Abstract
Objective To estimate the benefits and harms of using corticosteroids as an adjunct treatment for sore throat.
Design Systematic review and meta-analysis of randomised control trials.
Data sources Medline, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), trial registries up to May 2017, reference lists of eligible trials, related reviews.
Study selection Randomised controlled trials of the addition of corticosteroids to standard clinical care for patients aged 5 or older in emergency department and primary care settings with clinical signs of acute tonsillitis, pharyngitis, or the clinical syndrome of sore throat. Trials were included irrespective of language or publication status.
Review methods Reviewers identified studies, extracted data, and assessed the quality of the evidence, independently and in duplicate. A parallel guideline committee (BMJ Rapid Recommendation) provided input on the design and interpretation of the systematic review, including the selection of outcomes important to patients. Random effects model was used for meta-analyses. Quality of evidence was assessed with the GRADE approach.
Results 10 eligible trials enrolled 1426 individuals. Patients who received single low dose corticosteroids (the most common intervention was oral dexamethasone with a maximum dose of 10 mg) were twice as likely to experience pain relief after 24 hours (relative risk 2.2, 95% confidence interval 1.2 to 4.3; risk difference 12.4%; moderate quality evidence) and 1.5 times more likely to have no pain at 48 hours (1.5, 1.3 to 1.8; risk difference 18.3%; high quality). The mean time to onset of pain relief in patients treated with corticosteroids was 4.8 hours earlier (95% confidence interval −1.9 to −7.8; moderate quality) and the mean time to complete resolution of pain was 11.1 hours earlier (−0.4 to −21.8; low quality) than in those treated with placebo. The absolute pain reduction at 24 hours (visual analogue scale 0-10) was greater in patients treated with corticosteroids (mean difference 1.3, 95% confidence interval 0.7 to 1.9; moderate quality). Nine of the 10 trials sought information regarding adverse events. Six studies reported no adverse effects, and three studies reported few adverse events, which were mostly complications related to disease, with a similar incidence in both groups.
Conclusion Single low dose corticosteroids can provide pain relief in patients with sore throat, with no increase in serious adverse effects. Included trials did not assess the potential risks of larger cumulative doses in patients with recurrent episodes of acute sore throat.
Systematic review registration PROSPERO CRD42017067808.
Introduction
Sore throat is among the most common presenting complaints in both emergency departments and outpatient care settings. It is the cause of about 5% of medical visits in children and about 2% of all outpatient visits in adults.1 2 3 The most common cause of sore throat is acute pharyngitis caused by self limiting viral infections. Pain management with paracetamol (acetaminophen) or non-steroidal anti-inflammatory drugs (NSAIDs) therefore represents the mainstay of care.4 5 These drugs provide limited pain relief but also sometimes cause serious harm.6 7
Treatment of sore throat with antibiotics also provides modest benefit in reduction of symptoms and fever when the infection is bacterial, but their use could contribute to antibiotic resistance.8 9 Although most cases of sore throat have a viral aetiology, and the risk of secondary complications is low, clinicians commonly prescribe antibiotics.4 10 Though this could be because clinicians think that patients seeking care expect a course of antibiotics, in reality pain relief might be more important to them.10
Corticosteroids represent an additional therapeutic option for symptom relief. Randomised control trials suggest that a short course of low-to-moderate dose corticosteroids probably provides symptomatic benefit to patients with sore throat.11 12 13 14 Despite this evidence, clinicians do not commonly use steroids. Reasons might include uncertain applicability of the evidence to patients with less severe disease, as the initial studies enrolled only patients with severe sore throat presenting to emergency departments, almost all of whom received antibiotics.
This systematic review is part of the BMJ Rapid Recommendations project, a collaborative effort from the MAGIC research and innovation programme (www.magicproject.org) and BMJ. The aim of the project is to respond to new potentially practice changing evidence and provide a trustworthy practice guideline in a timely manner.15 In this case, the stimulus was the recent TOAST (Treatment Options without Antibiotics for Sore Throat) trial, which randomised over 500 patients with sore throat presenting to their primary care clinician who were not initially prescribed antibiotics; the TOAST authors reported beneficial effects of corticosteroids.16 In the light of this new potentially practice changing evidence, we updated the latest Cochrane review12 dealing with the effectiveness and safety of corticosteroids as an adjunct treatment for sore throat in addition to standard care compared with standard care alone. This systematic review informed the parallel guideline published in a multi-layered electronic format on bmj.com 17 and MAGICapp (https://www.magicapp.org/goto/guideline/JjXYAL/section/j79pvn).
Methods
Guideline panel and patient involvement
According to the BMJ Rapid Recommendations process,15 a guideline panel provided critical oversight to the review and identified populations, subgroups, and outcomes of interest. The panel included clinicians, methodologists, and patients with experience of sore throat. Patients received personal training and support to optimise contributions throughout the guideline development process. The patients on the panel led the interpretation of the results based on what they expected the typical patient values and preferences to be, as well as the variation between patients. Five patient representatives were full members of the guideline panel and contributed to the selection and prioritisation of outcomes, values and preferences assessments, and critical feedback to the protocol for the systematic review and the BMJ Rapid Recommendations manuscript.
Search strategy
We searched Medline, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) for relevant published randomised controlled trials based on the strategy reported in the most recent Cochrane systematic review,12 modified under the guidance of a research librarian (appendix 1). We limited the search from 1 January 2010, which included a two month overlap with the previous Cochrane review search,12 to 1 May 2017. There were no language restrictions. We reviewed reference lists from eligible new trials and related reviews for additional eligible trials and searched ClinicalTrials.gov for ongoing or unpublished trials and for additional data from published trials.
Study selection
Reviewers (BS, RACS, DP, RBP) independently and in duplicate screened the titles and abstracts of all identified studies using a priori selection criteria. Subsequently, the samereviewersindependently assessed eligibility of the full texts of potentially eligible studies. Reviewers resolved discrepancies through discussion or, if needed, by adjudication from a third reviewer.
We included randomised controlled trials that compared corticosteroids with standard of care or placebo and enrolled adults and/or children aged 5 and over in emergency departments and primary care settings with a clinical syndrome of sore throat (painful throat, odynophagia, or pharyngitis).
