Abstract
Objective
Few studies have examined the spectrum and trends of non-communicable diseases (NCDs) in inpatients in eastern coastal China, which is transforming from an industrial economy to a service-oriented economy and is the most economically developed region in the country. This study aimed to dynamically elucidate the spectrum and characteristics of severe NCDs in eastern coastal China by analysing patients’ longitudinal electronic health records (EHRs).
Setting
To monitor the spectrum of NCDs dynamically, we extracted the EHR data from 12 general tertiary hospitals in eastern coastal China from 2003 to 2014. The rankings of and trends in the proportions of different NCDs presented by inpatients in different gender and age groups were calculated and analysed.
Participants
We obtained a total sample of 1 907 484 inpatients with NCDs from 2003 to 2014, 50.05% of whom were men and 81.53% were aged 50 years or older.
Results
There was an increase in the number of total NCD inpatients in eastern coastal China from 2003 to 2014. However, the proportion of chronic respiratory diseases and cancer inpatients decreased over the 12-year period. Compared with men, women displayed a significant increase in the proportion of mental and behavioural disorders (p<0.001) over time. Additionally, digestive diseases and sensory organ diseases significantly decreased among men, but not women. The older group accounted for a larger and growing proportion of the NCD inpatients, and the most common conditions in this group were cerebral infarctions, coronary heart disease and hypertension. In addition, the proportion of 21-year-old to 50-year-old inpatients with diabetes, blood diseases or endocrine diseases skyrocketed from 2003 to 2014 (p<0.001).
Conclusions
The burden of inpatients’ NCDs increased rapidly, particularly among women and younger people. The NCD spectrum observed in eastern coastal China is a good source of evidence for developing prevention guides for regions experiencing transition.
Keywords: non-communicable diseases, electronic health record, eastern coastal China, health policy
Strengths and limitations of this study.
The concept of using longitudinal electronic health records to document the proportion of non-communicable disease (NCD) admissions in eastern coastal China hospitals can provide a reasonably simple and precise method of examining NCD trends over time.
This evidence provides a good foundation for the development of NCD prevention guides or policies for similar developing regions that are undergoing or will undergo an economic transformation.
The generalisability and reliability of the findings of this study are a concern, and more hospitals from other parts of China should be included in future studies to make a persuasive comparison.
Introduction
In recent years, an epidemiological shift in morbidity and mortality from infectious diseases and malnutrition to non-communicable diseases (NCDs) has occurred in many countries, including China.1–3 NCDs have become the major causes of death in China and globally. According to the 2012 WHO data repository, 87% of deaths in China were associated with NCDs.1 The Global Burden of Disease Study (GBD) revealed that of the 8.3 million deaths in China in 2010, 7.0 million resulted from NCDs.3 Stroke, ischaemic heart disease, cancers and chronic obstructive pulmonary disease are now the leading causes of premature death in China, and the burden of these diseases is substantial.4
Previous research on the epidemiological patterns of NCDs in China has primarily focused on the entire nation or cross-sectional studies of specific regions.1–6 However, both the WHO and the GBD have acknowledged that a national analysis conducted in a country as large and diverse as China can mask substantial variations in key outcomes.3 5 In addition, few studies have examined the NCD spectrum in inpatients, which can reflect the severe state of NCDs. In this study, we conducted a longitudinal study of NCD patterns in five provinces in eastern coastal China: Shandong, Jiangsu, Zhejiang, Shanghai and Guangdong provinces. Geographically speaking, these provinces are located in the three most productive and dynamic regions of China: the Bohai Sea, the Yangtze River Delta and the Pearl River Delta. The gross regional domestic product in these five provinces accounts for approximately half that of the 32 provinces/autonomous regions/municipalities in China. These provinces’ gross domestic product (GDP) per capita far exceeded the average value in China from 2005 to 20147 and was similar to the GDP of other developed countries in Asia. Moreover, since the 2000s, this region has experienced dramatic changes in both the economic and health sectors.8 According to the Health Statistics Yearbook, in 2015, the average life expectancy in eastern coastal China was around 78 years old, which is greater than the national average of approximately 76 years old.7 Due to the rapid urbanisation, economic development and population ageing in eastern coastal China, NCDs and disabilities are becoming more prevalent,1 3 and the spectrum of inpatients' diseases in this area is speculated to largely differ from that in other regions of China. More specific guidelines for preventing and curing NCDs that are tailored to the disease patterns observed in eastern coastal China must be developed.
