Abstract
Aim
Estrogen receptor-α (ER-α) activation drives the progression of luminal breast cancers. Signaling by transforming growth factor-β (TGF-β) typically opposes the actions of ER-α; it also induces epithelial-mesenchymal transition (EMT) programs that promote breast cancer dissemination, stemness, and chemoresistance. The impact of EMT programs on nongenomic ER-α signaling remains unknown and was studied herein.
Methods
MCF-7 and BT474 cells were stimulated with TGF-β to induce EMT programs, at which point ER-α expression, localization, and nongenomic interactions with receptor tyrosine kinases and MAP kinases (MAPKs) were determined. Cell sensitivity to anti-estrogens both before and after traversing the EMT program was also investigated.
Results
TGF-β stimulated MCF-7 and BT474 cells to acquire EMT phenotypes, which enhanced cytoplasmic accumulation of ER-α without altering its expression. Post-EMT cells exhibited (i) elevated expression of EGFR and IGF1R, which together with Src formed cytoplasmic complexes with ER-α; (ii) enhanced coupling of EGF, IGF-1 and estrogen to the activation of MAPKs; and (iii) reduced sensitivity to tamoxifen, an event reversed by administration of small molecule inhibitors against the receptors for TGF-β, EGF, and IGF-1, as well as those against MAPKs.
Conclusion
EMT stimulated by TGF-β promotes anti-estrogen resistance by activating EGFR-, IGF1R-, and MAPK-dependent nongenomic ER-α signaling.
Keywords: Breast cancer, EMT, Estrogen receptor-α, Growth factor, Signal transduction, tamoxifen resistance, TGF-β
INTRODUCTION
Transforming growth factor-β (TGF-β) normally acts as a suppressor of mammary tumorigenesis by inducing cellular arrest, apoptosis, or differentiation, and by creating a cell microenvironment that inhibits cell motility, invasion and metastasis. However, during breast cancer development, the tumor suppressing functions of TGF-β are frequently subverted, thus converting TGF-β from a tumor suppressor to a promoter of breast cancer growth and metastasis [1–3]. Although the molecular mechanisms responsible for eliciting the dichotomous activities of TGF-β remain to be fully elucidated, accumulating evidence implicates canonical Smad2/3-dependent signaling in mediating tumor suppression by TGF-β and noncanonical Smad2/3-independent signaling in mediating its tumor promoting activities [1–3]. Amongst the best characterized noncanonical signaling pathways operant in coupling TGF-β to tumorigenesis are (i) integrins and components of focal adhesion complexes; (ii) MAP kinase and small GTP-binding protein family members; and (iii) PI3K/AKT and NF-κB pathways [4]; they also function to drive epithelial-mesenchymal transitions (EMT) stimulated by TGF-β, thereby promoting breast cancer dissemination, stemness, and chemoresistance [5].
Within the mammary gland, signaling by estrogen receptor α (ER-α) plays an essential role not only during glandular development and differentiation, but also during the initiation and progression of luminal breast cancers [6–8]. Indeed, the oncogenic activities of dysregulated ER-α signaling underlie the clinical success of anti-estrogen drugs (e.g., tamoxifen) as first-line therapies to treat ER-positive breast cancers. However, despite their initial efficacy, anti-estrogen drugs often become ineffective as patient tumors develop resistance and undergo disease recurrence [9, 10]. At present, the mechanisms resulting in acquired anti-estrogen resistance are not fully understood. However, compelling evidence implicates nongenomic ER-α signaling as a major culprit of resistance to anti-estrogen-based therapies [9, 11–13]. Likewise, aberrant expression of a truncated metastasis tumor antigen 1 (MTA1) mutant was found to bind and sequester ER-α in the cytoplasm, thus enhancing the nongenomic actions of ER-α and disease progression in breast cancers [14].
Given the pathophysiologic parallels that exist between nongenomic ER-α and noncanonical TGF-β signaling in driving breast progression, we speculated that EMT programs induced by TGF-β may elicit nongenomic ER-α signaling and endocrine resistance in luminal breast cancers. The aim of this study was to test this hypothesis and further our understanding of how EMT programs drive disease progression and acquired resistance to anti-estrogen-based therapies in human breast cancers.
METHODS
Cell lines and chemical inhibitors
Human luminal A MCF-7 cells were obtained from ATCC (USA) and cultured as previously described [15], while human luminal B BT474 cells were kindly provided by Dr. Mark W. Jackson (Case Western Reserve University, USA) and propagated in DMEM supplemented with 10% fetal bovine serum (FBS; Thermo Fisher Scientific, USA) and 1% Pen/Strep (Invitrogen, USA). Pharmacological agonists and inhibitors used herein are described in the Supplementary Table 1
Cell biological assays
Analyzing the effects of TGF-β and EMT programs on ER-α signaling in MCF-7 and BT474 cells was determined as follows: (i) Cell proliferation assays: Cells were treated in the absence or presence of TGF-β1 (5 ng/ml; R&D Systems, USA) for 72 h to induce EMT, at which point they were subcultured in 96-well plates (10,000 cells/well) for 5 days with either diluent or inhibitors to the TGF-β type I receptor (TβR-I; 100 ng/ml), the epidermal growth factor receptor (EGFR; 1 μM), the insulin-like growth factor 1 receptor (IGF1R; 1 μM), mitogen-activated protein kinase kinase (MEK;10 μM), or ER-α (0.1 μM; Supplementary Table 1). Differences in cell growth and survival were determined by incubating the cells with MTS Plus reagent (20 μl; Promega, USA) for 1 hr at 37°C, followed by measuring absorbance at 490 nm on a Promega Modulus II Microplate Multimode instrument (Promega, USA). (ii) 3-dimensional (3D) growth assays: 3D-cultures were prepared by diluting pre- or post-EMT MCF-7 and BT474 cells in complete media supplemented with 5% Cultrex (Trevigen, Gaithersburg, USA), which subsequently were seeded onto solidified Cultrex cushions (500 μl/well) contained in 6-well plates (150,000 cells/well). Afterward, the cells were cultured in the absence or presence of TGF-β1 (5 ng/ml), estradiol (1 nM), tamoxifen (0.1 nM), or fulvestrant (0.1 μM; Supplementary Table 1) for 8 days, during which time they were fed every 3 days with full growth media supplemented with 5% Cultrex and pharmacological agents. Differences in organoid growth were calculated using NIH Image J. (iii) Luciferase reporter gene assays: Pre- and post-EMT MCF-7 and BT474 cells were allowed to adhere overnight to 24-well plates (40,000 cells/well). The cells were transiently transfected as described previously [16, 17] with the following reporter plasmids: (a) pSBE-luciferase, which contains 4 copies of the Smad3/4-binding element (4X-CAGA) and serves as a direct measure of canonical TGF-β signaling; (b) p3TP-lux [18], which contains 3 copies of TPA-responsive elements and 96 bp of the PAI-1 promoter and responds to both canonical (i.e., Smad3/4) and noncanonical (i.e., AP-1) TGF-β signaling; (c) pERE-TATA-luciferase [19], which contains 3 copies of the estrogen response element (3X-GGTCACAGTGACC) and responds to estrogen; (d) pTopFlash-luciferase [20], which contains 7 copies of the TCF/LEF-binding sites (7X-AGATCAAAGGgggta) and responds to β-catenin activation; and (e) pCMV-β-gal, which was used to control for differences in transfection efficiency. Afterward, the cells were incubated in the absence or presence of TGF-β1 (5 ng/ml), estradiol (0.1 nM), 4-OHT (0.1 μM), or TβRI inhibitor II (100 ng/ml; Supplementary Table 1) as described previously [16, 17]. (iv) Direct and indirect immunofluorescence: Pre- and post-EMT MCF-7 and BT474 cells were cultured overnight in 8-well chamber slides (80,000 cells/well) prior to being treated for 96 hr in serum-free media supplemented with TGF-β1 (5 ng/ml), estradiol (0.1 nM), 4-OHT (0.1 μM), or fulvestrant (0.1 μM; Supplementary Table 1). Afterwards, the cells were fixed in 4% paraformaldehyde and processed for direct immunofluorescence with phalloidin (0.25 μM; Molecular Probes, USA), or for indirect immunofluorescence with either anti-E-cadherin (E-cad) or anti-β-catetnin antibodies (1:250 dilution; BD Biosciences, San Jose, USA), followed by sequential incubation with biotinylated secondary antibodies (5 μg/ml; Jackson ImmunoResearch, USA) and Alexa-streptavidin (1.2 μg/ml; Molecular Probes, USA). Following extensive washing with PBS, the slides were mounted on glass slides with Prolong mounting medium (Molecular Probes) as described previously [16, 17].
