Abstract
Using a validated finite element (FE) protocol, we quantified cartilage and labrum mechanics, congruency, and femoral coverage in five male patients before and after they were treated for acetabular retroversion with peri-acetabular osteotomy (PAO). Three-dimensional models of bone, cartilage, and labrum were generated from computed tomography (CT) arthrography images, acquired before and after PAO. Walking, stair-ascent, stair-descent, and rising from a chair were simulated. Cartilage and labrum contact stress, contact area, and femoral coverage were calculated overall and regionally. Mean congruency (average of local congruency values for FE nodes in contact) and peak congruency (most incongruent node in contact) were calculated overall and regionally. Load supported by the labrum was represented as a raw change in the ratio of the applied force transferred through the labrum and percent change following surgery (calculated overall only). Considering all activities, following PAO, mean acetabular cartilage contact stress increased medially, superiorly and posteriorly; peak stress increased medially and posteriorly. Peak labrum stresses decreased overall and superiorly. Acetabular contact area decreased overall and laterally, and increased medially. Labral contact area decreased overall, but not regionally. Load to the labrum decreased. Femoral head coverage increased overall, anterolaterally, and posterolaterally, but decreased anteromedially. Mean congruency indicated the hip became less congruent overall, anteriorly, and posteriorly; peak congruency indicated a less congruent joint posteriorly.
Clinical Relevance
Medialization of contact and reductions in labral loading following PAO may prevent osteoarthritis, but this procedure increases cartilage stresses, decreases contact area, and makes the hip less congruent, which may overload cartilage.
Keywords: Hip, retroversion, morphology, chondrolabral mechanics, finite element analysis
Introduction
Approximately 25% of people will develop hip osteoarthritis (OA).1 As many as 20% of hip OA cases may be attributed to acetabular retroversion,2 an abnormality characterized by an acetabular opening that lies more posterolateral than normal.3 Studies suggest that retroverted hips are primarily characterized by deficiencies in posterior femoral head coverage,4,5 with secondary increases in anterior coverage.5 Loss of posterior coverage could cause chronic overload of cartilage6 and/or deleterious loading to the labrum,7,8 which may cause OA in much the same way as that hypothesized for hips with traditional acetabular dysplasia. Anterior over-coverage, on the other hand, may cause symptoms and soft-tissue damage patterns more characteristic of patients with pincer-type femoroacetabular impingement (FAI).9,10
Anteverting peri-acetabular osteotomy (PAO) is used to relieve pain, improve range of motion11 and prevent, or at least delay, OA in patients with acetabular retroversion.10–14 In the PAO procedure, the acetabulum is transected free from the pelvis and reoriented to improve coverage. However, rather than rotating the acetabulum to improve anterolateral coverage as is done for traditionally dysplastic hips, the socket is anteverted to improve posterior coverage in retroverted hips. Reorientation of the retroverted acetabulum may increase posterior coverage, and have the simultaneous benefit of decreasing anterior coverage. However, despite the purported benefits,10,11,15 there is scant biomechanical data to support the use of PAO in acetabular retroversion. One modeling study showed that peak and average contact stresses in retroverted hips were not significantly larger than those of asymptomatic screened controls on a regional or overall basis.15 Accordingly, one could make the logical argument that PAO would not normalize stresses in retroverted hips, as stresses are already within the range of normal hips. Measurements of cartilage and labrum (i.e. chondrolabral) stress, contact area, and load sharing, before and after PAO would clarify the biomechanical implications of surgery, but these data are not available.
Improving the anatomic orientation of the hip may be critical to the success of PAO. For example, reducing anterior over-coverage may be necessary to resolve symptoms of impingement. However, one risk of PAO is that the acetabular fragment will be over-rotated, leading to posteroinferior impingement.11 Comparisons of pre- and post-operative femoral head coverage would clarify the extent to which PAO is efficacious at improving the anatomic relationship between the femur and acetabulum. Coverage data could also form the basis of pre-operative planning or intra-operative guidance software that aims to prevent over-rotation.
Retroverted hips often present with aspherical femoral heads (e.g. 42% of patients with Legg-Calvé-Perthes disease have radiographic signs of retroversion2). Thus, PAO is likely to alter joint congruency in the retroverted hip. Minor deviations from a congruent joint have been shown to induce areas of high (or low) contact stress in a normal hip.16 It is possible that a loss of joint congruency following PAO could increase chondrolabral stresses. However, to our knowledge, congruency and chondrolabral stresses have not been measured in retroversion patients before and after PAO. These measurements may help identify patients who would benefit from a combined surgical procedure (e.g. one that combines PAO with femoral osteochondroplasty to correct femoral head coverage and hip joint congruency simultaneously).17
Chondrolabral mechanics cannot be measured in-vivo. However, patient-specific finite element (FE) models that incorporate anatomy for the bone, cartilage, and labrum from volumetric medical image data can predict contact stresses in good agreement with experimental results.19,20 The three-dimensional (3D) CT-based FE models can also be analyzed to quantify femoral head coverage5 and congruency.7 Use of an FE model to calculate coverage and congruency enables quantification of these metrics in a loaded state, which may be more clinically relevant than those based on 3D surfaces generated using volumetric image data obtained in an unloaded, supine position. In this study, we used patient-specific FE models to quantify chondrolabral mechanics, coverage, and congruency before and after PAO in patients with acetabular retroversion. We hypothesized PAO would reduce peak and mean cartilage contact stress, increase cartilage contact area, reduce labral contact area, and reduce load support by the labrum. We also hypothesized PAO would decrease anterior coverage, increase posterior coverage, and yield a less congruent interface.