We excluded studies of participants who were admitted to hospital or immunocompromised and those with infectious mononucleosis, sore throat after any surgery or intubation (postoperative sore throat), gastroesophageal reflux disease, croup, or peritonsillar abscess. We also excluded studies that enrolled children aged under 5 because they would not be able to provide trustworthy outcome measurements, especially for self reported pain.
Our outcomes of interest were complete resolution of pain at 24 and 48 hours; mean time to onset of pain relief; mean time to complete resolution of pain; absolute reduction of pain at 24 hours; duration of bad/non-tolerable symptoms (such as problems for eating, drinking, swallowing); recurrence/relapse of symptoms; days missed from school or work; need for antibiotics; and rate of adverse events related to treatment. We included any adverse events reported by the authors.
Data abstraction and risk of bias assessment
Reviewers extracted the following data, independently and in duplicate: general study information (authors, publication year, and study location); study population details (sample size, age, diagnosis, and percentage of participants with confirmed group A β haemolytic streptococcus (GAS) pharyngitis or culture positive for bacterial pathogens); setting (primary care versus hospital emergency department); details on the intervention and comparison (for example, type, form, duration, and dose of corticosteroids; type of control group); co-interventions (proportion of participants who received antibiotics and/or analgesics); and outcomes as listed above.
In randomised controlled trials with more than two arms, we extracted data from the arm closest to a single dose regimen or data from the arm that received corticosteroid as adjunct treatment to standard of care rather than instead of standard of care. In trials with data for both oral and parenteral corticosteroids, we used oral data for the main analysis and intramuscular data for the appropriate subgroup analysis.
Two reviewers independently assessed risk of bias using the modified Cochrane risk of bias instrument,18 19 which deals with random sequence generation; allocation concealment; blinding of study participants, healthcare providers, and outcome assessors; incomplete outcome data; and other potential sources of bias. Reviewers classified studies at high risk of bias when they had rated at least one item as high risk of bias.
To assess the quality of evidence, we used the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) approach that classifies evidence as high, moderate, low, or very low quality based on considerations of risk of bias, consistency, directness, precision, and publication bias.20 We resolved disagreements between reviewers in data extraction and assessments of risk of bias or quality of evidence by discussion and, if needed, by third party adjudication. We used the MAGICapp platform to generate the GRADE summary of findings table.
Data synthesis and statistical methods
For continuous outcomes, we calculated the mean difference and its corresponding 95% confidence interval. For dichotomous outcomes, we calculated the relative risk and its corresponding 95% confidence interval and determined the absolute effect by multiplying the relative risk and its confidence interval with the estimated baseline risk. The median of the placebo group of included randomised controlled trials provided the baseline risk.
Statistical heterogeneity was determined with the Q statistic and I2. We used the DerSimonian-Laird random effects model for the meta-analysis of all outcomes. Regardless of the observed statistical heterogeneity, we conducted the following prespecified subgroup analyses when each subgroup was represented by at least two studies: age (children v adults), postulating a larger effect in adults; route of administration of corticosteroids (oral v parenteral), postulating a larger effect for parenteral; presence or absence of positive results on culture for a bacterial pathogen or direct antigen test for group A β haemolytic streptococcus, postulating a larger effect in patients with positive test results; initial setting (emergency departments v family practice), postulating a larger effect in patients consulting the emergency department; and place of subsequent care (admitted to hospital v outpatient), postulating a larger effect among the patients admitted. For subgroup analysis, we tested for interaction using a χ2 significance test.21 We planned to examine publication bias using funnel plots for outcomes for which data from 10 or more studies were available.22 Data were analysed with STATA software (version 14.2, TX, USA).
Patient involvement
Five patient representatives were full members of the guideline panel, and contributed to the selection and prioritisation of outcomes, values and preferences assessments, and critical feedback to the protocol for the systematic review and the BMJ Rapid Recommendations manuscript.
Results
Description of included studies
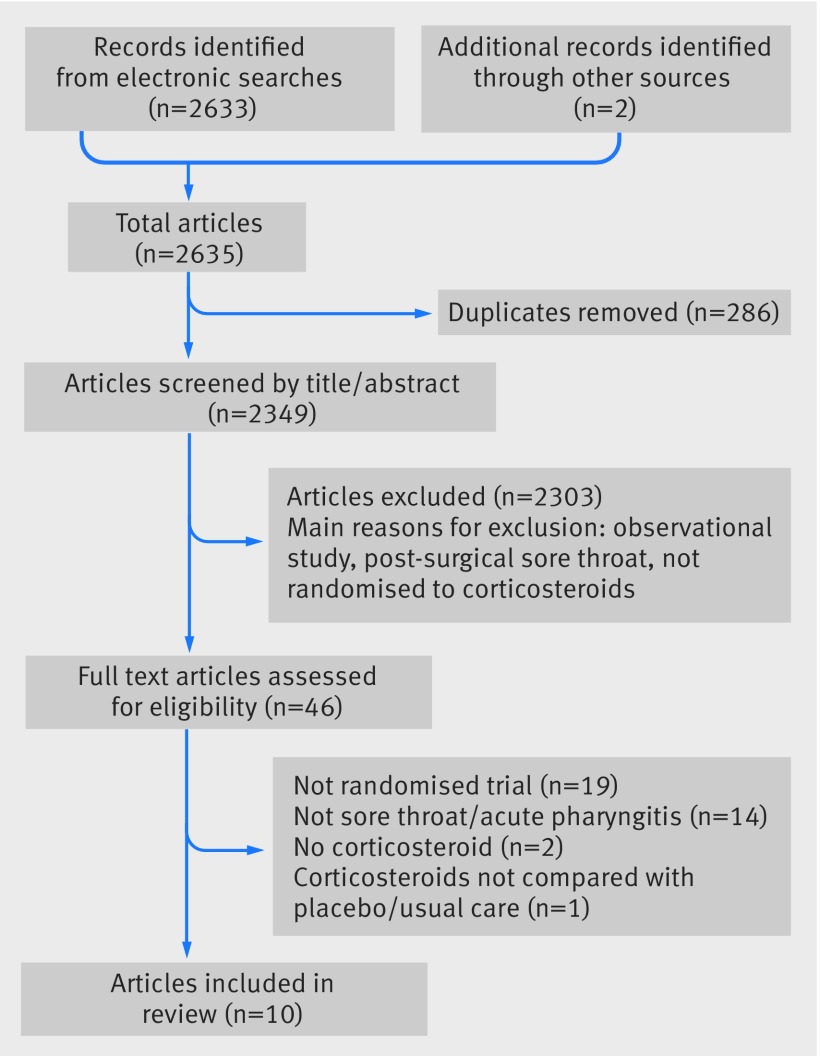
We identified 2349 titles and abstracts through our literature search, of which 46 were potentially eligible and 36 were excluded (19 were not randomised trials; 14 had no patients with sore throat/acute pharyngitis; in three corticosteroids were not among the interventions or were not compared with a placebo/usual care). Figure 1 shows the details of study selection process.
