Abstract
Objectives
To assess interest in, concerns about and knowledge of long-acting reversible contraceptives (LARC) among women in medication-assisted treatment (MAT) for opioid use disorder who were at risk of unintended pregnancy.
Study Design
Women in MAT completed a survey on contraceptive use, attitudes, and knowledge, including LARC methods, as part of eligibility screening for an ongoing trial evaluating family planning interventions for this population.
Results
Eighty-three women at risk of unintended pregnancy completed the survey, and a subset of 51 completed supplemental questions about implants. All participants had heard of IUDs and 75/83 (90%) had heard of implants, but only 34/83 (41%) and 14/51 (27%) reported being likely to use IUDs and implants, respectively. Thirty-five women reported they were unlikely to use IUDs, with 29/35 (83%) citing unspecified “other reasons” for this position and 24/35 (69%) endorsing concerns about side effects. Seventeen women reported they were unlikely to use implants, with 8/17 (47%) citing “other reasons” and 9/17 (53%) and 10/17 (59%) reporting concerns about insertion and removal, respectively. Participants reported they knew “a little” about LARCs, but only their knowledge of implants was limited. Only 50/83 (60%) participants were aware of the superior effectiveness of IUDs and 26/51 (51%) were aware of the superior effectiveness of implants relative to other reversible methods.
Conclusions
Participants reported relatively low interest in LARCs. Many women had unspecified reasons for not using LARCs. Participants also lacked information about LARC safety and effectiveness, especially with regard to implants.
Keywords: long-acting reversible contraception, opioid use disorder, medication-assisted treatment, unintended pregnancy
1. Introduction
A particularly unsettling aspect of the current US opioid epidemic is the high rate of in utero exposure and associated adverse health and economic outcomes. The cost of acute medical care for opioid-exposed neonates was recently estimated at nearly $67,000 per infant, due in part to extended inpatient stays to monitor and treat neonatal abstinence syndrome as well as increased risk of complications like respiratory problems, feeding difficulties, and seizures [1]. Since nearly 80% of pregnancies in women with opioid use disorder (OUD) are unintended, helping these women avoid unintended pregnancy is a public health imperative [2–5].
One of the most effective ways to reduce unintended pregnancies is through the use of effective contraception. Two contraceptive methods, the intrauterine device (IUD) and implant, are collectively referred to as long-acting reversible contraceptive (LARC) methods because they are effective for a minimum of three years and fertility is rapidly restored upon removal of the device. LARCs are the most effective reversible forms of contraception (<1% failure rate), in part because they require virtually no effort on the woman’s part after placement [6]. Modern LARCs also have relatively few disadvantages and complications are rare [7]. Their efficacy and safety likely contribute to high rates of continuation, with one recent study reporting significantly higher continuation rates of LARCs at 3 years compared to non-LARC methods (67% vs. 31%) [8]. Despite all this, opioid- and other substance-using women have tended to rely on less effective forms of contraception (e.g., condoms) or use no method at all [see review 9]. Lack of information about the safety and acceptability of LARCs, fear of LARC side effects, and concern about having the device placed are thought to be significant barriers to LARC use in the general population [10]. This study sought to examine interest in, concerns about and knowledge of LARCs among women with OUD and at risk of unintended pregnancy.
2. Methods and Materials
Study procedures were approved by the University of Vermont Institutional Review Board. We selected participants for this analysis from a convenience sample of women 18–49 years old who completed an eligibility screening for an ongoing randomized clinical trial evaluating behavioral economic interventions to increase contraceptive use among women with OUD who were at risk of unintended pregnancy (ClinicalTrials.gov NCT02411357). A nurse recruiter approached women who were patients at two Burlington, VT clinics that provide outpatient medication-assisted treatment (MAT) for OUD and invited them to complete the eligibility screening, for which they received $50 in compensation. We excluded women who were not at risk for unintended pregnancy (using contraception or not heterosexually active) or with incomplete data from the analysis.
The eligibility screening included a locally developed structured interview to collect information about participants’ sociodemographic, clinical and sexual/reproductive histories. The screening also included the National Campaign to Prevent Teen and Unplanned Pregnancy’s Survey of Reproductive and Contraceptive Knowledge [11]. The survey explored contraceptive use, attitudes, and knowledge across a wide range of contraceptive methods and was originally employed in a nationally representative sample of unmarried women and men ages 18–29 [12]. Early in the course of the present study, we became aware that the original survey did not assess likelihood of future use or knowledge-related items with regard to implants; therefore, a 15-item supplement assessing these areas was developed locally and completed by all participants enrolled from that point forward.
