Abstract
Living donor liver transplantation (LDLT) has been increasingly embraced around the world as an important strategy to address the shortage of deceased donor livers. The aim of this guideline, approved by the International Liver Transplantation Society (ILTS), is to provide a collection of expert opinions, consensus, and best practices surrounding LDLT. Recommendations were developed from an analysis of the National Library of Medicine living donor transplantation indexed literature using the Grading of Recommendations Assessment, Development and Evaluation methodology. Writing was guided by the ILTS Policy on the Development and Use of Practice Guidelines (www.ilts.org). Intended for use by physicians, these recommendations support specific approaches to the diagnostic, therapeutic, and preventive aspects of care of living donor liver transplant recipients.
Compared to cadaveric liver transplantation, live donor LT (LDLT) is challenged by ethical, medical and surgical considerations, many of which are still unresolved. The aim of this guideline is to provide a collection of expert opinions, consensus, and best practices surrounding LDLT.
PREAMBLE AND METHODS
Around the world, living donor liver transplantation (LDLT) has been increasingly embraced as an important strategy to address the shortage of deceased donor (DD) livers. However, compared with cadaveric liver transplantation, LDLT is challenged by ethical, medical and surgical considerations, many of which are still unresolved and understudied.
The aim of this guideline is to provide a collection of expert opinions, consensus, and best practices surrounding LDLT. With the leadership and guidance of the International Liver Transplantation Society (ILTS), this guideline will be updated regularly to accurately and effectively communicate newly gained experiences and advancements.
The following guideline has been approved by the ILTS and represents the position of the Society. Review of evidence was based on relevant clinical questions and outcomes of importance to patients, proposed by the ILTS-designated writing group chair and approved by the ILTS Guidelines Committee and Council. Acknowledged experts from around the world were recruited to address these questions after obtaining appropriate disclosures to exclude any conflict of interest. Recommendations were developed from analysis of National Library of Medicine indexed literature on “living donor liver transplantation” [Medline search] using Grading of Recommendations Assessment, Development and Evaluation methodology.1,2 Writing was guided by the ILTS Policy on the Development and Use of Practice Guidelines (www.ilts.org).
Drafts of a full-length version (>20 000 words) were freely accessible for review and comment on the ILTSEducation.org website from June 2014 and were presented for discussion at the ILTS Annual Congress the same year. Presentations were also posted online, and over 900 ILTS members and many more nonmembers were invited to comment until submission of an abridged version to Transplantation in December 2015. All comments were taken into account by the writing group chair. Formal external peer review was then undertaken by the journal, reviewers also having declared no conflict of interest. Final drafts were approved by the ILTS Council.
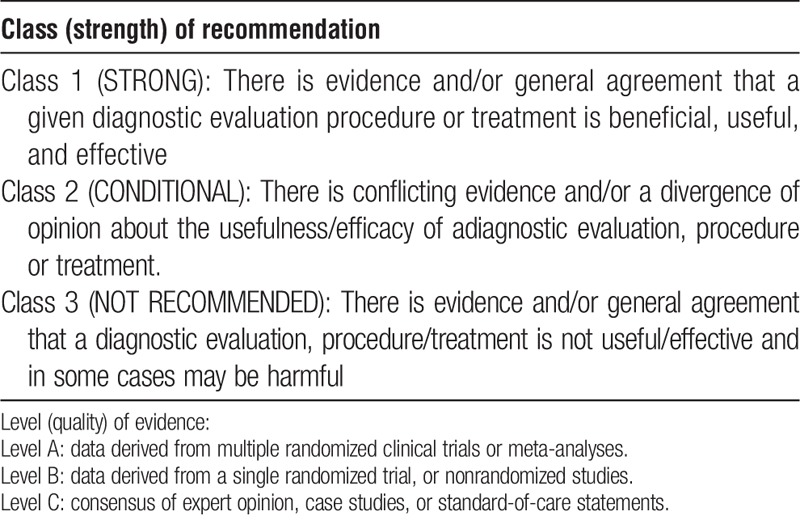
Recommendations have been based on information available at the time of final submission (March 2016). The lack of randomized controlled trials in this field to date is acknowledged and is reflected in the grading of evidence. Each recommendation (Table 1) has been classified as strong, conditional or not recommended,1,2 depending on quality of evidence, balance of benefit versus harm, importance to patients, and cost-effectiveness. The quality of supporting evidence was rated as high, moderate, or low (A, B, or C) according to Grading of Recommendations Assessment, Development and Evaluation criteria. Intended for use by physicians, these recommendations support specific approaches to the diagnostic, therapeutic, and preventive aspects of care. However, they do not necessarily represent standards of care and should be applied only according to the best judgment of the treating team after full consideration of the circumstances relating to an individual patient.
TABLE 1.
Evaluation
As for cadaveric liver transplantation, evaluation and selection of adult LDLT recipients should involve a multi-disciplinary team. An LDLT candidate should also qualify as a candidate for a deceased organ given the possibility of primary nonfunction and the need for immediate retransplantation. Specifically related to LDLT is the preoperative evaluation of recipient characteristics that could affect LDLT outcome. Preoperative work-up should aim to establish the degree of the recipient portal hypertension (some programs routinely perform indirect measurement of the portal venous pressure and gradient), the existence of portopulmonary hypertension (which, if severe, could affect the outflow of the graft) and the degree of immunological compatibility between donor and recipient (preoperative crossmatch).3-8 This information could not only help to select good candidate for LDLT but also the type of graft to use (right vs left lobe graft) as well as to implement strategies to optimize posttransplant outcomes (such as recipient desensitization in case of a positive cross match).4-6 Finally, the presence and extent of portal vein thrombosis should also be carefully assessed (see below).
Candidate selection in Asia differs quite significantly from candidate selection in Western countries. The root cause for this difference stems from the marked difference in deceased organ donation rates between the East and the West.
Candidate Selection: The Eastern and Western Perspectives
Compared with other region of the world, in Asia, there is a higher benefit and a stronger need for LDLT because of the critical shortage of DD organs. Except for mainland China, LDLT in Asia accounts for over 80% of all liver transplants compared with less than 5% in the United States and Europe.9 The most important differences in candidate selection between Eastern and Western countries involve high-urgency patients, patients with hepatocellular carcinoma (HCC) and challenging surgical situations.