In exploring disease patterns, particularly in longitudinal studies based on a large sample, secondhand data may be regarded as a good source. In particular, data from hospitals’ electronic health record (EHR) systems have unique advantages. For instance, Upshur et al applied time series methods to a population-based retrospective cohort for the 52 most common causes of hospital admissions in the province of Ontario from 1988 to 2001 and showed that hospital admissions displayed systematic patterns that are understandable, predictable and reasonably accurate.9 Using data from the admission and discharge/death register, Sani et al10 conducted a 3-year review of mortality patterns. Their result supported the emerging trend of a combined burden of communicable diseases and NCDs. In China, disease surveillance is conducted by the National Disease Surveillance Points System, which was founded in 1978; however, this system reports primarily on communicable diseases and reports on only a small subset of NCDs, such as cancer.11 12 Given these factors, the current study used the hospital-based EHR system as a data source. This relatively new database compiles clinical information from a large number of patients in a computationally accessible form. The EHR system provides us with a unique opportunity to elucidate the relatively severe NCD epidemiology and includes a diverse array of NCDs.13
The aim of this study was to dynamically elucidate the spectrum and characteristics of severe NCDs in eastern coastal China by analysing hospitals’ longitudinal EHR data. The results can provide insight into the aetiology of NCDs and aid in the development of evidence-based clinical guidelines for preventing and curing NCDs. In addition, the distribution of NCDs in eastern coastal China can inform the development of clinical guidelines for NCDs in other regions or countries in transition.
Methods
Study design and data collection
Longitudinal data (2003–2014) on NCDs were extracted from the EHR systems of 12 general tertiary hospitals in Shandong (two hospitals), Jiangsu (two hospitals), Zhejiang (two hospitals), Shanghai (three hospitals) and Guangdong provinces (three hospitals).
A multistage sample was obtained. To obtain a representative sample, when choosing the sites, we first selected three cities that represented high, middle and low socioeconomic statuses, as defined by GDP level, in each of the five provinces. Second, in each city, we selected the largest general tertiary hospital, resulting in 15 sampled hospitals. However, we did not obtain consent from three tertiary hospitals in some cities in Shandong, Jiangsu and Zhejiang provinces due to political reasons regarding EHR data collection. In China, EHR data are not openly available but can be obtained from consenting hospitals with the help of health authorities. However, for several reasons, the health authorities cannot support us in the future. Thus, 12 general tertiary hospitals were included in the study. In this study, one hospital in Shandong Province in the low-socioeconomic group, one hospital in Jiangsu Province in the middle socioeconomic group and one hospital in Zhejiang Province in the high group were missing from the dataset. However, due to the distribution of the missing hospitals, it was thought that lack of participation of these hospitals would not influence the final results. In most large cities in China, EHRs have used a uniform version composed of two parts since 2001. The first part contains the patients’ personal information, including their gender, age, identification card number, profession, address and so on. This information is usually provided by the patients or their family. The second part contains the inpatients’ hospitalisation information, including their diagnosis code, discharge status, pathologic diagnosis (if possible), operation code (if possible) and so on. This information is provided by the patient’s physician, which ensures its reliability. In terms of the diagnosis code, each inpatient is coded with an ICD-9 disease code by their physician. In addition, the GBD has well defined categories for NCDs. Therefore, we extracted the inpatients’ NCDs using their ICD-9 codes and classified them into different categories.
We selected tertiary hospitals for this study. In China, hospitals are classified into three categories according to their major functions. Although community institutions are intended to serve as gatekeepers, a patient’s freedom to select medical facilities and doctors is not restricted by policies or health insurance coverage. Consequently, patients with acute or chronic diseases frequently visit the higher tier, more sophisticated or specialised and more expensive hospitals rather than community health centres, and many of the community health centres do not have hospital beds. In addition, their EHR systems are defective and incomplete, limiting the use of the information they contain.14 Typically, the largest tertiary hospitals see most of the patients discharged in their cities.
Study subjects
In this study, information on inpatients with NCDs was extracted from the 2003–2014 hospital EHR data of each hospital, and only individuals who had been admitted to these hospitals during this period were included. We chose 2003 as the starting point because the first EHR system was formally launched in these hospitals in that year. In our study, the EHR systems of the tertiary hospitals include the admission information of patients who received their first diagnosis of an NCD between 2003 and 2014. We excluded any duplicated patients by searching and analysing their identification card number in the EHRs. In addition, because these hospitals may also attract patients from other districts or provinces, the inclusion criteria stipulated that participants must have a fixed address in the relevant region, regardless of whether they were registered or non-registered residents. After excluding non-residents, NCD information for a total of 1 907 484 inpatients was stripped of identifying information and extracted from the hospitals’ EHR systems. These patients were admitted to a variety of hospital divisions, and according to the ICD-9 and GBD NCD classification, we extracted the NCD patients from all of the inpatients and classified them into various disease groups based on their first-list diagnosis. The final dataset included the residents’ basic demographic information (gender and age) and the presence of chronic diseases (disease system/category, disorder and year of admission). Because there was no significant difference in disease spectrum between regions with high, middle and low socioeconomic status within eastern coastal China, we did not include region as a factor.
Statistical analysis
All data were analysed by using SAS Software V.9.20. Basic descriptive statistics were used to analyse the inpatients’ personal characteristics (gender, age and year of admission). The NCD systems and the most common disorders within each disease system were ranked according to their relative proportions. The Cochran-Armitage χ2 test was then used to examine significant increases or decreases in the proportions of NCDs in disease systems across different gender and age groups between 2003 and 2014.