Semi-quantitative real-time PCR analysis
Total RNA from MCF-7 or BT474 cells were purified using the RNeasy Plus Mini kit (Qiagen, USA) according to the manufacturer’s instruction. Afterwards, cDNAs were synthesized by iScript reverse transcription kit (Bio-Rad, USA), diluted 5-fold in H2O, and employed in semi-quantitative real-time PCR reactions (20 μl) using SYBR Green system (Bio-Rad, USA) that contained 5 μl of diluted cDNA and 0.1 μM of oligonucleotide pairs listed in Supplementary Table 2. Differences in RNA concentration were controlled by normalizing individual gene signals to their corresponding β-actin or GAPDH as indicated.
Western blotting analyses
Pre- and post-EMT MCF-7 and BT474 cells were lysed in Buffer H/1% Triton X-100 [21] and solubilized for 60 min on ice. After microcentrifugation, the clarified cell extracts were resolved through 10% SDS-PAGE electrophoresis gels, transferred electrophoretically to nitrocellulose membranes, and blocked in 5% milk prior to incubation with primary antibodies listed in Supplementary Table 3. The resulting immunocomplexes were visualized by enhanced chemiluminescence reactions, and differences in protein loading were monitored by reprobing stripped membranes with antibodies against either β-actin, ERK1/2, or p38 MAPK as indicated.
Co-immunoprecipitation assays
Clarified cell extracts (1mg/tube; see above) prepared from pre- and post-EMT MCF-7 cells were incubated under continuous rotation with 1 μg of antibodies against either β-catenin, E-cad, ERα, or Src overnight at 4°C. The resulting immunocomplexes were collected by microcentrifugation, washed, and fractionated through 10% SDS-PAGE gels prior to their immobilization to nitrocellulose membranes, which subsequently were probed with antibodies against either phospho-tyrosine, β-catenin, EGFR, IGF1R, or ER-α (Supplementary Table 3). Differences in protein loading and/or input were monitored by immunoblotting with corresponding antibodies as indicated.
Statistical Analysis
Statistical values were defined using an unpaired Student’s T-test, where a P value < 0.05 was considered significant. P values for all experiments analyzed are indicated.
RESULTS
TGF-β induces EMT in MCF-7 cells and potentiates noncanonical TGF-β signaling
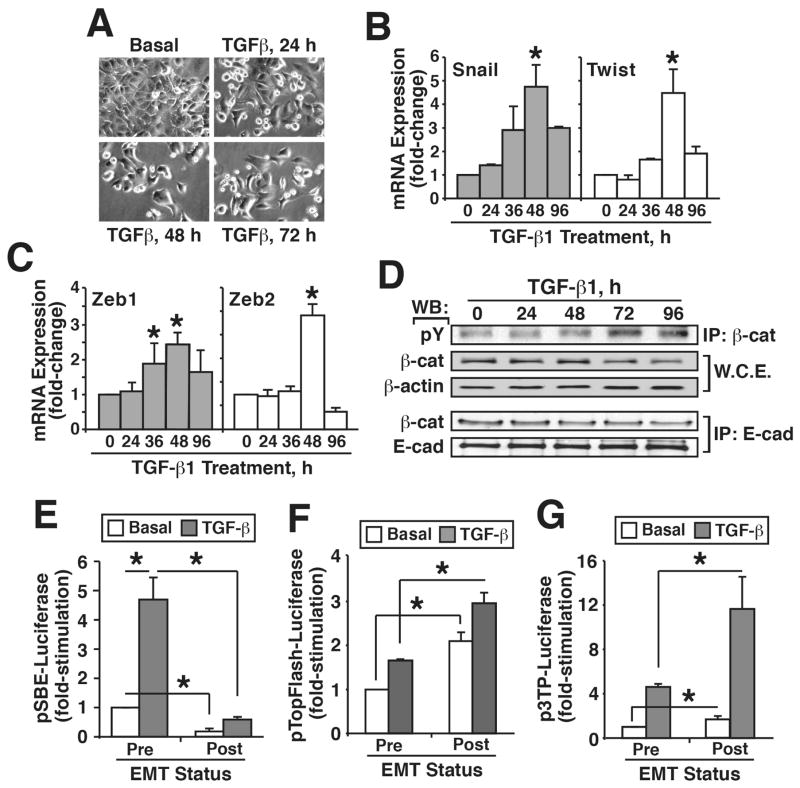
EMT programs stimulated by TGF-β have been associated with the acquisition of motile and metastatic phenotypes, and with the generation of cancer stem cells and chemoresistance [4, 22, 23]. With respect to cancers of the breast, these features of EMT are more commonly associated with basal-like/TNBC subtypes, with little evidence related to how TGF-β and its stimulation of EMT programs impact ER-α signaling in luminal breast cancers. To address this question, we administered TGF-β1 to human MCF-7 cells (i.e., luminal A subtype) propagated in 2D- and 3D-cultures to induce an EMT program. Figure 1A shows that MCF-7 cells readily transitioned from epithelial to mesenchymal morphologies when stimulated with TGF-β1. Moreover, these morphological alterations exhibited by MCF-7 cells coincided with their (i) downregulated expression of the epithelial marker E-cadherin in 3D-cultures (Supplementary Figure S1A), and (ii) upregulated expression of mesenchymal markers vimentin, N-cadherin, Cox-2, and MMP-9 (Supplementary Figure S1B–D), as well as that of the master EMT transcription factors, Snail, Twist, Zeb1, and Zeb2 (Figure 1B and C). Likewise, post-EMT MCF-7 cells showed a striking loss of β-catenin from the plasma membrane (Supplementary Figure S1E) that reflected its enhanced phosphorylation on tyrosine residue(s) and reduced capacity to bind E-cadherin (Figure 1D).