Methods
Patient Recruitment, Radiographic Evaluation, CT Arthrography
Five young adult males with symptomatic acetabular retroversion were recruited, imaged, and analyzed before and after PAO performed by a single surgeon (CLP). These five subjects represented a sub-set of 10 participants analyzed with FE analysis by Henak et al., prior to PAO.15 Pre-operatively, subjects were (mean (SD)) 185.4 (6.0) cm tall, weighed 81.0 (10.1) kg, had a body mass index of 23.5 (1.5) kg/m2, and were 21.5 (3.7) years old. Post-operatively subjects were 183.8 (6.2) cm, 79.0 (12.5) kg, 23.3 (2.3) kg/m2, and 24.7 (4.7) years old. All research procedures were performed in accordance with the Helsinki Declaration with informed consent and institutional board approval (University of Utah IRB 10983, 43600). Acetabular retroversion was diagnosed by the presence of a cross-over sign and posterior wall sign on an anteroposterior (AP) film.3 CT arthrography with hip traction was performed using a protocol described previously.18 The use of injected contrast agent and hip traction ensured that anatomy of the opposing layers of cartilage and the acetabular labrum was visible for 3D reconstruction. The CT protocol was repeated between 1 and 5 years after surgery.
Finite Element Mesh Generation and Analysis
FE models were generated from the CT images using a protocol that has been shown to predict cartilage contact stresses in good agreement with results obtained in-vitro19,20. Briefly, CT images were segmented semi-automatically to define surfaces for the outer cortex, trabecular-cortical bone boundary, cartilage, and acetabular labrum (Amira v6, FEI, Hillsboro, OR, USA) (Fig. 1). This method of semi-automatic segmentation has been shown to yield a reconstruction error less than 10% for representing cartilage21 and the thickness of the cortex,22 which is sufficient to obtain accurate predictions of hip cartilage contact stresses.19,20 Cortical bone was represented as triangular shell elements with position-dependent thickness, calculated as the geometric distance between the inner and outer cortex.19 Pelvic and femoral cartilage as well as the acetabular labrum was represented as hexahedral elements, generated by projecting a block mesh to the 3D reconstruction of segmented cartilage in TrueGrid (XYZ Scientific, Livermore, CA, USA).21,23–25 The boundary between cartilage and labrum was assumed to be located where the concave acetabulum transitioned into the convex acetabular rim.8 Element densities were based on previous mesh convergence analyses.19
Figure 1.
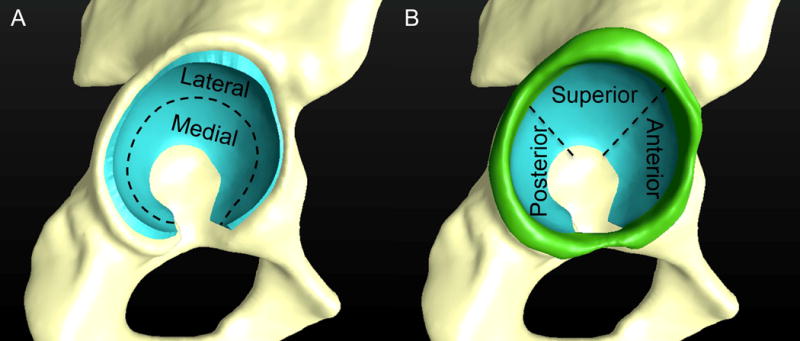
Patient-specific 3D reconstructions of the pelvis in the pre-operative state. Acetabular cartilage (blue) was divided into medial and lateral regions (A) as well as anterior, superior, and posterior regions (B) for analysis of contact stresses, contact area, and congruency. The acetabular labrum (green) was divided into anterior, superior, and posterior regions to calculate labral contact stress and contact area.
Constitutive models for bone, cartilage, and labrum followed other FE studies of the hip.8,19,23 Here, bone was represented as isotropic linear elastic (E = 17 GPa, ν = 0.29).24 Cartilage was represented as a nearly incompressible, neo-Hookean hyperelastic material (G = 13.6 MPa, K = 1359 MPa),21,28 which was a simplification of cartilage behavior.22,25,29 Despite this simplification, use of this constitutive model does not alter hip cartilage contact stresses substantially compared to more sophisticated representations of cartilage.20 The labrum was represented as transversely isotropic hyperelastic25 with material coefficients (C1 = 1.4 MPa, C3 = 0.005 MPa, C4 = 36, C5 = 66 MPa, λ* = 1.103) derived from experimental data of bovine tissue.26 Here, C1 referenced the shear modulus; equations describing the behavior of the fibers included material coefficients that scaled the exponential stress (C3), specified the rate of collagen uncramping (C4), the modulus of straightened collagen (C5), and the stretch at which collagen straightened (λ*). Although material properties were derived from bovine tissue, research has demonstrated that predictions of labral mechanics are relatively insensitive to perturbations in material coefficients.8
Bergmann’s data was used to apply identical loading conditions in subjects before and after PAO, scaled to each subject’s body weight (BW).27 Activities included walking at toe-off (TO, 205% BW), mid-stance during walking (MS 203% BW), the transition of heel-strike and mid-stance for stair descent (SD 230% BW), heel-strike during stair ascent (SA, 252% BW), and rising from a chair (RC 190% BW). During loading, the pubis and sacroiliac joints were rigid. All boundary and loading conditions were assigned using the pre-processing software, PreView.28 FE solutions were obtained using the nonlinear implicit solver NIKE3D.29
Analysis of Chondrolabral Contact Mechanics
FE solutions were visualized and post-processed in PostView.28 The distribution of chondrolabral contact mechanics predicted by patient-specific FE models is quite complex. For example, models often show areas of focal loading to cartilage.7,15,22,23 It is difficult to capture the complexity of FE predictions using numerical or graphical comparisons alone. Thus, the change in FE predictions were assessed qualitatively by examining fringe plots of stress for each individual subject and loading scenario. Fringe plots were also created to visualize average acetabular cartilage contact stress. The same number of nodes and elements were used to represent acetabular cartilage across subjects; nodal connectivity was also preserved. This one-to-one correspondence made it straightforward to calculate an average stress at each node, but it was still necessary to define a single, representative mesh in which to map stress values. To select this representative mesh, the articulating surface of acetabular cartilage from each patient mesh was fit to a sphere. The mesh that had a radius closest to the mean radius was designated as the representative mesh. Nodal contact stress values of all subjects were mapped onto this representative mesh, and then averaged.
