Abstract
Background: Resistance of Staphylococcus aureus to commonly used antibiotics is linked to their ability to acquire and disseminate antimicrobial-resistant determinants in nature, and the marine environment may serve as a reservoir for antibiotic-resistant bacteria. This study determined the antibiotic sensitivity profile of S. aureus isolated from selected beach water and intertidal beach sand in the Eastern Cape Province of South Africa. Methods: Two hundred and forty-nine beach sand and water samples were obtained from 10 beaches from April 2015 to April 2016. Staphylococcus aureus was isolated from the samples using standard microbiological methods and subjected to susceptibility testing to 15 antibiotics. Methicillin-resistant Staphylococcus aureus (MRSA) was detected by susceptibility to oxacillin and growth on Brilliance MRSA II agar. Antibiotic resistance genes including mecA, femA rpoB, blaZ, ermB, ermA, ermC, vanA, vanB, tetK and tetM were screened. Results: Thirty isolates (12.3%) were positive for S. aureus by PCR with over 50% showing phenotypic resistance to methicillin. Resistance of S. aureus to antibiotics varied considerably with the highest resistance recorded to ampicillin and penicillin (96.7%), rifampicin and clindamycin (80%), oxacillin (73.3%) and erythromycin (70%). S. aureus revealed varying susceptibility to imipenem (96.7%), levofloxacin (86.7%), chloramphenicol (83.3%), cefoxitin (76.7%), ciprofloxacin (66.7%), gentamycin (63.3%), tetracycline and sulfamethoxazole-trimethoprim (56.7%), and vancomycin and doxycycline (50%). All 30 (100%) S. aureus isolates showed multiple antibiotic-resistant patterns (resistant to three or more antibiotics). The mecA, femA, rpoB, blaZ, ermB and tetM genes were detected in 5 (22.7%), 16 (53.3%), 11 (45.8%), 16 (55.2%), 15 (71.4%), and 8 (72.7%) isolates respectively; Conclusions: Results from this study indicate that beach water and sand from the Eastern Cape Province of South Africa may be potential reservoirs of antibiotic-resistant S. aureus which could be transmitted to exposed humans and animals.
Keywords: S. aureus, antibiotic resistance, beaches, multiple-antibiotic resistance
1. Introduction
Staphylococcus aureus are Gram-positive cocci ranging from 0.5 to 1.5 μm in diameter, which may or may not contain a polysaccharide capsule. They are non-motile, non-spore forming facultative anaerobes that produce catalase and coagulase enzymes [1,2,3]. Yearly, microbial contamination of marine waters is predicted to be responsible for millions of gastrointestinal and acute respiratory infections (ARIs) [4], in addition to several skin infections [5]. Although S. aureus is typically a commensal organism, it has been known to be opportunistic. Invasive infections due to wound invasion can lead to numerous diseases, including scalded skin syndrome, abscesses, septicaemia, pneumonia, food poisoning, and toxic shock syndrome [6,7].
S. aureus is a potentially harmful human pathogen associated with both nosocomial and community-acquired infections, and it is increasingly becoming resistant to most antibiotics. Previous studies of S. aureus in marine environments have linked swimmers to the dissemination of S. aureus in marine water [8], via the shedding of the bacterium from their nose, skin, and respiratory tract [9]. On recreational beaches, S. aureus has occasionally been found in high abundance in both water and sand, which can be directly associated with bather density and human activities around the beach [9,10,11].
The human skin is directly exposed to infectious agents during swimming [12], and this exposure can lead to the colonization of S. aureus with the potential to invade the immune system and cause infections. There is a relationship between seawater exposure and S. aureus infection rates which suggests that recreational waters are potential sources of community-acquired S. aureus infections [9]. There is also a positive correlation between the concentrations of S. aureus and total staphylococci to skin, eye, and ear infections among bathers [13,14,15].
Methicillin-resistant Staphylococcus aureus (MRSA) is defined as any strain of S. aureus that has acquired resistance to methicillin and other beta lactam antibiotics [16] and it is responsible for several intractable infections in humans [17]. S. aureus and MRSA are both shed by swimmers [18,19] and have been reported in beach seawater and sand [18,20,21,22,23,24].
The resistance of S. aureus to methicillin is due to the production of penicillin-binding protein 2a (PBP2a), which is encoded by the mecA gene located on the mobile gene element (MGE) of the staphylococcal chromosome cassette mec (SCCmec), which has a low affinity for beta-lactam antibiotics [25,26].
The fact that S. aureus is resistant to multiple classes of antimicrobial agents in the hospital environment is a challenge currently facing clinicians when treating S. aureus infections [27]. This resistance stems from a history of over 50 years of recurrent adaptation of S. aureus to different antibiotics introduced into clinical practice over the years. Abuse of as well as indiscriminate use of antimicrobials are contributing factors to the spread of resistance [27]. Antibiotic-resistance genes are carried on plasmids and transposons, and can be transferred from one staphylococcal species to another and among other Gram-positive bacteria [28].
Antimicrobials act by targeting important bacterial functions such as cell wall synthesis (beta-lactams and glycopeptides), protein synthesis (aminoglycosides, tetracyclines, macrolides, lincosamides, chloramphenicol, mupirocin and fusidic acid), nucleic acid synthesis (quinolones), RNA synthesis (rifampin), and metabolic pathways such as folic acid metabolism (sulphonamides and trimethoprim) [29,30,31]. The overuse of antimicrobials elicits resistance either by the emergence of point mutations or by the acquisition of foreign resistance genes, which leads to alteration of the antimicrobial target and the degradation of the antimicrobial or reduction of the cell’s internal antimicrobial concentration [27,29,30,31].
This study was carried out to determine the antimicrobial resistance pattern of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus isolated from seawater and sand from selected beaches in the Eastern Cape Province of South Africa. We also determined whether isolates carried any antibiotic-resistance gene markers for methicillin, beta-lactams, tetracycline, vancomycin, erythromycin and rifampicin.
2. Materials and Methods
2.1. Study Site
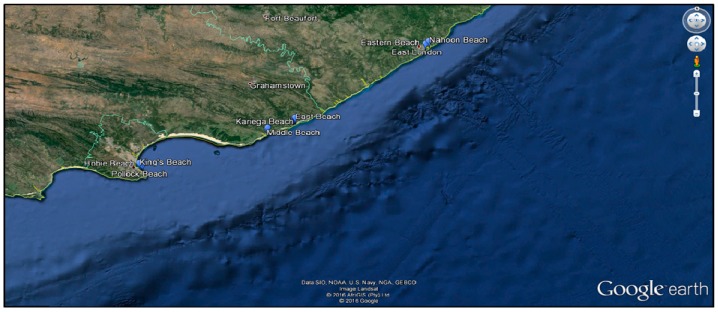
Sea water and sand samples were obtained from ten beaches in four major cities in the Eastern Cape Province; Nahoon beach (32°59′20.09′′ S 27°57′1.30′′ E), Eastern beach (33°0′32.00′′ S 27°55′31.02′′ E), East beach (33°36′6.07′′ S 26°54′4.94′′ E), West beach (33°36′18.80′′ S 26°53′56.53′′ E), Kelly’s beach (33°36′37.20′′ S 26°53′25.86′′ E), Kariega beach (33°41′1.05′′ S 26°40′59.28′′ E), Middle beach (33°41′21.16′′ S 26°40′36.09′′ E), King’s beach (33°58′16.92′′ S 25°38′49.87′′ E), Hobie beach (33°58′49.75′′ S 25°39′35.18′′ E), and Pollock beach (33°59′6.59′′ S 25°40′21.92′′ E) (Figure 1).