Figure 1.
TGF-β induces EMT in MCF-7 cells and potentiates noncanonical TGF-β signaling. (A) MCF-7 cells were treated with TGF-β1 (5 ng/ml) for 0–72 h to induce an EMT program. Photomicrographs depict accompanying alterations in cell morphology (X 400). (B and C) MCF-7 cells were stimulated with TGF-β1 (5 ng/ml) for 0–96 h, at which point total RNA was harvested and subjected to real-time PCR to monitor differences in the expression of Snail and Twist (B), and of Zeb1 and Zeb2 (C). Data are the mean fold-changes (±S.E.; n=3; *P< 0.05; Student’s t-test). (D) MCF-7 cells were treated with TGF-β1 (5 ng/ml) for 0–96 h, at which point detergent-solubilized extracts were immunoblotted for phospho-Tyr (pY), β-catenin (β-cat), or β-actin as indicated (top). Additionally, E-cad immunocomplexes were captured and immunoblotted for β-catenin (β-cat) and E-cad as indicated (bottom). Images are representative of 3-independent experiments. (E–G) Pre- and post-EMT MCF-7 cells were transiently transfected overnight with the pSBE- (E), TopFlash- (F), or p3TP- (G) luciferase reporter genes, as well as the pCMV-β-galactosidase reporter gene to control for differences in transfection efficiency. Afterward, the transfectants were stimulated overnight with TGF-β1 (5 ng/ml) prior to measuring luciferase and β-gal activities. Data are the mean fold-changes (±S.E.; n=3;*P<0.05; Student’s t-test).
We also investigated the impact of EMT programs on MCF-7 cell behavior and intracellular signaling. To do so, we incubated MCF-7 cells in the absence (i.e., pre-EMT) or presence (i.e., post-EMT) TGF-β1 for 72–96 hr to induce an EMT program, at which point pre- and post-EMT cells were subcultured and transiently transfected with the following reporter genes: (i) pSBE-luciferase, which monitors canonical Smad3/4 signaling stimulated by TGF-β; (ii) pTopFlash-luciferase, which monitors noncanonical β-catenin signaling stimulated by TGF-β; and (iii) p3TP-luciferase, which monitors canonical Smad2/3/4 and noncanonical AP-1 signaling stimulated by TGF-β. Figure 1E shows that luciferase expression driven by the synthetic SBE promoter was significantly inhibited in post-EMT cells, suggesting that EMT programs suppress canonical signaling Smad-based signaling in response to TGF-β. Accordingly, the coupling of TGF-β to noncanonical β-catenin (Figure 1F) and AP-1 (Figure 1G; p3TP) activation was dramatically augmented in a manner reminiscent of EMT-induced signaling alterations observed previously in basal-like/TNBCs [4, 24]. Interestingly, EMT-associated events transpired in both culture systems (i.e., 2D- and 3D-cultures), although the magnitude of EMT response was typically greater in 2D-cultures, suggesting that rigid microenvironments potentiate EMT programs stimulated by TGF-β [25–27].
Similar induction of EMT programs was observed in human BT474 cells (i.e., luminal B subtype) stimulated with TGF-β. For instance, BT474 cells displayed a more mesenchymal morphology in response to TGF-β (Supplementary Figure S2A); they also exhibited robust cadherin switching as the cells transitioned from pre- (e.g., E-cadherin dominant) to post-EMT (e.g., N-cadherin dominant) states (Supplementary Figure S2B). Likewise, BT474 cells undergoing EMT programs exhibited a time-dependent loss of epithelial markers (e.g., β-catenin, CK19, and ZO-1; Supplementary Figure S2C) and gain of mesenchymal markers (e.g., MMP9, Twist, and vimentin; Supplementary Figure S2D). Collectively, these events culminated in the redistribution of E-cadherin (Supplementary Figure S2E) and β-catenin (Supplementary Figure S2F) from the plasma membrane to the cytoplasm, consistent with the ability of TGF-β to induce EMT programs in luminal breast cancers.
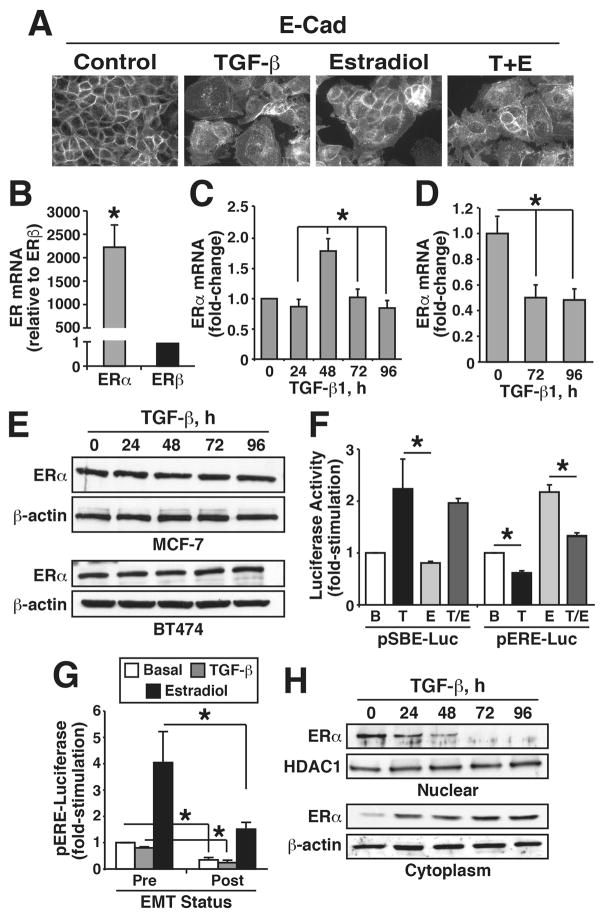
Induction of EMT programs by TGF-β promotes ER-α accumulation in the cytoplasm of MCF-7 cells
We next investigated the interplay between TGF-β and ER-α in regulating EMT programs in MCF-7 cells, especially in light of the ability of TGF-β to inhibit ER-α signaling and vice versa [28]. In doing so, we first determined whether ER-α signaling impacted the coupling of TGF-β to EMT programs in MCF-7 cells. Although estradiol treatment had no obvious effect on E-cad localization in MCF-7 cells, hormone administration did suppress the ability of TGF-β to induce the redistribution of E-cadherin from the plasma membrane (Figure 2A). ER-α was the predominant estrogen receptor expressed in MCF-7 (Figure 2B) and BT474 (Supplementary Figure S3A), indicating that the actions of estrogen are mediated entirely by ER-α in these breast cancer cells. As such, we also monitored the impact of TGF-β on ER-α expression in MCF-7 and BT474 cells. Figure 2C shows that TGF-β transiently increased the synthesis of ER-α transcripts when MCF-7 cells were propagated in 2D-cultures, an event that also trended to occur in BT474 cells (Supplementary Figure S3B). Conversely, ER-α transcript levels were dramatically repressed when MCF-7 organoids were stimulated with TGF-β in 3D-cultures (Figure 2D). Although TGF-β clearly regulated ER-α transcription, activation of the TGF-β pathway had little-to-no effect on ERα protein expression in both MCF-7 and BT474 cells (Figure 2E) despite remaining competent to inhibit luciferase expression driven by an estrogen-response element (ERE; Figure 2F and Supplementary Figure S3C). The antagonist activities of TGF-β on ER-α signaling are magnified in post-EMT MCF-7 cells as compared to their pre-EMT counterparts (Figure 2G). Mechanistically, we observed TGF-β stimulation of EMT programs to rapidly promote ER-α translocation from the nucleus to the cytoplasm, resulting in ER-α being entirely excluded from the nucleus by 72 h (Figure 2H). Collectively, these findings suggest that TGF-β and its stimulation of EMT programs inhibit the genomic functions of ER-α by inducing its cytoplasmic sequestration.
