SUMMARY
Using a cross-sectional probability sample with actigraphy data and two 24 hr dietary recalls, we quantified the association between sleep duration, continuity, variability and timing with the Alternative Healthy Eating Index-2010 diet quality score and its components in 2,140 Hispanic Community Health Study/Study of Latinos participants. The Alternative Healthy Eating Index diet quality-2010 score ranges from 0-110 with higher scores indicating greater adherence to the dietary guidelines and lower risk from major chronic disease.
None of the sleep measures was associated with total caloric intake as assessed using dietary recalls. However, both increase in sleep duration and sleep efficiency were associated with healthier diet quality. Each standard deviation increase in sleep duration (1.05 hr) and sleep efficiency (4.99%) was associated with a 0.30 point increase and 0.28 point increase respectively in the total AHEI-2010 score. The component of AHEI-2010 most strongly associated with longer sleep duration was increased nuts & legumes intake. The components of AHEI-2010 most strongly associated with higher sleep efficiency were increased whole fruit intake and decreased sodium intake.
Both longer sleep duration and higher sleep efficiency were significantly associated with better diet quality among US Hispanic/Latino adults. The dietary components most strongly associated with sleep duration and sleep efficiency differed suggesting potentially independent mechanisms by which each aspect of sleep impacts dietary choices. Longitudinal research is needed to understand directionality of these identified relationships and the generalizability of these data across other ethnic groups.
Keywords: diet quality assessment, dietary patterns, US minority populations, sleep quality, sleep quantity
INTRODUCTION
Adequate sleep and a healthy diet are important foundations for healthy living. Sleep is increasingly recognized as a third pillar of health (Watson et al., 2015). While short term physiologic data suggest perturbations in sleep can impact appetite and diet, (Spaeth et al., 2015) (Weiss et al., 2010) there are limited data on real world associations between sleep and diet and much of these data are self-reported. Furthermore, the evidence base is weak for minority populations such as Hispanics/Latinos in the US, who are at elevated risk for adverse health consequences such as obesity, diabetes, and stroke related to poor health behaviors (Daviglus et al., 2012, Schneiderman et al., 2014, Kaplan et al., 2014). Existing data show that Hispanics/Latinos living in the US are also more likely to report extremes of sleep duration compared to non-Hispanic US whites (Patel et al., 2006, Stamatakis et al., 2007).
Short sleep, in particular, is associated with unfavorable metabolic factors such as impaired glucose tolerance, insulin resistance, increased ghrelin, decreased leptin and increased body mass as well as preference for low nutrient energy dense foods such as sweets, salty snacks and starchy foods (Ayas et al., 2003, Spiegel et al., 2004, Patel and Hu, 2008). There is evidence that other aspects of sleep patterns such as sleep efficiency and sleep latency may also be associated with diet quality and obesity risk (Patel et al., 2014, Crispim et al., 2011, Stern et al., 2014) . However information on objective methods to assess other dimensions of sleep as they might relate to diet is limited. The purpose of this study is to explore associations between objectively measured sleep using actigraphy and diet quality in the Sueño Study (n=2,189), an ancillary study of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) focused on sleep.
METHODS
Study population
The HCHS/SOL is a community-based cohort study of 16,415 Hispanic/Latino adults aged 18-74 years living in four US cities (Bronx NY, Chicago IL, Miami FL, and San Diego CA) with baseline clinic examination from 2008-2011. The baseline clinical examination included comprehensive biological, behavioral and socio-demographic assessments (Sorlie et al., 2010, Lavange et al., 2010). This included use of a home sleep monitor (ARES Unicorder 5.2, Carlsbad CA) to measure the apnea hypopnea index (AHI) as previously described (Redline et al., 2014). HCHS/SOL selected households with a stratified 2-stage probability sampling design. Further details of the sample design and cohort selection have been previously described (Lavange et al., 2010).
