Abstract
Background
Wellbeing is often described as U-shaped over the life course, suggesting an apparent paradox that wellbeing remains high at older ages despite increases in impairments.
Objective/Hypotheses
We explore associations among age, lower body impairments—one of the most common late-life impairments—and three measures of wellbeing: life satisfaction, emotional wellbeing and somatic wellbeing. We hypothesize that age effects are positive, become stronger once lower body impairments are controlled, and are concentrated among those who have maintained their mobility. Net of confounding factors, we hypothesize that lower body impairments are associated with worse wellbeing and these effects diminish with advancing age.
Methods
We analyze the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics (N=1,607 adults ages 60 and older). We estimate nested regression models that include age, severity of lower body impairments and confounding demographic, psychological, and socioeconomic factors and activities; test age-impairment interactions; and estimate age- and impairment-stratified models.
Results
Positive age effects were observed after controlling for lower body impairments for life satisfaction (β=0.90;p<.05), although statistical significance weakened (p=0.07) in fully adjusted models. For emotional wellbeing, adjusted age effects were negative (β=−0.05; p<.05) and were concentrated among those with limitations (β=−0.14;p<.01). For all three outcomes, severity of impairments reduced wellbeing in adjusted models. These effects were strongest for somatic wellbeing, especially for 65-to-74 year olds.
Conclusions
Our study challenges the notion that wellbeing is U-shaped throughout the life course and underscores the critical role of mobility across wellbeing domains in later life.
Keywords: Aging, Mobility, Wellbeing
INTRODUCTION
Lower body impairments that impede mobility are highly prevalent in the U.S., have become more common among adults in recent years, and increase with age (1). Such impairments encompass deficits in both strength and movement of the lower extremities that interrupt basic motor functions and often result from underlying musculoskeletal or neurological conditions. Having lower body impairments predicts the onset of activity limitations related to self-care and secondary health conditions as well as reduced survival (2–5). Maintaining mobility is also important for older adults’ continued engagement in social and productive activities that enrich daily life and contribute to psychological wellbeing (6).
Disablement frameworks, such as the International Classification of Functioning, Disability, and Health, recognize that impairments in functioning, as mediated by the environment and personal factors, are salient for activities and participation and that the disablement process may in turn influence one’s quality of life (7). Gerontological literature has linked late-life activity limitations to reduced wellbeing, where limitations are typically defined as needing help with basic activities of daily living (ADLs, such as bathing or dressing) and more complex instrumental activities (IADLs, such as making meals and shopping) (8). This relatively narrow focus on ADLs and IADLs has overshadowed recognition of the centrality to quality of life of earlier stages of the disablement process, such as the development of underlying impairments in lower body functioning. Lower body impairments are more prevalent than activity limitations, and their onset often occurs at earlier ages. Such impairments may disrupt participation in productive or leisure activities and thus may have far-reaching consequences for of older adults (9), particularly if disruption is frequent..
To understand how aging, mobility, and wellbeing intersect requires careful attention to the diverse conceptual and operational definitions of wellbeing. Self-assessed wellbeing (or “subjective wellbeing”) has traditionally been measured with questions about satisfaction with global and specific aspects of life, such as one’s health or family (10). These cognitive appraisals involve an assessment of one’s life relative to some standard, such as a peer group or one’s own condition earlier in life. Such measures are susceptible to response shift, in which individuals change the reference group used as their standard as they age (11), and to aging positivity bias, in which older adults selectively remember and appraise experiences in an overly positive light (12). Consistent with these measurement properties, several studies have found a U-shape in life satisfaction over the life course, with higher levels in young adulthood and later life (13–14).
Measures that focus on emotional and somatic experiences while carrying out daily activities have gained acceptance recently as a powerful means of describing wellbeing as it is experienced in daily life (15–17). These constructs differ from satisfaction because they are more fluid and sensitive to one’s immediate circumstance. Because the reference period is a specific activity on the previous day, experienced wellbeing measures may be less susceptible than evaluative measures to response shift and positivity bias (16). Developmental theory suggests that adults accumulate strategies as they age to maximize positive and minimize negative experiences (18) so that experienced wellbeing should increase with age. Research on somatic wellbeing is consistent with this persepctive: diary-based measures of fatigue decline with age and pain is relatively flat above age 60 (19–20). Empirical studies of emotions, however, suggest positive experiences peak in the late 60s or mid-70s before returning to pre-retirement levels (18,21). At least one study suggests that declines in functioning that commonly accompany aging mask increases in emotional wellbeing at older ages and thata positive age gradient emerges after functional status is controlled (22).