Fig 1 Selection of studies in review of corticosteroids for treatment of sore throat
The 10 randomised controlled trials that proved eligible enrolled 1426 individuals. Eight studies recruited patients from hospital emergency departments23 24 25 26 27 28 29 30 and two from primary care.16 31 Three studies enrolled children,27 28 29 six studies enrolled adults,16 24 25 26 30 31 and one study included both children and adults.23 Oral dexamethasone (single dose of 10 mg for adults and 0.6 mg/kg, maximum 10 mg for children) was the most common intervention (five studies) followed by single dose intramuscular injection of dexamethasone (three studies). All patients in three trials received both antibiotics and analgesics as the usual care25 26 30; in two trials, all patients received antibiotics, while analgesics were prescribed at the physician’s discretion.23 24 In the five remaining trials, patients in usual care group received antibiotics or analgesics at the physician’s discretion.16 27 28 29 31Table 1 presents study details.
Table 1.
Characteristics of studies included in systematic review of corticosteroids for treatment of sore throat
| Study | Setting | Population | Mean age (years) | No randomised (intervention/control) | Pathogen positive* (%) | Type of steroid | Dose and duration | Antibiotic use (%) | Analgesic use (%) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |||||||||
| Hayward, 201716 | Primary care | Adults | 34.0 | 293/283 | 14.9 | Dexamethasone (oral) | 10 mg, single dose | 39.9 | 39.0 | 77.1 | 78.9 | |
| Tasar, 200830 | ED | Adults | 31.3 | 31/42 | NR | Dexamethasone (IM) | 8 mg, single dose | 100 | 100 | 100 | 100 | |
| Niland, 200629 | ED | Children | 7.7† | 30/30 | 100.0 | Dexamethasone (oral) | 0.6 mg/kg, max 10 mg, single dose | NR | NR | NR | NR | |
| Olympia, 200528 | ED | Children | 11.9 | 75/75 | 55.2 | Dexamethasone (oral) | 0.6 mg/kg, max 10 mg, single dose | 47.1 | 63.0 | 35.1 | 41.2 | |
| Kiderman, 200531 | Primary care | Adults | 33.9 | 40/39 | 57.5 | Prednisone (oral) | 60 mg, single dose (100%) or for 2 days (50%) | 51.4 | 63.2 | NR | NR | |
| Bulloch, 200327 | ED | Children | 9.7 | 92/92 | 46.2 | Dexamethasone (oral) | 0.6 mg/kg, max 10 mg, single dose | 48.9 | 43.5 | NR | NR | |
| Ahn, 200326 | ED | Adults | 35.3 | 36/36 | 45.0 | Dexamethasone (oral) | 5 mg for 2 days | 100 | 100 | 100 | 100 | |
| Wei, 200225 | ED | Adults | 28.1 | 42/38 | 39.0 | Dexamethasone (oral and IM) | 10 mg, single dose | 100 | 100 | 100 | 100 | |
| Marvez-Valls, 199824 | ED | Adults | 29.2 | 46/46 | 53.26 | Betamethasone (IM) | 8 mg/2 mL injection‡, single dose | 100 | 100 | NR | NR | |
| O’Brien 1993,23 | ED | Both | 26.4 | 31/27 | NR | Dexamethasone (IM) | 10 mg, single dose | 100 | 100 | NR | NR | |
ED=emergency department; NR=not reported.
*Positive result on culture or rapid test for group A β haemolytic streptococcus (GABHS).
†Median (interquartile range 6-12).
‡Dose is best guess from US formularies.
Among the included studies, four randomised controlled trials were at high risk of bias.23 24 26 28 One study had issues in more than one category of risk.26 The three remaining studies had issues in concealment of the treatment allocation, incomplete outcome reporting, and blinding of outcome assessors. Appendix 2 summarises the risk of bias assessments.
Table 2 shows findings for all outcomes. Interactive tables summarising findings are available at https://www.magicapp.org/goto/guideline/JjXYAL/section/j79pvn
Table 2.
