Breast cancer mortality rates in low‐ and middle‐income countries are higher than in the developed world. Programs aimed at enhancing education and awareness of breast cancer are a critical strategy to overcoming barriers to timely diagnosis in these countries. This article reports a program designed to educate adolescents on breast cancer with the end goal of promoting intergenerational transmission of breast cancer‐related knowledge to their older female relatives.
Keywords: Intergenerational relations, Breast cancer, Health education, Rural health, Adolescents
Abstract
Background.
Rural women have limited access to breast cancer education, which partially contributes to late diagnosis and treatment. In this pilot study, we tested the feasibility of implementing a school‐based breast cancer educational program for adolescents in a rural Mexican community. We hypothesized that the adolescents’ knowledge on breast cancer would increase as a result of the program, and that there would be intergenerational transmission of that knowledge to their older female relatives.
Materials and Methods.
Female adolescents from a rural middle school received the educational program. The program would be considered feasible and acceptable if more than 75% reported being satisfied with its contents. Changes in knowledge in the students and their relatives were evaluated using baseline and 4 months follow‐up questionnaires.
Results.
One hundred twenty‐six students were enrolled. The program was considered acceptable by 96% of the participants. The students’ knowledge regarding breast cancer increased significantly from baseline to 4 months follow‐up (63% to 82%). One hundred ninety‐four female relatives completed the initial knowledge questionnaires. The relatives’ knowledge regarding breast cancer showed a significant increase from baseline to 4 months follow‐up (55% to 61%).
Conclusion.
Implementing breast cancer educational programs for adolescents in rural communities is feasible and acceptable. The program increased the adolescents’ knowledge on breast cancer, and promoted the intergenerational transmission of that knowledge to their female relatives. Intergenerational transmission of knowledge represents a potential method for providing population‐based health awareness education globally.
Implications for Practice.
In limited‐resource settings, education is a valuable tool for achieving early detection and downstaging of breast cancer. Unfortunately, rural women lack access to educational opportunities and information about breast cancer, which is a factor contributing to late diagnosis and treatment. In this study, we demonstrated that implementing a school‐based breast cancer educational program for female adolescents in a rural Mexican community was feasible, acceptable, and increased their knowledge about breast cancer. Furthermore, the program encouraged the transmission of information to the students’ older relatives. Intergenerational transmission of knowledge represents a novel and potentially effective tool in cancer education and promotion.
Introduction
Breast cancer mortality rates in low‐ and middle‐income countries (LMIC) are higher than in the developed world, which is in part driven by the higher incidence of advanced disease at presentation and limited access to health care [1]. In Mexico, up to 56% of women with breast cancer present with locally advanced or metastatic disease, leading to a high incidence‐to‐mortality ratio [2]. Social, cultural, and economic barriers like poverty, poor awareness, and deficient screening programs can all lead to late diagnosis [3], [4], [5], [6]. In LMIC, programs aimed at enhancing education and awareness of breast cancer represent critical strategies to overcome barriers to timely diagnosis and to achieve downstaging of the disease [7], [8]. This is particularly relevant for women living in rural communities with less access to health care and education. For instance, studies have shown that while most urban Mexican women have basic knowledge of breast cancer, less than 25% of women living in rural areas possess knowledge about breast health [9], [10]. Unfortunately, due to marginalization and poverty, rural women lack educational opportunities to increase their knowledge [10], [11]. In Mexico, 25% of rural women are solely responsible for their household income, and only 12% of those older than 15 years participate in educational activities [12]. Surveys in rural areas have identified this lack of education regarding breast health as one of the main barriers to the timely diagnosis of breast cancer [6].
School‐based educational interventions have proven effective in raising cancer awareness among adolescents in developed [13], [14] and developing [15] nations. Because 60% of rural women in Mexico work at home [12], they are in constant interaction with their children, who could potentially act as educators within the household. Studies have demonstrated that children can influence their parents’ actions by providing information or by attempting to change their behaviors [16], [17]. Although adolescents exposed to educational interventions are more likely to talk about cancer [14], using intergenerational “reverse” transmission of cancer‐related information to increase adults’ knowledge has not been explored.
In this study, we assessed the feasibility and acceptability of implementing a school‐based breast cancer educational program for female adolescents in a rural Mexican community. Furthermore, we hypothesized that the program would increase the adolescents’ knowledge on breast cancer, and that it would promote the intergenerational transmission of breast‐cancer related knowledge to female relatives in their household.
Materials and Methods
This was a pilot study that evaluated the feasibility of a breast cancer educational program for adolescents attending middle school in a rural Mexican community. The effect of the program on the adolescents’ knowledge on breast cancer, and the intergenerational transmission of that knowledge to their female relatives, was also explored. This manuscript follows the recommendations for reporting the results of pilot studies developed by Thabane et al. [18]. The study received research ethics approval from the Ethics Committee at Salvador Zubiran National Institute of Medical Science and Nutrition. The educational program was first presented to the Health Education Department of the Ministry of Public Education of the State of Puebla, in central Mexico, which approved its contents. The Ministry provided a list of middle schools that fitted the study's requirements, of which one was selected at random. Local school authorities and teachers were contacted through the Ministry and approved the program before its implementation.
