Abstract
Background
We attempt to develop a relatively comprehensive structural model of risk factors for drug abuse (DA) in Swedish men that illustrates developmental and mediational processes.
Methods
We examined 20 risk factors for DA in 48,369 men undergoing conscription examinations in 1969–70 followed until 2011 when 2.34% (n = 1134) of them had DA ascertained in medical, criminal and pharmacy registries. Risk factors were organized into four developmental tiers reflecting i) birth, ii) childhood/early adolescence, iii) late adolescence, and iv) young adulthood. Structural equational model fitting was performed using Mplus.
Results
The best fitting model explained 47.8% of the variance in DA. The most prominent predictors, in order, were: early adolescent externalizing behavior, early adult criminal behavior, early adolescent internalizing behavior, early adult unemployment, early adult alcohol use disorder, and late adolescent drug use. Two major inter-connecting pathways emerged reflecting i) genetic/familial risk and ii) family dysfunction and psychosocial adversity. Generated on a first and tested on a second random half of the sample, a model from these variables predicted DA with an ROC area under the curve of 83.6%. Fifty-nine percent of DA cases arose from subjects in the top decile of risk.
Conclusions
DA in men is a highly multifactorial syndrome with risk arising from familial-genetic, psychosocial, behavioral and psychological factors acting and interacting over development. Among the multiple predisposing factors for DA, a range of psychosocial adversities, externalizing psychopathology and lack of social constraints in early adulthood are predominant.
Keywords: Drug abuse, Development, Environment, Personality, Structural equation model, Externalizing pathway
1. Introduction
Drug Abuse (DA) is a multifactorial syndrome influenced by a wide range of biological, psychological and socio-cultural risk factors (Hawkins et al., 1986; West, 2006). More specifically, individual risk factors for DA include genes (Tsuang et al., 1996), aspects of the childhood environment (Grant et al., 2009) (including child abuse (Kendler et al., 2000; Fergusson and Mullen, 1999), parental loss (Hawkins et al., 1986; Kendler et al., 2012), and parental behaviors (Hawkins et al., 1992; Hawkins et al., 1986)), urbanicity (Sundquist and Frank, 2004; Grant et al., 2009), peer group deviance (Farrington, 2005; Hawkins et al., 1998; Patterson et al., 2000; Marshal et al., 2003; Hawkins et al., 1992; Hawkins et al., 1986), internalizing traits and symptoms (Kessler et al., 2005), intellectual and school functioning (Gigi et al., 2014; Hawkins et al., 1992; Hawkins et al., 1986), externalizing traits and behaviors (Kessler et al., 2005; Kendler et al., 2003; Brook et al., 1996; Hawkins et al., 1992; Hawkins et al., 1986; Blanco et al., 2013)(including use of alcohol and cigarettes (Kessler et al., 2005; Kandel, 1975; Blanco et al., 2013)), and, later in development, absence of social constraints such as marriage, employment and church attendance (Grant et al., 2009; Blanco et al., 2013).
Given the wide range of these risk factors and the diversity of developmental stages at which they impact, a comprehensive understanding of the pathways to DA requires more than their enumeration in review articles (e.g., (Hawkins et al., 1986)) or their testing in multiple regression models (Blanco et al., 2013). Optimally informative will be models that capture the dynamic relations between individuals, their behavioral and psychiatric symptoms and their social contexts across development. Particularly, such models can clarify mediational mechanisms that could be targets for intervention. As articulated by Dodge et al. the goal of such research should be to provide “a map for how myriad genetic, biological, social, and ecological factors conspire to produce disorders in adolescence … [especially] substance abuse (Dodge et al., 2009, p. 3)”.
We here present such a study utilizing a sample of 48,276 Swedish males born 1947–1953 whom we followed until 2011. Detailed information on risk factors was available for this cohort at an average age of 18 from the Conscript Registry and has been supplemented from other registry resources that can provide risk factors from earlier and later ages. DA is ascertained from the Swedish national medical, pharmacy and criminal registers.
2. Materials and methods
This study utilizes men conscripted into military service in Sweden in 1969 and 1970. In those years, only 2–3% of all Swedish men were exempt from conscription, largely due to severe handicaps or congenital disorders (Neovius et al., 2009). We collected information from several sources on these individuals. First, we used information from the conscript register. The national birth cohorts used in this study are unique among all conscript material in Sweden, as more extensive data were collected at conscription during these years. Information from the conscript register about the individuals was collected through questionnaires, with questions about medical symptoms, childhood and adolescent traits and behaviors, and alcohol and tobacco use. We call these variables conscript self-report data (CSRD). Second, during conscription direct assessments of psychological function were performed. We call these conscript test scores register. We then linked the conscript database to the Multi-Generation Register, providing information on family relations and to Population Registers providing information on education and geographical status. We also linked the database to the Swedish Medical Registers consisting of the Swedish Hospital Discharge Register, containing all hospitalizations for all Swedish inhabitants from 1969 to 2011 and the Outpatient Care Register, containing information from outpatient clinics from 2001 to 2011; to the Swedish Criminal registers consisting of the Swedish Crime Register, containing national complete data on all convictions from 1973 to 2011, the Swedish suspicion register, containing national complete data on all individuals strongly suspected of crime from 1998 to 2011; and finally to the Swedish Prescribed Drug Register, containing all prescriptions in Sweden picked up by patients from 2005 to 2010. The linking was done using each person’s unique identification number. To preserve confidentiality, this ID number was replaced by a serial number. We secured ethical approval for this study from the Regional Ethical Review Board of Lund University (No. 2008/409).
2.1. Outcome variable
DA was identified in the Swedish medical and mortality registers by ICD codes (ICD8: Drug dependence (304); ICD9: Drug psychoses (292) and Drug dependence (304), Nondependent abuse of drugs (305; excluding 305.0); ICD10: Mental and behavioral disorders due to psychoactive substance use (F10–F19), except those due to alcohol (F10) or tobacco (F17)); in the Suspicion Register by codes 3070, 5010, 5011, and 5012, that reflect crimes related to DA; in the Crime Register by references to laws covering narcotics (law 1968:64, paragraph 1, point 6) and drug-related driving offences (law 1951:649, paragraph 4, Subsection 2 and paragraph 4A, Subsection 2); and in the Prescribed Drug Register in individuals (excluding those suffering from cancer) who had retrieved (in average) more than four defined daily doses a day for 12 months from either of Hypnotics and Sedatives (Anatomical Therapeutic Chemical (ATC) Classification System N05C and N05BA) or Opioids (ATC: N02A).
