plants. Patients sensitized to non-plant foods were grouped by seafood, which was further classified into crustaceans (shrimp, crab, and lobster), shellfish, cephalopods, and fish; meat; milk; eggs; and others. We categorized the subjects by age into younger (19 to 30 years old), middle-aged (31 to 50 years old), and older (≥51 years old) age groups.
In vivo and in vitro tests
Skin prick tests (SPT) were routinely performed with commercial extracts (Allergopharma, Reinbek, Germany). Allergens tested included pollens (grass, mugwort, ragweed, birch, oak, and alder), molds (alternaria, aspergillus, cladosporium), house dust mites (Dermatophagoides pteronissynus, D. farinae), animal dander (cat and dog), and foods (codfish, cacao, egg, cow's milk, tuna, mussel, potato, celery, soy bean, wheat flour, beef, pork, banana, salmon, garlic, mango, shrimp, apple, strawberry, tomato, chicken, buckwheat, rice, lobster, hazelnut, peanut, and walnut). A positive SPT reaction was defined when the ratio of the mean wheal diameter of the allergen to histamine was higher than 1, or it was lower than 1 but erythema was higher than 21 mm. Specific IgE (sIgE) levels were measured (ImmunoCAP, Phadia, Uppsala, Sweden), and those greater than 0.35 kU/l were regarded as positive.
Statistical analysis
Proportions were compared by the chi square test or Fisher's exact test. The Kruskal-Wallis test was used for comparing onset ages among different FA causes. To compare frequencies of causative foods in accordance with sex and age, the proportion test using R software, version 3.0.2 (R Foundation for Statistical Computing, http://www.R-project.org/) was performed. Other statistical analyses were performed using IBM SPSS software, version 22.0 (IBM Co., Armonk, NY, USA). A P value of <0.05 was considered statistically significant.
Ethics statement
This study was conducted under the approval of the Ajou University Hospital Research Ethics Committee (AJIRB-MED-SUR-15-281).
RESULTS
Demographics of the study subjects
Between October 2014 and September 2015, 181 FA events were recorded in 95 Korean adults. The mean age of the subjects was 38.5±14.1 years (range 19-72 years), and the mean age at which the first FA symptom occurred was 34.7±15.8 years (range 8-70 years). Male patients comprised 46 of all study subjects (48.4%). Eighty-four (88.4%) of the study subjects had a previous personal history of FA. Sixty (63.2%) subjects had previous history of allergic disease. Twenty-one (22.1%) patients had a family history of allergic disease. Overall data are shown in Table 1.
Table 1. Clinical characteristics of the study subjects.
| Characteristics | Patients (n=95) |
|---|---|
| Age (year) | 38.5±14.1 (19–72) |
| Sex, n (%) | |
| Male | 46 (48.4) |
| Female | 49 (51.6) |
| Onset age (year) | 34.7±15.8 (8-70) |
| Family history of Allergic diseases, n (%) | 21 (22.1) |
| Known food allergy, n (%) | 84 (88.4) |
| Comorbidities, n (%) | 60 (63.2) |
| Asthma | 10 (10.5) |
| Allergic rhinitis | 42 (44.2) |
| Allergic conjunctivitis | 17 (17.9) |
| Atopic dermatitis | 7 (7.4) |
| Drug allergy | 19 (20.0) |
| Chronic urticaria | 9 (9.5) |
| Log total IgE (IU/L) | 2.32±0.64 |
Values are presented as mean±standard deviation (range) or n (%).