Participants and Settings
Eligible participants were female adolescent students enrolled in grades 1–3 of secondary education in a public middle school (Escuela Secundaria Técnica Number 47) in the municipality of Santiago Miahuatlán. Santiago Miahuatlán is located in the state of Puebla, in central Mexico, and has 21,933 inhabitants (11,398 women) [19]. The town's main economic activity is agriculture, and its inhabitants have an average of 6.5 years of schooling [19], [20]. Male students were not invited to participate in the educational program in order to follow local social norms and customs.
Interventions
The research team attended the school during a regular school day and, with the teachers’ authorization, invited students to participate in the educational program in the classroom. Those students who were willing to participate provided written assent and answered a breast cancer knowledge questionnaire. The questionnaire was adapted from an English‐language questionnaire, which was translated, back‐translated, and linguistically validated by an expert panel (supplemental online Appendix 1) [21]. The students were then handed an informed consent form for their parents to sign, along with questionnaires on breast cancer for female relatives living in their household. The questionnaire included the same questions asked to the students, plus two additional questions on screening habits (supplemental online Appendix 1). The students were instructed to return the parental informed consent form and the questionnaires to the study team on the following morning. Only students who provided assent and signed parental informed consent were able to attend the educational program, which took place on school grounds on a non‐school day 1 week later. No incentives were offered to the students or their families in exchange for participation, but small gifts (pens, water bottles, children's books) and lunch were given to the students on the day of the intervention.
The educational program consisted of five 40‐minute sessions (Table 1) and was based on the “Breast Health Education for Young Women” program developed by the Prevent Cancer Foundation and the Howard University Cancer Center [21]. The sessions were the following: (a) breast cancer information, facts, and misconceptions (including an ice breaker activity in which the students had the opportunity to share personal stories about cancer; supplemental online Appendix 2); (b) a breast cancer survivor's story; (c) breast self‐examination (guided by the children's story book Mom's Brassiere by Edmée Pardo [22]); (d) critical thinking collage; and (e) role‐playing activity. The sessions were adapted by pedagogists and a psychologist (MP) in order to be culturally sensitive and age‐appropriate. All activities emphasized the importance of transmitting the obtained knowledge in their household. Students were divided into four groups of 25 to 30 students each, and activities took place simultaneously in different classrooms. The team that coordinated the sessions was composed of pedagogy students, a breast cancer survivor who coauthored the children's book (RG), medical students, and oncologists (ES, YC). All the sessions (except the breast cancer survivor's story) were led by pedagogy and medical students, with supervision from the two oncologists, who coordinated the program and were available to answer questions. School teachers attended the sessions alongside the students. At the end of the activities, the students answered a questionnaire assessing their satisfaction with the program (supplemental online Appendix 1). Additionally, they answered the same knowledge questionnaire as they had prior to the program. The school teachers who attended the program answered open‐ended questionnaires rating its appropriateness.