Results were quantitatively assessed by comparing mean and peak acetabular cartilage contact stress and mean contact area overall, and with respect to five anatomic regions (medial, lateral, superior, anterior, and posterior) (Fig. 1A). Mean and peak labral contact stress and contact area were assessed overall, and at three anatomic regions (anterior, superior and posterior regions) (Fig. 1B). Peak cartilage and labrum contact stress was obtained by selecting the FE mesh node with the highest value. Mean cartilage and labrum stress was calculated as the mean of all nodes within a region where contact stress exceeded 0.0 MPa (i.e. average stress was calculated over the region in contact, not as an average over the entire acetabulum). Cartilage and labral contact area were calculated as the area of the faces of the FE mesh of acetabular cartilage or labrum that had a contact stress value that exceeded 0.0 MPa, divided by the total surface area available, and reported as a percent. The change in contact area was represented as the raw difference in values between operative states, not as a percent change. Finally, load supported by the labrum was calculated as the load transferred to the labrum divided by the total load applied to the FE model (i.e. ratio), and was represented as both a raw change in the ratio and percent change following PAO. Here, load to the labrum was calculated when considering the entire labral structure (i.e. regional analysis was not performed).
Analysis of Coverage and Congruency
Pre- and post-operative coverage of the femoral head was analyzed during MS. The MS was used for this analysis due to its generalizability as a neutral, standing position, and because walking is a high frequency activity. Coverage was analyzed by first defining the femoral head-neck boundary with plots of principal curvature.5 The femoral head was then divided into four regions: anterior medial (AM), anterior lateral (AL), posterior medial (PM), and posterior lateral (PL) using methods described previously.5 The curve representing the apex of the bony rim of the acetabulum was then projected to the femoral head at the loaded position of the FE model during MS. Finally, overall and regional coverage was calculated as a percentage of the area available.5 The change in coverage was represented as the raw difference in values between operative states, not as a percent change.
Congruency between acetabular and femoral cartilage was measured using methods previously implemented by Henak et al.7 Briefly, the magnitude and orientation of the principal curvatures at each FE mesh node where the acetabular and femoral cartilage meshes contacted one another was estimated using quadric methods. The nodal magnitudes and orientations of principal curvature were then used to calculate the root mean square (RMS) curvature value to provide a single measure of congruency at each node.7 Here, a larger RMS curvature indicates a less congruent surface, whereas a smaller value indicates a more congruent surface. Congruency was calculated for both pre- and post-operative states using the MS model. The MS model was selected as it represents a neutral position and is a frequent activity of daily living. Peak and mean congruency were calculated overall, and on a regional basis according to the five anatomic regions used to analyze acetabular contact mechanics. Here, mean congruency was expressed as the average of local congruency values for FE nodes in contact, whereas peak congruency was expressed as the most incongruent FE node in contact.
Statistical Analysis
Paired-sample differences between pre- and post-operative states within the same subjects were assessed using a mixed-effects linear regression, where activities were nested within patients. We did not treat the various anatomical regions as independent tests when comparing chondrolabral contact mechanics, coverage, and congruency between pre- and post-operative configurations. As such, Finner’s procedure was used to correct for multiple comparisons.30 The number of comparisons required depended on the metric analyzed. For the analysis of acetabular cartilage contact mechanics (i.e. peak and mean contact stress, mean contact area), adjustment was made for two comparisons when analyzing the medial and lateral regions, and three comparisons when analyzing the anterior, posterior, and superior regions. Here, adjustments were not necessary for five comparisons since the medial/lateral regions overlapped with the anterior/superior/posterior regions (see Fig. 1). For the analysis of labral contact mechanics, adjustment was made for three comparisons when analyzing the anterior, posterior, and superior regions. For the analysis of coverage, adjustments were made according to the four anatomic regions about the femur (AL, AM, PL, PM). The analysis of congruency was adjusted in the same manner as that for acetabular cartilage contact mechanics since congruency was reported relative to the same anatomic regions. Adjustments were not required when analyzing load to the labrum, as this was reported as a single value. Mixed-effects linear regression reports the mean difference between two measures, not the discrete value in each state, to ascertain if they are significant. Thus, where appropriate, the discrete values for each metric were reported in addition to a 95% confidence interval (CI) of the mean differences between pre- and post-operative states. All statistical analyses were performed in Stata (v13.0, StataCorp LP, College Station, TX), with plots generated using SigmaPlot (v11.0; Systat Software, San Jose, CA). Significance for all tests was set at P ≤ 0.05.
Results
Surgery eliminated the posterior wall sign and cross-over sign in all five patients, indicating that, based on radiographic evaluation alone, PAO was successful in normalizing the anatomic relationship of the hip.
Chondrolabral Contact Mechanics
When examining the fringe plots for each patient, cartilage contact stresses were complex in shape, but in general, appeared bi-centric in both operative states (Fig. 2). There appeared to be greater variation in the pattern of acetabular contact stresses across patients as compared to the variation in stresses observed across operative states within the same subject. In general, acetabular contact stresses appeared to be higher throughout the acetabulum in the post-operative state. However, both operative states demonstrated areas of high, focal stress. The locations of these focal regions of high stress appeared to shift medially and posteriorly following PAO.
Figure 2.
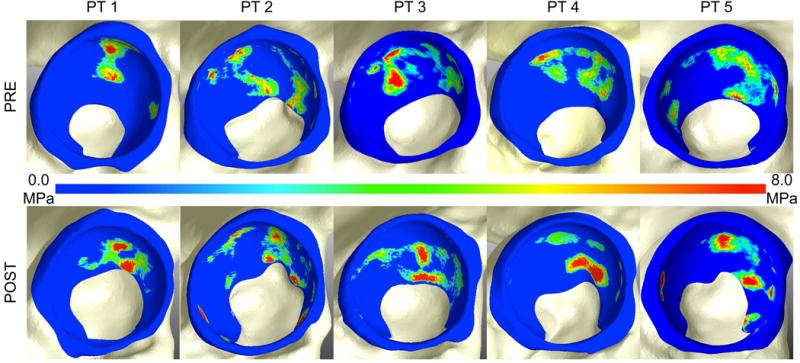
Acetabular and labral contact stress in the pre- (top row) and post-operative (bottom row) state for walking at midstance (MS) for each patient (PT). Contact stresses were complex in shape, but appeared bi-centric in both operative states. Acetabular contact stresses appeared higher in magnitude in the post-operative state, and were located more medial, near the acetabular fossa. There was greater variation in the location and magnitude of stress across patients than that measured between operative states within the same subject. Note – the fringe scale has been set to a maximum of 8 MPa to show areas of elevated contact stress. However, peak contact stresses often exceeded 8 MPa.