DA was treated as dichotomous variable with an assumed underlying normal liability distribution.
2.2. Sample
From the 50,529 individuals who were conscripted into military service during 1969–1970, we excluded those not born between 1947 and 1953, to insure our sample was of similar age; females; and cases with duplicate ID number (n = 834). Of the remaining 49,691 individuals, we excluded 1322 individuals with more than 10% missing values based on all our included covariates (see below for covariates). In total, we investigated 48,369 individuals. 99.1% of the sample were ages 18–20 at conscript evaluation.
2.3. Model variables
We organized the predictor variables into four groups approximating four developmental periods: 1) birth (Father alcohol consumption, Low parental education and genetic risk (for DA, criminal behavior or alcohol use disorder – all highly genetically correlated in the Swedish population (Kendler et al., 2016a)), 2) childhood and early adolescence (Frequency of Corporal Punishment, Disruption in family [i.e., loss of one or more parents through death or divorce before age 18], Low Parental monitoring, Move during childhood, Urbanization, Internalizing Behavior and Externalizing Behavior), 3) late adolescence (Neighborhood Socioeconomic Status, Low Resilience, Low IQ, Sniffing Glue and Drug use score), and 4) early adulthood (Low education, Unemployed, Unmarried, Criminal Behavior, Alcohol use disorder). Of the 20 final predictor variables, 4 were latent (internalizing behavior, externalizing behavior, Drug use score, and Neighborhood SES) and were constructed using a measurement model from other observed variables. Sniffing glue, assessed at conscription, loaded poorly on the drug use factor and therefore was included as an independent item in the model. See the Appendix Table A1 for a detailed definition of all variables. In addition to these 20, the following other variables were included in earlier drafts of the model but were excluded because they provided minimal additional predictive power: Peer Deviance (share of Drug Abusers in close geographical proximity during early adolescence (Kendler et al., 2015)), Prosocial Behavior (from CSRD), Familial Socioeconomic status (from CRSD), Repeat year in school (from CSRD), Psychiatric Genetic Risk Score (based on Psychiatric registrations in close relatives), Alcohol consumption during adolescence (from CSRD), Educational status (from population registers),Smoking status during adolescence (from CSRD).
2.4. Statistical methods
Of the 48,369 individuals, 37,843 had no missing values; 7271, had below 2%; and 3255 had between 2 and 10%. To impute values, we used the Predicted Regression imputation method within specific groups of questions; that is using regression models to predict missing values based on similar covariates. We divided the material into five groups and performed the predicted regression method within each group. The five groups were Drug-related questions (all questions for the DA score and the question on Sniffing Glue), Externalizing Behavior, Internalizing Behavior (all questions included in the factor analysis for internalizing behavior and Resilience), Socioeconomic and Family-variables (Low Parental education, Disruption in family, IQ, Urbanization, Low education, Unmarried, Parental monitoring, Unemployment, Move during childhood), and Others (Genetic Risk Score, Fathers Alcohol consumption and Frequency of Corporal Punishment).
Our structural equation model consisted of two parts. First a measurement model consisted of factor loadings for the observed variables that index the four latent variables and second a structural model that consisted of path and correlation coefficients connecting the four latent and the 16 observed variables of the model. For the structural model, we followed an approach developed in previous similar studies (Kendler et al., 2002; Kendler et al., 2011; Kendler et al., 2016b). We began with a fully saturated model and used a combination of three approaches to produce a model with the optimal balance of explanatory power and parsimony. Note that variables in the first tier are interconnected by correlations, depicted by two-headed arrows in the figures, rather than partial regression coefficients, depicted by one-headed arrows. In the first step, observing the significance levels of individual paths, we fixed sets of paths to zero when the associated z value was < 1.96. Second, some paths that remained significant were too small to be meaningful. Therefore, the second step was to set all path estimates to zero with a value of < 0.05, regardless of z value. Third, we added and subtracted paths that were marginal by significance and/or magnitude to see if we could arrive at a better overall fit and indeed produced a modest improvement in fit and explanatory power. We utilized two fit indices that reflect the success of the model in balancing explanatory power and parsimony: the Tucker-Lewis index (TLI) (Tucker and Lewis, 1973) and the root mean square error of approximation (RMSEA)(Steiger, 1990). For the Tucker-Lewis index and comparative fit index, values between 0.90 and 0.95 are considered acceptable and values ≥0.95 as good. For the RMSEA, good models have values ≤0.05. The fit function was weighted least squares. Model fitting was done by using Mplus, version 7.31 (Muthén and Muthén, 2015).
To evaluate the predictive power of our model variables, we performed a logistic regression model on a random half of the sample to predict DA and evaluated it on the other half of the sample using a ROC curve. We then divided the predicted probability in the validation sample into deciles and calculated the rates of DA in each decile.
3. Results
3.1. Model fitting
Our final sample for model fitting included 48,369 individuals of whom 1134 (2.34%) were registered for DA. We could follow 88.6% of the sample until 2011, with 7.5% lost to death and 3.9% to emigration. Mean length of follow-up (SD) was 36.4 (5.6) years and the mean age at first DA registration was 42.7 (12.4). The best-fit model fitted well (TLI = 0.99 and RMSEA = 0.03) and explained 47.8% of the variance in DA liability. The observed correlations between all 20 variables in the model are seen in Appendix Table A2.