GRADE summary of findings for corticosteroids (intervention) versus no corticosteroids (control) in patients with sore throat
| Outcome and timeframe | Study results (95% CI) and measurements | Absolute effect estimates | Quality of evidence | Summary | ||
|---|---|---|---|---|---|---|
| No corticosteroids | Corticosteroids | Difference (95% CI) | ||||
| Complete resolution of pain at 24 hours | Relative risk: 2.24 (1.17 to 4.29). 1049 patients in 5 studies | 100/1000 | 224/1000 | 124 more (17 more to 329 more | Moderate (inconsistency and imprecision)* † ‡ | Corticosteroids probably increase chance of complete resolution of pain at 24 hours |
| Complete resolution of pain at 48 hours | Relative risk: 1.48 (1.26 to 1.75). 1076 patients in 4 studies | 425/1000 | 629/1000 | 204 more (111 more to 319 more) | High‡ | Corticosteroids increase chance of complete resolution of pain at 48 hours |
| Recurrence/relapse of symptoms | Relative risk: 0.52 (0.16 to 1.73). 372 patients in 3 studies | 65/1000 | 34/1000 | 31 fewer (55 fewer to 47 more) | Moderate (serious imprecision)‡ § ¶ | Corticosteroids probably have no important effect on chance that symptoms recur |
| Antibiotics prescription | Relative risk: 0.83 (0.61 to 1.13). 342 patients in 1 study. Follow-up 28 days | 564/1000 | 468/1000 | 96 fewer (220 fewer to 73 more) | Low (very serious imprecision)** | Corticosteroids might decrease chance of taking antibiotics in patients given prescription with instructions to take antibiotic if unimproved or worse |
| Mean time to onset of pain relief (hours) | 907 patients in 8 studies | 12.3 hours | 7.4 hours | 4.8 fewer (7.8 fewer to 1.9 fewer) | Moderate (inconsistency and imprecision)‡ †† ‡‡ §§ | Corticosteroids probably shorten the time until pain starts to improve. |
| Mean time to complete resolution of pain (hours) | 720 patients in 6 studies | 44.0 hours | 33.0 hours | 11.1 fewer (21.8 fewer to 0.4 fewer) | Low (serious imprecision and inconsistency)‡ †† ‡‡ ¶¶ | Corticosteroids might shorten duration of pain |
| Pain reduction 24 hours | Scale: high better. 1247 patients in 8 studies | Mean 3.3 hours | Mean 4.6 hours | 1.3 higher (0.7 higher to 1.9 higher) | Moderate (inconsistency and imprecision)‡ †† ‡‡ *** | Corticosteroids probably reduce severity of pain at 24 hours |
| Duration of bad/non-tolerable symptoms | — | — | — | 0 (0 to 0) | — | No studies provided information on this outcome |
| Days missed from work or school | 181 patients in 2 studies. Follow-up to 14 days | Two trials reported days missed from work/school. In Kiderman et al, 22/40 (55%) in steroids group and 27/39 (69%) in placebo group took time off work (relative risk 0.79, 95% CI 0.56 to 1.13). Marvez-Valls et al reported average time patients in each arm missed from work/school: average 0.4 (SD 1.4) days in intervention group adults v and 0.7 (SD 1.4) days in placebo group adults; mean difference 0.30 days, −0.28 to 0.88) | Moderate (serious imprecision and some concerns of risk of bias)††† ‡‡‡ | Corticosteroids probably have no important effect on days missed from work or school | ||
| Serious adverse events | 808 patients in 3 studies. Follow-up to 10 days | Few adverse effects reported in trials, mostly disease related complications, and occurred with similar frequency in intervention and control groups (see table 3) | Moderate§§§ | Corticosteroids probably do not increase risk of adverse events | ||
*Considerable heterogeneity (I2=69%). Not rated down because clinical inconsistency was deemed not important as all results of included studies have similar clinical implication.
†Limits of confidence interval suggest small benefit in one extreme and benefit important to patients in other. Because imprecision is linked to inconsistency, certainty of evidence rated down by only one level.
‡Publication bias not tested because of small number of studies.
§Not rated down for risk of bias as one of three trials judged to be at high risk of bias from missing participant data.
¶Confidence interval suggests that corticosteroids increase chance of recurrence of symptoms in one extreme but decrease this chance in other extreme.
**Confidence interval suggest that corticosteroids could largely reduce chance of taking antibiotics in one extreme but could slightly increase this chance in other extreme.
††Not rated down for risk of bias as equal number of trials judged to be at high and low risk of bias, but P value for test of interaction showed no difference between two estimates.
‡‡Large unexplained clinical and statistical inconsistency.
§§Confidence interval suggests small benefit in one extreme and benefit that some patients might consider important in other extreme. As this imprecision was result of inconsistency, certainty of evidence rated down by only one level.
¶¶Confidence interval suggests trivial benefit in one extreme and benefit that would be considered important by most patients in other extreme.
***Confidence interval suggests small benefit in one extreme and benefit important to patients in other. As this imprecision was related to inconsistency, rated down by only one level.
†††One study was at high risk of bias from concerns with regards to allocate concealment.
‡‡‡Studies showed that corticosteroids could increase days missed from school or work in one extreme but decrease them in other extreme.
§§§High risk of bias studies showed similar results as low risk of bias studies; however, high risk of selective outcome reporting was possible.
Pain
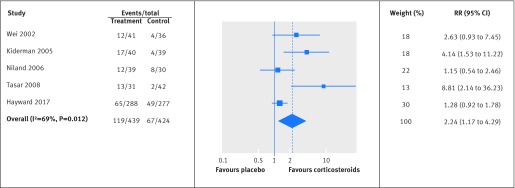
In the five randomised controlled trials that reported complete resolution of symptoms at 24 hours,16 25 29 30 31 patients who received a single dose of corticosteroids were twice as likely to experience complete symptom resolution than placebo patients (relative risk 2.24, 95% confidence interval 1.17 to 4.29; I2=69%, 22.4% v 10.0%; moderate quality evidence; fig 2, table 2). All studies reporting this outcome were at low risk of bias. Tests of interaction showed no evidence of any subgroup effect (table A in appendix 3).
Fig 2 Relative risk for complete resolution of pain at 24 hours for corticosteroid v placebo groups in review of treatment of sore throat. Pooled relative risk calculated by DerSimonian-Laird random effects model
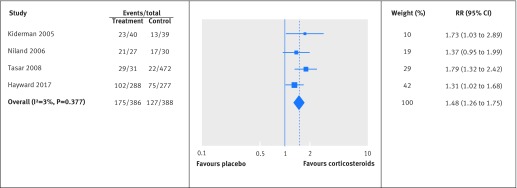
In the four trials that reported complete resolution of pain at 48 hours,16 29 30 31 patients treated with corticosteroids were 50% more likely to experience complete resolution (relative risk 1.48, 95% confidence interval 1.26 to 1.75; I2=3%, 60.8% v 42.5%; high quality; fig 3, table 2). These four studies were all at low risk of bias, and tests of interaction showed no evidence of any subgroup effect (table A in appendix 3).
Fig 3 Relative risk for complete resolution of pain at 48 hours for corticosteroid v placebo groups in review of treatment of sore throat. Pooled relative risk calculated by DerSimonian-Laird random effects model
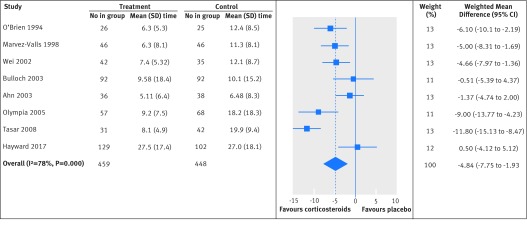
In the eight studies that reported mean time to onset of pain relief,16 23 24 25 26 27 28 30 patients who received corticosteroids experienced onset of pain relief on average 4.8 hours earlier than those who received placebo (95% confidence interval −1.9 to −7.8; I2=78%; moderate quality; fig 4, table 2). We found no evidence of subgroup effect for this outcome (table A in appendix 3).