On the Survey of Reproductive and Contraceptive Knowledge, familiarity with different methods was assessed with a single item per method asking whether participants had ever heard of the method; response options were “yes,” “no,” or “don’t know.” Past use of methods was assessed with a single item per method asking whether participants had ever used the method; response options were “yes,” “no,” or “don’t know.” Likelihood of future method use was assessed with a single item per method that asked participants how likely they were to use the method in the future; response options were “likely,” “unlikely,” or “don’t know.” Note that the original survey did not ask about the likelihood of future condom use, presumably because lifetime condom use approaches 95% [13]. Those participants who reported being unlikely to use an IUD or implant were asked further about their reasoning. Four reasons assessed that were potentially relevant to both of these methods were 1) doctor’s advice not to use the method, 2) friends or relatives’ bad experiences with the method, 3) worries about side effects or health problems, or 4) other reasons (not further specified); response options were “yes,” “no,” or “don’t know.” Specific to the IUD, participants who reported being unlikely to use an IUD were also asked how much the possibility of getting an infection reduced their likelihood of using this method. Specific to the implant, participants who reported being unlikely to use an implant were also asked how much their worries about implant insertion and removal and possible menstrual changes reduced their likelihood of using this method. Response options for method-specific reasons were “not at all,” “a little,” “somewhat,” “a lot,” and “don’t know”; those who answered “somewhat” or “a lot” were counted as endorsing the reason. Perceived method knowledge was assessed by a single item per method asking participants to rate how much they knew about each method, with possible scores ranging from 1 (“know nothing”) to 4 (“know everything”). To assess actual method knowledge, participants also answered 3–6 true/false basic knowledge questions per method and the percentage of correct responses was calculated for each. Knowledge of the relative effectiveness of methods was assessed using a series of questions comparing two methods (i.e., IUD vs. pills, implant vs. pills, and IUD vs. implant); response options included the two methods being compared, equal effectiveness, or “don’t know.”
Descriptive statistics were calculated to first examine familiarity with LARCs as compared to condoms, pills and injections. The three latter methods were chosen for comparison because they are the most commonly used nonpermanent methods [13]. Next, past use and likelihood of future use of LARCs compared to condoms, pills and injections were explored. Concerns about LARCs were also characterized among participants who reported that they were unlikely to use these methods in the future. Finally, perceived and actual contraceptive knowledge, and participants’ understanding of the relative efficacy of LARCs vs. other methods were also examined.
3. Results
Of the 164 women who completed the eligibility screening, we excluded 61 who were not at risk of unintended pregnancy and another 20 who had missing data, resulting in a final sample of 83. Of these 83, 51 (61%) completed the supplemental questions about implants. Table 1 provides participants’ demographic and clinical characteristics.
Table 1.
Demographic, clinical and reproductive characteristics of women in medication assisted treatment for opioid use disorder and at risk for unintended pregnancy (N=83).
| Characteristic |
n (%) or mean ± standard deviation |
|---|---|
| Age (years) | 30.8 ± 5.5 |
| Race | |
| White | 72 (86.7%) |
| Multiracial | 7 (8.4%) |
| Other | 4 (4.8%) |
| Education (years) | 12.1 ±1.6 |
| Unemployed | 48 (57.8%) |
| Never married | 53 (63.9%) |
| Has steady partner | 74 (89.2%) |
| Agonist medication | |
| Methadone | 51 (61.4%) |
| Buprenorphine | 32 (38.6%) |
| Smokes cigarettes | 76 (91.6%) |
| Age at first intercourse (years) | 14.5 ± 2.0 |
| Pregnancies | |
| None | 6 (7.2%) |
| 1–2 | 37 (44.6%) |
| 3–4 | 18 (21.7%) |
| 5+ | 22 (26.5%) |
| Age at first pregnancy (years)1 | 19.4 ± 3.7 |
| Unintended pregnancies1 | |
| None | 5 (6.5%) |
| 1–2 | 37 (48.1%) |
| 3–4 | 20 (26.0%) |
| 5+ | 15 (19.5%) |
| History of therapeutic abortion1 | 40 (51.9%) |
| History of prescription contraceptive use | 82 (98.8%) |
n = 77 who had at least one pregnancy
3.1 Method familiarity, past use and likelihood of future use
Of the 83 participants who completed the survey, all had heard of condoms, pills, injections and IUDs, and 75 (90%) had heard of implants. Twenty-five participants (30%) had used an IUD in the past and seven (8%) had used an implant. Overall, 28 participants (34%) had used an IUD and/or implant. These rates were considerably lower than past use of barrier and shorter-acting methods: 73 participants (88%) reported using condoms, 77 (93%) had used pills, and 43 (52%) had used injections.
