Abstract
Purpose
To determine the association between maternal exposure to childhood maltreatment (CM) and risk of stillbirth (≥ 20 weeks’ gestation).
Methods
Population-based case-control study from the Stillbirth Collaborative Research Network (SCRN) conducted in 2006–2008, and the follow-up study, SCRN-Outcomes after Study Index Stillbirth (SCRN-OASIS), conducted in 2009 in the United States. Cases (n = 133) included women who experienced a stillbirth, excluding stillbirths attributed to genetic/structural or umbilical cord abnormalities and intrapartum stillbirths. Controls (n = 500) included women delivering a healthy term live birth (excluding births <37 weeks gestation, neonatal intensive care unit admission, or death). CM exposure was measured using the Childhood Trauma Questionnaire, administered during the SCRN-OASIS study. Dichotomized scores for five subscales of CM (physical abuse, physical neglect, emotional abuse, emotional neglect, and sexual abuse) and an overall measure of CM exposure were analyzed using logistic regression.
Results
Generally, there was no association between CM and stillbirth, except for the emotional neglect subscale (OR: 1.93; 95% CI: 1.17, 3.19).
Conclusions
Childhood neglect is understudied in comparison to abuse and should be included in future studies of associations between CM and pregnancy outcomes, including stillbirth.
Keywords: African Americans, adult survivors of childhood trauma, child abuse and neglect, child maltreatment, stillbirth, stress, trauma
Introduction
Approximately 1 in 160 pregnancies ends in stillbirth in the United States, defined as a fetal death at or after 20 weeks’ gestation.1 The rate of stillbirth has plateaued in recent years, particularly for early stillbirths.1 While some clinical risk factors for stillbirth have been identified, including some pregnancy disorders, obesity, and maternal age, relatively little research has focused on psychosocial determinants of stillbirth, particularly those which encompass early life adversity.2 Childhood maltreatment (CM), defined as sexual, physical, or emotional abuse and/or neglect in childhood, is a prevalent stressor that has been associated with several health outcomes, such as hypertension, chronic pain, ischemic heart disease, and autoimmune diseases later in life.3–6 A growing number of studies have found that childhood sexual abuse, a component of CM, is associated with increased risk of adverse pregnancy outcomes, including preterm labor and preterm birth.7–12 However, few investigators have examined the relationship between CM and stillbirth.
CM may increase the risk for stillbirth via stress-related pathways in a manner similar to significant life events, which have been associated with stillbirth.13–16 For example, stress is linked to preeclampsia and placental abnormalities, which are risk factors for stillbirth.17, 18 Also, stress-related risky behaviors such as unhealthy coping devices, including overeating, smoking, and alcohol abuse, are associated with CM.19, 20 These coping devices increase the risk of adverse health outcomes, such as obesity, depression, and hypertension, which have been associated with adverse pregnancy outcomes, including stillbirth.19, 21–23 Additionally, CM is associated with common reproductive tract infections such as bacterial vaginosis and unsafe sexual practices that increase the risk of sexually transmitted infections, such as chlamydia, gonorrhea, and syphilis, which have also been associated with stillbirth.24–31
As previously reported, non-Hispanic black women may have a higher prevalence of CM and they experience a disproportionate burden of stillbirth, with a rate two times that of non-Hispanic white women.1, 14, 32 If CM increases the risk of adverse pregnancy outcomes, the potentially higher prevalence of CM among non-Hispanic black women may explain some of the disproportionate burden of stillbirth among these women. Similarly, among Hispanic women, acculturation is associated with both CM and adverse pregnancy outcomes and the relationship between CM and stillbirth may differ depending on level of acculturation.33–36 A better understanding of life course stressors that may drive racial and ethnic disparities has been identified as a priority research area for perinatal outcomes, including stillbirth.37
This study tests the hypothesis that history of exposure to CM is associated with stillbirth. In addition, we assess whether different types of CM (physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect) have different associations with stillbirth, and if this varies with respect to race/ethnicity and acculturation.
Materials and Methods
The Stillbirth Collaborative Research Network’s (SCRN) population-based case-control study and the SCRN-Outcomes after Study Index Stillbirth (SCRN-OASIS) study were conducted from 2006 – 2009. SCRN enrollment occurred between March 2006 and September 2008 from 59 hospitals representing five catchment areas of the United States: Rhode Island and counties in Massachusetts, Georgia, Texas, and Utah. Investigators chose hospitals to obtain a sample of at least 90% of all deliveries to residents in each area. The final cohort included 663 women with a stillbirth (cases) and 1,932 women with a live birth (controls) selected through a stratified random method.38 The study was approved by the Institutional Review Board at each study site. In 2009, women who had consented to future contact in SCRN and could be reached for follow-up underwent an extensive telephone interview in English or in Spanish between six months and three years after the index delivery.16 CM was assessed during this SCRN-OASIS interview using the Childhood Trauma Questionnaire (CTQ), a 28-item self-report that yields scores for five subscales: physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect, and a 3-item minimization/denial score.39, 40 The CTQ has been translated to Spanish, used in diverse populations, and administered over the telephone.41–44
For this analysis, we excluded multiple gestations, stillbirths attributed to genetic/structural or umbilical cord abnormalities, and intrapartum stillbirths because they are unlikely to cause CM-related stillbirth via a stress-related pathway and intrapartum stillbirths may instead reflect quality and timing of care.45 Controls excluded infants with a gestational age <37 weeks, those admitted to a neonatal intensive care unit, and those who died since they represent adverse outcomes that may be affected by CM.46 We also excluded individuals with a missing CTQ. Individuals missing ≥2 responses on a subscale were excluded from analysis of that scale. We imputed missing values for individuals missing one question on a subscale by using the average of the subscale. Our final sample included 133 stillbirths and 500 healthy term live births (Figure 1).
Figure 1.