3.2. Parameter estimates
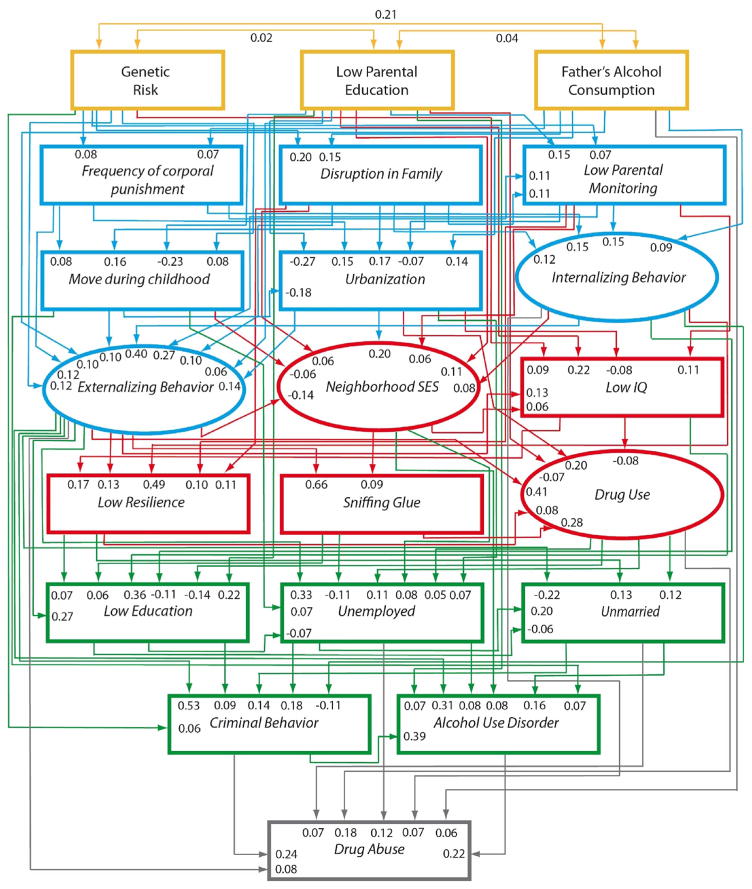
Table 1 provides a summary of the best-fit modeling results, which are presented in detail in Fig. 1 and Table 2. The four levels of our model are color-coded (see figure legend).
Table 1.
The Twenty Risk Factors for Drug Abuse Used in Our model, their total and indirect effects on Drug Abuse, the Origin of the Variable and the Major Mediating Variables.
| Total effecta | Total Indirect Effecta | Origin of Variable | Major Mediating Variables | |
|---|---|---|---|---|
| Genetic Risk (HRB) | 0.123 | 0.123 | MR, CR, PR | CB, Ext |
| Parental Education | 0.010 | 0.010 | CSRD | AUD, DU Score |
| Father’s Alcohol Consumption | 0.176 | 0.116 | CSRD | Ext, CB |
| Frequency of Corporal Punishment | 0.112 | 0.112 | CSRD | Ext, CB |
| Disruption in Family | 0.131 | 0.131 | CSRD | Ext, Int |
| Parental Monitoring | 0.162 | 0.162 | CSRD | CB, Ext |
| Move during childhood | 0.051 | 0.051 | CSRD | AUD, Ext |
| Urbanization | 0.130 | 0.130 | CSRD | DU Score, Ext |
| Internalizing Behavior | 0.244 | 0.175 | CSRD | Ext, CB |
| Externalizing Behavior | 0.474 | 0.392 | CSRD | CB, DU Score |
| Neighborhood SES | 0.038 | 0.038 | PR | AUD, Unemployed |
| Low IQ | −0.010 | −0.010 | CTS | DU Score, Education |
| Low Resilience | 0.037 | 0.037 | CTS | DU Score, Unmarried |
| Sniffing Glue | 0.035 | 0.035 | CSRD | DU Score, Unemployed |
| Drug Use Score | 0.211 | 0.029 | CSRD | Unmarried, Unemployed |
| Low education | 0.004 | 0.004 | PoR | CB, Unemployed |
| Unemployed | 0.225 | 0.106 | PoR | CB, AUD |
| Unmarried | 0.147 | 0.016 | PoR | CB, AUD |
| CB | 0.324 | 0.087 | CR | AUD |
| AUD | 0.221 | CR, MR | ||
| R2 | 0.478 | |||
| RMSEA | 0.032 (90% CI: 0.032; 0.033) | |||
| TLI | 0.987 | |||
CSRD: Conscript self-report data; PR: Population Register; MGR: Multi-generational Register: CR: Criminal Register; MR: Medical Register; PR: Prescription Register; CTS: Test-score from conscript register; CB: Criminal Behavior; AUD: Alcohol Use Disorder; Ext: Externalizing Behavior; Int: Internalizing Behavior; DU Score: Drug Use Score.
Total effect reflects the association between the variable and the outcome (drug abuse registration) via all the paths in the model. Total indirect effect reflects this association minus the direct effect of any path from the variable to the outcome. Direct effect (not given) is simple the total effect minus the total indirect effect.
Fig. 1.
Results of our best fit model for the prediction of drug abuse. Two-headed arrows represent correlation coefficients while one-headed arrows represent path coefficients or standardized partial regression coefficients. The variables were ordered to approximate a developmental process within 4 time periods which are colored coded: birth – yellow, 2) childhood and early adolescence – blue, 3) late adolescence – red, 4) and early adulthood – green. Three of the 20 predictor variables were latent and constructed, using a measurement model, from other observed variables: internalizing behavior, externalizing behavior, alcohol score and drug use/abuse. See the Appendix Table A1 for a detailed description of each variable.
Table 2.
All Path Values (Standardized Regression Coefficients) for Best Fit Model.