Figure 1.
Aerial view of sampling sites [32].
2.2. Sample Collection
A total of 245 (178 marine water, 67 marine sand) samples were collected monthly from 10 selected beaches in the Eastern Cape Province of South Africa between April 2015 and April 2016. Water samples were collected in 2 L sterile containers against an incoming wave. Beach sand was also collected in sterile 100 mL containers. Samples were transported at 4 °C and processed within 24 h.
Isolation and Molecular Confirmation of S. aureus
Sand samples were vigorously hand shaken in Phosphate Buffered Saline (PBS), where a ratio of 2 g of sand to 80 mL of PBS was used [20,33]. Both sand and water samples were enriched in tryptone soy broth and incubated at 37 °C for 24 h, followed by sub-culturing on mannitol salt agar (MSA), and further incubated at 37 °C for 24 h. Presumptive S. aureus, identified by the fermentation of mannitol (yellow colonies) were purified on nutrient agar. Presumptive isolates were stored in 25% glycerol at −80 °C.
Polymerase chain reaction (PCR) was used for confirmation of S. aureus as previously described [20]. DNA was extracted using the boiling method where 2 mL of overnight pure Nutrient broth cultures were transferred to sterile eppendorf tubes and centrifuged at 13,000 rpm for 3 min. The supernatant was discarded and cells re-suspended in 200 μL sterile distilled water. The cell solution was then heated at 100 °C in an Accu dri-block (Lasec, SA) for 10 min, followed by centrifugation at 13,000 rpm for 2 min to pellet the cells [34]. The supernatants were transferred to clean, sterile tubes and used directly as templates for PCR assay or stored at −20 °C for subsequent use.
A method previously described by Maes [35] was used for identification of S. aureus, based on the detection of a specie-specific nuc-gene. S. aureus ATCC 25923 was used as a positive control. Each 25 μL PCR reaction mix constituted 12.5 μL of 2X PCR master mix, 0.5 μL each of both reverse and forward primers (Table 1), 6.5 μL nuclease-free water and 5 μL of template DNA. PCR was conducted in a T1000 Touch Thermal Cycler (Bio-Rad, Hercules, CA, USA). Cycling conditions are shown in Table 1. The PCR products were separated by agarose gel electrophoresis in 1% agarose, stained with ethidium bromide. A 100 bp DNA ladder was included in each run.
Table 1.
Oligonucleotide primers and cycling conditions used in the molecular confirmation of S. aureus and antibiotic-resistance genes.
| Primer | Sequence (5′-3′) | Product Size (bp) | Cycling Conditions | Reference |
|---|---|---|---|---|
| nuc-F | GCGATTGATGGTGGATACGGT | 279 | Initial denaturation at 94 °C for 5 min, followed by 40 cycles of 94 °C for 45 s, 58 °C for 45 s and 72 °C for 90 s. Final extension at 72 °C for 10 min | [35] |
| nuc-R | AGCCAAGCCTTGACGAACTAAAGC | |||
| mecA-F | TCCAGGAATGCAGAAAGACCAAAGC | 499 | Initial denaturation at 94 °C for 3 min, followed by 40 cycles of 94 °C for 30 s, 59 °C for 30 s and 72 °C for 1 min. Final extension at 72 °C for 8 min. | [41] |
| mecA-R | GACACGATAGCCATCTTCATGTTGG | |||
| ermA-F | TATCTTATCGTTGAGAAGGGATT | 139 | Initial denaturation at 94 °C for 5 min, followed by 40 cycles of 94 °C for 40 s, 48 °C for 40 s and 72 °C for 90 s. Final extension at 72 °C for 8 min. | [42] |
| ermA-R | CTACACTTGGCTTAGGATGAAA | |||
| ermB-F | CTATCTGATTGTTGAAGAAGGATT | 142 | Initial denaturation at 94 °C for 5 min, followed by 40 cycles of 94 °C for 40 s, 47 °C for 40 s and 72 °C for 90 s. Final extension at 72 °C for 8 min. | [42] |
| ermB-R | GTTTACTCTTGGTTTAGGATGAAA | |||
| ermC-F | CTTGTTGATCACGATAATTTCC | 190 | Initial denaturation at 94 °C for 5 min, followed by 40 cycles of 94 °C for 40 s, 49 °C for 40 s and 72 °C for 90 s. Final extension at 72 °C for 8 min. | [42] |
| ermC-R | ATCTTTTAGCAAACCCGTATTC | |||
| blaZ-F | ACTTCAACACCTGCTGCTTTC | 173 | Initial denaturation at 94 °C for 3 min, followed by 35 cycles of 94 °C for 30 s, 49 °C for 30 s and 72 °C for 1 min. Final extension at 72 °C for 8 min. | [42] |
| blaZ-R | TGACCACTTTTATCAGCAACC | |||
| rpoB1-F | ACCGTCGTTTACGTTCTGTA | 460 | Initial denaturation at 94 °C for 5 min, followed by 40 cycles of 94 °C for 40 s, 45.5 °C for 40 s and 72 °C for 90 s. Final extension at 72 °C for 8 min. | [43] |
| rpoB2-R | TCAGTGATAGCATGTGTATC | |||
| tetM-F | AGTGGAGCGATTACAGAA | 158 | Initial denaturation at 94 °C for 3 min, followed by 40 cycles of 94 °C for 30 s, 45 °C for 30 s and 72 °C for 1 min. Final extension at 72 °C for 8 min. | [44] |
| tetM-R | CATATGTCCTGGCGTGTCTA | |||
| tetK-F | GTAGCGACAATAGGTAATAGT | 360 | Initial denaturation at 94 °C for 3 min, followed by 40 cycles of 94 °C for 30 s, 47 °C for 30 s and 72 °C for 1 min. Final extension at 72 °C for 8 min. | [44] |
| tetK-R | GTAGTGACAATAAACCTCCTA | |||
| vanA | GCGCGGTCCACTTGTAGATA | 314 | Initial denaturation at 94 °C for 3 min, followed by 35 cycles of 94 °C for 1 min, 56.5 °C for 1 min and 72 °C for 1 min. Final extension at 72 °C for 10 min. | [45] |
| vanA | TGAGCAACCCCCAAACAGTA | |||
| vanB | AGACATTCCGGTCGAGGAAC | 220 | Initial denaturation at 94 °C for 3 min, followed by 35 cycles of 94 °C for 1 min, 56.5 °C for 1 min and 72 °C for 1 min. Final extension at 72 °C for 10 min. | [45] |
| vanB | GCTGTCAATTAGTGCGGGAA | |||
| femA-F | AAAAAAGCACATAACAAGCG | 132 | Initial denaturation at 94 °C for 5 min, followed by 40 cycles of 94 °C for 40 s, 45.5 °C for 40 s and 72 °C for 90 s. Final extension at 72 °C for 8 min. | [40] |
| femA-R | GATAAAGAAGAAACCAGCAG |
2.3. Antimicrobial Susceptibility Testing
Isolates confirmed by PCR as S. aureus were subjected to antimicrobial susceptibility testing to 15 antibiotics. Profiling was performed by the Kirby-Bauer disk diffusion method on Mueller-Hinton agar according to Clinical and Laboratory Standards Institute guidelines [36,37]. An inoculum for each isolate was prepared by emulsifying colonies from an overnight pure culture in sterile normal saline (0.85%) in test tubes with the turbidity adjusted to 0.5 McFarland standard (0.5 mL of 1% w/v BaCl2 and 99.5 mL of 1% v/v H2SO4), equivalent to 1.0 × 108 cfu/mL. The bacterial suspension was uniformly streaked on Mueller Hinton agar plates using sterile swabs and left for 3 min prior to introduction of the antibiotics. Antibiotics commonly used for treatment of S. aureus infections were selected for this assay, namely penicillin, ampicillin, gentamycin, erythromycin, levofloxacin, ciprofloxacin, tetracycline, doxycycline, vancomycin, cefoxitin, imipenem, sulfamethoxazole-trimethoprim, clindamycin, rifampicin and chloramphenicol. Plates were incubated at 35 °C for 24 h, and the diameters of zone of inhibition were measured and results interpreted according to Clinical Laboratory Standards institute [37].