Ethics statement
All research activities were conducted with integrity according to generally accepted ethical principles and were approved by the ethics committees of Tongji University (ref: LL-2016-ZRKX-017). This study presented minimal risk of harm to its subjects, and the data were collected anonymously. None of the inpatients’ personal information included in the database was available to individuals outside of the research team.
Results
Description of the personal characteristics of inpatients with NCDs
The personal characteristics of the studied population are summarised in table 1. This population included 1 907 484 inpatients with NCDs, 50.05% of whom were men. Most of these patients were aged 50 years or older (81.53%). Furthermore, the number of inpatients with NCDs increased from 2003 to 2014.
Table 1.
Demographic characteristics of inpatients with non-communicable diseases
| Variable | Classification | n | % |
| Gender | Male | 954 612 | 50.05 |
| Female | 952 872 | 49.95 | |
| Age (years) | 0–10 | 1008 | 0.05 |
| 11–20 | 14 688 | 0.77 | |
| 21–30 | 47 484 | 2.49 | |
| 31–40 | 70 164 | 3.68 | |
| 41–50 | 219 060 | 11.48 | |
| 51–60 | 320 172 | 16.79 | |
| 61–70 | 268 176 | 14.06 | |
| 71–80 | 523 452 | 27.44 | |
| >80 | 443 280 | 23.24 | |
| Year of admission | 2003 | 110 796 | 5.81 |
| 2004 | 126 744 | 6.64 | |
| 2005 | 127 704 | 6.69 | |
| 2006 | 135 972 | 7.13 | |
| 2007 | 141 780 | 7.43 | |
| 2008 | 145 728 | 7.64 | |
| 2009 | 155 220 | 8.14 | |
| 2010 | 157 500 | 8.26 | |
| 2011 | 171 060 | 8.97 | |
| 2012 | 191 004 | 10.01 | |
| 2013 | 209 100 | 10.96 | |
| 2014 | 234 876 | 12.31 | |
| Total | 1 907 484 | 100.00 |
Ranking of the disorders in all NCD categories within gender and age groups
The ranks and proportions of all NCDs for each gender group are presented in table 2. Among men, each of the five most common disorders represented more than 4.0% of the total NCDs from 2003 to 2014. The three most frequently occurring disorders among male inpatients were cerebral infarction (12.61%), coronary heart disease (6.94%) and hypertension (6.05%). Similarly, those for women showed that cerebral infarction (9.63%) occurred most frequently. However, hypertension (6.84%) and uterine fibroids (4.15%) were the second and third most frequently occurring NCDs among women, respectively.
Table 2.
Ranking of the most common non-communicable diseases by group
| Variable | First disease | n (%) | Second disease | n (%) | Third disease | n (%) | Fourth disease | n (%) | Fifth disease | n (%) |
| Gender | ||||||||||
| Male | Cerebral infarction | 120 396 (12.61) | Coronary heart disease | 66 216 (6.94) | Hypertension | 57 708 (6.05) | Chronic obstructive pulmonary disease | 53 904 (5.65) | Chronic bronchitis | 45 252 (4.74) |
| Female | Cerebral infarction | 91 776 (9.63) | Hypertension | 65 136 (6.84) | Uterine fibroid | 39 564 (4.15) | Coronary heart disease | 31 188 (3.27) | Chronic bronchitis | 25 776 (2.71) |
| Age (years) | ||||||||||
| 0–10 | Chronic tonsillitis | 264 (16.19) | Redundant prepuce | 144 (14.29) | Adenoid vegetation | 72 (7.14) | Adenoidal hypertrophy | 48 (4.76) | Tonsil hypertrophy | 24 (2.38) |
| 11–20 | Redundant prepuce | 2064 (14.05) | Benign neoplasm of breast | 996 (6.78) | Spontaneous pneumothorax | 648 (4.41) | Chronic tonsillitis | 552 (3.76) | Respiratory failure | 444 (3.02) |
| 21–30 | Redundant prepuce | 4704 (9.91) | Benign neoplasm of breast | 2448 (7.51) | Ovarian cyst | 3564 (5.16) | Ureteral calculi | 1632 (3.44) | Chronic tonsillitis | 1032 (2.17) |
| 31–40 | Uterine fibroid | 5484 (7.82) | Ovarian cyst | 3156 (4.50) | Endometrial polyp | 2844 (4.05) | Ureteral calculi | 2556 (3.64) | Hyperplasia of mammary glands | 2268 (3.23) |
| 41–50 | Uterine fibroid | 25 644 (11.71) | Endometrial hyperplasia | 9408 (4.29) | Hyperplasia of mammary glands | 8052 (3.68) | Endometrial polyp | 7404 (3.38) | Ureteral calculi | 5640 (2.57) |
| 51–60 | Cerebral infarction | 23 124 (7.22) | Coronary heart disease | 14 016 (4.38) | Hypertension | 12 144 (3.79) | Ureteral calculi | 8364 (2.61) | Cerebral haemorrhage | 6636 (2.07) |
| 61–70 | Cerebral infarction | 29 508 (11.00) | Coronary heart disease | 14 016 (6.30) | Hypertension | 13 668 (5.10) | Vertebrobasilar insufficiency | 6480 (2.42) | Diabetes | 5640 (2.10) |
| 71–80 | Cerebral infarction | 75 972 (14.51) | Hypertension | 45 612 (8.71) | Coronary heart disease | 38 808 (7.41) | Chronic bronchitis | 30 720 (5.87) | Chronic obstructive pulmonary disease | 25 536 (4.88) |
| >80 | Cerebral infarction | 46 560 (17.58) | Hypertension | 31 488 (10.50) | Coronary heart disease | 77 928 (8.51) | Chronic obstructive pulmonary disease | 36 216 (8.17) | Chronic bronchitis | 37 728 (7.10) |
Table 2 also shows the ranks of the most frequently occurring disorders across age groups. The older group (>41 years of age) accounted for a larger proportion of NCD inpatients, and the most common conditions in this group were cerebral infarction, coronary heart disease and hypertension. In the 11-year-old to 50-year-old group, urogenital diseases, endocrine diseases and neoplasms including redundant prepuce, benign neoplasm of the breast and endometrial hyperplasia occurred frequently in men and women. In addition, hypertension, chronic obstructive pulmonary disease and diabetes were more common among the elderly than among individuals in the other age groups.