The percentages of participants likely to use various contraceptive methods in the future are shown in Figure 1. Rates of likely LARC use were somewhat lower than rates of other methods. Thirty-five participants (42%) reported being unlikely to use an IUD in the future, 23 (66%) of whom had never used an IUD before. Among these 35, 29 (83%) endorsed unspecified “other reasons” for this position, 24 (69%) reported concerns about side effects, 13 (37%) were discouraged by others’ negative experiences and only one (3%) reported that a doctor had advised her not to use an IUD. In response to a related question specific to IUDs, 16 (46%) of these 35 women said concerns about getting an infection reduced their likelihood of future IUD use.
Figure 1.
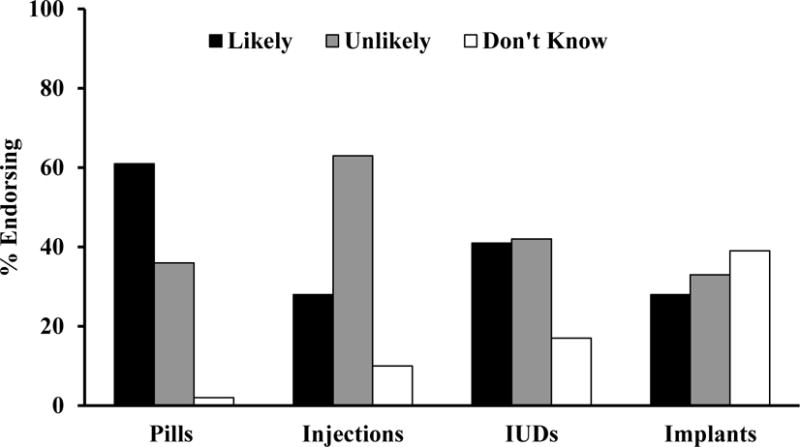
Self-rated likelihood of birth control pill, injection, intrauterine device (IUD) and implant use in the future among women in medication assisted treatment for opioid use disorder and at risk for unintended pregnancy. Note that the original survey did not ask about the likelihood of future condom use. N = 83 for pills, injections and IUDs and n = 51 for implants.
Of the 51 participants who completed the supplemental implant questions, 17 (33%) reported being unlikely to use an implant, 16 (94%) of whom had never used an implant before. Among these 17, 8 (47%) endorsed unspecified “other reasons” for being unlikely to use an implant in the future, 5 (29%) reported worries about side effects and/or others’ negative experiences and none cited a doctor’s advice not to use an implant. In response to related questions specific to implants, 9 (53%) of these 17 women reported concerns about the implant insertion and 10 (59%) about the removal process, while 7 (41%) expressed concerns about menstrual changes.
3.2 Perceived and actual LARC knowledge and relative effectiveness of methods
On average, the 83 participants reported only “knowing a little” about IUDs and answered 62% of the five IUD knowledge questions correctly. Although participants reported greater perceived knowledge of short-acting and barrier methods, their actual contraceptive knowledge was similar across condoms, pills, injections and IUDs (Figure 2). The subset of 51 participants asked about implants also reported only “knowing a little” about this method and answered only 40% of the six implant questions correctly, considerably lower than other contraceptive methods, and less than would be expected by chance (i.e., 50%). An item-level analysis revealed that poor performance was due to 13–28 participants (25–55%) responding “I don’t know” to each of these questions.
Figure 2.
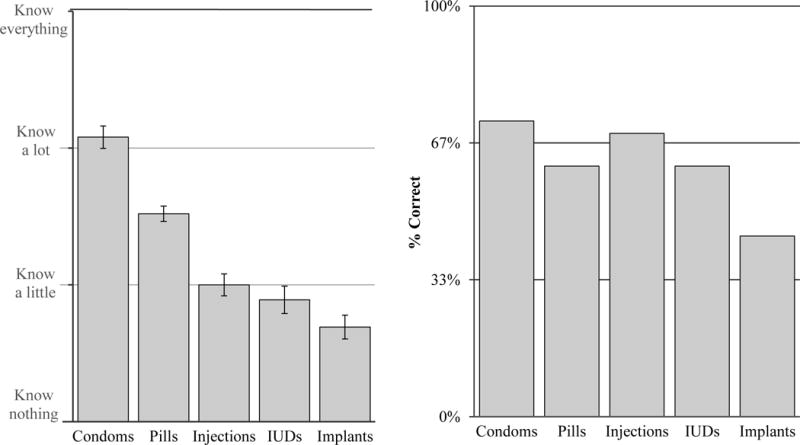
Mean ± standard error of the mean of self-rated contraceptive knowledge (left panel) and percentage of correct responses to contraceptive knowledge questions (right panel) as a function of method type (IUDs = intrauterine devices) among women in medication assisted treatment for opioid use disorder and at risk for unintended pregnancy. N = 83 for pills, injections and IUDs and n = 51 for implants.
