Abstract
Importance
Intimate partner violence (IPV) and heavy drinking are co-occurring public health problems, but integrated brief interventions for these conditions have not been tested.
Objective
To determine whether a brief motivational intervention provided at the time of an emergency department (ED) visit reduces IPV and heavy drinking.
Design, Setting, and Participants
A randomized clinical trial conducted at 2 US academic urban EDs between January 2011 and December 2014 to assess the effectiveness of a motivational intervention for IPV-involved female ED patients (ages: 18-64 years; N = 600) who exceeded sex-specific safe drinking limits. All received social service referrals; 2:2:1 to brief intervention (n = 242), assessed control (n = 237), or no-contact control (n = 121).
Interventions
A 20- to 30-minute manual-guided motivational intervention (recorded and monitored for fidelity) delivered by master's-level therapists with a follow-up telephone booster. The assessed control group received the same number of assessments as the brief intervention group; the no-contact control group was assessed only once at 3 months.
Main Outcomes and Measures
Incidents of heavy drinking and experiencing IPV measured over prespecified, 12 weekly assessments using an interactive voice response system.
Results
Of 600 participants, 80% were black women with a mean age of 32 years. Retention was 89% for 2 or more interactive voice response system calls. Seventy-eight percent of women completed the 3-month interview, 79% at 6 months, and 71% at 12 months. During the 12-week period following the brief motivational intervention, there were no significant differences between the intervention group and the assessed control group on weekly assessments for experiencing IPV (odds ratio [OR], 1.02; 95% CI, 0.98-1.06) or heavy drinking (OR, 0.99; 95% CI, 0.96-1.03). From baseline to 12 weeks, the number of women with any IPV in the past week decreased from 57% (134 of 237) in the intervention group to 43% (83 of 194) and from 63% (145 of 231) in the assessed control group to 41% (77 of 187) (absolute difference of 8%). From baseline to 12 weeks, the number of women with past week heavy drinking decreased from 51% (120 of 236) in the intervention group to 43% (83 of 194) and from 46% (107 of 231) in the assessed control group to 41% (77 of 187) (absolute difference of 3%). At 12 months, 43% (71 of 165) of the intervention group and 47% (78 of 165) of the assessed control group reported no IPV during the previous 3 months and 19% (29 of 152) of the intervention group and 24% (37 of 153) of the control group had reduced their alcohol consumption to sex-specific National Institute on Alcohol Abuse and Alcoholism safe drinking levels.
Conclusions and Relevance
For women experiencing IPV and heavy drinking, the use of a brief motivational intervention in the ED compared with assessed and no-contact controls did not significantly reduce the days of heavy drinking or incidents of IPV. These findings do not support a brief motivational intervention in this setting.
There is a strong and reciprocal association between 2 highly prevalent public health problems: intimate partner violence (IPV) and heavy drinking.1,2 Each risk individually represents major costs to individuals, families, and society3,4 and each may be amenable to intervention.5,6 The emergency department (ED) visit is conceptualized as a sensitive period or window of time during the life course when exposure to motivational health promotion might have an influence on behaviors.7
Brief motivational interventions are time-limited, clinically based interactions based on the principles of motivational enhancement therapy.8 In the ED setting, brief interventions have been found to be effective in reducing alcohol consumption and alcohol-related injury among patients with hazardous drinking; however, such interventions have been found to be less effective in women.9,10 These mixed results by sex have been attributed to higher rates of co-occurring psychosocial risk among female drinkers, including IPV.10,11
The relationship between heavy drinking, aggression, and experiencing or perpetrating IPV among both women and men is well recognized but complex and frequently bidirectional.1,2,12 Women who use violence to resolve conflict may be at increased risk of abuse and injury13; theoretically, an intervention that reduces a woman's aggression toward her partner may reduce the likelihood that her partner will perpetrate abuse. Recent evidence also suggests that women drink to cope with abuse.14,15 Due to the intensity and complexity of the relationship between heavy drinking and IPV, it is likely that both of these risk factors may need to be addressed to decrease the risk of the abuse of women who are heavy drinkers.
We sought to determine whether an intervention for co-occurring IPV and heavy drinking would be effective in the ED setting. Based on the available evidence, we hypothesized that a sex-specific brief motivational interview, an intervention that is ideally suited to the fast-paced ED setting, would have the potential to reduce both or either risk among IPV-involved female drinkers.
Methods
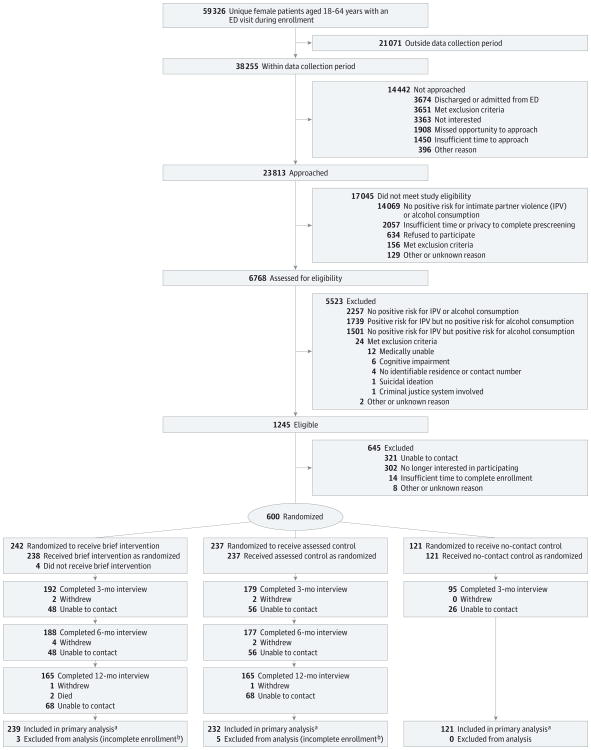
The study protocol has been previously reported16 and it also appears in Supplement 1. Between January 2011 and November 2013, we enrolled 600 female patients in a randomized clinical trial conducted at 2 affiliated urban academic EDs in Philadelphia, Pennsylvania, that serve approximately 100 000 patients per year (Figure 1). Twelve-month follow-up was completed in December 2014. Eligible participants were alert, English-speaking females between the ages of 18 and 64 years, who were not critically ill and could be approached in private and provide consent and safe contact information. Participants were block randomized in groups of 20 using a 2:2:1 distribution to the brief intervention group, the assessed control group, or the no-contact control group. The intervention group and the assessed control group completed verbal baseline interviews at enrollment, weekly assessments for 12 weeks, and follow-up measures by telephone at 3, 6, and 12 months. After eligibility screening, the no-contact control group was only assessed once at 3 months to determine the extent to which improvements over time might be due to assessment reactivity. All participants received usual care and a standard list of social service resources.
Figure 1. Flow of Female Patients Approached at Emergency Departments (EDs) to Participate in Study to Assess Effects of Intimate Partner Violence and Heavy Drinking.
aOf 592 total participants included in primary analysis.
bDefined as failing to complete all enrollment and any follow-up activities.
All participants provided written informed consent prior to enrollment in the study, which was approved by the University of Pennsylvania institutional review board. All protocols and blinded data were reviewed at intervals by a data and safety monitoring board.