A limitation of existing studies is that they typically focus on either life satisfaction or experienced wellbeing, but not both. Hence, it is difficult to sort out if disparate findings reflect differences between evaluative appraisals and actual experiences or differences in study design features. Another limitation is that existing studies often control for only a subset of correlates of wellbeing (8, 15, 23). Ample research documents that psychological and socioeconomic resources and continued engagement in activities may be linked to the maintenance of wellbeing in later life (23). For instance, older individuals with high levels of self-efficacy, conscientiousness, and religiosity and lower levels of neuroticism report higher levels of wellbeing (24–25). Strained familial and marital relationships and limited economic resources also are associated with reduced wellbeing in later life (17, 26). Activity levels also have been linked to maintenance of wellbeing (27). Because psychological and socioeconomic resources and activities shift with age and with functional status, failure to control for these covariates may lead to an overstatement or misspecification of their associations with wellbeing.
Finally, the literature has rarely addressed the intersection between age and physical impairments and how these effects may differ by type of wellbeing (23). Because social networks and related activities often contract in later life, the negative effects of functional decline on subjective wellbeing—particularly emotional wellbeing—may diminish with advancing age. Likewise, wellbeing may improve with age for particular subpopulations, such as persons who are able to continue participation because they have maintained their functional status.
In this study, we examine the relationships among age, lower body impairments and subjective wellbeing in later life. We use a national sample of older adults from the Panel Study of Income Dynamics (PSID) to examine three distinct aspects of subjective wellbeing. Unlike prior studies, we examine both evaluative reports of life satisfaction and two types of experienced wellbeing—emotional and somatic wellbeing—obtained from time diary interviews. We focus on severity of lower body limitations, that is, the number of days in the last week on which lower body impairments limited daily activities. We also control for well-documented psychological, social, and economic correlates of wellbeing. To assess the main effects of age and lower body limitations on wellbeing, we estimate a series of regression models. We also conduct moderation analyses to evaluate whether the effects of limitations attenuate at older ages and whether positive age effects are limited to those who preserve their mobility.
METHODS
Data
Data are from the 2013 Disability and Use of Time (DUST) supplement to the 2013 PSID. The PSID began in 1968 with a sample of approximately 5,000 families, and is the longest running longitudinal study of a representative sample of families in the United States. The sample grows over time as adult children who form independent households become eligible sample members. Interviews have been conducted annually through 1997 and biennially thereafter. Re-interview rates were consistently 95% or higher through 2013, and the sample of families exceeded 9,000 in that year. With sampling weights, the design produces a nationally representative cross-section of families each year (28), and the survey offers a rich set of sociodemographic and economic measures.
The DUST supplement was administered to 2013 PSID household heads age 60 or older at the end of 2012 (born 1952 or earlier); in couple-headed households both individuals were eligible if either spouse/partner was age 60 or older. Each respondent was interviewed twice by telephone about one randomly selected weekday and one randomly selected weekend day. The response rate was 71.7% (1,217 households completed at least one interview out of 1,698 eligible households).
The DUST instrument included a 30 to 40 minute diary, and, during the first of two interviews, a 15 to 20 minute supplemental questionnaire (including items on personality, marital/romantic partner and family relationship quality). Respondents were systematically assigned interview days that would yield one weekday and one weekend diary, resulting in two diaries per respondent. The diary asked about all activities occurring on the previous day, beginning at 4 a.m. and continuing until 4 a.m. the morning of the interview. Respondents also reported how they felt, how tired they were, and how much pain they experienced while doing up to three activities randomly selected from their diaries, a validated approach known as the Day Reconstruction Method (29).
Overall, 1,776 respondents completed 3,505 diaries that included experienced wellbeing reports for 9,955 randomly selected activities. We excluded 167 spouses and partners younger than age 60 so that the sample represents individuals ages 60 and older. We excluded two additional respondents because of missing reports of experienced wellbeing. The final analytic sample included 1,607 respondents and 9,020 activities for which experienced wellbeing reports were provided.
Outcomes
Global life satisfaction was assessed at the beginning of the first interview with the question, “Taking all things together, how satisfied are you with your life these days?” Response categories range from 0 (not at all) to 6 (very).
Reports of experienced and somatic wellbeing come from the time diary portion of the interviews. After providing details of the previous 24-hour day, respondents were asked to report on a scale from 0 (not at all) to 6 (very strong) how intensely they felt five emotions (happy, calm, frustrated, worried, and sad) during three randomly selected activities. These discrete emotions are among the most commonly experienced by older adults (30). Using the same scale, respondents also indicated how tired they felt and how much pain they experienced during the activities.
To facilitate comparisons between satisfaction and diary-based measures of wellbeing, we scaled the diary-based measures at the respondent level. Lee and colleagues (31) evaluated this approach with the American Time Use Survey and concluded that a respondent-level construct was both reliable and valid. Following Lee et al., we explored whether consistent domains could be formed for each measurement period (morning, afternoon, and evening for the weekday and weekend day diaries) and for a respondent-level weekly measure (calculated as a weighted sum of the daily averages). Using principal components factor analysis, we found that the seven items consistently formed two factors, one representing emotions (happy, calm, and reverse coding of frustrated, worried, sad) and the other representing somatic experiences (reverse coding of pain, tired), with higher values representing greater wellbeing. For both respondent-level summary measures we found strong factors (loadings 0.59–0.78) and internal consistency (Cronbach’s α=0.86 for the five-item emotion scale and 0.70 for the two-item somatic scale). The two respondent-level measures were correlated moderately (emotional wellbeing M=5.2 SD=0.8; somatic wellbeing M=4.5 SD=1.3; r=0.5).