Table 1. Educational program outline.
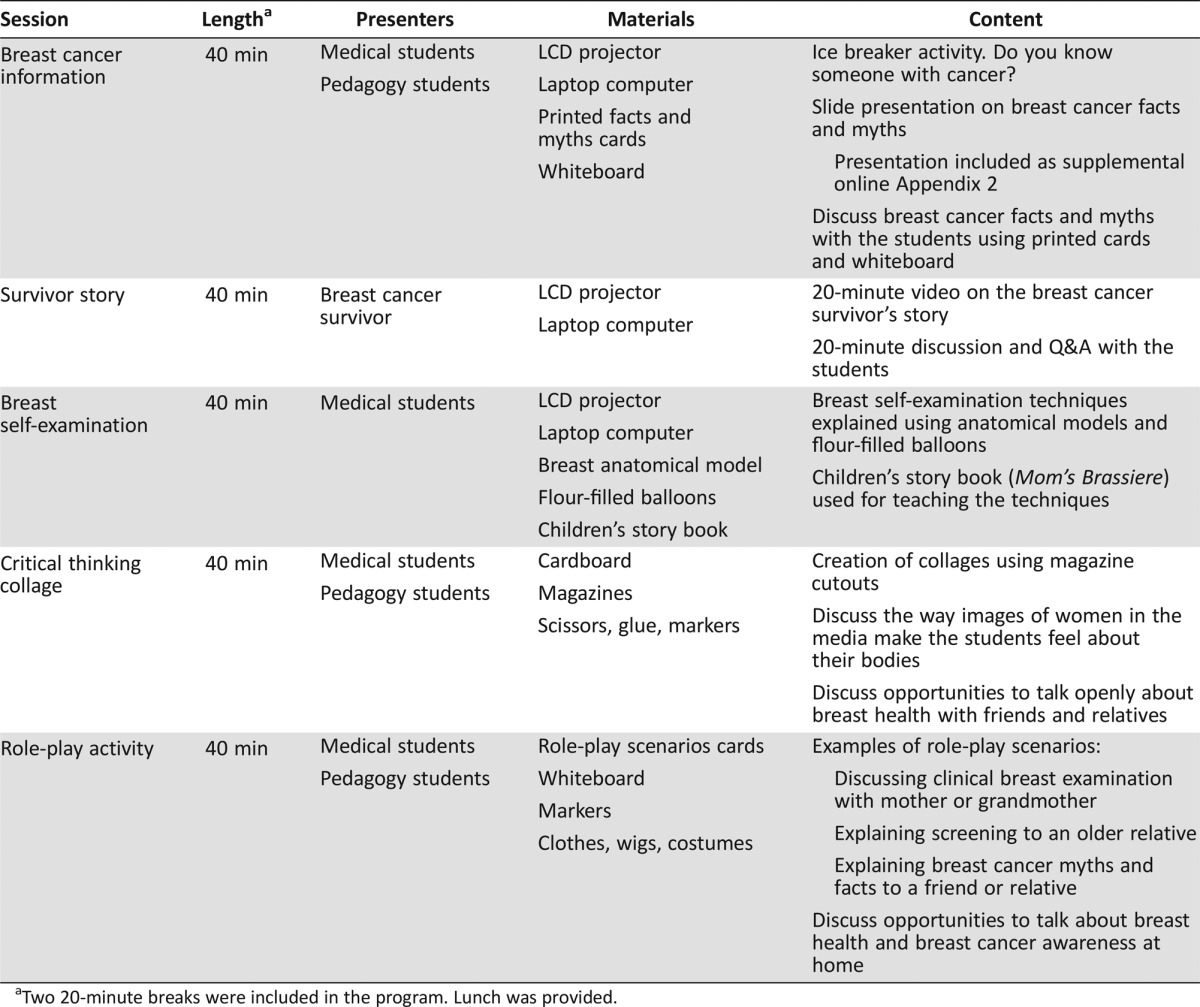
Two 20‐minute breaks were included in the program. Lunch was provided.
Four months after the program was implemented, the research team returned to the school to administer the same knowledge questionnaire to participating students. Students who did not attend school on the day the questionnaire was administered were considered lost to follow‐up. Additionally, knowledge questionnaires were once again handed to the students in a sealed envelope for the same female relatives living in their household to complete. The students were instructed to return the answered questionnaires to the study team the following morning.
Objectives, Outcomes, and Feasibility Criteria
As a primary objective, we assessed the educational program's feasibility by measuring its acceptability, appropriateness, and possibility for integration into middle school curricula. Acceptability was defined as the students’ satisfaction with the program, and was assessed using a Likert‐scale questionnaire (supplemental online Appendix 1) [21]. The program would be considered acceptable if at least 75% of the participants rated the activities as somewhat or very interesting, and the knowledge obtained as “some” or “a lot.” As secondary objectives, we assessed changes in knowledge on breast cancer following the program among the participants, and the intergenerational transmission of that knowledge to their female relatives. We measured changes in the students’ knowledge between before the educational program (T0), immediately after the educational program (T1), and 4 months after the educational program (T2). We expected that the students would show a relative increase of 30% in knowledge between T0 and T2. Changes in the relatives’ knowledge (intergenerational transmission) were measured from before the educational program (T0) to 4 months after the educational program (T2). The students’ willingness to communicate the information was measured using open‐ended questions. The appropriateness and the possibility for integration of the program into the curricula were evaluated using open‐ended questionnaires given to the school teachers immediately after the educational program ended.
Statistical Analysis and Sample Size
Confidence intervals (CI) of proportions were used to assess feasibility. Using a 95% CI and a margin of error of 0.1, we calculated that a sample size of at least 76 students who completed the program was necessary to establish feasibility. Our analysis included quantitative tabulation and qualitative review of the results.
We used paired Student's t test to assess changes in the students’ knowledge. We calculated that at least 90 students who completed T2 questionnaires were needed in order to detect a 30% relative change in knowledge from T0 to T2 with a two‐sided α of 0.05 and a power of 80%. The same methods and assumptions were used to assess changes in the relatives’ knowledge. In order to assess the correlation between the students’ and their relatives’ knowledge, we used Pearson's correlation coefficient. A p value of <.05 was considered as statistically significant.
Assuming a dropout rate of 20% between T0 and T2, we calculated that enrolling at least 115 female students and relatives was necessary to assess both feasibility and changes in knowledge.