Distribution of NCDs across the different groups from 2003 to 2014
Table 3 shows the changes in the proportions of the 12 NCD categories from 2003 to 2014. A significant decrease in the occurrence of cancer (Z=−20.525, p<0.001), other neoplasms (Z=−20.525, p<0.001), chronic respiratory diseases (Z=−18.290, p<0.001), urogenital diseases (Z=−5.329, p<0.001) and sensory organ diseases (Z=−2.403, p=0.008) was found. In contrast, the proportions of other NCDs increased to various extents over the 12-year period. Notably, the proportion of patients with diabetes and blood and endocrine diseases increased approximately fourfold (from 1.36% to 6.74%).
Table 3.
Distribution of non-communicable diseases from 2003 to 2014 in the total sample (%)
| Disorder | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||
| n =110 796 |
n =126 744 |
n =127 704 |
n =135 972 |
n =141 780 |
n =145 728 |
n =155 220 |
n =157 500 |
n =171 060 |
n =191 004 |
n =209 100 |
n =234 876 |
Z | p-Value | Trend | |
| Cancer | 11.57 | 10.16 | 8.15 | 9.33 | 8.37 | 8.28 | 7.24 | 7.18 | 7.19 | 7.80 | 6.12 | 5.78 | −20.525 | <0.001 | ↓↓↓ |
| Other neoplasms | 6.63 | 8.05 | 7.43 | 7.41 | 5.58 | 4.55 | 5.54 | 4.45 | 4.67 | 4.55 | 4.36 | 4.01 | −20.527 | <0.001 | ↓↓↓ |
| Cardiovascular and circulatory diseases | 28.30 | 29.38 | 29.18 | 29.52 | 31.43 | 33.33 | 34.68 | 36.21 | 35.64 | 35.65 | 34.87 | 34.60 | 19.861 | <0.001 | ↑↑↑ |
| Chronic respiratory diseases | 13.43 | 13.46 | 13.85 | 12.98 | 13.50 | 12.85 | 12.52 | 12.45 | 11.27 | 10.89 | 9.37 | 9.40 | −18.290 | <0.001 | ↓↓↓ |
| Diabetes and blood and endocrine diseases | 1.36 | 1.43 | 1.25 | 1.26 | 1.44 | 1.46 | 1.35 | 1.75 | 1.55 | 3.67 | 6.47 | 6.74 | 41.268 | <0.001 | ↑↑↑ |
| Digestive diseases | 10.54 | 11.57 | 10.98 | 11.24 | 9.58 | 10.56 | 10.00 | 10.81 | 10.12 | 9.67 | 10.00 | 10.98 | −2.757 | 0.003 | ↓↓ |
| Mental and behavioural disorders | 0.17 | 0.08 | 0.23 | 0.19 | 0.19 | 0.13 | 0.26 | 0.25 | 0.16 | 0.12 | 0.36 | 0.25 | 3.130 | 0.001 | ↑↑ |
| Musculoskeletal disorders | 5.44 | 4.74 | 4.85 | 4.64 | 5.18 | 4.48 | 4.58 | 3.86 | 4.67 | 4.54 | 5.80 | 6.23 | 4.668 | <0.001 | ↑↑↑ |
| Urogenital diseases | 14.97 | 13.24 | 15.95 | 14.93 | 15.68 | 14.65 | 13.29 | 13.12 | 15.34 | 14.81 | 13.83 | 12.72 | −5.329 | <0.001 | ↓↓↓ |
| Neurological disorders | 2.25 | 3.78 | 4.35 | 3.96 | 4.58 | 5.34 | 5.33 | 4.97 | 4.83 | 3.49 | 4.13 | 4.36 | 3.915 | <0.001 | ↑↑↑ |
| Sensory organ diseases | 4.14 | 3.20 | 2.69 | 3.15 | 3.50 | 2.97 | 3.64 | 3.18 | 2.84 | 3.26 | 3.02 | 3.15 | −2.403 | 0.008 | ↓↓ |
| Congenital anomalies | 0.40 | 0.44 | 0.28 | 0.38 | 0.37 | 0.26 | 0.49 | 0.41 | 0.32 | 0.28 | 0.60 | 0.63 | 3.750 | <0.001 | ↑↑↑ |
| Skin and subcutaneous disease | 0.80 | 0.47 | 0.82 | 0.99 | 0.59 | 1.14 | 1.06 | 1.35 | 1.38 | 1.26 | 1.08 | 1.15 | 7.294 | <0.001 | ↑↑↑ |
↓↓, p<0.01, negative trend; ↓↓↓, p<0.001, negative trend; ↑↑, p<0.01, positive trend; ↑↑↑, p<0.001, positive trend.