| From | To | Path Coefficient |
|---|---|---|
| Genetic Risk | Frequency of Corporal Punishment | 0.08 (0.07; 0.09) |
| Disruption in Family | 0.20 (0.19; 0.22) | |
| Parental Monitoring | 0.07 (0.05; 0.08) | |
| Externalizing Behavior | 0.12 (0.11; 0.13) | |
| Move during childhood | 0.08 (0.07; 0.09) | |
| Low IQ | 0.09 (0.08; 0.10) | |
| Criminal Behavior | 0.06 (0.04; 0.08) | |
|
| ||
| Low Parental Education | Externalizing Behavior | 0.06 (0.05; 0.07) |
| Parental Monitoring | 0.15 (0.14; 0.16) | |
| Low IQ | 0.22 (0.20; 0.23) | |
| Move during childhood | −0.23 (−0.24; −0.22) | |
| Urbanization | −0.27 (−0.28; −0.26) | |
| Neighborhood SES | 0.11 (0.10; 0.12) | |
| Drug Use | −0.07 (−0.08; −0.05) | |
| Low Education | 0.22 (0.21; 0.23) | |
| Alcohol Use Disorder | 0.07 (0.04; 0.10) | |
|
| ||
| Fathers Alcohol Consumption | Frequency of Corporal Punishment | 0.07 (0.05; 0.08) |
| Disruption in Family | 0.15 (0.14; 0.16) | |
| Urbanization | 0.14 (0.12, 0.15) | |
| Internalizing Behavior | 0.09 (0.08; 0.11) | |
| Externalizing Behavior | 0.10 (0.09; 0.11) | |
| Drug Abuse | 0.06 (0.04; 0.09) | |
|
| ||
| Frequency of Corporal Punishment | Parental Monitoring | 0.11 (0.10; 0.12) |
| Move during childhood | 0.08 (0.07; 0.09) | |
| Internalizing Behavior | 0.15 (0.14; 0.16) | |
| Externalizing Behavior | 0.12 (0.11; 0.13) | |
|
| ||
| Disruption in Family | Parental Monitoring | 0.11 (0.09; 0.12) |
| Move during childhood | 0.16 (0.14; 0.17) | |
| Urbanization | 0.17 (0.15; 0.19) | |
| Internalizing Behavior | 0.12 (0.11; 0.13) | |
| Externalizing Behavior | 0.10 (0.09; 0.12) | |
| Neighborhood SES | 0.06 (0.04; 0.07) | |
| Low Resilience | 0.11 (0.10; 0.12) | |
|
| ||
| Low Parental Monitoring | Urbanization | −0.07 (−0.08; −0.06) |
| Internalizing Behavior | 0.15 (0.14; 0.16) | |
| Externalizing Behavior | 0.27 (0.26; 0.28) | |
| Neighborhood SES | 0.06 (0.05; 0.07) | |
| Low IQ | 0.11 (0.10; 0.12) | |
| Low Resilience | 0.10 (0.09; 0.11) | |
|
| ||
| Move during childhood | Urbanization | −0.18 (−0.20; −0.17) |
| Externalizing Behavior | 0.10 (0.09; 0.11) | |
| Neighborhood SES | −0.06 (−0.07; −0.05) | |
| Unemployed | 0.07 (0.04; 0.10) | |
| Alcohol Use Disorder | 0.07 (0.04; 0.10) | |
|
| ||
| Urbanization | Externalizing Behavior | 0.14 (0.12; 0.15) |
| Neighborhood SES | 0.20 (0.19; 0.22) | |
| Low IQ | −0.08 (−0.09; −0.07) | |
| Drug Use | 0.20 (0.19; 0.22) | |
| Unemployed | 0.07 (0.04; 0.09) | |
|
| ||
| Internalizing Behavior | Externalizing Behavior | 0.40 (0.39; 0.41) |
| Neighborhood SES | 0.08 (0.0.7; 0.10) | |
| Low Resilience | 0.49 (0.49; 0.50) | |
| Low Education | −0.11 (−0.13; −0.10) | |
| Criminal Behavior | −0.11 (−0.13; −0.09) | |
| Drug Abuse | 0.07 (0.04; 0.10) | |
|
| ||
| Externalizing Behavior | Neighborhood SES | −0.14 (−0.15; −0.12) |
| Low IQ | 0.13 (0.12; 0.14) | |
| Low Resilience | 0.13 (0.12; 0.15) | |
| Sniffing Glue | 0.66 (0.65; 0.67) | |
| Drug Use | 0.41 (0.39; 0.43) | |
| Low Education | 0.27 (0.25; 0.29) | |
| Unemployed | 0.33 (0.29, 0.37) | |
| Unmarried | −0.22 (−0.25; 0.19) | |
| Criminal Behavior | 0.53 (0.51; 0.56) | |
| Alcohol Use Disorder | 0.31 (0.27; 0.34) | |
| Drug Abuse | 0.08 (0.03; 0.13) | |
|
| ||
| Neighborhood SES | Low IQ | 0.06 (0.05; 0.07) |
| Sniffing Glue | 0.09 (0.08; 0.11) | |
| Unemployed | 0.08 (0.05; 0.10) | |
| Alcohol Use Disorder | 0.08 (0.06; 0.11) | |
|
| ||
| Low IQ | Low Resilience | 0.17 (0.16; 0.18) |
| Drug Use | −0.08 (−0.10; −0.07) | |
| Low Education | 0.36 (0.35; 0.37) | |
|
| ||
| Low Resilience | Drug Use | 0.08 (0.07; 0.09) |
| Low Education | 0.07 (0.06; 0.09) | |
| Unmarried | 0.13 (0.12; 0.15) | |
|
| ||
| Sniffing Glue | Drug Use | 0.28 (0.26; 0.30) |
| Low Education | 0.06 (0.03; 0.08) | |
| Unemployed | −0.11 (−0.17; −0.06) | |
|
| ||
| Drug Use | Low Education | −0.14 (−0.16; −0.12) |
| Unemployed | 0.05 (0.00; 0.10) | |
| Unmarried | 0.12 (0.10; 0.15) | |
| Drug Abuse | 0.18 (0.15; 0.22) | |
|
| ||
| Low Education | Unemployed | −0.07 (−0.09; −0.04) |
| Unmarried | −0.06 (−0.08; −0.05) | |
| Criminal Behavior | 0.09 (0.07; 0.11) | |
|
| ||
| Unemployed | Unmarried | 0.20 (0.17; 0.23) |
| Criminal Behavior | 0.18 (0.15; 0.21) | |
| Alcohol Use Disorder | 0.08 (0.03; 0.12) | |
| Drug Abuse | 0.12 (0.08; 0.16) | |
|
| ||
| Unmarried | Criminal Behavior | 0.14 (0.12; 0.16) |
| Alcohol Use Disorder | 0.16 (0.13; 0.19) | |
| Drug Abuse | 0.07 (0.03; 0.10) | |
|
| ||
| Criminal Behavior | Alcohol Use Disorder | 0.39 (0.36; 0.43) |
| Drug Abuse | 0.24 (0.19; 0.28) | |
|
| ||
| Alcohol Use Disorder | Drug Abuse | 0.22 (0.17; 0.28) |
We first summarize the main findings and then review, selectively, more detailed results. We divided our 20 predictor variables into four groups based on their total effect on risk: large (≥0.20), moderate (0.10–0.19), modest (0.05–0.09), and small (≤0.05). Six variables had a large effect and, in order of effect-size, were: i) early adolescent externalizing behavior, ii) early adult criminal behavior, iii) early adolescent internalizing behavior, iv) early adult unemployment, v) early adult alcohol use disorder, and vi) late adolescent drug use. Seven variables had a moderate effect size: i) father’s alcohol consumption, ii) early adolescent parental monitoring, iii) early adult unmarried status, iv) early adolescent family disruption, v) early adolescent urbanization, vi) genetic risk, and vii) frequency of corporal punishment. The remaining seven variables had modest or small effect sizes, the largest of which were moving during childhood, late adolescent neighborhood SES and low resilience.