Figure 2.
Induction of EMT programs by TGF-β promotes ER-α accumulation in the cytoplasm of MCF-7 cells. (A) MCF-7 cells were treated with either TGF-β1 (5ng/ml), estradiol (1 nM), or both agonists for 96 h as indicated. Afterward, the cells were fixed in paraformaldehyde and processed for indirect E-cad immunofluorescence. Images are representative of 3-independent experiments (X 400). (B and C) MCF-7 cells were treated with TGF-β1 (5 ng/ml) in either 2D- (B) or 3D- (C) cultures for 0–96 h, at which point differences in ER-α expression were measured by real-time PCR. Data are the mean fold-changes (±S.E.; n=3; *P< 0.05; Student’s t-test). (D) Differential mRNA expression of ER-α and ER-β in quiescent MCF-7 cells. Data are the mean (±S.E.; n=3; *P<0.05; Student’s t-test). (E) MCF-7 (top) and BT474 (bottom) cells were stimulated with TGF-β1 (5 ng/ml) for 0–96 h. Afterward, ER-α expression levels were monitored by immunoblotting. Images are representative of 4-independent experiments. (F) MCF-7 cells were transiently transfected overnight with either the pSBE- or pERE-luciferase reporter genes, as well as with the pCMV-β-galactosidase reporter gene to control for differences in transfection efficiency. Afterward, the transfectants were stimulated overnight either singly or in combination with TGF-β1 (T; 5 ng/ml) or estradiol (E; 0.1 nM) prior to measuring luciferase and β-gal activities. Data are the mean fold-changes (±S.E.; n=3;*P<0.05; Student’s t-test). (G) Pre- and post-EMT MCF-7 cells were transiently transfected overnight with pERE-luciferase and pCMV-β-gal-luciferase cDNAs, followed by 24 h treatment with either TGF-β1 (5 ng/ml) or estradiol (0.1 nM). Data are the mean fold-changes (±SE; n=3; *P<0.05; Student’s t-test). (H) MCF-7 cells were treated with TGF-β1 (5 ng/ml) for 0–96 h, at which point the expression of ER-α in cytoplasmic and nuclear cell fractions was determined by immunoblotting. Stripped blots were reprobed with antibodies to either HDAC1 or β-actin to monitor integrity of nuclear and cytoplasmic fractions, respectively. Images are representative of at least 3-independent experiments.
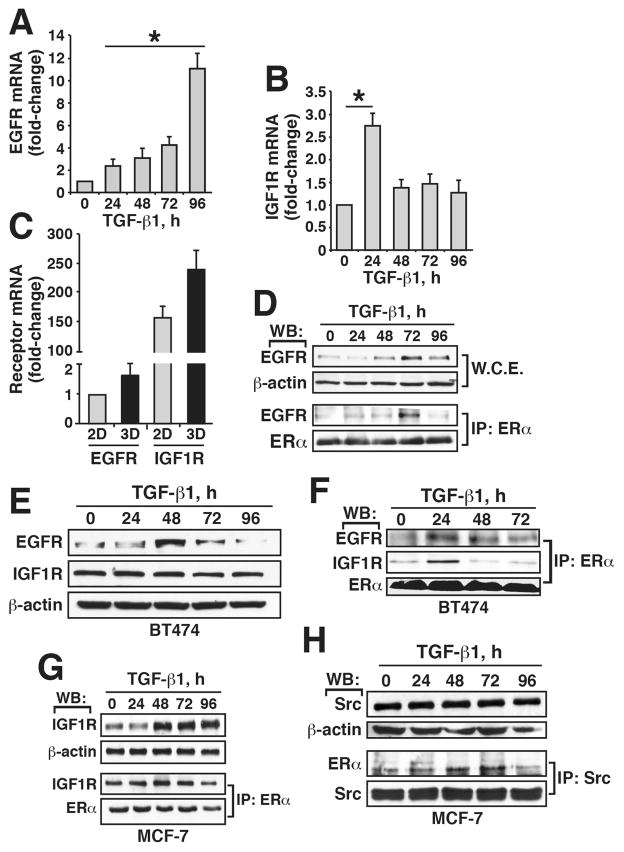
TGF-β stimulation of EMT promotes the interaction of ER-α with EGFR, IGF-1R and Src in MCF-7 and BT474 cells
Previous studies have shown the ability of cytoplasmic ER-α to interact physically with EGFR and IGF-1R, leading to the activation of MAP kinases and resistance to tamoxifen [9, 11–13]. Because EMT programs stimulated by TGF-β resulted in ER-α exclusion from the nucleus, we speculated that EMT programs may underlie the associations of ER-α with receptor tyrosine kinases (RTKs). To test this hypothesis, we determined the impact of TGF-β on the expression of EGFR and IGF-1R in luminal breast cancer cells. As shown in Figure 3A–C, TGF-β significantly stimulated the synthesis of EGFR and IGF-1R mRNA in MCF-7 cells propagated in either 2D- or 3D-cultures. Similar increases in EGFR transcript levels were also observed in BT474 cells stimulated with TGF-β (Supplementary Figure S4A), while the abnormally high levels of IGF-1R mRNA in BT474 cells (Supplementary Figure S4B) masked any apparent effects of TGF-β on IGF-1R transcript levels. We also observed TGF-β stimulation of MCF-7 and BT474 cells to induce the production of EGFR proteins, which were readily captured in ER-α immunocomplexes (Figure 3D–F). Likewise, IGF-1R was also readily captured in ER-α immunocomplexes isolated from MCF-7 and BT474 cells stimulated with TGF-β (Figure 3F and 3G). Finally, Src has been reported to facilitate the extranuclear activities and localization of ER-α in breast cancers [29]. Accordingly, we also found Src to associate with ER-α in a TGF-β-dependent manner in MCF-7 cells (Figure 3H), suggesting a potential role for Src in facilitating the extranuclear localization and function of ERα. Collectively, these findings suggest that TGF-β and EMT programs result in the upregulation of EGFR and IGF-1R, which form cytoplasmic complexes with ER-α and Src.