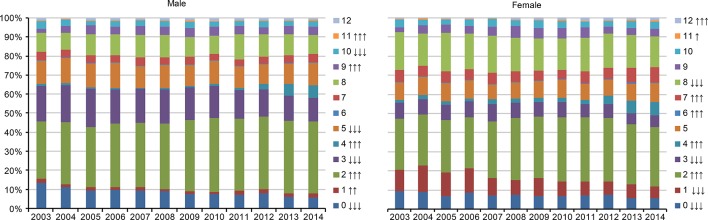
As shown in figure 1, the 12-year NCD percentages recorded in the hospitals varied widely by gender. The percentage of both men and women who were diagnosed with diabetes or blood and endocrine diseases increased substantially. We found a significant increase in mental and behavioural disorders (Z=5.130, p<0.001), and musculoskeletal disorders (Z=6.896, p<0.001) among women but no significant changes among men. Also, it is worth noting that the percentage of men who were diagnosed with digestive diseases (Z=−4.284, p<0.001) and sensory organ diseases (Z=−3.342, p<0.001) reduced significantly from 2003 to 2014, but there was no significant change for women. In addition, although the proportion of cancer and other neoplasms decreased in women, this decrease was less pronounced than that found in men.
Figure 1.
Distribution of non-communicable diseases by gender. 0: cancer, 1: other neoplasms, 2: cardiovascular and circulatory diseases, 3: chronic respiratory diseases, 4: diabetes and blood and endocrine diseases, 5: digestive diseases, 6: mental and behavioural disorders, 7: musculoskeletal disorders, 8: urogenital diseases, 9: neurological disorders, 10: sensory organ diseases, 11: congenital anomalies, 12: skin and subcutaneous diseases. ↓: p<0.05, negative trend; ↓↓: p<0.01, negative trend; ↓↓↓: p<0.001, negative trend. ↑: p<0.05, positive trend; ↑↑: p<0.01, positive trend; ↑↑↑: p<0.001, positive trend.
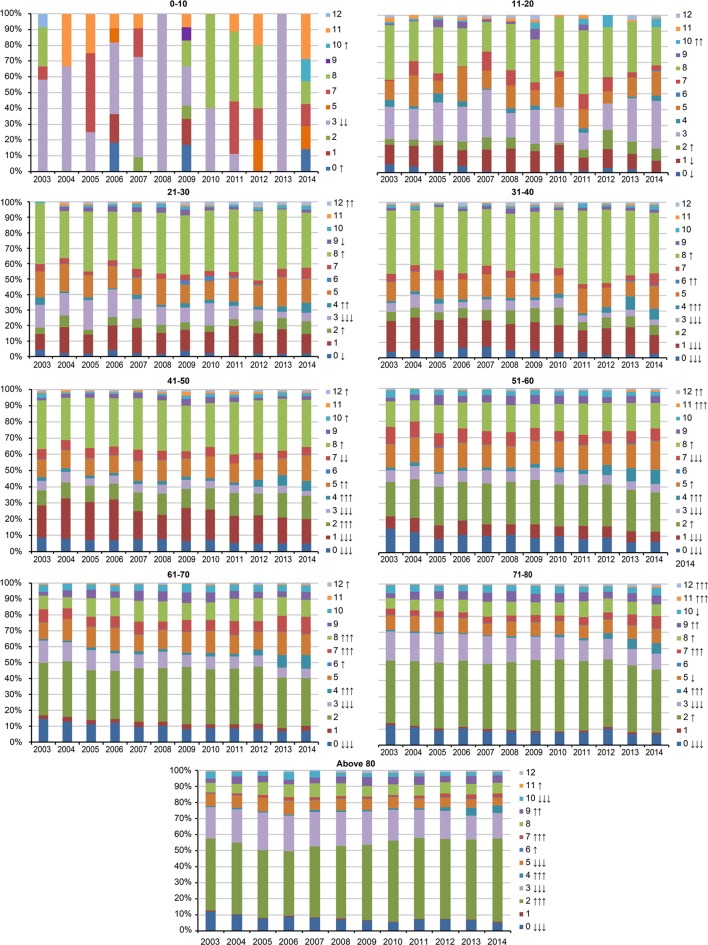
Changes in NCDs proportions across age groups were also examined (figure 2). NCDs were relatively rare among patients aged 10 years or younger, but chronic respiratory diseases occurred most frequently in this group. For 11-year-old to 20-year-old subjects, sensory organ diseases (Z=3.304, p<0.001) and cardiovascular and circulatory diseases (Z=2.090, p=0.018) occurred more frequently over time. We noted the proportions of patients with diabetes or blood and endocrine diseases increased in these two groups and in the below 30-year-old group. For the 41-year-old to 50-year-old group, the number of patients diagnosed with cancer decreased significantly but the proportions of patients with cardiovascular, circulatory (Z=7.918, p<0.001) and digestive diseases (Z=3.086, p<0.01) increased to a greater extent than in the younger population. In the ≥50-year-old group, the proportion of patients with diabetes or blood and endocrine diseases increased substantially (p<0.001).