Table 1 also notes the total indirect effect on DA from each variable (with the difference between the total and indirect effect equaling the direct effect). With structural models, the closer the predictor variable is to the outcome variable (here DA), the fewer indirect paths are available and, therefore, on average, the higher is the proportion of total effect that is direct. This trend is seen in Table 1, although it is noteworthy that three variables relatively early in the model (father’s alcohol consumption and early adolescent internalizing and externalizing behavior) have direct effects on DA risk.
One of the important advantages of structural over standard regression models is their ability to clarify mediational pathways. Table 1 notes the two most important mediational variables for all risk factors. The five most important mediators, from this list, were (along with number of variables they mediated): i) early adult criminal behavior (9), ii) early adolescent externalizing behavior (8), iii) early adult alcohol use disorder (6), iv) late adolescent drug use (5), v) and early adult unemployment (4). Of note, early adolescent externalizing behavior, drug use score and criminal behavior were often a key mediator for variables in the early, middle and later parts of our developmental model.
3.3. Pathways of risk
Five features of the full model (Fig. 1) are noteworthy. First, we see a strong interrelated set of psychosocial adversities in the top half of the model beginning with the highly interconnected low parental educational – with paths to nine diverse down-stream variables – and including low parental monitoring, low neighborhood SES in late adolescence and low educational attainment. Second, we see diverse influences of genetic/familial effects across a range of predictors including family disruption, frequency of corporal punishment, externalizing behavior, criminal behavior and DA itself. Third, internalizing behavior plays only a relatively modest role in the model despite a substantial total effect on DA. It is protective against criminal behavior and has a moderate, direct and positive path to DA itself. Fourth, externalizing behavior in late adolescence is a central mediational “hub” in the pathway to DA receiving paths from all nine variables above it and projecting paths to all eleven variables below it. Finally, four of the five variables measured in early adulthood (all but low education) have a direct path to DA and were diverse, including two other externalizing syndromes (criminality and AUD) and two variables reflecting social constraints: marriage and employment.
3.4. Aggregate prediction of risk
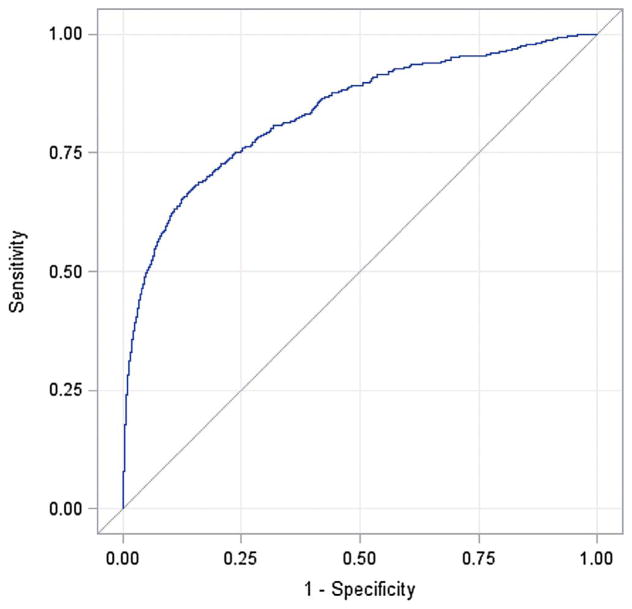
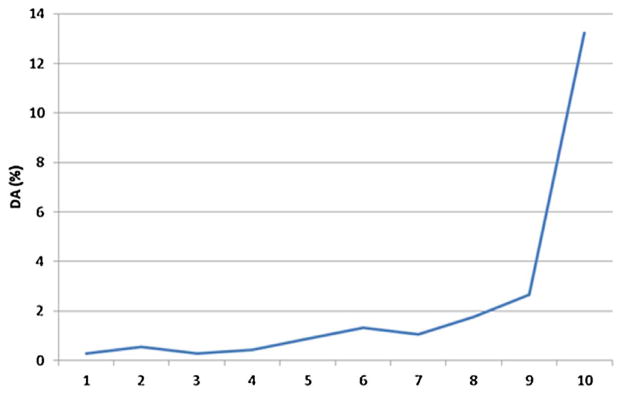
Using all 20 predictor variables, we developed a predictive index for DA risk on a random half of our sample and then applied it to the second random half (Table 3). ROC analysis of the replication sample (Fig. 2) produced an area under the curve of 83.6%. We then divided this score in the replicate sample into deciles which were strongly related to risk for DA (Fig. 3). Indeed, 58.8 and 70.6% of DA cases arose from those in, respectively, the top 10 and 20% of risk.
Table 3.
Multivariate Logistic Regression Model Predicting Drug Abuse Registration.
| Variable | OR |
|---|---|
| Genetic Risk (Mid vs Low) | 1.20 (0.94; 1.53) |
| Genetic Risk (High vs Low) | 1.63 (1.30; 2.04) |
| Fathers Alcohol Consumption (Mid vs Low) | 1.12 (0.87; 1.45) |
| Fathers Alcohol Consumption (High vs Low) | 1.32 (0.90; 1.94) |
| Parental Education (Low vs High) | 1.03 (0.73; 1.46) |
| Parental Education (Mid vs High) | 1.17 (0.83; 1.67) |
| Frequency of Corporal Punishment (Sometime vs Never) | 0.80 (0.65; 0.97) |
| Frequency of Corporal Punishment (Occasionally vs Never) | 0.90 (0.68; 1.18) |
| Frequency of Corporal Punishment (Often vs Never) | 0.59 (0.33; 1.05) |
| Disruption in Family | 1.05 (0.84; 1.30) |
| Parental Monitoring (MidLow vs Low) | 0.97 (0.76; 1.23) |
| Parental Monitoring (MidHigh vs Low) | 0.99 (0.74; 1.32) |
| Parental Monitoring (High vs Low) | 0.76 (0.50; 1.18) |
| Move during childhood 1 vs 0 | 0.95 (0.75; 1.20) |
| Move during childhood 2 vs 0 | 1.54 (0118; 2.02) |
| Move during childhood 3+ vs 0 | 1.50 (1.13; 1.99) |
| Urbanization vs Countryside | 1.38 (1.12; 1.70) |
| Sniffing Glue | 1.29 (1.04; 1.61) |
| Education (Low vs High) | 1.06 (0.77; 1.45) |
| Education (Mid vs High) | 1.14 (0.87; 1.50) |
| Unemployed vs Employed | 1.83 (1.37; 2.45) |
| Not Married vs Married | 1.56 (1.28; 2.91) |
| Low IQ (1 unit) | 1.15 (1.09; 1.21) |
| Low Resilience (1 unit) | 1.03 (0.97; 1.10) |
| Externalizing Behavior (1 Std) | 1.28 (1.16; 1.41) |
| Internalizing Behavior (1 Std) | 1.10 (0.99; 1.23) |
| Neighborhood SES (1 Std) | 0.94 (0.84; 1.05) |
| Drug Use (1 Std) | 1.44 (1.34; 1.54) |
| AUD Registration | 3.40 (2.51; 4.59) |
| Criminal Registration | 4.41 (3.54; 5.50) |
Fig. 2.
