Abstract
Aim
To assess the clinical benefits of introducing a medical emergency team system for early medical intervention in hospital care.
Methods
This prospective analysis included all cases of medical emergency team activation during the first year after the introduction of the medical emergency team system at Chiba University Hospital (Chiba, Japan) in February 2011. The rates of in‐hospital mortality and unexpected events before and after introduction of the medical emergency team system were compared.
Results
The total number of medical emergency team activation calls was 83 (4.9 per 1,000 admissions). The activation of the medical emergency team system was requested most frequently from the general ward (56.6%) and by a physician (57.8%), with the most important reasons for activation being cardiac arrest (37.3%), breathing abnormality (33.7%), and impaired consciousness (32.5%). The most frequent medical interventions by the medical emergency team were intubation (43.3%) and oxygen inhalation (41.0%). Approximately one‐half of the patients requiring activation of the medical emergency team system were critically ill and needed subsequent intensive care unit admission. Although no significant difference was observed between the pre‐ and post‐ medical emergency team in‐hospital mortalities (2.1% versus 2.0%, respectively), the incidence rate of serious events significantly decreased (12.4% versus 6.8%, respectively; P = 0.015).
Conclusion
Most patients requiring activation of the medical emergency team system were critically ill and needed emergency treatment at the location of the medical emergency team activation, with subsequent critical care. Although the introduction of the medical emergency team system did not affect the in‐hospital mortality rate, it reduced the incidence of unexpected serious adverse events, suggesting that it may be clinically useful.
Keywords: Medical emergency team, other, rapid response system
Introduction
In contrast to the recent marked improvement in prognosis after out‐of‐hospital cardiac arrest, improvement in prognosis after in‐hospital cardiac arrest remains minimal.1, 2 Abnormal changes in vital signs are commonly observed several hours preceding a cardiac arrest.3, 4 In recent years, rapid response systems (RRS) have been introduced in hospital care, to prevent unexpected sudden changes in the patient's condition and unexpected in‐hospital cardiac arrest.5 Although the clinical benefits associated with the introduction of RRS has been evaluated using various parameters such as in‐hospital mortality, Code Blue (used to alert the whole hospital staff that a sudden cardiac arrest has occurred and resuscitation is needed) rates, and unexpected events, they remain to be established.6, 7, 8, 9, 10, 11, 12, 13
The term RRS is used to describe a whole system dedicated to provide patient safety for those in a deteriorating condition. RRS are based on four components: afferent (event detection and response triggering) component, efferent (crisis response) component, patient safety/process improvement component and governance/administrative component. An RRS team consists of either a medical emergency team (MET), mostly led by a physician being able to initiate critical care at the bedside, or rapid response team, mostly led by a nurse.14
In February 2011, we introduced the MET system, consisting mainly of physicians and nurses belonging to the department of Emergency and Critical Care Medicine. In this study, all cases of MET activation that occurred in the first year after the introduction of MET were analyzed for the patients' background, condition at the time of MET activation, and details of the medical interventions carried out. Additionally, the in‐hospital mortality rates and unexpected events before and after the introduction of the MET system were compared to assess the clinical benefits of MET.
Methods
Medical emergency team
In February 2011, Chiba University Hospital (Chiba, Japan) introduced the MET system—in addition to the Code Blue emergency call system—to address sudden in‐hospital changes in the clinical condition of patients, and simultaneously initiated the collection of prospective data. The MET system at Chiba University Hospital consists of physicians belonging to the department of Emergency and Critical Care Medicine and ICU nurses. Any hospital staff, regardless of their occupation, is allowed to activate the MET system according to pre‐defined MET activation criteria. The MET system can be activated for inpatients and outpatients, as well as any individuals within the hospital compound, including visitors, hospital staff, and vendors. The MET activation criteria are as follows: airway obstruction in need of emergent airway management (e.g., asphyxia), respiratory insufficiency, shock, drastically depressed level of consciousness, trauma, unexpected cardiac arrest, a risk of these conditions, and any other deteriorating condition that the discoverer considered in need of MET activation (Table 1). These criteria were made to identify patients who are in a deteriorating condition or are at risk of a deteriorating condition. The MET system is activated by calling a dedicated extension number directly connected to the in‐hospital personal handyphone system device carried by the attending physician of the department of Emergency and Critical Care Medicine. The MET activation call is simultaneously broadcasted to the ICU, emergency room, and physician's lounge through pre‐installed loudspeakers, to inform all MET members of the place where the unexpected in‐hospital clinical instability was identified, the patient's conditions, and any other related information. Medical emergency team members bring a bag containing pre‐specified pharmaceuticals and medical devices that are regularly stocked in the ICU to the place requested by the activation call and initiate medical practice using the nearest emergency cart. The diagnosis and treatment are carried out in parallel with attempts to stabilize the patient's condition, and subsequently determine the patient's disposition. The present study was approved by the Ethical Review Board of the Graduate School of Medicine, Chiba University.