2.4. Detection of MRSA
2.4.1. Phenotypic
All isolates confirmed to be S. aureus by PCR were subjected to antibiotic susceptibility testing to oxacillin (5 μg) [37] by disc diffusion test as well as growth on Brilliance MRSA II agar [38], to determine phenotypic resistance to methicillin. Inoculated plates were incubated at 37 °C for 24 h [38]. All isolates that tested positive on Brilliance MRSA II agar (blue to violet colonies) or resistant by oxacillin disc were considered to be presumptive MRSA.
2.4.2. Molecular Confirmation of MRSA
Presumptive isolates from Brilliance MRSA II agar, as well as isolates that were phenotypically resistant to oxacillin, were further confirmed by PCR detection of the mecA gene (responsible for methicillin resistance) using specific primers (Table 1) as earlier described [20,39]. The femA gene, a factor essential for methicillin resistance, was also evaluated [40] by PCR using specific primers (Table 1). A 25 uL reaction was set up consisting of 12.5 μL master mix, 0.5 μL forward primer, 0.5 μL reverse primer, 6.5 μL nuclease-free water and 5 μL of DNA. PCR was conducted using a T1000 Touch Thermal Cycler (Bio-Rad, Johannesburg, SA, USA). The cycling conditions used for confirmation of the mecA and femA gene are shown in Table 1. The amplicons were separated using 1.5% agarose stained with ethidium bromide and visualized under a transilluminator (UVITEC Alliance 4.7, Bio-Active., Ltd., Bangkok, Thailand).
2.5. PCR Detection of Antibiotic Resistance Genes
Based on the phenotypic antibiotic resistance profiles, (29/30, 24/30, 22/30, 21/30, 17/30, 15/30) isolates showing resistance to β-lactam, rifampicin, methicillin, erythromycin, tetracycline, vancomycin respectively, were investigated for the presence of associated antibiotic-resistance genes (ARGs). These were blaZ, rpoB, mecA ermB, ermA, ermC, tetK, tetM, vanA and vanB genes respectively. The reactions were performed as singleplex PCRs in a total volume of 25 μL consisting of 12.5 μL 2X PCR master mix, 0.5 μL each of the forward and reverse primer, 6.5 μL nuclease-free water and 5 μL of template DNA performed in a T1000 Touch Thermal Cycler (Bio-Rad, Johannesburg, SA, USA). The amplicons were separated on 1.5% agarose stained with ethidium bromide, visualized and photographed using a transilluminator (UVITEC Alliance 4.7, Bio-Active., Ltd., Bangkok, Thailand). Table 1 shows the primer sequences used, and cycling conditions for PCR detection of S. aureus and antibiotic resistance gene markers.
3. Results
3.1. Molecular Identification of Staphylococcus aureus in Recreational Beach Water and Sand Samples
A total of 245 samples were screened; beach water (n = 178) and sand samples (n = 67) of which 143 isolates (one isolate from each sample) were presumptive by culture on MSA. A 12.3% (30/245) of the isolates were confirmed by PCR as S. aureus, with 12.4% (22/178) of isolates from seawater, and 11.9% (8/67) from marine sand. Of the 22 confirmed S. aureus isolates from seawater, 6 isolates each were from Middle beach and Eastern beach, 5 isolates from Nahoon beach, 2 each from Kariega beach and East beach and 1 isolate from West beach. Of the 8 confirmed S. aureus isolates from sand, 4 isolates were from Middle beach and 2 each were from East beach and Kariega beach respectively.
3.2. Antimicrobial Susceptibility Test (AST)
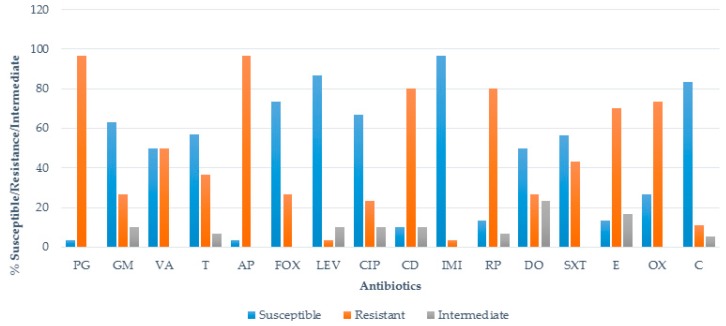
Antibiotic susceptibility of 30 S. aureus isolates revealed varying degrees of susceptibility patterns against the antimicrobial agents. Generally, cefoxitin 76.7% (23/30), chloramphenicol 83.3% (25/30), levofloxacin 86.7% (26/30), and imipenem 96.7% (29/30) were the most effective antibiotics to S. aureus. A low, ≥50% susceptibility was recorded to vancomycin and doxycycline (50%; 15/30), tetracycline and sulfamethoxazole-trimethoprim (56.7%; 17/30), gentamycin (63.3%; 19/30), and ciprofloxacin (66.7%; 20/30). A higher resistance to erythromycin (70%; 21/30) and clindamycin and rifampicin (80%, 24/30) was identified, with resistance to penicillin G and ampicillin the highest (each recording 96.7%; 29/30). The percentage of antimicrobial resistance of S. aureus isolates are shown in Figure 2.
Figure 2.
The percentage of antimicrobial resistance profiles of S. aureus isolates. PG = penicillin, GM = gentamicin, VA = vancomycin, T = tetracycline, AP = ampicillin, FOX = cefoxitin, LEV = levofloxacin, CIP = ciprofloxacin, CD = clindamycin, IMI = imipenem, RP = rifampicin, DO = doxycycline, SXT = sulfamethoxazole-trimethoprim, E = erythromycin, OX = oxacillin, C = chloramphenicol.
3.3. Phenotypic Detection of MRSA
A methicillin-resistant S. aureus isolate was defined as resistant by any of the two methods tested. Fifteen (50%) isolates showed phenotypic resistance to methicillin after culturing on selective media (Brilliance MRSA II agar) while 73.3% (22/30) of the isolates showed phenotypic resistance to oxacillin (Figure 2), which could be used as a proxy for determining methicillin resistance [46]. All those that were positive on Brilliance MRSA II agar were also positive for the oxacillin disc diffusion test.
3.4. Multiple Antibiotic Resistance (MAR)/MAR Phenotypes of S. aureus
All isolates tested were multi-drug resistant, (100%; 30/30) (resistant to three or more antimicrobials), with 3 isolates resistant to 12 of the 15 antibiotics tested. Resistance to 8 antibiotics was the most common, shown by 5 (16.7%) isolates, followed by resistance to 4 and 5 antibiotics recorded by 4 (13.3%) isolates each. Twenty-three different MAR patterns were observed from the 30 isolates. The most common of these were PG-GM-VA-T-AP-FOX-CIP-CD-RP-DO-SXT-E-OX, PG-VA-T-AP-FOX-CD-RP-DO-SXT-E-OX and PG-VA-AP-FOX-CD-RP-SXT-E-OX, observed in 3 (10%), 2 (6.7%), and 2 (6.7%) isolates, respectively.