Causative food allergens
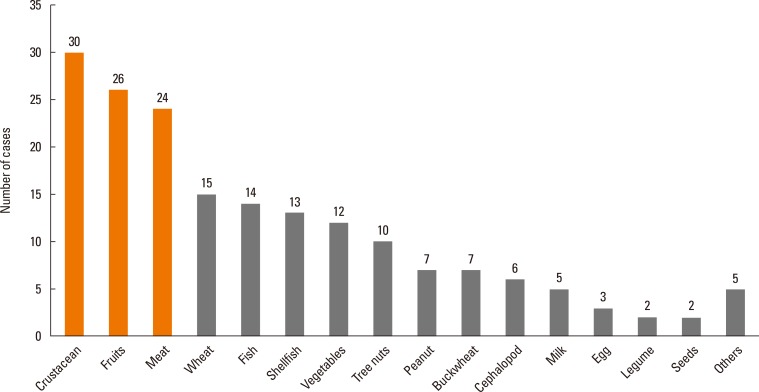
Crustaceans, including shrimp, crab and lobster, were found to be the major causes of FA (30, 16.6%) in the present study. Fruits were the second most frequent (26, 14.4%) food allergen, of which peach and apple were identified as causative food allergens (4.4% and 3.9%, respectively) (Fig. 1). Two events caused by chrysalis were grouped as others. Detection rate of sIgE using Immuno CAP and SPT according to causative food allergen is presented in Supplementary Table 1. In both methods of Immuno CAP and SPT, detection rates of sIgE were highest in seafood and grains. The total number of 8 events showed both positive to Immuno CAP and SPT of causative food allergen (buckwheat, 3 events; crab, 3 events; codfish, 1 event; peanut, 1 event). There were 27 (33.3%) patients with FA to plants who also showed positive results on SPT and/or serum sIgE to pollen.
Fig. 1. Causes of food allergy in adults.
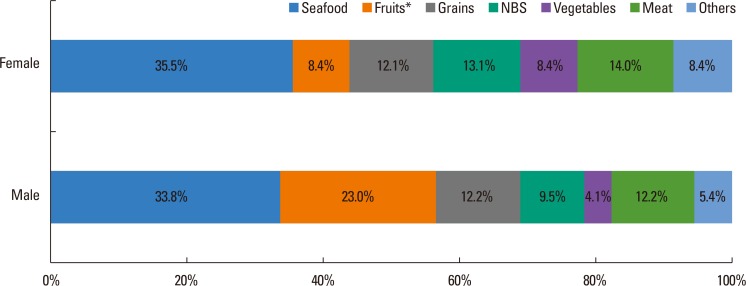
Fig. 2 shows a comparison of major causative food allergens between males and females. The most frequent causative food was seafood in both males and females (33.8% and 35.5%, respectively). The second most frequent causative foods in males were fruits (23.0%), which were the only causative food that showed a significant difference in frequency between males and females (P=0.011). In females, meats (14.0%) were the second frequent causes of FA.
Fig. 2. Comparison of major causative foods between male and female adults. *P value <0.05. NBS, nuts-beans-seeds.
Comparisons of causative food allergens according to age groups are shown in Table 2. FA events were more prevalent in younger subjects than in older subjects; there were 63 events (34.8%) in the 19- to 30-year age group, 79 (43.7%) in the 31- to 50-year age group, and 39 (21.6%) in the ≥51 year age group. Seafood was the main food allergen for all age groups. Fruits and nuts-beans-seeds caused FA more frequently in the younger age group than in the middle-aged and older age groups. Particularly, the frequencies of vegetables-induced FA were significantly different among the age groups (P<0.001). No one in the younger age group experienced FA to vegetables, whereas 4 (5.1%) in the middle-aged group and 8 (20.5%) in the older group showed FA to vegetables.
Table 2. Comparison of causative foods among three groups stratified by age.