Fig 4 Weighted mean difference in mean time to onset of pain relief (hours) between corticosteroids and placebo groups in review of treatment of sore throat. Pooled mean difference was calculated by DerSimonian-Laird random effects model
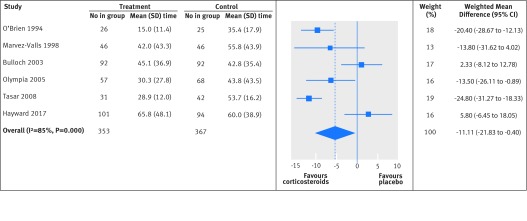
Time to complete resolution of pain was reported in six studies.16 23 24 27 28 30 On average, patients receiving a single dose corticosteroid experienced complete resolution 11.1 hours earlier (95% confidence interval −0.4 to −21.8; I2=85%; low quality; fig 5, table 2). In our subgroup analysis, we found a significantly larger effect among those treated with intramuscular corticosteroids (mean difference −22.4 (95% confidence interval −27.3 to −17.5) and −1.5 (−12.6 to 9.5), for intramuscular and oral corticosteroids, respectively; P=0.001 for interaction); however, the effect modification is suggested by comparison between rather than within studies. We found no other subgroup effect (table B in appendix 3).
Fig 5 Weighted mean difference in mean time to complete resolution of pain (hours) between corticosteroids and placebo groups in review of treatment of sore throat. Pooled mean difference calculated by DerSimonian-Laird random effects model
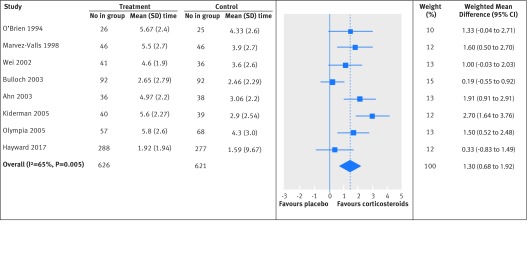
Meta-analysis from eight studies that assessed pain with a visual analogue scale (0=no pain, 10=maximum pain) at baseline and after 24 hours16 23 24 25 26 27 28 31 showed a 1.3 points lower pain score among patients treated with corticosteroids compared with those treated with placebo at 24 hours (95% confidence interval 0.7 to 1.9; I2=65%; moderate quality; fig 6, table 2). We found no evidence of subgroup effect for this outcome (table B in appendix 3).
Fig 6 Weighted mean difference in absolute reduction of pain at 24 hours (0-10; 0=no pain, 10=maximum pain) between corticosteroids and placebo groups in review of treatment of sore throat. Pooled mean difference calculated by DerSimonian-Laird random effects model
To assess the possibility that there was selective reporting, we examined the magnitude of effect on the time to onset of pain relief, time to complete resolution of pain, and absolute pain reduction in studies that did and did not report resolution of pain at 24 and 48 hours. The magnitude of effect on the other pain outcomes was similar in both sets of studies, making selective reporting less likely (table C in appendix 3).
Other outcomes
The authors of one study reported a possible decrease in the likelihood of receipt of antibiotics in patients treated with corticosteroids (relative risk 0.83, 95% confidence interval 0.61 to 1.13; moderate quality).16 Three studies27 28 31 suggested a possible lower risk of recurrence/relapse of the symptoms (0.52, 0.16to 1.73; I2=23%; moderate quality, table D in appendix 3, table 2).
Kiderman and colleagues reported that 22/40 (55%) patients treated with corticosteroids and 27/39 (69%) taking placebo took time off work because of sore throat (relative risk 0.8, 95% confidence interval 0.6 to 1.1).31 Marvez-Valls and colleagues reported that adult patients treated with corticosteroids missed an average of 0.4 (SD 1.4) days, whereas patients in the placebo arm missed an average of 0.7 (SD 1.4) days (mean difference −0.3 days, 95% confidence interval −0.87 to 0.27).24 None of the trials reported duration of bad/non-tolerable symptoms.
All studies except one sought information on adverse effects using different methods including standardised questionnaire (two studies), open ended questions or diaries to capture self reported adverse events (five studies), or a checklist of complications (two studies). Table 3 provides details of adverse effects assessed and methods used for capturing them. Six studies reported no adverse effects, and three studies reported adverse events, in both steroids and comparator arms, which were mostly complications related to disease and occurred with similar frequency in the intervention and control groups (table 3). Hayward and colleagues reported two serious adverse events (admission to hospital for pharyngeal or peritonsillar abscess, tonsillitis, and pneumonia) in the corticosteroids group (0.7%) and three in the placebo group (1.1%).16 Olympia and colleagues reported one out of the 57 (1.8%) children in the corticosteroids group and two out of the 68 (2.9%) children in the placebo group developed a peritonsillar abscess (moderate quality, table 2 and table 3).28
Table 3.