Receiver Operating Characteristic Curve for the prediction of Drug Abuse from our Aggregate Risk Factor index developed from a multivariate logistic regression analysis on a first random half of our sample and then tested on our second half. The X-axis assesses “1-specificity” while the Y-Axis reflects sensitivity. The area under the curve is estimated ( ± 95% CIs) at 0.836 (0.817–0.855).
Fig. 3.
The Proportion of Individuals in our Replication Sample with a Diagnosis of Drug Abuse (DA) in Each Decile of our Predictive Risk Index constructed from all twenty predictor variables.
4. Discussion
4.1. Main findings
We sought to increase our understanding of the etiologic pathways to DA in men by evaluating an etiologic developmental model for DA which included a diversity of risk factors integrated from a large representative population sample followed up into late middle age. While the value of “multifactorial” (Kendler, 2005), “biopsychosocial” (Engel, 1977), or “multi-level” (Schaffner, 1994) models are often noted in psychiatric research, their empirical implementation is challenging. The best such models require i) an adequately sized sample with a diversity of measured risk factors, ii) a sufficient follow-up period to generate an adequate number of cases and iii) a statistical approach that can capture the richness of the results avoiding over-simplification and overwhelming complexity. While not without limitations, we suggest our results represent a useful draft for such a model for DA in Swedish men.
Of our numerous specific findings, we emphasize six, which we discuss in turn. First, our set of risk factors were relatively successful in predicting DA in the general population. Our path model accounted for over 47% of the variance in risk for DA and an aggregate measure of our risk factors from a multiple regression was robustly predictive of DA in an ROC analysis. Using this measure, we demonstrated that the liability to DA was highly concentrated in a small at-risk proportion of the population.
Second, our results support the importance of environmental risk factors for DA and suggest that they can be meaningfully divided by developmental period. In childhood and adolescence, the environmental risks occurred both at the level of the family (dysfunction and disruption) and the community (urbanization and low SES). A wide variety of prior research suggests that these risk factors broadly predispose to a range of externalizing behaviors including DA (Dube et al., 2003; Hawkins et al., 1992; Farrington, 2005; Granic and Patterson, 2006; Hawkins et al., 1998). Notably, peer deviance, an environmental factor that is typically a robust predictor of risk for drug use and DA in males (Svensson, 2003), was insufficiently predictive in initial analyses to merit inclusion in the model. This may be due to the nature of the data, with peer deviance i operationalized as physical proximity while growing up to other future drug abusers. A more direct measure of deviancy in friends might have yielded different results. In early adulthood, the important environmental variables – marriage and employment – maybe qualitatively different as when earlier confounding influences are controlled for (as in our model), they likely reflect social constraints which protect against drug use, DA, and other externalizing syndromes (Compton et al., 2005; Bachman et al., 1997; Laub and Sampson, 2006; Dick and Kendler, 2012).
Third, our findings are congruent with prior evidence of the importance of an “externalizing pathway” to DA (Zucker, 2008; Agrawal et al., 2004; Iacono et al., 2008). We see this most clearly by the central role played in our model by the variable “externalizing behavior in early adolescence.” Of note, both genetic risk and parental alcohol consumption predict externalizing behaviors, consistent with prior evidence for an etiologic role for genetically influenced personality traits on externalizing behaviors in general and DA in particular (Hicks et al., 2004; Kendler and Myers, 2013; Elkins et al., 2006). We also show quite strong continuity in this externalizing pathway. Externalizing behavior in early adolescence robustly predicted future drug use, criminal behavior and AUD with paths of respectively +0.41, +0.53 and +0.31.
Fourth, our results demonstrate the developmental inter-weaving of genetic/temperamental and family/social risk factors in the etiology of DA. One cannot, in our best-fit model, cleanly disentangle the genetic/temperamental and environmental paths of risk. Early environmental adversities are, along with familial/genetic processes, strong predictors of externalizing behaviors in adolescence. Those same behaviors then predict key environmental exposures in early adulthood – single marital status and unemployment.
Fifth, our structural model shows the value of clarifying mediational mechanisms in pathways of risk. Just four risk factors – externalizing behavior, criminal behavior, being unmarried, and being unemployed –were key mediational variables to drug abuse for 75% of the risk factors in the model.
Sixth, our model identified a range of potentially malleable risk factors that could be points of intervention/prevention. Although a range of practical difficulties would arise in trying to implement such interventions, they include effects in childhood (reduction of corporal punishment, improvement in parental monitoring), early and late adolescence (reduction in externalizing behaviors, improvement in resilience, reduction in drug experimentation), and early adulthood (staying in school, steady employment, strong social support such as marriage and avoidance of criminal behaviors and alcohol abuse).
Our results can be usefully contrasted to parallel analyses using the same sample with many of the same predictors that we recently completed for AUD (Kendler et al., 2016b). Most notably, we could account for twice the risk variance in DA (47.8%) compared to AUD (23.4%). Variables which much more strongly predicted DA than AUD – urbanization, adolescent externalizing and internalizing behaviors, unemployment, unmarried status and prior criminal behavior – were distributed across development.
Our findings can also be helpfully compared with a prior effort, using hierarchical logistic regression, to predict lifetime cannabis use and last year cannabis use disorder (CUD) in wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (Blanco et al., 2013). While the specific predictors varied between the two studies, both agreed on the importance of a number of risk domains for DA (including disruptions in the home of origin, adolescent internalizing and externalizing symptoms, prior drug use, low educational attainment, and lack of current social constraints) and the need to understand these multiple domains in a developmental context (Blanco et al., 2013).