On qualitative inspection, when mapped to the representative mesh, acetabular cartilage contact stresses were generally increased in the post-operative state (Fig. 3). Contact shifted medially following surgery, which was most evident during the MS, TO, SA, and SD activities. A posteriorly directed shift in contact was also observed, especially during the SD and RC activities, where regions of increased acetabular cartilage contact stress observed in the anterior region prior to surgery were all but eliminated in the post-operative state.
Figure 3.
Average contact stresses in the pre- (top row) and post-operative (bottom row) state. Here, contact stresses for each patient have been mapped to a representative mesh and then averaged. Contact stresses were generally higher in the post-operative state. Contact also shifted medially following surgery, which was most evident during the MS, TO, SA, and SD activities. A posteriorly directed shift in contact was observed during the SD and RC activities. Note: the labrum has been removed as average labral stresses were very low. MS = mid-stance during walking; TO = walking at toe-off; SA = heel-strike during stair ascent, SD = transition of heel strike and mid-stance for stair descent; RC = maximum joint reaction force during rising from a chair.
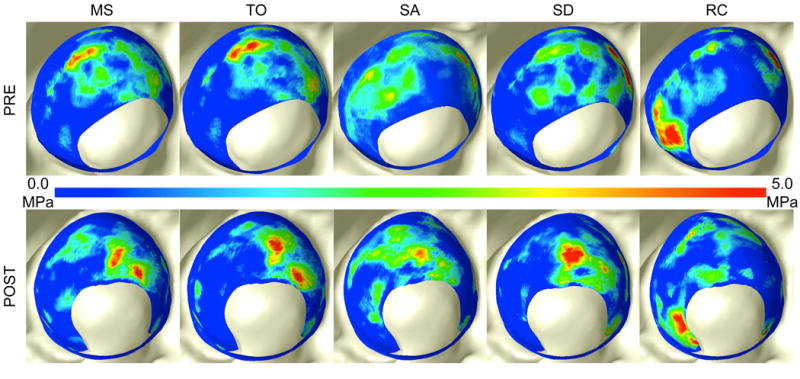
Significant changes in cartilage and labrum mean and peak contact stresses were observed (Fig. 4) (see Table S1 for the magnitudes of stress in each operative state). There were significant increases in the mean acetabular contact stress medially, superiorly and posteriorly, and a trend toward a significant increase overall (Fig. 4A). Acetabular cartilage peak contact stress increased medially and posteriorly and trended towards a significant decrease laterally, but there were no significant changes overall (Fig. 4B). There were no significant changes in the overall or regional mean contact stress on the labrum (Fig. 4C). However, significant decreases were observed in the peak stresses on the labrum in the superior region and overall (Fig. 4D).
Figure 4.
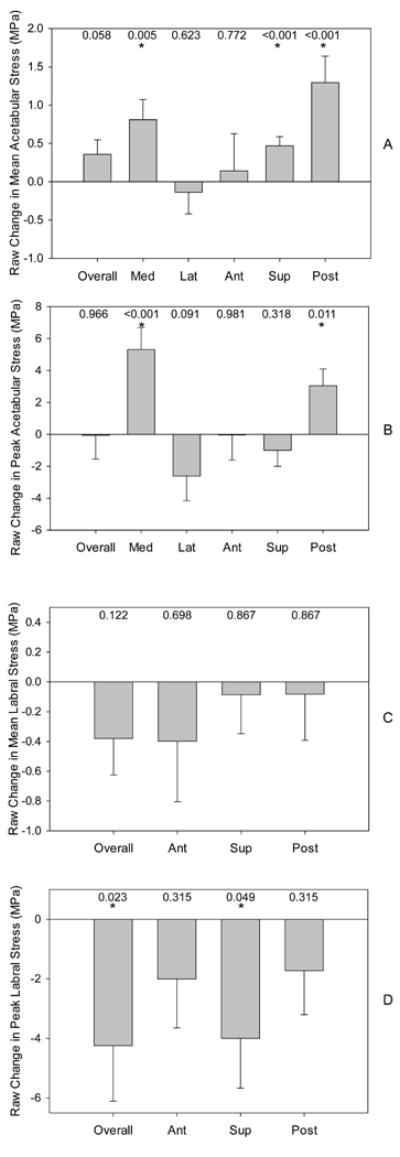
Raw changes in cartilage and labrum mean and peak contact stress following PAO. (A) Mean acetabular contact stress was increased significantly in the medial, superior, and posterior regions. (B) Peak acetabular contact stress was increased significantly in the medial and posterior regions. (C) There were no significant changes in mean labral contact stress. (D) Peak labral stresses were reduced significantly overall and in the anterior region. Bars indicate standard error. P values are listed and * indicates P ≤ 0.05.
Significant changes in acetabular cartilage and labrum contact area (Fig. 5) and load to the labrum were observed (Fig. 6) (see Table S2 for the magnitudes of contact area and load to the labrum in each operative state). Here, acetabular cartilage contact area decreased significantly overall and in the lateral region, but increased medially (Fig. 5A). There was a significant decrease in the contact area on the labrum overall, but no significant changes were observed on a regional basis (Fig. 5B). As a ratio, load to the labrum decreased significantly overall (load to the labrum was not calculated regionally) when considering data from all loading activities (Fig. 6A). On a per-activity basis, significant decreases were observed during MS and SA (Fig. 6A). Similar findings were observed when representing load to the labrum as a percent change, where the labrum was unloaded by up to 65% (MS activity, Fig. 6B).
Figure 5.