Figure 2.
Distribution of non-communicable diseases by age. 0: cancer, 1: other neoplasms, 2: cardiovascular and circulatory diseases, 3: chronic respiratory diseases, 4: diabetes and blood and endocrine diseases, 5: digestive diseases, 6: mental and behavioural disorders, 7: musculoskeletal disorders, 8: urogenital diseases, 9: neurological disorders, 10: sensory organ diseases, 11: congenital anomalies, 12: skin and subcutaneous diseases. ↓: p<0.05, negative trend; ↓↓: p<0.01, negative trend; ↓↓↓: p<0.001, negative trend. ↑: p<0.05, positive trend; ↑↑: p<0.01, positive trend; ↑↑↑: p<0.001, positive trend.
Discussion
By analysing the EHR information of inpatients with NCDs at 12 hospitals in eastern coastal China, our research team was able to elucidate the severe NCD patterns in a relatively unbiased fashion and to confirm that NCDs displayed regional heterogeneity to some extent. The increase in the number of NCD inpatients in eastern coastal China from 2003 to 2014 may be due to several reasons. First, owning to improvements in economics, health insurance and convenient transportation in China, even people with minor diseases may go to larger hospitals because they are equipped with better devices and doctors and do not adhere to strict referral policies. Second, the increase in the number of severe NCD patients appears to mainly result from the higher pressure, lack of exercise and increased air pollution, among other factors in rapidly developed cities,14 15 which is consistent with the findings of Allen et al16 who, in a systematic review, showed that NCD behavioural risk factors is well established in high-income countries. For example, high-socioeconomic groups were found to be less physically active and to consume more fats, salt and processed food than low-socioeconomic status individuals.16
In order of ranks, cardiovascular and circulatory diseases, urogenital diseases, chronic respiratory diseases and digestive diseases were the most common NCDs in this region. In eastern coastal China, severe cardiovascular and circulatory diseases may occur more frequently because of the greater degree of urbanisation and greater proportion of ageing population in the region.2 3 Goryakin et al17 studied the contribution of urbanisation to NCDs in 173 countries and found that when shifting from rural to urban areas, the average body mass index, total cholesterol level and systolic blood pressure, increased,17 demonstrating that high urbanisation increases the occurrence of cardiovascular and circulatory diseases, which is in consistent with this study. In addition, the frequency of urogenital diseases (second) and digestive diseases (fourth) in this region is potentially because of the more rapid pace of modern life, more sedentary lifestyle and longer working hours. In our search of existing studies on inpatients with NCDs, we rarely found this spectrum at the top of the list in other regions.18 However, interestingly, this study revealed that the proportion of chronic respiratory diseases and cancer inpatients decreased over the 12-year period, in stark contrast to the changes in the incidence observed throughout China.19 20 Often, previous studies have concluded that the incidence of respiratory diseases is increasing, likely due to ambient air pollution and tobacco use, resulting in tremendous threats to respiratory health.3 21 This difference may be a result of the data because the reported incidence also includes mild respiratory diseases. However, the opposite trend found in inpatients in eastern coastal China may have also resulted from this region’s transition from a heavy industrial district to a technologically focused area, which has been associated with a substantial reduction in environmental pollution. Moreover, regional public health media campaigns have focused on cancer prevention and the regional government has promoted early screening and the treatment of major cancers since the 2000s, particularly in these developed areas in China where the government can invest more money into public health activities,22 which likely explains the reduced proportion of cancer patients. However, particulate matter PM2.5 air pollution, household pollution, tobacco use, residents’ insufficient knowledge of NCD prevention, and so on, remain persistent risk factors in eastern coastal China and deserve considerable attention.23 24
Concerning the distribution of NCDs among the different age groups, we found that the older age group accounted for the largest proportion of individuals with NCDs, with cerebral infarction, coronary heart disease and hypertension being the most common conditions. This result is consistent with the epidemiological features of NCDs25 26 and indicates that these NCDs represent a significant burden on the Chinese government. Interestingly, in addition to the nearly fourfold increase in the proportion of older patients suffering from NCDs such as diabetes or blood and endocrine diseases between 2003 and 2014, the proportion of individuals with these diseases between the ages of 30 and 50 also increased significantly. However, this result could have been due to suboptimal nutrient intake and the high level of psychological pressure on the young population in this fast-paced area, a relationship that warrants further attention.