Intervention
The intervention group received a 20- to 30-minute manual-guided motivational intervention, delivered by master's-level therapists during the ED visit and a telephone booster at 10 days. The treatment training manual was modeled on brief ED interventions targeting drinking and risky driving17-19 and used motivational interviewing20 and empowerment theoretical frameworks21 (eMethods in Supplement 2). Extensively pilot tested and revised after input from female patients and experts in IPV,22 drinking among women,23 and motivational interviewing,24 the intervention formalizes measurable components of reflective feedback, avoidance of confrontation, respect, empathy, and empowerment, which are all consistent with the principles of IPV advocacy.21
The goal of the intervention was to elicit the patient's self-identified reasons for change and personal goals.20,24 During the intervention sessions, which were recorded and analyzed for fidelity, the therapists encouraged participants to identify any linkages between their drinking and IPV, and helped them to resolve ambivalence regarding behavioral change, while also supporting the patient's autonomy and personal choice.20,24 An unrecorded telephone follow-up booster with the same therapist occurred approximately 10 days later to consolidate and reinforce the motivational interviewing session.17
All therapists had training and experience working with abused women before the initiation of this study. They received extensive additional training and supervision by motivational interviewing experts through biweekly review of recorded sessions. Study participants had the option not to have their brief interventions recorded.
An independent motivational interviewing consultant reviewed and rated 10% of randomly sampled recordings throughout the study with ongoing feedback to the therapists. At study completion, 203 recordings (85%) were available for quality ratings by the developer of the motivational interviewing adherence scale.25 Three raters were used and a high intraclass correlation coefficient (ICC) was obtained for adherence scores (ICC = 0.86); there was 98.4% adherence to motivational interviewing techniques.25
Measures
All demographic, baseline, and outcome measures were collected from participants via self-report (Table 1). To describe our patient population, race/ethnicity was collected using fixed categories with the option for participants to specify other or multiple races. Primary outcomes were assessed weekly for 12 weeks using an the interactive voice response system (IVRS) among the brief intervention group and the assessed control group. The primary drinking outcome was days of heavy alcohol consumption (>4 drinks/day)29 during the past week from the Alcohol Use Disorders Identification Test alcohol consumption30 (AUDIT-C) questions. The primary IPV outcome was any past week verbal, physical, or sexual abuse (8 items from the Revised Conflict Tactics Scales [CTS2S]).31
Table 1. Baseline Demographics and Risk Factors by Study Groupa.
| Overall | Brief Intervention Group | Control Groups | ||
|---|---|---|---|---|
| Assessed | No Contact | |||
| Sociodemographics | ||||
| No. of women | 592 | 239 | 232 | 121 |
| Age, y | ||||
| Mean (95% CI) | 32.1 (31.3-33.0) | 32.3 (30.9-33.6) | 32.1 (30.6-33.6) | 32.0 (30.0-33.9) |
| Median (IQR) | 29 (23-40) | 29 (24-39) | 29 (24-41) | 28 (23-40) |
| Level of education | ||||
| Some high school | 116 (19.6) | 49 (20.5) | 48 (20.7) | 19 (15.7) |
| High school degree | 164 (27.7) | 61 (25.5) | 65 (28.0) | 38 (31.4) |
| Some college or degree | 273 (46.1) | 107 (44.8) | 106 (45.7) | 60 (49.6) |
| Some postgraduate or degree | 37 (6.3) | 22 (9.2) | 12 (5.2) | 3 (2.5) |
| Missing or unknown | 2 (0.3) | 0 | 1 (0.4) | 1 (0.8) |
| Household income, $ | ||||
| ≤10 000 | 174 (29.4) | 61 (25.5) | 72 (31.0) | 41 (33.9) |
| 10 000-19 999 | 129 (21.8) | 51 (21.3) | 52 (22.4) | 26 (21.5) |
| 20 000-49 999 | 164 (27.7) | 73 (30.5) | 60 (25.9) | 31 (25.6) |
| ≥50 000 | 70 (11.8) | 34 (14.2) | 23 (9.9) | 13 (10.7) |
| Missing | 55 (9.3) | 20 (8.4) | 25 (10.8) | 10 (8.3) |
| Employment | ||||
| No | 299 (50.5) | 119 (49.8) | 114 (49.1) | 66 (54.5) |
| Yes | 291 (49.2) | 120 (50.2) | 117 (50.4) | 54 (44.6) |
| Missing | 2 (0.3) | 0 | 1 (0.4) | 1 (0.8) |
| Marital status | ||||
| Single | 459 (77.5) | 184 (77.0) | 181 (78.0) | 94 (77.7) |
| Married | 86 (14.5) | 37 (15.5) | 31 (13.4) | 18 (14.9) |
| Divorced, widowed, or separated | 46 (7.8) | 18 (7.5) | 19 (8.2) | 9 (7.4) |
| Missing | 1 (0.2) | 0 | 1 (0.4) | 0 |
| Partnership status | ||||
| Single | ||||
| Not dating | 61 (10.3) | 27 (11.3) | 22 (9.5) | 12 (9.9) |
| Dating | 93 (15.7) | 34 (14.2) | 38 (16.4) | 21 (17.4) |
| Relationship | ||||
| Off and on | 96 (16.2) | 31 (13.0) | 41 (17.7) | 24 (19.8) |
| Committed | 330 (55.7) | 141 (59.0) | 128 (55.2) | 61 (50.4) |
| Missing | 12 (2.0) | 6 (2.5) | 3 (1.3) | 3 (2.5) |
| Sex of partner | ||||
| Male | 489 (82.6) | 203 (84.9) | 186 (80.2) | 100 (82.6) |
| Female | 41 (6.9) | 17 (7.1) | 16 (6.9) | 8 (6.6) |
| Other | 2 (0.3) | 1 (0.4) | 1 (0.4) | 0 |
| Missing | 60 (10.1) | 18 (7.5) | 29 (12.5) | 13 (10.7) |
| No. of children (age <18 y) in household | ||||
| 0 | 261 (44.1) | 116 (48.5) | 96 (41.4) | 49 (40.5) |
| 1 | 124 (20.9) | 49 (20.5) | 47 (20.3) | 28 (23.1) |
| ≥2 | 186 (31.4) | 65 (27.2) | 81 (34.9) | 40 (33.1) |
| Missing | 21 (3.5) | 9 (3.8) | 8 (3.4) | 4 (3.3) |
| Race/ethnicityb | ||||
| Black | 471 (80.1) | 178 (74.8) | 187 (81.3) | 106 (88.3) |
| White | 108 (18.4) | 53 (22.3) | 38 (16.5) | 17 (14.2) |
| Native American | 20 (3.4) | 11 (4.6) | 5 (2.2) | 4 (3.3) |
| Hispanic | 28 (4.8) | 13 (5.5) | 12 (5.2) | 3 (2.5) |
| Pacific Islander | 3 (0.5) | 2 (0.8) | 0 | 1 (0.8) |
| Asian | 8 (1.4) | 4 (1.7) | 3 (1.3) | 1 (0.8) |
| Other | 35 (6.0) | 14 (5.9) | 17 (7.4) | 4 (3.3) |
| Missing | 4 (0.7) | 1 (0.4) | 2 (0.9) | 1 (0.8) |
| Pregnant during the first 3 mo | ||||
| No | 477 (80.6) | 196 (82.0) | 199 (85.8) | 82 (67.8) |
| Yes | 86 (14.5) | 43 (18.0) | 33 (14.2) | 10 (8.3) |
| Missing | 29 (4.9) | 0 | 0 | 29 (24.0) |
| Chief concern at enrollment | ||||
| Injury | 78 (13.2) | 30 (12.6) | 30 (12.9) | 18 (14.9) |
| Medical | 420 (70.9) | 173 (72.4) | 165 (71.1) | 82 (67.8) |
| Gynecologic or urinary | 79 (13.3) | 28 (11.7) | 32 (13.8) | 19 (15.7) |
| Other | 15 (2.5) | 8 (3.3) | 5 (2.2) | 2 (1.7) |
| Risk Factors | ||||
| No. of women | 566 | 239 | 232 | 95c |
| Women's Experience with Battering Scale26 scored | ||||
| Mean (95% CI) | 19.6 (18.5-20.7) | 19.7 (17.8-21.4) | 20.5 (18.6-22.3) | 17.1 (14.5-19.5) |
| Median (IQR) | 13 (10-24) | 13 (10-25) | 13 (10-27) | 11 (10-20) |
| Danger Assessment27 scoree | ||||
| Mean (95% CI) | 9.9 (9.3-10.5) | 10.0 (9.1-10.9) | 10.3 (9.3-11.2) | 8.5 (7.2-9.8) |
| Median (IQR) | 13 (4-13) | 13 (4-14) | 9 (5-14) | 7.5 (4-12) |
| Alcohol dependencef | 87 (15.5) | 32 (13.0) | 39 (16.4) | 17 (17.9) |
| Smoking | 334 (59.0) | 135 (56.7) | 144 (62.3) | 55 (57.9) |
| Drug use | ||||
| Illegal, including marijuana | 258 (45.7) | 100 (46.1) | 105 (49.5) | 34 (35.8) |
| Illegal, not including marijuana | 98 (17.4) | 41 (17.2) | 46 (20.0) | 11 (11.6) |
| Prescription misuse | 64 (11.6) | 24 (10.4) | 33 (14.8) | 7 (7.4) |
| Depression scoreg | 488 (86.2) | 210 (87.9) | 231 (85.3) | 79 (84.0) |
| Posttraumatic stress disorderh | 228 (40.4) | 100 (41.8) | 95 (41.3) | 32 (34.0) |
| Childhood sexual abuse | 243 (43.2) | 100 (41.8) | 98 (42.8) | 45 (47.9) |
| Partner drinking | 110 (20.0) | 46 (19.4) | 38 (16.6) | 12 (12.5) |
Abbreviation: IQR, interquartile range.