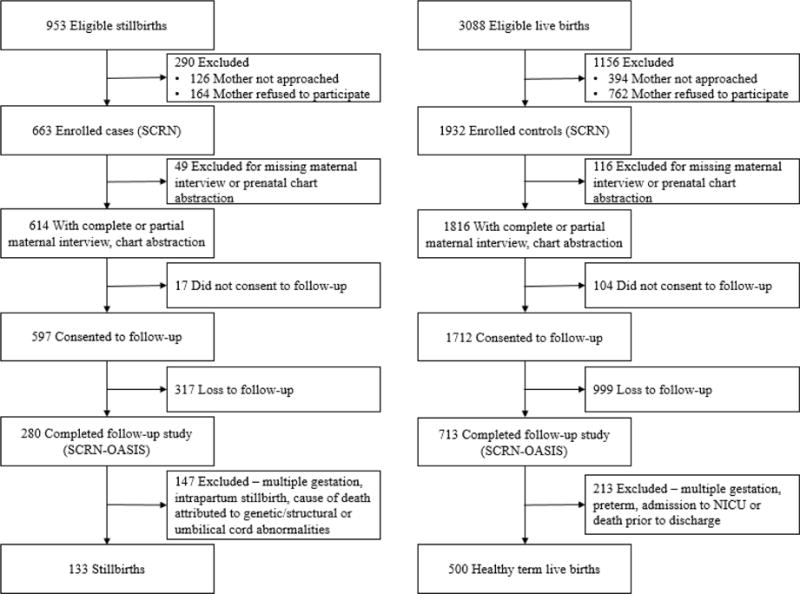
Study enrollment and inclusion.
Abbreviations: SCRN, Stillbirth Collaborative Research Network; SCRN-OASIS, SCRN Outcomes after Study Index Stillbirth
The SCRN study design requires a weighted analysis to account for differential consent, determined from characteristics documented for all eligible, screened deliveries, and sampling methods.38 Due to substantial loss to follow-up in the SCRN-OASIS study (53% in cases, 58% in controls), the SCRN weights could not be directly applied to this population (Figure 1). To adjust for loss to follow-up and to apply the SCRN study weights, we calculated a stabilized inverse probability weight to relate the SCRN-OASIS study population to the SCRN population. For this weight, we used factors related to participation in SCRN-OASIS (case/control status, maternal race/ethnicity, maternal education, maternal smoking status, insurance, and study site). We multiplied the stabilized inverse probability weight by the original study weight. This product was then multiplied by a separate constant for cases and controls so that the sum of the weights in each group was the same as in the original SCRN study.
Based on scoring guidelines, CM subscale scores CM were categorized as none to minimal, low to moderate, moderate to severe, and severe to extreme.39 Because CM is a sensitive topic and some research suggests that participants may be less comfortable disclosing such topics via a telephone interview, we chose the most sensitive cut point to dichotomize the exposure variable, comparing the “none to minimal” category to a combined category reflecting “low to extreme” exposure.47, 48 We also calculated a summary variable of overall CM exposure (any vs. none) using these dichotomous values.
We evaluated differences in covariates, including hypothesized mediators, and types of CM, between stillbirths and live births using Rao-Scott chi-square tests (Figure S1). In order to evaluate differential social determinants of stress experienced by non-Hispanic white women, non-Hispanic black women, and Hispanic women, we evaluated the distribution of CM stratified by race/ethnicity. Within the Hispanic group, we further stratified by language of the follow-up interview as a proxy for acculturation.
We used logistic regression models to assess the associations between types of CM and stillbirth in the total and stratified populations. We evaluated maternal education, as a proxy for childhood socioeconomic status, and maternal age as potential confounders based on the proposed relationships between variables (Figure S1). We did not evaluate variables such as smoking and obesity as confounders because we hypothesized that these variables were on the causal pathway. We conducted confounding assessment using the backwards change in estimate approach. We also evaluated time between index delivery and follow-up interview as a covariate due to the wide range in follow-up times (six months to three years).
Given the potential for exposure misclassification, we conducted a probabilistic bias analysis on the weighted summary data. Bias parameters were informed by the minimization/denial scale. This scale consists of three statements that are used to identify individuals with a tendency to give socially desirable responses or individuals who may be underreporting CM.39, 49 Due to uncertainty in estimating bias parameters, trapezoidal distributions were used.50 Based on the distribution of scores, the sensitivity among stillbirths and live births was assumed to fall between 0.60 and 1.00 (Table S1). The upper and lower modes specified in the trapezoidal distribution were altered for stillbirth and live births to reflect potential differential reporting. Since false positives are not perceived to be an issue in this study, the specificity ranged between 0.95 and 1.00. As the minimization/denial scale indicates general underreporting and is not specific to each type of CM, we used the same bias parameters for each type. Sensitivities and specificities were correlated since the proportion of underreporting was not substantially different between stillbirths and live births.
All statistical tests used a p-value of <0.05 to determine statistical significance. Analyses were performed using SAS, version 9.4 (SAS Institute INC., Cary, North Carolina) and SUDAAN version 11.0 (Research Triangle Institute, Research Triangle Park, North Carolina).51
Results
The results reported in this analysis reflect unadjusted models because there was no meaningful difference between unadjusted models and those adjusted for covariates using the backwards change in estimate approach (results not shown). Women with healthy term live births were more likely than women with stillbirths to be non-Hispanic white, have at least some college education, be married, have a BMI within the normal range, have insurance, and not have an intervening pregnancy (Table 1). There was no difference in the distribution of maternal age, depression score at the time of the follow-up interview, smoking, alcohol or drug use, and any of the significant life events between women with stillbirths and those with healthy term live births.
Table 1.