As part of the baseline exam, all participants were asked to complete two 24 hour dietary recalls, the first in person at the time of the baseline exam and the second done by telephone five days to three months later (Siega-Riz et al., 2014). Completion rates were high with 97% and 91% of participants completing the first and second recalls, respectively. Participants with at least one completed 24 hour recall were included in this analysis. Of the total of 2,189 SOL participants recruited for the Sueño ancillary study, 2,156 had at least 5 days of valid actigraphy data. Of these, 16 participants were excluded due to missing or unreliable dietary recall data leaving 2,140 subjects for this analysis.
Sueño Ancillary Study
The Sueño ancillary study recruited a subset of 2,189 HCHS/SOL participants aged 18-64 years free of severe sleep disorders (AHI < 50 events/hr, no treatment for sleep apnea, and no diagnosis of narcolepsy) between December, 2010 and December, 2013 (Redline et al., 2014). Further details of Sueño recruitment have been previously published (Patel et al., 2015). The study protocol was approved by the Institutional Review Boards at each of the participating sites and all participants provided written informed consent.
At the Sueño study visit, participants completed questionnaires with respect to employment status, work schedule, and use of caffeine and sleep medications. Depressive symptoms were assessed using a 10-item version of the Center for Epidemiological Studies — Depression (CESD-10) questionnaire (Andresen et al., 1994). Depressive symptoms were defined as a CESD-10 score ≥ 10 (Li et al., 2012). Height and weight were measured and body mass index (BMI) was calculated.
Actigraphy
As part of the Sueño exam, an Actiwatch Spectrum (Philips Respironics, Murrysville, PA) wrist actigraph was placed on the non-dominant wrist and participants were asked to wear the device continuously for 7 days. Activity and light data were collected throughout this period in 30-second epochs. Participants also completed a sleep diary upon awakening each day. A centralized reading center scored all records. Rest periods where the participant was trying to sleep were identified following a standardized protocol that made use of event markers, sleep diaries, light exposure and activity levels (Patel et al., 2015). Sleep-wake status for each 30 second epoch within each rest period was computed using the Actiware 5.59 scoring algorithm with sleep onset defined based on 5 immobile minutes, 0 immobile minutes for sleep offset, and a wake threshold of 40 counts. The scoring algorithm has been validated against polysomnography on an epoch-by-epoch basis (Kushida et al., 2001, Marino et al., 2013). Each day of actigraphy was considered valid if there was a minimum of 20 hours of data including the entire sleep period. Participants with at least 5 days of valid actigraphy data were included for analysis.
Sleep duration was defined as the total amount of time scored as sleep during the main rest period. Sleep efficiency was calculated as the number of epochs scored as sleep divided by the total number of epochs between sleep onset and sleep offset expressed as a percentage. The sleep fragmentation index was calculated as the sum of the proportion of all epochs from sleep onset to sleep offset with an activity count of 2 or greater and the proportion of all bouts of immobility (activity count less than 2 in every epoch) that were 1 minute or less in duration (van den Berg et al., 2008). Midpoint of sleep time was calculated as the halfway point between sleep onset and offset. Average sleep duration, efficiency and fragmentation index were obtained by averaging nightly results across all days of the recording. Sleep variability was assessed using the standard deviation of nightly sleep duration. Sleep duration was modelled both continuously as well as using pre-specified categorization into short (< 6 hours), intermediate (6≥ and <8 hours) and long (≥ 8 hours) sleep duration.
Diet Variables
Dietary variables were derived from the two 24-hour dietary recalls collected by certified bilingual interviewers using the Nutrition Data System for Research (NDSR) from the University of Minnesota. The Alternative Healthy Eating Index-2010 (AHEI-2010), a validated food based dietary scoring system was used to assess diet quality based on usual dietary intake (Liu et al., 2012, Chiuve et al., 2012). Usual dietary intake was estimated using the National Cancer Institute (NCI) method with valid dietary recalls (Tooze et al., 2010). This method accounts for intra-person variability by taking into account multiple 24-hour dietary recalls and covariates. For this analysis, adjustments were made for age, sex, Hispanic/Latino background, clinical center, weekend vs. weekday sequence, and self-reported intake amount (more or less than usual intake). Further details on processing of the dietary recalls have been previously reported (Siega-Riz et al., 2014).