Data are expressed as No. (%) unless otherwise indicated. For the between-treatment comparisons, age was analyzed using a general linear model and all categorical variables were analyzed using the χ2 test.
Participants instructed to “check all that apply”; therefore, percentages add to more than 100%. Differences between groups used a binary variable (black vs not black).
Data were only collected at 3 months for those who completed the follow-up interview (n = 95; 79% retention).
Score range: 10 to 40 (0-19 indicating lower severity and ≥20 indicating higher severity).
Score range: 0 to 39 (level of danger: 0-7, variable; 8-13, increased; 14-17, severe; ≥18, extreme).
Indicated by an Alcohol Use Disorders Identification Test28 (AUDIT) score of greater than 13.
Indicated by a Center for Epidemological Studies-Depression 10 score of 10 or greater (score range: 0-30).
Indicated by a Primary Care Post-Traumatic Stress Disorder score of 3 or greater (score range: 0-4).
Secondary outcomes were assessed at 3, 6, and 12 months for the brief intervention group and the assessed control group but only once at 3 months for the no-contact control group. Secondary drinking outcomes included changes in the full AUDIT28 score and both quantity and frequency of drinking using the Timeline Follow-Back technique.32 Secondary IPV outcomes included frequency and severity of experiencing or perpetrating IPV (16 items) from the full CTS2S31 and changes in the Composite Abuse Scale.33 Other health-related outcomes included measures of self-rated health, depression, sleep, social support, quality of life, satisfaction with relationship, and engagement with treatment.16 All non-IVRS post-baseline assessments were conducted by trained interviewers blinded to treatment assignment.
Statistical Analysis
We used a modified intent-to-treat analysis that included all participants with complete enrollment and at least 1 postbaseline assessment, regardless of whether the participant received the intervention. The presence or absence of past week heavy drinking and experiencing IPV collected by the IVRS were the primary binary end points for comparing the intervention group and the assessed control group. The analyses of the primary longitudinal end points from the 12 weeks of IVRS assessments used a hierarchical generalized linear model to accommodate the co-variance structure and the correlation among repeated measurements over time observed for each patient. Similarly, secondary outcome measures collected at baseline and at 3, 6, 9, and 12 months were compared (brief intervention group vs assessed control group) using the hierarchical generalized linear model. For outcomes demonstrating a large proportion of zeros, zero-inflated Poisson and zero-inflated negative binomial models were generated.
The mixed-effects models used a maximum likelihood estimation approach that assumed any missing outcome data to be missing at random (ie, missing data including those due to dropout can be dependent on any previously observed outcomes or treatment assignment). With this approach, all data that have been collected without regard to whether data are missing for a patient at another visit, including dropouts, and without explicit imputation of missing data, can be used. Analyses were generated to test whether missing data were related to key treatment or baseline demographic characteristics. Analyses of 3-month CTS2S and AUDIT data were performed to determine the assessment reactivity effect on the primary outcomes, with specific contrasts between the assessed control group and the no-contact control group.
A priori power analysis was based on a 2-sided .03 significance level to accommodate 2 primary outcomes: heavy drinking days and IPV incidents, with significance on either outcome providing evidence of a positive study. Based on prior studies,19 199 patients per group were required to achieve at least 80% power to detect 2 days of heavy drinking per month. Without prior effect sizes for IPV interventions, we designed the study to have 94% power to detect a 20% difference between groups in the incidence rate of IPV (assuming 30% attrition) during the first 12 weeks of treatment.
Results
From January 2011 to November 2013, there were a total of 112 167 ED visits by 59 326 unique female patients between the ages of 18 and 64 years (Figure 1). Approximately 53.4% of 59 924 total visits by 38 255 unique patients occurred during data collection time frames (Monday-Saturday, 9 am-7 pm). Of these, 28813 unique patients were approached and 6768 were assessed for study eligibility.
Based on positive screenings for past 3-month IPV(CTS2S score >1)31 and heavy drinking (National Institute on Alcohol Abuse and Alcoholism sex-specific criteria ≥4 drinks/day or AUDIT score >4),29 1245 women were eligible for the study. The main reason for ineligibility was failing to meet criteria for both risk factors. Of those eligible, 24% declined to participate and 27% were discharged before enrollment could occur; 48% (N = 600)signed written informed consent and were randomized (2:2:1) as planned into the 3 groups. Eight randomized participants were excluded due to incomplete enrollment without follow-up contact, leaving 592 (98.7%) for analysis with 239 in the brief intervention group, 232 in the assessed control group, and 121 in the no-contact control group.
Compared with women who did not enroll, eligible women who enrolled were older, more likely of black race, and had higher IPV and drinking severity scores (eTable 1 in Supplement 2). Overall attrition rates and missing data did not vary by group at any time point; 78% of participants completed the 3-month interview, 79% completed the 6-month interview, and 71% completed the 12-month interview without differential attrition by severity of IPV or drinking. Participant safety was carefully tracked; no harms related to the intervention were identified.
Baseline demographics and risk factors were fairly well balanced across the groups (Table 1). Exceptions were slightly more white patients in the intervention group, the no-contact control group had higher rates of IPV at baseline, and more women in the assessed control group had previously used community-based IPV services compared with the intervention group (10% vs 4%, respectively).