In our multivariate logistic regression model presented in Table 3, greater frequency of corporal punishment reduces risk for DA. This is odd given that the univariate correlation between the two variables is +0.14 (Appendix Table A2) and univariate logistic regression analyses show that frequent versus no parental abuse strongly predicts risk for DA (OR = 3.05 [1.92; 4.86]). Such apparently paradoxical results may arise in multivariate regression due to co-linearity among predictor variables and is likely a result of the substantial positive correlation in our data between frequency of corporal punishment and internalizing and externalizing behavior.
4.2. Limitations
These results should be interpreted in the context of nine potentially important methodologic limitations. First, this sample consisted of males born in Sweden and may not extrapolate to women or to other ethnic samples. Rates of drug use and abuse in Sweden are probably representative of other Northern European countries (Degenhardt et al., 2011). Second, DA was ascertained using medical and criminal records which are not dependent on subject cooperation or accurate recall. Compared to interviews, these methods likely generate both false positive and false negative diagnoses. While large interview-based studies of DA prevalence do not exist in Sweden, lifetime prevalence of drug abuse and dependence in near-by Norway – assessed at personal interview in the 1990s – was estimated in men at 4.4% (Kringlen et al., 2001), suggesting some false negatives in our sample. The validity of our ascertainment method is supported by the high concordance for registration across our inpatient and criminal registries (OR = 59.0 (47.3; 73.5)).
Third, our model assumes a causal relationship between predictor and dependent variables that is not likely to be always true. Some of the inter-variable relationships we assume to be A → B may be either A ← B or, more likely, A ↔ B. Others may result from confounding variables predicting both A and B. Fourth, some variables assessed at conscription required recall and may therefore be biased.
Fifth, the sequence of variables in our model was only approximate. However, when we switched the order of model variables we found either no change or slight deteriorations in model fit and explanatory power. This suggests that our results are not sensitive to the specific order of our model variables. Sixth, our model assumes that our predictor variables act additively and linearly in their impact on DA risk. This is unlikely to be always true; however, introducing non-linear relationships would have greatly increased the complexity of our model. Seventh, age at first DA registration in our sample was implausibly high. This likely results from the availability of the suspicion, out-patient and pharmacy registries only after 1997 and suggests that first registration in our sample is a poor index of actual onset of DA. Eighth, data on specific drugs of abuse were not available on most of this sample so we were unable to examine the similarity or differences of risk pathways to distinct forms of DA.
Finally, our model likely underestimated the impact of our early adult measures as a substantial number of individuals probably had a first registration for DA prior to completing their education or establishing stable employment or marital relationships. We therefore repeated our main analysis restricting first registrations for DA to age 25 or older, which included 85% of the onsets. While this sample was biased toward later onset DA, we found that the proportion of variance in liability to DA predicted by several of our early adult measures increased including especially low education (0.004 → 12.6%), but also unemployment (22.5 → 25.8%) and unmarried status (14.7 → 18.9%).
5. Conclusions
DA in men is an etiologically complex syndrome influenced by a wide diversity of risk factors that act and interact over development. Pathways of risk are complex and move fluidly between domains traditionally conceptualized as biological, psychological and environmental. Mediational paths for most risk factors include two key externalizing risk factors (externalizing behaviors of adolescence or crimes in early adulthood) or two exposures that likely increase social constraint assessed in early adulthood: marriage and employment. The risk factors identified in this study prospectively predict onset of DA with considerable power and show that the large majority of cases come from those at highest risk. Models of prevention and intervention for DA are likely to be most effective when built on empirical rigorous and relatively comprehensive etiologic models. We hope that our findings can be usefully integrated into primary health care, and both general psychiatric and addiction psychiatric practice.
Supplementary Material
Acknowledgments
This project was supported by grants R01DA030005 and K01AA021399 from the National Institutes of Health, the Swedish Research Council (K2012-70X-15428-08-3), the Swedish Research Council for Health, Working Life and Welfare (In Swedish: Forte; Reg.nr: 2013-1836), the Swedish Research Council (2012-2378; 2014-10134) and FORTE (2014-0804) as well as ALF funding from Region Skåne awarded.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.drugalcdep.2017.06.036.
Footnotes
Conflict of interest
The authors have no conflicts of interest to declare.
Role of the Funder/Sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Location
Center for Primary Health Care Research, Lund University, Malmö, Sweden and Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA.
Author contributions
All authors have materially participated in the research and/or article preparation and all authors have approved the final article.
Drs. Kendler and K. Sundquist had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Kendler, Ohlsson, K. Sundquist.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Kendler.
Critical revision of the manuscript for important intellectual content: Kendler, Ohlsson, J. Sundquist, K. Sundquist.
Statistical Analysis: Ohlsson, Kendler.
Obtained funding: K. Kendler, K. Sundquist, J. Sundquist.
Administration, technical, or material support: K. Sundquist, J. Sundquist, K. Kendler.
Study supervision: Kendler K, K Sundquist.