Figure 3.
TGF-β stimulation of EMT promotes the interaction of ER-α with EGFR, IGF-1R, and Src in MCF-7 and BT474 cells. (A and B) MCF-7 cells were treated with TGF-β1 (5 ng/ml) for 0–96 h, at which point EGFR (A) and IGF-1R (B) transcript levels were measured by real-time PCR. Data are the mean fold-changes (±S.E.; n=3;*P<0.05; Student’s t-test). (C) MCF-7 cells were propagated in 2D and 3D cultures. Afterward, total RNA was isolated and subjected to real-time PCR to monitor the expression of EGFR and IGF-1R. Data are the mean fold-changes (±S.E.; n=3; *P<0.05; Student’s t-test). (D) MCF-7 cells were treated with TGF-β1 (5 ng/ml) for 0–96 h, at which point detergent-solubilized extracts were immunoblotted with antibodies against either EGFR or β-actin as indicated (top). Additionally, ER-α immunocomplexes were captured and immunoblotted for EGFR and ER-α as indicated (bottom). Images are representative of 4-independent experiments. (E) BT474 cells were stimulated with TGF-β1 (5 ng/ml) as indicated, and subsequently were subjected to immunoblot analyses to monitor the expression of EGFR, IGF-1R, and β-actin. Images are representative of 3-individual experiments. (F and G) BT474 cells were stimulated with TGF-β1 (5 ng/ml) for 0–72 h, while MCF-7 cells were stimulated with TGF-β1 for 0–96 h. Afterward, detergent-solubilized extracts were immunoprecipitated with antibodies against ER-α and subsequently were immunoblotted with antibodies against IGF-1R and ER-α. Images are representative of at least 3-individual experiments. (H) MCF-7 cells were treated with TGF-β1 (5 ng/ml) for 0–96 h, at which point detergent-solubilized extracts were immunoblotted for Src or β-actin as indicated (top). Additionally, Src immunocomplexes were captured and immunoblotted for ER-α and Src as indicated (bottom). Images are representative of 4-independent experiments.
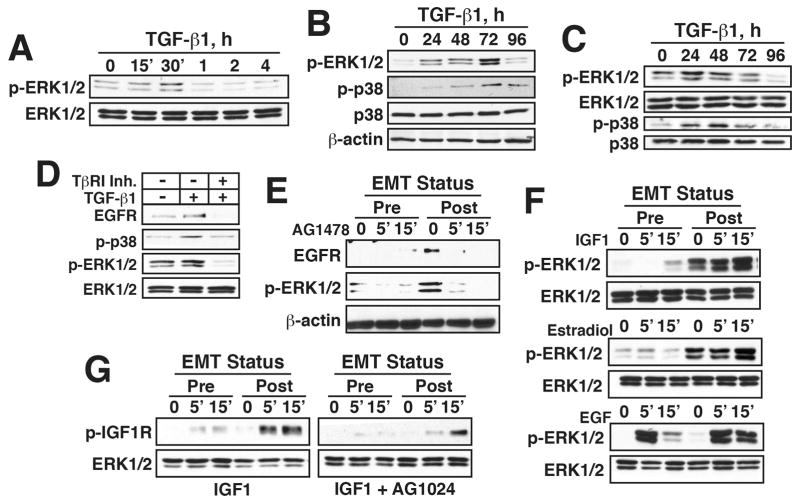
TGF-β stimulation of EMT programs enhances EGFR, IGF-1R, and MAP kinase signaling in MCF-7 and BT474 cells
The activation of MAP kinases by TGF-β is essential for its stimulation of EMT programs [4, 30]. Interestingly, nongenomic ER-α signaling is mediated in part through its ability to activate MAP kinases, thereby contributing to the acquisition of tamoxifen resistance in ER-positive breast cancer cells [31]. Given these parallels and reliance upon MAP kinases, we speculated that TGF-β and EMT programs would elicit the hyperactivation of MAP kinases downstream of upregulated expression of EGFR and IGF-1R in post-EMT cells, leading to the initiation of nongenomic ER-α signaling. In testing this hypothesis, we first monitored the activation status of MAP kinases in MCF-7 and BT474 cells when stimulated by TGF-β. Although TGF-β did indeed elicit a modest and transient activation of ERK1/2 in MCF-7 cells (Figure 4A), its ability to stimulate both ERK1/2 and p38 MAPK was greatly potentiated as MCF-7 and BT474 cells transitioned through the EMT program (Figure 4B and 4C). These events were specific for MAP kinases as no alterations in AKT phosphorylation were detected under both transient and prolonged TGF-β stimulations (data not shown). Interestingly, Figure 4D shows that administration of the TβR-I inhibitor II to inactivate TβR-I prevented both the upregulated expression of EGFR and the activation of MAP kinases (i.e., ERK1/2 and p38 MAPK) in MCF-7 cells stimulated with TGF-β. Moreover, administration of AG1478 to inactivate EGFR abrogated ERK1/2 activity in post-EMT MCF-7 cells (Figure 4E). Similar potentiation of ERK1/2 activity was also observed in post-EMT MCF-7 cells stimulated with either IGF-1, estradiol, or EGF (Figure 4F), a reaction partially dependent upon the greatly magnified activation of IGF-1R in these post-EMT cells (Figure 4G). Collectively, these findings demonstrate that EMT programs induced by TGF-β not only result in the robust stimulation of MAP kinases, but also elicit increased sensitivity and activation of post-EMT breast cancer cells to IGF1, estrogen, and EGF.
Figure 4.
TGF-β stimulation of EMT programs enhances EGFR, IGF-1R, and MAP kinase signaling in MCF-7 and BT474 cells. (A and B) MCF-7 cells were stimulated with TGF-β1 (5 ng/ml) as indicated. Afterward, the activation status of ERK1/2 and p38 MAPK was determined by immunoblotting. (C) BT474 cells were treated with TGF-β1 (5 ng/ml) for 0–96 h prior to monitoring the activation status ERK1/2 and p38 MAPK by immunoblotting. (D) MCF-7 cells were stimulated with TGF-β1 (5 ng/ml) in the absence or presence of the TβR-I inhibitor II (100 ng/ml) for 72 h. Afterward, the expression levels of EGFR and activation status of p38 MAPK and ERK1/2 were determined by immunoblotting. (E–G) Pre- and post-EMT MCF-7 cells were treated with AG1478 (1 μM; E), with IGF-1 (100 ng/ml; top), estradiol (0.1 nM; middle), and EGF (100 ng/ml; bottom; F), or with IGF-1 (100 ng/ml) in the absence or presence of AG1024 (1 μM; G) as indicated. Afterward, the expression levels of EGFR and activation status of ERK1/2 and IGF-1R were determined by immunoblotting as indicated. Data are representative images from at least 3-independent experiments.