Results
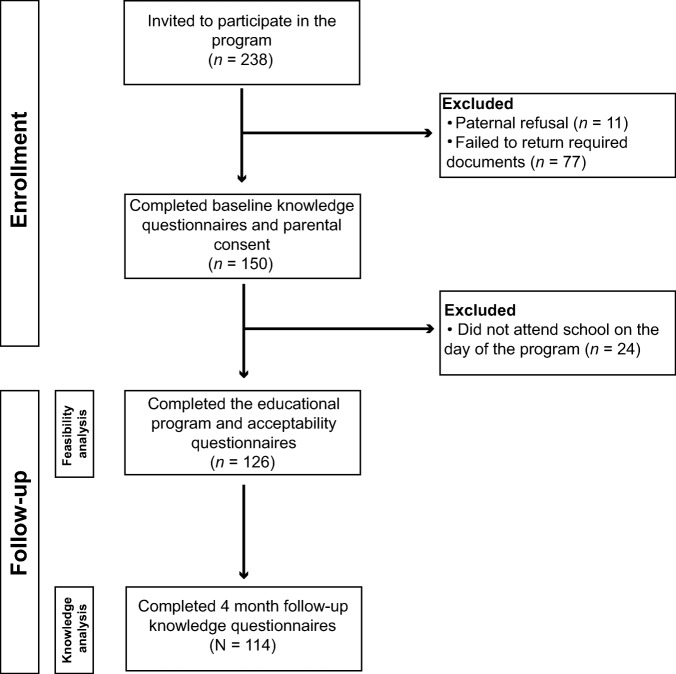
Two hundred thirty‐eight female students were invited to participate in the educational program, of which 150 (63%) provided both assent and parental consent. One hundred twenty‐six students provided baseline (T0) knowledge questionnaires, attended the program and answered the acceptability questionnaire. Ninety percent of the students (n = 114) answered the 4 month follow‐up questionnaire (T2; Fig. 1).
Figure 1.
Participant flow diagram.
The educational program took place in February 2015, and follow‐up questionnaires were administered in July 2015. The students’ median age was 13.5 years (range 12–16). Forty‐eight (38%) students were enrolled in first grade, 33 (26%) in second grade, 37 (29%) in third grade, and 8 (6%) did not provide their school grade. The median number of female relatives living in the same household as the student was three (range 1–8); 57 students (45%) said they knew of somebody with breast cancer; and 10 (7.9%) said they had a relative with breast cancer.
Eighteen teachers (72% women) with a median of 9.5 years of teaching experience attended the educational program and completed the open‐ended questionnaires.
One hundred ninety‐four female relatives (median age 36.6 years [range 11–90]) completed the baseline knowledge test (T0). Out of the 149 respondents who wrote down their relationship with the students, 79 (53%) were mothers, 24 (16%) were sisters, 20 (13%) were aunts, and 11 (7%) were grandmothers. One hundred eighty‐two female relatives answered the 4 month follow‐up knowledge questionnaire (T2).
Feasibility and Acceptability
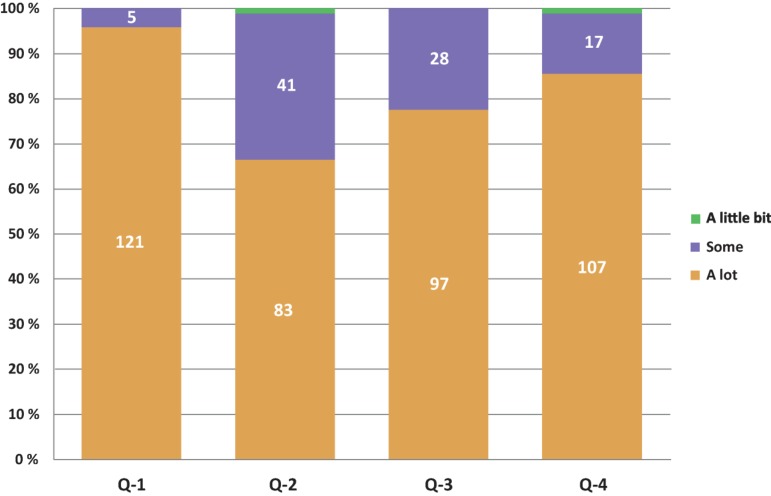
Out of the 126 students who completed the acceptability questionnaire, 121 (96%; 95% CI ±3.4) met our predefined acceptability criteria. Ninety‐six percent (n = 121) considered the program to be very interesting; 85.6% (n = 107) thought the presenters had “a lot” of knowledge about the topics, and 77.6% (n = 97) thought the information was very clearly presented. Sixty‐six percent (n = 83) thought they learned “a lot,” while 32.8% (n = 41) thought they learned “something” (Fig. 2). Eighteen teachers participated in the program, of which 72% (n = 13) were female. Their median duration of teaching experience was 9.5 years. All the teachers who attended the intervention rated it as culturally acceptable and appropriate for inclusion in middle school curricula. Eighty‐three percent (n = 15) of the teachers thought the activity would encourage the students to talk about breast cancer at home. For future interventions, the teachers recommended focusing on third grade students, creating a breast cancer educational program for males, and implementing the program biannually. All the teachers expressed interest in receiving training in order to implement the program.
Figure 2.
Acceptability questionnaire results. Each bar corresponds to a question. Q‐1: The activity was interesting. Q‐2: The activity helped you learn new things. Q‐3: The information was clearly presented. Q‐4: The presenters knew the topics (n = 126).