Table 1.
Criteria for medical emergency team activation
| Airway obstruction |
| Dyspnea |
| Hypotension |
| Altered conscious state |
| Trauma |
| Cardiac arrest |
| Staff concerned that deteriorating conditions are developing |
Subjects
At Chiba University Hospital, there are 835 beds in total, including 22 ICU beds (4 cardiac, 18 medical/surgical), with 740 physicians and dentists treating a total of 1,985 outpatients and 761 inpatients daily, on average (as of fiscal year 2012).
Our subjects included all patients for whom MET activation was requested between February 2012 and January 2013. First, the number of MET activation calls per unit number of hospital admissions was calculated for this period. The following parameters were subsequently recorded for each case of MET activation: background of the patient for whom MET activation was requested (MET‐activated patients), location of the MET activation, the activator's occupation, reason for the MET activation, the patient's condition and emergency treatment given on MET arrival, the patient's disposition, and survival outcome.
The period before MET introduction (from February 2011 to January 2012) was defined as the pre‐MET period; the period after MET introduction (from February 2012 to January 2013) was defined as the post‐MET period. Data for pre‐MET period were collected retrospectively. The pre‐MET and post‐MET in‐hospital mortality rates were calculated separately for comparison, by dividing the number of in‐hospital deaths by the number of hospital admissions. The sum of the number of unexpected life‐threatening events (including airway, breathing, hemodynamic, and consciousness abnormality in which resuscitative treatment was urgently carried out) and the number of unexpected cardiac arrests—both occurring for any reason other than deterioration of the underlying disease—was defined as the number of total serious events. The pre‐MET and post‐MET incidence rates of unexpected life‐threatening events, unexpected cardiac arrests, and total serious events among in‐hospital deaths were separately calculated for comparison.
Statistical analysis
The in‐hospital mortality, as well as the incidence of unexpected life‐threatening events, unexpected cardiac arrests, and total serious events before and after introduction of MET were compared using the χ2‐test. A commercial package software, GraphPad Prism 4 (GraphPad Software Inc., San Diego, CA, USA), was used for all statistical analyses. P‐values <0.05 were considered significant.
Results
The total number of MET activation calls during the first year after the introduction of the MET system (February 2012–January 2013) was 83. Given that the total number of hospital admissions during this period was 16,844, the mean number of calls per 1,000 admissions was calculated to be 4.9.
Table 2 summarizes the background characteristics of patients requiring MET activation (mean age, 57.0 years; male, 44.6%). The most frequent underlying disease was chronic heart failure (28.9%), followed by respiratory disease (15.7%). Medical emergency team activation was requested most frequently from the general ward (56.6%) and by a physician (57.8%) (Table 3).
Table 2.
Characteristics of patients requiring medical emergency team activation
| Age, years | 57.0 (11.3) |
| Male, n (%) | 37 (44.6) |
| Inpatients, n (%) | 55 (66.3) |
| Surgical, n (%) | 34 (41.0) |
| Pre‐existing conditions, n (%) | |
| Chronic heart failure | 24 (28.9) |
| Chronic pulmonary disease | 13 (15.7) |
| Chronic liver disease | 7 (8.4) |
| Chronic renal failure | 10 (12.0) |
| Chronic brain disease | 10 (12.0) |
| Chronic corticosteroid use | 13 (15.7) |
| Pulse steroid therapy | 5 (6.0) |
| Chemotherapy | 11 (14.5) |
| Other immune suppression | 5 (6.0) |
| Diabetes | 7 (8.4) |
| Hematologic disorder | 7 (8.4) |
| Solid malignancy | 3 (3.6) |
Data are mean (standard deviation) for continuous variables.