Additionally, the observation that an increasing proportion of women exhibit severe mental and behavioural disorders may indicate that, currently, women in China are employed in the same fast-paced jobs or roles as men.27 Furthermore, women are expected to devote more effort to balancing family and work28 29 in developed areas or cities, which is undoubtedly challenging for them and may induce the onset of these diseases. These factors imply that specific risk factors for frequently occurring NCDs in different gender groups should be monitored in addition to the diseases or groups that are currently monitored and screened for due to their significant burden. Other frequently occurring NCD diseases and a wider population should also be targeted, such as the prevention and screening of digestive diseases in women or increased preventative measures for diabetes and blood, endocrine, cardiovascular and circulatory diseases among the younger and population. In addition, these observations call for an improvement and greater investment in the prevention and control of NCDs by community health institutions, which has lagged even in the economically well-developed eastern coastal regions of China as well as in China as a whole compared with western countries.30 For instance, community health institutions typically compete with hospitals to attract patients, and only public health physicians (different from general physicians) take the responsibility of providing health education and follow-up visits for NCD patients. According to a survey conducted at a representative community health institution in Shanghai, public health physicians accounted for only 7.94% of total health personnel and are therefore in great shortage. Undoubtedly, reducing the incidence of NCDs and improving national health are significant political and public issues for China.31
Limitations
In this study, there were several limitations. First, the sampled hospitals were the largest hospitals in eastern coastal cities. These cities were selected to increase the sample’s representativeness of eastern coastal China. However, the generalisability and reliability of the findings are a concern. Because the EHR included a large number of inpatients with NCDs, it was a precise data source for determining the status of and trends in the occurrence of different diseases. To reduce selection bias, more representative hospitals from each of the cities must be investigated. Second, because socioeconomic data were absent in the EHRs, we were unable to compare the differences in socioeconomic groups in this study. Third, because the period of data collection spanned a long time, there may be some bias related to disease diagnosis caused by changes in policy, as well as changes in the availability of new treatments or therapies. Such changes could have resulted in patients with a given condition in the past becoming more or less likely to be inpatients in the present day. Fourth, because few longitudinal studies examining the spectrum of NCDs among many hospitals’ inpatients have been conducted in other areas of China, it was difficult to compare the current findings regarding inpatients’ NCDs with those in other parts of China.
Conclusions
In summary, the spectrum of NCD inpatients from 12 hospitals exhibits the severe NCDs condition and spectrum in eastern coastal China to a certain extent. Specific NCDs rapidly increased in women and the younger population over the studied 12-year period, underscoring the importance of healthcare policies or guidelines for developing countries or regions such as China. However, due to the limited generalisability and reliability of this study, stronger support must be obtained through future studies on the spectrum of inpatients’ NCDs in eastern coastal China and other regions.
Supplementary Material
Acknowledgments
The authors appreciate the assistance of all the hospitals involved in this research project in collecting the data.
Footnotes
Contributors: Conceived and designed the experiments: DY, JS and ZW. Analysed the data: JS, HZ and YL. Contributed reagents/materials/analysis tools: YL, BZ, YP, BW and PS. Wrote the paper: DY and JS.
Funding: The design of this study was financially supported by the Shanghai Health Policy Program (2016HP043). Data collection, analysis and interpretation were funded as part of a Central University Special Funds for Scientific Research Project (1500219099), and the writing and revision of the manuscript was funded by the National Natural Science Foundation of China (71603182) and the Shanghai Health Bureau Program (201440344).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi:10.5061/dryad.6f1t7
References
- 1. World Health Organization. Non communicable diseases progress monitor 2015. 2015. http://apps.who.int/iris/bitstream/10665/184688/1/9789241509459_eng.pdf (accessed 1 Apr 2016).
- 2. Lim SS, Vos T, Flaxman AD, et al. . A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang G, Wang Y, Zeng Y, et al. . Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2013;381:1987–2015. 10.1016/S0140-6736(13)61097-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liu Y, Yang G, Zeng Y, et al. . Policy dialogue on China’s changing burden of disease. Lancet 2013;381:1961–2. 10.1016/S0140-6736(13)61031-4 [DOI] [PubMed] [Google Scholar]
- 5. Fang P, Dong S, Xiao J, et al. . Regional inequality in health and its determinants: evidence from China. Health Policy 2010;94:14–25. 10.1016/j.healthpol.2009.08.002 [DOI] [PubMed] [Google Scholar]
- 6. Tang S, Meng Q, Chen L, et al. . Tackling the challenges to health equity in China. Lancet 2008;372:1493–501. 10.1016/S0140-6736(08)61364-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Bureau of Statistics of the People’s Republic of China. China Statistical Bullletin. 2015. http://www.stats.gov.cn/tjsj/tjgb/ndtjgb/ (accessed 1 Apr 2016).