High-Urgency Patients
In contrast to several initial reports from Western countries that have shown inferior outcome of LDLT in high-urgency situations, several studies in Asia have demonstrated excellent outcomes for LDLT in high-urgency situations.10-14 Coercion of donors and the possible increase of donor risks are among identified concerns with LDLT, especially in high urgency situations. Experienced liver transplant programs in Asia have addressed these concerns by developing protocols and logistics for fast tract evaluation of living donors (LDs), including, 24-hour radiology, endoscopy, clinical psychological assessment, and even legal support to assure the fulfillment of legal requirements.10-13 As a result, high-urgency patients with acute or acute-on-chronic liver failure are prime indications for LDLT in Asia. In western countries, LDLT is usually reserved to patients with a lower disease acuity, a practice supported by the A2ALL study.15,16 The National Institutes of Health funded consortium showed that LDLT is beneficial even at lower Model for End-Stage Liver Disease score by preventing liver transplant candidates from developing renal failure and malnutrition, key determinants for mortality on the waitlist and posttransplant complications. These findings are supported by another large national data base study showing that in more recent years (2012-2012) LDLT outcomes have improved dramatically. Furthermore, data showed that the benefit of LDLT extends to late posttransplant outcomes, going beyond the benefit of earlier transplantation.17
Hepatocellular Carcinoma
HCC comprises over one third of the indications for liver transplantation in Asia, as compared with 10% to 20% in the United States and Europe.9 With a higher demand for transplantation, yet a lower organ donation rate, these patients can rarely receive a DD liver graft in Asia. For these patients LDLT allows optimal timing of the transplant and plays a key role in reducing the dropout rate on the waiting list.18 As a result, many Asian centers have adopted extended HCC criteria19-22 for LDLT because a graft from an LD is a dedicated gift and is not subjected to any allocation system/criteria (such as the Milan criteria) to justify organ utilization. Consensus is lacking in the international liver transplant community on how far these criteria should be extended. Transplant centers must therefore balance donor risk with recipient benefit and determine a limit beyond which a transplant becomes futile and ethically unjustifiable.
Technical Challenges
Retransplantation, Budd-Chiari syndrome, and portal vein thrombosis especially with extension into the superior mesenteric vein had been regarded as contraindications for LDLT in most centers. In western countries, where there is a higher availability of DDs, the use of a whole liver graft avoids the technical challenges of LDLT. However, the increased experience and improved techniques that have been demonstrated in some transplant centers in Asia show that these technical hurdles can be overcome and are not absolute contraindications for LDLT.23
Recommendations
The availability of cadaveric liver grafts in different areas of the world affects LDLT recipient selection criteria. High-urgency LDLT represents a prime indication for LDLT in Asia and can be performed with acceptable outcomes (class 1, level B) whereas in western countries LDLT is usually reserved for patients with a lower disease acuity.
LDLT significantly reduces the dropout from the waiting list of patients with HCC (class 1, level B). Although patients with more advanced HCC beyond Milan criteria may benefit from LDLT (class 1, level B) there is no consensus on how far these criteria can be extended (class 2, level C).
Retransplantation, Budd-Chiari syndrome, and portal vein thrombosis are not absolute contraindications to LDLT in experienced LDLT centers (class 2, level B).
Hemodynamic and Size Considerations
The most common factor limiting LDLT is represented by small for size syndrome (SFSS). SFSS can be defined24 as functional impairment of a partial liver graft during the first postoperative week as evidenced by coagulopathy, cholestasis, encephalopathy and ascites after the exclusion of other causes (vascular, immunological, and so on). The etiology of SFSS is multifactorial and consist of graft and patient factors. Graft factor include size and parenchymal quality. Based on the existing literature, most of the LDLT transplant centers would consider as safe a graft greater than 40% of the recipient's standard liver volume25 or greater than 0.8% of the recipient's body weight.26 With improved experience, skills and better patient selection, the safety limit for minimum graft-weight-to-standard-liver-volume ratio can be reduced to 35%27 and to less than 0.8% of graft to recipient body weight. Importantly, the graft regeneration and size requirement has been shown to be higher when the donor is older than 50 years.16 Patient factors include the degree of portal hypertension and the overall clinical status. The severity of portal hypertension and the consequent graft hyperperfusion occurring after reperfusion have been object of intense animal and clinical research.28-32 Numerous studies have shown that modulation of portal vein pressure and flows are key in successful LDLT using small grafts. It is therefore important to carry out hemodynamic monitoring during surgery (intraoperative arterial and portal venous flow measurement, portal vein pressure measurement) for the identification and management of patients at risk of developing SFSS.33 If the portal pressure exceeds 20 mm Hg, portal inflow modulation can be achieved by performing splenic artery ligation,34,35 splenectomy,35,36 splenorenal shunting,37 hemiportocaval shunting,38,39 and mesocaval shunting.30 Various pharmacologic agents that may modulate portal flow and prevent SFSS have been tested in animal models but clinical studies are lacking. The importance of the outflow as a key factor to optimize graft function and prevent SFSS will be described in the following sections.
The degree of liver decompensation at the time of transplant has also been shown to affect graft and patient survival and should be kept into consideration when planning a LDLT with a small graft.16,40
Recommendations
Graft injury and dysfunction in SFSS is not only a reflection of the graft size but also related to graft quality and the degree of recipient portal hypertension causing graft hyperperfusion (class 1, level B).
Monitoring of the portal vein and hepatic artery hemodynamics are highly recommended for the early diagnosis, prevention and management of SFSS (class 1, level B).
Portal inflow modulation by splenic artery ligation/embolization or other portosystemic shunts is effective in the prevention and treatment of SFSS (class 1, level B).
The role of pharmacologic agents for the modulation of portal flow is unknown due to lack of clinical studies (class 2, level C).