Black women comprised 80% of the study, the mean age was 32 years, most were in relationships (88%) but unmarried (86%), 71% presented to the ED for medical concerns, 14.5% were pregnant, approximately half had children younger than 18 years, were employed, and living in households with incomes of less than $20 000. Comorbid risk factors were prominent: 60% smoked cigarettes, 17% disclosed using illicit drugs (46% including marijuana), 12% were positive for nonmedical use of prescription drugs, 43% disclosed a history of child sexual abuse, 40% screened positive for posttraumatic stress disorder, and 86% screened positive for depression. Baseline levels of alcohol dependence were 16% (AUDIT score >13)28 and mean IPV levels were severe on the Women's Experience with Battering Scale (score range: 10-40; ≥20 indicates higher severity)26 and Danger Assessment (score range: 0-39; ≥18 indicates extreme danger).27
Primary Outcomes
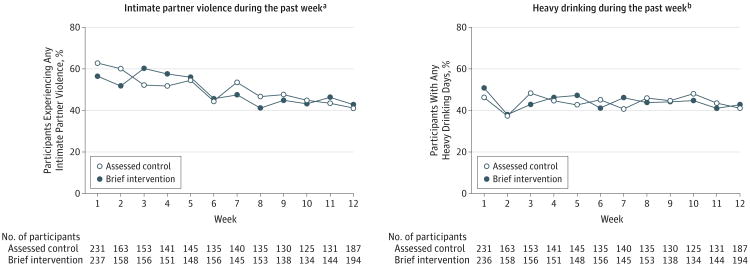
The primary outcomes of experiencing any IPV and any days of heavy drinking during the past week appear in Figure 2. This was tracked for 12 weeks after the ED visit only for women in the intervention group and the assessed control group; 89% of participants completed at least 2 of the weekly IVRS calls and 71% completed 50% or more. During the 12-week period following the brief motivational intervention, there were no significant differences between the intervention group and the assessed control group on weekly assessments for experiencing IPV (odds ratio [OR], 1.02; 95% CI, 0.98-1.06) or heavy drinking (OR, 0.99; 95% CI, 0.96-1.03) (eTable 2 in Supplement 2).
Figure 2. Participants Experiencing Intimate Partner Violence or Heavy Drinking in Assessed Control and Brief Intervention Groups.
aIndicates a response of 1 or more. Using a binary outcome of any overall violence experienced, this graph presents the percentage of participants in each group who reported any experience with intimate partner violence, including any incidence of physical, verbal, emotional, and sexual abuse for the 12-week follow-up period. Experiencing intimate partner violence is defined as answering “yes” to 1 or more of the questions coded as “Victimization” on the Revised Conflict Tactics Scales assessment.
bIndicates a response of at least 1 incidence. This graph presents the percentage of participants in each group who reported any heavy drinking days (≥4 drinks) during the past week for the 12-week follow-up period.
The incidence of past week heavy drinking at baseline (week 1) was 51%(95%CI, 44%-57%) in the intervention group (120 of 236 women) and 46% (95% CI, 40%-53%) in the assessed control group (107 of 231 women), which decreased by week 12 to 43% (95% CI, 36%-50%) in the intervention group (83 of 194 women) and 41% (95% CI, 34%-48%) in the assessed control group (77 of 187 women); however, the change was not statistically significant (P = .74 for treatment group × time interaction). The baseline incidence of past week IPV was 57% (95%CI, 50%-63%)in the intervention group (134 of 237 women)and 63%(95%CI, 57%-69%) in the assessed control group (145 of 231 women), which decreased by week12 to 43% (95% CI, 36%-50%) in the intervention group (83 of 194 women) and 41% (95% CI, 34%-48%) in the assessed control group (77 of 187 women) (P = .33 for treatment group × time interaction).
Secondary Outcomes
The test for assessment reactivity (assessed control group vs no-contact control group) and the comparison of IPV and drinking outcomes (intervention group vs each of the control groups at 3 months) appear in Table 2. Controlling for baseline differences, experiencing abuse during the last 3 months was significantly reduced for the no-contact control group compared with the assessed control group, indicating that the assessment did not serve as an intervention. However, there were no significant differences in IPV and drinking outcomes between the intervention group and either control group at 3 months.
Table 2. Incidence of Intimate Partner Violence (IPV) and Alcohol Consumption Outcomes at 3 Months and Assessment Reactivity.
| Brief Intervention Group | Control Groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Assessed | No Contact | |||||||||
| Baseline (n = 239)a | At 3 mo (n = 192) | At 6 mo (n = 188) | At 12 mo (n = 165) | Baseline (n = 232)a | At 3 mo (n = 179) | At 6 mo (n = 176) | At 12 mo (n = 165) | Baseline (n = 121)a | At 3 mo (n = 95) | |
| Incidence of IPV | ||||||||||
| CTS2S scoreb | ||||||||||
| Mean (95% CI) | 9.4 (8.3-10.6) | 8.5 (7.0-10.0) | 6.2 (5.1-7.3) | 5.6 (4.5-6.7) | 9.9 (8.6-11.2) | 8.5 (7.0-10.0) | 6.1 (4.8-7.4) | 6.2 (4.7-7.7) | 12.2 (10.2-14.2) | 7.4 (5.4-9.4) |
| Median (IQR) | 7 (3-12) | 4.5 (0.5-12.0) | 4 (0-8.5) | 3 (0-9) | 6 (3-12) | 5 (1-14) | 4 (0-8) | 2 (0-8) | 7 (5-18) | 4 (0-11) |
| Experienced IPVc | ||||||||||
| Mean (95% CI) | 4.5 (3.8-5.2) | 4.3 (3.5-5.2) | 3.0 (2.3-3.6) | 2.7 (2.1-3.3) | 4.9 (4.0-5.7) | 4.7 (3.8-5.6)d | 3.3 (2.6-4.1) | 3.3 (2.4-4.2) | 5.9 (4.7-7.2) | 3.3 (2.3-4.3)d |
| Median (IQR) | 3 (1-6) | 2 (0-6) | 1 (0-4) | 1 (0-4) | 3 (1-6) | 2.5 (0-7.0) | 2 (0-4) | 1 (0-3) | 3.5 (1.5-8.0) | 2 (0-5) |
| Perpetratione | ||||||||||
| Mean (95% CI) | 5.0 (4.4-5.5) | 4.2 (3.5-5.2) | 3.2 (2.6-3.8) | 2.9 (2.3-3.5) | 5.1 (4.4-5.7) | 3.8 (3.1-4.5) | 2.8 (2.2-3.4) | 2.9 (2.2-3.7) | 6.3 (5.3-7.3) | 4.2 (3.2-5.2) |
| Median (IQR) | 4 (2-6) | 3 (0-6) | 2 (0-5) | 2 (0-5) | 3 (2-6) | 3 (0-6) | 2 (0-4) | 1 (0-4) | 4.0 (2.5-9.0) | 2.5 (0-6.0) |
| Incidence of Risky Drinking | ||||||||||
| AUDIT scoref | ||||||||||
| Mean (95% CI) | 7.9 (7.3-8.6) | 9.0 (8.1-9.9) | 8.4 (7.3-9.5) | 7.4 (6.4-8.4) | 8.7 (7.9-9.5) | 9.7 (8.6-10.7) | 7.7 (6.8-8.6) | 7.4 (6.3-8.5) | 8.2 (7.2-9.3) | 8.3 (6.9-9.7) |
| Median (IQR) | 6.0 (4.4-10.0) | 7 (4-12) | 6 (3-11) | 6 (4-9) | 6 (5-10) | 7.0 (4.4-13.0) | 6 (4-10) | 5 (3-10) | 6.0 (5.0-9.5) | 7 (4-10) |
| Heavy episodic drinking, No. (%)g | ||||||||||
| Never | 20 (8.4) | 47 (24.6) | 51 (27.3) | 41 (24.9) | 27 (11.7) | 34 (19.1) | 44 (25.0) | 40 (24.4) | 10 (8.3) | 23 (24.4) |
| <Monthly | 98 (41.2) | 51 (26.7) | 48 (25.7) | 58 (35.2) | 92 (39.8) | 53 (29.8) | 51 (29.0) | 55 (33.5) | 56 (46.7) | 30 (31.9) |
| Monthly | 77 (32.4) | 37 (19.2) | 41 (21.9) | 40 (24.3) | 57 (24.7) | 46 (25.8) | 43 (24.4) | 39 (23.4) | 30 (25.0) | 24 (25.5) |
| Weekly | 35 (14.7) | 47 (24.6) | 34 (18.2) | 18 (10.9) | 45 (19.5) | 35 (19.7) | 31 (17.6) | 23 (14.0) | 21 (17.5) | 12 (12.8) |
| Daily or almost daily | 8 (3.4) | 9 (4.7) | 13 (7.0) | 8 (4.9) | 10 (4.3) | 10 (5.6) | 7 (4.0) | 7 (4.3) | 3 (2.5) | 5 (5.3) |
Abbreviation: IQR, interquartile range.