Lower body impairments and age
Respondents were asked during the DUST interview to report whether in the last seven days they had limited strength or movement in their hips, legs, knees, or feet and, if so, on how many days did these issues limit their activities. We created a severity measure that reflects the number of days an individual was limited by their lower body impairments; and, for model stratification purposes, a dichotomous measure that indicates whether a respondent reported having any days limited.
To establish the nature of the association between age and well-being, we examined the effects of age two ways. First, we explored both linear and quadratic forms to test whether age-effects accelerate with age (consistent with a U-shape through the end of the life course). In the quadratic models higher order (age-squared) terms were not significant, so we present linear age terms only. Second, to facilitate comparisons with stratified models, we grouped age into three categories of roughly equal size approximating pre-retirement, post-retirement and late retirement periods (e.g. ages 60–64, 65–74, and 75 and over).
Controls
Controls included demographic factors, psychological and socioeconomic resources, and recent participation in productive and leisure activities (see Table 1). Demographic factors include sex, race (black vs. non-black) and completed education (less than high school, high school graduate, more than high school). We also created an indicator of the duration of the underlying limiting condition by reviewing reports from the 1999 to 2013 core PSID interview about 12 chronic conditions and whether they limited the participant’s usual activities.
Table 1.
Characteristics of Adults Ages 60 and Older (n=1607)
| Weighted %/Mean (SD) | |
|---|---|
| Wellbeing | |
| Life satisfaction | 5.0 (1.1) |
| Emotional wellbeing | 5.2 (0.8) |
| Somatic wellbeing | 4.5 (1.3) |
| Limitations | |
| Has lower body limitation | 25.7 |
| Severity of lower body limitation (1–7)a | 4.3 (2.0) |
| Demographic Characteristics | |
| Age (mean years = 69.9; SD=7.9) | |
| 60–64 | 32.2 |
| 65–74 | 40.5 |
| 75+ | 27.3 |
| Female | 56.1 |
| Black (vs. non-Black) | 8.5 |
| Education | |
| Less than 12 years | 10.0 |
| 12 years | 29.6 |
| More than 12 years | 60.4 |
| Duration limiting chronic conditions (mean years) | 2.3 (4.5) |
| Psychological Resources (mean) | |
| Neuroticism (0–3) | 1.2 (0.7) |
| Extroversion (0–3) | 1.9 (0.7) |
| Conscientiousness (0–3) | 2.4 (0.6) |
| Spirituality (0–3) | 2.2 (0.9) |
| Self-efficacy (0–5) | 3.3 (1.4) |
| Social Resources | |
| Currently married (vs. not) | 64.2 |
| Number in household | 2.1 (1.0) |
| Mean marital/romantic relationship quality (0–4)b | 3.0 (0.3) |
| Mean family relationship quality (0–4) | 3.3 (0.6) |
| Economic Resources | |
| Median income 2012 ($ thousands) | 55.4 |
| Median wealth 2013 ($10 thousands) | 21.9 |
| Time Use Last 7 Days (mean days on which activity was performed) | |
| Work | 1.3 (2.3) |
| Volunteer | 0.5 (1.1) |
| Provide care | 0.4 (0.8) |
| Household tasks | 2.2 (1.3) |
| Manging finances | 1.4 (1.3) |
| Household repairs or improvements | 0.9 (1.4) |
| Leisure activities | 2.3 (1.4) |
Mean number of days lower body problem limited activities in the last 7 days among respondents with limitation.
Among respondents who are married or in a romantic relationship
Source: Authors’ analysis of the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics.
Psychological resources included measures of personality, spirituality and self-efficacy. Personality was measured using a five-domain instrument (32). For the three domains with the strongest relationship to health in later life—extraversion, neuroticism, and conscientiousness—we created scales by averaging items, with higher scores indicating a greater degree of the trait (alphas ranged from 0.54 to 0.66). Spirituality (α = 0.88) was measured with a standard scale assessing the strength and influence of religious beliefs (33) and self-efficacy (α =0.53) with a five-item scale (34).
Social resources included household size, marital status (married or partnered vs. not) and measures of marital/romantic relationship quality and family relationship quality (α = 0.80 and 0.47, respectively) derived from standardized instruments (35). We measured economic resources with 2012 family income and 2013 family wealth, which were available from the 2013 PSID family interview. Family income includes taxable income and cash transfers received by adult family members. Family wealth includes nine broad asset and liability categories including home equity (36). The two measures were moderately correlated (r=0.54).
Finally, we controlled for participation in productive and leisure activities. Respondents reported on how many of the last seven days they carried out 12 different activities. Based on a factor analysis, we combined activities into broader domains by averaging the number of days reported across activities within each domain. The final categories were work, volunteering, child or adult care, household chores, home repairs or improvements, managing finances, and leisure activities.