Transplant Procedure
Left Lobe LDLT
Due to donor safety concerns and better understanding of SFSS, adult-to-adult left lobe LDLT has been increasingly utilized around the world.25,41-47 Considering the relatively small-sized graft volume, large hepatic venous outflow is essential to optimize graft function and avoid SFSS. Hepatic venous outflow augmentation can be achieved with a number of surgical techniques and should always be considered.48-50 When the left lobe with a caudate lobe graft is used, revascularization of the caudate lobe may contribute to full graft regeneration and help preventing SFSS.42,48,51,52 Regarding arterial reconstruction, it is still controversial whether the routine reconstruction of multiple hepatic arteries of LD graft should be performed.44,53 Special attention should be given to the bile duct division site to avoid sizable, separate caudate ducts from the left hepatic duct.42,54
Recommendations
In selected donor/recipient combinations left lobe adult-to-adult LDLT can be carried out successfully (class 1, level B).
Hepatic venous outflow augmentation is essential to optimize graft function and can be achieved with a number of surgical techniques (class 1, level B).
Caudate lobe inclusion and revascularization in left lobe graft LDLT may help preventing SFSS (class 2, level C).
There is no consensus whether reconstruction of multiple hepatic arteries of LD grafts should be considered on a case by case basis or represent a routine (class 2, level C).
Special attention should be given to the bile duct division site to avoid multiple bile duct anastomosis (class 1, level C).
Right LDLT
Because of its size, right liver LDLT is the graft most commonly used in adult LDLT.9,15 Nonetheless, even a right liver graft can be subject to the catastrophic consequences of SFSS.
As for the left lobe, optimal hepatic venous outflow is key for a successful outcome.55,56
The issue of whether or not to include the middle hepatic vein (MHV) in right lobe liver grafts remains controversial and has been partly addressed in the previously published ILTS guideline on Living Liver Donation.57 When the MHV is not included in the graft, it is advisable to preserve and reconstruct sizable (>5 mm) right inferior hepatic veins and segments 5 and 8 hepatic venous branches (V5, V8). Different reconstructive techniques can be used to achieve this goal.56,58-60 If the MHV is included in the graft, a venoplasty that converts the right hepatic vein and MHV to a triangular cuff61 will facilitate a single, direct venous anastomosis to the recipient inferior vena cava. It is important to obtain a wide cavotomy to ensure optimal outflow.
Because there is a 10% to 35% chance of a portal vein anomaly in a right liver graft, surgeons performing this type of transplants should be familiar with various portal vein reconstructions techniques.62-64 Operating microscope has been used successfully65 for complex arterial reconstruction in addition to loupe magnification.66,67 Duct-to-duct anastomosis is currently the preferred technique for biliary reconstruction54,68 except in cases when the recipient bile duct is not healthy. It is controversial whether the use of an external or internal biliary stent can reduce biliary complications, as the stent itself may result in complications.68 When the graft has more than 1 right hepatic duct and they are close together, approximation of the adjacent ductal orifices to form a single cuff may be done and a single duct-to-duct anastomosis should be performed incorporating the hilar plate.69,70
Recommendations
Right liver LDLT can overcomes the restriction imposed by donor-recipient size matching and is the most common graft used in centers active in adult LDLT (class 1, level B).
Optimal hepatic venous outflow is key for a successful outcome. It is recommended to preserve and reconstruct major venous branches larger than 5 mm in diameter that drain a right liver graft (class 1, level B).
Surgical field magnification (either by operating microscope or surgical loops) should be used for hepatic artery anastomosis (class 1, level B).
Duct-to-duct anastomosis is the preferred technique for bile duct reconstruction (class 1, level B).
The role of external or internal biliary stents to reduce biliary complications is unclear (class 2, level B).
Dual-Graft LDLT
Dual-graft LDLT can be used as an alternative approach to prevent SFSS and to improve donor safety whenever a partial liver graft is unlikely to meet the metabolic demand of the recipient. Dual-graft LDLT has been performed since 2000 by the Asan group and recently at many other hospitals as well.55,71-74 The hepatectomy follows the same principle of distal hilar dissection used in single graft LDLT. Engraftment procedures and anastomosis sequence depends on the type of graft used (2 left grafts vs 1 right + 1 left grafts) as the anatomical 3-dimensional orientation of the hilar structures changes when a left graft is rotated 180 degrees and placed on the right upper quadrant.55 Engraftment procedures using both right and left liver grafts are a combination of 2 single-graft LDLTs using right and left liver grafts respectively, because both grafts are positioned orthotopically.75
The most common complications in dual-graft recipients are biliary strictures (18%) and hepatic venous outflow obstruction of the heterotopic, right-sided left liver graft (13%). Hepatic vein obstruction infrequently occurs in orthotopically positioned, left-sided left liver and right-sided right liver grafts. This might be related to the progressive compression of the hepatic vein anastomosis by the regeneration of a heterotopically positioned left liver graft. The overall survival rate and the incidence and severity of long-term complications between dual-graft and single graft recipients are similar.75,76 From time to time, unilateral graft atrophy developed in recipients left lobes, but this did not affect their liver function or survival.76
Recommendations
Dual-graft LDLT offers, in highly specialized LDLT centers, an important alternative to single graft LDLT when donor/recipient mismatch is prohibitive (class 1, level B).
Dual-graft LDLT could enhance donor safety through avoidance of right lobe procurement in case of donors with borderline future liver remnant (class 2, level C).
When performed in highly specialized centers, there is no difference in the overall survival rate and the incidence and severity of long-term complications between dual-graft and single graft recipients (class 1, level B).
The Impact of LDLT Transplant Volume on Outcomes
Several studies strongly support the concept that, as for many other complex surgical procedures, LDLT is characterized by a noticeable learning curve.77-82 After 15 to 20 cases, most LDLT centers reach a “steady state”. At this stage, most programs display comparable LD and cadaveric posttransplant outcomes.16 This is an important factor to keep in mind for those liver transplant programs embarking on LDLT as well as for programs performing sporadic LDLT.
Recommendations
Given the impact of volume on LDLT outcomes, transplant programs embarking on LDLT as well as programs performing LDLT sporadically should consider measures to mitigate the impact of the learning curve on patient outcomes (class 1, level B).