| Characteristics | 19-30 years | 31-50 years | ≥51 years | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=34) | Female (n=29) | Total (n=63) | Male (n=27) | Female (n=52) | Total (n=79) | Male (n=13) | Female (n=26) | Total (n=39) | |
| Plants, n (%) | 17 (50.0) | 11 (37.9) | 28 (44.4) | 11 (40.7) | 25 (48.1) | 35 (44.3) | 8 (61.5) | 9 (34.6) | 17 (43.6) |
| Fruits | 8 (23.5) | 5 (17.2) | 13 (20.6) | 8 (29.6) | 3 (5.8) | 11 (13.9) | 1 (7.7) | 1 (3.8) | 2 (5.1) |
| Grains | 5 (14.7) | 4 (13.8) | 9 (14.3) | 1 (3.7) | 8 (15.4) | 9 (11.4) | 3 (23.1) | 1 (3.8) | 4 (10.3) |
| Nuts-Beans-Seeds | 4 (11.8) | 2 (6.9) | 6 (9.5) | 2 (7.4) | 10 (19.2) | 12 (15.2) | 1 (7.7) | 2 (7.7) | 3 (7.7) |
| Vegetables | 0 | 0 | 0 | 0 | 4 (7.7) | 4 (5.1) | 3 (23.1) | 5 (19.2) | 8 (20.5)* |
| Seafood, n (%) | 12 (35.3) | 10 (34.5) | 22 (34.9) | 10 (37.0) | 20 (38.5) | 30 (38.0) | 3 (23.1) | 8 (30.8) | 11 (28.2) |
| Meat, n (%) | 3 (8.8) | 4 (13.8) | 7 (11.1) | 4 (14.8) | 4 (7.7) | 8 (10.1) | 2 (15.4) | 7 (26.9) | 9 (23.1) |
| Milk, n (%) | 1 (2.9) | 3 (10.3) | 4 (6.3) | 0 | 1 (1.9) | 1 (1.3) | 0 | 0 | 0 |
| Egg, n (%) | 1 (2.9) | 0 | 1 (1.6) | 1 (3.7) | 0 | 1 (1.3) | 0 | 1 (3.8) | 1 (2.6) |
| Others, n (%) | 0 (0) | 1 (3.4) | 1 (1.6) | 1 (3.7) | 2 (3.8) | 3 (3.8) | 0 (0) | 1 (3.8) | 1 (2.6) |
Values are presented as number of cases (%).
*P<0.001, P value was calculated in the comparison of FA frequencies according to age group.
Interestingly, onset ages of FA differed according to food type. Among 181 FA events, data on onset age for 107 events were available. Eighty-six events (80.4%) involved adult onset (≥19 years old). Onset ages of FA for each food allergen group were as follows: 38.5±17.0 years for plants-associated FA, 31.8±15.2 years for seafood-induced FA, and 33.4±14.1 years for FA to meats (P=0.169). Within the plant group, onset ages for FA to fruits, grains, nuts-beans-seeds, and vegetables also varied (23.4±13.7, 28.9±15.1, 37.3±13.5, and 55.3±10.6, respectively, P<0.001).
Clinical manifestations of food allergy
Among 181 FA events, the major clinical manifestation involved cutaneous reactions (151, 83.4%). The second most frequent manifestation accompanied with FA was anaphylaxis (47, 26.0%), followed by respiratory symptoms (43 23.8%) and oral allergy syndrome (OAS) (23, 12.7%). Clinical manifestations of FA in adults varied according to causative allergen (Table 3). In the cases of anaphylaxis, the main causative food allergens were crustacean (13, 27.7%), grains (7, 14.9%), and fish (6, 12.8%).
Table 3. Clinical manifestations according to causes of food allergy in adults.