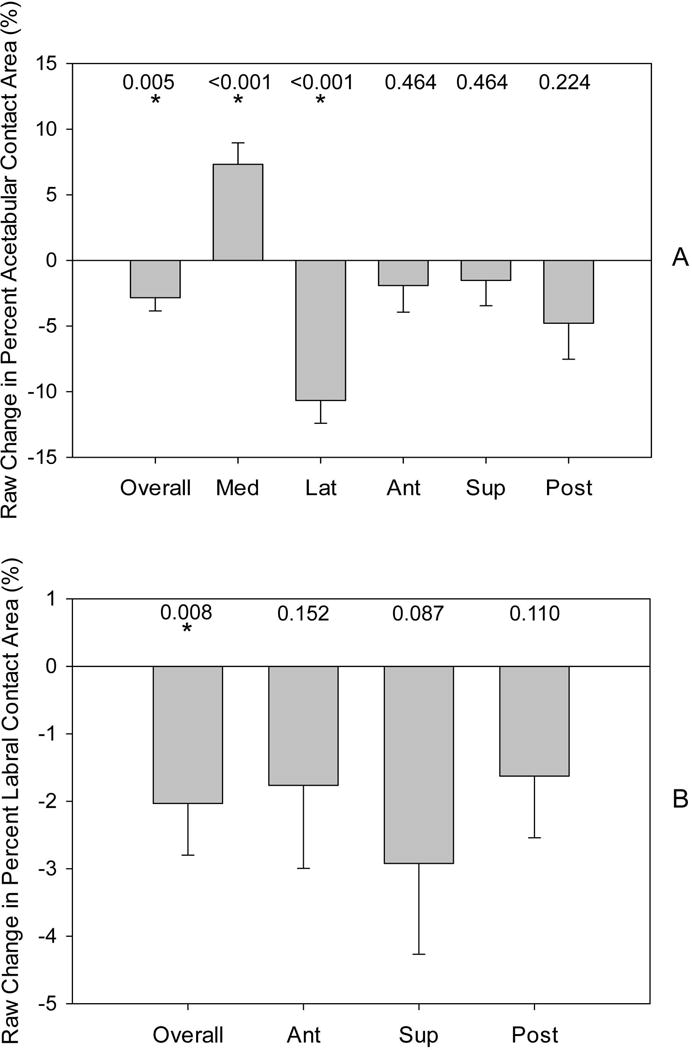
Raw changes in cartilage and labrum contact area following PAO. (A) Acetabular contact area was reduced significantly overall and in the lateral region, but increased significantly in the medial region. (B) Labral contact area was significantly reduced overall. Note: acetabular and labral contact area are in units of percent, which was calculated by dividing the area actually in contact by the total area available for contact. Bars indicate standard error. P values are listed and * indicates P ≤ 0.05. TO = walking at toe-off; MS = mid-stance during walking; SD = transition of heel strike and mid-stance for stair descent; SA = heel-strike during stair ascent, RC = maximum joint reaction force during rising from a chair.
Figure 6.
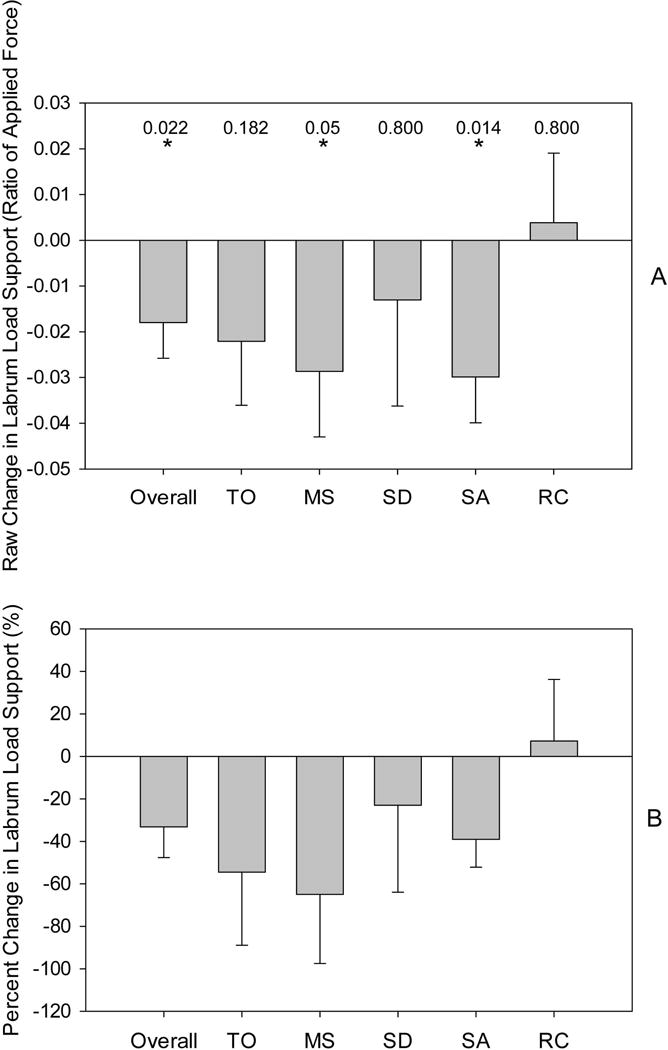
Changes to labrum load support following PAO. (A) The raw change in load support to the labrum, expressed as the load transferred to the labrum divided by the total force applied to the FE model, decreased significantly overall, and during the MS and SA activities. (B) The percent change in labrum load support demonstrated the same trends as the raw change. Note: both the raw change and percent change in labrum load support were calculated overall, not on a regional basis. Bars indicate standard error. Note: statistical testing was only performed on the raw change in labrum load support. P values are listed and * indicates P ≤ 0.05. TO = walking at toe-off; MS = mid-stance during walking; SD = transition of heel strike and mid-stance for stair descent; SA = heel-strike during stair ascent, RC = maximum joint reaction force during rising from a chair.
Coverage and Congruency
Significant changes in joint coverage and congruency were observed (Fig. 7) (see Table S3 for the magnitudes of joint coverage and congruency in each operative state). In particular, coverage of the femoral head was significantly increased overall and in the AL and PL regions; coverage was reduced significantly in the AM region (Fig. 7A). The RMS value indicated that the hip became significantly less congruent overall and in the anterior and posterior regions following PAO (Fig. 7B). Peak congruency indicated that the hip became less congruent in the posterior region only (Fig. 7C).
Figure 7.