Summary of adverse event assessments among trials included in systematic review of corticosteroids for treatment of sore throat
| Study | Methods used to assess adverse effects | Adverse effects assessed* | Adverse effects reported |
|---|---|---|---|
| O’Brien, 1993 | Standardised questionnaire | Nausea, vomiting, or diarrhoea | None reported |
| Marvez-Valls, 1998 | Self reported side effects at follow-up call | Any adverse event | None reported |
| Wei, 2002 | Self reported side effects at follow-up call | Any adverse event | 1 patient who received corticosteroids (3%) reported hiccups |
| Ahn, 2003 | Not reported | Not reported | None reported |
| Bulloch, 2003 | Checklist of complication at follow-up call | Rash, joint pain, movement disorder, persistent fever, or blood in urine or “cola coloured” urine in past month, peritonsillar abscess | None reported |
| Kiderman, 2005 | Not reported | Any adverse event | None reported |
| Olympia, 2005 | Checklist of complication at daily follow-up calls | Headache, nausea or vomiting, abdominal pain, myalgia, mood changes, dizziness, and swollen legs, peritonsillar abscess | 1/57 (1.8%) children in corticosteroids group and 2/68 (2.9%) in control group developed peritonsillar abscess. 3/57 (5.3%) children in corticosteroid group and 2/68 (2.9%) in placebo group were admitted for dehydration |
| Niland, 2006 | Patient completed diaries and by structured telephone interviews | Headache, abdominal pain (Wong-Baker FACES scale), fever, vomiting, and information sought regarding additional medical care | Steroid treatment did not result in additional patient adverse effects, symptom relapses, or complications related to disease |
| Tasar, 2008 | Self reported side effects at follow-up call | Complications related to dexamethasone and azithromycin | None reported |
| Hayward, 2017 | Attendance or telephone contact at any healthcare facility (including GP clinic, urgent care clinic, emergency department, or hospital admission) with symptoms or complications associated with sore throat (defined as direct suppurative complications or presentation with sore throat symptoms) | Any adverse event | 2 serious adverse events (admissions for pharyngeal or peritonsillar abscess, tonsillitis, and pneumonia) in corticosteroids group (0.7%) and 3 in placebo group (1.1%) |
*Reflect investigators’ attempts not only to detect adverse effect attributable to steroids, but also treatment failures, relapses, and complications related to disease.
Discussion
In patients with acute sore throat, there is primarily moderate to high quality evidence that one or two low doses of corticosteroids reduces the intensity and duration of pain—pain scores at 24 hours, complete resolution of pain at 24 and at 48 hours, time to onset of pain relief, and time to complete pain relief. In this review, results were consistent across studies and across all pain outcomes (table 2). The reduction in pain achieved was modest—for example, mean time to complete resolution of pain was about 11 hours shorter, and about 18% more patients had complete pain relief at 48 hours. At 24 hours, the mean improvement in pain scores was about 13 mm on a visual analogue scale from 0 to 100 mm (with the minimal important difference being about 10 mm).32 The relative effects were similar across severities, though patients with less severe sore throat had less absolute benefit from corticosteroids. The balance of benefits and harms therefore almost certainly depends on the severity of the patient’s sore throat.
Whether corticosteroids reduce recurrence/relapse of symptoms, number of days missed from school or work, duration of bad/intolerable symptoms, or antibiotic use remains uncertain. Regarding the safety of the short courses and low doses of corticosteroids, studies reported few adverse effects, with no apparent increase in events in patients treated with corticosteroid.
Strengths and limitations of study
Strengths of this review include explicit eligibility criteria; a comprehensive search developed with a research librarian; duplicate assessment of eligibility, risk of bias, and data abstraction; consideration of all outcomes important to patients; consideration of selective reporting bias; consideration of possible subgroup effects; and rigorous use of the GRADE approach to rate quality of evidence. The limitations of our review have to do with the underlying evidence. Only three trials explicitly reported adverse events, and they did so inconsistently.16 25 28 We observed substantial statistical heterogeneity in some of the outcomes. We explored the source(s) of heterogeneity by subgroup analysis and rated down for inconsistency in GRADE assessments for outcomes with unexplained heterogeneity.
In comparison with previous systematic reviews,11 12 we included two additional randomised controlled trials,16 26 which almost doubled the number of participants. Results from our meta-analysis are consistent with previous findings that corticosteroids reduce pain at 48 hours and probably reduce other pain outcomes. In addition to enhanced precision with the additional studies, our meta-analysis adds to the existing evidence in that we considered absolute in addition to relative effect measures, providing a clear picture of the magnitude of effect.33 In part because of input from the guideline panel, we considered additional outcomes that participating patients considered important, including risk of recurrence of symptoms, duration of bad/non-tolerable symptoms, need for antibiotics, and days missed from school or work. An important additional contribution of the new evidence is that it extends the applicability beyond patients with severe sore throat treated with antibiotics for group A β haemolytic streptococcus pharyngitis in the emergency department, to a broader range of patients not treated with antibiotics.
We explored and were able to dismiss subgroup effects, with one exception: the reduction in mean time to complete resolution of pain was greater with intramuscular than with oral corticosteroids. The subgroup effect and its direction was specified a priori, the difference between subgroups was relatively large (about 21 hours), and chance seems an unlikely explanation (P<0.001). Credibility of the effect, however, is undermined34 as the effect modification is suggested by comparison between rather than within studies, and we found no similar difference in any other outcome. In addition, the only randomised controlled trial that compared oral and intramuscular treatment with dexamethasone reported no significant difference in any outcome.25
The few serious adverse effects in the included trials occurred with similar frequency in the intervention and control groups, although some minor adverse effects reported by patients might not always have been noted. Potential adverse effects that appear later are more likely to occur after repeated use or are rare would not have been captured in the trials. Recent observational studies have raised the possibility of extremely rare but serious adverse effects after short courses of corticosteroids.35 The quality of this evidence is, for several reasons, low with respect to the current question. The studies used observational designs from large databases with suboptimal verification of diagnoses; serious confounding by indication raises the possibility that the association is a result of the underlying disease process (such as acute inflammation or exacerbation) rather than the corticosteroids themselves; and indirectness in that the doses used in the trials were lower and the duration of treatment was considerably shorter than the duration in the observational studies. Among children, a recent overview of reviews looked at evidence from 44 randomised controlled trials on conditions that required a short course of steroids (such as asthma, bronchiolitis, croup, wheeze, and pharyngitis/tonsillitis) and reported no major adverse events.36
Despite previous evidence that corticosteroids might be beneficial, several groups and guidelines currently recommend against their routine use on the basis that evidence was applicable only to patients with severe pharyngitis who were also prescribed antibiotics in an emergency department.1 37 38 The body of evidence now includes a broader representation of patients. The largest and most recent randomised controlled trial included 565 patients presenting to their general practitioner rather than an emergency department, and none of the patients initially received antibiotics.16 We found no subgroup differences with respect to patient group: the evidence seems to apply equally to patients who did and did not receive antibiotics. The evidence also seems to apply equally to patients with sore throat from group A β haemolytic streptococcus pharyngitis and some with sore throat negative for group A β haemolytic streptococcus.