Of the 83 participants asked about the relative effectiveness of IUDs, 50 (60%) correctly identified the IUD as more effective than birth control pills. Within the subset of 51 participants that was asked about the relative effectiveness of implants compared to other methods, only 26 (51%) identified the implant as more effective than birth control pills, while 16 (31%) knew that the IUD and implant are similarly effective and 20 (39%) reported that they were unsure which was more effective.
4. Discussion
This study provides insights into some of the factors that may reduce the likelihood of LARC use among women in MAT for OUD, a population at increased risk of unintended pregnancy. About 30% of participants reported having used LARCs in the past, a rate similar to estimates in the general population [14], but at odds with the substantially higher unintended pregnancy rate among women with OUD [2–5]. Some of the discrepancy may be an artifact of the sample, as the present study collected data from women in MAT who were interested in participating in a randomized clinical trial to increase contraceptive use. It is also possible that a higher percentage of women in MAT do receive these methods, but have them removed more frequently and/or earlier, thereby leaving them at greater overall risk of unintended pregnancy.
Only about a third of participants said they were likely to use LARCs in the future. While comparisons across populations are imperfect due to differences in methodology, this rate is somewhat higher than the 25% calculated for the nationally representative sample of unmarried young women surveyed with the same instrument by the National Campaign to Prevent Teen and Unplanned Pregnancy [15]. Of more importance, women in MAT appear to be 2.5 times as likely to endorse “other reasons” for not using an IUD in the future compared to women in the National Campaign sample (83% vs. 32%, respectively). It is possible that women in MAT encounter unique barriers to IUD use. Since the National Campaign sample was not asked about the likelihood of future implant use, it remains unclear whether other reasons also disproportionately dissuade women in MAT from using implants. These possibilities need to be explicated and explored more in future studies.
Despite thinking they do not know much about IUDs, women in MAT knew as much about that method as about short-acting and barrier methods and perceived and actual knowledge of IUDs, pills, condoms, and injections appear very similar to that reported by women in the National Campaign sample [15]. Within women in MAT, perceived and actual knowledge about implants were consistently lower than all other methods assessed. The high percentage of “don’t know” responses on implant knowledge questions suggests these deficits may reflect a lack of information, rather than misinformation, about the implant. Participants also knew relatively little about the relative efficacy of IUDs and implants, highlighting additional opportunities for education.
Lack of information and misinformation are not uncommon barriers to LARC use and systematic reviews have generally shown that contraceptive counseling and education increases choice of more effective methods like LARCs [see summary in 16]. Efforts to provide accurate information and correct misinformation among women in MAT may also benefit by providing services in unconventional settings, since some women with opioid and other substance use disorders may be hesitant to seek family planning in traditional settings due to stigma and concerns or experiences of coerced treatment [17].
The somewhat limited sample size, especially with regards to the sample that completed the supplemental implant questionnaire, and potential bias in the sample are limitations of the present study. Nevertheless, future efforts to document the reasons women with OUD are reluctant to use LARC and to enhance awareness of the efficacy of LARCs and correct misconceptions about these methods, especially implants, are likely to have far-reaching impacts in terms of reducing the high rate of unintended pregnancy among women with OUD and the very costly consequences associated with it.
Implications.
Women in medication-assisted treatment for opioid use disorder are at high risk of unintended pregnancy, yet contraceptive use is low and use of less effective methods is common. Women in MAT may benefit from efforts to increase knowledge about implants and assuage concerns about their insertion and removal as well as more general efforts to improve knowledge about the relative efficacy of LARCs. Many women in MAT endorsed unspecified “other reasons” for not using LARCs, which should be explored further.