Table 3.
Location of medical emergency team activation and activator's occupation
| Location of activation, n (%) | |
| General wards | 47 (56.6) |
| Outpatients department | 18 (21.7) |
| Computer tomography scan room | 4 (4.8) |
| Angiography suite | 3 (3.6) |
| Hallway | 2 (2.4) |
| Emergency room | 1 (1.2) |
| Operating room | 1 (1.2) |
| Dialysis room | 1 (1.2) |
| Others, inside hospital | 3 (3.6) |
| Others, in the vicinity of the hospital | 2 (2.4) |
| Caller's occupation, n (%) | |
| Physician | 48 (57.8) |
| Nurse | 19 (22.9) |
| Other | 16 (19.3) |
Table 4 shows the condition of the patients and treatment given on MET arrival. The major abnormalities in the vital signs were a decreased O2 saturation level and decreased level of consciousness. The most frequently encountered medical problems were cardiac arrest (37.3%), breathing abnormality (33.7%), and impaired consciousness (32.5%). The most frequent medical interventions by the MET were intubation (43.3%) and oxygen inhalation (41.0%). The most frequent disposition of the MET‐activated patients was ICU admission (49.4%), followed by general ward admission (30.1%). The 24‐h and 28‐day mortalities in the MET‐activated patients were 12.0% and 32.5%, respectively (Table 5).
Table 4.
Condition of patients and treatments needed on medical emergency team arrival
| Vital signs | |
| Heart rate | 99 (35) |
| Systolic blood pressure, mmHg | 115 (43) |
| Diastolic blood pressure, mmHg | 69 (27) |
| O2 saturation, % | 88 (12) |
| Respiratory rate, breaths/min | 22 (10) |
| Glasgow Coma Scale | 10 (5) |
| Medical problems, n (%) | |
| Airway abnormality | 14 (16.9) |
| Breathing abnormality | 28 (33.7) |
| Hemodynamic abnormality | 16 (19.3) |
| Consciousness abnormality | 27 (32.5) |
| Cardiac arrest | 31 (37.3) |
| Treatments, n (%) | |
| Intubation | 36 (43.3) |
| Oxygen inhalation | 34 (41.0) |
| Mechanical ventilation | 19 (22.9) |
| I.v. line insertion | 16 (19.3) |
| Fluid bolus | 8 (9.6) |
| Cardiovascular drug administration | 24 (28.9) |
| Chest compression | 31 (37.3) |
| Adrenaline administration | 27 (32.5) |
| Defibrillation | 10 (2.0) |
Data are mean (standard deviation) for continuous variables.
Table 5.
Outcome of patients requiring medical emergency team (MET) activation
| Disposition after MET intervention, n (%) | |
| General wards | 25 (30.1) |
| Intensive care units | 41 (49.4) |
| Home | 8 (9.6) |
| Death | 7 (8.4) |
| Mortality after MET call, n (%) | |
| 24‐h mortality | 10 (12.0) |
| 7‐day mortality | 18 (21.7) |
| 28‐day mortality | 27 (32.5) |
No significant difference was observed between the number of pre‐MET and post‐MET in‐hospital mortalities (calculated by dividing the number of in‐hospital deaths by the number of total hospital admissions) (pre‐MET 2.1% [331/15,514] versus post‐MET 2.0% [337/16,844], P = 0.38). Among the in‐hospital deaths, there was a non‐significant trend in the decreased incidence rate of unexpected life‐threatening events (pre‐MET 3.3% [11/331] versus post‐MET 1.5% [5/337], P = 0.14) and unexpected cardiac arrests (pre‐MET 9.1% [30/331] versus post‐MET 5.3% [18/337], P = 0.063) after the introduction of the MET system, whereas the incidence rate of total serious events (calculated as the sum of the two) was significantly decreased by the introduction of the MET system (pre‐MET 12.4% [41/331] versus post‐MET 6.8% [23/337], P = 0.015) (Fig. 1).