Analysis
We conducted t-tests to evaluate differences in mean emotional and somatic wellbeing scores by age and the presence of limiting lower body conditions. We then ran a series of linear regression models to test our hypotheses that positive age effects would strengthen once lower body impairments were controlled and that net of confounding factors, lower body impairments would be associated with worse wellbeing. The baseline model included age only (to assess unadjusted positivity effects). A second model included both age and severity of lower body impairments. Final main effects models incorporated duration of the limiting condition and demographic, psychological, social, and economic factors. We also ran a series of diagnostic tests to confirm that assumptions for linear regression were met.
To test moderation effects (e.g. mobility limitation effects dampen with advancing age; age effects are stronger among those without impaired mobility) we first added interactions between age and severity to the final main effects models. Next, to relax the assumption that covariates have the same effect by age group and impairment status, we estimated stratified models. We stratified models by age (60–64, 65–74, 75+) to test the hypothesis that lower body impairment effects are more muted with age. We then stratified models by the presence of a limiting lower body impairment to test whether age effects are concentrated among those maintaining lower body functioning. We used a Wald test to determine whether the effects of the key variable of interest (e.g. lower body impairments or age) differed across models. All analyses were run in Stata 14.0 with sampling weights and adjustments for the PSID and DUST sample designs (36–37).
RESULTS
Descriptive analysis
One in four older adults report a limiting lower body limitation; among those reporting a limitation, respondents report interference with activities on an average 4.3 out of the last 7 days (see Table 1).
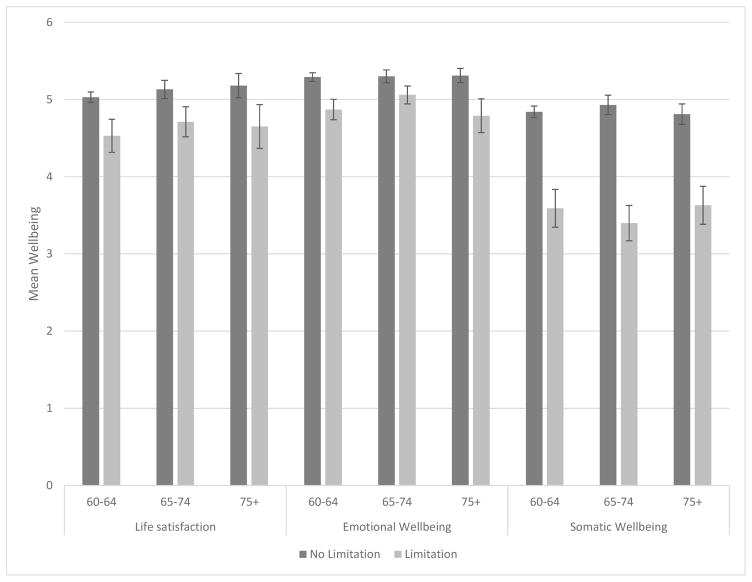
For life satisfaction only, wellbeing is higher among individuals ages 65–74 compared with those of pre-retirement age (60–64) (Figure 1; p < .05). No age differences are detected for emotional or somatic wellbeing. In contrast, for all three outcomes, wellbeing is worse for individuals with lower body limitations compared with individuals without such limitations, and these differences hold across all three age groups (p < .05). Differences in life satisfaction between those with and without lower body limitations range from 0.4 to 0.5 (roughly one-half SD), depending on the age group. For emotional wellbeing, differences range from 0.2 to 0.5 (one half to three-quarters SD). For somatic welling, differences are larger, ranging from 1.2 to 1.5 across age groups (about nine-tenths to over one SD).
Figure 1.
Mean (95% Confidence Interval) Life Satisfaction and Emotional and Somatic Wellbeing by Age Group and Presence of Limiting Lower Body Impairments: Population Ages 60 and Older
Source: Authors’ analysis of the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics.
Multivariate Analysis
In models including only continuous age (Table 2; Models 1A), age is not significantly associated with any of the three outcomes. Using the categorical measure of age (Models 1B), life satisfaction is higher among those ages 65–74 and ages 75 and older (vs. 60–64), but only the coefficient for the 65–74 age category reaches statistical significance. We do not detect significant age differences for either emotional or somatic wellbeing.
Table 2.