| Causative Food | Anaphylaxis (n=47) | Cutaneous (n=151) | OAS (n=23) | Respiratory (n=43) | CVS (n=6) | GI (n=12) | Nervous (n=6) |
|---|---|---|---|---|---|---|---|
| Plants | 16 (34.0) | 59 (39.1) | 22 (95.6) | 15 (34.9) | 2 (33.3) | 3 (25.0) | 0 |
| Fruits | 1 (2.1) | 13 (8.6) | 15 (65.2) | 1 (2.3) | 0 | 1 (8.3) | 0 |
| Grains | 7 (14.9) | 19 (12.6) | 1 (4.3) | 3 (7.0) | 2 (33.3) | 1 (8.3) | 0 |
| NBS | 4 (8.5) | 16 (10.6) | 1 (4.3) | 3 (7.0) | 0 | 1 (8.3) | 0 |
| Vegetables | 4 (8.5) | 11 (7.3) | 5 (21.7) | 8 (18.6) | 0 | 0 | 0 |
| Seafood | 24 (51.1) | 56 (37.1) | 1 (4.3) | 21 (48.8) | 4 (66.7) | 9 (75.0) | 7 (100) |
| Crustacean | 13 (27.7) | 28 (18.5) | 0 | 9 (20.9) | 0 | 2 (16.7) | 1 (16.7) |
| Shellfish | 4 (8.5) | 12 (7.9) | 1 (4.3) | 4 (9.3) | 1 (16.7) | 1 (8.3) | 1 (16.7) |
| Cephalopod | 1 (2.1) | 5 (3.3) | 0 | 1 (2.3) | 1 (16.7) | 1 (8.3) | 1 (16.7) |
| Fish | 6 (12.8) | 11 (7.3) | 0 | 7 (16.3) | 2 (33.3) | 5 (41.7) | 4 (66.7) |
| Meat | 3 (6.4) | 24 (15.9) | 0 | 5 (11.6) | 0 | 0 | 0 |
| Milk | 2 (4.3) | 4 (2.6) | 0 | 1 (2.3) | 0 | 0 | 0 |
| Egg | 1 (2.1) | 3 (2.0) | 0 | 1 (2.3) | 0 | 0 | 0 |
| Others | 1 (2.1) | 5 (3.3) | 0 | 0 | 0 | 0 | 0 |
Values are presented as number of cases (%).
CVS, cardiovascular symptoms; GI, gastrointestinal symptoms; NBS, Nuts-Beans-Seeds; OAS, oral allergy syndrome.
Four (44.4%) out of 9 FA events presented as anaphylaxis in subjects older than 60 years old. Eleven events (68.8%) of anaphylaxis caused by plants showed positive results on sIgE to causative allergen or related pollen (apple, 1 event; wheat, 4 events; buckwheat, 2 event; walnut, 1 event; peanut, 1 event; other vegetables 2 events). All 4 cases induced by wheat showed positive serum specific IgE to wheat. Eight events (61.5%) of crustacean-induced anaphylaxis showed serum specific IgE positivity to shrimp, crab, or lobster. In 23 events of OAS, almost all events were caused by plants (22, 95.6%). Eighteen events (81.8%) of OAS related to plants showed positive serum specific IgE to birch or alder pollen. Regarding the association between underlying allergic diseases and clinical manifestations of FA, 3 (30%) out of 10 asthmatics and 31 (36.5%) out of 85 subjects without asthma had anaphylaxis.
Cofactors related to the occurrence of food allergy
We found 19 (10.5%) events to be accompanied by cofactors with the following frequencies: exercise in 10 events, alcohol in 5 events, medicine in 2 events, and taking a shower in 2 events. In 10 events with exercise as cofactors, 5 and 3 events were caused by wheat and seafood, respectively. Four (80%) of 5 patients with wheat dependent exercise-induced anaphylaxis had positive results on serum specific IgE to ω5-gliadin. Common medications involved as cofactors of FA were nonsteroidal anti-inflammatory drugs and antibiotics.
DISCUSSION
This is the first study to investigate common causative food allergens according to age, sex, and clinical manifestations of FA in Korean adults. In the present study, seafood was found to be the most frequent cause of FA in adults, regardless of sex and age, consistent with previous study results.9,10,11 Additionally, more than half of the seafood-induced FA events presented as anaphylaxis. In agreement with our results, a recent study reported that seafood was the most common cause of food anaphylaxis in children between the ages of 7 and 18.12 Therefore, more intensive attention should be paid to adults with FA whose causative food allergens likely involve FA to seafood. The second most frequent causative food allergens were fruits in men and meats in women. Comparison of food allergens according to age groups demonstrated that the second most frequent food allergens were fruits and nuts-beans-seeds in the younger age group and vegetables and meats in the older age group. These findings may provide important additive information for clinicians seeking to determine causative food allergens in Korean adults.