Descriptive characteristics using the weighted data by outcome status.
| Characteristic – Weighted % | Stillbirths Nw = 182 |
Healthy Term Live Births1 Nw = 639 |
P value2 |
|---|---|---|---|
| Maternal Age3 | 0.32 | ||
| <20 | 3.0 | 3.9 | |
| 20 – 34 | 76.4 | 70.6 | |
| 35 – 39 | 13.4 | 20.0 | |
| 40+ | 7.2 | 5.5 | |
| Maternal Race/Ethnicity | 0.07 | ||
| Non-Hispanic white | 34.1 | 46.3 | |
| Non-Hispanic black | 17.0 | 12.0 | |
| Hispanic | 43.0 | 32.6 | |
| Other | 5.9 | 9.1 | |
| Maternal Education | <0.01 | ||
| 0 – 11(none/primary/some secondary) | 26.7 | 18.0 | |
| 12(completed secondary) | 34.4 | 24.0 | |
| 13+(college) | 38.9 | 58.0 | |
| Marital Status | <0.01 | ||
| Not married or cohabitating | 19.6 | 13.4 | |
| Cohabitating | 33.5 | 19.1 | |
| Married | 46.9 | 67.5 | |
| BMI4 | 0.02 | ||
| <18.5 | 1.3 | 3.3 | |
| 18.5 – 24.9 | 38.0 | 52.0 | |
| 25 – 29.9 | 22.1 | 22.9 | |
| 30 – 34.9 | 17.4 | 12.0 | |
| ≥35 | 21.2 | 9.8 | |
| Insurance | 0.02 | ||
| No insurance | 5.4 | 2.9 | |
| Any public/private insurance | 60.3 | 46.6 | |
| VA/commercial health ins/HMO | 34.3 | 50.5 | |
| Depression5 | 0.08 | ||
| EDS > 12 | 19.4 | 10.5 | |
| EDS ≤ 12 | 80.6 | 89.5 | |
| Intervening Pregnancy | <0.01 | ||
| No | 41.1 | 74.0 | |
| Yes – only incomplete6 | 8.9 | 8.0 | |
| Yes – at least one live birth | 43.1 | 16.5 | |
| Yes – no live births | 6.9 | 1.5 | |
| Smoking Status7 | 0.69 | ||
| Did not smoke | 84.0 | 86.5 | |
| < 10 | 10.3 | 7.0 | |
| ≥ 10 | 5.7 | 6.5 | |
| Alcohol Use8 | 0.19 | ||
| Did not drink | 62.8 | 56.8 | |
| Drank, no binging | 17.8 | 25.6 | |
| Binged | 19.4 | 17.6 | |
| Illicit Drug Use9 | 0.26 | ||
| Never used drugs | 71.3 | 68.3 | |
| Ever used drugs w/o addiction | 25.8 | 31.0 | |
| Ever used drugs w/ addiction | 2.9 | 0.7 | |
| SLE10 – Financial | 52.5 | 45.8 | 0.25 |
| SLE – Emotional | 46.0 | 45.1 | 0.88 |
| SLE – Traumatic | 25.7 | 17.0 | 0.09 |
| SLE – Partner-related | 34.8 | 27.6 | 0.19 |
| Number of SLE Factors | 0.41 | ||
| 0 | 19.1 | 26.3 | |
| 1 | 34.5 | 33.6 | |
| 2 | 22.3 | 23.7 | |
| 3 | 16.7 | 11.1 | |
| 4 | 7.4 | 5.3 |
Excluding live births <37 weeks gestation, admitted to neonatal intensive care unit, or died
P values calculated using Rao-Scott chi-square tests comparing all stillbirths to healthy term live births
Maternal age at the time of the follow up interview
Missing 250 observations (26%)
Depression at time of follow up interview, based on Edinburgh Depression Scale
The woman was pregnant at the time of interview
Average number of cigarettes during 3 months prior to pregnancy
Alcohol consumption during 3 months prior to pregnancy
Lifetime drug use
Significant Life Events
Women with stillbirths were not more likely than women with healthy term live births to report having experienced any CM (Table 2). However, women with stillbirths were more likely to report emotional neglect (p-value=0.02). When stratified by maternal race/ethnicity, Hispanic women had the highest proportion reporting emotional and physical neglect, especially among those who experienced a stillbirth and completed the follow-up interview in Spanish (emotional neglect: 78.5%; physical neglect: 84.7%; Table 3). Among healthy term live births, non-Hispanic white women had the highest proportion reporting none or minimal abuse or neglect for every subscale in comparison to non-Hispanic black women and Hispanic women. Consequently, non-Hispanic white women with a healthy term live birth had a lower proportion of women who reported experiencing at least one type of CM than non-Hispanic black women and Hispanic women. For example, 42.4% of non-Hispanic black women, 31.1% of Hispanic women, and 15.0% of non-Hispanic white women reported childhood exposure to sexual abuse.
Table 2.
Descriptive statistics of Childhood Trauma Questionnaire as a categorical variable by outcome status using the weighted data.
| Stillbirth % | Healthy Term Live Birth % | P value1 | |
|---|---|---|---|
| Overall CM | 0.66 | ||
| None | 43.6 | 46.1 | |
| Any | 56.4 | 53.9 | |
| Emotional Abuse | 0.52 | ||
| None or Minimal | 73.3 | 69.8 | |
| Low to Extreme | 26.7 | 30.2 | |
| Emotional Neglect | 0.02 | ||
| None or Minimal | 60.9 | 75.1 | |
| Low to Extreme | 39.1 | 24.9 | |
| Physical Abuse | 0.97 | ||
| None or Minimal | 79.9 | 79.7 | |
| Low to Extreme | 20.1 | 20.3 | |
| Physical Neglect | 0.14 | ||
| None or Minimal | 71.8 | 80.0 | |
| Low to Extreme | 28.2 | 20.0 | |
| Sexual Abuse | 0.47 | ||
| None or Minimal | 78.5 | 74.8 | |
| Low to Extreme | 21.5 | 25.2 | |
| Minimization/Denial | 0.39 | ||
| 0 | 53.7 | 48.8 | |
| ≥ 1 | 46.3 | 51.2 |
Abbreviations: CM, childhood maltreatment
P values calculated using chi square tests comparing stillbirths to healthy term live births
Table 3.