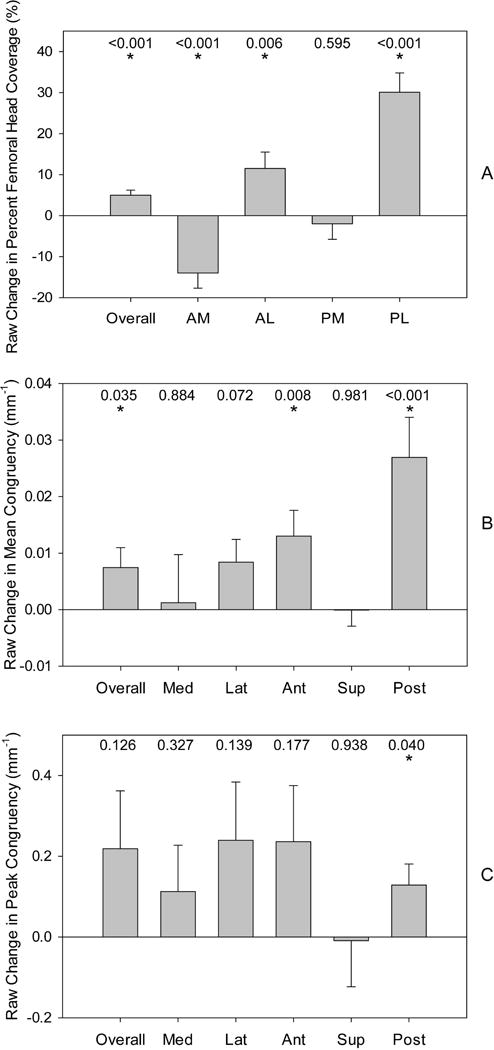
Raw changes in femoral head coverage and hip joint congruency following PAO. (A) The raw change in coverage of the femoral head indicated significant increases overall, and in the AL and PL regions; coverage decreased significantly in the AM region. Note: femoral head coverage was measured as the percent of the femoral head covered by the acetabulum. (B) Values for raw changes in mean congruency, expressed as the average of local congruency values for FE nodes in contact, indicated that the hip became less congruent overall, and the anterior and posterior regions. (C) Values for peak congruency, expressed as the most incongruent FE node in contact, indicated that the hip became less congruent in the posterior region. Bars indicate standard error. P values are listed and * indicates P ≤ 0.05. AM = anteromedial; AL = anterolateral; PM = posteromedial; PL = posterolateral.
Discussion
To our knowledge, this study is the first to analyze hip contact mechanics and morphometrics following PAO for the treatment of acetabular retroversion. Mean and peak acetabular cartilage contact stresses actually increased significantly following surgery and acetabular cartilage contact area decreased, which contradicts clinical intuition regarding the mechanical benefit of PAO. Despite these potentially negative changes, PAO medialized contact, thereby reducing load and stresses at the labrum. In addition, surgery increased posterior coverage. Although anterolateral coverage increased, anteromedial coverage decreased, and thus, it remains unclear if PAO is efficacious at preventing anterior hip impingement. Collectively, these results suggest that successful outcomes following PAO in retroverted hips11,31 may be due to a reduction in loads and stresses at the labrum and improved posterior coverage, and not the result of improved cartilage contact mechanics.
Reductions in cartilage contact stress may be important to prevent OA, as chronic exposure to static compression ex-vivo has been shown to damage hyaline cartilage.32 Be it for the treatment of dysplasia or acetabular retroversion, PAO has the common goal of preventing OA by reducing cartilage contact stresses via an increase in femoral head coverage.12,14,26 It was initially surprising to observe that, despite an increase in femoral head coverage, acetabular cartilage contact area decreased and contact stress increased following PAO. However, loss of congruency explained why cartilage contact stresses increased despite an improvement in coverage. Although none of the subjects in our study had Legg-Calvé-Perthes disease, each presented with loss of femoral head sphericity and head-neck offset. Also, three of the five subjects received a secondary radiographic diagnosis of cam-type FAI, which is not uncommon in hips with acetabular retroversion.33 Rotation of an aspherical femoral head made the hip less congruent, which in-turn induced areas of focal loading as evidenced by qualitative inspection of the contact stress plots as well as statistically significant changes in contact stress and contact area. These findings suggest that surgeons should not assume an increase in coverage will yield a proportional reduction in stress as congruency also plays an important mechanical role. This suggestion is reinforced by findings from a recent clinical study with a minimum follow-up of 10 years that determined traditionally dysplastic hips with aspherical femoral heads had lower survivorship rates following PAO compared to patients with more spherically-shaped femoral heads.34
In the setting of acetabular dysplasia, it has been hypothesized that hip OA occurs in an outward-to-in fashion,7 where excessive loads are placed on the acetabular labrum and chondrolabral junction, resulting in damage that progresses medially. OA could occur in a similar manner in retroverted hips, as both conditions are characterized by a loss of coverage. By medializing cartilage contact, PAO reduced lateral loading, thereby decreasing stress, contact area, and load transfer at the labrum. Although additional research is required, improvement in these metrics may halt the outward-to-in progression of OA. In addition, given that the labrum is nociceptive, reducing load sharing by the labrum may also alleviate pain. Furthermore, medializing contact may prevent feelings of instability, which is a common complaint among patients with acetabular insufficiency. However, medialization of the joint did not improve acetabular cartilage contact mechanics. In addition to the loss of joint congruency, we suspect that the orientation of the medial wall of the acetabulum may make it ill-suited to dissipate loads transferred across the hip. In particular, the medial wall is oriented roughly parallel with the applied joint reaction force.27 Thus, cartilage at the medial wall may have to undergo larger strains to dissipate the same amount of force as that absorbed by cartilage along the roof of the acetabulum.
The five subjects examined in our study were also analyzed in the FE modeling study by Henak et al., prior to undergoing PAO.15 Accordingly, our predictions in the pre-operative state agree with those reported by Henak. Nevertheless, minor differences were noted. For example, Henak et al. reported peak pressures in the range of 7–15 MPa, which is slightly less than 8–19 MPa reported in our study. In addition, average stresses predicted by Henak (~0.5–2.5 MPa) were less than our values (~2.4–4.7 MPa). These differences may arise because we only included a subset of the patients analyzed by Henak et al. In addition, we included the labrum in our FE models, Henak et al. did not. The labrum has been shown to bear load.8 Intuition would therefore suggest that cartilage stresses measured in our study would be less than those reported by Henak, yet this was not the case. We attribute these differences to the way cartilage stresses were calculated. Specifically, Henak averaged peak contact stress over six anatomical regions (see Figure 2 by Henak et al.15); this approach reduced the peak stress reported for each region since the location of peak stress was different between patients. Along these lines, Henak calculated an average based on the entire surface available for contact, whereas we calculated an average over the region that was actually in contact, which explains why our average stress was higher.