Posttransplant Care
Because of the increased technical complexity of the LD allograft, the overall complication rates are higher in LD recipients compared with cadaveric liver transplantation.15,83-86 Common early postoperative complications following LDLT include bleeding and hepatic artery thrombosis (HAT).83-85 Management of significant postoperative intra-abdominal bleeding is typically operative. Reoperation with attempted thrombectomy and revision of arterial anastomosis may also be successful in early HAT, especially if diagnosed via surveillance ultrasound.87 Primary nonfunction, an early postoperative complication which occurs in approximately 0.5-5 % of deceased donor liver transplantation (DDLT), is not commonly reported in LDLT, presumably due to the quality of the graft and relatively short cold ischemia time.15,84 Rejection, which is reported at similar rates compared to whole liver transplantation, is treated using a similar algorithm, with the use of steroid pulse and increased baseline immunosuppression followed by antibody treatment in case of refractory rejection. Overall, infection rates are higher following LDLT, likely related to higher rates of biliary complications leading to biloma and intra-abdominal abscess.15,83-86 Biliary leak rates track closely with center experience, and when the early cases are excluded, the reported incidence ranges from 15% to 30% for LDLT versus approximately 4% to 10% for DDLT.83,84,88 Management of a biliary leak includes biliary tract drainage via endoscopic retrograde cholangiopancreatogram, percutaneous transhepatic cholangiogram, or operative revision. SFSS represents another common complication in the early postoperative course.89,90 Treatment of SFSS is primarily supportive, with optimization of nutrition and physical therapy. Retransplantation should be considered if indicated and before development of systemic infection. Late biliary strictures are more common in LDLT (20-30%) than in cadaveric liver transplant and are more complex to manage due to the short length of an extrahepatic duct as well as the high frequency of multiple donor ducts (50-60% in most series).15,83-86,88 Recurrent disease is a critical issue impacting long term outcomes for both LD and DD transplant recipients. Although initial reports suggested that outcomes for recipients undergoing LDLT for hepatitis C virus may be inferior compared to DDLT recipients, others have disputed this data.91-93 HCC is one of the most common indication for LD liver transplant, particularly in Asia.94 Multiple authors have reported increased rates of HCC recurrence after LDLT. This is likely due to the reduced waiting time of LD liver transplant candidates, a fact that prevents waitlist dropout of those patients with a biologically unfavorable tumor.95,96 More recent series with closely matched patients undergoing LDLT or DDLT for HCC have demonstrated equivalent outcomes.97-99 Other diseases that may recur following liver transplant include primary sclerosing cholangitis, primary biliary cirrhosis, autoimmune hepatitis, alcohol, and nonalcoholic steatohepatitis. There is currently no evidence that recurrence is more likely following LDLT versus DDLT in these conditions.
Recommendations
Close monitoring of LDLT recipients in the early perioperative stage for the development of intra-abdominal bleeding and HAT is recommended (serial liver vascular ultrasound). (level 1, grade B).
Rejection rates are similar in LDLT and DDLT recipients, and therefore modification of immunosuppression protocols based on LD versus DD is not warranted. (level 1, grade B)
Biliary leaks are more common in LDLT recipients. Management is based on the clinical presentation and may include observation, percutaneous drain placement, biliary stenting, and/or operative intervention (level I, grade B).
Small-for-size syndrome is more common in LDLT. Allograft selection, potential use of inflow modification, and optimization of outflow are all strategies that should be used to decrease the incidence of SFSS (level 1, grade B).
Anastomotic biliary strictures are more common following LDLT and may be successfully managed with endoscopic/percutaneous balloon dilation and stenting or operative revision (level I, grade B).
Recurrent disease (in particular HCC, hepatitis C virus) does not appear to be more common in LDLT compared to DDLT recipients, which is useful in guiding donor and recipient selection criteria (class 1, level B).
Pediatric Considerations
The most frequent LDLT used in the pediatric population is the left lateral segment,100,101 followed by left lobe, reduced left lateral segment, right lobe and posterior segments.100
Overall outcomes for pediatric LDLT are good and generally better than for DD liver transplantation.102 Surgical complications include biliary complications (14%-20.6%),101,103 HAT (6%-10.7%)101,103,104 and portal vein complications (stenosis or thrombosis, 4%-9.1%).101,103,105,106 Acute cellular rejection is the most frequent histological abnormality (29.5%-48.7%).102 Chronic rejection has a lower incidence, at 2% to 3.4%,102,107 whereas in pediatric liver transplants overall rejection is reported at 5%.108 Posttransplant lymphoproliferative disease has also been described with an incidence of 2.4% to 11.3%.102 In comparison to split organ transplantation, at least in the short term, LDLT is associated with better graft function, most probably because of decreased injury to the graft before transplantation.109
Living related liver transplant donation is accompanied by some ethical considerations mainly related to the small, but existing, donor mortality. In most pediatric cases, the donor is a parent of the patient and therefore one needs to take family dynamics into consideration (eg, if the family may have more than 1 child or if the suitable donor is the family’s primary breadwinner).
Recommendations
Living related liver transplantation is an established form of liver transplantation in the pediatric population with excellent outcomes (class 1, level B).
LD work-up in pediatric LDLT should take into consideration family dynamics (eg if the family may have more than 1 child or if the suitable donor is the family’s primary breadwinner) (class 1, level C).
Footnotes
All authors contributed equally.
The authors declare no funding or conflicts of interest.