Descriptive statistics of Childhood Trauma Questionnaire by outcome status, stratified by race/ethnicity and language of follow-up interview.
| Weighted N (%) | Non-Hispanic White Women | Non-Hispanic Black Women | Total Hispanic | Hispanic Women English Interview |
Spanish Interview | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| SB | LB | SB | LB | SB | LB | SB | LB | SB | LB | |
| Overall CM | ||||||||||
| None | 33 (56.5) | 170 (57.7) | 10 (32.9) | 23 (30.9) | 30 (38.8) | 80 (38.5) | 28 (45.8) | 64 (41.2) | 3 (15.3) | 15 (30.2) |
| Any | 26 (43.5) | 125 (42.3) | 21 (67.1) | 51 (69.1) | 48 (61.2) | 127 (61.5) | 33 (54.2) | 92 (58.8) | 15 (84.7) | 36 (69.8) |
| Emotional Abuse | ||||||||||
| None or Minimal | 40 (68.1) | 223 (75.5) | 26 (82.8) | 41 (56.1) | 60 (76.8) | 135 (65.5) | 46 (75.5) | 99 (63.5) | 15 (81.5) | 35 (71.7) |
| Low to Extreme | 19 (31.9) | 72 (24.5) | 5 (17.2) | 32 (43.9) | 18 (23.2) | 71 (34.5) | 15 (24.5) | 57 (36.5) | 3 (18.5) | 14 (28.3) |
| Emotional Neglect | ||||||||||
| None or Minimal | 42 (71.6) | 238 (80.6) | 16 (51.2) | 53 (72.4) | 43 (55.1) | 142 (68.9) | 39 (65.1) | 108 (69.1) | 4 (21.5) | 34 (68.0) |
| Low to Extreme | 17 (28.4) | 57 (19.4) | 15 (48.8) | 20 (27.6) | 35 (44.9) | 64 (31.1) | 21 (34.9) | 48 (30.9) | 14 (78.5) | 16 (32.0) |
| Physical Abuse | ||||||||||
| None or Minimal | 50 (84.6) | 256 (86.8) | 17 (55.2) | 46 (62.1) | 69 (88.5) | 161 (77.5) | 55 (90.6) | 119 (76.4) | 15 (81.5) | 41 (80.7) |
| Low to Extreme | 9 (15.4) | 39 (13.2) | 14 (44.8) | 28 (37.9) | 9 (11.5) | 47 (22.5) | 6 (9.4) | 37 (23.6) | 3 (18.5) | 10 (19.3) |
| Physical Neglect | ||||||||||
| None or Minimal | 46 (77.6) | 258 (87.6) | 24 (75.9) | 61 (82.6) | 52 (65.9) | 143 (69.4) | 49 (80.9) | 119 (76.4) | 3 (15.3) | 23 (47.4) |
| Low to Extreme | 13 (22.4) | 37 (12.4) | 7 (24.1) | 13 (17.4) | 27 (34.1) | 63 (30.6) | 12 (19.1) | 37 (23.6) | 15 (84.7) | 26 (52.6) |
| Sexual Abuse | ||||||||||
| None or Minimal | 47 (79.9) | 249 (85.0) | 20 (63.5) | 43 (57.6) | 63 (80.4) | 141 (68.9) | 49 (81.9) | 101 (65.7) | 14 (75.3) | 40 (78.9) |
| Low to Extreme | 12 (20.1) | 44 (15.0) | 11 (36.5) | 31 (42.4) | 15 (19.6) | 64 (31.1) | 11 (18.1) | 53 (34.3) | 4 (24.7) | 11 (21.1) |
Abbreviations: SB, stillbirth; LB, healthy term live birth; CM, childhood maltreatment
The odds ratio (OR) for any CM experienced among the total population was 1.11 (95% confidence interval [95% CI]: 0.70, 1.74) (Table 4). The OR for emotional neglect among the total population was 1.93 (95% CI: 1.17, 3.19); stratified results were consistent in the direction of the association. However, the only significant stratified result was for Hispanic women interviewed in Spanish. The ORs for emotional abuse, physical abuse, physical neglect, and sexual abuse were not statistically significant in either the total or stratified populations. Additionally, tests of interaction between maternal race/ethnicity and each of the types of CM were not statistically significant. These findings were consistent in a sensitivity analysis that included preterm births in the control group (results not shown).
Table 4.
Stillbirth odds ratios for the total and stratified populations for the Childhood Trauma Questionnaire, analyzed as a dichotomous variable, using the weighted data.
| Total population | Non-Hispanic White Women |
Non-Hispanic Black Women |
Total Hispanic | Hispanic Women English Interview |
Spanish Interview | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Overall CM | ||||||||||||
| None | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Any | 1.11 | 0.70, 1.74 | 1.05 | 0.55, 1.99 | 0.91 | 0.30, 2.75 | 0.99 | 0.43, 2.24 | 0.83 | 0.33, 2.09 | 2.40 | 0.37, 15.74 |
| Emotional Abuse | ||||||||||||
| None or Minimal | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Low to Extreme | 0.84 | 0.50, 1.44 | 1.45 | 0.72, 2.92 | 0.27 | 0.05, 1.32 | 0.57 | 0.22, 1.49 | 0.57 | 0.20, 1.62 | 0.58 | 0.05, 6.22 |
| Emotional Neglect | ||||||||||||
| None or Minimal | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Low to Extreme | 1.93 | 1.17, 3.19 | 1.64 | 0.77, 3.51 | 2.50 | 0.78, 7.98 | 1.80 | 0.77, 4.20 | 1.20 | 0.45, 3.24 | 7.74 | 1.31, 45.72 |
| Physical Abuse | ||||||||||||
| None or Minimal | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Low to Extreme | 0.99 | 0.54, 1.82 | 1.20 | 0.47, 3.07 | 1.33 | 0.39, 4.48 | 0.44 | 0.14, 1.46 | 0.33 | 0.09, 1.24 | 0.95 | 0.09, 10.35 |
| Physical Neglect | ||||||||||||
| None or Minimal | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Low to Extreme | 1.57 | 0.90, 2.76 | 2.03 | 0.85, 4.87 | 1.51 | 0.36, 6.34 | 1.18 | 0.48, 2.86 | 0.76 | 0.24, 2.43 | 5.01 | 0.77, 32.61 |
| Sexual Abuse | ||||||||||||
| None or Minimal | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Low to Extreme | 0.81 | 0.45, 1.46 | 1.43 | 0.58, 3.51 | 0.78 | 0.22, 2.82 | 0.54 | 0.21, 1.41 | 0.42 | 0.14, 1.25 | 1.22 | 0.15, 9.89 |
Abbreviations: OR, odds ratio; CI, confidence interval; CM, childhood maltreatment
The minimization/denial score indicated that 46.3% of women with stillbirths and 51.2% of women with healthy term live births might be underreporting their exposure to CM (Table 2). Assuming the bias model and parameters used are correct, the ORs and simulation intervals presented in Table S2 reflect estimates adjusted for this potential underreporting through probabilistic bias analysis. The ORs from this analysis were not meaningfully different from those obtained in the total or stratified populations (Table S2). Many of the simulation intervals did not include the null, likely due to the shift in the distribution of exposure that occurs when correcting for underreporting.