The absence of the posterior wall sign and cross-over sign following PAO may be indicative of a reduction in anterior coverage, an increase in posterior coverage, or a combination thereof. Based on our results, we suspect that it was an increase in posterior coverage that was primarily responsible for elimination of these signs. Specifically, on average, posterolateral femoral head coverage was more than doubled as a result of surgery. Anteromedial femoral head coverage was reduced, but interestingly, anterolateral coverage was significantly increased in almost the same amount. We would anticipate that an increase in anterolateral coverage would serve to retain the cross-over sign, rather than eliminate it. Collectively, results for femoral head coverage indicate that surgeons should be cautious when making inferences regarding the positon of the anterior and posterior walls based only on the appearance of the posterior wall sign and cross-over sign. This suggestion is not new, as the ability of the cross-over sign to describe the true orientation of the acetabulum has been questioned extensively (e.g.35).
Our values of femoral head coverage in the anteromedial, anterolateral, posteromedial, and posterolateral regions were approximately 61, 20, 90, and 28%, respectively, which correspond well with those reported by Hansen et al. for 16 retroverted hips using the same methodology to calculate coverage (52, 19, 81, and 29%, respectively).5 After surgery, we measured femoral head coverage for these regions at approximately 47, 32, 88, and 58%, respectively, which, with the exception of anterolateral coverage, closely align with data reported by Hansen for 18 control subjects (44, 18, 89, and 65%, respectively). Overall, this suggests that PAO may normalize the anatomic relationship of the hip. However, anterolateral coverage in the post-op group was larger than that measured in both the pre-op and control groups. It is currently unknown if symptoms of pincer-type impingement are precipitated as a result of excessive anteromedial or anterolateral coverage. Thus, the clinical relevance of increased anterolateral coverage is unclear, but it at least calls into question the ability of PAO to eliminate pincer-type FAI. It is for this reason that future work should examine how changes in coverage following PAO affect dynamic motion of the hip, perhaps using techniques such as dual fluoroscopy to measure hip kinematics and estimate the location of the impingement site.36
There are a few limitations to the study warrant discussion. The time-intensive process to generate and analyze patient-specific FE models in both pre- and post-operative configurations as well as the need for repeated CT scans prohibited the use of a large sample size. Also, it is possible that bone and/or cartilage remodeling could occur following PAO, but we performed the post-operative CT scan at short-term follow-up. To maintain consistency, identical boundary and loading conditions were applied across subjects and operative states using the Bergmann dataset.27 Bergmann’s data were acquired from hip OA patients who underwent hip arthroplasty, who were substantially older than the subjects in our study. Also, given that many retroverted patients experience reduced range of motion on clinical exam, it is likely that they also have adaptations to their gait, which may have been misrepresented using the Bergmann dataset. The use of identical loading and boundary conditions was justified, however, as it enabled us to focus on alterations in chondrolabral mechanics due to changes in femoral head coverage and congruency; it would have been difficult to isolate the mechanical importance of changes in coverage and congruency if patient-specific loading parameters were included. Finally, patients had screws in their hips at the time of the post-operative CT. Metal artifact was minimal, and thus, we do not believe it affected the accuracy of our segmentation. It is possible that the screws contributed to the strength of the pelvis, but screws were located some distance away from the acetabulum, and the osteotomy site had healed completely in all patients. Thus, we believe inclusion of the screws would have minimal impact on FE predictions of chondrolabral mechanics.
In conclusion, we found that PAO nearly doubled posterior coverage, decreased contact stress, substantially decreased load sharing to the labrum, and medialized the location of contact. Others have proposed that hip OA occurs in an outward-to-in manner in dysplastic hips by overloading the labrum. Accordingly, PAO may prevent OA in retroverted hips by unloading the labrum. However, the hip became less congruent, anterolateral coverage increased, and acetabular cartilage contact mechanics were not improved following PAO. The lack of improvement in acetabular contact mechanics was likely caused by a less congruent hip following surgery. In addition, medialization of the hip put the medial wall of acetabulum in contact with the femoral head, but this region may not dissipate loads effectively. A longer term follow-up of these patients will be necessary to establish the association between hip contact mechanics and survivorship following PAO. Ideally, FE models could be developed and analyzed for these patients at various time points to develop predictive models of OA based on chondrolabral contact mechanics. However, our protocol may be ill-suited for this purpose, as it requires exposure to radiation. Nevertheless, results obtained herein are clinically important, as they suggest surgeons should not assume an increase in femoral head coverage will yield a proportional decrease in contact stress.
Supplementary Material
Acknowledgments
Financial support was provided by the National Institutes of Health (NIH R01-AR053344, R01-GM083925, R01-EB016701, R21-AR3466184, 5UL1TR001067), and the LS-Peery Discovery Program in Musculoskeletal Restoration The research content herein is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or LS-Peery Foundation. The authors also acknowledge Greg Stoddard for statistical consultation.
Footnotes
Author Contributions Statement: Spencer Knight processed data, conducted the study, and drafted the manuscript. Christine Abraham contributed to the design of the study, collected and processed data, performed the statistics, and interpreted study results. Christopher Peters contributed to the design of the study, assisted with clinical interpretation, and reviewed the results for accuracy. Jeffrey Weiss contributed to the design of the study and interpreted study results. Andrew Anderson designed the study, supervised the study, reviewed the results for accuracy, and assisted with clinical interpretation. All authors provided revisions and final approval of the manuscript.
Conflict of Interest: None of the authors report conflicts of interest associated with the design, execution, and publication of this study.
