Abstract
Background
The hypertension cure rate of unilateral adrenalectomy in primary aldosteronism (PA) patients varies widely in existing studies.
Methods
We conducted an observational meta-analysis to summarize the pooled hypertension cure rate of unilateral adrenalectomy in PA patients. Comprehensive electronic searches of PubMed, Embase, Cochrane, China National Knowledge Internet (CNKI), WanFang, SinoMed and Chongqing VIP databases were performed from initial state to May 20, 2016. We manually selected eligible studies from references in accordance with the inclusion criteria. The pooled hypertension cure rate of unilateral adrenalectomy in PA patients was calculated using the DerSimonian–Laird method to produce a random-effects model.
Results
Forty-three studies comprising approximately 4000 PA patients were included. The pooled hypertension cure rate was 50.6% (95% CI: 42.9–58.2%) for unilateral adrenalectomy in PA. Subgroup analyses showed that the hypertension cure rate was 61.3% (95% CI: 49.4–73.3%) in Chinese studies and 43.7% (95% CI: 38.0–49.4%) for other countries. Furthermore, the hypertension cure rate at 6-month follow-up was 53.3% (95% CI: 36.0–70.5%) and 49.6% (95% CI: 40.9–58.3%) for follow-up exceeding 6 months. The pooled hypertension cure rate was 50.9% (95% CI: 40.5–61.3%) from 2001 to 2010 and 50.2% (95% CI: 39.0–61.5%) from 2011 to 2016.
Conclusions
The hypertension cure rate for unilateral adrenalectomy in PA is not optimal. Large clinical trials are required to verify the utility of potential preoperative predictors in developing a novel and effective prediction model.
Keywords: Adrenalectomy, Hypertension, Primary aldosteronism, Meta-analysis, Review
Background
Primary aldosteronism (PA) is a group of disorders in which aldosterone production is inappropriately high for sodium status, relatively independent of the major regulators of secretion (e.g., angiotensin II, plasma potassium concentration), and is not suppressed by sodium loading [1]. Some studies have reported that PA is present in >5% of hypertensive patients and may exceed 10% [2–4]. PA is typically caused by an adrenal adenoma and unilateral or bilateral adrenal hyperplasia. However, in a small proportion of cases, adrenal carcinoma and familial hyperaldosteronism can also precipitate PA.
Idiopathic hyperaldosteronism (IHA) should be medically treated with a mineralocorticoid receptor antagonist, whereas unilateral primary aldosteronism, which includes aldosterone-producing adenoma (APA) and unilateral adrenal hyperplasia (UAH), is curable by surgical intervention [5]. However, after unilateral adrenalectomy, not all PA patients are completely cured of their hypertension, despite normalization of the biochemical marker abnormalities. After adrenalectomy for unilateral primary aldosteronism, complete hypertension cure rate and the factors associated with complete hypertension cure are variable. Previous studies have reported hypertension cure rates ranging from 35% to 63.8%, with intrinsic risk factors being identified. These include age, gender, duration of hypertension, body mass index (BMI), and preoperative prescribing of antihypertensive agents [6–9]. Furthermore, a meta-analysis of the 25 studies with 1685 patients showed that the pooled proportion of normotension following adrenalectomy is 52% [10]. However, the study selects 25 articles which 4 Chinese studies only. A multicenter epidemiologic study in 11 provinces of China between January 2010 and October 2011 reveals that PA prevalence is 7.1% among 1656 patients with resistant hypertension [11]. Given the high prevalence, PA patients in China are more and more interested in solving the problem of hypertension by adrenalectomy. Consequently, in the present study, we added the Chinese-language publication data and established more strict inclusion criteria to more comprehensively estimate the complete hypertension cure rate of unilateral adrenalectomy in PA patients.
Methods
Literature search strategy
Online retrieval of the following databases was conducted: PubMed, Embase, Cochrane, China National Knowledge Internet (CNKI), WanFang, SinoMed and Chongqing VIP. Eligible studies were manually selected from references according to the inclusion criteria. The search date was from initial state to May 20, 2016. The following keywords were used to identify potentially relevant studies from all databases: ‘hyperaldosteronism’ and ‘adrenalectomy’. We also retrieved the references from all relevant publications to obtain further salient studies. Two independent reviewers (Yu Zhou and Mei-Lian Zhang) conducted the literature screen of relevant titles and abstracts according to inclusion and excluding criteria. Su-jie Ke was the adjudicator for any articles that were disputed.
Inclusion and exclusion criteria
The following criteria were used for screening of the literature: (1) all PA patients to undergo unilateral adrenalectomy and sample size should be ≥20; (2) study design comprised case-control and cohort studies; (3) the study provided the complete hypertension cure rate of unilateral adrenalectomy, or sufficient data for derivation of the pooled hypertension cure rate; (4) hypertension cure criteria was defined as normal blood pressure (systolic blood pressure (SBP) <140 mmHg and diastolic blood pressure (DBP) <90 mmHg) without requirement for antihypertensive medications; (5) each study should provide a clear follow-up period; (6) the study was written in English and Chinese. Those studies which were not eligible for inclusion were excluded. If multiple published reports were from the same study cohort, we only included the study with the most detailed information and sample size.
Extraction of data
All data were extracted separately by the two aforementioned investigators. In the event of a dispute between the investigators, a discussion was conducted in order to arrive at consensus. Information obtained from each study included: author’s first name, year of publication, country, years of inclusion, follow-up time, patients cured, patients followed up, cure rate (%), pathological results, and study type.