Discussion
Overall, there was no association between CM and stillbirth, except for the emotional neglect subscale. Although not statistically significant, there is a suggestion that the magnitude and direction of the association may differ with respect to type of abuse or neglect, race/ethnicity, and level of acculturation. Neglect subscales were the only subscales where the ORs were consistently above 1.0 across all race/ethnicity groups. Notably, the ORs for non-Hispanic white women were consistently greater than 1.0 for all types of abuse and neglect evaluated, but this was not the case for either non-Hispanic black women or Hispanic women.
Only one other study has evaluated a similar association of CM and fetal loss. Hillis et al. (2004) analyzed data from a retrospective cohort study of adult women and reported that the risk of fetal death for first and second pregnancies increased as the number of adverse childhood experiences increased.32 Women in the Hillis et al. study were predominantly non-Hispanic white (77%) and college educated (72%), which may help explain the conflicting results. Further, Hillis et al. (2004) used a version of the Adverse Childhood Experiences scale, which measures a somewhat different construct of CM than that measured by the CTQ, with eight categories: three related directly to the child (verbal abuse, physical abuse, and sexual abuse) and five related to the environment in which the child grew up (intimate partner violence, household substance abuse, mental illness in household, incarcerated household member, and parental separation or divorce). The CTQ does not capture situations that may lead to a stressful environment for the child, such as separation or divorce. However, the CTQ captures both emotional and physical neglect, which are omitted from the Hillis et al. study and from many studies examining the effects of adverse childhood experiences.52
Despite lack of statistical significance, the variation in observed associations between women of different racial/ethnic groups and levels of acculturation merit discussion. Cultural differences may play an important role in this variation. Non-Hispanic black individuals are more likely than members of other groups to be punished physically, and studies suggest that their experience of physical punishment has a different psychological impact than it does in other populations.53–55 In the CTQ, psychological impact is not assessed, so that physical punishment may over-estimate physical abuse in a non-Hispanic black population.56
Another concern is that baseline exposure to non-measured stressors, including chronic exposure to racism and discrimination, may affect the impact of early life stressors on reproductive health.57 The high prevalence of these exposures in non-Hispanic black women may make it difficult to discern the effect of abuse in a chronically stressed population, thereby resulting in smaller effect sizes.57 A study evaluating abuse in childhood and adulthood in relation to preterm delivery also reported stronger relationships in white/other women (OR: 1.6; 95% CI: 1.1, 2.5) as compared to African-American women (OR: 0.8; 95% CI: 0.4, 1.5).58
The influence of additional stressors may also be relevant to the differences in ORs for Hispanic women who were interviewed in English versus Spanish. English-interviewed women had ORs similar to those of non-Hispanic black women, while the ORs for women who were interviewed in Spanish were more similar, and in some cases much larger in magnitude, than those for non-Hispanic white women. This was particularly true for the neglect subscales. It is plausible that English-interviewed Hispanic women, who have lived as minorities in the United States for several years or their entire lives, have experienced more instances of discrimination than Spanish-interviewed women, all of whom spent some of their lives not as minorities in the United States.59 However, these results should be interpreted with caution due to the small sample sizes for the stratified populations.
Strengths of this study include the relatively large sample size and sampling methods used to ensure a diverse population. Nonetheless, the sample size may have been too small to identify subtle differences, especially in stratified analyses. Another strength is that CM was evaluated using a validated questionnaire (CTQ) administered by trained interviewers using a standard protocol. Additionally, stillbirth cases with causes unlikely to be related to stress were excluded from the analysis. Analytic strengths also include adjustment for selection bias, loss to follow-up, and exposure misclassification.
An important limitation of our study is the substantial loss to follow-up (>50% in cases and controls) that occurred in the SCRN-OASIS study. We accounted for this using stabilized inverse probability weights based on characteristics deemed related to participation in the follow-up study. However, we were limited to characteristics evaluated in the SCRN study and it is possible that unmeasured factors influenced participation, which would limit our ability to control for bias introduced due to loss to follow-up.
Another limitation is possible underreporting of the exposure. Underreporting is more common than over-reporting, so our results may underestimate the true prevalence.60 Additionally, the CTQ is designed to be self-administered, and employing a telephone interview may have contributed to underreporting due to the respondent’s perceived lack of privacy and/or confidentiality. For this reason, we used the most sensitive cut point to dichotomize the exposures. We also conducted a probabilistic bias analysis to quantify the potential impact of underreporting and the results were consistent with our main findings. However, types of CM may have different rates of underreporting, which we were unable to account for in our bias analysis.
Recall bias is also a concern in this analysis. Since the CTQ was completed after the index delivery, responses could be affected by the outcome of the delivery. However, based on the minimization/denial scores, underreporting seems to have been similar irrespective of pregnancy outcome (Table 2). Additionally, a study evaluating test-retest reliability of the CTQ in pregnant women (before and after delivery) found at least moderate agreement for every subscale except physical neglect.61 This suggests that compared to other trauma types, physical neglect may be more prone to selective recall. Further, a study comparing prospective and retrospective measures of CM found that retrospective measures may underestimate the association of CM with objective adult health outcomes.62
Conclusions
Health professionals are increasingly recognizing the importance of a psychosocial life course perspective in studying and ultimately preventing adverse perinatal outcomes, although seldom with respect to stillbirth.63, 64 The results of this study, especially for neglect, should be replicated in future studies of CM. Where study design allows, prospective assessments of CM would also help eliminate possible recall bias. Longitudinal studies would also offer the opportunity to assess the development of risky health behaviors, which may serve as mediators of the relationship between CM and stillbirth.
Supplementary Material
Acknowledgments
We acknowledge the contribution of the Stillbirth Collaborative Research Network. We also acknowledge the members of the National Institute of Child Health and Human Development Scientific Advisory and Safety Monitoring Board for their review of the study protocol, materials, and progress, as well as all of the other physicians, study coordinators, and research nurses in the Stillbirth Collaborative Research Network.