Figure 1.
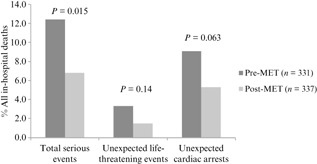
Unexpected life‐threating events and unexpected cardiac arrests among hospital‐wide deaths before and 1 year after introduction of a medical emergency team (MET) system. Unexpected life‐threatening events (pre‐MET 3.3% [11/331] versus post‐MET 1.5% [5/337], P = 0.14) and unexpected cardiac arrests (pre‐MET 9.1% [30/331] versus post‐MET 5.3% [18/337], P = 0.063) tended to decrease in the post‐MET period compared to the pre‐MET period. Total serious unexpected events were significantly decreased in the post‐MET period compared to the pre‐MET period (pre‐MET 12.4% [41/331] versus post‐MET 6.8% [23/331], P = 0.015).
Discussion
The total number of MET activation calls during the first year after the introduction of the MET system was 83 (4.9 per 1,000 admissions). Most patients requiring MET activation were critically ill and needed emergency treatment at the location of the MET activation with subsequent ICU care, including many with cardiac arrest on arrival of the MET.
The number of MET activation calls in this study (4.9 per 1,000 admissions) is smaller than the values previously reported in the USA and Europe.6, 7, 8, 9, 10, 11, 12, 13 This difference may be attributed to differences in the medical practices and MET activation criteria used, as well as differences between the MET and rapid response team. The present study showed that the patient's condition on MET arrival was highly urgent and serious in most cases (e.g., cardiac arrest, respiratory insufficiency, shock), with almost half being critically ill patients requiring urgent ICU/cardiac care unit admission after MET intervention.
Although the objective of the RRS is to improve the prognosis of inpatients by intervention prior to the occurrence of serious events, 33.7% of the MET activation calls were due to cardiac arrest. Sudden cardiac arrest preceded by no abnormality in vital signs does sometimes occur, such as in patients with acute coronary artery disease. Further investigation is needed to clarify whether the MET activation call could be made prior to the occurrence of the cardiac arrest, in any of the cases in which the MET system was activated due to cardiac arrest.
MET activation was most frequently requested by physicians at our hospital, in contrast to a report from a UK hospital showing that 83% of their MET activation calls were made by nurses.15 This difference may indicate that, in our hospital, the first person to identify sudden changes in the clinical condition of an inpatient (most probably a nurse) calls the physician in charge of the patient, instead of activating the MET system immediately. As a result, a delayed MET activation call may be made by the physician only after he/she arrives and finds it difficult to address the changes in the condition of the patient. We have held in‐hospital study sessions on the introduction of the MET system, followed by annual education seminars on addressing sudden in‐hospital clinical changes, held in every ward. The data presented in this article were obtained in the first year of the MET implementation. The continued efforts to improve education and communication are expected to change the composition of the MET activators in the future.
The MET activation criteria at our hospital are based on the signs indicating that a patient is in a serious condition. Conversely, based on previous reports that abnormalities in vital signs precede serious adverse events,3, 4 many medical institutions adopt abnormalities in vital signs as the MET activation criteria.16, 17 However, given that abnormal vital signs reportedly show a high sensitivity and a low specificity in the prediction of cardiac arrest and unexpected death,4 there is no general agreement regarding the appropriate MET activation criteria. Multiple scoring systems proposed for vital signs, such as the Modified Early Warning System18 and National Early Warning System,19 can be used as MET activation criteria to predict acute deterioration in critically ill patients. Although such vital sign scores are reported to show high specificity,20 they have not been supported by sufficient evidence at present.21, 22 Considering that the present study evaluates the data obtained during the first year of the MET implementation, further verification and assessment will be necessary regarding MET activation criteria.