Students’ Knowledge
The students’ baseline (T0) mean proportion of correct answers was 63% (range 12.5%–100%). Immediately after the program (T1), the mean proportion of correct answers increased to 89% (range 25%–100%), showing a relative increase in knowledge of 41% (p < .001). At 4 months follow‐up (T2), the students’ mean proportion of correct answers was 82% (range 37.5%–100%), showing a relative increase in knowledge of 30% when compared with basal knowledge at T0 (p < .001). A statistically significant increase in knowledge was found for six out of the eight questions in the questionnaire (Table 2).
Table 2. Students’ test results.
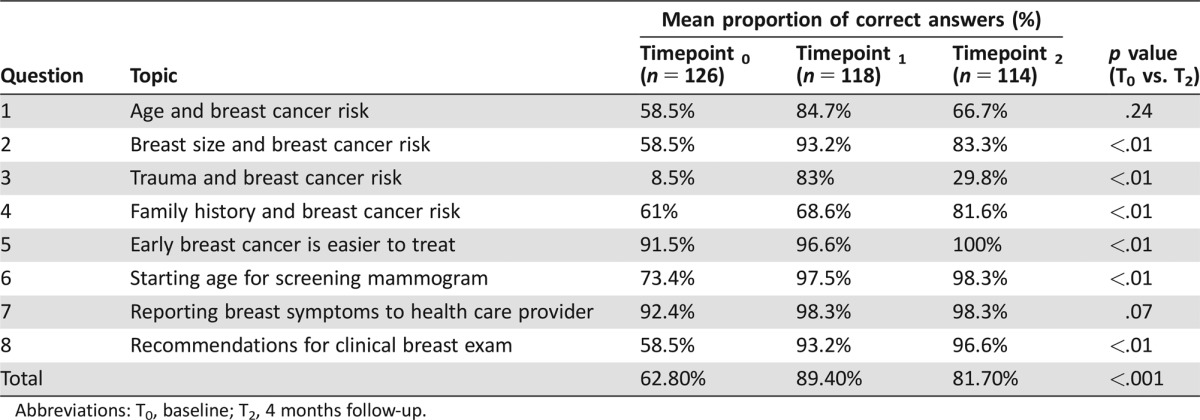
Abbreviations: T0, baseline; T2, 4 months follow‐up.
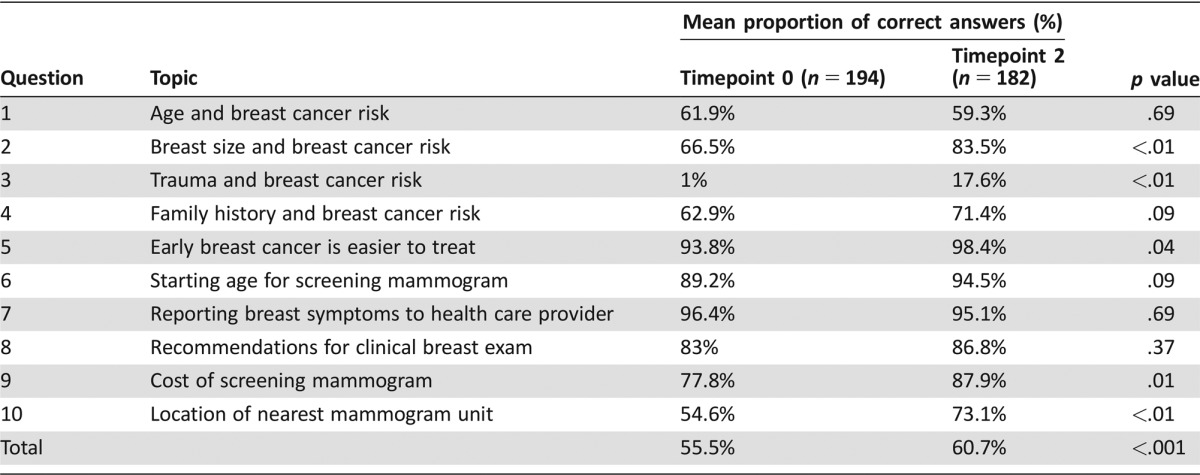
Female Relatives’ Knowledge
The relatives’ baseline (T0) mean proportion of correct answers was 55.5% (range 10%–80%). At 4 months follow‐up (T2), the relatives’ mean proportion of correct answers increased to 60.7% (range 30%–80%), showing a relative increase in knowledge of 9.3% when compared with basal knowledge at T0 (p < .001). A statistically significant increase in knowledge was found for 5 out of the 10 questions in the questionnaire (Table 3). The proportion of relatives who knew where to get a mammogram increased from 55% to 73% (p = .01), and the proportion who knew that mammograms are free in Mexico increased from 78% to 88% (p < .01).
Table 3. Relatives’ test results.
At baseline (T0), a correlation was found between the students’ and the relatives’ proportion of correct answers (r = 0.91, p < .01). At 4 months follow‐up (T2) this correlation remained significant (r = 0.99, p < .001; Fig. 3). Of note, the proportion of students who reported feeling comfortable talking about breast cancer at home increased from 71% at baseline (T0) to 90% at 4 months follow‐up (T2; p < .001).
Figure 3.
Correlation in the proportion of correct answers per question between the students and their relatives at baseline (A) and at 4 months follow‐up (B).
Abbreviation: Q, question.