The baseline value of the outcome variable was included in the model as a covariate.
Revised Conflict Tactics Scales (CTS2S) is a 16-item assessment. The scores range from 0 to 96 (higher scores indicate more instances of violence). No IPV during past 3 months is a score of zero on the CTS2S. All participants had a score of 1 or higher to be eligible for study enrollment.
Defined as answering yes to 1 or more of the questions coded as “Victimization” (8 items; score range: 0-48) on the CTS2S.
P = .03 for comparison between the assessed control group and the no-contact control group when controlling for baseline, which indicates a lack of any assessment reactivity because results favor greater reduction in IPV experience among participants in the no-contact control group. Calculated using analysis of variance.
Defined as answering yes to 1 or more of the questions coded as “Perpetration” (8 items; score range: 0-48) on the CTS2S.
The Alcohol Use Disorders Identification Test (AUDIT) consists of 10 items (score range: 4-40).
Indicates a single item on the AUDIT that indicates the frequency (on a Likert scale) of heavy drinking episodes, which for females is 4 or more drinks on any single occasion.
All secondary outcome measures for the intervention group and the assessed control group at 3, 6, and 12 months appear in Table 3. Controlling for any baseline differences, the intervention group reported improved outcomes compared with the assessed control group at 3 months (greater readiness to change their drinking and better quality of life) and at 6 months (greater social support, relationship satisfaction, and better self-rated health). Improvements in social support were the only secondary outcomes favoring the intervention group that remained significant at 12 months.
Table 3. All Secondary Outcome Measures for the Brief Intervention Group vs the Assessed Control Group at 3, 6, and 12 Monthsa.
| Brief Intervention Group | Assessed Control Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline (n = 239)b | At 3 mo (n = 192) | At 6 mo (n = 188) | At 12 mo (n = 165) | Baseline (n = 232)b | At 3 mo (n = 179) | At 6 mo (n = 176) | At 12 mo (n = 165) | |
| Composite Abuse Scalec | ||||||||
| Overall score, mean (95% CI) | 12.7 (10.3-15.0) | 12.2 (9.5-14.9) | 7.6 (5.5-9.6) | 7.3 (5.2-9.4) | 15.9 (13.0-18.8) | 12.6 (9.8-15.5) | 8.6 (6.5-10.6) | 11.1 (7.9-14.3) |
| Physical, No. (%) | 70 (29.3) | 61 (31.8) | 34 (18.1) | 33 (20.0) | 84 (36.4) | 57 (29.7) | 42 (24.3) | 38 (23.2) |
| Emotional, No. (%) | 179 (74.9) | 122 (63.5) | 94 (50.0) | 82 (49.7) | 186 (80.5) | 114 (63.7) | 95 (54.9) | 86 (52.4) |
| Stalking, No. (%) | 81 (33.9) | 70 (36.5) | 59 (31.4) | 44 (26.7) | 80 (34.6) | 65 (36.3) | 53 (30.6) | 44 (26.8) |
| Severe combined abuse, No. (%) | 53 (22.2) | 50 (26.0) | 25 (13.3) | 17 (10.3) | 51 (22.0) | 40 (22.3) | 22 (12.7) | 24 (14.6) |
| Timeline Follow-Backd | ||||||||
| Drinking frequency | ||||||||
| Days/mo, % (95% CI) | 27.0 (24.0-30.3) | 26.4 (22.5-30.3) | 23.3 (19.0-27.0) | 20.0 (17.0-24.0) | 26.8 (23.3-30.3) | 26.3 (22.0-30.0) | 26.4 (22.0-31.0) | 21.4 (18.0-25.0) |
| Days/wk, mean (95% CI) | 1.9 (1.7-2.0) | 1.8 (1.6-2.1) | 1.6 (1.4-1.9) | 1.4 (1.2-1.7) | 1.9 (1.7-2.1) | 1.8 (1.6-2.1) | 1.90 (1.57-2.14) | 1.5 (1.2-1.8) |
| No. of drinks/d, mean (95% CI) | 1.1 (0.9-1.1) | 0.9 (0.8-1.1) | 0.9 (0.7-1.1) | 0.7 (0.5-0.8) | 1.1 (0.9-1.2) | 1.0 (0.7-1.2) | 0.9 (0.7-1.1) | 0.7 (0.6-0.9) |
| Heavy alcohol consumption (≥4 drinks/d), mean (95% CI), d | 3.0 (2.5-3.6) | 3.1 (2.3-3.9) | 2.2 (1.5-2.8) | 2.3 (1.5-3.0) | 3.4 (2.7-3.8) | 3.1 (2.2-4.0) | 2.0 (1.4-2.5) | 2.2 (1.5-2.9) |
| Quality of Life (QOL) Scale, Mean (95% CI)e | ||||||||
| How would you rate your QOL? | 2.3 (2.2-2.4) | 2.2 (2.1-2.4) | 2.1 (2.0-2.3) | 2.2 (2.1-2.3) | 2.3 (2.2-2.5) | 2.4 (2.2-2.5) | 2.2 (2.0-2.3) | 2.2 (2.0-2.3) |
| How much do you enjoy life? | 2.3 (2.2-2.5) | 2.3 (2.2-2.4) | 2.3 (2.1-2.4) | 2.2 (2.0-2.4) | 2.4 (2.2-2.5) | 2.4 (2.2-2.5) | 2.3 (2.1-2.5) | 2.4 (2.2-2.5) |
| How safe do you feel in your daily life? | 2.2 (2.1-2.3) | 2.1 (2.0-2.3)f | 2.1 (2.0-2.3) | 2.1 (1.9-2.2) | 2.2 (2.1-2.3) | 2.3 (2.2-2.5)f | 2.2 (2.0-2.3) | 2.2 (2.1-2.4) |
| Self-Rated Health | ||||||||
| How would you say your health has been? mean (95% CI)g | 3.2 (3.0-3.3) | 3.0 (2.8-3.1) | 2.8 (2.6-2.9)h | 2.9 (2.7-3.1) | 3.4 (3.3-3.6) | 3.2 (3.1-3.4) | 3.1 (2.9-3.3)h | 3.0 (2.8-3.2) |
| Relationship Satisfaction Scale score, mean (95% CI)i | 3.2 (3.0-3.4) | 3.2 (3.0-3.5) | 3.6 (3.3-3.8)j | 3.3 (3.1-3.6) | 3.0 (2.8-3.2) | 2.9 (2.6-3.1) | 3.2 (2.9-3.4)j | 3.4 (3.1-3.6) |
| Exercise frequency, mean (95% CI), d/wk | 3.1 (2.8-3.4) | 3.2 (2.8-3.5) | 2.8 (2.5-3.1) | 3.2 (2.8-3.5) | 3.0 (2.7-3.4) | 3.2 (2.8-3.6) | 3.0 (2.7-3.5) | 3.2 (2.9-3.7) |
| Amount of sleep, mean (95% CI), h/night | 5.6 (5.4-5.9) | 5.8 (5.5-6.0) | 5.7 (5.5-6.0) | 6.0 (5.7-6.3) | 5.5 (5.2-5.7) | 5.8 (5.5-6.1) | 5.9 (5.6-6.2) | 5.8 (5.6-6.1) |