Effects of Limiting Lower Body Problems and Age on Wellbeing: Coefficients from Linear Regression Models (n=1607)
| Life Satisfaction (0–6)
|
Emotional Wellbeing (0–6)
|
Somatic Wellbeing (0–6)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Only Model (1) | Age and Severity Model (2) | Fully Adjusted Model (3)a | Age Only Model (1) | Age and Severity Model (2) | Fully Adjusted Model (3)a | Age Only Model (1) | Age and Severity Model (2) | Fully Adjusted Model (3)a | |
| Model A: Continuous age | |||||||||
| Severity of lower body limitation | −0.11** | −0.05** | −0.08** | −0.05** | −0.27** | −0.19**^ | |||
| Age (reported age/10) | 0.07 | 0.09* | 0.09 | −0.02 | −0.01 | −0.05*^ | −0.07 | −0.02 | 0.02 |
| Model B: Categorical age | |||||||||
| Severity of lower body limitation | −0.11** | −0.05** | −0.08** | −0.05** | −0.27** | −0.19**^ | |||
| Age (60–64 omitted) | |||||||||
| 65–74 | 0.11* | 0.12* | 0.04 | 0.05 | 0.06 | 0.00 | 0.01 | 0.03 | 0.05 |
| 75+ | 0.11 | 0.15 | 0.11 | −0.03 | −0.00 | −0.08 | −0.09 | 0.02 | 0.09 |
p < 0.01,
p < 0.05;
coefficient significantly (p < 0.05) differs from coefficient in fully adjusted life satisfaction model
Fully Adjusted Model includes all control variables in Table 1. Full models presented in Supplemental Table 1.
Source: Authors’ analysis of the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics
Adding severity of lower body limitations to the models (Models 2A and 2B) strengthens the relationship between age and life satisfaction, but does not alter conclusions about the lack of relationship between age and emotional or somatic wellbeing. Severity of lower body limitations is inversely related to all three outcomes; the strongest relationship is with somatic wellbeing (β=−0.27 p<.01 in Models 2A and 2B).
After controlling for additional confounders, the significance of the association between age and life satisfaction weakens (e.g. p=.07 in Model 3A) and there continues to be no association between age and somatic wellbeing. However, a negative effect of age on emotional wellbeing emerges using the continuous age specification (β=−0.05; p<.01). Severity of lower body limitations continues to be inversely related to all three outcomes. Although coefficients are attenuated relative to the unadjusted models, the relationship with somatic wellbeing remains strong (β=−0.19 p<.01).
Interactions between severity of lower body limitation and age are not statistically significant with one exception (Table 3; Models 4A and 4B). In the model with categorical age measures (Model B), the negative effect of lower body limitations is more pronounced among those ages 65 to 74 (vs. ages 60–64).
Table 3.
Effects of Limiting Lower Body Problems and Age on Wellbeing: Adjusted Linear Regression Models (n=1607)
| Life Satisfaction (0–6) | Emotional Wellbeing (0–6) | Somatic Wellbeing (0–6) | ||||
|---|---|---|---|---|---|---|
| Main Effects (3) | With Interactions (4) | Main Effects (3) | With Interactions (4) | Main Effects (3) | With Interactions (4) | |
|
| ||||||
| Model A: Continuous age | ||||||
| Severity of lower body limitation | −0.05** | −0.11 | −0.05** | 0.04 | −0.19** | −0.32* |
| Age (reported age/10) | 0.09 | 0.08 | −0.05* | −0.03 | 0.02 | −0.00 |
| Severity * Age | 0.01 | −0.01 | 0.02 | |||
| Model B: Categorical age | ||||||
| Severity of lower body limitation | −0.05** | −0.04 | −0.05** | −0.04* | −0.19** | −0.16** |
| Age (60–64 omitted) | ||||||
| 65–74 | 0.04 | 0.08 | 0.00 | −0.01 | 0.05 | 0.14* |
| 75+ | 0.11 | 0.11 | −0.08 | −0.05 | 0.09 | 0.06 |
| Severity * 65–74 | −0.03 | 0.01 | −0.09* | |||
| Severity * 75+ | −0.01 | −0.02 | 0.01 | |||
p < 0.01,
p < 0.05;
coefficient significantly (p < 0.05) differs from coefficient in fully adjusted life satisfaction model
Models include all control variables in Table 1.
Source: Authors’ analysis of the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics
This latter finding also is evident from models stratified by age (Table 4). Each one point increase on the lower body limitation severity scale reduces somatic wellbeing by one-quarter point; and this amount is significantly different from the coefficients for 60–64 year olds and for those ages 75 and older.
Table 4.
Effects of Severity of Lower Body Limitations on Wellbeing by Age Group: Coefficients from Stratified Linear Regression Modelsa
| Life Satisfaction (0–6) | Emotional Wellbeing (0–6) | Somatic Wellbeing (0–6) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 60–64 | 65–74 | 75+ | 60–64 | 65–74 | 75+ | 60–64 | 65–74 | 75+ | |
|
| |||||||||
| Severity of lower body limitations | −0.03 | −0.06** | −0.05 | −0.05** | −0.04* | −0.07** | −0.16** | −0.25**^ | −0.14** |
p < 0.01,
p < 0.05;
Coefficient significantly (p < .05) differs from coefficient for 60–64 and 75+ year olds.
Model includes all controls in Table 1.
Source: Authors’ analysis of the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics
As shown in Table 5, the negative relationship between age and emotional wellbeing is limited to those with a lower body limitation. That is, contrary to our hypothesis that a positive age gradient would be evident among those with preserved functioning, we found that aging has a negative influence on emotional wellbeing but only for those with a lower body limitation.