REFERENCES
- 1.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merriman RB, Tran TT. AASLD practice guidelines: The past, the present, and the future. Hepatology. 2016;63:31–34. [DOI] [PubMed] [Google Scholar]
- 3.Miller CM, Gondolesi GE, Florman S, et al. One hundred nine living donor liver transplants in adults and children: a single-center experience. Ann Surg. 2001;234:301–311; discussion 311–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jakab SS, Navarro VJ, Colombe BW, et al. Human leukocyte antigen and adult living-donor liver transplantation outcomes: an analysis of the organ procurement and transplantation network database. Liver Transpl. 2007;13:1405–1413. [DOI] [PubMed] [Google Scholar]
- 5.Suh KS, Kim SB, Chang SH, et al. Significance of positive cytotoxic cross-match in adult-to-adult living donor liver transplantation using small graft volume. Liver Transpl. 2002;8:1109–1113. [DOI] [PubMed] [Google Scholar]
- 6.Sugawara Y, Makuuchi M, Kaneko J, et al. Positive T lymphocytotoxic cross-match in living donor liver transplantation. Liver Transpl. 2003;9:1062–1066. [DOI] [PubMed] [Google Scholar]
- 7.Ogawa E, Hori T, Doi H, et al. Living-donor liver transplantation for moderate or severe porto-pulmonary hypertension accompanied by pulmonary arterial hypertension: a single-centre experience over 2 decades in Japan. J Hepatobiliary Pancreat Sci. 2012;19:638–649. [DOI] [PubMed] [Google Scholar]
- 8.Ogawa E, Hori T, Doi H, et al. Living-donor liver transplantation for congenital biliary atresia with porto-pulmonary hypertension and moderate or severe pulmonary arterial hypertension: Kyoto University experience. Clin Transplant. 2014;28:1031–1040. [DOI] [PubMed] [Google Scholar]
- 9.de Villa V, Lo CM. Liver transplantation for hepatocellular carcinoma in Asia. Oncologist. 2007;12:1321–1331. [DOI] [PubMed] [Google Scholar]
- 10.Liu CL, Fan ST, Lo CM, et al. Right-lobe live donor liver transplantation improves survival of patients with acute liver failure. Br J Surg. 2002;89:317–322. [DOI] [PubMed] [Google Scholar]
- 11.Park SJ, Lim YS, Hwang S, et al. Emergency adult-to-adult living-donor liver transplantation for acute liver failure in a hepatitis B virus endemic area. Hepatology. 2010;51:903–911. [DOI] [PubMed] [Google Scholar]
- 12.Ikegami T, Taketomi A, Soejima Y, et al. Living donor liver transplantation for acute liver failure: a 10-year experience in a single center. J Am Coll Surg. 2008;206:412–418. [DOI] [PubMed] [Google Scholar]
- 13.Lee SG, Ahn CS, Kim KH. Which types of graft to use in patients with acute liver failure? (A) Auxiliary liver transplant (B) Living donor liver transplantation (C) The whole liver. (B) I prefer living donor liver transplantation. J Hepatol. 2007;46:574–578. [DOI] [PubMed] [Google Scholar]
- 14.Yamashiki N, Sugawara Y, Tamura S, et al. Outcomes after living donor liver transplantation for acute liver failure in Japan: results of a nationwide survey. Liver Transpl. 2012;18:1069–1077. [DOI] [PubMed] [Google Scholar]
- 15.Olthoff KM, Merion RM, Ghobrial RM, et al. Outcomes of 385 adult-to-adult living donor liver transplant recipients: a report from the A2ALL Consortium. Ann Surg. 2005;242:314–323; discussion 323–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olthoff KM, Smith AR, Abecassis M, et al. Defining long-term outcomes with living donor liver transplantation in North America. Ann Surg. 2015;262:465–475; discussion 473–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldberg DS, French B, Abt PL, et al. Superior survival using living donors and donor-recipient matching using a novel living donor risk index. Hepatology. 2014;60:1717–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lo CM, Fan ST, Liu CL, et al. The role and limitation of living donor liver transplantation for hepatocellular carcinoma. Liver Transpl. 2004;10:440–447. [DOI] [PubMed] [Google Scholar]
- 19.Sugawara Y, Tamura S, Makuuchi M. Living donor liver transplantation for hepatocellular carcinoma: Tokyo University series. Dig Dis. 2007;25:310–312. [DOI] [PubMed] [Google Scholar]
- 20.Ito T, Takada Y, Ueda M, et al. Expansion of selection criteria for patients with hepatocellular carcinoma in living donor liver transplantation. Liver Transpl. 2007;13:1637–1644. [DOI] [PubMed] [Google Scholar]
- 21.Soejima Y, Taketomi A, Yoshizumi T, et al. Extended indication for living donor liver transplantation in patients with hepatocellular carcinoma. Transplantation. 2007;83:893–899. [DOI] [PubMed] [Google Scholar]
- 22.Kim JM, Kwon CH, Joh JW, et al. Expanded criteria for liver transplantation in patients with hepatocellular carcinoma. Transplant Proc. 2014;46:726–729. [DOI] [PubMed] [Google Scholar]
- 23.Choi GS, Park JB, Jung GO, et al. Living donor liver transplantation in Budd-Chiari syndrome: a single-center experience. Transplant Proc. 2010;42:839–842. [DOI] [PubMed] [Google Scholar]
- 24.Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant. 2005;5:2605–2610. [DOI] [PubMed] [Google Scholar]
- 25.Lo CM, Fan ST, Liu CL, et al. Minimum graft size for successful living donor liver transplantation. Transplantation. 1999;68:1112–1116. [DOI] [PubMed] [Google Scholar]
- 26.Kiuchi T, Kasahara M, Uryuhara K, et al. Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation. 1999;67:321–327. [DOI] [PubMed] [Google Scholar]
- 27.Chan SC, Lo CM, Ng KK, et al. Alleviating the burden of small-for-size graft in right liver living donor liver transplantation through accumulation of experience. Am J Transplant. 2010;10:859–867. [DOI] [PubMed] [Google Scholar]
- 28.Ito T, Kiuchi T, Yamamoto H, et al. Changes in portal venous pressure in the early phase after living donor liver transplantation: pathogenesis and clinical implications. Transplantation. 2003;75:1313–1317. [DOI] [PubMed] [Google Scholar]