Discussion
Implementing a school‐based breast cancer educational program for female adolescents in a rural Mexican middle school was feasible and acceptable. The students and the teachers who attended the program rated it favorably, and the predefined threshold for “acceptability” was met. The educational program significantly increased knowledge regarding breast cancer among the students, and this knowledge was retained at 4 months follow‐up. Furthermore, an increase in the students’ female relatives’ knowledge on breast cancer was demonstrated 4 months after initiation of the program. This finding, coupled with a rise in the number of students who felt comfortable talking about breast cancer at home, points towards intergenerational transmission of knowledge from the students to their female relatives.
In countries with limited resources, breast health educational interventions should aim at downstaging breast cancer by teaching women the importance of seeking timely evaluation of symptoms, and by emphasizing that survival is improved when breast cancer is detected early [8]. However, failure to assess the feasibility and acceptability of educational interventions may severely hamper their implementation and success [23]. Educational programs need to be culturally and socially appropriate, and must specifically address the unique barriers of a population that influence participation in cancer screening. Additionally, interventions should be designed to be efficiently implemented by local community health workers and breast cancer survivors [8]. We assembled a team of pedagogists and psychologists specialized in health education, as well as local educational authorities and teachers, who developed a culturally sensitive and age‐appropriate program. Implementing the program required only basic cancer knowledge, and it was coordinated by medical students, educators, and a survivor, with supervision from two oncologists. Furthermore, by obtaining feedback from relevant stakeholders, we were able to demonstrate that discussing a potentially controversial topic like breast cancer with adolescents is appropriate in a rural community.
Our results are potentially generalizable to other settings in Mexico and Latin America. The chosen site, Santiago Miahuatlán, is representative of rural townships in Mexico, with agriculture as the main economic activity and an average schooling of 6.5 years [19], [20]. Furthermore, 96% of Mexicans receive a middle school education [24], which makes middle school students the ideal target population for achieving the largest possible impact of the program. Although it could be argued that high school students could be a potentially better target, only 63% of Mexicans start high school [24]. This situation mirrors that of the rest of LMIC, where the middle school enrollment, albeit low (37% completion rates in low‐income countries), surpasses that of high school [25].
Our findings provide insight for health educators to address the unmet breast health education needs of women in LMIC. Our basal results showed that knowledge on breast cancer was low for both the students and their relatives, which is potentially related to limited educational opportunities and a lack of information about women's health issues [6]. Of note, breast health and breast cancer prevention are not included among the health issues addressed in the current educational program for public secondary education in Mexico [26]. Therefore, Mexican women obtain most of their information on breast cancer from public awareness campaigns, which have highly variable quality [27]. The significant increase in knowledge we found among the students after the program is consistent with that reported previously in other studies from LMIC, showing that educating adolescents is an effective intervention to raise cancer awareness and knowledge [14], [28].
When defining a target population for breast cancer educational programs, the priority should be to reach those subsets at higher risk [23]. In Mexico, the highest breast cancer incidence is seen in women aged 60–64, followed by those aged 50–59 and those aged 45–49, so the ideal educational intervention should primarily target those age groups [29]. However, rural women have very low access to educational forums in which to obtain new knowledge [12]. In this study, we explored whether breast cancer knowledge could be transmitted in an intergenerational fashion from the adolescents to their female relatives, thus amplifying the program's effect and increasing awareness among a population at higher risk. Children and adolescents influence and modify adult behaviors both directly and indirectly. Studies in environmental education have shown that information delivered to children can be successfully transferred between generations and induce behavioral changes in parents [30], [31]. Social studies have also suggested that children influence their parents’ values and attitudes, including how they allocate their budget and investments [17], [32]. Although companies and manufacturers have long recognized the benefits of marketing to children and adolescents, the potential of intergenerational influences has not been thoroughly explored in health care [33]. Our findings support the presence of intergenerational transmission of knowledge about breast cancer from the students to their female relatives. First, there was an improvement in the relatives’ knowledge 4 months after the intervention, which was not as large as the students’ but nevertheless significant. Interestingly, there was a significant increase in knowledge about where to get a mammogram, which was one of the topics addressed by the program (a map showing the nearest mammography unit was provided to the students). Additionally, we found significant correlation between the students’ and relatives’ correct answers. Finally, the students reported that they felt more comfortable talking about breast cancer at home after attending the program. This observed increase in breast cancer knowledge among the students’ female relatives is relevant because they were more likely to be in a target age group for breast cancer screening. Thus, implementing intergenerational educational programs could have both long‐term impact (by providing adolescents with knowledge on breast cancer prevention) and short‐term benefits (by encouraging the detection of symptomatic and asymptomatic disease among their older relatives) on breast cancer control.