References
- Agrawal A, Jacobson KC, Prescott CA, Kendler KS. A twin study of personality and illicit drug use and abuse/dependence. Twin Res. 2004;7:72–81. doi: 10.1375/13690520460741462. [DOI] [PubMed] [Google Scholar]
- Bachman JG, Wadsworth KN, O'Malley PM, Johnston LD, Schulenberg JE. Smoking, Drinking, and Drug Use in Young Adulthood: The Impacts of New Freedoms and New Responsibilities. Lawrence Erlbaum Associates; Mahwah, NJ: 1997. [Google Scholar]
- Blanco C, Rafful C, Wall MM, Ridenour TA, Wang S, Kendler KS. Towards a comprehensive developmental model of cannabis use disorders. Addiction. 2013;109:284–294. doi: 10.1111/add.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Whiteman M, Finch SJ, Cohen P. Young adult drug use and delinquency: childhood antecedents and adolescent mediators. J Am Acad Child Adolesc Psychiatry. 1996;35:1584–1592. doi: 10.1097/00004583-199612000-00009. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Bucello C, Calabria B, Nelson P, Roberts A, Hall W, Lynskey M, Wiessing L, Mora ME, Clark N, Thomas J, Briegleb C, McLaren J GBD illicit drug use writing group. What data are available on the extent of illicit drug use and dependence globally? Results of four systematic reviews. Drug Alcohol Depend. 2011;117:85–101. doi: 10.1016/j.drugalcdep.2010.11.032. [DOI] [PubMed] [Google Scholar]
- Dick DM, Kendler KS. The impact of gene-environment interaction on alcohol use disorders. Alcohol Res. 2012;34:318–324. [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Malone PS, Lansford JE, Miller S, Pettit GS, Bates JE. A dynamic cascade model of the development of substance-use onset. Monogr Soc Res Child Dev. 2009;74:vii–119. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, Iacono WG. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: prospective links from adolescence to young adulthood. J Abnorm Psychol. 2006;115:26–39. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- Engel GL. The need for a new medical model. A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Farrington D. Childhood origins of antisocial behavior. Clin Psychol Psychother. 2005;12:177–190. [Google Scholar]
- Fergusson DM, Mullen PE. Childhood Sexual Abuse: An Evidence Based Perspective. Sage Publications, Inc; Thousand Oaks, CA: 1999. [Google Scholar]
- Gigi K, Werbeloff N, Goldberg S, Portuguese S, Reichenberg A, Fruchter E, Weiser M. Borderline intellectual functioning is associated with poor social functioning, increased rates of psychiatric diagnosis and drug use-A cross sectional population based study. Eur Neuropsychopharmacol. 2014;24:1793–1797. doi: 10.1016/j.euroneuro.2014.07.016. [DOI] [PubMed] [Google Scholar]
- Granic I, Patterson GR. Toward a comprehensive model of antisocial development: a dynamic systems approach. Psychol Rev. 2006;113:101–131. doi: 10.1037/0033-295X.113.1.101. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use: mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Lishner DM, Catalano RF, Howard MO. Childhood predictors of adolescent substance abuse: toward an empirically grounded theory. J Child Contemp Soc. 1986;18:11–48. [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Herrenkohl T, Farrington DP, Brewer D, Catalano RF, Harachi TW. A review of predictors of youth violence. In: Loeber R, Farrington DP, editors. Serious and Violent Juvenile Offenders: Risk Factors and Successful Interventions. Sage Publications, Inc; London, U.K: 1998. pp. 106–146. [Google Scholar]
- Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: a twin-family study. Arch Gen Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Ann Rev Clin Psychol. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Kandel D. Stages in adolescent involvement in drug use. Science. 1975;190:912–914. doi: 10.1126/science.1188374. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J. The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychol Med. 2013;44:647–655. doi: 10.1017/S0033291713000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. Am J Psychiatry. 2002;159:1133–1145. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for alcohol use disorders in men. Twin Res Hum Genet. 2011;14:1–15. doi: 10.1375/twin.14.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Sundquist K, Ohlsson H, Palmer K, Maes H, Winkleby MA, Sundquist J. Genetic and familial environmental influences on the risk for drug abuse: a national Swedish adoption study. Arch Gen Psychiatry. 2012;69:690–697. doi: 10.1001/archgenpsychiatry.2011.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Ohlsson H, Mezuk B, Sundquist K, Sundquist J. Exposure to peer deviance during childhood and risk for drug abuse: a Swedish national co-relative control study. Psychol Med. 2015;45:855–864. doi: 10.1017/S0033291714001937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Lonn SL, Maes HH, Lichtenstein P, Sundquist J, Sundquist K. A Swedish population-based multivariate twin study of externalizing disorders. Behav Genet. 2016a;46:183–192. doi: 10.1007/s10519-015-9741-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Ohlsson H, Edwards AC, Sundquist J, Sundquist K. A developmental model for alcohol use disorders in Swedish men. Psychol Med. 2016b Jul;:1–12. doi: 10.1017/S0033291716001409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS. Toward a philosophical structure for psychiatry. Am J Psychiatry. 2005;163:433–440. doi: 10.1176/appi.ajp.162.3.433. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry. 2001;158:1091–1098. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]
- Laub JH, Sampson RJ. Shared Beginnings, Divergent Lives: Delinquent Boys to Age 70. Harvard University Press; Cambridge, MA: 2006. [Google Scholar]
- Marshal MP, Molina BS, Pelham WE., Jr Childhood ADHD and adolescent substance use: an examination of deviant peer group affiliation as a risk factor. Psychol Addict Behav. 2003;17:293–302. doi: 10.1037/0893-164X.17.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide: 1998–2015. 7. Muthén and Muthén; Los Angeles, CA: 2015. [Google Scholar]
- Neovius M, Sundstrom J, Rasmussen F. Combined effects of overweight and smoking in late adolescence on subsequent mortality: nationwide cohort study. BMJ. 2009;338:b496. doi: 10.1136/bmj.b496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Dishion TJ, Yoerger K. Adolescent growth in new forms of problem behavior: macro- and micro-peer dynamics. Prev Sci. 2000;1:3–13. doi: 10.1023/a:1010019915400. [DOI] [PubMed] [Google Scholar]
- Schaffner KF. Psychiatry and Molecular Biology: Reductionistic Approaches to Schizophrenia in Philosophical Perspectives on Psychiatric Diagnostic Classification. Johns Hopkins University Press; Baltimore, MD: 1994. [Google Scholar]
- Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivar Behav Res. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Sundquist K, Frank G. Urbanization and hospital admission rates for alcohol and drug abuse: a follow-up study of 4.5 million women and men in Sweden. Addiction. 2004;99:1298–1305. doi: 10.1111/j.1360-0443.2004.00810.x. [DOI] [PubMed] [Google Scholar]
- Svensson R. Gender differences in adolescent drug use – the impact of parental monitoring and peer deviance. Youth Soc. 2003;34:300–329. [Google Scholar]
- Tsuang MT, Lyons MJ, Eisen SA, Goldberg J, True W, Meyer JM, Toomey R, Faraone SV, Eaves L. Genetic influences on abuse of illicit drugs: a study of 3,297 twin pairs. Am J Med Genet. 1996;67:473–477. doi: 10.1002/(SICI)1096-8628(19960920)67:5<473::AID-AJMG6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- West R. Theory of Addiction. 1. Wiley-Blackwell, Addiction Press; 2006. [Google Scholar]
- Zucker RA. Anticipating problem alcohol use developmentally from childhood into middle adulthood: what have we learned? Addiction. 2008;103(Suppl 1):100–108. doi: 10.1111/j.1360-0443.2008.02179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.