The AHEI-2010 score was computed from the dietary recalls. This index is a widely used measure of dietary quality that has been shown to predict risk of diet-related chronic disease including diabetes and cardiovascular disease (Chiuve et al., 2012). It is the sum of 11 individual components (vegetables, whole fruit, whole grains, sugar sweetened beverages and fruit juice, nuts and legumes, red/processed meat, trans fats, long-chain fats, polyunsaturated fatty acids, sodium, and alcohol). Each component score ranges from 0 to 10 with 10 being the healthiest score. Among adults, the AHEI-2010 score has been shown to be stable within an individual for as long as 24 years reflecting that individual’s underlying dietary choices and preferences (Hagan et al., 2016).
Statistical Analysis
We considered sleep measures as the independent variable and dietary variables as the dependent variables of interest. Survey linear regression was used to estimate age- and sex-adjusted means for each dietary variable by sleep duration category (short, intermediate, and long) normalized to age and sex distributions from the 2010 US Census. Survey linear regression was also used to model the association of sleep measures with each of the dietary measures adjusting for age, sex, site, ethnic background, employment status, depression and log daily energy intake.
Except for the sample characteristics (Table 1), all other statistical procedures accounted for the clustering and stratification and to incorporate the sampling weights in the Sueño ancillary study. All analyses were performed using SAS version 9.3 (Cary, NC).
TABLE 1.
Demographic & lifestyle characteristics of participants in the HCHS/SOL Sueño Ancillary Study (n=2,140)
| Characteristic | Level | % |
|---|---|---|
| Sex | Female | 52.4% |
| Male | 47.6% | |
| Age (yrs) | <30 | 10.9% |
| 30-39 | 12.5% | |
| 40-49 | 29.2% | |
| 50-59 | 33.0% | |
| 60-65 | 14.5% | |
| BMI (kg/m2) | Underweight (BMI < 18.5) | 0.7% |
| Normal (BMI 18.5-25) | 18.0% | |
| Overweight (BMI 25-30) | 38.3% | |
| Obese (BMI ≥ 30) | 43.1% | |
| Employment | Not employed | 41.7% |
| Employed | 58.3% | |
| Background | ||
| Central American | 13.5% | |
| Cuban | 18.0% | |
| Dominican | 12.4% | |
| Mexican | 26.9% | |
| Puerto Rican | 20.9% | |
| South American | 8.3% | |
| Language of preference | Spanish | 79.4% |
| English | 20.6% | |
| Annual household | ||
| Income | < $20,000 | 45.4% |
| ≥ 20,000 | 47.0% | |
| Missing | 7.6% | |
| Education | Less than high school | 32.2% |
| At least high school | 67.8% | |
| Depressive symptoms* | Not Depressed | 70.3% |
| Depressed | 29.7% |
Abbreviations and definitions: BMI, body mass index;
Depressive symptoms defined as a 10 item Center for Epidemiology Study Depression Scale ≥ 10.
RESULTS
Characteristics of study population
The mean (SD) age for the analytic sample was 47.0 (11.6) years and over 52.4%% were female; 81.4% were overweight or obese; 41.7% were not employed and 79.4% indicated Spanish as the language of preference (Table 1). Overall, 22.1% of the cohort had a mean sleep duration <6 hours, 67.7% slept 6≥ and <8 hours and 10.3% slept ≥ 8 hours.