TGF-β stimulation of EMT programs promotes tamoxifen resistance in MCF-7 cells
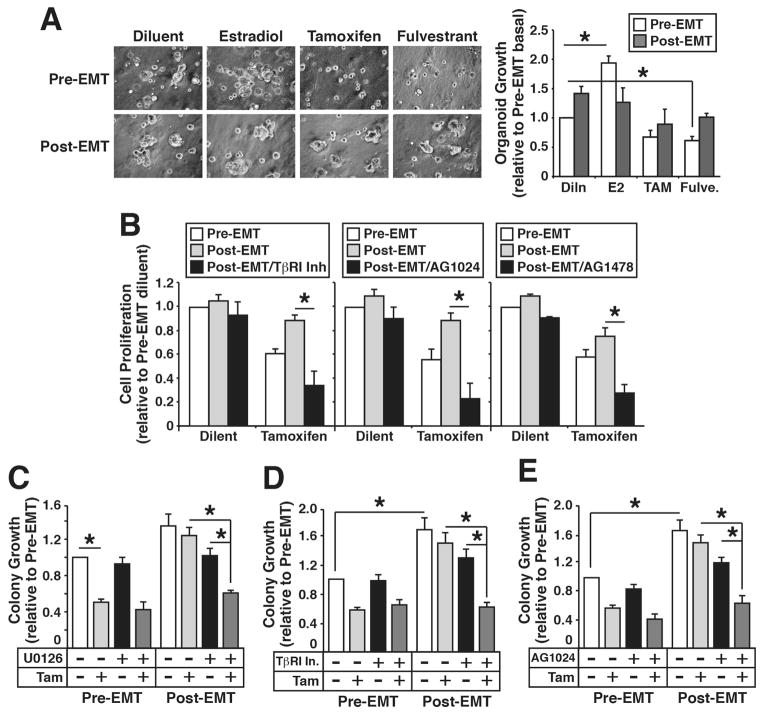
The aforementioned findings showed that TGF-β and its stimulation of EMT programs engendered the nuclear exclusion of ER-α, leading to its (i) physical interaction with EGFR, IGF-1R, and Src, and (ii) enhanced activation of MAP kinases (Figure 2–4). We next examined the functional consequences of these events on luminal breast cancer growth and their sensitivity to tamoxifen. In doing so, we first propagated pre- and post-EMT MCF-7 organoids in the absence of presence of ER-α modulators. Figure 5A shows that post-EMT MCF-7 organoids grew more robustly as compared to their pre-EMT counterparts; they were also significantly more sensitive to growth inhibition by administration of small molecule antagonists to either IGF-1R (i.e., AG1024; Supplementary Figure S5A) or EGFR (i.e., AG1478; Supplementary Figure S5B), findings consistent with the ability of post-EMT cells to upregulate their expression of IGF-1R and EGFR and activation of ERK1/2 (Figure 3 and 4). Additionally, post-EMT MCF-7 cells also exhibited significantly increased cell growth and decreased sensitivity to tamoxifen-induced cell death (Figure 5B). Importantly, co-administration of tamoxifen with small molecule inhibitors against either TβR-I (i.e., TβR-I inhibitor II), IGF-1R (i.e., AG1024), EGFR (i.e., AG1478), or MEK1/2 (i.e., U0126) restored MCF-7 cell sensitivity to tamoxifen as determined by MTS (Figure 5B) or clonogenic (Figure 5C–D) assays. Taken together, these results demonstrated that post-EMT cells acquire resistance to tamoxifen by upregulating EGFR and IGF-1R expression and MAP kinase activation, culminating in extranuclear localization and nongenomic signaling of ER-α in MCF-7 cells.
Figure 5.
TGF-β stimulation of EMT programs promotes tamoxifen resistance in MCF-7 cells. (A) Pre- and post-EMT MCF-7 organoids were treated with estradiol (0.1 nM), tamoxifen (0.1 μM), or fulvestrant (0.1 μM) for 8 days, at which point photomicrographs were captured and analyzed on Image J to assess differences in organoid growth. Images are representative of 3-independent experiments, while data are the mean fold-changes (±S.E.; n=3; *P<0.05; Student’s t-test; X 400). (B) Pre- and post-EMT MCF-7 cells were treated with tamoxifen (0.1 μM) in the absence or presence of TβR-I Inhibitor II (100 ng/ml; left), of AG1024 (1 μM; middle), or of AG1478 (1 μM; right) as indicated. Afterward, differences in cell growth and survival were analyzed by MTS assays. Data are the mean (±S.E.; n=3; *P<0.05; Student’s t-test). growth relative to untreated pre-EMT cells (* P< 0.05; Student’s t-test). (C–E) Pre- and post-EMT MCF-7 cells were treated with tamoxifen (0.1 μM) in the absence or presence of U0126 (10 μM; left), of TβR-I Inhibitor II (100 ng/ml; middle), or AG1024 (1 μM; right) for 10 days, at which point the number of surviving colonies in 11 random fields/plate was enumerated. Data are the mean (±S.E.; n=3; *P<0.05; Student’s t-test).
DISCUSSION
The induction of EMT programs by TGF-β plays important roles in driving the progression, dissemination, and recurrence of human breast cancers; these events also underlie the development, expansion, and self-renewal of cancer stem cells, as well as the acquisition of chemoresistant phenotypes [4, 22, 23]. Although EMT programs are more commonly associated with basal-like/TNBCs, we show herein that luminal A (e.g., MCF-7) and luminal B (e.g., BT474) breast cancer cells not only undergo EMT in response to TGF-β, but that they also exhibit diminished sensitivity to tamoxifen that results from the (i) upregulated expression of EGFR and IGF-1R, which interact physically with ER-α; (ii) hyperactivation states of MAP kinases (e.g., ERK1/2 and p38 MAPK); and (iii) extranuclear exclusion and nongenomic functions of ER-α. Importantly, the enhanced tumorigenic activities displayed by post-EMT cells were readily reversed by co-administration of tamoxifen with small molecule inhibitors against either TβR-I (i.e., TβR-I inhibitor II), IGF-1R (i.e., AG1024), EGFR (i.e., AG1478), or MEK1/2 (i.e., U0126), thereby laying the foundation for future investigations related to how inactivating EMT programs can be harnessed to improve the clinical outcomes of breast cancer patients.