Ethnic and regional differences may contribute to the disparity in common food allergens, because principal food and dietary habits, as well as environmental factors, such as common aeroallergens, also vary among countries. A study of 171 adult-onset FA cases from a single center in the US reported the 5 most common food allergens as shellfish, tree nut, non-shell fish, soy, and peanut.9 A population-based Canadian study reported that the most prevalent causative allergen of adult FA was seafood, followed by fruits, vegetables, and tree nut, in that order.10,11 Wheat was not reported as a common food allergen in these 2 studies. Meanwhile, 11.6% of all FA events involved grains-induced FA (15 wheat and 7 buckwheat) in the present study. In review of studies on FA in an Asian population, we noted similarities in causative food allergens for Japan with our results: common allergens included crustaceans, wheat, and fruits in that order.13 Chrysalis has been noted to be the most common allergen in a previous study which investigated the sensitization pattern of food allergens in Korean adults,14 whereas there were only 2 food allergy cases in our study population. Further studies on clinical manifestation along with the sensitization pattern to chrysalis should be performed.
A gender difference in FA has been reported only in the child population. Male gender was a risk factor in 2 kinds of FA phenotypes; multiple FA but predominantly peanut (odd ratio: 2.00) and multiple FA but predominantly egg (odd ratio: 2.27).15 In the present study, the male predominance of FA caused by fruits has been observed; however, further studies that include a larger number of patients are needed to elucidate the association between gender and FA.
The major manifestations of FA in Korean adults were cutaneous symptoms, such as urticaria, itching, rashes, and angioedema, in accordance with previous studies.9,16 Previous studies reported anaphylaxis rates ranging from 0.14%16 to 49%9 for the overall FA cases; 26% of all FA cases involved anaphylaxis in the present study. Differences in the study populations resulting from different methods of enrollment and inclusion criteria may have contributed to this disparity in the study results: the proportion of anaphylaxis was low in a self-reported questionnaire-based survey of the general population,16 and another study excluded OAS from major clinical types of FA resulting in a higher proportion of anaphylaxis.9
Among different study populations, different types of foods are reported as primary allergens in FA presenting as anaphylaxis. In a study in the United Kingdom, unidentified nut (23%) and peanut (22%) were leading causes of adult anaphylaxis.17 Nevertheless, another Asian studies reported crustacean (68%) as the primary causative food allergen in patients with moderate to severe FA.16,18,19 Crustacean and grains, including wheat and buckwheat, were more prevalent causative food allergens of anaphylaxis in Korea. Taken together, in contrast to Western countries, crustacean and wheat should be considered as not only common food allergens, but also allergens primarily associated with anaphylaxis in Asian adults.
Cofactors that can cause FA or increase the severity of FA have been reported to be present in 13% of all FA events.20 Exercise was the most common cofactor for FA and severe manifestations. Therefore, careful history taking to evaluate cofactors, including exercise, alcohol drinking, and taking medications, especially for patients presenting as anaphylaxis, is important for the prevention for unanticipated recurrence of anaphylaxis.
This study has several limitations as a retrospective observational study conducted at a single center. Onset age, latent periods, and types of trigger foods were dependent on the patients' recollection. Although 88.4% of the cases had a history of FA, no double-blind, placebo-controlled food challenge test was administered in the present study. Nevertheless, since we focused on cases of immediate food hypersensitivity in adults, allergen SPT and serum specific IgE to suspicious food allergens were helpful in confirming the causative foods.
In conclusion, information on demographic factors and clinical manifestations may be useful to physicians in assessing causes of FA in order to help patients avoid other FA events.
Footnotes
There are no financial or other issues that might lead to conflict of interest.