Sleep and Diet Quality
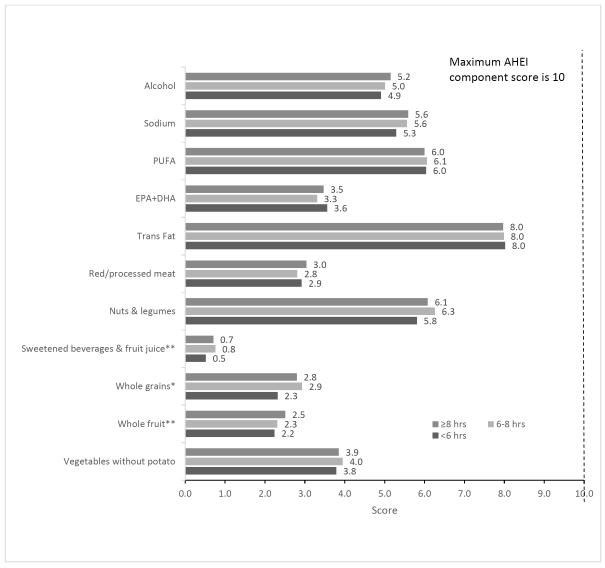
In age and sex-adjusted analyses, no association was found between total caloric intake and sleep duration (p=0.31). In contrast, increased sleep duration was associated with improved dietary quality as assessed with the AHEI-2010. In age and sex-adjusted analyses, the mean (SEM) total AHEI-2010 score was 47.2 (0.3) in participants with long sleep duration, 47.0 (0.8) in participants with intermediate sleep duration and 45.4 (0.4) in participants with short sleep duration (p<0.001). As displayed in Figure 1, the component scores that differed significantly between the three groups were whole grains and whole fruit scores. There were also non-significant trends seen with alcohol, sodium, and nut & legume scores where in all cases those with the shortest sleep duration had the most unhealthy diets. In contrast, no associations were seen between sleep duration and red/processed meat, long chain fats, trans fats, and polyunsaturated fats.
Figure 1.
Age- and sex-adjusted means of Alternative Healthy Eating Index -2010 component scores by short, intermediate and long sleep
AHEI-2010 score= Alternative Healthy Eating Index-2010 measures adherence to 2010 Dietary Guidelines for Americans for the following 11 components: vegetables without potatoes, whole fruit, whole grains, sugar sweetened beverages and fruit juice, nuts and legumes, red/processed meat, trans fat, long-chain fats, polyunsaturated fatty acids, sodium and alcohol. Each AHEI component score ranges from 0 to 10. Total score range: 0 to 110.
Abbreviations: EPA + DHA: eicosapentaenoic and docosahexaenoic (long chain) fatty acids; PUFA: polyunsaturated fatty acids; trans fats: trans unsaturated fatty acids.
*P−=0.01; **P=0.02
Table 2 shows that after adjustment for ethnic background, site, employment, depression, AHI, and log total daily energy intake, higher overall AHEI-2010 scores remained associated with longer sleep durations. Each standard deviation increase in sleep duration (corresponding to 1.05 hrs) was associated with a 0.30 point increase in the overall AHEI-2010 score (p=0.02). The component that contributed most strongly to this healthier diet was the nut & legumes score (β =0.12, SE= 0.05, P= 0.02). The components that contributed next most strongly to the overall improvement in AHEI-2010 score were whole fruits and whole grains, but neither regression coefficient met the threshold for statistical significance.
Table 2.