- 29.Man K, Lo CM, Ng IO, et al. Liver transplantation in rats using small-for-size grafts: a study of hemodynamic and morphological changes. Arch Surg. 2001;136:280–285. [DOI] [PubMed] [Google Scholar]
- 30.Boillot O, Delafosse B, Méchet I, et al. Small-for-size partial liver graft in an adult recipient; a new transplant technique. Lancet. 2002;359:406–407. [DOI] [PubMed] [Google Scholar]
- 31.Wang HS, Ohkohchi N, Enomoto Y, et al. Excessive portal flow causes graft failure in extremely small-for-size liver transplantation in pigs. World J Gastroenterol. 2005;11:6954–6959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pomposelli JJ, Verbesey J, Simpson MA, et al. Improved survival after live donor adult liver transplantation (LDALT) using right lobe grafts: program experience and lessons learned. Am J Transplant. 2006;6:589–598. [DOI] [PubMed] [Google Scholar]
- 33.Chan SC, Lo CM, Chok KS, et al. Modulation of graft vascular inflow guided by flowmetry and manometry in liver transplantation. Hepatobiliary Pancreat Dis Int. 2011;10:649–656. [DOI] [PubMed] [Google Scholar]
- 34.Troisi R, Cammu G, Militerno G, et al. Modulation of portal graft inflow: a necessity in adult living-donor liver transplantation? Ann Surg. 2003;237:429–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shimada M, Ijichi H, Yonemura Y, et al. The impact of splenectomy or splenic artery ligation on the outcome of a living donor adult liver transplantation using a left lobe graft. Hepatogastroenterology. 2004;51:625–629. [PubMed] [Google Scholar]
- 36.Sato Y, Yamamoto S, Oya H, et al. Splenectomy for reduction of excessive portal hypertension after adult living-related donor liver transplantation. Hepatogastroenterology. 2002;49:1652–1655. [PubMed] [Google Scholar]
- 37.Yagi S, Iida T, Hori T, et al. Optimal portal venous circulation for liver graft function after living-donor liver transplantation. Transplantation. 2006;81:373–378. [DOI] [PubMed] [Google Scholar]
- 38.Troisi R, Ricciardi S, Smeets P, et al. Effects of hemi-portocaval shunts for inflow modulation on the outcome of small-for-size grafts in living donor liver transplantation. Am J Transplant. 2005;5:1397–1404. [DOI] [PubMed] [Google Scholar]
- 39.Yamada T, Tanaka K, Uryuhara K, et al. Selective hemi-portocaval shunt based on portal vein pressure for small-for-size graft in adult living donor liver transplantation. Am J Transplant. 2008;8:847–853. [DOI] [PubMed] [Google Scholar]
- 40.Ben-Haim M, Emre S, Fishbein TM, et al. Critical graft size in adult-to-adult living donor liver transplantation: impact of the recipient's disease. Liver Transpl. 2001;7:948–953. [DOI] [PubMed] [Google Scholar]
- 41.Sugawara Y, Makuuchi M, Takayama T, et al. Small-for-size grafts in living-related liver transplantation. J Am Coll Surg. 2001;192:510–513. [DOI] [PubMed] [Google Scholar]
- 42.Hwang S, Lee SG, Ha TY, et al. Simplified standardized technique for living donor liver transplantation using left liver graft plus caudate lobe. Liver Transpl. 2004;10:1398–1405. [DOI] [PubMed] [Google Scholar]
- 43.Kokudo N, Sugawara Y, Imamura H, et al. Sling suspension of the liver in donor operation: a gradual tape-repositioning technique. Transplantation. 2003;76:803–807. [DOI] [PubMed] [Google Scholar]
- 44.Sugawara Y, Tamura S, Kaneko J, et al. Single artery reconstruction in left liver transplantation. Surgery. 2011;149:841–845. [DOI] [PubMed] [Google Scholar]
- 45.Ikegami T, Shirabe K, Soejima Y, et al. Strategies for successful left-lobe living donor liver transplantation in 250 consecutive adult cases in a single center. J Am Coll Surg. 2013;216:353–362. [DOI] [PubMed] [Google Scholar]
- 46.Soejima Y, Shirabe K, Taketomi A, et al. Left lobe living donor liver transplantation in adults. Am J Transplant. 2012;12:1877–1885. [DOI] [PubMed] [Google Scholar]
- 47.Botha JF, Langnas AN, Campos BD, et al. Left lobe adult-to-adult living donor liver transplantation: small grafts and hemiportocaval shunts in the prevention of small-for-size syndrome. Liver Transpl. 2010;16:649–657. [DOI] [PubMed] [Google Scholar]
- 48.Hashimoto T, Sugawara Y, Tamura S, et al. One orifice vein reconstruction in left liver plus caudate lobe grafts. Transplantation. 2007;83:225–227. [DOI] [PubMed] [Google Scholar]
- 49.Makuuchi M, Sugawara Y. Living-donor liver transplantation using the left liver, with special reference to vein reconstruction. Transplantation. 2003;75(3 Suppl):S23–S24. [DOI] [PubMed] [Google Scholar]
- 50.Lee SG. A complete treatment of adult living donor liver transplantation: a review of surgical technique and current challenges to expand indication of patients. Am J Transplant. 2015;15:17–38. [DOI] [PubMed] [Google Scholar]
- 51.Sugawara Y, Makuuchi M, Takayama T. Left liver plus caudate lobe graft with complete revascularization. Surgery. 2002;132:904–905; author reply 905–906. [DOI] [PubMed] [Google Scholar]
- 52.Kokudo N, Sugawara Y, Kaneko J, et al. Reconstruction of isolated caudate portal vein in left liver graft. Liver Transpl. 2004;10:1163–1165. [DOI] [PubMed] [Google Scholar]
- 53.Ikegami T, Kawasaki S, Matsunami H, et al. Should all hepatic arterial branches be reconstructed in living-related liver transplantation? Surgery. 1996;119:431–436. [DOI] [PubMed] [Google Scholar]
- 54.Dulundu E, Sugawara Y, Sano K, et al. Duct-to-duct biliary reconstruction in adult living-donor liver transplantation. Transplantation. 2004;78:574–579. [DOI] [PubMed] [Google Scholar]
- 55.Lee S, Hwang S, Park K, et al. An adult-to-adult living donor liver transplant using dual left lobe grafts. Surgery. 2001;129:647–650. [DOI] [PubMed] [Google Scholar]
- 56.Sugawara Y, Makuuchi M, Akamatsu N, et al. Refinement of venous reconstruction using cryopreserved veins in right liver grafts. Liver Transpl. 2004;10:541–547. [DOI] [PubMed] [Google Scholar]