This study has limitations. Participation in the program required a high level of commitment, so it's possible that only highly motivated students attended, creating a selection bias. Including the program as a regular school activity could potentially solve this problem. The program was implemented by our team, and not by community workers, which would be ideal. Nevertheless, pedagogy and medical students with basic breast cancer knowledge directed the activities, and we believe that training local teachers, community health care workers, and survivors to implement the program would certainly be feasible and effective. Furthermore, for this feasibility study we only included female students in order to reduce the number of confounding factors. However, we acknowledge that including males is very relevant, and we intend to develop a male‐specific program for future studies. Finally, while we supervised the students when answering knowledge questionnaires, we did not supervise their relatives. Thus, the students may have answered the questionnaires either with or instead of their relatives. We tried to minimize this possibility by sending the questionnaires in sealed envelopes with letters requesting relatives to answer them on their own.
Conclusion
In LMIC such as Mexico, education represents a powerful tool against misconceptions about breast cancer, which discourage women from seeking screening and treatment. Our results show that implementing a school‐based breast cancer educational program is feasible and acceptable in rural communities, that breast cancer education can be integrated into the regular school curricula, and that educational programs significantly increase knowledge on breast cancer among adolescents. Notably, our results support the concept of intergenerational transmission of knowledge as an innovative tool in cancer education, prevention, and early detection. This novel strategy could allow women with limited health information sources to obtain new knowledge about cancer, and it represents a potentially valuable tool for increasing cancer awareness and health‐seeking behaviors among women in LMIC as well as in underserved communities in high‐income countries.
See http://www.TheOncologist.com for supplemental material available online.
Supplementary Material
Acknowledgments
We sincerely thank the students and their families. We thank the teachers and authorities at Escuela Secundaria Técnica Number 47. We thank Patricia G. Vázquez del Mercado Herrera and the Ministry of Public Education of Puebla for their support in implementing the program. We thank the students from the Intercontinental University for their collaboration in the design and implementation of the sessions. This work was supported by a 2015 International Innovation Grant from the Conquer Cancer Foundation to Yanin Chavarri‐Guerra.
Author Contributions
Conception/design: Enrique Soto‐Perez‐de‐Celis, Arti Hurria, Yanin Chavarri‐Guerra
Provision of study material or patients: Yanin Chavarri‐Guerra
Collection and/or assembly of data: Enrique Soto‐Perez‐de‐Celis, Maria Patricia Rojo‐Castillo, Alba Milena Pavas‐Vivas, Rina Gitler‐Weingarten, Alejandro Mohar, Yanin Chavarri‐Guerra
Data analysis and interpretation: Enrique Soto‐Perez‐de‐Celis, David D. Smith, Yanin Chavarri‐Guerra
Manuscript writing: Enrique Soto‐Perez‐de‐Celis, Yanin Chavarri‐Guerra
Final approval of manuscript: Enrique Soto‐Perez‐de‐Celis, David D. Smith, Maria Patricia Rojo‐Castillo, Arti Hurria, Alba Milena Pavas‐Vivas, Rina Gitler‐Weingarten, Alejandro Mohar, Yanin Chavarri‐Guerra
Disclosures
Enrique Soto‐Perez‐de‐Celis: Amgen (travel expenses); Arti Hurria: Celegene, Novartis, GlaxoSmithKline (RF), Boehringer Ingelheim Pharmaceuticals, Carevive, Sanofi, GTx, Inc., Pierian Biosciences (C/A); Yanin Chavarri‐Guerra: Roche (C/A), Novartis (H). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1. Goss PE, Lee BL, Badovinac‐Crnjevic T et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol 2013;14:391–436. [DOI] [PubMed] [Google Scholar]
- 2. Chavarri‐Guerra Y, Villarreal‐Garza C, Liedke PE et al. Breast cancer in Mexico: A growing challenge to health and the health system. Lancet Oncol 2012;13:e335–e343. [DOI] [PubMed] [Google Scholar]
- 3. Unger‐Saldana K, Infante‐Castaneda C. Delay of medical care for symptomatic breast cancer: A literature review [in Spanish]. Salud Publica Mex: 2009;51(suppl 2):s270–s285. [DOI] [PubMed] [Google Scholar]
- 4. Mohar A, Bargallo E, Ramirez MT et al. Available resources for the treatment of breast cancer in Mexico [in Spanish]. Salud Publica Mex 2009;51(suppl 2):s263–s269. [PubMed] [Google Scholar]
- 5. Schwartsmann G. Breast cancer in South America: Challenges to improve early detection and medical management of a public health problem J Clin Oncol 2001;19(suppl 18):118S–124S. [PubMed] [Google Scholar]
- 6. Nigenda G, Caballero M, Gonzalez‐Robledo LM. Access barriers in early diagnosis of breast cancer in the Federal District and Oaxaca [in Spanish]. Salud Publica Mex 2009;51(suppl 2):s254–s262. [PubMed] [Google Scholar]
- 7. Anderson BO, Ilbawi AM, El Saghir NS. Breast cancer in low and middle income countries (LMICs): A shifting tide in global health. Breast J 2015;21:111–118. [DOI] [PubMed] [Google Scholar]
- 8. Eniu A, Carlson RW, El Saghir NS et al. Guideline implementation for breast healthcare in low‐ and middle‐income countries: Treatment resource allocation. Cancer 2008;113(suppl 8):2269–2281. [DOI] [PubMed] [Google Scholar]
- 9. Yépez‐Ramírez D, de la Rosa A, Guerrero‐Albarrán C et al. Breast Self‐Examination: Knowledge and perspective in women [in Spanish]. Rev Med Inst Mex Seguro Soc 2012;20:79–84. [Google Scholar]
- 10. Torres‐Echavarría E, García‐Martínez G, Marín‐Galindo M et al. Significant learning on women between 20 and 59 years old related to breast self‐examination [in Spanish]. Rev Med Inst Mex Seguro Soc 2004;12:131–135. [Google Scholar]
- 11. General Assembly resolution 54/135, Improvement of the situation of women in rural areas, A/RES/54/135 (7 February 2000).