- 8. Liu GF, Sun MP, Wang ZY, et al. . [Association analysis between urbanization and non-communicable diseases and health-related behavior]. Beijing Da Xue Xue Bao 2016;48:478–82. [PubMed] [Google Scholar]
- 9. Upshur RE, Moineddin R, Crighton E, et al. . Simplicity within complexity: seasonality and predictability of hospital admissions in the province of Ontario 1988-2001, a population-based analysis. BMC Health Serv Res 2005;5:13 10.1186/1472-6963-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sani MU, Mohammed AZ, Bapp A, et al. . A three-year review of mortality patterns in the medical wards of Aminu Kano Teaching Hospital, Kano, Nigeria. Niger Postgrad Med J 2007;14:347–51. [PubMed] [Google Scholar]
- 11. Duan L, Deng X, Wang Y, et al. . The National Injury Surveillance System in China: a six-year review. Injury 2015;46:572–9. 10.1016/j.injury.2014.12.013 [DOI] [PubMed] [Google Scholar]
- 12. Zhu M, Ruan W, Fei SJ, et al. . Approaches to the evaluation of malaria elimination at county level: case study in the Yangtze River Delta region. Adv Parasitol 2014;86:135–82. 10.1016/B978-0-12-800869-0.00006-8 [DOI] [PubMed] [Google Scholar]
- 13. Melamed RD, Khiabanian H, Rabadan R. Data-driven discovery of seasonally linked diseases from an Electronic Health Records system. BMC Bioinformatics 2014;15(Suppl 6):S3 10.1186/1471-2105-15-S6-S3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang H, Huang X, Zhou Z, et al. . Determinants of initial utilization of community healthcare services among patients with major non-communicable chronic diseases in South China. PLoS One 2014;9:e116051 10.1371/journal.pone.0116051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhou L. Analysis of the chronic diseases components of inpatient in a hospital of Wuhan from 2008-2012. Med Soc 2014;10:23–5. [Google Scholar]
- 16. Allen L, Williams J, Townsend N, et al. . Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health 2017;5:e277–e289. 10.1016/S2214-109X(17)30058-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goryakin Y, Rocco L, Suhrcke M. The contribution of urbanization to non-communicable diseases: evidence from 173 countries from 1980 to 2008. Econ Hum Biol 2017;26:151–63. 10.1016/j.ehb.2017.03.004 [DOI] [PubMed] [Google Scholar]
- 18. Zhu YJ, Yao YH, Xue SS, et al. . Analysis on condition of chronic diseases, distribution of disease spectrum and main risk factors of diseases of elderly in Jilin Province. J Jilin Univ (Med Ed) 2013;6:1275–81. [Google Scholar]
- 19. World Health Organization. Global health observatory data repository. 2016. http://apps.who.int/gho/data/node.main.A865?lang=en (accessed 3 Apr 2016).
- 20. Oyebode O, Pape UJ, Laverty AA, et al. . Rural, urban and migrant differences in non-communicable disease risk-factors in middle income countries: a cross-sectional study of WHO-SAGE data. PLoS One 2015;10:e0122747 10.1371/journal.pone.0122747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tao Y, Mi S, Zhou S, et al. . Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ Pollut 2014;185:196–201. 10.1016/j.envpol.2013.10.035 [DOI] [PubMed] [Google Scholar]
- 22. Dl L, Zheng Y, Lu W. Practice and probe into prevention and control for high incidence cancers in Shanghai. China Cancer 2010;19:80–5. [Google Scholar]
- 23. Zg T. The coordination of industrial growth with environment and resource. Econ Res J 2008;2:93–105. [Google Scholar]
- 24. Shanghai WF. China – study on global ageing and adult health, 2009/10. WAVE 2013. [Google Scholar]
- 25. Ding D, Zhong X, Lau JT, et al. . Behavioral medicine and prevention of non-communicable diseases in China: current challenges and future directions. Int J Behav Med 2014;21:584–9. 10.1007/s12529-014-9393-7 [DOI] [PubMed] [Google Scholar]
- 26. Zhai F, Wang H, Du S, et al. . Prospective study on nutrition transition in China. Nutr Rev 2009;67(Suppl 1):S56–S61. 10.1111/j.1753-4887.2009.00160.x [DOI] [PubMed] [Google Scholar]
- 27. Liu LN. Analysis on the overstrain women in the workforce in China. Reform & Opening 2013;1:33–4. [Google Scholar]
- 28. Yang H, He F, Wang T, et al. . Health-related lifestyle behaviors among male and female rural-to-urban migrant workers in Shanghai, China. PLoS One 2015;10:e0117946 10.1371/journal.pone.0117946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Du M, Prescott J, Kraft P, et al. . Physical activity, sedentary behavior, and leukocyte telomere length in women. Am J Epidemiol 2012;175:414–22. 10.1093/aje/kwr330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mathur R, Bhaskaran K, Edwards E, et al. . Population trends in the 10-year incidence and prevalence of diabetic retinopathy in the UK: a cohort study in the Clinical Practice Research Datalink 2004-2014. BMJ Open 2017;7:e014444 10.1136/bmjopen-2016-014444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhou XL, Kf W, Sun BH. Analysis on the current status and development strategies of public health physicians in community health institutions in Shanghai. Chin J Gen Pract 2012;10:1756–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.