In the five trials that reported co-interventions, about 80% of the participants received additional analgesics such as paracetamol and NSAIDs. Therefore, a single dose of corticosteroids seems to further reduce pain when used in combination with other analgesics. Although the benefits are relatively small, many patients are likely to consider them important. Patients with less severe sore throat, however, will obtain less absolute benefit from corticosteroids. Thus, the balance of benefits and harms almost certainly depends on the severity of the patient’s sore throat. With available evidence suggesting that serious adverse effects are rare or absent, the addition of one or two doses of steroids to the symptomatic management of sore throat is likely to appeal to many patients. More high quality data would be helpful to fully understand the net balance of benefits and harms according to severity of symptoms, particularly in primary care settings.
Linked articles in this BMJ Rapid Recommendations cluster
-
• Aertgeerts B, Agoritsas T, Siemieniuk RAC, et al. Corticosteroids for sore throat: a clinical practice guideline. BMJ 2017;358:j4090 doi:10.1136/bmj.j4090
summary of the results from the Rapid Recommendation process
-
Magic App (www.magicapp.org)
expanded version of the results with multilayered recommendations, evidence summaries, and decision aids for use on all devices
What is already known on this topic
Short course corticosteroids are one adjunct treatment option for relief of symptoms in patients with sore throat
Corticosteroids are not commonly prescribed as clinicians are uncertain about the balance of benefits and harms and the applicability of the evidence to patients with less severe disease
What this study adds
Moderate to high quality evidence suggests the addition of one (or two) dose(s) of corticosteroids reduces the intensity and duration of pain in patients with sore throat with no increase in serious adverse effects
The mean time to complete pain resolution was about 11 hours shorter with corticosteroids, and about 18% more patients experienced complete pain relief at 48 hours
There were no subgroup effects between patients consulting at the emergency departments or primary care family practice
Web Extra.
Extra material supplied by the author
Appendix 1: Search terms and strategies
Appendix 2: Summary of risk of bias assessments among the included trials
Appendix 3: Supplementary tables and figure
We thank Rachel Couban, librarian at McMaster National Pain Centre Research, for her advice on the search strategies and members of the Rapid Recommendations panel for critical feedback on outcome and subgroup selection and manuscript feedbacks.
Contributors: BS and RACS contributed equally to this work. TA, RACS, POV, and GHG conceived the study idea. BS, RACS, RB-P, TA coordinated the systematic review. BS, RACS, and TA wrote the first draft of the manuscript. BS and LL designed the search strategy. BS, RACS, LL, DP, and RB-P screened abstracts and full texts. BS, RACS, RB-P, and DP acquired the data and judged risk of bias in the studies. BS performed the data analysis and is guarantor. All authors interpreted the data analysis and critically revised the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing interests: All authors have completed the ICMJE uniform disclosure form and declare: no support from any organisation for the submitted work. RACS, AM, and GHG are members of the GRADE working group. There are no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required.
Data sharing: All data are freely available within the appendices. No additional data available.
Transparency: The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1.Pelucchi C, Grigoryan L, Galeone C, et al. ESCMID Sore Throat Guideline Group. Guideline for the management of acute sore throat. Clin Microbiol Infect 2012;18(Suppl 1):1-28. 10.1111/j.1469-0691.2012.03766.x. pmid:22432746. [DOI] [PubMed] [Google Scholar]
- 2.Principi N, Bianchini S, Baggi E, Esposito S. No evidence for the effectiveness of systemic corticosteroids in acute pharyngitis, community-acquired pneumonia and acute otitis media. Eur J Clin Microbiol Infect Dis 2013;32:151-60. 10.1007/s10096-012-1747-y. pmid:22993127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaikh N, Leonard E, Martin JM. Prevalence of streptococcal pharyngitis and streptococcal carriage in children: a meta-analysis. Pediatrics 2010;126:e557-64. 10.1542/peds.2009-2648. pmid:20696723. [DOI] [PubMed] [Google Scholar]
- 4.Herath VC, Carapetis J. Sore throat: Is it such a big deal anymore?J Infect 2015;71(Suppl 1):S101-5. 10.1016/j.jinf.2015.04.010. pmid:25917806. [DOI] [PubMed] [Google Scholar]
- 5.Kenealy T. Sore throat. BMJ Clin Evid 2011;2011:1509.pmid:21477389. [PMC free article] [PubMed] [Google Scholar]
- 6.Bally M, Dendukuri N, Rich B, et al. Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ 2017;357:j1909 10.1136/bmj.j1909. pmid:28487435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas M, Del Mar C, Glasziou P. How effective are treatments other than antibiotics for acute sore throat?Br J Gen Pract 2000;50:817-20.pmid:11127175. [PMC free article] [PubMed] [Google Scholar]
- 8.Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 2010;340:c2096 10.1136/bmj.c2096. pmid:20483949. [DOI] [PubMed] [Google Scholar]
- 9.Spinks A, Glasziou PP, Del Mar CB. Antibiotics for sore throat. Cochrane Database Syst Rev 2013;(11):CD000023 10.1002/14651858.CD000023.pub4. pmid:24190439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Driel ML, De Sutter A, Deveugele M, et al. Are sore throat patients who hope for antibiotics actually asking for pain relief?Ann Fam Med 2006;4:494-9. 10.1370/afm.609. pmid:17148626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayward G, Thompson M, Heneghan C, Perera R, Del Mar C, Glasziou P. Corticosteroids for pain relief in sore throat: systematic review and meta-analysis. BMJ 2009;339:b2976 10.1136/bmj.b2976. pmid:19661138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayward G, Thompson MJ, Perera R, Glasziou PP, Del Mar CB, Heneghan CJ. Corticosteroids as standalone or add-on treatment for sore throat. Cochrane Database Syst Rev 2012;10:CD008268 10.1002/14651858.CD008268.pub2. pmid:23076943. [DOI] [PubMed] [Google Scholar]