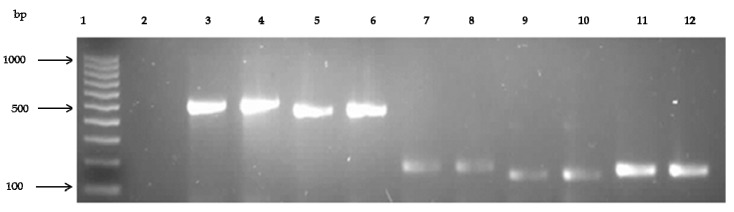
3.5. Prevalence of Antibiotic Resistance Genes
Generally, a total of five of 10 ARGs tested were detected in one or more resistant isolates, with higher frequencies recorded in isolates recovered from seawater. Of the ten ARGs tested (blaZ, mecA, rpoB, ermB, ermA, ermC, tetK, tetM, vanA and vanB), the blaZ gene, coding for resistance to beta-lactam antibiotics (penicillin & ampicillin), was detected in 16 (55.2%, n = 29) of the isolates, the mecA gene, coding for methicillin resistance was detected in 5 (22.7%, n = 22), the rpoB gene, coding for rifampicin resistance, was detected in 11 (45.8%, n = 24), the ermB gene, coding for erythromycin resistance, in 15 (71.4%, n = 21) and the tetM gene, coding for tetracycline resistance, was detected in 8 (72.7%, n = 11) of the isolates. However, other ARGs such as ermA, ermC, tetK, vanA and vanB investigated were absent in the isolates. Table 2 shows the various ARGs detected in beach sand and water while Figure 3 shows a representative gel of the PCR amplified products for these genes.
Table 2.
Antibiotic resistance genes detected in S. aureus isolates from beach sand and seawater.
| No. Resistant by Disc Diffusion | Associated ARG Tested | ARG Detected | ||
|---|---|---|---|---|
| Sand (%) | Water (%) | Total (%) | ||
| Ampicillin & Penicillin (n = 29) | blaZ | 4 (25%) | 12 (75%) | 16 (55.2%) |
| Methicillin (n = 22) | mecA | 1 (20%) | 4 (80%) | 5 (22.7%) |
| Rifampicin (n = 24) | rpoB | 2 (18.2%) | 9 (81.8%) | 11 (45.8%) |
| Erythromycin (n = 21) | ermB | 3 (20%) | 12 (80%) | 15 (71.4%) |
| Tetracycline (n = 11) | tetM | 1 (12.5%) | 7 (87.5%) | 8 (72.7%) |
Figure 3.
Representative gel showing PCR amplified products of antibiotic resistance genes of mecA, rpoB, blaZ, ermB and tetM separated on 1.5% agarose. Lane 1: 100 bp DNA ladder (Fermentas Life Sciences, Vilnius, Lithuania), Lane 2: negative control, Lane 3, 4: mecA (499 bp) positive isolates, Lane 5, 6: rpoB (460 bp) positive isolates, Lane 7, 8: blaZ (173 bp) positive isolates, Lane 9, 10: ermB (142 bp) positive isolates and Lane 11, 12: tetM (142 bp) positive isolates.
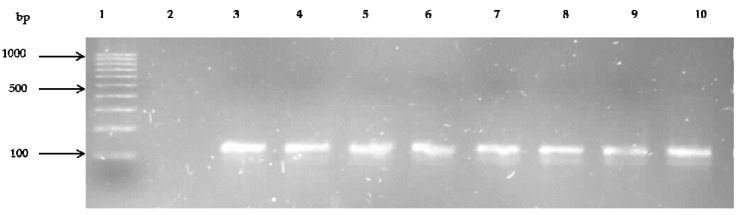
The femA gene, a factor also responsible for methicillin resistance [40], was identified in 53.3% (16/30) of the isolates. Figure 4 shows the gel electrophoresis of PCR amplified products for the femA gene.
Figure 4.
Representative gel showing PCR amplified products of femA gene separated on 1.5% agarose. Lane 1: 100 bp DNA ladder (Fermentas Life Sciences, Vilnius, Lithuania), Lane 2: negative control, Lane 3–10: femA (132 bp) positive isolate.
4. Discussion
Humans and animals have been reported as sources of antibiotic-resistant organisms in water environments and can transfer antibiotic resistance genes to other pathogens and naturally occurring water microbes through transposons, plasmids and integrons [47,48]. Bacteria isolated from beach sand, seawater and sediments have recorded resistance to various antimicrobials [48,49,50,51,52].
The occurrence of S. aureus and MRSA is on the rise, resulting in increased incidences of hospital-acquired and community-acquired infections worldwide, posing a major public health concern [53,54,55]. Moreover, microbial ecosystems can also be potentially altered by the presence of varying antibiotics of industrial origin, circulating in water environs [47]. S. aureus is one of the most successful and adaptable human pathogens due to its proficiency in acquiring antibiotic-resistant mechanisms and pathogenic determinants, leading to its emergence in both nosocomial and community settings [54]. Nosocomial colonisation of S. aureus and MRSA can go undetected, and signs of infection may only appear months after a patient is exposed to the infection. Infected patients may then serve as reservoirs for further transmission, especially as most of these strains carry SCCmec types coding for resistance to methicillin and other beta lactams [56].
To the best of our knowledge, this is the first study which has used a mixture of phenotypic and genotypic approaches simultaneously to determine the occurrence and antibiotic resistance profiles of S. aureus strains from beach water and sand in the study area. In this study, S. aureus was isolated from beach water and sand samples. Other studies have also reported this organism in marine water and/or sand [18,20,21,22,24,57,58,59], however, the frequency (12.2%) of isolation was lower in our study than observed in other studies [20,21,24]. This study only analyzed a single isolate for every sample, which could account for the lower detection frequency.
Of the isolates evaluated in this study, individual resistances of S. aureus to penicillin G and ampicillin was high (96.7%; 29/30). High resistance to these β-lactam antibiotics was not surprising, as ampicillin is one of the most commonly used antibiotics for treatment of infections in humans and animals [60], with penicillin developing resistance to S. aureus since the 1960s [61]. In addition, ampicillin-resistant isolates may cross-select for resistance to other beta-lactams [62]. Resistance to ampicillin may therefore indicate resistance of the isolates to other β-lactam antibiotics. This was observed in our study, as resistance to both ampicillin and penicillin occurred in equal proportion. Resistances observed to erythromycin, chloramphenicol, sulfamethoxazole-trimethoprim, and tetracycline were similar to that previously reported [21].
Given the relatively small number of isolates evaluated, a 50% vancomycin resistance was of concern, as this antibiotic is historically regarded as the antibiotic of final resort and the highest quality level antimicrobial for the treatment of genuine MRSA diseases [30]. The first case of a fully vancomycin-resistant S. aureus was described in Michigan, USA, in a renal dialysis patient [63]. The utilization of growth promoters such as tylosin, macrolide and avoparcin has been related to the occurrence of erythromycin and vancomycin resistance in S. aureus [64] in the environment, which might have then leached to marine waters. Based on the phenotypic identification of MRSA, 50% and 73.3% of the isolates were potentially MRSA by both methods. The poor specificity of the phenotypic methods in this study was not surprising, as higher specificity and sensitivity of these phenotypic methods have mostly been recorded in clinical isolates [38].