The effects of the introduction of the RRS system have previously been evaluated using different outcome measures such as the total in‐hospital mortality rate, unplanned ICU admissions, Code Blue rates, and incidence of adverse events.7, 8, 9, 10, 11, 12, 13 Most of the previous reports of decreased in‐hospital mortality rate, adverse events, and out‐of‐ICU cardiac arrests were single‐center studies.23, 24, 25 A multicenter randomized study, the MERIT study, failed to show a decrease in the number of cardiac arrests, unplanned admissions to the ICU, or unexpected deaths after the introduction of a MET system.6 A meta‐analysis revealed that the incidence of out‐of‐ICU cardiac arrests decreased after the introduction of a RRS; however, no change in the in‐hospital mortality rate was observed.8 In another meta‐analysis, an increasing number of more recent reports showed a decrease in the mortality rate after the introduction of a MET system; however, the overall results indicated a decrease in the incidence rate of the out‐of‐ICU cardiac arrests and no change in the in‐hospital mortality rate.13
Similarly, in our hospital, no difference was observed between the pre‐MET and post‐MET in‐hospital mortality rate. One possible reason may be a relatively small number of MET activation calls, namely 4.9 per 1,000 hospital admissions. The cardiac arrests reportedly decreased with an increase in the MET activation calls.26, 27, 28 A low pre‐MET in‐hospital mortality of 2.1% (331/15,514), in combination with the small number of MET activation calls, may explain the observed lack of significant effect of the MET system introduction on the number of in‐hospital mortalities. Furthermore, as the in‐hospital mortality cases included cases whose resuscitation code was modified to “do not attempt resuscitation” after MET treatment, due to deteriorating condition caused by an underlying disease, a significant reduction in the in‐hospital mortality rate may be difficult to achieve by the introduction of the MET system alone. Another reason could be the fact that most MET activations were made by physicians in our hospital. This suggests that some of the activations might have been delayed, as discussed above, resulting in no significant change in mortality. A decrease in the ratio of the number of total unexpected events to the number of patients discharged following death was also observed in the present study, which may indicate that MET activations due to unexpected acute clinical deterioration—as opposed to deterioration of an underlying disease—was beneficial to patients.
Conclusion
The clinical data obtained during the first year after the introduction of the MET system in February 2012 were examined. The results suggested that the introduction of the MET system could reduce the incidence of unexpected serious adverse events. The majority of the patients requiring activation of the MET system were critically ill and needed emergency treatment at the location of the MET activation, with subsequent ICU admission. Considering that many of these patients had cardiac arrest on arrival of the MET, further assessment is necessary to optimize the activation criteria and operational protocols of the MET system in our hospital.
Conflict of Interest
None.
Acknowledgement
This work was supported by a research grant from the Health Care Science Institute in Japan. The funding body was not involved in the study or the writing of the manuscript.
References
- 1. Wissenberg M, Lippert FK, Folke F et al Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA 2013; 310: 1377–1384. [DOI] [PubMed] [Google Scholar]
- 2. Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in‐hospital cardiac arrest. N. Engl. J. Med. 2012; 367: 1912–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in‐hospital cardiopulmonary arrest. Chest 1990; 98: 1388–1392. [DOI] [PubMed] [Google Scholar]
- 4. Hodgetts TJ, Kenward G, Vlachonikolis IG, Payne S, Castle N. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation 2002; 54: 125–131. [DOI] [PubMed] [Google Scholar]
- 5. Jones DA, DeVita MA, Bellomo R. Rapid‐response teams. N. Engl. J. Med. 2011; 365: 139–146. [DOI] [PubMed] [Google Scholar]
- 6. Hillman K, Chen J, Cretikos M et al Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial. Lancet 2005; 365: 2091–2097. [DOI] [PubMed] [Google Scholar]