Members of a study group
The Stillbirth Collaborative Research Network—University of Texas Health Science Center at San Antonio: Dr. Donald J. Dudley, Dr. Deborah Conway, Josefine Heim-Hall, Karen Aufdemorte, and Angela Rodriguez; University of Utah School of Medicine: Dr. Robert M. Silver, Dr. Michael W. Varner, and Kristi Nelson; Emory University School of Medicine and Rollins School of Public Health: Dr. Carol J. Rowland Hogue, Dr. Barbara J. Stoll, Janice Daniels Tinsley, Dr. Bahig Shehata, and Dr. Carlos Abromowsky; Brown University: Dr. Donald Coustan, Dr. Halit Pinar, Dr. Marshall Carpenter, and Susan Kubaska; University of Texas Medical Branch at Galveston: Dr. George R. Saade, Dr. Radek Bukowski, Jennifer Lee Rollins, Dr. Hal Hawkins, and Elena Sbrana; RTI International: Dr. Corette B. Parker, Dr. Matthew A. Koch, Vanessa R. Thorsten, Holly Franklin, and Pinliang Chen; Pregnancy and Perinatology Branch, Eunice Kennedy Shriver National Institute of Child Health and Human Development: Drs. Marian Willinger and Uma M. Reddy; Columbia University Medical Center: Dr. Robert L. Goldenberg.
The Stillbirth Collaborative Research Network Writing Group—Dr. Carol J. R. Hogue (Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia); Dr. Robert L. Goldenberg (Department of Obstetrics and Gynecology, Columbia University Medical Center, New York, New York); Drs. Radek Bukowski and George R. Saade (Department of Obstetrics and Gynecology, University of Texas Medical Branch at Galveston, Galveston, Texas); Dr. Barbara J. Stoll (McGovern Medical School, University of Texas Health Science Center, Houston, Texas); Drs. Marshall Carpenter, Donald Coustan, and Halit Pinar (Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, Brown University School of Medicine, Providence, Rhode Island); Dr. Deborah Conway (Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, University of Texas Health Science Center at San Antonio, San Antonio, Texas); Dr. Donald J. Dudley (Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, University of Virginia, Charlottesville, Virginia); Drs. Robert M. Silver and Michael W. Varner (Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, University of Utah School of Medicine, and Maternal Fetal Medicine Unit, Intermountain Healthcare, Salt Lake City, Utah); Drs. Uma M. Reddy and Marian Willinger (Pregnancy and Perinatology Branch, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Maryland); and Drs. Matthew A. Koch and Corette B. Parker (Statistics and Epidemiology Unit, Health Sciences Division, RTI International, Research Triangle Park, North Carolina).
Funding
The Stillbirth Collaborative Research Network was supported by grant funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (Grants U10-HD045953 (Brown University), U10-HD045925 (Emory University), U10-HD045952 (University of Texas Medical Branch at Galveston), U10-HD045955 (University of Texas Health Sciences Center at San Antonio), UK10-HD045944 (University of Utah Health Sciences Center), U10-HD045954 (RTI International)). Alexa Freedman was supported by the NICHD (Grant 5T32HD052460-10) and the Maternal Child Health Bureau, Health Resources and Services Administration (Grant T03MC07651).
LIST OF ABBREVIATONS AND ACRONYMS
- CI
Confidence interval
- CM
Childhood maltreatment
- CTQ
Childhood Trauma Questionnaire
- OR
Odds ratio
- SCRN
Stillbirth Collaborative Research Network
- SCRN-OASIS
Stillbirth Collaborative Research Network, Outcomes after Study Index Stillbirth
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.MacDorman MF, Kirmeyer SE, Wilson EC. Fetal and perinatal mortality, United States, 2006. Natl Vital Stat Rep. 2012;60:1–22. [PubMed] [Google Scholar]
- 2.Flenady V, Koopmans L, Middleton P, Froen JF, Smith GC, Gibbons K, et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet. 2011;377:1331–40. doi: 10.1016/S0140-6736(10)62233-7. [DOI] [PubMed] [Google Scholar]
- 3.Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. 2005;21:398–405. doi: 10.1097/01.ajp.0000149795.08746.31. [DOI] [PubMed] [Google Scholar]
- 4.Suglia SF, Clark CJ, Boynton-Jarrett R, Kressin NR, Koenen KC. Child maltreatment and hypertension in young adulthood. Bmc Public Health. 2014;14 doi: 10.1186/1471-2458-14-1149. doi:Artn 1149 10.1186/1471-2458-14-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110:1761–6. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 6.Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009;71:243–50. doi: 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Der Leder ME, Raskin VD. Psychological sequelae of childhood sexual abuse: relevant in subsequent pregnancy. American journal of obstetrics and gynecology. 1993;168:1336–7. doi: 10.1016/0002-9378(93)90401-4. [DOI] [PubMed] [Google Scholar]
- 8.Noll JG, Schulkin J, Trickett PK, Susman EJ, Breech L, Putnam FW. Differential pathways to preterm delivery for sexually abused and comparison women. Journal of pediatric psychology. 2007;32:1238–48. doi: 10.1093/jpepsy/jsm046. [DOI] [PubMed] [Google Scholar]
- 9.Leeners B, Richter-Appelt H, Imthurn B, Rath W. Influence of childhood sexual abuse on pregnancy, delivery, and the early postpartum period in adult women. Journal of psychosomatic research. 2006;61:139–51. doi: 10.1016/j.jpsychores.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Leeners B, Stiller R, Block E, Gorres G, Rath W. Pregnancy complications in women with childhood sexual abuse experiences. Journal of psychosomatic research. 2010;69:503–10. doi: 10.1016/j.jpsychores.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Leeners B, Rath W, Block E, Gorres G, Tschudin S. Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med. 2014;42:171–8. doi: 10.1515/jpm-2013-0003. [DOI] [PubMed] [Google Scholar]
- 12.Yampolsky L, Lev-Wiesel R, Ben-Zion IZ. Child sexual abuse: is it a risk factor for pregnancy? J Adv Nurs. 2010;66:2025–37. doi: 10.1111/j.1365-2648.2010.05387.x. [DOI] [PubMed] [Google Scholar]