In this study, all S. aureus isolates were multidrug resistant. This point is worth noting, as it potentially could lead to failure in treatment therapy, prolonged illnesses, increased expenses for health care, and in serious cases, risk of death if humans are infected with such strains [65]. The transmission of resistance (R-factor), a plasmid-mediated genetic determinant, may be credited with the development of MAR among these isolates [62]. Studies have shown an upward pattern in the incidences of S. aureus isolates with multiple antibiotic resistance [66,67,68,69]. It has also been reported that S. aureus isolates with multiple antibiotic resistance attributes have a negative impact on the treatment of staphylococcal infections, especially in elderly, children, and immune-compromised individuals [70].
Generally, a total of five out of 10 ARGs tested were detected, with a higher frequency of detection in beach water compared to sand isolates. The higher frequency of detection in seawater could be because water is exposed to a greater variety of potential contaminants than sand. These may include runoffs from pharmaceutical, hospital, and industrial waste as well as farmlands [71,72]. Sources may also include antibiotic-resistant bacteria from poorly treated or untreated sewage, as final effluents of waste water treatment plants that may leach into seawater [52].
The blaZ gene is responsible for the production of β- lactamase enzyme, which confers resistance to β- lactam antibiotics such as penicillin and ampicillin [73]. This gene was only detected in small proportions compared to its phenotypic detection. Molecular confirmation identified the mecA gene only in five (22.7%) of the MRSA isolates detected by at least one of the phenotypic methods. The presence of this gene encodes a penicillin-binding protein 2a (PBP2a), responsible for methicillin resistance in staphylococci, with this protein, rendering a reduced affinity for β-lactam antibiotics [74]. Various studies have reported the occurrence of methicillin-resistant S. aureus from water sources, animal-derived food and humans [55,75,76]. MRSA has also been previously reported from marine waters [21,24] and waste water treatment plants [77]. Oxacillin has been proposed as a proxy antibiotic for testing susceptibility not only to methicillin and to all β-lactams [46], which could explain why all oxacillin-resistant isolates were not carrying the mecA gene. Phenotypic resistance observed to oxacillin in this study was probably achieved through other mechanisms [78], which may include alteration of the penicillin binding proteins, which brings about hyper-production of methicillinase or beta-lactamase [37,79,80].
The mode of resistance of rifampin is inhibition of the process of RNA polymerase [81]. Mutations on the gene encoding the β-subunit of RNA polymerase (rpoB gene) account for rifampin resistance (Rifr) [82,83,84]. In our study, this gene was detected in 45.8% (11/24) of the rifampicin-resistant S. aureus isolates. Erythromycin resistance in staphylococci is mainly facilitated by the erm genes, coding for erythromycin resistant methylase [85], with ermA and ermC reported as the most frequently detected erm gene associated with staphylococci in human infections [86]. Results from this study however, detected ermB as the only gene coding for erythromycin resistance. The high incidence (72.7%) of tetM in our study is similar to that (74.2%) earlier reported [87]. Another study has also reported the presence of both tetM and tetK gene from S. aureus isolates from public beaches [21].
The femA gene was detected in 53.3% (16/30) of the confirmed S. aureus isolates. This gene is a chromosomally encoded factor in Staphylococcus aureus, which is crucial for the expression of advanced methicillin resistance, encoding proteins which influence the level of methicillin resistance [88]. Finding femA gene in all mecA positive isolates is evidence that these isolates had a functional methicillin resistance. The detection of femA together with mecA by PCR has long been considered a reliable indicator in the identification of MRSA [89].
5. Conclusions
This study is the first to report the occurrence of antibiotic resistant S. aureus on recreational beaches in the Eastern Cape Province, South Africa. Our results show that public beaches in the study area may be potential reservoirs for transmission of antibiotic resistant S. aureus to beach goers, particularly those with skin lesions. Results from this study are unlikely to be unique to the Eastern Cape or South Africa and further studies are needed to determine the distribution and level of antibiotic-resistant S. aureus in other public beaches.
Acknowledgments
The authors are grateful to the South African Institute for Aquatic Biodiversity (SAIAB) and the National Research Foundation of South Africa for financially supporting the research. We also acknowledge Gunda Spingies for critical English editing.
Author Contributions
Olufemi Emmanuel Akanbi and Anthony Otigbu collected the samples and performed the experiments; Justine Fri and Anna Clarke conceived and designed the experiment; Henry Akum Njom and Anna A. Clarke supervised the whole study; Olufemi Emmanuel Akanbi and Henry Akum Njom analyzed the data and wrote the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Ho J., O’donoghue M.M., Boost M.V. Occupational exposure to raw meat: A newly-recognized risk factor for Staphylococcus aureus nasal colonization amongst food handlers. Int. J. Hyg. Environ. Health. 2014;217:347–353. doi: 10.1016/j.ijheh.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 2.O’Riordan K., Lee J.C. Staphylococcus aureus capsular polysaccharides. Clin. Microbiol. Rev. 2004;17:218–234. doi: 10.1128/CMR.17.1.218-234.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Witte W., Strommenger B., Klare I., Werner G. Antibiotic-resistant nosocomial pathogens. Part I: Diagnostic and typing methods. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004;47:352–362. doi: 10.1007/s00103-004-0810-y. [DOI] [PubMed] [Google Scholar]
- 4.Shuval H. Estimating the global burden of thalassogenic diseases: Human infectious diseases caused by wastewater pollution of the marine environment. J. Water Health. 2003;1:53–64. [PubMed] [Google Scholar]
- 5.Yau V., Wade T.J., de Wilde C.K., Colford J.M., Jr. Skin-related symptoms following exposure to recreational water: A systematic review and meta-analysis. Water Qual. Expos. Health. 2009;1:79–103. doi: 10.1007/s12403-009-0012-9. [DOI] [Google Scholar]
- 6.Moore P.C.L., Lindsay J.A. Genetic variation among hospital isolates of methicillin-sensitive Staphylococcus aureus: Evidence for horizontal transfer of virulence genes. J. Clin. Microbiol. 2001;39:2760–2767. doi: 10.1128/JCM.39.8.2760-2767.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyd E.F., Brüssow H. Common themes among bacteriophage-encoded virulence factors and diversity among the bacteriophages involved. Trends Microbiol. 2002;10:521–529. doi: 10.1016/S0966-842X(02)02459-9. [DOI] [PubMed] [Google Scholar]
- 8.Robinton E.D., Mood E.W. A quantitative and qualitative appraisal of microbial pollution of water by swimmers: A preliminary report. J. Hyg. 1966;64:489–499. doi: 10.1017/S0022172400040808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charoenca N., Fujioka R. Association of staphylococcal skin infections and swimming. Water Sci. Technol. 1995;31:11–17. [Google Scholar]