Statistical analysis
This study was conducted and reported according to the recommendation of the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group [12]. Heterogeneity between the studies was estimated by calculating the I 2 statistic, which shows the percentage of variation between studies due to heterogeneity rather than by chance. I 2 < 25% is considered low, 25–50% considered moderate, and >50% is regarded as high-level heterogeneity [13, 14]. Given the high heterogeneity between studies, we used the DerSimonian and Laird method in generating the random effects models for the pooled estimation of prevalence. We conducted an analysis of subgroups to explore the potential sources of heterogeneity, including country (China and Other), follow-up time (≥6 months and <6 months), number of patients followed up (≥50 and <50), Publication Year (2001–2010 and 2011–2016), and pathology (APA Only and Other). Sensitivity analyses were conducted by excluding prospective studies. Funnel plots and the Egger test were used to test for publication bias. A P value of less than 0.05 was considered statistically significant. All statistical calculations were performed using STATA, version 12 (STATA, College Station, TX). Ethics approval was not required as this was a secondary, literature-based study.
Results
Literature search
The literature search process is depicted in Fig. 1. The literature search initially yielded a total of 3410 articles, of which 691 duplicates were excluded and 2634 studies were removed after reviewing titles and abstracts. Thus, 85 studies were chosen for full-text assessment and critical appraisal. We excluded the cited articles for the following reasons: no follow-up period (n = 1); no hypertension cure criteria (n = 18); sample size <20 (n = 4); article with overlapping data (n = 11); article with no calculation of cure rate (n = 4); non-English language (n = 1); Out of full-text (n = 3). Finally, there were 43 studies included in our meta-analyses [6–9, 15–53].
Fig. 1.

Flow diagram of included/excluded studies
Study characteristics
The main characteristics from the included studies are shown in Table 1. The relevant number of patients followed up ranged from 20 to 376, with a total sample size of 3776. All studies were in Chinese and English. Studies were carried out in different countries, including the USA, China, Japan, Italy, Sweden, Germany, Australia, Czech Republic, Singapore and France. Forty of the included studies were methodologically retrospective. In contrast, only three studies were prospective cohort studies. All the cases were pathologically confirmed postoperatively.
Table 1.
Characteristics of the Included Studies
| Study,Year | Country | Years of Inclusion | Follow-up Time | Patients Cured | Patients Followed | Cure Rate(%) | Pathology | Study Type |
|---|---|---|---|---|---|---|---|---|
| Horita et al. 2001 [15] | Japan | 1977–1999 | >6 months | 13 | 26 | 50.0 | APA | retrospective |
| Sawka et al. 2001 [16] | America | 1993–1999 | 0.1–77.9 months | 31 | 93 | 33.3 | APA + Other | retrospective |
| Fukudome et al. 2002 [17] | Japan | 1976–1998 | 1.2–23.1 years | 34 | 46 | 73.9 | APA | retrospective |
| Rossi et al. 2002 [18] | America | 1994–2000 | 1-63 months | 20 | 30 | 66.7 | APA + Other | retrospective |
| Tan et al. 2002 [19] | China | 1984–2001 | >3 months | 44 | 46 | 95.7 | APA + Other | retrospective |
| Goh et al. 2004 [20] | Singapore | 1996–2002 | 1-60 months | 23 | 46 | 50.0 | APA + Other | retrospective |
| Meyer et al. 2005 [21] | Germany | 1988–2001 | 38-134 months | 8 | 24 | 33.3 | APA + Other | retrospective |
| Omura et al.2006 [6] | Japan | 1995–2005 | 1 year | 44 | 69 | 63.8 | APA | retrospective |
| Han et al.2006 [22] | China | 2003–2005 | 3-37 months | 35 | 47 | 74.5 | APA + Other | retrospective |
| Pang et al.2007 [23] | Australia | 1995–2005 | >1 month | 18 | 53 | 34.0 | APA + Other | prospective |
| Ziaja et al.2007 [24] | Poland | 1995–2005 | 1-10 years | 10 | 31 | 32.3 | APA + Other | retrospective |
| Walz et al.2008 [25] | Germany | 1994–2007 | >1 years | 48 | 160 | 30.0 | APA + Other | prospective |
| Zarnegar et al.2008 [7] | America | 1994–2005 | >6 months | 35 | 100 | 35.0 | APA + Other | retrospective |
| White et al.2008 [26] | America | 1996–2007 | 0.1–96.7 months | 38 | 54 | 70.4 | APA + Other | retrospective |
| Mourad et al.2008 [27] | France | 1997–1999 | 30-56 months | 23 | 58 | 39.7 | APA | retrospective |
| Wu et al.2009 [8] | China | 1999–2007 | >1 year | 95 | 150 | 63.3 | APA | retrospective |
| Chiou et al.2009 [28] | China | 1987–2006 | >6 months | 18 | 51 | 35.3 | APA | retrospective |
| Campagnacci et al.2009 [29] | Italy | 1994–2006 | 20-128 months | 21 | 50 | 42.0 | APA | retrospective |