Table 5.
Effects of Age on Wellbeing by Lower Body Limitations: Coefficients from Stratified Linear Regression Modelsa
|
|
||||||
|---|---|---|---|---|---|---|
| Life Satisfaction (0–6) | Emotional Wellbeing (0–6) | Somatic Wellbeing (0–6) | ||||
|
| ||||||
| No limitation | Has Limitation | No limitation | Has Limitation | No limitation | Has Limitation | |
|
| ||||||
| Model A: Continuous age | ||||||
| Age (reported age/10) | 0.09 | 0.09 | −0.02 | −0.14** | 0.00 | 0.06 |
| Model B: Categorical age | ||||||
| Age 65–74 (vs. age 60–64) | 0.06 | 0.03 | −0.01 | 0.01 | 0.11 | −0.16 |
| Age 75 and over | 0.12 | 0.03 | −0.02 | −0.28**^ | 0.05 | 0.10 |
p < 0.01,
p < 0.05;
Coefficient significantly (p < 0.05) differs from coefficient for individuals with no limitations
Model includes all controls in Table 1.
Source: Authors’ analysis of the 2013 Disability and Use of Time supplement to the Panel Study of Income Dynamics
DISCUSSION
This study explored the relationships among age, lower body limitations, and three measures of wellbeing in a national sample of older adults in the US. We documented a positive age gradient with life satisfaction, but not with emotional or somatic wellbeing. These descriptive patterns are consistent with prior studies showing that life satisfaction remains high and even increases with age, that emotional wellbeing declines above age 75, and that pain has no age gradient in later life (13–14, 18, 21–22). Findings differ, however, from studies suggesting that fatigue declines with age (19–20). Although we cannot pinpoint the reason for this discrepancy, in sensitivity analyses (not shown) we found patterns for fatigue mirrored those for somatic wellbeing, which suggests that it does not stem from combining pain and fatigue into one measure.
Moderation analyses further revealed a negative association between age and emotional wellbeing that was concentrated among those living with mobility impairments. Why age effects differ for those with and without lower body limitations is unclear. It may be that for individuals whose lower body limitations disrupt their daily activities, age represents negative, repeated messages of being unable to continue one’s usual routine rather than positive opportunities to accumulate strategies to facilitate participation. We also found that interference of lower body impairments with daily activities was consequential for both evaluative and experienced well-being, with more sizeable effects for somatic components of well-being. Contrary to our expectations that these effects would diminish with age, we found a more complex pattern: negative effects of lower body limitations on somatic wellbeing peaked in the 65- to-74 age range. We speculate that in this age range there is a mismatch between activities and abilities that results in elevated pain and fatigue levels. More detailed controls for activity type, duration or intensity may be needed to uncover the reason for this finding.
Our analysis has several limitations. First, we were unable to examine whether the onset of impairments leads to a change in reports of experienced or somatic wellbeing. Others have pointed out the potentially bi-directional relationship between health and wellbeing (15); not only do impairments lead to worse emotional wellbeing, but maintenance of wellbeing may have a protective role in stemming the progression of disease into impairments and related limitations as well as mortality. Nevertheless, our results were robust net of the duration of the underlying condition giving rise to limitations, and to selected psychological mechanisms that may link wellbeing to underlying health. Second, individuals living in institutional settings and those with substantial cognitive or hearing impairments are excluded from the DUST sample. Whether this omission has substantially biased the coefficients of interest is not clear; if these groups have worse experienced wellbeing than those in the study, our findings are likely biased toward the null. Third, we did not explore whether linkages among age, lower body limitations and well-being differ by sex, race or other personal characteristics; extensions along these lines would be a fruitful next step.
Despite these limitations, our study contributes to the literature on aging, disability and wellbeing in late life. Our findings expand the literature on the consequences of mobility impairments, by underscoring consequences for both evaluative and experienced wellbeing. We also extend gerontological research linking disability and wellbeing by featuring measures of lower body limitations. Our findings also complement studies that challenge the notion that wellbeing is uniformly u-shaped throughout the life course. Instead, we find that the age-wellbeing relationship depends both on the domain of wellbeing considered and on the presence of impairments that limit activities, which may render the aging process particularly challenging for some individuals.
Our study is also the first we know of to explore linkages between lower body impairment and daily experiences of pain and fatigue. Pain, which affects an estimated one-third of all Americans, raises the risk of morbidity, disability, and mortality and places substantial demands on the health care system (38). Fatigue also is a common complaint among older adults, yet is often underdetected and undertreated (39). Our results suggest that “young old” adults (ages 65 to 74) are particularly vulnerable to daily pain and fatigue in the face of lower body limitations. These results called for heightened awareness, treatment and accommodation among older adults experiencing lower body limitations relatively early in the aging process.