Regression coefficients for actigraphic sleep measures on the Alternative Healthy Eating Index (AHEI-2010) and each of its components in the HCHS/SOL Sueño ancillary study 2011-2014
| Sleep Duration | SD of Sleep Duration | Sleep Efficiency | Sleep Fragmentation Index | |||||
|---|---|---|---|---|---|---|---|---|
| β (SE) | P Value | β (SE) | P Value | β (SE) | P Value | β (SE) | P Value | |
| AHEI 2010 total score | 0.30 (0.13) | 0.02 | −0.28 (0.17) | 0.10 | 0.28 (0.14) | <0.05 | −0.25 (0.16) | 0.10 |
| AHEI1 Veg without potato, score |
−0.02 (0.03) | 0.57 | −0.04 (0.03) | 0.22 | 0.01 (0.03) | 0.74 | 0.01 (0.03) | 0.77 |
| AHEI2 Whole fruit, score |
0.05 (0.04) | 0.20 | −0.10 (0.04) | 0.01 | 0.15 (0.04) | <0.001 | −0.14 (0.04) | 0.001 |
| AHEI3 Whole grains, score |
0.04 (0.03) | 0.15 | −0.08 (0.05) | 0.09 | 0.02 (0.03) | 0.46 | −0.02 (0.04) | 0.60 |
| AHEI4 Sweetened beverage & fruit juice, score |
0.05 (0.03) | 0.19 | −0.02 (0.03) | 0.62 | 0.03 (0.03) | 0.37 | −0.03 (0.03) | 0.34 |
| AHEI5 Nuts & legumes, score |
0.12 (0.05) | 0.02 | 0.03 (0.10) | 0.79 | 0.00 (0.06) | 0.97 | −0.04 (0.06) | 0.53 |
| AHEI6 Red/processed meat, score |
0.03 (0.04) | 0.47 | 0.02 (0.04) | 0.53 | 0.07 (0.04) | 0.11 | −0.07 (0.04) | 0.14 |
| AHEI7 Trans Fat, score |
0.01 (0.02) | 0.42 | −0.02 (0.03) | 0.45 | −0.01 (0.02) | 0.51 | 0.01 (0.02) | 0.50 |
| AHEI8 EPA+DHA, score |
−0.02 (0.03) | 0.61 | −0.01 (0.03) | 0.78 | −0.01 (0.03) | 0.73 | 0.02 (0.03) | 0.59 |
| AHEI9 PUFA, score |
−0.02 (0.03) | 0.61 | 0.01 (0.03) | 0.69 | −0.05 (0.03) | 0.06 | 0.06 (0.03) | 0.03 |
| AHEI10 Sodium, score |
0.02 (0.04) | 0.52 | −0.04 (0.05) | 0.45 | 0.09 (0.04) | 0.02 | −0.11 (0.04) | 0.01 |
| AHEI11 Alcohol, score |
0.03 (0.05) | 0.55 | −0.03 (0.05) | 0.54 | −0.01 (0.06) | 0.84 | 0.05 (0.06) | 0.43 |
All regressions are adjusted for age, sex, site, ethnic background, employment status, depression, log(daily energy intake) and apnea hypopnea index and account for the complex sampling study design. The regression coefficients are for one standard deviation (SD) change in each actigraphic sleep measure which corresponds to 1.05 hr for sleep duration, 0.60 hr for standard deviation of sleep duration, 4.99% for sleep efficiency, and 7.59% for sleep fragmentation index. Statistically significant values (P<0.05) displayed in bold.
Abbreviations: β: beta coefficient; SE: standard error; EPA: eicosapentaenoic acid; DHA: docosahexaenoic acid; PUFA: polyunsaturated fatty acids
A positive association was also identified between sleep efficiency and the overall AHEI-2010 score where each standard deviation increase in sleep efficiency (corresponding to 4.99%) was associated with a 0.28 point increase in overall AHEI-2010 score (p=<0.05). Unlike the data on sleep duration, nut & legume intake played no part in the relationship between better sleep efficiency and higher diet quality. Rather, the component that contributed the most to this relationship was whole fruit intake (β =0.15, SE= 0.04, P<0.001). A higher component score for sodium (β =0.09, SE= 0.04, P= 0.02) corresponding to a lower intake of sodium was also associated with greater sleep efficiency and contributed to the overall trend for improved dietary quality. The results for the sleep fragmentation index were fairly similar. Although the association between sleep fragmentation index and overall AHEI-2010 score was not statistically significant, the effect size per 1 standard deviation improvement in sleep fragmentation index was fairly similar to the magnitude seen with sleep efficiency and lower sleep fragmentation index was most strongly associated with improvements in whole fruit and sodium intake. Variability in sleep patterns as assessed by the standard deviation in nightly sleep duration was not significantly associated with overall dietary quality but greater stability in patterns or lower standard deviation of sleep duration was associated with a higher whole fruit intake. Sleep timing as assessed by midpoint of sleep time by contrast was not associated with total AHEI-2010 or any of the component scores (data not shown).