| Wang et al.2010 [30] | China | 2002–2007 | 1.2–5.3 years | 54 | 93 | 58.1 | APA | retrospective |
| Tresallet et al.2010 [31] | France | 1997–2008 | >6 months | 33 | 57 | 57.9 | APA + Other | retrospective |
| Mathur et al.2010 [32] | America | NA | 1 month-9 year | 17 | 85 | 20.0 | APA + Other | retrospective |
| Kim et al.2010 [33] | Korea | 1995–2008 | 6-159 months | 16 | 27 | 59.3 | APA | retrospective |
| Fu et al.2011 [34] | China | 2000–2004 | >1 years | 61 | 212 | 28.8 | APA | prospective |
| Waldmann et al.2011 [35] | Germany | 1993–2009 | >1 years | 17 | 30 | 56.7 | APA + Other | retrospective |
| Tang et al.2011 [36] | China | 1999–2009 | 6 months-2 years | 180 | 227 | 79.2 | APA + Other | retrospective |
| Wang et al.2011 [37] | China | 2008–2010 | 1 week-1 year | 10 | 25 | 40.0 | APA + Other | retrospective |
| Linden et al.2012 [38] | France | 2001–2009 | 6-12 months | 68 | 156 | 43.5 | APA + Other | retrospective |
| Wang et al.2012 [39] | China | 2008–2010 | >6 months | 43 | 83 | 51.8 | APA + Other | retrospective |
| Wang et al.2012 [40] | China | 2009–2011 | 6-18 months | 17 | 20 | 85.0 | APA + Other | retrospective |
| Wang et al.2012 [41] | China | 2002–2009 | >6 months | 44 | 82 | 53.7 | APA | retrospective |
| Zhang et al.2013 [42] | China | 2005–2011 | >6 months | 207 | 376 | 55.1 | APA | retrospective |
| Aronova et al.2014 [43] | America | 2004–2013 | >1 years | 21 | 47 | 44.7 | APA | retrospective |
| Jiang et al.2014 [44] | China | 2004–2011 | 15-110 months | 88 | 164 | 53.7 | UAH | retrospective |
| Lim et al.2014 [45] | China | 1993–2011 | 1.9–11.7 years | 127 | 133 | 95.4 | APA + Other | retrospective |
| Wachtel et al.2014 [46] | America | 1997–2013 | >1 years | 13 | 85 | 15.3 | APA + Other | retrospective |
| Hartmann et al.2014 [47] | Czech Republic | 2001–2011 | 1 year | 17 | 51 | 33.3 | APA + Other | retrospective |
| Utsumi et al.2014 [48] | Japan | 1995–2012 | >6 months | 56 | 132 | 42.4 | APA + Other | retrospective |
| Wolley et al.2015 [49] | Australia | 2000–2014 | 6-24 months | 29 | 80 | 36.3 | APA + Other | retrospective |
| Xie et al.2015 [9] | China | 2009–2014 | 0.17-5 years | 43 | 94 | 45.7 | APA | retrospective |
| Hu et al.2015 [50] | China | 2009–2014 | >1 years | 29 | 46 | 63.0 | APA + Other | retrospective |
| Citton et al.2015 [51] | Italy | 1990–2013 | 1 month | 67 | 122 | 54.9 | APA + Other | retrospective |
| Volpe et al.2015 [52] | Sweden | 1985–2010 | 0.5-26 years | 46 | 120 | 38.3 | APA + Other | retrospective |
| Fujita et al.2016 [53] | Japan | 2000–2015 | >1 years | 36 | 95 | 37.9 | APA + Other | retrospective |
Hypertension cure rate of unilateral adrenalectomy in PA
Unilateral adrenalectomy in PA resulted in an overall hypertension cure rate that ranged between 15.0% and 96.0%. The overall meta-analysis cure rate was 50.6% (95% CI: 42.9–58.2%; Fig. 2). The hypertension cure rate of unilateral adrenalectomy in PA also indicated a high level of heterogeneity between the studies (I2 = 96.6%, P < 0.0001).
Fig. 2.
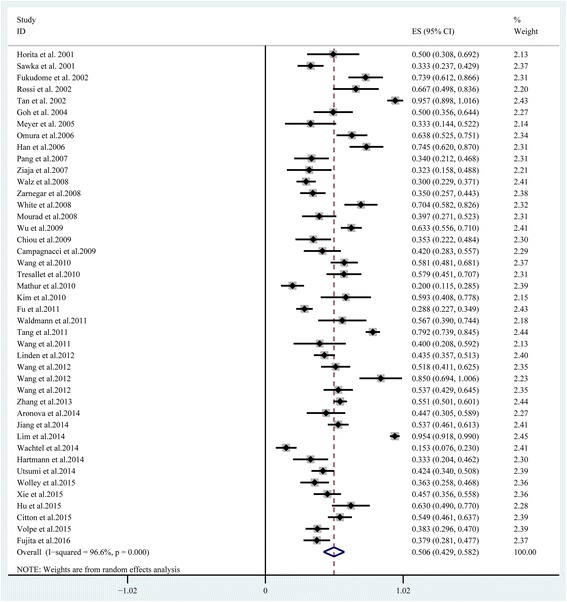
Forest plot of hypertension cure rate of unilateral adrenalectomy for all PA patients
The population of PA can be further stratified according to country (China and Other), follow-up time (≥6 months and <6 months), patients followed up (≥50 and <50), Publication Year (2001–2010 and 2011–2016), and pathology (APA Only and Other). The pooled hypertension cure rate of these subgroups is presented in Table 2. In the country setting, the hypertension cure rate of unilateral adrenalectomy in PA in China was 61.3% (95% CI: 49.4–73.3%) from 1849 patients. The pooled cure rate from other countries (43.7%, 95% CI: 38.0–49.4%) was significantly lower than that reported in China (P for subgroup difference < 0.0001). The hypertension cure rate of unilateral adrenalectomy for those followed up over a period of <6 months (53.3%, 95% CI: 36.0–70.5%) was higher than the group followed up over a period of ≥6 months (49.6%, 95% CI: 40.9–58.3%). The cure rate in the number of patients followed up being <50 (59.5%, 95% CI: 46.9–72.1%) was significantly higher than that of the ≥50 group (46.6%, 95% CI: 37.4–55.7%). The pooled hypertension cure rate did not change significantly over time. The pooled cure rate was 50.9% (95% CI: 40.5–61.3%) from 2001 to 2010, which was very similar to the rate of 50.2% (95% CI: 39.0–61.5%) from those studied in 2011 to 2016. In the postoperative pathology setting, there was no significant difference in the APA Only group (50.9%, 95% CI: 43.5–58.2%) and the Other group (50.4%, 95% CI: 39.9–60.8%). The aforementioned subgroups had a high level of heterogeneity.