- 57.Miller CM, Durand F, Heimbach JK, et al. The International Liver Transplantation Society Guideline on Living Liver Donation. Transplantation. 2016;100:1238–1243. [DOI] [PubMed] [Google Scholar]
- 58.de Villa VH, Chen CL, Chen YS, et al. Right lobe living donor liver transplantation-addressing the middle hepatic vein controversy. Ann Surg. 2003;238:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kasahara M, Takada Y, Fujimoto Y, et al. Impact of right lobe with middle hepatic vein graft in living-donor liver transplantation. Am J Transplant. 2005;5:1339–1346. [DOI] [PubMed] [Google Scholar]
- 60.Gyu Lee S, Min Park K, Hwang S, et al. Modified right liver graft from a living donor to prevent congestion. Transplantation. 2002;74:54–59. [DOI] [PubMed] [Google Scholar]
- 61.Lo CM, Fan ST, Liu CL, et al. Hepatic venoplasty in living-donor liver transplantation using right lobe graft with middle hepatic vein. Transplantation. 2003;75:358–360. [DOI] [PubMed] [Google Scholar]
- 62.Marcos A, Orloff M, Mieles L, et al. Reconstruction of double hepatic arterial and portal venous branches for right-lobe living donor liver transplantation. Liver Transpl. 2001;7:673–679. [DOI] [PubMed] [Google Scholar]
- 63.Sato K, Sekiguchi S, Watanabe T, et al. The use of recipient superficial femoral vein as a venous graft for portal vein reconstruction in right lobe living donor liver transplantation. Transplant Proc. 2009;41:195–197. [DOI] [PubMed] [Google Scholar]
- 64.Xu MQ, Yan LN, Li B, et al. Surgical procedures for management of right portal venous branching in right lobe living donor liver transplantation. Transplant Proc. 2008;40:1529–1533. [DOI] [PubMed] [Google Scholar]
- 65.Mori K, Nagata I, Yamagata S, et al. The introduction of microvascular surgery to hepatic artery reconstruction in living-donor liver transplantation–its surgical advantages compared with conventional procedures. Transplantation. 1992;54:263–268. [DOI] [PubMed] [Google Scholar]
- 66.Yagi T, Shinoura S, Umeda Y, et al. Surgical rationalization of living donor liver transplantation by abolition of hepatic artery reconstruction under a fixed microscope. Clin Transplant. 2012;26:877–883. [DOI] [PubMed] [Google Scholar]
- 67.Li PC, Jeng LB, Yang HR, et al. Hepatic artery reconstruction in living donor liver transplantation: running suture under surgical loupes by cardiovascular surgeons in 180 recipients. Transplant Proc. 2012;44:448–450. [DOI] [PubMed] [Google Scholar]
- 68.Liu CL, Lo CM, Chan SC, et al. Safety of duct-to-duct biliary reconstruction in right-lobe live-donor liver transplantation without biliary drainage. Transplantation. 2004;77:726–732. [DOI] [PubMed] [Google Scholar]
- 69.Zhang S, Zhang M, Xia Q, et al. Biliary reconstruction and complications in adult living donor liver transplantation: systematic review and meta-analysis. Transplant Proc. 2014;46:208–215. [DOI] [PubMed] [Google Scholar]
- 70.Sharma S, Gurakar A, Jabbour N. Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 2008;14:759–769. [DOI] [PubMed] [Google Scholar]
- 71.Lu CH, Chen TY, Huang TL, et al. Regeneration and outcome of dual grafts in living donor liver transplantation. Clin Transplant. 2012;26:E143–E148. [DOI] [PubMed] [Google Scholar]
- 72.Dayangac M, Taner CB, Akin B, et al. Dual left lobe living donor liver transplantation using donors unacceptable for right lobe donation: a case report. Transplant Proc. 2010;42:4560–4563. [DOI] [PubMed] [Google Scholar]
- 73.Chen Z, Zeng Y, Wen TF, et al. Dual grafts live donor liver transplantation for acute-on-chronic hepatitis B liver failure. Transplant Proc. 2010;42:4552–4554. [DOI] [PubMed] [Google Scholar]
- 74.Soejima Y, Taketomi A, Ikegami T, et al. Living donor liver transplantation using dual grafts from two donors: a feasible option to overcome small-for-size graft problems? Am J Transplant. 2008;8:887–892. [DOI] [PubMed] [Google Scholar]
- 75.Lee SG, Hwang S, Park KM, et al. Seventeen adult-to-adult living donor liver transplantations using dual grafts. Transplant Proc. 2001;33:3461–3463. [DOI] [PubMed] [Google Scholar]
- 76.Lee SG, Hwang S, Kim KH, et al. Toward 300 liver transplants a year. Surg Today. 2009;39:367–373. [DOI] [PubMed] [Google Scholar]
- 77.Lo CM, Fan ST, Liu CL, et al. Lessons learned from one hundred right lobe living donor liver transplants. Ann Surg. 2004;240:151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Axelrod DA, Guidinger MK, McCullough KP, et al. Association of center volume with outcome after liver and kidney transplantation. Am J Transplant. 2004;4:920–927. [DOI] [PubMed] [Google Scholar]
- 79.Edwards EB, Roberts JP, McBride MA, et al. The effect of the volume of procedures at transplantation centers on mortality after liver transplantation. N Engl J Med. 1999;341:2049–2053. [DOI] [PubMed] [Google Scholar]
- 80.Bak T, Wachs M, Trotter J, et al. Adult-to-adult living donor liver transplantation using right-lobe grafts: results and lessons learned from a single-center experience. Liver Transpl. 2001;7:680–686. [DOI] [PubMed] [Google Scholar]
- 81.Li C, Mi K, Wen T, et al. A learning curve for living donor liver transplantation. Dig Liver Dis. 2012;44:597–602. [DOI] [PubMed] [Google Scholar]
- 82.Kim SH, Cho SY, Park SJ, et al. Learning curve for living-donor liver transplantation in a fledgling cancer center. Transpl Int. 2009;22:1164–1171. [DOI] [PubMed] [Google Scholar]
- 83.Freise CE, Gillespie BW, Koffron AJ, et al. Recipient morbidity after living and deceased donor liver transplantation: findings from the A2ALL Retrospective Cohort Study. Am J Transplant. 2008;8:2569–2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Reichman TW, Katchman H, Tanaka T, et al. Living donor versus deceased donor liver transplantation: a surgeon-matched comparison of recipient morbidity and outcomes. Transpl Int. 2013;26:780–787. [DOI] [PubMed] [Google Scholar]