- 10.WHO . Guidelines for Safe Recreational Water Environments. Volume 1 World Health Organization; Geneva, Switzerland: 2003. Coastal and Fresh Waters. [Google Scholar]
- 11.Papadakis J.A., Mavridou A., Richardson S.C., Lampiri M., Marcelou U. Bather-related microbial and yeast populations in sand and seawater. Water Res. 1997;31:799–804. doi: 10.1016/S0043-1354(96)00377-6. [DOI] [Google Scholar]
- 12.Henrickson S.E., Wong T., Allen P., Ford T., Epstein P.R. Marine swimming-related illness: Implications for monitoring and environmental policy. Environ. Health Perspect. 2001;109:645–650. doi: 10.1289/ehp.01109645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabutti G., De Donno A., Bagordo F., Montagna M.T. Comparative survival of faecal and human contaminants and use of Staphylococcus aureus as an effective indicator of human pollution. Mar. Pollut. Bull. 2000;40:697–700. doi: 10.1016/S0025-326X(00)00007-2. [DOI] [Google Scholar]
- 14.Calderon R.L., Mood E.W., Dufour A.P. Health effects of swimmers and nonpoint sources of contaminated waters. Int. J. Environ. Health Res. 1991;1:21–31. doi: 10.1080/09603129109356701. [DOI] [PubMed] [Google Scholar]
- 15.Seyfried P.L., Tobin R.S., Brown N.E., Ness P.F. A prospective study of swimming-related illness. II. Morbidity and the microbiological quality of water. Am. J. Public Health. 1985;75:1071–1075. doi: 10.2105/AJPH.75.9.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stotts S.N., Nigro O.D., Fowler T.L., Fujioka R.S., Steward G.F. Virulence and antibiotic resistance gene combinations among Staphylococcus aureus isolated from coastal waters of Oahu, Hawaii. J. Young Investig. 2005;12:1–8. [Google Scholar]
- 17.McDougal L.K., Steward C.D., Killgore G.E., Chaitram J.M., McAllister S.K., Tenover F.C. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: Establishing a national database. J. Clin. Microbiol. 2003;41:5113–5120. doi: 10.1128/JCM.41.11.5113-5120.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plano L.R.W., Garza A.C., Shibata T., Elmir S.M., Kish J., Sinigalliano C.D., Gidley M.L., Miller G., Withum K., Fleming L.E., et al. Shedding of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus from adult and pediatric bathers in marine waters. BMC Microbiol. 2011;1:5. doi: 10.1186/1471-2180-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elmir S.M., Wright M.E., Abdelzaher A., Solo-Gabriele H.N., Fleming L.E., Miller G., Rybolowik M., Shih M.T., Pillai P., Copoer J.E., et al. Quantitative evaluation of bacteria released by bathers in marine water. Water Res. 2007;41:3–10. doi: 10.1016/j.watres.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodwin K.D., Pobuda M. Performance of CHROMagar Staph aureus and CHROMagar MRSA for detection of Staphylococcus aureus in beach water and sand-comparison of culture, agglutination, and molecular analyses. Water Res. 2009;43:4802–4811. doi: 10.1016/j.watres.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 21.Soge O.O., Meschke J.S., No D.B., Roberts M.C. Characterization of methicillin-resistant and methicillin-resistant coagulase-negative Staphylococcus spp. isolated from US West Coast public marine beaches. J. Antimicrob. Chemother. 2009;64:1148–1155. doi: 10.1093/jac/dkp368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tice A.D., Susan J.R. Meeting the challenges of methicillin-resistant Staphylococcus aureus with outpatient parenteral antimicrobial therapy. Clin. Infect. Dis. 2010;51:S171–S175. doi: 10.1086/653517. [DOI] [PubMed] [Google Scholar]
- 23.Shah A.H., Abdelzaher A.M., Phillips M., Hernandez R., Solo-Gabriele H.M., Kish J., Scorzetti G., Fell J.W., Diaz M.R., Scott T.M., et al. Indicator microbes correlate with pathogenic bacteria, yeasts and helminthes in sand at a subtropical recreational beach site. J. Appl. Microbiol. 2011;110:1571–1583. doi: 10.1111/j.1365-2672.2011.05013.x. [DOI] [PubMed] [Google Scholar]
- 24.Goodwin K.D., Melody M., Yiping C., Darcy E., Melissa M., John F.G. A multi-beach study of Staphylococcus aureus, MRSA, and enterococci in seawater and beach sand. Water Res. 2012;46:4195–4207. doi: 10.1016/j.watres.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Deurenberg R.H., Stobberingh E.E. The evolution of Staphylococcus aureus. Infect. Genet. Evol. 2008;8:747–763. doi: 10.1016/j.meegid.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 26.Hartman B.J., Tomasz A. Low-affinity penicillin-binding protein associated with beta-lactam resistance in Staphylococcus aureus. J. Bacteriol. 1984;158:513–516. doi: 10.1128/jb.158.2.513-516.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tavares A.L. Ph.D. Thesis. Universidade Nova de Lisboa; Lisbon, Portugal: Dec, 2014. Community-Associated Methicillin-Resistant Staphylococcus aureus (CA-MRSA) in Portugal: Origin, Epidemiology and Virulence. [Google Scholar]
- 28.Werckenthin C., Cardoso M., Martel J.L., Schwarz S. Antimicrobial resistance in staphylococci from animals with particular reference to bovine Staphylococcus aureus, porcine Staphylococcus hyicus and canine Staphylococcus intermedius. Vet. Res. 2001;32:341–362. doi: 10.1051/vetres:2001129. [DOI] [PubMed] [Google Scholar]
- 29.Alekshun M.N., Levy S.B. Molecular mechanisms of antibacterial multidrug resistance. Cell. 2007;128:1037–1050. doi: 10.1016/j.cell.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Tenover F.C., McDougal L.K., Goering R.V., Killgore G., Projan S.J., Patel J.B., Dunman P.M. Characterization of a strain of community-associated methicillin-resistant Staphylococcus aureus widely disseminated in the United States. J. Clin. Microbiol. 2006;44:108–118. doi: 10.1128/JCM.44.1.108-118.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wright G.D. Bacterial resistance to antibiotics: Enzymatic degradation and modification. Adv. Drug Deliv. Rev. 2005;57:1451–1470. doi: 10.1016/j.addr.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 32.GOOGLE MAPS . Google; 2016. [(accessed on 18 June 2016)]. Map of Eastern Cape Beaches. [Online] Available online: https://www.google.co.za/maps/search/eastern+cape+beaches+map+from+east+london+to+port+elizabeth/@33.9988012,22.5881698,2619m/data = !3m2!1e3!4b1?hl = en&authuser = 0. [Google Scholar]
- 33.Baums I.B., Goodwin K.D., Kiesling T., Wanless D., Fell J.W. Luminex detection of faecal indicators in river samples, marine recreational water, and beach sand. Mar. Pollut. Bull. 2007;54:521–536. doi: 10.1016/j.marpolbul.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Soumet C., Ermel G., Fach P., Colin P. Evaluation of different DNA extraction procedures for the detection of Salmonella from chicken products by polymerase chain reaction. Lett. Appl. Microbiol. 1994;19:294–298. doi: 10.1111/j.1472-765X.1994.tb00458.x. [DOI] [PubMed] [Google Scholar]
- 35.Maes N., Magdalena J., Rottiers S., De Gheldre Y., Struelens M. Evaluation of a triplex PCR assay to discriminate Staphylococcus aureus from coagulase-negative staphylococci and determine methicillin resistance from blood cultures. J. Clin. Microbiol. 2002;40:1514–1517. doi: 10.1128/JCM.40.4.1514-1517.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bauer A.W., Kirby W.M., Sherris J.C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am. J. Clin. Pathol. 1966;45:493–496. [PubMed] [Google Scholar]