| Smoke cigarettes, No. (%) | 135 (56.7) | 98 (51.0) | 96 (51.1) | 79 (47.9) | 144 (62.3) | 101 (56.4) | 102 (58.0) | 89 (53.9) |
| Self-efficacyk | ||||||||
| Mean (95% CI) | 30.5 (29.8-32.0) | 31.9 (30.6-33.2) | 31.7 (30.3-33.4) | 31.4 (30.4-32.4) | 29.6 (28.9-31.3) | 29.8 (28.4-31.3) | 29.7 (28.7-30.7) | 30.3 (29.4-31.3) |
| Median (IQR) | 30 (27-35) | 32 (28-36) | 31 (27-36) | 32 (28-36) | 30 (26-34) | 30 (25-34) | 30 (26-35) | 31 (26-36) |
| Readiness to Change Scalel | ||||||||
| Drinking | ||||||||
| Mean (95% CI) | 4.1 (3.6-4.6) | 4.4 (3.9-5.0)m | 4.3 (3.7-4.9) | 4.6 (3.9-5.2) | 4.3 (3.9-4.8) | 3.5 (2.9-4.0)m | 3.9 (3.3-4.4) | 3.9 (3.2-4.5) |
| Median (IQR) | 5 (0-8) | 5 (0-8) | 5 (0-8) | 5 (0-8) | 5 (1-8) | 2 (0-8) | 3 (0-8) | 2 (0-8) |
| Relationship | ||||||||
| Mean (95% CI) | 5.9 (5.5-6.3) | 5.8 (5.3-6.4) | 6.0 (5.5-6.5) | 5.9 (5.3-6.5) | 6.0 (5.6-6.4) | 5.5 (5.1-6.0) | 5.6 (5.1-6.1) | 6.0 (5.5-6.6) |
| Median (IQR) | 6 (5-8) | 8 (2-8) | 8 (2-9) | 8 (2-10) | 6 (5-8) | 5 (2-8) | 5 (2-8) | 8 (4-10) |
| Social Support, No. (%) | ||||||||
| Do you have someone to talk to about any problem? | 196 (83.1) | 170 (89.5) | 165 (87.8) | 146 (88.5) | 193 (83.9) | 154 (86.0) | 150 (85.2) | 140 (84.9) |
| Stay with if needed? | 188 (81.0) | 157 (82.6) | 160 (85.6)n | 141 (85.5)n | 174 (75.7) | 138 (77.1) | 136 (77.3)n | 125 (75.8)n |
| Borrow money from if needed? | 172 (74.1) | 145 (75.6) | 145 (77.5)o | 127 (80.0)o | 149 (65.1) | 124 (69.7) | 115 (65.0)o | 107 (65.6)o |
| Engagement With Services, No. (%) | ||||||||
| Any | 35 (14.6) | 28 (14.6) | 26 (13.9) | 13 (8.0) | 44 (19.1) | 26 (14.5) | 22 (12.6) | 20 (12.2) |
| Police or courts for family violence | 18 (7.5) | 12 (6.3) | 11 (5.9) | 5 (3.0) | 20 (8.7) | 13 (7.3) | 11 (6.3) | 9 (5.6) |
| Domestic violence | 10 (4.2) | 15 (7.8) | 9 (4.8) | 4 (2.4) | 23 (10.0) | 9 (5.0) | 7 (4.0) | 10 (6.1) |
| Alcohol or drug | 11 (4.6) | 13 (6.8) | 12 (6.4) | 6 (3.6) | 13 (5.7) | 10 (5.6) | 7 (4.0) | 6 (3.6) |
| Engagement With Treatment, No. (%) | ||||||||
| Any | 161 (67.7) | 132 (69.4) | 121 (64.7) | 107 (64.8) | 169 (73.2) | 120 (67.0) | 117 (66.5) | 122 (73.9) |
| Medical | 149 (62.6) | 117 (60.9) | 112 (60.2) | 97 (58.8) | 160 (69.3) | 109 (61.0) | 104 (59.1) | 114 (69.1) |
| Mental health | 40 (17.2) | 37 (19.4) | 30 (16.0) | 33 (20.1) | 49 (21.4) | 39 (22.0) | 39 (22.3) | 38 (23.0) |
| Drugs or alcohol | 12 (5.2) | 14 (7.3) | 7 (3.8) | 10 (6.1) | 9 (3.9) | 12 (6.7) | 11 (6.3) | 8 (4.9) |
| Family problems | 16 (7.7) | 13 (6.9) | 12 (6.4) | 8 (4.8) | 18 (8.2) | 9 (5.3) | 15 (8.7) | 12 (7.4) |
| Taken steps to obtain safetyp | 55 (29.0) | 45 (24.2) | 53 (32.1) | 58 (32.6) | 51 (29.5) | 47 (28.5) | ||
Abbreviation: IQR, interquartile range.
In creating composite variables, only those women who had at least 80% of nonmissing data for the individual items obtained a value for the composite variable. Otherwise, the composite score for the woman was set to missing.
The baseline value of the outcome variable was included in the model as a covariate.
Contains 30 questions (score range: 0-150). Specific individual items were used to determine if the results indicate the presence of physical, emotional, stalking, or severe combined abuse.
Data are collected using a calendar to record the number of drinks each day for the past month (28 days).
For the question regarding QOL, a score of 1 indicates very good and 5 indicates very poor. For the question regarding enjoyment of life, a score of 1 indicates extremely and 5 not at all. For the question regarding feelings of safety, a score of 1 indicates extremely and 5 not at all.
P = .03 at 3 months controlling for baseline. Calculated using analysis of variance.
A score of 1 indicates excellent and 5 indicates poor.
P = .006 at 6 months controlling for baseline. Calculated using analysis of variance.
This is 1 representative item from the Dynamic Relationship Scale (score range: 0, extremely unhappy; 6, extremely happy).
P = .03 at 6 months controlling for baseline. Calculated using analysis of variance.
The Self-Efficacy Scale scores range from 10 to 40; greater scores indicate greater levels of self-efficacy.
Measures readiness to make changes on a scale from 0 (okay with changes) to 10 (maintaining changes made).
P = .004 at 3 months controlling for baseline. Calculated using analysis of variance.
P = .04 at 6 months and P = .01 at 12 months (both controlling for baseline). Calculated using the χ2 test.
P = .02 at 6 months and P = .03 at 12 months (both controlling for baseline). Calculated using the χ2 test.
Captured with a binary and the following questions: “Have you taken any steps in the past 3 months to increase your safety? What are they?” These questions were only asked at the 3 follow-up time points and not at baseline.