- 12. Programa de Naciones Unidas para el Desarrollo‐México. Rural women in Mexico: Strategies for their development; [in Spanish]. Mexico City: Secretaria de Relaciones Exteriores, 2006. [Google Scholar]
- 13. Kyle RG, Forbat L, Rauchhaus P et al. Increased cancer awareness among British adolescents after a school‐based educational intervention: A controlled before‐and‐after study with 6‐month follow‐up. BMC Public Health 2013;13:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hubbard G, Stoddart I, Forbat L et al. School‐based brief psycho‐educational intervention to raise adolescent cancer awareness and address barriers to medical help‐seeking about cancer: A cluster randomised controlled trial. Psychooncology 2016;25:760–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gandeh MB, Milaat WA. Effect of a breast cancer health education program on the awareness and practice of jeddah female secondary school students. J Family Community Med 2000;7:31–36. [PMC free article] [PubMed] [Google Scholar]
- 16. Knafo A, Galansky N. The Influence of Children on Their Parents’ Values. Soc Personal Psychol Compass 2008;2:1143–1161. [Google Scholar]
- 17. Dillon JJ. The Role of the Child in Adult Development. J Adult Dev. 2002;9:267–275. [Google Scholar]
- 18. Thabane L, Ma J, Chu R et al. A tutorial on pilot studies: The what, why and how. BMC Med Res Methodol 2010;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Instituto Nacional de Estadistica y Geografia. National Population and Housing Census 2010 [in Spanish]. 2010.
- 20.Consejo Nacional de Poblacion. Marginality Index by Municipality 2010. [in Spanish]. 2010.
- 21. Breast Health Education for Young Women‐A Facilitator's Guide. Prevent Cancer Foundation and the Howard University Cancer Center, 2012. [Google Scholar]
- 22. Pardo E. Mom's Brassiere [in Spanish]. Mexico City: Fundacion Alma and TRILCE, 2013. [Google Scholar]
- 23. Anderson BO, Cazap E, El Saghir NS et al. Optimisation of breast cancer management in low‐resource and middle‐resource countries: Executive summary of the Breast Health Global Initiative consensus, 2010. Lancet Oncol 2011;12:387–398. [DOI] [PubMed] [Google Scholar]
- 24. Narro J, Martuscellil J, Barzana E. Ten year plan to develop the National Educational System [in Spanish]. Dirección General de Publicaciones y Fomento Editorial UNAM.
- 25. Eisenmann M, Summer T. Basic issues in EFL teaching and learning. 1., neue Ausg. ed. Heidelberg: Universitätsverlag Winter, 2012. [Google Scholar]
- 26.2011 Study Programs. Guide for Teachers. Basic Secondary Education. Science [in Spanish]. Subsecretaria de Educacion Basica de la Secretaria de Educacion Publica, 2011.
- 27. Tapia‐Curiel A, Nuno‐Gutierrez BL, Flores‐Padilla L et al. Perceptions of adolescents Jalisco campaign on breast cancer [in Spanish]. Rev Med Inst Mex Seguro Soc 2015;53:414–421. [PubMed] [Google Scholar]
- 28. Calderon‐ Garciduenas AL, Flores‐Pena Y, De Leon‐Leal S et al. An educational strategy for improving knowledge about breast and cervical cancer prevention among Mexican middle school students. Prev Med Rep 2015;2:250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Soto‐Perez‐de‐Celis E, Chavarri‐Guerra Y. National and regional breast cancer incidence and mortality trends in Mexico 2001–2011: Analysis of a population‐based database. Cancer Epidemiol 2016;41:24–33. [DOI] [PubMed] [Google Scholar]
- 30. Damerell P, Howe C, Milner‐Gulland EJ. Child‐orientated environmental education influences adult knowledge and household behaviour. Environmental Research Letters 2013;8:015016. [Google Scholar]
- 31. Vaughan C, Gack J, Solorazano H et al. The effect of environmental education on schoolchildren, their parents, and community members: A study of intergenerational and intercommunity learning. J Environ Educ 2003;34:12–21. [Google Scholar]
- 32. Perlmutter M, University of Minnesota. Institute of Child Development. Parent‐child interaction and parent‐child relations in child development. Hillsdale, NJ: L. Erlbaum Associates, 1984. [Google Scholar]
- 33. Calvert S. Children as Consumers: Advertising and Marketing. Future Child 2008;18:205–234. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.