DISCUSSION
Contrary to a recent study in the parent study of same cohort (n=11,888) (Mossavar-Rahmani et al., 2015a) where self-reported sleep duration was not associated with dietary quality, we found that short actigraphic sleep duration was associated with worse dietary quality as assessed by the AHEI-2010 score. This discrepancy may be related to biases in the self-reporting of habitual sleep duration (Cespedes et al., 2016). While the increase in the AHEI-2010 score was small, over the life course the cumulative effects of small changes in dietary patterns could have substantial downstream effects on risk of obesity, diabetes and other nutrition-associated chronic diseases.
An interesting finding of our work is that there were slightly different dietary patterns associated with longer sleep duration as opposed to greater sleep efficiency. The dietary component most strongly associated with longer sleep durations was greater nut and legume intake while there was no evidence for an association between sleep efficiency, sleep fragmentation index, or sleep variability with nut and legume intake. In contrast, increased sleep efficiency, reduced sleep fragmentation index, and reduced standard deviation of nightly sleep duration were all associated with greater whole fruit scores and both increased sleep efficiency and reduced sleep fragmentation index were associated with higher sodium scores corresponding to lower intake of sodium. This pattern of findings suggests that different aspects of sleep may impact different aspects of dietary choices.
While our study focused on a free-living cohort that likely has been following these food patterns long-term, our findings are consistent with a study on short term sleep restriction in a controlled laboratory setting that indicated increased preference for foods high in sweets, salty snacks, and starchy foods with preference for fruits, vegetables and high protein foods less affected in the sleep restricted group (Spiegel et al., 2004) . Additionally a novel finding from our study is that increased sleep duration was related to increased nuts and legume consumption, foods that are high in healthy vegetable proteins. Nuts and legumes are also nutrient rich and have a wide variety of cardiovascular and metabolic benefits (Aune et al., 2016). Legumes and nuts overall scored favorably in HCHS/SOL parent study according to AHEI-2010 criteria (Mattei et al., 2016).
Because of the cross-sectional nature of our study, we cannot exclude the possibility that dietary patterns influence sleep. Nuts are high in B vitamins such as folate, magnesium and fiber, nutrients that are associated with synthesis of serotonin and melatonin which may influence sleep (Peuhkuri et al., 2012). Similarly, prior studies have related intake of specific fruits such as kiwi and cherries to improvements in sleep quality (Garrido et al., 2013, Lin et al., 2011).
The absence of an association between total caloric intake and sleep duration may be related to the underreporting of energy intake that has been demonstrated in a validation study in the HCHS/SOL (Mossavar-Rahmani et al., 2015b). Future studies that apply error-free biomarker-calibrated energy intake may yield more definitive associations between sleep and total caloric intake.
Overall our findings strengthen evidence for the association between longer sleep duration and healthier eating patterns (Mossavar-Rahmani et al., 2015a, Kant and Graubard, 2014). Unexpectedly, there was no significant association of sleep duration with total sugar intake in this cohort as was previously reported in NHANES which could relate to underreporting. The lack of any signals from sleep measures on the important healthy fats such as the omega 3 fatty acids: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) is noteworthy and may relate to overall low usual fish intake in this cohort (mean intake of 0.7 oz./day) or that underestimation occurred because quantity and type of oils used in cooking were not fully captured (Siega-Riz et al., 2014).
Limitations of the study relate to both wrist actigraphy and diet measures. Wrist actigraphy uses motion to infer sleep/wake status and so does not actually measure sleep and cannot provide information on sleep stages. However, actigraphy has been well validated against the gold standard of polysomnography for the determination of sleep/wake status on an epoch by epoch level (Ancoli-Israel et al., 2003). An advantage of actigraphy over polysomnography is the absence of a first night effect and the ability to record over multiple nights to better assess habitual sleep patterns. We utilized a standardized scoring algorithm for actigraphy in this study which resulted in sleep measures that we have previously shown to be highly reproducible (Patel et al., 2015).