- 7. Konrad D, Jaderling G, Bell M, Granath F, Ekbom A, Martling CR. Reducing in‐hospital cardiac arrests and hospital mortality by introducing a medical emergency team. Intensive Care Med. 2010; 36: 100–106. [DOI] [PubMed] [Google Scholar]
- 8. Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital‐wide code rates and mortality before and after implementation of a rapid response team. JAMA 2008; 300: 2506–2513. [DOI] [PubMed] [Google Scholar]
- 9. Karpman C, Keegan MT, Jensen JB, Bauer PR, Brown DR, Afessa B. The impact of rapid response team on outcome of patients transferred from the ward to the ICU: A single‐center study. Crit. Care Med. 2013; 10: 2284–2291. [DOI] [PubMed] [Google Scholar]
- 10. Al‐Qahtani S, Al‐Dorzi HM, Tamim HM et al Impact of an intensivist‐led multidisciplinary extended rapid response team on hospital‐wide cardiopulmonary arrests and mortality. Crit. Care Med. 2013; 41: 506–517. [DOI] [PubMed] [Google Scholar]
- 11. Winters BD, Pham JC, Hunt EA, Guallar E, Berenholtz S, Pronovost PJ. Rapid response systems: A systematic review. Crit. Care Med. 2007; 35: 1238–1243. [DOI] [PubMed] [Google Scholar]
- 12. Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: A systematic review and meta‐analysis. Arch. Intern. Med. 2010; 170: 18–26. [DOI] [PubMed] [Google Scholar]
- 13. Winters BD, Weaver SJ, Pfoh ER, Yang T, Pham JC, Dy SM. Rapid‐response systems as a patient safety strategy: A systematic review. Ann. Intern. Med. 2013; 158: 417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Devita MA, Bellomo R, Hillman K et al Findings of the first consensus conference on medical emergency teams. Crit. Care Med. 2006; 34: 2463–2478. [DOI] [PubMed] [Google Scholar]
- 15. Kenward G, Castle N, Hodgetts T, Shaikh L. Evaluation of a medical emergency team one year after implementation. Resuscitation 2004; 61: 257–263. [DOI] [PubMed] [Google Scholar]
- 16. Jones D, Drennan K, Hart GK et al Rapid Response Team composition, resourcing and calling criteria in Australia. Resuscitation 2012; 83: 563–567. [DOI] [PubMed] [Google Scholar]
- 17. Psirides A, Hill J, Hurford S. A review of rapid response team activation parameters in New Zealand hospitals. Resuscitation 2013; 84: 1040–1044. [DOI] [PubMed] [Google Scholar]
- 18. Hammond NE, Spooner AJ, Barnett AG, Corley A, Brown P, Fraser JF. The effect of implementing a modified early warning scoring (MEWS) system on the adequacy of vital sign documentation. Aust. Crit. Care 2013; 26: 18–22. [DOI] [PubMed] [Google Scholar]
- 19. Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013; 84: 465–470. [DOI] [PubMed] [Google Scholar]
- 20. Cretikos M, Chen J, Hillman K, Bellomo R, Finfer S, Flabouris A. The objective medical emergency team activation criteria: A case–control study. Resuscitation 2007; 73: 62–72. [DOI] [PubMed] [Google Scholar]
- 21. Gao H, McDonnell A, Harrison DA et al Systematic review and evaluation of physiological track and trigger warning systems for identifying at‐risk patients on the ward. Intensive Care Med. 2007; 33: 667–679. [DOI] [PubMed] [Google Scholar]
- 22. Churpek MM, Yuen TC, Huber MT, Park SY, Hall JB, Edelson DP. Predicting cardiac arrest on the wards: A nested case–control study. Chest 2012; 141: 1170–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL. Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual. Saf. Health Care 2004; 13: 251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bellomo R, Goldsmith D, Uchino S et al A prospective before‐and‐after trial of a medical emergency team. Med. J. Aust. 2003; 179: 283–287. [DOI] [PubMed] [Google Scholar]
- 25. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: Preliminary study. BMJ 2002; 324: 387–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jones D, Bellomo R, DeVita MA. Effectiveness of the Medical Emergency Team: The importance of dose. Crit. Care 2009; 13: 313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shah SK, Cardenas VJ Jr, Kuo YF, Sharma G. Rapid response team in an academic institution: Does it make a difference? Chest 2011; 139: 1361–1367. [DOI] [PubMed] [Google Scholar]
- 28. Jones D, Bellomo R, Bates S et al Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit. Care 2005; 9: R808–815. [DOI] [PMC free article] [PubMed] [Google Scholar]