References
- 1.Murphy LB, Helmick CG, Schwartz TA, et al. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthritis Cartilage. 2010;18:1372–1379. doi: 10.1016/j.joca.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 4.Dandachli W, Islam SU, Liu M, et al. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031–1036. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 5.Hansen BJ, Harris MD, Anderson LA, et al. Correlation between radiographic measures of acetabular morphology with 3D femoral head coverage in patients with acetabular retroversion. Acta Orthop. 2012;83:233–239. doi: 10.3109/17453674.2012.684138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell ME, Shivanna KH, Grosland NM, et al. Cartilage contact pressure elevations in dysplastic hips: a chronic overload model. J Orthop Surg Res. 2006;1:6. doi: 10.1186/1749-799X-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henak CR, Abraham CL, Anderson AE, et al. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage. 2014;22:210–217. doi: 10.1016/j.joca.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henak CR, Ellis BJ, Harris MD, et al. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011;44:2201–2206. doi: 10.1016/j.jbiomech.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 10.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Siebenrock KA, Schaller C, Tannast M, et al. Anteverting periacetabular osteotomy for symptomatic acetabular retroversion: results at ten years. J Bone Joint Surg Am. 2014;96:1785–1792. doi: 10.2106/JBJS.M.00842. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Klaue K, Vinh TS, et al. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988:26–36. [PubMed] [Google Scholar]
- 13.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003:263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 14.Tibor LM, Sink EL. Periacetabular osteotomy for hip preservation. Orthop Clin North Am. 2012;43:343–357. doi: 10.1016/j.ocl.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Henak CR, Carruth ED, Anderson AE, et al. Finite element predictions of cartilage contact mechanics in hips with retroverted acetabula. Osteoarthritis Cartilage. 2013;21:1522–1529. doi: 10.1016/j.joca.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson AE, Ellis BJ, Maas SA, et al. Effects of idealized joint geometry on finite element predictions of cartilage contact stresses in the hip. J Biomech. 2010;43:1351–1357. doi: 10.1016/j.jbiomech.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clohisy JC, St John LC, Nunley RM, et al. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res. 2009;467:2221–2227. doi: 10.1007/s11999-009-0810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henak CR, Abraham CL, Peters CL, et al. Computed tomography arthrography with traction in the human hip for three-dimensional reconstruction of cartilage and the acetabular labrum. Clin Radiol. 2014;69:e381–391. doi: 10.1016/j.crad.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson AE, Ellis BJ, Maas SA, et al. Validation of finite element predictions of cartilage contact pressure in the human hip joint. J Biomech Eng. 2008;130:051008. doi: 10.1115/1.2953472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henak CR, Kapron AL, Anderson AE, et al. Specimen-specific predictions of contact stress under physiological loading in the human hip: validation and sensitivity studies. Biomech Model Mechanobiol. 2014;13:387–400. doi: 10.1007/s10237-013-0504-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson AE, Ellis BJ, Peters CL, et al. Cartilage thickness: factors influencing multidetector CT measurements in a phantom study. Radiology. 2008;246:133–141. doi: 10.1148/radiol.2461062192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson AE, Peters CL, Tuttle BD, et al. Subject-specific finite element model of the pelvis: development, validation and sensitivity studies. J Biomech Eng. 2005;127:364–373. doi: 10.1115/1.1894148. [DOI] [PubMed] [Google Scholar]
- 23.Harris MD, Anderson AE, Henak CR, et al. Finite element prediction of cartilage contact stresses in normal human hips. J Orthop Res. 2012;30:1133–1139. doi: 10.1002/jor.22040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dalstra M, Huiskes R. Load transfer across the pelvic bone. Journal Of Biomechanics. 1995;28:715–724. doi: 10.1016/0021-9290(94)00125-n. [DOI] [PubMed] [Google Scholar]
- 25.Quapp KM, Weiss JA. Material characterization of human medial collateral ligament. J Biomech Eng. 1998;120:757–763. doi: 10.1115/1.2834890. [DOI] [PubMed] [Google Scholar]
- 26.Ferguson SJ, Bryant JT, Ito K. The material properties of the bovine acetabular labrum. J Orthop Res. 2001;19:887–896. doi: 10.1016/S0736-0266(01)00007-9. [DOI] [PubMed] [Google Scholar]
- 27.Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech. 2001;34:859–871. doi: 10.1016/s0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 28.Maas SA, Ellis BJ, Ateshian GA, et al. FEBio: finite elements for biomechanics. J Biomech Eng. 2012;134:011005. doi: 10.1115/1.4005694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Puso MA, Maker BN, Ferencz RM, et al. NIKE3D: A Nonlinear, Implicit, Three-Dimensional Finite Element Code for Solid and Structural Mechanics. User’s Manual 2007 [Google Scholar]
- 30.Finner H. On a Monotonicity Problem in Step-Down Multiple Test Procedures. Journal of the American Statistical Association. 1993;88:920–923. [Google Scholar]
- 31.Parry JA, Swann RP, Erickson JA, et al. Midterm Outcomes of Reverse (Anteverting) Periacetabular Osteotomy in Patients With Hip Impingement Secondary to Acetabular Retroversion. Am J Sports Med. 2016;44:672–676. doi: 10.1177/0363546515620382. [DOI] [PubMed] [Google Scholar]
- 32.Guilak F, Fermor B, Keefe FJ, et al. The role of biomechanics and inflammation in cartilage injury and repair. Clin Orthop Relat Res. 2004:17–26. doi: 10.1097/01.blo.0000131233.83640.91. [DOI] [PubMed] [Google Scholar]
- 33.Albers CE, Steppacher SD, Tannast M, et al. Surgical Technique: Reverse Periacetabular Osteotomy. In: Nho SJ, Leunig M, Larson CM, et al., editors. Hip Arthroscopy and Hip Joint Preservation Surgery. Springer; 2014. pp. 637–651. [Google Scholar]
- 34.Albers CE, Steppacher SD, Ganz R, et al. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614. doi: 10.1007/s11999-013-2799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473:1247–1254. doi: 10.1007/s11999-014-4055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kapron AL, Aoki SK, Peters CL, et al. Subject-specific patterns of femur-labrum contact are complex and vary in asymptomatic hips and hips with femoroacetabular impingement. Clin Orthop Relat Res. 2014;472:3912–3922. doi: 10.1007/s11999-014-3919-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