Even though there were no differences between the groups in any of the IPV and drinking outcomes, both drinking and IPV continued to decrease over time. Longitudinal analyses of all IPV and drinking outcomes for the intervention group and the assessed control group found the effect of time to be significant for both heaving drinking (P < .001) and IPV (P < .001) (eTable 2 in Supplement 2).At 12 months, 43.0% (71 of 165) of the intervention group and 47.3% (78 of 165) of the assessed control group reported no IPV in the previous 3 months and 19.1% (29 of 152) of the intervention group and 24.2% (37 of 153) of the assessed control group had reduced their alcohol consumption to sex-specific National Institute on Alcohol Abuse and Alcoholism safe drinking levels.29
Similar to the first 12 weeks, there was no statistically significant treatment effect on any of the IPV or drinking outcomes variables over the full 12 months of the study (treatment group × time interaction: P = .58 for heavy drinking and P = .78 for IPV). Parameter estimates for longitudinal analysis of IPV and drinking outcomes over 12 months appear in eTable 3 in Supplement 2.
Discussion
In our study, a brief 20- to 30-minute motivational intervention delivered with high fidelity during an ED visit did not improve outcomes for women with heavy drinking involved in abusive relationships. We did find that over time, reports of experiencing and perpetrating IPV and days of heavy drinking decreased significantly within the intervention and the control groups alike. However, there was no evidence that these outcomes were influenced by the intervention. In addition, there was no evidence that frequent assessments served as an intervention compared with baseline screening and referral alone.
Preventive health services that involve brief counseling interventions have been found to reduce a variety of behavioral risks, including unhealthy alcohol use.17,18,29 Our results are consistent with previous findings that brief ED interventions are less effective in reducing hazardous drinking among women than among men.9,10 Likewise, Choo et al11 pooled the results from 3 positive brief ED alcohol intervention studies using motivational interviewing and identified that even though there was an overall positive effect with reduced hazardous drinking among men, there was no main effect of the intervention among women or among patients of either sex who were exposed to violence.
Lack of response to alcohol interventions in the ED and trauma settings among female compared with male drinkers has been attributed to the higher rates of psychosocial comorbidity, including IPV,10 which led to our hypothesis that an integrated IPV-alcohol intervention would improve both outcomes in women. Even though our intervention was not effective in the ED setting, it is possible a motivational intervention might be effective in other settings; therefore, we provided the treatment training manual (eMethods in Supplement 2).
Most studies of IPV interventions are far more intensive for longer periods than ours, however, few have found a reduction in IPV and some have shown improvement in other IPV-related outcomes.34 A cluster randomized counseling intervention conducted at family planning clinics found a 71% decrease in the odds of pregnancy coercion.35 A quasi-experimental study of advocacy based in primary care clinics found an advocacy-based intervention was associated with significant reductions in IPV severity scores (decrease in scores on the Danger Assessment and the Women's Experience with Battering) and a reduction in depression and suicidal ideation compared with participants at control clinics.36 However, no studies have rigorously monitored adherence to a model or protocol that would allow determination of what components of the intervention were associated with better outcomes.
Recently, the Institute of Medicine37 and the US Preventive Services Task Force38 both recommended counseling of all women of child-bearing age as an evidence-based preventative service and this has now been codified into the Affordable Care Act as one of the essential health benefits that should be provided to all women without cost sharing.39 These recommendations are largely based on a randomized clinical trial of an integrated psychosocial and IPV advocacy intervention that took place throughout prenatal and postpartum care.40 However, no high-quality studies of brief interventions in acute care settings have reported improved outcomes for IPV-involved women. More work is needed to determine what works for whom, at what dose or intensity, and in what clinical settings.
A number of limitations must be considered when interpreting the results of our study. It was conducted in 2 affiliated urban EDs serving a predominately urban black community. By design, women with only IPV or only risky drinking were ineligible, so we do not know if a motivational intervention would be effective in women with only 1 of the targeted risk factors. Only half of eligible women consented to the yearlong study and those who enrolled had very high rates of psychosocial and mental health comorbidity.
At 1 year, we had 29% loss to follow-up, although there was no differential loss by group or risk severity. Notably, the majority of participants were living in poverty and the prevalences were 43% for childhood sexual abuse, 40% for posttraumatic stress disorder, and 86%for depression, which may not be generalizable to other female drinkers in abusive relationships. These findings suggest that IPV does not occur independently of other risk factors.
Integrated interventions that address multiple risk factors in the context of violence exposure may require a more in-depth approach than can be feasibly provided in an ED setting. Although we included a no-contact control group, some concern for a Hawthorne effect remains because participants in this group were screened for eligibility and received a list of social service referrals. However, we did not find any evidence of assessment reactivity compared with the assessed control group and the very low rates of reported use of community-based services indicate that the referral information was not an important component of the overall decreases in IPV and drinking across all groups.
Conclusions
For women experiencing IPV and heavy drinking, the use of a brief motivational intervention in the ED compared with assessed and no-contact controls did not significantly reduce the days of heavy drinking or incidents of IPV. These findings do not support a brief motivational intervention in this setting.
Supplementary Material
Acknowledgments
Funding/Support: This project was funded by award R01-AA018705 from the National Institute on Alcohol Abuse and Alcoholism.
Role of the Funder/Sponsor: The National Institute on Alcohol Abuse and Alcoholism had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We acknowledge Theresa Moyers, PhD (University of New Mexico) who received compensation as our motivational interview consultant on the treatment manual and who led adherence monitoring and rating of all recorded interventions. We also acknowledge our research staff: Elizabeth Dailey, MSW, Kate Watson, MS, Katherine Carroll, MS, Julie Tennille, MSW, PhD, Casey Bohrman, MSW, Alyssa Goodin, MSW, Hannah Jones-Lewis, MSW, Megan Schutt, MSW, and Catherine Monsky, MSW (motivational interviewing therapists; all from the University of Pennsylvania); Cjloe Vinoya, BS, Salem Wolk Valentino, MS, Marissa Sherman, MSW, Erica Dobbins, MSW, Catherine Buttner, MSW, and Sheila Kelly, MPH (research assistants); Darryl Snead and Christopher Boedec (IT support); Therese Sammarco, MS, and Aleda Thompson, MS (statistical support); and William Baxt, MD, Jill Baren, MD, John Flamma, MD (University of Pennsylvania emergency department directors). We offer many thanks to our volunteer consultants: Sharon Wilsnack, PhD (University of North Dakota), Richard Gelles, PhD (University of Pennsylvania), Gail D'Onofrio, MD (Yale University), Catherine Kothari, PhD (Michigan State University), Melissa Dichter, PhD (University of Pennsylvania), and James Wiley, PhD (University of California–San Francisco). We also thank our volunteer data and safety monitoring board members: Catherine Cerulli, JD, PhD (University of Rochester), Lori Post, PhD (Yale University), and Linda Degutis, PhD (US Centers for Disease Control and Prevention). We also offer special thanks to the many emergency department staff members and all of the women who participated in this study.
Footnotes
Author Contributions: Drs Rhodes and Hanlon had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Rhodes, Rodgers, Sommers, Datner, Crits-Christoph.
Acquisition, analysis, or interpretation of data: Rhodes, Rodgers, Sommers, Hanlon, Chittams, Doyle, Datner.
Drafting of the manuscript: Rhodes, Rodgers, Sommers, Hanlon, Chittams, Doyle, Crits-Christoph.
Critical revision of the manuscript for important intellectual content: Rhodes, Sommers, Doyle, Datner.
Statistical analysis: Hanlon, Chittams, Crits-Christoph.
Obtained funding: Rhodes, Sommers, Crits-Christoph.