Table 2.
Hypertension cure rate of unilateral adrenalectomy by different categories
| Category | Subgroup | NO. of Studies | Cute Rate (95% CI) (%) | N | I2 (%) | P |
|---|---|---|---|---|---|---|
| Country | China | 16 | 0.613 (0.494–0.733) | 1849 | 97.5 | <0.0001 |
| Other | 27 | 0.437 (0.380–0.494) | 1972 | 85.9 | <0.0001 | |
| Follow-up Time | ≥6 months | 32 | 0.496 (0.409–0.583) | 3081 | 96.7 | <0.0001 |
| <6 months | 11 | 0.533 (0.360–0.705) | 695 | 96.6 | <0.0001 | |
| Patients Followed | 》50 | 29 | 0.466 (0.374–0.557) | 3285 | 97.2 | <0.0001 |
| <50 | 14 | 0.595 (0.469–0.721) | 491 | 91.3 | <0.0001 | |
| Publication Year | 2001–2010 | 22 | 0.509 (0.405–0.613) | 1396 | 94.9 | <0.0001 |
| 2011–2016 | 21 | 0.502 (0.390–0.615) | 2380 | 97.5 | <0.0001 | |
| Pathology | APA Only | 14 | 0.509 (0.435–0.582) | 1381 | 86.3 | <0.0001 |
| Other | 29 | 0.504 (0.399–0.608) | 2395 | 97.4 | <0.0001 |
Publication bias and sensitivity analysis
From visual examination of the funnel plots, considerable publication bias was evident (Fig. 3). Probability for the Egger test was less than 0.001. The sensitivity analysis was conducted by excluding the three prospective cohort studies and the results remained the same.
Fig. 3.

Begg funnel plot for hypertension cure rate of unilateral adrenalectomy
Discussion
Two reviews [38, 54] showed that the pooled cure rate of complete hypertension after unilateral adrenalectomy was 42% and 41%, respectively. However, these reviews only included partial studies comprising at least 50 consecutive patients, and the potential sources of high-level heterogeneity could not be further explored. In addition, the inclusion of such studies can result in ill-defined postoperative hypertension cure criteria. Thus we performed a systematic evaluation of published studies on the hypertension cure rate of unilateral adrenalectomy in PA patients.
Compared to patients with essential hypertension, those with PA have been shown to have more frequent cardiovascular events, including myocardial infarction, stroke, and atrial fibrillation [55, 56]. This higher incidence may be associated with aldosterone-driven excess left ventricular hypertrophy (LVH), myocardial fibrosis and endothelial dysfunction in PA patients [57–59]. Localization of the source of excessive aldosterone secretion is critical in guiding the management of PA. A biochemical cure with normalization of hypokalemia and aldosterone levels is almost certain following adrenalectomy [7], however, not all patients are completely cured of hypertension after adrenalectomy. This suggests that blood pressure alone is probably not a good outcome of interest in PA studies when viewed in isolation. Complete cure of hypertension as a binary benefit/no benefit variable is an oversimplification. Many patients would perceive achieving control of blood pressure and a large reduction in medications as worthwhile. Additional quality of life benefits have been reported, as have very recent metabolic effects.
In PA patients, surgical treatment is associated with quicker resolution of hypertension, shorter length of hospital stay, and decreased cumulative costs compared with lifelong medical therapy [11]. Most PA patients want a definitive prognosis regarding postoperative probability of hypertension cure when they consider surgical intervention. If such a prognosis could be calculated more precisely, surgeons would be able to explain postoperative hypertension outcome to PA patients with more confidence. In our meta-analysis, a total of 43 studies encompassing approximately 4000 PA patients were included. We found a pooled hypertension cure rate of 50.6% (95% CI: 42.9–58.2%) for unilateral adrenalectomy in PA patients. For different subgroups, the hypertension cure rate of unilateral adrenalectomy in PA was within the range of 43.7% to 61.3%. In the country setting, the pooled hypertension cure rate of unilateral adrenalectomy in PA reported by other countries was lower than that reported in China, most likely caused by the different extent in postoperative follow-up. Wachtel [46] demonstrated that the cure rate at long-term follow-up (≥12 months after surgery) was different from that of short-term follow-up (6–12 months after surgery). This may be associated with a slower return to physiologically normal state. Our study confirmed this: the hypertension cure rate of unilateral adrenalectomy for a follow-up time < 6 months was higher than that for patients followed up over a period of ≥6 months. We also found that sample size affected the hypertension cure rate. The cure rate in the number of patients followed being <50 was higher than that for the number of patients ≥50. The difference between the 2 periods (2001–2011 and 2011–2016) could be explained by an analysis of the type of imaging method used for the diagnostic and tree use of catheterism for adrenal vein samplings (AVS).