Several studies previously implicated the nongenomic actions of ER-α in promoting tamoxifen resistance and disease progression [9, 11–13, 32]. For instance, the aberrant expression of truncated MTA1 mutants that remain competent to bind ER-α and sequester it in the cytoplasm clearly contribute to the generation of nongenomic ER-α activity [14]. Indeed, MTA1 expression inactivates hormone-induced nuclear translocation of ER-α, an event that enhances tumor progression and correlates with a loss of ER-α in the nucleus [14]. Along these lines, ER-α expression and activity also require interactions with growth factor signaling systems to enable luminal breast cancer cells to become insensitive to ER-α modulating agents. For instance, tamoxifen-resistant MCF-7 cells house cytoplasmic complexes comprised of ER-α, EGFR, and Src that elicit hyperactivation of MAP kinases by either EGF or estradiol. Consequently, targeted inactivation of either Src, EGFR, or MAPK not only restores ER-α to the nucleus, but also reestablishes the antitumor activities of tamoxifen in ER-positive tumors [12, 32]. Besides its ability to bind EGFR, ER-α also complexes with the IGF-1R at the cell membrane, an interaction involving the adaptor protein Shc [31, 32]. Moreover, tamoxifen-resistant breast cancer cells can also undergo RTK switching as a means to evade targeted inactivation of either EGFR or IGF-1R, thereby preserving nongenomic ER-α signaling [12]. It should be noted that RTK switching is a mechanism associated TGF-β and its stimulation of EMT programs [33]. Given the parallels between the aforementioned findings and those presented herein, it is tempting to speculate that EMT programs function as essential drivers of nongenomic ER-α signaling and disease progression in luminal breast cancer cells. Future studies need to determine the exact molecular mechanisms whereby TGF-β and EMT programs elicit extranuclear exclusion of ER-α; they also need to explore the linkages between EMT programs and ER-α mutations in regulating metastasis and disease recurrence.
As mentioned previously, EMT programs are closely associated with the acquisition of drug-resistant phenotypes [4, 22, 23]. Indeed, tamoxifen-resistant MCF-7 cells exhibit post-EMT morphologies (i.e., mesenchymal-/fibroblastoid-like) that reflect a loss of E-cadherin expression and a gain of β-catenin signaling, events that were readily reversed following administration of EGFR inhibitors [34]. A similar dependence upon EMT programs was observed in pancreatic cancers as they acquired resistance to gemcitabine, 5-fluorouracil, and cisplatin, a reaction driven by the upregulated expression of Zeb1. Indeed, genetic inactivation of Zeb1 in post-EMT, chemoresistant pancreatic cancer cells was sufficient to induce a mesenchymal-to-epithelial transition (MET) that reinstated cellular sensitivity to conventional chemotherapeutic agents [35]. Likewise, resistance to EGFR and FGFR3 inhibitors in cancers of the bladder coincides with their completion of EMT programs engendered by the loss of miR-200 family member expression. Importantly, restoring miR-200 expression in post-EMT bladder cancer cells not only induced their undertaking of MET programs, but also reactivated their sensitivity to EGFR and FGFR3 inhibitors [36]. Our studies herein reinforce the central importance of EMT programs to elicit chemoresistance in developing and recurring cancers, particularly those arising in the breast. Moreover, we established TGF-β and EMT programs as drivers of tamoxifen resistance and nongenomic ER-α signaling in luminal breast cancers; we also provide a new and potentially impactful approach to eliminate tamoxifen-resistant, post-EMT breast cancer cells through the combined administration of tamoxifen with inhibitors against either TβR-I, EGFR, IGF-1R, or MEK1/2, thereby restoring the effectiveness of anti-hormone therapies in ER-positive tumors.
Supplementary Material
Acknowledgments
Financial support and sponsorship
Research support was provided in part by the National Institutes of Health to W.P.S. (CA129359, CA177069, and CA194518).
Footnotes
Conflict of Interest: The authors have declared that no conflict of interest exists.
Ethics approval
The study was approved by Institutional Scientific and Ethical Committees.
References
- 1.Massague J. TGFβ signalling in context. Nat Rev Mol Cell Biol. 2012;13:616–30. doi: 10.1038/nrm3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tian M, Neil JR, Schiemann WP. Transforming growth factor-β and the hallmarks of cancer. Cell Signal. 2011;23:951–62. doi: 10.1016/j.cellsig.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian M, Schiemann WP. The TGF-β paradox in human cancer: An update. Future Oncol. 2009;5:259–71. doi: 10.2217/14796694.5.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parvani JG, Taylor MA, Schiemann WP. Noncanonical TGF-β signaling during mammary tumorigenesis. J Mammary Gland Biol Neoplasia. 2011;16:127–46. doi: 10.1007/s10911-011-9207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor MA, Parvani JG, Schiemann WP. The pathophysiology of epithelial-mesenchymal transition induced by transforming growth factor-β in normal and malignant mammary epithelial cells. J Mammary Gland Biol Neoplasia. 2010;15:169–90. doi: 10.1007/s10911-010-9181-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arendt LM, Kuperwasser C. Form and function: how estrogen and progesterone regulate the mammary epithelial hierarchy. J Mammary Gland Biol Neoplasia. 2015;20:9–25. doi: 10.1007/s10911-015-9337-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finlay-Schultz J, Sartorius CA. Steroid hormones, steroid receptors, and breast cancer stem cells. J Mammary Gland Biol Neoplasia. 2015;20:39–50. doi: 10.1007/s10911-015-9340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali S, Coombes RC. Estrogen receptor α in human breast cancer: occurrence and significance. J Mammary Gland Biol Neoplasia. 2000;5:271–81. doi: 10.1023/a:1009594727358. [DOI] [PubMed] [Google Scholar]
- 9.Ali S, Coombes RC. Endocrine-responsive breast cancer and strategies for combating resistance. Nat Rev Cancer. 2002;2:101–12. doi: 10.1038/nrc721. [DOI] [PubMed] [Google Scholar]
- 10.Osborne CK, Fuqua SA. Mechanisms of tamoxifen resistance. Breast Cancer Res Treat. 1994;32:49–55. doi: 10.1007/BF00666205. [DOI] [PubMed] [Google Scholar]