- 37.Clinical Laboratory Standards Institute . Performance Standards for Antimicrobial Susceptibility Testing: Eighteenth Informational Supplement. Clinical Laboratory Standards Institute; Wayne, PA, USA: 2014. CLSI Document M100-S18. [Google Scholar]
- 38.Veenemans J., Verhulst C., Punselie R., Van Keulen P.H.J., Kluytmans J.A.J.W. Evaluation of brilliance MRSA 2 agar for detection of methicillin-resistant Staphylococcus aureus in clinical samples. J. Clin. Microbiol. 2013;51:1026–1027. doi: 10.1128/JCM.02995-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mason W.J., Blevins J.S., Beenken K., Wibowo N., Ojha N., Smeltzer M.S. Multiplex PCR protocol for the diagnosis of Staphylococcal infection. J. Clin. Microbiol. 2001;39:3332–3338. doi: 10.1128/JCM.39.9.3332-3338.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehrotra M., Wang G., Johnson W.M. Multiplex PCR for Detection of Genes for Staphylococcus aureus Enterotoxins, Exfoliative Toxins, Toxic Shock Syndrome Toxin 1, and Methicillin Resistance. J. Clin. Microbiol. 2000;38:1032–1035. doi: 10.1128/jcm.38.3.1032-1035.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmitz F.J., Jones M.E. Antibiotics for treatment of infections caused by MRSA and elimination of MRSA carriage. What are the choices? Int. J. Antimicrob. Agents. 1997;9:1–19. doi: 10.1016/S0924-8579(97)00027-7. [DOI] [PubMed] [Google Scholar]
- 42.Martineau F., Picard F.J., Lansac N., Menard C., Roy P.H., Ouellette M., Bergeron M.G. Correlation between the resistance genotype determined by multiplex PCR assays and the antibiotic susceptibility patterns of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob. Agents Chemother. 2000;44:231–238. doi: 10.1128/AAC.44.2.231-238.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aboshkiwa M., Rowland G., Coleman G. Nucleotide sequence of the Staphylococcus aureus RNA polymerase rpoB gene and comparison of its predicted amino acid sequence with those of other bacteria. Biochim. Biophys. Acta BBA Gene Struct. Express. 1995;1262:73–78. doi: 10.1016/0167-4781(95)00054-K. [DOI] [PubMed] [Google Scholar]
- 44.Strommenger B., Kettlitz C., Werner G., Witte W. Multiplex PCR assay for simultaneous detection of nine clinically relevant antibiotic resistance genes in Staphylococcus aureus. J. Clin. Microbiol. 2003;41:4089–4094. doi: 10.1128/JCM.41.9.4089-4094.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nam S., Kim M.J., Park C., Park J.G., Lee G.C. Detection and genotyping of vancomycin-resistant Enterococcus spp. by multiplex polymerase chain reaction in Korean aquatic environmental samples. Int. J. Hyg. Environ. Health. 2012;216:421–427. doi: 10.1016/j.ijheh.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 46.Kuehnert M.J., Hill H.A., Kupronis B.A., Tokars J.I., Solomon S.L., Jernigan D.B. Methicillin-resistant-Staphylococcus aureus hospitalizations, United States. Emerg. Infect. Dis. 2005;11:468. doi: 10.3201/eid1106.040831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baquero F.J.M., Rafael C. Antibiotics and antibiotic resistance in water environments. Curr. Opin. Biotechnol. 2008;19:260–265. doi: 10.1016/j.copbio.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 48.Oliveira A.J.C., de Franco P.T.R., Pinto A.B. Antimicrobial resistance of heterotrophic marine bacteria isolated from seawater and sands of recreational beaches with different organic pollution levels in southeastern Brazil: evidences of resistance dissemination. Environ. Monit. Assess. 2010;169:375–384. doi: 10.1007/s10661-009-1180-6. [DOI] [PubMed] [Google Scholar]
- 49.Manivasagan P., Rajaram G., Ramesh S., Ashokkumar S., Damotharan P. Occurrence and seasonal distribution of antibiotic resistance heterotrophic bacteria and physico-chemical characteristics of Muthupettai mangrove environment, southeast coast of India. J. Environ. Sci. Technol. 2011;4:139–149. [Google Scholar]
- 50.Mudryk Z., Perliński P., Skórczewski P. Detection of antibiotic resistant bacteria inhabiting the sand of non-recreational marine beach. Mar. Pollut. Bull. 2010;60:207–214. doi: 10.1016/j.marpolbul.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 51.Mudryk Z. Occurrence and distribution antibiotic resistance of heterotrophic bacteria isolated from a marine beach. Mar. Pollut. Bull. 2005;50:80–86. doi: 10.1016/j.marpolbul.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 52.Schwartz T.W., Kohenen W., Jansen B., Obst U. Detection of antibiotic resistant bacteria and their resistance genes in wastewater, surface water and drinking water biofilms. FEMS Microbiol Ecol. 2003;43:325–335. doi: 10.1111/j.1574-6941.2003.tb01073.x. [DOI] [PubMed] [Google Scholar]
- 53.David M.Z., Daum R.S. Community-Associated Methicillin-Resistant Staphylococcus aureus: Epidemiology and Clinical Consequences of an Emerging Epidemic. Clin. Microbiol. Rev. 2010;23:616–687. doi: 10.1128/CMR.00081-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zetola N., Francis J.S., Nuermberger E.L., Bishai W.R. Community-acquired meticillin-resistant Staphylococcus aureus: An emerging threat. Lancet Infect. Dis. 2005;5:275–286. doi: 10.1016/S1473-3099(05)70112-2. [DOI] [PubMed] [Google Scholar]
- 55.Klevens R.M., Morrison M.A., Nadle J., Petit S., Gershman K., Ray S., Harrison L.H., Lynfield R., Dumyati G., Townes J.M., et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- 56.Boyle-Vavra S., Robert S.D. Community-acquired methicillin-resistant Staphylococcus aureus: The role of Panton-Valentine leukocidin. Lab. Investig. 2007;87:3. doi: 10.1038/labinvest.3700501. [DOI] [PubMed] [Google Scholar]
- 57.Abdelzaher A.M., Wright M.E., Ortega C., Solo-Gabriele H.M., Miller G., Elmir S., Newman X., Shih P., Bonilla J.A., Bonilla T.D., et al. Presence of pathogens and indicator microbes at a non-point source subtropical recreational marine beach. Appl. Environ. Microbiol. 2010;76:724–732. doi: 10.1128/AEM.02127-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Levin-Edens E., Bonilla N., Meschke J.S., Roberts M.C. Survival of environmental and clinical strains of methicillin-resistant Staphylococcus aureus (MRSA) in marine and fresh waters. Water Res. 2011;45:5681–5686. doi: 10.1016/j.watres.2011.08.037. [DOI] [PubMed] [Google Scholar]
- 59.Yamahara K.M., Sassoubre L.M., Goodwin K.D., Boehm A.B. Occurrence and persistence of human pathogens and indicator organisms in beach sands along the California coast. Appl. Environ. Microbiol. 2011;78:1733–1745. doi: 10.1128/AEM.06185-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gundogan N., Citak S., Yucel N., Devren A. A note on the incidence and the antibiotic resistance of Staphylococcus aureus isolated from meat and chicken samples. Meat Sci. 2005;69:807–810. doi: 10.1016/j.meatsci.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 61.Chambers H.F., DeLeo F.R. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat. Rev. Microbiol. 2009;7:629–641. doi: 10.1038/nrmicro2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Akindolire M.A. Ph.D. Thesis. North West University; Mafikeng, North West Province, South Africa: 2013. Detection and Molecular Characterization of Virulence Genes in Antibiotic Resistant Staphylococcus aureus from Milk in the North West Province. [Google Scholar]