Given that the hypertension cure rate of unilateral adrenalectomy was not particularly high, it is necessary to preoperatively forecast hypertension outcome of unilateral adrenalectomy in PA patients. In an effort to more appropriately select candidates for surgery, previous studies have suggested a number of potential preoperative predictors for postoperative hypertension cure in PA patients. These include age, gender, BMI, duration of hypertension, family history of hypertension, preoperative number of antihypertensive agents and others. However, several studies have found no association with hypertension cure for each of the aforementioned predictors. Zarnegar et al. [7]. developed the Aldosteronoma Resolution Score (ARS), which was composed of 4 predictors (number of antihypertensive drugs, BMI, duration of hypertension, and gender), to predict hypertension outcome of adrenalectomy in PA patients. Furthermore, Steichen et al. [54] pointed out that the ARS models were the only prediction model validated to date, and provided only a weak prediction of hypertension cure in individual patients. According to the ARS models, even if none of these features was present in an individual patient, the patient still had a 25% probability of being completely cured by adrenalectomy. In this systematic review, due to the inconsistent data pertaining to risk factors and outcome, we could not obtain a pooled odds ratio through logistic regression analysis in our meta-analysis. Consequently, this hindered us from actually developing a new prediction model of hypertension cure rate of unilateral adrenalectomy. In follow-up studies, large-sample clinical trials are still required to verify these potential preoperative predictors and their utility. In doing so, an effective prediction model of hypertension cure rate of unilateral adrenalectomy will be created.
Although this meta-analysis includes more studies and studies with larger sample sizes than individual studies, there were some limitations of this meta-analysis that might affect the outcome. First, the study was limited to articles that were published in English and Chinese. In addition, the unpublished studies that were not included may have caused a potential bias. It is possible that this could have resulted in the exclusion of several articles pertaining to the hypertension cure rate of unilateral adrenalectomy. Secondly, this research does have publication bias. Thirdly, selection bias of PA patients cannot be fully excluded, resulting from the inclusion of the method of diagnosis of unilateral disease. A part of PA patients don’t be performed adrenalectomy for want of a clear diagnosis. For another, cure of hypertension is likely to depend at least in part on what is left in the remaining adrenal. Thus high-precision imaging and AVS should be used to improve diagnostic accuracy. Fourthly, most original studies do not report post-operative aldo-renin ratios and as such, biochemical cure cannot be ascertained. Lastly, extreme heterogeneity was present in this study and although groups were stratified, heterogeneity still persisted.
Conclusions
The hypertension cure rate of unilateral adrenalectomy in PA was assessed by meta-analysis and the results indicate that the hypertension cure rate is not high. We could not obtain a pooled odds ratio through logistic regression analysis by the method of meta-analysis because of inconsistent data pertaining to risk factors and outcome. Given the limitations of the included studies, particularly detection bias, large-sample clinical trials are required to verify the rationale of potential preoperative predictors in developing a new and effective prediction model.
Acknowledgments
None.
Funding
This study did not get any form of funding.
Availability of data and materials
All data and materials are from published papers and are available.
Abbreviations
- ACI
abdominal calcification index
- APA
aldosterone-producing adenoma
- ARS
aldosteronoma resolution score
- AVS
adrenal vein samplings
- BMI
Body mass index
- CNKI
China National Knowledge Internet
- DBP
diastolic blood pressure
- IHA
Idiopathic hyperaldosteronism
- LDL
Low Density Lipoprotein
- LVM
Left Ventricular Mass
- LVMI
Left Ventricular Mass Index
- MOOSE
Meta-analysis Of Observational Studies in Epidemiology
- PA
primary aldosteronism
- PAC
plasma aldosterone concentration
- SBP
systolic blood pressure
Authors’ contributions
YZ and LBL conceived the idea of the review. YZ, MLZ and SJK conducted the review. The initial draft of the manuscript was prepared by YZ and all authors (YZ, MLZ, SJK, and LBL) critically revised article drafts and approved the final version. LBL is the guarantor of this paper.
Ethics approval and consent to participate
This study did not require ethics approval or participant consent given the nature of the work undertaken.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yu Zhou, Email: 510713651@qq.com.
Meilian Zhang, Email: ccfjsczy@163.com.
Sujie Ke, Email: cccfjsczy@163.com.
Libin Liu, Email: Libin.Liu@hotmail.com.