- 13.Korb K, Scherer M, Chenot JF. Steroids as adjuvant therapy for acute pharyngitis in ambulatory patients: a systematic review. Ann Fam Med 2010;8:58-63. 10.1370/afm.1038. pmid:20065280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wing A, Villa-Roel C, Yeh B, Eskin B, Buckingham J, Rowe BH. Effectiveness of corticosteroid treatment in acute pharyngitis: a systematic review of the literature. Acad Emerg Med 2010;17:476-83. 10.1111/j.1553-2712.2010.00723.x. pmid:20536799. [DOI] [PubMed] [Google Scholar]
- 15.Siemieniuk RA, Agoritsas T, Macdonald H, Guyatt GH, Brandt L, Vandvik PO. Introduction to BMJ Rapid Recommendations. BMJ 2016;354:i5191 10.1136/bmj.i5191. pmid:27680768. [DOI] [PubMed] [Google Scholar]
- 16.Hayward GN, Hay AD, Moore MV, et al. Effect of Oral Dexamethasone Without Immediate Antibiotics vs Placebo on Acute Sore Throat in Adults: A Randomized Clinical Trial. JAMA 2017;317:1535-43. 10.1001/jama.2017.3417. pmid:28418482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aertgeerts B, Agoritsas T, Siemieniuk RAC, et al. Corticosteroids for sore throat: a clinical practice guideline. BMJ 2017;358:j4090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JPT, Altman DG, Gøtzsche PC, et al. Cochrane Bias Methods Group Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928 10.1136/bmj.d5928. pmid:22008217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akl EA, Sun X, Busse JW, et al. Specific instructions for estimating unclearly reported blinding status in randomized trials were reliable and valid. J Clin Epidemiol 2012;65:262-7. 10.1016/j.jclinepi.2011.04.015. pmid:22200346. [DOI] [PubMed] [Google Scholar]
- 20.Guyatt GH, Oxman AD, Vist GE, et al. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. 10.1136/bmj.39489.470347.AD. pmid:18436948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003;326:219 10.1136/bmj.326.7382.219 pmid:12543843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002 10.1136/bmj.d4002 pmid:21784880. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien JF, Meade JL, Falk JL. Dexamethasone as adjuvant therapy for severe acute pharyngitis. Ann Emerg Med 1993;22:212-5. 10.1016/S0196-0644(05)80205-7 pmid:8427434. [DOI] [PubMed] [Google Scholar]
- 24.Marvez-Valls EG, Ernst AA, Gray J, Johnson WD. The role of betamethasone in the treatment of acute exudative pharyngitis. Acad Emerg Med 1998;5:567-72. 10.1111/j.1553-2712.1998.tb02462.x pmid:9660281. [DOI] [PubMed] [Google Scholar]
- 25.Wei JL, Kasperbauer JL, Weaver AL, Boggust AJ. Efficacy of single-dose dexamethasone as adjuvant therapy for acute pharyngitis. Laryngoscope 2002;112:87-93. 10.1097/00005537-200201000-00016. pmid:11802044. [DOI] [PubMed] [Google Scholar]
- 26.Ahn JH, Woo WK, Kim YS, et al. Efficacy of adjuvant short term oral steroid therapy for acute pharyngitis. Korean J Otolaryngol Head Neck Surg 2003;46:971-4. [Google Scholar]
- 27.Bulloch B, Kabani A, Tenenbein M. Oral dexamethasone for the treatment of pain in children with acute pharyngitis: a randomized, double-blind, placebo-controlled trial. Ann Emerg Med 2003;41:601-8. 10.1067/mem.2003.136. pmid:12712025. [DOI] [PubMed] [Google Scholar]
- 28.Olympia RP, Khine H, Avner JR. Effectiveness of oral dexamethasone in the treatment of moderate to severe pharyngitis in children. Arch Pediatr Adolesc Med 2005;159:278-82. 10.1001/archpedi.159.3.278. pmid:15753273. [DOI] [PubMed] [Google Scholar]
- 29.Niland ML, Bonsu BK, Nuss KE, Goodman DG. A pilot study of 1 versus 3 days of dexamethasone as add-on therapy in children with streptococcal pharyngitis. Pediatr Infect Dis J 2006;25:477-81. 10.1097/01.inf.0000219469.95772.3f. pmid:16732143. [DOI] [PubMed] [Google Scholar]
- 30.Tasar A, Yanturali S, Topacoglu H, Ersoy G, Unverir P, Sarikaya S. Clinical efficacy of dexamethasone for acute exudative pharyngitis. J Emerg Med 2008;35:363-7. 10.1016/j.jemermed.2007.11.029. pmid:18468831. [DOI] [PubMed] [Google Scholar]
- 31.Kiderman A, Yaphe J, Bregman J, Zemel T, Furst AL. Adjuvant prednisone therapy in pharyngitis: a randomised controlled trial from general practice. Br J Gen Pract 2005;55:218-21.pmid:15808038. [PMC free article] [PubMed] [Google Scholar]
- 32.Powell CV, Kelly AM, Williams A. Determining the minimum clinically significant difference in visual analog pain score for children. Ann Emerg Med 2001;37:28-31. 10.1067/mem.2001.111517. pmid:11145767. [DOI] [PubMed] [Google Scholar]
- 33.Alonso-Coello P, Carrasco-Labra A, Brignardello-Petersen R, et al. Systematic reviews experience major limitations in reporting absolute effects. J Clin Epidemiol 2016;72:16-26. 10.1016/j.jclinepi.2015.11.002. pmid:26560992. [DOI] [PubMed] [Google Scholar]
- 34.Sun X, Briel M, Walter SD, Guyatt GH. Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ 2010;340:c117 10.1136/bmj.c117. pmid:20354011. [DOI] [PubMed] [Google Scholar]
- 35.Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ 2017;357:j1415 10.1136/bmj.j1415. pmid:28404617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fernandes RM, Oleszczuk M, Woods CR, Rowe BH, Cates CJ, Hartling L. The Cochrane Library and safety of systemic corticosteroids for acute respiratory conditions in children: an overview of reviews. Evid Based Child Health 2014;9:733-47. 10.1002/ebch.1980. pmid:25236311. [DOI] [PubMed] [Google Scholar]
- 37.Management of sore throat and indications for tonsillectomy. A national clinical guideline. Scottish Intercollegiate Guideline Network (SIGN), April 2010. http://www.sign.ac.uk/assets/sign117.pdf
- 38.Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 2012;55:1279-82. 10.1093/cid/cis847. pmid:23091044. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Search terms and strategies
Appendix 2: Summary of risk of bias assessments among the included trials
Appendix 3: Supplementary tables and figure