- 13.Laszlo KD, Svensson T, Li J, Obel C, Vestergaard M, Olsen J, et al. Maternal bereavement during pregnancy and the risk of stillbirth: a nationwide cohort study in Sweden. Am J Epidemiol. 2013;177:219–27. doi: 10.1093/aje/kws383. [DOI] [PubMed] [Google Scholar]
- 14.Hogue CJ, Parker CB, Willinger M, Temple JR, Bann CM, Silver RM, et al. A population-based case-control study of stillbirth: the relationship of significant life events to the racial disparity for African Americans. Am J Epidemiol. 2013;177:755–67. doi: 10.1093/aje/kws381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loomans EM, van Dijk AE, Vrijkotte TG, van Eijsden M, Stronks K, Gemke RJ, et al. Psychosocial stress during pregnancy is related to adverse birth outcomes: results from a large multi-ethnic community-based birth cohort. Eur J Public Health. 2013;23:485–91. doi: 10.1093/eurpub/cks097. [DOI] [PubMed] [Google Scholar]
- 16.Hogue CJ, Parker CB, Willinger M, Temple JR, Bann CM, Silver RM, et al. The association of stillbirth with depressive symptoms 6–36 months post-delivery. Paediatr Perinat Epidemiol. 2015;29:131–43. doi: 10.1111/ppe.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang S, Ding Z, Liu H, Chen Z, Wu J, Zhang Y, et al. Association between mental stress and gestational hypertension/preeclampsia: a meta-analysis. Obstet Gynecol Surv. 2013;68:825–34. doi: 10.1097/OGX.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 18.Marinescu IP, Foarfa MC, Pirlog MC, Turculeanu A. Prenatal depression and stress - risk factors for placental pathology and spontaneous abortion. Rom J Morphol Embryol. 2014;55:1155–60. [PubMed] [Google Scholar]
- 19.Felitti VJ. Adverse childhood experiences and adult health. Acad Pediatr. 2009;9:131–2. doi: 10.1016/j.acap.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 20.Chung EK, Nurmohamed L, Mathew L, Elo IT, Coyne JC, Culhane JF. Risky health behaviors among mothers-to-be: the impact of adverse childhood experiences. Acad Pediatr. 2010;10:245–51. doi: 10.1016/j.acap.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bodnar LM, Parks WT, Perkins K, Pugh SJ, Platt RW, Feghali M, et al. Maternal prepregnancy obesity and cause-specific stillbirth. Am J Clin Nutr. 2015;102:858–64. doi: 10.3945/ajcn.115.112250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woolner AM, Bhattacharya S. Obesity and stillbirth. Best Pract Res Clin Obstet Gynaecol. 2015;29:415–26. doi: 10.1016/j.bpobgyn.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 23.Coletta J, Simpson LL. Maternal medical disease and stillbirth. Clin Obstet Gynecol. 2010;53:607–16. doi: 10.1097/GRF.0b013e3181eb2ca0. [DOI] [PubMed] [Google Scholar]
- 24.Cammack AL, Buss C, Entringer S, Hogue CJ, Hobel CJ, Wadhwa PD. The association between early life adversity and bacterial vaginosis during pregnancy. Am J Obstet Gynecol. 2011;204:431 e1–8. doi: 10.1016/j.ajog.2011.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson HW, Donenberg GR, Emerson E. Childhood violence exposure and the development of sexual risk in low-income African American girls. J Behav Med. 2014;37:1091–101. doi: 10.1007/s10865-014-9560-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson HW, Widom CS. Pathways from childhood abuse and neglect to HIV-risk sexual behavior in middle adulthood. J Consult Clin Psychol. 2011;79:236–46. doi: 10.1037/a0022915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sutherland MA. Examining mediators of child sexual abuse and sexually transmitted infections. Nurs Res. 2011;60:139–47. doi: 10.1097/NNR.0b013e318209795e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:217–26. doi: 10.2471/BLT.12.107623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menezes EV, Yakoob MY, Soomro T, Haws RA, Darmstadt GL, Bhutta ZA. Reducing stillbirths: prevention and management of medical disorders and infections during pregnancy. BMC Pregnancy Childbirth. 2009;9(Suppl 1):S4. doi: 10.1186/1471-2393-9-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson HW, Widom CS. Sexually transmitted diseases among adults who had been abused and neglected as children: a 30-year prospective study. Am J Public Health. 2009;99(Suppl 1):S197–203. doi: 10.2105/AJPH.2007.131599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu B, Roberts CL, Clarke M, Jorm L, Hunt J, Ward J. Chlamydia and gonorrhoea infections and the risk of adverse obstetric outcomes: a retrospective cohort study. Sex Transm Infect. 2013;89:672–8. doi: 10.1136/sextrans-2013-051118. [DOI] [PubMed] [Google Scholar]
- 32.Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004;113:320–7. doi: 10.1542/peds.113.2.320. [DOI] [PubMed] [Google Scholar]
- 33.D’Anna-Hernandez KL, Hoffman MC, Zerbe GO, Coussons-Read M, Ross RG, Laudenslager ML. Acculturation, maternal cortisol, and birth outcomes in women of Mexican descent. Psychosom Med. 2012;74:296–304. doi: 10.1097/PSY.0b013e318244fbde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barcelona de Mendoza V, Harville E, Theall K, Buekens P, Chasan-Taber L. Acculturation and Adverse Birth Outcomes in a Predominantly Puerto Rican Population. Matern Child Health J. 2016;20:1151–60. doi: 10.1007/s10995-015-1901-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kimber M, Henriksen CA, Davidov DM, Goldstein AL, Pitre NY, Tonmyr L, et al. The association between immigrant generational status, child maltreatment history and intimate partner violence (IPV): evidence from a nationally representative survey. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1135–44. doi: 10.1007/s00127-014-1002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dettlaff AJ, Johnson MA. Child maltreatment dynamics among immigrant and U.S. born Latino children: Findings from the National Survey of Child and Adolescent Well-being (NSCAW) Child Youth Serv Rev. 2011;33:936–44. [Google Scholar]
- 37.Spong CY, Iams J, Goldenberg R, Hauck FR, Willinger M. Disparities in perinatal medicine: preterm birth, stillbirth, and infant mortality. Obstet Gynecol. 2011;117:948–55. doi: 10.1097/AOG.0b013e318211726f. [DOI] [PubMed] [Google Scholar]