References
- 1.Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, Stowasser M, Young WF., Jr The Management of Primary Aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(5):1889–1916. doi: 10.1210/jc.2015-4061. [DOI] [PubMed] [Google Scholar]
- 2.Hannemann A, Wallaschofski H. Prevalence of primary aldosteronism in patient's cohorts and in population-based studies--a review of the current literature. Horm Metab Res. 2012;44(3):157–162. doi: 10.1055/s-0031-1295438. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz GL, Turner ST. Screening for primary aldosteronism in essential hypertension: diagnostic accuracy of the ratio of plasma aldosterone concentration to plasma renin activity. Clin Chem. 2005;51(2):386–394. doi: 10.1373/clinchem.2004.041780. [DOI] [PubMed] [Google Scholar]
- 4.Hannemann A, Bidlingmaier M, Friedrich N, Manolopoulou J, Spyroglou A, Volzke H, Beuschlein F, Seissler J, Rettig R, Felix SB, et al. Screening for primary aldosteronism in hypertensive subjects: results from two German epidemiological studies. Eur J Endocrinol. 2012;167(1):7–15. doi: 10.1530/EJE-11-1013. [DOI] [PubMed] [Google Scholar]
- 5.Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, Mantero F, Pessina AC. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension. 2013;62(1):62–69. doi: 10.1161/HYPERTENSIONAHA.113.01316. [DOI] [PubMed] [Google Scholar]
- 6.Omura M, Sasano H, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Clinical characteristics of aldosterone-producing microadenoma, macroadenoma, and idiopathic hyperaldosteronism in 93 patients with primary aldosteronism. Hypertens Res. 2006;29(11):883–889. doi: 10.1291/hypres.29.883. [DOI] [PubMed] [Google Scholar]
- 7.Zarnegar R, Young WF, Jr, Lee J, Sweet MP, Kebebew E, Farley DR, Thompson GB, Grant CS, Clark OH, Duh QY. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg. 2008;247(3):511–518. doi: 10.1097/SLA.0b013e318165c075. [DOI] [PubMed] [Google Scholar]
- 8.Wu VC, Chueh SC, Chang HW, Lin LY, Liu KL, Lin YH, Ho YL, Lin WC, Wang SM, Huang KH, et al. Association of kidney function with residual hypertension after treatment of aldosterone-producing adenoma. Am J Kidney Dis. 2009;54(4):665–673. doi: 10.1053/j.ajkd.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 9.Xie LF, Ouyang JZ, Wang AP, Wang WB, Li XT, Wang BJ, Mu YM. Gene expression profile of persistent postoperative hypertension patients with aldosterone-producing adenomas. Chin Med J. 2015;128(12):1618–1626. doi: 10.4103/0366-6999.158318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benham JL, Eldoma M, Khokhar B, Roberts DJ, Rabi DM, Kline GA. Proportion of Patients With Hypertension Resolution Following Adrenalectomy for Primary Aldosteronism: A Systematic Review and Meta-Analysis. J Clin Hypertens (Greenwich) 2016;18(12):1205–1212. doi: 10.1111/jch.12916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sang X, Jiang Y, Wang W, Yan L, Zhao J, Peng Y, Gu W, Chen G, Liu W, Ning G. Prevalence of and risk factors for primary aldosteronism among patients with resistant hypertension in China. J Hypertens. 2013;31(7):1465–1471. doi: 10.1097/HJH.0b013e328360ddf6. [DOI] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed) 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horita Y, Inenaga T, Nakahama H, Ishibashi-Ueda H, Kawano Y, Nakamura S, Horio T, Okuda N, Ando M, Takishita S. Cause of residual hypertension after adrenalectomy in patients with primary aldosteronism. Am J Kidney Dis. 2001;37(5):884–889. doi: 10.1016/S0272-6386(05)80002-2. [DOI] [PubMed] [Google Scholar]
- 16.Sawka AM, Young WF, Thompson GB, Grant CS, Farley DR, Leibson C, van Heerden JA. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001;135(4):258–261. doi: 10.7326/0003-4819-135-4-200108210-00010. [DOI] [PubMed] [Google Scholar]
- 17.Fukudome Y, Fujii K, Arima H, Ohya Y, Tsuchihashi T, Abe I, Fujishima M. Discriminating factors for recurrent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res. 2002;25(1):11–18. doi: 10.1291/hypres.25.11. [DOI] [PubMed] [Google Scholar]
- 18.Rossi H, Kim A, Prinz RA. Primary hyperaldosteronism in the era of laparoscopic adrenalectomy. Am Surg. 2002;68(3):253–256. [PubMed] [Google Scholar]
- 19.Tan YW, Liu NB, Luo J, Jiang YJ, M Z. Diagnosis and treatment of primary aldosteronism (report of 46 cases) J China-Japan Friendship Hospital. 2002;16(3):149–151. [Google Scholar]
- 20.Goh BK, Tan YH, Yip SK, Eng PH, Cheng CW. Outcome of patients undergoing laparoscopic adrenalectomy for primary hyperaldosteronism. JSLS. 2004;8(4):320–325. [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer A, Brabant G, Behrend M. Long-term follow-up after adrenalectomy for primary aldosteronism. World J Surg. 2005;29(2):155–159. doi: 10.1007/s00268-004-7496-z. [DOI] [PubMed] [Google Scholar]
- 22.Han QH, Wei JX, Zhang XP, Zhang WX, Wang ZY, Wu YD, JG G. Transperitoneal laparoscopic procedure for primary aldosteronism:report of 47 cases. Clinical Medicine. 2006;26(4):3–4. [Google Scholar]