Our findings also have implications for understanding more fully the consequences of disability in the context of an aging society. The number of older adults in the US will increase markedly in the near future, as the large cohort of individuals born in the latter years of the baby boom generation continue to age. Although population aging alone is unlikely to drive large changes in wellbeing at the population level, current cohorts approaching late life have experienced an increase in the prevalence of lower body limitations relative to earlier cohorts (1), so that more adults will reach retirement age in the near future with mobility impairments already in place. Increasing rates of obesity among recent cohorts of midlife and older adults could further contribute to the increase in these limitations, and musculoskeletal conditions are increasingly cited as causes of limitation (1). Our findings suggest these health trends could have measurable consequences for the wellbeing of older adults, in terms of life satisfaction, daily emotions, and pain and fatigue levels.
Finally, our findings have implications for efforts to monitor the wellbeing of the US population, including older adults. Experienced wellbeing measures are not typically included in such tracking efforts. However, scientists have noted growing interest in adding subjective wellbeing measures to existing health monitoring systems, with the aim of enhancing policy relevant information (40). One concrete example of this interest is the addition of experienced wellbeing measures to several waves of the American Time Use Survey, although health and disability measures in that study are relatively limited. Our findings suggest that monitoring health and experienced wellbeing together periodically may be an effective strategy for documenting more fully the consequences of shifts in health and functioning for America’s aging population.
Supplementary Material
Acknowledgments
This work was supported by the National Institute on Aging of the National Institutes of Health (grant number P01AG029409). The views expressed are those of the authors alone and do not represent the views of their employers or the funding agency.
Footnotes
Findings to be presented at the annual meeting of the Population Association of America, April 25–28, 2016, Chicago, IL.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Vicki A. Freedman, Institute for Social Research, University of Michigan, Ann Arbor, MI
Deborah Carr, Department of Sociology, Rutgers University, New Brunswick, NJ
Jennifer C. Cornman, Jennifer Cornman Consulting, Granville, OH
Richard E. Lucas, Department of Psychology, Michigan State University, E. Lansing, MI
References
- 1.Martin LG, Schoeni RF. Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disabil Health J. 2014;7:S4–S14. doi: 10.1016/j.dhjo.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper R, Kuh D, Hardy R Mortality Review Group; FALCon and HALCyon Study Teams. Objectively measured physical capability levels and mortality: systematic review and meta-analysis. BMJ. 2010;341:c4467. doi: 10.1136/bmj.c446714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper R, Kuh D, Cooper C, et al. FALCon and HALCyon Study Teams. Objective measures of physical capability and subsequent health: a systematic review. Age Ageing. 2011;40:14–23. doi: 10.1093/ageing/afq11715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrucci L, Cooper R, Shardell M, Simonsick EM, Schrack JA, Kuh D. Age-Related Change in Mobility: Perspectives From Life Course Epidemiology and Geroscience. J Gerontol A Biol Sci Med Sci. 2016 Sep;71(9):1184–94. doi: 10.1093/gerona/glw043. Epub 2016 Mar 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satariano WA, Guralnik JM, Jackson RJ, Marottoli RA, Phelan EA, Prohaska TR. Mobility and aging: new directions for public health action. Am J Public Health. 2012;102(8):1508–15. doi: 10.2105/AJPH.2011.300631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine. The Future of Disability in America. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 8.Pinquart M, Sorensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: A meta-analysis. Psychology and Aging. 2000;15:187–224. doi: 10.1037//0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- 9.Oerlemans WG, Bakker AB, Veenhoven R. Finding the key to happy aging: a day reconstruction study of happiness. J Gerontol B Psychol Sci Soc Sci. 2011;66(6):665–74. doi: 10.1093/geronb/gbr040. Epub 2011 Jul 1. [DOI] [PubMed] [Google Scholar]
- 10.Campbell A, Converse PE, Rodgers WL. The Quality of American Life. New York: Russell Sage Foundation; 1976. [Google Scholar]
- 11.Wilson I. Clinical understanding and clinical implications of response shift. Soc Sci Med. 1999;48:1577–88. doi: 10.1016/s0277-9536(99)00050-7. [DOI] [PubMed] [Google Scholar]
- 12.Reed AE, Carstensen LL. The theory behind the age-related positivity effect. Frontiers in Psychology. 2012;3:339. doi: 10.3389/fpsyg.2012.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Social Science and Medicine. 2008;66:1733–49. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 14.Frijters P, Beatton T. The mystery of the U-shaped relationship between happiness and age. Journal of Economic Behavior & Organization. 2012;82:525–542. doi: 10.1016/j.jebo.2012.03.008. [DOI] [Google Scholar]