- 38.Parker CB, Hogue CJ, Koch MA, Willinger M, Reddy UM, Thorsten VR, et al. Stillbirth Collaborative Research Network: design, methods and recruitment experience. Paediatr Perinat Epidemiol. 2011;25:425–35. doi: 10.1111/j.1365-3016.2011.01218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- 40.Childhood Trauma Questionnaire: A Retrospective Self-Report (CTQ): Pearson Clinical, 1997
- 41.Medrano MA, Hatch JP, Zule WA, Desmond DP. Childhood trauma and adult prostitution behavior in a multiethnic heterosexual drug-using population. Am J Drug Alcohol Abuse. 2003;29:463–86. doi: 10.1081/ada-120020527. [DOI] [PubMed] [Google Scholar]
- 42.Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, et al. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA. 2008;299:1291–305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerke CK, Mazzeo SE, Kliewer W. The role of depression and dissociation in the relationship between childhood trauma and bulimic symptoms among ethnically diverse female undergraduates. Child Abuse Negl. 2006;30:1161–72. doi: 10.1016/j.chiabu.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 44.Thombs BD, Bennett W, Ziegelstein RC, Bernstein DP, Scher CD, Forde DR. Cultural sensitivity in screening adults for a history of childhood abuse: evidence from a community sample. J Gen Intern Med. 2007;22:368–73. doi: 10.1007/s11606-006-0026-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flenady V, Wojcieszek AM, Middleton P, Ellwood D, Erwich JJ, Coory M, et al. Stillbirths: recall to action in high-income countries. Lancet. 2016;387:691–702. doi: 10.1016/S0140-6736(15)01020-X. [DOI] [PubMed] [Google Scholar]
- 46.Selk SC, Rich-Edwards JW, Koenen K, Kubzansky LD. An observational study of type, timing, and severity of childhood maltreatment and preterm birth. J Epidemiol Community Health. 2016;70:589–95. doi: 10.1136/jech-2015-206304. [DOI] [PubMed] [Google Scholar]
- 47.Edwards KM, Greaney K, Palmer KM. Participants’ Reactions to and Suggestions for Conducting Intimate Partner Violence Research: A Study of Rural Young Adults. J Rural Health. 2016;32:3–12. doi: 10.1111/jrh.12126. [DOI] [PubMed] [Google Scholar]
- 48.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull. 2007;133:859–83. doi: 10.1037/0033-2909.133.5.859. [DOI] [PubMed] [Google Scholar]
- 49.MacDonald K, Thomas ML, Sciolla AF, Schneider B, Pappas K, Bleijenberg G, et al. Minimization of Childhood Maltreatment Is Common and Consequential: Results from a Large, Multinational Sample Using the Childhood Trauma Questionnaire. PLoS One. 2016;11:e0146058. doi: 10.1371/journal.pone.0146058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lash TL, Fox MP, Fink AK. Applying quantitative bias analysis to epidemiologic data. Dordrecht; New York: Springer; 2009. [Google Scholar]
- 51.Research Triangle Institute. SUDAAN Language Manual. 1 and 2. Research Triangle Park, NC: Research Triangle Institute; 2012. Release 11. [Google Scholar]
- 52.Stoltenborgh M, Bakermans-Kranenburg MJ, van Ijzendoorn MH. The neglect of child neglect: a meta-analytic review of the prevalence of neglect. Soc Psychiatry Psychiatr Epidemiol. 2013;48:345–55. doi: 10.1007/s00127-012-0549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Whaley AL. Sociocultural differences in the developmental consequences of the use of physical discipline during childhood for African Americans. Cultur Divers Ethnic Minor Psychol. 2000;6:5–12. doi: 10.1037/1099-9809.6.1.5. [DOI] [PubMed] [Google Scholar]
- 54.Gershoff ET, Lansford JE, Sexton HR, Davis-Kean P, Sameroff AJ. Longitudinal links between spanking and children’s externalizing behaviors in a national sample of White, Black, Hispanic, and Asian American families. Child Dev. 2012;83:838–43. doi: 10.1111/j.1467-8624.2011.01732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lansford JE, Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Ethnic differences in the link between physical discipline and later adolescent externalizing behaviors. J Child Psychol Psychiatry. 2004;45:801–12. doi: 10.1111/j.1469-7610.2004.00273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thombs BD, Lewis C, Bernstein DP, Medrano MA, Hatch JP. An evaluation of the measurement equivalence of the Childhood Trauma Questionnaire–Short Form across gender and race in a sample of drug-abusing adults. J Psychosom Res. 2007;63:391–8. doi: 10.1016/j.jpsychores.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 57.Widom CS, Czaja S, Wilson HW, Allwood M, Chauhan P. Do the long-term consequences of neglect differ for children of different races and ethnic backgrounds? Child Maltreat. 2013;18:42–55. doi: 10.1177/1077559512460728. [DOI] [PubMed] [Google Scholar]
- 58.Margerison-Zilko CE, Strutz KL, Li Y, Holzman C. Stressors Across the Life-Course and Preterm Delivery: Evidence From a Pregnancy Cohort. Matern Child Health J. 2016 doi: 10.1007/s10995-016-2151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ortiz V, Telles E. Racial Identity and Racial Treatment of Mexican Americans. Race Soc Probl. 2012;4 doi: 10.1007/s12552-012-9064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–73. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 61.Cammack AL, Hogue CJ, Drews-Botsch CD, Kramer MR, Pearce BD, Knight BT, et al. Test-retest reliability of retrospective self-reported maternal exposure to childhood abuse and neglect. Arch Womens Ment Health. 2016;19:415–21. doi: 10.1007/s00737-015-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. 2016;57:1103–12. doi: 10.1111/jcpp.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.St Fleur M, Damus K, Jack B. The future of preconception care in the United States: multigenerational impact on reproductive outcomes. Ups J Med Sci. 2016:1–5. doi: 10.1080/03009734.2016.1206152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7:13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