- 23.Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, Sywak MS. Outcomes of laparoscopic adrenalectomy for hyperladosteronism. ANZ J Surg. 2007;77(9):768–773. doi: 10.1111/j.1445-2197.2007.04225.x. [DOI] [PubMed] [Google Scholar]
- 24.Ziaja J, Chudek J, Krol R, Pawlicki J, Wiecek A, Cierpka L. Rare normalization of blood pressure after unilateral adrenalectomy in 31 patients with conn syndrome. Langenbecks Arch Surg. 2007;392(4):431–435. doi: 10.1007/s00423-006-0121-x. [DOI] [PubMed] [Google Scholar]
- 25.Walz MK, Gwosdz R, Levin SL, Alesina PF, Suttorp AC, Metz KA, Wenger FA, Petersenn S, Mann K, Schmid KW. Retroperitoneoscopic adrenalectomy in Conn's syndrome caused by adrenal adenomas or nodular hyperplasia. World J Surg. 2008;32(5):847–853. doi: 10.1007/s00268-008-9513-0. [DOI] [PubMed] [Google Scholar]
- 26.White ML, Gauger PG, Doherty GM, Cho KJ, Thompson NW, Hammer GD, Miller BS. The role of radiologic studies in the evaluation and management of primary hyperaldosteronism. Surgery. 2008;144(6):926–933. doi: 10.1016/j.surg.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Mourad JJ, Girerd X, Milliez P, Lopez-Sublet M, Lejeune S, Safar ME. Urinary aldosterone-to-active-renin ratio: a useful tool for predicting resolution of hypertension after adrenalectomy in patients with aldosterone-producing adenomas. Am J Hypertens. 2008;21(7):742–747. doi: 10.1038/ajh.2008.175. [DOI] [PubMed] [Google Scholar]
- 28.Chiou TT, Chiang PH, Fuh M, Liu RT, Lee WC, Lee WC, Ng HY, Tsai YC, Chuang FR, Huang CC, et al. Factors determining cardiovascular and renal outcomes after adrenalectomy in patients with aldosterone-producing adrenal adenoma. Tohoku J Exp Med. 2009;218(1):17–24. doi: 10.1620/tjem.218.17. [DOI] [PubMed] [Google Scholar]
- 29.Campagnacci R, Crosta F, De Sanctis A, Baldarelli M, Giacchetti G, Paganini AM, Coletta M, Guerrieri M. Long-term results of laparoscopic adrenalectomy for primary aldosteronism. J Endocrinol Investig. 2009;32(1):57–62. doi: 10.1007/BF03345680. [DOI] [PubMed] [Google Scholar]
- 30.Wang B, Zhang G, Ouyang J, Deng X, Shi T, Ma X, Li H, Ju Z, Wang C, Wu Z, et al. Association of DNA polymorphisms within the CYP11B2/CYP11B1 locus and postoperative hypertension risk in the patients with aldosterone-producing adenomas. Urology. 2010;76(4):1018. doi: 10.1016/j.urology.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 31.Tresallet C, Salepcioglu H, Godiris-Petit G, Hoang C, Girerd X, Menegaux F. Clinical outcome after laparoscopic adrenalectomy for primary hyperaldosteronism: the role of pathology. Surgery. 2010;148(1):129–134. doi: 10.1016/j.surg.2009.11.020. [DOI] [PubMed] [Google Scholar]
- 32.Mathur A, Kemp CD, Dutta U, Baid S, Ayala A, Chang RE, Steinberg SM, Papademetriou V, Lange E, Libutti SK, et al. Consequences of adrenal venous sampling in primary hyperaldosteronism and predictors of unilateral adrenal disease. J Am Coll Surg. 2010;211(3):384–390. doi: 10.1016/j.jamcollsurg.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim RM, Lee J, Soh EY. Predictors of resolution of hypertension after adrenalectomy in patients with aldosterone-producing adenoma. J Korean Med Sci. 2010;25(7):1041–1044. doi: 10.3346/jkms.2010.25.7.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu B, Zhang X, Wang GX, Lang B, Ma X, Li HZ, Wang BJ, Shi TP, Ai X, Zhou HX, et al. Long-term results of a prospective, randomized trial comparing retroperitoneoscopic partial versus total adrenalectomy for aldosterone producing adenoma. J Urol. 2011;185(5):1578–1582. doi: 10.1016/j.juro.2010.12.051. [DOI] [PubMed] [Google Scholar]
- 35.Waldmann J, Maurer L, Holler J, Kann PH, Ramaswamy A, Bartsch DK, Langer P. Outcome of surgery for primary hyperaldosteronism. World J Surg. 2011;35(11):2422–2427. doi: 10.1007/s00268-011-1221-5. [DOI] [PubMed] [Google Scholar]
- 36.Tang KL, Lin Y, Lm L. Laparoscopic management of primary aldosteronism: a report of 227 cases. Chin J Endocr Surg. 2011;5(2):117–119. [Google Scholar]
- 37.Wang ZS, Wang CY, H H. Clinical analysis of 32 cases with primary aldosteronism. HAINAN MEDICAL JOURNAL. 2011;22(4):9–11. [Google Scholar]
- 38.Van Der Linden P, Steichen O, Zinzindohoué F, Plouin PF. Blood pressure and medication changes following adrenalectomy for unilateral primary aldosteronism: a follow-up study. J Hypertens. 2012;30(4):761–769. doi: 10.1097/HJH.0b013e328350225d. [DOI] [PubMed] [Google Scholar]
- 39.Wang W, Hu WL, Zhang LC, Xiao YS, Liu J, Bin C. Polymorphic variation of CYP11B2 predicts postoperative resolution of hypertension in patients undergoing adrenalectomy for aldosterone-producing adenomas. Int J Urol. 2012;19(9):813–820. doi: 10.1111/j.1442-2042.2012.03048.x. [DOI] [PubMed] [Google Scholar]
- 40.L W. The laparoscopic surgical treatment of primary aldosteronism. Chin J Endocr Surg. 2012;6(4):260–264. [Google Scholar]
- 41.Wang YG, Wang Q, Qi FB, Ya LK, Liu L, Shi ZF, M S. Clinical diagnosis and analysis of primary aldosteronism: a report of 83 cases. Journal of Chinese Physician. 2012;14(10):1417–1419. [Google Scholar]