- 15.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385:640–8. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Research Council. Subjective Well-Being: Measuring Happiness, Suffering, and Other Dimensions of Experience. Washington DC: National Academies of Sciences Press; 2013. [PubMed] [Google Scholar]
- 17.Kahneman D, Krueger AB, Schkade D, Schwarz N, Stone AA. Would you be happier if you were richer? A focusing illusion. Science. 2006;312:1908–10. doi: 10.1126/science.1129688. [DOI] [PubMed] [Google Scholar]
- 18.Carstensen LL, Turan B, Scheibe S, et al. Emotional Experience Improves With Age: Evidence Based on Over 10 Years of Experience Sampling. Psychology and Aging. 2011;26(1):21–33. doi: 10.1037/a0021285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dolan P, Kudrna L. More years, less yawns: fresh evidence on tiredness by age and other factors. J Gerontol B-Psychol. 2015;70:576–80. doi: 10.1093/geronb/gbt118. [DOI] [PubMed] [Google Scholar]
- 20.Schneider S, Stone AA. Distinguishing between frequency and intensity of health-related symptoms from diary assessments. J Psychosom Res. 2014;77:205–12. doi: 10.1016/j.jpsychores.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone AA, Schwartz JE, Broderick JE, Deaton AA. A snapshot of the age distribution of psychological well-being in the United States. Proceedings of the National Academy of Sciences USA. 2010;107:9985–90. doi: 10.1073/pnas.1003744107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kunzmann U, Little TD, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychol Aging. 2000 Sep;15(3):511–26. doi: 10.1037//0882-7974.15.3.511. [DOI] [PubMed] [Google Scholar]
- 23.George L. Still Happy After All These Years. Journals of Gerontology: Psychological Sciences. 2010;65B:331–339. doi: 10.1093/geronb/gbq006. [DOI] [PubMed] [Google Scholar]
- 24.Steel P, Schmidt J, Shultz J. Refining the relationship between personality and subjective well-being. Psychological Bulletin. 2008;134:138–161. doi: 10.1037/0033-2909.134.1.138. [DOI] [PubMed] [Google Scholar]
- 25.Diener E, Tay L, Myers DG. The religion paradox: If religion makes people happy, why are so many dropping out? Journal of Personality and Social Psychology. 2011;101:1278–1290. doi: 10.1037/a0024402. [DOI] [PubMed] [Google Scholar]
- 26.Proulx CM, Helms HM, Buehler C. Marital quality and personal well-being: a meta-analysis. Journal of Marriage and Family. 2007;69:576–593. doi: 10.1111/j.1741-3737.2007.00393.x. [DOI] [Google Scholar]
- 27.Menec VH. The relation between everyday activities and successful aging: a 6-year longitudinal study. J Gerontol B Psychol Sci Soc Sci. 2003 Mar;58(2):S74–82. doi: 10.1093/geronb/58.2.s74. [DOI] [PubMed] [Google Scholar]
- 28.McGonagle KA, Schoeni RF, Sastry N, Freedman VA. The Panel Study of Income Dynamics: Overview, recent innovations, and potential for life course research. Longitud Life Course Stud. 2012;3:268–284. doi: 10.14301/llcs.v3i2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kahneman D, Krueger AB, Schkade D, Schwarz N, Stone AA. A survey method for characterizing daily life experience: The Day Reconstruction Method (DRM) Science. 2004;306:1776–1780. doi: 10.1126/science.1103572. [DOI] [PubMed] [Google Scholar]
- 30.Chipperfield JG, Perry RP, Weiner B. Discrete emotions in later life. J Gerontol. 2003;58:P23–P34. doi: 10.1093/geronb/58.1.p23. [DOI] [PubMed] [Google Scholar]
- 31.Lee Y, Hofferth SL, Flood SM, Fisher K. Reliability, validity, and variability of the subjective well-being questions in the 2010 American Time Use Survey. Soc Indic Res. 2016;126:1355–1373. doi: 10.1007/s11205-015-0923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gerlitz Y, Schupp J. German Institute of Economic Research (Research Notes 4) Berlin: DIW; 2005. Assessment of big five personality characteristics in the SOEP. [Google Scholar]
- 33.Fetzer Institute / National Institute on Aging Working Group. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research. Kalamazoo, MI: Fetzer Institute; 2003. [Google Scholar]
- 34.Converse PE, Dotson JD, Hoag WJ, McGee WH. American Social Attitudes Data Source Book, 1947–1978. Boston, MA: Harvard University Press; 1980. [Google Scholar]
- 35.Whalen HR, Lachman ME. Social support and strain from partner, family and friends: costs and benefits for men and women in adulthood. J Soc Pers Relat. 2000;17:5–30. [Google Scholar]
- 36.Panel Study of Income Dynamics. PSID Main Interview User Manual: Release 2015. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2015. [Google Scholar]
- 37.Freedman VA, Cornman JC. [Accessed October 19, 2016];The Panel Study of Income Dynamics Second Supplement on Disability and Use of Time User Guide. Available at http://psidonline.isr.umich.edu/DUST/dust13_UserGuide.pdf.
- 38.Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 39.Yu DSF, Lee DT, Man NW. Fatigue among older people: A review of the research literature. Int J Nurs Stud. 2010;47:216–28. doi: 10.1016/j.ijnurstu.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 40.Diener E. New findings and future directions for subjective well-being research. Am Psychol. 2012;67:590–597. doi: 10.1037/a0029541. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.