- 85.Jiang L, Yan L, Tan Y, et al. Adult-to-adult right-lobe living donor liver transplantation in recipients with hepatitis B virus-related benign liver disease and high model end-stage liver disease scores. Surg Today. 2013;43:1039–1048. [DOI] [PubMed] [Google Scholar]
- 86.Selzner M, Kashfi A, Cattral MS, et al. Live donor liver transplantation in high MELD score recipients. Ann Surg. 2010;251:153–157. [DOI] [PubMed] [Google Scholar]
- 87.Horrow MM, Blumenthal BM, Reich DJ, et al. Sonographic diagnosis and outcome of hepatic artery thrombosis after orthotopic liver transplantation in adults. AJR Am J Roentgenol. 2007;189:346–351. [DOI] [PubMed] [Google Scholar]
- 88.Zimmerman MA, Baker T, Goodrich NP, et al. Development, management, and resolution of biliary complications after living and deceased donor liver transplantation: a report from the adult-to-adult living donor liver transplantation cohort study consortium. Liver Transpl. 2013;19:259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Raut V, Alikhanov R, Belghiti J, et al. Review of the surgical approach to prevent small-for-size syndrome in recipients after left lobe adult LDLT. Surg Today. 2014;44:1189–1196. [DOI] [PubMed] [Google Scholar]
- 90.Roll GR, Parekh JR, Parker WF, et al. Left hepatectomy versus right hepatectomy for living donor liver transplantation: shifting the risk from the donor to the recipient. Liver Transpl. 2013;19:472–481. [DOI] [PubMed] [Google Scholar]
- 91.Lee SD, Kim SH, Kim YK, et al. Graft-to-recipient weight ratio lower to 0.7% is safe without portal pressure modulation in right-lobe living donor liver transplantation with favorable conditions. Hepatobiliary Pancreat Dis Int. 2014;13:18–24. [DOI] [PubMed] [Google Scholar]
- 92.Terrault NA, Shiffman ML, Lok AS, et al. Outcomes in hepatitis C virus-infected recipients of living donor vs. deceased donor liver transplantation. Liver Transpl. 2007;13:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thuluvath PJ, Yoo HY. Graft and patient survival after adult live donor liver transplantation compared to a matched cohort who received a deceased donor transplantation. Liver Transpl. 2004;10:1263–1268. [DOI] [PubMed] [Google Scholar]
- 94.Kim WR, Stock PG, Smith JM, et al. OPTN/SRTR 2011 Annual Data Report: liver. Am J Transplant. 2013;13(Suppl 1):73–102. [DOI] [PubMed] [Google Scholar]
- 95.Fisher RA, Kulik LM, Freise CE, et al. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007;7:1601–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lo CM, Fan ST, Liu CL, et al. Living donor versus deceased donor liver transplantation for early irresectable hepatocellular carcinoma. Br J Surg. 2007;94:78–86. [DOI] [PubMed] [Google Scholar]
- 97.Kulik LM, Fisher RA, Rodrigo DR, et al. Outcomes of living and deceased donor liver transplant recipients with hepatocellular carcinoma: results of the A2ALL cohort. Am J Transplant. 2012;12:2997–3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sandhu L, Sandroussi C, Guba M, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: comparable survival and recurrence. Liver Transpl. 2012;18:315–322. [DOI] [PubMed] [Google Scholar]
- 99.Bhangui P, Vibert E, Majno P, et al. Intention-to-treat analysis of liver transplantation for hepatocellular carcinoma: living versus deceased donor transplantation. Hepatology. 2011;53:1570–1579. [DOI] [PubMed] [Google Scholar]
- 100.Kasahara M, Umeshita K, Inomata Y, et al. Long-term outcomes of pediatric living donor liver transplantation in Japan: an analysis of more than 2200 cases listed in the registry of the Japanese Liver Transplantation Society. Am J Transplant. 2013;13:1830–1839. [DOI] [PubMed] [Google Scholar]
- 101.Heaton N, Faraj W, Melendez HV, et al. Living related liver transplantation in children. Br J Surg. 2008;95:919–924. [DOI] [PubMed] [Google Scholar]
- 102.Dattani N, Baker A, Quaglia A, et al. Clinical and histological outcomes following living-related liver transplantation in children. Clin Res Hepatol Gastroenterol. 2014;38:164–171. [DOI] [PubMed] [Google Scholar]
- 103.Tannuri AC, Gibelli NE, Ricardi LR, et al. Living related donor liver transplantation in children. Transplant Proc. 2011;43:161–164. [DOI] [PubMed] [Google Scholar]
- 104.Uchida Y, Sakamoto S, Egawa H, et al. The impact of meticulous management for hepatic artery thrombosis on long-term outcome after pediatric living donor liver transplantation. Clin Transplant. 2009;23:392–399. [DOI] [PubMed] [Google Scholar]
- 105.Ueda M, Egawa H, Ogawa K, et al. Portal vein complications in the long-term course after pediatric living donor liver transplantation. Transplant Proc. 2005;37:1138–1140. [DOI] [PubMed] [Google Scholar]
- 106.Ueda M, Oike F, Kasahara M, et al. Portal vein complications in pediatric living donor liver transplantation using left-side grafts. Am J Transplant. 2008;8:2097–2105. [DOI] [PubMed] [Google Scholar]
- 107.Oh SH, Kim KM, Kim DY, et al. Clinical experience of more than 200 cases of pediatric liver transplantation at a single center: improved patient survival. Transplant Proc. 2012;44:484–486. [DOI] [PubMed] [Google Scholar]
- 108.Ng VL, Fecteau A, Shepherd R, et al. Outcomes of 5-year survivors of pediatric liver transplantation: report on 461 children from a north american multicenter registry. Pediatrics. 2008;122:e1128–e1135. [DOI] [PubMed] [Google Scholar]
- 109.Farmer DG, Yersiz H, Ghobrial RM, et al. Early graft function after pediatric liver transplantation: comparison between in situ split liver grafts and living-related liver grafts. Transplantation. 2001;72:1795–1802. [DOI] [PubMed] [Google Scholar]