- 42.Zhang X, Zhu Z, Xu T, Shen Z. Factors affecting complete hypertension cure after adrenalectomy for aldosterone-producing adenoma: outcomes in a large series. Urol Int. 2013;90(4):430–434. doi: 10.1159/000347028. [DOI] [PubMed] [Google Scholar]
- 43.Aronova A, Gordon BL, Finnerty BM, Zarnegar R, Fahey TJ., 3rd Aldosteronoma resolution score predicts long-term resolution of hypertension. Surgery. 2014;156(6):1387–1392. doi: 10.1016/j.surg.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 44.Jiang SB, Guo XD, Wang HB, Gong RZ, Xiong H, Wang Z, Zhang HY, Jin XB. A retrospective study of laparoscopic unilateral adrenalectomy for primary hyperaldosteronism caused by unilateral adrenal hyperplasia. Int Urol Nephrol. 2014;46(7):1283–1288. doi: 10.1007/s11255-013-0614-9. [DOI] [PubMed] [Google Scholar]
- 45.Lim V, Guo Q, Grant CS, Thompson GB, Richards ML, Farley DR, Young WF., Jr Accuracy of adrenal imaging and adrenal venous sampling in predicting surgical cure of primary aldosteronism. J Clin Endocrinol Metab. 2014;99(8):2712–2719. doi: 10.1210/jc.2013-4146. [DOI] [PubMed] [Google Scholar]
- 46.Wachtel H, Cerullo I, Bartlett EK, Kelz RR, Cohen DL, Karakousis GC, Roses RE, Fraker DL. Long-term blood pressure control in patients undergoing adrenalectomy for primary hyperaldosteronism. Surgery. 2014;156(6):1394–1402. doi: 10.1016/j.surg.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 47.Hartmann I, Grepl M, Vidlar A, Smakal O, Vaclavik J, Frysak Z, Dolezel M, Student V. Outcomes of adrenalectomy in patients with primary hyperaldosteronism--a single centre experience. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(4):583–590. doi: 10.5507/bp.2014.059. [DOI] [PubMed] [Google Scholar]
- 48.Utsumi T, Kamiya N, Endo T, Yano M, Kamijima S, Kawamura K, Imamoto T, Naya Y, Ichikawa T, Suzuki H. Development of a novel nomogram to predict hypertension cure after laparoscopic adrenalectomy in patients with primary aldosteronism. World J Surg. 2014;38(10):2640–2644. doi: 10.1007/s00268-014-2612-1. [DOI] [PubMed] [Google Scholar]
- 49.Wolley MJ, Gordon RD, Ahmed AH, Stowasser M. Does contralateral suppression at adrenal venous sampling predict outcome following unilateral adrenalectomy for primary aldosteronism? A retrospective study. J Clin Endocrinol Metab. 2015;100(4):1477–1484. doi: 10.1210/jc.2014-3676. [DOI] [PubMed] [Google Scholar]
- 50.Hu YH, Wu CH, Er LK, Lin CD, Liu YB, Chueh SC, Tsai YC. Laparoendoscopic single-site adrenalectomy in patients with primary hyperaldosteronism: a prospective study with long-term follow up. Asian J Surg. 2015; [DOI] [PubMed]
- 51.Citton M, Viel G, Rossi GP, Mantero F, Nitti D, Iacobone M. Outcome of surgical treatment of primary aldosteronism. Langenbecks Arch Surg. 2015;400(3):325–331. doi: 10.1007/s00423-014-1269-4. [DOI] [PubMed] [Google Scholar]
- 52.Volpe C, Hamberger B, Höög A, Mukai K, Calissendorff J, Wahrenberg H, Zedenius J, Thorén M. Primary aldosteronism: functional histopathology and long-term follow-up after unilateral adrenalectomy. Clin Endocrinol. 2015;82(5):639–647. doi: 10.1111/cen.12645. [DOI] [PubMed] [Google Scholar]
- 53.Fujita N, Hatakeyama S, Yamamoto H, Imai A, Yoneyama T, Hashimoto Y, Koie T, Ohyama C: The implication of aortic calcification on persistent hypertension after laparoscopic adrenalectomy in patients with primary aldosteronism. European Urology, Supplements 2016, 15(3):e486. [DOI] [PubMed]
- 54.Steichen O, Zinzindohoue F, Plouin PF, Amar L. Outcomes of adrenalectomy in patients with unilateral primary aldosteronism: a review. Horm Metab Res. 2012;44(3):221–227. doi: 10.1055/s-0031-1299681. [DOI] [PubMed] [Google Scholar]
- 55.Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, Sechi LA. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008;168(1):80–85. doi: 10.1001/archinternmed.2007.33. [DOI] [PubMed] [Google Scholar]
- 56.Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45(8):1243–1248. doi: 10.1016/j.jacc.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 57.Muiesan ML, Salvetti M, Paini A, Agabiti-Rosei C, Monteduro C, Galbassini G, Belotti E, Aggiusti C, Rizzoni D, Castellano M, et al. Inappropriate left ventricular mass in patients with primary aldosteronism. Hypertension. 2008;52(3):529–534. doi: 10.1161/HYPERTENSIONAHA.108.114140. [DOI] [PubMed] [Google Scholar]
- 58.Liu G, Yin GS, Tang JY, Ma DJ, Ru J, Huang XH. Endothelial dysfunction in patients with primary aldosteronism: a biomarker of target organ damage. J Hum Hypertens. 2014;28(12):711–715. doi: 10.1038/jhh.2014.11. [DOI] [PubMed] [Google Scholar]
- 59.Lee HH, Hung CS, Wu XM, Wu VC, Liu KL, Wang SM, Lin LC, Chen PC, Guo YL, Chueh SC, et al. Myocardial ultrasound tissue characterization of patients with primary aldosteronism. Ultrasound Med Biol. 2013;39(1):54–61. doi: 10.1016/j.ultrasmedbio.2012.08.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials are from published papers and are available.