Administrative, technical, or material support: Rhodes, Rodgers, Doyle, Datner.
Study supervision: Rhodes, Rodgers, Doyle.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Sommers reported receiving book royalties from FA Davis. No other disclosures were reported.
References
- 1.Caetano R, Schafer J, Cunradi CB. Alcohol-related intimate partner violence among white, black, and Hispanic couples in the United States. Alcohol Res Health. 2001;25(1):58–65. [PMC free article] [PubMed] [Google Scholar]
- 2.Foran HM, O'Leary KD. Alcohol and intimate partner violence: a meta-analytic review. Clin Psychol Rev. 2008;28(7):1222–1234. doi: 10.1016/j.cpr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Black MM, Black MM, Basile K, et al. National Intimate Partner and Sexual Violence Survey 2010 summary report. http://www.cdc.gov/ViolencePrevention/pdf/NISVS_Report2010-a.pdf. Accessibility verified July 8, 2015.
- 4.Bonomi AE, Trabert B, Anderson ML, Kernic MA, Holt VL. Intimate partner violence and neighborhood income: a longitudinal analysis. Violence Against Women. 2014;20(1):42–58. doi: 10.1177/1077801213520580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke P, Chapman C, Hohman M, et al. Guiding as practice: motivational interviewing and trauma-informed work with survivors of intimate partner violence. Partner Abuse. 2010;1:92–104. [Google Scholar]
- 6.Saitz R. Clinical practice: unhealthy alcohol use. N EnglJ Med. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- 7.Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(suppl 3):S163–S175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- 8.Babor TF, McRee BG, Kassebaum PA, et al. Screening, Brief Intervention, and Referral to Treatment (SBIRT) Subst Abus. 2007;28(3):7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 9.Kaner EFS, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;(2):CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230(4):473–480. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choo EK, McGregor AJ, Mello MJ, Baird J. Gender, violence and brief interventions for alcohol in the emergency department. Drug Alcohol Depend. 2013;127(1-3):115–121. doi: 10.1016/j.drugalcdep.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Testa M, Hoffman JH, Leonard KE. Female intimate partner violence perpetration. Aggress Behav. 2011;37(4):362–373. doi: 10.1002/ab.20391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cascardi M, Langhinrichsen J, Vivian D. Marital aggression. Arch Intern Med. 1992;152(6):1178–1184. doi: 10.1001/archinte.152.6.1178. [DOI] [PubMed] [Google Scholar]
- 14.Kaysen D, Dillworth TM, Simpson T, et al. Domestic violence and alcohol use. Addict Behav. 2007;32(6):1272–1283. doi: 10.1016/j.addbeh.2006.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Øverup CS, DiBello AM, Brunson JA, et al. Drowning the pain. Addict Behav. 2015;41:152–161. doi: 10.1016/j.addbeh.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhodes KV, Rodgers M, Sommers M, et al. The Social Health Intervention Project (SHIP) BMC Emerg Med. 2014;14:10. doi: 10.1186/1471-227X-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62(6):806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- 18.Sommers MS, Lyons MS, Fargo JD, et al. Emergency department-based brief intervention to reduce risky driving and hazardous/harmful drinking in young adults. Alcohol Clin Exp Res. 2013;37(10):1753–1762. doi: 10.1111/acer.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D'Onofrio G, Degutis LC. Screening and brief intervention in the emergency department. Alcohol Res Health. 2004-2005;28(2):63–72. [PMC free article] [PubMed] [Google Scholar]
- 20.Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perez S, Johnson DM, Wright CV. The attenuating effect of empowerment on IPV-related PTSD symptoms in battered women living in domestic violence shelters. Violence Against Women. 2012;18(1):102–117. doi: 10.1177/1077801212437348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cerulli C. Research ethics in victimization studies. Violence Against Women. 2011;17(12):1529–1535. doi: 10.1177/1077801211436304. [DOI] [PubMed] [Google Scholar]
- 23.Wilsnack SC, Klassen AD, Schur BE, Wilsnack RW. Predicting onset and chronicity of women's problem drinking. Am J Public Health. 1991;81(3):305–318. doi: 10.2105/ajph.81.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moyers TB, Miller WR, Hendrickson SML. How does motivational interviewing work? J Consult Clin Psychol. 2005;73(4):590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- 25.Moyers T, Martin T. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1.1 (MITI 3.1.1) [Accessed July 13, 2015]; http://casaa.unm.edu/download/miti3_1.pdf.
- 26.Smith PH, Earp JA, DeVellis R. Measuring battering: development of the Women's Experience with Battering (WEB) Scale. Womens Health. 1995;1(4):273–288. [PubMed] [Google Scholar]
- 27.Campbell JC, Webster DW, Glass N. The Danger Assessment: validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence. 2009;24(4):653–674. doi: 10.1177/0886260508317180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT) Alcohol Clin Exp Res. 2002;26(2):272–279. [PubMed] [Google Scholar]
- 29.US Department of Health and Human Services; National Institutes of Health; National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician's guide. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessibility verified July 8, 2015.
- 30.Bush K, Kivlahan DR, McDonell MB, et al. The AUDIT alcohol consumption questions (AUDIT-C) Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 31.Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence Vict. 2004;19(5):507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- 32.Sobell L, Sobell M. Timeline Follow-Back: a technique for assessing self-reported ethanol consumption. In: Allen J, Litten RZ, editors. Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 33.Hegarty K, Fracgp, Bush R, Sheehan M. The Composite Abuse Scale. Violence Vict. 2005;20(5):529–547. [PubMed] [Google Scholar]
- 34.Bair-Merritt MH, Lewis-O'Connor A, Goel S, et al. Primary care-based interventions for intimate partner violence. Am J Prev Med. 2014;46(2):188–194. doi: 10.1016/j.amepre.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Miller E, Decker MR, McCauley HL, et al. A family planning clinic partner violence intervention to reduce risk associated with reproductive coercion. Contraception. 2011;83(3):274–280. doi: 10.1016/j.contraception.2010.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coker AL, Smith PH, Whitaker DJ, et al. Effect of an in-clinic IPV advocate intervention to increase help seeking, reduce violence, and improve well-being. Violence Against Women. 2012;18(1):118–131. doi: 10.1177/1077801212437908. [DOI] [PubMed] [Google Scholar]
- 37.Institute of Medicine. Clinical preventive services for women closing the gaps. [Accessed July 15, 2015]; http://iom.nationalacademies.org/∼/media/Files/Report%20Files/2011/Clinical-Preventive-Services-for-Women-Closing-the-Gaps/preventiveservicesforwomenreportbrief_updated2.pdf.
- 38.Nelson HD, Bougatsos C, Blazina I. Screening women for intimate partner violence and elderly and vulnerable adults for abuse: systematic review to update the 2004 US Preventive Services Task Force Recommendation. http://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=22675737&site=ehost-live. Accessibility verified July 16, 2015. [PubMed]
- 39.US Department of Health and Human Services. Health care providers' role in screening and counseling for interpersonal and domestic violence. http://womenshealth.gov/publications/our-publications/fact-sheet/cchw-ipv-factsheet-3-5-13-final.pdf. Accessibility verified July 8, 2015.
- 40.Kiely M, El-Mohandes AAE, El-Khorazaty MN, Blake SM, Gantz MG. An integrated intervention to reduce intimate partner violence in pregnancy: a randomized controlled trial. Obstet Gynecol. 2010;115(2 pt 1):273–283. doi: 10.1097/AOG.0b013e3181cbd482. published correction appears in Obstet Gynecol. 2011;117(5):1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.