Acknowledgments
The authors gratefully acknowledge the suggestions and advice of Drs. Lauren K. MacAfee and Anne K. Dougherty. This work was supported by the National Institutes of Health grant numbers R01 DA036670, T32 DA07242, and P20 GM103644. The sponsor had no role in study design; in the collection, analysis or interpretation of data; in the writing of the report; nor in the decision to submit this article for publication.
Footnotes
Conflicts of interest: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Patrick SW, Davis MM, Lehmann CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35:650–5. doi: 10.1038/jp.2015.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Black KI, Stephens C, Haber PS, Lintzeris N. Unplanned pregnancy and contraceptive use in women attending drug treatment services. Aust N Z J Obstet Gynaecol. 2012;52:146–50. doi: 10.1111/j.1479-828X.2012.01413.x. [DOI] [PubMed] [Google Scholar]
- 3.Burns L, Conroy E, Moore EA, Hutchinson D, Haber PS. Psychosocial characteristics and obstetric health of women attending a specialist substance use antenatal clinic in a large metropolitan hospital. Int J Pediatr. 2011 doi: 10.1155/2011/729237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heil SH, Jones HE, Arria A, Kaltenbach K, Coyle M, Fischer G, et al. Unintended pregnancy in opioid-abusing women. J Subst Abuse Treat. 2011;40:199–202. doi: 10.1016/j.jsat.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones HE, O’Grady KE, Tuten M. Reinforcement-based treatment improves the maternal treatment and neonatal outcomes of pregnant patients enrolled in comprehensive care treatment. Am J Addict. 2011;20:196–204. doi: 10.1111/j.1521-0391.2011.00119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stoddard A, McNicholas C, Peipert JF. Efficacy and safety of long-acting reversible contraception. Drugs. 2011;71:969–80. doi: 10.2165/11591290-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diedrich JT, Zhao Q, Madden T, Secura GM, Peipert JF. Three-year continuation of reversible contraception. Am J Obstet Gynecol. 2015;213:662.e1–8. doi: 10.1016/j.ajog.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Terplan M, Hand DJ, Hutchinson M, Salisbury-Afshar E, Heil SH. Contraceptive use and method choice among women with opioid and other substance use disorders: A systematic review. Prev Med. 2015;80:23–31. doi: 10.1016/j.ypmed.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foster DG, Barar R, Gould H, Gomez I, Nguyen D, Biggs MA. Projections and opinions from 100 experts in long-acting reversible contraception. Contraception. 2015;92:543–52. doi: 10.1016/j.contraception.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 11.National Campaign to Prevent Teen Pregnancy. Survey of Reproductive and Contraceptive Knowledge [Internet] Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2009. Available from: https://thenationalcampaign.org/sites/default/files/resource-supporting-download/survey_questionnaire.pdf [accessed 17.04.05] [Google Scholar]
- 12.Kaye K, Sullentrop K, Sloup C. The fog zone: How misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy [Internet] Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2009. Available from: https://thenationalcampaign.org/resource/fog-zone [accessed 17.04.05] [Google Scholar]
- 13.Guttmacher Institute [Internet] Contraceptive use in the United States. New York, NY: Guttmacher Institute; 2016. Available from: https://www.guttmacher.org/sites/default/files/factsheet/fb_contr_use_0.pdf [accessed 17.04.05] [Google Scholar]
- 14.[dataset] Centers for Disease Control [Internet] 2013–2015 National Survey on Family Growth: Public use data files, codebooks, and documentation. Atlanta, GA: Centers for Disease Control; 2016. Available from: https://www.cdc.gov/nchs/nsfg/nsfg_2013_2015_puf.htm [accessed 17.04.05] [Google Scholar]
- 15.[dataset] The National Campaign to Prevent Teen and Unplanned Pregnancy [Internet] National Survey of Reproductive and Contraceptive Knowledge dataset. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2010. Data request available from: https://thenationalcampaign.org/resource/fog-zone-data-request [accessed 17.04.05] [Google Scholar]
- 16.Harper CC, Rocca CH, Thompson KM, Morfesis J, Goodman S, Darney PD, et al. Reductions in pregnancy rates in the USA with long-acting reversible contraception: A cluster randomised trial. Lancet. 2015;386:562–8. doi: 10.1016/S0140-6736(14)62460-0. [DOI] [PubMed] [Google Scholar]
- 17.Black KI, Day CA. Improving access to long-acting contraceptive methods and reducing unplanned pregnancy among women with substance use disorders. Subst Abuse. 2016;10(Suppl 1):27–33. doi: 10.4137/SART.S34555. [DOI] [PMC free article] [PubMed] [Google Scholar]