Limitations with respect to diet relate to measurement error and timing. Due to the known measurement error associated with self-report measures of diet (Mossavar-Rahmani et al., 2015b) , we used the NCI-adjusted method to estimate usual dietary intake from the 24 hr dietary recalls and adjusted the models by log energy intake. As mentioned earlier, diet quality is relatively stable over time such that the two year period between dietary and sleep assessments would not be a significant limitation. If anything, associations may be stronger than presented here and our results may underestimate the true strength of associations. In addition, we note that our focus was on general categories that contribute to dietary quality rather than specific foods. As such, we do not have more granular details on for example the specific kinds of nuts and legumes that contributed to the associations observed with this overall category.
Another limitation of our work is the inability to determine causality. Our results cannot differentiate whether healthy sleep improves dietary quality or healthy diet improves sleep. Another possibility is that a third underlying factor such as greater interest in health leads to both healthier diet and sleep. Longitudinal studies are needed to better elucidate these relationships.
Nevertheless, this study highlights an association between sleep patterns and diet quality, specifically the AHEI-2010 score and its components in a large Hispanic/Latino cohort. The specific associations identified, in particular greater nut and legume intake with greater sleep duration and greater whole fruits and less sodium with greater sleep efficiency should be further investigated in other cohorts.
Acknowledgements
We are indebted to the participants in the Hispanic Community Health Study/Study of Latinos for their dedication to the study and thank investigators and staff for their valuable contributions. For a complete list of staff and investigators see: Sorlie P., et al. in Ann Epidemiol. 2010 Aug; 20: 642-649 and http://www.cscc.unc.edu/hchs/.
Sources of Financial Support: This work was supported by grants R01HL0958561, R01HL0982972, K01HL1298923 from the National Heart, Lung, and Blood Institute. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Center/Offices contribute to the Hispanic Community Health Study/Study of Latinos through a transfer of funds to the National Heart, Lung, and Blood Institute: the National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Abbreviations
- AHEI-2010
Alternative Healthy Eating Index-2010
- BMI
Body Mass Index
- HCHS/SOL
Hispanic Community Health Study/Study of Latinos
- CESD-10
Center for Epidemiological Studies Depression Questionnaire
Footnotes
YMR
SRP
Author Contribution: YMR, RW, PAS and SRP designed the research; YMR, ARR, KJR, SRP conducted the research; JW, RW analyzed the data; YMR, JW, RW, MJ, PAS, SFC, LCG, MDG, QQ, ARR, KJR, DSA, LVH and SRP wrote the manuscript.
Conflict of interest: The authors do not report any conflicts of interest.
References
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- Aune D, Keum N, Giovannucci E, et al. Nut consumption and risk of cardiovascular disease, total cancer, all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective studies. BMC Med. 2016;14:207. doi: 10.1186/s12916-016-0730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- Cespedes EM, Hu FB, Redline S, et al. Comparison of Self-Reported Sleep Duration With Actigraphy: Results From the Hispanic Community Health Study/Study of Latinos Sueno Ancillary Study. Am J Epidemiol. 2016;183:561–73. doi: 10.1093/aje/kwv251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–18. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crispim CA, Zimberg IZ, Dos Reis BG, Diniz RM, Tufik S, De Mello MT. Relationship between food intake and sleep pattern in healthy individuals. J Clin Sleep Med. 2011;7:659–64. doi: 10.5664/jcsm.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–84. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido M, Gonzalez-Gomez D, Lozano M, Barriga C, Paredes SD, Rodriguez AB. A Jerte valley cherry product provides beneficial effects on sleep quality. Influence on aging. J Nutr Health Aging. 2013;17:553–60. doi: 10.1007/s12603-013-0029-4. [DOI] [PubMed] [Google Scholar]