- 11.Song RX, Barnes CJ, Zhang Z, Bao Y, Kumar R, Santen RJ. The role of Shc and insulin-like growth factor 1 receptor in mediating the translocation of estrogen receptor α to the plasma membrane. Proc Natl Acad Sci U S A. 2004;101:2076–81. doi: 10.1073/pnas.0308334100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song RX, Chen Y, Zhang Z, Bao Y, Yue W, Wang JP, Fan P, Santen RJ. Estrogen utilization of IGF-1-R and EGF-R to signal in breast cancer cells. J Steroid Biochem Mol Biol. 2010;118:219–30. doi: 10.1016/j.jsbmb.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song RX, Zhang Z, Chen Y, Bao Y, Santen RJ. Estrogen signaling via a linear pathway involving insulin-like growth factor I receptor, matrix metalloproteinases, and epidermal growth factor receptor to activate mitogen-activated protein kinase in MCF-7 breast cancer cells. Endocrinology. 2007;148:4091–101. doi: 10.1210/en.2007-0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar R, Wang RA, Mazumdar A, Talukder AH, Mandal M, Yang Z, Bagheri-Yarmand R, Sahin A, Hortobagyi G, Adam L, Barnes CJ, Vadlamudi RK. A naturally occurring MTA1 variant sequesters oestrogen receptor-α in the cytoplasm. Nature. 2002;418:654–7. doi: 10.1038/nature00889. [DOI] [PubMed] [Google Scholar]
- 15.Parvani JG, Davuluri G, Wendt MK, Espinosa C, Tian M, Danielpour D, Sossey-Alaoui K, Schiemann WP. Deptor enhances triple-negative breast cancer metastasis and chemoresistance through coupling to survivin expression. Neoplasia. 2015;17:317–28. doi: 10.1016/j.neo.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tian M, Schiemann WP. Preclinical efficacy of cystatin C to target the oncogenic activity of transforming growth factor β in breast cancer. Transl Oncol. 2009;2:174–83. doi: 10.1593/tlo.09145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian M, Schiemann WP. PGE2 receptor EP2 mediates the antagonistic effect of COX-2 on TGF-β signaling during mammary tumorigenesis. FASEB J. 2010;24:1105–16. doi: 10.1096/fj.09-141341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wrana JL, Attisano L, Carcamo J, Zentella A, Doody J, Laiho M, Wang XF, Massague J. TGFβ signals through a heteromeric protein kinase receptor complex. Cell. 1992;71:1003–14. doi: 10.1016/0092-8674(92)90395-s. [DOI] [PubMed] [Google Scholar]
- 19.Hall JM, McDonnell DP. The estrogen receptor β-isoform (ERβ) of the human estrogen receptor modulates ERα transcriptional activity and is a key regulator of the cellular response to estrogens and antiestrogens. Endocrinology. 1999;140:5566–78. doi: 10.1210/endo.140.12.7179. [DOI] [PubMed] [Google Scholar]
- 20.Veeman MT, Slusarski DC, Kaykas A, Louie SH, Moon RT. Zebrafish prickle, a modulator of noncanonical Wnt/Fz signaling, regulates gastrulation movements. Curr Biol. 2003;13:680–5. doi: 10.1016/s0960-9822(03)00240-9. [DOI] [PubMed] [Google Scholar]
- 21.Schiemann WP, Pfeifer WM, Levi E, Kadin ME, Lodish HF. A deletion in the gene for transforming growth factor β type I receptor abolishes growth regulation by transforming growth factor β in a cutaneous T-cell lymphoma. Blood. 1999;94:2854–61. [PubMed] [Google Scholar]
- 22.Chaffer CL, San Juan BP, Lim E, Weinberg RA. EMT, cell plasticity and metastasis. Cancer Metastasis Rev. 2016;35:645–54. doi: 10.1007/s10555-016-9648-7. [DOI] [PubMed] [Google Scholar]
- 23.Wendt MK, Tian M, Schiemann WP. Deconstructing the mechanisms and consequences of TGF-β-induced EMT during cancer progression. Cell Tissue Res. 2012;347:85–101. doi: 10.1007/s00441-011-1199-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morrison CD, Parvani JG, Schiemann WP. The relevance of the TGF-β paradox to EMT-MET Programs. Cancer Lett. 2013;341:30–40. doi: 10.1016/j.canlet.2013.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor MA, Amin J, Kirschmann DA, Schiemann WP. Lysyl oxidase contributes to mechanotransduction-mediated regulation of transforming growth factor-β signaling in breast cancer cells. Neoplasia. 2011;13:406–18. doi: 10.1593/neo.101086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei SC, Fattet L, Tsai JH, Guo Y, Pai VH, Majeski HE, Chen AC, Sah RL, Taylor SS, Engler AJ, Yang J. Matrix stiffness drives epithelial-mesenchymal transition and tumour metastasis through a TWIST1-G3BP2 mechanotransduction pathway. Nat Cell Biol. 2015;17:678–88. doi: 10.1038/ncb3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilbert PM, Weaver VM. Cellular adaptation to biomechanical stress across length scales in tissue homeostasis and disease. Semin Cell Dev Biol. 2017;67:141–152. doi: 10.1016/j.semcdb.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Band AM, Laiho M. Crosstalk of TGF-β and estrogen receptor signaling in breast cancer. J Mammary Gland Biol Neoplasia. 2011;16:109–15. doi: 10.1007/s10911-011-9203-7. [DOI] [PubMed] [Google Scholar]
- 29.Song RX, Zhang Z, Santen RJ. Estrogen rapid action via protein complex formation involving ERα and Src. Trends Endocrinol Metab. 2005;16:347–53. doi: 10.1016/j.tem.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 30.Xie L, Law BK, Chytil AM, Brown KA, Aakre ME, Moses HL. Activation of the Erk pathway is required for TGF-β1-induced EMT in vitro. Neoplasia. 2004;6:603–10. doi: 10.1593/neo.04241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Santen RJ, Fan P, Zhang Z, Bao Y, Song RX, Yue W. Estrogen signals via an extra-nuclear pathway involving IGF-1R and EGFR in tamoxifen-sensitive and -resistant breast cancer cells. Steroids. 2009;74:586–94. doi: 10.1016/j.steroids.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 32.Fan P, Wang J, Santen RJ, Yue W. Long-term treatment with tamoxifen facilitates translocation of estrogen receptor α out of the nucleus and enhances its interaction with EGFR in MCF-7 breast cancer cells. Cancer Res. 2007;67:1352–60. doi: 10.1158/0008-5472.CAN-06-1020. [DOI] [PubMed] [Google Scholar]
- 33.Thomson S, Petti F, Sujka-Kwok I, Mercado P, Bean J, Monaghan M, Seymour SL, Argast GM, Epstein DM, Haley JD. A systems view of epithelial-mesenchymal transition signaling states. Clin Exp Metastasis. 2011;28:137–55. doi: 10.1007/s10585-010-9367-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hiscox S, Jiang WG, Obermeier K, Taylor K, Morgan L, Burmi R, Barrow D, Nicholson RI. Tamoxifen resistance in MCF7 cells promotes EMT-like behaviour and involves modulation of β-catenin phosphorylation. Int J Cancer. 2006;118:290–301. doi: 10.1002/ijc.21355. [DOI] [PubMed] [Google Scholar]
- 35.Arumugam T, Ramachandran V, Fournier KF, Wang H, Marquis L, Abbruzzese JL, Gallick GE, Logsdon CD, McConkey DJ, Choi W. Epithelial to mesenchymal transition contributes to drug resistance in pancreatic cancer. Cancer Res. 2009;69:5820–8. doi: 10.1158/0008-5472.CAN-08-2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McConkey DJ, Choi W, Marquis L, Martin F, Williams MB, Shah J, Svatek R, Das A, Adam L, Kamat A, Siefker-Radtke A, Dinney C. Role of epithelial-to-mesenchymal transition (EMT) in drug sensitivity and metastasis in bladder cancer. Cancer Metastasis Rev. 2009;28:335–44. doi: 10.1007/s10555-009-9194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.