SUPPLEMENTARY MATERIAL
Specific IgE detection rate according to causative food allergen
References
- 1.Mullins RJ, Dear KB, Tang ML. Time trends in Australian hospital anaphylaxis admissions in 1998-1999 to 2011-2012. J Allergy Clin Immunol. 2015;136:367–375. doi: 10.1016/j.jaci.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133:291–307. doi: 10.1016/j.jaci.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 3.Park M, Kim D, Ahn K, Kim J, Han Y. Prevalence of immediate-type food allergy in early childhood in Seoul. Allergy Asthma Immunol Res. 2014;6:131–136. doi: 10.4168/aair.2014.6.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008;51:343–350. [Google Scholar]
- 5.Branum AM, Lukacs S. In: Food allergy among U.S. children: trends in prevalence and hospitalizations. Lukacs S, editor. Atlanta (GA): Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 6.Sindher S, Fleischer DM, Spergel JM. Advances in the treatment of food allergy: sublingual and epicutaneous immunotherapy. Immunol Allergy Clin North Am. 2016;36:39–54. doi: 10.1016/j.iac.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126:S1–58. doi: 10.1016/j.jaci.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song TW. Diagnostic decision points of specific ige titers in patients with food allergy: are they appropriate in all clinical settings. Allergy Asthma Immunol Res. 2015;7:309–311. doi: 10.4168/aair.2015.7.4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamdar TA, Peterson S, Lau CH, Saltoun CA, Gupta RS, Bryce PJ. Prevalence and characteristics of adult-onset food allergy. J Allergy Clin Immunol Pract. 2015;3:114–115. doi: 10.1016/j.jaip.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ben-Shoshan M, Harrington DW, Soller L, Fragapane J, Joseph L, St Pierre Y, et al. A population-based study on peanut, tree nut, fish, shellfish, and sesame allergy prevalence in Canada. J Allergy Clin Immunol. 2010;125:1327–1335. doi: 10.1016/j.jaci.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Soller L, Ben-Shoshan M, Harrington DW, Fragapane J, Joseph L, St Pierre Y, et al. Overall prevalence of self-reported food allergy in Canada. J Allergy Clin Immunol. 2012;130:986–988. doi: 10.1016/j.jaci.2012.06.029. [DOI] [PubMed] [Google Scholar]
- 12.Lee SY, Ahn K, Kim J, Jang GC, Min TK, Yang HJ, et al. A multicenter retrospective case study of anaphylaxis triggers by age in Korean children. Allergy Asthma Immunol Res. 2016;8:535–540. doi: 10.4168/aair.2016.8.6.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, et al. Japanese guideline for food allergy 2014. Allergol Int. 2014;63:399–419. doi: 10.2332/allergolint.14-RAI-0770. [DOI] [PubMed] [Google Scholar]
- 14.Kim SR, Park HJ, Park KH, Lee JH, Park JW. IgE sensitization patterns to commonly consumed foods determined by skin prick test in Korean adults. J Korean Med Sci. 2016;31:1197–1201. doi: 10.3346/jkms.2016.31.8.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peters RL, Allen KJ, Dharmage SC, Lodge CJ, Koplin JJ, Ponsonby AL, et al. Differential factors associated with challenge-proven food allergy phenotypes in a population cohort of infants: a latent class analysis. Clin Exp Allergy. 2015;45:953–963. doi: 10.1111/cea.12478. [DOI] [PubMed] [Google Scholar]
- 16.Wu TC, Tsai TC, Huang CF, Chang FY, Lin CC, Huang IF, et al. Prevalence of food allergy in Taiwan: a questionnaire-based survey. Intern Med J. 2012;42:1310–1315. doi: 10.1111/j.1445-5994.2012.02820.x. [DOI] [PubMed] [Google Scholar]
- 17.Turner PJ, Gowland MH, Sharma V, Ierodiakonou D, Harper N, Garcez T, et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992-2012. J Allergy Clin Immunol. 2015;135:956–963. doi: 10.1016/j.jaci.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ye YM, Kim MK, Kang HR, Kim TB, Sohn SW, Koh YI, et al. Predictors of the severity and serious outcomes of anaphylaxis in Korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res. 2015;7:22–29. doi: 10.4168/aair.2015.7.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong L, Huang CH, Lee BW. Shellfish and house dust mite allergies: is the link tropomyosin? Allergy Asthma Immunol Res. 2016;8:101–106. doi: 10.4168/aair.2016.8.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Versluis A, van Os-Medendorp H, Kruizinga AG, Blom WM, Houben GF, Knulst AC. Cofactors in allergic reactions to food: physical exercise and alcohol are the most important. Immun Inflamm Dis. 2016;4:392–400. doi: 10.1002/iid3.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Specific IgE detection rate according to causative food allergen