- Hagan KA, Chiuve SE, Stampfer MJ, Katz JN, Grodstein F. Greater Adherence to the Alternative Healthy Eating Index Is Associated with Lower Incidence of Physical Function Impairment in the Nurses' Health Study. J Nutr. 2016;146:1341–7. doi: 10.3945/jn.115.227900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant AK, Graubard BI. Association of self-reported sleep duration with eating behaviors of American adults: NHANES 2005-2010. Am J Clin Nutr. 2014;100:938–47. doi: 10.3945/ajcn.114.085191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan RC, Aviles-Santa ML, Parrinello CM, et al. Body mass index, sex, and cardiovascular disease risk factors among Hispanic/Latino adults: Hispanic community health study/study of Latinos. J Am Heart Assoc. 2014;3:e000923. doi: 10.1161/JAHA.114.000923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2:389–96. doi: 10.1016/s1389-9457(00)00098-8. [DOI] [PubMed] [Google Scholar]
- Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–9. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Mirzaei F, O'reilly EJ, et al. Prospective study of restless legs syndrome and risk of depression in women. Am J Epidemiol. 2012;176:279–88. doi: 10.1093/aje/kws016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin HH, Tsai PS, Fang SC, Liu JF. Effect of kiwifruit consumption on sleep quality in adults with sleep problems. Asia Pac J Clin Nutr. 2011;20:169–74. [PubMed] [Google Scholar]
- Liu K, Daviglus ML, Loria CM, et al. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125:996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino M, Li Y, Rueschman MN, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36:1747–55. doi: 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei J, Sotres-Alvarez D, Daviglus ML, et al. Diet Quality and Its Association with Cardiometabolic Risk Factors Vary by Hispanic and Latino Ethnic Background in the Hispanic Community Health Study/Study of Latinos. J Nutr. 2016;146:2035–44. doi: 10.3945/jn.116.231209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossavar-Rahmani Y, Jung M, Patel SR, et al. Eating behavior by sleep duration in the Hispanic Community Health Study/Study of Latinos. Appetite. 2015a;95:275–84. doi: 10.1016/j.appet.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossavar-Rahmani Y, Shaw PA, Wong WW, et al. Applying Recovery Biomarkers to Calibrate Self-Report Measures of Energy and Protein in the Hispanic Community Health Study/Study of Latinos. Am J Epidemiol. 2015b;181:996–1007. doi: 10.1093/aje/kwu468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Hayes AL, Blackwell T, et al. The association between sleep patterns and obesity in older adults. Int J Obes (Lond) 2014;38:1159–64. doi: 10.1038/ijo.2014.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Weng J, Rueschman M, et al. Reproducibility of a Standardized Actigraphy Scoring Algorithm for Sleep in a US Hispanic/Latino Population. Sleep. 2015;38:1497–503. doi: 10.5665/sleep.4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res. 2012;32:309–19. doi: 10.1016/j.nutres.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Redline S, Sotres-Alvarez D, Loredo J, et al. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med. 2014;189:335–44. doi: 10.1164/rccm.201309-1735OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Diabetes Care. 2014;37:2233–9. doi: 10.2337/dc13-2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siega-Riz AM, Sotres-Alvarez D, Ayala GX, et al. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am J Clin Nutr. 2014;99:1487–98. doi: 10.3945/ajcn.113.082685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–41. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaeth AM, Dinges DF, Goel N. Resting metabolic rate varies by race and by sleep duration. Obesity (Silver Spring) 2015;23:2349–56. doi: 10.1002/oby.21198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern JH, Grant AS, Thomson CA, et al. Short sleep duration is associated with decreased serum leptin, increased energy intake and decreased diet quality in postmenopausal women. Obesity (Silver Spring) 2014;22:E55–61. doi: 10.1002/oby.20683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29:2857–68. doi: 10.1002/sim.4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Berg JF, Knvistingh Neven A, Tulen JH, et al. Actigraphic sleep duration and fragmentation are related to obesity in the elderly: the Rotterdam Study. Int J Obes (Lond) 2008;32:1083–90. doi: 10.1038/ijo.2008.57. [DOI] [PubMed] [Google Scholar]
- Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843–4. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S. The association of sleep duration with adolescents' fat and carbohydrate consumption. Sleep. 2010;33:1201–9. doi: 10.1093/sleep/33.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]