- 63.Bartley J. First case of VRSA identified in Michigan. Infect. Control Hosp. Epidemiol. 2002;23:480. doi: 10.1017/s0195941700082333. [DOI] [PubMed] [Google Scholar]
- 64.Boerlin P., Burnens A.P., Frey J., Kuhnert P., Nicolet J. Molecular epidemiology and genetic linkage of macrolide and aminoglycoside resistance in Staphylococcus intermedius of canine origin. Vet. Microbiol. 2001;79:155–169. doi: 10.1016/S0378-1135(00)00347-3. [DOI] [PubMed] [Google Scholar]
- 65.Tanwar J., Das S., Fatima Z., Hameed S. Multidrug resistance: An emerging crisis. Interdiscip. Perspect. Infect. Dis. 2014 doi: 10.1155/2014/541340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Skórczewski P., Jan Mudryk Z., Miranowicz J., Perlinski P., Zdanowicz M. Antibiotic resistance of Staphylococcus-like organisms isolated from a recreational sea beach on the southern coast of the Baltic Sea as one of the consequences of anthropogenic pressure. Int. J. Oceanogr. Hydrobiol. 2014;43:41–48. doi: 10.2478/s13545-014-0115-1. [DOI] [Google Scholar]
- 67.Ateba C.N., Mbewe M., Moneoang M.S., Bezuidenhout C.C. Antibiotic-resistant Staphylococcus aureus isolated from milk in the Mafikeng Area, North West province, South Africa. S. Afr. J. Sci. 2010;106:1–6. doi: 10.4102/sajs.v106i11/12.243. [DOI] [Google Scholar]
- 68.Pesavento G., Ducci B., Comodo N. Antimicrobial resistance profile of Staphylococcus aureus isolated from raw meat: A research for methicillin resistant Staphylococcus aureus (MRSA) Food Control. 2007;18:196–200. doi: 10.1016/j.foodcont.2005.09.013. [DOI] [Google Scholar]
- 69.Normanno G., La Salandra G., Dambrosio A., Quaglia N., Corrente M., Parisi A., Santagada G., Firinu A., Crisetti E., Celano G. Occurrence, characterization and antimicrobial resistance of entero-toxigenic Staphylococcus aureus isolated from meat and dairy products. Int. J. Food Microbiol. 2007;115:290–296. doi: 10.1016/j.ijfoodmicro.2006.10.049. [DOI] [PubMed] [Google Scholar]
- 70.Ito T., Okurna K., Ma X.X., Yuzawa H., Hiramatsu K. Insights on antibiotic resistance of Staphylococcus aureus from its whole genome: Genomic island SCC. Drug Resist. Updates. 2003;6:41–52. doi: 10.1016/S1368-7646(03)00003-7. [DOI] [PubMed] [Google Scholar]
- 71.Guardabassi L., Petersen A., Olsen J.E., Dalsgaard A. Antibiotic resistance in Acinetobacter sp. isolated from sewers receiving waste effluent from a hospital and a pharmaceutical plant. Appl. Environ. Microbiol. 1998;64:3499–3502. doi: 10.1128/aem.64.9.3499-3502.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kümmerer K. Drugs in the environment: Emission of drugs, diagnostic aids and disinfectants into wastewater by hospitals in relation to other sources—A review. Chemosphere. 2001;45:957–969. doi: 10.1016/S0045-6535(01)00144-8. [DOI] [PubMed] [Google Scholar]
- 73.Zscheck K.K., Murray B.E. Genes involved in the regulation of β-lactamase production in enterococci and staphylococci, Antimicrob. Agents Chemoth. 1993;37:1966–1970. doi: 10.1128/AAC.37.9.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee J.H. Methicillin (oxacillin)-resistant Staphylococcus aureus strains isolated from major food animals and their potential transmission to humans. Appl. Environ. Microbiol. 2003;69:6489–6494. doi: 10.1128/AEM.69.11.6489-6494.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kamal R.M., Bayourni M.A., Abd El Aal S.F.A. MRSA detection in raw milk, some dairy products and hands of dairy workers in Egypt, a mini-survey. Food Control. 2013;33:49–53. doi: 10.1016/j.foodcont.2013.02.017. [DOI] [Google Scholar]
- 76.Mirzaei H., Tofighi A., Sarabi H.K., Faraj1i M. Prevalence of Methicillin-Resistant Staphylococcus aureus in Raw Milk and Dairy Products in Sarab by Culture and PCR Techniques. J. Anim. Vet. Adv. 2011;10:3107–3111. [Google Scholar]
- 77.Börjesson S., Melin S., Matussek A., Lindgren P.E. A seasonal study of the mecA gene and Staphylococcus aureus including methicillin-resistant S. aureus in a municipal wastewater treatment plant. Water Res. 2009;43:925–932. doi: 10.1016/j.watres.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 78.Swenson J.M., Lonsway D., McAllister S., Thompson A., Jevitt L., Zhu W., Patel J.B. Detection of mecA-mediated resistance using reference and commercial testing methods in a collection of Staphylococcus aureus expressing borderline oxacillin MICs. Diagn. Microbiol. Infect. Dis. 2007;58:33–39. doi: 10.1016/j.diagmicrobio.2006.10.022. [DOI] [PubMed] [Google Scholar]
- 79.Oliveira D.C., de Lencastre H. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2002;46:2155–2161. doi: 10.1128/AAC.46.7.2155-2161.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chambers H.F. Methicillin resistance in staphylococci: Molecular and biochemical basis and clinical implications. Clin. Microbiol. Rev. 1997;10:781–791. doi: 10.1128/cmr.10.4.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wehrli W. Rifampin: Mechanisms of action and resistance. Rev. Infect. Dis. 1983;5:407–411. doi: 10.1093/clinids/5.Supplement_3.S407. [DOI] [PubMed] [Google Scholar]
- 82.Aubry-Damon H., Soussy C.J., Courvalin P. Characterization of mutants in the rpoB gene that confer rifampin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 1998;42:2590–2594. doi: 10.1128/aac.42.10.2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Severinov K., Mustaev A., Severinova E., Kozlov M., Darst S.A., Goldfarb A. The b-subunit rif-cluster I is only angstroms away from the active center of Escherichia coli RNA polymerase. J. Biol. Chem. 1995;270:29428–29432. doi: 10.1074/jbc.270.49.29428. [DOI] [PubMed] [Google Scholar]
- 84.Jin D.J., Gross C.A. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that lead to rifampicin resistance. J. Mol. Biol. 1988;202:45–58. doi: 10.1016/0022-2836(88)90517-7. [DOI] [PubMed] [Google Scholar]
- 85.Weisblum B. Erythromycin resistance by ribosomes modification. Antimicrob. Agents Chemother. 1995;39:577–585. doi: 10.1128/AAC.39.3.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nicola F.G., McDougal L.K., Biddle J.W., Tenover F.C. Characterization of erythromycin- resistant isolates of Staphylococcus aureus recovered in the United States from 1958 through 1969. Antimicrob. Agents Chemother. 1998;42:3024–3027. doi: 10.1128/aac.42.11.3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Simeoni D., Rizzotti L., Cocconcelli P., Gazzola S., Dellaglio F., Torriani S. Antibiotic resistance genes and identification of staphylococci collected from the production chain of swine meat commodities. Food Microbiol. 2008;25:196–201. doi: 10.1016/j.fm.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 88.Maidhof H., Reinicke B., Blumel P., Berger-Bachi B., Labischinski H. femA, Which Encodes a Factor Essential for Expression of Methicillin Resistance, Affects Glycine Content of Peptidoglycan in Methicillin-Resistant and Methicillin-Susceptible Staphylococcus aureus Strains. J. Bacterial. 1991;173:3507–3513. doi: 10.1128/jb.173.11.3507-3513.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kobayashi N., Wu H., Kojima K., Taniguchi K., Urasawa S., Uehara N., Omizu Y., Kishi Y., Yagihashi A., Kurokawa I. Detection of mecA, femA, and femB genes in clinical strains of staphylococci using polymerase chain reaction. Epidemiol. Infect. 1994;113:259–266. doi: 10.1017/S0950268800051682. [DOI] [PMC free article] [PubMed] [Google Scholar]